Abstract
Background. Reducing the under-30-day readmission for heart failure (HF) patients is a modifiable quality-of-care measure, yet the role of diet in HF readmissions and cost-effective HF care remain ill-defined. Methods. Medical chart review was conducted to determine cause(s) for HF treatment failure. Randomized controlled trial–backed machine learning models were employed to assess the relationship of culinary medicine education with HF 30-day readmission rate and cost. Results. Of 1031 HF admissions, 130 occurred within 30 days of discharge (12.61%.) Nearly two-thirds of individuals were male (64.02%), while the mean age and median length of stay were 64.33 ± 14.02 and 2, respectively. Medication noncompliance (34.62%) was the most common etiology for 30-day readmissions, followed by dietary noncompliance (16.92%), comorbidity (16.92%), a combination of dietary and medication noncompliance (10%), HF exacerbation (10%), iatrogenic (10%), and drug abuse (1.54%). Medication noncompliance contributed to the highest gross charge by readmission, costing a total of $1 802 096. Compared with traditional care, culinary medicine education for HF patients would prevent 93 HF readmissions and save $3.9 million in an estimated 4-year period. Conclusion. Though pharmacological treatment remains a focal point of HF management, diet-based approaches may improve tertiary HF prevention and reduce HF-associated health care expenditures.
Keywords: heart failure, cooking, nutrition therapy, patient readmission, lifestyle
‘Diet is an important modifiable risk factor for cardiovascular disease prevention and management . . .’
Approximately 6.5 million adults in the United States have heart failure (HF), and projections suggest that disease prevalence will increase to 8 million, or 1 in every 33, by 2030.1,2 HF is the number one cause of hospitalization among American adults, and the cost for treating such patients is expected to increase 3-fold to $160 billion over the next decade.3 The 30-day readmission rate for HF, a quality-of-care measure, continues to be an appealing target to address as a means to both improve morbidity and reduce overall health care expenditures.4 In light of these epidemiological trends, there is a new need to identify novel and region-specific risk factors for HF readmission in diverse populations to improve tertiary cardiovascular disease prevention.
Unplanned readmissions for HF remain a common event, as about 1 in every 5 patients are readmitted within 30 days.5,6 Most recent data have suggested a median risk-standardized 30-day readmission rate of 21.9%, with a range from 17.0% to 28.2%.5 Evidence suggests that approximately one-half of these readmissions are due to HF recurrence and related cardiovascular conditions,7 such as arrhythmias, while all other readmissions are due to comorbid and sociodemographic factors, including respiratory and renal dysfunction, medication noncompliance, non-white race, and female sex.8 Meta-analysis of observational studies however suggests that short-term risk for HF readmissions is greatest among individuals with noncardiac comorbidities, especially chronic kidney and cerebrovascular disease.9 Despite this multitude of research, there is very limited research on the etiological role of diet in HF readmissions. Diet is an important modifiable risk factor for cardiovascular disease prevention and management,10 and healthy dietary modifications may be an efficient means to reduce direct and indirect costs associated with HF.11
Several intervention approaches, both at the individual and systems-based level, have been conducted to reduce HF readmission and thus broader health care costs. For example, particularly among patients with HF with reduced ejection fraction, medication adherence to beta-blockers, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers are significantly associated with reductions in mortality, readmissions, and thus health system costs.12,13 Likewise, randomized controlled trial (RCT) evidence demonstrates that formal health education and telemonitoring in HF patients, compared with traditional care, is associated with over $7000 reduction in hospital cost per patient, primarily driven by a 30% decrease in HF readmissions.14 In a similar fashion, nurse-directed multidisciplinary interventions lead to an approximate $500 cost-savings and greater than 50% reduction in total readmissions when compared with routine clinical care in HF patients.15 These data suggest that a wide variety of interventions may help improve cost-efficacy in HF treatment and underline the fact that a majority of HF hospital readmissions remain preventable.
Nutritional interventions for reducing HF costs and readmissions remain largely unexplored. Among limited evidence exists a pilot randomized controlled trial coined, geriatric out-of hospital randomized meal trial in heart failure (GOURMET-HF), conducted in 66 HF patients.16 The intervention group in GOURMET-HF received 4 weeks of home-delivered sodium-restricted Dietary Approaches to Stop Hypertension (DASH) meals, while routine clinical care was provided to those randomized to the control group. Investigators observed a directionally favorable, but only borderline significant reduction 30-day HF readmissions in the intervention group. Therefore, while adherence to the DASH and Mediterranean diets have been associated with a reduced risk for developing HF,17-19 more research is required to determine the optimal delivery of dietary interventions for reducing 30-day readmissions and associated HF costs.
The age-adjusted HF mortality rate for the Southeastern region of the United States, including Louisiana, Alabama, Arkansas, Mississippi, Oklahoma, and Georgia, is 69% higher than the national rate.20 Obesity, hypertension, and type II diabetes may be key drivers of these trends and these upstream risk factors, similar to HF mortality, disproportionately affect the Southeastern United States.21,22 These sobering statistics suggest that the United States may be burdened by the presence of a “heart failure belt,” but more important, should be a call-to-action to seek novel, yet simple and generalizable strategies to help address HF and associated risk factor burden. The Mediterranean and DASH diets not only reduce risk not only for HF but also reduce risk for the disease’s upstream risk factors and subclinical correlates, including obesity, type II diabetes, hypertension, and left ventricular diastolic dysfunction.23,24 Given these data and the fact that Louisiana has the third highest rate of cardiovascular disability-adjusted life years in the country,22 Louisiana represents a population likely to benefit from a reduction in the 30-day readmission rate for HF via a dietary approach.
Given the above nutrition-related cardiovascular disease epidemic, novel research methodologies are increasingly being explored to accelerate the rate of clinically effective, cost-efficient, and socially equitable health care. Artificial intelligence–driven machine learning methods demonstrate comparable results to traditional statistics but on larger, more complex datasets, and provide closer to real-time automated analyses to inform faster community and clinical interventions.25 Recent studies have shown that machine learning and the even more advanced deep learning techniques can generate improved prediction of HF hospital readmission compared with more traditional methods.26,27 Yet there remains a paucity of studies assessing the application of these machine learning techniques to accelerate HF care by knowing who will decompensate and how to optimally prevent HF readmissions. By knowing what works clinically and financially, and effectively planning a proposed HF intervention in advance, machine learning has the potential to significantly increase the success rate of trials and thus enhance clinical and public health practices informed by such research. This study is the first known machine learning-guided prospective cohort study using RCT and observational evidence to assess the potential clinical and cost impact of culinary medicine interventions on improving HF outcomes.
Methods
Study Design
This prospective cohort study was conducted in 2 phases: first, adult patients older than 18 years were identified sequentially presenting to a tertiary academic medical center in the Southeastern United States from January 2012 to October 2015 with ICD-9 (International Classification of Diseases, Ninth Revision) and ICD-10 codes for HF and then analyzed according to their reason for HF admission; second, simulated machine learning–guided analysis was conducted based on the largest RCT on the Mediterranean diet and preventive cardiovascular disease (Primary Prevention of Cardiovascular Diseases with a Mediterranean Diet, PREDIMED) and the largest first known multisite prospective cohort study on culinary medicine and preventive cardiovascular disease (Cooking for Health Optimization with Patients, CHOP). ICD-9 and ICD-10 codes and billing data extracted from Casemix were utilized to obtain the admission date, discharge date, and medical record number. Inclusion criteria involved a documented readmission for diagnosis related to heart failure within thirty days of discharge. Any patient with multiple readmissions within a thirty-day window had etiologies considered separately. Causes of readmission were coded as dietary noncompliance (failure to restrict sodium or fluid intake), medication noncompliance (willful or inadvertent), comorbidity (pulmonary/renal disease), iatrogenic (insufficient dose/medication, exacerbation by medication for comorbidity), HF exacerbation, recreational drug use. The Mediterranean diet is high in fiber and healthy unsaturated fats, and low in sodium,28 thus adherence to the Mediterranean diet improves satiety and electrolyte balance, respectively. Improved post-meal satiety may in turn help to balance liquid intake, which is of particular relevance for individuals with congestive HF.
Verification of data collection was performed on 5% of all entries using a random number generator. Verification was performed blinded to initial observers and then statistical analysis of interobserver agreement was performed to assess validity. In addition, all readmissions deemed to have equivocal etiologic coding were reassessed by two additional independent observers and recoded. All readmissions deemed nonrepresentative of HF exacerbations were removed from analysis, while all entries that had previously not been included that actually did represent HF exacerbation were included in analysis.
Health Meets Food (HmF) Curriculum
The HmF curriculum, the curriculum intervention studied in CHOP, provides hands-on learning for medical students through culinary medicine classes via seminars, electives, and continuing medical education modules. The fundamental curriculum is a 32-hour nutrition and culinary course delivered through a sequence of eight modules, with each module session spanning 4 hours in length. All 32 hours instruct participants on evidence-based principles of the Mediterranean diet, through both case-based team learning and hands-on cooking, as well as validated approaches for patient nutrition counseling. The programming translates Mediterranean diet principals for the American kitchen making the diet both more relevant and accessible to participants. Each professional health care module involves an online 60-minute didactic program designed to introduce students to concepts of the Mediterranean diet. Individuals participate in an in-kitchen component involving 1.5 hours of team-based case studies and nutrition discussion along with 1.5 hours of hands-on cooking. The cooking component is intended to demonstrate the clinical and pathophysiologic concepts from the didactic phase, in a functional manner. Each module concludes with participants engaging in completion and discussion of clinical case studies, while consuming and sharing their prepared recipes. The HmF curriculum is of particular relevance in HF readmissions, due to the curriculum’s focus on the Mediterranean diet and its role in helping prevent obesity, type II diabetes, and hypertension, 3 primary risk factors for HF. While HmF classes are free for community members, the administrative and overhead costs associated with running each HmF class equate to on average $18.75 per-person.
Statistics
In traditional statistical analysis, continuous data were expressed as means and standard deviations, while percentages were utilized to present categorical data. Student’s t test was used in bivariate analysis to assess differences between age, gender, 30-day readmissions, readmission episodes, length of stay days, and gross charge between readmissions due to dietary noncompliance and readmissions due to all other causes.
Machine learning was utilized in 2 phases. In the first phase, the traditional statistical method of fixed effects panel analysis was used to calculate the increased Mediterranean diet adherence from the CHOP RCT (https://clinicaltrials.gov/ct2/show/NCT03443635; unique identifier: NCT03443635),29 with the results then compared by accuracy and root mean squared error (RMSE) to machine learning-based backward propagation neural networks. Data from the CHOP-Family RCT, specifically, was chosen for its external validity as its lower income patients were from comparable sociodemographic and hospital utilization groups as those hospitalized subjects in this study; this RCT was also used given its internal validity as the first known Bayesian adaptive randomized trial on culinary medicine as a nested RCT within CHOP for families. Grocery store receipts served as documented objective evidence of Mediterranean diet adherence for Goldring Center for Culinary Medicine–treated subjects compared with standard of care subjects (those receiving standard medical visits without additional hands-on cooking and nutrition education). An in-depth description and details of the machine learning methodology has been previously described and published elsewhere.29 In the second phase, the machine learning algorithm of random forest (RF) imputation was utilized for missing values in this study, given its superiority producing more unbiased, efficient, and narrow confidence interval results compared with the leading imputation method of multivariate imputation by chained equations (MICE).30 Compared with the traditional statistical method of MICE, RF has the additional advantage of handling interactions and nonlinearities, while not requiring the correct specification of the data distribution to produce valid results. RF was thus utilized with values close to zero for the normalized RMSE. Thus, training of individual patients was used in the machine learning simulation.
The multiplication rule in statistical independence theory was then used to multiply the increased probability of Mediterranean diet (30%) adherence from the CHOP-Family RCT and the decreased probability (30%) of myocardial infarction, stroke, and cardiovascular-related mortality from the PREDIMED trial.31 The value for predicted increases in adherence to the Mediterranean diet was chosen from previously published data regarding the association between HmF curriculum, the intervention studied in CHOP, and Mediterranean diet adherence.29 This study observed a 40% increase in Mediterranean diet adherence among those receiving HmF curricula, compared to individuals receiving traditional nutritional education; therefore we chose a conservative estimate of a predicted 30% increase in Mediterranean diet adherence for our machine learning model (traditional statistical and machine learning model both accuracy 89.35% and RMSE 0.31).The previous PREDIMED trial conducted by Estruch et al31 demonstrated a 30% reduction in a composite primary cardiovascular disease endpoint of myocardial infarction, stroke, and cardiovascular-related mortality among those randomized to a Mediterranean diet with extra virgin olive oil, compared with a control group receiving dietary advice to reduce consumption of saturated fat. Myocardial infarction and stroke relate to HF readmissions given that (1) myocardial infarction remains the most common cause of HF worldwide32 and (2) cerebrovascular disease is one of the most common noncardiac predictors of short-term HF readmissions.9 Analyses were achieved using a combination of STATA version 14.2 for statistical analysis as well as R package 3.1.1 for machine learning analysis.
Results
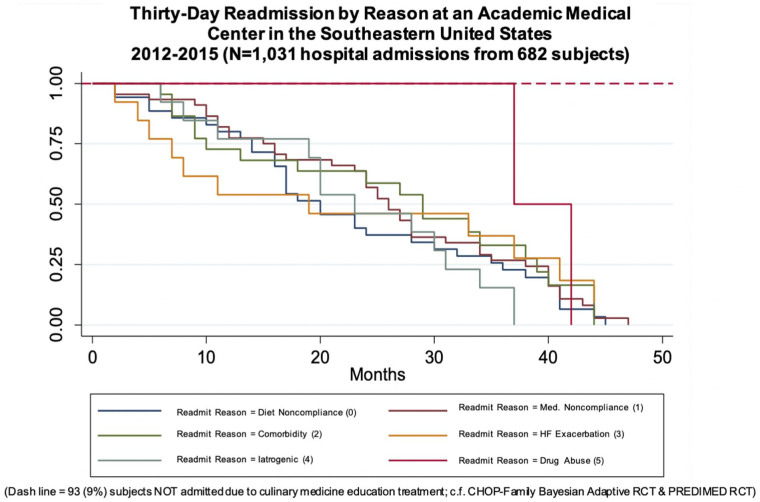
Characteristics of the 1031 admissions included in the study are presented in Table 1. The study cohort was composed of 37.59% females with a mean age of 64.33 ± 14.02 years. The overall readmission rate was 50.78% from January 2012 to October 2015, with approximately one-quarter of readmissions occurring within 30 days. The overall proportion of 30-day readmissions was 130 out of 1031 admissions, representing 12.42% of the sample. Among these 130 admissions, a total of 7 etiologies were identified with 13 admissions (2.5%) coded as having multiple etiologies for their readmission. Specific etiology rates for readmission included, medication noncompliance, 34.62%, dietary noncompliance, 16.92%, comorbidity, 16.92%, HF exacerbation, 10%, iatrogenic 10.0%, as well as drug use 1.54% (Table 1, Figure 1). Internal validity of 5% of entire database was performed with 51 medical records checked against prior database entries. Of those, 49 were in agreement with previous entries, while 1 record was not available, and 1 record showed a discrepancy between the discharge diagnosis and the database entry with other data points remaining accurate. Kappa statistic was calculated for interobserver agreement and was found to be 0.96.
Table 1.
Descriptive Statistics for Sample and Bivariable Analysis Based on Heart Failure (HF) Readmission Reason From 2012 to 2015.
| Variables | Sample (N = 1031) | Other Reason; n1 = 95 (73.08%) | Dietary noncompliant; n2 = 35 (26.92%) | P |
|---|---|---|---|---|
| Age, years, mean (SD) | 64.33 (14.02) | 64.32 (12.67) | 64.85 (13.26) | .853 |
| Female, n (%) | 371 (35.98) | 29 (37.66) | 10 (38.46) | .942 |
| 30-day readmission, n (%) | 130 (12.61) | 88 (92.63) | 34 (97.14) | .682 |
| Readmitted, n (%)a | 518 (50.24) | 88 (72.73) | 33 (27.27) | NA |
| Readmission episodes, median (range) | 1 (0, 2) | 3 (2, 5) | 4 (2, 6) | .130 |
| Readmission reason, n (%) | ||||
| Dietary noncompliance | 22 (16.92) | |||
| Medication noncompliance | 45 (34.62) | |||
| Dietary and medication noncompliance | 13 (10.00) | |||
| Comorbidity | 22 (16.92) | |||
| HF exacerbation | 13 (10.00) | |||
| Iatrogenic | 13 (10.00) | |||
| Drug Abuse | 2 (1.54) | |||
| Length of stays, days, median (range) | 2 (1, 4) | 3 (2, 6) | 2 (1, 4) | 0.112 |
| Gross charge, $, median (range) | 29 296 (19 603-47 462) | 34 294 (20 879-66 162) | 22 837 (18 164-38 598) | 0.036 |
| Gross charge, $, by readmission, total | ||||
| Dietary noncompliance | 890 344 | |||
| Medication noncompliance | 1 802 096 | |||
| Comorbidity | 866 439 | |||
| HF exacerbation | 1 059 117 | |||
| Iatrogenic | 780 157 | |||
| Drug abuse | 68 503 | |||
Row percentage.
Figure 1.
Graphical analysis of underlying etiology of a 30-day readmission for heart failure (HF) as the primary diagnosis at an academic medical center in the Southeastern United States for the 2012-2015 time period.
Bivariable analysis of 30-day readmission etiologies demonstrated that dietary noncompliance was implicated in 26.42% of HF 30-day readmissions. There were no significant differences between dietary noncompliance and all other causes of HF readmissions for age, sex, 30-day readmission number, or readmission episodes.
The median length of admission stay for the entire sample was 2 days. There were no significant differences between median length of stay for dietary noncompliance HF readmissions compared to other causes of HF readmission (P = .112). Medication noncompliance contributed to the highest gross charge by readmission, costing a total of $1 802 096. Gross hospital cost due to dietary noncompliance–attributed HF readmission ($22 837) was significantly lower than gross hospital cost due to all other causes of HF readmission ($34 294). Figure 2 demonstrates the clinical and cost savings of HF readmissions with GCCM based on RCT-guided machine learning analysis. Based on this model, providing HF patients with culinary medicine education would prevent 93 hospital admissions, 12 HF 30-day readmissions, and save $3 903 706.40 over a 3.8-year period for a 235-bed hospital.
Figure 2.
Clinical and cost savings of HF hospitalizations associated with culinary medicine education developed through randomized controlled trial–backed machine learning analysis.
Abbreviations: CHOP, Cooking for Health Optimization with Patients; HF, heart failure; Med., medication; PREDIMED, Primary Prevention of Cardiovascular Diseases with a Mediterranean Diet; RCT, randomized controlled trial.
Discussion
An aging population and improved therapies for cardiac patients have led to a higher prevalence of HF in the United States.2 Although progress has been made, HF mortality remains high and reducing 30-day readmission rates continues to be a national priority.33 We found that our academic medical center, located in downtown New Orleans, had a 12.61% 30-day readmission rate for HF, performing approximately 10 percentage points better than the national average.34 Our 30-day readmission rate was lower compared with other hospitals in the greater New Orleans area and also lower than overall 30-day readmission rate for state of Louisiana,35 in which 23.4% of HF patients have been noted to return to the hospital within 30 days.36 Additionally, we discovered that dietary noncompliance was to be implicated in up to one-fourth of all 30-day HF readmissions, and that culinary medicine education for HF patients may prevent over 12 HF readmissions and save the health care system nearly $4 million over a 4-year period. In aggregate, these results underline the need to develop robust and standardized diet–based therapies for the secondary prevention of HF in order to reduce patient morbidity and to improve cost-effectiveness in HF treatment.
Etiologies for HF 30-day readmission rates at our academic medical center are multifactorial. Medication noncompliance, dietary noncompliance, and HF exacerbation represented over three-fourths of readmissions in the current study. Though our study did not differentiate between cardiac and non-cardiac comorbidities, we found that HF comorbidities were implicated in almost one fifth of HF readmissions. Given this broad definition of comorbidity, it may thus be difficult to compare our comorbidity etiology to other studies which have surprisingly found that non-cardiac comorbidities play a larger role than cardiac pathology with regard to predicting short-term HF readmissions.9 Focusing solely on other similar analyses for 30-day readmissions for HF, our data are somewhat different from cited observations that HF and other cardiovascular-associated conditions are the leading causes of readmission37-39 That being said, it is likely that medication noncompliance, our leading readmission etiology, may have led to HF and cardiovascular exacerbations among individuals in our study. Therefore, discordance between our study and these studies may be more due to differences in coding or classification rather than actual unique differences in disease pathophysiology. A consistent body of literature as well as current HF guidelines suggest that medications, in particularly angiotensin-converting enzyme inhibitors and beta-blockers, reduce HF mortality and therefore should be prescribed to HF patients.12,13,40,41 Despite this fact, poor adherence to medication has been a tremendous problem among patients with HF, a problem that may be due to the amount of medication, regimen stability, and the number of daily doses associated with HF.42,43 While medication noncompliance must continue to be addressed through interventions such as disease education, medication education, telemonitoring, and improved provider skills training, lifestyle factors cannot be overlooked in the setting of HF management.
Most studies on HF and noncompliance focus on medication, rather than diet, as a means to manage disease. Our analysis indicated that nearly one quarter of all HF readmissions at an academic medical center in the Southeastern United States were due to dietary factors, as defined by failure to restrict dietary sodium. Previous studies have largely failed to report the role of diet in HF readmissions, though some have documented fluid and electrolyte imbalances as discrete entities for causes of HF readmissions.39 Given the chronic exposure and access to high-sodium foods among individuals living in United States,11,44 especially in the Southeastern region of the country,45 we believe that dietary exposures may be key drivers of fluid and electrolyte imbalances causing HF readmissions. Salt restriction, although controversial, is recommended as a lifestyle modification in the management of HF.41,46 Yet according to the American College of Cardiology (ACC) and American Heart Association (AHA) guidelines, there are insufficient data to recommend any specific level of sodium intake in patients.41 While the optimum sodium intake for HF patients is therefore not currently known, upper limits have been proposed. The ACC/AHA HF guidelines endorse restricting sodium intake to 2000 to 3000 mg per day.41 Contrastingly, the AHA Presidential Advisory Panel cited limiting sodium to less than 1500 mg per day.47 On the whole, the lack of data and also incongruences in clinical guidelines highlight the need to further study the effect of dietary sodium restriction in the setting of HF.
While there is ample evidence for the utilization of nutrition in the prevention and management, relatively few studies have explored cost savings associated with nutrition interventions for HF readmissions. Cost savings with regard to broader interventions, have yielded conflicting results. Results from a meta-analysis including 25 studies demonstrated that although multicomponent HF quality improvement interventions significantly reduced the hospital readmission rate by over 10%, these interventions yielded a nonsignificant mean net savings of approximately $1000 per patient.48 On the other hand, transitional care services that incorporate dietary counseling for HF patients have been shown to be effective in reducing HF readmissions and costs. For example, data suggest that nurse care management, nurse care home visits, and telemonitoring, all approaches that incorporate nutritional counseling, have net savings of $3435, $3810, and $12 570, respectively.49 But these studies and approaches have yet to isolate diet from other components of their respective interventions, thereby making it difficult to characterize the role of nutrition in HF cost savings. We further build on these findings, predicting that hands-on, kitchen-based culinary medicine education would prevent nearly 100 overall HF readmissions saving almost $4 million or just under $4000 per HF readmission over the course of 4 years. Our predicted nutrition education cost savings are comparable to nurse-oriented transitional care services but lower than telemonitoring services.49 However, we believe that a kitchen-based nutrition education intervention may continue have a lasting impact after the intervention period. Individuals participating in such programs are taught tangible cooking skills and knowledge that can be used in the future, unlike traditional transient HF readmission reduction intervention programs. Future prospective studies involving hands-on culinary medicine curricula are undoubtedly required to further characterize the relationship of culinary medicine education with HF readmissions and associated costs.
Given the fact that HF has many interrelated comorbidities and a patient population likely to be on multiple medications with changing regimens, it may be difficult to elucidate a single underlying cause of HF exacerbations. Nonetheless, it is important that we continue to delineate the different etiologies contributing to 30-day readmission rates for HF to improve health care quality and reduce costs. Though pharmacological treatment will always be a cornerstone of disease management, we believe that incorporating specific diet-based interventions for HF can be beneficial, especially for vulnerable populations in the Southeastern United States, including New Orleans, Louisiana. Creating specific dietary protocols to help manage HF patients will require both translational and quality improvement research. In order to achieve this goal, we must first determine the optimal dietary guidelines for HF patients through consistent observational and RCT evidence.
This study had several important strengths. We assessed the causes of 30-day HF readmissions in a racially diverse cohort in the Southeastern United States, a region disproportionately burdened by cardiovascular disease, specifically HF. Likewise, to our knowledge, this is one of the first studies to characterize the role of culinary medicine in the prevention of HF readmissions and associated HF cost savings. However, our study is not without limitations. HF readmission analysis and coding were user-dependent and may have thus been susceptible to information bias. To help alleviate this limitation, we performed data verification on 5% of our sample to assess the validity of HF readmission classification criteria. Additionally, though our study sample was diverse, our study sample was relatively small, and analyses were performed at a single institution, which may limit the external validity of findings. We hope to further expand on the findings from our study in future analyses, conducting readmission and cost analysis among other academic medical institutions whom also license and provide HmF education to their patients and broader communities.
Conclusion
In conclusion, we have observed that dietary noncompliance is implicated in just over one-fourth of all HF readmissions at an academic medical center in the Southeastern United States. Likewise, we estimated that hands-on teaching kitchen-based nutrition education may occupy a critical role in preventing HF readmissions and improving cost efficacy in HF care, as culinary medicine education was predicted to reduce nearly 100 hospital admissions and save approximately $4000 per patient over a 4-year period among individuals with HF. Future replication and longitudinal studies are required to further understand the role of diet and culinary medicine education in HF readmissions and cost-effective HF care. This knowledge will enable us to then incorporate specific dietary guidelines in all HF treatment protocols to reduce 30-day readmission rates, improve quality of patient care, and decrease health care expenditures at the state and federal levels.
Acknowledgments
The authors would like to thank all Tulane medical students and faculty for their contributions to the project and in data collection. ACR, DJM, AS, LS, ES, AD, and TSH have abided by the publication and authorship rules of the American Journal of Lifestyle Medicine. ACR, DJM, AS and TSH discussed the framework and outline of the study and manuscript. ACR, DJM, and TSH wrote and revised the manuscript. ACR, TSH, DJM, AS, LS, AD, ES, made substantial contributions to the interpretation of data, as well as edited and approved the submitted version. All individuals named in the Acknowledgments section have provided consent to be named in the article.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Culinary Medicine programming was supported in part by the Goldring Family Foundation, The Woldenberg Family Foundation, the Humana Foundation and the Robert Wood Johnson Foundation. ACR is currently supported through a predoctoral institutional training grant funded by the National Institute of Health under grant number 5TL1TR001418.
Ethical Approval: Ethics approval was obtained through the local (Tulane) and site-specific Institutional Review Boards for this research. Name of Institution Providing Institutional Review Board Review: The Administrators of the Tulane Educational Fund. IRB Registration #: 00000324. FWA#: 0000205. IRB Reference #:729959.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Cooking for Health Optimization with Patients (CHOP)-Family Bayesian adapted randomized controlled trial (https://clinicaltrials.gov/ct2/show/NCT03443635; unique identifier: 03443635),
ORCID iD: Alexander C. Razavi  https://orcid.org/0000-0002-3213-0876
https://orcid.org/0000-0002-3213-0876
References
- 1. Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933-944. doi: 10.1161/CIR.0b013e31820a55f5 [DOI] [PubMed] [Google Scholar]
- 2. Vigen R, Maddox TM, Allen LA. Aging of the united states population: impact on heart failure. Curr Heart Fail Rep. 2012;9:369-374. doi: 10.1007/s11897-012-0114-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224-2260. doi: 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ziaeian B, Fonarow GC. The prevention of hospital readmissions in heart failure. Prog Cardiovasc Dis. 2016;58:379-385. doi: 10.1016/j.pcad.2015.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bergethon KE, Ju C, DeVore AD, et al. Trends in 30-day readmission rates for patients hospitalized with heart failure: findings from the get with the Guidelines-Heart Failure Registry. Circ Heart Fail. 2016;9:e002594. doi: 10.1161/CIRCHEARTFAILURE.115.002594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Suter LG, Li SX, Grady JN, et al. National patterns of risk-standardized mortality and readmission after hospitalization for acute myocardial infarction, heart failure, and pneumonia: update on publicly reported outcomes measures based on the 2013 release. J Gen Intern Med. 2014;29:1333-1340. doi: 10.1007/s11606-014-2862-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Arora S, Patel P, Lahewala S, et al. Etiologies, trends, and predictors of 30-day readmission in patients with heart failure. Am J Cardiol. 2017;119:760-769. doi: 10.1016/j.amjcard.2016.11.022 [DOI] [PubMed] [Google Scholar]
- 8. Vader JM, LaRue SJ, Stevens SR, et al. Timing and causes of readmission after acute heart failure hospitalization—insights from the Heart Failure Network Trials. J Card Fail. 2016;22:875-883. doi: 10.1016/j.cardfail.2016.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Saito M, Negishi K, Marwick TH. Meta-analysis of risks for short-term readmission in patients with heart failure. Am J Cardiol. 2016;117:626-632. doi: 10.1016/j.amjcard.2015.11.048 [DOI] [PubMed] [Google Scholar]
- 10. Sotos-Prieto M, Bhupathiraju SN, Mattei J, et al. Changes in diet quality scores and risk of cardiovascular disease among US men and women. Circulation. 2015;132:2212-2219. doi: 10.1161/CIRCULATIONAHA.115.017158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation. 2016;133:187-225. doi: 10.1161/CIRCULATIONAHA.115.018585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. N Engl J Med. 1996;334:1349-1355. doi: 10.1056/NEJM199605233342101 [DOI] [PubMed] [Google Scholar]
- 13. Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007;297:61-70. doi: 10.1001/jama.297.1.61 [DOI] [PubMed] [Google Scholar]
- 14. Krumholz HM, Amatruda J, Smith GL, et al. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J Am Coll Cardiol. 2002;39:83-89. doi: 10.1016/S0735-1097(01)01699-0 [DOI] [PubMed] [Google Scholar]
- 15. Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333:1190-1195. doi: 10.1056/NEJM199511023331806 [DOI] [PubMed] [Google Scholar]
- 16. Hummel SL, Karmally W, Gillespie BW, et al. Home-delivered meals postdischarge from heart failure hospitalization. Circ Heart Fail. 2018;11:e004886. doi: 10.1161/CIRCHEARTFAILURE.117.004886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Levitan EB, Wolk A, Mittleman MA. Consistency with the DASH diet and incidence of heart failure. Arch Intern Med. 2009;169:851-857. doi: 10.1001/archinternmed.2009.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fitó M, Estruch R, Salas-Salvadó J, et al. Effect of the Mediterranean diet on heart failure biomarkers: a randomized sample from the PREDIMED trial. Eur J Heart Fail. 2014;16:543-550. doi: 10.1002/ejhf.61 [DOI] [PubMed] [Google Scholar]
- 19. Kerley CP. A review of plant-based diets to prevent and treat heart failure. Card Fail Rev. 2018;4:54-61. doi: 10.15420/cfr.2018:1:1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mujib M, Zhang Y, Feller MA, Ahmed A. Evidence of a “heart failure belt” in the southeastern United States. Am J Cardiol. 2011;107:935-937. doi: 10.1016/j.amjcard.2010.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liu L, Yin X, Chen M, Jia H, Eisen HJ, Hofman A. Geographic variation in heart failure mortality and its association with hypertension, diabetes, and behavioral-related risk factors in 1723 counties of the United States. Front Public Health. 2018;6:132. doi: 10.3389/fpubh.2018.00132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Global Burden of Cardiovascular Diseases Collaboration; Roth GA, Johnson CO, et al. The burden of cardiovascular diseases among US States, 1990-2016. JAMA Cardiol. 2018;3:375-389. doi: 10.1001/jamacardio.2018.0385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hummel SL, Seymour EM, Brook RD, et al. Low-sodium DASH diet improves diastolic function and ventricular-arterial coupling in hypertensive heart failure with preserved ejection fraction. Circ Heart Fail. 2013;6:1165-1171. doi: 10.1161/CIRCHEARTFAILURE.113.000481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kastorini C-M, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB. The effect of Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534 906 individuals. J Am Coll Cardiol. 2011;57:1299-1313. doi: 10.1016/j.jacc.2010.09.073 [DOI] [PubMed] [Google Scholar]
- 25. Krittanawong C, Zhang H, Wang Z, Aydar M, Kitai T. Artificial intelligence in precision cardiovascular medicine. J Am Coll Cardiol. 2017;69:2657-2664. doi: 10.1016/J.JACC.2017.03.571 [DOI] [PubMed] [Google Scholar]
- 26. Mortazavi BJ, Downing NS, Bucholz EM, et al. Analysis of machine learning techniques for heart failure readmissions. Circ Cardiovasc Qual Outcomes. 2016;9:629-640. doi: 10.1161/CIRCOUTCOMES.116.003039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Golas SB, Shibahara T, Agboola S, et al. A machine learning model to predict the risk of 30-day readmissions in patients with heart failure: a retrospective analysis of electronic medical records data. BMC Med Inform Decis Mak. 2018;18:44. doi: 10.1186/s12911-018-0620-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Widmer RJ, Flammer AJ, Lerman LO, Lerman A. The Mediterranean diet, its components, and cardiovascular disease. Am J Med. 2015;128:229-238. doi: 10.1016/j.amjmed.2014.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Monlezun DJ, Dart L, Vanbeber A, et al. Machine Learning-Augmented Propensity Score-adjusted multilevel mixed effects panel analysis of hands-on cooking and nutrition education versus traditional curriculum for medical students as preventive cardiology: multisite cohort study of 3248 trainees. Biomed Res Int. 2018;2018:5051289. doi: 10.1155/2018/5051289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shah AD, Bartlett JW, Carpenter J, Nicholas O, Hemingway H. Comparison of random forest and parametric imputation models for imputing missing data using MICE: a CALIBER study. Am J Epidemiol. 2014;179:764-774. doi: 10.1093/aje/kwt312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279-1290. doi: 10.1056/NEJMoa1200303 [DOI] [PubMed] [Google Scholar]
- 32. Cahill TJ, Kharbanda RK. Heart failure after myocardial infarction in the era of primary percutaneous coronary intervention: mechanisms, incidence and identification of patients at risk. World J Cardiol. 2017;9:407-415. doi: 10.4330/wjc.v9.i5.407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606-619. doi: 10.1161/HHF.0b013e318291329a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ross JS, Chen J, Lin Z, et al. Recent national trends in readmission rates after heart failure hospitalization. Circ Heart Fail. 2010;3:97-103. doi: 10.1161/CIRCHEARTFAILURE.109.885210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Burtch J. Telephonic Transitional Care Intervention to Reduce 30-Day Hospital Readmission Rates in Adults with Heart Failure [dissertation]. Lafayette: University of Louisiana at Lafayette; 2016. https://pqdtopen.proquest.com/doc/1844996228.html?FMT=ABS. Accessed May 12, 2019. [Google Scholar]
- 36. Casey M, Hung P, Evenson A, Distel E, Moscovice I. Hospital compare CAH quality measure results, Q2 2013-2014. http://www.flexmonitoring.org/wp-content/uploads/2015/04/Louisiana.pdf. Accessed May 12, 2019.
- 37. Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355-363. doi: 10.1001/jama.2012.216476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ranasinghe I, Wang Y, Dharmarajan K, Hsieh AF, Bernheim SM, Krumholz HM. Readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia among young and middle-aged adults: a retrospective observational cohort study. PLoS Med. 2014;11:e1001737. doi: 10.1371/journal.pmed.1001737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Davis JD, Olsen MA, Bommarito K, et al. All-payer analysis of heart failure hospitalization 30-day readmission: comorbidities matter. Am J Med. 2017;130:93.e9-93.e28. doi: 10.1016/j.amjmed.2016.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200. doi: 10.1093/eurheartj/ehw128 [DOI] [PubMed] [Google Scholar]
- 41. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:1810-1852. doi: 10.1161/CIR.0b013e31829e8807 [DOI] [PubMed] [Google Scholar]
- 42. van der Wal MHL, Jaarsma T, van Veldhuisen DJ. Non-compliance in patients with heart failure; how can we manage it? Eur J Heart Fail. 2005;7:5-17. doi: 10.1016/j.ejheart.2004.04.007 [DOI] [PubMed] [Google Scholar]
- 43. Ruppar TM, Cooper PS, Mehr DR, Delgado JM, Dunbar-Jacob JM. Medication adherence interventions improve heart failure mortality and readmission rates: systematic review and meta-analysis of controlled trials. J Am Heart Assoc. 2016;5:e002606. doi: 10.1161/JAHA.115.002606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obes Rev. 2013;14(suppl 2):21-28. doi: 10.1111/obr.12107 [DOI] [PubMed] [Google Scholar]
- 45. Howard G, Cushman M, Moy CS, et al. Association of clinical and social factors with excess hypertension risk in black compared with white US adults. JAMA. 2018;320:1338-1348. doi: 10.1001/jama.2018.13467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Philipson H, Ekman I, Forslund HB, Swedberg K, Schaufelberger M. Salt and fluid restriction is effective in patients with chronic heart failure. Eur J Heart Fail. 2013;15:1304-1310. doi: 10.1093/eurjhf/hft097 [DOI] [PubMed] [Google Scholar]
- 47. Antman EM, Appel LJ, Balentine D, et al. Stakeholder discussion to reduce population-wide sodium intake and decrease sodium in the food supply: a conference report from the American Heart Association Sodium Conference 2013 Planning Group. Circulation 2014;129:e660-e679. doi: 10.1161/CIR.0000000000000051 [DOI] [PubMed] [Google Scholar]
- 48. Nuckols TK, Keeler E, Morton S, et al. Economic evaluation of quality improvement interventions designed to prevent hospital readmission: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:975-985. doi: 10.1001/jamainternmed.2017.1136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Van Spall HGC, Rahman T, Mytton O, et al. Comparative effectiveness of transitional care services in patients discharged from the hospital with heart failure: a systematic review and network meta-analysis. Eur J Heart Fail. 2017;19:1427-1443. doi: 10.1002/ejhf.765 [DOI] [PubMed] [Google Scholar]