Abstract
Intraocular inflammation in patients with human immunodeficiency virus (HIV) infection is commonly due to infectious uveitis. Ocular lesions due to opportunistic infections (OI) are the most common and have been described extensively in the pre highly active antiretroviral therapy (HAART) era. Many eye lesions were classified as acquired immunodeficiency syndrome (AIDS) defining illnesses. HAART-associated improvement in immunity of the individual has changed the pattern of incidence of these hitherto reported known lesions leading to a marked reduction in the occurrence of ocular OI. Newer ocular lesions and newer ocular manifestations of known agents have been noted. Immune recovery uveitis (IRU), the new menace, which occurs as part of immune recovery inflammatory syndrome (IRIS) in the eye, can present with significant ocular inflammation and can pose a diagnostic and therapeutic challenge. Balancing the treatment of inflammation with the risk of reactivation of OI is a task by itself. Ocular involvement in the HAART era can be due to the adverse effects of some systemic drugs used in the management of HIV/AIDS. Drug-associated retinal toxicity and other ocular side effects are being increasingly reported. In this review, we discuss the ocular manifestations in HIV patients and its varied presentations following the introduction of HAART, drug-associated lesions, and the current treatment guidelines.
Keywords: AIDS, CMV retinitis, drug-induced uveitis, HAART, herpes zoster, HIV, intraocular inflammation, IRU, ocular opportunistic infections, ocular syphilis, ocular TB, ocular toxoplasmosis, retinopathy, uveitis
Human immunodeficiency virus (HIV) disease is a pandemic of global concern, not only due to serious health issues affecting all organs of the body but also due to its huge economic burden.[1] It has had a continuous effect on both high-and low-resource countries over the last four decades despite various national and international practice policies and guidelines in place.[2,3] The social stigma associated with the diagnosis, changing sexual practices in humans, lack of availability of a vaccine and the chronicity of the disease requiring lifelong treatment are major hurdles in containing the disease.[4]
Ocular involvement has been extensively described in the pre highly active antiretroviral therapy (HAART) era with, many of them classified as AIDS-defining illnesses. Ocular lesions due to opportunistic infections (OI) are on the decline with the advent of HAART. This has changed the pattern of incidence of ocular lesions in patients with HIV with newer manifestations such as due to systemic drugs being reported.[5,6,7]
A systematic literature search was carried out using Medline keywords and MESH terms used for literature search including HIV, AIDS, ocular manifestations, opportunistic infections, HAART, pre-HAART, combined anti-retroviral therapy (cART), anterior segment manifestations, adnexal, posterior segment, CMV retinitis, viral retinitis, ocular toxoplasmosis, ocular tuberculosis, ocular syphilis, immune recovery uveitis, immune recovery inflammatory syndrome (IRIS), pediatric HIV, drug-induced uveitis, World Health Organization (WHO), NACO. The results were filtered and appropriate articles were considered for this review. The authors have a collective experience of several decades in treating HIV patients with ophthalmic manifestations because of their work both across the globe and in India.
Here, we discuss the ocular lesions that potentially affect HIV-infected patients in the era of HAART. The changing trends in the prevalence of various OIs, variations in the clinical manifestations with HAART, drug associated lesions and the current treatment guidelines are described.
Epidemiology of HIV – Global and Indian Perspective
A new immunodeficiency syndrome was first described in the 1980s in patients with rare opportunistic infections and cancers.[8,9] HIV was isolated in 1983,[10] and the disease was identified and coined the name “acquired immunodeficiency syndrome (AIDS).” As of 2018, it is estimated that close to 38 million people are infected with this dreaded virus across the world, most of them from Eastern and Southern African regions (21 million). Worldwide, approximately 7,70,000 people have died from HIV-related causes.[2]
In India alone, 2.14 (1.59–2.84) million people are estimated to be living with HIV, the third largest HIV-infected population in the world. The last few years have shown a declining trend with an overall estimated HIV prevalence among adults being 0.22% in India.[11,12] However prevalence is higher in the high-risk sub-populations like female sex workers (FSW), men who have sex with men (MSM), injection drug users (IDU), and bridge populations (clients of sex workers-truck drivers and migrant workers); from these groups, there is onward transmission to the general population.[4] The National AIDS Control Organization (NACO) has sentinel surveillance and the districts with consistently higher HIV prevalence were found clustered in the North-East (Mizoram, Manipur, and Nagaland) and Southern (Telangana, Andhra Pradesh, Tamil Nadu, and Karnataka) regions of India.[4]
Ocular Disease and HIV
Ocular involvement in HIV was first described by Holland et al. in 1982, in the form of cotton wool spots, cytomegalovirus retinitis (CMVR) and Kaposi sarcoma (KS).[1] In India, it was first reported in 1995.[13] The treatment available for HIV in the early days was unfortunately limited and less effective. With the advent of HAART or combined anti-retroviral therapy (cART) around 1995, there has been a significant improvement in the systemic and hence the ocular status of HIV infected individuals.[5,6,7] In the pre-HAART era, 50% to 75% of untreated HIV-infected individuals were reported to have ocular involvement,[14] the lower the CD4 counts, the higher the risk. In a large study from a tertiary eye care center in India, which included predominantly patients in the pre-HAART era, ocular lesions were noted in 68.5% cases.[15] In a study from a systemic HIV/AIDS care center in Mumbai, India, prevalence of ocular disease was noted to be about 17.5 % among adults. This was found to be higher (24%) if CD4+ cell count was less than 200 cells/mm3 in HAART naïve patients.[16]
Better HIV detection and treatment strategies have led to a positive change in the spectrum of ocular disease in such patients over the past three decades. This has been possible due to increasing access to appropriate HAART regimen through various programs under the aegis of World Health Organization (WHO), NACO, Global Fund to fight AIDS, tuberculosis, malaria and others, US President's Emergency Plan for AIDS Relief (PEPFAR) as well as due to the availability of newer and better antiretroviral drugs.[17] As of 2018, up to 78% of HIV infected individuals have access to HAART worldwide according to WHO reports.[5] Current WHO and NACO guidelines suggest treatment initiation irrespective of the clinical stage of disease or absolute CD4+ T-cell counts.[18,19] These guidelines have resulted in a reduction in HAART naïve patients with a corresponding decrease in ocular OIs. This has led to a paradigm shift from infectious to other non–infectious manifestations along with a noticeable change in the previously described classical phenotypic presentations of ocular OIs with HAART.
Ocular involvement will be presented under the following subheadings
-
Attributable to HIV
- Due to HIV itself
- Opportunistic infections (OI).
-
Drug-related reactions
- Immune recovery uveitis (IRU)
- HAART associated ocular lesions.
Not directly attributable to HIV
Intraocular Inflammations Attributable to HIV/AIDS
Intraocular (IO) inflammation in HIV patients can either be due to the OIs or uncommonly due to HIV itself. Also, patients responding to HAART may develop immune recovery inflammatory syndromes (IRIS) as the recovering immune system begins to attack microbial antigens, which the devastating immune system previously had been unable to respond to.
Ocular Lesions Due to HIV Itself
HIV-related microangiopathy
HIV-associated microvascular retinopathy may manifest as cotton wool spots, retinal hemorrhages, and/or microaneurysms[1] [Fig. 1]. It rarely causes visual impairment other than subtle visual field defects.[20] Before HAART, it was noted in up to 15%–30% of patients.[6,19] In patients on HAART, HIV retinopathy (HIVR) may be an indicator of therapeutic failure. This could be due to drug resistance and/or suboptimal treatment adherence, given that HIVR is associated with lower CD4+ counts and shows spontaneous resolution with improvement in CD4 counts. HIV retinopathy also is a risk factor for retinal vascular occlusions, a rare ocular complication of HIV infection.[21]
Figure 1.
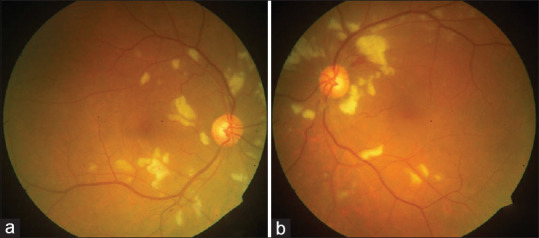
Color fundus photographs of a patient with HIV retinopathy of right eye (a) and left eye (b) showing extensive cotton wool spots in the posterior pole
HIV-induced uveitis
Intraocular inflammation in patients with HIV can be seen due to the direct effect of HIV itself apart from those due to OIs. HIV-induced uveitis should be suspected, especially in HAART naïve and/or non-responders who present with anterior uveitis and without any retinal lesions attributable to OIs.[22,23] It is important to differentiate HIV-induced uveitis and IRU in patients on HAART. HIV-induced uveitis patients have anterior segment inflammation despite low CD4 counts in contrast to IRU (see below) where there is increased inflammation, with higher CD4 counts and a corresponding decrease in plasma viral loads. HIV-induced uveitis is a diagnosis of exclusion. However, intraocular specimen quantification of HIV copies by RT-PCR techniques pre- and post- treatment is a useful indicator in confirming the diagnosis.[23]
Ocular Lesions Due to Opportunistic Infections
Opportunistic infections are still the major cause of visual morbidity in HIV/AIDS individuals.[2,6] Newer lesions and newer manifestations of older known infections have been noted in the HAART era.
Anterior Segment and Adnexal Lesions Associated with HIV/AIDS[24,25]
These include infections caused by viruses, bacteria, fungi, and protozoa.
Herpes Zoster Ophthalmicus (HZO)
Approximately 10%–20% of HIV positive patients are reported to be co-infected with herpes and about half of these seem to have eye lesions.[24,25] The risk of developing HZO is 6.6 times higher in HIV infected individuals than in the general population.[24,26]
The characteristic lesion is the vesiculobullous rash along the distribution of the ophthalmic branch of the trigeminal nerve [Fig. 2a] with necrotic skin lesions [Fig. 2b]. It may be associated with dendriform and stromal keratitis, conjunctivitis, blepharitis, uveitis (often with secondary glaucoma), hemorrhagic hypopyon, scleritis, retinitis, and encephalitis. Diagnosis is mainly clinical but rarely viral culture, Tzanck smear, and polymerase chain reaction (PCR) tests help confirm the diagnosis.[25,26]
Figure 2.
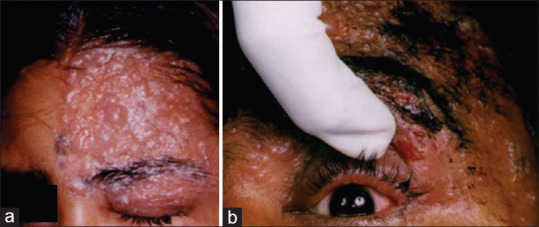
External photograph of a HIV positive patient with herpes zoster ophthalmicus (HZO) (a) showing the vesiculo bullous rash along the trigeminal nerve distribution V1, V2 segments, (b) note the necrotic skin lesions and ocular involvement
Viral Keratitis
Usually caused by Varicella -Zoster virus (VZV), Herpes Simplex 2 virus (HSV), and Cytomegalovirus (CMV) and can cause dendriform lesions. HSV keratitis in HIV patients is known to be twice as more recurrent than in non-HIV patients and is associated with corneal scarring, iritis, and raised intraocular pressure.[27]
Treatment is with topical agents and systemic antivirals [Table 1].[27,28] In recurrent cases, long term oral antiviral prophylaxis has been recommended [Table 1].[33] However, stromal keratitis, being immune- mediated, systemic antivirals seem to reduce only the viral load and thereby the magnitude of inflammation.[24,25] In such situations, cautious additional use of topical low dose steroids such as fluorometholone or loteprednol is recommended as anti-inflammatory therapy under cover of antivirals.[27]
Table 1.
Recommended treatment guidelines for major opportunistic infections
| Opportunistic infection | Recommended treatment regime | Alternate regime | Adverse effects/Remarks |
|---|---|---|---|
| HZO[24,26] | Oral Acyclovir 800 mg five times a day or Oral Valacyclovir 1 gram thrice daily (for 3 to 6 weeks) | Oral famciclovir or foscarnet- in resistant cases | Nephrotoxicity |
| Viral Keratitis[27,28] | Topical therapy | Vidarabine 3% ointment five times daily. | For Recurrent cases (Long term prophylaxis) |
| VZV and HSV - Acyclovir eye ointment five times daily. | Famciclovir (125 to 500 mg three times daily) | Tab Acyclovir 400 mg twice a day for one year[28] | |
| CMV- Ganciclovir gel 0.15% five times daily (until healing occurs) followed by three times daily for 7 days | |||
| Systemic therapy | |||
| VZV and HSV - Acyclovir, Valacyclovir CMV-Valganciclovir | |||
| CMVR[29] | Induction | Induction | Ganciclovir/Valganciclovir-Myelosuppression |
| Intravenous Ganciclovir: 5 mg/kg twice daily for 14-21 days; | Foscarnet (IV): -90 mg/kg twice daily for 14 days | Forcarnet- Nephrotoxicity | |
| Or | Cidofovir (IV): -5 mg/kg weekly for 3 weeks | Electrolyte disturbance | |
| Oral Valganciclovir – 900 mg twice daily | Nausea and vomiting | ||
| Maintenance | Maintenance | Cidofovir-nephrotoxicity | |
| IV Ganciclovir – 5 mg/kg/day to continue | Focarnet - 120 mg/kg/day; | (Probenecid coadministration for prevention) | |
| or | Cidofovir - 5 mg/kg every 2 weeks | ||
| Oral Valganciclovir – 900 mg once daily to continue | Intravitreal | ||
| Induction | Intravitreal cidofovir- anterior uveitis and hypotony | ||
| Intravitreal Ganciclovir | Foscarnet: 1.2-2.4 mg 1-2 times weekly | ||
| Induction - 2 mg/0.1 mL – twice weekly | CMV mutations in UL54 or UL97 genes cause ganciclovir resistance | ||
| Maintenance - 2 mg/0.1 mL weekly | Cidofovir: 20 µg 1-8 times as needed to halt retinitis | ||
| Maintenance | |||
| Foscarnet - 1.2 mg Weekly | |||
| OR | |||
| Cidofovir 20 µg every 5-6 weeks | |||
| ARN/PORN[29,30] | Induction | Nephrotoxicity | |
| Intravenous Acyclovir: -500 mg 8th hourly for 2 to 3 weeks; | |||
| Maintenance | |||
| Oral Acyclovir- 800 mg 5 times daily (15 mg/kg in three divided doses) for 6 weeks to 3 months. | |||
| OR | |||
| Oral Valacyclovir: 1 gram three times daily | |||
| Ocular toxoplasmosis[31] | 1) Pyrimethamine- 200 mg on the first day, followed by 75-100 mg daily | Atovaquone, Azithromycin | Myelosuppression Leucopenia, |
| 2) Sulfadiazine- 1-1.5 g four times daily, and | Pseudomembranous colitis | ||
| 3) Folinic acid-10-50 mg daily | |||
| With/or (in sulpha allergy) | |||
| Oral Clindamycin-300 mg 4 times a day for 6 weeks | |||
| Ocular TB | New: (never had treatment or less than 1 month of ATT) - | MDR TB: Aminoglycosides (Kanamycin, Amikacin), | Hepatotoxicity |
| Peripheral neuropathy | |||
| New* - 2H7 R7 Z7 E7. + 4H7 R7 E7 Previously Treated: (one month or more of ATT) - 2 H7 R7 Z7 E7 S7+1 H7 R7 Z7 E7+5 H7 R7 E7 | Fluoroquinolones (Ofloxacin, Levofloxacin), Linezolid, Bedaquiline | Optic neuropathy | |
| Ocular Syphilis[32] | Aqueous crystalline penicillin G: 18-24 million units/day, administered as 3-4 million units IV every 4 hours or continuous infusion for 10-14 days | Procaine penicillin G: 2.4 million units IM/day PLUS probenecid 500 mg orally four times a day, both for 10-14 day | Jarisch-Herxheimer reaction in ocular syphilis with worsening of signs with treatment |
| Penicillin allergy: | |||
| Ceftriaxone two grams daily either intramuscularly or intravenously for 10 to 14 days | |||
| OR | |||
| Doxycycline 100 mg orally twice daily for 14 days | |||
HZO=Herpes Zoster Ophthalmicus, CMVR=Cytomegalovirus retinitis, CMV=Cytomegalovirus, ARN=Acute retinal necrosis, PORN=Progressive outer retinal necrosis, IV=Intravenous, IM=Intramuscular, TB=Tuberculosis, ATT=Anti-tubercular treatment, H=Isoniazid, R=Rifampicin, Z=Pyrazinamide, E=Ethambutol, S=Streptomycin, MDR=TB multidrug resistant tuberculosis, *Never had treatment or less than 1 month of ATT
HZO needs aggressive systemic antivirals and can reduce ocular complications by 50%.[24,25] Recommended treatment guidelines with systemic antivirals are for 3 to 6 weeks [Table 1]. Treatment may need to be extended based on the clinical response especially in patients who have had acute retinal necrosis (ARN) or persistent chronic anterior uveitis. Oral famciclovir or foscarnet are used in resistant cases. Vaccines such as herpes zoster vaccine (Zostavax®), are found to be effective but are contraindicated in patients with CD4 counts <200 cells/cu.mm and/or if total lymphocytes <15%.[26] Varicella immunoglobulin (VZIG) is recommended in post exposure prophylaxis for immunodeficient patients.[26]
Molluscum contagiosum (MC)[25,34]
It is caused by a large DNA pox virus and is characterized by pink or pearly white wart like umbilicated nodules on the skin and can be seen in up to 5%–18% of HIV infected patients.[25,34] They are highly contagious, with fomite transmission and with a median incubation period of 6–8 weeks. It manifests aggressively in children and young adults, involving the eyelid and conjunctiva. Face, trunk, and genitalia are commonly affected, and distribution in the chin-strap region is common in HIV-positive patients.[25] They are characteristically larger in number and size, often confluent, bilateral, and resistant to therapy. The lash line should be examined carefully in all patients with chronic conjunctivitis so as not to miss a molluscum lesion.[34] It is believed to be more in HIV infected individuals due to the profound dysfunction of T-lymphocyte mediated immune response. The lesions usually subside with the institution of HAART. Topical agents like phenol and trichloroacetic acid, serial applications of liquid nitrogen, incision with or without curettage, excision, and cryotherapy are helpful. Topical (1%–3%) or intravenous cidofovir is required in some HIV-infected persons.[34,35]
Bacterial corneal ulcer in immunocompromised subjects is commonly bilateral, polymicrobial and with a higher risk of perforation. In a study of risk factors for microbial keratitis, HIV was identified as a major risk factor in 4.2% of patients while the more common ones were contact lens use, ocular trauma, diabetes, and others.[36] Common organisms causing corneal ulcer in immunodeficient individuals include Staphylococcus aureus, Staphylococcus epidermidis, and Pseudomonas aeruginosa and less frequently Klebsiella oxytoca, Streptococcus, Bacillus, Micrococcus, Capnocytophaga, and Acanthamoeba species in some regions.[24,25] Bacterial keratitis superimposed on pre-existing viral keratitis and keratoconjunctivitis sicca (KCS) has also been reported in HIV patients.[24] Identification of the causative agent by Gram stain and bacterial culture from corneal scraping or corneal biopsy is diagnostic. Topical therapy alone is insufficient; systemic treatment with parenteral antibiotics based on culture and sensitivity may be warranted in many cases. Despite aggressive local and systemic treatment, these ulcers may require therapeutic keratoplasty or may even progress to endophthalmitis/panophthalmitis leading to evisceration/enucleation of the eye.
Microsporidial keratitis in AIDS is characterized by bilateral superficial punctate epithelial keratitis, white intraepithelial infiltrates, and follicular conjunctivitis with/without minimal anterior chamber reaction. Masson trichrome or Giemsa stain from conjunctival scrapings or corneal biopsy aids in diagnosis. Treatment with fumagillin eye drops (70 mg/mL) and oral albendazole are effective.[37]
Neoplasms in HIV/AIDS[38]
Kaposi sarcoma (KS)[39]
It is a highly vascular mesenchymal tumor, presenting as multiple purple-to-red nodules on the skin and mucous membrane. It is caused by human herpesvirus 8 (HHV-8) or KS herpesvirus (KSHV), which is rare in India. It has been considered as AIDS -defining illness occurring in immune-deficient individuals.[24,25] The current post hoc analysis found a cut off of CD4 cells <150 cells/μL as a better indicator, although in the HAART era, CD4 counts alone in KS is not considered a prognostic factor.[40]
Conjunctival KS, which can present as subconjunctival hemorrhage and adnexal KS are the common ocular manifestations. HAART has reduced the incidence of primary KS including conjunctival KS. IRIS-associated KS often presents with rapidly progressive visceral lesions with high mortality. It is usually seen in patients with high HHV-8 and HIV loads prior to initiation of HAART. Different treatment options based on the extent and site of KS include radiotherapy, cryotherapy, surgical excision, and systemic chemotherapy. Localized lesions can be surgically excised with or without adjunctive cryotherapy to the margins. Multiple chemotherapy options are recommended factoring in the cost-effectiveness and the superior efficiency of the drugs including pegylated liposomal doxorubicin and paclitaxel.[41] While paclitaxel has been found to be most effective, bleomycin has also shown promising results.[41] Lenalidomide, interferon α, and immune checkpoint inhibitors (nivolumab, pembrolizumab) are being studied in clinical trials.[41] KSHV inflammatory cytokine syndrome (KICS), a cytokine mediated response (IL6/IL10), due to HHV-8 reactivation, presenting with multiple severe inflammatory symptoms has recently been reported.[40,42]
Ocular surface squamous neoplasia (OSSN)[24,43]
They are among the common primary malignancies of the eye. Different risk factors have been considered in the pathogenesis including ultraviolet rays (UV) exposure, human papillomavirus (HPV) infection and other chemicals such as arsenic and hydrocarbon. In HIV individuals it can occur at an earlier age (3rd/4th decade) and is more likely to affect both cornea and conjunctiva.[24,43] Seropositivity was higher in OSSN patients in Sub-Saharan Africa (49-92%) than in patients in India (38-41%). In up to 2/3rd of patients with OSSN, it can even be the presenting sign of HIV/AIDS. Hence all patients with OSSN have to be screened for HIV.[43]
Patients can be asymptomatic or may have mild symptoms such as foreign body sensation, irritation, or mild pain. It can appear as unilateral or bilateral, pigmented or non-pigmented papillary lesions with an intra-lesional blood vessel (feeder vessel) and fronds, raised plaque with keratinization, or as a diffuse gelatinous form.
OSSN can easily be misdiagnosed as benign lesions, such as pinguecula, pterygium, or papilloma. Diagnosis requires an incisional or excisional biopsy. Treatment options include tumor excision with amniotic membrane grafting for residual conjunctival defects. Adjunctive therapies like cryotherapy or chemotherapy are essential. For instance, topical Mitomycin-C (MMC) or 5-FU, four times weekly for one week, can be given followed by a drug holiday (one week in case of MMC and three weeks with 5-FU) and repeating this cycle until the lesion regresses.[43] It is important to monitor its side effects, especially epithelial toxicity. Interferon, on the other hand, is better tolerated and can be administered as eye drops, administered continuously four times daily until the tumor regresses, or as once weekly subconjunctival injection. HIV infection is associated with large aggressive tumors, higher-grade malignancy, higher incidence of corneal, scleral and orbital invasion, advanced-stage T4 tumors, higher need for extended enucleation/exenteration, and increased risk of tumor recurrence.[38,43] In contrast to the situation with many other opportunistic viral complications of AIDS, HAART does not seem to reduce the incidence of OSSN nor interrupt tumor growth or recurrence. Human papillomavirus (HPV) has been implicated in the pathogenesis of both uterine cervical cancer and OSSN. Although not clearly established, a possible role of HPV vaccination in the prevention of OSSN is being considered.
Conjunctival Lymphoma
Ocular adnexal lymphoma (OAL) and intraocular lymphomas are B-cell non-Hodgkins lymphomas (NHL), which are the next common neoplasia seen in HIV/AIDS.[38,44] Orbits, lacrimal glands, conjunctivae, and eyelids where it presents as erythematous lesions are most commonly affected.[44,45] Treatment for low-grade tumors is by chemotherapy with chlorambucil or fludarabine and for high grade tumours by CHOP (cyclophosphamide, vincristine, doxorubicin, and prednisolone) or by radiotherapy. However, despite treatment, prognosis is poor. Monoclonal antibodies targeted against CD40 (B-cell activating factor of the TNF family) are in an investigational stage. Bortezomib, a proteasome inhibitor, has been used to target intracellular pathways involved in tumor cell survival and growth with good results.[46]
Posterior segment manifestations[47,48]
Cytomegalovirus Retinitis(CMVR)
Despite a significant decrease in incidence, CMV retinitis (CMVR) remains the most common OI in HIV/AIDS even in the HAART era.[5,6,7] It accounted for 15%–40% of ocular lesions in HIV prior to HAART.[6,15] In a large study of 1000 patients from India, it was found to be the commonest seen in 24.8%.[15] The most important risk factor for CMVR in AIDS is low CD4 counts. There have been few reports of CMVR even with moderate CD4 counts, but is uncommon if CD4 counts are over 100 cells/mm3.
Genetic susceptibility characteristics such as specific haplotypes of interleukin 10 receptor (IL-10R1), chemokine receptor 5 (CCR5), and stromal- derived factor-1 (SDF-1) have been identified as possible risk factors.[48] Interestingly, HIV microangiopathy, with cotton wool spots (CWS), which are areas of retinal microinfarction, has also been found to be a risk factor, presumably by interrupting the blood-retinal barrier and thus facilitating the viral entry into the eye.[7,19,48] Although HAART does not completely prevent the occurrence of CMVR, it has contributed to the more rapid resolution of lesions without the need for long term maintenance therapy.[49]
CMVR can be unilateral or bilateral with hematological spread. Characteristic presentations in patients with low CD4 counts, include the classical “pizza pie” appearance with retinal hemorrhages [Fig. 3a] and/or the yellow-white necrotizing granular type retinitis with or without minimal vitritis. There may be extensive retinal involvement [Fig. 3b]. In patients on HAART with moderate counts, it can also present with vitreous or vascular inflammation. This perhaps represents a mixture of retinal necrosis with superimposed IRIS in cases recently started on HAART. In the active stage, lesions may be fulminant, indolent (granular CMV), or exudative form with extensive perivascular sheathing or frosted branch angiitis (FBA). The lesions can either progress to retinal necrosis and multiple tears leading to subsequent retinal detachment. Alternatively, they can heal, leaving behind an atrophic retina with fibrosis, calcification, and sclerotic retinal vessels, and thus retinal detachment risk declines. Retinal necrosis and multiple tears are more common in HSV and VZV retinitis than in CMVR.[49]
Figure 3.

Color fundus photograph of the right eye showing active cytomegalovirus retinitis (CMVR) in two different HIV positive patients. (a) Necrotizing retinitis with hemorrhages- the classical pizza pie appearance; (b) Montage picture showing extensive involvement of the retina
Diagnosis is mostly clinical, but in atypical presentations, intraocular fluid PCR testing for CMV aids in the diagnosis. The mainstay of treatment is to reinstate the immune status of the patient with HAART, which should be used in all cases since it reduces the risk of visual loss, retinal detachment, second eye involvement, and mortality.[49,50,51,52]
The recommended regime of choice historically [Table 1] is with intravenous ganciclovir as induction therapy for 2–3 weeks, followed by a maintenance dose. Oral Valganciclovir, a prodrug with good oral bioavailability is equally effective, and therefore now the preferred initial treatment avoiding hospitalization and risks related to indwelling catheters. Treatment is continued until the lesions have resolved completely and the patient's immune status has improved, with an increase of CD4 counts >100–150 cells/μL. Foscarnet or combination therapy has been attempted in drug -resistant cases. The use of Cidofovir is limited due to the increased risk of nephrotoxicity and uveitis.[29] Letermovir, a newly approved drug (2017) for CMV-seropositive allogeneic hematopoietic-cell transplantation recipients, has been tried in drug-resistant CMVR.[53] Intravitreal injections of either ganciclovir or foscarnet may be considered in addition to systemic ganciclovir in macula threatening lesions and/or in resource constraint settings. Intravitreal ganciclovir as a monotherapy option is not recommended. Studies have shown high mortality rates in patients treated with local therapy alone.[52]
CMVR threatens vision directly via extension of retinitis into vital visual structures, rhegmatogenous retinal detachment (RRD), contralateral eye involvement or retinal vascularisation, and/or as a sequelae of IRU- associated inflammation.[51,54] Pre-HAART rhegmatogenous RD, reported in about 30% of CMVR patients has been a leading cause of poor visual outcome. The estimated rate of retinal detachment (RD) with CMV retinitis in the HAART era is 0.06/person-years versus 0.33/person-years in the pre-HAART period. The treatment of choice is primary vitrectomy with higher viscosity silicone oil tamponade (5000 cs).[51,55] The inability to seal the multiple posteriorly located holes is among the main reasons for preferring silicone oil over gas tamponade in most cases. While benefits of immune recovery are obvious, IRU can occasionally result in proliferative vitreoretinopathy (PVR) with exuberant inflammation and higher chances of recurrent RD. With HAART, due to longevity of patients, additional procedures like cataract surgery, YAG capsulotomy, and silicon oil removal are sometimes required to maintain vision.[55]
Acute retinal necrosis (ARN)[30] and progressive outer retinal necrosis[56]
They are severe sight-threatening rapidly progressive necrotizing retinitis caused by VZV and HSV. The diagnosis is clinical. ARN presents classically with peripheral confluent lesions spreading circumferentially. Progressive outer retinal necrosis (PORN) presents with what appears to be an outer retinal whitening (cracked mud appearance). However histologically, it is a full thickness retinal necrosis with minimal or no intraocular inflammation. Vitritis is usually severe in ARN while it characteristically is absent or is very minimal in progressive outer retinal necrosis. The latter occurs commonly in immunocompromised patients with low CD4 counts. The more common presentations include necrotizing herpetic retinopathies with characteristic well-demarcated, multifocal, coalescing, and deep or full-thickness areas of predominantly posterior retinal necrosis.[57] In case of a diagnostic dilemma, PCR testing of IO sample can be helpful.
Treatment requires aggressive systemic acyclovir or valacyclovir with additional intravitreal antivirals in macula threatening lesions [Table 1]. Oral valacyclovir, at the recommended dose, has been shown to achieve about 50%–65% bioavailability similar to intravenous acyclovir.[30] Higher doses to increase the bioavailability is fraught with the risk of systemic side-effects and hence avoided. Low dose systemic steroids with caution can help resolve vitritis and reduce the destruction of the retina due to inflammation. Antivirals may need to be continued for 3 to 6 months or perhaps indefinitely with monitoring of side effects. Prophylactic laser barrage and/or vitrectomy as options to reduce the chances of RD have not been conclusively proven to be favorable.[30] In comparison to those due to CMVR, the incidence of RD post-ARN is incredibly high. PORN, which often has bad outcomes, may do better with combined systemic treatment with intravitreal foscarnet therapy.
End-stage of severe cases of CMVR, ARN and PORN can result in optic atrophy leading to permanent visual loss.
Ocular toxoplasmosis (OT)[31,58]
In HIV, ocular toxoplasmosis, is usually of the acquired variety, and reactivation is more a rule rather than an exception. In a study from India, ocular toxoplasmosis was the second most common OI seen in 2.8% patients.[15] Atypical toxoplasmosis in HIV infected individuals can present as focal, multifocal, or diffuse necrotizing retinitis type [Fig. 4a] with indistinct borders with or without hemorrhages. They can also present with active retinochoroiditis adjacent to a retinochoroidal scar [Fig. 4b]. Adjacent retinal vasculitis (Kyrieleis' arteriolitis) with varying amounts of vitreal inflammation (mild to extensive) occurring in the context of low CD4+ T-cell counts is more in favor of toxoplasmic infection. Toxoplasmic chorioretinitis can mimic CMVR and other ocular OIs such as syphilis and may follow a fulminant course. In most cases, early diagnosis and treatment gives satisfactory results. Diagnosis is clinical but atypical cases are confirmed based on raised serum IgM and IgG titers. Serology alone is of limited value since even normal persons demonstrate serologic evidence of toxoplasma infection. In a study from India, Meisheri et al. found the overall seroprevalence of toxoplasmosis to be 67.4% in HIV/AIDS patients.[59] In atypical presentations, intraocular specimen evaluation may be valuable.[60] High titers of specific anti-toxoplasma IgG antibodies have a very high positive predictive value. However, PCR method seems more efficient in immunocompromised individuals with atypical retinitis.[60] Antibody determination is advocated to complement PCR in the diagnosis of toxoplasmosis. Goldmann–Witmer coefficient is less sensitive than PCR in patients with advanced immunosuppression.[60,61]
Figure 4.

(a) Color fundus photograph of the right eye in a HIV positive patient showing intense vitritis with necrotizing retinochoroiditis at the posterior pole; (b) Color fundus photograph of the left eye in another HIV positive patient, showing an active toxoplasma lesion adjacent to a retino-choroidal scar
The most accepted treatment regime includes a combination of pyrimethamine and sulfadiazine with/without clindamycin [Table 1]. Azithromycin is an alternative drug. Oral corticosteroids (only given with antiprotozoal drugs), help resolve inflammation but need to be used with caution due to obvious systemic risks of further depression of host immunity outweighing the benefits.[31] Intravitreal clindamycin is helpful as an adjunct to systemic therapy, with promising results, especially in aggressive OT.[62] Maintenance therapy with cotrimoxazole (also indicated for pneumocystis prophylaxis) and folinic acid is mandatory if the CD4+ T cell count remains less than 100 cells/mm3. It helps reduce the risk of ocular recurrence or concurrent cerebral toxoplasmosis.[31]
Ocular Tuberculosis
Tuberculosis (TB) remains endemic throughout Latin America, Asia, and India. In studies from India,[63] OTB was seen in 3.8% of patients with HIV in the pre-HAART era, presenting as choroidal tubercles [Fig. 5a], sub-retinal abscess [Fig. 5b], conjunctival tuberculosis, and panophthalmitis.[64] Ocular TB may be seen as part of disseminated systemic disease and may be a clue to diagnose a miliary disease. Usually, they are found as asymptomatic choroidal tubercles during routine ophthalmic examination. They can occur in all ranges of CD4 counts and the ocular course does not always coincide with the systemic disease.[15,63] Systemic antitubercular therapy (ATT) is the treatment of choice along with HAART [Table 1]. Paradoxical worsening of tubercular infection following the initiation of HAART due to the improvement of the host's immune response to mycobacterial antigens is common and can have devastating complications.[65] With the widespread availability of HAART, IRIS is to be watched for in any patient undergoing treatment for HIV and tuberculosis.[54,65,66]
Figure 5.

(a) Color fundus photograph of the left eye in a HIV positive patient showing choroidal tubercle; (b) Color fundus photograph of the left eye of another HIV positive patient with yellowish sub-retinal mass lesion suggestive of a tuberculous sub-retinal abscess
HIV-positive patients maybe 10 times at greater risk of multidrug-resistant (MDR) TB than HIV-negative patients.[67] Management of MDR-TB is more complex among patients with HIV infection. The higher pill burden, drug interactions, IRIS, and other concurrent HIV-associated opportunistic diseases all pose unique challenges in their care.[67] Rifampicin resistance is noted more frequently in TB patients with HIV, than in non-HIV patients. Xpert® MTB/RIF (Xpert) an automated DNA-based diagnostic test detects the M. tuberculosis rpoB gene. Xpert also detects mutations in rpoB that may cause rifampicin resistance.[68,69] For ART initiation in HIV-infected patients with tuberculosis, specific guidelines have been framed for balancing the risks due to infection, inflammation, and systemic disease[70] [Table 2].
Table 2.
Recommendation on timing of ART in HIV-TB Coinfection (WHO-Guidelines)[70]
| Adults | TB treatment to be initiated first, followed by ART as soon as possible within the first 8 weeks (anytime between 2 weeks to 2 months) of ATT. CD4 counts <50 cells/µL-(HIV- TB patients with profound immunosuppression)- ART within the first two weeks of initiating TB treatment due to a higher risk of death. |
| Children | ART should be started in any child with active TB disease as soon as possible and within 8 weeks following the initiation of ATT, regardless of the CD4 cell count and clinical stage |
ART=Anti-retroviral treatment, HIV=Human immunodeficiency virus, TB=Tuberculosis WHO=World Health Organistion, ATT=Anti-tuberculosis therapy
It has seen a resurgence, especially in HIV co-infection who have the same susceptible high-risk population as sex workers and men who have sex with men (MSM).[72] It can mimic any uveitic entity and hence called “the great imitator”. Clinical features include anterior uveitis, significant vitritis, diffuse retinitis [Fig. 6], placoid chorioretinitis, panuveitis, and optic neuropathy. Due to its diverse and protean manifestations, a high index of suspicion is needed to diagnose the condition. It is diagnosed based on suspicious clinical features, a positive serology and after exclusion of other known ocular opportunistic infections. Diagnostic tests mainly depend on serum nontreponemal (VDRL, RPR) and treponemal tests (FTA-ABS, TPHA).[73] Due to varying sensitivity and specificity, PCR of ocular fluids for diagnosis of ocular syphilis has limited utility.[74] Although not routinely performed, patients with ocular syphilis and HIV are recommended to have a lumbar puncture (LP) due to a high risk of CNS involvement. LP in ocular syphilis is usually advised in patients with suspected neurological involvement, relapses, or in infants with congenital syphilis. CSF antibody testing (CSF–VDRL/TPHA) is diagnostic of neurosyphilis.[73]
Figure 6.

Color fundus photograph of the right eye of a patient with HIV showing a case of retinitis, retinal precipitates and vitritis due to ocular syphilis
Syphilitic uveitis can occur with any CD4 counts and in any stage of syphilis (primary, secondary, or latent), although it is more commonly seen in secondary syphilis. HAART does not prevent the occurrence of ocular syphilis but can help early resolution along with definitive anti-syphilitic treatment. Penicillin (benzathine penicillin, procaine penicillin) is the treatment of choice [Table 1]. In penicillin allergy, ceftriaxone or doxycycline can be used as an alternative treatment.[32] The Jarisch–Herxheimer reaction can be associated with ocular syphilis presenting as worsening of ocular signs following anti syphilitic treatment.[32]
Neuro-ophthalmic manifestations
Neuro-ophthalmic consequences of HIV infection may include afferent or efferent visual pathways and may result from direct HIV infection, associated OIs, or malignancies. Patients may present with complaints of headache, blurred or loss of vision, double vision, or difficulty in reading. In a study from India, optic atrophy (49.45%) and disc edema (21.97%) were the most common followed by optic neuritis (14.28%), cranial nerve palsies (9.89%), and retrobulbar neuritis (2.19%).[15] The most common associated infections are cryptococcosis, toxoplasmosis, CMV, syphilis, herpes, and tuberculosis.[75] Clinical evaluation may reveal visual field defects, papilledema or optic atrophy, pupillary abnormalities such as anisocoria and light near dissociation, cranial nerve palsies, ocular motility disorders, and retinal changes.[75] Cryptococcus is the most common cause of papilledema in HIV positive patients due to meningitis. It may present as multifocal choroiditis in disseminated disease.[75] Rare instances of Zidovudine-induced anemia, causing papilledema due to idiopathic intracranial hypertension (IIH) has been reported.[76] This highlights the multitude of presentations, which challenge the treating clinician in making an accurate and probably lifesaving diagnosis. Usually, neuro-ophthalmic manifestations are seen in end-stage debilitated patients. With the early institution of HAART, the incidence of neuro-ophthalmic manifestations can be reduced. Uncommonly, progressive multifocal leukoencephalopathy (PML), among the few rare infections, seen in HIV individuals can present with ocular manifestations. Cortical blindness without their classical neurological manifestations as the presenting feature has been reported.[77]
Cat-scratch disease (CSD), caused by Bartonella hensela presents as a neuro retinitis-like picture in immunocompetent individuals. In HIV positive patients, they present differently such as with vascular abnormalities, abnormal vascular network formations among others.[78] Systemic doxycycline for 3–4 weeks leads to complete resolution.
Ocular Lesions Related to Drug Therapy in HIV-Infected Patients
Immune recovery uveitis[54]
HAART has increased survival rate, improved quality of life, and reduced the incidence of fatal OIs in HIV infected individuals. In some individuals, improvement of CD4 counts with HAART may cause immune reconstitution inflammatory syndrome (IRIS). The most common type of ocular IRIS is immune recovery uveitis (IRU). It is defined as any new inflammation in an eye with controlled CMVR or other OI, not attributable to an alternative cause, following substantial recovery of immunity. Ocular IRIS can be noted in many ocular OIs in addition to CMVR such as ocular TB,[66] and Cryptococcus neoformans.[79] Ocular IRIS results in worsening of the clinical manifestations of the OI (paradoxical reaction), or in the appearance of new manifestations shortly after the initiation of HAART (unmasking syndromes). In a large retrospective study from India, ocular IRIS was seen in 17.4% of patients on HAART,[15] and more than half of these patients developed IRU when there was a minimum increase in CD4 counts of about 100 to 150 cells/mm3. Treatment is mostly aimed at controlling the inflammation by topical and/or systemic corticosteroids given that HAART is life-saving.
Drug-induced ocular lesions
Rifabutin is commonly used in the treatment of pulmonary TB and for prophylaxis of Mycobacterium avium complex (MAC) in patients with AIDS and low CD4+ T-cell counts. It can present with hypopyon uveitis,[80,81] and rarely vitritis both as a dose-related effect and/or as an idiosyncratic reaction. The likely reason for uveitis is considered to be due to direct chemical drug toxicity and/or immune complex deposition. The inflammation usually responds to topical corticosteroids. In recurrent or refractory cases, rifabutin may have to be withdrawn.
Cidofovir, used in the treatment of CMVR, has been associated with side effects both with intravitreal and parenteral administration. Granulomatous anterior uveitis is reported more commonly with the intravenous route and less after intravitreal administration.[29,82] Ocular hypotony is seen in up to 22%.[82] Co-administration of probenecid, a competitive inhibitor of organic anion transport in epithelial barriers, is shown to reduce the chances of anterior uveitis due to cidofovir by almost 50%. The frequency of uveitis and nephritis with this drug has reduced its popularity considerably.
Nevirapine-associated Steven Johnson Syndrome (SJS) has also been reported.[83]
Retinal toxicity and optic neuropathy
Retinal toxicity has been reported with didanosine,[84] which has been discontinued from HAART regimens in most countries. Ritonavir and Efavirenz-associated maculopathy have also been reported.[85,86] Optic neuropathy has been reported with ethambutol, linezolid, and the relatively novel drug combination of elvitegravir/cobicistat.[80] All these adverse effects are rare, and hence are not a blanket contraindication to use of these drugs, but might limit therapy in cases where ocular complications occur.
Ocular Lesions – Not Directly Attributable to HIV
Occurrence of immune mediated uveitic entities in an immunodeficient state is uncommon. Few cases of Vogt Koyanagi Harada (VKH),[87] and posterior scleritis[88] in HIV patients have been reported. A possible associated immune reconstitution is considered although not proven. Balancing immunomodulatory treatment with CD4+ T- cell counts and viral load (VL) of the patient is a challenge. Monitored use of IMTs like methotrexate, azathioprine, and even TNFα inhibitors have reported in HIV patients with inflammatory bowel disease, psoriasis, and arthritis with no major adverse events.[89] However, there are no standard recommendations as yet, but most authors do not encourage IMTs in patients with CD4+ cell counts <200 cells/μL and/or VL >60,000 copies/μL, due to associated risks, especially in endemic countries.[89]
Ocular Manifestations in Children with HIV[90,91]
HIV-related ocular lesions in children are different when compared to those seen in adults.
In a study from India, pediatric HIV was noted in 5.5% (12/218 patients).[91] CMVR was the commonest ocular OI even in children, reported in 1/3rd of patients in the pre-HAART era. With HAART, other ocular manifestations like keratoconjunctivitis sicca (KCS), dry eye, and ocular surface disorders like vernal keratoconjunctivitis (VKC) seem to be on the rise. Esposito et al. noted ocular involvement in the form of CMVR and ocular toxoplasmosis in 7.7% children prior to HAART but none with the advent of HAART.[92] CMVR in children is usually more aggressive, bilateral, has a predilection for the macula, and occurs only with much lower CD4 counts when compared to adults.[48] Since children may not complain even with advanced vision loss, frequent ophthalmic screening is a must for early detection and initiation of treatment.
Keratoconjunctivitis sicca (KCS) is noted more frequently in both adults and children with HIV. Decreased tear production occurs in up to 20%–25% of patients with HIV infection, but tear deficiency could not be correlated with CD4+ T-lymphocyte counts. The possible etiopathogenesis include lymphocytic infiltration, cytokine and chemokine response to viral particles destroying the lacrimal gland.[24]
In vernal keratoconjunctivitis (VKC), seen more frequently in children with HIV, increased expression of Th2 cells and its cytokines have been described in the conjunctiva. An improvement in CD4+ T-cell count may improve the ocular allergy, which is otherwise refractory to the regular treatment. Shwetha et al. reported a case of VKC in a child with HIV/AIDS who worsened when CD4 counts were low, but improved with rise in CD4 counts due to a change in the HAART regime. The authors suggest that a possible Th1-Th2 shift occurs as a part of immune response in progressive HIV patients with a decreasing CD4 count.[93]
Ophthalmic Surgery in Patients with HIV/AIDS
Universal precautions refer to a concept of blood-borne disease control. Protective barriers such as gloves, gowns, masks, and protective eyewear are recommended. Double gloving has been found to reduce the risk of percutaneous perforations, thus aiming to prevent prick injuries to health care workers (HCW) at workplace while handling sharps and surgical instruments.[94]
Early cataracts have been noted along with other evidence of early senescence occurring in patients with chronic HIV infection on HAART.[95] Cataract surgery is safe when ocular inflammation is under control and the systemic condition is optimized preoperatively. Perioperative systemic steroid cover in previously inflamed eyes needs to be used with caution. In orbital and squint surgeries in HIV infected individuals, the risk of transmission is high due to associated blood loss, and hence extreme caution is advised.
Systemic Therapy - Highly Active Anti-Retroviral Therapy
NACO provides free HAART to all affected by HIV in India.[96] HAART ensures improved life expectancy and better quality of life in the afflicted.[96] With HAART, HIV patients can now lead a near-normal life, more like chronic diseases such as diabetes mellitus or hypertension. A gist of various classes of anti-retroviral drugs and their mechanism of actions are mentioned in Table 3.
Table 3.
Highly active anti-retroviral drugs and treatment schedule as per NACO guidelines[96]
| Nucleoside reverse transcriptase inhibitors (NRTI) | Non-nucleoside reverse transcriptase inhibitors (NNRTI) | Fusion inhibitors (FI) | Protease inhibitors (PI) | Integrase Inhibitors (INI) (new) |
|---|---|---|---|---|
| Zidovudine (AZT/ZDV)* | Nevirapine* (NVP) | Enfuviritide | Saquinavir* (SQV) | Elvitegravir |
| Stavudine (d4T)* | Efavirenz*(EFV) | (T-20) | Ritonavir* (RTV) | Raltegravir CCR5 |
| Lamivudine (3TC)* | Delavirdine (DLV) | Nelfinavir* (NFV) | Entry Inhibitor (new) | |
| Didanosine (ddl)* | Amprenavir (APV) | |||
| Zalcitabine (ddC)* | Indinavir* (INV) | |||
| Abacavir (ABC)* | Lopinavir/Ritonavir (LPV)* | |||
| Emtricitabine (FTC) | Fosamprenavir (FPV) | |||
| (NtRTI) Tenofovir (TDF)* | Atazanavir (ATV)* | |||
| Tipranavir (TPV) | ||||
| Current National program - Fixed drug combinations | ||||
| (i) Stavudine (30 mg) + lamivudine (150 mg) | ||||
| (ii) Zidovudine (300 mg) + lamivudine (150 mg) | ||||
| (iii) Stavudine (30 mg) + lamivudine (150 mg) + nevirapine (200 mg) | ||||
| (iv) Zidovudine (300 mg) + lamivudine (150 mg) + nevirapine (200 mg) | ||||
| (v) Efavirenz (600 mg) | ||||
| (vi) Nevirapine (200 mg) | ||||
| First choice: AZT + 3TC + NVP (for patients with Hb >8 g/dL)† | ||||
| Second choice: d4T + 3TC + NVP | ||||
*Available in India. †Substitute NVP with EFV, for patients with TB or toxicity to NVP
Conclusion
Identification and early appropriate management of ocular lesions in HIV are of prime importance. Although HAART-associated immune reconstitution has led to a significant decrease in ocular OIs, they are still the most common cause of visual morbidity. In the HAART era, ocular OIs present differently, and newer manifestations including drug-associated lesions are noted. While infectious anterior segment lesions continue to occur, dry eye syndrome, VKC, and newer OSSN are seen in significant proportions. Similarly, while CMVR is still the most common ocular opportunistic infection, toxoplasma, and especially syphilis are on the rise while MDR-TB is the new scourge. With immune recovery, IRIS, and hence IRU causes vision-threatening ocular inflammation. Cautious use of anti-inflammatory therapy such as steroids helps prevent ocular complications due to IRU, which are similar to those found in immunocompetent uveitic eyes. Drug-related side effects both due to HAART and those used in the management of individual entities also have ocular manifestations. With advances in imaging and molecular diagnostics like PCR, there has been an increasing trend in the use of intraocular fluid testing with good yield. These test results need to be interpreted with caution in correlation to clinical findings. Since patients with HIV have a better life expectancy with HAART, the role of an ophthalmologist is pivotal. It does not end with just diagnosing and managing these patients, but to minimize long term complications, prevent irreversible visual loss, thus improving the quality of life in such patients. This review tries to encompass the varied ocular involvement in HIV in the HAART era with an up-to-date management strategy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Holland GN, Gottlieb MS, Yee RD, Schanker HM, Pettit TH. Ocular disorders associated with a new severe acquired cellular immunodeficiency syndrome. Am J Ophthalmol. 1982;93:393–402. doi: 10.1016/0002-9394(82)90127-1. [DOI] [PubMed] [Google Scholar]
- 2.WHO HIV/AIDS fact sheet. Geneva: World Health Organization; 2019. Available from: https://wwwwhoint/en/news-room/fact-sheets/detail/hiv-aids . Last cited on 2019 Jul 11. [Google Scholar]
- 3.National AIDS Control Organisation. Technical Report India HIV Estimates-2012. New Delhi: Ministry of Health & Family Welfare, Government of India; 2012. Available from: http://nacogovin/sites/default/files/Technical%20Report%20%20India%20HIV%20Estimates%202012%281%29pdf . Last cited on 2012 Nov 30. [Google Scholar]
- 4.Joshi RK, Mehendale SM. Determinants of consistently high HIV prevalence in Indian Districts: A multi-level analysis. PLoS One. 2019;14:e0216321. doi: 10.1371/journal.pone.0216321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holland GN. AIDS and ophthalmology: The first quarter century. Am J Ophthalmol. 2008;145:397–408. doi: 10.1016/j.ajo.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 6.Accorinti M, Pirraglia MP, Corradi R, Corsi C, Fabiani C, Pivetti-Pezzi P. Changing patterns of ocular manifestations in HIV seropositive patients treated with HAART. Eur J Ophthalmol. 2006;16:728–32. doi: 10.1177/112067210601600511. [DOI] [PubMed] [Google Scholar]
- 7.Goldberg DE, Smithen LM, Angelilli A, Freeman WR. HIV-associated retinopathy in the HAART era. Retina. 2005;25:633–83. doi: 10.1097/00006982-200507000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control (CDC) Pneumocystis pneumonia--Los Angeles. MMWR Morb Mortal Wkly Rep. 1981;30:250–2. [PubMed] [Google Scholar]
- 9.Gottlieb MS, Schroff R, Schanker HM, Weisman JD, Fan PT, Wolf RA, et al. Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men: Evidence of a new acquired cellular immunodeficiency. N Engl J Med. 1981;305:1425–31. doi: 10.1056/NEJM198112103052401. [DOI] [PubMed] [Google Scholar]
- 10.Barré-Sinoussi F, Chermann JC, Rey F, Nugeyre MT, Chamaret S, Gruest J, et al. Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS) Science. 1983;220:868–71. doi: 10.1126/science.6189183. [DOI] [PubMed] [Google Scholar]
- 11.HIV Facts and figures. Available from: http://nacogovin/hiv-facts-figures . Last cited on 2018 Oct 05.
- 12.National AIDS Control Organization & ICMR-National Institute of Medical Statistics (2018) HIVEstimations 2017: Technical Report. New Delhi: NACO, Ministry of Health and Family Welfare, Government of India; Available from: http://nacogovin/sites/default/files/HIV%20Estimations%202017%20Report_1pdf . Last cited on 2018 Aug 23. [Google Scholar]
- 13.Biswas J, Madhavan HN, Badrinath SS. Ocular lesions in AIDS: A report of first two cases in India. Indian J Ophthalmol. 1995;43:69–72. [PubMed] [Google Scholar]
- 14.Kestelyn PG, Cunningham ET., Jr HIV/AIDS and blindness. Bull World Health Organ. 2001;79:208–13. [PMC free article] [PubMed] [Google Scholar]
- 15.Sudharshan S, Kaleemunnisha S, Banu AA, Shrikrishna S, George AE, Babu BR, et al. Ocular lesions in 1,000 consecutive HIV-positive patients in India: A long-term study. J Ophthalmic Inflamm Infect. 2013;3:2. doi: 10.1186/1869-5760-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pathai S, Deshpande A, Gilbert C, Lawn SD. Prevalence of HIV-associated ophthalmic disease among patients enrolling for antiretroviral treatment in India: A cross-sectional study. BMC Ophthalmol. 2009;9:158. doi: 10.1186/1471-2334-9-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stangl AL, Grossman CI. Global action to reduce HIV stigma and discrimination. J Int AIDS Soc. 2013;16:18934. doi: 10.7448/IAS.16.3.18881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach. 2nd ed. Geneva: World Health Organization; 2016. Available from: http://www.who.int/hiv/pub/arv/arv-2016/en . Last cited on 2017 May 19. [PubMed] [Google Scholar]
- 19.Holland GN, Pepose JS, Pettit TH, Gottlieb MS, Yee RD, Foos RY. Acquired immune deficiency syndrome. Ocular manifestations. Ophthalmology. 1983;90:859–73. doi: 10.1016/s0161-6420(83)80009-8. [DOI] [PubMed] [Google Scholar]
- 20.Freeman WR, Van Natta ML, Jabs D, Sample PA, Sadun AA, Thorne J, et al. Vision function in HIV-infected individuals without retinitis: Report of the studies of ocular complications of AIDS research group. Am J Ophthalmol. 2008;145:453–62. doi: 10.1016/j.ajo.2007.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dunn JP, Yamashita A, Kempen JH, Jabs DA. Retinal vascular occlusion in patients infected with human immunodeficiency virus. Retina. 2005;25:759–66. doi: 10.1097/00006982-200509000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Kunavisarut P, Sirirungsi W, Pathanapitoon K, Rothova A. Clinical manifestations of human immunodeficiency virus-induced uveitis. Ophthalmology. 2012;119:1455–9. doi: 10.1016/j.ophtha.2012.01.030. [DOI] [PubMed] [Google Scholar]
- 23.Selvaraj JR, Sudharshan S, Therese LK, Janani MK, Selvamuthu P, Rewri P, et al. Real-time polymerase chain reaction for diagnosis and management of HIV-induced uveitis. Indian J Ophthalmol. 2018;66:1634–6. doi: 10.4103/ijo.IJO_509_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jeng BH, Holland GN, Lowder CY, Deegan WF, 3rd, Raizman MB, Meisler DM. Anterior segment and external ocular disorders associated with human immunodeficiency virus disease. Surv Ophthalmol. 2007;52:329–68. doi: 10.1016/j.survophthal.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 25.Biswas J, Sudharshan S. Anterior segment manifestations of human immunodeficiency virus/acquired immune deficiency syndrome. Indian J Ophthalmol. 2008;56:363–75. doi: 10.4103/0301-4738.42412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson JL, Amzat R, Martin N. Herpes Zoster ophthalmicus. Prim Care. 2015;42:285–303. doi: 10.1016/j.pop.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 27.Azher TN, Yin XT, Tajfirouz D, Huang AJ, Stuart PM. Herpes simplex keratitis: Challenges in diagnosis and clinical management. Clin Ophthalmol. 2017;11:185–91. doi: 10.2147/OPTH.S80475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oral acyclovir for herpes simplex virus eye disease: Effect on prevention of epithelial keratitis and stromal keratitis. Herpetic Eye Disease Study Group. Arch Ophthalmol. 2000;118:1030–6. [PubMed] [Google Scholar]
- 29.Lee JH, Agarwal A, Mahendradas P, Lee CS, Gupta V, Pavesio C, et al. Viral posterior uveitis. Surv Ophthalmol. 2017;62:404–45. doi: 10.1016/j.survophthal.2016.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schoenberger SD, Kim SJ, Thorne JE, Mruthyunjaya P, Yeh S, Bakri SJ, et al. Diagnosis and treatment of acute retinal necrosis: A report by the American Academy of Ophthalmology. Ophthalmology. 2017;124:382–92. doi: 10.1016/j.ophtha.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 31.de-la-Torre A, Gómez-Marín J. Disease of the year 2019: Ocular toxoplasmosis in HIV-infected patients. Ocul Immunol Inflamm. 2020:1–9. doi: 10.1080/09273948.2020.1735450. doi: 101080/0927394820201735450. [DOI] [PubMed] [Google Scholar]
- 32.Workowski KA, Bolan GA. Centers for disease control and prevention. Sexually transmitted diseases treatment guidelines, 2015 [published correction appears in MMWR Recomm Rep 2015;64:924] MMWR Recomm Rep. 2015;64:1–137. [PMC free article] [PubMed] [Google Scholar]
- 33.Barron BA, Gee L, Hauck WW, Kurinij N, Dawson CR, Jones DB, et al. Herpetic Eye Disease Study. A controlled trial of oral acyclovir for herpes simplex stromal keratitis. Ophthalmology. 1994;101:1871–82. doi: 10.1016/s0161-6420(13)31155-5. [DOI] [PubMed] [Google Scholar]
- 34.Meza-Romero R, Navarrete-Dechent C, Downey C. Molluscum contagiosum: An update and review of new perspectives in etiology, diagnosis, and treatment. Clin Cosmet Investig Dermatol. 2019;12:373–81. doi: 10.2147/CCID.S187224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Erickson C, Driscoll M, Gaspari A. Efficacy of intravenous cidofovir in the treatment of giant molluscum contagiosum in a patient with human immunodeficiency virus. Arch Dermatol. 2011;147:652–4. doi: 10.1001/archdermatol.2011.20. [DOI] [PubMed] [Google Scholar]
- 36.Jin H, Parker WT, Law NW, Clarke CL, Gisseman JD, Pflugfelder SC, et al. Evolving risk factors and antibiotic sensitivity patterns for microbial keratitis at a large county hospital. Br J Ophthalmol. 2017;101:1483–7. doi: 10.1136/bjophthalmol-2016-310026. [DOI] [PubMed] [Google Scholar]
- 37.Taju S, Tilahun Y, Ayalew M, Fikrie N, Schneider J, Kempen JH. Diagnosis and treatment of microsporidial keratoconjunctivitis: Literature review and case series. J Ophthalmic Inflamm Infect. 2011;1:105–10. doi: 10.1007/s12348-011-0025-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vangipuram R, Tyring SK. AIDS-associated malignancies. Cancer Treat Res. 2019;177:1–21. doi: 10.1007/978-3-030-03502-0_1. [DOI] [PubMed] [Google Scholar]
- 39.Dupin N. Update on oncogenesis and therapy for Kaposi sarcoma. Curr Opin Oncol. 2020;32:122–8. doi: 10.1097/CCO.0000000000000601. [DOI] [PubMed] [Google Scholar]
- 40.Cesarman E, Damania B, Krown SE, Martin J, Bower M, Whitby D. Kaposi sarcoma. Nat Rev Dis Primers. 2019;5:9. doi: 10.1038/s41572-019-0060-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Krown SE, Moser CB, MacPhail P, Matining RM, Godfrey C, Caruso SR, et al. Treatment of advanced AIDS-associated Kaposi sarcoma in resource-limited settings: A three-arm, open-label, randomised, non-inferiority trial. Lancet. 2020;395:1195–207. doi: 10.1016/S0140-6736(19)33222-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Polizzotto MN, Uldrick TS, Wyvill KM, Aleman K, Marshall V, Wang V, et al. Clinical features and outcome of patients with symptomatic Kaposi sarcoma herpesvirus-associated inflammation: Prospective characterization of KSHV inflammatory cytokine syndrome (KICS) Clin Infect Dis. 2016;62:730–8. doi: 10.1093/cid/civ996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rathi SG, Ganguly Kapoor A, Kaliki S. Ocular surface squamous neoplasia in HIV-infected patients: Current perspectives. HIV AIDS (Auckl) 2018;10:33–45. doi: 10.2147/HIV.S120517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ferry JA, Fung CY, Zukerberg L, Lucarelli MJ, Hasserjian RP, Preffer FI, et al. Lymphoma of the ocular adnexa: A study of 353 cases. Am J Surg Pathol. 2007;31:170–84. doi: 10.1097/01.pas.0000213350.49767.46. [DOI] [PubMed] [Google Scholar]
- 45.Coupland SE, Krause L, Delecluse HJ, Anagnostopoulos I, Foss HD, Hummel M, et al. Lymphoproliferative lesions of the ocular adnexa. Analysis of 112 cases. Ophthalmology. 1998;105:1430–41. doi: 10.1016/S0161-6420(98)98024-1. [DOI] [PubMed] [Google Scholar]
- 46.Fisher RI, Bernstein SH, Kahl BS, Djulbegovic B, Robertson MJ, de Vos S, et al. Multicenter phase II study of bortezomib in patients with relapsed or refractory mantle cell lymphoma. J Clin Oncol. 2006;24:4867–74. doi: 10.1200/JCO.2006.07.9665. [DOI] [PubMed] [Google Scholar]
- 47.Vrabec TR. Posterior segment manifestations of HIV/AIDS. Surv Ophthalmol. 2004;49:131–57. doi: 10.1016/j.survophthal.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 48.Munro M, Yadavalli T, Fonteh C, Arfeen S, Lobo-Chan AM. Cytomegalovirus retinitis in HIV and non-HIV individuals. Microorganisms. 2019;8:55. doi: 10.3390/microorganisms8010055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jabs DA, Ahuja A, Van Natta ML, Lyon AT, Yeh S, Danis R, et al. Long-term outcomes of cytomegalovirus retinitis in the era of modern antiretroviral therapy: Results from a United States Cohort. Ophthalmology. 2015;122:1452–63. doi: 10.1016/j.ophtha.2015.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kempen JH, Jabs DA, Wilson LA, Dunn JP, West SK, Tonascia JA. Risk of vision loss in patients with cytomegalovirus retinitis and the acquired immunodeficiency syndrome. Arch Ophthalmol. 2003;121:466–76. doi: 10.1001/archopht.121.4.466. [DOI] [PubMed] [Google Scholar]
- 51.Kempen JH, Jabs DA, Dunn JP, West SK, Tonascia J. Retinal detachment risk in cytomegalovirus retinitis related to the acquired immunodeficiency syndrome. Arch Ophthalmol. 2001;119:33–40. [PubMed] [Google Scholar]
- 52.Kempen JH, Jabs DA, Wilson LA, Dunn JP, West SK, Tonascia J. Mortality risk for patients with cytomegalovirus retinitis and acquired immune deficiency syndrome. Clin Infect Dis. 2003;37:1365–73. doi: 10.1086/379077. [DOI] [PubMed] [Google Scholar]
- 53.Turner N, Strand A, Grewal DS, Cox G, Arif S, Baker AW, et al. Use of letermovir as salvage therapy for drug-resistant cytomegalovirus retinitis. Antimicrob Agents Chemother. 2019;63:e02337–18. doi: 10.1128/AAC.02337-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Otiti-Sengeri J, Meenken C, van den Horn GJ, Kempen JH. Ocular immune reconstitution inflammatory syndromes. Curr Opin HIV AIDS. 2008;3:432–7. doi: 10.1097/COH.0b013e328302cc3d. [DOI] [PubMed] [Google Scholar]
- 55.Singh R, Bhalekar S, Parchand S, Sharma A, Gupta V, Dogra MR, et al. Outcome of surgery in post-cytomegalovirus retinal detachment: Experience before and in the era of highly active anti-retroviral therapy in Indian eyes. Indian J Ophthalmol. 2013;61:636–9. doi: 10.4103/0301-4738.119426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Engstrom RE, Jr, Holland GN, Margolis TP, Muccioli C, Lindley JI, Belfort R, et al. The progressive outer retinal necrosis syndrome. A variant of necrotizing herpetic retinopathy in patients with AIDS. Ophthalmology. 1994;101:1488–502. doi: 10.1016/s0161-6420(94)31142-0. [DOI] [PubMed] [Google Scholar]
- 57.Cunningham ET, Jr, Wong RW, Takakura A, Downes KM, Zierhut M. Necrotizing herpetic retinitis. Ocul Immunol Inflamm. 2014;22:167–9. doi: 10.3109/09273948.2014.925378. [DOI] [PubMed] [Google Scholar]
- 58.Holland GN, Engstrom RE, Jr, Glasgow BJ, Berger BB, Daniels SA, Sidikaro Y, et al. Ocular toxoplasmosis in patients with the acquired immunodeficiency syndrome. Am J Ophthalmol. 1988;106:653–67. doi: 10.1016/0002-9394(88)90697-6. [DOI] [PubMed] [Google Scholar]
- 59.Meisheri YV, Mehta S, Patel U. A prospective study of seroprevalence of Toxoplasmosis in general population, and in HIV/AIDS patients in Bombay, India. J Postgrad Med. 1997;43:93–7. [PubMed] [Google Scholar]
- 60.Moshfeghi DM, Dodds EM, Couto CA, Santos CI, Nicholson DH, Lowder CY, et al. Diagnostic approaches to severe, atypical toxoplasmosis mimicking acute retinal necrosis. Ophthalmology. 2004;111:716–25. doi: 10.1016/j.ophtha.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 61.Mahalakshmi B, Therese KL, Madhavan HN, Biswas J. Diagnostic value of specific local antibody production and nucleic acid amplification technique-nested polymerase chain reaction (nPCR) in clinically suspected ocular toxoplasmosis. Ocul Immunol Inflamm. 2006;14:105–12. doi: 10.1080/09273940500545692. [DOI] [PubMed] [Google Scholar]
- 62.Baharivand N, Mahdavifard A, Fouladi RF. Intravitreal clindamycin plus dexamethasone versus classic oral therapy in toxoplasmic retinochoroiditis: A prospective randomized clinical trial. Int Ophthalmol. 2013;33:39–46. doi: 10.1007/s10792-012-9634-1. [DOI] [PubMed] [Google Scholar]
- 63.Babu RB, Sudharshan S, Kumarasamy N, Therese L, Biswas J. Ocular tuberculosis in acquired immunodeficiency syndrome. Am J Ophthalmol. 2006;142:413–8. doi: 10.1016/j.ajo.2006.03.062. [DOI] [PubMed] [Google Scholar]
- 64.Rathinam SR, Lalitha P. Paradoxical worsening of ocular tuberculosis in HIV patients after antiretroviral therapy. Eye (Lond) 2007;21:667–8. doi: 10.1038/sj.eye.6702662. [DOI] [PubMed] [Google Scholar]
- 65.Ganesh SK, Abraham S, Sudharshan S. Paradoxical reactions in ocular tuberculosis. J Ophthalmic Inflamm Infect. 2019;9:19. doi: 10.1186/s12348-019-0183-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Walker NF, Stek C, Wasserman S, Wilkinson RJ, Meintjes G. The tuberculosis-associated immune reconstitution inflammatory syndrome: Recent advances in clinical and pathogenesis research. Curr Opin HIV AIDS. 2018;13:512–21. doi: 10.1097/COH.0000000000000502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mehta S, Mansoor H, Khan S, Saranchuk P, Isaakidis P. Ocular inflammatory disease and ocular tuberculosis in a cohort of patients co-infected with HIV and multidrug-resistant tuberculosis in Mumbai, India: A cross-sectional study. BMC Infect Dis. 2013;13:225. doi: 10.1186/1471-2334-13-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nahid P, Mase SR, Migliori GB, Sotgiu G, Bothamley GH, Brozek JL, et al. Treatment of drug-resistant tuberculosis. An official ATS/CDC/ERS/IDSA clinical practice guideline [published correction appears in Am J Respir Crit Care Med 2020;201:500-1] Am J Respir Crit Care Med. 2019;200:e93–e142. doi: 10.1164/rccm.201909-1874ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lutfey M, Della-Latta P, Kapur V, Palumbo LA, Gurner D, Stotzky G, et al. Independent origin of mono-rifampin-resistant Mycobacterium tuberculosis in patients with AIDS. Am J Respir Crit Care Med. 1996;153:837–40. doi: 10.1164/ajrccm.153.2.8564140. [DOI] [PubMed] [Google Scholar]
- 70.Masur H, Brooks JT, Benson CA, Holmes KK, Pau AK, Kaplan JE, et al. Prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: Updated Guidelines from the Centers for Disease Control and Prevention, National Institutes of Health, and HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2014;58:1308–11. doi: 10.1093/cid/ciu094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Durnian JM, Naylor G, Saeed AM. Ocular syphilis: The return of an old acquaintance. Eye (Lond) 2004;18:440–2. doi: 10.1038/sj.eye.6700687. [DOI] [PubMed] [Google Scholar]
- 72.Lee SY, Cheng V, Rodger D, Rao N. Clinical and laboratory characteristics of ocular syphilis: A new face in the era of HIV co-infection. J Ophthalmic Inflamm Infect. 2015;5:56. doi: 10.1186/s12348-015-0056-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Morshed MG, Singh AE. Recent trends in the serologic diagnosis of syphilis. Clin Vaccine Immunol. 2015;22:137–47. doi: 10.1128/CVI.00681-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Müller M, Ewert I, Hansmann F, Tiemann C, Hagedorn HJ, Solbach W, et al. Detection of Treponema pallidum in the vitreous by PCR. Br J Ophthalmol. 2007;91:592–5. doi: 10.1136/bjo.2006.110288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gordon LK, Danesh-Meyer H. Neuro-ophthalmic manifestations of HIV infection. Ocul Immunol Inflamm. 2020:1–9. doi: 10.1080/09273948.2019.1704024. doi: 101080/0927394820191704024. [DOI] [PubMed] [Google Scholar]
- 76.Ananth JV, Sudharshan S, Selvakumar A, Devaleenal BJ, Kalaivani K, Biswas J. Idiopathic intracranial hypertension associated with anaemia, secondary to antiretroviral drug in a human immunodeficiency virus positive patient. Indian J Ophthalmol. 2018;66:168–9. doi: 10.4103/ijo.IJO_592_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jeyaraman VA, Sudharshan S, Selvakumar A, Bassi S, Noronha OV, Selvamuthu P, et al. Isolated cortical blindness without simultaneous neurological involvement in progressive multifocal leukoencephalopathy in a patient with human immune deficiency virus infection. J Ophthalmic Inflamm Infect. 2013;3:3. doi: 10.1186/1869-5760-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Curi AL, Machado DO, Heringer G, Campos WR, Orefice F. Ocular manifestation of cat-scratch disease in HIV-positive patients. Am J Ophthalmol. 2006;141:400–1. doi: 10.1016/j.ajo.2005.08.072. [DOI] [PubMed] [Google Scholar]
- 79.Dhasmana DJ, Dheda K, Ravn P, Wilkinson RJ, Meintjes G. Immune reconstitution inflammatory syndrome in HIV-infected patients receiving antiretroviral therapy: Pathogenesis, clinical manifestations and management. Drugs. 2008;68:191–208. doi: 10.2165/00003495-200868020-00004. [DOI] [PubMed] [Google Scholar]
- 80.Testi I, Agarwal A, Agrawal R, Mahajan S, Marchese A, Miserocchi E, et al. Drug-induced uveitis in HIV patients with ocular opportunistic infections. Ocul Immunol Inflamm. 2019:1–7. doi: 10.1080/09273948.2019.1691240. doi: 101080/0927394820191691240. [DOI] [PubMed] [Google Scholar]
- 81.Tseng AL, Walmsley SL. Rifabutin-associated uveitis. Ann Pharmacother. 1995;29:1149–55. doi: 10.1177/106002809502901114. [DOI] [PubMed] [Google Scholar]
- 82.London NJ, Garg SJ, Moorthy RS, Cunningham ET. Drug-induced uveitis. J Ophthalmic Inflamm Infect. 2013;3:43. doi: 10.1186/1869-5760-3-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dodi F, Alessandrini A, Camera M, Gaffuri L, Morandi N, Pagano G. Stevens-Johnson syndrome in HIV patients treated with nevirapine: Two case reports. AIDS. 2002;16:1197–8. doi: 10.1097/00002030-200205240-00022. [DOI] [PubMed] [Google Scholar]
- 84.Whitcup SM, Butler KM, Caruso R, de Smet MD, Rubin B, Husson RN, et al. Retinal toxicity in human immunodeficiency virus-infected children treated with 2',3'-dideoxyinosine. Am J Ophthalmol. 1992;113:1–7. doi: 10.1016/s0002-9394(14)75744-7. [DOI] [PubMed] [Google Scholar]
- 85.Sen P, Sudharshan S, Banerjee A, Dhami A. Clinical and electrophysiological characteristics of Efavirenz-induced macular toxicity. GMS Ophthalmol Cases. 2020;10:Doc08. doi: 10.3205/oc000135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Papavasileiou E, Younis S, Zygoura V, Quijano C, Jackson TL. Ritonavir-associated toxicity mimicking retinitis pigmentosa in an HIV-infected patient on highly active antiretroviral therapy. Retin Cases Brief Rep. 2017;11:306–9. doi: 10.1097/ICB.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 87.Priya D, Sudharshan S, Biswas J. Management of a rare presentation of Vogt-Koyanagi-Harada disease in human immunodeficiency virus/acquired immunodeficiency disease syndrome patient. Indian J Ophthalmol. 2017;65:413–6. doi: 10.4103/ijo.IJO_544_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sherif M, Leon L, Clerc O, Guex-Crosier Y. Severe idiopathic posterior scleritis in a patient with HIV. Klin Monbl Augenheilkd. 2017;234:571–4. doi: 10.1055/s-0042-122442. [DOI] [PubMed] [Google Scholar]
- 89.Cordero-Coma M, Salazar-Méndez R, Yilmaz T. Treatment of severe non-infectious uveitis in high-risk conditions (Part 2): Systemic infections; management and safety issues. Expert Opin Drug Saf. 2015;14:1353–71. doi: 10.1517/14740338.2015.1061992. [DOI] [PubMed] [Google Scholar]
- 90.Dennehy PJ, Warman R, Flynn JT, Scott GB, Mastrucci MT. Ocular manifestations in pediatric patients with acquired immunodeficiency syndrome. Arch Ophthalmol. 1989;107:978–82. doi: 10.1001/archopht.1989.01070020040025. [DOI] [PubMed] [Google Scholar]
- 91.Biswas J, Kumar AA, George AE, Madhavan HN, Kumarasamy N, Mothi SN, et al. Ocular and systemic lesions in children with HIV. Indian J Pediatr. 2000;67:721–4. doi: 10.1007/BF02723926. [DOI] [PubMed] [Google Scholar]
- 92.Esposito S, Porta A, Bojanin J, Gualtieri L, Cesati L, Vismara E, et al. Effect of highly active antiretroviral therapy (HAART) on the natural history of ocular manifestations in HIV-infected children. Eye (Lond) 2006;20:595–7. doi: 10.1038/sj.eye.6702189. [DOI] [PubMed] [Google Scholar]
- 93.Agarwal S, Srinivasan B, Iyer G, Sudharshan S, Kalaivani K. Vernal keratoconjunctivitis in human immunodeficiency virus-The possible role of T-helper 1-T-helper 2 shift. Indian J Ophthalmol. 2018;66:1004–6. doi: 10.4103/ijo.IJO_76_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rewri P, Sharma M, Lohan A, Singh D, Yadav V, Singhal A. Practice pattern of cataract surgeons when operating on seropositive patients. Indian J Ophthalmol. 2019;67:335–9. doi: 10.4103/ijo.IJO_1437_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kempen JH, Sugar EA, Lyon AT, Lewis RA, Jabs DA, Heinemann MH, et al. Risk of cataract in persons with cytomegalovirus retinitis and the acquired immune deficiency syndrome. Ophthalmology. 2012;119:2343–50. doi: 10.1016/j.ophtha.2012.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Antiretroviral Therapy Guidelines for HIV-Infected Adults and Adolescents Including Post-exposure Prophylaxis. Available from: https://lmsnacogovin/frontend/content/1%20Antiretroviral%20Therapy%20Guidelines%20for%20HIVInfected%20Adults%20and%20Adolescents%20Including%20Post-exposurepdf . Last cited on 2017 May 03.


