To the Editor : In a well-catalogued multi-institutional case series, Freeman et al1 described a miscellaneous collection of dermatologic manifestations occurring in parallel to COVID-19. Although the face was affected in many cases, the study documented oral mucosa changes in only 4 individuals, without providing further information. Accordingly, we would like to highlight the variable clinical spectrum of oral manifestations associated with COVID-19 and pose the question about a link between oral and dermatologic findings. It is critical that health professionals recognize the COVID-19–related oral and/or dermatologic manifestations to allow timely patient referral.
The electronic database MEDLINE/PubMed was searched on October 11, 2020, for retrospective studies, case series, case reports, or letters on oral manifestations associated with COVID-19. Those with serologic tests and clinical characteristics sufficient for a definitive diagnosis were included. No language restrictions were adopted. The search was undertaken using the entry terms and keywords related to “oral cavity” and “SARS-CoV-2/COVID-19.” Articles reporting data on ageusia/hypogeusia as the main oral disease complaint were excluded.
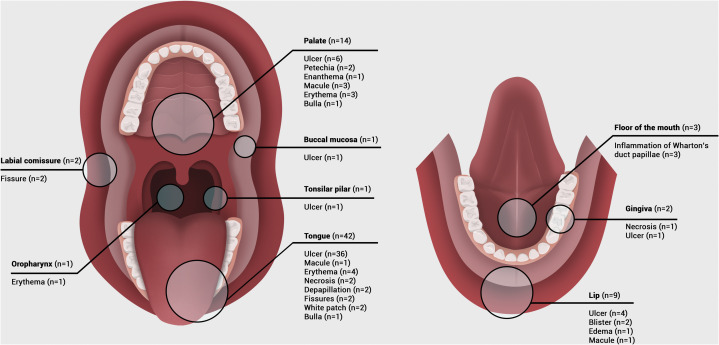
The search yielded 509 articles, 21 of which, involving 65 individuals, were selected after application of inclusion/exclusion criteria (Supplementary Table I, available via Mendeley at https://doi.org/10.17632/csvv7xgbr9.1). Studies were from Europe (n = 11), South America (n = 6), Asia (n = 3), and North America (n = 1). There were 35 women (53.8%) and 27 men (41.5%). The affected individuals were a mean age of 44.2 ± 17.8 years (range, 16-83 years). The more commonly reported comorbidities were hypertension (19.3%), diabetes (9.6%), and obesity (6.4%). The most frequently detected oral manifestation was ulcer (n = 46 [54.1%]). For all oral manifestations, the tongue (n = 42 [53.8%]) was the most commonly affected site, involving the dorsum (n = 35), border (n = 31), and ventral surface (n = 6), followed by the palate (n = 14 [17.9%]; hard, n = 11; soft, n = 3), and lip (n = 9 [11.5%]), involving labial (n = 5) and semimucosa (n = 5) (Figs 1 and 2 ).
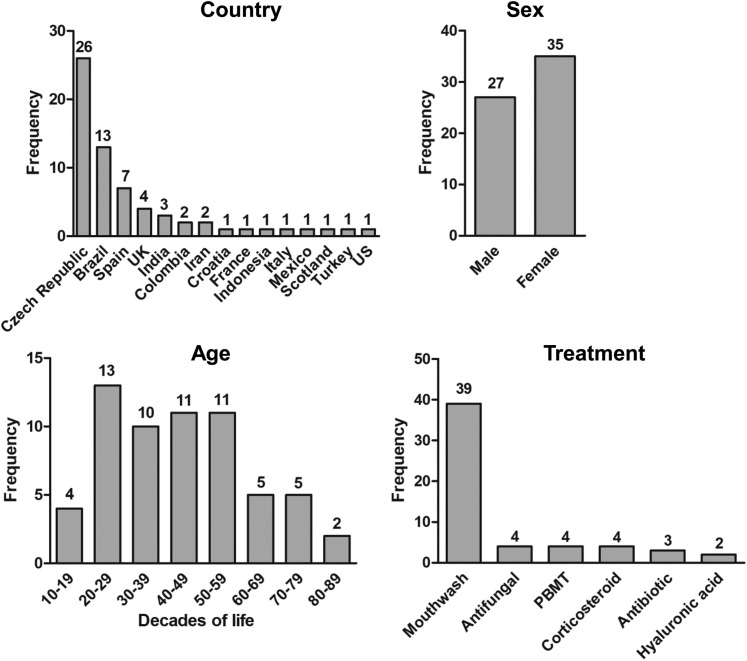
Fig 1.
Frequency of reported cases of oral and maxillofacial manifestations associated with COVID-19 by country (n = 65), sex (n = 62), decade of life (n = 62), and topical treatment (n = 56). Of note, local treatment was not analyzed by number of individuals but rather by of number of treatments (ie, the same individual may have used more than 1 therapy). PBMT, Photobiomodulation therapy; UK, United Kingdom; US, United States.
Fig 2.
Distribution of anatomic location and clinical manifestations associated with COVID-19 in the oral cavity. The parotid gland (n = 2) also showed manifestations. The anatomic location was not analyzed by number of individuals and the oral manifestation was not analyzed by the number of anatomic locations but rather by number of manifestations (ie, the same individual may have been affected at more than 1 anatomic site, and the same anatomic site may have shown more than 1 manifestation).
The oral mucosa is the first barrier against toxins, microorganisms, and trauma. Thus, the disruption of mucosal integrity increases the risk of oral changes.2 A variety of oral manifestations associated with COVID-19 have been reported since the outbreak. Concerns have been raised about whether the manifestations are indeed caused by SARS-CoV-2 or by different viruses that take advantage of systemic weakness during COVID-19.3
Soares et al4 and Ansari et al5 performed biopsies as well as immunohistochemical and serologic tests to rule out the presence of other viruses that commonly cause oral lesions such as herpes simplex viruses 1 and 2. The authors suggested that SARS-CoV-2 may be the causal agent of oral lesions.
Interestingly, we detected in our review that ulcerations were present in approximately 70% of individuals. Indeed, ulcers are classic presentations of a plethora of conditions such as trauma, infections, immunologic diseases, and others. Noteworthy, dermatologic manifestations, such as petechia-like and vesicobullous lesions, rash, erythematous lesion, and urticarial rash, were detected in 4 patients of our review. Ultimately, in-depth investigations using complementary assays (eg, histologic examination and polymerase chain reaction) are essential to elucidate the diagnosis of oral manifestation during COVID-19. Comprehensive oral and full-skin examinations are essential for clinical detection and referral for testing of COVID-19.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Freeman E.E., McMahon D.E., Lipoff J.B. The spectrum of COVID-19-associated dermatologic manifestations: an international registry of 716 patients from 31 countries. J Am Acad Dermatol. 2020;83(4):1118–1129. doi: 10.1016/j.jaad.2020.06.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Squier C.A., Kremer M.J. Biology of oral mucosa and esophagus. J Natl Cancer Inst Monogr. 2001;29:7–15. doi: 10.1093/oxfordjournals.jncimonographs.a003443. [DOI] [PubMed] [Google Scholar]
- 3.Amorim Dos Santos J., Normando A.G.C., Carvalho da Silva R.L. Oral manifestations in patients with COVID-19: a living systematic review. J Dent Res. Published online September 11, 2020 doi: 10.1177/0022034520957289. [DOI] [PubMed] [Google Scholar]
- 4.Soares C.D., Carvalho R.A., Carvalho K.A., Carvalho M.G., Almeida O.P. Letter to Editor: oral lesions in a patient with Covid-19. Med Oral Patol Oral Cir Bucal. 2020;25(4):e563–e564. doi: 10.4317/medoral.24044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ansari R., Gheitani M., Heidari F., Heidari F. Oral cavity lesions as a manifestation of the novel virus (COVID-19) Oral Dis. Published online June 8, 2020 doi: 10.1111/odi.13465. [DOI] [PubMed] [Google Scholar]