Abstract
Scleritis is a rare painful ocular disorder, associated with severe ocular pain and tissue destruction. Although a majority of these cases are immune mediated and at least half of these are associated with systemic immune-mediated diseases, a smaller minority are due to infections of the sclera. The two conditions closely mimic each other, and a thorough knowledge of the subtle differences is necessary in order to reach a timely diagnosis. Diagnostic delay can lead to a poor outcome both due to the destruction caused by the uncontrolled infection and also due to propagation of the infection with the use of corticosteroids which may have been started for presumed immune mediated scleritis. In this review, we present the clinical features, etiological agents, and the differentiating features between immune and infectious scleritis. We also present diagnostic and management guidelines for managing scleral infection.
Keywords: Fungal scleritis, immune mediated scleritis, infectious scleritis, management of infectious scleritis, scleral debridement, tubercular scleritis
Scleritis is a painful, chronic, destructive inflammatory disease of the sclera that may be associated with a systemic disease or infection.[1]
Classification
Non-infectious scleritis: The classification is based on the clinical appearance, etiology and anatomical location. The earliest classification was proposed by Watson and Hayreh which divides scleritis into anterior and posterior forms. Anterior scleritis is further divided into diffuse, nodular, necrotizing with inflammation (necrotizing), and necrotizing without inflammation (scleromalacia perforans).[2] In 1991, McCluskey et al. published a grading system based on clinical signs.[3] More recently, Sen et al. reclassified the disease based on standardized digital photographs to provide a more objective way of classification.[4]
The initial presentation of infectious scleritis is often similar to autoimmune scleritis, and differentiation is a challenge without relevant laboratory investigations. The importance in differentiating between the two processes is that although immunosuppressives are the mainstay for immune mediated scleritis, antimicrobials are the therapy of choice for infectious cases. Needless to state, the use of immunosuppressive therapy alone in infectious causes will lead to worsening of the condition.[5]
Infectious scleritis This is classified as follows
Exogenous scleritis: post-traumatic and post-surgical infections and extension from contiguous infections, such as keratitis
Endogenous scleritis: this entity is less frequent and can mimic non-infectious diffuse, nodular, or necrotizing scleritis. Scleritis associated with systemic infections such as syphilis and tuberculosis fall into this category.
Prevalence of Infectious Versus Non-Infectious Scleritis.
The prevalence of non-infectious scleritis depends on multiple factors including race, geographical location and gender.[6,7,8] The incidence of all scleritis in the Western world is reported as 3.4 per 100,000 person-years with an annual prevalence ratio of 5.2 per 100,000 persons.[6] In a study from Hawaii, incidence rates of 4.1 per 100 000 person-years was reported.[7] In a study from India, 42/235 (17.87%) patients who presented with scleritis were diagnosed to have an infection.[9]
Various studiesfrom Western literature report 5-10%[10] incidence of infectious etiology as compared to about 17% in the Indian study.[9] The prevalence of infectious etiology therefore appears to correlate with the geographical location and livelihood patterns of the population. In developing countries with agriculture as the major occupation, microbial scleritis has a higher incidence due to increased rate of trauma.[8,9,10,11]
Etiology of Scleritis
Non-infectious scleritis
Around 30 to 50% of this type of scleritis is associated with underlying autoimmune disease.[12,13,14] Within the non-infectious universe, several types of diseases, including immune-mediated disease, medication-induced as well as miscellaneous entities can cause scleritis [Table 1]. The challenge for the ophthalmologist is to diagnose and treat promptly any underlying systemic disorder, some of them being life threatening, in order to prolong survival while preventing long-term ocular complications. Around 15–59% of patients may present with scleritis as the first manifestation of a systemic immune-mediated disease.[15,16,17]
Table 1.
Classification of noninfectious diseases associated with scleritis
| 1. Associated with connective tissue diseases and other inflammatory conditions in which vasculitis may occur |
| Rheumatoid arthritis |
| Systemic lupus erythematosus |
| Relapsing polychondritis |
| HLA-B27 + without spondyloarthropathy |
| Ankylosing spondylitis |
| Reactive arthritis |
| Psoriatic arthritis |
| Arthritis and inflammatory bowel disease |
| Antiphospholipid syndrome |
| 2. Associated with vasculitic diseases |
| Granulomatosis with polyangiitis |
| Allergic granulomatous angiitis (Churg-Strauss syndrome) |
| Polyarteritis nodosa |
| IgA vasculitis |
| Takayasu×s arteritis |
| Giant cell arteritis |
| Behçet×s disease |
| Cogan×s syndrome |
| Hypocomplementeric urticarial vasculitis |
| 3. Medication-induced |
| Biphosphonates: pamidronate, alendronate, risedronate, zoledronate, ibandronate, |
| Anticonvulsants: topiramate |
| Biologics: etanercept |
| Anticancer immunotherapy: nivolumab/cabiralizumab |
| 4. Miscellaneous |
| Atopy |
| Rosacea |
| Gout |
| Foreign body granuloma |
| Chemical injury |
Rheumatoid arthritis (RA) and granulomatosis with polyangiitis (GPA) are the two common disease associated with scleritis.[5,16] Scleritis in GPA is often necrotizing and is a severe disease that can lead to permanent visual loss.[16,18] Scleritis in spondylo-arthropathies or in systemic lupus erythematosus (SLE) is usually a more benign and self-limiting condition, whereas scleritis in RA and relapsing polychodritis (RP) can range from mild to severe.[16] GPA tends to progress rapidly whereas RA has an insidious nature of progression.[19]
Other less commonly associated autoimmune conditions include inflammatory bowel disease, sarcoidosis, Vogt Koyanagi Harada disease, Cogan's syndrome, Takayasu disease and polyarteritis nodosa, carcinoma of lung and lymphoma[15] and drug induced scleritis due to bisphosphonates and topiramate.[20]
Surgically induced necrotizing scleritis (SINS), though rare, is a well-recognized entity and has been reported in cases of excessive conjunctival manipulation and episcleral vessel cautery, such as pterygium or extracapsular cataract extraction surgery. Studies show that upto 90% of such cases may have an undiagnosed systemic autoimmune condition. Surgically induced diffuse scleritis is also a rare iatrogenic entity in eyes undergoing multiple ocular surgeries.
Infectious scleritis
The properties of the sclera viz. resilient, avascular and compact structure, with low metabolic activity, and covered by the overlying episclera and conjunctiva, make it relatively impermeable to infection. A breach of these barriers can lead to microorganisms invading the sclera. Common predisposing factors for scleral infection include[21]
Ocular trauma
Contiguous spread from the cornea in microbial keratitis or in infectious endophthalmitis
Recent ocular surgery or after pterygium surgery (need not be recent)
Use of antimetabolites such as mitomycin C, local radiotherapy
Systemic immunosuppressed conditions such as Human Immunodeficiency Virus (HIV) infection, diabetes, or systemic immunosuppression
Debilitating ocular diseases such as herpes simplex virus (HSV) or varicella zoster virus (VZV) recurrent keratitis or dry eye
Chronic use of topical corticosteroids.
The two pathogenic mechanisms involved in the development of infectious scleritis[22] are:
Direct invasion of replicating organisms with the destruction of the tissue, and
Immune reactions triggered by the infective agent.
Histopathological Findings to Differentiate Infectious versus Non-Infectious Scleritis
Pathologically, scleritis is an inflammatory process occurring in the avascular extracellular matrix of the sclera. In non-infectious scleritis, scleral biopsy is rarely obtained for diagnostic purposes as it might worsen the inflammation and threaten the stability of the globe. Hence most such samples are obtained from painful blind eyes or when malignancy or infection is suspected or accidental detection during autopsy.[23]
Rao et al. reported two large studies on the histopathology of scleritis in 9 scleral biopsies and 87 eyes either enucleated or received at autopsy.[24] They described three types of inflammatory process. The first two groups showed necrotic changes, of which one group already had microbiologically proven infectious etiology and therefore necrosis was expected. The second group had autoimmune etiology, but still showed necrosis of collagen with surrounding neutrophils and palisading histiocytes, but no evidence of infection. There were no disease specific changes noted in the biopsies. In these specimens, few loci of vasculitis and giant cell presence were also seen.
In the third group, defined as idiopathic scleritis, there was absence of necrosis with features of chronic inflammation, such as lymphocytes, plasma cells and histiocytes. Granulation tissue and fibrosis was also occasionally found. More recently, some of these cases have been found to be related to IgG4 positive diseases.[25]
Therefore, histopathological examination can offer some evidence towards the etiology, at least to help differentiate infectious versus non-infectious etiologies when typical features are not seen. However, this classification system does not take into account certain disease processes such as Herpes zosterscleritis, where the infectious etiology is accompanied by zones of granulomatous inflammation as seen in immune-mediated injury.[24,26] Moreover, not all infectious scleritis cases show necrotic changes.
Clinical Features
Non-infectious scleritis: Clinical features
Clinical signs and symptoms at presentation are variable because they depend on the degree and site of inflammation.
Pain: The characteristic symptom of scleritis is pain which may have insidious onset and severe intensity and is often resistant to analgesics. The pain is often not localized to the eye but frequently radiates to involve the forehead, brow, ear, face or jaw, and can be severe enough to awaken the patient at night. It may be triggered by touching the eye or temple or by eye movements. Patients with necrotizing scleritis often present in extreme discomfort. The only exception being scleromalacia perforans, which is characterized by an almost lack of pain symptoms.
Nodules: Nodular anterior scleritis presents with a nodule (or nodules) that is firm, immobile, and tender to palpation. These nodules can be large, usually located a few millimeters behind the limbus, and do not show pus points. Examination in an established case reveals white, avascular areas of sclera and conjunctiva, with surrounding scleral edema and congestion. Uveal tissue may appear as the overlying sclera becomes thin and translucent. A staphyloma will result when bulging develops in the presence of a thin sclera.
Posterior scleritis: May be difficult to diagnose unless accompanied by anterior signs of inflammation.[27] Patients may complain of loss of vision, pain, or diplopia. Posterior segment findings include optic nerve edema, serous retinal detachment, macular edema, annular ciliochoroidal detachment and choroidal thickening, mass and folds, all commonly associated with visual loss.[28]
Infectious scleritis: Clinical features
The clinical symptoms and signs of infectious and immune mediated scleritis often overlap and the appearance may be identical to noninfectious diffuse, nodular, or necrotizing scleritis. The challenge lies in differentiating infectious scleritis from the more common autoimmune scleral inflammation. Table 2 describes the differentiating features between infectious and non-infectious scleritis.
Table 2.
Differentiating features between infectious and non-infectious scleritis
| Infectious scleritis | Non-infectious scleritis | |
|---|---|---|
| Etiopathogenesis | Direct invasion of the pathogenic organisms including bacteria, fungi, viruses and protozoans | Connective tissue disorders |
| Rheumatoid Arthritis | ||
| Autoimmune response to microbes | Systemic Lupus Erythematosus | |
| Post-surgical and post traumatic infection | Relapsing Polychondritis | |
| Spread from contiguous structures | Systemic Vasculitis | |
| Granulomatosis with Polyangiitis | ||
| Microscopic Polyangiitis | ||
| Polyarteritis Nodosa | ||
| Churg Strauss Syndrome | ||
| Key clinical features | Purulent exudates, scleral ulcers, scleral abscesses, and scleritis associated with hypopyon. | Not associated with pus/abscesses. Diffuse/nodular tender congestion of deep episcleral vessels with oedema of sclera |
| Investigations | Culture and staining | Biopsy is contraindicated |
| Tissue biopsy | Antinuclear antibody | |
| Mantoux test | Anti-neutrophil cytoplasmic antibody | |
| Syphilis serology | Rheumatoid factor | |
| Treatment | Anti-microbial therapy. | Topical and systemic corticosteroids |
| Role of steroids is controversial/contra indicated | Immunosuppressive agents |
The salient features for infectious scleritis are discussed under the following headings:
Mode of onset
Course of the disease
Clinical examination
Response to immunosuppressants.
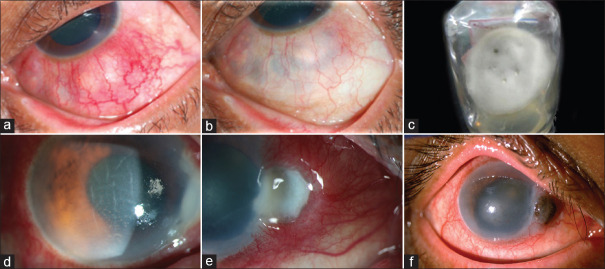
Mode of onset: The presentation, natural history and course depend on the precipitating cause. In infectious exogenous scleritis, this is readily apparent, for example obvious concurrent keratitis [Fig. 1a] or recent trauma with organic matter, or previous ocular surgery with acute onset of symptoms.[8,11,29,30,31] The latent period between trauma and onset inflammation can be shorter for post-traumatic compared to post-surgical cases,[8,30] perhaps due to the expected higher load of the infectious agent in trauma. In surgical cases, the commonest reported association is with pterygium surgery [Fig. 1b].[32,33,34] Use of extensive cautery, excessive scleral dissection, bare sclera technique and the use of antimetabolites such as mitomycin C or beta irradiation have been postulated to lead to altered local immunity.[35,36,37] Post-surgical infectious scleritis need to be differentiated from surgically induced necrotizing scleritis (SINS), the latter having a longer latent period.[38,39]
Figure 1.

(a) Case of fungal keratitis following history of trauma with vegetative matter one months ago, a scleral nodule is noted. (b) A case of post-pterygium and cataract surgery with scleral abscess nasally, microbiology revealed multi-drug resistant pseudomonas aeroginosa which was treated with topical and intravenous colistin. After multiple surgical interventions, the patient could recover vision of 20/320. (c) Ulcerated conjunctiva and a focus of scleral necrosis in a case of Pseudomonas aeruginosa, responded to fluroquinolones. (d) Yellowish appearance of nodular lesion with underlying suppuration. (e) Multiple small nodules are seen in this case of bacterial scleritis. (f) Fungal scleritis with multiple infective nodules noted after partial response to antifungals, note that the lesions are located 4 mm away from the limbus in a girdle-shaped fashion
Course of the disease: Immune mediated scleritis has a protracted course in accordance with the underlying systemic condition. When the systemic disease is in remission, the scleritis usually wanes.[11] The median time to resolution after starting treatment has been found to be longer for infectious scleritis.[40] Primarily, the virulence of the causative organism influences the course of the disease. Fastidious microorganism such as non-tubercular Mycobacteria, Nocardia sp. or fungi can present as indolent infection.[8,38,41,42,43,44,45,46,47] In contrast, Pseudomonas sp, Staphylococcal sp or viral infections have a shorter course of disease.[11,29,30,48,49,50,51,52,53]
Clinical examination: Immune-mediated scleral lesion have a dense purplish hue with superficial conjunctival congestion.[1,2] In less obvious cases, where the disease closely mimics non-infectious nature, a scleral nodule with slow progression not responding to corticosteroid therapy is noted.[11,39,47] In the more obvious cases, the overlying conjunctiva may be intact or ulcerated [Fig. 1c]. Necrotizing scleritis is the most common presentation of infectious scleritis, with yellowish or reddish hue of the nodule due to underlying suppuration [Fig. 1d]. Subconjunctival abscesses ranging from multiple small [Fig. 1e] to large lesions with mucopurulent discharge noted in some cases. Concomitant uveitis and/or keratitis may appear, or keratitis may be the initial disease with spread to sclera. Occasionally, multiple nodules may appear over the course of the disease which may coalescence and lead to scleral necrosis [Fig. 1f]. Such nodules are seen about 4-5 mm from the limbus in a circumferential pattern. Spread of lesions to contiguous structures is an indication of infectious cause.[41,42,43,51,52] Hypopyon has been strongly associated with infectious scleritis.[8] Once the lesions heal, a fibrous tissue band may be noted with scleral thinning indicating previous infectious etiology, unlike immune lesions which heal with only scleral thinning.
Some of the pathognomonic features of infection are:
Purulent exudates-
Conjunctival ulceration and slough
Visible pus points or scleral abscesses
Presence of scleritis lesion, associated with hypopyon or keratic precipitates.
Endogenous infectious scleritis may appear similar to non-infectious scleritis, necessitating a careful history, review of systems, physical examination, and laboratory investigations. Sometimes it would be considered as a diagnosis of exclusion and therapeutic trial would be the ultimate test (for example in presumed tubercular scleritis)
Response to corticosteroids and immunosuppressants: As corticosteroids and immunosuppressants reduce the inflammatory process, the acute features such as pain and congestion of an infectious nodule can be masked whilst on these drugs.[11] This leads to diagnostic delay while allowing the organism to proliferate. An initial apparent response followed by subsequent worsening of the infection when the patient has been started on immunosuppressants alone especially topical corticosteroids should alert the clinician to the possibility of an infectious etiology [Fig. 2a-d].[54,55]
Figure 2.

(a) Worsening of scleritis after injection of posterior subtenon triamconolone in a 48-year-old female patient with history of presumed recurrent episcleritis. The residual depot is noted. (b) Multilobulated nodular congested lesion are present nasally. (c) Picture shows improvement three weeks post-deroofing and excision of the depot and starting antibiotics for gram positive cocci and topical steroids were started. (d) Resolution of the infection at 2 months follow up
Types of Infectious Scleritis
Table 3 lists the classification of infectious organisms implicated in scleritis.
Table 3.
Classification of common infectious organisms in scleritis
| Organism | Sub-type |
|---|---|
| Bacteria | Gram-positive cocci |
| Gram-negative rods | |
| Mycobacteria | |
| Nontuberculous mycobacteria | |
| Mycobacterium tuberculosis | |
| Spirochetes | |
| Treponema pallidum | |
| Borrelia burgdorferi | |
| Actinomycetes | |
| Nocardia asteroides | |
| Fungi | Filamentous fungi |
| Dimorphic fungi | |
| Viruses | Herpes zoster |
| Herpes simplex type I | |
| Parasites | Acanthamoeba |
| Toxoplasma gondii | |
| Toxocaracanis |
Viral Scleritis
The herpes family including varicella zoster virus (VZV) and herpes simplex virus type-1 (HSV-1) are most frequent to cause scleritis. Other viruses such as Cytomegalovirus and Epstein Barr virus have also been implicated[56,57,58,59,60]
Herpes zoster scleritis is the most common cause of infectious scleritis.[61,62] As keratitis and anterior uveitis are often associated with herpetic scleritis, the detection of unilateral sclerokeratitis or sclerouveitis should raise the suspicion of herpetic scleritis and a therapeutic trial of antivirals can be considered
Zoster scleritis presents as painful, persistent, circumscribed nodules with translucent areas, with the risk of perforation or staphyloma formation.[5] Scleritis may occur months or years after the onset of VZV infection. A careful review of past history and examination of the face for pigmented scars would help clinch the diagnosis of herpes zoster scleritis. Reduced corneal sensation in the affected area and sectorial iris atrophy are other helpful diagnostic indicators
As the scleritis in herpes zoster is a viral-induced immune-mediated manifestation, methods to detect the virus such as Giemsa staining, immunofluorescence techniques, electron microscopy studies, and cultures from involved scleral tissue have been attempted but have been reported as negative for evidence of VZV[5]
The diagnosis in HSV anterior scleritis is challenging, as the condition mimics nodular immune mediated scleritis as it can occur without corneal involvement. The lack of improvement with immunosuppressants and resolution only on starting anti-viral therapy, presence of corneal scars are clinical indicators for viral disease.
Bacterial scleritis
Pseudomonas aeruginosa is the most common cause of microbial scleritis reported in Western literature; as high as in 51–81% of cases.[31,33,63] It is often associated with primary corneal infection and subsequent scleral extension or in a compromised host, prior ocular surgery such as pterygium surgery[33]
Streptococcus pneumoniae scleritis also has been described as an extension of corneal infection or after pterygium removal followed by β-irradiation or mitomycin-C[64]
In scleral buckle surgery, apart from Pseudomonas infection, involvement of methicillin resistant Staphylococcus Aureu (MRSA) is also reported.[8,11,40,41]
Mycobacterial scleritis
Non-tuberculous Mycobacterial Scleritis (NTM)
NTM can occur more commonly in in immunosuppressed individual.[29,30] The most common NTM causing scleritis is M. chelonae, a rapid-growing Mycobacterium which may be associated with minor office ophthalmic procedures, or abscesses following intramuscular injections in immunocompromised patient[65]
Scleritis also may be caused by M. marinum, a slow-growing Mycobacterium, that is often linked with skin diseases.[66] NTM scleritis has also been reported following scleral buckle surgery and pterygium excision[65]
These microbes are difficult to isolate by conventional laboratory techniques and Ziehl-Neelsen stain shows the presence of acid-fast bacilli and culture on Löwenstein-Jensen culture medium at 30°C yields the organisms
Therapy for mycobacterial infection includes topical Amikacin eye drops (2.5% to 5%), and oral rifampicin, clarithromycin or doxycycline in combination. The treatment must last from 4 weeks to 6 months after the resolution of the clinical signs. In cases with scleral abscesses, surgical debridement is recommended
Differential diagnosis of infectious scleritis with or without keratitis must include NTM, mainly if the scleritis occurs following either minor office ophthalmic procedures or ocular injuries associated with soil or contaminated water.
Tuberculous scleritis
Although the incidence of pulmonary and extra-pulmonary tuberculosis has decreased in developed countries since the last century, infection by M. tuberculosis (MTB) still remains a major medical problem in developing countries like India. In a multicentric study by Lane et al., presumed ocular tuberculosis accounted for 75% of infectious cases in India.[67] Tuberculous scleritis may be the result either of a direct MTB scleral invasion but more often is caused by an immune-mediated process[68,69,70] [Fig. 3a-c].
Figure 3.
(a) Shows a case of necrotizing scleritis in the RE in a 19-year-old girl, LE had diffuse scleritis. Extensive work up was done to rule out immune mediated pathology. Scrapings were negative. Mantoux test was positive. (b) shows improvement after starting oral Anti tubercular therapy and topical corticosteroids. (c) shows complete resolution at two months follow up. (d) shows show scleral abscess in a case of pulmonary tuberculosis. (e) High-resolution chest tomography shows tubercular lung cavitation
Diagnosis of tuberculous scleritis requires scleral biopsy which may show caseating granulomas with multinucleated giant cells and characteristic acid- fast bacilli. In view of paucibacillary nature of the infection, histopathology specimens may not reveal the bacteria but can show Langhans giant cells with caseating necrosis. Detection of the bacilli on Gram's stain and acid-fast stain of the scleral tissue samples will clinch the diagnosis
The patient should be thoroughly investigated to look for systemic involvement (primary focus) with Mantoux test, sputum examination and high resolution scan chest CT. Anti-tubercular therapy includes ethambutol (400 mg orally twice a day), isoniazid (300 mg orally once a day), rifampin (600 mg orally once a day), and pyridoxine (50 mg orally once a day) for 6–12 months.[70] [Fig. 3d] shows clinical photograph of a patient with tubercular scleral abscess and lung cavitation [Fig. 3e]
Immune-mediated tuberculous scleritis
This is considered to be a host immune response (Type IV hypersensitivity reaction) to cell wall components of MTB proteins. It is associated with phlyctenular keratitis, phlyctenular keratoconjunctivitis, and episcleritis
Although there is no direct mycobacterial invasion of sclera, immune-mediated tuberculous scleritis often occurs in conjunction with active systemic disease. Histologically, scleral specimens show a granulomatous reaction without acid-fast bacilli
Treatment includes both topical corticosteroids with meticulous tapering and systemic anti-tuberculous drugs. The anti-tuberculous treatment should be prolonged for more than 6 months due to the poor penetration of the drugs through sclera.
Nocardial scleritis
Nocardia is an gram-positive, weakly acid-fast staining actinomycetic bacterium which resembles fungi on smear examination. It causes opportunistic infections especially in immunosuppressed patients or after trauma[29]
In a retrospective study from India, Nocardia was found to be was the etiological organism in 24% of patients with infectious scleritis.[11] Fig. 4a shows a case of endogenous Nocardial scleral abscess. The patient also had lung cavitation [Fig. 4b].
Figure 4.

(a) RE shows Nocardial scleral abscess from endogenous spread. (b) lung shows cavitatory lesion which was the primary source of infection in the same patient. (c) Clinical photograph shows a localized nodule is noted with yellowish appearance, in case of injury with thorn. Microbiology revealed Nocardia sp. (d) Complete resolution two months later after debridement and therapy with Amikacin 2.5% eyedrops
The classical clinical presentation is chronic diffuse scleritis with nodules and/or necrotic abscesses [Fig. 4c and d]. In suspected cases, a direct smear shows Gram-positive, thin, beading and branching filaments. Also, the organism grows on blood agar and Lowenstein–Jensen media. The infection is controlled by surgical debridement of necrotic areas and topical amikacin drops (2.5% or 5%) accompanied by oral sulfamethoxazole–trimethoprim.[71]
Protozoal scleritis
Acanthamoeba and Toxoplasma infections of the sclera are uncommon.[72,73] Most cases of Acanthamoeba scleritis are presumed to be inflammatory response to the primary keratitis. Granulomatous inflammation with presence of the organism may be detected in scleral biopsies.
Fungal scleritis
Fungal scleritis is one of the most devastating types of infectious scleritis due the difficulty in controlling the infection and the potential to progress to destruction of the globe and visual loss. In cases reported from tropical and developing countries, fungal scleritis ranged from 5 to 38%[8,54]
The infection can originate either from exogenous contamination by trauma or ocular surgeries, or it can be endogenously transmitted in immunocompromised patients or via intravenous drug use. Debilitating ocular or systemic diseases, contact lens use, intravenous narcotic addiction, and chronic topical corticosteroid use increase the risk of fungal infection
Zia et al. in their retrospective case series on culture proven infectious scleritis showed that 25% were of fungal etiology.[74] The most common fungi that may cause scleritis are filamentous fungi. Aspergillus flavus is the most frequent fungus isolated, but several other species can cause infection[75,76,77,78]
In all cases of suspected fungal scleritis, microbiological diagnosis should be made before starting therapy. Fig. 5a and b shows the clinical photograph of fungal scleritis following trauma, which resolved after surgical debridement and treatment with topical and oral Voriconazole. Scedosporium species was grown in culture in this case [Fig. 5c].
Figure 5.
(a) LE shows nodular lesion, following trauma which turned out to be fungus. (b) Complete resolution after surgical debridement and treatment with topical and oral Voriconazole. (c) Culture on Sabouraud dextrose agar shows Scedosporium species. (d) A case of fungal scleritis presenting with corneal edema and keratic precipitates, initial diagnosis and treatment was for viral keratouveitis. (e) The scleral infection is noted at the limbus, repeat biopsy revealed fungal filaments. (f) The infected area perforated and healed by anterior staphyloma formation
Unusual organisms such as Mycobacterium, Acanthamoeba, or anaerobes can cause indolent scleritis or scleritis-keratitis with clinical picture resembling fungal etiology and therefore anti-fungal agents should not be empirically started as first line therapy in microbiologically negative cases.[5] Often, multiple biopsies are required to reach to the diagnosis [Fig. 5d-f]
Visual prognosis in fungal scleritis is often poor because of delayed diagnosis, poor penetration of the available small pool of antifungals agents into the avascular sclera, and non-availability of fungicidal agents
Topical corticosteroid agents are contraindicated in fungal scleritis because of the potential enhancement of fungal growth. Topical Cyclosporine A has been shown to have a suppressive effect on fungal growth when steroids cannot be used.[79] Oral voriconazole and intravenous caspofungin along with repeated surgical debridement of scleral abscesses have been helpful in some cases.[75]
Infectious Posterior Scleritis
Posterior scleritis itself is rare and the true incidence of infectious posterior scleritis is unknown. Clinically, patients can present with severe deep-seated radiating pain around the orbit. In acute zoster, the pain may be profound. Painful proptosis, painful and decreased extra-ocular movement and episcleral congestion may be noted. Diminution of vision secondary to serous retinal detachment, macular edema or disc edema may be noted.
Posterior scleritis may present as diffuse, nodular or necrotizing variety. A few cases may show anterior uveitis. Fundus examination would reveal the presence of serous retinal detachment with pockets of subretinal fluid mainly in the posterior pole [Fig. 1]. Sub-retinal mass (yellowish-brown elevation), choroidal folds, disc edema and vitritis are other features.[28]
Diagnosis
B-scan ultrasonography may reveal T-sign or scleral mass lesion which may represent the abscess. In some cases, only diffuse choroidal thickening with sub-tenons fluid may be picked up. Fundus Fluorescein Angiography is preferred over ICGA to clinch the diagnosis. Imaging modalities such as computerized tomogram (CT), magnetic resonance imaging (MRI and EDI-OCT can help us to rule out differentials.[80,81,82,83]
Etiology
Infectious posterior scleritis may be secondary to systemic or local infectious process, surgical or accidental trauma often with a retained intraocular foreign body (IOFB).
Systemic infections include the following
Tuberculosis: Scleral involvement in tuberculosis can present as nodular anterior or posterior scleritis.[84,85,86] In a case series by Majumdar et al., three patients had tuberculosis scleritis- one had bilateral necrotizing scleritis with posterior scleritis and two had nodular anterior scleritis.[86] Cheung and Chee[85] observed concurrent anterior uveitis in 75% of the patients with posterior scleritis. Paul L et al. have reported an unusual case of both anterior and posterior tuberculous non-necrotizing scleritis in a young Asian girl.[87]
Leprosy: Anterior nodular scleritis is common in lepromatous leprosy but much less common in the tuberculoid type. Necrotizing scleritis may occur secondary to scleral infection or an immune response. Posterior scleritis is rare in this entity.
Syphilis: Diffuse scleritis and rarely necrotizing scleritis maybe the presenting feature of secondary stage of syphilis. Nodular scleritis may occur in tertiary syphilis.
Lyme disease: scleritis is common but the time interval between initial disease and scleritis maybe prolonged.[88]
Herpes Simplex Virus: nodular posterior scleritis is a rare but known entity
Varicella Zoster Virus: is the commonest systemic infection associated with recurrent nodular scleritis. Necrotizing scleritis is less common but very resistant to treatment. Metastatic infectious abscesses- are rare in occurrence, can be seen in septicemia. Other causes: mumps, toxoplasmosis and toxocariasis
Local infections include the following-post-surgical such as following pterygium surgery,[89] suture abscess, scleral buckle infection or retained IOFBs following trauma
Work-Up for a Case of Scleritis
Diagnostic tests
Biopsy specimens
Scrapings: In cases where there is adjoining keratitis or an ulcerated scleral nodule with visible slough or plaque at the base of the ulcer, samples for microbiology can be taken by corneal or scleral scrapings at the slit lamp or in the minor operating room, with the help of a 15-no blade on a bard parker handle, or a simple nick with a needle and collection and inoculation of the purulent material. Care should be taken to avoid contamination by the lashes or the bare conjunctiva which would lodge commensals. Specimens obtained from cornea, conjunctiva and episclera should be stained for Grams, Giemsa and 1% acid fast staining (for detection of mycobacteria and actinomycetes) along with cultures on blood, chocolate and Sabouraud's dextrose agar.
Tissue Biopsy: Scleral or sclero-corneal biopsy is advised in the following settings of a suspected infectious scleritis:
This is often the initial investigative modality in most cases in a hospital set up with good microbiology access as the yield is better than simple scrapings
If smears and cultures of scrapings are negative after 48 hours and there is no clinical response
Scraping reports are available, but the patient is not improving on the initial broad-spectrum antimicrobial therapy
Large area of abscess needing drainage
When surgical intervention is anyway warranted for example removal of the inciting agent such as infected band, foreign body or depot steroid injections.
Technique of scleral biopsy: Tissue samples taken directly from within the depth of the infected site is a much better technique than scrapings or swabs to obtain adequate material for microbiological diagnosis. This procedure needs to be performed in the operating room under local anesthesia.
The procedure is described in brief as follows: a peritomy is performed to expose the underlying area of scleral infection. In the case of an abscess, the superficial sough and pus is allowed to drain and scrapings are taken from the base of the infected areas as well as the edges and smeared on at least two slides: 10% potassium hydroxide (KOH) mount, Grams, 1% acid fast or Geimsa stain, and inoculated on blood agar, chocolate agar, Sabourauds dextrose agar, thioglycolate broth and non-nutrient agar if acanthamoeba is suspected. In addition, a small 4 × 4 mm strip of partial thickness scleral tissue is excised and sent for histopathology. Additional material can also be sent for polymerase chain reaction (PCR) test for virology or for pan-fungal, eubacterial and mycobacterial detection, based on the diagnosis suspected and availability of laboratory facility for testing.
Serological investigations: Endogenous infectious scleritis should be ruled out by investigations for the primary focus of infection and should include appropriate serological testing, blood and urine cultures or other tissues as relevant.
Treatment Modalities
Medical therapy
While awaiting microbiological results, broad-spectrum fortified antimicrobial therapy, covering both Gram-positive and Gram-negative organisms should be started and the therapy should be modified based on the initial smear results and subsequent culture and sensitivity results. The reason for starting antibiotics is the fact that bacterial etiology is the commonest etiology for infection, rather than fungal, therefore empirical antifungals are best avoided. Oral and topical ciprofloxacin and that would cover Pseudomonas aeruginosa, gram-positive organisms, and Nocardia sp until tailored therapy based on culture results is feasible. A therapeutic response can be expected in 24 to 48 hours as antibiotics are bactericidal, and lack of response can enable the clinician to make corrections as necessary
It should also be noted that an initial apparent worsening can occur in bacterial cases due to the bactericidal effect of the drugs and release of endotoxins from dying bacteria. If microorganisms are not isolated despite repeated testing, and histopathological study reveals an inflammatory picture, auto-immune scleritis must be suspected, and therapy with oral corticosteroids, immunosuppressive, or biologics should be considered under antibiotic coverage as a last resort
There are proponents for starting empirical antifungal therapy with an agent such as Natamycin or Voriconazole in patients with trauma, particularly involving organic matter. However empirical antifungal therapy as a primary therapy has several pitfalls, firstly, irrespective of trauma history, bacterial infection by far the most common entity and therefore antifungals should be started only after a failure of; or worsening on antibiotics, and negative smears and cultures. Secondly, response to antifungals would take several days to weeks, and crucial time may be lost if the final etiology is altogether different. In addition, fungal scleritis is chronic and indolent and prone to recurrences therefore having concrete evidence of fungus via microbiology would embolden the clinician to continue with therapy for weeks together. Therefore, based on microbiological investigations, aggressive and prolonged topical and systemic anti-microbial therapy must be started
-
Role of topical corticosteroids: patients where corticosteroid therapy is started must be carefully monitored. Although tissue destruction is reduced, host immune response is also suppressed. In scleritis, this may be of benefit in selected indications:
- After prolonged and adequate anti-infectious therapy, once the infection shows good control but there is significant inflammation
- Fungal infection should be ruled out by more than one biopsy if the first is negative for all organism. (Also, repeat biopsies should be performed when mixed infections are suspected)
- If the histopathological study reveals an inflammatory microangiopathy
- In acanthamoeba keratitis with scleritis, oral corticosteroids are recommended as the scleritis component is immune-mediated.
Surgical therapy
Surgical intervention improves the chance of globe preservation but does not appear to improve the visual outcome as per published reports. This may also be because advanced cases require surgical intervention more often. If scleral necrosis is severe, progression is rapid, or if there are multifocal abscesses not responding to medical treatment, surgical debridement of scleral abscess and irrigation with either 2.5% betadine solution or with broad spectrum antibiotics or antifungals such as 2% voriconazole has been recommended.
These measure aid in reducing necrotic tissue and the infective load, thereby increasing drug penetration. The necrotic area is often found intraoperatively to be much larger than clinically judged by slit lamp examination. Wound irrigation with antibiotics or antifungals is advisable. Tectonic procedures such as amniotic membrane graft or tenon's patch graft or scleral graft and/or lamellar or penetrating keratoplasty with continued antibiotic coverage may be needed in cases of extensive scleral involvement with threat to globe tectonicity.
Masquerade Scleritis
Although rare, malignancies can masquerade as scleritis. Chrysanthi et al. reported two cases in which malignancy mimicked scleritis, thereby delaying the diagnosis.[90] Although not as the first differential diagnosis, treatment resistant scleritis should raise the suspicion of a malignant masquerade. Choroidal melanoma can initially manifest as episcleritis, uveitis, endophthalmitis, or panophthalmitis.[91] Nodulo-ulcerative form of ocular surface squamous neoplasia can mimic necrotising scleritis.[92]
Therefore, in order to avoid ocular morbidity or mortality from the underlying malignancy, early diagnosis and appropriate management are crucial. The ophthalmologist is able to diagnose early by harvesting tissue for histopathologic analysis in those instances in which the inflammation is atypical and/or fails to respond in the expected way to anti-inflammatory therapy.
Conclusion
There are several clinical clues to differentiate between infectious and immune mediated forms of scleritis. In the obvious cases, presence of systemic disease associated with scleritis make the diagnosis of immune mediated scleritis very simple. History of trauma or recent surgery with evolution of nodular and ulcerative type of scleritis will be easy to diagnose as infectious scleritis. However, the diagnostic dilemmas are for those case where the clinical picture is equivocal and there is no antecedent history in favor of either diagnosis. In these instances, subtle signs and response to therapy need to be used to come to a definite diagnosis regarding the etiology of the scleritis [Fig. 6].
Figure 6.
Scleritis Flow chart
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
For Somasheila I Murthy Hyderabad Eye Research Foundation.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
G S Naresh (formatting of photograph).
References
- 1.Watson PG. Doyne Memorial Lecture, 1982.The nature and the treatment of scleral inflammation. Trans Ophthalmol Soc U K. 1982;102:257–81. [PubMed] [Google Scholar]
- 2.Watson PG, Hayreh SS. Scleritis and episcleritis. Br J Ophthalmol. 1976;60:163–91. doi: 10.1136/bjo.60.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCluskey PJ, Wakefield D. Prediction of response to treatment in patients with scleritis using a standardized scoring system. Aust N Z J Ophthalmology. 1991;19:211–5. doi: 10.1111/j.1442-9071.1991.tb00663.x. [DOI] [PubMed] [Google Scholar]
- 4.Sen HN, Sangave AA, Goldstein DA, Suhler EB, Cunningham D, Vitale S, et al. A standardized grading system for scleritis. Ophthalmology. 2011;118:768–71. doi: 10.1016/j.ophtha.2010.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sainz de la Maza M, Tauber J, Foster CS. The Sclera. New York: Springer-Verlag; 2012. [Google Scholar]
- 6.Honik G, Wong IG, Gritz DC. Incidence and prevalence of episcleritis and scleritis in Northern California. Cornea. 2013;32:1562–6. doi: 10.1097/ICO.0b013e3182a407c3. [DOI] [PubMed] [Google Scholar]
- 7.Homayounfar G, Nardone N, Borkar DS, Vivien MT, Travis CP, Wayne TAE, et al. Incidence of scleritis and episcleritis: Results from the Pacific ocular inflammation study. Am J Ophthalmol. 2013;156:752–8. doi: 10.1016/j.ajo.2013.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ho YF, Yeh LK, Tan HY, Chen HC, Yeong-Fong Chen YF, Lin HC, et al. Infectious scleritis in Taiwan—A 10-year review in a tertiary-care hospital. Cornea. 2014;33:838–43. doi: 10.1097/ICO.0000000000000174. [DOI] [PubMed] [Google Scholar]
- 9.Reddy JC, Murthy SI, Reddy AK, Garg P. Risk factors and clinical outcomes of bacterial and fungal scleritis at a tertiary eye care hospital. Middle East Afr J Ophthalmol. 2015;22:203–11. doi: 10.4103/0974-9233.150634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sainz de la Maza M, Jabbur NS, Foster CS. Severity of scleritis and episcleritis. Ophthalmology. 1994;101:389–96. doi: 10.1016/s0161-6420(94)31325-x. [DOI] [PubMed] [Google Scholar]
- 11.Jain V, Garg P, Sharma S. Microbial scleritis: Experience from a developing country. Eye. 2009;23:255–61. doi: 10.1038/sj.eye.6703099. [DOI] [PubMed] [Google Scholar]
- 12.Okhravi N, Odufuwa B, McCluskey P, Lightman S. Scleritis. Surv Ophthalmol. 2005;50:351–63. doi: 10.1016/j.survophthal.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 13.McCluskey P, Wakefield D. Current concepts in the management of scleritis. Aust NZ J Ophthalmol. 1988;16:169–76. doi: 10.1111/j.1442-9071.1988.tb01206.x. [DOI] [PubMed] [Google Scholar]
- 14.Wakefield D, Girolamo ND, Thurau S, Wildner G, McCluskey P. Scleritis: Immunopathogenesis and molecular basis for therapy. Prog Retin Eye Res. 2013;35:44–62. doi: 10.1016/j.preteyeres.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Sainz de la Maza M, Molina N, Gonzalez-Gonzalez LA, Doctor PP, Tauber J, Foster CS. Clinical characteristics of a large cohort of patients with scleritis and episcleritis. Ophthalmology. 2012;119:43–50. doi: 10.1016/j.ophtha.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 16.Sainz de la Maza M, Foster CS, Jabbur NS. Scleritis associated with systemic vasculitic diseases. Ophthalmology. 1995;102:687–92. doi: 10.1016/s0161-6420(95)30970-0. [DOI] [PubMed] [Google Scholar]
- 17.Gu J, Zhou S, Ding R, Aizezi W, Jiang A. Chen J Necrotizing scleritis and peripheral ulcerative keratitis associated with Wegener's granulomatosis. Ophthalmol Ther. 2013;2:99–111. doi: 10.1007/s40123-013-0016-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carrasco MA, Cohen EJ, Rapuano CJ, Laibson PR. Therapeutic decision in anterior scleritis: Our experience at a tertiary care eye center. J Fr Ophthalmol. 2005;28:1065–9. doi: 10.1016/s0181-5512(05)81139-8. [DOI] [PubMed] [Google Scholar]
- 19.Cocho L, Gonzalez-Gonzalez LA, Molina-Prat N, Doctor P, Sainz-de-la-Maza M, Foster CS. Scleritis in patients with granulomatosis with polyangiitis (Wegener) Br J Ophthalmol. 2016;100:1062–5. doi: 10.1136/bjophthalmol-2015-307460. [DOI] [PubMed] [Google Scholar]
- 20.Fraunfelder FW, Fraunfelder FT. Adverse ocular drug reactions recently identified by the national registry of drug-induced ocular side effects. Ophthalmology. 2004;111:1275–9. doi: 10.1016/j.ophtha.2003.12.052. [DOI] [PubMed] [Google Scholar]
- 21.Pavesio C, editor. Scleritis. Cham: Springer International Publishing; 2017. [Google Scholar]
- 22.Ramenaden ER, Raiji VR. Clinical characteristics and visual outcomes in infectious scleritis: A review. Clin Ophthalmol. 2013;7:2113–22. doi: 10.2147/OPTH.S37809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hankins M, Margo CE. Histopathological evaluation of scleritis. J Clin Pathol. 2019;72:386–90. doi: 10.1136/jclinpath-2018-205360. [DOI] [PubMed] [Google Scholar]
- 24.Rao NA, Marak GE, Hidayat AA. Necrotizing scleritis. A clinico-pathologic study of 41 cases. Ophthamology. 1985;92:1542–8. [PubMed] [Google Scholar]
- 25.Karim F, de Hoog J, Paridaens D. IgG4-related disease as an emerging cause of scleritis. Acta Ophthalmol. 2017;95:e795–6. doi: 10.1111/aos.13376. [DOI] [PubMed] [Google Scholar]
- 26.Mondino BJ. Discussion. Ophthalmology. 1985;92:1548–9. [Google Scholar]
- 27.McCluskey PJ, Watson PG, Lightman S, Haybittle J, Restori M, Branley M. Posterior scleritis: Clinical features, systemic associations, and outcome in a large series of patients. Ophthalmology. 1999;106:2380–6. doi: 10.1016/S0161-6420(99)90543-2. [DOI] [PubMed] [Google Scholar]
- 28.Benson WE. Posterior scleritis. Surv Ophthalmol. 1988;32:297–316. doi: 10.1016/0039-6257(88)90093-8. [DOI] [PubMed] [Google Scholar]
- 29.Hodson KL, Galor A, Karp CL, Davis JL, Albini TA, Perez VL, et al. Epidemiology and visual outcomes in patients with infectious scleritis. Cornea. 2013;32:466–72. doi: 10.1097/ICO.0b013e318259c952. [DOI] [PubMed] [Google Scholar]
- 30.Sahu SK, Das S, Sharma S, Sahu K. Clinico-microbiological profile and treatment outcome of infectious scleritis: Experience from a tertiary eye care center of India. Int J Inflamm. 2012;2012:753–60. doi: 10.1155/2012/753560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin CP, Shih MH, Tsai MC. Clinical experiences of infectious scleral ulceration: A complication of pterygium operation. Br J Ophthalmol. 1997;81:980–3. doi: 10.1136/bjo.81.11.980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hsiao CH, Chen JJ, Huang SC, Ma H, Chen P, Tsai R. Intrascleral dissemination of infectious scleritis following pterygium excision. Br J Ophthalmol. 1998;82:29–34. doi: 10.1136/bjo.82.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang FC, Huang SP, Tseng SH. Management of infectious scleritis after pterygium excision. Cornea. 2000;19:34–9. doi: 10.1097/00003226-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Moriarty AP, Crawford GJ, McAllister IL, Constable IJ. Severe corneoscleral infection. A complication of beta irradiation scleral necrosis following pterygium excision. Arch Ophthalmol. 1993;111:947–51. doi: 10.1001/archopht.1993.01090070065021. [DOI] [PubMed] [Google Scholar]
- 35.Moriarty AP, Crawford GJ, McAllister IL, Constable IJ. Fungal corneoscleritis complicating beta-irradiation-induced scleral necrosis following pterygium excision. Eye. 1993:7:525–8. doi: 10.1038/eye.1993.114. [DOI] [PubMed] [Google Scholar]
- 36.Moriarty AP, Crawford GJ, McAllister IL, Constable IJ. Bilateral streptococcal corneoscleritis complicating beta irradiation induced scleral necrosis. Br J Ophthalmol. 1993;77:251–2. doi: 10.1136/bjo.77.4.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yamazoe K, Shimazaki-Den S, Otaka I, Hotta K, Shimazaki J. Surgically induced necrotizing scleritis after primary pterygium surgery with conjunctival autograft. Clin Ophthalmol. 2011;5:1609–11. doi: 10.2147/OPTH.S24885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cunningham MA, Alexander JK, Matoba AY, Jones DB, Wilhemus KR. Management and outcome of microbial anterior scleritis. Cornea. 2011;30:1020–3. doi: 10.1097/ICO.0b013e31820967bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ahn SJ, Oh JY, Kim MK, Lee JH, Wee WR. Clinical features, predisposing factors, and treatment outcomes of scleritis in the Korean population. Korean J Ophthalmol. 2010;24:331–5. doi: 10.3341/kjo.2010.24.6.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Basti S, Gopinathan U, Gupta S. Nocardial necrotizing scleritis after trauma. Cornea. 1994;13:274–5. doi: 10.1097/00003226-199405000-00015. [DOI] [PubMed] [Google Scholar]
- 41.Knox CM, Whitcher JP, Cevellos V, Margolis TP, Irvine AR. Nocardia scleritis. Am J Ophthalmol. 1997;123:713–4. doi: 10.1016/s0002-9394(14)71096-7. [DOI] [PubMed] [Google Scholar]
- 42.Seth RK, Gaudio PA. Nocardia asteroides necrotizing scleritis associated with subtenon triamcinolone acetonide injection. Ocul Immunol Inflamm. 2008;16:139–40. doi: 10.1080/09273940802140804. [DOI] [PubMed] [Google Scholar]
- 43.Moorthy RS, Valluri S, Rao NA. Nontuberculous mycobacterial ocular infection. Surv Ophthalmol. 2012;57:202–35. doi: 10.1016/j.survophthal.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 44.Smiddy WE, Miller D, Flynn HW., Jr Scleral buckle infections due to atypical mycobacteria. Retina. 1991;11:394–8. doi: 10.1097/00006982-199111040-00005. [DOI] [PubMed] [Google Scholar]
- 45.Pope J, Jr, Sternberg P, Jr, McLane NJ, Potts DW, Stulting RD. Mycobacterium chelonae scleral abscess after removal of a scleral buckle. Am J Ophthalmol. 1989;107:557–8. doi: 10.1016/0002-9394(89)90511-4. [DOI] [PubMed] [Google Scholar]
- 46.Kesen MR, Edwards DP, Rao NA. Atypical infectious nodular scleritis. Arch Ophthalmol. 2009;127:1079–80. doi: 10.1001/archophthalmol.2009.197. [DOI] [PubMed] [Google Scholar]
- 47.Brooks JGJ, Mills RAD, Coster DJ. Nocardial scleritis. Am J Ophthalmol. 1992;114:371–2. doi: 10.1016/s0002-9394(14)71811-2. [DOI] [PubMed] [Google Scholar]
- 48.Hessburg PC. Pseudomonas corneoscleral ulcers. Am J Ophthalmol. 1982;93:256. doi: 10.1016/0002-9394(82)90430-5. [DOI] [PubMed] [Google Scholar]
- 49.Huang SC, Lai HC, Lai IC. The treatment of Pseudomonas keratoscleritis after pterygium excision. Cornea. 1999;18:608–11. [PubMed] [Google Scholar]
- 50.Lee JE, Oum BS, Choi HY, Lee JS. Methicillin-resistant Staphylococcus aureus sclerokeratitis after pterygium excision. Cornea. 2007;26:744–6. doi: 10.1097/ICO.0b013e31804e45ba. [DOI] [PubMed] [Google Scholar]
- 51.Feiz V, Redline DE. Infectious scleritis after pars plana vitrectomy because of methicillin-resistant Staphylococcus aureus resistant to fourth-generation fluoroquinolones. Cornea. 2007;26:238–40. doi: 10.1097/01.ico.0000248383.09272.ee. [DOI] [PubMed] [Google Scholar]
- 52.Rich RM, Smiddy WE, Davis JL. Infectious scleritis after retinal surgery. Am J Ophthalmol. 2008;145:695–9. doi: 10.1016/j.ajo.2007.11.024. [DOI] [PubMed] [Google Scholar]
- 53.Murthy SI, Sati A, Sangwan VS. Infectious scleritis mimicking severe ocular inflammation: Atypical initial presentation? BMJ Case Rep. 2013;2013:bcr2013008686. doi: 10.1136/bcr-2013-008686. doi: 10.1136/bcr-2013-008686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Murthy SI, Reddy JC, Sharma S, Sangwan VS. Infectious Scleritis. Curr Ophthalmol Rep. 2015;3:147–57. [Google Scholar]
- 55.Gonzalez LAG, Molina-Prat N, Doctor P, Tauber J, Sainz de la Maza MT, Foster CS. Clinical features and presentation of infectious scleritis from herpes viruses: A report of 35 cases. Ophthalmology. 2012;119:1460–4. doi: 10.1016/j.ophtha.2012.01.033. [DOI] [PubMed] [Google Scholar]
- 56.Livir-Rallatos C, El-Shabrawi Y, Zatirakis P, Pellett PE, Stamey FR, Foster CS. Recurrent nodular scleritis associated with varicella zoster virus. Am J Ophthalmol. 1998;126:594–7. doi: 10.1016/s0002-9394(98)00120-2. [DOI] [PubMed] [Google Scholar]
- 57.Accorinti M, Abbouda A, Gilardi M, Zito R, Iannetti L. Cytomegalovirus-related scleritis. Ocul Immunol Inflamm. 2013;21:413–5. doi: 10.3109/09273948.2013.805787. [DOI] [PubMed] [Google Scholar]
- 58.Kamoi K, Mochizuki M. HTLV infection and the eye. Curr Opin Ophthalmol. 2012;23:557–61. doi: 10.1097/ICU.0b013e328358b9ec. [DOI] [PubMed] [Google Scholar]
- 59.Furukawa H, Hamada T, Nagaya K, Akiya S, Hamada T. A case of necrotizing scleritis associated with Epstein–Barr virus infection. Nihon Ganka Gakkai Zasshi. 1993;97:1337–42. [PubMed] [Google Scholar]
- 60.Loureiro M, Rothwell R, Fonseca S. Nodular scleritis associated with herpes zoster virus: An infectious and immune-mediated process Case. Reports in Ophthalmological Medicine. 2016 doi: 10.1155/2016/8519394. doi: 101155/2016/8519394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Raiji VR, Palestine AG, Parver DL. Scleritis and Systemic Disease Association in a Community-Based Referral Practice. Am J Ophthalmol. 2009;148:946–50. doi: 10.1016/j.ajo.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 62.Gonzalez-Gonzalez LA, Molina-Prat N, Doctor P, Tauber J, Sainz de la Maza M, Foster CS. Clinical features and presentation of infectious scleritis from herpes viruses. Ophthalmology. 2012;119:1460–4. doi: 10.1016/j.ophtha.2012.01.033. [DOI] [PubMed] [Google Scholar]
- 63.Ahmad S, Lopez M, Attala M, Galor A, Stanciu NA, Miller D, et al. Interventions and outcomes in patients with infectious Pseudomonas scleritis: A 10-year Pperspective. Ocular Immunol Inflamm. 2019;27:499–506. doi: 10.1080/09273948.2017.1372484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Altman AJ, Cohen EJ, Berger ST, Mondino BJ. Scleritis and streptococcus pneumoniae. Cornea. 1991:10:341–5. doi: 10.1097/00003226-199107000-00010. [DOI] [PubMed] [Google Scholar]
- 65.David DB, Hirst LW, McMillen J, Whitby M. Mycobacterium marinum keratitis: Pigmentation a clue to diagnosis. Eye. 1999;13:377–9. doi: 10.1038/eye.1999.98. [DOI] [PubMed] [Google Scholar]
- 66.Kheir WJ, Sheheitli H, Fattah MA, Hamam RN. Nontuberculous mycobacterial ocular infections: A systematic review of the literature? Biomed Res Int. 2015;2015:164989. doi: 10.1155/2015/164989. doi: 10.1155/2015/164989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lane J, Nyugen E, Lim L, Stawell R, Hodgson L, Ismail MAB, et al. Clinical features of scleritis across the Asia-Pacific region. Ocular Immunol Inflamm. 2019;27:920–6. doi: 10.1080/09273948.2018.1484496. [DOI] [PubMed] [Google Scholar]
- 68.Bloomfield SE, Mondino B, Gray GF. Scleral tuberculosis. Arch Ophthalmol. 1976;94:954–6. doi: 10.1001/archopht.1976.03910030482009. [DOI] [PubMed] [Google Scholar]
- 69.Agarwal A, Majumder PD. Tubercular posterior scleritis: A case report and review of literature. Indian J Ophthalmol. 2019;67:1362–5. doi: 10.4103/ijo.IJO_1942_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Murugan SB. Commentary: Tubercular posterior scleritis-Nuances in practice! Indian J Ophthalmol. 2019;67:1366–7. doi: 10.4103/ijo.IJO_695_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.da Cunha P, Juncal V, Carvalhaes CG, Leão SC, Chimara E, Freitas D. Nocardial scleritis: A case report and a suggested algorithm for disease management based on a literature review. Am J Ophthalmol Case Rep. 2018;10:1–5. doi: 10.1016/j.ajoc.2018.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Iovieno A, Gore DM, Carnt N, Dart JK. Acanthamoeba sclero- keratitis: Epidemiology, clinical features, and treatment outcomes. Ophthalmology. 2014;121:2340–7. doi: 10.1016/j.ophtha.2014.06.033. [DOI] [PubMed] [Google Scholar]
- 73.Kamath YS, Rathinam SR, Kawali A. Ocular toxoplasmosis associated with scleritis. Indian J Ophthalmol. 2013;61:295–7. doi: 10.4103/0301-4738.111130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pradhan Z, Jacob P. Infectious scleritis: Clinical spectrum and management outcomes in India. Indian J Ophthalmol. 2013;61:590–3. doi: 10.4103/0301-4738.121085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fincher T, Fulcher SFA. Diagnostic and therapeutic challenge of Aspergillus flavus scleritis. Cornea. 2007;26:618–20. doi: 10.1097/ICO.0b013e318033de67. [DOI] [PubMed] [Google Scholar]
- 76.Howell A, Midturi J, Sierra-Hoffman M, Carpenter J, Hurley D, Winn R. Aspergillus flavus Scleritis: Successful treatment with voriconazole and caspofungin. Med Mycol. 2005;43:651–5. doi: 10.1080/13693780500271772. [DOI] [PubMed] [Google Scholar]
- 77.Todokoro D, Hoshino J, Yo A, Makimura K, Hirato J, Akiyama H. Scedosporiumapiospermum infectious scleritis following posterior subtenon triamcinolone acetonide injection: A case report and literature review. BMC Ophthalmol. 2018;18:40. doi: 10.1186/s12886-018-0707-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.De Doncker RML, de Keizer RJW, Oosterhuis JA, Maes A. Scleral melting in a patient with conjunctival rhinosporidiosis. Br J Ophthalmol. 1990;74:635–7. doi: 10.1136/bjo.74.10.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sahu SK, Das S, Sahani D, Sharma S. Fungal scleritis masquerading as surgically induced necrotizing scleritis: A case report. J Med Case Reports. 2013;7:288. doi: 10.1186/1752-1947-7-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Diogo MC, Jager MJ, Ferreira TA. Am J Neuroradiol. 2016;37:2334–9. doi: 10.3174/ajnr.A4890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Murugan S B. Commentary: Posterior scleritis: Nuances to discern and handle effectively! Indian J Ophthalmol. 2018;66:1113–4. doi: 10.4103/ijo.IJO_639_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shields CL, Pellegrini M, Ferenczy SR, Shields JA. Enhanced depth imaging optical coherence tomography of intraocular tumors: From placid to seasick to rock and rolling topography--The 2013 Francesco Orzalesi Lecture. Retina. 2014;34:1495–512. doi: 10.1097/IAE.0000000000000288. [DOI] [PubMed] [Google Scholar]
- 83.Biswas J, Mittal S, Ganesh SK, Shetty NS, Gopal L. Posterior scleritis: Clinical profile and imaging characteristics. Indian J Ophthalmol. 1998;46:195–202. [PubMed] [Google Scholar]
- 84.Yadav S, Rawal G. Tubercular nodular episcleritis: A case report. J Clin Diagn Res. 2015;9:1–2. doi: 10.7860/JCDR/2015/15023.6335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cheung CM, Chee SP. Posterior scleritis in children: Clinical features and treatment. Ophthalmology. 2012;119:59–65. doi: 10.1016/j.ophtha.2011.09.030. [DOI] [PubMed] [Google Scholar]
- 86.Majumder PD, Ali S, George A, Ganesh S, Biswas J. Clinical profile of scleritis in children. Ocul Immunol Inflamm. 2018;25:1–5. doi: 10.1080/09273948.2017.1423333. [DOI] [PubMed] [Google Scholar]
- 87.Paul L, Agarwal M, Singh S, Katre P, Arora AS. Tuberculous scleritis in a young Asian Indian girl—A case presentation and literature review. J Ophthalmic Inflamm Infect. 2019;9:22. doi: 10.1186/s12348-019-0192-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Doreen K, Wenkel H. Posterior scleritis associated with Borrelia burgdorferi (Lyme disease) infection. Ophthalmology. 2002;109:143–5. doi: 10.1016/s0161-6420(01)00868-5. [DOI] [PubMed] [Google Scholar]
- 89.Taravella MJ, Johnson DW, Petty JG, Keyser RB, Foster CS, Ludberg BE. Infectious posterior scleritis caused by Pseudallescheria boydii: Clinicopathologic findings. Ophthalmology. 1997;104:1312–6. doi: 10.1016/s0161-6420(97)30142-0. [DOI] [PubMed] [Google Scholar]
- 90.Kafkala C, Daoud YJ, Paredes I, Foster CS. Masquerade scleritis. Ocul Immunol Inflamm. 2005;13:479–82. doi: 10.1080/09273940591004133. [DOI] [PubMed] [Google Scholar]
- 91.Fraser DJ, Jr, Font RL. Ocular inflammation and hemorrhage as initial manifestations of uveal malignant melanoma: Incidence and prognosis. Arch Ophthalmol. 1979;97:1482–6. doi: 10.1001/archopht.1979.01020020053012. [DOI] [PubMed] [Google Scholar]
- 92.Kaliki S, Freitag SK, Chodosh J. Nodulo-Ulcerative ocular surface squamous neoplasia in 6 patients: A rare presentation. Cornea. 2017;36:322–32. doi: 10.1097/ICO.0000000000001031. [DOI] [PubMed] [Google Scholar]