Abstract
Objectives
To identify factors associated with the continuum of maternal, newborn and child health care in The Gambia.
Design
A secondary statistical analysis using Demographic and Health Survey conducted in 2013.
Setting
The Gambia.
Participants
1308 married women (or with a partner) whose most recent children were aged 12–23 months at the time of the survey.
Outcome measures
The main outcome was continuum of care for maternal, newborn and child health. The modified composite coverage index was calculated to express the completion level of continuum of care.
Results
The following factors were associated with the continuum of maternal, newborn and child health care: women’s autonomy in decision-making of her own healthcare (β=0.063, p=0.015), having higher educated husbands (β=0.138, p<0.001), listening to the radio at least once a week (β=0.078, p=0.006), having a child with birth order less than 5 (β=0.069, p=0.037), initiating the first antenatal care within 16 weeks of pregnancy (β=0.170, p<0.001), having been informed of signs of pregnancy complications (β=0.057, p=0.029), living in rural areas (β=−0.107, p=0.006) and having higher burden due to distance to health facility (β=−0.100, p<0.001), with an explanatory power of 15.5% (R2=0.155).
Conclusions
Efforts on future policies and programmes should focus on the concept of continuum of care considering the associated factors. In particular, more attention should be given to providing country-wide family planning and education to women, men and community members in The Gambia.
Keywords: public health, health policy, international health services
Strengths and limitations of this study.
This study analysed the level of continuum of care from pregnancy to childhood and the maternal healthcare period.
This study used a nationally representative sample to investigate factors associated with the continuum of maternal, newborn and child health (MNCH) care in The Gambia.
This study developed modified composite coverage index to measure the level of continuity of MNCH care in The Gambia.
This study did not use quality approach to measure the level of continuity of MNCH care.
The cross-sectional nature of the study does not display a causal relationship.
Introduction
Globally, maternal mortality ratio declined by 38% between 2000 and 2017,1 with an average annual decline of 2.9%. However, more efforts are needed because a reduction of 6.4% per year is required to achieve the Sustainable Development Goal (SDG) of 70 maternal deaths per 100 000 live births by 2030.2 Similarly, the number of newborn and child deaths remains high.3 In 2018, almost 7000 newborns4 and 15 000 children under-5 died every day worldwide.3
The Gambia is a low-income country, located in Western Africa. The gross national income per capita in 2018 was US$710.5 In line with global trends, The Gambia has also seen substantial improvements in maternal, newborn and child health (MNCH).6 In 2018, four or more visits to antenatal care (ANC) and postnatal care of mothers within 2 days after birth were 75.6% and 86.7%, respectively. Facility delivery was estimated at 81.5% and skilled attendant delivery at 82.7%.7 However, under-5 mortality rate was still high, at 58 per 1000 in 2018,8 which was more than double the SDG target of 25 per 1000 live births. Maternal mortality ratio also remained unacceptably high at 433 deaths per 100 000 live births, compared with 230 deaths per 100 000 live births that occurred in low/middle-income countries (LMICs) in 2013.9 In LMICs including The Gambia, most maternal mortality is due to preventable causes related to pregnancy and childbirth, which is preventable if MNCH services or necessary care is provided along the continuum of care.10
According to the study by Kerber et al and other previous studies, continuum-of-care approach emphasises access to comprehensive, integrated and continuous interventions throughout the life cycle (pregnancy, childbirth, postnatal period, infancy, childhood and maternal health period) and between places (including households and communities, outpatient and outreach services, and health facilities).11 Mothers, newborns and children are closely connected in life and in healthcare needs.12 However, mothers and children used to be considered separately in the past MNCH policies and programmes, resulting in gaps within care.12 Considering the tight inter-relationship between mothers and children along the continuum has become an effective strategy to reduce the gaps in care and will save the most lives of mothers, newborns and children.13–15
To date, a representative measurement tool for the continuum of MNCH care is not available.16 Some of the previous studies narrowed down the scope of continuum of care focusing on analysing the use of individual maternal services such as antenatal care, skilled birth attendance and postnatal care.13 16–19 Some other previous work presented the level of continuum of care using the composite coverage index (CCI) to summarise measures of coverage.20 21 The CCI is a weighted average of coverage of eight preventive and curative interventions.22 A study conducted in Lao People’s Democratic Republic modified CCI to reflect 10 maternal and child health (MCH) services.23 Another study used skilled birth attendance and antenatal care as the indicators for maternal and newborn care in the CCI.21 In this study, we modified CCI to add more MNCH care, such as postnatal services, breast feeding and polio vaccination, as elements of continuum of care. The modified CCI provides an overall estimate of the coverage of MNCH care along the continuum in The Gambia.
According to a wealth of studies, individual and family characteristics, community characteristics, socioeconomic status, baby’s characteristics and interaction with healthcare system were associated with the continuum of care.17 19 23 24 For example, mother’s age,13 14 18 marital status,16 mother’s education attainment,13 16 18 19 23 25 mother’s occupation,23 birth order of child,13 access to media,17 18 women’s decision-making,18 25 wealth index,13 14 17–19 25 number of birth,17 area of residence (urban or rural),13 16–18 distance to health facilities,23 months of first antenatal visit23 and health insurance coverage13 were shown to be the determinants of the continuum of MNCH care.
Given the importance of the continuum of care, the purpose of this study was to examine factors associated with the continuum of MNCH care in The Gambia using a modified CCI constructed for identifying the level of continuum of care. These study results provided a basis for policy recommendations.
Methods
Data source
This study used secondary data from the 2013 Gambia Demographic and Health Survey (GDHS) carried out by The Gambia Bureau of Statistics. The 2013 GDHS is a nationally representative survey of household samples and is typically conducted about every 5 years.26 The survey provides comprehensive information on the population and health of The Gambia, including MCH. The data on the selected MCH indicators were taken from the women’s questionnaire of the sixth round of Demographic and Health Survey (DHS) surveys, and the data set is available on request. Further details of methodology, sampling and questionnaires can be found in the publicly available survey report.27
Study population
The 2013 GDHS used a stratified two-stage probability-based sampling method. In the first stage of selection, 281 clusters were included using the probability proportional to size method from urban and rural strata. In the second stage, 25 households per cluster were selected through systematic sampling from a household listing. A total of 11 279 eligible women from 7009 households were selected for the survey. The survey interviewed 10 233 women aged 15–49 years from 6217 households, yielding a response rate of 91%.
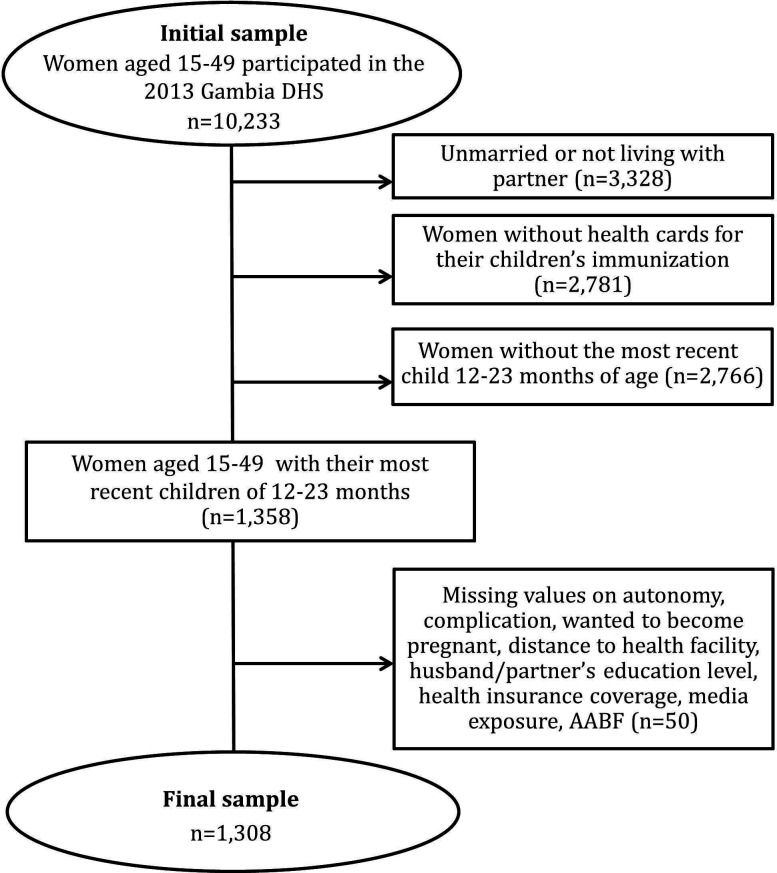
Of the 10 233 women who participated in the 2013 GDHS, 6905 (67.5%) married women (or with a partner) who had a live birth in the 2 years preceding the survey were included in the study. We selected married women (or with a partner) to identify the rate of modern contraceptive use, one of the elements of the continuum of care. To minimise information bias, 2781 women without health cards for their children’s immunisation were excluded. Since children in The Gambia are recommended to receive all four vaccinations before 12 months of age,28 2766 women with the most recent children under 12 months or above 23 months of age were excluded to estimate the child’s coverage of BCG, diphtheria–pertussis–tetanus (DPT), polio and measles vaccination. The final analytical sample for the study included 1308 married women (or with a partner) aged 15–49 years with their most recent children being 12–23 months of age at the time of the survey (figure 1).
Figure 1.
Study population selection process. AABF, age-appropriate breast feeding; DHS, Demographic and Health Survey.
Outcome measure
Measurement of continuum of care
The outcome variable indicates the level of continuity of care which was calculated using CCI. Measurement approaches to assess the level of continuum of care have not yet been defined29; however, previous studies mainly used coverage of MNCH services or care along the continuum using composite coverage metrics such as CCI, co-coverage index, coverage gap index and other various methods.29 In this study, we used the comprehensive approach to measure the level of continuity instead of focusing on the use of individual MNCH care. We applied the concept of CCI with some modifications based on Kerber et al’s definition of the continuum of care11 and on WHO’s recommended MNCH care. Spearman’s rank correlation coefficient was used to identify the correlation between the CCI and the modified CCI (Spearman’s correlation=0.916, p<0.01).
Continuum-of-care calculation
CCI reflects a composite score of coverage of essential MNCH interventions. Original CCI includes 8 interventions, whereas modified CCI in this study involves the following 11 essential MNCH interventions provided throughout the life cycle and between places.
ANC refers to four or more visits to antenatal care with a skilled provider (doctor, nurse, midwife or auxiliary nurse); TTN represents two or more doses of tetanus injections before birth; FD is facility-based (hospital, health centre, clinic or health post) delivery; SBA implies skilled birth attendant (doctor, nurse, midwife, auxiliary nurse); and PNCM indicates women who received the first health check within 2 days of delivery. Postnatal care for newborns was not involved in this index because DHS data on the postnatal indicator only provide the information of the newborns who were not delivered at the facility, but received postnatal care. We could not estimate the coverage of postnatal care for newborns who were delivered at the health facility; AABF refers to age-appropriate breast feeding. Children aged 12–23 months are recommended to continue breast feeding with appropriate complementary and solid, semisolid or soft foods.30 Therefore, women who continued to breastfeed their children at the time of the survey and fed solid, semisolid or soft foods in the 24 hours preceding the survey were considered to have completed AABF; FP indicates family planning that includes women who are currently using (or whose partners are using) modern methods of family planning at the point of the survey; BCG is Bacille de Calmette et Guérin vaccination; DPT3 indicates three doses of diphtheria–pertussis–tetanus vaccine; PL involves four doses of poliomyelitis vaccination; and MSL indicates measles vaccination.
Respondents were asked whether she or her child received each of the 11 care interventions. Then, individual answer was entered into the CCI equation as 0 (no) and 1 (yes), yielding the level of continuum of care on each study participant. The calculated index ranges from 0 to 1, where 0 indicates no intervention completed and 1 indicates completion of all the 11 essential MNCH interventions in addition to following six stages of the continuum of care: (1) pregnancy care (ANC and TTN), (2) birth care (FD and SBA), (3) postnatal care (PNCM), (4) infancy care (AABF), (5) childhood care (BCG, DPT3, PL and MSL) and (6) maternal healthcare (FP). The level of continuum of care is calculated with the following formula:
Independent variables
Building on the conceptual model adapted from the previous literature,17 19 23 24 we developed five categories of determinants influencing the continuum of MNCH. The categories included family and individual characteristics, community characteristics, socioeconomic status, baby’s characteristics and interactions with the healthcare system.
All the independent variables were represented by dummy variables. The determinants of family and individual characteristics comprised women’s age, whether the last child’s pregnancy was wanted, woman’s autonomy in decision-making of her own healthcare and health insurance coverage. Community characteristics factors included women’s geographical location— whether urban or rural—and whether the distance to health facilities is a big problem. Socioeconomic status factors were measured using women’s educational attainment, husband’s/partner’s educational attainment, wealth quintile and media exposure at least once a week. As baby’s characteristics, sex of the newborn, size of the newborn at birth and child’s birth order were selected. The determinants of interactions with the healthcare system included timing of the first antenatal check and whether the women were told about signs of pregnancy complications at the time of the last antenatal visit.
Statistical analysis
Descriptive analysis was carried out to illustrate the background characteristics of the study sample and to identify coverage of each care along the continuum of care. Simple linear regression analysis was applied to examine the unadjusted relationship between each independent variable and the continuum of care with a significance level of 0.05. Those significant variables were entered into multiple linear regression analysis to identify factors affecting the continuum of MNCH care in The Gambia. Multiple linear regression analysis was adjusted for mother’s current age. A p value <0.05 was considered as statistically significant for all analyses. All the independent variables were represented by dummy variables. The analysis was conducted using IBM SPSS V.23.
Patient and public involvement
Patient and public were not involved in the planning and design of this study.
Results
Background characteristics of the study population
Table 1 summarises the characteristics of 1308 women included in this study. Among all, 71.5% of women were aged 20–34 years. Of the study population, 87.2% wanted the child at the time of pregnancy. Women who decided their own healthcare were 70.5%, whereas women who did not participate in the decision-making process of their own healthcare were 29.5%. Women who were covered by health insurance were only 1.1% of the respondents. The majority was from rural areas (70.7%), and nearly 62.0% of women reported that distance to the health facility was not a big problem in the case where the respondent was sick.
Table 1.
Characteristics of the study population (n=1308)
| Characteristics | N | % |
| Individual and family characteristics | ||
| Woman’s current age (years) | ||
| 15–19 | 71 | 5.4 |
| 20–34 | 935 | 71.5 |
| 35–49 | 302 | 23.1 |
| Marital status | ||
| Married or have a partner | 1308 | 100 |
| Wanted to become pregnant | ||
| Yes | 1141 | 87.2 |
| No or later | 167 | 12.8 |
| Woman’s autonomy in decision-making of her own healthcare | ||
| Yes | 922 | 70.5 |
| No | 386 | 29.5 |
| Health insurance coverage | ||
| Covered by a health insurance | 15 | 1.1 |
| Not covered | 1294 | 98.9 |
| Community characteristics | ||
| Geographical classification | ||
| Rural | 925 | 70.7 |
| Urban | 383 | 29.3 |
| Distance to health facility | ||
| Big problem | 505 | 38.6 |
| Not a big problem | 803 | 61.4 |
| Socioeconomic status | ||
| Woman’s education | ||
| None | 844 | 64.5 |
| Primary and higher | 464 | 35.5 |
| Husband’s/partner’s education | ||
| None | 868 | 66.4 |
| Primary and higher | 440 | 33.6 |
| Wealth quintile | ||
| Poorest | 321 | 24.5 |
| Poor middle | 667 | 51.0 |
| Rich | 184 | 14.1 |
| Richest | 136 | 10.4 |
| Exposure to television at least once a week | ||
| Yes | 425 | 32.5 |
| No | 883 | 67.5 |
| Exposure to radio at least once a week | ||
| Yes | 702 | 53.7 |
| No | 606 | 46.3 |
| Exposure to newspaper at least once a week | ||
| Yes | 48 | 3.7 |
| No | 1260 | 96.3 |
| Baby’s characteristics | ||
| Sex of the child | ||
| Boy | 683 | 52.2 |
| Girl | 625 | 47.8 |
| Size of the child at birth | ||
| Very small/smaller than average | 280 | 21.4 |
| Average | 354 | 27.1 |
| Very large/larger than average | 674 | 51.5 |
| Birth order | ||
| 1st–4th | 839 | 64.1 |
| ≥5th | 469 | 35.9 |
| Interactions with the healthcare system | ||
| 1st antenatal care within 16 weeks of pregnancy | ||
| Yes | 842 | 64.4 |
| No | 466 | 35.6 |
| Informed of signs of pregnancy complications | ||
| Yes | 972 | 74.3 |
| No | 336 | 25.7 |
More than half of the women (64.5%) and their husbands or partners (66.4%) had no education, whereas 35.5% of the women and 33.6% of their husbands or partners had primary and higher education. Most of the respondents (75.5%) were from the poorest or poor middle quartile. The mass media exposed at least once a week to the respondents was radio (53.7%), followed by television (32.5%) and newspapers (3.7%).
The sex of about half (52.2%) of the women’s last child was boy, 27.1% of the women had an average-sized child at birth and 35.9% of the women’s last child were fifth-born or more.
Overall, 64.4% of the women had their first antenatal care visit within 16 weeks of their pregnancy, whereas the majority of the women (74.3%) were informed of signs of pregnancy complications at the time of their last antenatal visits.
MNCH care coverage and continuum-of-care achievement
Table 2 indicates the MNCH care coverage along the continuum of care. Among 1308 women, 24 (1.8%) women completed the continuum of care. Most of the women (83.2%) reported that their child aged 12–23 months completed the recommended dose for BCG, DPT, polio and measles. Among the four vaccinations, BCG coverage was almost 100%. Child immunisation showed the highest coverage, followed by AABF (81.4%), mothers’ postnatal care within 48 hours after birth (69.7%) and delivery care (54.6%). While 80.4% of women received four or more times of antenatal care, 43.7% of women received two doses of neonatal tetanus protection. Women who completed both pregnancy care were 36.9%. Only 10.0% of women or their partner used a modern method of family planning.
Table 2.
MNCH care coverage and continuum-of-care achievement (n=1308)
| Life cycle | MNCH care | N | % |
| Pregnancy | Pregnancy care | 482 | 36.9 |
| Antenatal care (received 4+ times) | 1052 | 80.4 | |
| Neonatal tetanus protection | 571 | 43.7 | |
| Birth | Delivery care | 714 | 54.6 |
| Facility-based delivery | 716 | 54.7 | |
| Skilled birth attendant at delivery | 734 | 56.1 | |
| Postnatal (mother) | Postnatal care within the first 2 days after birth | 912 | 69.7 |
| Infancy | Child immunisation | 1088 | 83.2 |
| BCG | 1304 | 99.7 | |
| DPT3 | 1188 | 90.8 | |
| Polio4 | 1249 | 95.5 | |
| Measles | 1173 | 89.7 | |
| Childhood | Age-appropriate breast feeding | 1065 | 81.4 |
| Maternal health | Current use of modern contraceptive method | 131 | 10.0 |
| Women who completed the MNCH care along the life cycle | 24 | 1.8 | |
BCG, Bacille de Calmette et Guérin vaccination; DPT3, three doses of diphtheria–pertussis–tetanus vaccine; MNCH, maternal, newborn and child health; Polio4, four doses of poliomyelitis vaccination.
Factors associated with the continuum-of-care completion
Table 3 shows the results of simple linear regression analysis. All independent variables, except mother’s current age, wanted pregnancy, sex of child and size of child at birth, were significantly associated with the continuum of care.
Table 3.
Results of simple linear regression analysis
| Independent variables | R2 | P value | |
| Individual and family characteristics | Mother’s current age | 0.003 | 0.109 |
| Wanted pregnancy | 0.000 | 0.750 | |
| Woman’s autonomy in decision-making of her own healthcare | 0.007 | 0.003 | |
| Health insurance coverage | 0.086 | 0.002 | |
| Community characteristics | Geographical classification | 0.056 | <0.001 |
| Distance to health facility | 0.039 | <0.001 | |
| Socioeconomic status | Mother’s education | 0.018 | <0.001 |
| Husband’s/partner’s education | 0.059 | <0.001 | |
| Wealth index | 0.051 | <0.001 | |
| Exposure to television at least once a week | 0.198 | <0.001 | |
| Exposure to radio at least once a week | 0.161 | <0.001 | |
| Exposure to newspaper at least once a week | 0.100 | <0.001 | |
| Baby’s characteristics | Sex of the child | 0.053 | 0.055 |
| Size of the child at birth | 0.056 | 0.126 | |
| Birth order | 0.102 | <0.001 | |
| Interactions with healthcare system | Timing of the 1st antenatal care | 0.164 | <0.001 |
| Informed of signs of pregnancy complications | 0.064 | 0.021 | |
The significant variables from the simple linear regression analysis were entered into multiple linear regression analysis to identify factors associated with the continuum-of-care completion. Table 4 presents the results of the multiple linear regression analysis, adjusted for mother’s current age with an explanatory power of 15.5% (R2=0.155). Women with autonomy in decision-making of their own healthcare (β=0.063, p=0.015), having higher educated husbands (β=0.138, p<0.001), listening to the radio at least once a week (β=0.078, p=0.006), having a child with birth order less than 5 (β=0.069, p=0.037), initiating the first antenatal visit within the first trimester of pregnancy (β=0.170, p<0.001), having been informed of signs of pregnancy complications (β=0.057, p=0.029), living in rural areas (β=−0.107, p=0.006) and having higher burden due to distance to health facility (β=−0.100, p<0.001) were significantly associated with completing all the 11 essential MNCH care interventions. However, health insurance coverage, mother’s education level, wealth quintile, and watching television and reading newspapers at least once a week were not associated with the continuum of MNCH care.
Table 4.
Results of multiple linear regression analysis adjusted for mother’s current age
| Independent variables | Adjusted* | |||
| B | SE | β | P value | |
| Woman’s autonomy in decision-making of her own healthcare | ||||
| Yes | 0.025 | 0.010 | 0.063 | 0.015 |
| No | Ref. | |||
| Health insurance coverage | ||||
| Covered by health insurance | 0.053 | 0.047 | 0.030 | 0.260 |
| Not covered | Ref. | |||
| Geographical classification | ||||
| Rural | −0.043 | 0.016 | −0.107 | 0.006 |
| Urban | Ref. | |||
| Distance to health facility | ||||
| Big problem | −0.038 | 0.010 | −0.100 | <0.001 |
| Not a big problem | Ref. | |||
| Mother’s education level | ||||
| No education | Ref. | |||
| Primary and higher | −0.012 | 0.011 | −0.032 | 0.283 |
| Husband’s/partner’s education level | ||||
| No education | Ref. | |||
| Primary and higher | 0.053 | 0.012 | 0.138 | <0.001 |
| Wealth quintile | ||||
| Poor | Ref. | |||
| Poor middle | −0.003 | 0.012 | −0.007 | 0.814 |
| Rich | 0.017 | 0.019 | 0.032 | 0.381 |
| Richest | 0.018 | 0.023 | 0.030 | 0.433 |
| Exposure to television at least once a week | ||||
| Yes | 0.018 | 0.012 | 0.046 | 0.132 |
| No | Ref. | |||
| Exposure to radio at least once a week | ||||
| Yes | 0.029 | 0.010 | 0.078 | 0.006 |
| No | Ref. | |||
| Exposure to newspaper or magazine at least once a week | ||||
| Yes | 0.017 | 0.027 | 0.018 | 0.516 |
| No | Ref. | |||
| Child’s birth order | ||||
| 1st–4th | 0.026 | 0.013 | 0.069 | 0.037 |
| ≥5th | Ref. | |||
| Timing of 1st antenatal care | ||||
| ≤16 weeks | 0.065 | 0.010 | 0.170 | <0.001 |
| >16 weeks | Ref. | |||
| Informed of signs of pregnancy complications | ||||
| Yes | 0.024 | 0.011 | 0.057 | 0.029 |
| No | Ref. | |||
R2=0.155; R2(adj)=0.145; F=14.801; p<0.001.
*Adjusted for mothers’ current age.
β, standardised beta coefficient; ANC, four or more visits to antenatal care; B, unstandardised beta coefficient.;
Discussion
Our results indicated that women’s autonomy, geographical accessibility to health facilities, husband’s education attainment, radio accessibility, child’s birth order, timing of the first antenatal care and informed of signs of pregnancy complications were significant predictors of continuum of care. This study also identified very low level of continuum of care from the pregnancy to childhood period in The Gambia. This highlights the importance of addressing determinants of MNCH care continuation and making appropriate policies to enhance the continuum of MNCH care.
Among individual and family-related factors, a positive association was detected between women’s decision-making autonomy and continuum of care. Similarly, a recent analysis based on nine countries in South Asia and sub-Saharan Africa showed that women who have received all elements of the continuum of care tended to have a high degree of decision-making autonomy.25
Furthermore, our study found that only 1.8% of Gambian women completed 11 MNCH care interventions along the continuum. Along the continuum, the lowest coverage was identified at the use of modern contraceptives. This may be due to the timing of data collection and low levels of women’s autonomy. DHS collects the percentage of currently married and sexually active unmarried women who currently use any method of contraception, also called as the contraceptive prevalence rate at the point of the survey.27 Low level of use of modern contraceptives may be due in part to the fact that data were collected after the delivery. Another possible explanation could be that of low levels of women’s autonomy. Previous studies illustrated that women’s autonomy was directly related to modern contraceptive use.31–34 For example, findings from the study in Isfahan showed that women who had higher autonomy used more efficient method of contraception and for a longer period.31 Among our study population, only 23.5% of women independently decided their own healthcare, whereas women who decided their own healthcare jointly with their husbands were 46.9%. However, under the Islamic culture in The Gambia, cultural influences such as unequal gender relations may undervalue women’s opinion.35 36 In this context, imbalance of gender power plays a critical role in the use of contraception method as reported in other studies.37 Another possible explanation for the low rate of contraceptive use may be that of inadequate and incorrect knowledge, myths and misconceptions of modern contraceptives among women as well as family members.38 These study findings emphasise the importance of national family planning programmes and interventions, providing adequate and correct knowledge of the benefits of small families. Given the fact that cultural context affects contraceptive use or discontinuation, providing a quality programme on family planning for both women and men as well as community members could be a major intervention in The Gambia.37 39 40
This study revealed that a child birth order of less than 5 positively influenced the continuum of MNCH care. In The Gambia, the fertility rate was 5.48 per woman in 2013. This was relatively higher than the average of sub-Saharan African countries, excluding high-income countries where its fertility rate was 5.06 per woman in 2013. The fertility rate per woman in sub-Saharan Africa has recently declined to 4.77, whereas the fertility rate in The Gambia has fallen to 5.28 per woman in 2017.41 However, the pace of fertility decline was slower in The Gambia than that observed in sub-Saharan Africa. Reflecting these results, the government of The Gambia recently joined the Family Planning 2020 in March 2019, expressing the government’s commitment to increasing accessibility to family planning.42 A study by Bongaarts illustrated that sub-Saharan Africa has a higher fertility rate than other continents.43 High fertility rates are related to high desired family size. The ideal family size is higher in sub-Saharan Africa, but so are the unmet needs. Previous studies have demonstrated that the higher the child’s birth orders, the lower the MNCH service or care.44–46 This might explain that women tend to think that they do not need to receive healthcare services for higher order births because they have childbearing experience.
Although women and husbands’ education level would be expected to influence continuum of MNCH care achievement, this study demonstrated that only husband’s or partner’s educational attainment was associated with the continuum of MNCH care. This differs from the pattern usually seen in many previous studies where women’s education level is an important determinant for the utilisation of MCH care services.47 48 In addition, a study of cross-sectional data conducted in 31 LMICs revealed that the odds of having a skilled attendant at delivery and attending four or more antenatal care visits were almost 5 times and 2.89 times, respectively, higher for women who completed primary education compared with those less educated.49 The findings of this study illustrated that a husband or partner with a primary education and higher positively affected completion of MNCH care.
The study findings suggest that listening to the radio at least once a week positively affects continuum of care. Delivering carefully developed messages over the radio to uneducated men and women living in rural areas might be more effective than delivering them through television or newspapers.
Consistent with previous studies in Haiti,50 Indonesia51 and Nigeria,52 women who were living in rural areas and women with higher burden due to distance to health facilities had a negative association with continuum-of-care completion. This is likely due to not having enough travel time, lack of timely transportation and costs involved.53 A survey conducted in The Gambia illustrated that a donkey cart as a means of transport may be affordable but can be slow, whereas taxis are fast but may be expensive and mostly unavailable. In addition, a qualitative study conducted in rural Gambia demonstrated that women’s work burden is one of the barriers to access to healthcare. Gambian women are exhausted physically and mentally because of the heavy household chores and farming from the moment they wake up until they go to sleep.36 These findings imply that increasing accessibility to health services and care should become a priority in rural areas.
Our study had several limitations. First, this study did not use quality approach to measure the level of continuity of MNCH care. For example, completion of four or more antenatal care visits did not indicate that a woman received all the recommended components of antenatal care. Further research should develop a measurement of continuum of care focusing more on the dimension of quality of care. Second, it was impossible to include timing of the postnatal care of newborns as an element of continuum of care. GDHS only provided data about whether newborns received the postnatal check either before discharge or after discharge without indicating the specific timing of the postnatal care. Future studies using recent DHS are encouraged to include timing of the postnatal care of newborns in the modified CCI, since the recent phase of DHS provides those data. Third, the data were collected based on women’s self-reports. This may lead to recall bias, information bias or social desirability bias. To minimise the effects of this limitation, we selected study population who had a live birth in the 2 years preceding the survey and who had child’s immunisation card to increase the accuracy of the information. Finally, the cross-sectional nature of the study does not display a causal relationship. Prospective studies are necessary to build on this research in future.
Despite these limitations, to our knowledge, this is the first study to explore the level of continuum of MNCH care in The Gambia, as well as to investigate factors associated with the continuum of MNCH care in The Gambia. Our study is unique as continuum of care in this study indicates continuum of MNCH care throughout the life cycle (pregnancy, birth, postpartum, infancy, childhood and maternal health period) and between places of caregiving (households and communities, outpatient and outreach services, and clinical care settings) based on Kerber et al’s definition of continuum of care.11 The developed CCI makes it easy to interpret and can be used to monitor the progress of the level of continuum of care.
In conclusion, our study identified factors associated with the continuum of MNCH in The Gambia. Women’s autonomy, husband’s education attainment, radio accessibility, child’s birth order, timing of the first ANC, geographical classification and distance to health facility were significantly associated with the continuum of MNCH care. Along the continuum, the lowest coverage was identified at the use of modern contraceptives. Our study suggests that efforts on future policies and programmes should focus on the concept of continuum of care considering the associated factors, and in particular, more attention should be given to providing country-wide family planning and education to women, men and community members in The Gambia.
Supplementary Material
Footnotes
Contributors: OJ conceptualised the data; OJ, CJW and KKH developed the methods; OJ developed the software; and all authors validated the data. OJ conducted formal analysis, all authors conducted the investigation, OJ curated the data, OJ prepared the original draft and all authors reviewed and edited the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Ethics approval: This study used secondary data from the DHS, which are available on request. Approval on the request was obtained from the DHS. This study was reviewed by Korea University Institutional Review Board and exempted from ethical approval (KUIRB-2019-0285-01).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. The data on the selected maternal and child health indicators were taken from the women’s questionnaire of the sixth round of DHS surveys, and the data set is available on request after registering as a user (https://dhsprogram.com/data/available-datasets.cfm).
References
- 1.World Health Oragnization Maternal mortality. Available: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality [Accessed 4 Dec 2019].
- 2.United Nations Children’s Fund Maternal mortality. Available: https://data.unicef.org/topic/maternal-health/maternal-mortality/ [Accessed 4 Dec 2019].
- 3.United Nations Inter-agency Group for Child Mortality Estimation (UN IGME) Levels & Trends in Child Mortality Report 2019. New York: UN IGME, 2019. [Google Scholar]
- 4.World Health Oragnization Newborns: reducing mortality. Available: https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality [Accessed 4 Dec 2019].
- 5.World Bank Data GNI per capita, Atlas method (current US$) - Gambia, The. Available: https://data.worldbank.org/indicator/NY.GNP.PCAP.CD?locations=GM [Accessed 24 Mar 2020].
- 6.World Health Oragnization Gambia: who statistical profile. Available: http://www.who.int/gho/countries/gmb.pdf [Accessed 2 Dec 2019].
- 7.The Gambia Bureau of Statistics The Gambia multiple indicator cluster survey 2018, survey findings report. Banjul, The Gambia, 2019. [Google Scholar]
- 8.World Bank Data Mortality rate, under-5 (per 1,000 live births). Available: https://data.worldbank.org/indicator/SH.DYN.MORT [Accessed 10 Dec 2019].
- 9.UNICEF, UNFPA WHO Trends in maternal mortality: 1990 to 2013 2014.
- 10.Bhutta ZA, Das JK, Bahl R, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet 2014;384:347–70. 10.1016/S0140-6736(14)60792-3 [DOI] [PubMed] [Google Scholar]
- 11.Kerber KJ, de Graft-Johnson JE, Bhutta ZA, et al. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet 2007;370:1358–69. 10.1016/S0140-6736(07)61578-5 [DOI] [PubMed] [Google Scholar]
- 12.The Partnership for Maternal NaCH Opportunities for Africa’s newborns: Practical data, policy and programmatic support for newborn care in Africa In: Graft-Johnson J, Kerber K, Tinker A, eds The continuum of care for maternal, newborn and child health, 2006. [Google Scholar]
- 13.Wang W, Hong R. Levels and determinants of continuum of care for maternal and newborn health in Cambodia-evidence from a population-based survey. BMC Pregnancy Childbirth 2015;15:62. 10.1186/s12884-015-0497-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohan D, LeFevre AE, George A, et al. Analysis of dropout across the continuum of maternal health care in Tanzania: findings from a cross-sectional household survey. Health Policy Plan 2017;32:791–9. 10.1093/heapol/czx005 [DOI] [PubMed] [Google Scholar]
- 15.Lawn JE, Tinker A, Munjanja SP, et al. Where is maternal and child health now? Lancet 2006;368:1474–7. 10.1016/S0140-6736(06)69387-2 [DOI] [PubMed] [Google Scholar]
- 16.Yeji F, Shibanuma A, Oduro A, et al. Continuum of care in a maternal, newborn and child health program in Ghana: low completion rate and multiple obstacle factors. PLoS One 2015;10:e0142849. 10.1371/journal.pone.0142849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chalise B, Chalise M, Bista B, et al. Correlates of continuum of maternal health services among Nepalese women: evidence from Nepal multiple indicator cluster survey. PLoS One 2019;14:e0215613. 10.1371/journal.pone.0215613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iqbal S, Maqsood S, Zakar R, et al. Continuum of care in maternal, newborn and child health in Pakistan: analysis of trends and determinants from 2006 to 2012. BMC Health Serv Res 2017;17:189. 10.1186/s12913-017-2111-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shibanuma A, Yeji F, Okawa S, et al. The coverage of continuum of care in maternal, newborn and child health: a cross-sectional study of woman-child pairs in Ghana. BMJ Glob Health 2018;3:e000786. 10.1136/bmjgh-2018-000786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wehrmeister FC, Restrepo-Mendez M-C, Franca GV, et al. Summary indices for monitoring universal coverage in maternal and child health care. Bull World Health Organ 2016;94:903–12. 10.2471/BLT.16.173138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Countdown 2008 Equity Analysis Group, Boerma JT, Bryce J, et al. Mind the gap: equity and trends in coverage of maternal, newborn, and child health services in 54 countdown countries. Lancet 2008;371:1259–67. 10.1016/S0140-6736(08)60560-7 [DOI] [PubMed] [Google Scholar]
- 22.Barros AJD, Victora CG. Measuring coverage in MNCH: determining and interpreting inequalities in coverage of maternal, newborn, and child health interventions. PLoS Med 2013;10:e1001390 10.1371/journal.pmed.1001390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sakuma S, Yasuoka J, Phongluxa K, et al. Determinants of continuum of care for maternal, newborn, and child health services in rural Khammouane, Lao PDR. PLoS One 2019;14:e0215635. 10.1371/journal.pone.0215635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Owili PO, Muga MA, Chou Y-J, et al. Associations in the continuum of care for maternal, newborn and child health: a population-based study of 12 sub-Saharan Africa countries. BMC Public Health 2016;16:414. 10.1186/s12889-016-3075-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh K, Story WT, Moran AC. Assessing the continuum of care pathway for maternal health in South Asia and sub-Saharan Africa. Matern Child Health J 2016;20:281–9. 10.1007/s10995-015-1827-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The Demographic and Health Survey Program DHS overview. Available: https://dhsprogram.com/What-We-Do/Survey-Types/DHS.cfm [Accessed 10 Dec 2019].
- 27.The Gambia Bureau of Statistics (GBOS), ICF International The Gambia demographic and health survey 2013. Banjul, The Gambia, and Rockville, Maryland, USA, 2014. [Google Scholar]
- 28.Scott S, Odutola A, Mackenzie G, et al. Coverage and timing of children's vaccination: an evaluation of the expanded programme on immunisation in the Gambia. PLoS One 2014;9:e107280. 10.1371/journal.pone.0107280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mothupi MC, Knight L, Tabana H. Measurement approaches in continuum of care for maternal health: a critical interpretive synthesis of evidence from LMICs and its implications for the South African context. BMC Health Serv Res 2018;18:539. 10.1186/s12913-018-3278-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization, UNICEF, USAID Indicators for assessing infant and young child feeding practices, Part II Measurement, 2010: 81. [Google Scholar]
- 31.Kohan S, Talebian F, Ehsanpour S. Association between women's autonomy and family planning outcome in couples residing in Isfahan. Iran J Nurs Midwifery Res 2014;19:451–5. [PMC free article] [PubMed] [Google Scholar]
- 32.Hogan DP, Berhanu B, Hailemariam A. Household organization, women's autonomy, and contraceptive behavior in southern Ethiopia. Stud Fam Plann 1999;30:302–14. 10.1111/j.1728-4465.1999.t01-2-.x [DOI] [PubMed] [Google Scholar]
- 33.Sano Y, Antabe R, Atuoye KN, et al. Married women's autonomy and post-delivery modern contraceptive use in the Democratic Republic of Congo. BMC Womens Health 2018;18:49. 10.1186/s12905-018-0540-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DeRose LF, Ezeh AC. Decision-Making patterns and contraceptive use: evidence from Uganda. Popul Res Policy Rev 2010;29:423–39. 10.1007/s11113-009-9151-8 [DOI] [Google Scholar]
- 35.Ganle JK. Why Muslim women in Northern Ghana do not use skilled maternal healthcare services at health facilities: a qualitative study. BMC Int Health Hum Rights 2015;15:10. 10.1186/s12914-015-0048-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lowe M, Chen D-R, Huang S-L. Social and cultural factors affecting maternal health in rural Gambia: an exploratory qualitative study. PLoS One 2016;11:e0163653. 10.1371/journal.pone.0163653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kriel Y, Milford C, Cordero J, et al. Male partner influence on family planning and contraceptive use: perspectives from community members and healthcare providers in KwaZulu-Natal, South Africa. Reprod Health 2019;16:89. 10.1186/s12978-019-0749-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gueye A, Speizer IS, Corroon M, et al. Belief in family planning myths at the individual and community levels and modern contraceptive use in urban Africa. Int Perspect Sex Reprod Health 2015;41:191–9. 10.1363/intsexrephea.41.4.0191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levandowski BA, Kalilani-Phiri L, Kachale F, et al. Investigating social consequences of unwanted pregnancy and unsafe abortion in Malawi: the role of stigma. Int J Gynaecol Obstet 2012;118 Suppl 2:S167–71. 10.1016/S0020-7292(12)60017-4 [DOI] [PubMed] [Google Scholar]
- 40.Pranitha M. Promoting male involvement in reproductive health. Agenda: Empowering Women for Gender Equity 2000;44:11. [Google Scholar]
- 41.World Bank Data Fertility rate, total (births per woman). Available: https://data.worldbank.org/indicator/SP.DYN.TFRT.IN [Accessed 6 Dec 2019].
- 42.Family planning 2020: Gambia commitment maker since 2019. Available: https://www.familyplanning2020.org/gambia [Accessed Dec 2019].
- 43.Bongaarts J. Can family planning programs reduce high desired family size in sub-Saharan Africa? Int Perspect Sex Reprod Health 2011;37:209–16. 10.1363/3720911 [DOI] [PubMed] [Google Scholar]
- 44.Srivastava A, Mahmood S, Mishra P, et al. Correlates of maternal health care utilization in rohilkhand region, India. Ann Med Health Sci Res 2014;4:417–25. 10.4103/2141-9248.133471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Somefun OD, Ibisomi L. Determinants of postnatal care non-utilization among women in Nigeria. BMC Res Notes 2016;9:21. 10.1186/s13104-015-1823-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bell J, Curtis SL, Alayon S. Trends in delivery care in six counries. DHS Analytical Studies No. 7. Calverton, Maryland, USA: ORC Macro, 2003. [Google Scholar]
- 47.Elo IT. Utilization of maternal health-care services in Peru: the role of women's education. Health Transit Rev 1992;2:49–69. [PubMed] [Google Scholar]
- 48.Rai RK, Singh PK, Singh L. Utilization of maternal health care services among married adolescent women: insights from the Nigeria demographic and health survey, 2008. Womens Health Issues 2012;22:e407–14. 10.1016/j.whi.2012.05.001 [DOI] [PubMed] [Google Scholar]
- 49.Ahmed S, Creanga AA, Gillespie DG, et al. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS One 2010;5:e11190. 10.1371/journal.pone.0011190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.King-Schultz L, Jones-Webb R. Multi-method approach to evaluate inequities in prenatal care access in Haiti. J Health Care Poor Underserved 2008;19:248–57. 10.1353/hpu.2008.0015 [DOI] [PubMed] [Google Scholar]
- 51.Titaley CR, Hunter CL, Heywood P, et al. Why don't some women attend antenatal and postnatal care services?: a qualitative study of community members' perspectives in Garut, Sukabumi and Ciamis districts of West Java Province, Indonesia. BMC Pregnancy Childbirth 2010;10:61. 10.1186/1471-2393-10-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stock R. Distance and the utilization of health facilities in rural Nigeria. Soc Sci Med 1983;17:563–70. 10.1016/0277-9536(83)90298-8 [DOI] [PubMed] [Google Scholar]
- 53.Lerberg PM, Sundby J, Jammeh A, et al. Barriers to skilled birth attendance: a survey among mothers in rural Gambia. Afr J Reprod Health 2014;18:35–43. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.