Abstract
Introduction:
Chronic paediatric diseases, as bronchial asthma, affect the quality of life, which can be defined as the ability to preserve personal well-being despite sickness. These diseases have a huge impact on the quality of life of both the children, their parents and or caregivers.
Methodology:
A cross-sectional study using convenient sampling was conducted in the paediatric pulmonology clinics at Hamad General Hospital in Qatar aiming to evaluate the quality of life among caregivers of asthmatic children. The quality of life of caregivers was assessed using the standard Paediatric Asthma Caregiver Quality of Life questionnaire. Depression and asthma control were assessed using the Beck Depression Inventory; second edition and the Paediatric Asthma Control and Communication Instrument, respectively.
Results:
Total number of the caregivers was 330. Majority of the asthmatic children had controlled or partially controlled asthma (47% and 44%, respectively). Most of the caregivers had either very good or good quality of life (63% and 31%, respectively). Mean quality of life score was 5.55 ± 1.14. Males, married and father caregivers had significantly higher mean quality of life. In addition, gender, getting bothered about child’s asthma, asthma control score and depression score were significant predictors of quality of life among the caregivers.
Conclusion:
Most of the caregivers had either very good or good quality of life. Being a female, degree of asthma control and depression were important determinants of the quality of life of the caregivers. Provision of needed support to caregivers and effective approach to controlling asthma are recommended to improve the quality of life of caregivers.
Keywords: Caregivers, asthmatic children, quality of life, depression, asthma control
Introduction
Asthma is a very common chronic disease affecting 10%–20% of children and the prevalence is increasing worldwide. Asthma is a significant burden on health care costs with a great loss of productivity and reduced participation in family life.1 It was reported that asthma affects children’s social activities, physical and emotional life, and school performance. More than 14 million school days are missed per year due to asthma, and it has been associated with poor scholastic achievement. Among all chronic diseases, asthma is the most common reason for school absenteeism.2 Care for a child with asthma is a difficult and complex task. This involves monitoring of symptoms, medication supplementation, and visits to health care facilities for follow-up and in emergency situations. Due to the chronicity of asthma, caregivers could suffer from long-term stressors that affect their decision-making, work responsibilities and productivity.3 Moreover, caregivers frequently suffer from poor quality sleep because they need to be vigilant to observe any child’s symptoms especially in the midnight. They easily get stressed and wake many times to check on the child and provide care if needed.4 Some studies have found an association between asthma severity in children and reduced quality of life (QoL) and absenteeism while others have reported conflicting results.5,6 In addition, caregivers of children with controlled asthma reported higher health-related quality of life (HRQOL) scores than caregivers with uncontrolled asthma, suggesting that a child with uncontrolled asthma exacts a great burden on the caregiver and family. Achieving optimal asthma control can improve the daily functioning of the child, the caregivers and other family members.7 It was also found that, lower parental HRQOL is associated with greater asthma symptoms among affected children. Moreover, when children’s symptoms improve, parents show higher HRQOL.3 In 2006, the prevalence rate of asthma among Qatari school children was 19.8%. Despite high level of asthma among children in Qatar, studies assessing the QoL among their caregivers are scarce. So, this study aimed to assess the QoL among caregivers of asthmatic children in Qatar.
Methodology
Sample size calculation and sampling technique
In order to obtain a precise estimate and to calculate the sample size, a pilot test was conducted to assess the QoL among caregivers. The pilot test included 30 caregivers of asthmatic children selected at random. The total score of the PACQLQ questionnaire was 91. From the pilot test, the three percentiles were:
25th (56.8), 50th (71) and 75th (80.1). Accordingly, 4 quartiles were defined: poor QOL (<25th), fair (25th–<50th), good (50th–<75th) and very good (75+).
The prevalence of poor QoL in the pilot test was 23.3%
According to this, sample size was calculated as:
n = (Z2 1–α/2 × p × (1–p))/d2.
d = absolute precision on either side of the proportion = 5% (0.5)
Z = statistic for an α-error of 0.05 corresponding to a 95% confidence level = 1.96.
n = 1.96 × 1.96 × 0.233 × 0.767/0.0025 = 275.
An inflation of 20% was added to compensate for non-response, so the total sample size was 275 + 55 = 330.
The required approvals were obtained from the Institutional Review Board (IRB) committee and the Department of Paediatrics. A cross-sectional study was conducted in the paediatric pulmonology clinics at Hamad General Hospital (HGH) which are the main referral sites for asthmatic children in the country. Using non-probability convenience sampling technique, 16 pulmonology clinics that run 5 days per week were visited daily in sequence. Face to face interviews were conducted with the caregivers who attended the clinics (appointment and walk-in) and fulfilled the inclusion criteria till the desired sample size was reached. The criteria included primary caregivers of asthmatic children aged 3–13 years (3 years was selected in order to establish a proper diagnosis of asthma and 13 years as the maximum age for eligibility to receive health care at the paediatric pulmonology clinics). Verbal consent was obtained from each caregiver and full description of the study was also offered.
Study tools
QoL was assessed using the Paediatric Asthma Caregiver Quality of Life Questionnaire (PACQLQ).8 The tool consists of 13 item questions. Responses to each item were given on a 7-point Likert-type Scale where 1 denotes severe impairment and 7 denotes no impairment. Four items concern activity limitations and nine concern emotional function of caregiver. The questionnaire asked caregivers to report impairments experienced during the previous week taking into account, their response at the prior visit. The original PACQLQ has been shown to have good test–retest stability and ability to detect change.9
Asthma control was assessed using Paediatric Asthma Control and Communication Instrument (PACCI)10 which is an 11-item parent-completed questionnaire that assesses five conceptual domains of asthma status. The time frame of recall for the control domain items is 1 week, except for nocturnal awakening, which was 2 weeks. The PACCI Control domain is scored in the following way: The total score is a summation of the score assigned to each response option ranging from 0 (best asthma control) to 19 (worst asthma control). A score range of 0–3 denoted (controlled asthma), score range 4–13 denoted (partially controlled asthma) while a score range of 14–19 denoted (uncontrolled asthma). PACCI control showed good internal reliability and strong concurrent, discriminative, and known groups’ validity.10
PACQLQ and PACCI questionnaires were translated into Arabic by professional translation service, as to ensure language accuracy and to be culturally suitable to the participants. The questionnaires were translated back into English and assessed by experts in Public Health and Community Medicine. Face and translational validity were established for both PACQLQ and PACCI with scale-level content validity with universal average method (S-CVI/UA) values of .61 and .91, respectively.
Depression was assessed using the Beck’s Depression Inventory; second edition (BDI-II).11 The questionnaire includes 21 item questions which can detect possible depression in normal population and assess the severity of depression in already diagnosed patients as well. Each item includes four statements arranged in increasing severity about a particular symptom of depression. The time frame of recall for the tool is the 2 weeks prior to the onset of the interview. The maximum total score is 63. Total score was divided into four categories as follows: (0–13) minimal range that may have few symptoms but not considered depressed, (14–19) mild depression, (20–28) moderate depression and (29–63) severe depression. Evidence for estimates of concurrent, convergent and discriminant validity were established for the BDI-II.12 For the Arabic version, coefficient alphas were computed for samples of male and female undergraduates recruited from different Arab countries. The values of alpha ranged between .82–.93 and the inventory seems viable in the Arabic context.13
The questionnaires were used according to the mother tongue of the caregiver interviewed.
Data analysis
Statistical Package for Social Sciences (SPSS) version 21 was used for data analysis. QoL was expressed as the mean score per item for each domain of PACQLQ. The overall score was derived from the mean score of all items. Estimates of means, standard error and confidence intervals (CIs) were performed for each of the QoL’s domains and the total QoL. Student t-test and one-way analysis of variance (ANOVAs) were used to assess differences in the QoL mean score. Correlations were performed to explore the bivariate relations between the variables. All statistically significant variables in the univariate analysis were included in the regression analysis. Beta-coefficient, 95% CI and p values were reported. P values < 0.05 were considered statistically significant.
Results
The study included 330 caregivers with a response rate of 94.6%. Caregivers were females (76.1%), biological mothers (74.2%) and mostly married (95.8%). The majority of the caregivers aged between 30 and 49 years (80.9%) with a mean age of (37.4 ± 7.4).
Less than half of the caregivers (46.4%) were Qatari, unemployed (47.6%) and (67.6%) completed university or higher education. The majority of the caregivers (65.2%) had three or more children and were taking care of only one asthmatic child (62.1%). The majority (70.6%) of the caregivers did not complain of any chronic disease (Table 1). It was also revealed that most of the asthmatic children had either controlled (47%) or partially controlled asthma (44%) (Figure 1). Moreover, most of the caregivers had either very good (63%) or good QoL (31%). The mean QoL score was 5.55 ± 1.14 (Figure 2).
Table 1.
Sociodemographic characteristics of the caregivers of asthmatic children (N = 330).
| Variable | No. | (%) |
|---|---|---|
| Age (years) | ||
| ⩽29 | 46 | (13.9) |
| 30–49 | 267 | (80.9) |
| ⩾50 | 17 | (5.2) |
| (Mean ± SD) (37.4 ± 7.4) | ||
| Gender | ||
| Female | 251 | (76.1) |
| Nationality | ||
| Qatari | 153 | (46.4) |
| Indians | 29 | (8.8) |
| Egyptians | 21 | (6.4) |
| Jordanians | 12 | (3.6) |
| Others | 115 | (34.8) |
| Marital status | ||
| Married | 316 | (95.8) |
| Relation to child | ||
| Biological mother | 245 | (74.2) |
| Father | 77 | (23.3) |
| Grandmother | 3 | (0.9) |
| Others | 5 | (1.6) |
| Education | ||
| University and higher | 223 | (67.6) |
| Secondary | 56 | (17.0) |
| Preparatory or lower | 51 | (15.4) |
| Occupation | ||
| Employed | 173 | (52.4) |
| Household income (QR) | ||
| <10,000 | 84 | (25.5) |
| 10,000– | 87 | (26.4) |
| 20,000+ | 159 | (48.1) |
| Number of children | ||
| 1–2 | 115 | (34.8) |
| 3+ | 215 | (65.2) |
| Number of children with asthma cared by the caregiver | ||
| 1 | 205 | (62.1) |
| 2+ | 125 | (37.9) |
| Physical activity | ||
| None | 139 | (42.1) |
| Low | 122 | (37.0) |
| Moderate or high | 69 | (20.9) |
| Number of diseases* | ||
| None | 233 | (70.6) |
| One | 62 | (18.8) |
| Two or above | 35 | (10.6) |
| Family history of depression | ||
| Yes | 29 | (8.8) |
SD: standard deviation; QR: Qatari Riyal.
Mostly hypertension, diabetes mellitus and bronchial asthma.
Figure 1.
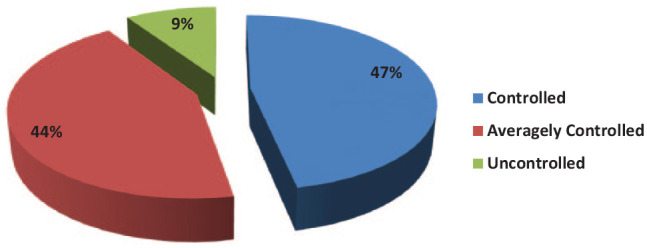
Distribution of asthmatic children according to the degree of asthma control (N = 330).
Figure 2.
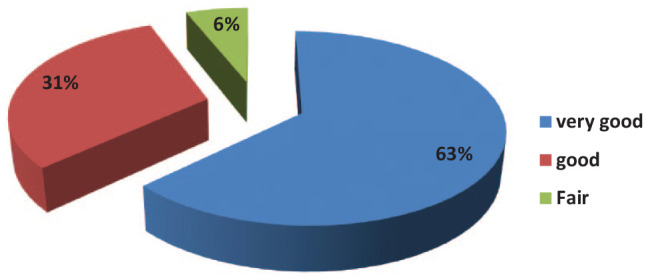
Distribution of the caregivers of asthmatic children according to the categories of QoL (N = 330).
Significantly higher mean QoL score was found among male caregivers compared to female caregivers, among married caregivers compared to unmarried caregivers and among caregivers other than biological mothers of asthmatic children (p = 0.001, p = 0.043 and p = 0.006, respectively). Depression score and number of diseases in caregivers were significantly associated with the QoL. However, all other sociodemographic characteristics showed no significant associations (Table 2).
Table 2.
Relationship between QoL mean score and sociodemographic characteristics of the caregivers of asthmatic children (N = 330).
| Variable | QoL Mean ± SD | p value |
|---|---|---|
| Age (years) | ||
| ⩽29 | 5.45 ± 1.06 | 0.54 |
| 30–49 | 5.55 ± 1.16 | |
| ⩾50 | 5.81 ± 1.00 | |
| Gender | ||
| Male | 5.90 ± 0.97 | 0.001# |
| Female | 5.44 ± 1.17 | |
| Nationality | ||
| Qatari | 5.51 ± 1.13 | 0.55# |
| Non-Qatari | 5.59 ± 1.16 | |
| Marital status | ||
| Married | 5.58 ± 1.12 | 0.043# |
| Others | 4.95 ± 1.44 | |
| Relation to child | ||
| Biological mother | 5.45 ± 1.17 | 0.006# |
| Others | 5.83 ± 1.01 | |
| Education | ||
| Below university level | 5.50 ± 1.12 | 0.600# |
| University and higher | 5.57 ± 1.15 | |
| Occupation | ||
| Unemployed | 5.47 ± 1.10 | 0.245# |
| Employed | 5.62 ± 1.17 | |
| Household income (QR) | ||
| <10,000 | 5.58 ± 1.08 | 0.948 |
| 10,000– | 5.55 ± 1.17 | |
| 20,000+ | 5.53 ± 1.16 | |
| Number of children | ||
| ⩽2 | 5.45 ± 1.18 | 0.127# |
| 3+ | 5.60 ± 1.12 | |
| Number of children with asthma cared by the caregiver | ||
| 1 | 5.54 ± 1.11 | 0.805# |
| 2+ | 5.57 ± 1.20 | |
| Physical activity | ||
| None | 5.46 ± 1.20 | 0.21 |
| Low | 5.70 ± 1.07 | |
| Moderate or higher | 5.46 ± 1.13 | |
| Number of diseases | ||
| None | 5.57 ± 1.16 | 0.035 |
| One | 5.74 ± 1.03 | |
| Two and above | 5.12 ± 1.15 | |
| Family history of depression | ||
| Yes | 5.38 ± 1.20 | 0.395# |
| No | 5.57 ± 1.14 | |
| Depression score | ||
| Minimal | 5.76 ± 1.01 | 0.000 |
| Mild | 5.01 ± 1.30 | |
| Moderate | 4.69 ± 1.28 | |
| Severe | 4.37 ± 1.08 | |
SD: standard deviation; QR: Qatari Riyal.
Student’s t-test was used. All other comparisons used ANOVA.
Significant associations were observed between QoL mean score and all indicators of asthma control. QoL mean score was significantly higher among those who have not been bothered by their children’s condition. Moreover, QoL mean score was significantly higher among caregivers of children who have not visited the emergency rooms or have not been hospitalized since their last visit. QoL mean score was also significantly higher among caregivers of children who have not used oral steroids. In addition, QoL mean score was significantly higher among caregivers of children with controlled asthma (6.30 ± 0.66) compared to those with partially controlled (4.99 ± 1.03) and uncontrolled asthma (4.42 ± 1.14; Table 3).
Table 3.
Relationship between QoL mean score and asthma control indicators among the caregivers of asthmatic children (N = 330).
| Variable | Mean ± SD | p value |
|---|---|---|
| Asthma status since last visit to the doctor: | ||
| Better | 5.60 ± 1.12 | 0.03 |
| Same | 5.57 ± 1.13 | |
| Worse | 4.97 ± 1.23 | |
| Been bothered by child’s asthma since last visit to the doctor: | ||
| Not bothered | 5.88 ± 0.97 | 0.000 |
| Somehow bothered | 5.24 ± 1.18 | |
| Very bothered | 4.83 ± 1.22 | |
| Been to the emergency since last visit to the doctor: | ||
| No | 5.83 ± 1.04 | 0.000# |
| Yes | 5.18 ± 1.16 | |
| Hospitalized for asthma since last visit to the doctor: | ||
| No | 5.59 ± 1.11 | 0.043# |
| Yes | 4.73 ± 1.48 | |
| Used oral steroids since last visit to the doctor: | ||
| No | 5.67 ± 1.10 | 0.000# |
| Yes | 5.12 ± 1.19 | |
| Forgets to give asthma medicine when the child feels fine: | ||
| Not supposed to take asthma medicine | 5.88 ± 1.01 | 0.003 |
| None of the time | 5.53 ± 1.10 | |
| Some of the time | 5.13 ± 1.30 | |
| Most of the time/all of the time | 5.29 ± 1.32 | |
| Asthma control score | ||
| Controlled | 6.30 ± 0.66 | 0.000 |
| Partial control | 4.99 ± 1.03 | |
| Uncontrolled | 4.42 ± 1.14 | |
SD: standard deviation.
Student’s t-test was used. All other comparisons used ANOVA.
The correlation matrix presented in (Table 4) demonstrates significant positive correlations between PACQLQ score and each of emotional function (r = .955) and activity limitation (r = .851). A positive correlation between both domains was also found (r = .665). The table also revealed significant negative correlations between PACQLQ score and each of asthma control score (r = –.647) (Graph1) and depression score (r = –.364) (Graph 2). All correlations were statically significant at (p < 0.01).
Table 4.
Correlations between PACQLQ score and its domains (emotional function and activity limitation) with asthma control score and depression score among the caregivers of asthmatic children (N = 330).
| PACQLQ score “r” | PACQLQ Emotional function “r” | PACQLQ Activity limitation “r” | Asthma control Score “r” | Depression score “r” | |
|---|---|---|---|---|---|
| PACQLQ score | 1 | 0.955 | 0.851 | −0.647 | −0.364 |
| PACQLQ emotional function | 0.955 | 1 | 0.665 | −0.566 | −0.384 |
| PACQLQ activity limitation | 0.851 | 0.665 | 1 | −0.654 | −0.262 |
| Asthma control score | −0.647 | −0.566 | −0.654 | 1 | 0.174 |
| Depression score | −0.364 | −0.384 | −0.262 | 0.174 | 1 |
PACQLQ: paediatric asthma caregiver quality of life questionnaire.
All correlations are statistically significant at p < 0.01.
Graph 1.
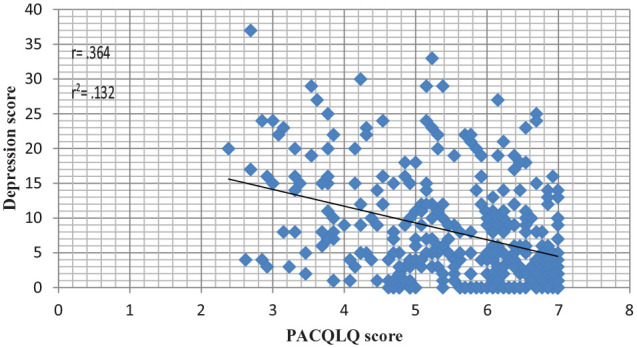
Relation between depression score and PACQLQ score.
Graph 2.
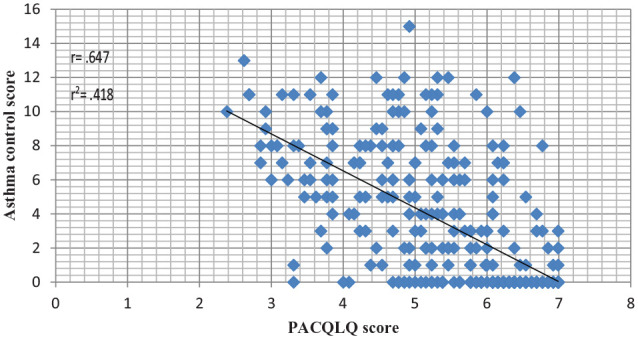
Relation between asthma control score and PACQLQ score.
In multivariate regression analysis, gender, been bothered about child’s asthma, asthma control score, and depression score were the predictors of QoL among the caregivers of asthmatic children (Table 5).
Table 5.
Multivariate regression analysis for the predictors of QoL among the caregivers of asthmatic children (N = 330).
| Variable | B | Standardized beta coefficient | 95% CI | p value |
|---|---|---|---|---|
| Gender (female) | −0.135 | −0.050 | −0.83 to 0.12 | 0.010 |
| Been bothered by child’s asthma since last visit to the doctor | −0.274 | −0.176 | −0.39 to 0.15 | 0.000 |
| Asthma control score | −0.166 | −0.555 | –0.19 to 0.14 | 0.000 |
| Depression score | −0.034 | −0.228 | –0.04 to 0.02 | 0.000 |
| Constant | 6.58 |
The prediction model was statically significant p < 0.001.
Discussion
Asthma is a very common chronic disease among paediatric population and has a great impact on the HRQOL of affected children and their caregivers.14 Poorly controlled asthma affects children physically, socially, emotionally and also can impair their educational level. However, the impact of asthma is not only on the children, but also on their caregivers, who suffer from the burden of care and the disturbance in their daily life.7
QoL of caregivers of asthmatic children was studied in different countries with varying results. This study revealed that most of the caregivers had either very good or good QoL, with a mean score of 5.55 ± 1.14 (Figure 2). Higher QoL mean scores were found among caregivers of asthmatic children in Sweden (6.07 ± 0.93)9 and Spain (5.83 ± 1.2),15 while lower values were found in United States (4.3)16 and Saudi Arabia (3.8).17 This could be explained by the different factors that determine the QoL and how these determinants are valued by caregivers.
Determinants of the QoL of caregivers varied in different studies. Younger caregivers were found to have a significantly lower QoL than older ones.18 This study also confirmed the non-significant trend towards a lower QoL among younger caregivers. However, the literature highlighted conflicting opinions regarding caregivers’ age and QoL. Older caregivers may suffer from lower physical health, and they are more affected by depression, while younger caregivers usually try to keep a balance between their care responsibilities and work demands that affect their social and mental lives. On the other hand, typically middle-aged caregivers get anxious about missed workdays, taking leaves of absence, work disruptions and decreased productivity.19,20
Income was another socioeconomic factor that found to have an impact on the QoL of the caregivers in some studies.21,22 Mothers in less-affluent socioeconomic groups were found to have worse QoL scores than those in higher ones.23 Children from low socioeconomic families commonly have many health risks and are more likely to suffer from health problems early in life. Access to health care is also difficult for many families in low-income groups. Moreover, in lower socio-economical classes, parents are less likely to receive high-quality education and qualifications, and fewer job opportunities and services. They also face harder social life including complicated personal relationships and are more exposed to mental and physical health problems and therefore have a lower QoL.24 So, it can be clearly suggested that higher income was associated with higher QoL.21 However, this study did not find a significant relation between house-hold income and the QoL of the caregivers.
This study also revealed significant associations between some demographic variables and caregiver’s QoL mean score. Married caregivers were found to have better QoL than other categories. This was also agreed by other different studies.25,26 Unmarried caregivers carry physical and psychological burdens for taking care of their asthmatic children and may suffer from lack of support and difficulties in taking decisions. Lower QoL was also found among biological mothers and female caregivers. These findings agree with other previous studies.17,27 Furthermore, chronic illness in children especially that developed early in life has an impact on the QoL of mother caregivers and their children.28 Moreover, this study reported that female gender was the only sociodemographic variable appeared to be a significant determinant of the QoL among the caregivers in the multivariate analysis (Table 5).
It was also found that men and women caregivers had behaviour problems. However, women were more likely to have stress and severe depression than men.29 It was reported that 75% of caregivers who experienced very stressful feelings physically, financially and economically were women.30 This finding was also presented in a study conducted in Las Vegas.26
It is also worth mentioning that no significant association was unexpectedly found between child characteristics and the QoL of the caregivers in the present study.
The multivariate analysis in this study agreed with other previous studies.7,9 Multiple studies31,32 revealed that parents caring for older children with asthma are having better QoL than those caring for younger ones. Caregivers of older children also reported less missed workdays. Moreover, a study conducted in Iran,33 found lower QoL among caregivers of male asthmatic patients. However, gender and age of the child were not significant determinants of the QoL among the caregivers in this study.
Asthma control score was a significant predictor of the QoL among the caregivers in the multivariate analysis in this study (Table 5). This was also established in other multiple studies.25,34,35 In a previous study, negative correlation was found between PACQLQ scores and asthma severity scores for children. This was reported using a 7-item questionnaire that explores different parameters such as day and night symptoms, frequency of wheezes, and others (r = –.39, p < .001).14
Caregivers of children with poorly controlled asthma showed significantly greater work and activity impairment. They also showed lower emotional QoL and limitations in normal daily activities.8 Those findings agreed with this study which reported a significant negative correlation between PACQLQ score and asthma control score (r = –.647; p < .01). Similarly, significant negative correlations were also found between asthma control score and each of the two QoL domains (activity limitation and emotional function). These findings suggest that caregivers of children with either moderate or severe asthma are more likely to have activity limitations and to get more emotionally responsible. Therefore, it is recommended to provide caregivers with the support and care they need and to properly manage asthma in children. This may help improve the QoL of both the child and his or her caregiver.
Study limitations
The most important limitations of this study are the inability to generalize the results to all caregivers' population. Although HGH is the main referral site, enrolment of caregivers from one hospital may limit generalization. Moreover, causality between depression and QoL could not be determined. In addition, the subjective assessment of asthma status through self-report questions concerning last visits to the clinic or last 2 months may not be so precise. It is worth mentioning that other confounders such as life stressors and events may influence QoL. Furthermore, the short period of follow-up may have not revealed the long-term effect of asthma control on the QoL of the caregivers.
Conclusion
Most of the caregivers reported very good or good QoL. Being female, degree of asthma control, and depression were important determinants of the QoL among caregivers. Asthma control score had significant associations with both the QoL and depression score.
Recommendations
From this study, it is highly recommended to manage and control asthma in children. Physicians and health care providers should work closely with caregivers. This could be achieved through regular visits, follow-ups, and strengthening communication. Furthermore, engaging caregivers in caregiver education programmes will help them develop control skills and promote coping strategies. In addition, establishing support groups for caregivers would provide support and inspiration. Members can share ideas, learn from the experience of others and find useful information related to asthma.
Supplemental Material
Supplemental material, sj-pdf-1-smo-10.1177_2050312120973500 for Quality of life among caregivers of asthmatic children attending pulmonology clinics at Hamad General Hospital, Qatar by Fahad Mohammed Shaikhan and Mohamed M Makhlouf in SAGE Open Medicine
Supplemental material, sj-pdf-2-smo-10.1177_2050312120973500 for Quality of life among caregivers of asthmatic children attending pulmonology clinics at Hamad General Hospital, Qatar by Fahad Mohammed Shaikhan and Mohamed M Makhlouf in SAGE Open Medicine
Supplemental material, sj-pdf-3-smo-10.1177_2050312120973500 for Quality of life among caregivers of asthmatic children attending pulmonology clinics at Hamad General Hospital, Qatar by Fahad Mohammed Shaikhan and Mohamed M Makhlouf in SAGE Open Medicine
Supplemental material, sj-pdf-4-smo-10.1177_2050312120973500 for Quality of life among caregivers of asthmatic children attending pulmonology clinics at Hamad General Hospital, Qatar by Fahad Mohammed Shaikhan and Mohamed M Makhlouf in SAGE Open Medicine
Acknowledgments
The authors would like to express their sincere thanks to Hamad Medical Corporation Research Centre for their support. They express their appreciation to the paediatric pulmonology clinics staff at Hamad General Hospital for their support during data collection. They are immensely grateful to the caregivers for their valuable participation in the research. They also thank Dr Rajvir Singh for his contribution in data analysis.
Footnotes
Authors contributions: F.S. conceived the research and participated in the design and collection of data. Also, F.S. drafted the manuscript. M.M. participated in the design of the study, in the interpretation of data and in revising it critically for data contents. All authors read and approved the final manuscript.
Consent to publish: The research did not involve any individual person’s data in any form (including individual details, images or videos) and no access to the patients’ files was needed.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The manuscript was approved by the Institutional Review Board (IRB) committee – Hamad Medical Corporation, RP No. (13448/13). In addition, the requirement for written consent was waived ‘exempted’ by the Committee. As per IRB policy, no breach of confidentiality that is of high risk to participants or may cause potential harm. The study did not involve any individual person’s data in any form (including individual details, images or videos) and no access to the patients’ files (records) was needed
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Participation in the research study was voluntary and a consent form ‘information sheet’ was given to each participant before the interview. The sheet explained the aim of the research study and participant rights.
ORCID iD: Fahad Mohammed Shaikhan  https://orcid.org/0000-0001-6077-9923
https://orcid.org/0000-0001-6077-9923
Supplemental material: Supplemental material for this article is available online.
References
- 1. Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention, 2008, http://www.ginasthma.org
- 2. Butz AM, Riekert KA, Eggleston P, et al. Factors associated with preventive asthma care in inner-city children. Clin Pediatr 2004; 43(8): 709–719. [DOI] [PubMed] [Google Scholar]
- 3. Halterman JS, Yoos HL, Conn KM, et al. The impact of childhood asthma on parental quality of life. J Asthma 2004; 41(6): 645–653. [DOI] [PubMed] [Google Scholar]
- 4. Rebecca A, Natalie R, Toby C, et al. Night watch: sleep disruption of caregivers of children with asthma in Detroit. J Asthma Allerg Educ 2013; 4: 217–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Moonie S, Sterling DA, Figgs LW, et al. Asthma status and severity affects missed school days. J School Health 2006; 76: 18–24. [DOI] [PubMed] [Google Scholar]
- 6. Everhart RS, Fiese BH. Asthma severity and child quality of life in pediatric asthma: a systematic review. Patient Educ Couns 2009; 75(2): 162–168. [DOI] [PubMed] [Google Scholar]
- 7. Dean BB, Calimlim BC, Sacco P, et al. Uncontrolled asthma: assessing quality of life and productivity of children and their caregivers using a cross-sectional Internet-based survey. Health Qual Life Outcomes 2010; 8: 96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Juniper EF, Guyatt GH, Feeny DH, et al. Measuring quality of life in the parents of children with asthma. Qual Life Res 1996; 5(1): 27–34. [DOI] [PubMed] [Google Scholar]
- 9. Reichenberg K, Broberg A. The paediatric asthma caregiver’s quality of life questionnaire in Swedish parents. Acta Paediatr 2001; 90(1): 4560–4550. [DOI] [PubMed] [Google Scholar]
- 10. Okelo SO, Eakin MN, Patino CM, et al. The pediatric asthma control and communication instrument asthma questionnaire: for use in diverse children of all ages. J Allergy Clin Immunol 2013; 132(1): 55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Beck AT, Gregory KB, Robert AS. Beck depression inventory-II (BDI-II). San Antonio, TX: The Psychological Corporation, 1996 [Google Scholar]
- 12. Osman A, Kopper BA, Barrios F, et al. Reliability and validity of the Beck depression inventory-II with adolescent psychiatric inpatients. Psychol Assess 2004; 16(2): 120–132. [DOI] [PubMed] [Google Scholar]
- 13. Alansari BM. Internal consistency of an Arabic adaptation of the beck depression inventory-II with college students in eighteen Arab countries. Soc Behav Pers 2006; 34(4): 425–430. [Google Scholar]
- 14. Asher I, Pearce N. Global burden of asthma among children. Int J Tuberc Lung Dis 2014; 18(11): 1269–1278. [DOI] [PubMed] [Google Scholar]
- 15. Cano G, Diaz V, Carvajal U, et al. Group education on asthma for children and caregivers: a randomized, controlled trial addressing effects on morbidity and quality of life. J Investig Allergol Clin Immunol 2007; 17(4): 216–226. [PubMed] [Google Scholar]
- 16. Lindsay T, Elizabeth W, Susan S, et al. Boston Children's Hospital Community Asthma Initiative (CAI): comparing changes in caregiver quality of life (QOL) and child asthma control, and geographic information systems (GIS) localization of asthma triggers, 2014, https://apha.confex.com/apha/142am/webprogram/Paper305506.html
- 17. Fatma Z, Noha A. Quality of life among caregivers of asthmatic children. SSFCM J 2006, http://www.ssfcm.org/public/english/Content/index/secId/321/cntId/583/page/1/
- 18. Barrera M, Atenafu E, Doyle J, et al. Differences in mothers’ and fathers’ health-related quality of life after pediatric SCT: a longitudinal study. Bone Marrow Transplant 2012; 47(6): 855–859. [DOI] [PubMed] [Google Scholar]
- 19. Braman SS. The global burden of asthma. Chest 2006; 130(1): 4–12. [DOI] [PubMed] [Google Scholar]
- 20. Given B, Sherwood PR, Given B, Sherwood PR. Family care for the older person with cancer. Semin Oncol Nurs 2006; 22(1): 43–50. [DOI] [PubMed] [Google Scholar]
- 21. US Department of Health and Human Services; Agency for Healthcare Research and Quality. National Healthcare Disparities Report, 2012, https://www.ahrq.gov/research/findings/nhqrdr/index.html
- 22. Bloom B, Cohen RA, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey2010. Vital Health Stat 2011; 10(250): 1–80. [PubMed] [Google Scholar]
- 23. Victorino CC, Gauthier AH. The social determinants of child health: variations across health outcomes – a population-based cross-sectional analysis. BMC Pediatr 2009; 9(17): 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cerdan NS, Alpert PT, Moonie S, et al. Asthma severity in children and the quality of life of their parents. Appl Nurs Res 2012; 25(3): 131–137. [DOI] [PubMed] [Google Scholar]
- 25. Wyrwich KW, Ireland AM, Navaratnam P, et al. An assessment of change in asthma control among adolescents and adults with persistent asthma in mometasone furoate/formoterol fumarate clinical trials. J Asthma 2011; 48(1): 48–56. [DOI] [PubMed] [Google Scholar]
- 26. Noelle C. Asthma severity in school-children and the quality of life of their parents 2009, digitalscholarship.unlv.edu/cgi/viewcontent.cgi?article=2187&context… [Google Scholar]
- 27. Waxmonsky J, Wood BL, Stern T, et al. Association of depressive symptoms and disease activity in children with asthma: methodological and clinical implications. J Am Acad Child Adolesc Psychiatry 2006; 45(8): 945–954. [DOI] [PubMed] [Google Scholar]
- 28. Center on the developing child at harvard university. The foundations of lifelong health are built in early childhood 2010, http://www.developingchild.harvard.edu [Google Scholar]
- 29. Harvard Health Publishing. Harvard Mental Health Letter. Women and depression, 2011, https://www.health.harvard.edu/womens-health/women-and-depression
- 30. Office on Women Health, US Department of Health Human Services. Caregiver stress fact sheet, 2012, www.womenshealth.gov›publications›OurePublications
- 31. Duncan CL, Hogan MB, Tien KJ, et al. Efficacy of a parent-youth teamwork intervention to promote adherence in pediatric asthma. J Pediatr Psychol 2013; 38(6): 617–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sheniz M, Xuan H, David AS. Quality of life estimation with structural equation modeling in school aged children with asthma. Global Health Governance 2009; 3(1); 1–16. [Google Scholar]
- 33. Fariborz Z, Mostafa M, Masoud M. Assessment of quality of life in Iranian asthmatic children Iranian journal of allergy. Asthma Immunol 2006; 5(2): 79–83. [PubMed] [Google Scholar]
- 34. Gordon RB, Christina B, Jane MG. Socioeconomic, family and pediatric practice factors affecting the level of asthma control. Pediatrics 2009; 123(3): 829–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Annett RD, Bender BG, Skipper B, et al. Predicting moderate improvement and decline in pediatric asthma quality of life over 24 months. Qual Life Res 2010; 19(10): 1517–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-smo-10.1177_2050312120973500 for Quality of life among caregivers of asthmatic children attending pulmonology clinics at Hamad General Hospital, Qatar by Fahad Mohammed Shaikhan and Mohamed M Makhlouf in SAGE Open Medicine
Supplemental material, sj-pdf-2-smo-10.1177_2050312120973500 for Quality of life among caregivers of asthmatic children attending pulmonology clinics at Hamad General Hospital, Qatar by Fahad Mohammed Shaikhan and Mohamed M Makhlouf in SAGE Open Medicine
Supplemental material, sj-pdf-3-smo-10.1177_2050312120973500 for Quality of life among caregivers of asthmatic children attending pulmonology clinics at Hamad General Hospital, Qatar by Fahad Mohammed Shaikhan and Mohamed M Makhlouf in SAGE Open Medicine
Supplemental material, sj-pdf-4-smo-10.1177_2050312120973500 for Quality of life among caregivers of asthmatic children attending pulmonology clinics at Hamad General Hospital, Qatar by Fahad Mohammed Shaikhan and Mohamed M Makhlouf in SAGE Open Medicine


