Abstract
Introduction
In the United States, 1.4–1.65 million people identify as transgender, many of whom will seek genital gender-affirming surgery (GAS). The number of surgeons, geographic proximity thereof, and exclusionary insurance policies has limited patient access to genital GAS.
Aim
To assess the accessibility of both feminizing and masculinizing genital GAS (vaginoplasty, metoidioplasty, and phalloplasty) by identifying the location of GAS surgeons, health insurance, or payment forms accepted.
Methods
Between February and April 2018, genital GAS surgeons were identified via Google search. Surgeons’ offices were contacted by telephone or e-mail.
Main Outcome Measure
We queried the type of genital GAS performed, the health insurance or payment forms accepted, and the type of medical practice (academic, private, or group managed-care practice).
Results
We identified 96 surgeons across 64 individual medical centers offering genital GAS. The survey response rate was 83.3%. Only 61 of 80 (76.3%) surgeons across 38 of 53 (72%) locations confirmed offering genital GAS. Only 20 (40%) U.S. states had at least one genital GAS provider. 30 of 38 (79%) locations reported accepting any form of insurance. Only 24 of 38 (63%) locations (14 academic; 10 private/group) accepted Medicaid (P = .016); 18 of 38 (47%) locations (13 academic; 5 private/group) accepted Medicare (P = .001).
Clinical Translation
Reconciliation of the public policies regarding insurance coverage for GAS with the actual practices of the providers is necessary for improving access to GAS for transgender individuals.
Strengths & Limitations
We purposefully used a methodology mirroring how a patient would find GAS surgeons, which also accounts for key limitations: only surgeons whose services were featured on the internet were identified. We could not verify the services or insurance-related information surgeons reported.
Conclusion
This study suggests that access to genital GAS is significantly limited by the number of providers and the uneven geographic distribution across the United States, in which only 20 of 50 U.S. states have at least one genital GAS surgeon.
Feldman AT, Chen A, Poudrier G, et al. How Accessible Is Genital Gender-Affirming Surgery for Transgender Patients With Commercial and Public Health Insurance in the United States? Results of a Patient-Modeled Search for Services and a Survey of Providers. Sex Med 2020;8:664–672.
Key Words: Genital Gender Affirming Surgery, Vaginoplasty, Phalloplasty, Transgender
Introduction
In the United States, 1.4–1.65 million adults (0.30–0.78% of each state) and 150,000 teens identify as transgender.1,2 Gender-affirming surgery (GAS), which refers to any surgical procedure that modifies an individual's body in accordance with their gender identity and expression, is sought after by some transgender and gender nonbinary individuals. Masculinizing genital GAS includes phalloplasty and metoidioplasty (creation of a phallic organ); feminizing genital GAS includes bilateral orchiectomy (at the time of vaginoplasty and as a stand-alone procedure) and vaginoplasty (with and without creation of a vaginal canal). These procedures have been performed by urologists, plastic surgeons, gynecologists, and general surgeons. Comprehensive perioperative care is ideally provided by a multidisciplinary surgical team.3, 4, 5
Financial constraints, inadequate insurance coverage, and variation in expertise and competence among surgeons pose significant obstacles for patients seeking high-quality genital GAS in the United States. Transgender and gender nonconforming individuals are currently either more likely to use government-funded insurance (eg, Medicare/Medicaid) or to be uninsured, than the general (cisgender) population.6,7 Historically, reimbursement for genital GAS under Medicaid or Medicare has been lower than the rates of private insurance.
This study assesses the availability of genital GAS for patients seeking these medical services throughout the United States. Our approach sought to mirror how patients gain access to providers of genital GAS, using national transgender patient care and advocacy forums coupled with internet-based keyword searches for genital GAS services.8, 9, 10, 11 We aimed to identify not only objective barriers to access to care (eg, insurance coverage; whether or not there were surgeons in the area) but also more nuanced barriers, such as the ease of access to information regarding services offered. We present data from an internet-based search for U.S. surgeons (designed to emulate how ordinary patients might seek services) who self-report providing masculinizing and/or feminizing genital GAS, and from a telephone survey of the surgeons, we identified to learn more about what specific genital GASs they offered. We assessed the geographic distribution of genital GAS providers, the specific surgery options each provider offered, and, most significantly, the proportion of providers who accept commercial, and/or Federal/State health insurance, and/or cash-only reimbursement for genital GAS services. All survey data were collected between February and April of 2018.
Methods
Identification of Providers
We used 3 methods to identify providers of genital GAS:
I. 3 of the most popular transgender community advocacy group's online GAS provider lists were queried in February of 2018: (1) transhealthcare.org,12 (2) tssurgerguide.com,13 and (3) Callen Lorde's 2015 TGNC surgery list.14 Transhealthcare.org is a search engine managed by Trans Media Network where individuals can input a desired surgery, the geographic location, and the type of insurance to locate an appropriate provider.15 Tssurgeryguide is a popular GAS information resource that is independently operated by an male-to-female transgender woman.16 Callen-Lorde Community Health Center is a renowned NYC-based LGBTQ health-care center that provides comprehensive services to New York's lesbian, gay, bisexual, and transgender communities regardless of the ability to pay.17 Using these 3 sources, we compiled a preliminary roster of surgeons listed as performing phalloplasty, metoidioplasty, and/or vaginoplasty for transgender patients on one or more of the lists.
II. A Google search for genital GAS surgeons in the United States was performed using a variety of genital GAS-related search terms: ‘gender affirming surgery surgeons,’ ‘gender confirming surgery surgeons,’ ‘sex reassignment surgery surgeons,’ ‘SRS surgeons,’ gender reassignment surgery surgeons,' ‘transgender genital reconstruction surgeons,’ ‘bottom surgery surgeons,’ ‘vaginoplasty surgeons,’ ‘phalloplasty surgeons,’ ‘metoidioplasty surgeons.’ Publicly available contact information (practice phone number and e-mail) was retrieved for all surgeons from Google in February 2018.
III. Surgeons and their office staff identified by methods I and II mentioned previously were asked to provide the names, specialties, types of surgeries offered, reimbursement options, and other survey items described in the following section. Those contacted were also asked to identify surgeons within the same practice/group if the latter were not named by search methods I and II.
Survey Distribution and Data Collection
Survey questions were generated to query providers about what specific surgery options they offer and what forms of reimbursement they accept. Each surgeon's office was contacted by phone to complete the survey. Up to 5 phone call attempts were made when necessary, and surgeons whom we were unable to reach by phone were contacted via e-mail where possible.
Each surgeon or a designated staff member (ie, medical assistant or nurse practitioner) was asked the following questions: (1) whether or not they offer genital GAS; (2) what type(s) of genital GAS they performed (vaginoplasty, phalloplasty, and/or metoidioplasty); (3) what surgical techniques (eg, skin flap and graft types) they use; (4) the names of all surgeons at the institution who currently perform genital GAS; (5) what forms of payment they accept; and (6) whether surgeries were performed at a teaching hospital or at a private facility. A complete list of survey questions can be found in Appendix.
Data Analysis
We report descriptive statistics for the data collected stratified by the surgeon and location. The location was defined as a medical center, individual or group practice of one or more surgeons who offer genital GAS.
Statistical analyses were performed using the R Statistical Computing Environment (R Core Team; Vienna, Austria) by Jonathan Grotts, MA (Department of Medicine, University of California at Los Angeles, Los Angeles, CA, USA) and supported by the NIH/National Center for Advancing Translational Science UCLA CTSI (University of California Los Angeles Clinical and Translational Science Institute) grant number UL1TR001881.
Results
Survey Respondent Characteristics
Our internet search identified 96 individual surgeons across 64 different medical centers (which we refer to as “locations”) who reported performing genital GAS. 80 of 96 surgeons (response rate: 83%) across 53 locations were successfully contacted and completed the survey. Of these respondents, only 61 of 80 (76.3%) surgeons across 38 of 53 (71.7%) locations confirmed that they performed genital GAS (any type of vaginoplasty, phalloplasty, or metoidioplasty, excluding orchiectomy as a stand-alone procedure).
Survey respondent characteristics are included in Table 1. 31 of 61 (51%) surgeons practiced across 16 academic medical centers, and 30 of 61 (49%) surgeons practiced across 22 private single and group practices.
Table 1.
Survey respondent characteristics
| Demographic | Surgeons | Locations |
|---|---|---|
| Original search | N = 96 | N = 64 |
| Survey respondents | 80 (83%) | 53 (83%) |
| Respondents performing GAS | 61 (64%) | 38 (59%) |
| Total GAS providers | N = 61 | N = 38 |
| Academic center | 31 (51%) | 16 (42%) |
| Private practice | 30 (49%) | 22 (58%) |
| Surgical specialty | ||
| General surgery | 2 (3%) | 0 (0%) |
| Gynecology | 4 (7%) | 2 (5%) |
| Plastic | 40 (66%) | 24 (63%) |
| Plastic/urology | -- | 8 (21%) |
| Plastic/urology/general surgery | -- | 1 (3%) |
| Urology | 15 (25%) | 2 (5%) |
| Urology/gynecology | -- | 1 (3%) |
| Region of the United States | ||
| West | 23 (38%) | 13 (34%) |
| Midwest | 7 (11%) | 7 (18%) |
| South | 11 (18%) | 7 (18%) |
| Northeast | 20 (33%) | 11 (29%) |
| Feminizing genital GAS (vaginoplasty) | 47 (77%) | 35 (92%) |
| Intestinal vaginoplasty | 8 (13%) | 7 (18%) |
| Penile inversion vaginoplasty | 41 (67%) | 30 (79%) |
| Scrotal skin pedicle flap vaginoplasty | 12 (20%) | 12 (32%) |
| Zero-depth vaginoplasty | 36 (59%) | 28 (74%) |
| Masculinizing genital GAS | 51 (84%) | 33 (87%) |
| Metoidioplasty | 42 (69%) | 29 (76%) |
| Phalloplasty | 46 (75%) | 30 (79%) |
| Phalloplasty with urethral lengthening | 40 (66%) | 25 (66%) |
| Radial forearm flap phalloplasty | 37 (61%) | 22 (58%) |
| Anterolateral thigh flap phalloplasty | 33 (54%) | 22 (58%) |
| Groin flap phalloplasty | 22 (36%) | 17 (45%) |
GAS = gender-affirming surgery.
With respect to surgical specialties, the majority of survey respondents were plastic surgeons (40/61; 66%), followed by urologists (15/61; 25%), gynecologists (4/61; 6.6%), and general surgeons (2/61; 3.3%).
Regarding the geographic region, the highest number of surgeon respondents were located in the Western United States, with 23 of 61 (38%) surgeons completing the survey across 13 practice locations. This was closely followed by surgeons in the Northeast region, with 20 of 61 (33%) surgeon respondents across 11 practice locations. In the Southern United States, there were 11 of 61 (18%) surgeon respondents across 7 practice locations, while in the Midwestern United States region, there were 7 of 61 (12%) responding surgeons across 7 practice locations.
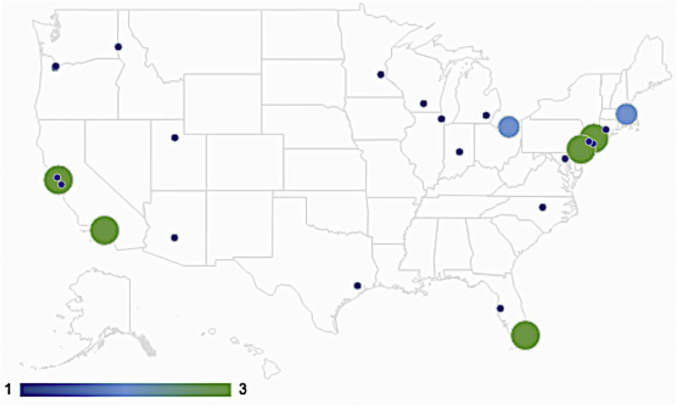
Only 20 (40%) U.S. states had at least one genital GAS surgeon (Figure 1). California had the greatest number of genital GAS surgeons: 13 surgeons across 7 practice locations. Massachusetts, Texas, New York, and Florida had 6, 6, 5, and 4 surgeons across 2, 2, 4, and 4 locations, respectively.
Figure 1.
Geographic distribution of the number of medical centers (locations) in the United States providing gender affirming surgery (GAS). Locations are identified by city. No city had greater than 3 locations performing GAS.
Insurance Coverage for Gender-Affirming Surgery
30 of 38 (79%) locations nationally reported accepting any form of insurance. 4 of 38 (11%) locations exclusively accepted commercial health insurance for reimbursement; 3 of these 4 locations were private practices and one was an academic medical center.
24 of 30 (80%) locations reported accepting Medicaid, and 18 of 30 (60%) locations reported accepting Medicare reimbursement. 14 of 16 (88%) academic centers and 10 of 22 (64%) privately operated locations accepted Medicaid (P = .016); 13 of 16 (81%) academic and only 5 of 22 (23%) private locations accepted Medicare (P = .001). All academic center locations (16/16; 100%) accepted some form of insurance. Among private practice locations, however, only 14 of 22 (64%) accepted any form of insurance; throughout the United States, 8 of 22 (36%) private practice locations accepted only cash payment for surgery, and there were no geographical differences regarding where these were located (Table 2). The locations that did not accept any form of insurance were all privately operated practices; there were no geographical differences in their location.
Table 2.
Comparison of the location type—academic centers vs private practice—and geographic region accepting different types of insurance or cash reimbursement exclusively
| Types of Insurance or Reimbursement | Academic centers (N = 16) | Private practice (N = 22) | P-value | West (N = 11) | Midwest (N = 6) | South (N = 7) | Northeast (N = 11) | P-value |
|---|---|---|---|---|---|---|---|---|
| Commercial insurance | 16 (100%) | 14 (64%) | .012 | 11 (85%) | 6 (86%) | 4 (57%) | 9 (82%) | .58 |
| Medicare | 13 (81%) | 5 (23%) | .001 | 4 (31%) | 5 (71%) | 3 (43%) | 6 (55%) | .34 |
| Medicaid | 14 (88%) | 10 (46%) | .016 | 8 (62%) | 4 (57%) | 3 (43%) | 9 (82%) | .39 |
| Cash reimbursement exclusively | 0 (0%) | 8 (36%) | -- | 2 (18%) | 3 (50%) | 1 (14%) | 2 (18%) | -- |
Academic Center vs Private Practice
We found relatively comparable numbers of academic centers (16 locations) and private practices (22 locations) offering GAS. In the Western United States, we identified 3 academic centers and 10 private practices. The Southern United States reported one academic center and 10 private practices. 5 academic centers and 2 private practices were identified in the Midwestern United States. The Northeastern United States had 7 academic centers and 4 private practices.
Availability of Feminizing Genital GAS (Vaginoplasty)
All academic (16/16; 100%) and 19 of 22 (86%) private locations offered vaginoplasty (Table 3). Each academic location (16/16; 100%) and the majority of private locations (15/19; 79%) performed both penile inversion vaginoplasty and zero-depth vaginoplasty. Intestinal vaginoplasty was the least-commonly offered feminizing surgery; only 2 of 16 (13%) academic centers and 5 of 19 (26%) private practice locations offered this. Similarly, only 4 of 16 (25%) academic and 8 of 19 (42%) private locations offered scrotal skin pedicle flap vaginoplasty.
Table 3.
Comparison of academic centers and private practices and of geographic regions offering vaginoplasty, phalloplasty, and metoidioplasty
| Type of Genital-Affirming Surgery | Academic centers (N = 16) | Private practice (N = 22) | Total (N = 38) | West (N = 13) | Midwest (N = 7) | South (N = 7) | Northeast (N = 11) | Total (N = 38) |
|---|---|---|---|---|---|---|---|---|
| Vaginoplasty | 16 | 19 | 35 | 11 | 6 | 7 | 11 | 35 |
| Intestinal vaginoplasty | 2 | 5 | 7 | 3 | 1 | 3 | 0 | 7 |
| Penile inversion vaginoplasty | 14 | 15 | 29 | 9 | 6 | 7 | 8 | 30 |
| Scrotal skin pedicle flap vaginoplasty | 4 | 8 | 12 | 5 | 2 | 3 | 2 | 12 |
| Zero-depth vaginoplasty | 13 | 15 | 28 | 10 | 6 | 7 | 5 | 28 |
| All vaginoplasty techniques | 2 | 4 | 6 | 2 | 1 | 3 | 0 | 6 |
| Phalloplasty | 15 | 15 | 30 | 10 | 5 | 6 | 9 | 30 |
| Phalloplasty with urethral lengthening | 11 | 13 | 24 | 10 | 4 | 6 | 5 | 25 |
| Radial forearm flap phalloplasty | 11 | 10 | 21 | 9 | 4 | 4 | 5 | 22 |
| Anterolateral thigh flap phalloplasty | 10 | 11 | 21 | 8 | 4 | 3 | 7 | 22 |
| Groin flap phalloplasty | 7 | 9 | 16 | 7 | 3 | 3 | 4 | 17 |
| All phalloplasty techniques | 6 | 7 | 13 | 6 | 2 | 2 | 3 | 13 |
| Metoidioplasty | 10 | 19 | 29 | 12 | 3 | 6 | 7 | 29 |
The bold indicates the total number of locations performing vaginoplasty, phalloplasty, metoidioplasty - respectively - including all surgical techniques.
Availability of Masculinizing Genital GAS (Phalloplasty and/or Metoidioplasty)
An equal number of academic and private locations (15/16; 94% and 15/22; 68%, respectively) performed phalloplasty (Table 3). 12 of 16 (80%) academic locations and 13 of 15 (87%) private locations provided phalloplasty with urethral lengthening. Most academic and private locations offer phalloplasty using a radial forearm flap (11/15; 73% and 10/15; 67%, respectively) or with an anterolateral thigh flap (10/15; 67% and 11/15; 73%, respectively). Only 7 of 15 (47%) academic and 9 of 15 (60%) private locations performed phalloplasty using groin pedicle flaps. A greater number of private practices (19/22; 86%) than academic centers (10/16; 63%) offered metoidioplasty. 17 of the 33 (52%) locations offering masculinizing procedures performed both phalloplasty and metoidioplasty. Of note, one location declined having their information regarding surgical techniques included.
Geographic Region
13 locations in the Western United States, 7 locations in the Midwestern United States, 7 locations in the Southern United States, and 11 locations in the Northeastern United States offered genital GAS (Table 3). Each region contained providers who performed vaginoplasty. The majority of locations within each region reportedly offered penile inversion vaginoplasty and zero-depth vaginoplasty; fewer used scrotal skin pedicle flap vaginoplasty. Intestinal vaginoplasty was offered almost exclusively in the Western (3/11; 27%) and Southern (3/7; 43%) United States, albeit in a relatively small number of centers (7) nationally.
Phalloplasty was also performed by providers in each region. There were no major differences in the number of locations that offered a specific technique among the regions. All of the western locations offered phalloplasty with urethral lengthening, and a majority offered the other techniques. There was no predominant technique in the Midwest. In the South, the technique offered by each provider was also phalloplasty with urethral lengthening; half of the locations performed anterolateral thigh flap and groin flap phalloplasty (3/6; 50% each). Within the Northeast, a slightly greater number (7/9; 78%) of locations offered anterolateral thigh flap phalloplasty as opposed to the other techniques. The Western United States contained the greatest number of locations offering groin flap phalloplasty (7/17; 45%), but this also reflected the overall proportion of providers within each region. Metoidioplasty was more likely to be offered in the Western United States (12/29; 76%) locations than elsewhere in the United States.
Discussion
Overall Accessibility of GAS Surgeons
Through this study, the design of which was modeled after the perspective of a patient, we sought to assess the availability of genital GAS in the United States. We focused not only on the number of U.S. providers but also the degree of access to providers: the geographic location and regional distribution, ease of contacting and speaking with providers, affordability (the forms of payment that providers do and do not accept), and the specific surgical services offered. This report uniquely explores the nationwide accessibility of genital GAS across these important access and quality care–related domains. Overall, we identified 96 providers across 64 locations, and of these, confirmed that 61 of 80 (76%) responding providers across 38 of 53 (72%) locations (16 academic institutions and 22 private single or group practices) provide genital GAS in the United States.
Consistent with what many transgender and gender nonbinary patient reports, our study findings suggest that the process to find a surgeon who offers genital GAS and accepts a specific type of insurance can indeed be difficult and frustrating. For example, despite numerous voice messages left by our group simply requesting a callback from the surgeon and/or knowledgeable staff to learn more about what surgical services the provider offered, 16 of 96 (17%) of providers across 11 of 64 (17%) locations either could not be reached or did not respond to phone calls and e-mails inquiring about GAS services. Although a number of surgeons did respond to explain what surgeries they offered, in the majority of cases, only office staff were ever available to explain what surgeries were and were not offered. Furthermore, of the 80 providers identified by our search, 19 of 80 (24%) of surgeons across 15 of 53 (28%) locations did not perform genital GAS. Approximately 80% of these providers were identified because they were featured on one or more of the advocacy group lists of providers to contact for genital GAS. Nonetheless, approximately 20% of the remaining providers who confirmed that they do not offer any type of genital GAS were identified by Google keyword searches for services that, at least at the time of our survey, they did not provide. Such discrepancies could presumably be frustrating for patients.
Another aspect of our experience contacting surgeon's offices was that after speaking with 26 of 80 (33%) of providers or their offices, 1–4 additional calls (with or without accompanying follow-up e-mail), performed over the course of a median of 5 days, were necessary to complete the survey questionnaire. Our experience suggests that, from a patient perspective, for a patient to clarify what genital GAS services a surgeon offers is very time-consuming and potentially frustrating. This inaccessibility potentially fosters increased wariness of GAS providers among transgender and gender nonbinary patients.
Insurance Coverage
Insurance coverage for genital GAS is the most important factor to improving the accessibility of genital GAS for patients. We found that only 30 of 38 (79%) locations nationwide reported accepting any form of health insurance for genital GAS. 8 medical centers, all of which were private practices, accepted cash only. 24 locations self-reported accepting Medicaid, and 18 locations self-reported accepting Medicare. Compared with private centers, a greater number of academic centers accepted Medicaid and Medicare. There were no differences in the number of locations accepting public insurance in each geographic region of the United States.
Research has shown that genital GAS can decrease gender dysphoria and improve health and the quality of life for patients who undergo it.18,19 This is recognized by all major U.S. medical organizations and is the basis for coverage of genital GAS under Medicaid and Medicare by the Department of Health and Human Services and the Affordable Care Act (ACA).20 Insurance coverage, however, remains inconsistent and varies greatly by the geographic region.2,20 As of March 2018, the Medicaid policies of 19 U.S. states (including the District of Columbia and Puerto Rico) explicitly include coverage for transition-related care, whereas in 11 states, Medicaid policies specifically exclude transition-related care, and in the remaining 22 states, there is no explicit Medicaid policy about transition-related care.21 Interestingly, in our survey, we found 2 states—Ohio and Wisconsin—where Medicaid policy explicitly excludes coverage, but at least one provider reported accepting out-of-state Medicaid reimbursement for genital GAS (Figure 2).21 In addition, our analysis identified 5 states—Florida, Idaho, Michigan, Texas, and Utah—where Medicaid has no explicit policy, but at least one provider reported accepting Medicaid reimbursement for genital GAS (Figure 2).21 This highlights the discrepancies among provider-reported insurance coverage and official government policy for gender-affirming services.
Figure 2.
U.S. Map of Medicaid/Medicare policy regarding insurance coverage for GAS and of survey data of respondents reporting acceptance of Medicare/Medicaid. Reported Policies: States whose Medicaid policy explicitly includes coverage for gender affirming surgery (GAS) (CA, CO, CT, DC, HI, IL, MD, MA, MN, MT, NV, NH, NJ, NY, OR, PA, RI, VT, and WA) (yellow). States where Medicaid policy explicitly excludes coverage of GAS (AL, GA, IA, ME, MO, NE, OH, TN, WI, and WY) (Red). States that have no explicit policy on genital GAS (AL, AZ, AK, DE, FL, ID, IN, KS, KY, LA, MI, MS, NM, NC, ND, OK, SC, SD, TX, UT, VA, and WV) (gray).17 Results from our study: States where Medicaid explicitly covers GAS and at least 1 provider in our survey reported accepting Medicaid reimbursement for genital GAS (CA, CT, MD, MA, MN, NJ, NY, NY, OR, and PA) (yellow with green vertical lines). States where Medicaid explicitly covers GAS, but our survey found no provider that accepts Medicaid for GAS (CO, DC, HI, MT, NV, NH, RI, VT, and WA) (yellow with red horizontal lines). States where Medicaid explicitly excludes GAS, but where our study identified 2 states with providers who reported that they accept Medicaid for GAS (OH, WI) (red with blue dots). States where Medicaid has no explicit policy on genital GAS, but where our survey identified 5 states with providers who reported that they accept Medicaid for GAS (FL, ID, MI, TX, and UT) (gray with green dots).
Within the United States, the cost of genital GAS can vary widely depending on the type of surgery, the surgeon's fees, length of hospitalization and hospitalization costs, travel, follow-up appointments, and related expenses.22,23 Depending on a patient's geographic location, both insured patients and GAS providers can frequently face a lengthy process to simply confirm whether or not specific genital GAS procedures are a covered benefit under the particular health insurance plan, as these are often decided by some insurance companies and State Medicaid programs on a “case-by-case” basis.22, 23, 24, 25 In our professional experience, some insurance companies impose genital GAS eligibility requirements that are not consistent with World Professional Association for Transgender Health Standards of Care guidelines (eg, requiring that, in addition to the 2 referral letters by mental-health providers confirming readiness for surgery, that patients have undergone 3 months of continuous mental health therapy before surgery, regardless of the need).18
Historically, public and commercial U.S. health insurance plans categorically excluded coverage for all GASs, with genital GAS performed only for those patients who could afford to pay cash.26 Medicare's 1981 ban on genital surgery for transgender patients was lifted in May 2014, and before the gender nondiscrimination provisions set forth in the 2010 ACA, insurance carriers could legally refuse to insure transgender people outright, on grounds that being transgender constituted a pre-existing health condition.2,4,27 Before the 2010 ACA, the majority of GAS performed in the United States was not covered by health insurance; since the ACA, the incidence of GAS in the United States that was covered by some form of health insurance has increased severalfold.28 However, whether commercial, state, and federal insurance will continue to cover GAS is far from assured. For example, on June 12, 2020, the White House administration announced a health-care policy change that narrows the definition of sex-based discrimination in health care to include discrimination based only on the sex an individual is assigned at birth and excludes discrimination on the basis of an individual's gender and sexual orientation.29, 30, 31 A similar policy change by the current White House administration had also sought to narrow the definition of sex discrimination in the workplace to exclude discrimination based on the gender and sexual identity, which was challenged in U.S. courts; on June 14, 2020, the U.S. Supreme Court, in a landmark ruling, found that the gender and sexual identity could not be parsed from “personhood,” and therefore, workplace discrimination based on the gender and sexual identity constitutes sex discrimination and is illegal.31,32 The fate of the current White House administration efforts to narrow the definition of sex discrimination to exclude the gender and sexual orientation, which is being challenged in U.S. courts, is uncertain.
Availability of Surgeons
The relatively small number of U.S. surgeons who have specialized training to perform genital GAS limits accessibility to genital GAS as there are often long waitlists and patients may be required to travel far distances to see the provider. After significant changes to Medicare/Medicaid policy in 2014 under the ACA, genital GAS has quickly become more common than it was 3 years ago. As patient demand has increased, so has interest among surgeons. While the overall number of U.S. surgeons who perform genital GAS is still small relative to other surgical subspecialties, over the course of the last 3 years, there has been a sharp rise in both the number of surgeons who offer genital GAS and the overall interest in the field. Of note, this sharp rise has not necessarily translated into increased access to genital GAS, and surgeons with training to perform genital GAS do not always accept insurance as payment.24 In addition, specific licensing programs for surgical trainees interested in performing GAS are limited in number.3,33
Limitations
This study has several limitations. Providers were identified by internet searches and based on surgeon lists generated by LGBTQ advocacy groups, and so very likely not all surgeons who perform GAS in the United States were identified by our method. In addition, some surgeon contact information was out of date (eg, some surgeons had retired or stopped performing GAS). The counterpoint to these limitations is that the methods we used to find GAS surgeons are likely used by actual patients. Another limitation is that data were self-reported, and therefore, data could not be verified (such that surgeons could in reality perform more or fewer services than what they or their staff reported) and respondents were free to potentially bias responses in a way that was positive for their institution or private practice group and/or failed to mention cost-related factors such as whether they required monetary deposits to hold a surgery date or charged additional fees outside of what is covered by insurance plans. For example, respondents from a significant number of locations were vague regarding whether they were potentially amenable to providing care for publicly insured patients as opposed to already regularly performing surgery on these patients—with systems in place (ie, letters of agreement with one or more Medicaid programs) to provide standardized care. Others were not clear about whether they already routinely accepted publicly insured patients vs whether this was something they planned to do in the future.
Another limitation was that some offices were unfamiliar with the insurance they accepted or had to qualify their responses. For example, providers stated that although they accepted a particular insurance, the insurance policy usually did not cover genital forms of GAS. Because payment agreement contracts are negotiated and/or may often require additional action from providers, the medical provider being “open to” accepting insurance does not guarantee that coverage will be available. Moreover, in a majority of cases, survey questions were answered by practice staff members rather than by surgeons directly.
It is important to note that the methodologic limitations described previously encapsulate the motivation behind this study—we aimed to expose the same challenges that patients experience when seeking services. Our experience in speaking with surgeons and staff who were unable to answer our questions about what GASs they offer, whether they accept Medicaid and Medicare health insurance (Figure 2), and what specific surgeries/techniques they offer demonstrates these challenges. In essence, the methodologic challenges and limitations of our study reflect the very same “real-world” challenges and limitations that actual patients face when seeking GAS services.8, 9, 10, 11
Conclusions
Although feminizing (vaginoplasty) and masculinizing (phalloplasty and/or metoidioplasty) genital GAS are available in the United States, these are offered by only a relatively small number of U.S. providers, clustered in greater numbers on the West Coast and Northeast. Genital GAS is more widely accessible to patients with Medicaid and Medicare health insurance at academic medical centers, as compared with private single and group practices. Based on the geographic distribution of genital GAS services, transgender and gender nonbinary people seeking surgery may be required to travel long distances for care, particularly in instances where the patient has Medicaid or Medicare insurance. Reconciliation of the public policies regarding insurance coverage for GAS (ie, Medicaid or Medicare inclusions) with the actual practices of the providers (ie, what insurance types medical practices can accept) is necessary to improve access to GAS for transgender people in the United States. Finally, other key factors that would serve to improve access to GAS care include strategies that increase the reliability, transparency, and consistency of resources available to patients to help them identify GAS surgeons and their services. Examples include databases of GAS providers, centers, and the specific surgeries/services that they provide, verified by the health-care providers and/or insurance companies, with direct contact information for patients to use to discuss services.
Statement of authorship
Alexandra Terris-Feldman: Writing - Original Draft, Formal Analysis, Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing, Funding Acquisition, Project Administration; Alessandra Chen: Writing - Original Draft, Formal Analysis, Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing, Funding Acquisition, Project Administration; Grace Poudrier: Writing - Original Draft, Formal Analysis, Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing, Funding Acquisition, Project Administration; Maurice Garcia: Conceptualization, Methodology, Investigation, Resources, Writing - Review & Editing, Funding Acquisition.
Footnotes
Conflict of Interest: Maurice Garcia, MD is the Director of the Cedars-Sinai Transgender Surgery and Health Program in Los Angeles, CA. The authors report no conflicts of interest.
Funding: None.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.esxm.2020.08.005.
Supplementary Data
References
- 1.Flores A.R., Brown T.N.T., Herman J.L. Race and ethnicity of adults who idenitfy as transgender in the United States. 2016. https://williamsinstitute.law.ucla.edu/wp-content/uploads/Race-and-Ethnicity-of-Transgender-Identified-Adults-in-the-US.pdf Available at:
- 2.Baker K.E. The future of transgender coverage. N Engl J Med. 2017;379:1801–1804. doi: 10.1056/NEJMp1702427. [DOI] [PubMed] [Google Scholar]
- 3.Schechter L.S., D’Arpa S., Cohen M.N. Gender confirmation surgery: guiding principles. J Sex Med. 2017;14:852–856. doi: 10.1016/j.jsxm.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Ettner F., Ettner R. Choosing a surgeon: an exploratory study of factors influencing selection of a gender affirmation surgeon. Transgend Health. 2016;1 doi: 10.1089/trgh.2016.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frey J.D., Poudrier G., Chiodo M.V. An update on genital reconstruction options for the female-to-male transgender patient: a review of the literature. Plast Reconstr Surg. 2017;139 doi: 10.1097/PRS.0000000000003062. [DOI] [PubMed] [Google Scholar]
- 6.James S.E., Herman J.L., Rankin S. National Center for Transgender Equality; 2015. The report of the 2015 U.S. transgender survey. Washington, DC. [Google Scholar]
- 7.Proctor K., Haffer S.C., Ewald E. Identifying the transgender population in the medicare program. Transgend Health. 2016;1:250–265. doi: 10.1089/trgh.2016.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sherman R.E., Anderson S.A., Dal Pan G.J. Real-world evidence - what is it and what can it tell us? N Engl J Med. 2016;375:2293–2297. doi: 10.1056/NEJMsb1609216. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Food & Drug Administration Real-world evidence — what is it and what can it tell us? FDA Science & Research special topics. 2019. https://www.fda.gov/science-research/science-and-research-special-topics/real-world-evidence
- 10.Mc Cord K.A. The personalized medicine challenge: shifting to population health through real-world data. Int J Public Health. 2019;64:1255–1256. doi: 10.1007/s00038-019-01293-2. [DOI] [PubMed] [Google Scholar]
- 11.Bowrin K., Briere J.B., Levy P. Cost-effectiveness analyses using real-world data: an overview of the literature. J Med Econ. 2019;22:545–553. doi: 10.1080/13696998.2019.1588737. [DOI] [PubMed] [Google Scholar]
- 12.Trans HealthCare SRS Surgeon Directory Find a surgeon for gender reassignment surgery. http://www.transhealthcare.org/find-surgeon/ Available at:
- 13.Transgender surgery guide | TSSurgeryGuide.com. http://www.tssurgeryguide.com/Welcome.html Available at:
- 14.Callen Lorde Community Health Center Gender confirming/GRS surgeon list and resources for preparing for surgery. 2015. http://callen-lorde.org/graphics/2014/12/Updated-TGNC-Surgeon-List-2015-31.pdf Available at:
- 15.About - trans health care. 2019. http://www.transhealthcare.org/about/ Available at:
- 16.About the webmaster of TSSURGERYGUIDE.COM. http://www.tssurgeryguide.com/About_me.html Available at:
- 17.About us - callen-lorde. Callen-lorde. 2019. https://callen-lorde.org/about/ Available at:
- 18.Coleman E., Bockting W., Botzer M. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgend. 2012;13:165–232. [Google Scholar]
- 19.Garcia M.M., Christopher N., Thomas A., Philip R.D. American Urologic Association (AUA). American Urological Association Education and Research, Inc; Linthicum, MD: 2017. American Urologic Association (AUA) updates series, lesson 5, volume 36: genital gender affirming surgery for transgender patients. [Google Scholar]
- 20.Padula W.V., Heru S., Campbell J.D. Societal implications of health insurance coverage for medically necessary services in the U.S. transgender population: a cost-effectiveness analysis. J Gen Intern Med. 2016;31:394–401. doi: 10.1007/s11606-015-3529-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Movement advancement project. Healthcare laws and policies: medicaid coverage for transition-related care; current as of March 5, 2018. Denver. 2018. https://www.lgbtmap.org/img/maps/citations-medicaid.pdf Available at:
- 22.Cotten T.T. 1st ed. Transgress Press; Oakland, CA: 2012. Hung jury: testimonies of genital surgery by transsexual men. [Google Scholar]
- 23.van Eijk M. Insuring care: paperwork, insurance rules, and clinical labor at a U.S. transgender clinic. Cult Med Psychiatry. 2017;41:590–608. doi: 10.1007/s11013-017-9529-8. [DOI] [PubMed] [Google Scholar]
- 24.Arnold J.D., Nelson A.E., Loubier E.M. Transgender surgery - not the benchmark for gender marker determination. JAMA Surg. 2017;152:1099–1100. doi: 10.1001/jamasurg.2017.3432. [DOI] [PubMed] [Google Scholar]
- 25.Spade D. Medicaid policy and GCS for trans people an interview with advocates. Seattle J Soc Justice. 2010;8:497–514. [Google Scholar]
- 26.Meyerowitz J. Harvard University Press; Cambridge, MA: 2009. How sex changed. [Google Scholar]
- 27.Kim M.K. National Center for Transgender Equality; Washington D.C.: 2010. Being a transgender person is no longer a pre-existing condition. Available at: https://transequality.org/blog/being-a-transgender-person-is-no-longer-a-pre-existing-condition. Accessed January 9, 2019. [Google Scholar]
- 28.Canner J.K., Harfouch O., Kodadek L.M. Temporal trends in gender-affirming surgery among transgender patients in the United States. JAMA Surg. 2018;21287:1–8. doi: 10.1001/jamasurg.2017.6231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pear R. Trump plan would cut back health care protections for transgender people. The New York Times. The New York Times, April 21, 2018. Available at: www.nytimes.com/2018/04/21/us/politics/trump-transgender-health-care.html. Accessed September 29, 2020.
- 30.Huetteman E. Shifting federal policies threaten health coverage for trans Americans. National public radio shots: health News from NPR. 2018. https://www.npr.org/sections/health-shots/2018/08/02/634583749/shifting-federal-policies-threaten-health-coverage-for-trans-americans Available at: Accessed January 9, 2019.
- 31.Simmons-Duffin S. Transgender health protections reversed by trump administration. National public radio. 2020. https://www.npr.org/sections/health-shots/2020/06/12/868073068/transgender-health-protections-reversed-by-trump-administration Available at: Accessed January 9, 2019.
- 32.Totenberg N. Supreme court delivers major victory to LGBTQ employees. 2020. https://www.npr.org/2020/06/15/863498848/supreme-court-delivers-major-victory-to-lgbtq-employees Available at: Accessed January 9, 2019.
- 33.Shuster S.M. Uncertain expertise and the limitations of clinical guidelines in transgender healthcare. J Health Soc Behav. 2016;57:319–332. doi: 10.1177/0022146516660343. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.