Abstract
Background
A renal biopsy is needed to define active inflammatory infiltration and guide therapeutic management in drug-induced acute tubulointerstitial nephritis (D-ATIN). However, factors such as various contraindications, refusal of informed consent and limited technical support may stop the biopsy process. It is thus of great importance to explore approaches that could deduce probable pathologic changes.
Methods
A total of 81 biopsy-proven D-ATIN patients were enrolled from a prospective cohort of ATIN patients at Peking University First Hospital. The systemic inflammation score (SIS) was developed based on the CRP and ESR levels at biopsy, and patients were divided into high-SIS, median-SIS, and low-SIS groups. The demographic data, clinicopathologic features, and renal outcomes were compared.
Results
The SIS was positively correlated with inflammatory cell infiltration and was inversely correlated with interstitial fibrosis. The number of interstitial inflammatory cells increased significantly with increasing SISs. The proportions of neutrophils and plasma cells were the highest in the high-SIS group compared with the other two groups. Prednisone (30–40 mg/day) was prescribed in all patients. The high-SIS group tended to have more favorable renal restoration than the other two groups. By 12 months postbiopsy, a decreased eGFR (< 60 mL/min/1.73 m2) was observed in 66.7% of medium-SIS patients, 32.4% of high-SIS patients, and 30.4% of low-SIS patients.
Conclusion
The SIS was positively correlated with active tubulointerstitial inflammation and therefore could help to aid therapeutic decisions in D-ATIN.
Keywords: C reactive protein, Erythrocyte sedimentation rate, Interstitial inflammation, Drug-induced acute tubulointerstitial nephritis
Background
Acute tubulointerstitial nephritis (ATIN) is a common renal lesion histopathologically characterized by inflammation and edema of the renal interstitium. It is responsible for 15–27% of acute kidney injury (AKI) [1–5], with drugs being the most common cause [6–10]. Unlike ischemic or toxic AKI, which usually induces acute tubular injury and results in an abrupt decline in renal function, patients with drug-induced ATIN (D-ATIN) sometimes have insidious renal dysfunction and are therefore more likely experience delayed recognition. A renal biopsy is needed to make a definitive diagnosis of D-ATIN and reveals the activity and severity of interstitial inflammation that usually directs immunosuppressive treatment [11–13]. However, factors such as various contraindications, refusal of informed consent and limited technical support may stop the process of renal biopsy. It is thus of great importance for those patients clinically suspected of having D-ATIN, in whom renal biopsy cannot be conducted, to explore approaches that could deduce probable pathologic changes and indicate the severity of interstitial inflammatory cell infiltration, which could therefore help make therapeutic decisions.
The erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are traditional inflammatory markers that have been used to help assess the activity of inflammation in various diseases, such as systemic lupus erythematosus [14–17], rheumatoid arthritis [18, 19], and vasculitis [20]. However, there is still a lack of knowledge about the relevance of these systemic inflammatory parameters to renal inflammation. The current study was performed in a prospective cohort of D-ATIN patients. The clinical-pathological features and renal recovery of patients with different CRP and ESR levels were compared. Associations between systemic inflammation and renal tubulointerstitial inflammation as well as long-term renal outcomes were further analyzed.
Methods
Patients
The study was approved by the Committee on Research Ethics of Peking University First Hospital. Patients who were clinicopathologically diagnosed with D-ATIN from January 1, 2005, to December 31, 2018, and who were followed for at least 12 months were screened in a prospective cohort of ATIN patients in Peking University First Hospital as previously described [21]. The diagnosis of D-ATIN was made based on previously described criteria [22]. The presence of prominent interstitial inflammation in the nonfibrotic cortex and tubulitis was essential for the pathologic diagnosis of ATIN. All patients were screened for autoimmune diseases, malignancy and infectious diseases and accepted ophthalmological examinations to identify tubulointerstitial nephritis and uveitis syndrome (TINU) during their hospital stay. The cause of ATIN was reevaluated at every visit by the follow-up nephrologist group. Altogether, 81 patients with a final diagnosis of D-ATIN were enrolled in the current study.
Clinical parameter evaluation and grouping for systemic inflammation
Clinical parameters and laboratory data were documented. Acute kidney disease (AKD) was defined using the Kidney Disease: Improving Global Outcomes (KDIGO) criteria [23] and consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup [24]. The ESR was assessed by the Westergren method (Greiner bio-one, Germany), and CRP was detected by rate nephelometry (IMMAGE 800, Beckman Coulter, America) at the time of biopsy. The ESR and CRP levels were categorized by quartile and ranked from 0 ~ 3 points (Table 1). The systemic inflammatory score (SIS) was calculated by combining the ESR and CRP points, and patients were classified into 3 systemic inflammation groups: low-SIS (score 0–1), medium-SIS (score 2–3) and high-SIS (score 4–6) groups. The scatter plot for CRP versus ESR values in different SIS groups was shown in Fig. 1.
Table 1.
Scoring system based on values of ESR and CRP
| CRP (mg/dL) | ESR (mm/hr) | |||
|---|---|---|---|---|
| < 30 (0 Point) |
30–50 (1 Points) |
50–86 (2 Points) |
≥86 (3 Points) |
|
| < 3.6 (0 Point) | 0 | 1 | 2 | 3 |
| 3.6–9.6 (1 Points) | 1 | 2 | 3 | 4 |
| 9.6–25.0 (2 Points) | 2 | 3 | 4 | 5 |
| ≥25.0 (3 Points) | 3 | 4 | 5 | 6 |
Fig. 1.
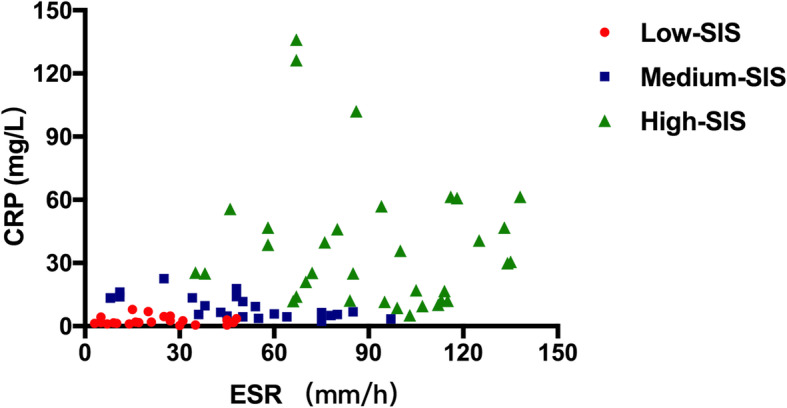
Scatter plot for CRP versus ESR values in different SIS groups
Evaluation of renal pathologic features
All kidney biopsy tissues were processed for light microscopy, immunofluorescence, and electron microscopy. Semiquantitative scores for interstitial edema, infiltration, fibrosis, tubulitis and tubular atrophy were assessed by two pathologists referring to a modification of the Banff Working Classification [25, 26]. The activity index was the total of the scores for interstitial edema, infiltration and tubulitis. The chronicity index was the total of the scores for interstitial fibrosis and tubular atrophy.
Immunofluorescence staining of infiltrated inflammatory cells
Infiltrating cells were identified by immunofluorescence staining with antibodies against CD3 (T lymphocytes, 1:100, ZM-0417, ZSGB-BIO), CD20 (B lymphocytes, 1:100, ZA-0293, ZSGB-BIO), CD38 (plasma cells, 1:250, ab108403, Abcam), CD68 (monocytes/macrophages, 1:500, ZM-0060, ZSGB-BIO), and neutrophil elastic protease antibodies (neutrophils, 1:200, GWB-8F72C4, Genway-Bio) and were counted at 400x magnification. Eosinophils were detected with hematoxylin and eosin staining and counted at 200x magnification. The quantitation of tubulointerstitial infiltration was determined by averaging the counts of five randomly selected fields. The mean values are expressed as cells per millimeter squared.
Follow-up, renal recovery and renal outcome
Serum creatine (sCr) was routinely performed during the follow-up periods. Renal recovery was based on sCr levels at 6 months postbiopsy. Complete recovery was defined as improvement in sCr levels to within 25% of baseline (or to 133 μmol/L if the baseline was not available); partial recovery as a > 50% decrease in sCr level from its peak value but not reaching within 25% of its baseline value; and no recovery as the failure to meet the criteria for complete or partial recovery or remaining on renal replacement therapy (RRT). The renal outcome was defined by the estimated glomerular filtration rate (eGFR) at 12 months postbiopsy. The eGFR was calculated by the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [27] and expressed as milliliters per minute per 1.73 m2.
Statistical analysis
Analyses were performed using SPSS 22.0 Statistics software (IBM Corp., Armonk, NY) and GraphPad Prism version 6 (GraphPad Software, San Diego, CA). Categorical variables were expressed as counts and percentages. Continuous data with a normal distribution were presented as the mean and s.d., and those with an abnormal distribution were presented as the median and 25th–75th percentile. To assess group differences, one-way analyses of variance and Chi-squared analyses were conducted. Bonferroni post hoc comparisons were computed when significant differences emerged. Spearman’s rank correlation coefficient was used as a measure of correlations between the SIS and clinicopathological parameters. Multiple linear regression analysis was computed with the activity index as the dependent variable and with the following variables as explanatory variables: SIS, sex, age, disease course, and hemoglobin and eGFR levels at biopsy. Binary logistic regression analysis was used for predictors and ROC for cutoff points. A two-sided P < 0.05 was considered statistically significant.
Results
Baseline demographic and clinical data
As expressed in Table 2, the average age of the 81 D-ATIN patients was 45.4 ± 12.9 years, with a female predominance (51/81, 63.0%). The interval from the initiation of drug use to the diagnostic biopsy was 30 (14, 63) days. The majority of patients (77/81, 95.1%) were identified as having AKD, and 4 patients (4.9%) were classified with CKD. Eighteen patients (22.2%) required and initiated RRT before the biopsy. Seven patients (8.6%) were oliguric. Twenty patients (24.7%) had an allergic history. Common clinical features included digestive symptoms (61.7%), weakness (48.1%), fever (45.7%) and rash (16.0%). Beta-lactams, herbal medicine and nonsteroidal anti-inflammatory drugs were the most prevalent culprit agents (45.7, 39.5 and 32.1%, respectively). Thirty-eight patients (46.9%) were identified as using more than one kind of culprit drug.
Table 2.
Demographic and clinical features in different SIS groups
| Variables | Total N = 81 |
Low-SIS N = 23 |
Medium-SIS N = 24 |
High-SIS N = 34 |
P-value |
|---|---|---|---|---|---|
| Female, n(%) | 51 (63.0) | 11 (47.8) | 16 (66.7) | 24 (70.6) | 0.197 |
| Age (year) | 45.4 ± 12.9 | 44.4 ± 13.2 | 47.5 ± 13.1 | 44.5 ± 12.96 | 0.643 |
| Disease course (day)a | 30 (14, 63) | 30 (20, 52) | 30 (20, 57) | 17 (10, 60) | 0.798 |
| Allergic history, n(%) | 20 (24.7) | 6 (26.1) | 6 (25.0) | 8 (23.5) | 0.975 |
| Fever, n(%) | 37 (45.7) | 8 (34.8) | 11 (45.8) | 18 (52.9) | 0.402 |
| Rash, n(%) | 13 (16.0) | 4 (17.4) | 3 (12.5) | 6 (17.6) | 0.847 |
| AKD, n(%) | 77 (95.1) | 19 (82.6) | 20 (100.0)* | 27 (100.0)* | 0.005 |
| RRT, n(%) | 18 (22.2) | 1 (4.3) | 9 (37.5)* | 8 (23.5)* | 0.023 |
| Oliguria, n(%) | 7 (8.6) | 0 (0) | 2 (8.3) | 5 (14.7) | 0.064 |
| Suspected drug, n(%) | |||||
| Beta-lactams | 37 (45.7) | 11 (47.8) | 8 (33.3) | 18 (52.9) | 0.326 |
| Herbal medicine | 32 (39.5) | 13 (56.5) | 10 (41.7) | 9 (26.5) | 0.072 |
| NSAIDs | 26 (32.1) | 7 (30.4) | 7 (29.2) | 12 (35.3) | 0.868 |
| PPIs | 6 (7.4) | 2 (8.7) | 4 (16.7) | 0 (0.0)# | 0.023 |
| Laboratory tests | |||||
| SCr at peak (μmol/L) | 322 (220, 531) | 269 (158, 329) | 417 (242, 646) * | 358 (248, 521) * | 0.021 |
| SCr at biopsy (μmol/L) | 249 (160, 386) | 151 (118, 235) | 274 (205, 585) * | 321 (185, 449) * | < 0.001 |
| Hematuria, n (%) | 21 (25.9) | 3 (13.0) | 9 (37.5) | 9 (26.5) | 0.160 |
| Leukocyturia, n (%) | 46 (56.8) | 8 (34.8) | 11 (45.8) | 27 (79.4)* # | 0.002 |
| UTP (g/24 h) | 1.1 (0.5, 1.5) | 0.6 (0.2, 1.3) | 1.1 (0.3, 1.5) | 1.2 (0.9, 1.6) * | 0.038 |
| U-NAG (U/L) | 26 (15, 47) | 37 (16, 57) | 20 (13, 33) | 25 (15, 48) | 0.215 |
| U-α1MG (mg/L) | 171 (74, 238) | 76 (26, 218) | 154 (73, 252) | 206 (136, 271) * | 0.031 |
| U-mAlb (mg/L) | 64 (36, 134) | 49 (15, 134) | 60 (36, 110) | 75 (56, 159) | 0.147 |
| Renal glycosuria, n (%) | 62 (76.5) | 15 (65.2) | 18 (75.0) | 29 (85.3) | 0.210 |
| U-Osm decrease, n(%) | 60 (74.1) | 14 (60.9) | 20 (83.3) | 26 (76.5) | 0.196 |
| RTA, n (%) | 43 (53.1) | 6 (26.1) | 15 (62.5) * | 22 (64.7) * | 0.009 |
| Hemoglobin (g/L) | 104.0 ± 16.6 | 114.7 ± 14.0 | 103.0 ± 20.2* | 97.5 ± 12.6* | 0.001 |
| Hypokalemia, n (%) | 37 (45.7) | 9 (39.1) | 10 (41.7) | 18 (52.9) | 0.853 |
| ESR (mm/h) | 61.0 ± 37.1 | 25.6 ± 14.3 | 48.8 ± 25.6* | 91.5 ± 28.5*# | < 0.001 |
| CRP (mg/L) | 9.7 (3.6, 25.1) | 1.9 (1.3, 3.6) | 6.7 (4.9, 13.4) * | 27.6 (12.3, 49.0)*# | < 0.001 |
| IgG (g/L) | 15.6 ± 4.4 | 14.0 ± 4.0 | 15.2 ± 3.3 | 16.9 ± 5.7 | 0.681 |
| C3 (mg/L) | 1.1 ± 0.3 | 0.9 ± 0.2 | 1.1 ± 0.2* | 1.3 ± 0.2*# | < 0.001 |
Abbreviations: SIS systemic inflammatory score; AKD acute kidney disease; RRT renal replacement therapy; NSAIDs non-steroidal anti-inflammatory drugs; PPIs proton pump inhibitors; sCr serum creatinine; eGFR estimated glomerular filtration rate; UTP urinary total protein; U-KIM1 urinary kidney injury molecular 1; U-NAG urinary N-acetyl-β-D-glucosaminidase; U-α1MG urinary α1 microglobulin; U-mAlb urinary microalbumin; U-Osm urinary osmolality; RTA renal tubular acidosis; IgG immunoglobulin G; C3 complement 3
Normal range: U-NAG (0.3–12) U/L, U-α1MG (0–12) mg/L, U-mAlb (0–19) mg/L, ESR (0–15) mm/h, CRP (0–8) mg/L, IgG (7.2–16.9) g/L, C3 (0.6–1.5) mg/L
a Disease course was defined as the interval from initiation of drug use to the diagnostic biopsy
*compared with low-SIS group, P < 0.05; # compared with medium-SIS group, P < 0.05
Clinical relevance of the SIS in D-ATIN patients
Of the 81 D-ATIN patients, the ESR was elevated in 70 (86.4%), with an average level of 61.0 mm/hr. CRP was elevated in 44 patients (54.3%), with a median value of 9.7 mg/L (Table 2). SISs evaluated by both ESR and CRP levels were positively correlated with sCr values at renal biopsy (r = 0.440; P < 0.001), leukocyturia (r = 0.366; P = 0.001) and C3 levels (r = 0.533; P < 0.001) (Additional Table 1).
Based on the SIS values, there were 23 patients in the low-SIS group, 24 in the medium-SIS group and 34 in the high-SIS group. There was no significant difference in age, sex, allergic manifestations, or causal medications among the three groups of patients. Patients in the low-SIS group had the mildest kidney injuries, with the lowest sCr levels at renal biopsy (median value: 151 μmol/L, P < 0.001), lowest RRT rate (4.3%, P = 0.023) and highest hemoglobin concentration (114.7 ± 14.0 g/L, P = 0.001). It is interesting to note that patients in the medium-SIS group tended to have higher peak sCr levels (median 417 vs 358 μmol/L) and RRT rates (37.5% vs 23.5%) than those in the high-SIS group, yet their disease courses were relatively longer (median 30 vs 17 days) with lower levels of sCr at biopsy (median 274 vs 321 μmol/L). In addition, patients in the high-SIS group had significantly higher C3 levels (1.3 ± 0.2 vs 1.1 ± 0.2 mg/L, P < 0.001) with a greater prevalence of leukocyturia (79.4% vs 45.8%, P = 0.002) than those in the medium-SIS group (Table 2).
Pathological relevance of the SIS in D-ATIN patients
Compared to patients in the low-SIS and medium-SIS groups, those in the high-SIS group had the highest degree of interstitial inflammation (P < 0.001) and the lowest degree of interstitial fibrosis (P = 0.030) (Table 3). The SIS was positively correlated with renal interstitial inflammatory cell infiltration (r = 0.508; P < 0.001) and interstitial edema (r = 0.294; P = 0.008) and inversely correlated with interstitial fibrosis (r = − 0.266; P = 0.016) (Additional Table 1). Multiple linear regression analysis demonstrated that only the SIS was significantly correlated with the renal activity index (β coefficient = 0.293, P = 0.003).
Table 3.
Pathology features in different SIS groups
| Variables | Total N = 81 |
Low-SIS N = 23 |
Medium-SIS N = 24 |
High-SIS N = 34 |
P-value |
|---|---|---|---|---|---|
| Semiquantitative pathologic score | |||||
| Activity index | 4 (3, 5) | 3 (2, 4) | 3 (2, 4) | 4 (4, 5)*# | < 0.001 |
| Interstitial edema | 1 (0, 1) | 1 (0, 1) | 1 (0, 1) | 1 (1, 1)* | 0.044 |
| Interstitial inflammation | 3 (2, 4) | 2 (2, 3) | 2 (2, 3) | 4 (3, 4)*# | < 0.001 |
| Tubulitis | 0 (0, 0) | 0 (0, 1) | 0 (0, 1) | 0 (0, 0) | 0.218 |
| Chronicity index | 1 (0, 2) | 1 (0, 3) | 0 (0, 2) | 1 (0, 2) | 0.438 |
| Interstitial fibrosis | 0 (0, 1) | 0 (0, 2) | 0 (0, 2) | 0 (0, 0)* | 0.030 |
| Tubular atrophy | 0 (0, 2) | 1 (0, 2) | 0 (0, 1) | 1 (0, 2) | 0.629 |
| Interstitial inflammatory cell counts | |||||
| Total cellsa | 391.5 ± 135.5 | 294.8 ± 145.4 | 378.2 ± 97.8 | 450.4 ± 124.0* | 0.001 |
| T lymphocytes | 173.9 ± 63.6 | 137.6 ± 72.3 | 170.5 ± 64.0 | 195.5 ± 50.08* | 0.019 |
| B lymphocytes | 45.4 (30.4, 62.0) | 34.7 (14.4, 41.6) | 45.6 (30.7, 60.4) | 56.4 (40.1, 69.1)* | 0.040 |
| Monocytes/macrophages | 101.8 ± 34.8 | 77.6 ± 35.9 | 90.7 ± 30.5 | 121.6 ± 24.9*# | < 0.001 |
| Plasma cells | 43.8 ± 24.3 | 30.3 ± 20.7 | 32.6 ± 19.3 | 57.9 ± 21.7*# | < 0.001 |
| Neutrophils | 15.4 (4.9, 33.0) | 2.9 (1.7, 13.8) | 7.9 (4.7, 20.4) | 31.7 (15.7, 48.8)*# | < 0.001 |
| Eosinophilsb | 2.1 (0.5, 5.1) | 0.4 (0.1, 1.7) | 0.8 (0.0, 1.9) | 3.8 (2.2, 9.0) *# | < 0.001 |
| Percentages of Interstitial inflammatory cells (%) | |||||
| T lymphocytes | 44.3 ± 9.0 | 46.9 ± 8.5 | 46.1 ± 10.1 | 41.7 ± 8.2 | 0.136 |
| B lymphocytes | 11.7 (9.1, 14.2) | 10.6 (8.8, 14.5) | 12.6 (9.4, 14.9) | 11.5 (8.7, 14.0) | 0.263 |
| Monocytes/macrophages | 26.0 (21.3, 29.9) | 25.8 (21.5, 30.9) | 25.7 (19.9, 30.1) | 26.2 (23.4, 29.1) | 0.670 |
| Plasma cells | 10.9 ± 5.2 | 9.4 ± 4.4 | 9.2 ± 5.7 | 12.6 ± 4.9*# | 0.047 |
| Neutrophils | 4.2 (1.6, 7.8) | 1.1 (0.9, 5.4) | 2.4 (1.7, 4.8) | 7.5 (4.3, 11.7)*# | < 0.001 |
Abbreviations: SIS systemic inflammatory score
a Total cells count was the sum of T lymphocytes, B lymphocytes, macrophages, plasma cells and neutrophil under 400× magnification
b Eosinophils were counted under 200× magnification
*: compared with low-SIS group, P < 0.05; #: compared with medium-SIS group, P < 0.05
We next investigated renal interstitial inflammatory cell types through immunofluorescence staining. The number of each kind of interstitial inflammatory cell increased significantly with the increase in SISs (Table 3). When focusing on the constitution of inflammatory cells, the proportions of neutrophils (7.5% vs 2.4% in medium-SIS vs 1.1% in low-SIS; P < 0.001) and plasma cells (12.6% vs 9.2% in medium-SIS vs 9.4% in low-SIS; P = 0.047) were the highest in patients in the high-SIS group compared with those in the other two groups. There was no significant difference in the proportions of T lymphocytes, B lymphocytes or macrophages among the three groups of patients. Eosinophils, which favor a diagnosis of drug-induced ATIN, were also highest in the high-SIS group (median value: 3.8 vs 0.8 in medium-SIS vs 0.4 in low-SIS; P < 0.001).
Treatment and outcome among three groups with different SISs
As shown in Table 4, prednisone was prescribed at a dosage of 30–40 mg/day in all the patients. Additional immunosuppressive agents, such as mycophenolate, azathioprine and cyclophosphamide, were used in 27.2% (22/81) of patients, with no significant difference among the three groups (P = 0.436). Methylprednisolone pulse therapy was performed in 22.2% (18/81) of all patients, and none of the low-SIS patients received methylprednisolone pulse therapy.
Table 4.
Treatment and renal outcome in different SIS groups
| Variables | Total N = 81 |
Low-SIS N = 23 |
Medium-SIS N = 24 |
High-SIS N = 34 |
P-value |
|---|---|---|---|---|---|
| Immunosuppressive treatment, n (%) | |||||
| Prednisone only | 52 (64.2) | 19 (82.6) | 15 (62.5) | 18 (52.9) | 0.071 |
| Methylprednisolone pulse therapy | 18 (22.2) | 0 (0) | 6 (25.0)* | 12 (35.3)* | 0.007 |
| Immunosuppressive medications | 22 (27.2) | 4 (17.4) | 8 (33.3) | 10 (29.4) | 0.436 |
| Renal recovery at 6 months post-biopsy, n(%) | |||||
| Complete | 52 (64.2) | 15 (65.2) | 12 (50.0) | 25 (73.5) | 0.195 |
| Partial | 28 (34.6) | 7 (30.4) | 12 (50.0) | 9 (26.5) | |
| None | 1 (1.2) | 1 (4.3) | 0 (0) | 0 (0) | |
| Renal outcome evaluated by eGFR (mL/min/1.73 m2) | |||||
| ≥ 60 | 47 (58.0) | 16 (69.6) | 8 (33.3)* | 18 (67.6)# | 0.014 |
| < 60 | 28 (42.0) | 7 (30.4) | 16 (66.7) | 11 (32.4) | |
Abbreviations: SIS systemic inflammatory score; eGFR estimated glomerular filtration rates; CKD chronic kidney disease; CRP C reactive protein; ESR erythrocyte sedimentation rate
*: compared with low-SIS group, P < 0.05; #: compared with medium-SIS group, P < 0.05
Patients were followed for at least 12 months (range: 12–132 months, median 38 months). The high-SIS group tended to have more favorable renal restoration than the other two groups (Fig. 2). At 6 months postbiopsy, complete recovery was achieved in 73.5% of high-SIS patients, 50.0% of medium-SIS patients, and 65.2% of low-SIS patients (P = 0.195). A decreased eGFR (< 60 mL/min/1.73 m2) was observed in 32.4% of high-SIS patients, 66.7% of medium-SIS patients, and 30.4% of low-SIS patients (P = 0.014) at 12 months postbiopsy (Table 4). Adding SIS as a continuous variable to age and eGFR measured at biopsy made a small increase for the area under receiver operating characteristic curve by using the logistic regression analysis (from 0.696 to 0.731 for complete recovery at 6 months and from 0.852 to 0.875 for decreased eGFR at 12 months).
Fig. 2.
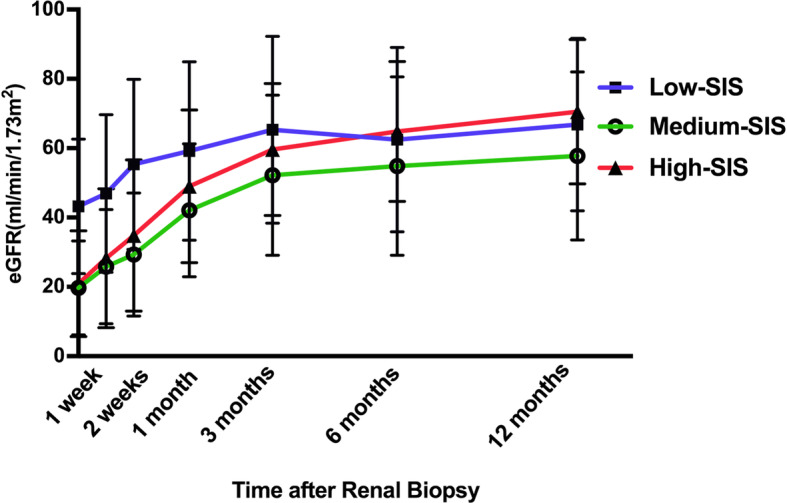
The restoration of renal function in different SIS groups during the first year postrenal biopsy. Patients in both the medium-SIS and high-SIS groups had significant renal dysfunction at the time of renal biopsy, and high-SIS patients presented with more rapid renal function restoration. Low-SIS patients had modest renal dysfunction and modest restoration of renal function
Fifty-four patients with severe renal dysfunction at the time of biopsy (eGFR < 30 mL/min/1.73 m2) were divided into high-score (N = 26) and low-score (N = 28) subgroups based on the SIS. The eGFR values at biopsy were similar in the two subgroups (14.3 ± 7.8 mL/min/1.73 m2 in high-score vs 17.7 ± 8.5 in low-score, P = 0.131). At 12 months postbiopsy, the eGFR values were significantly higher in the high-score subgroup (65.3 ± 20.2 vs 52.9 ± 20.9 mL/min/1.73 m2 in low-score, P = 0.032).
Discussion
D-ATIN is a relatively common cause of AKI. Previously, the ESR and CRP were reported to be significantly elevated in D-ATIN patients [13, 28]. The current study first demonstrated that the SIS evaluated by the ESR and CRP was correlated with active renal tubulointerstitial inflammation and renal restoration in a prospective cohort of D-ATIN patients and therefore could help to aid therapeutic decisions when a renal biopsy is not acceptable or cannot be performed serially in this disease condition.
Patients with D-ATIN often present with a relatively insidious onset and a disease process of subacute renal dysfunction, with oliguria not commonly seen [13]. Therefore, a delayed diagnosis is likely to be encountered, especially when patients initially present at non-nephrology departments, as shown in our study, where the median time course from the initial use of suspicious drugs to diagnostic renal biopsy was 30 days, even exceeding 3 months in some cases. Once acute interstitial inflammation sets in, it can progress rapidly to a less reversible, more destructive fibrogenic process [29]. Therefore, the delay in diagnosis and treatment may result in complexity in the pathophysiologic process containing both active inflammation and fibrotic lesions in patients with D-ATIN. It is crucial to make a treatment decision with evidence that reflects renal interstitial active inflammation, yet renal biopsy, the gold standard for histological evaluation, is invasive and not acceptable for all patients. Following multivariate analysis, we observed that systemic inflammatory markers were closely correlated with renal inflammation regardless of the disease course. More importantly, it has been reported that D-ATIN patients might experience recurrent kidney injury during long-term follow-up due to various medications [21]. Elevated systemic inflammatory markers combined with abnormal urinary markers during follow-up may play an important role in reflecting the degree of renal inflammation and providing proper management for these patients.
During follow-up, for patients with similar eGFR values at biopsy, better renal outcomes were achieved in those with higher systemic inflammatory scores, suggesting that the SIS might serve as an indicator of renal outcome. Regarding pathological findings, the SIS was positively correlated with renal interstitial inflammatory cell infiltration, especially with neutrophils and eosinophils, which participate in the acute phase of inflammation [30], and was inversely correlated with interstitial fibrosis, which suggests its ability to reflect the activity of renal interstitial inflammatory injury in D-ATIN. A positive correlation was also observed between the SIS and plasma cell ratio. Plasma cell infiltration was found to be positively correlated with CRP levels and tubulointerstitial inflammation scores in antineutrophil cytoplasmic autoantibody-associated vasculitis [31]. The radical role of plasma cells in D-ATIN remains unclear, but we suppose that aggregated plasma cells in the kidney may play a role in local inflammation in the early phase. In summary, our findings indicate that the SIS may serve as a noninvasive biomarker for ongoing inflammatory processes and active kidney injury in D-ATIN patients, who might benefit from prompt treatment.
Our study has limitations related to the retrospective observational design. Due to the limited sample size of the patients that had both renal biopsy-proven D-ATIN and scheduled follow-up for at least 1 year, we were not able to test the scoring system in a new set of patients. Further study in a larger independent D-ATIN population is needed to validate our findings. CRP and ESR values are nonspecific markers that could be elevated in various conditions, such as infection and systemic autoimmune diseases. Therefore, the introduction of SISs in D-ATIN should be implemented after excluding these conditions.
Conclusions
Our study first demonstrated the relationship between systemic inflammation and local renal inflammation in D-ATIN. The SIS based on ESR and CRP values may serve as a marker of the activity of tubulointerstitial inflammation and assist with decision-making in the immunosuppressive treatment of D-ATIN.
Supplementary Information
Additional file 1: Table S1. Correlation of systemic inflammatory markers with clinicopathological parameters.
Acknowledgments
The results presented in this paper have not been published previously in whole or part, except in abstract form at 3rd Asia Pacific AKI CRRT 2019 Congress. We have obtained the necessary permission from the copyright holder. We thank the patient for devotion.
Abbreviations
- D-ATIN
Drug-induced acute tubulointerstitial nephritis
- CRP
C reactive protein
- ESR
Erythrocyte sedimentation rate
- SIS
Systemic inflammation score
- HPF
High power field
- sCr
Serum creatine
- AKD
Acute kidney disease
- KDIGO
Kidney Disease: Improving Global Outcomes
- ADQI
The Acute Disease Quality Initiative
- RRT
Renal replacement therapy
- eGFR
Estimated glomerular filtration rate
- CKD-EPI
Chronic Kidney Disease Epidemiology Collaboration
- CKD
Chronic kidney disease
- NSAIDs
Non-steroidal anti-inflammatory drugs
- PPIs
Proton pump inhibitors
- UTP
Urinary total protein
- U-KIM1
Urinary kidney injury molecular 1
- U-NAG
Urinary N-acetyl-β-D-glucosaminidase
- U-α1MG
Urinary α1 microglobulin
- U-mAlb
Urinary microalbumin
- U-Osm
Urinary osmolality
- RTA
Renal tubular acidosis
- IgG
Immunoglobulin G
- C3
Complement 3
Authors’ contributions
Research idea and study design: TS, XJZ, GL and LY. Reacher Data acquisition: XZZ, YHG, DMX, JWH and PPS. Histological examination: SXW, JWH, PPS and YJ. Data analysis/interpretation and statistical analysis: XZZ, YHG and DMX. Draft: XZZ. Revise: LY. All authors read and approved the final manuscript.
Funding
This study was supported by grants from the National Natural Science Foundation of China (No. 91742205 and No. 81625004) and the National Science and Technology Major Projects for “Major New Drugs Innovation and Development” of China (No. 2017ZX09304028) and Peking University Clinical Scientist Program (BMU2019LCKXJ002). The funder played a role in the design of the study, follow-up of the patients, interpretation of the data and writing of the manuscript.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics approval and consent to participate
The study was performed in compliance with the Declaration of Helsinki and approved by the Ethics Committee of Peking University First Hospital (approval number 2017[1280]). Written informed consent for obtaining tissue, blood and urine samples was obtained from each participant or their parents or guardian (for participants under 16 years old).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information accompanies this paper at 10.1186/s12882-020-02175-z.
References
- 1.Raghavan R, Eknoyan G. Acute interstitial nephritis - a reappraisal and update. Clin Nephrol. 2014;82(3):149–162. doi: 10.5414/CN10838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Praga M, Sevillano A, Aunon P, et al. Changes in the aetiology, clinical presentation and management of acute interstitial nephritis, an increasingly common cause of acute kidney injury. Nephrol Dial Transplant. 2015;30(9):1472–1479. doi: 10.1093/ndt/gfu326. [DOI] [PubMed] [Google Scholar]
- 3.Clarkson MR, Giblin L, O'Connell FP, et al. Acute interstitial nephritis: clinical features and response to corticosteroid therapy. Nephrol Dial Transplant. 2004;19(11):2778–2783. doi: 10.1093/ndt/gfh485. [DOI] [PubMed] [Google Scholar]
- 4.Michel DM, Kelly CJ. Acute interstitial nephritis. J Am Soc Nephrol. 1998;9(3):506–515. doi: 10.1681/ASN.V93506. [DOI] [PubMed] [Google Scholar]
- 5.Perazella MA, Markowitz GS. Drug-induced acute interstitial nephritis. Nat Rev Nephrol. 2010;6(8):461–470. doi: 10.1038/nrneph.2010.71. [DOI] [PubMed] [Google Scholar]
- 6.Schwarz A, Krause PH, Kunzendorf U, et al. The outcome of acute interstitial nephritis: risk factors for the transition from acute to chronic interstitial nephritis. Clin Nephrol. 2000;54(3):179–190. [PubMed] [Google Scholar]
- 7.Muriithi AK, Leung N, Valeri AM, et al. Biopsy-proven acute interstitial nephritis, 1993-2011: a case series. Am J Kidney Dis. 2014;64(4):558–566. doi: 10.1053/j.ajkd.2014.04.027. [DOI] [PubMed] [Google Scholar]
- 8.Muriithi AK, Leung N, Valeri AM, et al. Clinical characteristics, causes and outcomes of acute interstitial nephritis in the elderly. Kidney Int. 2015;87(2):458–464. doi: 10.1038/ki.2014.294. [DOI] [PubMed] [Google Scholar]
- 9.Perazella MA. Diagnosing drug-induced AIN in the hospitalized patient: a challenge for the clinician. Clin Nephrol. 2014;81(6):381–388. doi: 10.5414/CN108301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Valluri A, Hetherington L, McQuarrie E, et al. Acute tubulointerstitial nephritis in Scotland. QJM. 2015;108(7):527–532. doi: 10.1093/qjmed/hcu236. [DOI] [PubMed] [Google Scholar]
- 11.Krishnan N, Perazella MA. Drug-induced acute interstitial nephritis: pathology, pathogenesis, and treatment. Iran J Kidney Dis. 2015;9(1):3–13. [PubMed] [Google Scholar]
- 12.Ulinski T, Sellier-Leclerc AL, Tudorache E, et al. Acute tubulointerstitial nephritis. Pediatr Nephrol. 2012;27(7):1051–1057. doi: 10.1007/s00467-011-1915-9. [DOI] [PubMed] [Google Scholar]
- 13.Li C, Su T, Chu R, et al. Tubulointerstitial nephritis with uveitis in Chinese adults. Clin J Am Soc Nephrol. 2014;9(1):21–28. doi: 10.2215/CJN.02540313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vila LM, Alarcon GS, McGwin G, Jr, et al. Systemic lupus erythematosus in a multiethnic cohort (LUMINA): XXIX. Elevation of erythrocyte sedimentation rate is associated with disease activity and damage accrual. J Rheumatol. 2005;32(11):2150–2155. [PubMed] [Google Scholar]
- 15.Eudy AM, Vines AI, Dooley MA, et al. Elevated C-reactive protein and self-reported disease activity in systemic lupus erythematosus. Lupus. 2014;23(14):1460–1467. doi: 10.1177/0961203314543915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang M, Ma N, Fu H, et al. Hematocrit level could reflect inflammatory response and disease activity in patients with systemic lupus Erythematosus. Clin Lab. 2015;61(7):801–807. doi: 10.7754/clin.lab.2015.141246. [DOI] [PubMed] [Google Scholar]
- 17.Dima A, Opris D, Jurcut C, et al. Is there still a place for erythrocyte sedimentation rate and C-reactive protein in systemic lupus erythematosus? Lupus. 2016;25(11):1173–1179. doi: 10.1177/0961203316651742. [DOI] [PubMed] [Google Scholar]
- 18.Nielung L, Christensen R, Danneskiold-Samsoe B, et al. Validity and agreement between the 28-joint disease activity score based on C-reactive protein and erythrocyte sedimentation rate in patients with rheumatoid arthritis. Arthritis. 2015;2015:401690. doi: 10.1155/2015/401690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martire MV, Marino Claverie L, Duarte V, et al. Factors associated with sustained remission in patients with rheumatoid arthritis. Reumatol Clin. 2015;11(4):237–241. doi: 10.1016/j.reuma.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 20.Monach PA, Warner RL, Tomasson G, et al. Serum proteins reflecting inflammation, injury and repair as biomarkers of disease activity in ANCA-associated vasculitis. Ann Rheum Dis. 2013;72(8):1342–1350. doi: 10.1136/annrheumdis-2012-201981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Su T, Gu Y, Sun P, et al. Etiology and renal outcomes of acute tubulointerstitial nephritis: a single-center prospective cohort study in China. Nephrol Dial Transplant. 2018;33(7):1180–1188. doi: 10.1093/ndt/gfx247. [DOI] [PubMed] [Google Scholar]
- 22.Wu Y, Yang L, Su T, et al. Pathological significance of a panel of urinary biomarkers in patients with drug-induced tubulointerstitial nephritis. Clin J Am Soc Nephrol. 2010;5(11):1954–1959. doi: 10.2215/CJN.02370310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kidney Disease Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group: KDIGO clinical practice guideline for acute kidney injury. Kidney Int. 2012;2:138. [Google Scholar]
- 24.Chawla LS, Bellomo R, Bihorac A, et al. Acute kidney disease and renal recovery: consensus report of the acute disease quality initiative (ADQI) 16 workgroup. Nat Rev Nephrol. 2017;13(4):241–257. doi: 10.1038/nrneph.2017.2. [DOI] [PubMed] [Google Scholar]
- 25.Solez K, Colvin RB, Racusen LC, et al. Banff 07 classification of renal allograft pathology: updates and future directions. Am J Transplant. 2008;8(4):753–760. doi: 10.1111/j.1600-6143.2008.02159.x. [DOI] [PubMed] [Google Scholar]
- 26.Racusen LC, Solez K, Colvin RB, et al. The Banff 97 working classification of renal allograft pathology. Kidney Int. 1999;55(2):713–723. doi: 10.1046/j.1523-1755.1999.00299.x. [DOI] [PubMed] [Google Scholar]
- 27.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Simpson IJ, Marshall MR, Pilmore H, et al. Proton pump inhibitors and acute interstitial nephritis: report and analysis of 15 cases. Nephrology (Carlton) 2006;11(5):381–385. doi: 10.1111/j.1440-1797.2006.00651.x. [DOI] [PubMed] [Google Scholar]
- 29.Gonzalez E, Gutierrez E, Galeano C, et al. Early steroid treatment improves the recovery of renal function in patients with drug-induced acute interstitial nephritis. Kidney Int. 2008;73(8):940–946. doi: 10.1038/sj.ki.5002776. [DOI] [PubMed] [Google Scholar]
- 30.Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol. 2013;13(3):159–175. doi: 10.1038/nri3399. [DOI] [PubMed] [Google Scholar]
- 31.Masuzawa N, Nishimura A, Mihara Y, et al. Clinicopathological analysis of ANCA-associated glomerulonephritis focusing on plasma cell infiltrate. Clin Exp Nephrol. 2019;23(12):1373–1381. doi: 10.1007/s10157-019-01785-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Correlation of systemic inflammatory markers with clinicopathological parameters.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.


