Abstract
Introduction:
The need to educate medical students on the social forces shaping disease and health patterns is paramount in preparing incoming physicians with the aptitudes to address health inequities. Despite its well-documented merit as a model of practice, social medicine remains underrepresented at the undergraduate medical education level. We hypothesize that the success of this student-led COVID-19 initiative proposes a tangible and innovative solution to address the lack of social medicine exposure in undergraduate medical education.
Methodology:
We sought to evaluate the impact of sustaining clinical learning during the pandemic using the social pediatrics model as a didactic vector for clerkship students. We extracted learning objectives relevant to the teaching of social medicine from the Royal College of Physicians and Surgeons of Canada’s CanMEDS framework and developed a survey aimed at evaluating the attainability of each of those objectives. The survey was distributed to students enrolled in the social pediatrics COVID-19 initiative after 6 weeks (April-May), as well as a control group.
Results:
Completing the survey were 19 students from the University of Ottawa Faculty of Medicine, 7 in the intervention group and 12 in the control group. Students that participated in the social pediatrics initiative yielded significantly higher values for the achievement of 6 out of 9 social medicine learning objectives when compared to the control group. Although the values followed a similar trend for the remaining 3 objectives, favoring the intervention group, they were not statistically significant.
Conclusion:
The positive results from this study and the COVID-19 student-led initiative template can serve as a catalyst for curricular change so as to ensure graduates are adequately trained to contend with the realities of the social landscape in which they will practice. Future plans include the incorporation of interactive social medicine experiences throughout all 4 years of medical school.
Keywords: Undergraduate medical curriculum, medical education, global health, COVID-19, social pediatrics
Introduction
The correlation between socioeconomic disadvantage and poor health outcomes over the course of one’s life is well documented,1 particularly with regards to children’s health and development.2 This unfortunate reality gave rise to social pediatrics, developed in Canada by Dr. Gilles Julien, a community and strengths-based integrated health model that seeks to understand children within the context of their own distinct biopsychosocial milieus. Such a model facilitates multi-disciplinary collaboration between experts from medicine and mental health, social work, education, law and others, and uses a wraparound approach to optimize the health and wellbeing of children and youth living in vulnerable circumstances. In this way, clinicians expand on the traditional biomedical model of curing disease, focusing on prevention and promotion of the child’s human rights thereby enabling each child to reach their full potential.
Social accountability, an accreditation requirement for all Canadian medical schools, provides a framework by which undergraduate medical curricula are meant to orient both didactic and clinical education.3 The World Health Organization delineates social accountability as a principle obligation for medical schools in order to ensure that ever-evolving health needs in the larger community are being properly identified and addressed.4 Such a guiding principle calls for intimate partnership between communities and neighborhoods in order to effectively identify and address relevant health needs.3 However, despite those principles having been put into place, most medical schools disregard the importance of incorporating social medicine electives during the clinical training of their future physicians.5 As such, the need to educate medical students on the social forces shaping disease and health patterns is paramount in preparing incoming physicians with the aptitude to competently address social and health inequities.
Despite its well-documented merit as a model of practice, social pediatrics, admittedly still in its infancy, remains underrepresented at the undergraduate medical education level. In parallel, social medicine as a whole, continues to be a neglected section of pedagogical training, particularly during clinical years.6 The ramifications of such an oversight in education lays in the continued inadequate training of generations of budding clinicians in their ability to both perceive and appreciate fundamental root causes of disease in the community and subsequently manage care appropriately.6
The advent of COVID-19 and ensuing physical distancing measures offers a unique position by which to explore the potential benefit of incorporating practical social medicine training during clinical study years, particularly through the lens of social pediatrics. Like never before, the current economic impact of physical distancing and countless other restrictions have been seen to intensify pre-existing socio-economic disparities and social isolation experienced by children and families living in vulnerable circumstances.7
In parallel with rigid public health protocols, clinical clerks across the country had seen their busy schedules grind to a halt, leaving faculties struggling to conceptualize remedies for lost clinical time. Thus, we report on an innovative social initiative and approach to clinical education geared toward empowering vulnerable families during this highly stressful time through the use of home visits, while providing students with a rare and enriching clinical learning experience. We hypothesize that the success of this student-led COVID-19 initiative proposes a tangible and innovative solution to address the lack of social medicine exposure in undergraduate medical education.
Methodology
Intervention
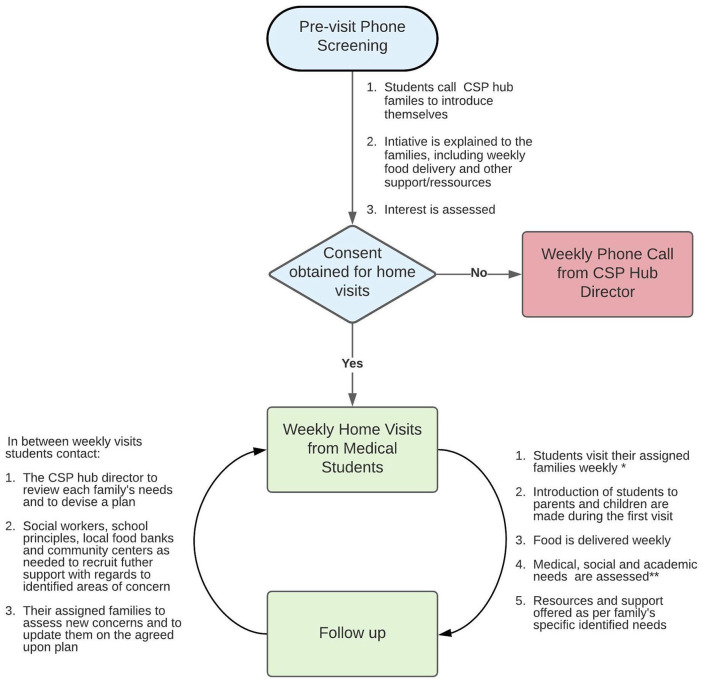
We sought to evaluate the impact of sustaining clinical learning using the social pediatrics model as a didactic vector for clerkship (ie, third and fourth year medical) students. Due to recent budget constraints, a previously established (2017) community based Social Pediatrics (CSP) hub, decided to involve clerkship students to conduct home visits for marginalized families. The clerkship students were notified about the opportunity to participate in this project through an online group dedicated to 3rd year medical students at the University of Ottawa. 10 students proceeded to contact the CSP medical director which ultimately gave rise to “More Than Just Soup,” student-led COVID19 initiative. This group of clerks was tasked to deliver donated food to families already known by the CSP hub while strictly adhering to local public health protocols. Each visit sought to provide support and resources to families (Figure 1) while also allowing students to learn about unique pediatric and domestic concerns that were later discussed with the CSP medical director. As direct liaisons between the CSP hub staff and families, students were immersed in clinical learning. To enhance the academic experience, these home visits were complemented with social medicine articles, as well as virtual guest speakers and grand round presentations (Table 1). Furthermore, teleconferences were held in order to provide the group with the opportunity to discuss and reflect on their diverse experiences.
Figure 1.
Home-visit framework.
*Ottawa Public Health Protocols were respected during the visits.
**Due to physical distancing restraints, some families opted for a subsequent phone conversation to discuss more sensitive matters/needs.
Table 1.
Topics discussed at weekly virtual meetings.
| What is Social Pediatrics? |
| How does a global pandemic affect children and families with socioeconomic disadvantages? |
| How to identify domestic violence |
| Social accountability: helping refugees, the homeless and the indigenous |
| Supports available in the community for children living with autism spectrum disorder |
| Parenting resources from a child-rights perspective |
Evaluation
Learning objectives to be acquired during clinical Clerkship training (third and fourth year medical school) are defined in a document by the Royal College of Physicians and Surgeons of Canada and follows the CanMEDS framework which delineates 7 roles: Medical Expert, Collaborator, Communicator, Health Advocate, Leader, Professional and Scholar. From that document, we extracted 9 learning objectives relevant to the teaching of social medicine. We used a 5-point Likert scale (1 = strongly disagree to 5 = strongly disagree), to develop a survey (Electronic SI) to evaluate the satisfaction and attainability of each of those objectives. The survey served as a post intervention evaluation and was distributed to all 10 students enrolled in the social pediatrics COVID-19 initiative for 6 weeks, as well as a control group made up of 20 students.
Recruitment of the control group was done by sending out an email to all 3rd year medical students at the University of Ottawa (Graduating Class of 2021) having already completed their 6-week core pediatric rotation. The rationale behind this was to compare the level of social medicine exposure and learning from the conventional Clerkship curriculum with that of our additional complementary learning experience.
Statistical analysis
A Mann–Whitney U Test was used to examine differences between intervention and control group. An alpha value of 0.05 was considered significant. All data were compiled and analyzed using Microsoft excel 2016 (version 16.16.22)
Ethical approval was waived for this project as it was deemed a quality improvement project by the Children Hospital of Easter Ontario (CHEO)’s Institutional Review Board.
Results
In total, 19 students from the University of Ottawa Faculty of medicine completed the survey, 7 in the intervention group and 12 in the control group. Medical students participating in the Social Pediatrics “More Than Just Soup” initiative exhibited a stronger overall grasp on the CanMEDS roles as compared to the control group (Table 2). Such roles included those of Communicator, Health Advocate, Medical Expert, Collaborator, Leader/Manager and Professional.
Table 2.
Royal College of Physicians and Surgeons of Canada learning objectives satisfaction and attainability differences between intervention and control groups.
| Role | Learning objective | Intervention group* | Control group* | P-value |
|---|---|---|---|---|
| Communicator | Appropriately develop and maintain ethical relationships, rapport and trust with patients, families and communities | 4.86 | 4.25 | .03 |
| Health advocate | Identify the important determinants of health, the risk factors for illness, the interaction between the population and their physical, biological and social environments, and personal attributes | 4.71 | 4 | .02 |
| Identify and propose fair means of resolving issues within the context of available resources | 4.42 | 3.75 | .08 | |
| Medical expert | Understand how variation in the determinants of health in different populations promotes or harms their health status. | 4.71 | 3.83 | .03 |
| List and interpret critical clinical findings, including psychosocial history (eg, maternal mental health, home environment, family supports). | 4.71 | 3.92 | .02 | |
| Construct an effective initial management plan, including providing support to family and/or caregivers | 4.43 | 4 | .22 | |
| Collaborator | Discuss the role of, and work collaboratively with, community and social service agencies (eg, schools, municipalities and non-governmental organizations) | 4.43 | 2.92 | <.01 |
| Leader/manager | Contribute to the delivery of high-quality health care services by advocating for and participating in quality improvement | 4.43 | 2.92 | <.01 |
| Professional | Recognize that providing quality care includes attention to the specific psychosocial needs of patients | 4.86 | 4.08 | .28 |
Mean displayed for the Likert scale (1-5).
We further analyzed and compared each learning objective within each specific role. Students that participated in the social pediatrics initiative yielded significantly higher values for the achievement of 6 of the 9 learning objectives when compared to the control group. Although the values followed a similar trend for the remaining 3 objectives, favoring the intervention group, they were not statistically significant (P > .05).
Discussion
Based on the positive results of our surveys, such an integrated pedagogic approach and take on social accountability could serve as an effective model by which to strengthen medical student understanding of essential learning objectives with regards to children and families living in vulnerable circumstances. Conducting home visits for families associated with the CSP hub provided students enrolled in this study with an opportunity to develop a more holistic experiential understanding of the social determinants of health’s impact on children’s health, wellbeing and development. This exploration of strengthened capacity becomes particularly evident when comparing the Communicator and Health Advocacy role findings, wherein the intervention group consistently scored higher, in all such learning objectives when compared to the control group. Likewise, when examining the Medical Expert role findings, it was found that medical students directly engaged in our initiative, were able to more aptly discern and appreciate each patient in the context of their own unique milieus thereby raising consciousness of the various diverse populations they might serve in future. As such, this experience allowed students to be confronted with certain biases they may have carried prior to the study. Similarly, participants worked closely with a multidisciplinary team while advocating for the wellbeing of their assigned children and families, a skill they wouldn’t otherwise have had the chance to refine during their conventional clerkship years, reinforcing their collaborator and Leader/Manager role.
Our experience highlights an innovative approach to suspended clinical time, that is meant to be synergistically beneficial to both patients and learners. In a time of uncertainty and clinical discontinuity, medical students have proven that they can mobilize to empower the most vulnerable populations, while establishing new educational opportunities to enhance their academic training. This innovative approach to learning has created an opportunity for medical students to not only glean an authentic understanding of well-known socioeconomic disparities in the community, but to truly appreciate their direct impact on health disparities.2 This experience allowed students to familiarize themselves with the social forces affecting patient wellbeing and assisted them in navigating the collaborative multidisciplinary approach to treating ailment.
This COVID-19 student-led initiative can and should serve as a template for developing social medicine electives. Future plans include working with the director of social accountability at the University of Ottawa Faculty of Medicine to collaborate with local community centers, such as the Vanier Social Pediatrics Hub, to make curricular changes that incorporate interactive social medicine experiences throughout all 4 years of medical school. Such experiences would be in the form of Pre-Clerkship and Clerkship electives, under the supervision of physicians working directly with patients living in vulnerable circumstances and experiencing socioeconomic disparities, paired with didactic learning and self-reflection. The benefits of such proposed curricular changes built on integrated learning are supported by this current study, as well as past literature.8,9 Furthermore, it has been shown that incorporating social medicine in our curriculum will likely lead to an increased number of physicians choosing to work with vulnerable sectors thereby promoting ever-improving long term health outcomes for these populations in future.9
Limitations
This study has several limitations. Firstly, the post-test nature of the data collection renders it difficult to extrapolate on the true impact of the intervention on enriching CanMEDS roles. Furthermore, as with every educational intervention involving voluntary enrollment, selection bias might have occurred. Readers should interpret these results with caution and use the study to guide the implementation of social pediatrics in undergraduate medical education that is best tailored to their institution.
Conclusion
The positive results from this study might serve as a catalyst for such curricular changes at the University of Ottawa Faculty of Medicine and for subsequent implementation of social medicine learning opportunities on an international scale.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: Institutional Review Board approval was waived as this project was considered within the realm of Quality Improvement as per the Research Ethics Board (REB) of the Children’s Hospital of Eastern Ontario
ORCID iDs: Jennifer Daccache  https://orcid.org/0000-0001-7839-4036
https://orcid.org/0000-0001-7839-4036
Michel Khoury  https://orcid.org/0000-0003-2062-7428
https://orcid.org/0000-0003-2062-7428
References
- 1. Stansfeld SA, Clark C, Rodgers B, Caldwell T, Power C. Repeated exposure to socioeconomic disadvantage and health selection as life course pathways to mid–life depressive and anxiety disorders. Soc Psychiatry Psychiatr Epidemiol. 2011;46:549-558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gupta RP, de Wit ML, McKeown D. The impact of poverty on the current and future health. Paediatr Child Health. 2007;12:667–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Health Canada. Social Accountability: A Vision for Canadian Medical School. AFMC; 2001. [Google Scholar]
- 4. Boelen C, Heck JE. Defining and measuring the social accountability of medical schools. World Health Organization; 2020. Accessed June 29, 2020 WHO/HRH/95.7. https://apps.who.int/iris/bitstream/handle/10665/59441/WHO_HRH_95.7.pdf [Google Scholar]
- 5. Kasper J, Greene JA, Farmer PE, Jones DS. All health is global health, all medicine is social medicine. Acad Med. 2016;91:628-632. [DOI] [PubMed] [Google Scholar]
- 6. Westerhaus M, Finnegan A, Haidar M, Kleinman A, Mukherjee J, Farmer P. The necessity of social medicine in medical education. Acad Med. 2015;90:565-568. [DOI] [PubMed] [Google Scholar]
- 7. Kantamneni N. The impact of the COVID-19 pandemic on marginalized populations in the United States: a research agenda. J Vocat Behav. 2020;119:103439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chin MH, Clarke AR, Nocon RS, et al. A roadmap and best practices for organizations to reduce racial and ethnic disparities in health care. J Gen Intern Med. 2012;27:992-1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff. 2010;29:799-805. [DOI] [PubMed] [Google Scholar]