Abstract
Purpose:
Re-emergent ocular syphilis in patients with Human immunodeficiency virus (HIV) co-infection has both diagnostic and management difficulties because of the overlapping risk factors. The clinical manifestations described in non-HIV may not be the same in patients with HIV coinfection. Immune recovery uveitis (IRU) may also alter the course of the disease causing recurrences. We studied the clinical features in correlation with CD4 counts, systemic immune status, sexual preferences and management outcomes in HIV/AIDS patients with ocular syphilis in the highly active antiretroviral treatment (HAART) era from a high endemic HIV population like India.
Methods:
Retrospective analysis of all patients with ocular syphilis and HIV/AIDS seen between 2016 and 2019 was done.
Results:
A total of 33 patients (56 eyes) with a CD4 count range of 42–612 cells/cu.mm were included. Ocular syphilis was found to be higher in individuals with high risk behavior such as men who have sex with men (MSMs) (45%). Panuveitis was the commonest manifestation (53.57%) and was even the presenting feature of HIV and syphilis in many patients. Significant vitritis, usually uncommon in HIV/AIDS immunocompromised patients was noted even with low CD4 counts in patients with ocular syphilis. Significant correlation was noted between ocular presentation and CD4 counts (P < 0.05).
Conclusion:
Ocular syphilis presents differently in patients with HIV/AIDS. Diffuse retinitis is seen commonly in low counts (<100 cells/cu.mm). Classical placoid chorioretinitis lesions usually described in non-HIV individuals is uncommon in HIV patients and is seen in higher CD4 counts ( >400 cells/cu.mm). Ocular manifestations can be an indicator of the immune status of the patient. Not all patients with ocular manifestations have associated features of systemic syphilis. Ocular manifestations can be the first presentation of HIV/AIDS. Although, there is good response to systemic penicillin and HAART, recurrences and immune recovery uveitis (IRU) can also occur.
Keywords: HIV, AIDS, Men who have sex with men (MSM), Necrotizing retinitis, Ocular syphilis, Penicillin, Placoid chorioretinitis, HAART
Ocular syphilis, can result either from acquired or congenital infection and because of its varied manifestations, is aptly termed the “great masquerader.”[1,2] It is usually seen in the active secondary syphilis stage but can also occur during the tertiary or latent phase of systemic disease. It has to be considered and managed as neurosyphilis. Although syphilis was highly endemic in the pre-antibiotic era, it nearly disappeared in the high-income countries after the discovery of penicillin and there was a corresponding decline in the incidence of ocular syphilis. However, the last few years have seen a resurgence of syphilitic uveitis in the developed as well as developing nations.[3,4] This resurgence is especially common in individuals co-infected with human immunodeficiency virus (HIV).[5] The risk factors for HIV and syphilis are overlapping and include heterosexual unprotected promiscuous sex, male homosexuality, and exchange of sex for drugs.[5,6] The coexistence of both diseases can make the diagnosis and management of both difficult. Coexisting HIV infection has also been incriminated as a cause of increased risk of ocular syphilis relapses. The clinical manifestations which have been described in non-HIV individuals are not always the same as those found in patients with co-existing HIV infection.[7] Ocular syphilis in patients with HIV/AIDS and its correlation to the systemic immune status, CD4 counts, sexual preferences, and its response to highly active antiretroviral treatment (HAART) and anti-syphilitic treatment have not been described especially from a high-endemic HIV population like India.
Immune recovery uveitis (IRU), in patients with ocular syphilis, can alter the course of the disease and may cause ocular morbidity due to recurrent inflammation.[8,9,10]
We describe the ocular features and treatment outcome in correlation to systemic status in HIV/AIDS patients with ocular syphilis in the current era of HAART.
Methods
All patients with a diagnosis of HIV and ocular syphilis seen in the previous 3 years (2016-2019) were included. A diagnosis of ocular syphilis was made based on clinical suspicion and positive syphilis serology. Blood investigations and aqueous aspirate findings, whenever done, to rule out other ocular opportunistic infections (OI), were noted and analysed. Every patient had undergone complete ophthalmic examination and laboratory investigations including ELISA for toxoplasma, HIV and syphilis serology, Mantoux test and chest X-ray. Ancillary investigations findings including fundus fluorescein angiography (FFA), optical coherence tomography (OCT), and/or ultrasonography (USG) whenever done were noted and analysed.
Patients not known to be HIV positive underwent testing in the form of ELISA followed by Western blot for confirmation either at our center or at the HIV/AIDS care center where they were referred for further management of the systemic condition.
Complete systemic evaluation and management was done under the care of an HIV/AIDS physician at a specialized tertiary AIDS care center. A retrospective analysis of all these findings was performed. The study was approved by the institutional ethics committee. All patients were confirmed to have syphilis based both on positive Treponema serologic test (Treponema pallidum hemagglutination or fluorescent Treponema antigen–antibody) and positive non-Treponema test (Venereal Disease Research Laboratory/Rapid plasma reagin). The clinical outcomes after treatment along with follow-up serology titers were analyzed.
A diagnosis of recurrence was made when there was reactivation of inflammation after complete resolution with treatment and if associated with high titers of RPR/TPHA with low or insignificant increase in CD4 counts.
A diagnosis of IRU was made in patients on HAART with resolved primary lesions, if signs of active inflammation were noted and if associated with increased CD4 counts, reduced RPR/TPHA titers and/or low HIV loads.
Statistical analysis was done to note the association between CD4 counts and the phenotypic presentation and vitritis and also between baseline RPR/TPHA values and the clinical phenotypes with the help of Pearson Chi-Square tests. Patients were grouped based on their CD4 counts into those less than 100 cells/cu.mm, 101–250 cells/cu.mm, and those greater than 250 cells/cu.mm. SPSS software version 21.0 was used for the same. A 'P' value < 0.05 was considered statistically significant.
Results
A total of 33 patients (56 eyes) were included in the study. Twenty three patients had bilateral presentation while 10 patients had unilateral presentation. There were 31 males and 2 females in the study. The age range of the patients was 24–60 years and the mean age at presentation was 38.3 ± 11.24 years and the median age was 38 years. Twenty-four patients were known HIV-positive patients, while 9 patients were detected with HIV while investigating for ocular disease. HAART was initiated soon after the diagnosis in all newly diagnosed patients. In the remaining 24 patients, the mean duration from HIV diagnosis to presentation with ocular disease was 15.95 months and all these patients were already on HAART at ocular presentation. The range of CD4 counts at presentation was 42–612 cells/cu.mm. The mean CD4 count was 252.69 ± 148.1 cells/cu.mm (Median count-212 cells/cu.mm). Sexual orientation of the patients was enquired and was found that 18 patients (males 16, females 2) were heterosexual and 15 of them were MSMs (men having sex with men). Of the 15 patients, four of them were bisexual and 11 were male homosexuals. On specific questioning, five patients, when presenting with ocular complaints, revealed to have associated genital ulcers and two of them had cutaneous lesions as well.
Ocular manifestations
Panuveitis was the commonest, seen in 30 eyes, followed by posterior uveitis in 12 eyes, vitritis alone in 10 eyes, and anterior uveitis in 4 eyes. Overall, diffuse retinitis/retinochoroiditis [Fig. 1a and b] was the commonest fundus picture seen in 19 eyes; retinitis pigmentosa (RP)-like picture was found in 11 eyes and placoid chorioretinitis [Fig. 2] was found in 6 eyes. Panuveitis was the commonest presentation and was seen in a wide range of CD4 counts. Panuveitis presentations included – non-granulomatous anterior uveitis with vitritis which was associated with diffuse retinitis/retinochoroiditis in 13 eyes, RP like picture in 9 eyes, placoid chorioretinitis in 5 eyes, retinal vasculitis in 2 eyes, and optic disc edema in one eye. Posterior uveitis was noted in 12 eyes which included diffuse retinitis/retinochoroiditis in 6 eyes, retinal vasculitis in 3 eyes [Fig. 3], RP like picture in 2 eyes and placoid chorioretinitis in 1 eye.
Figure 1.
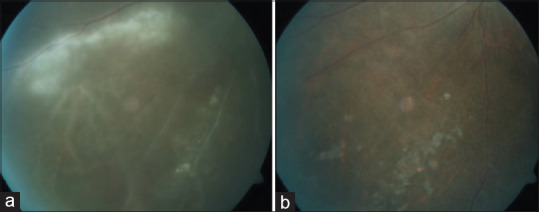
(a and b)– Composite color fundus picture showing diffuse necrotizing retinitis in a patient with ocular syphilis (pre-treatment) (a) and resolved retinitis (post-treatment) (b)
Figure 2.
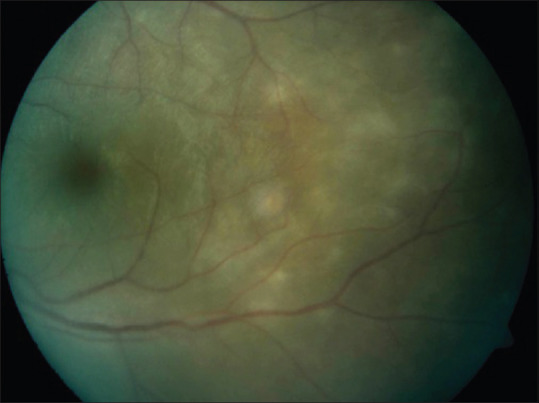
Color fundus photograph showing placoid chorioretinitis lesions
Figure 3.
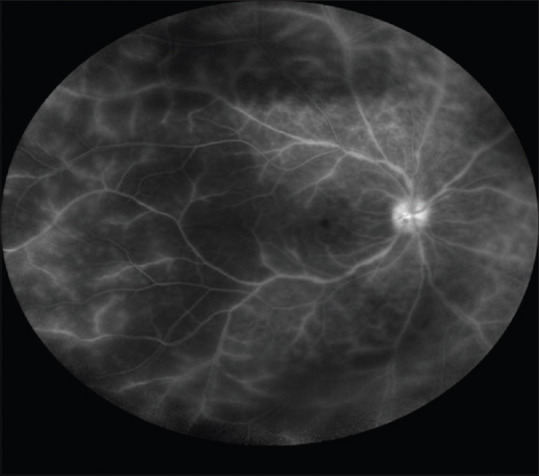
Ultrawide field FFA picture of the right eye showing extensive retinal perivasculitis
Significant vitreous inflammation of more than 2+ vitreous haze was noted in patients even with CD4 counts <100 cells/cu.mm. There was no significant difference in the severity of vitritis in patients with low, moderate, or high CD4 counts (P = 0.150). No association was noted between the baseline RPR/TPHA values and vitreous inflammation (P = 0.679).
Diffuse necrotizing retinitis was commonly seen in patients with low and/or moderate CD4 counts (< 250 cells/cu.mm), while placoid chorioretinitis was seen in patients with higher CD4 counts only (> 400 cells/ cu.mm). The Chi-square test results showed a “P” value of 0.04 (P < 0.05) denoting a significant correlation between the phenotypic variants and the CD4 counts. However, no statistical association was noted between the baseline RPR/TPHA values and the pattern of ocular manifestation among the patients in our study (P = 0.209).
Among patients with vitritis in our study, four of them presented with snowball like opacities and in one of them, the other eye had panuveitis with retinitis. Anterior uveitis was of the nongranulomatous type with moderate to severe anterior segment inflammation. All other known infective and inflammatory causes attributable to HIV and related ocular OIs were ruled out by blood investigations and/or aqueous tap evaluation wherever required. The clinical presentations are summarized in Table 1.
Table 1.
List of clinical features, laboratory investigations, and treatment of all patients included in the study
| Age | Sex | Laterality | CD4 @ presentation cells/cu.mm | RPR/TPHA | Ocular features | Treatment | Visual outcome | F/U (months) | HIV duration | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|
| 49 | M | B/L | 113 | RPR>1:32 TPHA>1:1280 |
OU-Panuveitis | CP + systemic steroids | Improved | 8 | 1d | Retinitis, Vitritis 2 + 1st diagnosis HIV |
| 56 | M | B/L | 432 | RPR>1:32 TPHA>1:1280 |
OD - Panuveitis OS - Anterior uveitis | CP + Systemic steroids Doxycycline | Worsened | 24 | 36 m | Placoid Chorioretinitis Vitritis 2+ |
| 28 | F | B/L | 218 | RPR 1:16, TPHA 1:640 | OU - Anterior | CP + topical | Improved | 12 | 18 m | |
| 25 | M | B/L | 382 | RPR>1:32 TPHA>1:1280 |
OD - Panuveitis OS - Vitritis 3+ | CP + steroids | Worsened Improved | 58 | 1d | 1st diagnosis HIV RP like picture |
| 55 | M | U/L | 198 | VDRL>1:16 TPHA -> 1:640 |
OS - Vitritis 2+ | CP + systemic steroids | Improved | 9 | 12 | Snowball Complicated Cataract |
| 29 | M | U/L | 386 | RPR>1:16, RPHA 1:640 | OD Anterior | CP + topical Doxycycline |
Stable | 8 | 38 m | NGA |
| 47 | M | B/L | 120 | RPR>1:32 TPHA>1:1280 |
OU - Posterior uveitis | CP + steroids Doxycycline |
Worsened | 6 | 1d | 1st diagnosis HIV Macular scar Retinal vasculitis Complicated cataract |
| 29 | M | B/L | 472 | RPR 1:16, RPHA 1:640 | OU - Panuveitis | CP + steroids | Improved | 30 | 1m | Vitritis 2+Retinal vasculitis Placoid Chorioretinitis |
| 27 | M | U/L | 83 | RPR - 1:32 TPHA - 1:640 |
OS - Posterior uveitis | CP + steroids | Worsened | 6 | 1d | 1st diagnosis HIV Retinitis scarred macula |
| 25 | M | B/L | 96 | RPR>1:32 TPHA>1:1280 |
OD - Posterior uveitis OS - Vitritis 2+ | CP + steroids | Same | 26 | 60m | Retinal vasculitis |
| 24 | M | B/L | 128 | RPR - 1:32 TPHA - 1:640 |
OU - Panuveitis | CP + steroids | Improved | 8 | 12 m | Vitritis 2+Retinitis Optic Atrophy |
| 27 | M | B/L | 148 | RPR - 1:32 TPHA - 1:640 |
OU - Posterior uveitis | CP + steroids | Same | 6 | 12 m | RPE mottling RP like picture |
| 43 | M | B/L | 600 | RPR - 1:32 TPHA - 1:640 | OU - Vitritis 3+ | CP + Steroids | Improved | 8 | 96 m | OS - status post vitreo retinal surgery |
| 36 | M | U/L | 160 | RPR - 1:32 TPHA - 1:640 |
OS - Posterior uveitis | CP + systemic steroids | Improved | 18 | 18 m | Retinitis |
| 39 | M | B/L | 612 | RPR - 1:32 TPHA - 1:640 |
OU- Panuveitis | CP + steroids | Worsened | 23 | 6m | Vitritis 2 + Complicated cataract Vitreous debris Placoid chorioretinitis |
| 60 | M | B/L | 42 | RPR - 1:32 TPHA - 1:640 |
OU - Panuveitis | CP + steroids | Improved | 6 | 1d | Vitritis 1 + Macular scar Healed retinitis Complicated Cataract 1st diagnosis HIV |
| 38 | M | U/L | 269 | RPR>1:32 TPHA>1:1280 |
OD- Panuveitis | CP + steroids | Improved | 20 | 1m | Vitritis 2 + Retinitis/disc edema |
| 31 | M | B/L | 515 | RPR>1:32 TPHA>1:1280 |
OU - Panuveitis | CP + steroids | Worsened | 8 | 1m | Vitritis 2 + Retinal detachment Optic atrophy |
| 28 | M | U/L | 159 | RPR>1:32 TPHA>1:1280 |
OS - Panuveitis | CP + steroids | Worsened | 12 | 36m | Retinal detachment |
| 53 | M | B/L | 57 | RPR>1:32 TPHA>1:1280 |
OU- Panuveitis | CP + steroids | Worsened | 11 | 24 | Vitritis 1 + Retinal detachment/Retinitis |
| 52 | F | U/L | 308 | RPR>1:32 TPHA>1:1280 |
OD - Posterior uveitis | CP + steroids Doxycycline |
Stable | 9 | 58 | Diffuse retinochoroiditis |
| 30 | M | B/L | 220 | RPR>1:32 TPHA>1:1280 |
OU - Vitritis 2+ | CP + Steroids | Stable | 8 | 1d | 1st diagnosis HIV Snowball |
| 59 | M | U/L | 250 | RPR>1:32 TPHA>1:1280 |
OS - Posterior uveitis | CP + steroids | Improved | 10 | 60 m | Retinitis |
| 43 | M | B/L | 182 | RPR>1:32 TPHA>1:1280 |
OU- Panuveitis | CP + steroids | Improved | 6 | 1d | Vitritis 2+RP like picture 1st diagnosis HIV |
| 54 | M | B/L | 232 | RPR 1:16, RPHA 1:640 | OU - Vitritis 2+ | CP + steroids | Improved | 8 | 24m | Snowballs |
| 28 | M | B/l | 212 | RPR>1:32 TPHA>1:1280 |
OU - Posterior uveitis | CP + steroids Ozurdex Cataract Surgery |
Improved | 36 | 1d | 1st diagnosis HIV Retinitis Complicated Cat |
| 38 | M | B/L | 171 | RPR>1:32 TPHA>1:1280 |
OU - Panuveitis | CP + Steroids | Improved | 8 | 1d | Vitritis 2+RP like picture 1st diagnosis HIV |
| 32 | M | U/L | 186 | RPR>1:32 TPHA>1:1280 |
OS - Vitritis 2+ | CP + steroids | Improved | 19 | 2m | |
| 46 | M | B/L | 212 | RPR 1:16, RPHA 1:640 | OU - Panuveitis | CP + steroids Cefalosporin | Improved | 23 | 1m | Vitritis 1+RP like picture/RPE mottling |
| 45 | M | B/L | 235 | VDRL>1:32 TPHA>1:1280 |
OU -Panuveitis | CP + steroids | Improved | 7 | 30m | Vitritis 2+Diffuse retinochoroiditis |
| 24 | M | U/L | 435 | VDRL>1:32 TPHA>1:1280 |
OS -Posterior uveitis | CP + steroids | Improved | 10 | 18m | Placoid Chorioretinitis |
| 38 | M | B/L | 180 | VDRL>1:32 TPHA>1:1280 |
OU-Panuveitis | CP + steroids | Improved | 8 | 1m | Vitritis 2 + Diffuse retinochoroiditis |
| 28 | M | B/L | 326 | RPR>1:32 TPHA>1:1280 |
OU -Panuveitis | CP, Cefixime, steroids | Stable | 10 | 48 | RP-like picture/RPE mottling |
OD - Right eye, OS - Left eye, OU- Both eyes. RPR - Rapid plasma reagin, VDRL - Venereal disease lab test, TPHA - Treponema pallidum hemagglutination assay. U/L - Unilateral, B/L- Bilateral, CP - Crystalline penicillin, Duration - d (days), m (months), RP - Retinitis pigmentosa, RPE - Retinal pigment epithelium
A total of 11 patients had undergone CSF analysis as advised by the treating physician, and in three of them, CSF showed significantly raised TPHA titers. Other systemic associations included three patients with Hepatitis B infection and three patients in maintenance phase of anti-tuberculosis therapy (ATT) for systemic tuberculosis. None of these patients had any active ocular lesion attributable to their systemic opportunistic infection (OI).
The median RPR titer was 1:32 (range 1:8 to 1:128) and the median TPHA was 1:1280 (range 1:640 to 1:5120). The follow-up titers were done after 2, 6, and 12 weeks and at 6 months. The RPR titers showed a decreasing trend at 2 weeks in 16 patients, at 6 weeks in nine patients, and at 3 months in six others. In two patients, there was persistent raised titers which reached the normal at about 4 months. At 6-month follow-up, all the patients had normal titers.
All patients were treated under the care of an infectious disease specialist at a specialized HIV/AIDS care center with standard HAART regimen. The treatment regimen for syphilis included intravenous (IV) benzyl penicillin for 10 to 14 days along with monitored systemic anti-inflammatory therapy in the form of low-dose prednisolone whenever required under the care of an infectious disease specialist [Fig. 4a and b]. There was no difference in the mean-time of regression of lesions between previously known HIV patients on HAART and the newly detected ones. Alternate regimens included cephalosporins and doxycycline especially for patients allergic to penicillin [Table 1].
Figure 4.
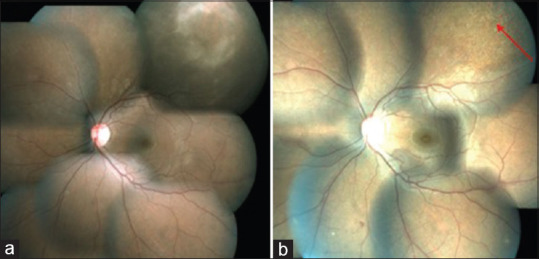
Montage color fundus images of left eye of a patient with ocular syphilis showing retinitis (a) (pre-treatment) and resolved lesions (b) (post-treatment)
Four patients with recurrences after 6 weeks were retreated with long-term penicillin therapy. There was no definite association found with the baseline RPR/TPHA values, CD4 counts, or initial severity of inflammation as possible risk factors for recurrence in these patients.
Two patients had recurrent inflammation after 3 months despite reduced RPR titers. They had increased CD4 counts and low HIV loads. They were diagnosed to have immune recovery uveitis (IRU) with significant vitritis and persistent cystoid macular edema (CME). They were retreated with topical steroids and/or periocular triamcinolone acetonide. A maintenance dose of topical nonsteroidal anti-inflammatory drugs was advised for 3-6 months.
The mean logMAR visual acuity at presentation was 1.205 or a Snellen equivalent of 20/320 which improved to a logMAR value of 0.63 or a Snellen equivalent of 20/80 at final follow up visit. The mean duration follow-up was 14.58 months (range 6 to 58 months). Two eyes developed cataract during the follow-up period and underwent cataract surgery with intraocular lens implantation. Therapeutic vitrectomy was performed in two other eyes for dense persistent vitreous opacification. At final follow-up, vision improved or remained stable in 42 eyes and worsened in 14 eyes. Causes of worsening visual acuity included epiretinal membrane (ERM) formation, progression of tractional retinal detachment (TRD) and progression of cataract among others. At final follow-up of 6 months, all patients had reduced titers of non-Treponema tests with complete control of inflammation and no recurrences.
Discussion
Ocular syphilis has varied manifestations and there has been a re-emergence in the current era especially in patients with HIV.[1,2] In a large study published in the pre-HAART era from our center, it was found that only 1.2% of patients had ocular syphilis.[11] It is interesting to note that while other OIs in patients with HIV/AIDS on HAART are on the decline, unprecedented rise in syphilis is being noted. Although a strong association of genital ulcers in syphilis facilitating HIV infection has been considered, it was noted in only about 15 percent of our patients in the current study.[11]
Male preponderance was noted as in other studies. Socioeconomic factors alone appear insufficient to explain the predominance of males as sexual orientation also seems to play a significant role. Fifteen of our patients were MSMs (either male homosexuals or bisexuals) pointing to the increased risk of such sexual behavior for syphilis.[12,13] All patients in whom ocular syphilis was the first presentation of HIV were MSMs. Considering the stigma and medicolegal issues attached to it, it is possible that the numbers in this group might be higher than those who had confessed to the same. Studies have shown this to be a high-risk behavior for incidence of sexually transmitted infections (STI) including syphilis and HIV.[12,13] This subpopulation of MSM may require access to STI screening at close intervals.
Optic neuritis and anterior uveitis were reported to be common in earlier studies. A relatively less number seen in the current study can be attributed to the fact that our study included ambulatory patients who presented to us with ocular complaints. A study on severely ill non-ambulatory patients, with associated neurosyphilis, could possibly record more cases of syphilitic optic neuritis.
Re-emergent syphilis seems to present with significant inflammation in the HAART era,[14,15] with panuveitis seen in more than half of our patients. Vitritis with snow ball–like opacities were also noted in a few patients. In patients presenting with panuveitis or vitritis, significant inflammation was noted even with CD4 < 100 cells/cu.mm. It was found that CD4 counts at presentation may not have a significant association in the occurrence or severity of vitritis (P = 0.150).
Ocular syphilis is known to mimic other infectious and noninfectious uveitic entities even in non-HIV individuals.[3] While distinctive patterns include posterior placoid chorioretinitis,[16] punctate inner retinitis,[17] or white focal preretinal opacities, wider spectrum of manifestations such as anterior uveitis (both granulomatous and nongranulomatous), intermediate uveitis, and scleritis have also been described in non-HIV individuals.[18] Anterior uveitis as the only presentation of ocular syphilis is reported to be lesser in patients with HIV, where posterior and panuveitis predominate. This was the finding noted even in our study.
A diffuse retinitis/retinochoroiditis type of presentation was the commonest in our study. Although it was noted even in patients with CD4 counts >250 cells/cu.mm, diffuse atypical retinitis was more commonly seen in association with lower and moderate CD4 counts (<250 cells/cu.mm) in our study. Significantly, the classical placoid chorioretinitis, commonly described in non-HIV patients, was seen in patients with higher CD4 counts only (>400 cells/cu.mm). There is a need to be cautious in not misdiagnosing syphilitic retinitis as CMV retinitis or ocular toxoplasmosis which can also present in HIV/AIDS patients with lower CD4 counts.
Studies have shown the usefulness of optical coherence tomography (OCT) in patients with ocular syphilis.[19] Although, OCT may not be conclusive in defining etiology, it has been found to be useful in grading the lesion, identifying the layers involved and in prognostication.
About 1/4th of the patients, had significantly raised titres,[20,21] even at the end of 6 weeks which resolved by 3 months after treatment with doxycycline.[20] Recurrences presented mainly as vitritis and/or as cystoid macular edema (CME). Post-treatment IRU can be seen in HIV patients with ocular syphilis as was seen in our patients and can also present with CME.[8]
Studies have reported significant differences in the visual morbidity between HIV-positive and HIV-negative patients mainly due to the anatomical location of the uveitis; the incidence rates being higher with posterior/panuveitis while being lesser for anterior segment manifestations. However, otherwise, rates of vision loss and changes in follow-up visual acuity in HIV patients were equivalent to those reported in HIV-negative individuals with similar ocular manifestations, especially in the HAART era.[22]
Associated systemic syphilitic features were uncommonly seen in our study; three of them had genital ulcers and three patients had raised titers in CSF although without confirmed neurological features.[21] Several studies have reported an RPR titer of >1:32 and a reactive CSF Treponema pallidum hemagglutination assay (CSF TPHA) titer of ≥1:640 in HIV co-infected patients with clinical and CSF abnormalities to be consistent with neurosyphilis.[21] Ocular syphilis can occur during the latent phase of the disease.
In the current era of HAART, although the incidence of opportunistic infections (OIs) like CMV retinitis is decreasing, ocular syphilis is on the rise. The immune reconstitution due to HAART does not seem to offer any preventive influence in the occurrence of ocular syphilis, but can help early resolution of the manifestations along with systemic penicillin. Hence, the disease remains a major threat, especially more so now in patients with HIV/AIDS even if on HAART.[23]
The study has its limitations inherent in any retrospective study. Medline search did not reveal any larger case series of ocular syphilis reported in the current era of HAART in HIV/AIDS patients in a high-endemic HIV population like India. It is of more significance, considering the rise in systemic syphilitic patients especially in HIV individuals with changing social habits and behavior in the Indian population.
Conclusion
Ocular syphilis can have varied presentations and is on the rise. A high index of suspicion is needed to diagnose these cases. Panuveitis is the most common ocular manifestation and can even be the presenting feature of HIV/AIDS. Hence in all patients with ocular syphilis underlying HIV infection needs to be ruled out. Patients with higher CD4 counts presented with placoid chorioretinits while diffuse necrotizing retinitis was seen in patients with lower CD4 counts and these lesions should not be mistaken for CMV or toxoplasmic retinitis. Thus, the phenotype of ocular syphilitic presentation can be an indicator of the immune status of the patient. MSMs who are reported to be at a higher risk for syphilis also seem to be at a higher risk for ocular syphilis. Although, syphilitic uveitis usually responds well to systemic penicillin, these patients can have recurrences and need retreatment. IRU, commonly considered in patients post-CMVR and ocular TB, is also seen post syphilitic uveitis. They need to be managed with appropriate anti-inflammatory therapy with caution.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chao JR, Khurana RN, Fawzi AA, Reddy HS, Rao NA. Syphilis: Reemergence of an old adversary. Ophthalmology. 2006;113:2074–9. doi: 10.1016/j.ophtha.2006.05.048. [DOI] [PubMed] [Google Scholar]
- 2.Fonollosa A, Giralt J, Pelegrín L, Sánchez-Dalmau B, Segura A, García-Arumí J, et al. Ocular syphilis–back again: Understanding recent increases in the incidence of ocular syphilitic disease. Ocul Immunol Inflamm. 2009;17:207–12. doi: 10.1080/09273940902741709. [DOI] [PubMed] [Google Scholar]
- 3.Davis JL. Ocular syphilis. Curr Opin Ophthalmol. 2014;25:513–8. doi: 10.1097/ICU.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 4.Oliver GF, Stathis RM, Furtado JM, Arantes TE, McCluskey PJ, Matthews JM, et al. Current ophthalmology practice patterns for syphilitic uveitis. Br J Ophthalmol. 2019;103:1645–9. doi: 10.1136/bjophthalmol-2018-313207. [DOI] [PubMed] [Google Scholar]
- 5.Mitchell JP, Huang LL, Rosberger DF. Ocular syphilis in patients with Human Immunodeficiency Virus infection. J Natl Med Assoc. 2015;107:130–2. doi: 10.1016/S0027-9684(15)30037-7. [DOI] [PubMed] [Google Scholar]
- 6.Lee SY, Cheng V, Rodger D, Rao N. Clinical and laboratory characteristics of ocular syphilis: A new face in the era of HIV co-infection. J Ophthalmic Inflamm Infect. 2015;5:56. doi: 10.1186/s12348-015-0056-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shen J, Feng L, Li Y. Ocular syphilis: An alarming infectious eye disease. Int J Clin Exp Med. 2015;8:7770–7. [PMC free article] [PubMed] [Google Scholar]
- 8.Dutta PM, Mayilvakanam L, Palker AH, Sridharan S, Biswas J. Intravitreal sustained-release dexamethasone implant for the treatment of persistent cystoid macular edema in ocular syphilis. Indian J Ophthalmol. 2019;67:1487–90. doi: 10.4103/ijo.IJO_1795_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lautredou CC, Hardin JS, Chancellor JR, Uwaydat SH, Ellabban AA, Sallam AB. Repeat intravitreal dexamethasone implant for refractory cystoid macular edema in syphilitic uveitis. Case Rep Ophthalmol Med. 2018;19:7419823. doi: 10.1155/2018/7419823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Balaskas K, Sergentanis TN, Giulieri S, Guex-Crosier Y. Analysis of significant factors influencing visual acuity in ocular syphilis. Br J Ophthalmol. 2011;95:1568–72. doi: 10.1136/bjo.2010.194498. [DOI] [PubMed] [Google Scholar]
- 11.Sudharshan S, Kaleemunnisha S, Banu AA, Shrikrishna SS, George AE, Babu RB, et al. Ocular lesions in 1,000 consecutive HIV-positive patients in India: A long-term study. J Ophthalmic Inflamm Infect. 2013;3:2. doi: 10.1186/1869-5760-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bernstein KT, Stephens SC, Strona FV, Kohn RP, Philip SS. Epidemiologic characteristics of an ongoing syphilis epidemic among men who have sex with men, San Francisco. Sex Transm Dis. 2013;40:11–7. doi: 10.1097/OLQ.0b013e31827763ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Werner RN, Gaskins M, Nast A, Dressler C. Incidence of sexually transmitted infections in men who have sex with men and who are at substantial risk of HIV infection – A meta-analysis of data from trials and observational studies of HIV pre-exposure prophylaxis. PLoS One. 2018;13:e0208107. doi: 10.1371/journal.pone.0208107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chhablani JK, Biswas J, Sudharshan S. Panuveitis as a manifestation of ocular syphilis leading to HIV diagnosis. Oman J Ophthalmol. 2010;3:29–31. doi: 10.4103/0974-620X.60019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rishi E, Govindarajan MV, Biswas J, Agarwal M, Sudharshan S, Rishi P. Syphilitic uveitis as the presenting feature of HIV. Indian J Ophthalmol. 2016;64:149–50. doi: 10.4103/0301-4738.179714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eandi CM, Neri R, Adelman AR, Yanuzzi AL, Cunningham ET International syphilis study group. Acute syphilitic posterior placoid chorioretinitis: Report of a case series and comprehensive review of the literature. Retina. 2012;32:1915–41. doi: 10.1097/IAE.0b013e31825f3851. [DOI] [PubMed] [Google Scholar]
- 17.Wickremasinghe S, Ling C, Stawell R, Yeoh J, Hall A, Zamir E. Syphilitic punctate inner retinitis in immunocompetent gay men. Ophthalmology. 2009;116:1195–200. doi: 10.1016/j.ophtha.2008.12.055. [DOI] [PubMed] [Google Scholar]
- 18.Furtado JM, Arantes TE, Nascimento H, Vasconcelos-Santos DV, Noguiera N, de Pinho QR, et al. Clinical manifestations and ophthalmic outcomes of ocular syphilis at a time of re-emergence of the systemic infection. Sci Rep. 2018;8:12071. doi: 10.1038/s41598-018-30559-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schlaen A, Aquino MP, Ormaechea MS, Couto C, Saravia M. Spectral optical coherence tomography findings in an adult patient with syphilitic bilateral posterior uveitis and unilateral punctate inner retinitis. Am J Ophthalmol Case Rep. 2019;15:100489. doi: 10.1016/j.ajoc.2019.100489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.González-López JJ, Guerrero MLF, Luján R, Tostado SF, de Górgolas M, Requena L. Factors determining serologic response to treatment in patients with syphilis. Clin Infect Dis Off Publ Infect Dis Soc Am. 2009;49:1505–11. doi: 10.1086/644618. [DOI] [PubMed] [Google Scholar]
- 21.Marra CM, Maxwell CL, Smith SL, Lukehart SA, Rompalo AM, Eaton M, et al. Cerebrospinal fluid abnormalities in patients with syphilis: Association with clinical and laboratory features. J Infect Dis. 2004;189:369–76. doi: 10.1086/381227. [DOI] [PubMed] [Google Scholar]
- 22.Mathew D, Smit D. Clinical and laboratory characteristics of ocular syphilis and neurosyphilis among individuals with and without HIV infection. Br J Ophthalmol. 2020 doi: 10.1136/bjophthalmol-2019-315699. doi: 101136/bjophthalmol-2019-315699. [DOI] [PubMed] [Google Scholar]
- 23.Testi I, Mahajan S, Agrawal R, Agarwal A, Marchese A, Curi A, et al. Management of intraocular infections in HIV. Ocul Immunol Inflamm. 2020;14:1–10. doi: 10.1080/09273948.2020.1727533. [DOI] [PubMed] [Google Scholar]


