Abstract
Background:
With climate change, mean annual air temperatures are getting hotter and extreme weather events will become more and more common in most parts of the world.
Objectives:
As part of the EU funded project HEAT-SHIELD we conducted a systematic review to summarize the epidemiological evidence of the effects of global warming-related heat exposure on workers’ health and productivity.
Methods:
Three separate searches, focused, respectively, on: i) heat-related illness (HRI), cardiovascular, respiratory and kidney diseases; ii) traumatic injuries; and iii) vector-borne diseases or vectors distribution, were conducted in PubMed. EMBASE was also consulted to retrieve relevant studies focused on the health effects of climate change. A fourth search strategy to assess the effects on work productivity was conducted both in PubMed and in the SCOPUS database.
Results:
A significant proportion of studies reported findings regarding the Mesoamerican nephropathy issue. This is a disease occurring especially among young and middle-aged male sugarcane workers, without conventional risk factors for chronic kidney disease. For injuries, there is a reversed U-shaped exposure-response relationship between Tmax and overall daily injury claims. Outdoor workers are at increased risk of vector-borne infectious diseases, as a positive correlation between higher air temperatures and current or future expansion of the habitat of vectors is being observed. As for productivity, agriculture and construction are the most studied sectors; a day with temperatures exceeding 32°C can reduce daily labour supply in exposed sectors by up to 14%.
Conclusions:
The present findings should inform development of further research and related health policies in the EU and beyond with regard to protecting working people from the effects of workplace heat during climate change.
Key words: Climate change, heat-related illness, occupational diseases, occupational injury, productivity, vector-borne infectious diseases
Abstract
«Cambiamento climatico ed effetti sulla salute e sulla produttività dei lavoratori: revisione della letteratura sugli effetti dell’esposizione al calore nei luoghi di lavoro».
Introduzione:
Negli ultimi decenni si è registrato un importante aumento della temperatura atmosferica media e degli eventi meteorologici estremi.
Obiettivi:
Nell’ambito del Progetto Europeo HEAT-SHIELD abbiamo condotto una revisione sistematica allo scopo di valutare gli effetti del riscaldamento globale sulla salute e sulla produttività dei lavoratori.
Metodi:
Abbiamo utilizzato tre diverse strategie di ricerca, interrogando PubMed, per indagare, rispettivamente: i) il rischio di sviluppare malattie da calore, malattie cardiovascolari, respiratorie e renali; ii) il rischio di infortuni causati da eventi meteorologici estremi; iii) l’estendersi della presenza di vettori di malattie infettive nuove o di nuovo presenti. Inoltre abbiamo consultato anche il database EMBASE per valutare gli effetti dei cambiamenti climatici sulla salute dei lavoratori. Una quarta strategia, condotta sia su PubMed che su SCOPUS, ci ha permesso di esplorare il tema della produttività.
Risultati:
Di rilevante importanza è il problema della nefropatia mesoamericana, una condizione che interessa soprattutto i lavoratori maschi impiegati nella produzione della canna da zucchero in America Centrale. In generale, sembra esistere una relazione dose-risposta a forma di U rovesciata tra Tmax e infortuni. I lavoratori hanno un rischio aumentato di contrarre malattie infettive trasmesse da vettori poiché esiste una correlazione positiva tra temperature più elevate e l’espansione attuale o futura dell’habitat dei vettori. Per quanto riguarda la produttività, l’agricoltura e le costruzioni sono i settori più studiati; temperature superiori a 32°C possono ridurre la produttività fino al 14%.
Conclusioni:
I risultati della revisione potranno essere utili ai decisori politici per pianificare adeguatamente le azioni di salvaguardia della salute e della produttività dei lavoratori, messe a repentaglio da condizioni sempre più frequenti di disagio da caldo intenso e persistente.
Background
The risks of heat exposure on human health are well known. The Italian physician Bernardino Ramazzini was probably the first, already in the 17th century, to report in his book “De Morbis Artificum Diatriba” on the ailments suffered by workers excessively exposed to heat stress. Bakers, he wrote: “…are afflicted by serious illnesses; in summer in particular, when they put the bread in the ovens and take it out, you can see them dripping with sweat…. I have observed that, in crowded cities, these workers fall ill more often than other workers”; as for soap-makers: “the ailments that afflict these workers are caused by the toil they endure day and night and the excessive heat from the fire that is constantly burning in the workshop. Indeed, it is so hot that they often have to go out for a moment to take a breath of fresh air….” (80).
At the beginning of the 20th century, J. S. Haldane reported the results of experiments evaluating the influence of high air temperatures on the health status of Cornish miners, and on subjects placed partly in incubating room at the Lister Institute in London, in a warmed room at the Physiological Laboratory in Oxford, and in a Turkish bath (39). He observed an increase in the pulse rate of 36 beats for each 1°C, the occurrence of hyperpnoea from 39.4°C and a general feeling of exhaustion and discomfort when wet-bulb thermometer exceeds 25.5°C, when hard work becomes impracticable. In 1914 Luigi Carozzi wrote that when the “external temperature is higher than body temperature, and the air is saturated with moisture, the evaporation is hindered, and a heatstroke may occur if internal temperature reaches 40.5°C” (17). Moreover, he underscored the effects on workers productivity, as he reported strikes in the textile and mining industries due to the harsh conditions posed by working in a hot, humid environment (16). A few decades later, in the 1960s, Cyril H. Wyndham described the health hazards and the effects on productivity posed by heat stress on South African gold mine workers (98). The occurrence of heat-related illness is maximum when the high temperatures are accompanied by high humidity levels, a condition which determines an impairment of the human thermoregulatory system.
Workers involved in moderate- or high-intensity activities in hot locations during the hot season are prone to heat-related health problems, as physical work activities create intra-body heat production, which adds to the environmental heat stress. A growing body of scientific evidence indicates that the exposure to excessively high heat levels is already resulting in excess morbidity and mortality in the general population, particularly among the elderly (23, 93, 96, 97). Although workers in hot locations are also a vulnerable group for heat exposure and climate change, the impact of climate change on workers’ health has not been extensively investigated. Guidelines and heat management systems to counteract increasing heat exposure in the occupational settings are still far from appropriately being implemented in at-risk regions (63). In addition, several studies have confirmed significant loss of productivity due to excessive heat exposure (53-55, 73).
With climate change, mean annual air temperatures are getting hotter in most parts of the world. Since thermometer-based observations began, the year 2015 and the period 2006-2015 were the warmest year and decade on record respectively. The global average surface temperature has risen at an average rate of 0.07°C per decade since 1901 (3). During the same period extreme weather events, such as heat waves, droughts, floods, cyclones and wildfires, have become more and more common, according to the findings from the Fifth Assessment Report of the Intergovernmental Panel on Climate Change (IPCC), and impacts from recent climate-related extremes revealed, with very high confidence, “significant vulnerability and exposure of some ecosystems and many human systems to current climate variability” (91). For the 21st century, climate models have projected further increases of between 0.3 and 1.7°C for the lowest greenhouse gas emissions scenario adopted by the Intergovernmental Panel on Climate Change for its fifth Assessment Report (RCP2.6), and between 2.6 and 4.8°C for the highest emissions scenario (RCP8.5) (29). This will represent a public health issue, especially considering the ongoing process of the European working population ageing (the proportion of workers aged ≥50 years has markedly increased, from 24% in 2005 to 31% in 2015, when, for the first time in many years, the proportion of workers pertaining to this age group has surpassed that of the younger cohort (27)), which is resulting in more workers at greater risk of heat stress.
Objectives
The present study has been conducted as part of HEAT-SHIELD, a project funded by the European Union under the Horizon 2020 Framework Programme for Research and Innovation (https://www.heat-shield.eu/), dedicated to address the negative impact of increased workplace heat stress on the health and productivity of five strategic European industries: manufacturing, construction, transportation, tourism and agriculture. We performed a systematic review with the aim to summarize the epidemiological evidence of the effects of climate change, with a special focus on high temperatures and heat waves, on workers’ health and productivity, in order to better inform health policies in the EU and beyond.
Methods
Brownson et al. distinguished three types of scientific evidence for public health practice (14); the aim of our review was to provide Brownson’s type 1 scientific evidence, in that our objective was to identify size and severity of the existing relationship between heat related to climate change and workers’ health and productivity.
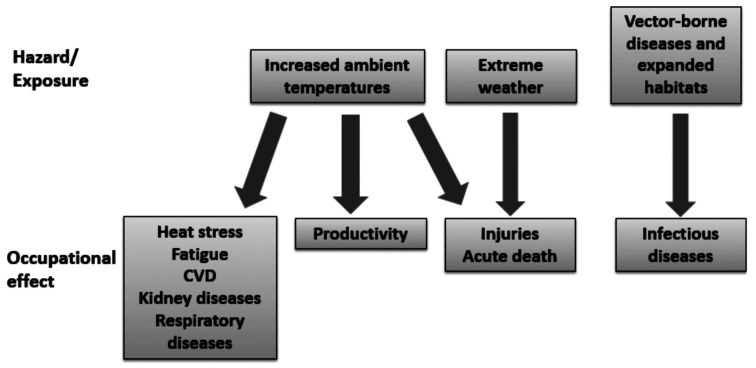
To retrieve the relevant scientific literature on the effects of workplace heat on occupational health, it was decided to carry out three separate searches, one for each of the main health effects identified in a logical framework derived by the conceptual model produced by Schulte et al., with health outcomes varying depending on the exposure types (85, 86). These three search strategies were conducted in PubMed using pre-specified search terms and were focused on: i) heat-related illness (HRI), cardiovascular, respiratory and kidney diseases; ii) traumatic injuries and acute death; iii) vector-borne diseases or vectors distribution; they are shown in Appendix Table 1. To complement the search in PubMed, the EMBASE database was consulted, using a more concise search strategy [(‘climate change’/exp OR ‘climate change’) AND worker* AND (‘health’/exp OR health OR injur* OR disease*)], to assess climate change effects on workers’ health.
A fourth search strategy was conducted to retrieve the effects of climate change on work productivity. Since both PubMed and EMBASE databases are focused on biomedical topics, and generally do not include studies based solely on economics aspects, in this case it was decided to also conduct the search strategy in SCOPUS, a database which contains abstracts of academic journal articles with a broader focus (Appendix Table 2). In figure 1 the analytic framework developed to guide the selection of studies addressing the topics of interest is shown. An iterative process was used to build the search strategies, as there was no way for us to anticipate some concepts prior to encountering them while performing the review. Therefore, while the review of the first two topics of interest was carried out systematically, applying a modified versions of the PICO scheme (83), using a search syntax comprising three categories ( i) Exposure ii) Setting ; iii) Health outcome), for the third and the fourth strategies it was decided to assess the distribution of hazards, and to opt for a scoping review, instead. During the review process, it was acknowledged that the increased risk of vector-borne infectious diseases for outdoor workers has not been studied extensively yet. The topic of productivity is mainly assessed by econometric studies, which was not the focus of our analysis. When building the search syntax, for prompt identification of studies conducted in the occupational setting, we made reference to the strings developed precisely for this purpose by Mattioli et al. (67).
Figure 1.
Logical framework used to guide the study selection. Modified from Schulte et al, 2009 (86) and Schulte et al, 2016 (85)
Inclusion criteria were:
- Studies published from 01/01/2000 until 16/06/2017
- Studies focused on heat-related illness and injuries among workers or on workers’ productivity with special attention to the construction and agricultural sectors.
Exclusion criteria:
- Experimental studies (e.g. studies involving subjects performing exercise in climatic chambers), under controlled conditions of heat stress
- Studies assessing the effects on subgroups whose exposure to heat is determined by industrial processes (e.g. workers of foundries or glass mills) or by environmental conditions potentially not related to climate change (e.g. underground miners, firefighters), unless the unfavourable environmental conditions described were explicitly correlated to the heat conditions that climate change brings
- Studies devoted solely to the analysis of the health effects of natural disasters (e.g. Hurricane Katrina)
- Studies assessing the impact of workplace heat on the production, rather than on workers’ productivity at the individual level
- Editorials, commentaries, letters to the editor.
A two-step selection process was applied: relevant studies were selected by screening first the titles and then the abstracts; if the information in titles or abstracts was not sufficient to decide on inclusion or exclusion of the study, the full-text was retrieved and evaluated. The study selection process was done twice, independently by two researchers (ML and AB), to ensure that the predefined selection criteria were met. Disagreements about eligibility were resolved through discussion. Information on the selected studies was extracted by one reviewer based on the following items: source (first author and year of publication), study design, year of publication, country/region considered, study population, heat-exposure index employed, outcome evaluated and association measures employed (incidence rate ratio, odds ratio, proportions comparison) and main findings (Appendix Table 3 and Appendix Table 4).
Results
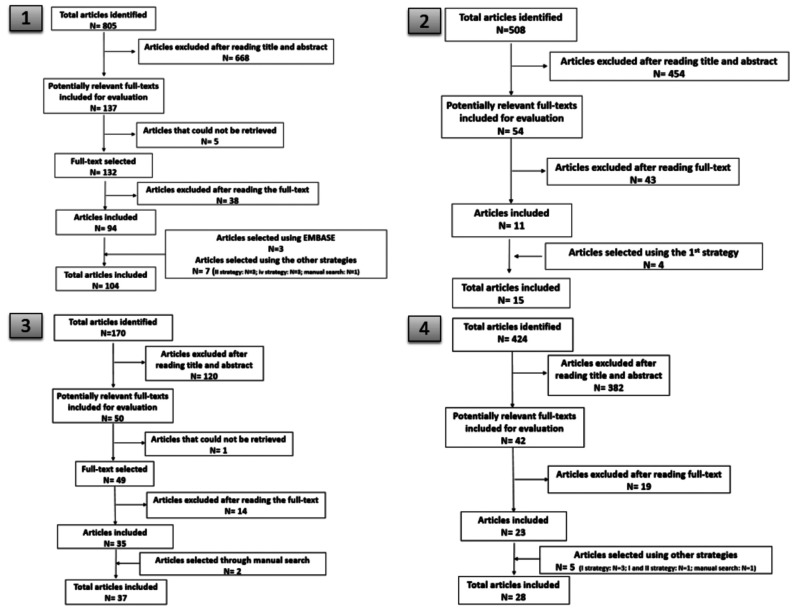
Using PubMed, the first search, focused on heat-related illness, cardiovascular, respiratory and kidney, diseases, resulted in 805 articles. Based on titles and abstracts, the full text of 132 potentially relevant articles was retrieved and reviewed, whereas 5 articles could not be retrieved. This resulted in 94 articles, and seven additional papers were included manually or using other strategies, for a total of 101 papers. Using EMBASE, three additional studies were retained: two studies (a case series and a narrative review, respectively) on the impact on kidney diseases in agricultural workers (18, 79) and one cross-sectional study focused on the mental health impact of recently observed patterns of climate change (26).
The second search, focused on traumatic injuries and acute death, resulted in 508 articles. Based on titles and abstracts, the full text of 54 potentially relevant articles was retrieved and reviewed. This resulted in 11 articles, and four additional papers were selected using the other strategies (total articles selected: 15).
The third search, focused on vector-borne diseases or vector distribution, resulted in 170 articles. Based on titles and abstracts, the full text of 50 potentially relevant articles was retrieved and reviewed, whereas 1 study could not be retrieved. The review resulted in a total of 35 articles, and two additional papers were selected manually (total articles selected: 37).
The fourth search strategy, focused on workers’ productivity, when conducted in PubMed, resulted in 424 articles. Based on titles and abstracts, the full text of 42 potentially relevant articles was retrieved and reviewed. The review resulted in a total of 23 articles, and five additional papers were selected (manually or using other strategies), for a total of 28 articles selected. When conducted in the SCOPUS database, the fourth strategy resulted in 380 articles. Based on titles and abstracts, the full text of 21 potentially relevant articles was retrieved and reviewed. This resulted in a total of 9 articles. In total, combining the search conducted in PubMed with the search in SCOPUS, 36 relevant studies focused on workers’ productivity were retrieved. In figure 2 and figure 3 the flow charts of study selection are depicted.
Figure 2.
Publication selection process for the first three search strategies conducted in PubMed and EMBASE and the fourth in PubMed
Figure 3.
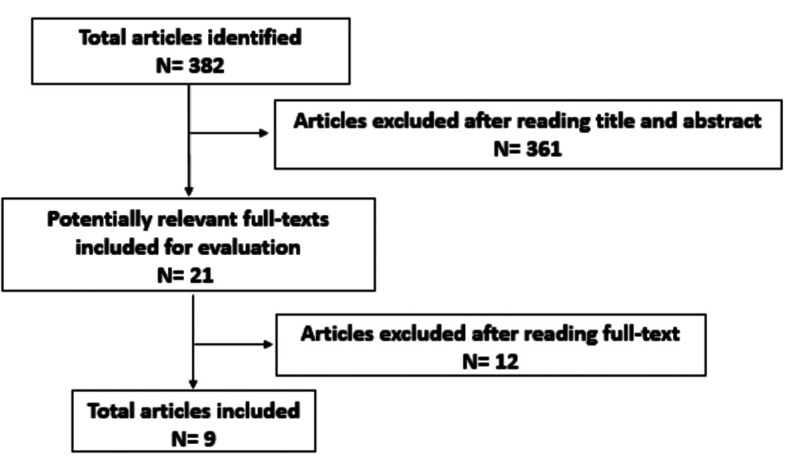
Article selection process for the fourth search strategy in SCOPUS
In table 1 the studies selected are reported by study design. One fifth (N=39; 23.6%) were cross- sectional studies. Other common study designs were simulations based on climate driven models (22; 13.3%) (these represented the 28.8% of all relevant studies assessing the impact on vector-borne diseases or vector distribution and on labour productivity), within-group comparisons for the evaluation of physiological parameters such as body temperature, body weight change, heart rate, urinary specific gravity, and fluid intake at start, middle, and end of shift (mostly before-after studies without control group) (N=16; 9.7%), ecological (N=14; 8.5%) or case reports or case series (N=12; 7.3%). The studies employing more robust study design such as case-crossover, cohort or case-control, were relatively few (table 1). While in the years 2000-2004 no review was produced on any of the topics of interest, in the periods 2005-2008 and 2009-2012 two and ten narrative reviews, respectively, were published. In the last period examined, from 2013 until the first half of 2017, the number of reviews addressing the effects of climate change on workers’ health and productivity increased, as 14 narrative reviews and 9 systematic reviews were published.
Table 1.
Selected papers reported by study design
| Type of study design | N | % |
| Cross-sectional | 39 | 23.6 |
| Narrative/scoping review | 26 | 15.8 |
| Simulation based on climate driven model | 22 | 13.3 |
| Within-group comparison (e.g. physiological parameters monitoring) | 16 | 9.7 |
| Ecological | 14 | 8.5 |
| Case series/case report | 12 | 7.3 |
| Case surveillance | 9 | 5.5 |
| Systematic review | 9 | 5.5 |
| Case-crossover | 5 | 3.0 |
| Cohort | 4 | 2.4 |
| Time-series | 3 | 1.8 |
| Case-control | 2 | 1.2 |
| Cross-sectional with nested case-control analysis | 1 | 0.6 |
| Econometric model | 1 | 0.6 |
| Physiological parameters monitoring and productivity | 1 | 0.6 |
| Time series analysis/case-crossover | 1 | 0.6 |
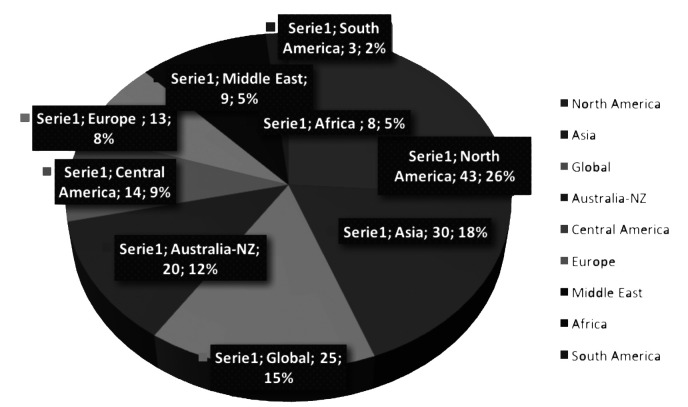
The majority of studies were conducted in North America (N=43; 26%), Asia (N=30; 18.2%), Australia/New Zealand (N=20; 12.1%), Central America (N=14; 8.5%) or Europe (N=13; 7.9%) (figure 4).
Figure 4.
Geographical distribution of the selected papers
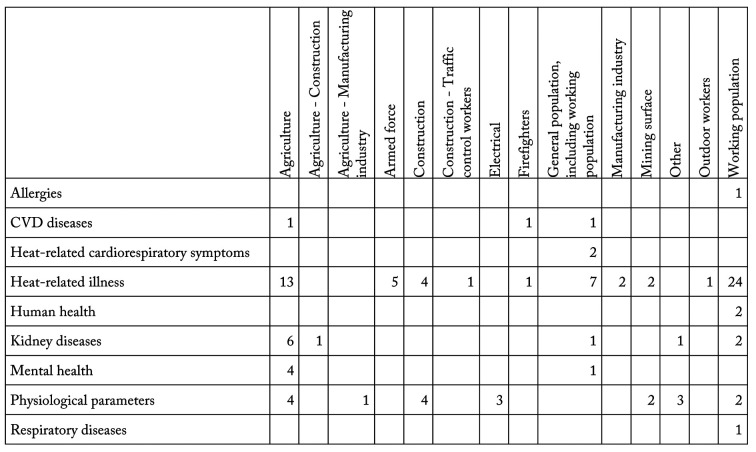
In table 2 the number of selected publications is reported by specific outcome assessed per each search strategy. The first retrieved studies assessed mainly the impact on heat-related illness (N=60; 57.7%), physiological parameters (N=19; 18.3%), or kidney and urinary diseases (N=11; 10.6%). A significant proportion focused on the mental health impact (N=5; 4.8%) of recently observed patterns of climate change. Only three studies assessed the effects on cardiovascular diseases, and only one evaluated the effects on acute respiratory problems.
Table 2.
Selected publications by specific outcome assessed using each search strategy
| N | %* | |
| Search strategy 1 | ||
| Heat-related illness | 60 | 57.7 |
| Physiological parameters | 19 | 18.3 |
| Kidney diseases and urinary diseases | 11 | 10.6 |
| Mental health | 5 | 4.8 |
| Cardiovascular diseases | 3 | 2.9 |
| Heat-related cardiorespiratory symptoms | 2 | 1.9 |
| Human health | 2 | 1.9 |
| Allergies | 1 | 1.0 |
| Respiratory diseases | 1 | 1.0 |
| Search strategy 2 | ||
| Injuries | 15 | 100.0 |
| Search strategy 3 | ||
| Vector-borne diseases | 17 | 45.9 |
| Communicable diseases | 12 | 32.4 |
| Vectors distribution | 8 | 21.6 |
| Search strategy 4 | ||
| Productivity | 36 | 100.0 |
* The proportion of papers focusing on each specific outcome out of the total papers selected per each strategy is shown.
The majority of papers retrieved using the first, second and fourth strategies (80/129; N=62.0%) considered all groups of workers, especially when the source of data is represented by administrative databases, e.g. Adam-Poupart et al, 2015 (1), or Arbury et al, 2014 (7). Those working in agriculture/forestry were taken into consideration by over one fourth of studies included (N=37; 28.7%), and construction workers were the target population of 14 publications (10.8%) (in table 3 the working groups targeted by the selected papers are shown by search strategy).
Table 3.
Working groups targeted by the selected papers by search strategy
| N | % | |
| First strategy | ||
| Population group | ||
| Working population | 32 | 30.8 |
| Agriculture | 28 | 26.9 |
| General population, including working population | 12 | 11.5 |
| Construction | 8 | 7.7 |
| Armed force | 5 | 4.8 |
| Mining | 4 | 3.8 |
| Electrical | 3 | 2.9 |
| Firefighters | 2 | 1.9 |
| Manufacturing industry | 2 | 1.9 |
| Agriculture - Construction | 1 | 1.0 |
| Agriculture - Manufacturing industry | 1 | 1.0 |
| Construction - Traffic control | 1 | 1.0 |
| Outdoor workers | 1 | 1.0 |
| Other | 4 | 3.8 |
| Second strategy | ||
| Population group | ||
| Working population | 9 | 64.3 |
| Construction | 2 | 14.3 |
| Agriculture | 1 | 7.1 |
| General population, including working population | 1 | 7.1 |
| Manufacturing industry | 1 | 7.1 |
| Firefighters | 1 | 7.1 |
| Third strategy | ||
| Population group (excluding papers focusing on animals, vectors, Infectious agent) | ||
| General population, including working population | 17 | 77.3 |
| Agriculture | 1 | 4.5 |
| Humans, animals and vectors | 1 | 4.5 |
| Working population | 1 | 4.5 |
| School workers | 1 | 4.5 |
| Fish market workers | 1 | 4.5 |
| Fourth strategy | ||
| Population group | ||
| Working population | 23 | 63.9 |
| Agriculture | 5 | 13.9 |
| Outdoor workers | 2 | 5.6 |
| Manufacturing industry | 2 | 5.6 |
| Agriculture - Construction | 1 | 2.8 |
| Construction | 1 | 2.8 |
| Other | 1 | 2.8 |
| General population, including working population | 1 | 2.8 |
First strategy
In total, as far as the first search strategy is concerned, the majority of papers selected (60/104) were focused on HRI, whereas nearly one fifth assessed the thermophysiological effect on workers. Studies that evaluated HRI are mainly of two types. The first type (N=16) made use of data drawn from administrative databases (e.g. emergency department data (N=7) (32-34, 42-44, 82), workers’ compensation claims (N=6) (2, 13, 37, 89, 99, 101), or hospital discharge records (N=3) (42-44)) and of a standard definition of heat-related illness, generally based on the International Classification of Diseases, Ninth or Tenth Revision, Clinical Modification (ICD9 CM codes 992 and ICD10 codes T67, V93.2, X30 and X32). Some of these studies (N=6) took the lag effect into account when analysing the health effects of heat (2, 13, 32, 37, 82, 89), however the lag times considered vary. The only two studies that analysed the effect of heat-waves are comprised in this group (99, 101). Six out of these 16 studies did not use heat exposure indicators to examine the association between heat or heat-waves and HRI, implicitly considering the causal relationship: in these cases the analysis was mainly focused on the different occupational categories, age and gender. In the 10 studies that used heat exposure indicators, seven used the Daily Maximum Temperature, one used the Wet-Bulb Globe Temperature (WBGT), one the average annual summer temperature (Tmax) and the remaining study used the Apparent Temperature.
In the second type of study, the sources of data were represented by questionnaire surveys or interviews. The occurrence of HRI was generally based on the self-reported subjective symptoms in the workers. The list of symptoms examined varied; in some cases, particular attention was paid to the renal function, in other cases the questionnaire had open questions and the workers were free to report whichever symptom they needed to report and symptoms were a posteriori grouped by organ system. Two of these studies considered the lag effect (in both cases it was 0). Heat exposure indicators were used in 11 out of 18 studies: in eight studies the WBGT was measured, one used both the hourly humidity and the hourly maximum temperature, another both the mean maximum temperatures and the maximum heat index.
The physiological parameters generally assessed to examine heat stress and dehydration include body temperature, fluid intake, body weight change, urinary specific gravity and heart rate. A significant proportion of articles retrieved (N=11) dealt with genitourinary disorders, in particular kidney injury, chronic kidney disease and urolithiasis. Six out of 11 of these articles reported findings from studies conducted in Central America, where an increased incidence and prevalence of chronic kidney disease has been observed since the early 2000s, particularly in Nicaragua (18, 59, 78, 95), Costa Rica (20) and El Salvador (36, 74). The disease occurs especially among young and middle-aged male sugarcane workers, without conventional risk factors such as diabetes or hypertension. Since the aetiology is still unknown, the label “Chronic Kidney Disease of unknown aetiology” (CKDu) is being used in the scientific literature. Another label is “Mesoamerican nephropathy”. The exposure to increased temperatures, dehydration and exposure to certain agrochemicals are thought to be the most important risk factors associated with its occurrence.
As for mental health, farmers seem to be at higher risk of developing depression, anxiety and other mental health problems, including suicide, on account of drought-related pressures (25, 26, 40, 41, 76).
The number of papers retrieved using the first search strategy is shown in table 4, reported by specific working group and outcome assessed. In Appendix Table 5, the papers selected using the first search strategy are listed.
Table 4.
Number of papers retrieved using the first search strategy by specific working group and outcome assessed
Second strategy
Six out of the included fifteen studies that assessed the effects of heat on the occurrence of occupational injuries did not allow to draw a quantitative synthesis of the results: four were systematic reviews not homogeneous in the methodology and two were descriptive studies. Nine studies made use of association measures, e.g. incidence rate ratio (N=3), or odds ratio (N=1). Seven studies made use of workers’ compensation claim data (1, 37, 68, 81, 88, 99, 100), one of hospital discharge records (71), and one of a questionnaire survey (90). The lag effects were taken into account when assessing the impact of increased temperatures, but not when the effects of heat-waves were assessed. This is because the definition of heat-wave per se does include the notion of conditional lag time. The most common definition is that of 3 or more days of maximum temperature in excess of 35°C. Alternatively, the following are used: 5 or more days of maximum temperature in excess of 35°C or 3 or more days of maximum temperature in excess of 40°C (81, 99).
In general, the included studies showed a positive correlation between heat indices and injury occurrence. A reversed U-shaped exposure-response relationship between Tmax and overall daily injury claims is apparent (71, 100). Furthermore, in a case-crossover study, McInnes et al. (68) reported that the odds of injury increased by 1% for each 1°C increase in daily minimum temperature registered during the night before the day of injury. In Appendix Table 6 the papers selected using the second search strategy are listed.
Third strategy
The increased risk of infectious diseases for workers on account of climate change has not been thoroughly assessed. Outdoor workers are considered at increased risk for schistosomiasis (10) and malaria (102) in China, dengue in Japan and Taiwan, leishmaniasis in Colombia (10) and West Nile Virus in Canada (103). The unusually warm winter of 2006-2007 supported vole population growth and contributed to the resurgence of leptospirosis in Germany among seasonal strawberry harvesters from Romania, Slovakia, and Poland (22). Electricity and pipeline utility workers are thought to be at increased risk of infection with Lyme Disease in the United States (9). Also in the Czech Republic the increasing trend of mean air temperatures found during the last three decades, most pronounced in the spring and summer months, was put in correlation with the highest activity of Ixodes ricinus ticks (21), and a simulation based on a climate driven model demonstrated that the habitat suitable for the distribution of I. scapularis in the Texas-Mexico transboundary region will remain relatively stable until 2050 (30).
The studies showed, in general, a positive correlation between higher air temperatures and current or future expansion of the habitat of vectors. Alimi et al. reported that altitude, annual precipitation and temperature are influential in both current and future models (4). Rift Valley fever outbreaks occurred after months of abnormal rainfall in Eastern and Southern Africa. Chikungunya outbreaks occurred in conditions of anomalous heat and drought in Eastern Africa. In Southeast Asia, such outbreaks were positively correlated with higher temperatures and rainfall (6).
Another infectious disease that is resurging on account of unusually warm weather or more frequent weather events (typhoon, droughts) is fascioliasis, a foodborne trematode infection caused by Fasciola hepatica and Fasciola gigantica. According to a simulation based on a climate driven model, the season suitable for the development of Fasciola hepatica in the environment will possibly be extended by up to four months in northern Europe; for southern Europe the risk will increase during the winter months (15). Tick-borne encephalitis virus is also on the rise (the northward expansion of I. ricinus has been well-documented in Scandinavia). Expansions have also been observed in African ticks (60), Crimean- Congo haemorrhagic fever (35) and enteric diseases such as campylobacteriosis, salmonellosis, giardiasis and cryptosporidiosis (56, 57).
In Appendix Table 7 the papers selected using the third search strategy are listed.
Fourth strategy
Generally, work hours loss is used as a proxy for labour productivity loss. A day with temperatures exceeding 32°C can reduce daily labour supply in exposed sectors by up to 14% (45). In Australia workers carried out on average one hour less work per day when temperatures exceeded 37°C (compared with days in which temperature is below 30°C), as workers self-paced to maintain thermal comfort. Heat-related health risks increase when work is “externally paced” (41). Approximately one-third of baseline work productivity can be lost in physically demanding jobs when working at 40°C (87). In India, at WBGT>26°C the hourly number of rice bundles collected by farm workers was reduced approximately 5% per °C of increased WBGT (84). In the USA, at daily maximum temperature >29.4°C, workers in industries with high exposure to climate reduced daily time allocated to labour by as much as one hour. Almost all of the decrease in time allocated to labour happened at the end of the day (104). When subjects are dehydrated, productivity is reduced (12, 19, 52). Agriculture and construction are the most studied sectors (5, 12, 19, 58, 61, 69, 72, 84).
In Appendix Table 8 the papers selected using the fourth search strategy are listed.
Discussion
The physiological mechanisms of extreme heat on human health have been well documented. Many experimental studies (e.g. climatic chambers, trials, workplace simulation studies) have proved that working in hot environments can increase the risk of injury. While those studies are at an individual level, there is lack of heat-injury evidence at a population level, where mostly ecological and observational studies have been conducted. After assessing the evidence from both individual and population level studies, we can confirm the heat-injury association. Given the different characteristics of the data sources and of the heat exposure indicators used in the analysed studies it is not easy to further synthesize the results. However, the present findings confirm the relationship between high workplace heat levels and health effects in workers, even in younger age groups. The majority of studies employed a weak design (e.g. cross-sectional, case series) which does not allow to draw definitive conclusions. With regard to heat-related illness and injury, the data sources most used to conduct large, robust studies are workers compensations claims, emergency department data or hospital discharge records. Studies based on these data sources often employ heat indices such as the daily maximum temperature to assess the impact on workers’ health. These are generally ecological studies, where the exposure is measured at the group, not at the individual level. On the contrary, the WBGT is the most frequently measured index employed by ad hoc studies. Studies conducted to assess the association between heat exposure and acute injuries either considered the impact of heat-waves, or of increased temperatures the day of the injury, and/or the climate conditions in the previous days, taking into account the lag effect. The effects of high temperatures are generally assessed, whereas that of heat-waves currently appear to be the most neglected.
The EU strategy on adaptation to climate change supports action aimed at making Europe more climate-resilient by promoting greater coordination and information-sharing (28). Meteorological early warning systems, timely public and medical advice, and ensuring that health care and social systems are ready to act are among the action recommended by the Health Action Plan, a product of EuroHEAT project on improving public health responses to heat-waves and extreme weather events, co-funded by the European Commission (66). Almost all countries have their own heat stress management guidelines in place. Currently, heat prevention policies mainly focus on the impact of extreme heat on occupational health. However, heat appears to be a silent killer. As a matter of fact, evidence has shown that the heat-injury relationship is a reversed U-shaped curve: work-related injuries start to increase with the increase of maximum temperature when temperatures are still not too high. Furthermore, considering that heat stress is affected by external heat (weather-related heat and machine-generated heat), as well as by internal heat (physical activity) and clothing, some workers may still be at high risk of injury even under mild heat stress conditions. The evidence we found regarding the health effects on construction workers is surprisingly scarce, and we have not found studies targeting susceptible workers, such as those affected by cardiovascular or respiratory chronic diseases, who are particularly at risk of suffering the worst consequences.
The kidney disease affects also countries and occupations not currently categorised among those affected by the problem of the CKDu, suggesting that future research continues to search for causes and evaluate the condition particularly among outdoor workers directly exposed to sunlight in the summer months, even in other areas of the world (e.g. seasonal tomato harvesters in Italy) currently still not considered at-risk.
Since the evidence on the effects of climate change on vector-borne infectious diseases is currently still very scarce with reference to the working population, it was decided to focus the analysis on the increased risk of infections in general, and to also consider as possible effect of climate change the altered distribution of vectors. In this case, the conclusion that outdoor workers will experience an increased risk of developing this type of health outcomes was made by deductive reasoning, given the present and future expansion of vectors’ habitats. A recent study suggested that climate change and the increasing frequency of extreme events such as desert dust storms are significantly changing the microbial communities of our soils, moving entire microbial communities (bacteria and fungi), including organisms which are extremely resistant and able to survive in different environments far away from their origins (94). A recent overview of current climate change-infectious diseases research indicated that climate change contribution results may be underestimated from the failure to account for co-factors, such as the human-induced snail elimination in the case of schistosomiasis and chemotherapy effects (62). Furthermore, climate change may also affect the pathogens’ life cycle stages within vectors, the incubation period duration, as well as vector-human interactions. In the meantime, while we were writing this paper, the first potential cases of occupational malaria among migrant seasonal farmers were being notified in Italy (105).
For the assessment of the impact on vector-borne diseases or vector distribution, and on labour productivity, the evidence is largely based on climate driven model simulations. This means that to draw definitive conclusions we must rely on the precision of baseline estimates. In addition to the reduction of afternoon working hours loss in hot days and the reduction of work efficiency, days lost due to heat-related illnesses/injuries result in productivity losses as well.
The present study has several limitations that need to be commented on. The first is that mortality data, on which health surveillance systems are often based, are used to assess the impact of heat on population health. However, in the working population the increased mortality risk is only a small part of the health impact. The second limitation is that important health outcomes (e.g. mental health problems) were not assessed, or were only briefly mentioned. Finally, the topic of productivity loss was not exhaustively treated: the effects were measured as working hours loss, but the decreased production output and the quality of the products were not assessed.
Nonetheless, the results of our systematic review are helpful to inform continued search and development health policies, to protect workers from current and future heat exposures as climate change increases the problems. The challenges from heat exposure to the health and productivity of workers are significant problems already in tropical areas, and will become more and more common also in EU countries. The workforce in Italy is particularly at risk given the country’s geographic and meteorological conditions; however, no specific study has been carried out so far, even if many heat-related deaths, mainly regarding agricultural and construction workers, appeared in the news in recent years (particularly in 2015) (48). Within the HEAT-SHIELD Project, the intention in the near future is to carry out studies to assess the effectiveness of several public health interventions in mitigating the health effects of climate change, and to assessing the adaptation and translation of such interventions in Italy and other Mediterranean countries.
Appendixes
Appendix Table 1.
Search strategies employed in PubMed to identify scientific literature focused on the health effects of climate change
| 1. Search strategy to identify publications focused on hea^related illness, cardiovascular, respiratory and kidney diseases | ||
| #1 | It identifies hazards/exposures | ("air temperature" OR "climate change" OR "climate variability" OR "global warming" OR heat OR "hot temperature" OR "heat wave*") |
| #2 | It identifies the occupational setting | ("occupational diseases"[MeSH Terms] OR "occupational health"[TW] OR "occupational exposure"[MeSH Terms] OR "occupational medicine"[MeSH Terms] OR "occupational risk"[TW] OR "occupational hazard"[TW] OR "Industry"[Mesh:noexp] OR "construction industry"[MeSH Terms] OR agriculture[MeSH Terms] OR "occupational group"[TW] OR "work: related" [Al l Fields] OR "air pollutants, occupational"[MeSH Terms] OR "working environment"[TW] OR worker*[TW]) |
| #3 | It identifies the outcomes | (cardiovascular OR renal OR respiratory OR kidney OR dehydration OR fatigue OR "heat stress" OR syncope OR faint* OR heatstroke OR exhaustion OR mortality OR morbidity) |
| Overall search strategy | #1 AND #2 AND #3 NOT animal* | |
| 2. Search strategy used to identify publications focused on traumatic injuries and acute death | ||
| #1 | It identifies hazards/exposures | ("air temperature" OR "climate change" OR "climate variability" OR "global warming" OR heat OR "hot temperature" OR "heat wave*" OR flood* OR landslide* OR storm* OR draught* OR wildfire* OR hurricane*) |
| #2 | It identifies the occupational setting | ("occupational diseases"[MeSH Terms] OR "occupational health"[TW] OR "occupational exposure"[MeSH Terms] OR "occupational medicine"[MeSH Terms] OR "occupational risk"[TW] OR "occupational hazard"[TW] OR "Industry"[Mesh:noexp] OR "construction industry"[MeSH Terms] OR agriculture[MeSH Terms] OR "occupational group*" OR "work: related"[All Fields] OR "air pollutants, occupational"[MeSH Terms] OR "working environment"[TW] OR worker*[TW]) |
| #3 | It identifies the outcomes | (injur* OR "acute death" OR fatalit* OR safety) |
| Overall search strategy | #1 AND #2 AND #3 NOT animal* (Filters activated: English, From 2000/01/01) | |
| 3. Search strategy to identify publications focused on the expansion of vector habitats on the increased risk of infectious diseases due to climate change | ||
| #1 | It identifies hazards/exposures | ("air temperature" OR "climate change" OR "climate variability" OR "global warming" OR heat OR "hot temperature" OR "heat wave*") |
| #2 | It identifies the occupational setting | ("occupational diseases"[MeSH Terms] OR "occupational health"[TW] OR "occupational exposure"[MeSH Terms] OR "occupational medicine"[MeSH Terms] OR "occupational risk"[TW] OR "occupational hazard"[TW] OR "construction industry"[MeSH Terms] OR agriculture[MeSH Terms] OR occupational group*[TW] OR "work:related"[All Fields] OR "air pollutants, occupational"[MeSH Terms] OR "working environment"[TW] OR worker*[TW] OR livestock OR aviculture) |
| #3 | It identifies the outcomes | ((infect* OR vector* OR zoonos* OR mosquito* OR tick*) AND (distribution OR geographic* OR region* OR emergen*)) |
| Overall search strategy | #1 AND #2 AND #3 | |
Appendix Table 2.
Search strategies employed to retrieve the scientific literature on the effects of climate change on work capacity and productivity
| PubMed | ||
| #1 | It identifies hazards/exposures | ("air temperature" OR "Climate change" OR "climate variability" OR "global warming" OR heat OR "hot temperature" OR "heat wave*") |
| #2 | It identifies the occupational setting | ("occupational diseases"[MeSH Terms] OR "occupational health"[TW] OR "occupational exposure"[MeSH Terms] OR "occupational medicine"[MeSH Terms] OR "occupational risk"[TW] OR "occupational hazard"[TW] OR "Industry"[Mesh:noexp] OR "construction industry"[MeSH Terms] OR agriculture[MeSH Terms] OR "occupational group*"[TW] OR "work:related"[All Fields] OR "air pollutants, occupational"[MeSH Terms] OR working environment[TW] OR worker*[TW]) |
| #3 | It identifies the outcomes | ("work capacity" OR strike* OR productivity OR break* OR efficiency OR rest) |
| Overall search strategy | #1 AND #2 AND #3 NOT animal* | |
| SCOPUS Database | ||
| productivity AND "Climate change" AND worker* All fields; Filters: Economics, Sociological | ||
Appendix Table 3.
Synthesis of studies found using the first search strategy focusing on HRI
| Studies making use of administrative databases | ||||||||
| Paper | Codes employed to identify HRI | Study period | Heat index | Administrative database | Association measure | Type of study | Lag time | Definition of heatwave employed |
| Adam-Poupart et al (2) | Can_Stand_Assoc_Standard Z795 07200-Effects of heat or light, 07210-Heat stroke, 07220-Heat syncope, 07280-Multiple effects of heat or light, 07290-Effects of heat or light (not elsewhere classified) including heat-related fatigue and edema |
From May 1st to September 30th of each year between 1998 and 2010 | Daily maximum temperature | Workers' Compensation Board (WCB) of Quebec. | IRR per 1°C increase | Incidence | 0-1-2; moving average (01; 0-1-2) |
N/A |
| Bonauto et al (13) | ICD-9 codes: 992.0—Heat stroke and sunstroke; 992.1—Heat syncope; 992.2—Heat cramps; 992.3—Heat exhaustion, anhydrotic; 992.4—Heat exhaustion due to salt depletion; 992.5—Heat exhaustion, unspecified; 992.6—Heat fatigue, transient; 992.7—Heat edema; 992.8—Other specified heat effects; or 992.9—Effects of heat and light, unspecified; and/or an ANSI Z16.2 type code 151 (Contact with general heat—atmosphere or environment) | January 1, 1995 and December 31, 2005 | Maximum daily temperature | Workers' compensation insurance | N/A | Descriptive; Incidence rates | 3 days | N/A |
| Fortune et al (33) | In ED records, a case of heat illness was defined on the basis of ICD-10-CA codes for conditions diagnosed as heatstroke, sunstroke, heat collapse, heat cramps, heat exhaustion, heat fatigue, heat edema or other effects of heat and light. Among lost time claims, a case of heat illness was defined by information describing the nature, event or source of injury. | January 2004 to December 2010 | N/A | Emergency Department visits and Workplace Compensation Lost Time Claims | Proportionate morbidity ratio (PMR) | Incidence rates | N/A | N/A |
| Fortune et al (32) | (a) Heat-related Main or Other Problem listed: T57: Effects of heat and light X30: Exposure to excessive natural heat W92: Exposure to excessive heat of man-made origin |
January 1, 2004 and December 31, 2010 | Maximum daily T° | Emergency department, work-related, non-scheduled visits | Generalized Linear Mixed Model, with Bayesian inference | Ecologic time series analysis | The sum of the differences between temperature on the current day and that on the previous three days (Tlag3) | N/A |
| Fuhrmann et al (34) | ICD-9-CM code 992.x | 2007-2011 | Heat emergency response plan by National Weather Service (NWS). Apparent temperature. | Emergency Department Visits | Observed versus expected ED visits | ?? | N/A | At least one heat product must have been issued and verified across four or more NWS county warning areas in North Carolina for five or more consecutive days. A heat event was terminated if there was a lapse in these conditions for at least 5 days. |
| Garzon Villalba et al (37) | Incidents with a primary or secondary code that suggested a heat-related disorder (e.g., 0721-0724). EHI included acute health events related to heat such as heat stroke, heat syncope, and heat exhaustion. | May 2010-March 2011 | WBGTmax | British Petroleum Workers' compensation database | IRR per 1°C above - WBGTmax 20 | Incidence | 1 | N.A. |
| Gubernot et al (38) | A heat-related death is identified in CFOI as an exposure to environmental heat with the BLS Occupational Injury and Illness Classification System event/exposure code 321 and the nature code of 072 | 2000-2010 | N/A | Census of Fatal Occupational Injuries (CFOI) database | Rate Ratios per state | Incidence | N/A | N/A |
| Harduar-Morano et al (42) | HRI (ICD-9-CM 992.0-992.9 and E900.0, E900.1, E900.9). Work relatedness was identified through workers' compensation as the expected payer or the presence of a work-related Ecode | 2007-2011 | N/A | Inpatient hospitalization (IH) and emergency department (ED) data from nine southeastern states USA | Relative Risk for different categories of independent variables | Survey, incidence | N/A | N/A |
| Harduar-Morano et al (44) | HRI was defined as the presence of an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM, morbidity or Tenth Revision (ICD-10, mortality) code for the effects of heat and light (992-992.9/T67-T67.9) or an excessive heat external cause of injury (Ecode) (E900.0/X30, E900.1/W92, E900.9) [ |
May and October (2005-2012) | N/A | Emergency department (ED) and hospital discharge data from the Florida Agency for Health Care Administration. Death certificate data from the Florida Department of Health (FDOH), Bureau of Vital Statistics | Crude rate ratios (RR) and corresponding 95% confidence intervals (CI) | Survey, incidence | N/A | N/A |
| Harduar-Morano et al (43) | HRI as occurring when: presence of (1) an ICD injury diagnosis code for the effects of heat and light (ICD-9-CM codes 992 or 992.0-992.9 or ICD-10 codes T67 or T67.0-T67.9) and/or (2) the presence of an ICD-9-CM or ICD-10 code for external cause of injury for excessive heat due to weather conditions (E900.0 or X30, respectively), excessive heat due to man-made conditions (E900.1 or W92, respectively), or excessive heat of unspecified origins (E900.9) or ICD-9-CM E900 | 2005 through 2012 | N/A | ED visits and hospital Discharges. data on deaths for the same years from the Florida Department of Health, Office of Vital Statistics |
N/A | Survey, descriptive | N/A | N/A |
| Mirabelli et al (70) | Heat-related deaths (ICD9 codes 692.71, 992.0-992.9, E900.0, E900.1, and E900.9) | 1977-2001 | Average annual summer temperatures | Medical examiner's records; statewide temperature data from the National Climatic Data Center | Rate ratio | Incidence | N.A. | N.A. |
| According to the Maricopa County Department of Public Health surveillance system, using both the ICD-10 codes and key phrased in the text fields (a death was considered environmental heat-associated if it was related to heat generated by the climate (e.g., sun, humidity, etc.) and excludes heat from man-made sources such as ovens or manufacturing equipment.) | May-October 2002-2009 | NOT specified | Death certificates | Assessing the risk of HR death by occupation | Case-control | |||
| HRI International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) at least one among the following codes: 992.xx (Effects of heat and light), E900 (Excessive heat), E900.0 (Excessive heat due to weather conditions, or E900.9 (Excessive heat of unspecified origin) |
From May through September 2008-2010 | Daily maximum temperature | Emergency department (ED) data | Mean daily HRI ED visits for increase in daily maximum ambient temperature | Ecological | 0 | N.A. | |
| Petitti et al (75) | Industry/Sector Codes Used to Identify Heat-Related Illness Claims OR ICD9 CM codes (705.1 Prickly heat 276 Hyperosmolality and/or hypernatremia Volume depletion Volume depletion, unspecified Dehydration Hypovolemia 584 Acute renal failure 584.9 Acute renal failure, unspecified 992 Effects of heat and light 992 Heat stroke and sunstroke Heat syncope Heat cramps Heat exhaustion Heat exhaustion, anhidrotic Heat exhaustion due to salt depletion Heat exhaustion, unspecified Heat fatigue, transient Heat edema Other specified heat effects Effects of heat and light) |
January 1, 1995 to December 31, 2009 | Maximum daily temperature (Tmax) and Heat Index (HImax) | workers' compensation claims | Mean Tmax and mean HImax for outdoor claims (TABLE III) | Ecological | 0 | N.A. |
| The Type of Occurrence Classification System Other diseases and injuries; mental disorders; nervous systems and sense organ dis; skin and subcutaneous tissue dis; digestive system dis; resp. system diseases; infectious and parasitic dis; circulatory system dis; neoplasm; cancer | 1 July 2001 to 30 June 2010 | Daily maximum and minimum temperatures | Workers' compensation claim data | Incidence rate ratios (IRR) with 95% CIs, and interpreted as % in the N of daily work-related injury claims during heatwave periods compared with non-heat wave periods | Time-series | N.A. | ≥3 consecutiv e days over 35°C);≥5 days of max temp in excess of 35°C OR ≥3 days of max temp in excess of 40°C | |
| Rhea et al (82) | claims due to heat illnesses were identified using each of the following four codes: TOOCS nature classification G313 (heat stress/heat stroke), TOOCS mechanism classification G53 (exposure to environmental heat), TOOCS agency classification G7100 (weather and water) and TOOCS agency classification G7110 (sun) | 2001-2010 | Daily maximum temperature (Tmax) | Workers' compensation claim data | Incidence rate ratios (IRR) with 95% CIs, | Time series analysis/Case-crossover | N.A. | ≥3 consecutiv e days with Tmax ≥35°C |
| Spector et al (89) | Definition of HRI | Study period | Heat index | Data source | Association measure | Type of study | Lag time | Definition of heatwave employed |
| Reported sudden muscle cramps; nausea or vomiting; hot, dry skin; confusion; dizziness; or fainting | 2012-2013 | Reported "high temperature" | Data are from PACE4, a community-based participatory research project Participants were recruited from three agricultural counties. A total of 235 farm workers completed the baseline interviews | Prevalence of characteristics among different subgroups. Chi square test of differences | Cross sectional | N.A. | N/A | |
| Xiang 2 et al (99) | Reported skin rash/skin bumps, painful muscle cramps/spasms, dizziness/light-headedness, fainting, headache, heavy sweating, extreme weakness/fatigue, nausea/vomiting, and confusion. | Interviews from Jul to Aug 2013 | N/A | Eligible participants were: (1) 18 years or older; (2) farm workers engaging in outdoor crop production at the time of the interview; (3) able to speak English or Spanish; and (4) able to provide informed consent | Chi-square test and Fisher's exact test. Logistic regression models. Prevalence Rate. | Cross-sectional | N/A | N/A |
| Heat-related symptoms were headache, tachycardia, muscle cramps in the arms or legs, fever, nausea, difficulty breathing, swelling of hands or feet, dizziness, vomiting and fainting. Dehydration symptoms were dry mouth and dysuria | February 2011 | N/A | Harvesters were interviewed. A 64 items' symptom questionnaire with questions based on the US Military recommendations | Chi-square tests and Fisher's exact test | Cross-sectional survey with control group | N/A | N/A | |
| Xiang et al (101) | Neurological symptoms Headache Loss of co-ordination Dizziness Tingling in hands/feet Blurred vision Fainting Electrolyte imbalances Abdominal cramps Spasms Systemic symptoms Fatigue Nausea Loss of appetite Early heat stress symptoms Heavy sweating Intense thirst Anxiety Dark coloured urine output Rashes Itching skin Dry mouth Elevated temperature Hot red or flushed dry skin |
2013-2014 winter and summer | WBGT | Construction workers. Structured questionnaire | N/A | Cross sectional survey | N/A | N/A |
| Symptoms of HRI (sudden muscle cramps; nausea or vomiting; hot, dry skin; confusion; dizziness; fainting; headache). The outcome of interest was experiencing three or more symptoms in the past week. Because HRI symptoms are common and general symptoms, using three or more symptoms was designed to improve the identification of HRI specifically | June 11-23, 2011 | During data collection for the current study, temperatures ranged between 95°F and 104°F, and the heat index was 100°F or hotter every day, peaking at 108°F | Structured questionnaire | Ors Migrant farm-workers versus "ideal" | Cross sectional survey | N/A | N/A | |
| Studies making use of ad hoc questionnair e surveys | Eight heat exhaustion symptoms (headache, nausea, vomiting, weakness, fatigue, dizziness, clammy/moist skin or irritability), and seven heat stroke symptoms (high body temperature, hot and dry skin, confusion, low muscle coordination, irrational behaviour, loss of consciousness or convulsions), | N/A | N/A | Data were collected from participants via a questionnaire. In completing the questionnaire, participants indicated whether they had experienced any symptoms of heat illness in the past 12 months. | Independent samples t-test One-way analysis of variance Pearson's Chi-square analysis Rate ratios were calculated for significant Chi-square observations |
Cross-sectional with control | N/A | N/A |
| Paper |
Symptom Feeling tired Cramps Nausea Dizziness Thirst Vomiting Confusion Muscle weakness Heat sensations Chills Feeling light-headed |
N/A | WBGT | Direct measurements on workers and symptoms' referral | Independent samples t-test One-way analysis of variance Pearson's Chi-square analysis Rate ratios were calculated for significant Chi-square observations |
Cross-sectional | N/A | N/A |
| Arcury et al (8) | Overall 42 symptoms, of them 18 MSK and the rest "General" | The survey was carried out in the middle of August 2001 | WBGT | self-administered questionnaire | Chi2 test or Student's t-test | Cross-sectional | N/A | N/A |
| Bethel et al (11) | A section of Critical Incident Report was included in the worker data collection sheet to obtain workers' personal heat illness experiences. Reported symptoms of heat disorders include heat rash (1 case), fatigue (10 cases), feeling thirsty (3 cases), feeling discomfort (5 cases), dizziness (18 cases), difficulty in breathing (4 cases), heat cramp (3 cases), dehydration (3 cases), over sweating (4 cases), dry and hot skin (1 case), fever (8 cases), headache (6 cases), vomiting (8 cases), loss of control (2 cases), fainting (7 cases), non-sweating (1 case), and heat stroke (2 cases). | N/A | Predicted Heat Strain (PHS) model WBGT and many others | Data collection sheet for the construction workers sample, a questionnaire and interview guide for the managers sample and a site observation checklist | N/A | Ethnographic study. Qualitative study | N/A | N/A |
| Crowe et al (20) | A range of health symptoms including minor conditions such as heat cramps, heat syncope, and heat exhaustion to life-threatening heat stroke | August to September 2013 | Mean maximum temperatures; Maximum heat index | interviewer-administered questionnaire that included standard questions related to heat-related symptoms | Logistic and log-binominal regression models were used to assess associations between sun protection behaviors and heat-related symptoms and to calculate prevalence ratios. | Cross-sectional | N.A. | N.A. |
| Dutta et al (24) | Only heat stroke considered | November 2003 | None | Questionnaire | Multiple linear regression analysis (BODY TEMP registered) | Cross-sectional : no association between heat index and heatstroke was evaluated | N.A. | N.A. |
| Fleischer et al (31) | A variety of symptoms (e.g. increased thirst, excessive perspiration, itchy skin, tiredness, dry nose, blister formation, sinus problems, teary or burning eyes, exhaustion, malaise, dehydration, headaches, backache, leg pains, nose bleeds, premature baldness, dizziness) | March 2009 | Hourly humidity and hourly maximum temperature | Focus group discussions and interviews | NONE | Cross-sectional | N.A. | N.A. |
| Hunt et al (46) | Subjective symptoms; Physiological parameters: Systolic and diastolic blood pressure and heart rate, electrolyte and blood urea | August 18th and 19th in 1998 ("fine days") | WBGT | Field study | Systolic and diastolic blood pressure and heart rate measurement before and during work Did not study association with WBGT data |
Physiological parameters monitoring | 0 | N.A. |
| Pradhan et al (77) | Faint, tension, irritation, laziness, lack of sleep, rash, diarrhoea, eye infection, etc. | 2010 | Heat index, humidity index, and WBGT, based on the HOTHAPS approach | Household survey | None | Cross-sectional | N.A. | N.A. |
| Sahu et al (84) | NO MENTION OF HRI Health complains: pain in different parts of the body, digestive problems, CV problems, other problems (eye, ears, respiratory) ; Heat concerns (Aware of heat symptoms, discomfort or exhaustion during hottest days) |
April to June 2011 | WBGT | Questionnaire | Student t-test used to test for any significant differences between the measured parameters at different times and heat exposures | Cross-sectional | 0 | N.A. |
| Singh et al (87) | perceptions of heat discomfort, occurrence of health symptoms, heat exhaustion | summer of 2010 | Not specified | semi-structured telephone interviews | No association measure used | Cross-sectional | N.A. | N.A. |
| Venugopal et al (92) | self-reported heat related health illnesses One of the following heat related symptoms at work i.e., excessive sweating, excessive thirst, tiredness, cramps, headache, nausea/vomiting, fainting or prickly heat | 2 Seasons, once during the "hotter season" (April-June 2013 and another during the "cooler season" (November-January 2012) | WBGT (The minimum, maximum and standard deviation of WBGT values from each workplace was computed from the total number of ambient heat stress measurements taken at various locations in the each workplace). | Questionnaire | Chi square test was used to compare seasonal differences in qualitative assessments of heat for workers assessed in both hotter and cooler seasons. | Cross-sectional | N.A. | N.A. |
Appendix Table 4.
Synthesis of studies found using the second search strategy focusing on injuries.
| Paper | Study period | Heat index | Data source | Association measures | Study design | Lag time | Heat wave definition |
| Adam-Poupart et al (2) | 2003-2010 | Maximum daily outdoor temperature | Workers' Compensation Board | IRR per 1°C increase | Incidence | 0-1-2; moving average (0-1; 0-1-2 | N.A. |
| Bonauto et al (13) | May 2010-March 2011 | WBGTmax | British Petroleum Workers' compensation database | IRR per 1°C above - WBGTmax 20 | Incidence | 1 | N.A. |
| Fortune et al (33) | 2002-2012 | Maximum daily temperature and minimum daily temperature (minimum temperature during the night before the day of injury ) | Workers' compensation claims database | OR per 1°C increase in temperature measure | Case-crossover | 0 | N.A. |
| Fortune et al (32) | 1998-2003 | Apparent temperature (AT AT max, AT24 and AT day were assessed | Hospital discharge data | Proportions comparison | Ecological | 0 1 |
N.A. |
| Fuhrmann et al (34) | 200-2013 | Daily maximum and minimum temperatures | Workers' compensation claims database | Proportions comparison | Case-crossover | N.A. | ≥3 days of max temp in excess of 35°C |
| Garzon-Villalba et al (37) | 2000-2012 | Maximum daily humidex exposures | Workers' compensation claims database | OR per category of humidex index | Case-crossover | 0 | N.A. |
| Gubernot et al (38) | 2005 | Experiences of heat stress derived from survey question | Questionnaire survey | OR | Cohort study | N.A. | N.A. |
| Harduar-Morano et al (42) | 2001-2010 | Daily maximum and minimum temperatures | Workers' compensation claims database | IRR | Time series | N.A. | ≥3 days of max temp in excess of 35°C; ≥5 days of max temp in excess of 35°C OR ≥3 days of max temp in excess of40°C |
| Harduar-Morano et al (44) | 2001-2010 | Daily maximum temperature | Workers' compensation claims database | IRR per 1°C between 14.2°C and 37.7°C | Ecological | 0 | N.A. |
Appendix Table 5.
Papers selected using the first search strategy
| Paper | Year | Country/Region | Population | Heat exposure index | Study design | Outcome | Main results |
| Adam-Poupart et al (1) | 2014 | Canada | Working population | Maximum daily temperature | Ecological | Heat-related illness | The relationship between daily counts of compensations and maximum daily temperatures was log-linear; the pooled incidence rate ratio of daily heat-related compensations per 1 °C increase in daily maximum temperatures was 1.419 (95% CI 1.326 to 1.520). |
| Adam-Poupart et al (2) | 2015 | Canada | Working population | Daily mean temperature | Case-crossover | Respiratory diseases | It was unclear if the observed trends for outdoor workers are due to ozone levels, to high temperatures or to other unmeasured parameters that are associated with them. |
| Arbury et al (3) | 2014 | USA | Working population | Heat index | Case surveillance | Heat-related illness | Nine of the 13 deaths reported occurred in the first 3 days of working on the job, 4 of them occurring on the worker's 1st day. In 7 cases, 2 or more employees had a HRI. All heat illnesses and deaths occurred on days with a heat index 29.0°C–41.0°C. |
| Arcury et al (4) | 2015 | USA | Agriculture | Ambient temperature | Cross-sectional | Heat-related illness | The majority of days were in the heat index range of 90° to 103° F. Factors associated with HRI while working outside included working in wet clothes and shoes, harvesting and topping tobacco, and spending after-work time in an extremely hot house |
| Balbus et al (5) | 2009 | USA | General population, including working population | Not specified | Narrative review | Heat-related illness | Electricity and pipeline utility workers are at increased risk of heat stress, especially if work tasks involve heavy exertion. |
| Bates et al (6) | 2008 | United Arab Emirates | Construction | TWL (thermal work limit) and WBGT | Physiological parameters monitoring | Physiological parameters | Workers were not physiologically challenged despite fluctuating harsh environmental conditions |
| Bates et al (7) | 2010 | Middle East | Construction | Not specified | Cross-sectional | Physiological parameters | Although the expatriate workers were found in general to be better hydrated than their Australian counterparts, a high proportion were still found to be inadequately hydrated both on presentation for work and throughout the shift. |
| Bedno et al (8) | 2014 | USA | Armed force | Not specified | Cohort | Heat-related illness | There were 67 incidents of Exertional heat illness (EHI). Among weight qualified (WQ) subjects, step test failure was significantly associated with EHI (OR 2.00, 95% CI 1.13, 3.53). For those passing the step test, the risk of EHI was significantly higher in those who exceeded body fat than in WQ subjects. |
| Berry et al (9) | 2011 | Australia | Agriculture | Not specified | Narrative review | Mental health | Currently there is inconclusive evidence for the proposition that (all) farmers have elevated rates of mental health problems, even in the face of extreme adversities. |
| Bethel et al (10) | 2014 | USA (Oregon) | Agriculture | Not specified | Cross-sectional | Heat-related illness | 64% of respondents reported experiencing a symptom consistent with HRI during a hot day at work in the past week. Nearly 30% of participants reported experiencing ≥ 2 HRI symptoms during the previous work; 11% experienced ≥3 HRI symptoms. |
| Biswas et al (11) | 2011 | India | Other | WBGT | Cross-sectional | Physiological parameters | The WBGT index was above the recommended range in summer. In the summer, the relative cardiac cost above 30 was recorded for 35% of the work shift in the young workers and 47% of the work shift for older workers. |
| Bodin et al (12) | 2016 | El Salvador | Agriculture | WBGT | Physiological parameters monitoring | Heat-related illness | WBGT was >26°C from 9:00 (average max.: 29.3±1.7°C). There was a reduction of HR symptoms and dehydration before and after the intervention. Individual daily production increased from 5.1 to a high of 7.3 tons/person/day. |
| Bonauto et al (13) | 2007 | USA (Washington State) | Working population | Outdoor ambient temperature | Ecological | Heat-related illness | There were 480 Washington HRI claims during the study period. The significantly increased average daily Tmax on days with multiple HRI claims compared to those with a single HRI claim suggests a dose-response effect of environmental ambient temperature. |
| Boodosingh et al (14) | 2014 | Puerto Rico | Armed force | Not specified | Case report | Heat-related illness | A case of heat stroke with altered mental status was managed with mechanical ventilatory support, intravenous fluids and external cooling measures. The man was later discharged home without any neurological sequelae. |
| Brake et al (15) | 2003 | Australia | Mining underground | WGBT | Physiological parameters monitoring | Physiological parameters | Average environmental conditions were severe (WBGT 30.9°C, SD 2.0 ° C), range 25.7-35.2 ° C). A majority of workers were coming to work in a moderately hypohydrated state (average urinary specific gravity 1.024, SD 0.0059). |
| Bray (16) | 2010 | USA | Agriculture | Not specified | Case report | Heat-related illness | A case-report of a 19-year-old male landscaper in Delaware who died of heat stroke on his first day of work on a hot, humid day in late June. |
| Brearley et al (17) | 2015 | Australia (Northern territory) | Electrical | WGBT | Cross-sectional | Physiological parameters | The values of gastrointestinal temperature showed a peak of 38.4°C. The mean physiological strain index (PSI) was 2.6 (=overall low strain), with periods of moderate strain. They were dehydrated prior to and following the work shift. |
| Clark P.A. et al (18) | 2016 | Central America (Nicaragua) | Agriculture | Not specified | Narrative review | Kidney diseases | Sugarcane workers are working under direct sun exposure, high temperatures, for very long hours with minimal breaks. Those working conditions alone can cause severe rhabdomyolysis and acute kidney injury. Prolonged glyphosate use and exposure further damages renal tissue and worsens kidney function. Inappropriate use of antibiotics, NSAID, diuretics can also greatly aggravate kidney damage. Unremitting acute kidney injury eventually transitions to chronic kidney disease. |
| Crowe et al (19) | 2015 | Central America (Costa Rica) | Agriculture | Not specified | Cross-sectional | Heat-related illness | Heat and dehydration symptoms were experienced at least once per week more frequently among harvesters (P<0.05). Percentages of workers reporting such symptoms increased in accordance with increasing heat exposure categories. |
| Delgado Cortez (20) | 2009 | Nicaragua | Agriculture | WBGT | Physiological parameters monitoring and productivity | Physiological parameters | Although temperature increased to maximum values early in the morning, many workers did not follow the rehydration measures and drank less than 6 L, a potentially dangerously low volume. |
| D'Ovidio et al (21) | 2016 | Global | Working population | Not specified | Narrative review | Allergies | Workplaces may be an important source of exposure to air pollution not only for dust and fumes, but also for vegetable and animal allergens. |
| Dutta et al (22) | 2015 | India | Construction | WBGT | Cross-sectional | Heat-related illness | 59% of all reports in summer were positive for symptoms (from mild to severe) as compared to 41% in winter. |
| Edwards et al (23) | 2015 | Australia | General population, including working population | Drought | Cross-sectional | Mental health | Overall, 15.7 % of farmers had a mental health problem compared to 9.1 % of farm workers, 8.9 % of those in non-agricultural employment and 17.4 % of those who were not employed. |
| Ellis et al (24) | 2017 | Australia | Agriculture | Not specified | Cross-sectional | Mental health | The recently observed patterns of climate change have exacerbated farmers' worries about the weather, undermined notions of self-identity, and contributed to cumulative and chronic forms of place-based distress, culminating in heightened perceived risk of depression and suicide. |
| Farshad et al (25) | 2014 | Iran | Construction | WBGT and TWL | Physiological parameters monitoring | Physiological parameters | There was a significant difference in Thermal Work Limit (TWL), WBGT and urinary specific gravity (USG) between exposed and non-exposed group (P<0.01). Mean USG was 1.0213 ± 0.0054 in control group and 1.026 ± 0.005 in exposure group, which does not show a clinically dehydration status |
| Fleischer et al (26) | 2013 | USA (Georgia) | Agriculture | Ambient temperature, heat index | Cross-sectional | Heat-related illness | Temperatures ranged between 95°F and 104°F, and the heat index was 100°F or hotter every day, peaking at 108°F. Most farmworkers (71%) reported experiencing at least 1 symptom, and one third reported experiencing ≥3 symptoms in the past week. |
| Fortune et al (27) | 2013 | Canada (Ontario) | Working population | Not specified | Case series | Heat-related illness | The peak incidence was observed in the summer. The risk of HRI was elevated for men, young workers, manual workers and those with shorter employment tenure. |
| Fortune et al (28) | 2014 | Canada (Ontario) | Working population | Ambient temperature | Ecological | Heat-related illness | The median increase in the daily rate of emergency department (ED) visits for HRI was 75% for each degree above 22°C (posterior 95% credible interval (CI) relative rate=1.56-1.99) in the daily maximum temperature. |
| Fuhrmann et al (29) | 2016 | USA | General population, including working population | Ambient temperature | Case series | Heat-related illness - cardiorespiratory diseases | Heat exhaustion was the most common HRI, while heat stroke was relatively low (<10 % of visits). About 1/3 of all HRI visits were work-related. |
| Galvao Barbosa et al (30) | 2012 | Brazil | Agriculture | WBGT | Physiological parameters monitoring | Physiological parameters | Work during the harvest period was associated with changes in blood markers and higher blood pressure, which may be related to autonomic imbalance. |
| Garcia-Trabanino et al (31) | 2015 | El Salvador | Agriculture | Temperature,WBGT,and HI | Cross-sectional | Physiological parameters | The mean urine specific gravity, urine osmolality and creatinine, serum creatinine, uric acid and urea nitrogen increased; urinary pH, chloride and potassium decreased; pre-shift eGFR was reduced (<60 mL/min) in 14% of male workers. |
| Garzon-Villalba et al (32) | 2016 | USA | Working population | WBGTmax | Incidence | Heat-related illness | Exertional Heat Illness (EHI) were higher in workers exposed above a WBGTmax of 20°C (RR 1.40). Exposures above 28°C-WBGTmax on the day of the EHI and/or the day before were associated with higher risk of EHI (RRs from 1.0-10.4). |
| Gubernot et al (33) | 2014 | USA | Working population | Not specified | Scoping review | Heat-related illness | Around 40% of HRI cases occur among workers. The length of service appears inversely related to the occurrence of HRI. Working in direct sunshine can add up to 15°F to the perceived temperature. Increased heat decreases workers’ productivity. |
| Gubernot et al (34) | 2015 | USA | Working population | Not specified | Case surveillance | Heat-related illness | A higher rate of HR deaths for the years 2005-2010 than for the years 2000-2004 was found (RR=1.4) The largest N of deaths occurred in July (34%) (86% occurred in June-August); 65% of workers fell ill between 12 and 6:00 pm. |
| Hanigan et al (35) | 2012 | Australia | Agriculture | Hutchinson Drought Index | Time-series | Mental health | Authors found an increased relative risk of suicide of 15% (95% CI 8%-22%) for rural males aged 30-49 y when the drought index rose from the 1st to the 3rd quartile. An increased risk of suicide was observed in spring and early summer. |
| Hanna et al (36) | 2011 | Australia | Working population | Ambient temperature | Narrative review | Heat-related illness | Workplaces with risks of extreme heat exposure include outdoor and maintenance work, mining, shearing, farmwork, firefighting, and other emergency and essential services. Indoor work near heat-generating equipment with poor ventilation is also potentially hazardous on hot days. Those with high aerobic fitness can tolerate core temperatures 0.9°C higher than those who are less fit before succumbing to heat exhaustion. The impacts of extreme heat are not restricted to physiological effects: cognitive impairment and psychological and behavioural effects have been demonstrated and climate change has been linked to increased suicide rates and other mental health concerns. |
| Harari-Arjona et al (37) | 2016 | Ecuador | Agriculture | Not specified | Narrative review | Heat-related illness | Farmers suffer dehydration and frequent episodes of sudden onset of cramps in limbs, which make workers unable to work again. Also, a higher prevalence of kidney diseases has been reported. In particular, there is great concern about an epidemic CKD. |
| Harduar-Morano et al (38) | 2015 | USA | Working population | Not specified | Case series | Heat-related illness | There were 8,315 occupational HRI ED visits (6.5/100,000 workers) and 1,051 IHs (0.61/100,000). Younger workers had elevated rates for ED visits, while older workers had higher IH rates. The majority of IHs and ED visits occurred in the summer months. |
| Harduar-Morano et al (39) | 2016 | USA | General population, including working population | Not specified | Case series | Heat-related illness | The largest proportion of work-related (WR) HRI morbidity and mortality occurred in August. The WR HRI cases accounted for 0.66%, 0.98%, and 2.3% of all-cause WR ED visits, hospitalizations, and deaths during the warm season. |
| Harduar-Morano et al (40) | 2017 | USA (Florida) | General population, including working population | Not specified | Case series | Heat-related illness | There 2979 ED visits, 415 hospitalizations, and 23 deaths in patients with work-related HRI. The proportion of patients with a severe HRI diagnosis increased with data source severity. |
| Holmes et al (41) | 2011 | Dubai | Other | Not specified | Cross-sectional | Physiological parameters | 55% of workers were found to be clinically hyponatraemic during the summer period compared with only 8% during the winter period. |
| Hunt et al (42) | 2013 | Australia | Mining surface | Not specified | Cross-sectional | Heat-related illness | Heat illness symptoms were experienced by 87 and 79 % of surface and underground mine workers, respectively (p = 0.189), with 81-82 % of the symptoms reported being experienced by miners on more than one occasion. |
| Hunt et al (43) | 2014 | Australia | Mining surface | Not specified | Cross-sectional | Heat-related illness | Core body temperature averaged 37.46 ± 0.13°C, with the group maximum 37.98 ± 0.19°C. Mean urine-specific gravity was 1.024 ± 0.007, with 78.6% of samples 1.020 or more. 73% of workers reported at least one HR symptom during the shift. |
| Inaba et al (44) | 2007 | Japan | Construction - Traffic control | WBGT | Cross-sectional | Heat-related illness | Work difficulty due to hot weather was significantly less prevalent in traffic control workers than among construction workers (p <0.01). |
| Jackson et al (45) | 2010 | USA | Working population | Not specified | Case surveillance | Heat-related illness | From 1992 through 2006, 68 workers employed in crop production and related services died from heat-related illness. The Ag/For/Fis/ Hun sector had the highest average heat fatality rate (~0.3 deaths/100,000 full-time workers). |
| Jia et al (46) | 2016 | China (Hong Kong) | Construction | WBGT | Case-report | Heat-related illness | Among the 207 workers, 36 valid heat illness cases (17.4%) were reported. There was a peak in HRI right before lunch, and another at 2 pm, lasting until 3 pm. No incident was reported after 4 pm. |
| Joubert et al (47) | 2011 | United Arab Emirates | Working population | Not specified | Case surveillance | Heat-related illness | One company reported a combined 79.5% decrease in cases (15.3 vs 1.16 cases per 1000 workers) while the other experienced a 50% reduction in serious cases (0.08-0.04 cases per 100,000 work hours). |
| Kearney et al (48) | 2015 | USA | Agriculture | Mean maximum temperatures and maximum heat index | Cross-sectional | Heat-related illness | Mean max. temp. ranged between 86°F and 95°F; max. heat index was 117°F. The prevalence of having 1 HRI symptom was 72% and 27% among workers had ≥3 HRI symptoms. |
| Kenefick et al (49) | 2007 | USA | Working population | Ambient temperature | Narrative review | Physiological parameters | Bishop et al. observed that, in simulated industrial work conditions, encapsulated protective clothing increased sweat rates up to 2.25 L/h. Likewise, wearing protective equipment such as full or half face masks can make fluid consumption more difficult and can further contribute to dehydration in the work place. Firefighters, who wear heavy protective clothing and are exposed to intense heat., were reported to have sweat rates up to 2.1 L/h. Brake et al. observed fluid losses and hydration status of mine workers under thermal stress working extended shifts (12 hours): 60% of the miners reported to work dehydrated and that their hydration status did not improve throughout the 10 to 12 hour shift. |
| Kjellstrom 1 et al (50) | 2009 | Global, with a special focus on LMIC | Working population | WBGT | Narrative review | Heat-related illness | 423 heat-related deaths were reported among agricultural workers in the USA, 1992-2006. There are few studies in low and middle-income countries of deaths or serious clinical heat stroke among heat-exposed workers, except for India. Beyond the acute heat stress, more chronic effects on the heart and kidneys may develop after repeated excessive body heating or dehydration. |
| Kjellstrom et al (51) | 2011 | Global, with a special focus on Central America | Working population | WBGT | Narrative review | Heat-related illness | 28°C is the WBGT threshold limit value for risks to health for heat-acclimatized workers carrying out moderate labor, and 27°C for heavy labour. 4% of HR deaths in the USA were in the Ag/For/Fis/ Hun sector and of these 67% were in workers employed in crop production. Above 26°C, the increasing need for rest periods can be approximated by straight lines that differ depending on the work intensity |
| Kjellstrom et al (52) | 2016 | Global | Working population | WBGT | Narrative review | Heat-related illness | Death from heat stroke have been reported among South African mine workers, US agricultural workers, as well as in China, India, Qatar, and other countries. Specific serious heat stroke symptoms and heat exhaustion were notified in many hot workplaces, including China and India. Clinical damage of organs, heart overload and kidney damage were reported among US military, Central American sugar workers and migrant construction workers in Qatar. Heat exhaustion, and cognitive and psychological performance effects among South African mine workers; Australian farmers. Reports on HR deaths show that symptoms of heat strain are often ignored. |
| Krake et al (53) | 2003 | USA (Grand Canyon) | Other | WBGT | Cross-sectional | Physiological parameters | All participant hiking into the canyon exceeded the heart rate and core body temperature (CBT) criteria. Al but one participant developed mild dehydration; 1 case of hypernatremia occurred. The majority had a history of HR symptoms or illness |
| Kravchenko et al (54) | 2013 | USA and Europe | General population, including working population | Not specified | Narrative review | Heat-related illness | A total of 423 workers died from exposure to heat (an average annual heat-related death rate of 0.39 deaths per 100,000 workers for crop workers, compared with 0.02 deaths per 100,000 for all U.S. civilian workers) between 1992 and 2006 in the U.S. |
| Lao et al (55) | 2016 | Australia | Working population | Not specified | Cross-sectional | Heat-related illness | Common heat-related symptoms including headaches, sweating, dizziness, and tiredness. Most workers highlighted that heat impedes their work efficiency and causes a substantial slowing of work rate. |
| Laws et al (56) | 2016 | Nicaragua | Agriculture | Not specified | Physiological parameters monitoring | Kidney diseases | Mean estimated glomerular filtration rate (eGFR) was 113 mL/min/1.73 m2 and <5% of workers had albuminuria. Field workers had increases in neutrophil gelatinase-associated lipocalin and IL-18 levels that were 1.49 (95% CI, 1.06 to 2.09) and 1.61 (95% CI, 1.12 to 2.31) times as high, respectively, as in non-field workers. |
| Lundgren et al (57) | 2013 | Global | Working population | Not specified | Narrative review | Heat-related illness | The years 1995-2006 have rank among the warmest. Effects of increasing temperatures include a high prevalence of CKD, in Central America, especially among sugarcane workers, and a global reduction of work productivity. |
| Lundgren et al (58) | 2014 | India | Working population | WBGT | Within-group comparison | Physiological parameters | Avg WBGT was 29.7. Significant impacts on productivity in all workplaces, apart from the laundry facility, were shown, e.g. in the canteen, the core temperature limit of 38°C predicted by the model was reached in only 64 min for women. |
| Lunyera et al (59) | 2016 | Global | General population, including working population | Not specified | Systematic review | Kidney diseases | Assessment of the associations between dehydration and CKDu across studies was limited by inconsistent reporting of the measurements for assessing dehydration. |
| Luo et al (60) | 2014 | China | Other | Not specified | Case-control | Urinary system diseases | Outdoor workers were more likely to present with urolithiasis compared with indoor ones; workers with longer cumulative exposure time (OR=1.5; 95% CI: 1.2, 1.8) and abnormal blood pressure (OR=1.6; 95% CI: 1.0, 2.5) had higher risk for urolithiasis. |
| Maeda et al (61) | 2006 | Japan | Forestry | Not specified | Cross-sectional | Heat-related illness | 1/3 of forestry workers developed some symptoms of early heatstroke. A short duration of forestry service was one of the risk factors contributing to the onset of heatstroke, in addition to heat stress, loss of body water and electrolytes, and obesity. |
| Marchetti et al (62) | 2016 | World | Working population | Not specified | Narrative review | Human health | A recent CDC report identified, during 1992-2006, a total of 423 worker deaths from exposure to environmental heat were reported in the United States. Of these 423 deaths, 102 (24%) occurred in workers employed in the agriculture, forestry, fishing, and hunting industries (rate: 0.16 per 100 000 workers) |
| Mathee et al (63) | 2010 | South Africa | Outdoor workers | Ambient temperature | Cross-sectional | Heat-related illness | Hourly max. temp. ranged from 23-36°C in Upington and 21-27°C in Johannesburg. Heat-related effects reported included sunburn, sleeplessness, irritability, and exhaustion leading to difficulty in maintaining work levels and output during very hot weather. |
| Mbanu et al (64) | 2007 | USA | Firefighters | Apparent temperature | Case-crossover | CHD | Overall, temperature was not associated with increased risk of on-duty death. |
| Meade et al (65) | 2015 | USA | Electrical | Not specified | Physiological parameters monitoring | Physiological parameters | Prior to the start of the work shift, 38% of workers were euhydrated, whereas 75% were dehydrated (USG > 1.020) after. The high levels of thermal strain were paralleled by high mean and peak HR and PSI responses, which were greater in Manual Pole Workers. |
| Mirabelli et al (66) | 2005 | USA (North Carolina) | General population, including working population | Average annual summer temperatures | Incidence | Heat-related illness | Of the 161 HR deaths, 40 occurred on the job: of these 45% were among farm labourers. All decedents whose HR injuries occurred in occupational settings were men, and most were young adults. All HR deaths among Hispanic men occurred on the job. For each 1°F increase in average summer temperature, the rate of heat-related death in the working population increased 37% (Rate Ratio=1.37; 95% CI=0.99, 1.90). |
| Mirabelli et al (67) | 2010 | USA (North Carolina) | Agriculture | Not specified | Cross-sectional | Heat-related illness | Working in extreme heat was reported by 281 respondents (94%), among whom 112 (40%) reported symptoms of heat illness. 37% reported changes in their work hours and 34% in their work activities. |
| MMWR - | 2008 | USA | Working population | Not specified | Case surveillance | Heat-related illness | 423 HR deaths were reported among workers. Of these, 24% occurred in the agriculture, forestry, fishing, and hunting industries and 2/3 of whom occurred in the crop production. A not statistically significant increase in fatality rates over time was observed. |
| CDC (68) | 2013 | Iran | Construction | Thermal Work Limit | Physiological parameters monitoring | Physiological parameters | In the exposed group, 38% of workers had a USG level between 1.026-1.030 and 12.72% had a USG level above 1.030 (in the control group 15.2% and 0.58%, respectively). The Pearson correlation measure showed a significant correlation between USG and TWL. |
| Montazer et al (69) | 2006 | Japan | Construction | WBGT | Physiological parameters monitoring | Heat-related illness | The WBGT outdoors varied from 23 to 34 °C. Few items of subjective symptoms increased after work compared with before work. Electrolytes and blood urea nitrogen did not change. Blood sugar before work was higher than before lunch and after work. |
| Morioka et al (70) | 2017 | USA | Agriculture | Not specified | Physiological parameters monitoring | Kidney diseases | Among men, 10 experienced heat strain, as estimated by physiological strain index (PSI) ≥7.5, and 3 of those met criteria for Acute kidney injury (AKI); 35 participant were incident AKI (12.3%). Adjusted OR of AKI was 1.34 (95% CI 1.04 to 1.74) among those experiencing heat strain. |
| Moyce et al (71) | 2011 | USA | Armed force | Not specified | Case surveillance | Heat-related illness | Overall, in 2010 crude incidence rates of "heat stroke" and “other heat injury” were 0.21 and 1.77 per 1,000 p-yrs, respectively. The overall unadjusted incidence rate of "other heat injury" was higher in 2010 than in any prior year of the period. |
| MSMR - Armed Forces Health Surveillance Branch (72) | 2016 | USA | Armed force | Not specified | Case surveillance | Heat-related illness | The incidence rate of heat stroke in 2015 was higher than rates in the previous 4 years. More service members were treated for "other heat injuries" in 2015 (n=1,933) than in either of the previous 2 years. |
| MSMR - Armed Forces Health Surveillance Branch (73) | 2016 | Finland | General population, including working population | Mean temperature, highest daily temperature | Cross-sectional | Heat-related cardiorespiratory symptoms | In the summer preceding the survey, the temperatures exceeded the long-term average by 1-2 °C in the areas studied. Farmers had a higher risk of presenting HR cardio-respiratory symptoms (OR 2.27; 1.14-4.46) compared with those working in industry. |
| Näyhä et al (74) | 2013 | USA (Northern Illinois) | Agriculture | Temperature and humidity | Case report | Heat-related illness | Case-report of multiple organ failure due to heatstroke. |
| Nevarez (75) | 2014 | Finland | Electrical | Ambient temperature | Physiological parameters monitoring | Physiological parameters | AT varied between - 30°C and +28°C. Average cardiorespiratory strain was 48 ± 3%VO2max. 40% exceeded the recommended 50%VO2max level. Both muscular and cardiorespiratory strain may reduce work efficiency. Thermal strain remained at a tolerable level. |
| Oksa et al (76) | 2014 | Global | General population, including working population | Not specified | Systematic review | Heat-related illness | The adverse health aspects related to climate change may include heat-related disorders, such as heat stress and respiratory disorders, including those exacerbated by air pollution and aeroallergens, such as asthma. |
| Patz et al (77) | 2013 | Australia | Mining surface | WBGT | Physiological parameters monitoring | Physiological parameters | A significant effect for time was observed for core temperature with greater mean core temperatures measured mid-shift (37.5±0.4°C) and post-shift (37.6±0.3°C) compared with pre-shift values (37.0±0.5°C). |
| Peiffer et al (78) | 2012 | El Salvador | Agriculture | Not specified | Cross-sectional | Physiological parameters | The adjusted ORs of decreased kidney function for 10-year increments of coastal sugarcane or cotton plantation work were 3.1 (95% CI, 2.0-5.0) in men and 2.3 (95% CI, 1.4-3.7) in women. |
| Peraza et al (79) | 2013 | USA (Arizona) | Working population | Not specified | Case-control | Heat-related illness | 75% of HR deaths occurred in men: the age-adjusted ORs for HR death were 2.32 (95% CI 1.55, 3.48) for construction/extraction and 3.50 (95% CI 1.94, 6.32) for agriculture occupations. Men aged ≥ 65 y.o. in agriculture were at especially high risk. |
| Petitti et al (80) | 2011 | Australia | Agriculture | Not specified | Cross-sectional | Mental health | Older farmers faced the same drought-related pressures as their younger peers but these pressures were compounded by the discomforts of ageing and by fighting a losing battle to cope with rapid social and agricultural change. |
| Polain et al (81) | 2013 | Nepal | Manufacturing industry | Heat index, humidity index, and WBGT, based on the HOTHAPS approach | Cross-sectional | Heat-related illness | The average temperature in the summer reached to over 39°C: the environmental conditions were inadequate for workers to work continuously during the day. HRI included fainting, mental irritation, laziness, sleepless nights, dehydration and giddiness. |
| Pradhan et al (82) | 2014 | Nicaragua | Agriculture | Not specified | Cross-sectional with nested case-control analysis | Kidney diseases | Prevalence of GFR <60mL/min/1.73m2 was 10% among women and 42% among men. Risk factors included increased lifetime days cutting sugarcane in the dry season, non-deliberate pesticide inhalation and sugarcane chewing. |
| Raines et al (83) | 2014 | India | Working population | Not specified | Case series | Kidney diseases | Most of the CKD (48.4%) cases were registered relatively high between the months of March and May; most were agricultural workers (24%), construction workers or laborers (23%) and industrial labor workers (19%) who belong to low income group. |
| Raju et al (84) | 2012 | North Carolina | General population, including working population | Daily maximum temperature | Ecological | Heat-related illness | 7.6% of HRI ED visits were work-related. These were more common than other causes in 19-45 year-olds. A threshold ambient maximum daily temperature of 98°F is apparent. The mean daily number of HRI ED visits increased by 1.4 for each 1°F increase from 90°F to 98°F and by 15.8 for each 1°F increase from 98°F to 100°F. Beyond 100°F, the mean number of HRI ED visits decreased with an increasing daily maximum ambient temperature: between 100°F and 102°F, the mean daily number of HRI ED visits decreased by 12.5 for each 1°F increase. |
| Rhea et al (85) | 2016 | Central America | Agriculture | Not specified | Physiological parameters monitoring | Kidney diseases | The presence of urate crystals in the urine and high end-of-workday urinary uric acid concentrations were common. Hyperuricemia may induce glomerular hypertension, whereas the increased urinary uric acid may directly injure renal tubules. |
| Roncal-Jimenez et al (86) | 2013 | India | Agriculture | WBGT | Cross-sectional | Heat-related illness: health complains: pain in different parts of the body, digestive problems, CV problems, other problems (eye, ears, respiratory); Heat concerns (Aware of heat symptoms, discomfort or exhaustion during hottest days) | Most workers reported exhaustion and pain in hot days. Heart rate recovered more slowly at high heat, indicating cardiovascular strain. Peak HR was significantly higher in the air temperature (Ta) ranges of 31-33.5°C (p<0.05) and 35-36°C (p<0.001) than at 28-30°C. The % of resting heart rate also increases with temperature, as do the sum of recovery heartbeats and the cardiac cost variables. |
| Sahu et al (87) | 2014 | India | Manufacturing industry | WBGT | Cross-sectional | Cardiovascular parameters | The cardiac parameters were significantly higher on hotter days for the brick molders. |
| Sett et al (88) | 2015 | Australia | Working population | Not specified | Cross-sectional | Heat-related illness | All interviewees reported that exposure to high temperatures was routine for workers during the summer months, and many reported varying degrees of symptomatology of heat-related illnesses. More than half of respondents (15/20) reported known cases of heat exhaustion in their industry, and several offered that there were frequent episodes each summer amongst the workforce. |
| Singh et al (89) | 2014 | USA (Washington State) | Agriculture - Forestry | Maximum daily temperature (Tmax) and Heat Index (HImax) | Ecological | Heat-related illness | There were 84 HRI claims and 60 citations. HRI claims and citations were most common in crop production and support subsectors; 95% of outdoor claims occurred between May and September, and 84% occurred between June and August. The mean (IQR) Tmax for outdoor HRI claims was 95 (89, 100) °F, and the mean (IQR) HImax was 99 (90, 106) °F. |
| Spector et al (90) | 2010 | Arabian Gulf | Armed force | Ambient Air Temperature | Cohort | Heat-related illness | No cases of heat illness were reported due to employing simple strategies, such as maintaining hydration, rest periods outside of hot workspaces and using cooling techniques. |
| Stevenson et al (91) | 2010 | Thailand | Working population | Not specified | Cross-sectional | Human health | Working under heat stress conditions is associated with worse overall health and psychological distress (aOR ranging from 1.49 to 1.84). The heat stress effects are increased for workers >45 years, the better educated, and for work located in rural areas. |
| Tawatsupa et al (92) | 2012 | Thailand | Working population | Experiences of heat stress derived from survey question | Cross-sectional | Kidney diseases | A significant association between heat stress and incident kidney disease was observed in men (aOR = 1.48, 95% CI: 1.01-2.16). The incidence of kidney disease was even higher among men aged ≥35 years in a physical job. |
| Tawatsupa et al (93) | 2015 | India | Working population | WBGT | Cross-sectional | Heat-related illness | Workplace WBGT > 27 °C was associated with significantly more heat-related symptoms (74%; chi square = 5.152, p = 0.023), as compared to workplaces where WBGT ≤27 °C .Workers with heavy workloads reported more heat-related health issues (chi square = 23.67, p ≤ 0.001) and reduced productivity (chi square =15.82, p ≤ 0.001), especially outdoor workers. Of the workers’ assessed in both hotter and cooler seasons, 65% vs. 32% were exposed to higher than recommended WBGT levels in hotter and cooler seasons respectively. This corresponded to a significant increase in self-reported heat-related health impacts (p = 0.011) as well as an increase of 1.8 °C–4.3 °C WBGT in the hotter season, as compared to the cooler. |
| Venugopal et al (94) | 2016 | India | Agriculture - Manufacturing industry | WBGT | Cross-sectional | Physiological parameters | Avg. WBGT was 30°C. Above normal CBT, Sweat rate (SwR), and USG in about 10% women indicated heat strain and moderate dehydration; those who had no access to proper toilet facilities reported more HR symptoms (n=194) (χ2=4.03, p=0.0444), including dehydration. |
| Venugopal et al (95) | 2003 | Austria | Construction | Not specified | Case report | Heat-related illness | A case of heatstroke-induced acute hepatic failure with complete recovery under conservative management in a 24 year-old male is reported. |
| Wagner et al (96) | 2016 | Nicaragua | Agriculture | Not specified | Physiological parameters monitoring | Kidney diseases | The pre-shift renal function decreased significantly during 9 weeks of work in the cane cutters. Mean serum creatinine increased (20%), mean eGFR decreased (9%, 10mL/min), blood urea nitrogen (BUN) increased (41%), and mean urinary Neutrophil gelatinase-associated lipocalin (NGAL) increased four times. |
| Wesseling 1 et al (97) | 2016 | Nicaragua | Agriculture - Construction | Not specified | Cross-sectional | Kidney diseases | The study found evidence for more frequent heat stress, dehydration and kidney dysfunction among sugarcane cutters, and to a lesser degree also reduced kidney function among construction workers but not among small-scale farmers. |
| Wesseling et al (98) | 2015 | North America | Firefighters | Not specified | Narrative review | Heat-related illness | The trend in fatalities follows that of climate change, with a general upward trend in deaths from the 1980s to the present. |
| Withen (99) | 2014 | Australia | Working population | Daily maximum and minimum temperatures | Time-series | Heat-related illness | The mean Tmax during heat waves was 38.8 °C. Daily claims increased significantly by 6.2% during heatwaves for outdoor industries. Burns, wounds, lacerations, amputations and HRI were significantly associated with heatwaves. |
| Xiang et al (100) | 2014 | Global | Working population | 25 (60%) studies used WGBT, 7 (16%) used subjective heat stress and 6 %14%) used air temperature | Systematic review | Heat-related illness | Manual workers be at risk of heat stress, especially those in LMIC. 79% of identified studies indicated that participants were suffering from heat strain, with outdoor workplaces (90%) being much higher than indoor workplaces (65%). |
| Xiang et al (101) | 2015 | Australia | Working population | Daily maximum temperature (Tmax) | Time series analysis/Case-crossover | Heat-related illness | The overall risk of HRI was positively associated with Tmax, especially when Tmax was over 35.5 °C. 1°C increase of Tmax was associated with a 12.7% increase of occupational heat illness claims. The risk was 4-7 times higher during heatwaves periods. |
| Xiang et al (102) | 2017 | China (Beijing) | General population, including working population | Daily maximum temperature, daily mean relative humidity, and daily mean atmospheric pressure | Ecological | CVD diseases | When the daily maximum temperature was > 33 °C from the 10th consecutive day onward, the excess mortality risk (ER) of CVD death among outdoor workers was 149%, considerably higher than the ER for the overall population (87%; p < 0.05). |
| Yin et al (103) | 2016 | USA (Colorado) | Agriculture | Daily maximum, mean and minimum temperatures, and mean apparent temperature (meAT) | Time-series | CVD diseases | Estimates of heat effects on average daily clinic visits among migrant farm workers were positive (88.0%, 95% CI: 26.2% to 180.0%). Authors did not observe statistically significant associations between heat and clinic visits among other groups. |
References
- 1.Adam-Poupart A, Smargiassi A, Busque MA, Duguay P, Fournier M, Zayed J, et al. Summer outdoor temperature and occupational heat-related illnesses in Quebec (Canada) Environ Res [Internet]. Elsevier. 2014;134:339–44. doi: 10.1016/j.envres.2014.07.018. Available from: http://dx.doi.org/10.1016/j.envres.2014.07.018 . [DOI] [PubMed] [Google Scholar]
- 2.Adam-Poupart A, Labreche F, Busque MA, Brand A, Duguay P, Fournier M, et al. Association between outdoor ozone and compensated acute respiratory diseases among workers in Quebec (Canada) Ind Health [Internet] 2015;53:171–5. doi: 10.2486/indhealth.2014-0136. Available from: http://dx.doi.org/10.2486/indhealth.2014-0136 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arbury S, Jacklitsch B, Farquah O, Hodgson M, Lamson G, Martin H, et al. Heat illness and death among workers - United States, 2012-2013. MMWR Morb Mortal Wkly Rep [Internet] 2014 Aug 8;63(31):661–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25102413 . [PMC free article] [PubMed] [Google Scholar]
- 4.Arcury TA, Summers P, Talton JW, Chen H, Sandberg JC, Spears Johnson CR, et al. Heat Illness Among North Carolina Latino Farmworkers. J Occup Environ Med [Internet] 2015 Dec;57(12):1299–304. doi: 10.1097/JOM.0000000000000552. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00043764-201512000-00007 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balbus John M, Malina Catherine M. Identifying Vulnerable Subpopulations for Climate Change Health Effects in the United States. J Occup Environ Med. 2009;51(1):33–7. doi: 10.1097/JOM.0b013e318193e12e. [DOI] [PubMed] [Google Scholar]
- 6.Bates GP, Schneider J. Hydration status and physiological workload of UAE construction workers: A prospective longitudinal observational study. J Occup Med Toxicol [Internet] 2008;3:21. doi: 10.1186/1745-6673-3-21. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2561022&tool=pmcentrez&rendertype=abstract . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bates GP, Miller VS, Joubert DM. Hydration status of expatriate manual workers during summer in the Middle East. Ann Occup Hyg. 2010;54(2):137–43. doi: 10.1093/annhyg/mep076. [DOI] [PubMed] [Google Scholar]
- 8.Bedno SA, Urban N, Boivin MR, Cowan DN. Fitness, obesity and risk of heat illness among army trainees. Occup Med (Chic Ill) 2014;64(6):461–7. doi: 10.1093/occmed/kqu062. [DOI] [PubMed] [Google Scholar]
- 9.Berry HL, Hogan A, Owen J, Rickwood D, Fragar L. Climate Change and Farmers’ Mental Health: Risks and Responses. Asia-Pacific J Public Heal [Internet] 2011;23(2 Suppl):119S–132S. doi: 10.1177/1010539510392556. Available from: http://aph.sagepub.com/cgi/doi/10.1177/1010539510392556 . [DOI] [PubMed] [Google Scholar]
- 10.Bethel JW, Harger R. Heat-related illness among Oregon farmworkers. Int J Environ Res Public Health. 2014;11(9):9273–85. doi: 10.3390/ijerph110909273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biswas R, Saha P, Samanta A. Cardiac strain of confectionery worker in relation to heat exposure during regular work shift. Indian J Occup Environ Med [Internet] 2011;15(3):120. doi: 10.4103/0019-5278.93202. Available from: http://www.ijoem.com/text.asp?2011/15/3/120/93202 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bodin T, Garcia-Trabanino R, Weiss I, Jarquin E, Glaser J, Jakobsson K, et al. Intervention to reduce heat stress and improve efficiency among sugarcane workers in El Salvador: Phase 1. Occup Environ Med [Internet] 2016 doi: 10.1136/oemed-2016-103555. oemed-2016-103555. Available from: http://oem.bmj.com/lookup/doi/10.1136/oemed-2016-103555 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bonauto D, Anderson R, Rauser E, Burke B. Occupational Heat Illness in Washington State, 1995 – 2005. Am J Ind Med. 2007;950(50):1995–2005. doi: 10.1002/ajim.20517. [DOI] [PubMed] [Google Scholar]
- 14.Boodosingh DR, Robles-Arias C, Aleman-Ortiz JR, Rodriguez-Cintron W. A rare cause of altered mental status and fever in a young military recruit in Puerto Rico. P R Health Sci J. 2014;33(4):200–2. [PubMed] [Google Scholar]
- 15.Brake DJ, Bates GP. Fluid losses and hydration status of industrial workers under thermal stress working extended shifts. Occup Environ Med [Internet] 2003;60(2):90–6. doi: 10.1136/oem.60.2.90. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1740457&tool=pmcentrez&rendertype=abstract . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bray P. Heat-Related Illnesses: Opportunities for Prevention. J Occup Environ Med. 2010;52(8):844–5. doi: 10.1097/JOM.0b013e3181ed4c36. [DOI] [PubMed] [Google Scholar]
- 17.Brearley M, Harrington P, Lee D, Taylor R. Working in Hot Conditions—A Study of Electrical Utility Workers in the Northern Territory of Australia. J Occup Environ Hyg [Internet] 2015 Mar 4;12(3):156–62. doi: 10.1080/15459624.2014.957831. Available from: http://www.tandfonline.com/doi/full/10.1080/15459624.2014.957831 . [DOI] [PubMed] [Google Scholar]
- 18.Clark PA, Chowdhury J, Chan B, Radigan N. Chronic kidney disease in Nicaraguan sugarcane workers: A historical, medical, environmental analysis and ethical analysis. Internet J Third World Med [Internet] 2016;12(1):1–16. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed18b&AN=613372262%5Cnhttps://www.mobilelibrary.com/vlib/orde r/OpenURLReceive.aspx?sid=OVID:embase&id=pmid:&id=doi:10.5580%2FIJWH.39545&issn=1539-4646&isbn=&volume=12&issue=1&spage=no+ [Google Scholar]
- 19.Crowe J, Nilsson M, Kjellstrom T, Wesseling C. Heat-Related symptoms in sugarcane harvesters. Am J Ind Med. 2015;58(5):541–8. doi: 10.1002/ajim.22450. [DOI] [PubMed] [Google Scholar]
- 20.Cortez OD. Heat stress assessment among workers in a Nicaraguan sugarcane farm. Glob Health Action. 2009;2(1):1–6. doi: 10.3402/gha.v2i0.2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.D’Ovidio MC, Annesi-Maesano I, D’Amato G, Cecchi L. Climate change and occupational allergies: an overview on biological pollution, exposure and prevention. Ann Ist Super Sanita [Internet] 52(3):406–14. doi: 10.4415/ANN_16_03_12. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27698299 . [DOI] [PubMed] [Google Scholar]
- 22.Dutta P, Rajiva A, Andhare D, Azhar G, Tiwari A, Sheffield P, et al. Perceived heat stress and health effects on construction workers. Indian J Occup Environ Med [Internet] 2015;19(3):151. doi: 10.4103/0019-5278.174002. Available from: http://www.ijoem.com/text.asp?2015/19/3/151/174002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Edwards B, Gray M, Hunter B. The Impact of Drought on Mental Health in Rural and Regional Australia. Soc Indic Res. 2015;121(1):177–94. [Google Scholar]
- 24.Ellis NR, Albrecht GA. Climate change threats to family farmers’ sense of place and mental wellbeing: A case study from the Western Australian Wheatbelt. Soc Sci Med [Internet]. Elsevier Ltd. 2017;175:161–8. doi: 10.1016/j.socscimed.2017.01.009. Available from: http://dx.doi.org/10.1016/j.socscimed.2017.01.009 . [DOI] [PubMed] [Google Scholar]
- 25.Farshad A, Montazer S, Monazzam MR, Eyvazlou M, Mirkazemi R. Heat stress level among construction workers. Iran J Public Health. 2014;43(4):492–8. [PMC free article] [PubMed] [Google Scholar]
- 26.Fleischer NL, Tiesman HM, Sumitani J, Mize T, Amarnath KK, Bayakly AR, et al. Public health impact of heat-related illness among migrant farmworkers. Am J Prev Med [Internet]. Elsevier Inc. 2013;44(3):199–206. doi: 10.1016/j.amepre.2012.10.020. Available from: http://dx.doi.org/10.1016/j.amepre.2012.10.020 . [DOI] [PubMed] [Google Scholar]
- 27.Fortune MK, Mustard CA, Etches JJC, Chambers AG. Work-attributed illness arising from excess heat exposure in Ontario, 2004-2010. Can J Public Heal. 2013;104(5):2004–10. doi: 10.17269/cjph.104.3984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fortune M, Mustard C, Brown P. The use of Bayesian inference to inform the surveillance of temperature-related occupational morbidity in Ontario, Canada, 2004-2010. Environ Res [Internet]. Elsevier. 2014;132:449–56. doi: 10.1016/j.envres.2014.04.022. Available from: http://dx.doi.org/10.1016/j.envres.2014.04.022 . [DOI] [PubMed] [Google Scholar]
- 29.Fuhrmann CM, Sugg MM, Konrad CE, Waller A. Impact of Extreme Heat Events on Emergency Department Visits in North Carolina (2007–2011) J Community Health. Springer US. 2016;41(1):146–56. doi: 10.1007/s10900-015-0080-7. [DOI] [PubMed] [Google Scholar]
- 30.Barbosa CMG, Terra-Filho M, de Albuquerque ALP, Di Giorgi D, Grupi C, Negrao CE, et al. Burnt Sugarcane Harvesting - Cardiovascular Effects on a Group of Healthy Workers, Brazil. PLoS One. 2012;7(9):1–10. doi: 10.1371/journal.pone.0046142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garcia-Trabanino R, Jarquin E, Wesseling C, Johnson RJ, Gonzalez-Quiroz M, Weiss I, et al. Heat stress, dehydration, and kidney function in sugarcane cutters in El Salvador - A cross-shift study of workers at risk of Mesoamerican nephropathy. Environ Res [Internet]. Elsevier. 2015;142:746–55. doi: 10.1016/j.envres.2015.07.007. Available from: http://dx.doi.org/10.1016/j.envres.2015.07.007 . [DOI] [PubMed] [Google Scholar]
- 32.Garzon-Villalba XP, Mbah A, Wu Y, Hiles M, Moore H, Schwartz SW, et al. Exertional heat illness and acute injury related to ambient wet bulb globe temperature. Am J Ind Med. 2016;59(12):1169–76. doi: 10.1002/ajim.22650. [DOI] [PubMed] [Google Scholar]
- 33.Gubernot DM, Anderson GB, Hunting KL. The epidemiology of occupational heat exposure in the United States: a review of the literature and assessment of research needs in a changing climate. Int J Biometeorol [Internet] 2014 Oct 11;58(8):1779–88. doi: 10.1007/s00484-013-0752-x. Available from: http://link.springer.com/10.1007/s00484-013-0752-x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gubernot DM, Anderson GB, Hunting KL. Characterizing occupational heat-related mortality in the United States, 2000-2010: An analysis using the census of fatal occupational injuries database. Am J Ind Med. 2015;58(2):203–11. doi: 10.1002/ajim.22381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hanigan IC, Butler CD, Kokic PN, Hutchinson MF. Suicide and drought in New South Wales, Australia, 1970-2007. Proc Natl Acad Sci. 2012;109(35):13950. doi: 10.1073/pnas.1112965109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hanna EG, Kjellstrom T, Bennett C, Dear K. Climate Change and Rising Heat: Population Health Implications for Working People in Australia. Asia-Pacific J Public Heal [Internet] 2011 Mar 1;23(2 Suppl):14S–26S. doi: 10.1177/1010539510391457. Available from: http://aph.sagepub.com/cgi/doi/10.1177/1010539510391457 . [DOI] [PubMed] [Google Scholar]
- 37.Harari Arjona R, Pineiros J, Ayabaca M, Harari Freire F. Climate change and agricultural workers’ health in Ecuador: occupational exposure to UV radiation and hot environments. Ann Ist Super Sanita [Internet] 52(3):368–73. doi: 10.4415/ANN_16_03_08. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27698295 . [DOI] [PubMed] [Google Scholar]
- 38.Harduar Morano L, Bunn TL, Lackovic M, Lavender A, Dang GTT, Chalmers JJ, et al. Occupational heat-related illness emergency department visits and inpatient hospitalizations in the southeast region, 2007-2011. Am J Ind Med. 2015;58(10):1114–25. doi: 10.1002/ajim.22504. [DOI] [PubMed] [Google Scholar]
- 39.Harduar Morano L, Watkins S, Kintziger K. A Comprehensive Evaluation of the Burden of Heat-Related Illness and Death within the Florida Population. Int J Environ Res Public Health [Internet] 2016 May 31;13(6):551. doi: 10.3390/ijerph13060551. Available from: http://www.mdpi.com/1660-4601/13/6/551 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Harduar Morano L, Watkins S. Evaluation of Diagnostic Codes in Morbidity and Mortality Data Sources for Heat-Related Illness Surveillance. Public Health Rep [Internet] 2017;132(3):326–35. doi: 10.1177/0033354917699826. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28379784%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC5415256%5Cnhttp://journals.sag epub.com/doi/10.1177/0033354917699826 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Holmes NA, Miller VS, Schneider J, Hasan O, Bates GP. Plasma sodium levels and dietary sodium intake in manual workers in the middle east. Ann Occup Hyg. 2011;55(4):397–402. doi: 10.1093/annhyg/mer004. [DOI] [PubMed] [Google Scholar]
- 42.Hunt AP, Parker AW, Stewart IB. Symptoms of heat illness in surface mine workers. Int Arch Occup Environ Health. 2013;86(5):519–27. doi: 10.1007/s00420-012-0786-0. [DOI] [PubMed] [Google Scholar]
- 43.Hunt AP, Parker AW, Stewart IB. Heat strain and hydration status of surface mine blast crew workers. J Occup Environ Med [Internet] 2014;56(4):409–14. doi: 10.1097/JOM.0000000000000114. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24504322 . [DOI] [PubMed] [Google Scholar]
- 44.Inaba R, Kurokawa J, Mirbod SM. Comparison of subjective symptoms and cold prevention measures in winter between traffic control workers and construction workers in Japan. Ind Health. 2009;47(3):283–91. doi: 10.2486/indhealth.47.283. [DOI] [PubMed] [Google Scholar]
- 45.Jackson LL, Rosenberg HR. Preventing heat-related illness among agricultural workers. J Agromedicine. 2010 15(April):200–15. doi: 10.1080/1059924X.2010.487021. [DOI] [PubMed] [Google Scholar]
- 46.Jia YA, Rowlinson S, Ciccarelli M. Climatic and psychosocial risks of heat illness incidents on construction site. Appl Ergon [Internet]. Elsevier Ltd. 2016;53:25–35. doi: 10.1016/j.apergo.2015.08.008. Available from: http://dx.doi.org/10.1016/j.apergo.2015.08.008 . [DOI] [PubMed] [Google Scholar]
- 47.Joubert D, Thomsen J, Harrison O. Safety in the heat: A comprehensive program for prevention of heat illness among workers in Abu Dhabi, United Arab Emirates. Am J Public Health. 2011;101(3):395–8. doi: 10.2105/AJPH.2009.189563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kearney GD, Hu H, Xu X, Hall M, Balanay JA. Estimating the Prevalence of Heat-Related Symptoms and Sun Safety Related Behavior among Latino Farmworkers in Eastern North Carolina. J Agromedicine [Internet] 2015 813(April):15–23. doi: 10.1080/1059924X.2015.1106377. Available from: http://dx.doi.org/10.1080/1059924X.2015.1106377 . [DOI] [PubMed] [Google Scholar]
- 49.Kenefick RW, Sawka MN. Hydration at the work site. J Am Coll Nutr. 2007;26(5 Suppl):597S–603S. doi: 10.1080/07315724.2007.10719665. [DOI] [PubMed] [Google Scholar]
- 50.Kjellstrom T, Holmer I, Lemke B. Workplace heat stress, health and productivity-an increasing challenge for low and middle-income countries during climate change. Glob Health Action. 2009;2(1):1–6. doi: 10.3402/gha.v2i0.2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kjellstrom T, Crowe J. Climate Change, Workplace Heat Exposure, and Occupational Health and Productivity in Central America. Int J Occup Environ Health [Internet] 2011 Jul;17(3):270–81. doi: 10.1179/107735211799041931. Available from: http://www.tandfonline.com/doi/full/10.1179/107735211799041931 . [DOI] [PubMed] [Google Scholar]
- 52.Kjellstrom T, Briggs D, Freyberg C, Lemke B, Otto M, Hyatt O. Heat, Human Performance, and Occupational Health: A Key Issue for the Assessment of Global Climate Change Impacts. Annu Rev Public Health [Internet] 2016 Mar 18;37(1):97–112. doi: 10.1146/annurev-publhealth-032315-021740. Available from: http://www.annualreviews.org/doi/10.1146/annurev-publhealth-032315-021740 . [DOI] [PubMed] [Google Scholar]
- 53.Krake A, McCullough J, King B. Health Hazards to Park Rangers from Excessive Heat at Grand Canyon National Park. Appl Occup Environ Hyg [Internet] 2003 May;18(5):295–317. doi: 10.1080/10473220301364. Available from: http://www.tandfonline.com/doi/abs/10.1080/10473220301364 . [DOI] [PubMed] [Google Scholar]
- 54.Kravchenko J, Abernethy AP, Fawzy M, Lyerly HK. Minimization of heatwave morbidity and mortality. Am J Prev Med [Internet]. Elsevier Inc. 2013;44(3):274–82. doi: 10.1016/j.amepre.2012.11.015. Available from: http://dx.doi.org/10.1016/j.amepre.2012.11.015 . [DOI] [PubMed] [Google Scholar]
- 55.Lao J, Hansen A, Nitschke M, Hanson-Easey S, Pisaniello D. Working smart: An exploration of council workers’ experiences and perceptions of heat in Adelaide, South Australia. Saf Sci [Internet]. Elsevier Ltd. 2016;82:228–35. Available from: http://dx.doi.org/10.1016/j.ssci.2015.09.026 . [Google Scholar]
- 56.Laws RL, Brooks DR, Amador JJ, Weiner DE, Kaufman JS, Ramirez-Rubio O, et al. Biomarkers of Kidney Injury among Nicaraguan Sugarcane Workers. Am J Kidney Dis. 2016;67(2):209–17. doi: 10.1053/j.ajkd.2015.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lundgren K, Kuklane K, Gao C, Holmer I. Effects of heat stress on working populations when facing climate change. Ind Health [Internet] 2013;51(1):3–15. doi: 10.2486/indhealth.2012-0089. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23411752 . [DOI] [PubMed] [Google Scholar]
- 58.Lundgren K, Kuklane K, Venugopal V. Occupational heat stress and associated productivity loss estimation using the PHS model (ISO 7933): A case study from workplaces in Chennai, India. Glob Health Action. 2014;7(1):1–9. doi: 10.3402/gha.v7.25283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lunyera J, Mohottige D, von Isenburg M, Jeuland M, Patel UD, Stanifer JW. CKD of uncertain etiology: A systematic review. Clin J Am Soc Nephrol. 2016;11(3):379–85. doi: 10.2215/CJN.07500715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Luo H, Turner LR, Hurst C, Mai H, Zhang Y, Tong S. Exposure to ambient heat and urolithiasis among outdoor workers in Guangzhou, China. Sci Total Environ [Internet]. Elsevier B.V. 2014;472:1130–6. doi: 10.1016/j.scitotenv.2013.11.042. Available from: http://dx.doi.org/10.1016/j.scitotenv.2013.11.042 . [DOI] [PubMed] [Google Scholar]
- 61.Maeda T, Kaneko SY, Ohta M, Tanaka K, Sasaki A, Fukushima T. Risk factors for heatstroke among Japanese forestry workers. J Occup Health. 2006;48(4):223–9. doi: 10.1539/joh.48.223. [DOI] [PubMed] [Google Scholar]
- 62.Marchetti E, Capone P, Freda D. Climate change impact on microclimate of work environment related to occupational health and productivity. Ann Ist Super Sanita [Internet] 2016;52(3):338–42. doi: 10.4415/ANN_16_03_05. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27698292 . [DOI] [PubMed] [Google Scholar]
- 63.Mathee A, Oba J, Rose A. Climate change impacts on working people (the HOTHAPS initiative): findings of the South African pilot study Angela. Glob Health Action. 2010;3(5612):1–9. doi: 10.3402/gha.v3i0.5612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mbanu I, Wellenius GA, Mittleman MA, Peeples L, Stallings LA, Kales SN. NIH Public Access. 2013;24(4):715–26. doi: 10.1080/07420520701535787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Meade RD, Lauzon M, Poirier MP, Flouris AD, Kenny GP. An Evaluation of the Physiological Strain Experienced by Electrical Utility Workers in North America. J Occup Environ Hyg [Internet] 2015;12(10):708–20. doi: 10.1080/15459624.2015.1043054. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26011148 . [DOI] [PubMed] [Google Scholar]
- 66.Mirabelli MC, Richardson DB. Heat-related fatalities in North Carolina. Am J Public Health. 2005;95(4):635–7. doi: 10.2105/AJPH.2004.042630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mirabelli MC, Quandt SA, Crain R, Grzywacz JG, Robinson EN, Vallejos QM, et al. Symptoms of heat illness among Latino farm workers in North Carolina. Am J Prev Med [Internet]. Elsevier Inc. 2010;39(5):468–71. doi: 10.1016/j.amepre.2010.07.008. Available from: http://dx.doi.org/10.1016/j.amepre.2010.07.008 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Centers for Disease Control and Prevention (CDC) Heat-related deaths among crop workers-United States, 1992-2006. MMWR Morb Mortal Wkly Rep [Internet] 2008 Jun 20;57(24):649–53. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18566563 . [PubMed] [Google Scholar]
- 69.Montazer S, Farshad AA, Monazzam MR, Eyvazlou M, Yaraghi AAS, Mirkazemi R. Assessment of construction workers’ hydration status using urine specific gravity. Int J Occup Med Environ Health [Internet] 2013;26(5):762–9. doi: 10.2478/s13382-013-0143-x. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24464540 . [DOI] [PubMed] [Google Scholar]
- 70.Morioka I, Miyai N, Miyashita K. Hot environment and health problems of outdoor workers at a construction site. Ind Health. 2006;44(3):474–80. doi: 10.2486/indhealth.44.474. [DOI] [PubMed] [Google Scholar]
- 71.Moyce S, Mitchell D, Armitage T, Tancredi D, Joseph J, Schenker M. Heat strain, volume depletion and kidney function in California agricultural workers. Occup Environ Med [Internet] 2017 doi: 10.1136/oemed-2016-103848. d:oemed-2016-103848. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28093502 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Armed Forces Health Surveillance Center (AFHSC) Update: heat injuries, active component, U.S. Armed Forces, 2010. MSMR [Internet] 2011 Mar;18(3):6–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21793607 . [Google Scholar]
- 73.Armed Forces Health Surveillance Branch. Update: Heat injuries, active component, U.S. Army, Navy, Air Force, and Marine Corps, 2015. MSMR [Internet] 2016 Mar;23(3):16–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27030928 . [PubMed] [Google Scholar]
- 74.Nayha S, Rintamaki H, Donaldson G, Hassi J, Jousilahti P, Laatikainen T, et al. The prevalence of heat-related cardiorespiratory symptoms: the vulnerable groups identified from the National FINRISK 2007 Study. Int J Biometeorol [Internet]. International Journal of Biometeorology. 2017;61(4):657–68. doi: 10.1007/s00484-016-1243-7. Available from: http://link.springer.com/10.1007/s00484-016-1243-7 . [DOI] [PubMed] [Google Scholar]
- 75.Nevarez J. OSHA Compliance Issues. J Occup Environ Hyg [Internet] 2013 Jun;10(6):D67–70. doi: 10.1080/15459624.2013.784177. Available from: http://www.tandfonline.com/doi/abs/10.1080/15459624.2013.784177 . [DOI] [PubMed] [Google Scholar]
- 76.Oksa J, Hosio S, Makinen T, Lindholm H, Rintamaki H, Rissanen S, et al. Muscular, cardiorespiratory and thermal strain of mast and pole workers. Ergonomics [Internet] 2014 May 4;57(5):669–78. doi: 10.1080/00140139.2014.895854. Available from: http://www.tandfonline.com/doi/abs/10.1080/00140139.2014.895854 . [DOI] [PubMed] [Google Scholar]
- 77.Patz JA, Frumkin H, Holloway T, Vimont DJ, Haines A. Climate Change. Jama [Internet] 2014;312(15):1565. doi: 10.1001/jama.2014.13186. Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2014.13186 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Peiffer JJ, Abbiss CR. Thermal stress in North Western Australian iron ore mining staff. Ann Occup Hyg. 2013;57(4):519–27. doi: 10.1093/annhyg/mes084. [DOI] [PubMed] [Google Scholar]
- 79.Peraza S, Wesseling C, Aragon A, Leiva R, Garcia-Trabanino RA, Torres C, et al. Decreased kidney function among agricultural workers in El Salvador. Am J Kidney Dis [Internet]. Elsevier Inc. 2012;59(4):531–40. doi: 10.1053/j.ajkd.2011.11.039. Available from: http://dx.doi.org/10.1053/j.ajkd.2011.11.039 . [DOI] [PubMed] [Google Scholar]
- 80.Petitti DB, Harlan SL, Chowell-Puente G, Ruddell D. Occupation and Environmental Heat-Associated Deaths in Maricopa County, Arizona: A Case-Control Study. PLoS One. 2013;8(5) doi: 10.1371/journal.pone.0062596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Polain JD, Berry HL, Hoskin JO. Rapid change, climate adversity and the next “big dry”: Older farmers’ mental health. Aust J Rural Health. 2011;19(5):239–43. doi: 10.1111/j.1440-1584.2011.01219.x. [DOI] [PubMed] [Google Scholar]
- 82.Pradhan B, Shrestha S, Shrestha R, Pradhanang S, Kayastha B, Pradhan P. Assessing climate change and heat stress responses in the Tarai region of Nepal. Ind Health [Internet] 2013;51(1):101–12. doi: 10.2486/indhealth.2012-0166. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23411760 . [DOI] [PubMed] [Google Scholar]
- 83.Raines N, Gonzalez Quiroz M, Wyatt C, Kurzrok M, Pool C, Lemma T, et al. Risk factors for reduced glomerular filtration rate in a nicaraguan community affected by mesoamerican nephropathy. MEDICC Rev [Internet] 2014;16(2):16–22. doi: 10.37757/MR2014.V16.N2.4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24878645 . [DOI] [PubMed] [Google Scholar]
- 84.Raju DSSK, Kiranmayi P, Vijaya Rachel K. Climate change and chronic kidney disease. Asian J Pharm Clin Res [Internet] 2014;7(2):53–7. Available from: http://innovareacademics.in/journals/index.php/ajpcr/article/download/953/615%5Cnhttp://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=em ed12&NEWS=N&AN=2014240557 . [Google Scholar]
- 85.Rhea S, Ising A, Fleischauer AT, Deyneka L, Vaughan-Batten H, Waller A. Using near real-time morbidity data to identify heat-related illness prevention strategies in North Carolina. J Community Health. 2012;37(2):495–500. doi: 10.1007/s10900-011-9469-0. [DOI] [PubMed] [Google Scholar]
- 86.Roncal-Jimenez C, Garcia-Trabanino R, Barregard L, Lanaspa MA, Wesseling C, Harra T, et al. Heat Stress Nephropathy from Exercise-Induced Uric Acid Crystalluria: A Perspective on Mesoamerican Nephropathy. Am J Kidney Dis. 2016;67(1):20–30. doi: 10.1053/j.ajkd.2015.08.021. [DOI] [PubMed] [Google Scholar]
- 87.Sahu S, Sett M, Kjellstrom T. Heat exposure, cardiovascular stress and work productivity in rice harvesters in India: implications for a climate change future. Ind Health [Internet] 2013;51(4):424–31. doi: 10.2486/indhealth.2013-0006. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23685851 . [DOI] [PubMed] [Google Scholar]
- 88.Sett M, Sahu S. Effects of occupational heat exposure on female brick workers in West Bengal, India. Glob Health Action. 2014;7(1):1–11. doi: 10.3402/gha.v7.21923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Singh S, Hanna EG, Kjellstrom T. Working in Australia’s heat: Health promotion concerns for health and productivity. Health Promot Int. 2015;30(2):239. doi: 10.1093/heapro/dat027. [DOI] [PubMed] [Google Scholar]
- 90.Spector JT, Krenz J, Rauser E, Bonauto DK. Heat-related illness in Washington State agriculture and forestry sectors. Am J Ind Med. 2014;57(8):881–95. doi: 10.1002/ajim.22357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Stevenson T, Roiz de Sa D. Managing the risk of heat illness on board type 23 frigates deploying to the Arabian Gulf. J R Nav Med Serv. 2010;96(3):150–7. [PubMed] [Google Scholar]
- 92.Tawatsupa B, Lim LL-Y, Kjellstrom T, Seubsman S-A, Sleigh A. The Thai Cohort Study Team. The association between overall health, psychological distress, and occupational heat stress among a large national cohort of 40,913 Thai workers. Glob Health Action. 2010;3(9):1–10. doi: 10.3402/gha.v3i0.5034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Tawatsupa B, Lim LL-Y, Kjellstrom T, Seubsman S, Sleigh A. Study Team the TC. Association Between Occupational Heat Stress and Kidney Disease Among 37 816 Workers in the Thai Cohort Study (TCS) J Epidemiol [Internet] 2012;22(3):251–60. doi: 10.2188/jea.JE20110082. Available from: http://japanlinkcenter.org/JST.JSTAGE/jea/JE20110082?from=CrossRef&type=abstract . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Venugopal V, Chinnadurai JS, Lucas RAI, Kjellstrom T. Occupational heat stress profiles in selected workplaces in India. Int J Environ Res Public Health. 2015;13(1):1–13. doi: 10.3390/ijerph13010089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Venugopal V, Rekha S, Manikandan K, Latha PK, Vennila V, Ganesan N, et al. Heat stress and inadequate sanitary facilities at workplaces an occupational health concern for women. Glob Health Action. 2016;1(March 2017):1–9. doi: 10.3402/gha.v9.31945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wagner M, Kaufmann P, Fickert P, Trauner M, Lackner C, Stauber RE. Successful conservative management of acute hepatic failure following exertional heatstroke. Eur J Gastroenterol Hepatol [Internet] 2003;15(10):1135–9. doi: 10.1097/00042737-200310000-00013. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14501625 . [DOI] [PubMed] [Google Scholar]
- 97.Wesseling C, Aragon A, Gonzalez M, Weiss I, Glaser J, Bobadilla NA, et al. Kidney function in sugarcane cutters in Nicaragua - A longitudinal study of workers at risk of Mesoamerican nephropathy. Environ Res [Internet]. Elsevier. 2016;147:125–32. doi: 10.1016/j.envres.2016.02.002. Available from: http://dx.doi.org/10.1016/j.envres.2016.02.002 . [DOI] [PubMed] [Google Scholar]
- 98.Wesseling C, Aragon A, Gonzalez M, Weiss I, Glaser J, Rivard CJ, et al. Heat stress, hydration and uric acid: a cross-sectional study in workers of three occupations in a hotspot of Mesoamerican nephropathy in Nicaragua. BMJ Open [Internet] 2016;6(12):e011034. doi: 10.1136/bmjopen-2016-011034. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27932336%0Ahttp://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2016-011034 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Withen P. Climate change and wildland firefighter health and safety. New Solut a J Environ Occup Heal policy. 2015;24(4):577–84. doi: 10.2190/NS.24.4.i. [DOI] [PubMed] [Google Scholar]
- 100.Xiang J, Bi P, Pisaniello D, Hansen A. The impact of heatwaves on workers’ health and safety in Adelaide, South Australia. Environ Res [Internet]. Elsevier. 2014;133:90–5. doi: 10.1016/j.envres.2014.04.042. Available from: http://europepmc.org/abstract/med/24906072%5Cnhttp://www.ncbi.nlm.nih.gov/pubmed/24906072 . [DOI] [PubMed] [Google Scholar]
- 101.Xiang J, Bi P, Pisaniello D, Hansen A. Health impacts of workplace heat exposure: An epidemiological review. Ind Health [Internet] 2014;52(2):91–101. doi: 10.2486/indhealth.2012-0145. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24366537 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Xiang J, Hansen A, Pisaniello D, Bi P. Extreme heat and occupational heat illnesses in South Australia, 2001-2010. Occup Environ Med [Internet] 2015;72(8):580–6. doi: 10.1136/oemed-2014-102706. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26081622 . [DOI] [PubMed] [Google Scholar]
- 103.Yin Q, Wang J. The association between consecutive days’ heat wave and cardiovascular disease mortality in Beijing, China. BMC Public Health [Internet]. BMC Public Health. 2017;17(1):223. doi: 10.1186/s12889-017-4129-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28228117%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC5322604 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhang K, Arauz RF, Chen T-H, Cooper SP. Heat effects among migrant and seasonal farmworkers: a case study in Colorado. Occup Environ Med. 2016;73(5):324–8. doi: 10.1136/oemed-2015-103332. [DOI] [PubMed] [Google Scholar]
Appendix Table 6.
Papers selected using the second search strategy
| Papers selected using search strategy N.2 | ||||||
| Paper | Year | Country/Region | Population | Heat exposure index | Study design | Main results |
| Adam-Poupart 1 et al (1) | 2015 | Canada | Working population | Maximum daily outdoor temperature | Ecological | The relationship between daily counts of compensations and maximum daily temperatures reached statistical significance for three health regions. The incidence rate ratio of daily compensations per 1°C increase was 1.002 (95%CI 1.002 to 1.003). |
| Bonafede et al (2) | 2016 | Global | Working population | Daily maximum temperature daily mean temperature or apparent temperature | Systematic review | Only 2 studies analysed the dose-response relationship between temperature and the health outcomes finding a reversed U-shaped exposure-response relationship, or linear relationship or linear above/below a threshold. |
| Dutta et al (3) | 2015 | India | Construction | WBGT | Cross-sectional | Injuries reported in summer were among workers with < 36 months of experience. |
| Garzon-Villalba et al (4) | 2016 | USA | Working population | WBGTmax | Incidence | Acute injuries (AI) were higher in workers exposed above a WBGTmax of 20°C (RR 1.06/°C). The unadjusted model showed a 13% increment in risk to experience an AI when the ambient thermal conditions increase 1°C-WBGT. |
| McInnes et al (5) | 2017 | Australia | Working population | Maximum daily temperature and minimum daily temperature (minimum temperature during the night before the day of injury) | Case-crossover | Significant positive associations between temperature and acute injury were seen for younger workers, with the odds of injury increasing by 1% for each 1°C increase in daily minimum temperature, and by 0.8% for each 1°C increase in daily maximum temperature. |
| Morabito et al (6) | 2006 | Italy (Tuscany) | Working population | Apparent temperature (AT) AT max, AT24 and AT day were assessed | Ecological | The peak of work-related accidents occurred on days characterized by high, but not extreme, thermal conditions. The maximum peak of work accidents in each month occurred on days characterized by a mean ATday ranging between 24.8°C and 27.5 °C. |
| Nag et al (7) | 2001 | India | Manufacturing industry | Ambient temperature | Case surveillance | Accident prevalence was significantly high in the summer months (May-June) when the ambient temperature ranged between 42 and 48°C (hot-dry). Permanent night workers were more vulnerable and less tolerant to heat compared to the rotating day workers. |
| Otte-im-Kampe et al (8) | 2016 | High-income countries | General population, including working population | Not specified | Systematic review | Two out of 3 studies found an increase in work-related accidents during increased temperatures; the other reported no association. |
| Rameezdeen et al (9) | 2017 | Australia | Construction | Daily maximum and minimum temperatures | Case-crossover | The number of accidents reported during heat wave periods was less compared to control periods, suggesting some control measures are in operation in construction sites to prevent accidents during heat waves |
| Spector et al (10) | 2016 | USA | Agriculture | Maximum daily humidex exposures | Case-crossover | The traumatic injury OR was 1.14 (95% CI 1.06, 1.22), 1.15 (95% CI 1.06, 1.25), and 1.10 (95% CI 1.01, 1.20) for daily maximum humidex of 25±29, 30±33, and ≥34, respectively, compared to < 25, adjusted for self-reported duration of employment. |
| Tawatsupa et al (11) | 2013 | Thailand | Working population | Experiences of heat stress derived from survey question | Cohort | Nearly 20% of workers experienced occupational heat stress, which strongly and significantly associated with occupational injury (adjusted OR 2.12, 95%CI 1.87-2.42 for males and 1.89, 95%CI 1.64-2.18 for females). |
| Withen (12) | 2015 | North America | Firefighters | Not specified | Narrative review | The trend in fatalities follows that of climate change, with a general upward trend in deaths from the 1980s to the present. |
| Xiang et al (13) | 2014 | Australia | Working population | Daily maximum temperature | Ecological | A reversed U-shaped exposure-response relationship between Tmax and overall daily injury claims was observed. Overall, a 1°C increase in maximum temperature between 14.2°C and 37.7°C was associated with a 0.2% increase in daily injury claims. |
| Xiang et al (14) | 2014 | Australia | Working population | Daily maximum and minimum temperatures | Time-series | The mean Tmax during heat waves was 38.8 °C. Daily claims increased significantly by 6.2% during heatwaves for outdoor industries. Burns, wounds, lacerations, amputations and HRI were significantly associated with heatwaves. |
| Xiang et al (15) | 2014 | Global | Working population | 25 (60%) studies used WGBT, 7 (16%) used subjective heat stress and 6 %14%) used air temperature | Systematic review | Manual workers are at risk of heat stress, especially those in LMIC; 79% of identified studies indicated that participants were suffering from heat strain, with outdoor workplaces (90%) being much higher than indoor workplaces (65%). |
References
- 1.Adam-Poupart A, Smargiassi A, Busque M-A, Duguay P, Fournier M, Zayed J, et al. Effect of summer outdoor temperatures on work-related injuries in Quebec (Canada) Occup Environ Med [Internet] 2015;72(5):338–45. doi: 10.1136/oemed-2014-102428. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25618108 . [DOI] [PubMed] [Google Scholar]
- 2.Bonafede M, Marinaccio A, Asta F, Schifano P, Michelozzi P, Vecchi S. The association between extreme weather conditions and work-related injuries and diseases. A systematic review of epidemiological studies. Ann Ist Super Sanita [Internet] 52(3):357–67. doi: 10.4415/ANN_16_03_07. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27698294 . [DOI] [PubMed] [Google Scholar]
- 3.Dutta P, Rajiva A, Andhare D, Azhar G, Tiwari A, Sheffield P, et al. Perceived heat stress and health effects on construction workers. Indian J Occup Environ Med [Internet] 2015;19(3):151. doi: 10.4103/0019-5278.174002. Available from: http://www.ijoem.com/text.asp?2015/19/3/151/174002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garzon-Villalba XP, Mbah A, Wu Y, Hiles M, Moore H, Schwartz SW, et al. Exertional heat illness and acute injury related to ambient wet bulb globe temperature. Am J Ind Med. 2016;59(12):1169–76. doi: 10.1002/ajim.22650. [DOI] [PubMed] [Google Scholar]
- 5.McInnes JA, Akram M, Macfarlane EM, Keegel T, Sim MR, Smith P. Association between high ambient temperature and acute work-related injury: A case-crossover analysis using workers??? compensation claims data. Scand J Work Environ Heal. 2017;43(1):86–94. doi: 10.5271/sjweh.3602. [DOI] [PubMed] [Google Scholar]
- 6.Morabito M, Cecchi L, Crisci A, Modesti PA, Orlandini S. Relationship between work-related accidents and hot weather conditions in Tuscany (central Italy) Ind Health [Internet] 2006;44(3):458–64. doi: 10.2486/indhealth.44.458. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16922190 . [DOI] [PubMed] [Google Scholar]
- 7.Nag PK, Nag A. Shiftwork in the hot environment. J Hum Ergol (Tokyo) [Internet] 2001;30(1-2):161–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14564876 . [PubMed] [Google Scholar]
- 8.Otte im Kampe E, Kovats S, Hajat S. Impact of high ambient temperature on unintentional injuries in high-income countries: a narrative systematic literature review. BMJ Open [Internet] 2016;6(2):e010399. doi: 10.1136/bmjopen-2015-010399. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26868947%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4762150%5Cnhttp://bmjopen.bmj .com/lookup/doi/10.1136/bmjopen-2015-010399 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rameezdeen R, Elmualim A. The impact of heat waves on occurrence and severity of construction accidents. Int J Environ Res Public Health. 2017;14(1):1–13. doi: 10.3390/ijerph14010070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spector JT, Bonauto DK, Sheppard L, Busch-Isaksen T, Calkins M, Adams D, et al. A case-crossover study of heat exposure and injury risk in outdoor agricultural workers. PLoS One [Internet] 2016;11(10):30–3. doi: 10.1371/journal.pone.0164498. Available from: http://dx.doi.org/10.1371/journal.pone.0164498 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tawatsupa B, Yiengprugsawan V, Kjellstrom T, Berecki-Gisolf J, Seubsman S-A, Sleigh A. Association between heat stress and occupational injury among Thai workers: findings of the Thai Cohort Study. Ind Health [Internet] 2013;51(1):34–46. doi: 10.2486/indhealth.2012-0138. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23411755 . [DOI] [PubMed] [Google Scholar]
- 12.Withen P. Climate change and wildland firefighter health and safety. New Solut a J Environ Occup Heal policy. 2015;24(4):577–84. doi: 10.2190/NS.24.4.i. [DOI] [PubMed] [Google Scholar]
- 13.Xiang J, Bi P, Pisaniello D, Hansen A, Sullivan T. Association between high temperature and work-related injuries in Adelaide, South Australia, 2001-2010. Occup Environ Med [Internet] 2014;71(4):246–52. doi: 10.1136/oemed-2013-101584. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24334260 . [DOI] [PubMed] [Google Scholar]
- 14.Xiang J, Bi P, Pisaniello D, Hansen A. The impact of heatwaves on workers’ health and safety in Adelaide, South Australia. Environ Res [Internet]. Elsevier. 2014;133:90–5. doi: 10.1016/j.envres.2014.04.042. Available from: http://europepmc.org/abstract/med/24906072%5Cnhttp://www.ncbi.nlm.nih.gov/pubmed/24906072 . [DOI] [PubMed] [Google Scholar]
- 15.Xiang J, Bi P, Pisaniello D, Hansen A. Health impacts of workplace heat exposure: An epidemiological review. Ind Health [Internet] 2014;52(2):91–101. doi: 10.2486/indhealth.2012-0145. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24366537 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Appendix Table 7.
Papers selected using the fourth search strategy
| Paper | Year | Country/Region | Population | Heat exposure index | Study design | Main results |
| Altinsoy et al (1) | 2015 | Turkey | Working population | WBGT | Simulation based on climate driven model | Between 2071 and 2100, deficiency in labour productivity may reach up to 52 % during the summer across so Central Anatolia, Cyprus, and parts of the Aegean and eastern Mediterranean coastal areas, particularly in agriculture and construction. |
| Bodin et al (2) | 2016 | El Salvador | Agriculture | WBGT | Physiological parameters monitoring | WBGT was >26°C from 9:00 (average max.: 29.3±1.7°C). There was a reduction of HR symptoms and dehydration before and after the intervention. Individual daily production increased from 5.1 to a high of 7.3 tons/person/day. |
| Delgado_Cortez (3) | 2009 | Nicaragua | Agriculture | WBGT | Physiological parameters monitoring and productivity | Output production increased significantly (p=0.005) among those best hydrated, from 5.5 to 8 tons of cut sugarcane per worker per day. |
| Dell et al (4) | 2014 | Global | Working population | Not specified | Narrative review | Many of the papers discussed seek to address the impact of "harvesting". Temperatures can also affect income through labour productivity, which can in turn affect health. |
| Esteban et al (5) | 2009 | Taiwan | Working population | Not specified | Simulation based on climate driven model | Annual downtime from tropical cyclones could increase from 1.5% nowadays to up to 2.2% by 2085, an increase of almost 50%. This decrease in productivity could result in a loss of up to 0.7% of the annual Taiwanese GDP by 2085. |
| Gubernot et al (6) | 2014 | USA | Working population | Not specified | Scoping review | Around 40% of HRI cases occur among workers. The length of service appears inversely related to the occurrence of HRI. Working in direct sunshine can add up to 15°F to the perceived temperature. Increased heat decreases workers’ productivity. |
| Hanna et al (7) | 2011 | Australia | Working population | Ambient temperature | Narrative review | Workers carried out on average 1 hour less work per day when temperatures exceeded 37°C (compared with days <30°C), as workers self-paced to maintain thermal comfort. Heat-related health risks increase when work is "externally paced". |
| Heal et al (8) | 2016 | Global | Working population | Not specified | Systematic review | A day with temperatures exceeding 32°C can increase local monthly mortality rates by more than 1% and reduces daily labour supply in exposed sectors by up to 14%. |
| Kenefick et al (9) | 2007 | USA | Working population | Ambient temperature | Narrative review | A study showed that when subjects were dehydrated, productivity of stacking and debarking pulpwood was reduced by 12%. Decision-making and cognitive performance are also adversely influenced by dehydration |
| Kershaw et al (10) | 2013 | United Kingdom | Other | Different levels of climate change | Simulation based on climate driven model | As we move further into the future there is an increase in summertime overheating and hence a decrease in productivity but also a decrease in cold related winter discomfort and an associated increase in productivity. |
| Kjellstrom (11) | 2016 | Global | Working population | WBGT | Simulation based on climate driven model | In South-East Asia as much as 15% to 20% of annual work hours may already be lost in heat-exposed jobs, and this may double by 2050. The annual cost of reduced labour productivity at country level already in 2030 can be several percent of GDP. |
| Kjellstrom et al (12) | 2009 | Global, with a special focus on LMIC | Working population | WBGT | Narrative review | The resulting work capacity during different hours for a person who works at a heavy work intensity of 500 W is very low: on average only 20% of work capacity remains at 12 noon. |
| Kjellstrom et al (13) | 2009 | Global | Working population | WBGT | Simulation based on climate driven model | In terms of absolute change in labour productivity by the 2080s, the greatest losses (11.4% to 26.9%) are seen under A2 in Southeast Asia, Andean and Central America, Eastern Sub-Saharan Africa, and the Caribbean. |
| Kjellstrom et al (14) | 2011 | Global, with a special focus on Central America | Working population | WBGT | Narrative review | 24% of HR deaths in the USA were in the Ag/For/Fis/ Hun sector and of these 67% were in workers employed in crop production. Above 26°C, the increasing need for rest periods can be approximated by straight lines that differ depending on the work intensity |
| Kjellstrom et al (15) | 2013 | South-East Asia | Working population | WBGT | Simulation based on climate driven model | Heavy work in the shade is now affected in the hottest areas so that 50-60% of afternoon work time is lost due to heat. Heavy work in the sun has losses up to 80% and above, and even moderate work is affected: >50% of afternoon work time is lost. |
| Kjellstrom et al (16) | 2016 | Global | Working population | WBGT | Narrative review | Reduced work capacity, labour productivity, and economic loss, as well as heat impact on gross domestic product were reported in India, USA and South Africa. When hourly WBGT exceeds 26◦C, work capacity is reduced in heavy-labour jobs, and above 32◦C (90◦F) any work activity is made difficult. GDP losses will be greater than 20% by 2100. |
| Langkulsen et al (17) | 2010 | Thailand | Agriculture - Construction | WBGT | Cross-sectional | Productivity as perceived by the workers revealed that for more than half (60%) the workers, productivity loss varied from 10 to 66.7%, whereas vegetable field workers displayed no loss of productivity. |
| Lao et al (18) | 2016 | Australia | Working population | Not specified | Cross-sectional | Common heat-related symptoms including headaches, sweating, dizziness, and tiredness. Most workers highlighted that heat impedes their work efficiency and causes a substantial slowing of work rate. |
| Li et al (19) | 2016 | China | Construction | WBGT | Within-group comparison | Direct work time decreased by 0.57% and idle time increased by 0.74% when the WBGT increased by 1 °C; direct work time increased by 0.33% when the workers' experience increased by 1 year and decreased by 0.72% when the workers' age increased by 1 year. |
| Lundgren et al (20) | 2013 | Global | Working population | Not specified | Narrative review | The years 1995-2006 have rank among the warmest. Effects of increasing temperatures include a high prevalence of CKD, in Central America, especially among sugarcane workers, and a global reduction of work productivity. |
| Lundgren et al (21) | 2014 | India | Working population | WBGT | Within-group comparison | Avg WBGT was 29.7. Significant impacts on productivity in all workplaces, apart from the laundry facility, were shown, e.g. in the canteen, the core temperature limit of 38°C predicted by the model was reached in only 64 min for women. |
| Marchetti et al (22) | 2016 | World | Working population | Not specified | Narrative review | Productivity is affected after 1 hour of moderate physical work above 32 °C. In SE Asia up to 20% of annual work hours may already be lost in heat-exposed jobs. By 2080, the greatest losses are foreseen in SE Asia, Central America, Sub-Saharan Africa. |
| Mathee et al (23) | 2010 | South Africa | Outdoor workers | Ambient tremparture | Cross-sectional | Hourly max. temp. ranged from 23-36°C in Upington and 21-27°C in Johannesburg. Heat-related effects reported included sunburn, sleeplessness, irritability, and exhaustion leading to difficulty in maintaining work levels and output during very hot weather. |
| Mirabelli et al (24) | 2010 | USA (North Carolina) | Agriculture | Not specified | Cross-sectional | Working in extreme heat was reported by 281 respondents (94%), among whom 112 (40%) reported symptoms of heat illness. 37% reported changes in their work hours and 34% in their work activities. |
| Oyekale (25) | 2015 | Nigeria | Agriculture | Not specified | Cross-sectional | Missing regular times scheduled for spraying cocoa pods (45.7% in Ondo state) was one of the forms of reported climate change induced occupational stresses |
| Patz et al (26) | 2014 | Global | General population, including working population | Not specified | Systematic review | Heat stress has reduced labour capacity by 10% in summer’s peak over the past few decades. Projected reduction may double by 2050. |
| Pradhan et al (27) | 2013 | Nepal | Manufacturing industry | Heat index, humidity index, and WBGT, based on the HOTHAPS approach | Cross-sectional | The average temperature in the summer reached to over 39°C: the environmental conditions were inadequate for workers to work continuously during the day. HRI included fainting, mental irritation, laziness, sleepless nights, dehydration and giddiness. |
| Sahu et al (28) | 2013 | India | Agriculture | WBGT | Cross-sectional | At WBGT>26°C the hourly N of rice bundles collected was reduced approximately 5% per °C of increased WBGT. |
| Sett et al (29) | 2014 | India | Manufacturing industry | WBGT | Cross-sectional | There is a linear decline in productivity with an increase in maximum air temperature above 34.9°C, and the lost productivity for every degree rise in temperature is about 2%. |
| Singh et al (30) | 2015 | Australia | Working population | Not specified | Cross-sectional | Productivity is significantly reduced at 35°C, and approximately one-third of baseline work productivity can be lost in certain physically demanding jobs when working at 40°C. |
| Suzuki-Parker et al (31) | 2016 | Japan | Working population | WBGT | Simulation based on climate driven model | "Light labour safe" hours are projected to decrease by 30-40 % by the end of the 21st century. The number of "heavy labour restricted days" is projected to increase from~5 days in the 2000s to nearly 2/3 of the days in August in the 2090s. |
| Venugopal et al (32) | 2015 | India | Working population | WBGT | Cross-sectional | Workers with heavy workloads reported more heat-related health issues (chi square = 23.67, p ≤ 0.001) and reduced productivity (chi square =15.82, p ≤ 0.001), especially outdoor workers. Of the workers’ assessed in both hotter and cooler seasons, 65% vs. 32% were exposed to higher than recommended WBGT levels in hotter and cooler seasons respectively. This corresponded to a significant increase in self-reported productivity losses (p ¤ 0.016). |
| Xiang et al (33) | 2014 | Global | Working population | WGBT, heat stress and air temperature | Systematic review | Manual workers be at risk of heat stress, especially those in LMIC. 79% of identified studies indicated that participants were suffering from heat strain, with outdoor workplaces (90%) being much higher than indoor workplaces (65%). |
| Zander et al (34) | 2015 | Australia | Working population | Not specified | Cross-sectional | 70% said heat made them less productive on at least 1 day in the previous year: on average, they were 35% less productive on days on which they had suffered from heat, were less productive on 10 days, and worked for 27.1 h less. |
| Zhao et al (35) | 2016 | China | Outdoor workers | Daily Tmax | Simulation based on climate driven model | The total HTS is estimated at 38.6 billion yuan/y over the 1979-2005 period (0.2% of GDP), the share of GDP devoted to HTS could become as high as 3% at the end of 21st century. |
| Zivin et al (36) | 2014 | USA | Working population | Historical and forecasted temperature distribution-daily maximum and minimum temperature, precipitation, snowfall, and relative humidity. | Econometric model | At daily max. temp. >85°F, workers in industries with high exposure to climate reduce daily time allocated to labour by as much as 1 h. Almost all of the decrease in time allocated to labour happens at the end of the day. |
References
- 1.Altinsoy H, Yildirim HA. Labor productivity losses over western Turkey in the twenty-first century as a result of alteration in WBGT. Int J Biometeorol. 2015;59(4):463–71. doi: 10.1007/s00484-014-0863-z. [DOI] [PubMed] [Google Scholar]
- 2.Bodin T, García-Trabanino R, Weiss I, Jarquín E, Glaser J, Jakobsson K, et al. Intervention to reduce heat stress and improve efficiency among sugarcane workers in El Salvador: Phase 1. Occup Environ Med [Internet] 2016 doi: 10.1136/oemed-2016-103555. oemed-2016-103555. Available from: http://oem.bmj.com/lookup/doi/10.1136/oemed-2016-103555 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cortez OD. Heat stress assessment among workers in a Nicaraguan sugarcane farm. Glob Health Action. 2009;2(1):1–6. doi: 10.3402/gha.v2i0.2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dell M, Jones BF, Olken BA. What Do We Learn from the Weather? The New Climate-Economy Literature. J Econ Lit [Internet] 2014 Sep;52(3):740–98. Available from: http://pubs.aeaweb.org/doi/abs/10.1257/jel.52.3.740 . [Google Scholar]
- 5.Esteban M, Webersik C, Shibayama T. Effect of a global warming-induced increase in typhoon intensity on urban productivity in Taiwan. Sustain Sci. 2009;4(2):151–63. [Google Scholar]
- 6.Gubernot DM, Anderson GB, Hunting KL. The epidemiology of occupational heat exposure in the United States: a review of the literature and assessment of research needs in a changing climate. Int J Biometeorol [Internet] 2014 Oct 11;58(8):1779–88. doi: 10.1007/s00484-013-0752-x. Available from: http://link.springer.com/10.1007/s00484-013-0752-x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanna EG, Kjellstrom T, Bennett C, Dear K. Climate Change and Rising Heat: Population Health Implications for Working People in Australia. Asia-Pacific J Public Heal [Internet] 2011 Mar 1;23(2 Suppl):14S–26S. doi: 10.1177/1010539510391457. Available from: http://aph.sagepub.com/cgi/doi/10.1177/1010539510391457 . [DOI] [PubMed] [Google Scholar]
- 8.Heal G, Park J. Reflections—Temperature Stress and the Direct Impact of Climate Change: A Review of an Emerging Literature. Rev Environ Econ Policy [Internet] 2016 Jul;10(2):347–62. Available from: https://academic.oup.com/reep/article-lookup/doi/10.1093/reep/rew007 . [Google Scholar]
- 9.Kenefick RW, Sawka MN. Hydration at the work site. J Am Coll Nutr. 2007;26(5 Suppl):597S–603S. doi: 10.1080/07315724.2007.10719665. [DOI] [PubMed] [Google Scholar]
- 10.Kershaw T, Lash D. Investigating the productivity of office workers to quantify the effectiveness of climate change adaptation measures. Build Environ. Elsevier Ltd. 2013;69:35–43. [Google Scholar]
- 11.Kjellstrom T. Impact of Climate Conditions on Occupational Health and Related Economic Losses: A New Feature of Global and Urban Health in the Context of Climate Change. Asia-Pacific J Public Heal. 2015:1–10. doi: 10.1177/1010539514568711. [DOI] [PubMed] [Google Scholar]
- 12.Kjellstrom T, Holmer I, Lemke B. Workplace heat stress, health and productivity-an increasing challenge for low and middle-income countries during climate change. Glob Health Action. 2009;2(1):1–6. doi: 10.3402/gha.v2i0.2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kjellström T, Kovats RS, Lloyd SJ, Holt T, Tol RSJ. The direct impact of climate change on regional labor productivity. Arch Environ Occup Health [Internet] 2009;64(4):217–27. doi: 10.1080/19338240903352776. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20007118 . [DOI] [PubMed] [Google Scholar]
- 14.Kjellstrom T, Crowe J. Climate Change, Workplace Heat Exposure, and Occupational Health and Productivity in Central America. Int J Occup Environ Health [Internet] 2011 Jul;17(3):270–81. doi: 10.1179/107735211799041931. Available from: http://www.tandfonline.com/doi/full/10.1179/107735211799041931 . [DOI] [PubMed] [Google Scholar]
- 15.Kjellstrom T, Lemke B, Otto M. Mapping occupational heat exposure and effects in South-East Asia: ongoing time trends 1980-2011 and future estimates to 2050. Ind Health [Internet] 2013;51(1):56–67. doi: 10.2486/indhealth.2012-0174. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23411757 . [DOI] [PubMed] [Google Scholar]
- 16.Kjellstrom T, Briggs D, Freyberg C, Lemke B, Otto M, Hyatt O. Heat, Human Performance, and Occupational Health: A Key Issue for the Assessment of Global Climate Change Impacts. Annu Rev Public Health [Internet] 2016 Mar 18;37(1):97–112. doi: 10.1146/annurev-publhealth-032315-021740. Available from: http://www.annualreviews.org/doi/10.1146/annurev-publhealth-032315-021740 . [DOI] [PubMed] [Google Scholar]
- 17.Langkulsen U, Vichit-Vadakan N, Taptagaporn S. Health impact of climate change on occupational health and productivity in Thailand. Glob Health Action [Internet] 2010 Dec 9:3. doi: 10.3402/gha.v3i0.5607. Available from: http://www.globalhealthaction.net/index.php/gha/article/view/5607 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lao J, Hansen A, Nitschke M, Hanson-Easey S, Pisaniello D. Working smart: An exploration of council workers’ experiences and perceptions of heat in Adelaide, South Australia. Saf Sci [Internet]. Elsevier Ltd. 2016;82:228–35. Available from: http://dx.doi.org/10.1016/j.ssci.2015.09.026 . [Google Scholar]
- 19.Li X, Chow KH, Zhu Y, Lin Y. Evaluating the impacts of high-temperature outdoor working environments on construction labor productivity in China: A case study of rebar workers. Build Environ [Internet]. Elsevier Ltd. 2016;95:42–52. Available from: http://dx.doi.org/10.1016/j.buildenv.2015.09.005 . [Google Scholar]
- 20.Lundgren K, Kuklane K, Gao C, Holmér I. Effects of heat stress on working populations when facing climate change. Ind Health [Internet] 2013;51(1):3–15. doi: 10.2486/indhealth.2012-0089. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23411752 . [DOI] [PubMed] [Google Scholar]
- 21.Lundgren K, Kuklane K, Venugopal V. Occupational heat stress and associated productivity loss estimation using the PHS model (ISO 7933): A case study from workplaces in Chennai, India. Glob Health Action. 2014;7(1):1–9. doi: 10.3402/gha.v7.25283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marchetti E, Capone P, Freda D. Climate change impact on microclimate of work environment related to occupational health and productivity. Ann Ist Super Sanita [Internet] 2016;52(3):338–42. doi: 10.4415/ANN_16_03_05. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27698292 . [DOI] [PubMed] [Google Scholar]
- 23.Mathee A, Oba J, Rose A. Climate change impacts on working people (the HOTHAPS initiative): findings of the South African pilot study Angela. Glob Health Action. 2010;3(5612):1–9. doi: 10.3402/gha.v3i0.5612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mirabelli MC, Quandt SA, Crain R, Grzywacz JG, Robinson EN, Vallejos QM, et al. Symptoms of heat illness among Latino farm workers in North Carolina. Am J Prev Med [Internet]. Elsevier Inc. 2010;39(5):468–71. doi: 10.1016/j.amepre.2010.07.008. Available from: http://dx.doi.org/10.1016/j.amepre.2010.07.008 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oyekale AS. Climate change induced occupational stress and reported morbidity among cocoa farmers in South-Western Nigeria. Ann Agric Environ Med. 2015;22(2):357–61. doi: 10.5604/12321966.1152095. [DOI] [PubMed] [Google Scholar]
- 26.Patz JA, Frumkin H, Holloway T, Vimont DJ, Haines A. Climate Change. Jama [Internet] 2014;312(15):1565. doi: 10.1001/jama.2014.13186. Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2014.13186 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pradhan B, Shrestha S, Shrestha R, Pradhanang S, Kayastha B, Pradhan P. Assessing climate change and heat stress responses in the Tarai region of Nepal. Ind Health [Internet] 2013;51(1):101–12. doi: 10.2486/indhealth.2012-0166. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23411760 . [DOI] [PubMed] [Google Scholar]
- 28.Sahu S, Sett M, Kjellstrom T. Heat exposure, cardiovascular stress and work productivity in rice harvesters in India: implications for a climate change future. Ind Health [Internet] 2013;51(4):424–31. doi: 10.2486/indhealth.2013-0006. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23685851 . [DOI] [PubMed] [Google Scholar]
- 29.Sett M, Sahu S. Effects of occupational heat exposure on female brick workers in West Bengal, India. Glob Health Action. 2014;7(1):1–11. doi: 10.3402/gha.v7.21923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singh S, Hanna EG, Kjellstrom T. Working in Australia’s heat: Health promotion concerns for health and productivity. Health Promot Int. 2015;30(2):239–50. doi: 10.1093/heapro/dat027. [DOI] [PubMed] [Google Scholar]
- 31.Suzuki-Parker A, Kusaka H. Future projections of labor hours based on WBGT for Tokyo and Osaka, Japan, using multi-period ensemble dynamical downscale simulations. Int J Biometeorol. 2016;60(2):307–10. doi: 10.1007/s00484-015-1001-2. [DOI] [PubMed] [Google Scholar]
- 32.Venugopal V, Chinnadurai JS, Lucas RAI, Kjellstrom T. Occupational heat stress profiles in selected workplaces in India. Int J Environ Res Public Health. 2015;13(1):1–13. doi: 10.3390/ijerph13010089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xiang J, Bi P, Pisaniello D, Hansen A. Health impacts of workplace heat exposure: An epidemiological review. Ind Health [Internet] 2014;52(2):91–101. doi: 10.2486/indhealth.2012-0145. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24366537 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zander KK, Botzen WJW, Oppermann E, Kjellstrom T, Garnett ST. Heat stress causes substantial labour productivity loss in Australia. Nat Clim Chang [Internet] 2015;5(May):1–6. Available from: http://www.nature.com/doifinder/10.1038/nclimate2623 . [Google Scholar]
- 35.Zhao Y, Sultan B, Vautard R, Braconnot P, Wang HJ, Ducharne A. Potential escalation of heat-related working costs with climate and socioeconomic changes in China. Proc Natl Acad Sci U S A [Internet] 2016;113(17):4640–5. doi: 10.1073/pnas.1521828113. Available from: http://www.pnas.org/content/113/17/4640.full . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zivin JG, Neidell MJ. Temperature and the Allocation of Time: Implications for Climate Change. 2010;32(1) Available from: http://www.nber.org/papers/w15717 . [Google Scholar]
Appendix Table 8.
Papers selected using the third search strategy
| Paper | Year | Country/Region | Population | Heat exposure index | Study design | Outcome | Main results |
| Afshan et al (1) | 2014 | Pakistan | General population | Mean environmental temp; Mean, min and max temp; Relative humidity; Mean evaporation; Mean sunshine hours; Mean solar radiation; Wet Day Index (Mt) | Ecological | Fascioliasis | Increased fascioliasis risk throughout the Punjab plain and its decrease in the northern highlands of the province became evident during the study period. The results point in the direction of evident trend modifications for the summer months |
| Alimi et al (2) | 2015 | northern South America (nSA) | Vectors | Temperature and precipitation | Simulation based on climate driven model | Malaria | While areas with malaria are expected to decrease, both vectors are predicted to experience range expansions in the future. Elevation, annual precipitation and temperature were influential in all models both current and future. |
| Anyamba et al (3) | 2012 | Eastern and Southern Africa | General population | Surface air temperature; precipitation anomalies | Ecological | Rift Valley fever | RVF outbreaks occurred after mo. of abnormal rainfall. Chikungunya outbreaks in conditions of anomalous heat and drought in Eastern Africa; in Southeast Asia, they were negatively correlated with drought, but positively correlated with higher temperatures and rainfall. |
| Atkinson et al (4) | 2013 | Global | General population | Not specified | Systematic review | Echinococcus granulosus and E. multilocularis | Causal links between specific environmental variables and echinococcosis in humans are yet to be established. Authors recommend for incorporation of environmental, animal and human data collection within a sentinel site surveillance network |
| Balbus et al (5) | 2009 | USA | General population, including working population | Not specified | Narrative review | Vector-borne diseases | Electricity and pipeline utility workers are at increased risk of infection with Lyme Disease, although evidence is lacking for greater risk of clinical illness. |
| Bennet et al (6) | 2010 | Global | Working population | Not specified | Narrative review | Infectious diseases | Incidence schistosomiasis, distribution of Aedes albopictus, prevalence of leishmaniosis, have increased. Outbreaks and endemic diarrhoeal disease are already a major source of lost work days, especially in developing countries |
| Bett et al (7) | 2017 | Global | General population | Not specified | Narrative review | Vector-borne diseases | Some of the studies are used to show a positive association between temperature and expansion of the geographical ranges of arthropod vectors, while others are used to illustrate an opposite trend. |
| Bostan et al (8) | 2016 | Pakistan | General population | Average temperature and rainfall trends | Ecological | Dengue fever | An immense potential for the sustenance of DF in major metropolitan cities in Pakistan for more than 9 months, with temperature at ≥18°C (Punjaband Sindh Province, where maximum incidences have been reported over the years). |
| Caminade et al (9) | 2015 | Europe | Livestock | Maximum and minimum temperatures | Simulation based on climate driven model | Fascioliasis | The estimated pattern of climate change for northern Europe will possibly extend the season suitable for development of the parasite in the environment by up to four months. For southern Europe, the risk will increase during the winter months. |
| Chaves et al (10) | 2010 | East African highlands | Vectors | Not specified | Narrative review | Malaria | Authors reviewed the evidence for the role of climate as a driving force for highland invasion by malaria and concluded that it is robust. However, other aspects are involved (e.g. deforestation, predators, competitors) and should be taken into account. |
| Daniel et al (11) | 2009 | Czech Republic | Vectors | Ground-level temperature | Cross-sectional | Tick-borne Encephalitis Virus and Borrelia burgdorferi s.l. | A trend of increasing mean air temperatures during the last three decades was found. The trend was most pronounced in the spring and summer months with the highest activity of I. ricinus ticks. |
| Desai et al (12) | 2009 | Romania, Slovakia, Poland | Agriculture | Not specified | Retrospective cohort study | Leptospirosis | The unusually warm winter of 2006-2007 supported vole population growth and contributed to this resurgence of leptospirosis in Germany |
| Elbers et al (13) | 2015 | Global | Vectors | Not specified | Narrative review | Mosquitoes' geographic distribution | Over the last few decades, multiple Asian species have established themselves in Europe, spread and are unlikely to ever be eradicated. Ecological interactions with newly encountered species can also be modified by factors, such as photoperiodism. |
| Escobedo et al (14) | 2015 | Cuba | Other | the Oceanic Ni˜no Index (ONI) | Ecological | Giardiasis | The cumulated rates for children were significantly higher, 244.73 cases/10,000 pop. (95%CI 238.5-251.0),compared to the workers, 101.82 cases/10,000 pop.(95%CI 93.5-110.2) |
| Feria-Arroyo et al (15) | 2014 | Texas and a portion of northeast Mexico | Vectors | Annual mean temperature, Max temp (warmest month); min temp (coldest month); temp annual range; mean temp driest, warmest and coldest quarter + precipitation indexes | Simulation based on climate driven model | Lyme disease | The habitat suitable for the distribution of I. scapularis in the Texas-Mexico transboundary region will remain relatively stable until 2050. |
| Gale et al (16) | 2009 | Global | Livestock | Not specified | Narrative review | Vector-borne diseases | Warmer night-time temperatures influence many insect vectors that fly and feed at night. Rainfall affects mosquito abundance. Climate change could promote biological invasion of nonindigenous species with their associated pathogens and parasites. |
| Gale et al (17) | 2010 | Europe | Livestock | Not specified | Simulation based on climate driven model | Crimean-Congo haemorrhagic fever | Southern European bird species may expand their breeding ranges into more northern parts. The chances of moulting and survival of immature ticks may increase. An expansion of H. marginatum distribution northwards may be expected. |
| Gikungu et al (18) | 2016 | Kenya | Livestock | Mean maximum and minimum monthly temperature, relative humidity, sea surface temperatures | Simulation based on climate driven model | Rift valley fever | Besides rainfall, minimum temperature was found to be the most significant predictor in each of the models. |
| Holy et al (19) | 2011 | Germany | General population | Mean monthly air temperatures | Simulation based on climate driven model | Malaria | Both modelling approaches employed resulted in prolonged seasonal transmission gates in the future, enabling malaria transmissions up to 6 months in the climate reference period 2051-2080. |
| Ivanescu et al (20) | 2016 | Romania | General population | Mean monthly temperature | Simulation based on climate driven model | Malaria | Doing an extrapolation of the evolution of temperatures in 2030, a slight increase of temperatures by an average of 24°C in 2030 can be estimated, which may ensure a favourable climate for the development of Culicidae. |
| Jiménez-Clavero (21) | 2012 | Global | General population | Not specified | Narrative review | West Nile fever | West Nile virus (WNV) has expanded in the last 12 years, particularly in the Americas, where it first occurred in 1999, extending relentlessly since then. In Europe, is since the last years of the XX century that its incidence has risen substantially. |
| Joyner et al (22) | 2010 | Kazakhstan | Infectious agent | Emissions scenarios produced by the IPCC | Simulation based on climate driven model | Bacillus anthracis | Overall the predicted current distribution of B. anthracis stretches across the northern tier, eastern quarter, and south-eastern regions of Kazakhstan. It is predicted that these areas are potentially maintaining suitable environments for B. anthracis. |
| Konrad et al (23) | 2012 | USA | Infectious agent | Daily maximum and minimum temperatures | Simulation based on climate driven model | Rift Valley fever | Areas most at risk include the Baltimore and NYC metro areas, most of Texas, especially around Houston; Florida; Atlanta; southwest Nebraska; southern California and Arizona; and the central valley of California. |
| Lal et al (24) | 2013 | Global | General population | Several, depending on the selected studies | Narrative review | Cryptosporidiosis and giardiasis | Future environmental change is expected to have the greatest health impacts in countries with limited resources. |
| Lal et al (25) | 2015 | New Zealand | General population | Ambient temperature | Systematic review | Campylobacteriosis, salmonellosis, giardiasis and cryptosporidiosis. | Enteric disease risk from environmental reservoirs is pathogen specific. In some rural regions, environmental pathogen load is considerable, with multiple opportunities for zoonotic transmission. |
| Léger et al (26) | 2013 | Global | Vectors | Not specified | Narrative review | Ticks distribution | The northward expansion of I. ricinus has been well-documented in Scandinavia; Ixodes uriae, a tick associated with colonial seabirds, may be increasing in abundance and occurrence at high latitudes. Expansions have also been observed in African ticks. |
| Lindsay et al (27) | 2001 | Great Britain | Vectors | Temperature surfaces and future temperature change scenarios | Simulation based on climate driven model | Vivax malaria | Under all climate-change scenarios, the risk of transmission increases in the south of England, spreading northwards to southern Scotland. |
| Moore et al (28) | 2012 | Africa | Humans, animals and vectors | Mean temperature | Simulation based on climate driven model | African trypanosomiasis | The model predicts that epidemics can occur when mean temperatures are between 20.7°C and 26.1°C. It predicts a large shift of up to 60% in the geographical extent of the range, and that 46-77 million additional people may be at risk of exposure by 2090. |
| Patz et al (29) | 2008 | Global | General population | Not specified | Narrative review | Infectious diseases | Although in isolated cases, disease resurgence has been attributed to recent warming trends, some of the long-term and complex problems posed by climate change may not be readily discernible from other causal factors. |
| Paz et al (30) | 2007 | Israel | Other | Mean, maximum and minimum temperatures | Ecological | Systemic V. vulnificus | Significant correlations between temperature values and hospital admission dates were revealed. Higher significant results were detected for the daily minimum temperatures in summer 1996 compatible with the disease eruption. |
| Sainz-Elipe et al (31) | 2010 | Spain | General population | Mean max. and min temperatures, mean environmental temperature, relative humidity, potential evapo transpiration, wind speed, vapour pressure, global radiation | Simulation based on climate driven model | Malaria | Climatological analyses and Gradient Model Risk index show that a transmission risk presently exists, lasting from May until September for P. falciparum, and from May until October for P. vivax. |
| Singh et al (32) | 2011 | India | Vectors | Not specified | Narrative review | Zoonoses | In recent years, vector-borne diseases have emerged as a serious public health issue in countries of the South-East Asia region. Many of these, particularly dengue fever and Japanese encephalitis, now occur in epidemic form, almost on an annual basis. |
| Tanga et al (33) | 2010 | Cameroon | Vectors | Monthly mean maximum and minimum temperatures | Cross-sectional | Vectors of malaria | There was a strong positive correlation between the abundance of the Anopheles species and the maximum, mean and minimum temperatures, whereas, for An. hancocki, the correlation was significant (positive) only for minimum temperature. |
| WHO (34) | 2014 | Global | General population | Mean temp (coldest and warmest month); mean annual temperature; mean precipitation (driest and wettest month); mean annual precipitation. | Simulation based on climate driven model | Malaria and dengue | Compared with a future without climate change, 60,000 additional deaths due to malaria are projected for the year 2030. There is very little projected increase in deaths due to dengue fever. |
| Xue et al (35) | 2011 | Ethiopia | General population | Monthly maximum air temperature, monthly average land surface temperature, monthly total precipitation and precipitation estimates | Ecological | Schistosoma mansoni | An apparent association between temperature and number of patients was observed: most peaks and valleys of the two time series appeared synchronized. This correlation was stronger for land surface temperature than for air temperature |
| Yang et al (36) | 2017 | China | General population, including working population | Annual average temperature (AAT), annual cumulative rainfall (ACR) | Case surveillance | Vectors of malaria | Annual average temperature, annual cumulative rainfall, rice yield per square kilometre and proportion of rural employees mainly showed a positive association with the malaria incidence rate. |
| Yusa et al (37) | 2015 | Canada | General population, including working population | Not specified | Systematic review | Infectious diseases | Exposure to vector-borne diseases, such as WNV, that may be linked to drought is increased in people spending greater amounts of time outdoors (e.g., agricultural workers, parks services) |
References
- 1.Afshan K, Fortes-Lima CA, Artigas P, Valero AM, Qayyum M, Mas-Coma S. Impact of climate change and man-made irrigation systems on the transmission risk, long-term trend and seasonality of human and animal fascioliasis in Pakistan. Geospat Health. 2014;8(2):317–34. doi: 10.4081/gh.2014.22. [DOI] [PubMed] [Google Scholar]
- 2.Alimi TO, Fuller DO, Qualls WA, Herrera SV, Arevalo-Herrera M, Quinones ML, et al. Predicting potential ranges of primary malaria vectors and malaria in northern South America based on projected changes in climate, land cover and human population. Parasit Vectors [Internet]. Parasites & Vectors. 2015;8(1):431. doi: 10.1186/s13071-015-1033-9. Available from: http://www.parasitesandvectors.com/content/8/1/431 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anyamba A, Linthicum KJ, Small JL, Collins KM, Tucker CJ, Pak EW, et al. Climate teleconnections and recent patterns of human and animal disease outbreaks. PLoS Negl Trop Dis. 2012;6(1) doi: 10.1371/journal.pntd.0001465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atkinson JAM, Gray DJ, Clements ACA, Barnes TS, Mcmanus DP, Yang YR. Environmental changes impacting Echinococcus transmission: Research to support predictive surveillance and control. Glob Chang Biol. 2013;19(3):677–88. doi: 10.1111/gcb.12088. [DOI] [PubMed] [Google Scholar]
- 5.Balbus John M, Malina Catherine M. Identifying Vulnerable Subpopulations for Climate Change Health Effects in the United States. J Occup Environ Med. 2009;51(1):33–7. doi: 10.1097/JOM.0b013e318193e12e. [DOI] [PubMed] [Google Scholar]
- 6.Bennett CM, McMichael AJ. Non-heat related impacts of climate change on working populations. Glob Health Action [Internet] 2010 Dec 17:3. doi: 10.3402/gha.v3i0.5640. Available from: http://journals.sfu.ca/coaction/index.php/gha/article/view/5640 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bett B, Kiunga P, Gachohi J, Sindato C, Mbotha D, Robinson T, et al. Effects of climate change on the occurrence and distribution of livestock diseases. Prev Vet Med [Internet]. Elsevier B.V. 2017;137(November 2015):119–29. doi: 10.1016/j.prevetmed.2016.11.019. Available from: http://dx.doi.org/10.1016/j.prevetmed.2016.11.019 . [DOI] [PubMed] [Google Scholar]
- 8.Bostan N, Javed S, Nabgha-e-Amen , Eqani SAMAS, Tahir F, Bokhari H. Dengue fever virus in Pakistan: effects of seasonal pattern and temperature change on distribution of vector and virus. Rev Med Virol. 2017;27(1):1–17. doi: 10.1002/rmv.1899. [DOI] [PubMed] [Google Scholar]
- 9.Caminade C, van Dijk J, Baylis M, Williams D. Modelling recent and future climatic suitability for fasciolosis in Europe. Geospat Health. 2015;9(2):301–8. doi: 10.4081/gh.2015.352. [DOI] [PubMed] [Google Scholar]
- 10.Chaves LF, Koenraadt CJM. Climate change and highland malaria: fresh air for a hot debate. Q Rev Biol [Internet] 2010 Mar;85(1):27–55. doi: 10.1086/650284. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20337259 . [DOI] [PubMed] [Google Scholar]
- 11.Daniel M, Materna J, Honig V, Metelka L, Danielová V, Harcarik J, et al. Vertical distribution of the tick Ixodes ricinus and tick-borne pathogens in the northern Moravian mountains correlated with climate warming (Jeseníky Mts., Czech Republic) Cent Eur J Public Health [Internet] 2009 Sep;17(3):139–45. doi: 10.21101/cejph.a3550. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20020603 . [DOI] [PubMed] [Google Scholar]
- 12.Desai S, van Treeck U, Lierz M, Espelage W, Zota L, Sarbu A, et al. Resurgence of field fever in a temperate country: an epidemic of leptospirosis among seasonal strawberry harvesters in Germany in 2007. Clin Infect Dis. 2009;48(6):691–7. doi: 10.1086/597036. [DOI] [PubMed] [Google Scholar]
- 13.ELBERS ARW, KOENRAADT C, MEISWINKEL R. Mosquitoes and Culicoides biting midges: vector range and the influence of climate change. Rev Sci Tech l’OIE [Internet] 2015 Apr 1;34(1):123–37. doi: 10.20506/rst.34.1.2349. Available from: http://doc.oie.int:8080/dyn/portal/index.seam?page=alo&aloId=32331 . [DOI] [PubMed] [Google Scholar]
- 14.Escobedo AA, Almirall P, Rumbaut R, Rodríguez-Morales AJ. Potential impact of macroclimatic variability on the epidemiology of giardiasis in three provinces of Cuba, 2010-2012. J Infect Public Health [Internet]. King Saud Bin Abdulaziz University for Health Sciences. 2015;8(1):80–9. doi: 10.1016/j.jiph.2014.06.001. Available from: http://dx.doi.org/10.1016/j.jiph.2014.06.001 . [DOI] [PubMed] [Google Scholar]
- 15.Feria Arroyo TP, Castro-Arellano I, Gordillo-Peréz G, Cavazos AL, Vargas-Sandoval M, Grover A, et al. Implications of climate change on the distribution of the tick vector Ixodes scapularis and risk for Lyme disease in the Texas-Mexico transboundary region. Parasit Vectors [Internet] 2014;7(1):199. doi: 10.1186/1756-3305-7-199. Available from: http://parasitesandvectors.biomedcentral.com/articles/10.1186/1756-3305-7-199 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gale P, Drew T, Phipps LP, David G, Wooldridge M. The effect of climate change on the occurrence and prevalence of livestock diseases in Great Britain. J Appl Microbiol. 2009;106(5):1409–23. doi: 10.1111/j.1365-2672.2008.04036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gale P, Estrada-Peña A, Martinez M, Ulrich RG, Wilson A, Capelli G, et al. The feasibility of developing a risk assessment for the impact of climate change on the emergence of Crimean-Congo haemorrhagic fever in livestock in Europe: A Review. J Appl Microbiol. 2010;108(6):1859–70. doi: 10.1111/j.1365-2672.2009.04638.x. [DOI] [PubMed] [Google Scholar]
- 18.Gikungu D, Wakhungu J, Siamba D, Neyole E, Muita R, Bett B. Dynamic risk model for Rift Valley fever outbreaks in Kenya based on climate and disease outbreak data. Geospat Health. 2016;11(2):95–103. doi: 10.4081/gh.2016.377. [DOI] [PubMed] [Google Scholar]
- 19.Holy M, Schmidt G, Schröder W. Potential malaria outbreak in Germany due to climate warming: Risk modelling based on temperature measurements and regional climate models. Environ Sci Pollut Res. 2011;18(3):428–35. doi: 10.1007/s11356-010-0388-x. [DOI] [PubMed] [Google Scholar]
- 20.Ivanescu L, Bodale I, Florescu SA, Roman C, Acatrinei D, Miron L. Climate Change Is Increasing the Risk of the Reemergence of Malaria in Romania. Biomed Res Int. 2016;2016 doi: 10.1155/2016/8560519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jiménez-Clavero MA. Animal viral diseases and global change: Bluetongue and West Nile fever as paradigms. Front Genet. 2012;3(JUN):1–15. doi: 10.3389/fgene.2012.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joyner TA, Lukhnova L, Pazilov Y, Temiralyeva G, Hugh-Jones ME, Aikimbayev A, et al. Modeling the potential distribution of Bacillus anthracis under multiple climate change scenarios for Kazakhstan. PLoS One. 2010;5(3) doi: 10.1371/journal.pone.0009596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Konrad SK, Miller SN. A temperature-limited assessment of the risk of Rift Valley fever transmission and establishment in the continental United States of America. Geospat Health. 2012;6(2):161–70. doi: 10.4081/gh.2012.134. [DOI] [PubMed] [Google Scholar]
- 24.Lal A, Baker MG, Hales S, French NP. Potential effects of global environmental changes on cryptosporidiosis and giardiasis transmission. Trends Parasitol [Internet]. Elsevier Ltd. 2013;29(2):83–90. doi: 10.1016/j.pt.2012.10.005. Available from: http://dx.doi.org/10.1016/j.pt.2012.10.005 . [DOI] [PubMed] [Google Scholar]
- 25.Lal A, Lill AWT, McIntyre M, Hales S, Baker MG, French NP. Environmental change and enteric zoonoses in New Zealand: A systematic review of the evidence. Aust N Z J Public Health. 2015;39(1):63–8. doi: 10.1111/1753-6405.12274. [DOI] [PubMed] [Google Scholar]
- 26.Léger E, Vourc’h G, Vial L, Chevillon C, McCoy KD. Changing distributions of ticks: Causes and consequences. Exp Appl Acarol. 2013;59(1-2):219–44. doi: 10.1007/s10493-012-9615-0. [DOI] [PubMed] [Google Scholar]
- 27.Lindsay SW, Thomas CJ. Global warming and risk of vivax malaria in Great Britain. Glob Chang Hum Heal. 2001;2(1):80–4. [Google Scholar]
- 28.Moore S, Shrestha S, Tomlinson KW, Vuong H, Colwell RR, Pascual M, et al. Predicting the effect of climate change on African trypanosomiasis: integrating epidemiology with parasite and vector biology. J R Soc Interface [Internet] 2012;9(70):817–30. doi: 10.1098/rsif.2011.0654. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22072451%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC3306657 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patz JA, Olson SH, Uejio CK, Gibbs HK. Disease Emergence from Global Climate and Land Use Change. Med Clin North Am. 2008;92(6):1473–91. doi: 10.1016/j.mcna.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 30.Paz S, Bisharat N, Paz E, Kidar O, Cohen D. Climate change and the emergence of Vibrio vulnificus disease in Israel. Environ Res. 2007;103(3):390–6. doi: 10.1016/j.envres.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 31.Sainz-Elipe S, Latorre JM, Escosa R, Masia M, Fuentes MV, Mas-Coma S, et al. Malaria resurgence risk in southern Europe: climate assessment in an historically endemic area of rice fields at the Mediterranean shore of Spain. Malar J [Internet] 2010;9:221. doi: 10.1186/1475-2875-9-221. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20673367%5Cnhttp://www.ncbi.nlm.nih.gov/pmc/articles/PMC2924348/pdf/1475-2875-9-221.pdf . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Singh BB, Sharma R, Gill JPS, Aulakh RS, Banga HS. Climate change, zoonoses and India. Rev Sci Tech [Internet] 2011;30(3):779–88. doi: 10.20506/rst.30.3.2073. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22435190 . [DOI] [PubMed] [Google Scholar]
- 33.Tanga MC, Ngundu WI, Judith N, Mbuh J, Tendongfor N, Simard F, et al. Climate change and altitudinal structuring of malaria vectors in south-western Cameroon: Their relation to malaria transmission. Trans R Soc Trop Med Hyg. 2010;104(7):453–60. doi: 10.1016/j.trstmh.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 34.Hales S, Kovats S, Lloyd S, Campbell-Lendrum D World Health Organization. Geneva, Switzerland: WHO Library Cataloguing-in-Publication Data; 2014. Quantitative risk assessment of the effects of climate change on selected causes of death, 2030s and 2050s [Internet] Available from: www.who.int/about/licensing/copyright_form/en/index.html . [Google Scholar]
- 35.Xue Z, Gebremichael M, Ahmad R, Weldu ML, Bagtzoglou AC. Impact of temperature and precipitation on propagation of intestinal schistosomiasis in an irrigated region in Ethiopia: Suitability of satellite datasets. Trop Med Int Heal. 2011;16(9):1104–11. doi: 10.1111/j.1365-3156.2011.02820.x. [DOI] [PubMed] [Google Scholar]
- 36.Yang D, Xu C, Wang J, Zhao Y. Spatiotemporal epidemic characteristics and risk factor analysis of malaria in Yunnan Province, China. BMC Public Health [Internet]. BMC Public Health. 2017;17(1):66. doi: 10.1186/s12889-016-3994-9. Available from: http://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-016-3994-9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yusa A, Berry P, Cheng JJ, Ogden N, Bonsal B, Stewart R, et al. Climate change, drought and human health in Canada. Int J Environ Res Public Health. 2015;12(7):8359–412. doi: 10.3390/ijerph120708359. [DOI] [PMC free article] [PubMed] [Google Scholar]
Financing
This study has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 668786, as part of the Project “HEAT-SHIELD - Integrated inter-sector framework to increase the thermal resilience of European workers in the context of global warming”. All researchers are independent from funders. The funder had no role in the design of the study, data collection, analysis, interpretation of results, writing of the manuscript or in the decision to submit the article for publication. Responsibility for the information and views set out in this study lies entirely with the authors. The European Commission is not responsible for any use that may be made of the information contained herein.
No potential conflict of interest relevant to this article was reported by the authors
References
- 1.Adam-Poupart A, Smargiassi A, Busque M-A, et al. Effect of summer outdoor temperatures on work-related injuries in Quebec (Canada) Occup Environ Med. 2015;72:338–345. doi: 10.1136/oemed-2014-102428. [DOI] [PubMed] [Google Scholar]
- 2.Adam-Poupart A, Smargiassi A, Busque MA, et al. Summer outdoor temperature and occupational heat-related illnesses in Quebec (Canada) Environ Res. 2014;134:339–344. doi: 10.1016/j.envres.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 3.Agency USEP. Climate Change Indicators: U.S. and Global Temperature. 2016 Retrieved 30 June 2017 from https://www.epa.gov/climate-indicators/climate-change-indicators-us-and-global-temperature#ref1 . [Google Scholar]
- 4.Alimi TO, Fuller DO, Qualls WA, et al. Predicting potential ranges of primary malaria vectors and malaria in northern South America based on projected changes in climate, land cover and human population. Parasit Vectors. 2015;8:431. doi: 10.1186/s13071-015-1033-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Altinsoy H, Yildirim HA. Labor productivity losses over western Turkey in the twenty-first century as a result of alteration in WBGT. Int J Biometeorol. 2015;59:463–471. doi: 10.1007/s00484-014-0863-z. Retrieved from http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L615308446 . [DOI] [PubMed] [Google Scholar]
- 6.Anyamba A, Linthicum KJ, Small JL, et al. Climate teleconnections and recent patterns of human and animal disease outbreaks. PLoS Negl Trop Dis. 2012:6. doi: 10.1371/journal.pntd.0001465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arbury S, Jacklitsch B, Farquah O, et al. Heat illness and death among workers - United States, 2012-2013. MMWR Morb Mortal Wkly Rep. 2014;63:661–665. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25102413 . [PMC free article] [PubMed] [Google Scholar]
- 8.Arcury TA, Summers P, Talton JW, et al. Heat Illness Among North Carolina Latino Farmworkers. J Occup Environ Med. 2015;57:1299–1304. doi: 10.1097/JOM.0000000000000552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balbus John M, Malina Catherine M. Identifying Vulnerable Subpopulations for Climate Change Health Effects in the United States. J Occup Environ Med. 2009;51:33–37. doi: 10.1097/JOM.0b013e318193e12e. [DOI] [PubMed] [Google Scholar]
- 10.Bennett CM, McMichael AJ. Non-heat related impacts of climate change on working populations. Glob Health Action. 2010:3. doi: 10.3402/gha.v3i0.5640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bethel JW, Harger R. Heat-related illness among Oregon farmworkers. Int J Environ Res Public Health. 2014;11:9273–9285. doi: 10.3390/ijerph110909273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bodin T, García-Trabanino R, Weiss I, et al. Intervention to reduce heat stress and improve efficiency among sugarcane workers in El Salvador: Phase 1. Occup Environ Med. 2016 doi: 10.1136/oemed-2016-103555. oemed-2016-103555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bonauto D, Anderson R, Rauser E, Burke B. Occupational Heat Illness in Washington State, 1995 - 2005. Am J Ind Med. 2007;950:1995–2005. doi: 10.1002/ajim.20517. [DOI] [PubMed] [Google Scholar]
- 14.Brownson RC, Fielding JE, Maylahn CM. Evidence-Based Public Health: A Fundamental Concept for Public Health Practice. Annu Rev Public Health. 2009;30:175–201. doi: 10.1146/annurev.publhealth.031308.100134. [DOI] [PubMed] [Google Scholar]
- 15.Caminade C, van Dijk J, Baylis M, Williams D. Modelling recent and future climatic suitability for fasciolosis in Europe. Geospat Health. 2015;9:301–308. doi: 10.4081/gh.2015.352. [DOI] [PubMed] [Google Scholar]
- 16.Carozzi L. [Il lavoro in ambiente caldo umido] Work in a hot, humid environment. Lav. 1914;VII:247–255. [Google Scholar]
- 17.Carozzi L. [Il lavoro in ambiente caldo umido] Working in a hot, humid environment. Lav. 1914;VII:247–255. [Google Scholar]
- 18.Clark PA, Chowdhury J, Chan B, Radigan N. Chronic kidney disease in Nicaraguan sugarcane workers: A historical, medical, environmental analysis and ethical analysis. Internet J Third World Med. 2016;12:1–16. [Google Scholar]
- 19.Cortez OD. Heat stress assessment among workers in a Nicaraguan sugarcane farm. Glob Health Action. 2009;2:1–6. doi: 10.3402/gha.v2i0.2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crowe J, Nilsson M, Kjellstrom T, et al. Heat-Related symptoms in sugarcane harvesters. Am J Ind Med. 2015;58:541–548. doi: 10.1002/ajim.22450. Retrieved from http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L612766721 . [DOI] [PubMed] [Google Scholar]
- 21.Daniel M, Materna J, Honig V, et al. Vertical distribution of the tick Ixodes ricinus and tick-borne pathogens in the northern Moravian mountains correlated with climate warming (Jeseníky Mts., Czech Republic) Cent Eur J Public Health. 2009;17:139–145. doi: 10.21101/cejph.a3550. [DOI] [PubMed] [Google Scholar]
- 22.Desai S, van Treeck U, Lierz M, et al. Resurgence of Field Fever in a Temperate Country: An Epidemic of Leptospirosis among Seasonal Strawberry Harvesters in Germany in 2007. Clin Infect Dis. 2009;48:691–697. doi: 10.1086/597036. [DOI] [PubMed] [Google Scholar]
- 23.Deschenes O. Temperature, human health, and adaptation: A review of the empirical literature. Energy Econ. 2014;46:606–619. [Google Scholar]
- 24.Dutta P, Rajiva A, Andhare D, et al. Perceived heat stress and health effects on construction workers. Indian J Occup Environ Med. 2015;19:151. doi: 10.4103/0019-5278.174002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Edwards B, Gray M, Hunter B. The Impact of Drought on Mental Health in Rural and Regional Australia. Soc Indic Res. 2015;121:177–194. [Google Scholar]
- 26.Ellis NR, Albrecht GA. Climate change threats to family farmers’ sense of place and mental wellbeing: A case study from the Western Australian Wheatbelt. Soc Sci Med. 2017;175:161–168. doi: 10.1016/j.socscimed.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 27.Eurofound: Sixth European Working Conditions Survey - Overview report (2017 update) Luxembourg: 2017. Retrieved from https://www.eurofound.europa.eu/sites/default/files/ef_publication/field_ef_document/ef1634en.pdf . [Google Scholar]
- 28.European Commission: Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions. An EU Strategy on adaptation to climate change. Brussels: 2013 [Google Scholar]
- 29.European Environment Agency: Global and European temperature. https://www.eea.europa.eu/ . 2017; Retrieved 26 February 2018 from https://www.eea.europa.eu/data-and-maps/indicators/global-and-european-temperature-4/assessment . [Google Scholar]
- 30.Feria Arroyo TP, Castro-Arellano I, Gordillo-Peréz G, et al. Implications of climate change on the distribution of the tick vector Ixodes scapularis and risk for Lyme disease in the Texas-Mexico transboundary region. Parasit Vectors. 2014;7:199. doi: 10.1186/1756-3305-7-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fleischer NL, Tiesman HM, Sumitani J, et al. Public health impact of heat-related illness among migrant farmworkers. Am J Prev Med. 2013;44:199–206. doi: 10.1016/j.amepre.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 32.Fortune M, Mustard C, Brown P. The use of Bayesian inference to inform the surveillance of temperature-related occupational morbidity in Ontario, Canada, 2004-2010. Environ Res. 2014;132:449–456. doi: 10.1016/j.envres.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 33.Fortune MK, Mustard CA, Etches JJC, Chambers AG. Work-attributed illness arising from excess heat exposure in Ontario, 2004-2010. Can J Public Heal. 2013;104:2004–2010. doi: 10.17269/cjph.104.3984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fuhrmann CM, Sugg MM, Konrad CE, Waller A. Impact of Extreme Heat Events on Emergency Department Visits in North Carolina (2007-2011) J Community Health. 2016;41:146–156. doi: 10.1007/s10900-015-0080-7. [DOI] [PubMed] [Google Scholar]
- 35.Gale P, Drew T, Phipps LP, et al. The effect of climate change on the occurrence and prevalence of livestock diseases in Great Britain. J Appl Microbiol. 2009;106:1409–1423. doi: 10.1111/j.1365-2672.2008.04036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.García-Trabanino R, Jarquín E, Wesseling C, et al. Heat stress, dehydration, and kidney function in sugarcane cutters in El Salvador - A cross-shift study of workers at risk of Mesoamerican nephropathy. Environ Res. 2015;142:746–755. doi: 10.1016/j.envres.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 37.Garzon-Villalba XP, Mbah A, Wu Y, et al. Exertional heat illness and acute injury related to ambient wet bulb globe temperature. Am J Ind Med. 2016;59:1169–1176. doi: 10.1002/ajim.22650. [DOI] [PubMed] [Google Scholar]
- 38.Gubernot DM, Anderson GB, Hunting KL. Characterizing occupational heat-related mortality in the United States, 2000-2010: An analysis using the census of fatal occupational injuries database. Am J Ind Med. 2015;58:203–211. doi: 10.1002/ajim.22381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haldane JS. The Influence of High Air Temperatures: No. 1. J Hyg (Lond) 1905;5:494–513. doi: 10.1017/s0022172400006811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hanigan IC, Butler CD, Kokic PN, Hutchinson MF. Suicide and drought in New South Wales, Australia, 1970-2007. Proc Natl Acad Sci. 2012;109:13950–13955. doi: 10.1073/pnas.1112965109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hanna EG, Kjellstrom T, Bennett C, Dear K. Climate Change and Rising Heat: Population Health Implications for Working People in Australia. Asia-Pacific J Public Heal. 2011;23:14S–26S. doi: 10.1177/1010539510391457. [DOI] [PubMed] [Google Scholar]
- 42.Harduar Morano L, Bunn TL, Lackovic M, et al. Occupational heat-related illness emergency department visits and inpatient hospitalizations in the southeast region, 2007-2011. Am J Ind Med. 2015;58:1114–1125. doi: 10.1002/ajim.22504. [DOI] [PubMed] [Google Scholar]
- 43.Harduar Morano L, Watkins S. Evaluation of Diagnostic Codes in Morbidity and Mortality Data Sources for Heat-Related Illness Surveillance. Public Health Rep. 2017;132:326–335. doi: 10.1177/0033354917699826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harduar Morano L, Watkins S, Kintziger K. A Comprehensive Evaluation of the Burden of Heat-Related Illness and Death within the Florida Population. Int J Environ Res Public Health. 2016;13:551. doi: 10.3390/ijerph13060551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heal G, Park J. Reflections - Temperature Stress and the Direct Impact of Climate Change: A Review of an Emerging Literature. Rev Environ Econ Policy. 2016;10:347–362. [Google Scholar]
- 46.Hunt AP, Parker AW, Stewart IB. Symptoms of heat illness in surface mine workers. Int Arch Occup Environ Health. 2013;86:519–527. doi: 10.1007/s00420-012-0786-0. [DOI] [PubMed] [Google Scholar]
- 47.Hunt AP, Parker AW, Stewart IB. Heat strain and hydration status of surface mine blast crew workers. J Occup Environ Med. 2014;56:409–414. doi: 10.1097/JOM.0000000000000114. [DOI] [PubMed] [Google Scholar]
- 48.Hunter I, Di Pietro L. The terrible truth about your tin of Italian tomatoes. Guard. 2017 Retrieved from https://www.theguardian.com/global-development/2017/oct/24/the-terrible-truth-about-your-tin-of-italian-tomatoes . [Google Scholar]
- 49.Inaba R, Kurokawa J, Mirbod SM. Comparison of subjective symptoms and cold prevention measures in winter between traffic control workers and construction workers in Japan. Ind Health. 2009;47:283–291. doi: 10.2486/indhealth.47.283. [DOI] [PubMed] [Google Scholar]
- 50.Jia YA, Rowlinson S, Ciccarelli M. Climatic and psychosocial risks of heat illness incidents on construction site. Appl Ergon. 2016;53:25–35. doi: 10.1016/j.apergo.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 51.Kearney GD, Hu H, Xu X, et al. Estimating the Prevalence of Heat-Related Symptoms and Sun Safety Related Behavior among Latino Farmworkers in Eastern North Carolina. J Agromedicine. 2015;813:15–23. doi: 10.1080/1059924X.2015.1106377. [DOI] [PubMed] [Google Scholar]
- 52.Kenefick RW, Sawka MN. Hydration at the work site. J Am Coll Nutr. 2007;26:597S–603S. doi: 10.1080/07315724.2007.10719665. [DOI] [PubMed] [Google Scholar]
- 53.Kjellstrom T. Impact of Climate Conditions on Occupational Health and Related Economic Losses. Asia Pacific J Public Heal. 2016;28:28S–37S. doi: 10.1177/1010539514568711. [DOI] [PubMed] [Google Scholar]
- 54.Kjellstrom T, Briggs D, Freyberg C, et al. Heat, Human Performance, and Occupational Health: A Key Issue for the Assessment of Global Climate Change Impacts. Annu Rev Public Health. 2016;37:97–112. doi: 10.1146/annurev-publhealth-032315-021740. [DOI] [PubMed] [Google Scholar]
- 55.Kjellstrom T, Kovats RS, Lloyd SJ, et al. The Direct Impact of Climate Change on Regional Labor Productivity. Arch Environ Occup Health. 2009;64:217–227. doi: 10.1080/19338240903352776. [DOI] [PubMed] [Google Scholar]
- 56.Lal A, Baker MG, Hales S, French NP. Potential effects of global environmental changes on cryptosporidiosis and giardiasis transmission. Trends Parasitol. 2013;29:83–90. doi: 10.1016/j.pt.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 57.Lal A, Lill AWT, McIntyre M, et al. Environmental change and enteric zoonoses in New Zealand: A systematic review of the evidence. Aust N Z J Public Health. 2015;39:63–68. doi: 10.1111/1753-6405.12274. [DOI] [PubMed] [Google Scholar]
- 58.Langkulsen U, Vichit-Vadakan N, Taptagaporn S. Health impact of climate change on occupational health and productivity in Thailand. Glob Health Action. 2010:3. doi: 10.3402/gha.v3i0.5607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Laws RL, Brooks DR, Amador JJ, et al. Biomarkers of Kidney Injury among Nicaraguan Sugarcane Workers. Am J Kidney Dis. 2016;67:209–217. doi: 10.1053/j.ajkd.2015.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Léger E, Vourc’h G, Vial L, et al. Changing distributions of ticks: Causes and consequences. Exp Appl Acarol. 2013;59:219–244. doi: 10.1007/s10493-012-9615-0. [DOI] [PubMed] [Google Scholar]
- 61.Li X, Chow KH, Zhu Y, Lin Y. Evaluating the impacts of high-temperature outdoor working environments on construction labor productivity in China: A case study of rebar workers. Build Environ. 2016;95:42–52. [Google Scholar]
- 62.Liang L, Gong P. Climate change and human infectious diseases: A synthesis of research findings from global and spatio-temporal perspectives. Environ Int. 2017;103:99–108. doi: 10.1016/j.envint.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 63.Lucas RAI, Epstein Y, Kjellstrom T. Excessive occupational heat exposure: a significant ergonomic challenge and health risk for current and future workers. Extrem Physiol Med. 2014;3:14. doi: 10.1186/2046-7648-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Maeda T, Kaneko SY, Ohta M, et al. Risk factors for heatstroke among Japanese forestry workers. J Occup Health. 2006;48:223–229. doi: 10.1539/joh.48.223. [DOI] [PubMed] [Google Scholar]
- 65.Mathee A, Oba J, Rose A. Climate change impacts on working people (the HOTHAPS initiative): findings of the South African pilot study Angela. Glob Health Action. 2010;3:1–9. doi: 10.3402/gha.v3i0.5612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Matthies F, Bickler G, Marin N, Hales S. Heat-health action plans. Copenhagen: 2008. Retrieved from http://www.euro.who.int/__data/assets/pdf_file/0006/95919/E91347.pdf . [Google Scholar]
- 67.Mattioli S, Zanardi F, Baldasseroni A, et al. Search strings for the study of putative occupational determinants of disease. Occup Environ Med. 2010;67:436–443. doi: 10.1136/oem.2008.044727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.McInnes JA, Akram M, MacFarlane EM, et al. Association between high ambient temperature and acute work-related injury: a case-crossover analysis using workers’ compensation claims data. Scand J Work Environ Health. 2017;43:86–94. doi: 10.5271/sjweh.3602. [DOI] [PubMed] [Google Scholar]
- 69.Mirabelli MC, Quandt SA, Crain R, et al. Symptoms of heat illness among Latino farm workers in North Carolina. Am J Prev Med. 2010;39:468–471. doi: 10.1016/j.amepre.2010.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mirabelli MC, Richardson DB. Heat-related fatalities in North Carolina. Am J Public Health. 2005;95:635–637. doi: 10.2105/AJPH.2004.042630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Morabito M, Cecchi L, Crisci A, et al. Relationship between work-related accidents and hot weather conditions in Tuscany (central Italy) Ind Health. 2006;44:458–464. doi: 10.2486/indhealth.44.458. [DOI] [PubMed] [Google Scholar]
- 72.Oyekale AS. Climate change induced occupational stress and reported morbidity among cocoa farmers in South-Western Nigeria. Ann Agric Environ Med. 2015;22:357–361. doi: 10.5604/12321966.1152095. [DOI] [PubMed] [Google Scholar]
- 73.Parsons K. Third Edit. CRC Press; 2014. Human Thermal Environments: The Effects of Hot, Moderate, and Cold Environments on Human Health, Comfort, and Performance. [Google Scholar]
- 74.Peraza S, Wesseling C, Aragon A, et al. Decreased kidney function among agricultural workers in El Salvador. Am J Kidney Dis. 2012;59:531–540. doi: 10.1053/j.ajkd.2011.11.039. [DOI] [PubMed] [Google Scholar]
- 75.Petitti DB, Harlan SL, Chowell-Puente G, Ruddell D. Occupation and Environmental Heat-Associated Deaths in Maricopa County, Arizona: A Case-Control Study. PLoS One. 2013:8. doi: 10.1371/journal.pone.0062596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Polain JD, Berry HL, Hoskin JO. Rapid change, climate adversity and the next “big dry”: Older farmers’ mental health. Aust J Rural Health. 2011;19:239–243. doi: 10.1111/j.1440-1584.2011.01219.x. [DOI] [PubMed] [Google Scholar]
- 77.Pradhan B, Shrestha S, Shrestha R, et al. Assessing Climate Change and Heat Stress Responses in the Tarai Region of Nepal. Ind Health. 2013;51:101–112. doi: 10.2486/indhealth.2012-0166. [DOI] [PubMed] [Google Scholar]
- 78.Raines N, González Quiroz M, Wyatt C, et al. Risk factors for reduced glomerular filtration rate in a nicaraguan community affected by mesoamerican nephropathy. MEDICC Rev. 2014;16:16–22. doi: 10.37757/MR2014.V16.N2.4. [DOI] [PubMed] [Google Scholar]
- 79.Raju DSSK, Kiranmayi P, Vijaya Rachel K. Climate change and chronic kidney disease. Asian J Pharm Clin Res. 2014;7:53–57. [Google Scholar]
- 80.Ramazzini B. Works. Cierre edi. Verona: Cierre edizioni; 2009. [Google Scholar]
- 81.Rameezdeen R, Elmualim A. The impact of heat waves on occurrence and severity of construction accidents. Int J Environ Res Public Health. 2017;14:1–13. doi: 10.3390/ijerph14010070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rhea S, Ising A, Fleischauer AT, et al. Using near real-time morbidity data to identify heat-related illness prevention strategies in North Carolina. J Community Health. 2012;37:495–500. doi: 10.1007/s10900-011-9469-0. [DOI] [PubMed] [Google Scholar]
- 83.Richardson WS, Wilson MC, Nishikawa J, Hayward RS. The well-built clinical question: a key to evidence-based decisions. ACP J. Club. 123:A12–A13. [PubMed] [Google Scholar]
- 84.Sahu S, Sett M, Kjellstrom T. Heat exposure, cardiovascular stress and work productivity in rice harvesters in India: implications for a climate change future. Ind Health. 2013;51:424–431. doi: 10.2486/indhealth.2013-0006. [DOI] [PubMed] [Google Scholar]
- 85.Schulte PA, Bhattacharya A, Butler CR, et al. Advancing the framework for considering the effects of climate change on worker safety and health. J Occup Environ Hyg. 2016;13:847–865. doi: 10.1080/15459624.2016.1179388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Schulte PA, Chun H. Climate Change and Occupational Safety and Health: Establishing a Preliminary Framework. J Occup Environ Hyg. 2009;6:542–554. doi: 10.1080/15459620903066008. [DOI] [PubMed] [Google Scholar]
- 87.Singh S, Hanna EG, Kjellstrom T. Working in Australia’s heat: Health promotion concerns for health and productivity. Health Promot Int. 2015;30:239–250. doi: 10.1093/heapro/dat027. [DOI] [PubMed] [Google Scholar]
- 88.Spector JT, Bonauto DK, Sheppard L, et al. A case-crossover study of heat exposure and injury risk in outdoor agricultural workers. PLoS One. 2016;11:30–33. doi: 10.1371/journal.pone.0164498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Spector JT, Krenz J, Rauser E, Bonauto DK. Heat-related illness in Washington State agriculture and forestry sectors. Am J Ind Med. 2014;57:881–895. doi: 10.1002/ajim.22357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tawatsupa B, Yiengprugsawan V, Kjellstrom T, et al. Association between heat stress and occupational injury among Thai workers: findings of the Thai Cohort Study. Ind Health. 2013;51:34–46. doi: 10.2486/indhealth.2012-0138. [DOI] [PubMed] [Google Scholar]
- 91.Geneva, Switzerland: 2015. The Intergovernmental Panel on Climate: Climate Change 2014: Synthesis Report. Contribution of Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change [Core Writing Team, R.K. Pachauri and L.A. Meyer (eds.)] Retrieved from http://www.ipcc.ch/pdf/assessment-report/ar5/syr/SYR_AR5_FINAL_full_wcover.pdf . [Google Scholar]
- 92.Venugopal V, Chinnadurai JS, Lucas RAI, Kjellstrom T. Occupational heat stress profiles in selected workplaces in India. Int J Environ Res Public Health. 2015;13:1–13. doi: 10.3390/ijerph13010089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Watts N, Adger WN, Agnolucci P, Blackstock J, et al. Health and climate change: policy responses to protect public health. Lancet. 2015;386:1861–1914. doi: 10.1016/S0140-6736(15)60854-6. [DOI] [PubMed] [Google Scholar]
- 94.Weil T, De Filippo C, Albanese D, et al. Legal immigrants: invasion of alien microbial communities during winter occurring desert dust storms. Microbiome. 2017;5:32. doi: 10.1186/s40168-017-0249-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wesseling C, Aragón A, González M, et al. Kidney function in sugarcane cutters in Nicaragua - A longitudinal study of workers at risk of Mesoamerican nephropathy. Environ Res. 2016;147:125–132. doi: 10.1016/j.envres.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 96.World Health Organization. Geneva, Switzerland: 2014. Quantitative risk assessment of the effects of climate change on selected causes of death, 2030s and 2050s. Retrieved from www.who.int/about/licensing/copyright_form/en/index.html . [Google Scholar]
- 97.World Health Organization. Climate change and health - Fact sheet. 2017 Retrieved 5 July 2017 from http://www.who.int/mediacentre/factsheets/fs266/en/ [Google Scholar]
- 98.Wyndham CH. Adaptation to heat and cold. Environ Res. 1969;2:442–469. doi: 10.1016/0013-9351(69)90015-2. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/5381589 . [DOI] [PubMed] [Google Scholar]
- 99.Xiang J, Bi P, Pisaniello D, Hansen A. The impact of heatwaves on workers’ health and safety in Adelaide, South Australia. Environ Res. 2014;133:90–95. doi: 10.1016/j.envres.2014.04.042. [DOI] [PubMed] [Google Scholar]
- 100.Xiang J, Bi P, Pisaniello D, et al. Association between high temperature and work-related injuries in Adelaide, South Australia, 2001-2010. Occup Environ Med. 2014;71:246–252. doi: 10.1136/oemed-2013-101584. [DOI] [PubMed] [Google Scholar]
- 101.Xiang J, Hansen A, Pisaniello D, Bi P. Extreme heat and occupational heat illnesses in South Australia, 2001-2010. Occup Environ Med. 2015;72:580–586. doi: 10.1136/oemed-2014-102706. [DOI] [PubMed] [Google Scholar]
- 102.Yang D, Xu C, Wang J, Zhao Y. Spatiotemporal epidemic characteristics and risk factor analysis of malaria in Yunnan Province, China. BMC Public Health. 2017;17:66. doi: 10.1186/s12889-016-3994-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yusa A, Berry P, Cheng JJ, et al. Climate change, drought and human health in Canada. Int J Environ Res Public Health. 2015;12:8359–8412. doi: 10.3390/ijerph120708359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zivin JG, Neidell MJ. Temperature and the Allocation of Time: Implications for Climate Change. 2010:32. Retrieved from http://www.nber.org/papers/w15717 . [Google Scholar]
- 105.Malaria a Taranto, la malattia contratta in Italia dai 4 migranti ricoverati. www.ansa.it . 2017; Retrieved from http://www.ansa.it/canale_saluteebenessere/notizie/medicina/2017/10/04/asl-taranto-i-4-rucoverati-hanno-contratto-la-malaria-in-italia_6374af9c-9c6f-45e4-af53-746109614027.html . [Google Scholar]