Abstract
Diseases caused by Escherichia coli (E. coli) and Salmonella spp. can negatively impact turkey farming. The aim of this study was to isolate and characterize multidrug-resistant (MDR) E. coli and Salmonella spp. in healthy and diseased turkeys. A total of 30 fecal samples from healthy turkeys and 25 intestinal samples from diseased turkeys that died of enteritis were collected. Bacterial isolation and identification were based on biochemical properties and polymerase chain reaction (PCR). Antibiogram profiles were determined by disk diffusion. The tetracycline-resistance gene tetA was detected by PCR. All samples were positive for E. coli. Only 11 samples (11/30; 36.67%) were positive for Salmonella spp. from healthy turkeys, whereas 16 (16/25; 64%) samples were positive for Salmonella spp. from diseased turkeys. E. coli isolated from diseased turkeys showed higher resistance to levofloxacin, gentamicin, chloramphenicol, ciprofloxacin, streptomycin, and tetracycline. Salmonella spp. isolated from healthy turkeys exhibited higher resistance to gentamicin, chloramphenicol, ciprofloxacin, streptomycin, imipenem, and meropenem. All E. coli and Salmonella spp. from both healthy and diseased turkeys were resistant to erythromycin. Salmonella spp. from both healthy and diseased turkeys were resistant to tetracycline. Multidrug resistance was observed in both E. coli and Salmonella spp. from diseased turkeys. Finally, the tetA gene was detected in 93.1% of the E. coli isolates and in 92.59% of the Salmonella spp. isolates. To the best of our knowledge, this is the first study to isolate and characterize tetA-gene-containing MDR E. coli and Salmonella spp. from healthy and diseased turkeys in Bangladesh. Both microorganisms are of zoonotic significance and represent a significant public health challenge.
Keywords: avian colibacillosis, salmonellosis, antibiotic resistance, MDR, tetA, public health
1. Introduction
Turkey (Meleagris gallopavo) farming is a profitable business in many countries. In Bangladesh, turkey farming generates a higher profit than broiler and layer farming due to lower feeding cost, higher market price, and high demand from consumers. In addition, turkey is generally more adaptable under different weather conditions and less prone to disease than other poultry birds [1,2]. In Bangladesh, there are more than 600 small- and medium-sized commercial turkey farms [3]. With strong support of the Bangladesh government, the number of farms is increasing [3]. According to the Household Income and Expenditure Survey 2016 in Bangladesh [4], the average daily protein intake per capita was 63.50 g, of which meat, poultry, and eggs contributed 12.65% of the total proteins. Furthermore, poultry contributed 37% of the overall meat production in Bangladesh [5]. In rural areas, rearing poultry is a common additional source of income [6]. The challenges of turkey farming include potential outbreaks of infectious and non-infectious diseases, which have been shown to impact more than a third of turkey farmers in Bangladesh [7]. Infections caused by Escherichia coli and Salmonella spp. have negative impacts on turkey farming as they lower egg production, reduce hatchability, and increase mortality rates [8]. Thus, the control of E. coli and Salmonella infections in turkey farms is crucial.
E. coli is a zoonotic commensal pathogen that is capable of causing infections in the gastrointestinal tract (GIT), respiratory tract, and bloodstream in both humans and animals [9,10]. Avian colibacillosis caused by E. coli is responsible for turkey cellulitis, colisepticemia, swollen head syndrome, synovitis, salpingitis, coligranuloma, osteomyelitis, omphalitis, peritonitis, panophthalmitis, and is often deadly for turkeys [11,12]. It also causes urinary tract infections (UTIs), abdominal sepsis, and meningitis. It is important to note that E. coli is responsible for about 80% of UTIs in humans [13,14].
Salmonella spp. can cause salmonellosis (especially pullorum disease and fowl typhoid) in turkeys [15,16]. Salmonella infections reduce hatchability, fertility, growth, and increase mortality rates in poultry [17]. Due to their zoonotic nature, Salmonella spp. can be transmitted to humans through the food chain. This can lead to the development of salmonellosis, gastroenteritis, enteric fever [18,19], and can sometimes cause life-threatening consequences [20].
The excessive use of antibiotics in farms led to the emergence of antibiotic-resistant bacteria such as E. coli, Salmonella spp., and Campylobacter spp. in poultry [21,22]. High levels of antibiotic-resistant or multidrug-resistant (MDR) E. coli and Salmonella spp. can constitute a more significant problem in turkeys than in other livestock species [21,23]. Mutations in E. coli and Salmonella spp. could result in the acquisition of antibiotic resistance [24]. Mobile genetic elements allowed bacteria to acquire and disseminate antibiotic resistance [25]. The implications of this acquired antibiotic resistance for public health necessitates attention from both clinical and economic experts [26].
Antimicrobial resistance (AMR) poses a significant threat to human health [27]. AMR is responsible for approximately 700,000 human deaths every year throughout the world [28]. This figure could significantly increase in the near future if we do not discover novel and effective antibiotics [29]. The antibiotic resistance in farm animals is clearly intertwined with the presence of this problem in humans [30,31]. In addition, the indiscriminate use of antibiotics in livestock is one of the main causes of AMR [25,26]. The overuse of antibiotics by farm owners in poultry farms, a common practice in developing countries, is a major reason for the development of MDR bacteria [32,33]. This overuse typically occurs without consulting any veterinarians and without any previous testing of the animals. The development of MDR bacteria in poultry has been previously reported in previous studies [22,33,34,35]. Poultry farmers have been using different types of poultry in recent years including broilers, layers, and turkeys. These animals are hosted close to each other, which can lead to the horizontal transmission of MDR bacteria to turkeys. The dissemination of MDR bacteria to humans exposes the population to risk, especially the immunocompromised individuals, and exacerbates healthcare costs, and ultimately increases the usage of antibiotics [36].
The present study was designed to isolate and characterize MDR E. coli and Salmonella spp. from both healthy and diseased turkeys. There is an urgent need to design proper surveillance and control programs for the detection and control of antibiotic-resistant bacteria in turkey farms.
2. Results
2.1. Prevalence of E. coli and Salmonella spp.
All 55 samples were positive for E. coli (using PCR targeting the malB gene), whereas 27 samples (27/55; 49.09%) were positive for Salmonella spp. (using PCR targeting the invA gene). The prevalence of E. coli in turkeys was significantly higher than Salmonella spp. (chi-square test, 95% CI, p < 0.001). The prevalence of Salmonella spp. was significantly higher in diseased (64%; 16/25) than in healthy turkeys (36.67; 11/30) (chi-square test, 95% CI, p < 0.05). No significant difference between healthy and diseased turkeys was observed in the case of E. coli (Table 1).
Table 1.
Prevalence and resistance profiles of E. coli and Salmonella spp. isolated from turkeys.
| Microorganism | Categories | Prevalence | Antibiotic Resistance Pattern (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| LEV | E | GEN | C | CIP | S | IMP | MEM | TE | |||
| E. coli | Healthy | 30 | 4 | 30 | 0 | 0 | 17 | 4 | 0 | 30 | 4 |
| (100) | (13.33) | (100) | (0) | (0) | (56.67) | (13.33) | (0) | (100) | (13.33) | ||
| Diseased | 25 | 11 | 25 | 9 | 11 | 20 | 5 | 0 | 10 | 25 | |
| (100) | (44) | (100) | (36) | (44) | (80) | (20) | (0) | (40) | (100) | ||
| p-value (Healthy vs. Diseased) | N/C | 0.011 | N/C | <0.001 | <0.001 | 0.066 | 0.716 | N/C | <0.001 | <0.001 | |
| Salmonella spp. | Healthy | 11 | 2 | 11 | 5 | 6 | 6 | 4 | 4 | 7 | 11 |
| (36.67) | (18.18) | (100) | (45.45) | (54.54) | (54.54) | (36.36) | (36.36%) | (63.63) | (100) | ||
| Diseased | 16 | 4 | 16 | 0 | 2 | 6 | 2 | 4 | 4 | 16 | |
| (64) | (25) | (100) | (0) | (12.5) | (37.5) | (12.5) | (25%) | (25) | (100) | ||
| p-value (Healthy vs. Diseased) | 0.043 | 1.000 | N/C | 0.006 | 0.033 | 0.438 | 0.187 | 0.675 | 0.061 | N/C | |
A p-value less than 0.05 was deemed to be statistically significant; N/C, not computed; E. coli, Escherichia coli; LEV, Levofloxacin; E, Erythromycin; GEN, Gentamicin; C, Chloramphenicol; CIP, Ciprofloxacin; S, Streptomycin; IMP, Imipenem; MEM, Meropenem; TE, Tetracycline.
2.2. Antibiotic Profiles of Isolated E. coli and Salmonella spp.
Antibiotic sensitivity tests revealed that all E. coli isolates were resistant to erythromycin; whereas all Salmonella isolates were resistant to erythromycin and tetracycline. Additionally, E. coli isolates were resistant to ciprofloxacin (67.27%), meropenem (72.73%), and tetracycline (52.73%). Salmonella spp. were resistant to ciprofloxacin (44.44%) and meropenem (40.74%). E. coli isolates were highly sensitive to imipenem (92.73%)
E. coli isolated from diseased turkeys showed higher resistance to levofloxacin (chi-square test, 95% CI, p = 0.011), gentamicin (p < 0.001), chloramphenicol (p < 0.001), and tetracycline (p < 0.001); whereas isolates from healthy turkeys showed higher resistance to meropenem (p < 0.001). Interestingly, Salmonella spp. isolated from healthy turkeys exhibited higher resistance to gentamicin, chloramphenicol, ciprofloxacin, streptomycin, imipenem, and meropenem than Salmonella spp. isolated from diseased turkeys. However, only a few cases were statistically significant (Table 1).
2.3. Detection of tetA Gene
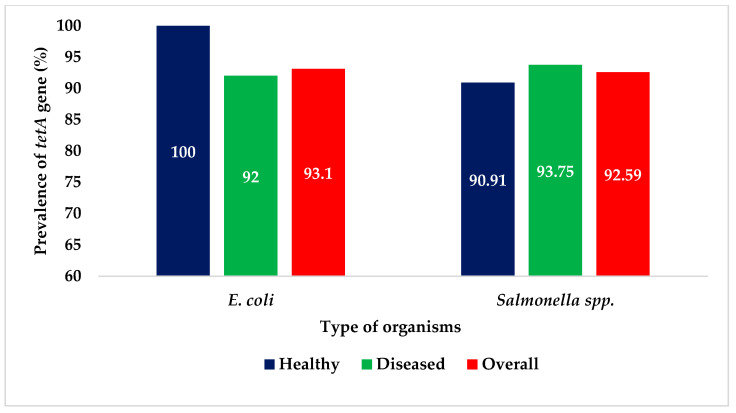
Of the 29 E. coli isolates phenotypically resistant to tetracycline, tetA was detected in 27 (27/29; 93.1%). In the case of Salmonella spp., tetA was detected in 25 of the 27 isolates (25/27; 92.59%). The prevalence of tetA was similar in healthy and diseased turkeys for both E. coli and Salmonella spp. (Figure 1).
Figure 1.
Prevalence of tetA gene in E. coli and Salmonella spp. isolated from turkeys.
2.4. Detection of MDR E. coli and Salmonella spp.
As shown in Table 2, antibiogram typing revealed that most E. coli isolates (48/55; 87.27%) and most Salmonella isolates (24/27; 88.89%) exhibited multi-drug resistance. For E. coli, the percentage of MDR isolates was higher from diseased turkeys (24/25; 96%) than from healthy turkeys (24/30; 80%). For Salmonella, the percentage of MDR isolates was also higher in diseased turkeys (16/16; 100%) than in healthy turkeys (11/16; 72.72%). However, the differences were not statistically significant in either case (chi-square test, 95% CI, p > 0.05).
Table 2.
Multidrug resistance profiles of E. coli and Salmonella spp. isolated from healthy and diseased turkeys.
| Microorganism | Source | Pattern No. | Antibiotic Resistance Patterns | No. of Antibiotics (Classes) | No. of MDR Isolates (%) | Total (%) |
p-Value (Healthy vs. Diseased) |
|---|---|---|---|---|---|---|---|
|
E. coli (n = 55) |
Healthy Turkeys (n = 30) |
1 | E, MEM, CIP | 3 (3) | 14 | 24 (80%) |
0.112 |
| 2 | E, MEM, TE | 3 (3) | 1 | ||||
| 3 | E, MEM, LEV | 3 (3) | 2 | ||||
| 4 | E, MEM, S | 3 (3) | 3 | ||||
| 5 | E, MEM, CIP, LEV | 4 (3) | 1 | ||||
| 6 | E, MEM, LEV, TE | 4 (4) | 1 | ||||
| 7 | E, MEM, CIP, TE | 4 (4) | 1 | ||||
| 8 | E, MEM, S, CIP, TE | 5 (5) | 1 | ||||
| Diseased Turkeys (n = 25) |
1 | E, CIP, TE | 3 (3) | 4 | 24 (96%) |
||
| 2 | E, MEM, TE | 3 (3) | 3 | ||||
| 3 | E, CIP, LEV, TE | 4 (3) | 3 | ||||
| 4 | E, GEN, S, CIP, TE | 5 (4) | 3 | ||||
| 5 | E, MEM, C, CIP, TE | 5 (5) | 2 | ||||
| 6 | E, MEM, C, S, TE | 5 (5) | 1 | ||||
| 7 | E, C, GEN, CIP, LEV, TE | 6 (5) | 4 | ||||
| 8 | E, MEM, C, CIP, LEV, TE | 6 (5) | 2 | ||||
| 9 | E, MEM, C, GEN, CIP, LEV, TE | 7 (6) | 1 | ||||
| 10 | E, MEM, C, GEN, S, CIP, LEV, TE | 8 (6) | 1 | ||||
|
Salmonella spp. (n = 27) |
Healthy Turkeys (n = 11) |
1 | E, MEM, C, CIP, TE | 5 (5) | 3 | 8 (72.73%) | 0.056 |
| 2 | E, C, GEN, CIP, TE | 5 (5) | 1 | ||||
| 3 | E, MEM, IMP, C, GEN, S, TE | 7 (5) | 2 | ||||
| 4 | E, MEM, IMP, GEN, S, CIP, LEV, TE | 8 (6) | 2 | ||||
| Diseased Turkeys (n = 16) |
1 | E, MEM, TE | 3 (3) | 3 | 16 (100%) | ||
| 2 | E, IMP, TE | 3 (3) | 3 | ||||
| 3 | E, CIP, TE | 3 (3) | 5 | ||||
| 4 | E, LEV, TE | 3 (3) | 2 | ||||
| 5 | E, IMP, C, TE | 4 (4) | 1 | ||||
| 6 | E, C, S, LEV, TE | 5 (5) | 1 | ||||
| 7 | E, MEM, S, CIP, LEV, TE | 6 (5) | 1 |
A p-value less than 0.05 was deemed to be statistically significant; E. coli, Escherichia coli; TE, Tetracycline; E, Erythromycin; C, Chloramphenicol; LEV, Levofloxacin; GEN, Gentamicin; MEM, Meropenem; IMP, Imipenem; S, Streptomycin; CIP, Ciprofloxacin.
E. coli isolated from healthy turkeys showed eight resistance patterns, while E. coli isolated from diseased turkeys showed ten resistance patterns. Salmonella isolated from healthy and diseased turkeys showed four and seven resistance patterns, respectively (Table 2). Among the antibiogram types, pattern E-MEM-CIP showed the highest prevalence in E. coli (14 isolates). On the other hand, the E-CIP-TE pattern showed the highest prevalence in Salmonella (five isolates) (Table 2).
3. Discussion
In this study, we report the detection of MDR E. coli and Salmonella spp. from healthy and diseased turkeys. This is significant to human health due to the zoonotic nature of these pathogens. Moreover, most E. coli and Salmonella spp. isolates were found to be MDR, which makes it difficult to treat the infected turkeys [37,38,39,40,41,42]. Antibiograms can guide the choice of therapies for colibacillosis and salmonellosis in turkeys. The incorrect choice of antibiotics is not only associated with the development of AMR but can also have significant negative economic impacts.
Whereas all samples were positive for E. coli, only 49.09% (27/55) of the samples were positive for Salmonella spp., which were significantly more prevalent in diseased than in healthy turkeys. The isolation and characterization of E. coli and Salmonella spp. from turkeys revealed the presence of the tetA gene. The gut microflora of poultry typically includes E. coli and Salmonella spp. [43]. Detection of Salmonella spp. in diseased turkeys that died of enteritis suggests that Salmonella was the causative factor of enteritis. Previously, Kar et al. [8] reported the detection of E. coli and Salmonella spp. from cloacal swabs of turkeys but did not use any molecular techniques, such as the PCR technology used in this study. PCR is a robust and rapid detection method with increased sensitivity and specificity for detecting Salmonella in food, environmental, and clinical samples [44]. The invA gene has been the target for many PCR protocols, as it is found in almost all known serovars of Salmonella [45]. This gene encodes an inner membrane protein necessary for invasion of epithelial cells by Salmonella [46]. We were able to observe higher rates of E. coli and Salmonella spp. compared to the study of Kar et al. [8], which may be attributed to the highly sensitive nature of the molecular techniques used in this study.
The detection of E. coli and Salmonella spp. from fecal materials and intestinal contents of healthy turkeys indicates intestinal colonization [47]. The findings also indicate that fecal materials may be a source of transmission of E. coli and Salmonella spp. to other birds. The detection of the virulence gene invA in the isolated Salmonella spp. indicates the potential pathogenic nature of these isolates. It is also possible for these pathogens to be introduced into the food chain causing food-borne diseases [48].
Antibiotic resistance is a major public health problem. The misuse and abuse of antimicrobial agents contributed to the emergence and dissemination of antibiotic-resistant pathogens in animals and humans [49]. Location-specific information on antibiotic resistance patterns in different geographical areas is important for the successful treatment of outbreaks and infections. The isolated E. coli and Salmonella spp. were found to be resistant to levofloxacin, erythromycin, ciprofloxacin, meropenem, and tetracycline. This antibiotic resistance profile can be due to the frequent use of antibiotics in poultry for therapeutic and growth promotion purposes [32,33]. The presence of antibiotic-resistant E. coli and Salmonella spp. in fecal materials of healthy turkeys indicates the role of these birds as spreaders of resistant microorganisms in farm environments.
Several studies detected the tetA gene in E. coli and Salmonella spp. from dairy farms, boiler farms, house flies, and aquatic environments [31,33,50,51,52]. However, there were no studies on the detection of the tetA gene in E. coli and Salmonella from turkeys. Among the isolates phenotypically resistant to tetracycline, 93.1% of the E. coli isolates and 92.59% of Salmonella spp. isolates were positive for the tetA gene. The tetA has been shown to be the most common genetic component in tetracycline-resistant E. coli and Salmonella spp. [9,53,54,55]. Generally remaining in mobile genetic components (integrons, transposons, and plasmids), tetA can be easily transferred to different bacteria.
Resistance to carbapenems (imipenem and meropenem) may be due to the transmission of bacteria from human sources, especially that carbapenems are not approved for use in livestock [56]. Future detailed studies at the genetic level are needed to test this hypothesis. According to the WHO, carbapenem-resistant E. coli and Salmonella spp. are considered to be among the most critical pathogens [57]. The detection of carbapenem-resistant E. coli and Salmonella spp. in turkeys has to be treated as an urgent public health problem.
Antibiotic treatment failures in poultry has been highly attributed to the MDR nature of the pathogens [58]. In the present study, the majority of the isolated E. coli (48/55; 87.27%) and Salmonella spp. (24/27; 88.89%) were MDR. More MDR E. coli and Salmonella spp. were retrieved from diseased turkeys than from healthy turkeys. The higher MDR in diseased turkeys may have been caused by the selection pressure resulting from the excessive use of several classes of antibiotics. However, the differences were statistically insignificant as in Table 2 (p = 0.112 and p = 0.056 for E. coli and Salmonella spp., respectively). The statistical insignificance indicates that the bacteria were MDR regardless of whether the source was healthy or diseased turkeys. To avoid the development of MDR, the use of antibiotics should be more strategic and selective.
4. Materials and Methods
4.1. Ethics Statement
No ethical permission was required for the study. During sample collection, verbal permission was taken from farm owners.
4.2. Study Design
A pilot survey was conducted prior to the start of the current study to identify the different turkey farming areas in Bangladesh, disease outbreaks in these farms, and antibiotic treatment regimens. Based on the survey results, seven antibiotics were selected. In addition, two carbapenem antibiotics were included based on reports that indicated that E. coli could be resistant to carbapenems in poultry [31,50,59]. Guided by bird mortality rates and antibiotic use reports from the survey, five farms from two districts were selected for sample collection. The birds were categorized into healthy and diseased birds. Six healthy and five diseased bird samples were randomly collected from each farm resulting in a total of 55 samples from the five farms. Freshly dropped feces from healthy birds and intestinal contents from diseased birds that had avian colibacillosis and/or Salmonellosis were collected for analysis.
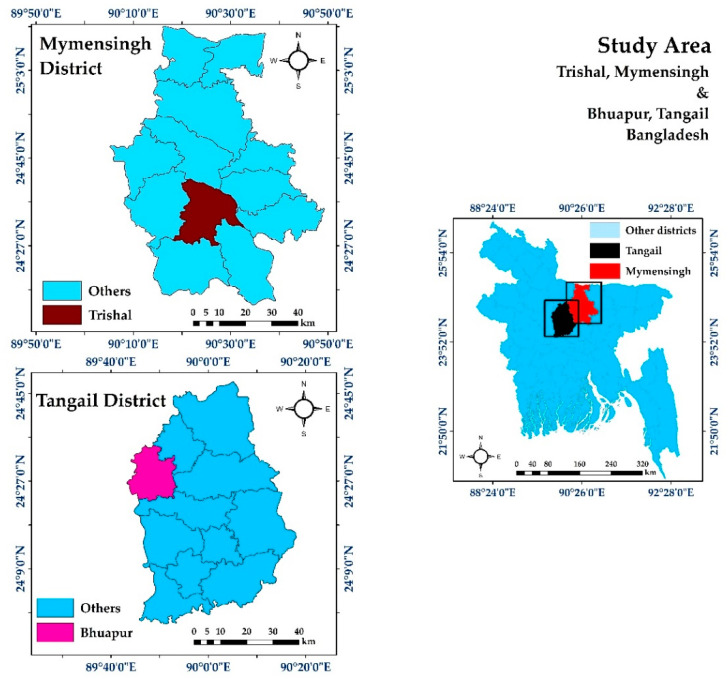
4.3. Study Areas and Collection of Samples
The study was conducted in two districts of Bangladesh namely Mymensingh (24.7539° N, 90.4073° E) and Tangail (24.2513° N, 89.9167° E) during the period from June 2018 to November 2019. The study areas are represented in Figure 2.
Figure 2.
Map of the study area. Images were extracted from DIVA-GIS using Geographical Information System (GIS). The map was developed using ArcMap version 10.7.
Freshly dropped fecal samples (n = 30) were aseptically collected using sterile cotton buds from healthy turkeys. During the postmortem examination, 5 g of intestinal contents (n = 25) was collected from each turkey that died of enteritis and had lesions of avian colibacillosis and/or salmonellosis.
Immediately after collection, samples were transferred to sterile zip-lock bags. Samples were transported to the laboratory maintaining cold chain. Collected samples were transferred into sterile test tubes containing freshly prepared nutrient broth (5 mL) and were incubated aerobically at 37 °C overnight for the growth of bacteria.
4.4. Isolation of E. coli and Salmonella spp.
Isolation of E. coli and Salmonella spp. was based on culture on Eosin Methylene Blue (EMB) and Xylose Lysine Deoxycholate (XLD) agar (HiMedia, India) plates, respectively. Initially, freshly grown broth cultures were streaked on EMB and XLD agar media using sterile inoculating loops. This was followed by aerobic incubation of the inoculated agar plates at 37 °C overnight to obtain pure colonies. Single green-colored metallic-sheen colonies on EMB agar media and black-centered colonies on XLD agar media represented the growth of E. coli and Salmonella spp., respectively. For further confirmation, selected colonies were subjected to morphological study by Gram staining and biochemical tests such as the methyl red test, sugar fermentation test, Voges–Proskauer test, motility test, urease test, and indole test [22,31].
4.5. Molecular Detection of E. coli and Salmonella spp.
Isolation of E. coli and Salmonella spp. were confirmed by polymerase chain reaction (PCR) targeting E. coli 16S rRNA gene and Salmonella genus specific invA genes respectively (Table 3).
Table 3.
List of primers used for detecting E. coli, Salmonella spp., and tetracycline-resistance gene.
For PCR, genomic DNA of E. coli and Salmonella spp. was extracted by the boiling method as described by Sobur et al. [50]. Briefly, a pure colony collected from freshly grown culture was initially taken into an Eppendorf tube containing molecular-grade water (100 μL) followed by mixing gently through vortexing. Subsequently, the mixture was boiled for 10 min, cooled for 10 min, and centrifuged for 10 min at 1400 rpm. Finally, the supernatant was collected as the source for the genomic DNA for PCR and stored at −20 °C until further use.
PCR tests were carried out in a final volume of 25 μL with 12.5 μL of the master mix (2X) (Promega, Madison, WI, USA), 4 μL of genomic DNA (50 ng/μL), 1 μL of each primer, and 6.5 μL of nuclease-free water. After amplification, PCR products were subjected to gel electrophoresis in 1.5% agarose, followed by staining and visualizing by 0.25% ethidium bromide solution and ultraviolet trans-illuminator (Biometra, Göttingen, Germany). A DNA ladder (100 bp; Promega, Madison, WI, USA) was used to assess the sizes of PCR amplicons.
4.6. Antibiotic Sensitivity Test
Antibiotic sensitivity testing of isolated E. coli and Salmonella spp. was carried out using the disk diffusion assay as previously described [63]. Antibiotic classes included fluoroquinolones (levofloxacin, LEV—5 μg; ciprofloxacin, CIP—5 μg), aminoglycosides (gentamicin, GEN—10 μg; streptomycin, S—10 μg), carbapenems (Meropenem, MEM—10 μg; imipenem, IMP—10 μg), amphenicols (chloramphenicol, C—10 μg), macrolides (erythromycin, E—15 μg), and tetracyclines (tetracycline, TE—30 μg) purchased from Hi Media (India). Sensitivity tests were performed on freshly grown isolates having a concentration equivalent to 0.5 McFarland standard using Mueller-Hinton agar media (Hi Media, India). All results were interpreted according to the guidelines provided by Clinical and Laboratory Standards Institute [64]. Furthermore, isolates showing resistance against three or more different classes of antibiotics were defined as MDR [65].
4.7. Molecular Detection of Tetracycline Resistance tetA Gene
E. coli and Salmonella isolates resistant to tetracycline were screened by PCR for the detection of the tetracycline-resistance tetA gene using the primer and protocol described by Randall et al. [62].
4.8. Statistical Analysis
Chi-square tests were performed using the SPSS software (IBM SPSS version 25.0, IBM, Chicago, IL, USA). p-values less than 0.05 (p < 0.05) were considered to be statistically significant.
5. Conclusions
The isolation and characterization of tetA-gene-containing-MDR E. coli and Salmonella spp. from turkeys are concerning. The potential ability of these MDR bacteria to enter into the food chain can expose humans to serious health risks. Bacterial surveillance programs should be implemented in order to control the emergence of bacterial resistance in turkey farms in Bangladesh and elsewhere in the world. This should be a concerted effort that is best carried out via bacterial surveillance networks across different countries. Additionally, holistic and multi-sectoral approaches, such as the one health approach, need to be implemented [66]. Guided by top health professionals and scientists, these strategies can provide effective solutions to the complex, multifaceted global challenge of AMR.
Acknowledgments
We are grateful to farm owners for giving us access to samples during the course of the study.
Author Contributions
Conceptualization and design of the study, H.M.A. and M.T.R.; Sampling, M.T. and M.M.M.; Methodology, M.T., M.S.I., M.A.S. and S.P.; data analysis and interpretation, M.S.I., M.A.S., H.M.A. and M.T.R.; writing—original draft preparation, M.T., M.S.I., M.A.S., M.J.H., H.M.A. and M.T.R.; supervision, M.T.H., H.M.A., and M.T.R.; critical revisions and writing of the revised manuscript, H.M.A. and M.T.R. All authors have read and agreed to the final published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Anandh M.A., Jagatheesan P.N.R., Kumar P.S., Rajarajan G., Paramasivam A. Effect of egg weight on egg traits and hatching performance of turkey (Meleagris gallopavo) eggs. Iran. J. Appl. Anim. Sci. 2012;2:391–395. [Google Scholar]
- 2.Jahan B., Ashraf A., Rahman M.A., Molla M.H.R., Chowdhury S.H., Megwalu F.O. Rearing of high yielding turkey poults: Problems and future prospects in Bangladesh: A review. SF J. Biotechnol. Biomed. Eng. 2018;1:1008. [Google Scholar]
- 3.The Independent Turkey Rearing Gains Popularity. [(accessed on 12 September 2020)]; Available online: http://www.theindependentbd.com/printversion/details/185891.
- 4.Bangladesh Bureau of Statistics (BBS) Report of the Household Income and Expenditure Survey 2016. [(accessed on 12 September 2020)]; Available online: https://drive.google.com/file/d/1TmUmC-0M3wC5IN6_tUxZUvTW2rmUx-Mce/view?usp=sharing.
- 5.Begum I.A., Alam M.J., Buysse J., Frija A., Van Huylenbroeck G. A comparative efficiency analysis of poultry farming systems in Bangladesh: A Data Envelopment Analysis approach. Appl. Econ. 2011;44:3737–3747. doi: 10.1080/00036846.2011.581216. [DOI] [Google Scholar]
- 6.Islam M.S., Sabuj A.A.M., Haque Z.F., Pondit A., Hossain M.G., Saha S. Seroprevalence of avian reovirus in backyard chickens in different areas of Mymensingh district in Bangladesh. J. Adv. Vet. Anim. Res. 2020;7:546–553. doi: 10.5455/javar.2020.g452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Asaduzzaman M., Salma U., Ali H.S., Hamid M.A., Miah A.G. Problems and prospects of turkey (Meleagris gallopavo) production in Bangladesh. Res. Agric. Livest. Fish. 2017;4:77–90. doi: 10.3329/ralf.v4i2.33719. [DOI] [Google Scholar]
- 8.Kar J., Barman T.R., Sen A., Nath S.K. Isolation and identification of Escherichia coli and Salmonella sp. from apparently healthy Turkey. Int. J. Adv. Res. Biol. Sci. 2017;4:72–78. [Google Scholar]
- 9.Hopkins K.L., Davies R.H., Threlfall E.J. Mechanisms of quinolone resistance in Escherichia coli and Salmonella: Recent developments. Int. J. Antimicrob. Agents. 2005;25:358–373. doi: 10.1016/j.ijantimicag.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Rahman M.T., Sobur M.A., Islam M.S., Ievy S., Hossain M.J., El Zowalaty M.E., Rahman A.T., Ashour H.M. Zoonotic Diseases: Etiology, Impact, and Control. Microorganisms. 2020;8:1405. doi: 10.3390/microorganisms8091405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barnes H.J., Gross W.B. Diseases of Poultry. 10th ed. Mosby-Wolfe Medical Publication Ltd; London, UK: 1997. Colibacillosis; pp. 131–139. [Google Scholar]
- 12.De Oliveira A.L., Newman D.M., Sato Y., Noel A., Rauk B., Nolan L.K., Barbieri N.L., Logue C.M. Characterization of Avian Pathogenic Escherichia coli (APEC) Associated With Turkey Cellulitis in Iowa. Front. Vet. Sci. 2020;7:380. doi: 10.3389/fvets.2020.00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foxman B. The epidemiology of urinary tract infection. Nat. Rev. Urol. 2010;7:653–660. doi: 10.1038/nrurol.2010.190. [DOI] [PubMed] [Google Scholar]
- 14.Mellata M. Human and avian extraintestinal pathogenic Escherichia coli: Infections, zoonotic risks, and antibiotic resistance trends. Foodborne Pathog. Dis. 2013;10:916–932. doi: 10.1089/fpd.2013.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aury K., Chemaly M., Petetin I., Rouxel S., Picherot M., Michel V., Le Bouquin S. Prevalence and risk factors for Salmonella enterica subsp. enterica contamination in French breeding and fattening turkey flocks at the end of the rearing period. Prev. Vet. Med. 2010;94:84–93. doi: 10.1016/j.prevetmed.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 16.Abdukhalilova G., Kaftyreva L., Wagenaar J.A., Tangyarikov B., Bektimirov A., Akhmedov I., Khodjaev Z., Kruse H. World Health Organization. Occurrence and antimicrobial resistance of Salmonella and Campylobacter in humans and broiler chicken in Uzbekistan. Public Health Panor. 2016;2:340–347. [Google Scholar]
- 17.Andino A., Hanning I. Salmonella enterica: Survival, Colonization, and Virulence Differences among Serovars. Sci. World J. 2015;2015:520179. doi: 10.1155/2015/520179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao S., Qaiyumi S., Friedman S., Singh R., Foley S.L., White D.G., McDermott P.F., Donkar T., Bolin C., Munro S., et al. Characterization of Salmonella enterica serotype Newport isolated from humans and food animals. J. Clin. Microbiol. 2003;41:5366–5371. doi: 10.1128/JCM.41.12.5366-5371.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Varga C., Guerin M.T., Brash M.L., Slavic D., Boerlin P., Susta L. Antimicrobial resistance in fecal Escherichia coli and Salmonella enterica isolates: A two-year prospective study of small poultry flocks in Ontario, Canada. BMC Vet. Res. 2019;15:1–10. doi: 10.1186/s12917-019-2187-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Helms M., Vastrup P., Gerner-Smidt P., Mølbak K. Excess mortality associated with antimicrobial drug-resistant Salmonella Typhimurium. Emerg. Infect. Dis. 2002;8:490–495. doi: 10.3201/eid0805.010267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yeh J.C., Chen C.L., Chiou C.S., Lo D.Y., Cheng J.C., Kuo H.C. Comparison of prevalence, phenotype, and antimicrobial resistance of Salmonella serovars isolated from turkeys in Taiwan. Poult. Sci. 2018;97:279–288. doi: 10.3382/ps/pex293. [DOI] [PubMed] [Google Scholar]
- 22.Ievy S., Islam M.S., Sobur M.A., Talukder M., Rahman M.B., Khan M.F.R., Rahman M.T. Molecular Detection of Avian Pathogenic Escherichia coli (APEC) for the First Time in Layer Farms in Bangladesh and Their Antibiotic Resistance Patterns. Microorganisms. 2020;8:1021. doi: 10.3390/microorganisms8071021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Poppe C., Martin L.C., Gyles C.L., Reid-Smith R., Boerlin P., McEwen S.A., Prescott J.F., Forward K.R. Acquisition of resistance to extended-spectrum cephalosporins by Salmonella enterica subsp. enterica serovar Newport and Escherichia coli in the turkey poult intestinal tract. Appl. Environ. Microbiol. 2005;71:1184–1192. doi: 10.1128/AEM.71.3.1184-1192.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blair J.M., Webber M.A., Baylay A.J., Ogbolu D.O., Piddock L.J. Molecular mechanisms of antibiotic resistance. Nat. Rev. Microbiol. 2015;13:42–51. doi: 10.1038/nrmicro3380. [DOI] [PubMed] [Google Scholar]
- 25.Fluit A., Schmitz F.J. Class 1 integrons, gene cassettes, mobility, and epidemiology. Eur. J. Clin. Microbiol. Infect. Dis. 1999;18:761–770. doi: 10.1007/s100960050398. [DOI] [PubMed] [Google Scholar]
- 26.Tirumalai M.R., Karouia F., Tran Q., Stepanov V.G., Bruce R.J., Ott C.M., Pierson D.L., Fox G.E. Evaluation of acquired antibiotic resistance in Escherichia coli exposed to long-term low-shear modeled microgravity and background antibiotic exposure. Mbio. 2019;10:e02637-18. doi: 10.1128/mBio.02637-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alexander H.K., MacLean R.C. Stochastic bacterial population dynamics restrict the establishment of antibiotic resistance from single cells. Proc. Natl. Acad. Sci. USA. 2020;117:19455–19464. doi: 10.1073/pnas.1919672117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clifford K., Darash D., da Costa C.P., Meyer H., Islam M.T., Meyer H., Klohe K., Winklerc A., Rahman M.T., Islam M.T., et al. Antimicrobial resistance in livestock and poor quality veterinary medicines. Bull. World Health Organ. 2018;96:662–664. doi: 10.2471/BLT.18.209585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O’Neill J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. [(accessed on 18 August 2020)];2016 Available online: https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf.
- 30.Woolhouse M., Ward M., van Bunnik B., Farrar J. Antimicrobial resistance in humans, livestock and the wider environment. Philos. Trans. R. Soc. B. 2015;370:20140083. doi: 10.1098/rstb.2014.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sobur M.A., Sabuj A.A.M., Sarker R., Rahman A.M.M.T., Kabir S.M.L., Rahman M.T. Antibiotic-resistant Escherichia coli and Salmonella spp. associated with dairy cattle and farm environment having public health significance. Vet. World. 2019;12:984–993. doi: 10.14202/vetworld.2019.984-993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wright G.D. The antibiotic resistome: The nexus of chemical and genetic diversity. Nat. Rev. Microbiol. 2007;5:175–186. doi: 10.1038/nrmicro1614. [DOI] [PubMed] [Google Scholar]
- 33.Alam S.B., Mahmud M., Akter R., Hasan M., Sobur A., Nazir K.H.M., Noreddin A., Rahman T., El Zowalaty M.E., Rahman M. Molecular detection of multidrug resistant Salmonella species isolated from broiler farm in Bangladesh. Pathogens. 2020;9:201. doi: 10.3390/pathogens9030201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nandi S.P., Sultana M., Hossain M.A. Prevalence and characterization of multidrug-resistant zoonotic Enterobacter spp. in poultry of Bangladesh. Foodborne Pathog. Dis. 2013;10:420–427. doi: 10.1089/fpd.2012.1388. [DOI] [PubMed] [Google Scholar]
- 35.Azad M.A.R.A., Amin R., Begum M.I.A., Fries R., Lampang K.N., Hafez H.M. Prevalence of antimicrobial resistance of Escherichia coli isolated from broiler at Rajshahi region, Bangladesh. Br. J. Biomed. Multidisc. Res. 2017;1:6–12. [Google Scholar]
- 36.Van Duin D., Paterson D.L. Multidrug-resistant bacteria in the community: Trends and lessons learned. Infect. Dis. Clin. 2016;30:377–390. doi: 10.1016/j.idc.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lu Y., Zhao H., Sun J., Liu Y., Zhou X., Beier R.C., Wu G., Hou X. Characterization of multidrug-resistant Salmonella enterica serovars Indiana and Enteritidis from chickens in Eastern China. PLoS ONE. 2014;9:e96050. doi: 10.1371/journal.pone.0096050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Routh J.A., Pringle J., Mohr M., Bidol S., Arends K., Adams-Cameron M., Hancock W.T., Kissler B., Rickert R., Folster J., et al. Nationwide outbreak of multidrug-resistant Salmonella Heidelberg infections associated with ground turkey: United States, 2011. Epidemiol. Infect. 2015;143:3227–3234. doi: 10.1017/S0950268815000497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sinwat N., Angkittitrakul S., Coulson K.F., Pilapil F.M.I.R., Meunsene D., Chuanchuen R. High prevalence and molecular characteristics of multidrug-resistant Salmonella in pigs, pork and humans in Thailand and Laos provinces. J. Med. Microbiol. 2016;65:1182–1193. doi: 10.1099/jmm.0.000339. [DOI] [PubMed] [Google Scholar]
- 40.Shecho M., Thomas N., Kemal J., Muktar Y. Cloacael carriage and multidrug resistance Escherichia coli O157: H7 from poultry farms, eastern Ethiopia. J. Vet. Med. 2017;2017:8264583. doi: 10.1155/2017/8264583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davis G.S., Waits K., Nordstrom L., Grande H., Weaver B., Papp K., Horwinski J., Koch B., Hungate B.A., Liu C.M., et al. Antibiotic-resistant Escherichia coli from retail poultry meat with different antibiotic use claims. BMC Microbiol. 2018;18:174. doi: 10.1186/s12866-018-1322-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Díaz-Jiménez D., García-Meniño I., Fernández J., García V., Mora A. Chicken and turkey meat: Consumer exposure to multidrug-resistant Enterobacteriaceae including mcr-carriers, uropathogenic E. coli and high-risk lineages such as ST131. Int. J. Food Microbiol. 2020;331:108750. doi: 10.1016/j.ijfoodmicro.2020.108750. [DOI] [PubMed] [Google Scholar]
- 43.Winsor D.K., Bloebaum A.P., Mathewson J.J. Gram-negative, aerobic, enteric pathogens among intestinal microflora of wild turkey vultures (Cathartes aura) in west central Texas. Appl. Environ. Microbiol. 1981;42:1123–1124. doi: 10.1128/AEM.42.6.1123-1124.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Toze S. PCR and the detection of microbial pathogens in water and wastewater. Water Res. 1999;33:3545–3556. doi: 10.1016/S0043-1354(99)00071-8. [DOI] [Google Scholar]
- 45.Chiu C.H., Ou J.T. Rapid identification of Salmonella serovars in feces by specific detection of virulence genes, invA and spvC, by an enrichment broth culture-multiplex PCR combination assay. J. Clin. Microbiol. 1996;34:2619–2622. doi: 10.1128/JCM.34.10.2619-2622.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Darwin K.H., Miller V.L. Molecular Basis of the Interaction of Salmonella with the Intestinal Mucosa. Clin. Microbiol. Rev. 1999;12:405–428. doi: 10.1128/CMR.12.3.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Saelinger C.A., Lewbart G.A., Christian L.S., Lemons C.L. Prevalence of Salmonella spp. in cloacal, fecal, and gastrointestinal mucosal samples from wild North American turtles. J. Am. Vet. Med. Assoc. 2006;229:266–268. doi: 10.2460/javma.229.2.266. [DOI] [PubMed] [Google Scholar]
- 48.Havelaar A.H., Kirk M.D., Torgerson P.R., Gibb H.J., Hald T., Lake R.J., Praet N., Bellinger D.C., de Silva N.R., Gargouri N., et al. World Health Organization global estimates and regional comparisons of the burden of foodborne disease in 2010. PLoS Med. 2015;12:e1001923. doi: 10.1371/journal.pmed.1001923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Simonsen G.S., Tapsall J.W., Allegranzi B., Talbot E.A., Lazzari S. The antimicrobial resistance containment and surveillance approach-a public health tool. Bull. World Health. 2004;82:928–934. [PMC free article] [PubMed] [Google Scholar]
- 50.Sobur A., Haque Z.F., Sabuj A.A., Ievy S., Rahman A.T., El Zowalaty M.E., Rahman T. Molecular detection of multidrug and colistin-resistant Escherichia coli isolated from house flies in various environmental settings. Future Microbiol. 2019;14:847–858. doi: 10.2217/fmb-2019-0053. [DOI] [PubMed] [Google Scholar]
- 51.Sobur A., Hasan M., Haque E., Mridul A.I., Noreddin A., El Zowalaty M.E., Rahman T. Molecular Detection and Antibiotyping of Multidrug-Resistant Salmonella Isolated from Houseflies in a Fish Market. Pathogens. 2019;8:191. doi: 10.3390/pathogens8040191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nahar A., Islam M.A., Sobur M.A., Hossain M.J., Binte S., Zaman M., Rahman B., Kabir S.L., Rahman M.T. Detection of tetracycline resistant E. coli and Salmonella spp. in sewage, river, pond and swimming pool in Mymensingh, Bangladesh. Afr. J. Microbiol. Res. 2018;13:382–387. [Google Scholar]
- 53.Bryan A., Shapir N., Sadowsky M.J. Frequency and distribution of tetracycline resistance genes in genetically diverse, nonselected, and nonclinical Escherichia coli strains isolated from diverse human and animal sources. Appl. Environ. Microbiol. 2004;70:2503–2507. doi: 10.1128/AEM.70.4.2503-2507.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Strahilevitz J., Jacoby G.A., Hooper D.C., Robicsek A. Plasmid-mediated quinolone resistance: A multifaceted threat. Clin. Microbiol. Rev. 2009;22:664–689. doi: 10.1128/CMR.00016-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Møller T.S., Overgaard M., Nielsen S.S., Bortolaia V., Sommer M.O., Guardabassi L., Olsen J.E. Relation between tetR and tetA expression in tetracycline resistant Escherichia coli. BMC Microbiol. 2016;16:1–8. doi: 10.1186/s12866-016-0649-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Poirel L., Stephan R., Perreten V., Nordmann P. The carbapenemase threat in the animal world: The wrong culprit. J. Antimicrob. Chemother. 2014;69:2007–2008. doi: 10.1093/jac/dku054. [DOI] [PubMed] [Google Scholar]
- 57.Tacconelli E., Carrara E., Savoldi A., Harbarth S., Mendelson M., Monnet D.L., Pulcini C., Kahlmeter G., Kluytmans J., Carmeli Y., et al. Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 2018;18:318–327. doi: 10.1016/S1473-3099(17)30753-3. [DOI] [PubMed] [Google Scholar]
- 58.Jajere S.M. A review of Salmonella enterica with particular focus on the pathogenicity and virulence factors, host specificity and antimicrobial resistance including multidrug resistance. Vet. World. 2019;12:504–521. doi: 10.14202/vetworld.2019.504-521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sobur A.M., Ievy S., Haque Z.F., Nahar A., Zaman S.B., Rahman M.T. Emergence of colistin-resistant Escherichia coli in poultry, house flies, and pond water in Mymensingh, Bangladesh. J. Adv. Vet. Anim. Res. 2019;6:50–53. doi: 10.5455/javar.2019.f311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang R., Cao W., Cerniglia C.E. PCR detection and quantitation of predominant anaerobic bacteria in human and animal fecal samples. Appl. Environ. Microbiol. 1996;62:1242–1247. doi: 10.1128/AEM.62.4.1242-1247.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fratamico P.M. Comparison of culture, polymerase chain reaction (PCR), TaqMan Salmonella, and Transia Card Salmonella assays for detection of Salmonella spp. in naturally-contaminated ground chicken, ground turkey, and ground beef. Mol. Cell. Probes. 2003;17:215–221. doi: 10.1016/S0890-8508(03)00056-2. [DOI] [PubMed] [Google Scholar]
- 62.Randall L.P., Cooles S.W., Osborn M.K., Piddock L.J., Woodward M.J. Antibiotic resistance genes, integrons and multiple antibiotic resistance in thirty-five serotypes of Salmonella enterica isolated from humans and animals in the UK. J. Antimicrob. Chemother. 2004;53:208–216. doi: 10.1093/jac/dkh070. [DOI] [PubMed] [Google Scholar]
- 63.Bayer A.W., Kirby W.M., Sherris J.C., Turck M. Antibiotic susceptibility testing by a standardized single disc method. Am. J. Clin. Pathol. 1966;45:493–496. doi: 10.1093/ajcp/45.4_ts.493. [DOI] [PubMed] [Google Scholar]
- 64.CLSI . Performance Standards for Antimicrobial Susceptibility Testing. 26th ed. Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2016. CLSI Supplement M100s. [Google Scholar]
- 65.Sweeney M.T., Lubbers B.V., Schwarz S., Watts J.L. Applying definitions for multidrug resistance, extensive drug resistance and pandrug resistance to clinically significant livestock and companion animal bacterial pathogens. J. Antimicrob. Chemother. 2018;73:1460–1463. doi: 10.1093/jac/dky043. [DOI] [PubMed] [Google Scholar]
- 66.Ashour H.M. One Health—People, Animals, and the Environment. Clin. Infect. Dis. 2014;59:1510. doi: 10.1093/cid/ciu625. [DOI] [Google Scholar]