Abstract
Uveitis is a complex disorder including both infectious and non-infectious etiologies. Clinical diagnosis is a challenge because many diseases share common clinical signs. Laboratory support is crucial for confirming the clinical diagnosis. Laboratory diagnosis includes direct tests and indirect tests. For example smear, culture, and molecular diagnostics demonstrate the pathogens, hence they are direct tests. Immunologic tests employ an antigen to detect presence of antibodies to a pathogen, or an antibody to detect the presence of an antigen, of the pathogen in the specimens. The immunological tests used in laboratories are made by producing artificial antibodies that exactly “match” the pathogen in question. When these antibodies come into contact with a sample they bind to the matching pathogen if found in the sample. Hence they are grouped under indirect evidence. There are several investigations in uveitis to reach the confirmed diagnosis including microbiological, immunological, imaging and molecular diagnostic testing. In this section we will discuss immunological investigations of infectious and non-infectious uveitis.
Keywords: Infectious, investigations, non-infectious, novel infections, uveitis
Uveitis is an ocular condition wherein a single disease can present with myriad presentations, while a single presentation can be seen in varied diseases. Example: scleritis can be seen in an infectious disease like tuberculosis while can be part of an autoimmune disease too. In 70% of the uveitic conditions, a diagnosis can be reached with proper systemic/ocular history and the ophthalmologist's clinical acumen. A tailored laboratorial approach is needed for identification in rest of the cases [Table 1]. These investigations are also needed to confirm the diagnosis and to start the patient on treatment which may be poles apart.
Table 1.
Immunological tests in uveitis
| Uveitic entity | Disease type | Immunological tests |
|---|---|---|
| Infectious Uveitis | ||
| Bacterial disease | Tuberculosis | Mantoux Test, |
| Interferon-gamma release Assay (IGRA) 6 | ||
| QuantiFeron-Gold In-Tube & T-SPOT TB | ||
| Leprosy | Lepromin test | |
| Syphilis | Treponemal tests | |
| Non Treponemal tests | ||
| Leptospirosis | Microagglutination test, ELISA | |
| Lyme disease | ELISA | |
| Rickettsiae | ELISA Weil Felix test, | |
| Viral diseases | HIV | ELISA. Westren Blot |
| Dengue | ELISA, Plaque Reduction Neutralization test (PRNT) | |
| Chikungunya | ELISA, (PRNT) | |
| West Nile virus | ELISA, RT PCR | |
| Parasitic diseases | Toxoplasmosis | ELISA |
| Toxocariasis | ELISA | |
| Non-infectious Uveitis | ||
| Collagen vascular disease | Rheumatological disorders | |
| Juvenile idiopathic arthritis Systemic lupus erythematosus | Antinuclear Antibody: | |
| Systemic lupus erythematosus | dsDNA, ssDNA (double- and single-stranded deoxyribonucleic acid,) | |
| Scleroderma | Anticentromere antibody, Sm | |
| Rheumatoid arthritis | Rheumatoid Factor: | |
| Anti-Cyclic Citrullinated Peptide: | ||
| Wegener’s granulomatosis | Antineutrophil Cytoplasmic Antibody: C ANCA, | |
| Polyarteritis nodosa (PAN) group | P ANCA, |
Infectious Uveitis
Tuberculin skin test (TST)/Mantoux test
It was first described by Koch in 1890 but was modified to intradermal use by Charles Mantoux in 1912.[1] Its a delayed type IV hypersensitivity reaction to purified protein derivative (PPD) which is prepared by precipitation of proteins from heat killed cultures of Mycobacterium tuberculosis. The sensitized T-cells are recruited to the site of injection where they release lymphokines leading to erythema and induration. A standard dose of 5 tuberculin units (0.1 ml) is injected intradermally on the volar surface of the forearm and the result is interpreted after 48–72 h in terms of erythema and induration [Fig. 1]. Diameter of the induration is measured perpendicular to the long axis in millimeters. An induration of 10 mm or more is considered positive, 5–9 mm doubtful and less than 5 mm negative.[2] However, this also depends on the endemicity of tuberculosis in the region. An induration of more than 5 mm is considered positive in cases of recent TB contact, HIV-positive patients, or immunosuppressed patients like post-organ transplant. On the other hand, patients without any risk for TB are considered to have a positive reaction if it exceeds 15 mm. TST has limited sensitivity and specificity of 71% and 66%, respectively.[3] It fails to distinguish latent infection from active disease.
Figure 1.
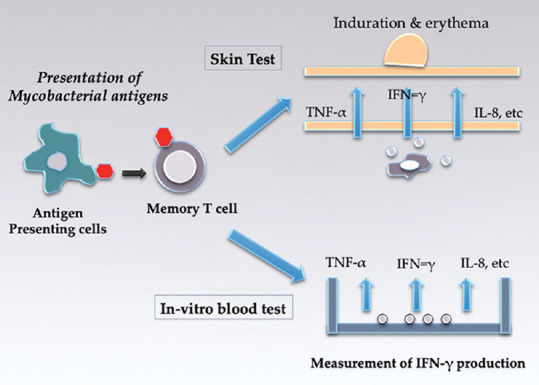
Figure shows both in vivo (TST test) and in vitro (IGRAs) release of inflammatory cytokines by T-cells sensitized to mycobacterial antigens. In the skin test, antigens are injected intra dermally which bring specific lymphocytes to the site causing release of cytokines resulting in induration. In the blood test, mononuclear cells from peripheral blood produce IFN-γ from sensitized T-cells which is measured by ELISA.[6] Adapted from: Andersen P, Munk ME, Pollock JM, et al. Specific immune- based diagnosis of tuberculosis. Lancet 2000;356:1099-04
False positivity is seen post Bacillus–Calmette–Guérin (BCG) vaccination, atypical mycobacterial infection, and also faulty administration. False negative, on the other hand, is due to inability or reduced ability to mount a response to the tuberculin antigen.[4,5,6]
This is usually seen in recent TB infection (less than 8–10 weeks), miliary tuberculosis, sarcoidosis, recent live-virus vaccination, malnutrition, immunocompromised states like HIV infection, post-organ transplants or patients on chronic corticosteroid and immunosuppressive medications, diabetes, and renal disease.
TST is a subjective test that requires technical skill for proper administration and interpretation. It is also a two-step procedure requiring multiple visits of the patient.
Interferon-gamma release assay (IGRA)
It measures the interferon gamma release after in vitro stimulation of T-lymphocytes with MTB antigens (ESAT-6, CFP-10, TB7-7) which are specifically absent in BCG strains and non-tuberculous mycobacteria.[6,7] There are two commercially available IGRAs.
QuantiFeron-Gold In-Tube (QFT, Cellestis Inc, Carnegie, Australia) – It is a whole blood enzyme-linked immunosorbent assay (ELISA) which measures IFN-γ secreted in response to stimulation with ESAT-6, CFP-10, and TB-77 antigens.
T-SPOT TB (Oxford Immunotec, Abingdon, UK) – It is a T cell-based enzyme-linked immunospot assay (ELISPOT) which measures T-cell spot formation after exposure to ESAT-6 and CFP-10 antigens.
Not only IGRAs indicate infection but also help quantify the severity. Higher the mycobacterial load, higher is the T-cell sensitization producing high IFN-γ levels. It is a more specific test of M. tuberculosis indicating infection or previous exposure. Also it is not influenced by prior BCG vaccination or exposure to atypical mycobacteria. It requires a single patient visit and gives an ex vivo objective measure of IFN-γ release. The main disadvantages of IGRAs are higher cost, need for trained technician, specialized instruments, and logistic issues as the blood samples are time and temperature sensitive. Also, IGRA has reduced sensitivity in immunocompromised patients and children.[8] Recently, QuantiFeron-TB Gold PLUS (QFT-PLUS) has been introduced as a new generation QFT-GIT. The QFT-PLUS contains two antigen tubes, TB1 and TB2: the TB1 tube contains ESAT-6 and CFP-10 derived peptides (TB 7.7 was removed) and is designed to induce CD4+ response; the TB2 contains both the same long peptides of TB1 and newly designed peptides which stimulate IFN-γ production by both CD4+ and CD8+ T cells. In a recent meta-analysis concerning the diagnostic test accuracy of QFT-PLUS in detection of TB, the authors conclude that QFT-PLUS performs equivalently to the QFT-GIT for detection of patients at risk for latent TB. Further studies are still needed to prove their efficacy in immunocompromised patients and children.[9]
The role of TST and IGRAs in the diagnosis of intraocular tuberculosis depends significantly on whether the patient is from low or high TB endemic areas.[10] IGRAs can be used in diagnosing latent TB in low endemic areas where its specificity is 92–97%.[10] In a study by Chee et al., the authors reported that QFT is only slightly superior to TST in the diagnosis of TB-related uveitis. It is helpful to perform both tests simultaneously to improve accuracy and avoid negative or indeterminate test results.[11] Most of the referral uveitis centers in India now prefer a combination of Mantoux test and IGRA to diagnose ocular tuberculosis.[12,13] The pros and cons of TST and IGRA is discussed in the table [Table 2].
Table 2.
Pros and Cons of TST and IGRA
| TST | IGRA |
|---|---|
| Measures skin induration after PPD injection | Detection of IFN-γ |
| Affected by BCG vaccination and other mycobacteria | Unaffected by BCG vaccination and other mycobacteria |
| Less sensitive and specific | More sensitive and specific |
| Cheaper/easy availability | costlier |
| Need for review within 48-72 h | Sample handling difficult |
Serological tests for leprosy
Lepromin test
As the incidence of leprosy is coming down, this test is rarely used. The lepromin skin test is used to determine whether the patient has leprosy and if so the type of leprosy he or she has. Inactivated leprosy bacteria is injected just under the skin, on the forearm and examined after 28 days to see if there is a reaction. People who do not have leprosy will have little or no skin reaction to the antigen. People with lepromatous leprosy, will also have no skin reaction to the antigen because they are anergic to the antigen even though their body is loaded with leprosy bacilli. A positive skin reaction will be seen in people with tuberculoid and borderline tuberculoid leprosy.[14]
Serological tests for syphilis
Syphilis, a great mimicker, is caused by Treponema pallidum. It has diverse ocular manifestations and can present as anterior, intermediate, posterior, or panuveitis usually in the late secondary stage. It also shares clinical features with other treponemal and non-treponemal diseases. Hence, it is important that the clinical diagnosis is always supported by appropriate laboratory investigations. It can be diagnosed either by direct or indirect methods. Direct method includes detection of T. pallidum by dark field microscopy, direct fluorescent antibody stains, polymerase chain reaction (PCR), and immunohistochemistry. The sensitivity and specificity of dark field microscopy in the diagnosis of syphilis is 90% and 100%, respectively.[15,16] But this method is seldom applicable as it not commonly available, is technically challenging, and requires an experienced microbiologist. Indirect methods include the serological tests which remain the standard detection method.[17] Serological tests are categorized into two groups: non-treponemal and treponemal.
Non-treponemal tests
The term “non treponemal” refers to the antigens cardiolipin and lecithin which are extracts of normal mammalian tissues. The test detects both IgG and IgM antiphospholipid antibodies against these antigens formed by the host in response to the lipoidal material released from the damaged host cells as well as to lipids on the surface of T. pallidum. Seroconversion usually occurs from 21 days of exposure till 6 weeks after infection. Two tests commonly used are the VDRL (Venereal Disease Research Lab) & the RPR (rapid plasma reagin). These are rapid, simple, and inexpensive tests used as screening tools. But they have their limitations such as reduced sensitivity in primary, late latent and tertiary syphilis. False-positive results due to cross-reactivity are seen in bacterial (leprosy, chancroid, endocarditis), viral (HIV, chickenpox) and parasitic (malaria, trypanosomiasis) infections besides connective tissue diseases (systemic lupus erythematosus, rheumatoid arthritis), advanced age, drug addiction, and pregnancy.[18] False-negative results can be seen in patients with concomitant ocular syphilis and HIV infection due to prozone phenomenon.[19]
The tests are interpreted as reactive, weakly reactive, and non-reactive. A four-fold increase in antibody titer indicates infection, reinfection, or treatment failure. A four-fold reduction in antibody titer suggests response to treatment. These tests are recommended to monitor the course of disease during and after treatment. Patients are evaluated after 3, 6, and 12 months post-treatment to assess the response of therapy and detect any reinfection. If the non-treponemal test shows persistent reactivity at 6 months despite treatment or fails to show a four-fold decrease in antibodies titers within a year, it is reported as sero-resistance or serofast state.[20]
Treponemal tests
These tests detect specific treponemal antibodies. Various tests used more commonly are:
-
T pallidum hemagglutination assay (TPHA):
It is a microhemagglutination assay for Ig G & IgM antibodies where sensitized sheep RBCs are coated with T. pallidum (Nichol's strain). The test is reported as reactive if agglutination occurs in a dilution of 1:80 or more. It is usually seen at 4th to 5th week of infection.
-
Fluorescent treponemal antibody absorption (FTA-ABS)
It is an indirect immunofluorescence antibody test where the reactivity shows by 3rd week of infection.
Chemo luminescence immunoassays (CLIA)
Enzyme immunoassays (EIA)
Rapid tests.
These are used either as agglutination tests or as immunochromatographic strips at the point of care sites. They are easy to perform, require minimal training, and results are available in less than 30 min. However, due to poor quality control, laboratory based tests are recommended.
Treponemal tests remain reactive for years with or without treatment. They are mainly used to confirm the reactivity in non-treponemal tests. Also, they are not useful to monitor the response to treatment, relapse or re-infection and correlate poorly with disease activity. These are more expensive and difficult to perform.[21]
Three testing algorithms are recommended now-a-days, which includes traditional algorithm, reverse sequence algorithm, and the European Centre for Disease Prevention and Control (ECDC) algorithm.[22,23] The traditional algorithm uses a non-treponemal test for screening and the reactive samples are then tested by a treponemal assay for confirmation. The reverse sequence algorithm recommended by the Centers for Disease Control and Prevention (CDC) uses an automated, treponemal test such as EIA or CIA as a screening test followed by a non-treponemal test like RPR for reactive samples. This technique allows rapid analysis. However, the results of EIA screening and RPR are often reported to be discordant. In such situations, CDC recommends a different treponemal test to identify active syphilis.[24,25]
The European Centre for Disease Prevention and Control algorithm uses a treponemal immunoassay that is followed by a second, different treponemal assay as a confirmatory test in high-prevalence populations.[26] All the algorithms have their own pros and cons, hence it is important that the clinician decides about these tests based upon local syphilis prevalence, careful history of the patient including sexual history, medical history or previous treatment history of syphilis and the clinical presentation.
In India, the traditional algorithms including both non-treponemal and treponemal tests is commonly used by uveitis experts. If the clinical assessment suggests a syphilis etiology but the screening tests are non-reactive, one can repeat the tests after 2–3 weeks to confirm the diagnosis. As syphilitic ocular manifestations can mimic other uveitic conditions, routine use of serological tests in all patients with intraocular inflammation of unknown origin is essential. CDC also recommends lumbar puncture for cerebrospinal fluid (CSF) analysis in all patients with ocular syphilis to detect neurosyphilis.[24] The diagnosis is based upon positive VDRL, elevated total protein, and CSF pleocytosis. The CSF VDRL has a very high (99.8%) specificity but sensitivity is only 50%. Consequently, a negative CSF–VDRL does not rule out neurosyphilis. Specific treponemal tests are not useful due to false-positive reaction. The diagnosis is then confirmed with co-relation with serological tests. Besides serological tests in ocular syphilis, intraocular fluid analysis of non-treponemal and treponemal antibodies may also play an important role in diagnostic dilemma.[26,27] In a recent study by Silpa-Archa et al., authors have concluded that vitreous treponemal antibodies can act as a supplementary test to serology for confirmation of syphilitic chorio-retinitis.[27]
Leptospirosis
Leptospirosis is a waterborne spirochete, dark field microscopy can visualize the organisms from body fluids, but the test is less specific and false positives are more common. Microagglutination test (MAT) is the gold standard test where the alive motile bacteria is added to titrated amounts of patients serum.[28] If the serum has antibodies agglutination happens which can be visualized by dark field microscopy. The sensitivity of the test is low, however it is highly specific.
The MAT is a complex test to control, perform, and interpret. Live cultures of all serovars required for use as antigens have to be sub-cultured every week. The repeated weekly subculture of large numbers of strains presents hazards for laboratory workers and laboratory-acquired infections have been reported. Other drawbacks include the continuous risk of cross-contamination of the cultures, necessitating periodic verification of each serovar.
The IgM-ELISA is more readily commercially available and is less labor-intensive than MAT. The result of IgM-ELISA should be considered preliminary and further confirmation by MAT is recommended. Other serological tests that are available include macroscopic agglutination, indirect haemagglutination, lepto dipstick, microcapsule agglutination tests, and lateral flow assay. In addition to the above serologic assays, polymerase chain reaction and immunohistochemical (IHC) assays are sensitive methods of diagnosis.[29]
A short description on the methodology of ommunological test used in these diseases. Enzyme immunoassays, Western blot test are commonly used immunological tests. These tests use an antigen to identify the presence of antibodies to a microbe, or an antibody to identify the presence of an antigen or of the pathogen in the samples.
ELISA
It is a plate based assay technique to detect and quantify viruses, proteins, antibodies and hormones. We can use various antigen–antibody combinations. The procedure includes either an enzyme labelled antigen or antibody. From the final enzymatic activity the result can be interpreted qualitatively [Fig. 2].
Figure 2.
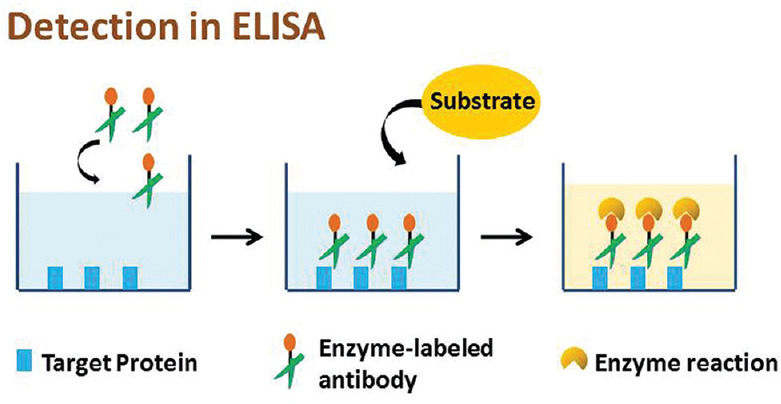
Depicts the steps in Enzye Immuno Assay
Western blot
This is a sensitive assay for identification of proteins. It is based on the immunochromotography principle. In this test, the proteins are first separated into polyacrylamide gel according to their molecular weight and then transferred to nitrocellulose membrane. Then proteins are identified using initial specific primary antibody followed by secondary enzyme labelled antibody and substrate [Fig. 3].
Figure 3.
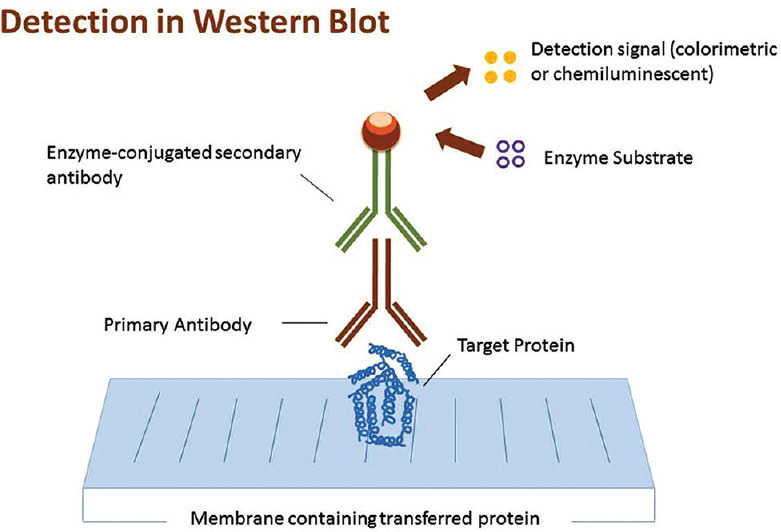
Depicts the steps in Western Blot
Lymes disease
ELISA
This test is used most often to detect Lyme disease, ELISA detects antibodies to Borrelia burgdorferi. But because it can sometimes provide false-positive results, it's not used as the sole basis for diagnosis. This test might not be positive during the early stage of Lyme disease, but the rash is distinctive enough to make the diagnosis without further testing in people who live in areas infested with ticks that transmit Lyme disease.[30]
Western blot test
If the ELISA test is positive, this test is usually done to confirm the diagnosis. In this two-step approach, the Western blot detects antibodies to several proteins of Borrelia burgdorferi.[30]
Serological tests for rickettsiae
Rickettsial infections are caused by obligate intracellular gram-negative bacteria. It is usually transmitted to humans by the bite of ticks and mites. Rickettsial agents are classified into three groups: the scrub typhus (ST), murine typhus (MT), and spotted fever (SF). Diagnosis is based on culture, nucleic acid amplification, and serological tests including Weil-Felix test (WFT), ELISA, rapid diagnostic tests (RDT), and immunofluoresceny assay (IFA).[31] WFT is a hemagglutination test which is widely used for screening due to low cost and easy availability, but it lacks specificity. ELISA is less expensive and easy to perform. IFA is the gold standard for diagnosis of rickettsial infection but it needs skill, precision and is not routinely available. Serological diagnosis of rickettsial disease has various disadvantages due to poor sensitivity during acute infection where antibodies are not detectable within 10–14 days, cross-reactions with other rickettsial infections and being an indirect methods depending upon host responses. A recent study from India compared Weil-Felix test and IgM ELISA in the diagnosis of scrub typhus and it concluded that IgM–ELISA is more sensitive, rapid and specific in early phase of disease while Weil-Felix test specificity increases with increasing titres.[32]
Serological tests for HIV
HIV continues to be one of the major infectious causes of global public health issue. But with the availability of early diagnostic techniques and treatment for HIV and its associated opportunistic infections, patients living with HIV AIDS can still lead a long and productive life.[33]
Diagnosing HIV is the first crucial step in the treatment and prevention of AIDS. To diagnose the disease early with proper serological investigations, we should know the pattern of emergence of antigens and antibodies in the serum.
Immediately after HIV infection low levels of HIV RNA will be present intermittently in the patient's plasma. Nearly after 10 days, this RNA quantitatively increases in the plasma. Next, the p24 antigen is expressed and it quantitatively increases to levels that are microbiologically detectable. But this increase is transient. It is because of the development of antibody against P24 antigen which then forms immune complexes making their detection difficult. After 2 weeks of RNA development, IgM antibodies develop which is followed by IgG antibodies. These IgG antibodies will be present throughout the course of the disease.
Appropriate selection of the right investigation according to the timeline of the disease is mandatory to detect the disease at the earliest.
The following are the Lab investigations available for HIV:[34]
HIV Enzyme Immuno Assay
p24 antigen
Western Blot
Qualitative and quantitative PCR.
Enzyme immunoassay (EIA)[35]
Enzyme immunoassay was developed as the initial screening test for HIV infected patients before the window period. Five generations of assays have been developed so far based on the sensitivity and specificity of the tests to detect the HIV variants. The first generation could detect only the IgG antibodies against HIV. The recent generations can detect both IgG/IgM antibodies of both HIV I/II and also P24 antigen. The third and fourth generation assays reduce the window period to 20–25 days post-infection and the fifth generation assays reduce it to 1 week.
While the third generation immunoassay is commonly used in screening, the fourth generation is being used in facilities like Blood bank.
The disadvantage of this test is the chances of false-positive cases. So the EIA positive cases has to be re-evaluated either with a confirmatory test like Western blot or with a second EIA test using a different part of viral antigen for the detection of the antibody.
p24 antigen immuno assay
This test again uses EIA base to detect disrupted p24 antigen from the serum. This test may be positive in a recently infected patient with a HIV EIA negative test, necessitating a follow up evaluation weeks after the initial testing. p24 may not be detectable in all patients who are already positive for HIV antibodies.
Western blot[36]
This immunosorbent blot technique has been used to detect antibody to each viral protein. The test as discussed earlier contains a nitrocellulose strip having both the core and envelope protein of the HIV virus. The patient serum reacts with the strip after Gel Electrophoresis. According to the type of antibody present, the serum will bind to the antigen and produce a characteristic color band. Presence of one core band and one envelope band is mandated to declare a positive result. If the bands are indeterminate, a follow-up test has to be done after a month for acquiring a definitive band pattern. In case of failure to acquire a definitive band in a repeat test confirms that the patient is HIV negative and the band is due to nonspecific antibody. True HIV negative can be further confirmed by PCR.
These nonspecific antibodies make it difficult in using this test as a screening tool. This test is also difficult to perform in a high volume due to its labor intensive nature.
Rapid diagnostic tests (RDT)[37]
RDT is fast becoming the primary methodology of HIV testing in recent years in resource limited settings. It uses both immunochromatographic and immunofiltration techniques. It can detect HIV I/II antibodies and/or p24 antigen. It takes less than 30 min and does not need venepuncture blood. All these make it the ideal test for community based testing.
But studies have proven that it is still not as effective as ELISA in screening for HIV.[38]
Other immunuological test commonly done in these HIV patients is PCR when they develop opportunistic ocular infections. Previous studies have revealed that the sensitivity of PCR for the CMV retinitis identification can be as high as 95% and the specificity 99% in immunocompromised patients.[38] Similarly the sensitivity of the assay for the diagnosis of herpetic retinitis in HIV patients is 100% and the specificity 97%.[38] Again the sensitivity of PCR in ocular fluid in Ocular Toxoplasmosis is as high as 75% in immunocompromised patient in contrast to their immunocompetent counterpart where the sensitivity is only 30–40%.[39]
Newer rare infections
Newer viral infections such as Chikungunya, West Nile virus and rickettsial infections are tested by ELISA tests usually in reference laboratories.[40] Commercial kits have to be checked whether they are validated in different population.
Serological tests for dengue
Dengue is a mosquito-borne infection, transmitted by mosquitoes Aedes aegypti and Aedes albopictus. Four dengue virus serotypes of Flavivirus genus have been known to infect humans, which includes DEN-1, DEN-2, DEN-3, and DEN-4.[41] Primary infection with dengue virus results in serum IgM antibodies by 3–5 days post-infection and persist for 1–2 months post infection. Secondary infections show a rapid increase in serum IgG as early as 3 days of illness and late appearance of IgM antibodies. Hence, a ratio of IgM to IgG during the acute phase of the disease can help identify whether it is a primary or a secondary infection. The standard serological test for dengue virus infection is enzyme linked immunosorbent assay (ELISA) for IgM and IgG antibodies. This is a simple, easy to perform test with high sensitivity.
IgM- antibody capture ELISA (MAC-ELISA)[42,43] - is used for qualitative detection of serum IgM antibodies. The only limitation is that it lacks specificity and shows cross-reactivity with other flavi viruses. Anti-dengue IgM is a marker of recent infection and anti-dengue IgG in the serum denotes past infection. However, presence of a high titre or a four-fold increase in the serum titres of IgG confirms dengue infection.
Plaque Reduction Neutralization test (PRNT)[42,43]- It can detect specific neutralizing antibodies against dengue virus and other flavi viruses. It measures the titres of neutralizing antibodies in the serum of patients. It is usually used to distinguish dengue virus from other viruses like Zika or yellow fever. The limitations of PRNT are that it is labor intensive, expensive to perform, and requires special laboratories to perform.
Serological tests for chikungunya
Chikungunya is caused by chikungunya virus (CHIKV), an arthropod virus and a member of Alphavirus genus. This infection has a clinical similarity with other arboviruses like dengue virus and Zika virus, so it is important to have a good diagnostic evaluation. Common laboratory tests for chikungunya include serological tests for IgM and IgG antibodies and viral RNA detection by reverse transcription–polymerase chain reaction (RT-PCR).[44] Center for Disease Control and Prevention (CDC) has proposed a testing algorithm for diagnosing chikungunya based upon the characteristics of infection and the timing of collection of serum for analysis. During the first week of infection, RT–PCR, a molecular diagnostic test should be ordered to detect viremia. As IgM levels rise by day 7, IgM antibody assay is helpful. After 14–21 days, both IgM and IgG test will be positive. IgM levels wane over next few months and IgG remains for years as a marker of past infection. A four-fold rise in antibody titre in acute and convalescent sera or specific IgM antibodies are diagnostic of Chikungunya infection.[44] Various serological tests available are:
IgM- antibody capture ELISA (MAC-ELISA )
Immunofluorescent assay
Hemagglutination – inhibition tests
Plaque Reduction Neutralisation test (PRNT) – It is highly specific and gold standard for confirmation of serological tests.
Serological tests for toxoplasmosis
Ocular toxoplasmosis, caused by Toxoplasma gondii, is the leading cause of infectious posterior uveitis worldwide.[45] It can be congenital and acquired or can be primary or secondary due to reactivation of the previous latent infection.[46,47] Diagnosis is mainly clinical but serological assay helps in confirming the same. Seroprevalence of anti- T. gondii antibodies is highly variable in various population and ranges from 5 to 54% in Europe, 12 to 58% in Asia, 16 to 40% in North America, and upto 80% in South America.[45,48] In India, the seroprevalence of toxoplasmosis is 24.3%, varying from 4.7% to 51.8% in North India to 37.3% in South India.[49] Active infection stimulates both innate as well as acquired immunity leading to production of antibodies like IgM, IgA, IgE and IgG from B-cells. IgM antibodies appear at the end of first week of infection, begin to fall in 4–8 weeks and may persist in low levels upto a year. IgG antibodies appear after 2 weeks, peak by 3 months of infection and persist throughout life due to the presence of latent cysts.[49] Serological tests which are available for diagnosing ocular toxoplasmosis can be divided into two groups.[50]
Screening methods
These are simple to perform, low cost and require small amount of serum.
ELISA (enzyme-linked immunosorbent assay)
CLIA (Chemiluminescence immuno assay).
Confirmation methods
These are complex and expensive to perform.
IFAT (immunofluorescent antibody test)
ISAGA (immunosorbent agglutination assay)
Avidity test.
Interpretation of serological analysis plays the vital role in determining the need for anti-toxo medications in uveitis. Absence of both the IgM and IgG antibodies in the serum rules out the presence of any toxoplasmic infection. A positive IgG and negative IgM only denotes previous infection and can be misleading. High serum IgG titres are not the reliable indicators of either recent or reactivation of latent infection. However, if the level of IgG is 3–4 times higher than normal or repeat serology 3 weeks later shows increasing titres, it may be considered active infection. In congenital toxoplasmosis, presence of IgM and/or IgA antibodies confirm acute infection. Only IgG antibodies in a neonate rules out toxoplasmosis as these are maternal antibodies which cross the placenta and are later eliminated by the neonate. In immunosuppressed patients like HIV+ or post organ transplant patients with chronic immunosuppressive therapy, positive serology suggests infection, however negative tests donot exclude concurrent infection. Besides serum, levels of antibodies can also be tested in aqueous humor. The Goldmann–Witmer or Witmer–Desmonts coefficient (GWC) is a valuable test that compares the intraocular antibody production to that of serum as measured by ELISA. GWC greater than 4 is suggestive of recent infection.[51,52] In a study by Fekkar et al., the authors have compared the sensitivities and specificities of three biological methods including immunoblotting, GWC and real time PCR for diagnosis of ocular toxoplasmosis. The study concluded that a combination of all the three techniques improved the sensitivity to 97%. thus increasing the diagnostic yield of ocular toxoplasmosis especially in atypical lesions.[53]
Serological tests for toxocariasis
Toxocariasis is a common zoonotic disease worldwide mainly in children. But diagnosis of ocular toxocariasis is underrated. Usually the diagnosis in ocular toxocariasis is clinical. Serological evidence may help to confirm the diagnosis. But seroprevalance is high in general population due to socio economic conditions. ELISA-based IgG antibodies may add a value to the clinical diagnosis. Still a negative result does not exclude ocular toxocariasis. In such scenario, a positive vitreous titre for toxocara antibody may help.[54,55,56]
Non-Infectious Uveitis
Antinuclear antibody
Antinuclear antibodies (ANA) are a specific group of antibodies that recognize nuclear and cytoplasmic cell structures. ANA testing by immunofluorescence (IF) is the standard method and is used as a first-step screening test for autoimmune diseases.[57] Other laboratory tests used for ANA detection are enzyme immunoassay (EIA) and enzyme-linked immunosorbent assay (ELISA). Immunofluorescence test detects the presence of ANA in the blood of the patient which adhere to reagent test cells and forms different fluorescence patterns. Different patterns of ANA staining on IF may be grouped broadly into 3 subclasses including nuclear, cytoplasmic, and mitotic. These distinct fluorescence patterns are associated with certain autoimmune diseases. Another test parameter is ANA titer, which is directly proportional to the antibody concentration and is expressed with a quantitative scale of values.[58] Higher titers of ANA are more clinically significant.[57] Although the ANA test has a nearly 100% sensitivity for the diagnosis of systemic lupus erythematosus (SLE), it is not specific for this diagnosis and may be positive in other systemic autoimmune rheumatic diseases as well.[57] ANA may also be found in organ-specific autoimmune diseases, in viral infections and even in healthy individuals.[59] Therefore, in case of a positive ANA result, additional testing for anti-double stranded DNA (anti-dsDNA) antibodies and antibodies to specific extractable nuclear antigens (ENAs) such as anti-Ro (also called anti-SSA), anti-La (also called anti-SSB), anti-Sm, anti-RNP should be performed.[58,60]
ANA in healthy individuals is generally in low titers. Usually a titer of 1:160 is considered as significant for the diagnosis of connective tissue diseases; however, the results need interpretation within the clinical context.[61]
Routine testing of all uveitis patients for ANA has been shown to have a low positive predictive value of 0.6–2.9% in different studies; therefore, ANA testing should be included in the work up of patients with specific signs and symptoms of SLE such as a rash, symmetric polyarthritis, nephritis or pleuropericarditis and patients presenting with possible ocular manifestations of SLE including episcleritis, scleritis, and retinal/choroidal vasculitis.[62,63] Retinal vasculitis in SLE patients correlates with the systemic disease activity and may indicate inadequate control of the systemic disease. Hence, early diagnosis may aid as a prognostic factor for survival.[64] The presence of anti-dsDNA and antiphospholipid antibodies should also be tested in patients with retinal vasculitis; because anti-dsDNA which is a lupus specific antibody also correlates with the disease activity in SLE patients and there is a known association of antiphospholipid syndrome with SLE retinopathy.[65]
In addition to the entities above, all non-infectious pediatric anterior uveitis patients should be screened for ANA positivity. Anterior uveitis is the most common type of uveitis seen in pediatric population and juvenile idiopathic arthritis (JIA) is the predominant systemic disease associated with uveitis in children.[66,67] One of the main diagnostic criteria for JIA is ANA positivity and it is a known risk factor for ocular involvement in patients with JIA. Moreover, the presence of ANA is significantly associated with ocular complications at presentation.[68,69] Therefore, testing pediatric patients with anterior uveitis for ANA has a tremendous value in that it may affect the management of the systemic disease and also it identifies those patients at high risk for chronic anterior uveitis.
Rheumatoid factor
Rheumatoid factors (RFs) are a class of immunoglobulins (Igs) that have different isotypes and affinities and are defined as antibodies directed against the C-terminal domain of the constant region of the heavy chain (Fc fragment) of IgG. Different RFs recognize different parts of the IgG-Fc. IgM RFs are the most frequently observed isotype, but IgG, IgA, IgE, and IgD RFs are also detected. Nephelometry and ELISA are the methods used to detect RF in clinical practice.[70]
High levels of RF is usually associated with systemic autoimmune diseases, such as rheumatoid arthritis (RA), SLE, mixed connective tissue disease, and Sjogren's syndrome. However; RFs may also be detected in patients with nonrheumatic conditions such as infections and chronic diseases, as well as in healthy subjects.[71,72]
Rheumatoid factor titer in RA patients may be used in monitoring disease activity and treatment response since decrease in the RF levels parallels the decrease of clinical activity in patients under treatment.[73] High titers of RF in RA patients is associated with more aggressive joint disease and increased frequency of extra-articular manifestations including ocular involvement which may also be the initial manifestation of the disease.[74,75] Therefore, RF testing is usually included in the work-up of patients with episcleritis, scleritis, peripheral ulcerative keratitis (PUK), anterior uveitis, and dry eye which are known ocular manifestations of rheumatic diseases including RA that may have RF seropositivity. RF testing is also included in the workup of pediatric patients with noninfectious ocular inflammation. According to the International League of Associations for Rheumatology (ILAR) classification JIA has 7 subtypes and 1 of them is RF positive polyarticular JIA which is genetically more similar to adult RA.[76] The risk of anterior uveitis in patients with RF positive polyarticular JIA is less than other subtypes of JIA.
Although RF is known as the cheapest modality for the screening of RA especially in ophthalmology clinics, it is often not detected early in the course of the disease and it is not specific for RA. Anti-Cyclic Citrullinated Peptide (Anti-CCP) antibody testing can enable earlier and more specific diagnosis. Hence, anti-CCP should also be tested when there is high suspicion of RA, despite RF being within normal range.
Anti-Cyclic citrullinated peptide
Citrulline is an atypical amino acid that has been implicated in the pathogenesis of RA. Citrullinated proteins are present in the inflamed synovium of RA patients and this increased citrullination of peptides in an inflamed joint leads to the development of antibodies to citrullinated protein antigens. Anti-CCP in blood is detected by ELISA and is found to be a more specific serum test for RA than the RF titer and may be detected positive before the onset of clinical RA symptoms. Based on the American College of Rheumatology criteria the sensitivity and specificity of anti-CCP positivity for the diagnosis of RA were detected as 73.5% and 100%, respectively.[77] Therefore, Anti-CCP antibody testing is useful when the diagnosis of RA is still not definite, especially early in the disease course.[78]
It was shown that anti-CCP and RF positive RA patients tend to have more and worse ocular involvement.[75] Anti-CCP test is useful when attempting to confirm the diagnosis of RA in patients with typical ocular symptoms such as episcleritis, scleritis, or PUK despite the absence of systemic signs.
Antineutrophil cytoplasmic antibody
Antineutrophil cytoplasmic antibody (ANCA) reacts against the proteins located in the granules of neutrophil cytoplasm and creates 3 different characteristic appearances on IF. Two of these are cytoplasmic and perinuclear that are well-defined staining patterns and regarded as positive. The last one is a non-specific reaction as a result of an excess of various antibodies that creates a diffuse pattern. The cytoplasmic appearance called c-ANCA is almost always directed against PR3-ANCA and is usually found in granulomatosis with polyangiitis (GPA). The perinuclear pattern called p-ANCA is usually directed against MPO-ANCA and is more commonly found in microscopic polyarteritis.[79,80]
ANCA-associated vasculitides (AAV) are a group of systemic diseases that primarily effect small and medium sized vessels with multisystem involvement including the eyes.[81]
Frequency of ocular involvement in AAV in different studies goes up to 70%. Ocular inflammation is the initial manifestation leading to diagnosis to AAV in some of these studies.[81,82,83,84,85] Therefore, patients with scleritis, PUK, orbital inflammation, and retinal or orbital vasculitis who are being investigated for an underlying systemic disease should be screened for ANCA for the possibility of AAV including GPA, eosinophilic GPA (Churg- Strauss Syndrome), and microscopic polyarteritis which can be life threatening. Since ANCA specifity is predictive for response to treatment and long-term prognosis both p-ANCA and c-ANCA should be screened in these patients as c-ANCA positive patients are at higher risk for relapse.[86] Early diagnosis and treatment of the ocular inflammation and the underlying disease can be lifesaving. Hence, ANCA serology could be considered as a screening laboratory test in these patients.
HLA typing
Human leucocyte antigens (HLA) are cell surface molecules encoded by a highly polymorphic family of genes involved in immunity and responsible for identifying self versus non-self. The HLA loci are a part of the genetic region known as the major histocompatibility complex (MHC) located at 6p21.3 on the short arm of chromosome 6. MHC Class I includes the HLA-A, HLA-B, and HLA-C antigens that are expressed, to varying degrees, on the surface of all nucleated cells and present endogenously produced peptides, including native proteins as well as damaged, degraded, or misfolded proteins, and also viral proteins to CD8-positive T lymphocytes. MHC Class II includes the HLA-DP, HLA-DQ, and HLA-DR antigens that have a more limited expression on specific immune cells and present exogenously produced peptides, such as bacterial proteins, to CD4-positive T lymphocytes.[87,88]
HLA typing has been conventionally based on serologic methods.[89] Molecular typing methods used in modern medicine allows the definition of HLA alleles to different levels of resolution. The “four-digit” typing distinguishes alleles based on the sequence of peptide-binding region of the HLA molecule (e.g, HLA-B*51:01).[87,89]
HLA typing is essential for solid organ and bone marrow transplantation as well as in non-transplant settings such as disease association and pharmacogenomics.[87] Numerous diseases, particularly those that are immune-mediated, are associated with certain HLA alleles.[87] Table 3 shows HLA associations of selected uveitic entities.
Table 3.
HLA associations of selected uveitis entities
| Uveitis entity | HLA antigen | Frequency (%) |
|---|---|---|
| Birdshot chorioretinopathy | A29 | 96-100 |
| Acute anterior uveitis | B27 | 40-82 |
| Ankylosing spondylitis | B27 | 92 |
| Behçet disease | B51 | 59 |
| Vogt-Koyanagi-Harada disease | DQ4 | 83 |
| DQA1*0301 | Up-100% | |
| DR4 | 93 | |
| DRB1*0405 | Up to 95% | |
| Intermediate uveitis | DR15 | 47-72 |
| Multiple sclerosis | DRB1*1501 | Up-62 |
| Tubulointerstitial nephritis and uveitis | DQA1*01/ | 72 |
| DQB1*05/DRB1*01 |
In general, HLA typing has limited usefulness for the diagnosis of uveitis and routine screening is not recommended.[90,91] When there is a weak association, because of the low percentage of patients with the disease having the HLA type or the high prevalence of the HLA type in the normal population, HLA typing is not useful. Even when there is a strong HLA association, the positive predictive value of HLA typing, that is, the likelihood that a patient with a specific HLA antigen will have the uveitic entity in question, depends not only on the sensitivity and specificity of the HLA test, but also on the prevalence of the disease in question.[90] Although birdshot chorioretinopathy has the strongest association with an MHC Class I antigen, HLA-A29, routine testing in all patients with posterior uveitis is not recommended because birdshot chorioretinopathy is a rare entity even among posterior uveitides seen in Caucasians who have an HLA-A29 prevalence of 5%.[92,93,94] Zamecki and Jabs reported that the positive predictive value of HLA-A29 was 0.47 in patients with posterior uveitis.[90] Thus only patients with clinical features consistent with this entity should be tested because a positive result is diagnostic and a negative result will indicate that a diagnosis of birdshot chorioretinopathy is highly unlikely.[92,93,94] Birdshot chorioretinopathy has not been reported in any of the recent uveitis series from India,[95,96,97,98,99] which is not surprising because the HLA-A29 antigen is extremely rare or even nonexistent in the Indian populations of diverse ethnicity.[100,101,102]
Indiscriminate testing for HLA-B27 is not recommended in all patients with uveitis. On the other hand, routine HLA-B27 testing is included in the diagnostic algorithm for patients with acute anterior uveitis as it can help to identify a distinct uveitis entity and also a previously undiagnosed systemic disease association.[90,91] Patients with HLA-B27–associated uveitis typically have a recurrent, acute, unilateral or unilateral alternating, nongranulomatous anterior uveitis of limited duration.[103,104] In a meta-analysis of studies comparing HLA-B27-positive and HLA-B27-negative patients with acute anterior uveitis, specific characteristics linked to the antigen included a strong association with ankylosing spondylitis (RR = 9.9), hypopyon (RR = 5.5), and fibrinous reaction (RR = 8.7).[105] Therefore, in patients who first present with acute anterior uveitis, HLA-B27 testing is performed to confirm the specific phenotype of acute anterior uveitis, to predict its recurrent nature, and most importantly, to predict systemic disease association for an early referral to a rheumatologist.[90,103] Approximately 50–75% of patients with HLA-B27 acute anterior uveitis have an associated spondyloarthropathy.[104] Acute anterior uveitis is significantly more common in HLA-B27-positive than in HLA-B27-negative patients with ankylosing spondylitis.[106] Haroon et al.[107] have proposed a diagnostic algorithm (DUET; Dublin Uveitis Evaluation Tool) that would be useful to determine which patient presenting with acute anterior uveitis, should be referred to a rheumatologist. In this algorithm, HLA-B27 was checked in all patients who presented with acute anterior uveitis and back pain (onset <45 years of age and duration >3 months) or joint pains; and those who were HLA-B27-positive were referred to a rheumatologist. Patients who were HLA-B27-negative, but had psoriasis were also referred to a rheumatologist. The algorithm identified a previously undiagnosed spondyloarthropathy in around 40% of patients who presented with acute anterior uveitis.[107] The reported frequencies of HLA-B27-associated uveitis at tertiary care centers were 6% and 10.5% in South India[95,96] and 9.5% in North India.[97] This entity accounted for 12–30% of anterior uveitis in these series.[95,96,97] While systemic disease association of HLA-B27-positive patients was not specified in any of these series, in a recent report from a tertiary eye care center of central India, 7% of uveitis cases had spondyloartropathy.[98] Mishra and Bharucha[108] reported that the HLA-B27 frequency was 65.7% in acute anterior uveitis patients seen at a tertiary care center in Maharashtra. Only 4.5% of their HLA-B27-positive cases had systemic disease.[108] HLA-B27 is present in approximately 6–8% of the normal population in the Indian subcontinent;[109] and the frequency of HLA-B27 uveitis is similar to the figures in uveitis series reported from North America (6.7%),[110] Italy (7.7%)[111], Germany (10%),[112] and France (17.4%).[113] While more than 90% of Caucasian patients with ankylosing spondylitis have the HLA-B27 antigen,[104] only 21% of a south Indian population of ankylosing spondylitis patients tested positive for HLA-B27 antigen by the serologic method, but the HLAB*27 allele frequency was found to be 74% by the molecular method.[114] Thus the method of HLA-B27 typing should be taken into consideration when it is used as a diagnostic test in patients presenting with acute anterior uveitis.
Although HLA associations have been identified in other uveitic entities, the diagnostic value of routine HLA typing is questionable. Zamecki and Jabs[90] have shown that the positive predictive value of HLA test for uveitic entities such as Behçet's disease and Vogt-Koyanagi-Harada disease was 0.3 or lower.
The diagnosis of Behçet's disease is based on a combination of clinical manifestations, including intraocular inflammatory findings, recurrent oral ulcers, genital ulcers, and skin lesions. Although HLA-B51 antigen is associated with the disease,[115] HLA-B51-positivity has not been included as a diagnostic criterion in any of the diagnostic or classification criteria sets that are currently used.[116,117,118] The value of HLA-B51 testing in predicting disease severity is also controversial.[115]
Vogt-Koyanagi-Harada (VKH) disease is a clinical diagnosis and HLA-typing is not routinely performed when this diagnosis is considered. In a meta-analysis of articles relevant to the genetics of VKH disease, MHC Class II genes, specifically HLA-DQ A1*0301 and HLA-DRB1*0405 alleles showed the strongest association in various ethnic groups.[119]
Both idiopathic intermediate uveitis (pars planitis) and multiple sclerosis have been found to be associated with the HLA-DR15 subtype of HLA-DR2.[120,121,122] Thus HLA typing has no value in predicting the development of multiple sclerosis in patients with intermediate uveitis.
Strong associations have been found between specific HLA-DQ and HLA-DR alleles and the tubulointerstitial nephritis and uveitis (TINU) syndrome.[123] However, there is limited value of HLA typing as a routine test in this rare entity.
Conclusion
Investigations are an integral part in managing patients with infectious and non-infectious uveitis. But; it should be tailored to the patient's presentation. Tests should add value to the clinical diagnosis. Sometimes even negative test results have equally important value in diagnosing a disease. Few tests helps in diagnosing the disease, few in prognosticating the disease course and few in deciding the treatment pattern. Clinicians should never hesitate to re-evaluate/investigate the patient if the disease does not follow the anticipated course.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Menzies D. Tuberculin skin testing. In: Reichman LB, Hershfield ES, editors. Tuberculosis: A Comprehensive International Approach. New York: Marcel Dekker; 2000. pp. 279–322. [Google Scholar]
- 2.Mazurek GH, Jereb J, Lobue P, Iademarco MF, Metchock B, Vernon A. Guidelines for using the QuantiFERON-TB Gold test for detecting Mycobacterium tuberculosis infection, United States. MMWR Recomm Rep. 2005;54:49–55. [PubMed] [Google Scholar]
- 3.Gupta V, Gupta A, Rao NA. Intraocular tuberculosis – an update. Surv Ophthalmol. 2007;52:561–87. doi: 10.1016/j.survophthal.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 4.American Thoracic Society. Diagnostic standards and classification of tuber culosis. Am Rev Respir Dis. 1990;142:725–35. doi: 10.1164/ajrccm/142.3.725. [DOI] [PubMed] [Google Scholar]
- 5.Huebner RE, Schein MF, Bass JB., Jr The tuberculin skin test. Clin Infect Dis. 1993;17:968–75. doi: 10.1093/clinids/17.6.968. [DOI] [PubMed] [Google Scholar]
- 6.Andersen P, Munk ME, Pollock JM, Doherty TM. Specific immune-based diagnosis of tuberculosis. Lancet. 2000;356:1099104. doi: 10.1016/s0140-6736(00)02742-2. [DOI] [PubMed] [Google Scholar]
- 7.Menzes D, Pai M, Comstock G. Meta analysis: New tests for the diagnosis of latent tuberculosis infection: Areas of uncertainty and recommendations for research. Ann Intern Med. 2007;146:340–54. doi: 10.7326/0003-4819-146-5-200703060-00006. [DOI] [PubMed] [Google Scholar]
- 8.Dewan PK, Grinsdale J, Kawamura LM. Low sensitivity of a whole blood interferon-gamma release assay for detection of active tuberculosis. Clin Infect Dis. 2007;44:69–73. doi: 10.1086/509928. [DOI] [PubMed] [Google Scholar]
- 9.Pourakbari B, Mamishi S, Benvari S, Mahmoudi S. Comparison of the QuantiFERON-TB GOLD plus and QuantiFERON-TB GOLD in-tube interferon-γ release assays: A systematic review and meta-analysis. Adv Med Sci. 2019;64:437–43. doi: 10.1016/j.advms.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Trad S, Bodaghi B, Saadoun D. Update on immunological test (Quantiferon-TB Gold) contribution in the management of tuberculosis related ocular inflammation. Ocul Immunol Inflamm. 2018;26:1192–9. doi: 10.1080/09273948.2017.1332232. [DOI] [PubMed] [Google Scholar]
- 11.Ang M, Htoon HM, Chee SP. Diagnosis of tuberculous uveitis: Clinical application of an interferon-gamma release assay. Ophthalmology. 2009;116:1391–6. doi: 10.1016/j.ophtha.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Sudharshan S, Ganesh SK, Balu G, Mahalakshmi B, Therese LK, Madhavan HN, et al. Utility of QuantiFERON®-TB Gold test in diagnosis and management of suspected tubercular uveitis in India. Int Ophthalmol. 2012;32:217–23. doi: 10.1007/s10792-012-9554-0. [DOI] [PubMed] [Google Scholar]
- 13.Babu K, Philips M, Subbakrishna DK. Perspectives of Quantiferon TB Gold test among Indian practitioners: A survey. J Ophthalmic Inflamm Infect. 2013;3:9. doi: 10.1186/1869-5760-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Renault CA, Ernst JD. Mycobacterium leprae (leprosy) In: Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, Updated Edition. 8th ed. 252. Philadelphia, PA: Elsevier Saunders; 2015. [Google Scholar]
- 15.Larsen SA, Pope V, Johnson RE, Kennedy EJ., Jr . A Manulal of Tests for Syphilis. Wasington DC: American Public Health Association; 1998. [Google Scholar]
- 16.Tsang RS, Morshed M, Chernesky MA, Jayaraman GC, Kadkhoda K. Canadian public health laboratory network laboratory guidelines for the use of direct tests to detect syphilis in Canada. Can J infect Dis Med Microbiol. 2015;26(Supl A):13A–7A. doi: 10.1155/2015/685603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Larson SA, Steiner BM, Rudolp AH. Laboratory diagnosis and interpretation of tests for syphilis. Clin Microbio. 1995;8:1–21. doi: 10.1128/cmr.8.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiwanitkit V. Biological false reactive VDRL tests: When to re-test? Southeast Asian J Trop Med Public Health. 2002;33:131–2. [PubMed] [Google Scholar]
- 19.Tucker JD, Li JZ, Robbins GK, Davis BT, Lobo AM, Kunkel J, et al. Ocular syphilis amog HIV infected patients: A systematic analysis of the literature. Sex Transm Infect. 2011;87:4–8. doi: 10.1136/sti.2010.043042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ratnam S. The laboratory diagnosis of syphilis. Can J Infect Dis Med Microbiol. 2005;16:45–51. doi: 10.1155/2005/597580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tong ML, Lin LR, Liu LL, Zhang HL, Huang SJ, Chen YY, et al. Analysis of 3 algorithms for syphilis serodiagnosis and implications for clinical management. Clin Infect Dis. 2014;58:1116–24. doi: 10.1093/cid/ciu087. [DOI] [PubMed] [Google Scholar]
- 22.Morshed MG. Current trend on syphilis diagnosis: Issues and challenges. Adv Exp Med Biol. 2014;808:51–64. doi: 10.1007/978-81-322-1774-9_5. [DOI] [PubMed] [Google Scholar]
- 23.Pillay A. Centers for disease control and prevention syphilis summit-diagnostics and laboratory issues. Sex Transm Dis. 2018;45(9S Suppl 1):S13–6. doi: 10.1097/OLQ.0000000000000843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morshed MG, Singh AE. Recent trends in the serologic diagnosis of syphilis. Clin Vaccine Immunol. 2015;22:137–47. doi: 10.1128/CVI.00681-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sena AC, White BL, Sparling PF. Novel treponema pallidum serologic tests: A paradigm shift in syphilis screening for the 21st century. Clin Infect Dis. 2010;51:700–70. doi: 10.1086/655832. [DOI] [PubMed] [Google Scholar]
- 26.Kobayashi T, Katsumura C, Shoda H, Takai N, Takeda S, Okamoto T, et al. A case of syphilitic uveitis in which vitreous surgery was useful for the diagnosis and treatment. Case Rep Ophthalmol. 2017;8:55–60. doi: 10.1159/000455910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Silpa-Archa S, Preble JM, Foster CS. Vitreous treponemal antibody as a supplementary test to serology for the confirmation of syphilitic chorioretinitis. Retin Cases Brief Rep. 2020;14:166–9. doi: 10.1097/ICB.0000000000000676. [DOI] [PubMed] [Google Scholar]
- 28.Marga GA, Goris and Rudy A. Hartskeertl. Leptospirosis serodiagnosis by the microscopic agglutination test. Curr Protoc Microbiol. 2014;32 doi: 10.1002/9780471729259.mc12e05s32. Unit 12E. 5. [DOI] [PubMed] [Google Scholar]
- 29.Haake DA, Levett PN. Leptospirosis in humans. Curr Top Microbiol Immunol. 2015;387:65–97. doi: 10.1007/978-3-662-45059-8_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schoen RT. Lyme disease: Diagnosis and treatment. Curr Opin Rheumatol. 2020;32:247–54. doi: 10.1097/BOR.0000000000000698. [DOI] [PubMed] [Google Scholar]
- 31.Paris DH, Dumler JS. State of the art of diagnosis of rickettsial diseases: The use of blood specimen for diagnosis of scrub typhus, spotted fever group rickettsiosis and murine typhus. Curr Opin Infect Dis. 2016;29:433–9. doi: 10.1097/QCO.0000000000000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sood A, Rani S, Thakur K, Chauhan V, Jaryal SC, Sood A. Comparison of Weil Felix Test and IgM ELISA in the diagnosis of Scrub Typhus in Kangra, Himachal Pradesh. Int J Health Sci Res. 2016;6:28–32. [Google Scholar]
- 33.Laboratory testing for the diagnosis of HIV infection: Updated recommendations. CDC 2014. [Last accessed on 2020 Mar 10]. Available from http://dx.doi.org/10.15620/cdc.23447 .
- 34.Fearon M. The laboratory diagnosis of HIV infections. Can J Infect Dis Med Microbiol. 2005;16:26–30. doi: 10.1155/2005/515063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barik SK, Mohanty KK, Bisht D. An overview of enzyme immunoassay: The test generation assay in HIV/AIDS testing. J AIDS Clin Res. 2018;9:762. [Google Scholar]
- 36.Sands A. Consolidated Guidelines on HIV Testing Services: 5Cs: Consent, Confidentiality, Counselling, Correct Results and Connection 2015. Geneva: World Health Organization; 2015. Jul, [Last accessed on 2020 Mar 10]. Diagnostics for HIV diagnosis. ANNEX 7. Available from: https://www.ncbi.nlm.nih.gov/books/NBK316033/ [PubMed] [Google Scholar]
- 37.Mehra B, Bhattar S, Bhalla P, Rawat D. Rapid Tests versus ELISA for Screening of HIV Infection: Our Experience from a Voluntary Counselling and Testing Facility of a Tertiary Care Centre in North India. ISRN AIDS. 2014;2014:296840. doi: 10.1155/2014/296840. Published 2014 Apr 7. doi:10.1155/2014/296840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Knox CM, Chandler D, Short GA. Polymerase chain reaction-based assays of vitreous samples for the diagnosis of viral retinitis. Use in diagnostic dilemmas. Ophthalmology. 1998;105:37–44. doi: 10.1016/s0161-6420(98)71127-2. [DOI] [PubMed] [Google Scholar]
- 39.Farhadi A, Haniloo A, Fazaeli A. PCR-based diagnosis of Toxoplasma parasite in ocular infections having clinical indications of toxoplasmosis. Iran J Parasitology. 2017;12:56–62. [PMC free article] [PubMed] [Google Scholar]
- 40.Khairallah M, Chee SP, Rathinam SR, Attia S, Nadella V. Novel infectious agents causing uveitis. Int Ophthalmol. 2010;30:465–83. doi: 10.1007/s10792-009-9319-6. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. New ed. Geneva, Switzerland: WHO; 2009. [PubMed] [Google Scholar]
- 42.Beaty BJ, Calisher CH, Shope RE. Arboviruses. In: Lennette ELD, Lennette E, editors. Diagnostic Procedures for Viral, Rickettsial, and Chlamydial Infections. Washington, DC: American Public Health Association; 1995. pp. 189–212. [Google Scholar]
- 43.Katzelnick LC, Coloma J, Harris E. Dengue: Knowledge gaps, unmet needs and research priroties. Lancet Infect Dis. 2017;17:e88–100. doi: 10.1016/S1473-3099(16)30473-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vu DM, Jungkind D, Angelle Desiree LaBeaud. Chikungunya virus. Clin Lab Med. 2017;37:371–82. doi: 10.1016/j.cll.2017.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Montoya G, Liesenfeld O. Toxoplasmosis. Lancet. 2004;363:1965–76. doi: 10.1016/S0140-6736(04)16412-X. [DOI] [PubMed] [Google Scholar]
- 46.Silveira C, Belfort R, Jr, Muccioli C, Abreu MT, Martins MT, Victora C, et al. A follow-up study of Toxoplasma gondii infection in southern Brazil. Am J Ophthalmol. 2001;131:351–54. doi: 10.1016/s0002-9394(00)00830-8. [DOI] [PubMed] [Google Scholar]
- 47.Stanford MR, Tan HK, Gilbert RE. Toxoplasmic retinochoroiditis presenting in childhood: Clinical findings in a UK survey. Br J Ophthalmol. 2006;90:1464–7. doi: 10.1136/bjo.2005.083543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Da Mata AP, Orefice F. Toxoplasmosis. In: Foster CS, Vitale AT, editors. Diagnosis and Treatment of Uveitis. Philadelphia: WB Saunders; 2002. pp. 385–410. [Google Scholar]
- 49.Dhumne M, Sengupta C, Kadival G, Rathinaswamy A, Velumani A. National seroprevalence of Toxoplasma gondii in India. J Parasitol. 2007;93:1520–1. doi: 10.1645/GE-1159.1. [DOI] [PubMed] [Google Scholar]
- 50.Filisetti D, Candolfi E. Immune response to Toxoplasma gondii. Ann Ist Super Sanita. 2004;40:71–80. [PubMed] [Google Scholar]
- 51.Villard O, Cimon B, L'Olliver C, Fricker-Hidalgo H, Godineau N, Houze S, et al. Seological diagnosis of Toxoplasma gondii infection: Recommendations from the French national reference center for toxoplasmosis. Diagn Microbiol Infect Dis. 2016;84:22–33. doi: 10.1016/j.diagmicrobio.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 52.Desmonts G. Definitive serological diagnosis of ocular toxoplasmosis. Arch Ophthalmol. 1966;76:839–51. doi: 10.1001/archopht.1966.03850010841012. [DOI] [PubMed] [Google Scholar]
- 53.Fekkar A, Bodaghi B, Touafek F, Le Hoang P, Mazier D, Paris L. Comparison of immunoblotting, calculation of the Goldmann-Witmer coefficient, and real-time PCR using aqueous humor samples for diagnosis of ocular toxoplasmosis. J Clin Microbiol. 2008;46:1965–7. doi: 10.1128/JCM.01900-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Abd El-Aal NF, Basha MAA, Eid AM. New insight into the diagnostic cut-off value of serum anti-Toxocara IgG for ocular toxocariasis in uveitis patients. J Helminthol. 2018;94:e12. doi: 10.1017/S0022149X18000895. [DOI] [PubMed] [Google Scholar]
- 55.Rubinsky-Elefant G, Yamamoto JH, Hirata CE, Prestes-Carneiro LE. Toxocariasis: Critical analysis of serology in patients attending a public referral center for ophthalmology in Brazil. Jpn J Ophthalmol. 2018;62:77–83. doi: 10.1007/s10384-017-0543-8. [DOI] [PubMed] [Google Scholar]
- 56.Inchauspe S, Echandi LV, Dodd EM. Diagnosis of ocular toxocariasis by detecting antibodies in the vitreous humor. Arch Soc Esp Oftalmol. 2018;93:220–4. doi: 10.1016/j.oftal.2017.11.012. [DOI] [PubMed] [Google Scholar]
- 57.Satoh M, Vazquez-Del Mercado M, Chan EK. Clinical interpretation of antinuclear antibody tests in systemic rheumatic diseases. Mod Rheumatol. 2009;19:219–28. doi: 10.1007/s10165-009-0155-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kumar Y, Bhatia A, Minz RW. Antinuclear antibodies and their detection methods in diagnosis of connective tissue diseases: A journey revisited. Diagn Pathol. 2009;4:1. doi: 10.1186/1746-1596-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tan EM, Feltkamp TE, Smolen JS, Butcher B, Dawkins R, Fritzler MJ, et al. Range of antinuclear antibodies in “healthy” individuals. Arthritis Rheum. 1997;40:1601–11. doi: 10.1002/art.1780400909. [DOI] [PubMed] [Google Scholar]
- 60.Shaikh MF, Jordan N, D'Cruz DP. Systemic lupus erythematosus. Clin Med (Lond) 2017;17:78–83. doi: 10.7861/clinmedicine.17-1-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ghosh P, Dwivedi S, Naik S, Agarwal V, Verma A, Aggarwal A, et al. Antinuclear antibodies by indirect immunofluorescence: Optimum screening dilution for diagnosis of systemic lupus erythematosus. Indian J Med Res. 2007;126:34–8. [PubMed] [Google Scholar]
- 62.Rosenbaum JT, Wernick R. The utility of routine screening of patients with uveitis for systemic lupus erythematosus or tuberculosis. A Bayesian analysis. Arch Ophthalmol. 1990;108:1291–3. doi: 10.1001/archopht.1990.01070110107034. [DOI] [PubMed] [Google Scholar]
- 63.Gallagher K, Viswanathan A, Okhravi N. Association of systemic lupus erythematosus with uveitis. JAMA Ophthalmol. 2015;133:1190–3. doi: 10.1001/jamaophthalmol.2015.2249. [DOI] [PubMed] [Google Scholar]
- 64.Arevalo JF, Lowder CY, Muci-Mendoza R. Ocular manifestations of systemic lupus erythematosus. Curr Opin Ophthalmol. 2002;13:404–10. doi: 10.1097/00055735-200212000-00011. [DOI] [PubMed] [Google Scholar]
- 65.Nangia PV, Viswanathan L, Kharel R, Biswas J. Retinal involvement in systemic lupus erythematosus. Lupus Open Access. 2017;2:1000129. [Google Scholar]
- 66.Tugal-Tutkun I, Havrilkova K, Power WJ, Foster JS. Changing patterns of uveitis of childhood. Ophthalmology. 1996;103:375–83. doi: 10.1016/s0161-6420(96)30682-9. [DOI] [PubMed] [Google Scholar]
- 67.Kump LI, Cervantes-Castaneda RA, Androudi SN. Analysis of pediatric uveitis cases at a tertiary referral center. Ophthalmology. 2005;112:1287–92. doi: 10.1016/j.ophtha.2005.01.044. [DOI] [PubMed] [Google Scholar]
- 68.Campanilho-Marques R, Bogas M, Ramos F, Santos MJ, Fonseca JE. Prognostic value of antinuclear antibodies in juvenile idiopathic arthritis and anterior uveitis. Results from a systematic literature review. Acta Rheumatol Port. 2014;39:116–22. [PubMed] [Google Scholar]
- 69.Woreta F, Thorne JE, Jabs DA, Kedhar SR, Dunn JP. Risk factors for ocular complications and poor visual acuity at presentation among patients with uveitis associated with juvenile idiopathic arthritis. Am J Ophthalmol. 2007;143:647–55. doi: 10.1016/j.ajo.2006.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ingegnoli F, Castelli R, Gualtierotti R. Rheumatoid factors: Clinical applications. Dis Markers. 2013;35:727–34. doi: 10.1155/2013/726598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shmerling RH, Delbanco TL. The rheumatoid factor: An analysis of clinical utility. Am J Med. 1991;91:528–34. doi: 10.1016/0002-9343(91)90190-9. [DOI] [PubMed] [Google Scholar]
- 72.Newkirk MM. Rheumatoid factors: What do they tell us? J Rheumatol. 2002;29:2034–40. [PubMed] [Google Scholar]
- 73.Mikuls TR, O'Dell JR, Stoner JA, Parrish LA, Arend WP, Norris JM, et al. Association of rheumatoid arthritis treatment response and disease duration with declines in serumlevels of IgM rheumatoid factor and anticyclic citrullinated peptide antibody. Arthritis Rheum. 2004;50:3776–82. doi: 10.1002/art.20659. [DOI] [PubMed] [Google Scholar]
- 74.Lindqvist E, Eberhardt K, Bendtzen K, Heinegard D, Saxne T. Prognostic laboratory markers of joint damage in rheumatoid arthritis. Ann Rheum Dis. 2005;64:196–201. doi: 10.1136/ard.2003.019992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Itty S, Pulido JS, Bakri SJ, Baratz KH, Matteson EL, Hodge DO. Anti-cyclic citrullinated peptide, rheumatoid factor and ocular symptoms typical of rheumatoid arthritis. Trans Am Ophthalmol Soc. 2008;106:75–83. [PMC free article] [PubMed] [Google Scholar]
- 76.Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, et al. International league of associations for rheumatology classification of juvenile idiopathic arthritis: Second revision, Edmonton, 2001. J Rheumatol. 2004;31:390–2. [PubMed] [Google Scholar]
- 77.El-Banna H, Jiman-Fatani A. Anti-cyclic citrullinated peptide antibodies and paraoxonase-1 polymorphism in rheumatoid arthritis. BMC Musculoskelet Disord. 2014;15:379. doi: 10.1186/1471-2474-15-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Farid SSh, Azizi G, Mirshafiey A. Anti-citrullinated protein antibodies and their clinical utility in rheumatoid arthritis. Int J Rheum Dis. 2013;16:379–86. doi: 10.1111/1756-185X.12129. [DOI] [PubMed] [Google Scholar]
- 79.Weiner M, Segelmark M. The clinical presentation and therapy of diseases related to anti-neutrophil cytoplasmic antibodies (ANCA) Autoimmun Rev. 2016;15:978–82. doi: 10.1016/j.autrev.2016.07.016. [DOI] [PubMed] [Google Scholar]
- 80.Young DW. The antineutrophil antibody in uveitis. Br J Ophthalmol. 1991;75:208–11. doi: 10.1136/bjo.75.4.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ungprasert P, Crowson CS, Cartin-Ceba R, Garrity JA, Smith WM, Specks U, et al. Clinical characteristics of inflammatory ocular disease in anti-neutrophil cytoplasmic antibody associated vasculitis: A retrospective cohort study. Rheumatology (Oxford) 2017;56:1763–70. doi: 10.1093/rheumatology/kex261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hagen EC, Van de Vijver-Reenalda H, de Kiezer RJW, Kijlstra A, Van Es LA, Daha MR, et al. Uveitis and anti-neutrophil cytoplasmic antibodies. Clin Exp Immunol. 1994;95:56–9. doi: 10.1111/j.1365-2249.1994.tb06014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fauci AS, Haynes BJ, Katz P, Wolff SM. Wegener's granulomatosis: Prospective clinical and therapeutic experience with 85 patients for 21 years. Ann Intern Med. 1983;98:76–85. doi: 10.7326/0003-4819-98-1-76. [DOI] [PubMed] [Google Scholar]
- 84.Englund M, Merkel PA, Tomasson G, Segelmark M, Mohammad AJ. Comorbidities in patients with antineutrophil cytoplasmic antibody-associated vasculitis versus the general population. J Rheumatol. 2016;43:1553–8. doi: 10.3899/jrheum.151151. [DOI] [PubMed] [Google Scholar]
- 85.Reinhold-Keller E, Beuge N, Latza U, de Groot K, Rudert H, Nölle B, et al. An interdisciplinary approach to the care of patients with Wegener's granulomatosis.Long-term outcome in 155 patients. Arthritis Rheum. 2000;43:1021–32. doi: 10.1002/1529-0131(200005)43:5<1021::AID-ANR10>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 86.Cornec D, Cornec-Le Gall E, Fervenza FC, Specks U. ANCA-associated vasculitis-clinical utility of using ANCA specificity to classify patients. Nat Rev Rheumatol. 2016;12:570–9. doi: 10.1038/nrrheum.2016.123. [DOI] [PubMed] [Google Scholar]
- 87.Madden K, Chabot-Richards D. HLA testing in the molecular diagnostic laboratory. Virchows Arch. 2019;474:139–47. doi: 10.1007/s00428-018-2501-3. [DOI] [PubMed] [Google Scholar]
- 88.Pichi F, Carrai P, Srivastava SK, Lowder CY, Nucci P, Neri P. Genetic of uveitis. Int Ophthalmol. 2016;36:419–33. doi: 10.1007/s10792-015-0136-9. [DOI] [PubMed] [Google Scholar]
- 89.Berger A. HLA typing. BMJ. 2001;322:218. doi: 10.1136/bmj.322.7280.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zamecki KJ, Jabs DA. HLA typing in uveitis: Use and misuse. Am J Ophthalmol. 2010;149:189–93e2. doi: 10.1016/j.ajo.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 91.Jabs DA, Busingye J. Approach to the diagnosis of the uveitides. Am J Ophthalmol. 2013;156:228–36. doi: 10.1016/j.ajo.2013.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yang MM, Lai TY, Luk FO, Pang CP. The roles of genetic factors in uveitis and their clinical significance. Retina. 2014;34:1–11. doi: 10.1097/IAE.0b013e31829f7415. [DOI] [PubMed] [Google Scholar]
- 93.Minos E, Barry RJ, Southworth S, Folkard A, Murray PI, Duker JS, et al. Birdshot chorioretinopathy: Current knowledge and new concepts in pathophysiology, diagnosis, monitoring and treatment. Orphanet J Rare Dis. 2016;11:61. doi: 10.1186/s13023-016-0429-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Papadia M, Herbort CP., Jr New concepts in the appraisal and management of birdshot retinochoroiditis, a global perspective. Int Ophthalmol. 2015;35:287–301. doi: 10.1007/s10792-015-0046-x. [DOI] [PubMed] [Google Scholar]
- 95.Sabhapandit S, Murthy SI, Singh VM, Gaitonde K, Gopal M, Marsonia K, et al. Epidemiology and clinical features of uveitis from urban populations in South India. Ocul Immunol Inflamm. 2017;25(Supl 1):S39–45. doi: 10.1080/09273948.2016.1236971. [DOI] [PubMed] [Google Scholar]
- 96.Biswas J, Kharel Sitaula R, Multani P. Changing uveitis patterns in South India - Comparison between two decades. Indian J Ophthalmol. 2018;66:524–7. doi: 10.4103/ijo.IJO_851_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dogra M, Singh R, Agarwal A, Sharma A, Singh SR, Gautam N, et al. Epidemiology of uveitis in a tertiary-care referral institute in North India. Ocul Immunol Inflamm. 2017;25(Sup 1):S46–53. doi: 10.1080/09273948.2016.1255761. [DOI] [PubMed] [Google Scholar]
- 98.Borde P, Priyanka, Kumar K, Takkar B, Sharma B. Pattern of uveitis in a tertiary eye care center of central India: Results of a prospective patient database over a period of two years. Indian J Ophthalmol. 2020;68:476–81. doi: 10.4103/ijo.IJO_1724_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Das D, Bhattacharjee H, Bhattacharyya PK, Jain L, Panicker MJ, Das K, et al. Pattern of uveitis in North East India: A tertiary eye care center study. Indian J Ophthalmol. 2009;57:144–6. doi: 10.4103/0301-4738.45506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rani R, Marcos C, Lazaro AM, Zhang Y, Stastny P. Molecular diversity of HLA-A, -B and -C alleles in a North Indian population as determined by PCR-SSOP. Int J Immunogenet. 2007;34:201–8. doi: 10.1111/j.1744-313X.2007.00677.x. [DOI] [PubMed] [Google Scholar]
- 101.Dedhia L, Gadekar S, Mehta P, Parekh S. HLA haplotype diversity in the South Indian population and its relevance. Indian J Transplant. 2015;9:138–43. [Google Scholar]
- 102.Kankonkar S, Sangita R, Sonal T. HLA antigen distribution in selected population groups from Maharashtra. Int J Hum Genet. 2004;4:115–8. [Google Scholar]
- 103.Chang JH, McCluskey PJ, Wakefield D. Acute anterior uveitis and HLA-B27. Surv Ophthalmol. 2005;50:364–88. doi: 10.1016/j.survophthal.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 104.Kopplin LJ, Mount G, Suhler EB. Review for disease of the year: Epidemiology of HLA-B27 associated ocular disorders. Ocul Immunol Inflamm. 2016;24:470–5. doi: 10.1080/09273948.2016.1175642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.D'Ambrosio EM, La Cava M, Tortorella P, Gharbiya M, Campanella M, Iannetti L. Clinical features and complications of the HLA-B27-associated acute anterior uveitis: A metanalysis. Semin Ophthalmol. 2017;32:689–701. doi: 10.3109/08820538.2016.1170158. [DOI] [PubMed] [Google Scholar]
- 106.Khan MA, Haroon M, Rosenbaum JT. Acute anterior uveitis and spondyloarthritis: More than meets the eye. Curr Rheumatol Rep. 2015;17:59. doi: 10.1007/s11926-015-0536-x. [DOI] [PubMed] [Google Scholar]
- 107.Haroon M, O'Rourke M, Ramasamy P, Murphy CC, FitzGerald O. A novel evidence-based detection of undiagnosed spondyloarthritis in patients presenting with acute anterior uveitis: The DUET (Dublin Uveitis Evaluation Tool) Ann Rheum Dis. 2015;74:1990–5. doi: 10.1136/annrheumdis-2014-205358. [DOI] [PubMed] [Google Scholar]
- 108.Mishra MN, Bharucha KM. HLA-B27 association with uveitis in an Asian Indian population. Iran J Immunol. 2011;8:85–9. [PubMed] [Google Scholar]
- 109.Malaviya AN, Sawhney S, Mehra NK, Kanga U. Seronegative arthritis in South Asia: An up-to-date review. Curr Rheumatol Rep. 2014;16:413. doi: 10.1007/s11926-014-0413-z. [DOI] [PubMed] [Google Scholar]
- 110.Bajwa A, Osmanzada D, Osmanzada S, Khan I, Patrie J, Xin W, et al. Epidemiology of uveitis in the mid-Atlantic United States. Clin Ophthalmol. 2015;9:889–901. doi: 10.2147/OPTH.S80972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Luca C, Raffaella A, Sylvia M, Valentina M, Fabiana V, Marco C, et al. Changes in patterns of uveitis at a tertiary referral center in Northern Italy: Analysis of 990 consecutive cases. Int Ophthalmol. 2018;38:133–42. doi: 10.1007/s10792-016-0434-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Grajewski RS, Caramoy A, Frank KF, Rubbert-Roth A, Fätkenheuer G, Kirchhof B, et al. Spectrum of uveitis in a German tertiary center: Review of 474 consecutive patients. Ocul Immunol Inflamm. 2015;23:346–52. doi: 10.3109/09273948.2014.1002567. [DOI] [PubMed] [Google Scholar]
- 113.Bodaghi B, Cassoux N, Wechsler B, Hannouche D, Fardeau C, Papo T, et al. Chronic severe uveitis: Etiology and visual outcome in 927 patients from a single center. Medicine (Baltimore) 2001;80:263–70. doi: 10.1097/00005792-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 114.Haridas V, Shetty P, Kumar MN, Vasanthakumar KC, Haridas K, Khode V, et al. Human leukocyte Antigen-B*27 allele subtype prevalence and disease association of ankylosing spondylitis among south Indian population. Indian J Rheumatol. 2018;13:38–43. [Google Scholar]
- 115.Gul A, Ohno S. HLA-B*51 and behçet disease. Ocul Immunol Inflamm. 2012;20:37–43. doi: 10.3109/09273948.2011.634978. [DOI] [PubMed] [Google Scholar]
- 116.Criteria for diagnosis of Behcet's disease. International study group for Behcet's disease. Lancet. 1990;335:1078–80. [PubMed] [Google Scholar]
- 117.Namba K, Goto H, Kaburaki T, Kitaichi N, Mizuki N, Asukata Y, et al. A major review: Current aspects of ocular Behçet's disease in Japan. Ocul Immunol Inflamm. 2015;23(Suppl 1):S1–23. doi: 10.3109/09273948.2014.981547. [DOI] [PubMed] [Google Scholar]
- 118.International Team for the Revision of the International Criteria for Behçet's Disease (ITR-ICBD) The International Criteria for Behçet's Disease (ICBD): A collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol. 2014;28:338–47. doi: 10.1111/jdv.12107. [DOI] [PubMed] [Google Scholar]
- 119.Ng JY, Luk FO, Lai TY, Pang CP. Influence of molecular genetics in Vogt-Koyanagi-Harada disease. J Ophthalmic Inflamm Infect. 2014;4:20. doi: 10.1186/s12348-014-0020-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Tang WM, Pulido JS, Eckels DD, Han DP, Mieler WF, Pierce K. The association of HLA-DR15 and intermediate uveitis. Am J Ophthalmol. 1997;123:70–5. doi: 10.1016/s0002-9394(14)70994-8. [DOI] [PubMed] [Google Scholar]
- 121.Raja SC, Jabs DA, Dunn JP, Fekrat S, Machan CH, Marsh MJ, et al. Pars planitis: Clinical features and class II HLA associations. Ophthalmology. 1999;106:594–9. doi: 10.1016/S0161-6420(99)90122-7. [DOI] [PubMed] [Google Scholar]
- 122.Schmidt H, Williamson D, Ashley-Koch A. HLA-DR15 haplotype and multiple sclerosis: A HuGE review. Am J Epidemiol. 2007;165:1097–109. doi: 10.1093/aje/kwk118. [DOI] [PubMed] [Google Scholar]
- 123.Levinson RD, Park MS, Rikkers SM, Reed EF, Smith JR, Martin TM, et al. Strong associations between specific HLA-DQ and HLA-DR alleles and the tubulointerstitial nephritis and uveitis syndrome. Invest Ophthalmol Vis Sci. 2003;44:653–7. doi: 10.1167/iovs.02-0376. [DOI] [PubMed] [Google Scholar]


