Abstract
Pre-exposure prophylaxis (PrEP) is an effective biomedical HIV prevention method. PrEP uptake has been persistently low among US women, particularly Black women, who account for 61% of new HIV diagnoses among women. Further understanding of barriers to Black women accessing PrEP is needed. This 2017 cross-sectional survey study explored race-based differences in PrEP interest and intention among women and the indirect association between race and comfort discussing PrEP with a healthcare provider through medical mistrust. The sample consisted of 501 adult women (241 Black; 260 White) who were HIV-negative, PrEP-inexperienced, and heterosexually active. Black women reported greater PrEP interest and intention than White women. However, Black women expressed higher levels of medical mistrust, which, in turn, was associated with lower comfort discussing PrEP with a provider. Medical mistrust may operate as a unique barrier to PrEP access among Black women who are interested in and could benefit from PrEP.
Keywords: Black/African American, Women, Pre-exposure prophylaxis (PrEP), Medical mistrust, HIV/AIDS
INTRODUCTION
Black women are disproportionately affected by HIV, constituting 61% of all US women diagnosed in 2016 [1] despite representing only 13% of women in the US [2]. Improved access to HIV prevention resources is needed to reduce this disparity. Pre-exposure prophylaxis (PrEP) is an effective biomedical HIV prevention method shown to significantly reduce the risk of HIV acquisition [3–5]. PrEP uptake, however, has been slow in general [6] and is especially lagging among women who stand to benefit from its use [7, 8]. For instance, in a national study measuring PrEP uptake among persons in the US, women accounted for only 5% of the estimated number of PrEP users based on fourth quarter 2017 data [9]. In a study projecting PrEP uptake based on retail pharmacy records, PrEP prescription among Black women was significantly lower than among White women [10]. Given the disproportionally high incidence of HIV and low PrEP uptake among Black women, understanding the factors that inhibit or promote Black women’s uptake of PrEP and the degree to which these factors account for racial disparities among women can critically inform interventions to enhance PrEP utilization. In the present cross-sectional survey study, we investigated the role of medical mistrust in the relationship between women’s race (Black vs. White) and comfort discussing PrEP with a healthcare provider, a key precursor to PrEP uptake.
Background
Medical mistrust refers to a lack of confidence in the medical system and in the intentions and work of medical professionals [11]. Medical mistrust is a self-preserving response borne of a long history of race-based differential treatment, unequal dissemination of effective medical innovations, and other racist injustices within the medical establishment [12, 13]. Prior studies that have explored healthcare experiences among different populations have identified a significant association between race and medical mistrust such that Black Americans are significantly more likely than White Americans to mistrust healthcare personnel and the medical system as a whole [14, 15].
Medical mistrust may operate as a key mediating mechanism in the relationship between race and PrEP uptake. Medical mistrust has been found to negatively influence utilization of healthcare services [16–18]. For example, Eaton et al. [19] found that Black men who have sex with men (MSM) who were higher in medical mistrust were less likely to attend routine medical follow-up appointments. Other studies have reported a similar negative association between medical mistrust and medication adherence among African American men and women living with HIV [20, 21].
Regarding utilization of HIV prevention resources, existing research shows an association between medical mistrust and infrequent HIV testing [22–24] and inconsistent condom use [25]. With respect to PrEP use, a study by Brooks et al. found that Black MSM who more strongly held HIV conspiracy beliefs (a form of medical mistrust involving suspicion of government involvement in the origin and treatment of HIV) had lower intentions to initiate PrEP [26]. Other studies, most of which have been qualitative and primarily focused on MSM, have similarly reported that greater medical mistrust is associated with lower levels of PrEP interest or intention [27–29]. These studies collectively offer early indications that medical mistrust may function as a barrier to PrEP utilization among Black MSM. However, little is known about the potential impact medical mistrust may have on PrEP uptake among Black women.
Given reported gender differences in the level of HIV service utilization [30] – which suggest less optimal HIV service use among women than among men – and observed gender disparities in level of trust in the healthcare system [31, 32], the relevance of medical mistrust to PrEP attitudes and uptake among Black women cannot be inferred based on research with Black men. Rather, the potential impact of medical mistrust among Black women needs to be studied directly within this population. Early qualitative research with Black women has suggested that mistrust in the government as well as the pharmaceutical industry may operate as barriers for PrEP uptake [7, 33], but more research is needed to understand the specific implications that medical mistrust can have for Black women’s interactions with the healthcare system in the process of obtaining PrEP. Because PrEP is a prescription-based medication, communicating with a healthcare provider about PrEP is a necessary step to accessing the medication. Given that many providers are not consistently broaching the topic with women [34], requiring women who are seeking PrEP to initiate the conversation, the issue of women’s comfort discussing PrEP with a provider is especially salient.
Study Overview
The aim of the current study was to investigate the indirect association between race and women’s comfort discussing PrEP with a provider through medical mistrust. We focused our work on women because PrEP uptake has been generally low among women [8, 9], and particularly low for Black women [10] despite their disproportionately large risk for HIV [1]. Understanding why Black woman may be less likely than White women to receive prescriptions for PrEP may help explain, and ultimately address, the stark disparities in HIV infection and PrEP uptake between the two groups [1, 10]. In the present research, we hypothesized that Black women would exhibit greater levels of medical mistrust than White women, and this greater mistrust would, in turn, be associated with less comfort discussing PrEP with a provider. Thus, we tested the indirect path from women’s race to comfort discussing PrEP through medical mistrust.
We also considered, in an exploratory post-hoc analysis, two factors recognized to be necessary precursors to individuals seeking a prescription for PrEP from a provider within existing theoretical models of PrEP uptake, including PrEP cascade models [35, 36] and the Information-Motivation-Behavioral Skills (IMB) model [37]. These factors included interest in learning about PrEP and intention to use PrEP, and we explored whether there were racial differences in women’s interest and intention and how these factors may relate to Black and White women’s comfort discussing PrEP with a provider. Previous research has found that, perhaps due to greater HIV burden among this population, Black women express strong interest in learning about PrEP [7] and sometimes report greater intention than White women to use PrEP [38, 39].
METHODS
Procedure
Data for the present study were obtained via a 2017 cross-sectional online survey of 973 clients from Planned Parenthood reproductive health centers in the three cities with the highest rates of HIV infection in Connecticut: Bridgeport (HIV prevalence of 924 per 100,000), New Haven (1,118 per 100,000), and Hartford (1,494 per 100,000) [40]. In 2017, approximately 26 health centers in Connecticut and 13 in Bridgeport, New Haven, and Hartford specifically were listed as PrEP providers with the Connecticut Department of Public Health [41]. State-sponsored public health campaigns promoting PrEP awareness, including advertisements featuring heterosexual women, had previously targeted these three cities. The survey was administered about eight months after PrEP had been available at the three Planned Parenthood centers from which present data were collected.
Clientele who attended a Planned Parenthood appointment in the past 10 months, were over the age of 18, and had been enrolled in the online patient portal system were emailed a link directing them to an online survey that took approximately 35 minutes to complete. In the survey, which was administered in English, participants were given background information regarding daily oral PrEP (emtricitabine/tenofovir disoproxil fumarate - Truvada®) including: purpose of the medication, administration method (daily oral dosing), potential side effects, efficacy, and approval by the US Food and Drug Administration (FDA). We refer readers to Appendix 1, which contains the background information provided regarding PrEP and PrEP-related measures. Following survey completion, participants were compensated with a $10 gift card and provided with additional information regarding PrEP and other HIV prevention and health promotion resources. All study procedures were approved by the Yale University Institutional Review Board.
MEASURES
Medical mistrust.
In this study, medical mistrust was measured using the Group-Based Medical Mistrust Scale (GBMMS), which assesses previous experiences of racial discrimination as well as feelings of discomfort and suspicion that one has toward healthcare personnel and pharmacological treatment [42]. The GBMMS is a 12-item questionnaire that uses a 5-point Likert-type scale for the response key, ranging from (1) Strongly disagree to (5) Strongly agree. In the original study that assessed the psychometric properties of the GBMMS among 186 African American and Latina urban women, Thomas et al. [42] reported a Cronbach’s alpha of 0.83. In the current study, α = 0.88 for the full sample (α = 0.87 among Black women, α = 0.86 among White women).
Similar to others studies [43, 44], wording from this scale was adapted to fit the characteristic of interest for our sample population. Specifically, the scale was modified to state “people of my race” rather than “people of my ethnic group” due to our focus on race-based medical mistrust and the potential heterogeneity in ethnic group identification within our Black and White comparison groups. In the present study, Latina/Hispanic women were grouped according to the racial group with which they identified (e.g. Black/African American, White).
Interest in learning more about PrEP.
Interest in learning more about PrEP was assessed using a single-item measure, which asked participants to rate their level of interest in learning more about PrEP on a 5-point scale ranging from (1) Not at all interested to (5) Extremely interested.
Intention to use PrEP.
Intention to use PrEP was assessed using a single-item measure, which asked participants to rate their likelihood of taking PrEP if it were available for free on a 5-point scale ranging from (1) Definitely would not take PrEP to (5) Definitely would take PrEP. This measure was previously used in a study exploring factors predicting PrEP intention among MSM [45].
Comfort discussing PrEP with a provider.
Comfort discussing PrEP with a healthcare provider was measured using a single-item measure, which asked participants to rate their level of comfort talking with a healthcare provider about PrEP. Participants were asked to rate this item on a 5-point scale ranging from (1) Not at all comfortable to (5) Extremely comfortable.
Gender.
Participant’s gender was collected using a single multiple-choice item, which asked participants to select the gender that best describes them: (1) Woman, (2) Man, (3) Transgender woman, (4) Transgender man, (5) Gender queer, (6) Other, or (7) I prefer not to say.
Race.
Race was measured in the present study as the subjective identification of one’s racial identity [46]. Participants’ self-identified race was collected using a single multiple-choice item, which asked participants to select the race that best describes them: (1) American Indian or Alaska Native, (2) Asian, (3) Black or African American, (4) Native Hawaiian/ Other Pacific Islander, (5) White, or (6) Other race. This item was asked separately from the item assessing ethnicity (Latina/Hispanic vs. non-Latina/Hispanic).
Other background characteristics.
In addition to gender and race, participants also reported their age (years); ethnicity (Latina/Hispanic or non-Latina/Hispanic); sexual orientation (Heterosexual, Bisexual, Gay/Lesbian, Queer, Asexual, or Other); marital status (Married, Widowed, Divorced, Separated, or Never married); education level (No diploma, High school diploma or the equivalent, Some college but no degree, Bachelor’s degree, Master’s degree, or Professional or doctoral degree); annual income (amount); employment status (Employed full/part-time, Unemployed, or Other); insurance status (Insured, Uninsured, or Unknown); type of insurance if applicable (Private, Medicaid, Online Marketplace/Obamacare, and/or Other), prior PrEP knowledge (Ever having heard of PrEP or Never/Unknown); condom use consistency (Always, Mostly, Sometimes, Rarely, or Never); number of male sex partners (past 6 months); HIV testing (lifetime and past 12 months); and perceived HIV risk (Not at all, A Little Bit, Somewhat, Very, or Extremely likely to get HIV in lifetime).
Analysis
All analyses were conducted using IBM SPSS Statistics Version 24. For the purpose of this study, analyses were restricted only to respondents who self-reported being a woman, Black or White, HIV-negative, PrEP-inexperienced, and heterosexually active (i.e., anal or vaginal sex with a man) in the past six months. Frequencies and means were calculated to describe the sample and measures of interest. Pearson’s product-moment correlations were run to assess bivariate relationships between main measures separately for Black and White women and within the combined sample. Chi-square tests of independence and independent samples t-tests were employed to identify group-level differences in background characteristics, medical mistrust, and PrEP-related outcomes between Black women and White women.
To analyze the indirect relationship between race and comfort discussing PrEP with a provider via medical mistrust, Hayes’ PROCESS macro for SPSS, which employs bootstrapping, was used [47]. Bootstrapping is an analytic technique that utilizes random resampling to analyze direct and indirect relationships in structural models [48]. Compared to other analytic tests of indirect effects, it has the highest power and offers the greatest reduction in the Type I error that is associated with conducting multiple statistical tests. Moreover, this technique does not require a significant bivariate X-Y relationship to establish mediation [49, 50]. We used bias-corrected confidence intervals and generated 10,000 bootstrapped samples (resampling from the original sample data) to test our hypothesized indirect effect. The model was adjusted for background characteristics, including those that were empirically significant (p < .05) and/or theoretically relevant. These characteristics were age, ethnicity, insurance status, marital status, prior PrEP knowledge, annual income, employment status, level of education, and perceived HIV risk.
RESULTS
Sample Characteristics
The survey link was emailed to 11,238 Planned Parenthood patients; a total of 973 participants took the online survey before it was closed to new enrollment. The survey was closed after 973 had enrolled (achieved within the first 100 hours of survey distribution) to avoid exceeding the enrollment maximum of n = 1,000. Of the 973 participants enrolled, 501 met criteria for the present study in accordance with aforementioned inclusion criteria. The subsample consisted of 260 (52%) White and 241 (48%) Black/African American women. Women ranged in age from 18 to 65 years (M = 28.63; SD = 7.45). Ninety-three percent had some form of health insurance: In response to a question asking insured respondents to select all forms of insurance that applied, 44% indicated that they had Medicaid; 42% had private insurance through their school, employer, partner, or family; 15% had insurance through the online marketplace/Patient Protection and Affordable Care Act (i.e. Obamacare); and less than 1% had another form of insurance. Before initiating the survey, 24% had heard of PrEP. Sixty-five percent reported some level of interest in learning more about PrEP (“A little bit” to “Extremely” interested), 58% would consider initiating PrEP if it were available for free (“Might” to “Definitely” would take PrEP), and 42% reported some level of discomfort in speaking with healthcare providers about PrEP (“Not at all” to “Somewhat” comfortable).
Between-Group Race Comparisons
Table I presents sample characteristics for Black women, White women, and the combined sample as well as results of between-group comparisons. We found no statistically significant racial differences in age, sexual orientation, and health insurance status. Group-level differences were, however, observed in ethnicity, marital status, employment status, annual income, and level of education; Black women reported a higher rate of employment, lower annual income, and lower education level. They were less likely to be married compared to White women. There was no significant difference in perceived HIV risk, number of male sexual partners in the past six months, or condom use consistency between the two racial groups. Black women were more likely to have been tested for HIV in the past year and in their lifetime but less likely to have prior PrEP knowledge compared to White women.
Table I.
Sample background characteristics by racial group
| Characteristic | White | Black | Total |
|---|---|---|---|
| (n = 260) | (n = 241) | (n = 501) | |
| n (%) or M [SD] | n (%) or M [SD] | n (%) or M [SD] | |
| Ethnicity | |||
| Hispanic** | 58 (22.3) | 17 (7.1) | 75 (15.0) |
| Age- M [SD] | 29.14 [7.0] | 28.08 [7.9] | 28.63 [7.5] |
| 18–25 | 85 (32.7) | 109 (45.2) | 194 (38.7) |
| 26–35 | 140 (53.8) | 95 (39.4) | 235 (46.9) |
| 36–45 | 28 (10.8) | 29 (12.0) | 57 (11.4) |
| >45 | 7 (2.7) | 8 (3.3) | 15 (3.0) |
| Married** | 45 (17.3) | 23 (9.5) | 68 (13.6) |
| Annual Income** | |||
| <10,000 | 55 (21.2) | 67 (27.8) | 122 (24.4) |
| 11,000–30,000 | 73 (28.1) | 91 (37.8) | 164 (32.7) |
| 31,000–50,000 | 58 (22.3) | 59 (24.5) | 117 (23.4) |
| 51,000–70,000 | 33 (12.7) | 20 (8.3) | 53 (10.6) |
| >70,000 | 41 (15.8) | 4 (1.7) | 45 (9.0) |
| Insured (private, Medicaid, online marketplace, or other) | 239 (91.9) | 226 (93.8) | 465 (92.8) |
| Employment** | |||
| Employed | 164 (63.1) | 180 (74.7) | 344 (68.7) |
| Unemployed | 34 (13.1) | 26 (10.8) | 60 (12.0) |
| Other | 62 (23.8) | 35 (14.5) | 97 (19.4) |
| Education Level** | |||
| Less than bachelor’s | 156 (60.0) | 206 (85.5) | 362 (72.3) |
| Bachelor’s or higher | 104 (40.0) | 35 (14.5) | 139 (27.7) |
| Sexual Orientation | |||
| Heterosexual | 200 (76.9) | 191 (79.3) | 391 (78.0) |
| Bisexual | 37 (14.2) | 34 (14.1) | 71 (14.2) |
| Gay/Lesbian | 3 (1.2) | 2 (0.8) | 5 (1.0) |
| Other | 20 (7.7) | 14 (5.8) | 34 (6.8) |
| HIV tested in lifetime** | 200 (76.9) | 215 (89.2) | 415 (82.8) |
| Recent HIV test ** | |||
| Within 12 mos.a | 131 (65.5) | 175 (81.4) | 306 (73.3) |
| Number of sex partnersb | |||
| One | 194 (75.8) | 161 (67.4) | 355 (71.1) |
| Two | 29 (11.3) | 39 (16.3) | 68 (12.7) |
| Three or more | 33 (12.9) | 39 (16.3) | 72 (14.5) |
| Perceived HIV risk | 57 (21.9) | 49 (20.3) | 106 (21.2) |
| Prior PrEP knowledge* | 73 (28.1) | 48 (19.9) | 121 (24.2) |
| Condom usec | |||
| Always | 20 (7.8) | 27 (11.3) | 47 (9.5) |
| Sometimesd | 108 (42.2) | 116 (48.7) | 224 (45.3) |
| Never | 128 (50.0) | 95 (39.9) | 223 (45.1) |
Note. Asterisks denote significant differences between Black and White women in our sample.
p < .05
p < .01
For this variable White n = 200, Black n = 215
This variable assessed number of male sexual partners in the past six months; White n=256 Black n = 239
White n = 256 Black n = 238
Represents combination of “Rarely,” “Sometimes,” and “Never” responses
As indicated in Table II, compared to White women, Black women reported significantly higher medical mistrust. Black women reported greater interest in learning more about PrEP and greater intention to use PrEP if it were available for free. No significant racial difference was observed in comfort discussing PrEP with a healthcare provider.
Table II.
Mean differences of main measures in separate racial groups and combined sample
| White | Black | Total | ||||
|---|---|---|---|---|---|---|
| Variables | n | M [SD] | n | M [SD] | n | M [SD] |
| Medical mistrust** | 252 | 2.04 [0.65] | 218 | 2.50 [0.69] | 470 | 2.25 [0.71] |
| Interest in learning more about PrEP** | 260 | 2.05 [1.11] | 240 | 2.45 [1.24] | 500 | 2.24 [1.19] |
| Intention to use PrEP* | 260 | 2.72 [1.31] | 241 | 2.96 [1.38] | 501 | 2.83 [1.35] |
| Comfort discussing PrEP with a provider | 260 | 3.57 [1.18] | 241 | 3.51 [1.21] | 501 | 3.54 [1.19] |
p < .05
p < .01
Correlation Analyses
Table III presents correlation coefficients for bivariate relationships among race, medical mistrust, interest in learning more about PrEP, intention to use PrEP, and comfort discussing PrEP with a provider for the full sample (Table IIIa) and for Black and White women separately (Table IIIb). For both stratified and combined samples, medical mistrust was not associated with PrEP interest or PrEP intention but was negatively correlated with comfort discussing PrEP with a healthcare provider. Interest in learning more about PrEP, intention to use PrEP, and comfort discussing PrEP with a provider were all positively correlated.
Table IIIa.
Bivariate correlations among main measures for full sample
| Variables | Race | Medical mistrust | PrEP interest | PrEP intention | Comfort discussing PrEP with a provider |
|---|---|---|---|---|---|
| Race | - | .321** | .170** | .089* | −.023 |
| Medical mistrust | - | .046 | −.004 | −.166** | |
| PrEP interest | - | .487** | .262** | ||
| PrEP intention | - | .165** | |||
| Comfort discussing PrEP with a provider | - |
p < .05
p < .01
Table IIIb.
Bivariate correlations among main measures stratified by patient race
| Variables | Medical mistrust | PrEP interest | PrEP intention | Comfort discussing PrEP with a provider |
|---|---|---|---|---|
| Medical mistrust | - | −.020 | −.058 | −.158* |
| PrEP interest | .001 | - | .518** | .281** |
| PrEP intention | .010 | .439** | - | .197** |
| Comfort discussing PrEP with a provider | .181** | .257** | .139* | - |
Note. Intercorrelations for Black women are presented above the diagonal separation and those for White women are presented below.
p < .05
p < .01
Bootstrapping Analysis of Indirect Effects
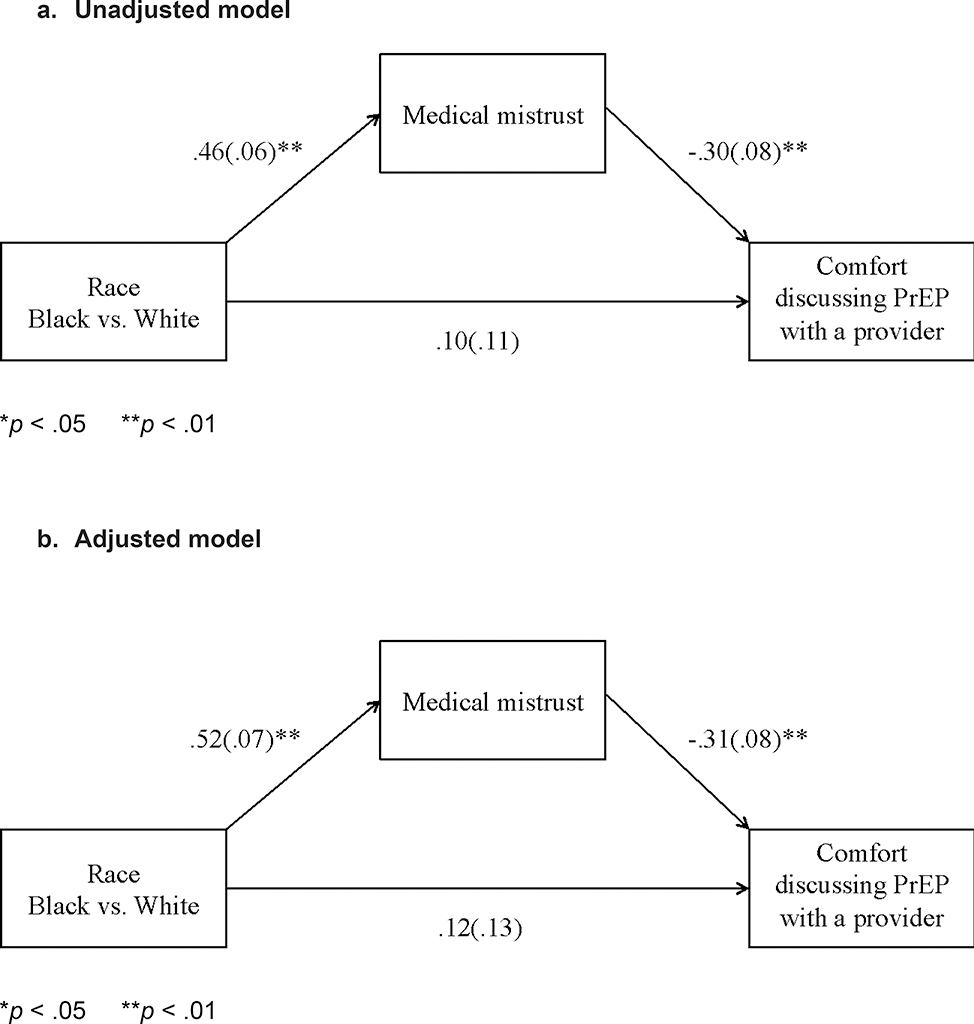
We found a significant indirect relationship between race and comfort discussing PrEP with a healthcare provider (Figure I; unadjusted model: −0.137, SE = .037, 95% CI [−0.233, −0.061]; adjusted model: −0.163, SE = .051, 95% CI [−0.273, −0.072]. Consistent with our hypothesis, Black women had a greater level of medical mistrust, which, in turn, was associated with lower comfort discussing PrEP with a provider.
Figure 1.
Models of the indirect effect of race on comfort discussing PrEP with a provider through medical mistrust; a unadjusted and b adjusted for age, ethnicity, insurance status, marital status, prior PrEP knowledge, annual income, employment status, level of education, and perceived lifetime risk of HIV. In both unadjusted and adjusted models, there was a significant indirect relationship between race and comfort discussing PrEP with a healthcare provider; unadjusted model: − 0.137, SE = 0.037, 95% CI [− 0.233, − 0.061]; adjusted model: − 0.163, SE = 0.051, 95% CI [− 0.273, − 0.072]
We also conducted an exploratory analysis of a multiple-mediator model that added interest in learning more about PrEP and intention to use PrEP as parallel mediators to our original single-mediator model. Thus, the model included three parallel mediational pathways between race and comfort discussing PrEP with a provider through interest in learning more about PrEP, intention to use PrEP, and medical mistrust. The negative indirect association through medical mistrust remained significant (unadjusted model: −0.133, SE = 0.042, 95% CI [−0.224, −0.060]; adjusted model: −0.139, SE = 0.044, 95% CI [−0.236, −0.063]). There was also a positive indirect association through interest in learning more about PrEP (unadjusted model: 0.100, SE = 0.033, 95% CI [.046, 0.178]; adjusted model: 0.081, SE = 0.033, 95% CI [0.025, 0.158]). Black women had greater interest in learning more about PrEP, which, in turn, was associated with greater comfort discussing PrEP with a healthcare provider. The indirect path for intention to use PrEP was not significant.
DISCUSSION
In the current study, we examined the implications of race and medical mistrust for comfort discussing PrEP with a provider and explored racial differences in PrEP interest and intended uptake among Black and White women. We found that Black women had significantly more medical mistrust than White women, which, in turn, was associated with lower comfort discussing PrEP with a healthcare provider. Nonetheless, Black women expressed higher interest in learning about PrEP and greater intention to use PrEP, and our exploratory post-hoc analysis suggested that the former could help to offset the detrimental impact of medical mistrust on patient-provider communication among this group. Thus, our finding that Black and White women did not differ overall in their expressed comfort discussing PrEP with a provider occurred, in part, because of underlying racial differences among women that were related to expressed comfort but in opposite directions.
In our sample, only 24% of women had prior knowledge of PrEP and there was a clear racial disparity in awareness, with Black women significantly less likely than White women to have prior PrEP knowledge. However, after being provided information about PrEP, Black women had significantly more interest in learning about PrEP and greater likelihood of initiating the medication if it were available for free. These findings are consistent with other studies, which found greater PrEP acceptability among Black women compared to other racial groups [7, 38, 39]. Despite high interest, however, existing research shows that PrEP uptake among Black women has been disproportionately low [10], suggesting that PrEP awareness and interest, although important, are insufficient for PrEP initiation. Kelly et al.’s [35] multi-step theoretical model of the PrEP care continuum identifies potential facilitators and barriers to PrEP use at multiple points between medication awareness and medication adherence. The model suggests that although awareness is a necessary step toward uptake, additional steps involving interaction with the healthcare system are also needed. These steps require the patient to be willing to see a medical provider and to discuss risk behavior in the process of establishing their PrEP eligibility. The indirect association identified in the present study suggests that these requirements could function as barriers to PrEP access that are particularly salient for Black women, contributing to the observed disparities in uptake of this potentially life-changing preventive medication.
Implications for Intervention
It is valuable to understand the dynamics underlying racial differences in PrEP uptake in order to develop effective interventions that facilitate access to PrEP among Black women. Previous work has demonstrated, consistent with the proposed dynamic in the IMB model of health behavior change in general [51] and as applied to PrEP uptake in particular [37, 52], that acquisition of appropriate behavioral skills is a key mechanism through which knowledge of a health issue and motivation to address the issue leads to adoption of a preventive behavior. Increasing Black women’s comfort discussing PrEP with providers may be a critical issue to consider when developing interventions aimed at increasing PrEP uptake among this key population.
Our findings suggest multiple points of intervention that could help to improve comfort communicating with a provider about PrEP, including addressing medical mistrust and stimulating interest in learning more about PrEP. Given the negative impact of medical mistrust on comfort discussing PrEP with healthcare providers and general utilization of healthcare services [16–18], collective efforts are needed at an individual and structural level to build greater trust in the healthcare system among racial minority women. For instance, in healthcare settings, educating providers on the principles of shared decision-making and providing communication skills training that helps to cultivate a trusting patient-provider relationship may serve as one potentially fruitful avenue for increasing utilization of PrEP among women who stand to benefit from the protection it affords. Furthermore, medical mistrust may be reduced through greater cultural competency training among providers and having more racially diverse healthcare providers who reflect the communities they serve [12, 53]. Reductions in medical mistrust would encourage patient-provider dialogue around PrEP, sexual behavior, and other potentially sensitive health topics.
This study further supports the recommendation for PrEP to be included in routine discussions with patients about preventative health [54]. Routinization of PrEP education can help to raise generalized awareness about PrEP and increase its acceptability in society; consequently, women with high levels of medical mistrust who avoid utilization of most healthcare services may be more likely to hear about PrEP and willing to consider it as a prevention option for themselves [54]. Public awareness campaigns can also help to this end by spreading awareness and normalizing PrEP use. Promoting interest in learning about PrEP by making more aggressive efforts to increase PrEP awareness among Black women may offset any deterring effect of medical mistrust and motivate Black women to broach the topic of PrEP with a healthcare provider as was reflected in our post-hoc analyses.
While acknowledging the findings of the present study, it is also important to keep in mind the multifaceted nature of health inequalities and the interplay of multiple factors that function at various ecological levels and contribute to higher HIV rates and disproportionately lower PrEP uptake among Black women [55]. Individual-level factors may include socioeconomic conditions, insurance status, health literacy, and attitudes regarding preventative healthcare [12]. HIV and PrEP stigma, sexual networking, and norms around negotiating power in sexual relationships can contribute to disparities at the interpersonal level [56–58]. Within the healthcare system, provider explicit and/or implicit (conscious and unconscious) biases, stereotyping, and prejudice can function as contributing factors [12, 59, 60]. At the structural level, residential segregation, poverty, availability of healthcare resources, and fragmentation of care are important factors that may contribute to disproportionately higher HIV incidence among Black women and likely contribute to PrEP disparities [12, 61]. Aforementioned variables, in addition to medical mistrust, must be considered to fully understand and effectively address socio-structural barriers that contribute to general inequitable health and specifically to disparity in PrEP access among Black women.
Limitations and Future Research
This study was subject to limitations, which one should be mindful of when interpreting results. The main purpose of the present study was to assess the impact that race-based medical mistrust can have on comfort discussing PrEP with a provider among Black and White women; thus, our analysis focused on race and adjusted for ethnicity. Further investigation is warranted to determine whether the observed associations generalize to ethnic minorities and other social groups experiencing medical mistrust. Future research might also consider more directly how factors that could potentially relate both with medical mistrust and with discomfort discussing treatment with providers, such as socioeconomic status (SES) [62] and health literacy [63], interact with race to influence comfort discussing PrEP with providers.
It is important to note that our study sample was recruited using a Planned Parenthood listserv and, thus, included only women who were already engaged in care and therefore likely to have lower medical mistrust than the general population. Additionally, it is possible that among the Planned Parenthood patients invited to participate in the survey, those with greater levels of medical mistrust were less likely to do so, yielding a study sample that may be particularly low in medical mistrust relative to US women more broadly. Furthermore, it is important to keep in mind that the observed racial difference in medical mistrust, although statistically significant, was relatively small (Table II). This finding may suggest that medical mistrust, although more salient, is not isolated to the Black/African American community. It is also possible that racial disparities in mistrust are more dramatic among individuals not engaged in care.
There are also limitations inherent in the study measures and design used to assess PrEP knowledge and attitudes. In the absence of pre-validated scales, several key constructs (e.g., PrEP interest and comfort discussing PrEP with a provider) were measured with single items constructed for the purpose of the present survey. We did not assess the extent or accuracy of participants’ prior PrEP knowledge; rather, participants were asked if they had ever “heard of” PrEP. Similarly, the measure used to assess participants’ comfort discussing PrEP with a provider was a single item that did not consider contextual details (e.g., type of provider, type of healthcare setting); thus, responses likely varied depending on participants’ supposition of such contextual information. Use of multi-item scales and qualitative methods in future research could offer a more nuanced understanding of the results presented here.
It is also worth noting that prior to responding to items assessing PrEP interest, intention, and comfort discussing PrEP with a provider, participants were presented with background information regarding PrEP (see Appendix 1). It is possible that the background information influenced participants’ subsequent responses. However, all participants received the same information; thus, we have no reason to believe that it would have differentially influenced the two racial groups.
Participant responses on the measure assessing intention to use PrEP [45] may not reflect subsequent medication uptake. Longitudinal methods should be employed in future research to examine the predictive value this measure offers and to directly examine medical mistrust as a predictor of PrEP uptake. Moreover, the present study is cross-sectional and therefore we cannot assume directionality, which precludes inferences about causation.
We also note that although we did observe a significant indirect effect between women’s race and comfort discussing PrEP through medical mistrust, the direct effect between race and comfort discussing PrEP was not significant. Although one reason may be that tests of indirect effects have more statistical power, and thus are more sensitive than are direct effects [64], our exploratory analyses suggest that another plausible explanation is the presence of another variable – interest in learning more about PrEP – is limiting the direct effect (i.e. a “suppressor variable”). Our findings suggest the importance of considering, in a more complex and comprehensive way, the multiple factors that can simultaneously affect women’s responses to PrEP as a function of race.
CONCLUSIONS
PrEP is a prescription medication, which means that one has to discuss PrEP with a medical professional in order to gain access. In this study of care-engaged women, knowledge of PrEP was low, particularly among Black women. However, once participants were educated about PrEP, the majority expressed some openness to learning more and potentially using PrEP, and interest and intention were relatively high among Black women. Medical mistrust, which was more prevalent among Black women, was associated with lower comfort discussing PrEP with a provider, suggesting medical mistrust could limit access to this medication among one of the groups who stand to benefit the most. We believe optimal and equitable dissemination of PrEP hinges upon improved efforts to increase PrEP awareness and build trust in the healthcare system among Black women and other priority populations.
Supplementary Material
Acknowledgment/Funding:
The authors are grateful to all individuals who participated in the present study. This study was funded by Yale Center for Interdisciplinary Research on AIDS (CIRA), which is funded by the National Institute of Mental Health under award number P30-MH062294. The efforts of S. K. Calabrese were supported by the NIMH via Award Number K01-MH103080. T. Taggart was supported by the NIMH via Award Number T32-MH02003 and the National Institute on Drug Abuse (NIDA) via the HIV/AIDS, Substance Abuse, and Trauma Training Program at the University of California, Los Angeles (R25-DA035692). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health, the National Institutes of Health, or Planned Parenthood Federation of America, Inc.
Footnotes
Compliance with Ethical Standards
Conflicts of Interest: S. K. Calabrese has received compensation for her efforts in developing and delivering PrEP education materials. S. Hull receives honoraria for serving on PrEP for Women Steering Committee for Gilead and subcontracts on a Gilead funded research study. The authors do not have other conflicts of interest to disclose.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individuals included in the study.
References
- 1.US Centers for Disease Control and Prevention. HIV/AIDS. 2018. Available from: https://www.cdc.gov/hiv/group/gender/women/ [Google Scholar]
- 2.US Census Bureau. Projections of the population by sex, hispanic origin, and race for the United States: 2015 to 2060. 2014.
- 3.Fonner VA, Dalglish SL, Kennedy CE, et al. Effectiveness and safety of oral HIV preexposure prophylaxis for all populations. AIDS. 2016;30(12):1973–1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riddell J, Amico KR, Mayer KH. HIV preexposure prophylaxis: a review. JAMA. 2018;319(12):1261–8. [DOI] [PubMed] [Google Scholar]
- 5.Hanscom B, Janes HE, Guarino PD, Huang Y, Brown ER, Chen YQ, et al. Preventing HIV-1 infection in women using oral pre-exposure prophylaxis: a meta-analysis of current evidence. J Acquir Immune Defic Syndr. 2016;73(5):606–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mayer KH, Krakower DS. Editorial commentary: scaling up antiretroviral preexposure prophylaxis: moving from trials to implementation. Clin Infect Dis. 2015;61(10):1598–1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Auerbach JD, Kinsky S, Brown G, Charles V. Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDS. 2015;29(2):102–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mera Giler R, Magnuson D, Trevor H, Bush S, Rawlings K, McCallister S. Changes in Truvada (TVD) for HIV pre-exposure prophylaxis (PrEP) utilization in the United States: (2012–2016). 9th International AIDS Society Conference on HIV Science; Paris, France 2017. [Google Scholar]
- 9.Siegler AJ, Mouhanna F, Mera Giler R, et al. The prevalence of PrEP use and the PrEP-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol. 2018; Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bush S, Magnuson D, Rawlings MK, Hawkins T, McCallister S, Mera Giler R. Racial characteristics of FTC / TDF for pre-exposure prophylaxis ( PrEP ) users in the US. ASM Microbe; Boston, MA: 2016. [Google Scholar]
- 11.Ball K, Lawson W, Alim T. Medical mistrust, conspiracy beliefs & HIV-related behavior among African Americans. J Psychol Behav Sci. 2013;1(1):1–7. [Google Scholar]
- 12.Institute of Medicine. (2002). Unequal treatment: confronting racial and ethnic disparities in health care. Smedley BD, Stith A, Nelson AR (Eds.). Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- 13.Washington HA. Medical apartheid: The dark history of medical experimentation on Black Americans from colonial times to the present. Paw Prints. 2010. [Google Scholar]
- 14.Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med. 2000;9(10):1156–63. [DOI] [PubMed] [Google Scholar]
- 15.Halbert CH, Armstrong K, Gandy OH, Shaker L. Racial differences in trust in health care providers. Arch Intern Med. 2006;166(8):896–901. [DOI] [PubMed] [Google Scholar]
- 16.Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care. Soc Sci Med. 2008;67(3):478–86. [DOI] [PubMed] [Google Scholar]
- 17.Laveist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. 2009;44(6):2093–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whetten K, Leserman J, Whetten R, Ostermann J, Thielman N, Swartz M. Exploring lack of trust in care providers and the government as a barrier to health service use. Am J Public Health. 2006;96(4):716–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eaton LA, Driffin DD, Kegler C, Smith H, Conway-Washington C, White D, et al. The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. Am J Public Health. 2015;105(2):e75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dale SK, Bogart LM, Wagner GJ, Galvan FH, Klein DJ. Medical mistrust is related to lower longitudinal medication adherence among African-American males with HIV. J Health Psychol. 2016;21(7):1311–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kalichman SC, Eaton L, Kalichman MO, Cherry C. Medication beliefs mediate the association between medical mistrust and antiretroviral adherence among African Americans living with HIV/AIDS. J Health Psychol. 2017;22(3):269–279. [DOI] [PubMed] [Google Scholar]
- 22.Ford CL, Wallace SP, Newman PA, Lee SJ, Cunningham WE. Belief in AIDS-related conspiracy theories and mistrust in the government: relationship with HIV testing among at-risk older adults. Gerontologist. 2013;53(6):973–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoyt MA, Rubin LR, Nemeroff CJ, Lee J, Huebner DM, Proeschold-Bell RJ. HIV/AIDS-related institutional mistrust among multiethnic men who have sex with men: effects on HIV testing and risk behaviors. Health Psychol. 2012;31(3):269–77. [DOI] [PubMed] [Google Scholar]
- 24.Malebranche DJ, Peterson JL, Fullilove RE, Stackhouse RW. Race and sexual identity: perceptions about medical culture and healthcare among black men who have sex with men. J Natl Med Assoc. 2004;96(1):97–107. [PMC free article] [PubMed] [Google Scholar]
- 25.Bogart LM, Thorburn S. Are HIV/AIDS conspiracy beliefs a barrier to HIV prevention among African Americans? J Acquir Immune Defic Syndr. 2005;38(2):213–8. [DOI] [PubMed] [Google Scholar]
- 26.Brooks RA, Allen VC, Regan R, Mutchler MG, Cervantes-Tadeo R, Lee S-J. HIV/AIDS conspiracy beliefs and intention to adopt preexposure prophylaxis among black men who have sex with men in Los Angeles. Int J STD AIDS. 2018;29(4):375–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eaton LA, Driffin DD, Smith H, Conway-Washington C, White D, Cherry C. Psychosocial factors related to willingness to use pre-exposure prophylaxis for HIV prevention among Black men who have sex with men attending a community event. Sexual Health. 2014;11(3):244–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eaton LA, Kalichman SC, Price D, Finneran S, Allen A, Maksut J. Stigma and conspiracy beliefs related to pre-exposure prophylaxis (PrEP) and interest in using PrEP among Black and White men and transgender women who have sex with men. AIDS Behav. 2017;21(5):1236–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cahill S, Taylor SW, Elsesser SA, Mena L, Hickson D, Mayer KH. Stigma, medical mistrust, and perceived racism may affect PrEP awareness and uptake in black compared to white gay and bisexual men in Jackson, Mississippi and Boston, Massachusetts. AIDS Care. 2017;29(11):1351–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sohler NL, Li X, Cunningham CO. Gender disparities in HIV health care utilization among the severely disadvantaged : can we determine the reasons? AIDS Patient Care STDS. 2009;23(9):775–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Altice FL, Mostashari F, Friedland GH. Trust and the acceptance of and adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;28(1):47–58. [DOI] [PubMed] [Google Scholar]
- 32.Hammond WP, Matthews D, Mohottige D, Agyemang A, Corbie-Smith G. Masculinity, medical mistrust, and preventive health services delays among community-dwelling African-American men. J Gen Intern Med. 2010;25(12):1300–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hill BS, Patel VV, Haughton LJ, Blackstock OJ. Leveraging social media to explore Black women’s perspectives on HIV pre-exposure prophylaxis. J Assoc Nurses AIDS Care. 2018;29(1):107–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adams LM, Balderson BH, Brown K, Bush SE, Packett BJ. Who starts the conversation and who receives preexposure prophylaxis (PrEP)?: A brief online survey of medical providers’ PrEP practices. Health Educ Behav. 2018. (Advance Online Publication). [DOI] [PubMed] [Google Scholar]
- 35.Kelley CF, Kahle E, Siegler A, et al. Applying a PrEP continuum of care for men who have sex with men in Atlanta, Georgia. Clin Infect Dis. 2015;61(10):1590–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Parsons JT, Rendina HJ, Lassiter JM, Whitfield THF, Starks TJ, Grov C. Uptake of HIV pre-exposure prophylaxis (PrEP) in a national cohort of gay and bisexual men in the United States. J Acquir Immune Defic Syndr. 2017;74(3):285–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dubov A, Altice FL, Fraenkel L. An information-motivation-behavioral skills model of PrEP uptake. AIDS and Behav. 2018. (Advance Online Publication). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garfinkel DB, Alexander KA, McDonald-Mosley R, Willie TC, Decker MR. Predictors of HIV-related risk perception and PrEP acceptability among young adult female family planning patients. AIDS Care. 2017;29(6):751–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wingood GM, Dunkle K, Camp C, et al. Racial differences and correlates of potential adoption of preexposure prophylaxis (PrEP): results of a national survey. J Acquir Immune Defic Syndr. 2013;63(0 1):S95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Connecticut Department of Public Health. Epidemiological profile of HIV Connecticut. 2016.
- 41.Connecticut Department of Public Health. CT Pre-exposure Prophylaxis (PrEP) Local Medical Services. 2017. Available from: https://portal.ct.gov/-/media/Departments-and-Agencies/DPH/dph/aids_and_chronic/prevention/pdf/PrEPServicespdf.pdf?la=en
- 42.Thompson HS, Valdimarsdottir HB, Winkel G, Jandorf L, Redd W. The group-based medical mistrust scale: psychometric properties and association with breast cancer screening. Prev Med. 2004;38(2):209–18. [DOI] [PubMed] [Google Scholar]
- 43.Shelton RC, Winkel G, Davis SN, et al. Validation of the group-based medical mistrust scale among urban Black men. J Gen Intern Med. 2010;25(6):549–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Valera P, Boyas JF, Bernal C, Chiongbian VB, Chang Y, Shelton RC. A validation of the group-based medical mistrust scale in formerly incarcerated Black and Latino men. Am J Mens Health. 2018;12(4):844–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gamarel KE, Golub SA. Intimacy motivations and pre-exposure prophylaxis (PrEP) adoption intentions among HIV-negative men who have sex with men (MSM) in romantic relationships. Ann Behav Med. 2015;49(2):177–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.United States Department of Commerce Economics and Statistics Administration USCB. Race & Ethnicity. 2017. Available from: https://www.census.gov/mso/www/training/pdf/race-ethnicity-onepager
- 47.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- 48.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–91. [DOI] [PubMed] [Google Scholar]
- 49.Hayes AF. Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun Monogr. 2009;76(4):408–20. [Google Scholar]
- 50.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fisher WA, Fisher JD, Shuper PA. Social psychology and the fight against AIDS: An Information–Motivation–Behavioral Skills model for the prediction and promotion of health behavior change. Adv Exp Soc Psychol. 2014;50:105–193. [Google Scholar]
- 52.Shrestha R, Altice FL, Huedo-Medina TB, Karki P, Copenhaver M. Willingness to use Pre-Exposure Prophylaxis (PrEP): An empirical test of the Information-Motivation-Behavioral Skills (IMB) model among high-risk drug users in treatment. AIDS Behav. 2017;21(5):1299–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Eiser AR, Ellis G. Cultural competence and the African American experience with health care: The case for specific content in cross-cultural education. Acad Med. 2007; 82:176–183. [DOI] [PubMed] [Google Scholar]
- 54.Calabrese SK, Krakower DS, Mayer KH. Integrating HIV pre-exposure prophylaxis (PrEP) into routine preventive health care to avoid exacerbating disparities. Am J Public Health. 2017;107(12):1883–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Davis SK, Tucker-Brown A. The efffects of social deterinants on Black women’s HIV rik. J Black Stud. 2013;44(3):273–289. [Google Scholar]
- 56.Calabrese SK, Dovidio JF, Tekeste M, Taggart T, Galvao RW, Safon CB, Willie TC, Caldwell A, Kaplan C, Kershaw TS. HIV pre-exposure prophylaxis stigma as a multidimensional barrier to uptake among women who attend Planned Parenthood. J Acquir Immune Defic Syndr. 2018. (Advance Online Publication). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol. 2014; 68(4):225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mays VM, Mass RM, Ricks J, Cochran SD. HIV and African American women in the U.S. South: a social determinants approcach to population level HIV prevention and Interncention efforts In Baum A, Revenson TA, Singer J, eds. Handbook of helath psychology. et al. ed. New York: Guilford; 2012. p. 771–802. [Google Scholar]
- 59.Calabrese SK, Earnshaw VA, Underhill K, Hansen NB, Dovidio JF. The impact of patient race on clinical decisions related to prescribing HIV pre-exposure prophylaxis (PrEP): assumptions about sexual risk compensation and implications for access. AIDS Behav. 2014;18(2):226–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dovidio JF, Fiske ST. Under the radar: how unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. Am J Public Health. 2012;102(5):945–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mignone J Social determinants of HIV/AIDS: implications for policies in emergnig markers countries. Int J Bus Emerg Market. 2013;5(1):83–97. [Google Scholar]
- 62.Willems S, De Maesschalck S, Deveugele M, Derese A, De Maeseneer J. Socio-economic status of the patient and doctor–patient communication: does it make a difference? Patient Educ Couns. 2005;56(2):139–146. [DOI] [PubMed] [Google Scholar]
- 63.White RO, Chakkalakal RJ, Presley CA, Bian A, Schildcrout JS, Wallston KA et al. Perceptions of provider communication among vulnerable patients with diabetes: influences of medical mistrust and health literacy. J Health Commun. 2016;21(sup2):127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kenny DA, Judd CM. Power anomalies in testing mediation. Psychol Sci. 2014;25(2):334–339. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.