Abstract
Dipeptidyl peptidase-4 inhibitors (DPP-4is) have gained a key place in the management of type 2 diabetes mellitus (T2DM) essentially because of their good safety profile even in the frail population. DPP-4, originally known as ‘T-cell antigen CD26’, is expressed in many immune cells and regulates their functions, so the initial concern over the use of DPP-4is was the possible increased susceptibility to infections. Furthermore, because of the high affinity between human DPP-4 and the spike (S) receptor-binding domain of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), it was suspected that this virus, responsible for coronavirus disease 2019 (COVID-19), might be able to use the DPP-4 enzyme as a functional receptor to gain entry into the host. However, DPP-4is also exert anti-inflammatory effects, which could be beneficial in patients exposed to cytokine storms due to COVID-19. Yet, when observational (mostly retrospective) studies compared clinical outcomes in DPP-4i users vs non-users among diabetes patients with COVID-19, the overall results regarding the risk of progression towards more severe forms of the disease and mortality were heterogeneous, thereby precluding any definite conclusions. Nevertheless, new expectations have arisen following recent reports of significant reductions in admissions to intensive care units and mortality in DPP-4i users. However, given the limitations inherent in such observational studies, any available results should be considered, at best, as hypothetical and only suggestive of potentially substantial benefits with DPP-4is in diabetes patients with COVID-19. While the safe use of DPP-4is in COVID-19 patients appears to be an acceptable hypothesis, all such positive findings still need to be confirmed in randomized controlled trials (a few of which are currently ongoing) before any recommendations can be made for clinical practice.
Keywords: Gliptin, Incretin, Inflammation, Mortality, Outcome, SARS-CoV-2
Introduction
As diabetes, especially type 2 diabetes mellitus (T2DM), is a recognized risk factor for developing the more severe forms of coronavirus disease 2019 (COVID-19) [1], [2], [3], increasing interest is emerging regarding the potential impact of different glucose-lowering agents on the clinical outcomes associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection [4], [5], [6], [7]. The potentially positive influence of metformin [8] and the pros and cons regarding the use of sodium–glucose cotransporter type-2 inhibitors (SGLT2is) have recently been reviewed [9]. However, although the role of dipeptidyl peptidase-4 inhibitors (DPP-4is) has been recently discussed in many short reports, mostly commentaries and hypothesis-based papers, there have been no clear-cut conclusions [10], [11], [12], [13], [14].
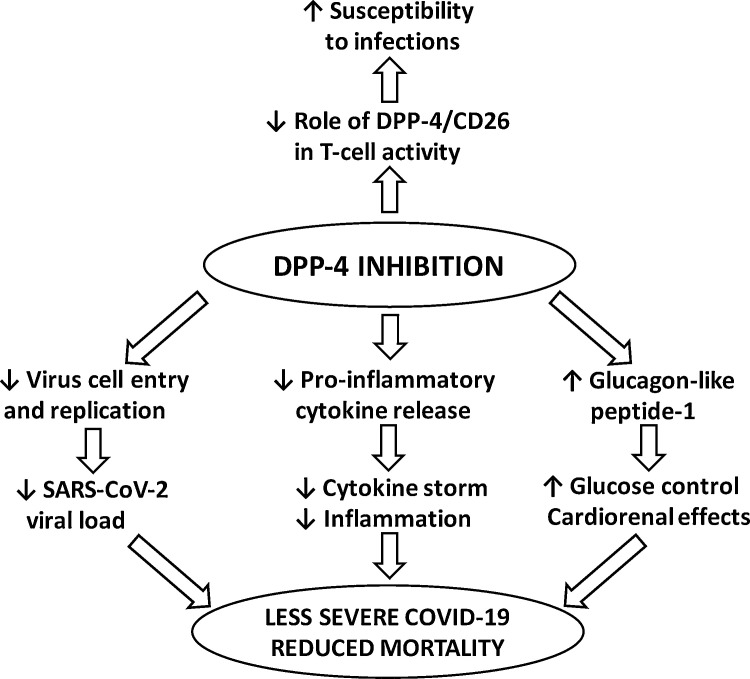
DPP-4is have raised considerable interest because of the extensive use of this pharmacological class in the management of T2DM that has resulted in an excellent well-recognized safety profile [15], the potential involvement of DPP-4 (originally known as ‘lymphocyte cell surface protein CD26’) in infectious disease processes [16] and, more recently, the possible contribution of the DPP-4 enzyme, recognized as coronavirus receptor protein, to intracellular entry of SARS-CoV-2 [17]. Within the immune system, DPP-4/CD26 proteins may be involved in amplifying the signals derived from interactions with an antigen, thereby leading to T-cell activation. Interestingly, this immune function appears to be independent of the catalytic activity of DPP-4 [16]. Given its various roles, the altered expression and/or activity of DPP-4 have been implicated in several pathological processes, including viral entry and inflammation as well as immune-mediated disorders [18]. In addition, because DPP-4 can be viewed as a multifunctional protein with a wide spectrum of actions that go beyond its role as a proteolytic enzyme, it can be difficult to predict the possible effects of its inhibition [18], [19]. Thus, among the multiple risk and protective factors that have so far been identified [20], the effects of DPP-4is on clinical outcomes in T2DM patients exposed to COVID-19 remain unclear [4], [10] (Fig. 1 ). However, until there is real-life evidence with reports of clear-cut observational findings and, ideally, robust results of randomized controlled trials (RCTs) regarding the impact of DPP-4is in patients with T2DM, no definite conclusions can as yet be made as to whether these glucose-lowering agents are beneficial, neutral or harmful in the setting of COVID-19 infection [21], [22].
Fig. 1.
Hypothetical interactions between dipeptidyl peptidase (DPP)-4 inhibition and infections such as coronavirus disease 2019 (COVID-19) in patients with type 2 diabetes: (upper) initial concerns for a possibly increased risk of infection; (lower) recent expectations that DPP-4 inhibition might improve the prognosis of patients exposed to COVID-19 through various yet-to-be-confirmed mechanisms. SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
The aim of the present short narrative review is to summarize all the available data regarding the potential impact of DPP-4is on clinical outcomes, especially disease severe enough to require patient management in intensive care units (ICUs), and on the in-hospital mortality of patients with T2DM during the COVID-19 outbreak.
Rationale supporting potential interference by DPP-4is
DPP-4, originally known as ‘T-cell antigen CD26’, is a multifunctional soluble and cell-bound serine protease that is abundantly expressed in lymphocytes and adipocytes as well as many other cellular types, including endothelial and epithelial cells in the lungs [16], [23]. It is also widely expressed in many types of immune cells (CD4+ and CD8+ T cells, B cells, natural killer (NK) cells, dendritic cells, macrophages) and regulates their functions. Thus, DPP-4 plays a critical role not only in glucose homoeostasis, but also in inflammatory and immune responses. In addition, DPP-4 is capable of modulating numerous cytokines, chemokines and peptide hormones, all of which may be involved in cardiovascular biology [24], [25].
Accordingly, DPP-4/CD26 is speculated to be involved in various immune/inflammatory disorders, while DPP-4is are known to modify the biological activities of multiple immunomodulatory substrates [16], [23], [26]. The anti-inflammatory properties of antidiabetic drugs have been considered the ‘promised land’ during this COVID-19 era [6] and DPP-4is may be able to exert anti-inflammatory effects that might be positive for cardiovascular and renal protection [27]. DPP-4is such as sitagliptin can reduce inflammation intensity mostly by affecting the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) signalling pathway [28], and the potent and rapid anti-inflammatory effect of sitagliptin was confirmed by another study in patients with T2DM [29]. Also, a meta-analysis of 16 studies reported a significant reduction in the inflammatory biomarker C-reactive protein following DPP-4i therapy compared with placebo [30]. As inflammatory mediators are strongly active in patients with COVID-19 and contribute to disease severity, pneumonia leading to acute respiratory distress syndrome (ARDS) and also coagulopathies, DPP-4is could also help to block pathways leading to cytokine storms (Fig. 1, lower).
DPP-4is and infections before the COVID-19 era
Initially, there were some questions as to whether or not DPP-4is might compromise immune function and increase the risk of respiratory tract infections (RTIs), given the role of DPP-4/CD26 in the regulation of T-cell activity (Fig. 1, upper) [16]. However, neither innate nor adaptive immune responses are affected by the DPP-4is routinely used in clinical practice [31]. On the other hand, a nested case–control study using VigiBase, the World Health Organization’s adverse drug reactions (WHO-ADR) database, indicated an increased reporting of infections, particularly upper RTIs, in users of DPP-4is compared with users of other antidiabetic drugs [32]. Reassuringly, though, there has been no evidence of any increased risk of infections in either pooled safety analyses or large prospective cardiovascular outcome trials comparing DPP-4is with placebo [15]. One meta-analysis of 29 RCTs concluded that DPP-4is could increase the risk of nasopharyngitis and urinary tract infections, but not of RTIs [33]; the latter finding was also confirmed in a real-life setting using the UK-based Clinical Practice Research Datalink (CPRD) [34]. A more recent meta-analysis of two observational studies and 41 RCTs published before the COVID-19 pandemic showed no effect of DPP-4is on pneumonia risk. Thus, in general, the use of DPP-4is can be considered safe as regards the risk of common pneumonia [35]. This conclusion is in line with the idea that the catalytic activity of DPP-4 is not essential for the co-stimulatory role of CD26 in T-cell activation [16].
In 2013, DPP-4 was identified as a functional receptor for human coronavirus Erasmus Medical Centre (hCoV-EMC), the virus responsible for Middle East respiratory syndrome (MERS) that is genetically similar to SARS-CoV-2 [36]. Interestingly, the naturally occurring polymorphisms in DPP-4 that negatively impact cellular entry of MERS-CoV have recently been identified and may thus help to modulate MERS development in infected patients [37]. Also, the spatial and cellular localization of DPP-4 was investigated to evaluate its association with MERS clinical disease [38]: within the human respiratory tract, immunoreactive DPP-4 was localized to immune and endothelial cells, pneumocytes, the pleural mesothelium and lymphatic vessels [38]. However, if SARS-CoV-2 is also able to interact with the DPP-4 enzyme as a coreceptor, this interaction is not as strong as that with angiotensin-converting enzyme 2 (ACE2), the most important coreceptor used by the virus for cellular entry [39].
Of note, in a mouse model of ARDS, DPP-4 inhibition by sitagliptin alleviated the histological alterations caused by lung injury by inhibiting the proinflammatory cytokines interleukin (IL)-1β, tumour necrosis factor (TNF)-α and IL-6 [40]. However, there is little evidence that such animal findings can be translated to the human lung.
Findings in silico with SARS-CoV-2
Bioinformatics approaches combining human–virus protein interaction prediction and protein docking based on crystal structures have revealed a high affinity between human DPP-4 and the spike (S) receptor-binding domain of SARS-CoV-2 [39]. This observation raises the hypothesis that SARS-CoV-2 might also use the DPP-4 enzyme as a functional receptor to gain entry into the host [41].
The three-dimensional (3D) structure of the main SARS-CoV-2 protease was compared with the 3D structures of several proteases, including DPP-4. Although results in silico warrant further evaluation for viral anticipation, it has nonetheless been suggested that DPP-4is with antiviral actions may be useful for COVID-19-infected patients with diabetes [42]. However, another study failed to show that SARS-CoV-2 binds to DPP-4, but found instead that beta-coronaviruses are capable of entering human cells through an unknown receptor in addition to the well-recognized ACE2 [43]. As most of the current data point to membrane-bound ACE2 in contrast to DPP-4 as the major binding partner for COVID-19 internalization into host immune cells, the finding that the circulating soluble form of DPP-4 is reduced in patients hospitalized with SARS-CoV-2 suggests a regulatory role of both ACE2 and DPP-4 enzymes in the course of COVID-19 infection [44].
In addition, computational studies have raised further speculation as to whether or not using DPP-4is to target one of the potential host determinants of virulence would be useful for attenuating COVID-19 severity after viral exposure [10], [45], even though this hypothesis has also been disputed [46].
Observational studies with DPP-4is during COVID-19
DPP-4 distribution in the human respiratory tract may facilitate entry of the virus into the airways tract itself, thereby contributing to the development of cytokine storms and immunopathology by causing fatal COVID-19 pneumonia. Thus, theoretically, the use of DPP-4is in patients with COVID-19 with, or even without, T2DM might offer a simple way to reduce virus entry and replication in the airways, and hamper sustained cytokine storms and inflammation within the lungs of patients diagnosed with COVID-19 infection (Fig. 1, lower) [47].
Given this hypothesis, several observational retrospective studies have been performed to investigate the impact of DPP-4is on clinical outcomes in T2DM patients hospitalized for COVID-19. The results regarding transition to more severe disease—generally requiring the transfer of patients to an ICU—are summarized in Table 1 [48], [49], [50], [51], [52], [53], [54], [55]. In fact, there was wide heterogeneity across these studies, with hazard ratios (HRs) ranging from 0.36 to 1.81. Although outcomes differed slightly among the reports, such differences cannot explain the widely divergent results. Likewise, the effects of DPP-4is on in-hospital mortality are summarized in Table 2 [48], [49], [50], [53], [49], [50], [51], [52], [53], [54], [55] and, here again, there was marked heterogeneity across these studies with HRs ranging from 0.13 to 1.48. In fact, there is no obvious explanation for such between-study heterogeneity. It is worth noting, however, that most of these studies were not designed to investigate the hypothesis—for example, the French Coronavirus SARS-CoV-2 and Diabetes Outcomes (CORONADO) study [49] —and some recruited only a limited number of patients treated with DPP-4is, thereby attenuating the level of confidence and exposing results to a lack of statistical power. Nevertheless, of potential interest is the study that specifically investigated the effect of a DPP-4i (sitagliptin) using a case–control design and recruiting a relatively large number of patients, and reported the most impressive results [HR: 0.51, 95% confidence interval (CI): 0.27–0.95; P = 0.03] for ICU admission (Table I), and an HR of 0.44 (95% CI: 0.29–0.66; P = 0.0001) for mortality (Table 2) when comparing sitagliptin users vs non-users [53]. However, as the methodology of the study has come under criticism [56], caution is therefore required before translating this approach into clinical practice (see below).
Table 1.
Relationship between dipeptidyl peptidase (DPP)-4 inhibitor therapy and poorer outcomes/prognoses during the coronavirus disease 2019 (COVID-19) pandemic.
| References | Country | Type of study | n/N | OR or HR (95% CI) | Outcome |
|---|---|---|---|---|---|
| Chen et al. [48] | China | Retrospective | 20/120 | 1.81 (0.51–6.37), P = 0.36 | Poor prognosis |
| Cariou et al. [49] | France | Observational cohort | 285/1317 | 1.01 (0.75–1.34), P = NR | Tracheal intubation and/or death |
| Fadini et al. [50] | Italy | Retrospective | 9/85 | 1.73 (33.3% vs 19.2%), P = 0.33 | ICU admission |
| Montastruc et al. [51] | France | Case series | 10/27 | 0.53 (43% vs 81%), P = NR | Intubation |
| Rhee et al. [52] | South Korea | Population-based | 263/832 | 0.36 (0.14–0.97), P = NR | Severe COVID-19 |
| Solerte et al. [53] | Italy | Case–control, retrospective observational | 169/338 | 0.51 (0.27–0.95), P = 0.03 | ICU admission |
| Kim et al. [54] | South Korea | Retrospective | 85/235 | 1.05 (0.44–2.49), P = 0.92 | Severe COVID-19 |
| Mirani et al. [55] | Italy | Case series | 11/90 | NR, P = 0.029 | Less mechanical ventilation |
n/N, DPP-4 inhibitor users/all type 2 diabetes patients; OR, odds ratio; HR, hazard ratio; CI, confidence interval; NR, not reported; ICU, intensive care unit.
Table 2.
Relationship between dipeptidyl peptidase (DPP)-4 inhibitor therapy and in-hospital mortality during the coronavirus disease 2019 (COVID-19) pandemic.
| References | Country | Type of study | n/N | OR or HR (95% CI) |
|---|---|---|---|---|
| Chen et al. [48] | China | Retrospective | 20/120 | 1.48 (0.40–5.53), P = 0.56 |
| Cariou et al. [49] | France | Observational cohort | 285/1317 | 0.85 (0.55–1.32), P = NR |
| Fadini et al. [50] | Italy | Retrospective | 9/85 | 0.80 (11.1% vs 13.9%), P = 0.82 |
| Solerte et al. [53] | Italy | Case–control, retrospective, observational | 169/338 | 0.44 (0.29–0.66), P = 0.0001 |
| Kim et al. [54] | South Korea | Retrospective | 85/235 | 1.47 (0.45–4.78), P = 0.52 |
| Mirani et al. [55] | Italy | Case series | 11/90 | 0.13 (0.02–0.92), P = 0.042 |
Data are adapted from Mirabelli et al. [4]; n/N, DPP-4 inhibitor users/all type 2 diabetes patients; OR, odds ratio; HR, hazard ratio; CI, confidence interval; NR, not reported.
Limitations of the available data
First, findings in T2DM patients were mostly collected from retrospective observational studies, and the potential biases inherent in such studies are well known [57]. Also, in the absence of randomization, selection biases (possible differences between subjects included in two compared groups) cannot be excluded, and both the indications and contraindications may differ between various antidiabetic medications. Thus, the patients’ characteristics among DPP-4i users vs non-users may have differed (in age, renal function, established cardiovascular disease …) and potentially influenced outcomes independently of any effect of the DPP-4i itself. As a consequence, it is possible that selection biases and confounding factors may have led to misleading results [57].
Second, it is accepted that the quality of glucose control during hospitalization can influence the outcome of COVID-19 in patients with T2DM [2]. Yet, in all published studies thus far, no information on glucose control during hospital stays has been reported. Furthermore, it is unclear whether any DPP-4i treatment, which was noted at the time of hospital admission, was maintained during hospitalization or not.
Finally, the results recently reported by Solerte et al. [53] and Mirani et al. [55] were discussed and criticized in an accompanying commentary [56] because of several limitations and shortcomings. Therefore, the evidence for DPP-4is reducing the mortality associated with COVID-19 should be considered as only suggestive at best. Nevertheless, it is certainly mandatory to consider those two reports, along with those listed in Table 1, Table 2, as hypothesis-generating clues pointing to potentially substantial benefits with DPP-4is (for example, sitagliptin) in patients with T2DM and COVID-19 infection. These findings now need to be confirmed in well-designed, prospective, high-quality RCTs [56].
Ongoing randomized controlled trials
Because of the possible biases inherent in observational retrospective studies, and the divergent and inconclusive findings derived from such studies until now (Table 1, Table 2), definitive answers will only be provided by RCTs. For this reason, at least three parallel-group RCTs investigating the effects of DPP-4is on the prognosis for COVID-19 are currently ongoing: two of them are looking at the effects of linagliptin added to background insulin therapy (one in the US, ClinicalTrials.gov identifier: NCT 04341935; 20 participants only), the other in Israel (ClinicalTrials.gov identifier: NCT 04371978; 100 participants); and the third is the open-label Effect of Sitagliptin Treatment in COVID-19-Positive Diabetic Patients (SIDIACO) RCT in Italy to evaluate the effect of sitagliptin as an add-on to standard care with nutritional therapy with or without insulin treatment (ClinicalTrials.gov identifier: NCT 04365517; 170 participants).
It has been hypothesized that, thanks to their ancillary effects, DPP-4is could potentially be ‘repurposed’ as salutary drugs against COVID-19 even for non-diabetes patients [58]. Interestingly, DPP-4is are known to be associated with little or no risk of hypoglycaemia [15], which means they could also be used safely in patients without diabetes. Clinical studies need to be specifically designed to investigate this possibility but, to our knowledge, none is currently underway to test this hypothesis in patients without diabetes.
Real-life and practical recommendations
To test the hypothesis that treatment with DPP-4is might be able to influence COVID-19 progression in patients with T2DM, a nationwide study of 3818 charts of patients with fatal COVID-19 found that geographical differences in DPP-4i use across regions of Italy did not correlate with diabetes prevalence among COVID-19 deaths. Thus, these findings do not support the hypothesis of any clinically relevant involvement of DPP-4is in COVID-19 development and progression [59].
As COVID-19 is a new viral infection with as yet numerous unknowns and uncertainties, and with data that are still rather limited, the expert recommendations conform to strategies classically used for diabetes patients with severe infections [60]. Thus, the importance of good glycaemic control during this COVID-19 pandemic has been emphasized [61], and it has even been suggested that optimalizing glycaemic control might reduce the risk of severe COVID-19 infection [2], [3]. Furthermore, discontinuing glucose-lowering agents in general is not recommended prophylactically for asymptomatic outpatients with T2DM nor in the absence of evidence of a serious case of COVID-19 [60]. On the other hand, DPP-4is are associated with a low risk of hypoglycaemia even when combined with insulin, and are relatively safe across a wide range of renal function. At present, there is no convincing evidence to suggest that DPP-4is be discontinued even in hospitalized patients with mild-to-moderate symptoms, and the recommendation is that they may be continued in non-critically ill patients [60]. Indeed, in addition to glucagon-like peptide (GLP)-1 receptor agonists and insulin, DPP-4is are the preferred options for glucose control, given their flat profile and low glycaemic variability particularly in hospitalized patients [62]. Nevertheless, despite the recent positive findings reported with sitagliptin in reducing mortality [53], there are insufficient data to support the introduction of a DPP-4i to the treatment of a patient with T2DM exposed to SARS-CoV-2 with the aim of avoiding a poorer outcome [56]. New-onset diabetes has been reported in some patients exposed to COVID-19, and may be explained by both increased insulin resistance and defective insulin secretion due to cytokine storms and the tropism of SARS-CoV-2 towards pancreatic beta cells [63]. Possible deterioration of glucose homoeostasis could also be amplified if glucocorticoids such as dexamethasone are administered [3]. Although the use of DPP-4is in such patients with new-onset diabetes may be potentially helpful, their efficacy and safety are as yet insufficiently documented [60]. Finally, as DPP-4is are likely to be of less therapeutic benefit for patients with severe COVID-19 infection, they should be omitted in cases of acute severe illness (such as patients hospitalized in ICUs) and replaced by insulin, the alternative treatment of choice, where necessary [60], [62].
Further analyses of affected patients using various antidiabetic treatments who also have COVID-19 could allow more precise counselling regarding the use of glucose-lowering agents in general, while elucidating the effects of DPP-4is in particular.
Conclusion
Given that the DPP-4 enzyme is involved in so many biological processes, including immune and inflammatory mechanisms, the hypothesis was proposed that DPP-4is might be able to moderate the outcomes in T2DM patients infected by SARS-CoV-2. However, some mechanisms appear to be deleterious whereas others might be associated with favourable effects in patients exposed to infections such as COVID-19. Thus, it is difficult to determine whether DPP-4is would be beneficial, neutral or harmful in the setting of COVID-19 infection. Whereas findings from observational studies have been heterogeneous, collectively the available data indicate that DPP-4is do no harm to patients with both T2DM and COVID-19. However, except for one case–control retrospective study showing a significant reduction in ICU admission and mortality in sitagliptin users vs non-users, no other sufficiently large observational study has yet found any clear-cut protection in patients treated with DPP-4is compared with patients receiving other glucose-lowering agents. Moreover, while there is no reason to eliminate DPP-4i use in patients with T2DM and COVID-19 except for those who are critically ill, there is still insufficient evidence to support the introduction of a DPP-4i with the intention to improve the prognosis of patients exposed to SARS-CoV-2. Thus, the conclusion at this time is that DPP-4is do not modify the outcome of COVID-19, a finding that remains to be confirmed by the results of ongoing RCTs.
Conflict of interest
The author declares no direct conflicts of interest in relation to the content of this paper.
References
- 1.Targher G., Mantovani A., Wang X.B., Yan H.D., Sun Q.F., Pan K.H. Patients with diabetes are at higher risk for severe illness from COVID-19. Diabetes Metab. 2020;46:335–337. doi: 10.1016/j.diabet.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu L., She Z.G., Cheng X., Qin J.J., Zhang X.J., Cai J. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020;31:1068–1077. doi: 10.1016/j.cmet.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Apicella M., Campopiano M.C., Mantuano M., Mazoni L., Coppelli A., Del Prato S. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. 2020;8:782–792. doi: 10.1016/S2213-8587(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mirabelli M., Chiefari E., Puccio L., Foti D.P., Brunetti A. Potential benefits and harms of novel antidiabetic drugs during COVID-19 crisis. Int J Environ Res Public Health. 2020;17:3664. doi: 10.3390/ijerph17103664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pal R., Bhadada S.K. Should anti-diabetic medications be reconsidered amid COVID-19 pandemic? Diabetes Res Clin Pract. 2020;163 doi: 10.1016/j.diabres.2020.108146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katsiki N., Ferrannini E. Anti-inflammatory properties of antidiabetic drugs: a “promised land” in the COVID-19 era? J Diabetes Complications. 2020;34 doi: 10.1016/j.jdiacomp.2020.107723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Filardi T., Morano S. COVID-19: is there a link between the course of infection and pharmacological agents in diabetes? J Endocrinol Invest. 2020;43:1053–1060. doi: 10.1007/s40618-020-01318-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scheen A.J. Metformin and COVID-19: from cellular mechanisms to reduced mortality. Diabetes Metab. 2020;46:423–426. doi: 10.1016/j.diabet.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scheen A.J. SGLT2 inhibition during the COVID-19 epidemic: friend or foe? Diabetes Metab. 2020;46:343–344. doi: 10.1016/j.diabet.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iacobellis G. COVID-19 and diabetes: can DPP4 inhibition play a role? Diabetes Res Clin Pract. 2020;162 doi: 10.1016/j.diabres.2020.108125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barchetta I., Gisella Cavallo M., Giorgio Baroni M. COVID-19 and diabetes: is this association driven by the DPP4 receptor? Potential clinical and therapeutic implications. Diabetes Res Clin Pract. 2020;163 doi: 10.1016/j.diabres.2020.108165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Strollo R., Pozzilli P. DPP4 inhibition: preventing SARS-CoV-2 infection and/or progression of COVID-19? Diabetes Metab Res Rev. 2020;36:e3330. doi: 10.1002/dmrr.3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dastan F., Abedini A., Shahabi S., Kiani A., Saffaei A., Zare A. Sitagliptin repositioning in SARS-CoV-2: effects on ACE-2, CD-26, and inflammatory cytokine storms in the lung. Iran J Allergy Asthma Immunol. 2020;19:10–12. doi: 10.18502/ijaai.v19i(s1.r1).2849. [DOI] [PubMed] [Google Scholar]
- 14.Danta C.C. Dipeptidyl peptidase-4: a potential therapeutic target in diabetic kidney disease with SARS-CoV-2 infection. ACS Pharmacol Transl Sci. 2020;3:1020–1022. doi: 10.1021/acsptsci.0c00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scheen A.J. The safety of gliptins: updated data in 2018. Expert Opin Drug Saf. 2018;17:387–405. doi: 10.1080/14740338.2018.1444027. [DOI] [PubMed] [Google Scholar]
- 16.Deacon C.F. Physiology and pharmacology of DPP-4 in glucose homeostasis and the treatment of type 2 diabetes. Front Endocrinol (Lausanne) 2019;10:80. doi: 10.3389/fendo.2019.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Drucker D.J. Coronavirus infections and type 2 diabetes-shared pathways with therapeutic implications. Endocr Rev. 2020;41 doi: 10.1210/endrev/bnaa011. bnaa011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klemann C., Wagner L., Stephan M., von Horsten S. Cut to the chase: a review of CD26/dipeptidyl peptidase-4’s (DPP4) entanglement in the immune system. Clin Exp Immunol. 2016;185:1–21. doi: 10.1111/cei.12781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stoian A.P., Papanas N., Prazny M., Rizvi A.A., Rizzo M. Incretin-based therapies role in COVID-19 era: evolving insights. J Cardiovasc Pharmacol Ther. 2020;25:494–496. doi: 10.1177/1074248420937868. [DOI] [PubMed] [Google Scholar]
- 20.Scheen A.J., Marre M., Thivolet C. Prognostic factors in patients with diabetes hospitalized for COVID-19: findings from the CORONADO study and recent reports. Diabetes Metab. 2020;46:265–271. doi: 10.1016/j.diabet.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dalan R. Is DPP4 inhibition a comrade or adversary in COVID-19 infection. Diabetes Res Clin Pract. 2020;164 doi: 10.1016/j.diabres.2020.108216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh A.K., Singh R. Dipeptidyl-peptidase-4 inhibitors in type 2 diabetes and COVID-19: from a potential repurposed agent to a useful treatment option. J Diabetol. 2020;11:131–136. [Google Scholar]
- 23.Drucker D.J. The biology of incretin hormones. Cell Metab. 2006;3:153–165. doi: 10.1016/j.cmet.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 24.Ussher J.R., Drucker D.J. Cardiovascular biology of the incretin system. Endocr Rev. 2012;33:187–215. doi: 10.1210/er.2011-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scheen A.J. Cardiovascular effects of gliptins. Nat Rev Cardiol. 2013;10:73–84. doi: 10.1038/nrcardio.2012.183. [DOI] [PubMed] [Google Scholar]
- 26.Shao S., Xu Q., Yu X., Pan R., Chen Y. Dipeptidyl peptidase 4 inhibitors and their potential immune modulatory functions. Pharmacol Ther. 2020;209 doi: 10.1016/j.pharmthera.2020.107503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tomovic K., Lazarevic J., Kocic G., Deljanin-Ilic M., Anderluh M., Smelcerovic A. Mechanisms and pathways of anti-inflammatory activity of DPP-4 inhibitors in cardiovascular and renal protection. Med Res Rev. 2019;39:404–422. doi: 10.1002/med.21513. [DOI] [PubMed] [Google Scholar]
- 28.Mozafari N., Azadi S., Mehdi-Alamdarlou S., Ashrafi H., Azadi A. Inflammation: a bridge between diabetes and COVID-19, and possible management with sitagliptin. Med Hypotheses. 2020;143 doi: 10.1016/j.mehy.2020.110111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Makdissi A., Ghanim H., Vora M., Green K., Abuaysheh S., Chaudhuri A. Sitagliptin exerts an antinflammatory action. J Clin Endocrinol Metab. 2012;97:3333–3341. doi: 10.1210/jc.2012-1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu X., Men P., Wang B., Cai G., Zhao Z. Effect of dipeptidyl-peptidase-4 inhibitors on C-reactive protein in patients with type 2 diabetes: a systematic review and meta-analysis. Lipids Health Dis. 2019;18:144. doi: 10.1186/s12944-019-1086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anz D., Kruger S., Haubner S., Rapp M., Bourquin C., Endres S. The dipeptidylpeptidase-IV inhibitors sitagliptin, vildagliptin and saxagliptin do not impair innate and adaptive immune responses. Diabetes Obes Metab. 2014;16:569–572. doi: 10.1111/dom.12246. [DOI] [PubMed] [Google Scholar]
- 32.Willemen M.J., Mantel-Teeuwisse A.K., Straus S.M., Meyboom R.H., Egberts T.C., Leufkens H.G. Use of dipeptidyl peptidase-4 inhibitors and the reporting of infections: a disproportionality analysis in the World Health Organization VigiBase. Diabetes Care. 2011;34:369–374. doi: 10.2337/dc10-1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Amori R.E., Lau J., Pittas A.G. Efficacy and safety of incretin therapy in type 2 diabetes: systematic review and meta-analysis. JAMA. 2007;298:194–206. doi: 10.1001/jama.298.2.194. [DOI] [PubMed] [Google Scholar]
- 34.Gamble J.M., Donnan J.R., Chibrikov E., Twells L.K., Midodzi W.K., Majumdar S.R. Comparative safety of dipeptidyl peptidase-4 inhibitors versus sulfonylureas and other glucose-lowering therapies for three acute outcomes. Sci Rep. 2018;8:15142. doi: 10.1038/s41598-018-33483-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morieri M.L., Bonora B.M., Longato E., Di Camilo B., Sparacino G., Tramontan L. Exposure to dipeptidyl-peptidase 4 inhibitors and the risk of pneumonia among people with type 2 diabetes: retrospective cohort study and meta-analysis. Diabetes Obes Metab. 2020;20(Jul) doi: 10.1111/dom.14142. [DOI] [PubMed] [Google Scholar]
- 36.Raj V.S., Mou H., Smits S.L., Dekkers D.H., Muller M.A., Dijkman R. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature. 2013;495:251–254. doi: 10.1038/nature12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kleine-Weber H., Schroeder S., Kruger N., Prokscha A., Naim H.Y., Muller M.A. Polymorphisms in dipeptidyl peptidase 4 reduce host cell entry of Middle East respiratory syndrome coronavirus. Emerg Microbes Infect. 2020;9:155–168. doi: 10.1080/22221751.2020.1713705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meyerholz D.K., Lambertz A.M., McCray P.B., Jr. Dipeptidyl peptidase 4 distribution in the human respiratory tract: implications for the Middle East respiratory syndrome. Am J Pathol. 2016;186:78–86. doi: 10.1016/j.ajpath.2015.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li Y., Zhang Z., Yang L., Lian X., Xie Y., Li S. The MERS-CoV receptor DPP4 as a candidate binding target of the SARS-CoV-2 spike. iScience. 2020;23 doi: 10.1016/j.isci.2020.101400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kawasaki T., Chen W., Htwe Y.M., Tatsumi K., Dudek S.M. DPP4 inhibition by sitagliptin attenuates LPS-induced lung injury in mice. Am J Physiol Lung Cell Mol Physiol. 2018;315 doi: 10.1152/ajplung.00031.2018. L834-L45. [DOI] [PubMed] [Google Scholar]
- 41.Vankadari N., Wilce J.A. Emerging WuHan (COVID-19) coronavirus: glycan shield and structure prediction of spike glycoprotein and its interaction with human CD26. Emerg Microbes Infect. 2020;9:601–604. doi: 10.1080/22221751.2020.1739565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eleftheriou P., Amanatidou D., Petrou A., Geronikaki A. In silico evaluation of the effectivity of approved protease inhibitors against the main protease of the novel SARS-CoV-2 virus. Molecules. 2020;25:2529. doi: 10.3390/molecules25112529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Letko M., Marzi A., Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020;5:562–569. doi: 10.1038/s41564-020-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schlicht K., Rohmann N., Geisler C., Hollstein T., Knappe C., Hartmann K. Circulating levels of soluble dipeptidylpeptidase-4 are reduced in human subjects hospitalized for severe COVID-19 infections. Int J Obes (Lond) 2020;44:2335–2338. doi: 10.1038/s41366-020-00689-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bassendine M.F., Bridge S.H., McCaughan G.W. Gorrell MD. COVID-19 and comorbidities: a role for dipeptidyl peptidase 4 (DPP4) in disease severity? J Diabetes. 2020;12:649–658. doi: 10.1111/1753-0407.13052. [DOI] [PubMed] [Google Scholar]
- 46.Pitocco D., Tartaglione L., Viti L., Di Leo M., Pontecorvi A., Caputo S. SARS-CoV-2 and DPP4 inhibition: is it time to pray for Janus Bifrons? Diabetes Res Clin Pract. 2020;163 doi: 10.1016/j.diabres.2020.108162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Solerte S.B., Di Sabatino A., Galli M., Fiorina P. Dipeptidyl peptidase-4 (DPP4) inhibition in COVID-19. Acta Diabetol. 2020;57:779–783. doi: 10.1007/s00592-020-01539-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen Y., Yang D., Cheng B., Chen J., Peng A., Yang C. Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication. Diabetes Care. 2020;43:1399–1407. doi: 10.2337/dc20-0660. [DOI] [PubMed] [Google Scholar]
- 49.Cariou B., Hadjadj S., Wargny M., Pichelin M., Al-Salameh A., Allix I. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia. 2020;63:1500–1515. doi: 10.1007/s00125-020-05180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fadini G.P., Morieri M.L., Longato E., Bonora B.M., Pinelli S., Selmin E. Exposure to dipeptidyl-peptidase-4 inhibitors and COVID-19 among people with type 2 diabetes: a case-control study. Diabetes Obes Metab. 2020;28(May) doi: 10.1111/dom.14097. 10.1111/dom.14097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Montastruc F., Romano C., Montastruc J.L., Silva S., Seguin T., Minville V. Pharmacological characteristics of patients infected with SARS-Cov-2 admitted to Intensive Care Unit in South of France. Therapie. 2020;75:381–384. doi: 10.1016/j.therap.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rhee S.Y., Lee J., Nam H., Kyoung D.S., Kim D.J. Effects of a DPP-4 inhibitor and RAS blockade on clinical outcomes of patients with diabetes and COVID-19. medRxiv. 2020 doi: 10.4093/dmj.2020.0206. Preprint 2020 doi:101101/2020052020108555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Solerte S.B., D’Addio F., Trevisan R., Lovati E., Rossi A., Pastore I. Sitagliptin treatment at the time of hospitalization was associated with reduced mortality in patients with type 2 diabetes and COVID-19: a multicenter, case-control, retrospective, observational study. Diabetes Care. 2020;43:2999–3006. doi: 10.2337/dc20-1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kim M.K., Jeon J.H., Kim S.W., Moon J.S., Cho N.H., Han E. The clinical characteristics and outcomes of patients with moderate-to-severe coronavirus disease 2019 infection and diabetes in Daegu, South Korea. Diabetes Metab J. 2020;44:602–613. doi: 10.4093/dmj.2020.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mirani M., Favacchio G., Carrone F., Betella N., Biamonte E., Morenghi E. Impact of comorbidities and glycemia at admission and dipeptidyl peptidase 4 inhibitors in patients with type 2 diabetes with COVID-19: a case series from an academic hospital in Lombardy. Italy. Diabetes Care. 2020;43:3042–3049. doi: 10.2337/dc20-1340. [DOI] [PubMed] [Google Scholar]
- 56.Nauck M.A., Meier J.J. Reduced COVID-19 mortality with sitagliptin treatment? Weighing the dissemination of potentially lifesaving findings against the assurance of high scientific standards. Diabetes Care. 2020;43:2906–2909. doi: 10.2337/dci20-0062. [DOI] [PubMed] [Google Scholar]
- 57.Reveiz L., Haby M.M., Martinez-Vega R., Pinzon-Flores C.E., Elias V., Smith E. Risk of bias and confounding of observational studies of Zika virus infection: a scoping review of research protocols. PLoS One. 2017;12 doi: 10.1371/journal.pone.0180220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pantanetti P., Cangelosi G., Ambrosio G. Potential role of incretins in diabetes and COVID-19 infection: a hypothesis worth exploring. Intern Emerg Med. 2020;15:779–782. doi: 10.1007/s11739-020-02389-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Strollo R., Maddaloni E., Dauriz M., Pedone C., Buzzetti R., Pozzilli P. Use of DPP4 inhibitors in Italy does not correlate with diabetes prevalence among COVID-19 deaths. Diabetes Res Clin Pract. 2020;171 doi: 10.1016/j.diabres.2020.108444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bornstein S.R., Rubino F., Khunti K., Mingrone G., Hopkins D., Birkenfeld A.L. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 2020;8:546–550. doi: 10.1016/S2213-8587(20)30152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Katulanda P., Dissanayake H.A., Ranathunga I., Ratnasamy V., Wijewickrama P.S.A., Yogendranathan N. Prevention and management of COVID-19 among patients with diabetes: an appraisal of the literature. Diabetologia. 2020;63:1440–1452. doi: 10.1007/s00125-020-05164-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ceriello A., Standl E., Catrinoiu D., Itzhak B., Lalic N.M., Rahelic D. Issues of cardiovascular risk management in people with diabetes in the COVID-19 era. Diabetes Care. 2020;43:1427–1432. doi: 10.2337/dc20-0941. [DOI] [PubMed] [Google Scholar]
- 63.Sathish T., Tapp R.J., Cooper M.E., Zimmet P. Potential metabolic and inflammatory pathways between COVID-19 and new-onset diabetes. Diabetes Metab. 2020 doi: 10.1016/j.diabet.2020.10.002. Epub: Oct 28:S1262-3636(20)30155-5. [DOI] [PMC free article] [PubMed] [Google Scholar]