Dear Editor,
Coronavirus disease 2019 (COVID-19) was declared as a pandemic by the World Health Organization on March 11, 2020.1 Globally, there have been 24,299,923 confirmed cases of COVID-19 and 827,730 deaths due to COVID-19 as on 29 August 20.2 Currently, the positive detection of severe acute respiratory syndrome coronavirus 2 RNA in nasopharyngeal or oropharyngeal swab samples is the gold standard for diagnosis. Serological tests have primarily been used as an indicator of past infection as evidenced through serosurveys, which have been conducted at community levels. The discharge policy as promulgated by the Ministry of Health and Family Welfare (MoHFW) does not mandate a negative Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR) report before discharge except in severe cases.3 There is no policy that prescribes the requirement of a predischarge antibody test for ascertaining antibody response in clinically recovered patients.4 More than six months into the pandemic, data regarding the kinetics of the immune response among Indian patients are lacking to a large extent. Hence, this study has been undertaken to describe the patterns of antibody response in hospitalized patients with COVID-19.
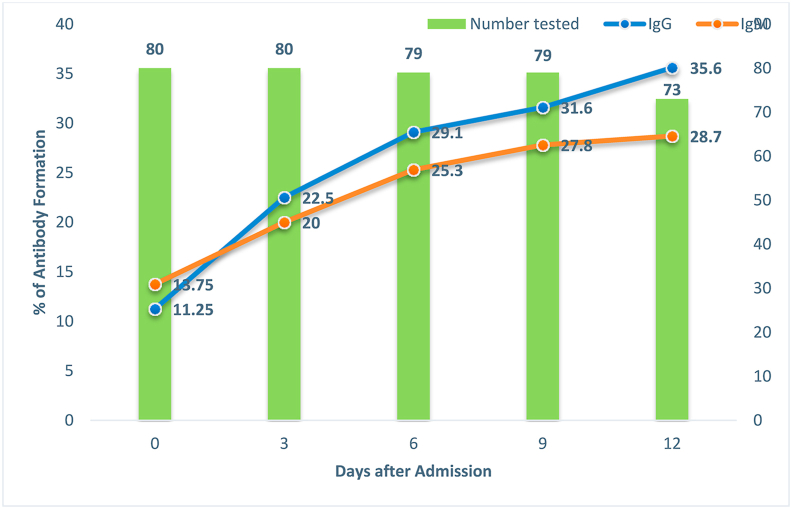
The study was conducted in a dedicated COVID-19 hospital, where only patients with COVID-19 are admitted. All admitted patients were approached for the study, and the exclusion criteria included contraindication for phlebotomy and existing coagulation disorders. The following data were collected from the patient's case sheet: date of admission, date of onset of symptoms, date of molecular testing, contact details and reason for testing. The clinical severity of the patient was classified as mild, moderate and severe as per the Indian Council of Medical Research (ICMR) guidelines.5 The cases were tested for antibodies on admission and then every third day until discharge/death. The Rapid Antibody Detection kit, manufactured by M/S SD Biosensor, was used, which tests for both IgM and IgG antibodies. The specimen collection of venous blood for antibody testing was banded together with other investigations. The study is ongoing, and currently, the initial results for first 80 patients with COVID-19 enrolled in the study are being presented here. The patients were admitted from July 14, 2020 to July 25, 2020. The serological test were conducted every third day till discharge of the patient. A total of 391 serological tests for IgM and IgG were conducted. The last samples were taken on the 12th day for all patients, except 6 patients, for whom they were taken on the 9th day. Only two samples could be taken from one patient. All patients were positive with molecular testing at the time of admission. A total of 18 (22.5%) patients were women. The mean age of the patients was 39.75 years (standard deviation [SD] = ± 16.5 years), and the median was 40 years, with a range from 10 years to 80 years. Among all participants, 58 (72.5%) cases were mild, 18 cases (22.5%) were moderate and 4 (5%) were severe cases. The mean time of molecular testing was 2.9 days (SD = ± 2.3 days) after the onset of symptoms; the median was two days, with a range from 0 to 13 days. A total of 56 patients (70%) were admitted on the same day of the positive testing, and 8 (10%) patients were admitted the next day of the testing. The rest were admitted between 3 and 11 days after testing positive. One death occurred on the seventh day of admission. The result of antibody testing is shown in Fig. 1.
Fig. 1.
Kinetics of antibody response after hospital admission.
The study conducted on the hospitalized patients with COVID-19 shows a consistent increase in IgG and IgM antibody response over a period of time. However, as per the initial finding of the study, the majority of the patients (approximately 65%) did not have detectable antibodies at the time of discharge. The comparison among the group of clinical similarities was not carried out as the numbers are very small in severe and moderate cases to do any meaningful comparison as of now. These estimates may further be revised as the number of cases enrolled in the study increases and with sensitivity analysis of the data based on the sensitivity and specificity of the manufactured kit and availability of data from the validation study. Because the study does not allow for the scope of follow-up, it would be difficult to comment as to how many discharged cases would eventually go on to develop a positive IgM/IgG response. Nevertheless, the study emphasized the need for isolation and monitoring even after discharge from the hospital because a negative antibody response translates to the ongoing susceptible state of the individual.6 This gained importance in view of relapse and isolated cases of reinfection.7 The study has implication for convalescent plasma therapy also as those who all have recovered might not be eligible for donation of plasma for convalescent plasma therapy.
Disclosure of competing interest
The authors have none to declare.
Acknowledgements
The authors are grateful to all the patients and the healthcare workers in the coronavirus disease 2019 hospital.
References
- 1.Coronavirus Disease (COVID-19) - events as they happen [Internet]. [cited 2020 Mar 19]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen.
- 2.WHO Coronavirus Disease (COVID-19) Dashboard [Internet]. [cited 2020 Aug 29]. Available from: https://covid19.who.int.
- 3.ReviseddischargePolicyforCOVID19.pdf [Internet]. [cited 2020 Aug 30]. Available from: https://www.mohfw.gov.in/pdf/ReviseddischargePolicyforCOVID19.pdf.
- 4.Testing Strategy [Internet]. [cited 2020 Aug 30]. Available from: https://www.icmr.gov.in/cteststrat.html.
- 5.ClinicalManagementProtocolforCOVID19.pdf [Internet]. [cited 2020 Aug 30]. Available from: https://www.mohfw.gov.in/pdf/ClinicalManagementProtocolforCOVID19.pdf.
- 6.La Marca A., Capuzzo M., Paglia T., Roli L., Trenti T., Nelson S.M. Testing for SARS-CoV-2 (COVID-19): a systematic review and clinical guide to molecular and serological in-vitro diagnostic assays. Reprod Biomed Online. 2020 Jun 14 doi: 10.1016/j.rbmo.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yadav AK, Ghosh S, Dubey S. Is There Any Evidence for Reinfection of the SARS COV 2: A Systematic Review. Under publication ( Personal communication).