Abstract
Background: Death certificates are considered the most reliable source of information to compare cause-specific mortality across countries. The aim of the present study was to examine death certificates of persons who tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) to (a) quantify the number of deaths directly caused by coronavirus 2019 (COVID-19); (b) estimate the most common complications leading to death; and (c) identify the most common comorbidities. Methods: Death certificates of persons who tested positive for SARS-CoV-2 provided to the National Surveillance system were coded according to the 10th edition of the International Classification of Diseases. Deaths due to COVID-19 were defined as those in which COVID-19 was the underlying cause of death. Complications were defined as those conditions reported as originating from COVID-19, and comorbidities were conditions independent of COVID-19. Results: A total of 5311 death certificates of persons dying in March through May 2020 were analysed (16.7% of total deaths). COVID-19 was the underlying cause of death in 88% of cases. Pneumonia and respiratory failure were the most common complications, being identified in 78% and 54% of certificates, respectively. Other complications, including shock, respiratory distress and pulmonary oedema, and heart complications demonstrated a low prevalence, but they were more commonly observed in the 30–59 years age group. Comorbidities were reported in 72% of certificates, with little variation by age and gender. The most common comorbidities were hypertensive heart disease, diabetes, ischaemic heart disease, and neoplasms. Neoplasms and obesity were the main comorbidities among younger people. Discussion: In most persons dying after testing positive for SARS-CoV-2, COVID-19 was the cause directly leading to death. In a large proportion of death certificates, no comorbidities were reported, suggesting that this condition can be fatal in healthy persons. Respiratory complications were common, but non-respiratory complications were also observed.
Keywords: death certificates, COVID-19, comorbidities
1. Introduction
Italy was the first country in Europe to be affected by the coronavirus 2019 (COVID-19) pandemic. The first confirmed case was reported at the end of January 2020, and a case-based surveillance system was established on 27 February 2020 [1]. The system collects data regarding all laboratory-confirmed cases of COVID-19, as well as deaths associated with COVID-19, which are defined as deaths in patients confirmed to have tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). At the beginning of the pandemic, the lethality of COVID-19 in Italy was estimated to be greater than that in other countries, partly because of methods used to estimate and define deaths related to COVID-19 [2]. In Italy, all deaths in patients who tested positive for SARS-CoV-2 are counted as COVID-19–related by a national surveillance system. However, because different causes of death can occur in SARS-CoV-2–positive patients, this approach can lead to an overestimate of COVID-19-related deaths.
In patients infected by SARS-CoV-2, death can occur as the consequence of various complications, including pneumonia, acute respiratory distress syndrome, shock, and heart disease. In addition, the presence of comorbidities, and hypertension, diabetes, cardiovascular diseases, and chronic respiratory conditions in particular, can increase vulnerability to the development of these complications [3,4]. Death certificates are considered the most reliable source of information to compare cause-specific mortality across countries. However, limited data are available on the complications and comorbidities reported on death certificates of patients who presented with COVID-19. Some analyses of conditions existing prior to contracting COVID-19 were conducted by the UK Office of National Statistic [5].
The aim of the present study was to examine death certificates of persons who tested positive for SARS-CoV-2 to (a) quantify the number of deaths directly caused by COVID-19; (b) estimate the most common complications leading to death; and (c) assess the most common comorbidities.
2. Experimental Section
The surveillance system managed by the Italian National Institute of Health (Istituto Superiore di Sanità—ISS) collects information on all SARS-CoV-2-positive individuals throughout the country [1,2]. Data on all positive cases were obtained from all Italian regions and autonomous provinces. All deaths of patients who tested positive for SARS-CoV-2 through reverse transcription polymerase chain reaction amplification, independently from pre-existing diseases that may have caused or contributed to death, were tracked by the surveillance system.
Regions and autonomous provinces were also asked to supply copies of ISS death certificates of patients who died after testing positive for SARS-CoV-2. A joint group of researchers from the ISS and Italian National Institute of Statistics (Istat) was established to analyse these certificates.
Causes of death were classified according to provisions of the tenth edition of the International Classification of Diseases (ICD-10) [6] and the most recent guidelines issued by World Health Organisation on COVID-19–related deaths [7]. Iris software updated for COVID-19 (version 5.7 www.iris-institute.org) was used for cause-of-death coding. Approximately 80% of the death certificates were automatically coded by the software; the remaining certificates were coded by study researchers.
Death certificates completed by physicians comprise two parts. Part 1 contains the events leading to death, including the underlying cause (UC) that initiated the chain of events leading to death and the causal sequence of conditions caused by it. Part 2 includes other relevant conditions contributing to death but not part of the sequence reported in Part 1. According to ICD-10 coding procedures, a death due to COVID-19 is defined as a death for which COVID-19 was the UC.
Comorbidities were identified as conditions reported in Part 2 of the certificate or conditions different from COVID-19 that initiated chains of events reported in Part 1. To select comorbidities, a pre-existing validated algorithm developed for the study of multiple causes of death was used [8]. Details on the algorithm are provided in Appendix A. Complications of COVID-19 were identified among conditions reported in the sequence in Part 1 in which COVID-19 was the UC. Conditions that appeared due to COVID-19 more frequently than expected were considered complications of COVID-19. The expected frequency was calculated under the null hypothesis of random distribution of conditions within Part 1. Under the null hypothesis, and denoting P as the joint frequency in Part 1 of a given condition c and COVID-19 on different lines, we would expect that half of P times the condition c reported was due to COVID-19, and half P times the contrary would be the case. A comparison of the observed and expected frequencies was carried out using a chi-square test (further details are provided in Appendix B).
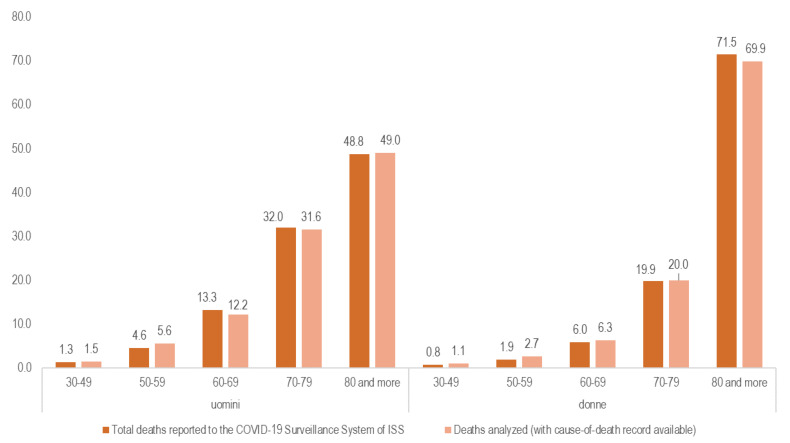
As of 28 May 2020, a total of 31,851 deaths in SARS-CoV-2–positive patients were reported in Italy. The 5311 death certificates received, analysed, and coded represented 16.7% of all deaths. These records were representative of the regional distribution of COVID-19 related deaths (see Appendix C).
Ethical Issues
On 27 February 2020, the Italian Presidency of the Council of Ministers authorised the collection and scientific dissemination of data related to COVID-19 by the ISS and other public health institutions [9].
3. Results
Of the 5311 analysed death certificates, 3298 (62.1%) referred to men, and 2009 (37.8%) to women. Gender was not specified in four certificates. Age at death was specified in 5211 certificates: 305 (5.7%) deaths occurred in the age class 30–59 years, 1940 (36.5%) in the class 60–79 years, and 2966 (55.8%) in those 80 years of age or older. No death occurring in persons younger than 30 years was recorded in the study sample.
3.1. Deaths Due to COVID-19
Table 1 provides the distribution of underlying causes by sex and age in the study group. COVID-19 was the UC in 4691 of 5311 certificates (88.3%), with men representing a slightly higher percentage than women (89.4% versus 86.5%). The lowest proportion of deaths with COVID-19 as the UC was observed in the 30–59 age group (86.2%), and the highest was in the 60–79 age group (90.4%). The most common UCs besides COVID-19 included diseases of the circulatory system (4.4%), neoplasms (2.6%), and diseases of the respiratory system (1.1%); the latter nearly exclusively represented by chronic lower-respiratory conditions. The group aged 30–59 demonstrated the highest proportions of deaths with UCs of neoplasms (6.9%) and diabetes (2.0%), while circulatory system diseases were substantially more frequent in the group aged 80 or older (5.4%).
Table 1.
Underlying causes of death by gender and age group.
| ICD-10 | Underlying Cause of Death | Whole Sample | Gender | Age Group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | 30–59 | 60–79 | 80 and Older | |||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | ||
| U07.1 | COVID-19 | 4691 | 88.3 | 2950 | 89.4 | 1737 | 86.5 | 263 | 86.2 | 1754 | 90.4 | 2590 | 87.3 |
| A00-B99 | Infectious and parasitic diseases | 12 | 0.2 | 7 | 0.2 | 5 | 0.2 | 0 | 0.0 | 4 | 0.2 | 6 | 0.2 |
| C00-D48 | Neoplasms | 137 | 2.6 | 87 | 2.6 | 50 | 2.5 | 21 | 6.9 | 54 | 2.8 | 57 | 1.9 |
| E00-E99 | Endocrine, nutritional and metabolic diseases | 46 | 0.9 | 28 | 0.8 | 18 | 0.9 | 7 | 2.3 | 13 | 0.7 | 25 | 0.8 |
| of which | |||||||||||||
| E10-E14 | Diabetes | 37 | 0.7 | 22 | 0.7 | 15 | 0.7 | 6 | 2.0 | 11 | 0.6 | 19 | 0.6 |
| F01-F03, G30 | Dementia and Alzheimer | 38 | 0.7 | 13 | 0.4 | 25 | 1.2 | 0 | 0.0 | 3 | 0.2 | 35 | 1.2 |
| G00-H99 | Diseases of the nervous system (excluding Alzheimer) | 15 | 0.3 | 12 | 0.4 | 3 | 0.1 | 0 | 0.0 | 8 | 0.4 | 7 | 0.2 |
| I00-I99 | Diseases of the circulatory system | 235 | 4.4 | 131 | 4.0 | 104 | 5.2 | 8 | 2.6 | 61 | 3.1 | 161 | 5.4 |
| of which | |||||||||||||
| I10-I15 | Hypertensive diseases | 40 | 0.8 | 16 | 0.5 | 24 | 1.2 | 1 | 0.3 | 8 | 0.4 | 28 | 0.9 |
| I20-I25 | Ischaemic heart diseases | 87 | 1.6 | 58 | 1.8 | 29 | 1.4 | 1 | 0.3 | 33 | 1.7 | 52 | 1.8 |
| I48 | Atrial fibrillation | 12 | 0.2 | 5 | 0.2 | 7 | 0.3 | 0 | 0.0 | 2 | 0.1 | 10 | 0.3 |
| I60-I69 | Cerebrovascular diseases | 55 | 1.0 | 29 | 0.9 | 26 | 1.3 | 2 | 0.7 | 11 | 0.6 | 41 | 1.4 |
| J00-J99 | Diseases of the respiratory system | 58 | 1.1 | 33 | 1.0 | 25 | 1.2 | 0 | 0.0 | 18 | 0.9 | 39 | 1.3 |
| of which | |||||||||||||
| J40-J47 | Chronic lower-respiratory diseases | 55 | 1.0 | 33 | 1.0 | 22 | 1.1 | 0 | 0.0 | 17 | 0.9 | 37 | 1.2 |
| K00-K99 | Diseases of the digestive system | 36 | 0.7 | 18 | 0.5 | 18 | 0.9 | 2 | 0.7 | 15 | 0.8 | 17 | 0.6 |
| S00-T98 | External causes of death | 26 | 0.5 | 12 | 0.4 | 14 | 0.7 | 1 | 0.3 | 6 | 0.3 | 18 | 0.6 |
| Other causes | 28 | 0.6 | 13 | 0.4 | 15 | 0.7 | 4 | 1.3 | 9 | 0.5 | 15 | 0.5 | |
| Total | 5311 | 100.0 | 3298 | 100.0 | 2009 | 100.0 | 305 | 100.0 | 1940 | 100.0 | 2966 | 100.0 | |
3.2. Comorbidities
No comorbidities besides COVID-19 were reported in 1469 death certificates (27.7%), with no sex differences and only a small variation among age groups (Table 2). In 3842 (72.3%) cases, at least one comorbidity was reported besides COVID-19: 32.0% reported one condition, 26.8% two comorbidities, and 13.6% three or more. The 30–59 age group showed a lower prevalence of deaths with two or more comorbidities and a slightly lower mean number of comorbidities compared with older age groups.
Table 2.
Number of comorbidities by gender and age group.
| Number of Comorbidities Besides COVID-19 | Total | Gender | Age Group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | 30–59 | 60–79 | 80 and More | ||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| None | 1469 | 27.7 | 911 | 27.6 | 554 | 27.6 | 80 | 26.2 | 550 | 28.4 | 819 | 27.6 |
| at least 1 | 3842 | 72.3 | 2387 | 72.4 | 1455 | 72.4 | 225 | 73.8 | 1390 | 71.6 | 2147 | 72.4 |
| of which: | ||||||||||||
| 1 | 1699 | 32.0 | 1059 | 32.1 | 640 | 31.9 | 124 | 40.7 | 621 | 32.0 | 920 | 31.0 |
| 2 | 1422 | 26.8 | 866 | 26.3 | 556 | 27.7 | 66 | 21.6 | 494 | 25.5 | 841 | 28.4 |
| 3 or more | 721 | 13.6 | 462 | 14.0 | 259 | 12.9 | 35 | 11.5 | 275 | 14.2 | 386 | 13.0 |
| Total | 5311 | 100.0 | 3298 | 100.0 | 2009 | 100.0 | 305 | 100.0 | 1940 | 100.0 | 2966 | 100.0 |
| Mean number | 1.3 | 1.3 | 1.3 | 1.2 | 1.3 | 1.3 | ||||||
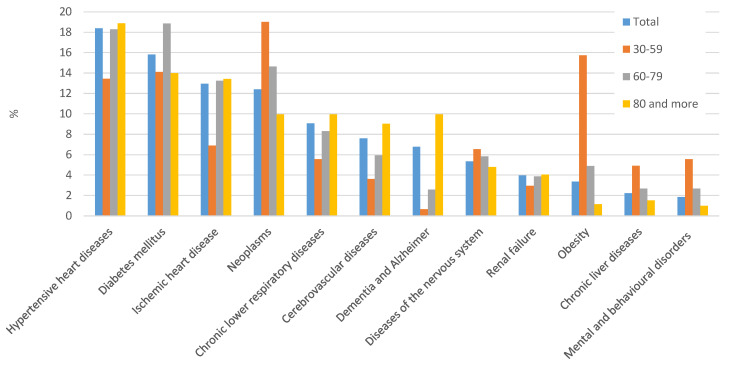
Overall, the most frequently reported comorbidities (Figure 1) were hypertensive heart diseases (18.4% of death certificates), diabetes mellitus (15.8%), ischaemic heart disease (13.0%), and neoplasms (12.4%). Conditions such as chronic lower-respiratory diseases, cerebrovascular diseases, dementia, and Alzheimer’s disease were also frequently reported (between 5% and 10% of cases). Differences by sex were observed only for hypertensive heart diseases, while dementia and Alzheimer’s disease were more frequent in women than in men (20.0% versus 17.5% and 11.3% versus 4.1%, respectively), while ischaemic heart disease was more frequent in men (15.3% versus 9.2%).
Figure 1.
Distribution of the main comorbidities on death certificates, by age group.
Prevalence of most conditions increased with age, with some exceptions. Diabetes demonstrated the highest prevalence in the group aged 60–79 years, while prevalence of neoplasms and obesity decreased with age; these latter conditions were the most common comorbidities in the 30–59 age group, being reported in 19.0% and 15.7%, respectively. The youngest age group also showed the highest prevalence of diseases of the nervous system (6.6%), chronic liver diseases (4.9%), and mental and behavioural disorders (5.6%).
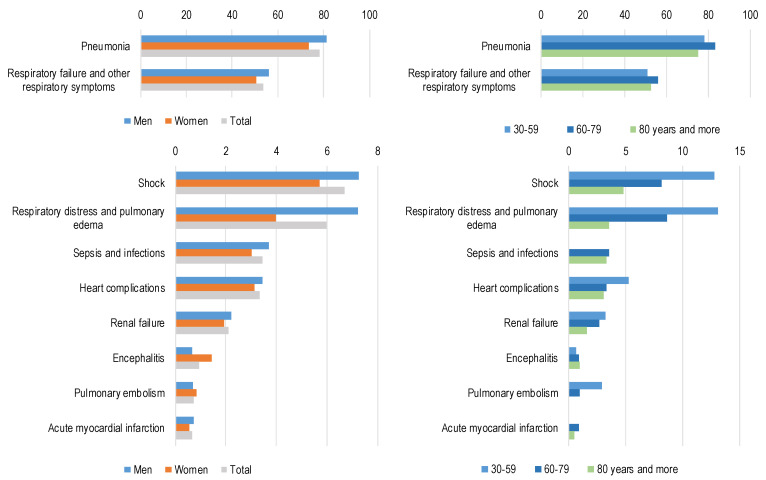
3.3. Complications
Conditions frequently reported as complications of COVID-19 are shown in Figure 2 (all conditions analysed are reported in Appendix B, Table A2). Pneumonia and respiratory failure were the most common complications, being identified in 78% and 54% of certificates, respectively. Complications with an overall prevalence below 8% included shock, respiratory distress and pulmonary oedema, sepsis, heart complications such as heart failure, renal failure, encephalitis, pulmonary embolism, and acute myocardial infarction. For the most frequent conditions (pneumonia and respiratory failure), little variation was observed by sex and age, while some differences by age were observed for the least-frequent conditions. In the 30–59 age group, shock, respiratory distress, pulmonary oedema, and heart complications were more prevalent compared with older age groups.
Figure 2.
Main fatal complications of COVID-19 by gender and age group. Percentage of mention of the condition as complication of COVID-19 on total deaths.
4. Discussion
The present study analysed death certificates, which are widely considered the most reliable source of information to compare cause-specific mortality across countries. Results show that approximately 88% of deaths in SARS-COV2–positive patients were due to COVID-19 and their comorbidities, and cardiovascular conditions, diabetes, and neoplasms in particular, are common in patients dying with COVID-19. Respiratory conditions were the most common complications leading to death, and other non-respiratory complications were observed less frequently.
Consistent with previous studies, more deaths due to COVID-19 were reported for men than women. This finding contrasts with the case distribution documented in the Italian population, which displayed the opposite pattern (case distribution on August 10, 2020: 46.2% men, 53.8% women). Reasons for the higher number of deaths observed in men are not yet known [10].
Comorbidities were common in patients dying with COVID-19, suggesting that death was often the result of the concomitance and interaction of different chronic diseases with SARS-COV-2 infection. In line with other studies, we observed that patients dying with COVID-19 often present with hypertensive heart disease, ischaemic heart disease, cerebrovascular diseases, diabetes mellitus, chronic diseases of the low respiratory tract, or obesity [3,4].
The high prevalence of comorbidities in patients who died after a positive test for SARS-COV-2 led to a debate in the Italian media regarding the main causes of death in COVID-19 patients. In the presence of a high level of comorbidities (i.e., neoplasms, dementia, heart disease), COVID-19 may represent the final event leading to death, but not necessarily the main UC. The analysis of death certificates addressed this issue by showing that the vast majority of deaths occurring in patients who tested positively to SARS-COV2 were due to COVID-19.
The quality of the information reported by the certifying physicians may vary greatly: both under- and overreporting may occur [11] and causes of death are not generally confirmed by autopsies. Despite these limitations, data based on death certificates represent a primary source of epidemiologic information since they cover the overall population and the procedures for selecting and coding causes of death are highly standardized and internationally agreed leading to comparable and reliable figures.
Some relevant differences were evident in the clinical aspects of COVID-19 among younger adults. They suffer from slightly fewer comorbidities compared with older adults and often present with a single severe comorbidity (i.e., neoplasms), but they are more likely to die with non-respiratory complications. This finding suggests that, while in older adults, mortality is closely related to a pre-existing vulnerability due to presence of chronic conditions, COVID-19–related deaths in adults younger than 60 may be due to the development of complications.
Obesity is observed more commonly in younger adults than in older adults. It can increase the severity of respiratory complications by restricting ventilation, impeding diaphragm excursion, and reducing immune responses to viral infection [12]. This condition has been shown to increase the risk of mortality and admission to intensive care units in patients with COVID-19, and this association appears to be stronger in younger adults [13]. This observation confirms the obesity paradox hypothesis for older persons, for whom a higher body mass index is associated with superior outcomes.
5. Conclusions
Comorbidities were observed in a high percentage (72%) of deaths of people who tested positive for SARS-CoV-2. Nevertheless, COVID-19 was the cause directly leading to death in the vast majority (88%) of the cases. Moreover, in a relevant proportion of death certificates (28%), and also in younger people, no comorbidity besides COVID-19 was reported, suggesting that this condition can be fatal in healthy persons. The comorbidities most commonly associated with COVID-19 were hypertensive heart diseases, diabetes, ischaemic heart diseases, and obesity, with this latter condition found in younger people. A high percentage of people (78%) presented with pneumonia, but non-respiratory complications were also observed, particularly in younger age groups. This finding suggests that to reduce COVID-19 case fatality, treatment of respiratory conditions should be combined with appropriate management of comorbidities and strategies to prevent and mitigate the effects of non-respiratory complications.
Acknowledgments
† Group authorship—Italian National Institute of Health COVID-19 Mortality Group: Luigi Palmieri, Xanthi Andrianou, Pierfrancesco Barbariol, Antonino Bella, Stefania Bellino, Eva Benelli, Luigi Bertinato, Stefano Boros, Gianfranco Brambilla, Giovanni Calcagnini, Marco Canevelli, Maria Rita Castrucci, Federica Censi, Alessandra Ciervo, Elisa Colaizzo, Fortunato D’Ancona, Martina Del Manso, Corrado Di Benedetto, Chiara Donfrancesco, Massimo Fabiani, Francesco Facchiano, Antonietta Filia, Marco Floridia, Fabio Galati, Marina Giuliano, Tiziana Grisetti, Yllka Kodra; Martin Langer, Ilaria Lega, Cinzia Lo Noce, Pietro Maiozzi, Fiorella Malchiodi Albedi, Valerio Manno, Margherita Martini, Alberto Mateo Urdiales, Eugenio Mattei, Claudia Meduri, Paola Meli, Giada Minelli, Manuela Nebuloni, Lorenza Nisticò, Marino Nonis, Graziano Onder, Lucia Palmisano, Nicola Petrosillo, Patrizio Pezzotti, Flavia Pricci, Ornella Punzo, Vincenzo Puro, Valeria Raparelli, Giovanni Rezza, Flavia Riccardo, Maria Cristina Rota, Paolo Salerno, Debora Serra, Andrea Siddu, Paola Stefanelli, Manuela Tamburo De Bella, Dorina Tiple, Brigid Unim, Luana Vaianella, Nicola Vanacore, Monica Vichi, Emanuele Rocco Villani, Amerigo Zona, Silvio Brusaferro.
Appendix A
Appendix A.1. Procedure for the Selection of Comorbidities
A programme in the programming language C was developed for the selection of comorbidities. The algorithm aims to identify causes that are at the origin of independent trains of events (also referred to as sequences) reported on the death certificates, and the conditions that contributed to death but are not part of any sequence. If there is a single sequence with no other conditions in the second part, the originating cause is 1 and it corresponds to the underlying cause.
Appendix A.2. Detailed Description
The end goal of the programme is to attribute a role to each ICD code reported on a death certificate. The roles can be:
-
-
“originating cause”—the originating causes of the sequences reported on the death certificate. If there is a single sequence.
-
-
“precipitating condition”—a code that can be considered a complication of another on the death certificate.
-
-
“associated cause”—the independent codes in Part 2.
-
-
“ill-defined codes”—codes at the origin of a sequence or reported as associated causes that are considered ill-defined by the ICD-10.
-
-
“deleted codes”—it is possible that during the process, two or more codes are condensed together in a single code; those codes including others are marked as “deleted”.
Comorbidities are codes flagged by the programme as “originating” or “associated” causes.
For the identification of comorbidities, the program follows the steps described below. In each step, relations between codes are taken into account. The tool used to evaluate of relationships between codes is the Iris Decision Tables, which summarise the provisions of the ICD-10 describing the relationships between the codes to be used. The steps described are similar to the ones performed during the selection of the underlying cause (Iris Institute. Information about the coding rule types for mortality coding with Iris. https://www.dimdi.de/dynamic/.downloads/iris-institute/manuals/information-about-coding-rule-types-for-mortality.pdf (accessed 23 July 2020)).
-
(1)
All codes in Part 1 are initially marked as “originating”, and all codes in Part 2 are marked as “associated cause”.
-
(2)
Check for “due to” relation in Part 1: starting from line a to line f, each code is compared with any other in lower lines, if the first code can be due to the second (according to Iris Decision Tables), the first code will be identified as “precipitating condition”.
-
(3)
Check for obvious causes: if any “originating” code is an obvious consequence (according to Iris Decision Tables) of another code, then the first code is marked as “precipitating” and the second as “originating”.
-
(4)
Check for Ill-defined causes, if an “originating” code is an ill-defined condition (the list of ill-defined codes is provided by ICD-10 and included in Iris Decision Tables), the code will be marked as “ill-defined”.
-
(5)
Check for linkages: if two or more codes are linked together (according to Iris Decision Tables), the first code is marked as “deleted” and the second is preferred (and sometimes modified).
-
(6)
Check for specificity: if one code is considered less specific than another (according to Iris Decision Tables), the first code is marked as “deleted” and the second is preferred (and sometimes modified).
Appendix B
Appendix B.1. Selection of Complications
To identify complications of COVID-19, we considered an ICD-10 code or group of codes as mentioned as complications of COVID-19 if it is reported in the “due to” position with respect to COVID-19 or if it is reported as an “obvious consequence” of COVID-19 and the code (or group of codes) is considered an “obvious consequence” of COVID-19 by the Iris Decision Tables.
A code is reported in the “due to” position with respect to COVID-19 when it is placed in Part 1 together with COVID-19 in a line above it. A code is reported as an “obvious consequence” of COVID-19 if it is reported in the same line of COVID-19 or it is in Part 1 with COVID-19 in Part 2, and the “obvious consequence” relationship is acceptable according to Iris Decision Tables. On the basis of this definition, we calculated the percentages of mention for each group of codes as complications of COVID-19 on total deaths, as shown in Figure 2.
Successively, and for each group of codes, we evaluated if the corresponding condition can be considered a complication of COVID-19. We considered complications of COVID-19 to be those reported in the position of “due to” COVID-19 more than expected. The expected frequencies were calculated under the null hypothesis that the conditions were randomly placed in Part 1 of the death certificate. According to this hypothesis, when a condition c is jointly reported with COVID-19 in Part 1 but in a different line, we expect that half of the time it is reported “due to” COVID-19 and half of the time the contrary is the case, as illustrated in Table A1. This calculation was performed for each group of codes by sex and age group. The comparison between observed and expected has been tested with chi-square distributions. Results of the tests for the whole group of deaths without a breakdown by age or sex are presented in Table A2. In Figure 2, only conditions that result in complications of COVID-19 on the basis of this analysis are shown. Some examples on how certificates were treated for the analysis are provided.
Appendix B.1.1. Example 1
-
P1
a. Respiratory failure;
b. Pneumonia;
c. COVID-19.
In this example, both respiratory failure and pneumonia are mentioned as complications of COVID-19. Moreover, the chi-square analysis showed that they are both reported in the “due to” position with respect to COVID-19 more than expected; therefore, they are both classified as complications of COVID-19.
Appendix B.1.2. Example 2
-
P1
a. Respiratory failure;
b. Pneumonia.
-
P2
COVID-19.
In this example both respiratory failure and pneumonia are mentioned as complications of COVID-19. COVID-19 is reported in Part 2, and the two conditions in Part 1 can be considered obvious consequences of COVID-19.
Appendix B.1.3. Example 3
-
P1
a. Liver failure;
b. Liver metastasis;
c. Lung cancer, positive to SARS-CoV-2 (by swamp).
In this example, liver failure and liver metastasis are reported in a position of “due to” SARS-CoV-2, but liver metastasis is ruled out from complications after the chi-square as it is not reported in the “due to” position with respect to COVID-19 more than expected.
Table A1.
Comparison between observed and expected.
| Observed | Expected | |
|---|---|---|
| Frequency of condition c reported as “due to” COVID-19 (in a line of Part 1 above the line where COVID-19 is reported) |
Dtc | ½ Fc |
| Frequency of condition c reported as “cause of” COVID-19 (in a line of Part 1 below the line where COVID-19 is reported) |
Coc | ½ Fc |
| Total frequency of the condition c reported in Part 1 together with COVID-19 but in a different line | Fc | Fc |
Table A2.
Analysis performed for the inclusion of conditions as complication of COVID-19.
| ICD10 | (Fc) Observed Total in “Due to” or “Cause of” with COVID-19 (A) |
(Dtc) Observed in Due to Position |
(½ Fc) Expected in Due to (=1/2 A) |
Chi-Square Value | Total Number Considered as Complication of COVID-19: Due to and Obvious Consequence | ||
|---|---|---|---|---|---|---|---|
| N | N | N | |||||
| A00-A09 | Intestinal infections | 6 | 3 | 3 | 0.0 | 3 | |
| A00-B99 | Some infectious diseases | 12 | 6 | 6 | 0.0 | 6 | |
| A40-A41, A49, B34, B37, B44, B99 | Sepsis and bacterial infections of unspecified site | 144 | 120 | 72 | 64.0 * | 187 | |
| C00-D48 | Neoplasms | 140 | 19 | 70 | 74.3 § | 25 | |
| D50-D99 | Diseases of blood and blood forming organs | 27 | 13 | 13.5 | 0.0 | 13 | |
| E10-E14 | Endocrine diseases | 67 | 13 | 33.5 | 25.1 § | 13 | |
| E40-E46 | Nutritional disorders | 2 | 2 | 1 | 0.0 | 2 | |
| E66 | Obesity | 12 | 2 | 6 | 5.3 § | 2 | |
| E70-E90 | Other diseases of the metabolism | 33 | 25 | 16.5 | 8.8 * | 26 | |
| F00-F99 | Mental and behavioural disorders | 73 | 13 | 36.5 | 30.3 § | 13 | |
| G00-H99 | other diseases of the nervous system | 58 | 8 | 29 | 30.4 § | 8 | |
| G04, G93 | Encephalitis, myelitis and encephalomyelitis | 46 | 39 | 23 | 22.3 * | 51 | |
| I00-I09, I27-I45, I47, I52 | Specified cardiac diseases | 36 | 20 | 18 | 0.4 | 21 | |
| I10-I5 | Hypertensive heart diseases | 73 | 13 | 36.5 | 30.3 * | 12 | |
| I20-I24 | Myocardial infarction | 47 | 35 | 23.5 | 11.3 * | 35 | |
| I25 | Chronic ischaemic heart disease | 76 | 22 | 38 | 13.5 § | 22 | |
| I26 | Pulmonary embolism | 31 | 28 | 15.5 | 20.2 * | 40 | |
| I70-I79, I83-I89, I95-I99 | Other circulatory diseases | 40 | 21 | 20 | 0.1 | 21 | |
| I46 | Cardiac arrest | 713 | 698 | 356.5 | 654.3 * | 698 | |
| I48-I49 | Atrial fibrillation and other arrhythmias | 59 | 29 | 29.5 | 0.0 | 29 | |
| I50-I51 | Heart complications (heart failure and unspecified cardiac disease) | 242 | 177 | 121 | 51.8 * | 183 | |
| I60-I64 | Acute cerebrovascular accidents | 48 | 20 | 24 | 1.3 | 31 | |
| I80-I82 | Phlebitis, thrombophlebitis and thrombosis of peripheral vessels | 7 | 7 | 3.5 | 0.0 | 7 | |
| J00-J99 | Other respiratory diseases | 98 | 32 | 49 | 11.8 § | 43 | |
| J12-J18, J84, J98 | Pneumonia | 1277 | 1198 | 638.5 | 980.5 * | 4207 | |
| J80-J81 | ARDS and pulmonary oedema | 278 | 273 | 139 | 258.4 * | 318 | |
| J96, R04, R06, R09 | Respiratory failure and related symptoms | 2952 | 2824 | 1476 | 2462.2 * | 3007 | |
| Tutte le altre intestinali | Other diseases of digestive system | 18 | 10 | 9 | 0.2 | 15 | |
| K50-K67 | Other diseases of intestine and peritoneum | 17 | 4 | 8.5 | 4.8 § | 4 | |
| K70-K77 | Chronic liver diseases | 21 | 11 | 10.5 | 0.0 | 11 | |
| M00-M99 | Diseases of the musculoskeletal system and connective tissue | 10 | 3 | 5 | 1.6 | 3 | |
| N00, N04, N17, N19 | Kidney failure | 142 | 112 | 71 | 47.4 * | 112 | |
| N00-N99 | Other diseases of the genitourinary system | 44 | 15 | 22 | 4.5 § | 15 | |
| R57 | Shock | 319 | 311 | 159.5 | 287.8 * | 364 | |
| S00-T98, V01-Y98 | External causes | 55 | 14 | 27.5 | 13.3 § | 59 |
* p < 0.05 and the condition is reported as due to COVID-19; § p < 0.05 and the condition is reported as “cause of” COVID-19.
Appendix C. Age and Gender Distribution of Death Certificates
Figure A1.
Age and gender distribution of all deaths occurring in SARS-CoV-2–positive patients on 28 May 2020 (n = 31,851) and in the study sample (n = 5311).
Author Contributions
Conceptualization, F.G., G.O., and G.M.; methodology, F.G., S.N., C.O., V.M., E.G., R.C., L.F., S.M., M.P., and S.S.; software, S.N., F.G.; formal analysis, F.G., S.N., and G.M.; investigation, G.O.; resources, C.L.N., L.P., C.D., and G.O.; data curation, L.D.P. and A.C.; writing—original draft preparation, F.G. and S.N.; writing—review and editing, G.O.; visualization, all; supervision, G.O.; project administration, G.O.; COVID-19 Mortality Group: acquisition of data and revision of the draft. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Riccardo F., Ajelli M., Andrianou X.D., Bella A., Del Manso M., Fabiani M., Bellino S., Boros S., Urdiales A.M., Marziano V., et al. Epidemiological characteristics of COVID-19 cases in Italy and estimates of the reproductive numbers one month into the epidemic. medRxiv. 2020 doi: 10.1101/2020.04.08.20056861. preprint. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323:1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 3.Zheng Z., Peng F., Xu B., Zhao J., Liu H., Peng J., Li Q., Jiang C., Zhou Y., Liu S., et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J. Infect. 2020;81:e16–e25. doi: 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palmieri L., Vanacore N., Donfrancesco C., Lo Noce C., Canevelli M., Punzo O., Raparelli V., Pezzotti P., Riccardo F., Bella A., et al. Clinical characteristics of hospitalized individuals dying with COVID-19 by age group in Italy. J. Gerontol. A Biol. Sci. Med. Sci. 2020;75:1796–1800. doi: 10.1093/gerona/glaa146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.ONS Measuring Pre-Existing Health Conditions in Death Certification—Deaths Involving COVID-19: March 2020. [(accessed on 27 August 2020)]; Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/methodologies/measuringpreexistinghealthconditionsindeathcertificationdeathsinvolvingcovid19march2020.
- 6.WHO . International Classification of Diseases and Related Health Problems. 5th ed. WHO; Geneva, Switzerland: 2016. [Google Scholar]
- 7.Iss, Istat, Inail Rapporto ad Interim su Definizione, Certificazione e Classificazione Delle Cause di Morte. Versione dell’8 Giugno 2020, ISS COVID-19 n. 49/2020. [(accessed on 27 August 2020)]; Available online: https://www.iss.it/documents/20126/0/Rapporto+ISS+COVID-19++49_2020+%281%29.pdf/9378da12-76ae-f51f-9666-14c7c2078a17?t=1592583825077.
- 8.Grippo F., Désesquelles A., Pappagallo M., Frova L., Egidi V., Meslé F. Multi-morbidity and frailty at death: A new classification of death records for an aging world. Popul. Stud. 2019 doi: 10.1080/00324728.2020.1820558. in press. [DOI] [PubMed] [Google Scholar]
- 9. [(accessed on 27 August 2020)]; Available online: https://www.gazzettaufficiale.it/eli/id/2020/02/28/20A01348/SG.
- 10.Agrawal H., Das N., Nathani S., Saha S., Saini S., Kakar S.S., Roy P. An assessment on impact of COVID-19 infection in a gender specific manner. Stem Cell Rev. Rep. 2020;838:3. doi: 10.1007/s12015-020-10048-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson R.N. Coding and classifying causes of death: Trends and international differences. In: Rogers R.G., Crimmins E.M., editors. International Handbook of Adult Mortality. Springer; Dordrech, The Netherlands: 2011. pp. 467–489. [Google Scholar]
- 12.Dietz W., Santos-Burgoa C. Obesity and its implications for COVID-19 mortality. Obesity. 2020;28:1005. doi: 10.1002/oby.22818. [DOI] [PubMed] [Google Scholar]
- 13.Onder G., Palmieri L., Vanacore N., Giuliano M., Brusaferro S., Italian National Institute of Health COVID-19 mortality group Non-respiratory complications and obesity in patients dying with COVID-19 in Italy. Obesity. 2020 doi: 10.1002/oby.23007. [DOI] [Google Scholar]