Abstract
Aims
There are reports of a marked increase in perioperative mortality in patients admitted to hospital with a fractured hip during the COVID-19 pandemic in the UK, USA, Spain, and Italy. Our study aims to describe the risk of mortality among patients with a fractured neck of femur in England during the early stages of the COVID-19 pandemic.
Methods
We completed a multicentre cohort study across ten hospitals in England. Data were collected from 1 March 2020 to 6 April 2020, during which period the World Health Organization (WHO) declared COVID-19 to be a pandemic. Patients ≥ 60 years of age admitted with hip fracture and a minimum follow-up of 30 days were included for analysis. Primary outcome of interest was mortality at 30 days post-surgery or postadmission in nonoperative patients. Secondary outcomes included length of hospital stay and discharge destination.
Results
In total, 404 patients were included for final analysis with a COVID-19 diagnosis being made in 114 (28.2%) patients. Overall, 30-day mortality stood at 14.4% (n = 58). The COVID-19 cohort experienced a mortality rate of 32.5% (37/114) compared to 7.2% (21/290) in the non-COVID cohort (p < 0.001). In adjusted analysis, 30-day mortality was greatest in patients who were confirmed to have COVID-19 (odds ratio (OR) 5.64, 95% confidence interval (CI) 2.95 to 10.80; p < 0.001) with an adjusted excess risk of 20%, male sex (OR 2.69, 95% CI 1.37 to 5.29; p = 0.004) and in patients with ≥ two comorbidities (OR 4.68, CI 1.5 to 14.61; p = 0.008). Length of stay was also extended in the COVID-19 cohort, on average spending 17.6 days as an inpatient versus 12.04 days in the non-COVID-19 group (p < 0.001).
Conclusion
This study demonstrates that patients who sustain a neck of femur fracture in combination with COVID-19 diagnosis have a significantly higher risk of mortality than would be normally expected.
Cite this article: Bone Joint Open 2020;1-11:697–705.
Keywords: Hip fracture, Neck of femur fracture, NOF, Coronavirus, COVID-19
Introduction
Despite a nationally imposed lockdown in the UK to combat COVID-19, the number of elderly patients admitted to hospital with fractured neck of femur (NOF) has remained fairly consistent1,2 The most recent report from the National Hip Fracture Database for England, Wales and Northern Ireland concluded that for the year 2018 there were 66,140 hip fractures, with an annualized 30-day mortality of 6.1% across 175 trusts.3 Many patients who sustain a fractured NOF live in institutional care, where there is considerable risk of COVID-19 infection.4
Trauma teams from the USA, Spain, Italy, and regions of the UK have all published their preliminary data on the effect COVID-19 has had on patients with fractured NOF, with all observing a marked increase in perioperative mortality.5-9 The team from the USA5 included 136 NOF fracture patients from seven emergency departments in the city and county of New York. Of these, 31 were deemed COVID-19 positive with 11 (34.5%) patients not surviving beyond 30 days post-surgery. Similar mortality figures among their respective COVID-19 positive cohorts were observed by the Spanish (30.4%, 7/23) and Italian (43.75%, 4/31) teams.6,7 Within the UK, regional teams have published their own cohort results, identifying the prevalence of COVID-19 to range from 19.4% (82/422) in London to 8.5% (27/317) in Scotland, with 30-day mortality rates of 30.5% (25/82) and 33.3% (9/27), respectively.8,9
This study aims to understand the perioperative clinical outcome for elderly patients admitted to hospital with NOF fracture during the COVID-19 pandemic in the UK. Our primary objectives were to report the 30-day mortality for patients admitted to hospital with a fractured NOF and report the prevalence of COVID-19 in this same cohort.
Methods
This was a multicentre observational cohort study involving a collaboration between ten orthopaedic units within England, with the region of West Midlands supplying majority of centres (Supplementary Table i).
Local collaborators from each centre collected data both retrospectively and prospectively from the 1 March 2020 to 6 April 2020. The ten centres see approximately 3,775 patients per year and so we anticipated 400 to 435 patients in the study period. Patients were identified from handover lists, theatre operating, and local hospital digital systems. Patients ≥ 60 years of age admitted to ten hospitals who had sustained a fractured NOF were included in the study. We excluded patients with pelvic fractures, femoral shafts fractures and periprosthetic fractures.
Ethics
The study was registered with the research and audit department of each participating UK centre. As we were using routinely collected anonymized data, formal research ethics approval was not required. We used the online National Research Ethics Service decision tool (http://www.hra-decisiontools.org.uk) to confirm this.
Outcomes
Primary outcome was mortality at 30 days post-surgery. In addition to this, patients were followed up throughout their hospital stay in order to determine two cohorts. The COVID-19 cohort was based on either a positive virology test (SARS-CoV-2 RNA reverse transcription polymerase chain reaction (RT-PCR) detection), or suspected signs, symptoms of COVID-19 and/or imaging (chest radiograph or CT). The non-COVID-19 cohort was based on either a negative virology test (SARS-CoV-2 RNA RT-PCR detection) or not fulfilling the Public Health England (PHE) criteria required for COVID-19 testing (applicable to all NHS hospitals during the time of this study).
Patients
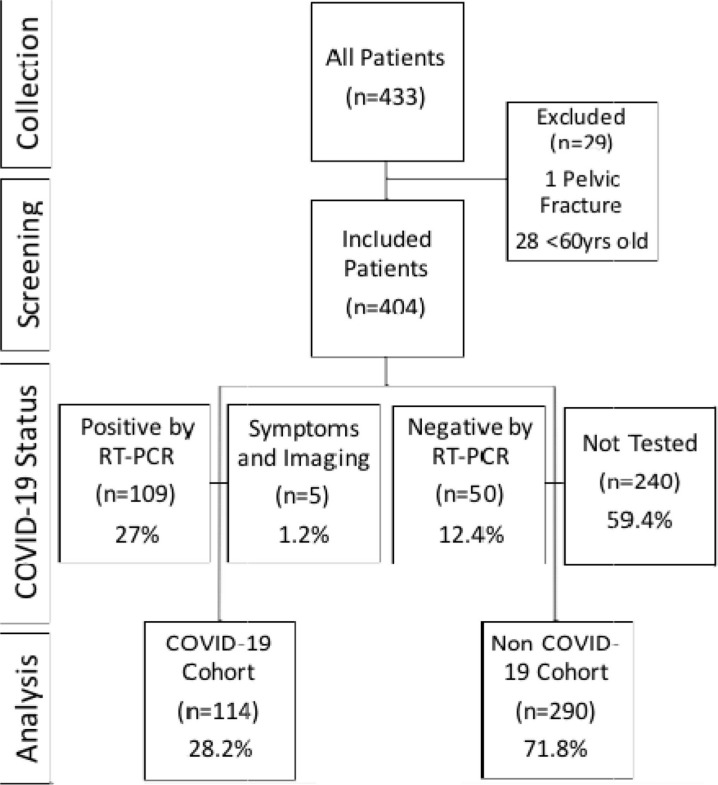
We obtained data from ten centres which entered 433 patients. Of these, 404 patients met our inclusion criteria. COVID-19 diagnosis was made in 114 patients (28.2%), with 109 RT-PCR confirmations (27%), while five patients (1.2%) had their diagnosis confirmed from clinical signs and imaging. Fifty patients (12.4%) had negative RT-PCR results whereas 245 patients (60.6%) did not meet PHE criteria for testing (Figure 1).
Fig. 1.
Flow diagram depicting included patients for analysis. RT-PCR, reverse transcription polymerase chain reaction.
Confounding variables
We collected the following variables: age, sex, type of fracture, type of surgery, type of anaesthesia, ASA (American Society of Anasthesiologists) grading, and side of injury. We also collected variables needed to calculate the Nottingham Hip Fracture Score (NHFS); admission haemoglobin (Hb), pre-admission living status, history of malignancy, Abbreviated Mental Test Score (AMTS), and number of comorbidities.10 The variables were input on a predesigned database and only those with < 20% missing data were reported within this study. In addition to this, the National Hip Fracture Database was accessed by each institution and patients cross referenced for data completion.
Statistical analysis
Data are reported in accordance with Strengthening The Reporting of Observational studies in Epidemiology guidelines for Observational Studies and Statistical Analyses and Methods in the Published Literature guidelines.11 Data were summarized using descriptive statistics including count and percentages for categorical variables. Continuous variables were described using the mean and SD. To test for differences in variables and outcomes, we used chi-squared and Fisher’s exact test for categorical variables and Mann-Whitney U test for continuous variables as appropriate. A multivariate logistic regression model was fitted to assess the impact of COVID-19 on mortality at 30 days while adjusting for potential confounders. The variables included in the multivariate logistic regression model were selected based on the statistically significant results of univariate logistic regression model including only one potential predictor. Adjusted excess mortality rate was obtained as the difference of the averages of the predicted mortality probabilities of the adjusted model assuming all patients had COVID-19 and assuming they did not have COVID-19. A two-sided p-value of < 0.05 was considered statistically significant. All analysis were performed using IBM SPSS v. 26 (Armonk, New York, USA) software for Mac.12
Results
Cohort characteristics
Patients with a diagnosis of COVID-19 tended to be older (mean age 85.16 years (SD 8.67) vs 82.88 years (SD 8.59); p = 0.017, Mann-Whitney U test), had larger proportion of males (37.7% (n = 43) vs 27.6% (n = 80); p = 0.046, chi-squared test), were more likely to come from institutional care (26.3% (n = 30) vs 20.3% (n = 59); p = 0.038, chi-squared test), as well as obtain higher mean ASA (3.16 (SD 0.68) vs 3.01 (0.63); p = 0.04, Mann-Whitney U test) and mean NHFS (5.51 (SD 1.5) vs 5.08 (SD 1.54); p = 0.012, Mann-Whitney U test) scores. While surgical interventions between the two groups proved similar, it was noted that the two cohorts had equal distribution of patients managed non-operatively. Table I describes the other variables collected among further sub grouping for age, time to surgery, AMTS, ASA, NHFS, of which none demonstrated statistical significance between the cohorts.
Table I.
Characteristics for COVID-19 status.
| Variable | Total | COVID-19 (n = 114) | Non-COVID-19 (n = 290) | p-value |
|---|---|---|---|---|
| Mean age, yrs (SD) | 83.52 (8.66) | 85.16 (8.67) | 82.88 (8.59) | 0.017* |
| Age, n (%) | ||||
| < 85 | 194 (48) | 44 (38.6) | 150 (51.7) | 0.017† |
| ≥ 85 | 210 (52) | 70 (61.4) | 140 (48.3) | |
| Sex, n (%) | ||||
| Male | 123 (30.4) | 43 (37.7) | 80 (27.6) | 0.046† |
| Female | 281 (69.6) | 71 (62.3) | 210 (72.4) | |
| NOF type, n (%) | ||||
| Extracapsular | 206 (51) | 53 (46.5) | 153 (52.8) | 0.257† |
| Intracapsular | 198 (49) | 61 (53.5) | 137 (47.2) | |
| Side of injury n (%) | ||||
| Right | 191 (47) | 58 (50.9) | 133 (45.9) | 0.376† |
| Left | 209 (52) | 54 (47.4) | 155 (53.4) | |
| Unknown | 4 (1) | 2 (1.8) | 2 (0.7) | |
| Pre-admission residence, n (%) | ||||
| Home | 309 (76.5) | 80 (70.2) | 229 (79) | 0.038† |
| Institution | 89 (22) | 30 (26.3) | 59 (20.3) | |
| Unknown | 6 (1.5) | 4 (3.5) | 2 (0.7) | |
| Mean AMTS (SD) | 7.09 (3.49) | 6.58 (3.92) | 7.27 (3.31) | 0.086* |
| AMTS, n (%) | ||||
| ≥ 7 | 253 (62.6) | 65 (57) | 188 (64.8) | 0.071† |
| ≤ 6 | 128 (31.7) | 38 (33.3) | 90 (31) | |
| Unknown | 23 (5.7) | 11 (9.6) | 12 (4.1) | |
| Mean ASA grade | 3.06 (0.65) | 3.16 (0.68) | 3.01 (0.63) | 0.040* |
| ASA grade, n (%) | ||||
| 1 | 4 (1) | 1 (0.9) | 3 (1) | 0.196† |
| 2 | 54 (13.7) | 12 (10.5) | 42 (14.5) | |
| 3 | 257 (65.2) | 76 (66.7) | 181 (62.4) | |
| 4 | 75 (19) | 30 (26.3) | 45 (15.5) | |
| 5 | 3 (0.8) | 1 (0.9) | 2 (0.7) | |
| 6 | 1 (0.3) | 1 (0.9) | 0 (0) | |
| 1 to 2 | 58 (14.4) | 12 (10.5) | 46 (15.9) | 0.293† |
| 3+ | 336 (83.2) | 98 (86) | 238 (82.1) | |
| Unknown | 10 (2.5) | 4 (3.5) | 6 (2.1) | |
| Mean NHFS (SD) | 5.2 (1.54) | 5.51 (1.5) | 5.08 (1.54) | 0.012* |
| NHFS, n (%) | ||||
| ≤ 5 | 219 (54.2) | 57 (50) | 162 (55.9) | 0.287† |
| ≥ 6 | 185 (45.8) | 57 (50) | 128 (44.1) | |
| Malignancy, n (%) | ||||
| Yes | 52 (13) | 12 (10.5) | 40 (13.8) | 0.368† |
| No | 347 (86) | 101 (88.6) | 246 (84.8) | |
| Unknown | 5 (1) | 1 (0.9) | 4 (1.4) | |
| Preoperative Hb < 100, n (%) | ||||
| Yes | 50 (12) | 17 (14.9) | 33 (11.4) | 0.328† |
| No | 351 (87) | 96 (84.2) | 255 (87.9) | |
| Unknown | 3 (1) | 1 (0.9) | 2 (0.7) | |
| Comorbidities ≥ 2, n (%) | () | () | () | |
| Yes | 303 (75) | 92 (80.7) | 211 (72.8) | 0.087† |
| No | 98 (24) | 21 (18.4) | 77 (26.6) | |
| Unknown | 3 (1) | 1 (0.9) | 2 (0.7) | |
| Surgery, n (%) | ||||
| THA | 13 (3.2) | 4 (3.5) | 9 (3.1) | 0.073† |
| Hemiarthroplasty | 160 (39.6) | 46 (40.4) | 114 (39.3) | |
| DHS | 121 (30.0) | 26 (22.8) | 95 (32.8) | |
| IM nail | 91 (22.5) | 33 (28.9) | 56 (19.3) | |
| Cannulated screws | 6 (1.5) | 0 (0) | 6 (2.1) | |
| Conservative | 10 (2.5) | 5 (4.4) | 5 (1.7) | |
| Unknown | 3 (0.7) | 0 (0) | 3 (1) | |
| Anaesthesia, n (%) | ||||
| GA | 219 (54.2) | 63 (55.3) | 156 (53.8) | 0.376† |
| Spinal | 160 (39.6) | 41 (36) | 119 (41) | |
| N/A | 15 (3.7) | 5 (4.4) | 10 (3.4) | |
| Unknown | 10 (2.5) | 5 (4.4) | 5 (1.7) | |
| Mean time to surgery, days (SD) | 1.46 (1.27) | 1.49 (1.01) | 1.45 (1.36) | 0.756* |
| Time to surgery, n (%) | ||||
| < 48 hrs | 270 (66.8) | 70 (61.4) | 200 (69) | 0.316† |
| ≥ 48 hrs | 118 (29.2) | 38 (33.3) | 80 (27.6) | |
| Unknown/N/A | 16 (4.0) | 6 (5.3) | 10 (3.4) |
Mann-Whitney U test.
Chi-squared test.
AMTS, Abbreviated Mental Test Score; ASA, American Society of Anesthesiologists Score; DHS, dynamic hip screw; GA, general anaesthesia; Hb, haemoglobin; IM, intramedullary; N/A, not applicable; NHFS, Nottingham Hip Fracture Score; NOF, neck of femur fracture; THA, total hip arthroplasty.
Clinical outcomes
Table II demonstrates significant differences in 30-day postoperative mortality between the two groups. Overall, 58 patients (14.4%) did not survive beyond 30 days postoperatively, with the majority of these being in the COVID-19 cohort group (32.5% vs 7.2%; p = < 0.001). Conversely, most (48/58) of the deaths occurred while patients were still in a hospital. The mean length of stay was 17.66 days (SD 11.16), which proved five days longer in the COVID-19 group when compared to the non-COVID-19 group. In terms of timing to COVID-19 status (i.e. positive or negative result), in those that were tested this occurred predominantly in the postoperative period (mean 9.23 days post-surgery (SD 8.06; -4 to 30). However, 15 patients underwent testing prior to their operation with five of them recording a positive COVID-19 result.
Table II.
Outcome measures.
| Variable | Total | COVID-19 (n = 114) | Non-COVID-19 (n = 290) | p-value |
|---|---|---|---|---|
| Status at discharge, n (%) | ||||
| Alive | 358 (88.6) | 84 (73.7) | 274 (94.5) | < 0.001* |
| Deceased | 46 (11.4) | 30 (26.3) | 16 (5.5) | |
| Status at 30 days postoperative, n (%) | ||||
| Alive | 346 (85.6) | 77 (67.5) | 269 (92.8) | < 0.001* |
| Deceased | 58 (14.4) | 37 (32.5) | 21 (7.2) | |
| Discharge destination, n (%) | ||||
| Home | 184 (46) | 42 (22.8) | 142 (77.2) | < 0.001* |
| Rehabilitation facility | 71 (18) | 17 (23.9) | 54 (76.1) | |
| Residential care | 33 (8) | 6 (18.2) | 27 (81.8) | |
| Nursing home | 36 (9) | 8 (22.2) | 28 (77.8) | |
| Other hospital ward | 17 (4) | 3 (17.6) | 14 (82.4) | |
| Inpatient | 12 (3) | 6 (50) | 6 (50) | |
| Deceased at discharge | 45 (11) | 31 (68.9) | 14 (31.1) | |
| Unknown | 6 (1) | 1 (16.7) | 5 (83.3) | |
| Mean LOS, days (SD) | 13.59 (8.81) | 17.66 (11.16) | 12.04 (7.17) | < 0.001† |
| Mean time to COVID-19 diagnosis, days (SD) | 9.23 (8.06) | 10.1 (7.69) | 7.26 (8.58) | < 0.038† |
Chi-squared test
Mann-Whitney U test.
LOS, length of stay.
Modalities used to confirm COVID-19 status
Table III, which corresponds to Figure 1, separates the different methods used to confirm COVID-19 status and their effects on mortality, revealing that patients who were confirmed positive by RT-PCR (31.2%; n = 34) had a significantly higher risk of death compared to negative (16%; n = 8) and not tested cohorts (5.4%; n = 13; p = 0.015, Fisher's exact test).
Table III.
Differences in mortality between the different methods of COVID-19 confirmation at 30 days postoperatively.
| COVID-19 status, n (%) | Total | Alive (n = 346) |
Deceased (n = 58) |
p-value* |
|---|---|---|---|---|
| Positive by RT-PCR | 109 (27.0) | 75 (68.8) | 34 (31.2) | 0.015 |
| Negative by RT-PCR | 50 (12.4) | 42 (84.0) | 8 (16.0) | |
| Not tested | 240 (59.4) | 227 (94.6) | 13 (5.4) | |
| Clinical signs and imaging | 5 (1.2) | 2 (40.0) | 3 (60.0) |
Fisher's exact test.
RT-PCR, reverse transcription polymerase chain reaction.
Predictors of outcome
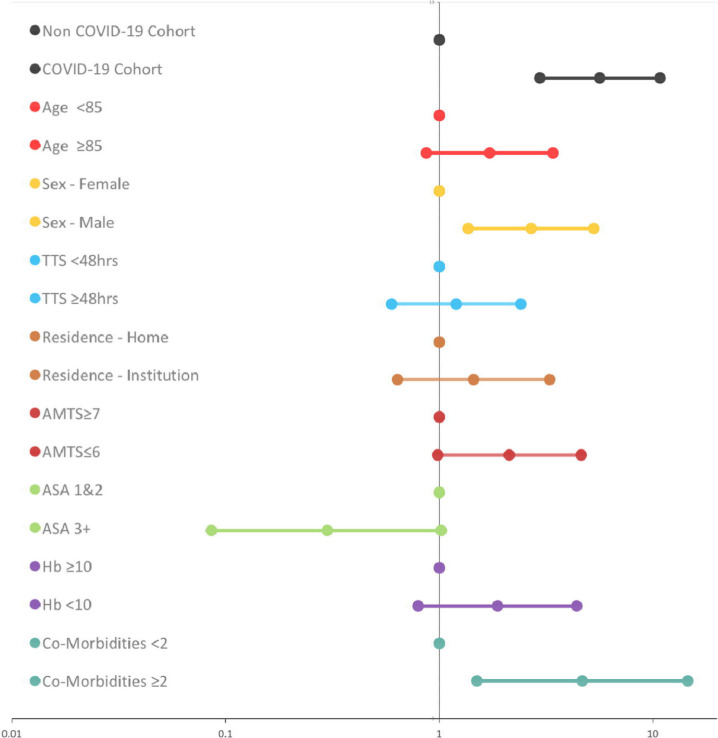
Patients with a proven positive or suspected COVID-19 diagnosis had almost a six fold increased odds of mortality (OR = 5.64, 95% CI 2.95 to 10.80, p < 0.001) and an adjusted excess risk of 20% (Supplementary Table ii). Likewise, when adjusted analysis was made to include the same significant unadjusted covariates, the only predictors that remained relevant were positive COVID-19 diagnosis, male sex, and patients with ≥ two co-morbidities (Table IV and Figure 2).
Table IV.
Unadjusted and adjusted sensitivity analysis of predictors of 30 day postoperative mortality.
| Characteristics | n (% deceased) | Unadjusted analysis | Adjusted analysis (R2 0.312) | ||
|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | ||
| COVID-19 status | |||||
| COVID-19 cohort | 114 (32.5) | 6.15 (3.40 to 11.13) | < 0.001 | 5.64 (2.95 to 10.80) | < 0.001 |
| Non COVID-19 cohort* | 290 (7.2) | N/A | N/A | N/A | N/A |
| Age | |||||
| Mean | N/A | 1.05 (1.01 to 1.08) | 0.015 | N/A | N/A |
| Age < 85 yrs* | 194 (9.8) | N/A | N/A | N/A | N/A |
| Age ≥ 85 yrs | 210 (18.6) | 2.10 (1.17 to 3.78) | 0.013 | 1.72 (0.87 to 3.41) | 0.120 |
| Sex | |||||
| Male | 123 (22.8) | 2.47 (1.40 to 4.35) | 0.002 | 2.69 (1.37 to 5.29) | 0.004 |
| Female* | 281 (10.7) | N/A | N/A | N/A | N/A |
| Time to surgery | |||||
| Mean | N/A | 1.32 (1.09 to 1.59) | 0.004 | N/A | N/A |
| < 48 hrs* | 270 (12.2) | N/A | N/A | N/A | N/A |
| ≥ 48 hrs | 118 (16.9) | 1.47 (0.80 to 2.68) | 0.214 | 1.20 (0.60 to 2.41) | 0.606 |
| Unknown/ N/A | 16 (8.6) | 3.26 (1.07 to 9.99) | 0.038 | 4.12 (0.94 to 18.05) | 0.600 |
| Pre-admission residence | |||||
| Home* | 309 (11.7) | N/A | N/A | N/A | N/A |
| Institutional care | 89 (22.5) | 2.20 (1.20 to 4.03) | 0.011 | 1.44 (0.64 to 3.28) | 0.377 |
| Unknown | 6 (33.3) | 3.79 (0.67 to 21.44) | 0.132 | 1.16 (0.09 to 14.32) | 0.911 |
| AMTS | |||||
| Mean | N/A | 0.87 (0.80 to 0.94) | < 0.001 | N/A | N/A |
| AMTS ≥ 7* | 253 (10.3) | N/A | N/A | N/A | N/A |
| AMTS ≤ 6 | 128 (21.1) | 2.33 (1.30 to 4.20) | 0.005 | 2.13 (0.99 to 4.62) | 0.540 |
| Unknown | 23 (21.7) | 2.43 (0.83 to 7.08) | 0.105 | 1.64 (0.42 to 6.40) | 0.479 |
| ASA score | |||||
| Mean | N/A | 1.95 (1.26 to 3.02) | 0.003 | N/A | N/A |
| ASA 1 and 2* | 58 (12.1) | N/A | N/A | N/A | N/A |
| ASA 3+ | 336 (15.2) | 1.30 (0.56 to 3.03) | 0.538 | 0.30 (0.09 to 1.02) | 0.055 |
| Unknown | 10 (0) | Not estimable | 0.999 | Not estimable | 0.999 |
| NHFS | |||||
| Mean | N/A | 1.68 (1.34 to 2.09) | < 0.001 | N/A | N/A |
| NHFS ≤ 5* | 219 (9.1) | 2.57 (1.44 to 4.60) | 0.001 | N/A | N/A |
| NHFS ≥ 6 | 185 (20.5) | N/A | N/A | N/A | N/A |
| Malignancy | |||||
| Yes | 52 (11.5) | 0.69 (0.08 to 6.29) | 0.741 | N/A | N/A |
| No* | 347 (14.7) | N/A | N/A | N/A | N/A |
| Unknown | 5 (20) | 0.59 (0.05 to 5.47) | 0.588 | N/A | N/A |
| Pre-admission Hb | |||||
| < 10 | 50 (24) | 2.15 (1.05 to 4.41) | 0.038 | 1.87 (0.80 to 4.41) | 0.151 |
| ≥ 10* | 351 (14.8) | N/A | N/A | N/A | N/A |
| Unknown | 3 (33) | 3.4 (0.30 to 38.26) | 0.322 | 6.13 (0.09 to 410.60) | N/A |
| Comorbidities | |||||
| < 2* | 303 (5.1) | N/A | N/A | N/A | N/A |
| ≥ 2 | 98 (17.2) | 3.85 (1.49 to 9.94) | 0.005 | 4.68 (1.50 to 14.61) | 0.008 |
| Unknown | 3 (50) | 9.3 (0.72 to 120.73) | 0.088 | N/A | N/A |
Reference.
AMTS, Abbreviated Mental Test Score; ASA, American Society of Anesthesiologists Score; CI, confidence interval; NHFS, Nottingham Hip Fracture Score; OR, odds ratio.
Fig. 2.
Adjusted analysis for predictors of 30 day postoperative mortality. AMTS, Abbreviated Mental Test Score, ASA, American Society of Anesthesiologists grade, Hb,haemoglobin, TTS, time to surgery.
Discussion
Our study found that perioperative mortality was 14.4% (CI 11.07 to 17.73) across the whole cohort of patients. However, the risk of perioperative mortality was higher among those patients who had a positive test or high clinical suspicion for COVID-19. Furthermore, the overall perioperative mortality in our cohort is higher than data reported in the National Hip Fracture Database for England, Wales and Northern Ireland which reports an overall annualized 30-day mortality rate of 6.1%.3 Our data suggest an almost sixfold increased likelihood of mortality and an adjusted excess risk of 20% among hip fracture patients with a confirmed or suspected COVID-19 status when compared to those without a COVID-19 diagnosis. This also held true for male sex (OR 2.7, 95% CI 1.37 to 5.29) and patients with two or more comorbidities (OR 4.7, 95% CI 1.5 to 14.61) although with reduced odds ratios. Nevertheless, such findings ought to be interpreted with caution as the model of adjusting the analysis to factors that proved significant individually can conclude different results depending on which factors were analyzed, as shown in Supplementary Table iii, which demonstrates an example when combining COVID-19 status, age, sex, TTS, ASA and NHFS, male sex no longer held the same statistical significance. Reassuringly, irrespective of the differing covariates analyzed, positive COVID-19 status holds its clinically and statistically significant impact on mortality.
The exact cause of death was not collected and hence is a limitation of our study’s findings. There was heterogeneity in the way data was obtained with some centres reporting COVID-19 as a cause of death while others did not. Hence we could not group the patients nor could we seek further clarification through official death certificate reports during the early phase of the COVID-19 pandemic when the healthcare system was under significant strain. Furthermore the effects on allied services such as those provided by orthogeriatric colleagues, whose involvement in the care of hip fracture patients has proven to reduce mortality, was not determined within this study and is a further limitation.13
The COVIDSURG international collaborative group reported a 23.8% 30-day mortality rate among 1,128 surgical patients with perioperative COVID-19 infection between 1 January 2020 and 31 March 2020. It is of note that of the 302 orthopaedic patients, 262 were emergency. At least 115 were hip fracture patients (likely more) and though no sub-group analysis was reported, these rates of mortality are certainly similar to those observed in this study and others in significantly affected countries.5-9,14
Overall, 40% (159/404) of the included patients underwent COVID-19 testing by RT-PCR, with 96% (109/114) of the cases confirmed this way. Unfortunately, with our study occurring during the early stages of the pandemic and as per Public Health England guidance, routine laboratory testing across the included centres was not carried out on all patients but instead was limited to only those who experienced symptoms suggestive of the COVID-19 infection. Hence, routine invasive testing of all patients regardless of clinical status would have required further ethical approval. Additionally it would have further strained the healthcare system’s testing capacity which was already under considerable pressure. Routine testing of all emergency patients admitted to NHS hospitals only came in to force on the 27 April 2020.
A small number of patients (5/114, 1.2%) were included within our COVID-19 cohort as their clinical picture and imaging strongly favoured such a diagnosis. Given that COVID-19 diagnosis can be accurately made by appropriate imaging, we felt it valid to include such patients within our analysis.15 Conversely, 12.4% (50/114) of the patients proved negative by RT-PCR. The moderate sensitivity of this test to provide false negative results of 2% to 29% and with our data showing that the positive cohort had a 30-day postoperative mortality of 31.2%, and negative cohort 16%, it is possible that some of the confirmed negative patients were indeed positive and hence misplaced for final analysis.16,17 This is especially notable as the “not tested” cohort demonstrated a mortality rate of 5.4%, which is similar to that observed prior to the pandemic.3
Differences in length of hospital stay between the two cohorts were also observed, with the COVID-19 cohort group having a longer stay by a mean of 5.5 days. While our study was not designed to discern the true reason behind this, it would not be unfair to assume that the positive group were significantly sicker, requiring greater input, effort and time for their care and recovery. Relatedly, with the non-COVID-19 cohort technically being asymptomatic and hence assumed safer for discharge and with hospitals under pressure to retain appropriate capacity for the anticipated COVID-19 peak in early April 2020, it is possible that some of the observed length of hospital stay disparity could be construed to this. Reiterating the false-negative issue with testing, a proportion of otherwise COVID-19 positive patients might have been discharged to institutional care given that the non-COVID-19 group (55/69; 80%) accounted for a large proportion of these. Equally, COVID-19 doesn’t always lead to a clinical manifestation with up to 40% of patients remaining asymptomatic throughout the duration of COVID-19 infection.18,19 From 15 April 2020 it became mandatory for all patients being discharged to care institutions to undergo routine testing prior to discharge from hospital.20
With regard to patients who underwent COVID-19 testing, we found that the majority of testing and subsequent confirmation of a positive result occurred in the postoperative period (mean 9.23 days after surgery (SD 8.06). One could hypothesize that their infection was perhaps secondary to nosocomial spread. However, given the incubation period of COVID-19 (which ranges from 2 to 14 days), such conjecture would be incorrect. It is just as likely that these patients acquired the infection in the community prior to admission.21
We are also aware that there has been a wide regional variation of COVID-19 prevalence and hence our findings must be applied cautiously across the whole of the UK. The West Midlands, which is one of the most populous regions in the UK with 5.9 million inhabitants, was particularly hard hit.22 At the time of undertaking this work, it was the second-worst hit region with COVID-19 disease behind London (43.2 deaths per 100,000).23 Interestingly, there were no observed deaths in the other centre from the northwest of England. Conversely, the two UK-based published studies have reported differences in COVID-19 prevalence among their cohorts with the Scottish team recording a prevalence of 9% while the team from London reported 18%, which are considerably different to our figure of 28%.8,9
The testing strategy in the UK has changed significantly since the undertaking of this study; however, the prevalence of the disease has also evolved. Therefore, though future studies within the UK may provide us with a more accurate reflection of disease prevalence, this will be at a very different stage of the pandemic. Serological antibody testing has now also been introduced and in time this may give us a clearer idea of previous infection rates and regional variability. Additionally, this study was undertaken during the peak of the pandemic in England (R number = 4) and therefore does not reflect the current situation where rates of new infection and mortality have fallen considerably. Nevertheless, COVID-19 prevalence is ever evolving given the developments of September 2020 reporting an increase in the R number from < 1 toward 1.5, hence the findings reported here and elsewhere maintain their importance and relevance.24
The limitations of this study have been alluded to above in terms of data collection, testing variability, sensitivity and geographical differences in COVID-19 prevalence. These were unfortunately unavoidable, with testing variability being a product of Public Health England policy.
Although our sample size may be deemed small given the wide confidence intervals this is nevertheless one of the largest studies looking at the impact of COVID-19 on hip fracture patients worldwide, containing more or an equivalent number of patients to the published studies to date.5-9 Additionally, the presence of the non-COVID-19 comparator allows differences among the two groups to be highlighted unlike the COVIDSURG Collaborative who reviewed only COVID-19 surgical cases.14
The findings from this study clearly demonstrate the significant additional risk to hip fracture patients who develop COVID-19 infection within 30 days of surgery (or admission if managed nonoperatively). It also highlights factors associated with acquiring COVID-19 infection, although the results may not present a new or surprising finding given the detrimental effect COVID-19 has had on the world’s population. We nevertheless feel that this piece of work is important, as it allows us to counsel patients and their families of the potential risks of being admitted with a hip fracture during a period when hospitals are placed under pressure from highly infectious diseases.
Acknowledgements
NOF-COV19 Study Collaborative Group
Local data collection:
Worcestershire Acute Hospitals NHS Trust
Ms Rosemary Wall (SpR in Trauma and Orthopaedics)
Dr Katerina Thomas-Fernandez (Foundation Year Doctor)
Heart of England NHS Foundation Trust
Mr Rajpreet Sahemey (SpR in Trauma and Orthopaedics)
Mr Ciaran Nolan (SpR in Trauma and Orthopaedics)
Mr Mohammed Remtulla (SpR in Trauma and Orthopaedics)
Mrs Caroline Plant (SpR in Trauma and Orthopaedics)
The Royal Wolverhampton NHS Trust
Mr Sukhraj Dhillon (Consultant)
Mr Sabri Bleibeh (SpR in Trauma and Orthopaedics)
Mr Abdus Burahee (CT2)
Mr Suribabu Gudipati (SpR in Trauma and Orthopaedics)
Sandwell and West Birmingham NHS Trust
Mr Kanthan Theivendran (Consultant)
Mr Chiranjit De (SpR in Trauma and Orthopaedics)
Mr Vishal Paringe (Consultant)
University Hospitals Birmingham NHS Foundation Trust (Queen Elizabeth Hospital)
Mr Samuel Chan (Consultant)
Mrs Gemma Marie Smith (SpR in Trauma and Orthopaedics)
Eleanor Burden (Medical student)
Anna Douthwaite (Medical student)
Royal Orthopaedic Hospital NHS Foundation Trust
Mr Alistair Beaven (SpR in Trauma and Orthopaedics)
Mr Rajpal Nandra (SpR in Trauma and Orthopaedics)
Walsall Healthcare NHS Trust
Mr Fahad Hossain (Consultant)
Mr Srinivasan Gangadharan (SpR in Trauma and Orthopaedics)
Manchester University NHS Foundation Trust
Mr Ananthan Ebinesan (Consultant)
Mr Louai Abdeh (Clinical fellow in Trauma and Orthopaedics)
Ms Natalie Cheyne (Clinical fellow in Trauma and Orthopaedics)
George Eliot Hospital NHS Trust
Mr Gurbinder Nandhara (Consultant)
Mr Kishore Dasari (Consultant)
Ethical review statement
The study was registered with the research and audit department of each participating UK centre.
Footnotes
Author contributions: D. Rasidovic: Lead author, Designed and managed the study, Collected and analyzed the data.
I. Ahmed: Collected local data, Wrote the manuscript.
C. Thomas: Local data collection, Wrote the manuscript.
P. K. Kimani: Performed the statistical analysis, Wrote the manuscript.
P. Wall: Wrote the manuscript, Oversaw the final document.
K. Mangat: Lead co-author, Designed and managed the study.
Funding statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Twitter: Follow C. Thomas @doctorthomaschr
Follow K. Mangat @mr_upper_limb
References
- 1. Liebensteiner MC, Khosravi I, Hirschmann MT, Heuberer PR, Thaler M, Board of the AGA-Society of Arthroscopy and Joint-Surgery . Massive cutback in orthopaedic healthcare services due to the COVID-19 pandemic. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1705–1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pfefferle KJ, Shemory ST, Dilisio MF, Fening SD, Gradisar IM. Risk factors for manipulation after total knee arthroplasty: a pooled electronic health record database study. J Arthroplasty. 2014;29(10):2036–2038. [DOI] [PubMed] [Google Scholar]
- 3. No authors listed National Hip Fracture Database (NHFD) annual report 2019. Royal College of Physicians. 2019. https://www.nhfd.co.uk/20/hipfractureR.nsf/docs/2019Report (date last accessed 27 October 2020).
- 4. O'Dowd A, O’Dowd A. Covid-19: deaths in care home deaths in England and Wales rise sharply. BMJ. 2020;369:m1727. [DOI] [PubMed] [Google Scholar]
- 5. Egol KA, Konda SR, Bird ML, et al. Increased mortality and major complications in hip fracture care during the COVID-19 pandemic: a new York City perspective. J Orthop Trauma. 2020;34(8):395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vives JMM, Jornet-Gibert M, Cámara-Cabrera J, et al. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic: preliminary results of the Spanish HIP-COVID observational study. JBJS. 2020;102(13):e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maniscalco P, Poggiali E, Quattrini F, et al. Proximal femur fractures in COVID-19 emergency: the experience of two Orthopedics and Traumatology departments in the first eight weeks of the Italian epidemic. Acta Biomed. 2020;91(2):89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kayani B, Onochie E, Patil V, et al. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Joint J. 2020;102-B(9):1136–1145. [DOI] [PubMed] [Google Scholar]
- 9. Hall AJ, Clement ND, Farrow L, et al. IMPACT-Scot report on COVID-19 and hip fractures: a multicentre study assessing mortality, predictors of early SARS-CoV-2 infection, and the effects of social lockdown on epidemiology. Bone Joint J. 2020;102(9):1219–1228. [DOI] [PubMed] [Google Scholar]
- 10. Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth. 2008;101(4):511–517. [DOI] [PubMed] [Google Scholar]
- 11. von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. [DOI] [PubMed] [Google Scholar]
- 12. George D, Mallery P. IBM SPSS statistics 23 step by step: a simple guide and reference. Abingdon-on-Thames, UK: Routledge, 2016. [Google Scholar]
- 13. Mukherjee K, Brooks SE, Barraco RD, et al. Elderly adults with isolated hip fractures- orthogeriatric care versus standard care: a practice management guideline from the eastern association for the surgery of trauma. J Trauma Acute Care Surg. 2020;88(2):266–278. [DOI] [PubMed] [Google Scholar]
- 14. Nepogodiev D, Glasbey JC, Li E, COVIDSurg Collaborative . Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215(1):87–93. [DOI] [PubMed] [Google Scholar]
- 16. Li Y, Yao L, Li J, et al. Stability issues of RT-PCR testing of SARS-CoV-2 for hospitalized patients clinically diagnosed with COVID-19. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Watson J, Whiting PF, Brush JE. Interpreting a covid-19 test result. BMJ. 2020;369:m1808. [DOI] [PubMed] [Google Scholar]
- 18. Nishiura H, Kobayashi T, Miyama T, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int J Infect Dis. 2020;94:154–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mizumoto K, Kagaya K, Zarebski A, Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the diamond Princess cruise SHIP, Yokohama, Japan, 2020. Eurosurveillance. 2020;25(10):2000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Winn M, Willett K . New requirement to test patients being discharged from hospital to a care home. NHS. 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/04/C0324-New-requirement-to-test-patients-being-discharged-from-hospital-to-a-care-home.pdf (date last accessed 27 October 2020).
- 21. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172(9):577–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. No authors listed Population estimates for the UK, England and Wales, Scotland and Northern Ireland. Office for National Statistics. 2019. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (date last accessed 27 October 2020).
- 23. No authors listed Deaths involving COVID-19 by local area and socioeconomic deprivation: deaths occurring between 1 March and 17 April 2020. Office for National Statistics. 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19bylocalareasanddeprivation/deathsoccurringbetween1marchand17april (date last accessed 29 October 2020).
- 24. No authors listed Government publishes coronavirus (COVID-19) R value and growth rates. Government Office for Science and Scientific Advisory Group for Emergencies. 2020. https://www.gov.uk/government/news/government-publishes-coronavirus-covid-19-r-value-and-growth-rates (date last accessed 27 October 2020).