Abstract
Background
Active surveillance has been proposed for patients with oesophageal cancer in whom there is a complete clinical response after neoadjuvant chemoradiotherapy (nCRT). However, endoscopic biopsies have limited negative predictive value in detecting residual disease. This study determined the location of residual tumour following surgery to improve surveillance and endoscopic strategies.
Methods
The present study was based on patients who participated in the prospective preSANO trial with adenocarcinoma or squamous cell carcinoma of the oesophagus or oesophagogastric junction treated in four Dutch hospitals between 2013 and 2016. Resection specimens and endoscopic biopsies taken during clinical response evaluations after nCRT were reviewed by two expert gastrointestinal pathologists. The exact location of residual disease in the oesophageal wall was determined in resection specimens. Endoscopic biopsies were assessed for the presence of structures representing the submucosal layer of the oesophageal wall.
Results
In total, 119 eligible patients underwent clinical response evaluations after nCRT followed by standard surgery. Residual tumour was present in endoscopic biopsies from 70 patients, confirmed on histological analysis of the resected organ. Residual tumour was present in the resection specimen from 27 of the other 49 patients, despite endoscopic biopsies being negative. Of these 27 patients, residual tumour was located in the mucosa in 18, and in the submucosa beneath tumour‐free mucosa in eight. One patient had tumour in muscle beneath tumour‐free mucosa and submucosa.
Conclusion
Most residual disease after nCRT missed by endoscopic biopsies was located in the mucosa. Active surveillance could be improved by more sampling and considering submucosal biopsies.
Remnant cancer missed by endoscopic biopsies was located in the mucosa in two‐thirds of patients with residual disease after neoadjuvant chemoradiotherapy (nCRT). One‐third of patients had residual disease in the submucosa underneath a tumour‐free mucosa. The yield of biopsies in active surveillance after nCRT could be improved by sampling larger areas of oesophageal mucosa and using biopsies targeting the submucosa.
What lies beneath
Antecedentes
Se ha propuesto un seguimiento activo para los pacientes con cáncer de esófago en los que se logra una respuesta clínica completa tras quimiorradioterapia neoadyuvante (neoadjuvant chemoradiotherapy, nCRT). Sin embargo, las biopsias endoscópicas tienen un valor predictivo limitado para detectar la enfermedad residual. En este estudio se evaluó la localización del tumor residual tras la cirugía para poder determinar estrategias de seguimiento y endoscópicas.
Métodos
Este estudio se basa en pacientes que participaron en el ensayo prospectivo preSANO (adenocarcinoma o carcinoma escamoso del esófago o unión esofagogástrica en cuatro hospitales de los Países Bajos entre 2013 y 2016). Los especímenes quirúrgicos, así como las biopsias endoscópicas efectuadas durante las evaluaciones de la respuesta clínica después de nCRT fueron revisadas por dos patólogos gastrointestinales expertos. En los especímenes de resección, se determinó la localización exacta de la enfermedad residual en la pared del esófago. Se evaluaron las biopsias endoscópicas para identificar estructuras que constituyeran la capa submucosa de la pared del esófago.
Resultados
En total, 119 pacientes elegibles fueron sometidos a evaluaciones de la respuesta clínica tras nCRT seguida de cirugía estándar. Se detectó tumor residual en las biopsias endoscópicas de 70 pacientes, luego confirmadas en la histología de la pieza extirpada. Se identificó tumor residual en la pieza de resección de 27 de los otros 49 pacientes, a pesar de que las biopsias endoscópicas fueron negativas. En estos 27 pacientes, 18 presentaban tumor residual en la mucosa y ocho pacientes en la submucosa mas allá de una mucosa libre de tumor. Un paciente tenía tumor en el músculo más allá de una mucosa y submucosa libres de tumor.
Conclusión
La mayoría de los casos de enfermedad residual tras nCRT que no se detectaron en las biopsias endoscópicas, se localizaban en la mucosa. El seguimiento activo podría mejorar con la toma de más muestras y considerando las biopsias submucosas.
Introduction
After neoadjuvant chemoradiotherapy (nCRT) for locally advanced oesophageal cancer, nearly one‐third of patients have a pathologically complete response (pCR; no residual tumour cells in the resection specimen) 1 . This underlines the need to reconsider standard oesophageal resection for all patients after nCRT. Oesophagectomy is associated with postoperative mortality and high morbidity rates. Therefore, it would be beneficial if patients who continue to have a clinically complete response (cCR) during active surveillance could be spared oesophagectomy 2 . During active surveillance, frequent clinical response evaluations (CREs) are performed to assess the presence of residual locoregional disease or distant metastases. The main concern in active surveillance is residual disease remaining undetected during follow‐up. Small nests of residual disease could progress to an unresectable tumour or metastases. Accurate CREs are crucial to an active surveillance strategy.
The preSANO trial 3 , 4 assessed the accuracy of detecting residual disease after nCRT. Endoscopy with biopsies had a sensitivity of 69 per cent for detecting residual tumour with a tumour regression grade (TRG) of 3–4 (more than 10 per cent residual tumour cells), according to the modified Mandard score described by Chirieac and colleagues 5 . The sensitivity increased to 90 per cent when the endoscopic biopsy protocol included bite‐on‐bite biopsies to obtain tissue from the deeper layers of the oesophageal wall. Theoretically, bite‐on‐bite biopsies have the potential to reach deeper layers of the oesophageal wall and therefore to detect submucosal tumours located underneath a tumour‐free mucosa 6 . Submucosal tissue can be identified histologically by the presence of specific anatomical structures that are absent from mucosal biopsies, that is mucinous glands and thick‐walled blood vessels 7 . Although the sensitivity for detection of residual disease increased after the introduction of bite‐on‐bite biopsies, it remains unclear whether this was achieved by deeper sampling of the oesophageal wall or by the fact that, for instance, more biopsies were taken. Furthermore, biopsies alone still have a limited negative predictive value for detection of residual disease after nCRT 8 .
There is a need to investigate how endoscopic surveillance and biopsy protocols can be optimized to minimize sampling errors in this patient population. The aims of this study were to assess the exact location of undetected residual disease after nCRT and to determine the depth of bite‐on‐bite biopsies.
Methods
The present study included patients who participated in the prospective preSANO trial 4 . All patients diagnosed with adenocarcinoma or squamous cell carcinoma of the oesophagus or oesophagogastric junction in four Dutch hospitals (2 academic hospitals and 2 high‐volume teaching hospitals) between 2013 and 2016 were screened for eligibility. Patients were considered eligible for the study if they were scheduled to undergo nCRT followed by oesophagectomy. The nCRT regimen consisted of weekly administration of carboplatin (area under the curve 2 mg per ml per min) and paclitaxel (50 mg per m2 body surface area) for 5 weeks concurrently with 41·4 Gy radiotherapy in 23 fractions. Patients for whom surgical resection specimens were not available for review were excluded from analysis. All patients with detected residual disease from the initiating centre (Erasmus MC – University Medical Centre) were included consecutively and comprised the control group. This group was included to gain more insight in the location of residual tumours that could be detected during CREs. Patients with undetected residual disease from all centres were defined as the study group. The study protocol was approved by the medical ethics committee of Erasmus MC (Rotterdam, MEC‐2013‐211). All patients provided written informed consent for analysis and publication. The study was registered with the Netherlands Trial Register (NTR4834).
Baseline clinical staging and response evaluations
All patients underwent baseline clinical staging using endoscopic biopsies, endoscopic ultrasonography (EUS) with fine‐needle aspiration (FNA) of suspected relevant lymph nodes, and PET–CT. During baseline endoscopy, the distance between the incisors and upper and lower border of the primary tumour was measured. The quadrants of the oesophagus that involved tumour were specified as well. After completion of nCRT, patients underwent one or two clinical response evaluations (CREs). The first (CRE‐1) was planned 4–6 weeks after completion of nCRT, and included endoscopy with biopsies. During CREs, white‐light endoscopy was used with either regular or bite‐on‐bite biopsies using standard‐sized forceps. If no lesions were visible, at least four random biopsies were taken from the original location of the primary tumour described at baseline endoscopy. Additionally, biopsies were taken from all suspected lesions and from the borders of all ulcers. When residual vital tumour cells were detected, patients underwent PET–CT to exclude distant metastases, before oesophagectomy was performed. When no tumour cells were detected during CRE‐1, a second examination (CRE‐2) was planned 10–14 weeks after completion of nCRT. CRE‐2 consisted of PET–CT followed by endoscopic biopsies and EUS with FNA of all suspected lymph nodes. When distant metastases were detected, patients were referred for palliative care. Patients were considered to have achieved a cCR if no residual vital tumour cells were detected during CRE‐1 and CRE‐2 in endoscopic biopsies and in EUS‐guided FNA cytology. In the preSANO trial, all patients underwent standard oesophagectomy. In the present study, undetected residual disease was defined as all residual tumour with TRG 2–4 (at least 1 per cent residual tumour) in the resection specimen that was not detected during CRE‐1 and CRE‐2.
Pathological analysis
Resection specimens and endoscopic biopsies were reviewed in all patients with residual tumour that was not detected by endoscopy during CRE (study group). The exact location of the residual tumour in the resection specimen was determined and compared with that from the control group of patients who had residual tumour detected endoscopically during CRE. Review of the resection specimens and biopsies was done independently by two experienced upper gastrointestinal pathologists. All resection specimens were processed and sampled using a standard protocol 9 . In brief, the surgical tumour bed was sampled extensively or totally. Tissue slides were stained using haematoxylin and eosin, and were subsequently evaluated to acquire information on resection margins, presence of vital tumour cells, tumour type and differentiation grade.
Tumour cells in the resection specimen were considered vital if their cytomorphological integrity was intact. A microscopically radical resection (R0) was defined by the absence of cancer cells at the proximal, distal and circumferential margin of the resection specimen. The resection specimen was scored for overall TRG using the modified Mandard score 5 : TRG 1, no residual tumour cells; TRG 2, 1–10 per cent residual tumour cells; TRG 3, 11–50 per cent residual tumour cells; and TRG 4, more than 50 per cent residual tumour cells. The TRG was also determined for each oesophageal layer: mucosa, submucosa, proper muscle layer and adventitia. The presence of vital tumour cells was assessed relative to the area showing regressional changes (Fig. 1 ). Further quantification of residual vital tumour cells was undertaken in all resection specimens that had undetected residual tumour cells in the mucosal layer, or in the submucosal layer underneath a tumour‐free mucosa. To evaluate the potential for detecting specific submucosal histological structures in the submucosal layer of the oesophageal wall, the relative presence of these structures (mucinous glands and thick‐walled vessels) was assessed in the non‐irradiated distal part of the oesophageal submucosa from three randomly chosen oesophageal resection specimens (Fig. 2 ) 7 .
Fig. 1.
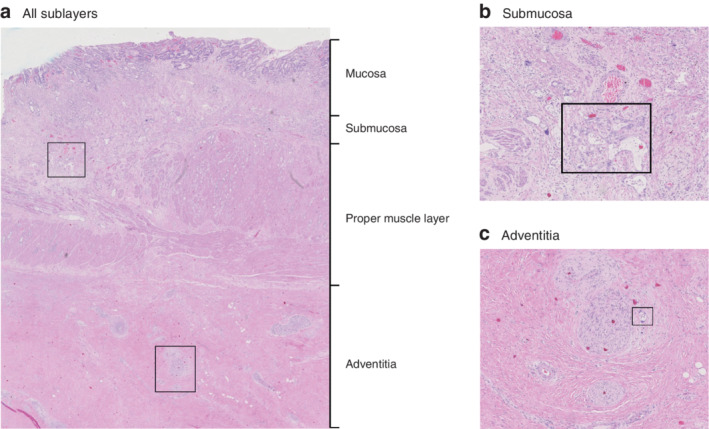
Histology of oesophageal resection specimen a Section from an oesophageal resection specimen showing sublayers. Detailed examples of boxed areas in the submucosa and adventitia are shown in b and c respectively. b The boxed area indicates glandular adenocarcinoma within an area of regressional changes in the submucosa. The submucosa was scored as tumour regression grade (TRG) 3 (more than 10 per cent vital tumour cells). c The boxed area shows vital tumour cells within an area of regressional changes in the adventitia. The adventitia was scored TRG 2 (10 per cent or less vital tumour cells). (Haematoxylin and eosin staining; a × 10 magnification, b,c × 40 magnification.)
Fig. 2.
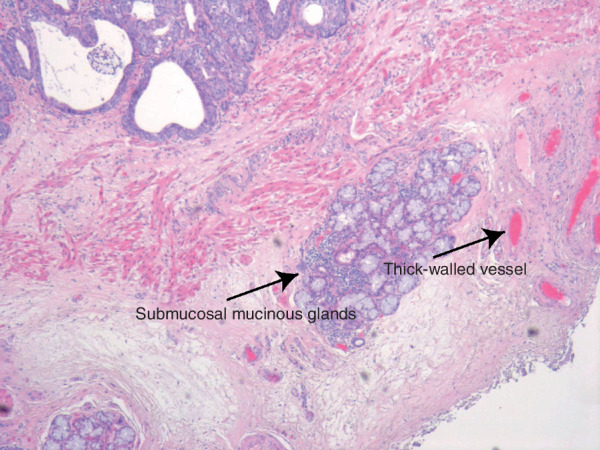
Submucosal mucinous glands and thick‐walled vesselsHistological example of a non‐irradiated (normal) area in an oesophageal resection specimen. The arrows indicate submucosal structures used to identify submucosal tissue in the endoscopic biopsies (haematoxylin and eosin staining, × 40 magnification).
To gain insight into the depth of tissue sampled by endoscopic biopsies, and the potential to detect mucosal and submucosal tumours, all endoscopic biopsies taken during CRE‐1 and CRE‐2 were reviewed for both the presence of mucosal and submucosal tissue, and the presence of vital tumour cells in the submucosal tissue if applicable. The presence of submucosal tissue was defined as described above. If only mesenchymal or ulcerative tissue was detected, the nature of the tissue present in the biopsy was defined as uncertain; otherwise, the tissue was defined as mucosal.
Statistical analysis
Descriptive statistics were used to describe baseline characteristics. Continuous variables are reported as median (i.q.r.). Student's t test or Mann–Whitney U test was used for analysis of continuous variables, and χ2 or Fisher's exact test for comparison of categorical data (the latter when comparing 2 categorical variables, or when events were rare). P < 0·050 (2‐sided) was considered statistically significant. All statistical analyses were done using the tableone package of R version 3.5.1 (R Core Team, R Foundation for Statistical Computing, Boston, Massachusetts, USA).
Results
Between 2013 and 2016, 207 patients underwent nCRT, of whom 119 had one or two CREs followed by standard surgical resection. Tumour cells were detected in 70 of 119 patients during CREs, including 32 patients from the Erasmus MC – University Medical Centre who served as control group. No tumour cells were detected at CREs in 49 of 119 patients, of whom 22 had a pCR in the resection specimen. Vital tumour cells were identified in the resection specimen, which had not been detected in the endoscopic biopsies, in 27 of 49 patients (study group) (Fig. 3 ; Table S1 , supporting information). All included patients underwent CRE‐1 and CRE‐2 within a range of 28–44 and 68–91 days respectively. The bite‐on‐bite technique was used less frequently in patients with residual tumour that remained undetected. These patients also had a lower pathological T status and more often had TRG 2 residual tumour than patients in whom residual tumour was detected during CREs (control group) (Table 1 ).
Fig. 3.
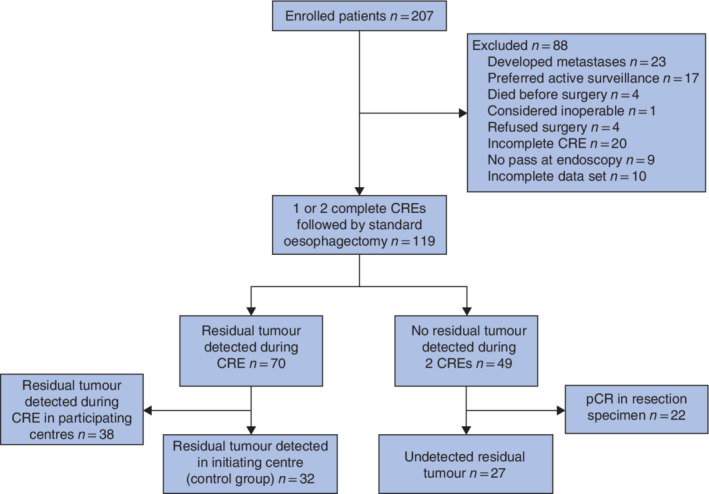
Study flow chart CRE, clinical response evaluation; pCR, pathologically complete response.
Table 1.
Clinicopathological characteristics of patients included in analysis
| Detected residual tumour (n = 32) | Undetected residual tumour (n = 27) | P † | |
|---|---|---|---|
| Age (years) * | 66 (59–70) | 66 (62–70) | 0·937‡ |
| Sex ratio (M : F) | 28 : 4 | 22 : 5 | 0·782 |
| Histology | 0·447 | ||
| Adenocarcinoma | 25 | 24 | |
| Squamous cell carcinoma | 6 | 3 | |
| Adenosquamous cell carcinoma | 1 | 0 | |
| Preoperative T status | 0·112 | ||
| cT2 | 2 | 6 | |
| cT3 | 25 | 20 | |
| cT4 | 5 | 1 | |
| Preoperative N status | 0·554 | ||
| cN0 | 12 | 7 | |
| cN1 | 11 | 9 | |
| cN2 | 8 | 10 | |
| cN3 | 1 | 0 | |
| cNx | 0 | 1 | |
| Type of biopsy | 0·016 | ||
| Regular | 6 | 14 | |
| Bite on bite | 26 | 13 | |
| R0 resection status | 32 | 27 | 1·000 |
| ypT category | 0·016 | ||
| ypT1 | 3 | 11 | |
| ypT2 | 8 | 4 | |
| ypT3 | 21 | 12 | |
| ypN category | 0·079 | ||
| ypN0 | 17 | 21 | |
| ypN1 | 10 | 4 | |
| ypN2 | 5 | 1 | |
| ypN3 | 0 | 1 | |
| TRG | 0·016 | ||
| TRG 2 | 8 | 16 | |
| TRG 3 | 15 | 9 | |
| TGR 4 | 9 | 2 |
Values are median (i.q.r.). TRG, tumour regression grade.
χ2 or Fisher's exact test, except
Mann–Whitney U test.
Analysis of control group with detected residual disease
Some 21 of 32 patients with detected residual disease had vital tumour cells in all layers of the oesophageal wall (Fig. 4a ). The mucosa and submucosa were most frequently involved; both layers were involved in 30 of 32 patients. One patient had residual disease in the submucosal layer underneath a tumour‐free mucosal layer.
Fig. 4.
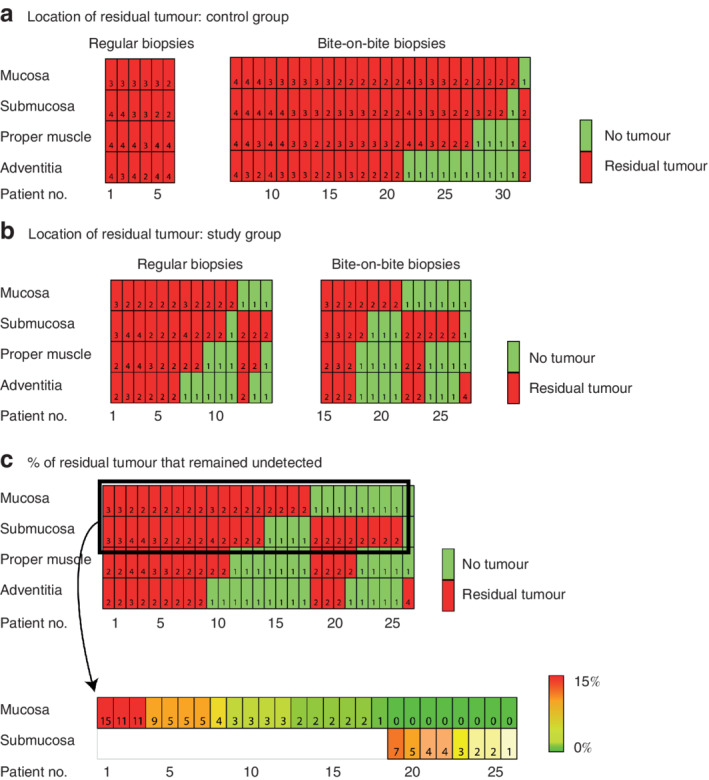
Location of residual tumours and percentage that remained undetected Location of residual tumours in a 32 resection specimens (control group) that were detected accurately by endoscopic biopsy after neoadjuvant chemoradiotherapy and b 27 resection specimens (study group) that remained undetected by endoscopic biopsy after neoadjuvant chemoradiotherapy, according to biopsy type used during clinical response evaluation (CRE). The number in each cell represents the tumour regression grade (TRG): TRG 1, no residual tumour; TRG 2–4, residual tumour. c Percentage of residual tumour cells present in the mucosa or submucosa that remained undetected during CRE in the study group. The results of further quantification are shown in the most superficial layer containing residual tumour cells in the mucosa or submucosa. The number in each cell in the lower part represents the percentage of vital residual tumour cells present.
For these 32 patients, tissue from endoscopic biopsies taken during 41 CREs in total were available for review (32 CRE‐1, 9 CRE‐2) (Table 2 ). Only specific mucosal tissue was detected in the endoscopic biopsies from 16 of 41 CREs. Specific submucosal structures were detected in the endoscopic biopsies from one of the 41 CREs, using bite‐on‐bite biopsies. The origin of the tissue was uncertain in endoscopic biopsies from 24 of 41 CREs.
Table 2.
Specific submucosal structures in endoscopic biopsies
| Detected residual tumour (32 patients) | Undetected residual tumour (27 patients) | |||||
|---|---|---|---|---|---|---|
| All CREs (n = 41) | CRE‐1 (n = 32) | CRE‐2 (n = 9) | All CREs (n = 47) | CRE‐1 (n = 23) | CRE‐2 (n = 24) | |
| Submucosal structures present | ||||||
| Yes | 1 | 1 | 0 | 3 | 1 | 2 |
| No | 16 | 12 | 4 | 34 | 17 | 17 |
| Uncertain | 24 | 19 | 5 | 10 | 5 | 5 |
| Type of biopsy overall | ||||||
| Regular | 10 | 6 | 4 | 26 | 13 | 13 |
| Bite on bite | 31 | 26 | 5 | 21 | 10 | 11 |
| Type of biopsy containing submucosa | ||||||
| Regular | 0 | 1 | ||||
| Bite on bite | 1 | 2 | ||||
| Tumour cells present in truly submucosal biopsies | 0 | 0 | ||||
CRE, clinical response evaluation.
Analysis of study group with undetected residual disease
Nine of 27 patients with undetected residual disease had tumour cells involving all layers of the oesophageal wall. Residual disease was present in the mucosa in 18 patients, and in the submucosa underneath a tumour‐free mucosa in eight patients. In one patient tumour cells were present underneath tumour‐free mucosal and submucosal layers (Fig. 4b ). In the 26 patients with residual tumour present in the mucosa and/or submucosa, residual vital tumour cells were further quantified (Fig. 4c ).
The 27 patients underwent 54 CREs (Table 2). Of these, pathological material from endoscopic biopsies was available from 47 CREs. Specific mucosal tissue was detected in the biopsies from 34 of 47 CREs. Specific submucosal structures were identified in biopsies of three of 47 CREs from two patients, and the origin of the tissue was uncertain in ten of 47 CREs. No tumour cells were present in the biopsies that contained submucosal structures.
Specific submucosal structures in oesophageal submucosa
In all three resection specimens, specific submucosal structures in the normal non‐irradiated oesophagus comprised 1–2 per cent of the submucosal area. Furthermore, in the irradiated part of the oesophagus, (deep) ulceration, scarring and atrophy of the subepithelial layers of the oesophagus in several instances resulted in a more superficial location of these layers than expected. Fig. 5 shows an example of a resection specimen in which the subepithelial tissue (lamina propria) and the submucosal tissue are fibrotic and so the upper border of the proper muscle layer lies adjacent to the epithelial surface.
Fig. 5.
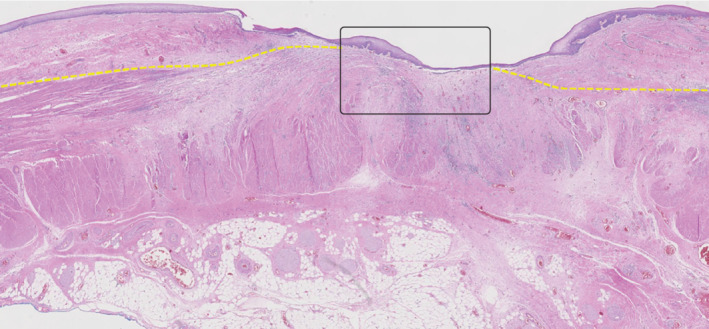
Proper muscle layer adjacent to epithelium Histological example of a resection specimen showing that the proper muscle layer, which is normally located beneath the submucosal layer, is now located adjacent to the epithelium (box), most probably owing to fibrosis after neoadjuvant chemoradiotherapy. Structures normally present in the deeper layers of the oesophageal wall have the potential to be present more superficially after neoadjuvant chemoradiotherapy. The yellow line represents the upper border of the proper muscle layer (haematoxylin and eosin staining, × 10 magnification).
Discussion
In this study, cancer cells were still located in the oesophageal mucosa in two‐thirds of patients with residual disease after nCRT that could not be detected by endoscopic biopsies during CREs. Furthermore, nearly one‐third of patients had undetected residual disease in the submucosa underneath a tumour‐free mucosa. Whether endoscopic biopsies or bite‐on‐bite biopsies had the potential to detect these submucosal tumours is unclear, as submucosal structures were identified in only two of the 27 patients with undetected residual disease. Only one patient had undetected residual disease in deeper layers of the oesophagus beneath a tumour‐free mucosa and submucosa.
All patients included in the present study participated in a multicentre prospective trial with the objective to identify patients who might benefit from an active surveillance strategy in the future. As a result, all patients underwent standardized CREs at two fixed time points after completion of nCRT.
Undetected residual disease was found in the mucosa in two‐thirds of patients, comparable to the findings of a previous retrospective study 10 that reported 68 per cent mucosal involvement. That study from Taiwan included solely patients with squamous cell carcinoma who had a cCR as determined by one CRE at 4–6 weeks after completion of nCRT. Unfortunately, the limited number of patients with squamous cell carcinoma in the present study makes it hard to compare squamous cell carcinoma and adenocarcinoma based on the available data. The undetected residual mucosal disease in the present study was most likely missed owing to sampling error. This could be explained by the presence of very limited and scattered residual disease in the mucosa and submucosa, which could be why endoscopic biopsies alone have shown limited negative predictive value for detection of residual disease after nCRT, both for oesophageal cancer and rectal cancer 8 , 11 , 12 . Sampling of larger mucosal areas, additional biomarkers or imaging is needed to decrease such sampling errors. Wide‐area transepithelial sampling (WATS) involves use of a brush (WATS3D®; CDx diagnostics, Suffern, New York, USA) that is able to sample larger areas of the oesophageal mucosal surface as deep as the muscularis mucosae. WATS has previously been used in an RCT 13 for the detection of high‐grade dysplasia or adenocarcinoma in patients undergoing surveillance for Barrett's oesophagus. An absolute increase of 14 per cent in detection of high‐grade dysplasia and oesophageal adenocarcinoma was reported in a high‐risk referral Barrett's oesophagus population by using WATS compared with random endoscopic biopsies. No studies yet have reported on the use of WATS for CREs in patients with oesophageal cancer after nCRT.
Potentially valuable imaging or biomarker techniques include PET–CT with radiomics or circulating tumour DNA (ctDNA) 14 , 15 , 16 . Although use of PET–CT 12 weeks after completion of nCRT in the preSANO trial resulted in high false‐positive rates, its value is currently being tested in the therapeutic SANO trial beyond 12 weeks after completion of nCRT 17 . Radiomics analysis of PET–CT images (quantification of numerous imaging features) could help enhance prediction of pCR after nCRT 18 , 19 . Use of ctDNA has shown potential in several malignancies, such as colorectal cancer, non‐small cell lung cancer and also oesophageal squamous cell cancer 20 , 21 , 22 , 23 . Imaging and biomarkers could also be of value in patients who have residual disease beneath a normal mucosa and submucosa (4 per cent (1 of 27) here versus 9 per cent in the study of Chao et al.10) as routine endoscopic biopsies do not have the potential to reach these deeper layers.
In this study, 30 per cent of patients (8 of 27) had submucosal residual tumour below a tumour‐free mucosal layer, which is comparable to the 22 per cent reported previously 10 . Earlier studies 6 , 24 suggested that such tumours limited to the submucosa could be detected by bite‐on‐bite biopsies in 17–38 per cent of patients. However, most of these patients had gastric tumours and none underwent neoadjuvant therapy or had carcinoma. Therefore, these results cannot be extrapolated to the setting of oesophageal cancer after nCRT. Here, bite‐on‐bite biopsies were able to detect the cancer cells in only one of nine patients with submucosal residual disease underneath a tumour‐free mucosa. It should be noted, however, that all residual submucosal tumours underneath a tumour‐free mucosa had 10 per cent or less residual tumour (TRG 2). The preSANO trial reported that the sensitivity for detection of TRG 3–4 residual tumours increased from 69 to 90 per cent after the introduction of bite‐on‐bite biopsies. It was hypothesized that this was due to the detection of residual submucosal tumours underneath a tumour‐free mucosa. It is possible that the percentage of detected residual tumours could increase more in a surveillance setting, with endoscopic biopsies performed beyond 12 weeks after nCRT.
This study has several limitations. First, submucosal mucinous glands and thick‐walled vessels comprised only 1–2 per cent of the submucosal layer in the distal part of the non‐irradiated, normal oesophagus. Therefore, it cannot be concluded that the submucosa had not been sampled when these structures were absent from biopsies, especially if radiation‐induced atrophy and therefore the possible disappearance of these specific submucosal structures is also taken into consideration. Conversely, structures located in the deeper layers of the oesophageal wall in the healthy oesophagus could be present more superficially after nCRT owing to ulceration and fibrosis (Fig. 5 ). As such, specific structures do not unconditionally correlate with the depth of biopsy. Second, the group of patients with undetected residual tumour was relatively small and not all resection specimens or pathological material from endoscopic biopsies were available for review. Finally, only patients with detected residual tumour from the initiating centre (Erasmus MC – University Medical Centre) were included, which could have resulted in selection bias. As the primary aim of this study was to determine the location of undetected residual tumour, additional inclusion of patients with detected residual disease would most likely not have affected the main outcomes of this study.
Supporting information
Table S1 ypTNM status and TRG‐status of five patients with undetected residual disease of which resection specimens were not available for revision.
Acknowledgements
The authors declare no conflict of interest.
References
- 1. van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP et al Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 2012; 366: 2074–2084. [DOI] [PubMed] [Google Scholar]
- 2. van der Wilk BJ, Noordman BJ, Neijenhuis LKA, Nieboer D, Nieuwenhuijzen GAP, Sosef MN et al Active surveillance versus immediate surgery in clinically complete responders after neoadjuvant chemoradiotherapy for esophageal cancer: a multicenter propensity matched study. Ann Surg 2019; 10.1097/SLA.0000000000003636 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 3. Noordman BJ, Shapiro J, Spaander MC, Krishnadath KK, van Laarhoven HW, van Berge Henegouwen MI et al Accuracy of detecting residual disease after cross neoadjuvant chemoradiotherapy for esophageal cancer (preSANO Trial): rationale and protocol. JMIR Res Protoc 2015; 4: e79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Noordman BJ, Spaander MCW, Valkema R, Wijnhoven BPL, van Berge Henegouwen MI, Shapiro J et al Detection of residual disease after neoadjuvant chemoradiotherapy for oesophageal cancer (preSANO): a prospective multicentre, diagnostic cohort study. Lancet Oncol 2018; 19: 965–974. [DOI] [PubMed] [Google Scholar]
- 5. Chirieac LR, Swisher SG, Ajani JA, Komaki RR, Correa AM, Morris JS et al Posttherapy pathologic stage predicts survival in patients with esophageal carcinoma receiving preoperative chemoradiation. Cancer 2005; 103: 1347–1355. [DOI] [PubMed] [Google Scholar]
- 6. Ji JS, Lee BI, Choi KY, Kim BW, Choi H, Huh M et al Diagnostic yield of tissue sampling using a bite‐on‐bite technique for incidental subepithelial lesions. Korean J Intern Med 2009; 24: 101–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kaye PV, O'Donovan M, Mapstone N, Disep B, Novelli M, Ragunath K. Pathologists are able to differentiate reliably the lamina propria associated with Barrett's musculofibrous anomaly from submucosa in oesophageal endoscopic resections. Histopathology 2015; 67: 914–917. [DOI] [PubMed] [Google Scholar]
- 8. Sarkaria IS, Rizk NP, Bains MS, Tang LH, Ilson DH, Minsky BI et al Post‐treatment endoscopic biopsy is a poor‐predictor of pathologic response in patients undergoing chemoradiation therapy for esophageal cancer. Ann Surg 2009; 249: 764–767. [DOI] [PubMed] [Google Scholar]
- 9. van Meerten E, van der Gaast A, Tilanus HW, Poley JW, Muller K, van Dekken H. Pathological analysis after neoadjuvant chemoradiotherapy for esophageal carcinoma: the Rotterdam experience. J Surg Oncol 2009; 100: 32–37. [DOI] [PubMed] [Google Scholar]
- 10. Chao YK, Chuang WY, Yeh CJ, Chang HK, Tseng CK. Anatomical distribution of residual cancer in patients with oesophageal squamous cell carcinoma who achieved clinically complete response after neoadjuvant chemoradiotherapy. Eur J Cardiothorac Surg 2018; 53: 201–208. [DOI] [PubMed] [Google Scholar]
- 11. Eyck BM, Onstenk BD, Noordman BJ, Nieboer D, Spaander MCW, Valkema R et al Accuracy of detecting residual disease after neoadjuvant chemoradiotherapy for esophageal cancer: a systematic review and meta‐analysis. Ann Surg 2020; 271: 245–256. [DOI] [PubMed] [Google Scholar]
- 12. Perez RO, Habr‐Gama A, Pereira GV, Lynn PB, Alves PA, Proscurshim I et al Role of biopsies in patients with residual rectal cancer following neoadjuvant chemoradiation after downsizing: can they rule out persisting cancer? Colorectal Dis 2012; 14: 714–720. [DOI] [PubMed] [Google Scholar]
- 13. Vennalaganti PR, Kaul V, Wang KK, Falk GW, Shaheen NJ, Infantolino A et al Increased detection of Barrett's esophagus‐associated neoplasia using wide‐area trans‐epithelial sampling: a multicenter, prospective, randomized trial. Gastrointest Endosc 2018; 87: 348–355. [DOI] [PubMed] [Google Scholar]
- 14. Creemers A, Krausz S, Strijker M, van der Wel MJ, Soer EC, Reinten RJ et al Clinical value of ctDNA in upper‐GI cancers: a systematic review and meta‐analysis. Biochim Biophys Acta Rev Cancer 2017; 1868: 394–403. [DOI] [PubMed] [Google Scholar]
- 15. Tian X, Sun B, Chen C, Gao C, Zhang J, Lu X et al Circulating tumor DNA 5‐hydroxymethylcytosine as a novel diagnostic biomarker for esophageal cancer. Cell Res 2018; 28: 597–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Valkema MJ, van der Wilk BJ, Eyck BM, Wijnhoven BPL, Spaander MCW, Lagarde SM et al Surveillance using FDG‐uptake in the primary tumour on PET/CT in patients with oesophageal cancer and a clinically complete response after neoadjuvant chemoradiotherapy. Dis Esophagus 2019; 32(Suppl 2): doz092.112. [Google Scholar]
- 17. Noordman BJ, Wijnhoven BPL, Lagarde SM, Boonstra JJ, Coene PPLO, Dekker JWT, Doukas M et al; SANO‐study group. Neoadjuvant chemoradiotherapy plus surgery versus active surveillance for oesophageal cancer: a stepped‐wedge cluster randomised trial. BMC Cancer 2018; 18: 142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lambin P, Leijenaar RTH, Deist TM, Peerlings J, de Jong EEC, van Timmeren J et al Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol 2017; 14: 749–762. [DOI] [PubMed] [Google Scholar]
- 19. Tan S, Kligerman S, Chen W, Lu M, Kim G, Feigenberg S et al Spatial‐temporal [18F]FDG‐PET features for predicting pathologic response of esophageal cancer to neoadjuvant chemoradiation therapy. Int J Radiat Oncol Biol Phys 2013; 85: 1375–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chaudhuri AA, Chabon JJ, Lovejoy AF, Newman AM, Stehr H, Azad TD et al Early detection of molecular residual disease in localized lung cancer by circulating tumor DNA profiling. Cancer Discov 2017; 7: 1394–1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tie J, Wang Y, Tomasetti C, Li L, Springer S, Kinde I et al Circulating tumor DNA analysis detects minimal residual disease and predicts recurrence in patients with stage II colon cancer. Sci Transl Med 2016; 8: 346ra92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hsieh CC, Hsu HS, Chang SC, Chen YJ. Circulating cell‐free DNA levels could predict oncological outcomes of patients undergoing esophagectomy for esophageal squamous cell carcinoma. Int J Mol Sci 2016; 17: pii: E2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Luo H, Li H, Hu Z, Wu H, Liu C, Li Y et al Noninvasive diagnosis and monitoring of mutations by deep sequencing of circulating tumor DNA in esophageal squamous cell carcinoma. Biochem Biophys Res Commun 2016; 471: 596–602. [DOI] [PubMed] [Google Scholar]
- 24. Cantor MJ, Davila RE, Faigel DO. Yield of tissue sampling for subepithelial lesions evaluated by EUS: a comparison between forceps biopsies and endoscopic submucosal resection. Gastrointest Endosc 2006; 64: 29–34. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 ypTNM status and TRG‐status of five patients with undetected residual disease of which resection specimens were not available for revision.


