Abstract
Nontuberculous mycobacteria (NTM) and many fungal species (spp.) are commonly associated with opportunistic infections (OPIs) in immunocompromised individuals. Moreover, occurrence of concomitant infection by NTM (mainly spp. of Mycobacterium avium complex and Mycobacterium abscessus complex) and fungal spp. (mainly, Aspergillus fumigatus, Histoplasma capsulatum and Cryptococcus neoformans) is very challenging and is associated with poor patient prognosis. The most frequent clinical symptoms for coinfection and infection by single agents (fungi or NTM) are similar. For this reason, the accurate identification of the aetiological agent(s) is crucial to select the best treatment approach. Despite the significance of this topic it has not been sufficiently addressed in the literature. This review aims at summarizing case reports and studies on NTM and fungi coinfection during the last 20 years. In addition, it briefly characterizes OPIs and coinfection, describes key features of opportunistic pathogens (e.g., NTM and fungi) and human host predisposing conditions to OPIs onset and outcome. The review could interest a wide spectrum of audiences, including medical doctors and scientists, to improve awareness of these infections, leading to early identification in clinical settings and increasing research in the field. Improved diagnosis and availability of therapeutic options might contribute to improve the prognosis of patients’ survival.
Keywords: Nontuberculous mycobacteria (NTM), coinfection, Aspergillus, Histoplasma capsulatum, Cryptococcus neoformans, HIV/AIDS, immunosuppression, opportunistic infections
1. Introduction
Infectious diseases are still a major burden worldwide, causing critical outbreaks such as corona virus disease (COVID-19) and being a persistent cause of mortality, especially in low-income countries. Malaria, HIV/AIDS (Human Immunodeficiency Virus/ Acquired Immune Deficiency Syndrome), lower respiratory tract infections including tuberculosis and diarrheal diseases, account for one-eighth of the total deaths worldwide. In developed countries, cardiovascular diseases are the major cause of death, but infectious diseases are still a huge challenge. In this settings, infectious diseases contribute significantly to morbidity and increased health costs, mainly through chronic infectious and healthcare-associated diseases [1].
Nontuberculous mycobacteria (NTM) disease is generally non-notifiable [2,3], which hinders the correct assessment of its significance [4]. However, it is consensual that an ongoing growth in incidence and prevalence has been observed [5]. Given the lack of mandatory reporting, data are limited to case reviews and research studies, thus incidence and prevalence may be far greater than estimated. To overcome this issue, further prevalence studies and implementation of systematic tracking of NTM diseases using a reporting system are advisable. Despite this drawback, there is an increased body of knowledge on NTM due to the effort of scientific and medical communities, as well as organized study groups such as the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Study Group for Mycobacterial Infection [6] and NTM- network [7].
Fungal infections are common in humans, and the majority of fungi causing disease are opportunistic pathogens [8]. The scope of current knowledge on fungi is very extensive and continuously updated, not only with basic science findings but also with data collected in clinical setting (e.g., mapping occurrence, prevalence, spread and treatment of fungal disease). This information is summarized by working groups established within the International Society for Medical Mycology [9] as well as the ESCMID study group for fungi and fungal diseases [10]. In spite of this, interaction between fungi and bacteria lacks mandatory reporting, published data being collected on a voluntary basis. Human pathogenic fungi are classified into two groups: the commensals (Candida spp.) and the environmental pathogens (Cryptococcus neoformans, Cryptococcus gattii, Aspergillus fumigatus, and thermally dimorphic fungi) [11]. Fungi have frequently caused diseases in immunocompromised patients with HIV, cancer, diabetes and patients treated with immunosuppressive drugs [12,13,14,15,16,17]. In a separate category are healthy individuals with flaws in the immune system due to age (children and elderly), antibiotic treatment or pregnancy [18,19,20,21]. In addition to common diseases, fungi can cause very serious life-threatening infections [14,16,22,23].
Two main concerns are underlined regarding fungal infections: (i) increased rates of multiresistant fungi and (ii) strong potential to colonize host and participate in polymicrobial infections, mainly with bacteria.
Although a great deal of information is available concerning fungi and NTM alone, only little is known about coparticipation of NTM and fungi in human infections. Here, we attempt to fill the gaps, summarizing the clinical significance of coinfection by two groups of opportunistic pathogens (NTM and fungi) from different kingdoms that are able to cooperate and significantly affect the disease course and treatment.
2. Opportunistic Infections and Coinfection
Generally, an opportunistic infection occurs when loss of established innate or adaptive immune responses allow none-strictly pathogenic organisms to infect a host. These infections are a major cause of morbidity and mortality among immunocompromised individuals. The type and severity of the immune defect determines the profile of the potential aetiological agent and the opportunistic infection [24]. Taking into account an infectious trait of NTM and major fungal pathogens, as well as the already mentioned definition of OPIs, there are two different points of view. While Mycobacterium is associated with host colonization and/or infection, some fungal spp. are members of the common human microbiome and others are environmental pathogens. For example, Candida albicans colonizes over 50% of the population without any symptoms. It can be present in the skin, oral cavity, intestine, upper respiratory tract and female reproductive tract [25,26,27,28,29,30]. However, under optimal circumstances, this yeast is able to switch from a safe commensal to a dangerous pathogen able to cause infections whose treatment is very challenging [31]. A distinct situation is the case of airborne microorganisms, such as filamentous fungi (Aspergillus, Rhizopus, Mucor, etc.) and other already mentioned environmental pathogens (H. capsulatum, C. neoformans) colonizing the host via the upper respiratory tract [14,16,17].
Coinfection occurs when pathogens (e.g., viruses, bacteria, fungi, parasites) co-occur within an individual [32], most often with a chronic infection [33]. Parasite coinfections [34] and HIV/Mycobacterium tuberculosis coinfection [35,36] are huge burdens for human health. Accurate knowledge of coinfection prevalence is missing, but it is estimated that at least one-sixth of the human population is affected by this condition. In addition, a negative effect of coinfection on human health is more frequent than no effect or positive effect [32]. The fact that individuals with poor health are more prone to coinfection might contribute to this outcome. Other contributing factors are synergistic relations between pathogens by modulation of the host immune system, resource competition, interfering with the performance of diagnostic tests, drug-drug interaction and emergence of drug resistance [32,37,38]. Coinfection can dramatically modify infection dynamics through ecological mechanisms such as convalescence and disease-induced mortality, and an effort has been made to develop models to evaluate the risk assessment [33,39].
Although in this review, the focus is on coinfection by opportunistic pathogens from the bacteria kingdom (NTM) and fungi kingdom, there are many reports of coinfection by different representatives of viruses, bacteria, fungi and parasites. Among them, coinfection in HIV-patients is very frequent. For example, yeasts of the genus Candida or the fungus Pneumocystis jirovecii occur frequently and can cause life-threatening pneumonia in these patients [22,23]. HIV infection is also strongly associated with a higher prevalence of chronic human papillomavirus, resulting in increased risk for anal cancer [40]. In HIV-Leishmania coinfected patients, visceral leishmaniosis can accelerate disease, decreasing the likelihood of patient survival [41]. C. neoformans and H. capsulatum are the only agents that have been isolated, particularly from immunocompromised individuals [14,16]. Their participation in coinfection is very rare, but Nunez and colleagues reported simultaneous infections in an HIV-negative 69-year-old man with chronic obstructive pulmonary disease and type II diabetes mellitus [42]. Invasive pulmonary aspergillosis is a fungal disease strongly associated with immunocompromised patients [43]. Invasive pulmonary aspergillosis was reported in immunocompetent patients severely infected either with influenza B or influenza A H1N1 virus [44]. A. fumigatus and Pseudomonas aeruginosa coinfection in patients with cystic fibrosis is often observed [45]. Concomitant aspergillosis and mucormycosis is very rare, but this combined disease was described in a 17-year-old girl with subsequent treatment of a recurrent glioma [46]. Coinfections by multiple NTM species have been reported mainly as case reports. Mycobacterium malmoense and Mycobacterium chimaera in a kidney transplanted patient [47], pleural effusion by Mycobacterium fortuitum and Mycobacterium mageritense [48], mixed pulmonary infection by Mycobacterium avium or Mycobacterium intracellulare (MAC) and M. abscessus or Mycobacterium massiliense (MABC) [49,50] are examples of case reports. Furthermore, it has been recently described that coinfection by multiple NTM spp. could exacerbate the symptoms of pulmonary lung disease by these pathogens [51]. Finally, coronavirus infection together with influenza A virus or different bacteria, were summarized in the work of Cheng-Lai and colleagues [52]. The difficulties with treatment of all above mentioned coinfections underline the fact that the majority of them resulted in mortality.
3. The Aetiological Agents: NTM and Fungi
NTM and fungi are ubiquitous environmental microorganisms potentially pathogenic to humans. NTM are a heterogeneous group formed by almost 200 species [53], with only two strict pathogens: Mycobacterium marinum and Mycobacterium ulcerans, which are responsible for the fish tank granuloma and buruli ulcer, respectively [54,55,56]. Although the majority are nonpathogenic to humans, NTM are recognized aetiological agents of OPIs, in particular species belonging to the MAC and the MABC. NTM infections are phenotypically diverse, manifesting themselves as a large spectrum of diseases affecting nearly all organs [57]. Being ubiquitous in nature, NTM share with humans and animals a wide variety of habitats and niches leading to high rates of human–pathogen contact [58].
The majority of fungi associated with human diseases are able to switch from a transient environmental contaminant or a saprophytic life-style to a parasitic life-style [11,59,60]. Generally, the yeast C. albicans and the mold A. fumigatus are the most frequent pathogens causing invasive mycoses, candidaemia being the most common infection [61,62]. Koehler and colleagues provided a systematic review (from January 2000 to February 2019) on candidaemia morbidity and mortality in Europe [63]. From a retrospective study, they extrapolated from approximately 79 cases of candidaemia per day why 29 patients out of 25 may be fatal at day 30. Environmental pathogen C. neoformans is associated with invasive infections of the central nervous system (CNS), mainly in HIV/AIDS patients but, like C. gattii, it can also cause pulmonary cryptococcosis [64]. CNS infection caused by molds (A. fumigatus) and other aspergilli typically register mortality rates between 50–100%. Aspergillosis usually occurs after manifestation of pulmonary disease in immunocompromised and organ transplant patients [17]. Aspergilli rarely cause fungaemia, with the exception of Fusarium spp. [65,66].
The transmission of NTMs can occur through an environmental source or clinical settings to the patient [67]. Person to person transmission has been suggested for M. abscessus but has not been fully demonstrated [68,69,70]. This ubiquity and exposure poses an enormous challenge for clinicians, since isolation of NTM from a clinical sample may only indicate a transient or persistent colonization, or an infection [71]. Aspergillus, Cryptococcus and Histoplasma, as typical environmental fungi, are not transmissible between humans. Human infection occurs by inhalation of spores or the yeast form via the respiratory tract [11]. Therefore, ventilation or air conditioning with intensive aerosol production facilitates these pathogens spreading [72]. In contrast to the mentioned fungal spp., as well as to NTM, certain Candida spp. can be transmitted by direct contact with medical staff or other patients, making it difficult to determine if an infection has an endogenous or exogenous origin [60,73].
Despite being globally disseminated, NTM spp. exhibit uneven geographic distribution, which can be attributed to the environmental nature of the genus. With the exception of Japan, MAC is the most common species in Asia, in most of western countries (European Union (EU) included) and African countries. In most western countries and in the EU, Mycobacterium gordonae and Mycobacterium xenopi [74], together with M. intracellulare and the rapidly growing M. fortuitum, are the next most common NTM spp. [3]. In the United States of America (USA), Mycobacterium kansasii and M. abscessus follow MAC spp. [5], and in Asia, M. intracellulare is more common than M. avium among MAC spp, with the known exception of northern Japan, in which species from MABC are the second most frequent [75]. Common species in Africa are Mycobacterium sherrisii, and species related to occupational or geographic incidence, such as M. kansasii in mining workers and Mycobacteriu lentiflavum in Zambia, respectively [75]. The relatively organized distribution portrayed above is punctuated by several divergences reported in the literature [76,77,78]. The uneven geographical spread of NTM represents a challenge in terms of pathogenesis knowledge, diffusion and infectious disease management requiring a wide array of distinct therapeutic approaches. NTM growth rate is another factor that influences the therapeutic scheme. NTM are divided into rapidly growing mycobacteria (RGM, e.g., M. fortuitum, MABC: Mycobacterium chelonae and M. abscessus), and slowly growing mycobacteria (SGM, e.g., MAC, M. xenopi and M. kansasii) exhibiting differential epidemiology of infection. Usually, RGM infections are mostly cutaneous and osteoarticular, whereas SGM infections are located in lungs and lymph nodes [79], implicating a direct correlation between growth rate and virulence.
Despite the global distribution of H. capsulatum, its variety capsulatum is preferentially endemic in the soils of specific American regions, sub-Saharan Africa and South-East Asia [80,81]. C. neoformans, H. capsulatum, and A. fumigatus are common environmental pathogens distributed worldwide [11]. Another example of yeasts with a worldwide distribution is Candida. It has been already mentioned that C. albicans is the predominant spp. However, an increased proportion of Candida spp. other than C. albicans is the current trend, as illustrated by candidaemia cases by non-C. albicans spp. observed worldwide [63,82]. Candidaemia is strongly associated with patient catheterization (49.7%), with C. parapsilosis being the most common causative agent of candidiasis in this population (58%) [83]. In USA, C. albicans remains the leading aetiological agent of invasive candidiasis, followed by C. glabrata [84]. In EU, the situation in adults is similar, with the prevalence of C. albicans highest (>50%), followed by C. glabrata (13–22%) then by C. parapsilosis (about 15%) depending on the hospital or region monitored [66,85]. In children and teenagers, C. albicans (>50%) is also the predominant yeast, followed by C. parapsilosis (28%). A higher proportion of candidemia caused by C. albicans was observed among newborns (60.2%), with highest rates of C. parapsilosis being observed among infants (42%) [86].
4. The Human Host: Predisposing Conditions for NTM, Fungal Infections and Coinfections
Some predisposing conditions of human hosts to develop NTM or fungal disease are similar, but some of them differ with respect to fungal spp. In general, NTM and invasive fungal infections mostly occur in immunocompromised patients. For instance, histoplasmosis or cryptococcosis are strongly associated with acquired immunodeficiency [87,88]. Nevertheless, predisposing nonimmunological conditions can significantly contribute to the development of infections caused by Candida spp., namely diabetes, pregnancy and age, but also burn-patients and healthcare associated infections [15,18,21,89,90]. Although NTM can cause infection at a wide variety of body sites (e.g., skin, soft tissues and lymphatic nodes), lung infections are the most frequent. Patients with structural lung diseases such as chronic obstructive pulmonary disease (COPD), bronchiectasis, pneumoconiosis, prior tuberculosis and pulmonary alveolar proteinosis, are more prone to NTM infections [5]. Rheumatoid arthritis, cystic fibrosis (CF), gastroesophageal motility disorders and other chronic diseases with pulmonary manifestations including lung malignancies, are other factors that can predispose an individual to NTM pulmonary infections [5,91,92]. Pre-existing pulmonary diseases are also a predisposing factor for opportunistic pulmonary infections by Aspergillus spp. the severity of the clinic manifestations being conditioned by the host immune status [93]. The existence of underlying pulmonary disease and immune disorders favor infections by both opportunistic pathogens fungi and NTM [71].
Patients with immune suppression, either primary or acquired, are more susceptible to NTM infections, namely to disseminated NTM infections [94]. Disseminated infections by MAC in AIDS patients brought NTM to the spotlight back in the 1980s [95]. Until the introduction of antiretroviral therapy (ART) in the 1990s, OPIs by mycobacteria and fungi, among other pathogens, were a major cause of mortality and morbidity in HIV-infected patients. In order to overcome this problem, treatment guidelines for OPIs were implemented and further updated over the years [96,97].
Primary immune suppression, such as Mendelian susceptibility to mycobacterial disease mediated by mutations in IFN-γ and IL-12 receptors, deformities in the STAT1, IKKKG, GATA2 genes and production of autoantibodies to IFN-γ (interfering with STAT1 phosphorylation and IL-12 production) [98] increase the risk of disseminated NTM [68,94], Cocccidioides and Histoplasma infections [99]. Additionally, a STAT1-gain-of-function has been described to cause Th17 deficiency resulting in chronic mucocutaneous candidiasis (CMC) [100]. Similarly, impairment of STAT3 signaling affecting IL-6, IL-21 and IL-23 pathways, and defective generation of Th17 responses, are associated with Hyper-IgE Syndrome. Patients with this syndrome are vulnerable to CMC, but also to Histoplasma, Coccidioides, and Cryptococcus [101,102,103]. Caspase domain containing protein 9 (CARD9) has a key role in regulation, being a central regulator of innate immunity expressed in neutrophils, macrophages and dendritic cells. The correlation between autosomal recessive CARD9 deficiency and susceptibility to invasive fungal infections, including Candida spp. or A. fumigatus, has been described [104], but this deficiency is also associated with CMC [105]. Chronic pulmonary aspergillosis was observed to be a risk in the variants of genes coding for cytokines (IL1B, IL1RN, IL15), pattern recognition receptors of TLR1, CLEC7A (Dectin-1), DENND1B and VEGFA genes [106,107].
Acquired immunosuppression induced by drugs such as corticosteroids, chemotherapeutics to treat cancer, immunosuppressive drugs to prevent rejection after organ transplant, TNF-α antagonists and other biologic chemotherapeutics to treat inflammatory conditions, are other factors that could promote OPIs [68,71,94]. Macrophages play a key role in mycobacterial pathogenesis. Mycobacteria-infected macrophages trigger CD4+ T-helper cell pathways through IL-12 and IFN-γ that activate macrophages promoting pathogen clearance [108]. This explains why low CD4+ counts in HIV-patients (a determinant for initiation of ART) and the presence of circulating anti-IFN-γ promote OPIs by NTM. On the other hand, the proinflammatory cytokine, TNF-α, plays a key role in granuloma formation and maintenance, controlling mycobacteria spread ([109,110] for recent review on host immune response to NTM). A similar scenario was observed for histoplasmosis, with milder cases of the disease being reported in patients with cell-mediated immunodeficiency treated with TNF-α inhibitors [111]. TNF-α, being a proinflammatory cytokine, stimulates the production of other cytokines such as IL-2 and IL-12, important for the host immune response. TNF-α stimulates IL-12 and IFN-γ production, promoting a Th- mediated response to C. neoformans lung infection [112]. In Candida biofilms, resistance to phagocytosis was associated with a modified cytokine profile, especially by TNF-α downregulation [113]. This observation was confirmed in a study with patients manifesting recurrent vulvovaginal candidiasis, in which TNF-α production triggered by C. albicans hyphae was significantly higher compared to the control group [114]. Fungal cell wall components play a crucial role in the interaction with host cells. The β-1,3 –glucan, a basal component of the fungal cell wall, is specifically recognized by a pattern recognition-receptor named Dectin-1. This cell wall component plays an important role in the adaptive immune response to A. fumigatus infection mediated by increased production of CXCL1, CXCL2, and TNF-α by bone marrow-derived macrophages [115].
5. Coinfection by NTM and Fungi
Concomitant isolation of mycobacteria and fungi from patients’ respiratory samples is a complex situation that could lead to misdiagnosis and inadequate therapy. The majority of reports concerning concomitant NTM and fungal infections, during mainly the last 20 years, is presented in Table 1 although ancient reports are also quoted in this section. First, as previously described in this manuscript, being opportunistic pathogens, isolation of NTM and fungi does not necessarily indicate an infection, a colonization scenario being also possible. This duality is present in the literature reports on NTM and fungi spp. isolation in patients’ samples. The case reports describe infection cases [116,117,118,119,120,121,122,123,124,125,126], but for several prospective and retrospective studies either it is not clear, or both infection and colonization are present [71,120,127,128,129,130,131,132]. There is evidence that coinfection by fungal and mycobacterial spp. worsens the prognosis of patients with lung disease, an increase in morbidity and mortality being observed for both M. tuberculosis and NTM [127,128,133,134]. For patients with pulmonary tuberculosis, A. fumigatus, Aspergillus niger, H. capsulatum, and C. neoformans are the main aetiological agents of infection [129]. Although for coinfection with NTM, all the previously mentioned fungi were identified, Aspergillus spp. being predominant and other fungi such as Talaromyces marneffei, and Candida spp. also described (Table 1).
Table 1.
NTM and fungal coinfection.
| Underlying Diseases * | Aetiological Agents | Reference | Observations | |
|---|---|---|---|---|
| NTM | Fungi | |||
| Immunosuppression (steroids treatment) | MAC | A. niger | [117] | Case report. |
| HIV infection | MAC | Cryptococcus | [118] | Case report. |
| Cancer | MAC | Aspergillus sp. | [119] | Case report. |
| Chronic pulmonary infection | MAC | Aspergillus sp. | [120] | Case report. |
| Multiple diseases (oral and colon cancer, hematologic malignancies, connective tissue disease, diabetes, corticosteroid immunosuppression) | M. kansasii | T. marneffei** | [121] | Case report. |
| Autoimmune disease (anti IFN-γ ab) | M. abscessus | Cryptococcus sp. | [122] | Case report of triple infection. |
| AIDS (Kaposi sarcoma) | M. avium intracellulare | C. neoformans | [123] | Case report. |
| Pulmonary MAC disease | MAC (M. avium and M. intracellulare) |
Aspergillus spp. (A. fumigatus and A. niger) |
[135] | Chronic necrotizing pulmonary aspergillosis (CNPA) as a complication of pulmonary MAC disease. |
| AIDS | M. intracellulare | T. marneffei | [124] | Case report. |
| AIDS | M. avium | H. capsulatum | [154] | Case report. |
| Pneumonia | M. monacense | C. glabrata | [125] | Case report of M. monacense was isolated from blood whereas C. glabrata and K. pneumoniae were isolate from bronchoalveolar lavage fluid. |
| Not reported | M. chelonae | S. apiospermum | [126] | Case report in an immunocompetent patient. |
| anti-IFN-γ ab | M. intermedium | T. marneffei | [143] | Case report. |
| Bronchiectasis, anti-IFN-γ ab | M. fortuitum | Aspergillus sp. | [144] | Case report. |
| Alcoholics, COPD | M. avium, M. xenopi | Aspergillus sp. | [142] | Case report. |
| Miscellaneous conditions (previous M. xenopi infection, bronchectasia, cancer) | M. xenopi | Aspergillus sp. | [157] | Case report. |
| AIDS | MAC | H. capsulatum | [151] | Case report.Disseminated Histoplasma and MAC with recurrence of Pneumocystis carinii pneumonia. |
| AIDS | MAC | H. capsulatum | [152] | Case report of disseminated infection (E. coli bacteremia). |
| AIDS | NTM (probably M. avium-M. intracellulare) |
H. capsulatum | [153] | Autopsy Case Report. |
| Bronchiestasis | MAC | C. albicans, A. fumigatus | [137] | |
| Several including MAC pulmonary infection, COPD, bronchiestasis, autoimmune disease, rheumatoid arthritis, corticosteroids use. | MAC | Aspergillus sp. | [138] | Patients with pulmonary MAC disease frequently had chronic coinfection with MSSA, P. aeruginosa and Aspergillus. |
| Lung disease, corticosteroid use | MAC | A. fumigatus | [71] | Retrospective monocentric study. |
| HIV infection | Not specified | Cryptococcus | [131] | Prospective study. |
| Several including COPD and cancer | M. avium and M. intracellulare (most frequent) M. abscessus and M. gordonae | Aspergillus sp. | [139] | Retrospective study. |
| Pulmonary disease (e.g., tuberculosis, COPD) and steroid treatment | MAC and MABC | Aspergillus spp. (A fumigatus, A niger, A. terreus, A. flavus) | [132] | Retrospective study. Only the group infected with NTM that developed chronic pulmonary aspergillosis (CPA) was considered. |
| Non-cystic fibrosis bronchiectasis with different etiologies, immunosuppression and MAC disease | MAC | Aspergillus sp. | [128] | Retrospective study. |
| Pulmonary MAC disease and several comorbidities (rheumatoid arthritis, steroid use) | MAC | A. fumigatus | [127] | Retrospective cohort study. |
| AIDS | MAC | H. capsulatum | [136] | Multicenter Study. |
| AIDS | NTM | H. capsulatum | [155] | Case report. |
| HIV infection | M. sherrisii | H. capsulatum | [156] | Case report. |
| COPD | M. avium | A. fumigatus | [130] | Review including case report. |
Search performed in PubMed database (https://pubmed.ncbi.nlm.nih.gov) using the terms coinfection/ co-infection, immunosuppressed, nontuberculous mycobacteria and fungi. Alternatively, the name of specific NTM and fungi were used as keywords being the search focused on the last 20 years. Ab (antibodies), AIDS (acquired immune deficiency syndrome), HIV (human immunodeficiency virus), MAC (M. avium complex), COPD (chronic obstructive pulmonary disease), MSSA (methicillin susceptible Staphylococcus aureus), CPA (chronic pulmonary aspergillosis). * Clinical conditions predisposing to NTM infection or likely to affect the immune status causing immunosuppression. ** Previously known as Penicillium marneffei.
Retrospective and prospective studies, mainly monocentric, have been designed to answer different questions related to NTM/ fungi coinfection. Providing evidence that these opportunistic pathogens could be isolated from sputum is either the most frequent, or a starting point for others [71,127,128,130,131,132,135,136,137,138,139]. Comparing the results from different studies is not straightforward due to differences in study designs and studied populations. For instance, Samayoa and colleagues aimed at evaluating the incidence and mortality of tuberculosis, histoplasmosis and cryptococcosis in HIV patients, with the identification of NTM and fungi coinfection as a side result [131]. An attempt to identify risk factors for coinfection in patients with specific clinical conditions was made [132,138,139]. COPD, pulmonary M. intracellulare disease and systemic corticosteroid use were identified as main risk factors for coinfection with Aspergillus [138]. Although colonization of pre-existing pulmonary lesions (cavities) by fungi, namely Aspergillus spp., is well-documented [130,140,141,142], NTM-fungi coinfection is rare [71,137,140] and the clinical relevance of its coisolation is species-dependent. Isolation of nonfumigatus Aspergillus strains (e.g., A. niger, Aspergillus terreus, Aspergillus flavus) from respiratory samples was most often associated with colonization [127]. In cystic fibrosis patients A. fumigatus and Scedosporium sp. are regarded as threats.
M. monacense, M. kansasii, M. xenopi, M. intermedium and M. fortuitum were the non-MAC or non-MABC NTM spp. responsible for coinfection with fungi in immunosuppressed patients. Coinfection of M. intermedium and M. fortuitum with T. marneffei and Aspergillus spp., respectively, were reported in patients with high titers of anti-IFN-γ antibodies [143,144].
A severe case of pneumonia, with isolation of Candida glabrata among other microorganisms from bronchoalveolar lavage fluid (BALF), and M. monacense from hemoculture, was reported by Yuan and colleagues [125]. M. monacense, an NTM was newly identified in 2006 [145], with few reports of isolation from human samples and clinical significance not clearly understood. This last feature is shared with C. glabrata in which isolation from BALF was transitory suggesting that in this case cross-contamination, transient infection or colonization are plausible scenarios [125]. The relevance of Candida spp. is still unclear [146] despite frequent reports of oral candidiasis in AIDS patients with disseminated infections [147,148]. The under-valorization of Candida isolation from respiratory samples was illustrated in a case report with concomitant isolation of M. kansasii from sputum and the prescription of a therapeutic scheme directed exclusively to MNT [149].
MAC (M. avium and M. intracellulare) and MABC (M. abscessus and M. massiliense) were considered more prone to cause infection, whereas M. chelonae, M. gordonae and M. fortuitum were more likely to be regarded as colonizers [71]. Curiously, a coinfection by M. chelonae and Scedosporium apiospermum was reported in an immunocompetent individual [126]. The patient had a history of diabetes (a predisposing condition for NTM infection) and hyperlipidemia controlled by medication and, after a skin antibiotic test as part of a prechirurgical procedure, presented skin lesions compatible with an infectious process. The two opportunistic pathogens were isolated, but it was not clear how the patient was infected. All the other case reports summarized in Table 1 occurred in patients with at least one predisposing condition for NTM infection. Coinfection by M. avium and A. fumigatus was described in a 65-year-old female with previously diagnosed COPD, productive cough, fatigue and weight loss for three months [130].
In the past, other opportunistic fungal infections started by being neglected and then included in the definition of a clinical situation. This was the case of histoplasmosis that only in 1985 was taken into account for the definition of AIDS by the Centers for Diseases Control and Prevention (CDC) [150]. Curiously, all but one of the H. capsulatum-NTM coinfections reported in Table 1 are cases of disseminated infections in AIDS patients, M. avium being the predominant NTM [136,151,152,153,154,155] and M. sherrisii the other NTM [156]. In Table 1, several cases of coinfection by MAC and H. capsulatum are presented, whereas other pathogens such as E.coli [152], herpes virus and Pneumocystis jirovecii [153] were isolated. In two case reports of non-HIV patients, in addition to NTM-fungi coinfection either cytomegalovirus (CMV) or varicella zoster virus were involved [119,122]. Triple coinfections with CMV, MAC and Aspergillus, or varicella zoster virus (VZV), M. abscessus and Cryptococcus, were reported in immunosuppressed patients by cancer or autoimmune disease with IFN-γ antibodies production, respectively [122]. The virulence of the NTM and the imbalance of the host immune system certainly played a role in this outcome.
6. Treatment: Major Challenges and Future Perspectives
NTMs’ susceptibility to standard antituberculosis (TB) drugs displays significant heterogeneity, standard anti-TB drug regimens being ineffective on NTM disease treatment [158]. Anti-NTM regimens are long (at least 18 months), and a 12 months period with sputum-negative results is required to confirm the cure [159,160]. Sputum-conversion, from a positive to negative finding of bacteria, is often difficult to achieve in NTM cases, especially for infection with macrolide-resistant NTM spp. [161]. Despite the existence of specific guidelines, based on the nature of infecting mycobacteria and requiring spp. identification, treatment of NTM disease is mostly empirical and not entirely successful [161]. The treatment of NTM diseases usually involves the use of macrolides and injectable aminoglycosides. Resection surgery of affected organ(s) in the case of patients that do not respond to antibiotic based treatments, is also an option [162].
Drug susceptibility tests (DSTs) for NTM are challenging and controversial because of inconsistency between in vitro results and clinical outcomes [161]. Macrolides are an exception exhibiting a good correlation between in vitro susceptibility results and clinical response. For this reason, macrolides are the pillar of current NTM infection treatment protocols [163,164], clarithromycin or azithromycin being the usual options [165]. For patients with nonsevere MAC-pulmonary disease, the recommended initial therapy consists of a clarithromycin or azithromycin, ethambutol (ETB) and rifampicin (RIF) regimen. In the case of severe conditions, injectable amikacin or streptomycin is advised [159,160]. For clarithromycin-resistant MAC infections a regimen including RIF, ETB, either isoniazid (INH) or a quinolone, and an injectable aminoglycoside should be adopted [160].
The treatment of M. abscessus lung disease faces significant challenges due to intrinsic antibiotic resistance [164], oral macrolides combined with two parenteral drugs being the medication of choice [161]. M. massiliense, one of the three subspecies of MABC, harbors a partial erm41 gene deletion preventing inducible macrolide resistance and leading to higher rates of successful treatment with macrolide-based antibiotic regimens compared to infections by M. abscessus (functional erm41 gene) [166,167]. Therefore, the correct identification of these subspecies, and precise diagnosis, are crucial for the treatment of infected patients [166,167].
M. kansasii has similar disease/ pathology presentation to pulmonary TB, a regimen with RIF, ETB, INH being recommended for drug-sensitive M. kansasii [159]. Alternatively, BTS (2017) recommends INH combined with pyridoxine, as an alternative to macrolides [160]. A three-drug regimen is recommended for rifampin-resistant strains including azithromycin, ETB and a fluoroquinolone [159].
Pulmonary disease due to M. malmoense is a challenge to treat [159]. The use of INH, RIF, ETB with and without quinolones and macrolides [159] is recommended. However, the BTS guidelines recommend a minimum three-drug regimen including RIF, ETB and a macrolide as a daily treatment, in the case of nonsevere disease, and the use of additional injectable drugs, such as amikacin or streptomycin, for severe cases [160].
In individuals with M. xenopi pulmonary disease, improved outcomes may be achieved using a four-drug antibiotic regimen comprising RIF, ETB and a macrolide (clarithromycin or azithromycin), with either a quinolone or INH. For severe NTM diseases, injectable or nebulized amikacin is added to the above regimen for up to three months [160].
In severely disseminated or recalcitrant disease, and in cases of macrolide-resistant MAC, second-line drugs are extremely important. Aminoglycosides (e.g., amikacin or streptomycin) are most often used in such cases [5]. Fluoroquinolones, in addition to having significant activity against M. kansasii, play a crucial role in cases of RIF-resistant M. kansasii [168]. Clofazimine has also shown favorable activity against pulmonary disease [169]. Linezolid has been used with success in the treatment of skin and soft tissue diseases caused by RGM M. chelonae and M. abscessus.
Fungal infections can be treated with antifungal compounds from several groups, but the selection of the appropriate drug depends on fungal species, type of infection and, in the case of concomitant infection, possible interferences has to be assumed. Taking into account information from Table 1 on distribution of fungal spp. participating in coinfection with NTM, amphotericin B and azoles, namely itraconazole and voriconazole, are the most frequently used drugs for treatment. Amphotericin B is a polyene antibiotic binding to ergosterol, the main sterol of fungal membranes. This interaction causes disruption of the cytoplasmic membrane through the formation of ion channels leading to leakage of monovalent protons and cytoplasmic contents. Additionally, it promotes reactive oxygen species production leading to oxygen depletion [170,171]. Amphotericin B in lipid formulations is preferred over amphotericin B deoxycholate, as it is more pleasant to patients and provides better delivery to organs such as lungs, liver, and spleen [172,173]. Azoles interfere with ergosterol biosynthesis through binding to the cytochrome P450-associated enzyme 14-α-demethylase that converts lanosterol to ergosterol [172,174]. The antifungal drug 5-fluorocytosine is an inhibitor of nucleic acid synthesis [175], being used only in combination with the azole derivative fluconazole in the treatment of cryptococcosis. Amphotericin B, its lipid formulations, and fluconazole are other options for monotherapy [176,177]. NTM/ fungal coinfection is not easy to treat, as amphotericin B causes a wide spectrum of adverse effects including reversible nephrotoxicity and, similarly to azoles, an interference with human cholesterol pathway was observed, including mammalian CYP 450 enzymes, resulting in abnormal profiles of liver enzymes [178]. Although better tolerated, fluconazole is not recommended for treatment of C. glabrata, Candida krusei, and Aspergillus spp. infections due to residual or nonexistent activity. Therefore, other azole derivatives, namely itraconazole and voriconazole, are used in the therapy of pulmonary aspergillosis [122]. Severe histoplasmosis cases requiring patient hospitalization are treated with liposomal amphotericin B and therapy is usually changed to itraconazole after one to two weeks. For nonlife-threatening histoplasmosis cases, itraconazole is the drug of choice [179]. The next groups of antifungal agents are echinocandins, produced by fungi as secondary metabolites. Currently, caspofungin, micafungin and anidulafungin are on the market, being effective against invasive Candida infections, and are reserve drugs for infections by Aspergillus spp. in monotherapy regimens when amphotericin B is not well tolerated [180,181]. Echinocandins block function of β-(1,3)-D-glucan synthase, the key enzyme in fungal cell wall synthesis, and are inefficient against the capsulated C. neoformans [182]. Echinocandins can be also used in combination with azoles and amphotericin B [183].
In the case of coinfection by fungi and NTM, the same drugs are used for treatment. Next, treatments used in coinfection cases will be mentioned in more detail. In a patient with steroid-treated sarcoidosis a coinfection by A. niger and MAC was described. Liposomal amphotericin B was selected for aspergillosis treatment but the patient prognosis was poor [117]. In another case of coinfection by M. avium and A. fumigatus, antifungal itraconazole and antibacillar RIF were administered, but a drug interaction was observed, and RIF was suspended. Later on, itraconazole was replaced by voriconazole, an improvement in patient condition being observed only after six months treatment. The observed drug-drug interaction supports the combination of RIF with voriconazole instead of itraconazole. The analysis of other case reports summarized in Table 1 shows that amphotericin B and/or new triazole derivatives are the drugs of choice to treat concomitant invasive aspergillosis and NTM infection [119]. In the already mentioned case of a 53-year-old man with combined infection of Cryptococcus, M. abscessus, and VZV [122], amphotericin B together with fluconazole was selected to treat cryptococcosis in combination with amikacin, imipenem, azithromycin and levofloxacin for NTM, and intravenous acyclovir for VZV [122]. In another coinfection case by C. glabrata, M. monocense and other bacteria, voriconazole was administered together with cefoperazone, sulbactam and linezolid, an improvement in the patient’s conditions being observed after 10-days therapy [125]. In a previously mentioned report by Basso and colleagues, the treatment of a patient with HIV infection and histoplasmosis was described [154]. The regimen was complex including several antifungal drugs over time (intravenous amphotericin B deoxycholate, itraconazole, itraconazole), antiretroviral (tenofovir, lamivudine, efavirenz) and antibacillar drugs (sulfamethoxazole-trimethoprim, clarithromycin, ETB, streptomycin and levofloxacin). The likelihood of drug-drug interaction with occurrence of adverse drug effects increases in such regimens when the patient takes multiple drugs (polypharmacy) [184]. In the case of NTM-fungi coinfection in immunocompromised patients, other factors such as the immune status of the patient, existence of background diseases (e.g., diabetes) and the interaction with other compounds such as anticancer drugs, has to be considered in order to select a successful therapy.
Because NTM diseases require long treatment periods, often leading to severe secondary effects and often disappointing clinical outcomes, there is an urgent demand to discover and develop new, more efficacious anti-NTM conventional drugs [158] and to explore alternative approaches. Several new drugs currently in the drug–discovery pipeline might improve the treatment of NTM diseases, offering additional choices and new drug combination options [158]. For example, bedaquiline, in addition to being promising against several species of RGM and SGM NTMs, may also have potential clinical applications in patients with MAC or MABC lung disease [185,186]. Nevertheless, the repurposing of conventional drugs is also a promising alternative, e.g., chloroquine and primaquine with activity against M. avium [187,188]. Tests conducted in mice models with M. avium and M. abscessus showed promising results for clofazimine administered by inhalation [189]. The same option has been developed for pulmonary aspergillosis, where aerosolized delivery of liposomal amphotericin B, voriconazole or posaconazole is applicable [190,191]. Antimicrobial peptides exhibit a broad-spectrum of antimicrobial activity against bacteria, viruses, parasites and fungi, and could be alternatives for the treatment of mycobacterial infections [192]. Other alternatives include a phage therapy with the use of bacteriophages [193] and host-directed therapies (HDT), which might improve the clinical outcome of NTM therapy and/or reduce the duration of treatment [161]. Natural approaches are also gaining consideration in overcoming antimicrobial resistance in NTMs, especially compounds from plants and venoms [194]. Another alternative are mycogenic metal nanoparticles produced by filamentous fungi with antimicrobial and anti-inflammatory activity [195]. However, conventional therapy is still the most effective to treat immunocompromised patients coinfected with multiple infectious agents.
7. Conclusions
This review summarizes information on concomitant infection by NTM, represented mainly by, but not restricted to MAC spp., and pathogenic fungi. Members of MABC, mainly the RGM M. abscessus is gaining growing relevance due to intrinsic antibiotic resistance and recently proposed human to human transmission. A panoply of other RGM (e.g., M. fortuitum, M. chelonae, M. monassence) and SGM (e.g., M. kansasii, M. xenopi, M. gordonae, M. sherrisii) have been associated with coinfection.
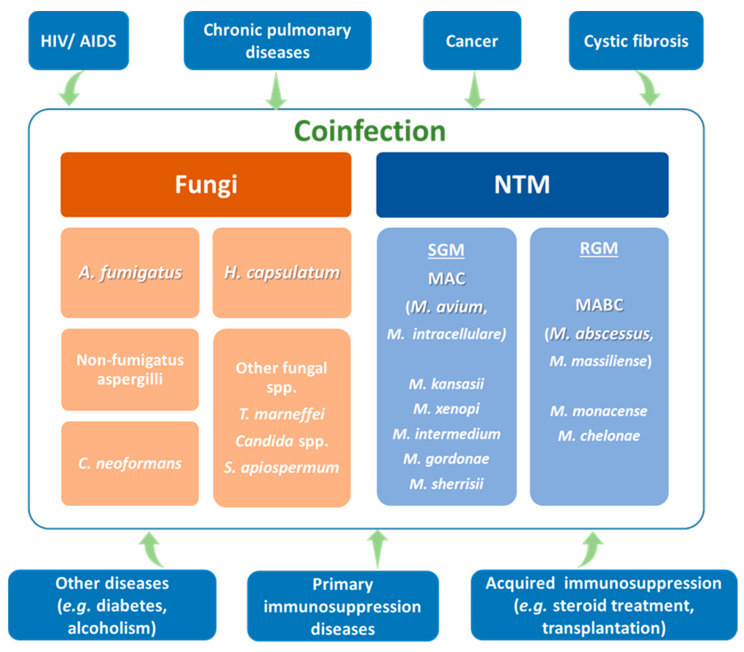
Figure 1 provides a short summary from literature reports listed in Table 1. Taking into account information from this table, A. fumigatus, together with nonfumigatus spp., identified Aspergilli and H. capsulatum as the major aetiological agents observed in coinfection with NTM. Fewer reports for C. neoformans, T. marneffei and Candida spp. were found, suggesting that they play a minor role in those infections. This representation of fungal spp. confirms that air-transmitted fungi named as environmental pathogens play a key role in coinfection with NTM in pulmonary infections. The huge diversity of pathogens involved makes the diagnostic and implementation of effective therapeutics with the currently available chemotherapeutic options quite challenging. This scenario is worsened by the poor immune status of the patients, polypharmacy leading, most likely, to drug-drug interaction, and the appearance of more or less serious side effects. The prognosis of such patients is usually uncertain. However, a prediction of possible complications, taking into account the nature of the patient’s original disease, or an early evaluation of symptoms and correct identification of infectious agents, improves the prognosis of patient’s survival.
Figure 1.
Schematic representation of the most relevant nontuberculous mycobacteria (NTM) and fungal spp. participating in coinfection, and their relation to factors affecting host health status. Rapidly growing mycobacteria (RGM), slowly growing mycobacteria (SGM), MAC (M. avium complex), MABC (M. abscessus complex).
Acknowledgments
We thank the agencies mentioned in the funding section for financial support.
Author Contributions
Conceptualization, L.J. and H.B.; writing—review and editing, L.J., H.B. and I.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Portuguese Fundação para a Ciência e a Tecnologia and by the Slovak Research and Development Agency under contract SK-PT-18-0006 as a part of the Bilateral Cooperation Program (2019–2021), APVV-15-0347,and by the grant VEGA 1/0537/19 from the Ministry of Education, Science, Research, and the Sport of the Slovak Republic.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO The Top 10 Causes of Death. [(accessed on 24 September 2020)]; Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
- 2.Daniel-Wayman S., Ricotta E., Prevots D.R., Adjemian J. Epidemiology of Nontuberculous Mycobacteriosis. Semin. Respir. Crit. Care Med. 2018;39:325–335. doi: 10.1055/s-0038-1651491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Der Werf M.J., Kodmon C., Katalinić-Janković V., Kummik T., Soini H., Richter E., Papaventsis D., Tortoli E., Perrin M., Van Soolingen D., et al. Inventory study of non-tuberculous mycobacteria in the European Union. BMC Infect. Dis. 2014;14:62. doi: 10.1186/1471-2334-14-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aksamit T.R., Philley J.V., Griffith D.E. Nontuberculous mycobacterial (NTM) lung disease: The top ten essentials. Respir. Med. 2014;108:417–425. doi: 10.1016/j.rmed.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 5.Griffith D.E., Aksamit T., Brown-Elliott B.A., Catanzaro A., Daley C., Gordin F., Holland S.M., Horsburgh R., Huitt G., Iademarco M.F., et al. An Official ATS/IDSA Statement: Diagnosis, Treatment, and Prevention of Nontuberculous Mycobacterial Diseases. Am. J. Respir. Crit. Care Med. 2007;175:367–416. doi: 10.1164/rccm.200604-571ST. [DOI] [PubMed] [Google Scholar]
- 6.ESCMID: ESGMYC. [(accessed on 25 September 2020)]; Available online: https://www.escmid.org/research_projects/study_groups/study_groups_g_n/mycobacterial_infection/
- 7.NTM-NET. [(accessed on 25 September 2020)]; Available online: http://www.ntm-net.org/
- 8.Richardson M. Opportunistic and pathogenic fungi. J. Antimicrob. Chemother. 1991;28:1–11. doi: 10.1093/jac/28.suppl_A.1. [DOI] [PubMed] [Google Scholar]
- 9.Working Groups: ISHAM. [(accessed on 25 September 2020)]; Available online: https://www.isham.org/working-groups.
- 10.ESCMID: Mission & Objectives. [(accessed on 25 September 2020)]; Available online: https://www.escmid.org/research_projects/study_groups/study_groups_a_f/fungal_infection/mission_objectives/
- 11.Reedy J.L., Bastidas R.J., Heitman J. The Virulence of Human Pathogenic Fungi: Notes from the South of France. Cell Host Microbe. 2007;2:77–83. doi: 10.1016/j.chom.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Muskett H., Shahin J., Eyres G., Harvey S., Rowan K.M., Harrison D. Risk factors for invasive fungal disease in critically ill adult patients: A systematic review. Crit. Care. 2011;15:R287. doi: 10.1186/cc10574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dekhuijzen P.R., Batsiou M., Bjermer L., Bosnic-Anticevich S., Chrystyn H., Papi A., Rodríguez-Roisin R., Fletcher M., Wood L., Cifra A., et al. Incidence of oral thrush in patients with COPD prescribed inhaled corticosteroids: Effect of drug, dose, and device. Respir. Med. 2016;120:54–63. doi: 10.1016/j.rmed.2016.09.015. [DOI] [PubMed] [Google Scholar]
- 14.Ferreira G.D.S.A., Watanabe A.L.C., Trevizoli N.D.C., Jorge F.M.F., De Camposa P.B., Couto C.D.F., De Lima L.V., Raupp D.R.L. Colonic Infection by Histoplasma capsulatum in a Liver Transplant Patient: A Case Report. Transplant. Proc. 2020;52:1413–1416. doi: 10.1016/j.transproceed.2020.01.071. [DOI] [PubMed] [Google Scholar]
- 15.Lim S.M.S., Sinnollareddy M., Sime F.B. Challenges in Antifungal Therapy in Diabetes Mellitus. J. Clin. Med. 2020;9:2878. doi: 10.3390/jcm9092878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mann S., Tobolowsky F., Purohit S., Henao-Martínez A., Bajrovic V., Ramanan P., Wolfel E., Khazanie P., Barron M., Madinger N., et al. Cryptococcal pericarditis in a heart transplant recipient. Transpl. Infect. Dis. 2020:e13366. doi: 10.1111/tid.13366. [DOI] [PubMed] [Google Scholar]
- 17.Zarei F., Hashemi S.J., Salehi M., Mahmoudi S., Zibafar E., Ahmadinejad Z., Foroushani A.R., Ardi P., Ghazvini R.D. Molecular characterization of fungi causing colonization and infection in organ transplant recipients: A one-year prospective study. Curr. Med. Mycol. 2020;6:30–35. doi: 10.18502/cmm.6.1.2505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang Y.-L., Hospitals T., Hsieh L.-Y., Wang A.-H., Lo H.-J. Characterization of Candida Species from Different Populations in Taiwan. Mycopathologia. 2011;172:131–139. doi: 10.1007/s11046-011-9408-8. [DOI] [PubMed] [Google Scholar]
- 19.Vainionpää A., Tuomi J., Kantola S., Anttonen V. Neonatal thrush of newborns: Oral candidiasis? Clin. Exp. Dent. Res. 2019;5:580–582. doi: 10.1002/cre2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xiao J., Fogarty C.T., Wu T., Alkhers N., Zeng Y., Thomas M., Youssef M., Wang L., Cowen L., Abdelsalam H., et al. Oral health and Candida carriage in socioeconomically disadvantaged US pregnant women. BMC Pregnancy Childbirth. 2019;19:1–13. doi: 10.1186/s12884-019-2618-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waikhom S.D., Afeke I., Kwawu G.S., Mbroh H.K., Osei G.Y., Louis B., Deku J.G., Kasu E.S., Mensah P., Agede C.Y., et al. Prevalence of vulvovaginal candidiasis among pregnant women in the Ho municipality, Ghana: Species identification and antifungal susceptibility of Candida isolates. BMC Pregnancy Childbirth. 2020;20:1–14. doi: 10.1186/s12884-020-02963-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pang W., Shang P., Li Q., Xu J., Bi L., Zhong J., Pei X. Prevalence of Opportunistic Infections and Causes of Death among Hospitalized HIV-Infected Patients in Sichuan, China. Tohoku J. Exp. Med. 2018;244:231–242. doi: 10.1620/tjem.244.231. [DOI] [PubMed] [Google Scholar]
- 23.Fauchier T., Hasseine L., Gari-Toussaint M., Casanova V., Marty P.M., Pomares C. Detection of Pneumocystis jirovecii by Quantitative PCR To Differentiate Colonization and Pneumonia in Immunocompromised HIV-Positive and HIV-Negative Patients. J. Clin. Microbiol. 2016;54:1487–1495. doi: 10.1128/JCM.03174-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.José R.J., Brown J.S. Opportunistic bacterial, viral and fungal infections of the lung. Medicine. 2016;44:378–383. doi: 10.1016/j.mpmed.2016.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sobel J. Vaginal Infections in Adult Women. Med. Clin. N. Am. 1990;74:1573–1602. doi: 10.1016/S0025-7125(16)30496-5. [DOI] [PubMed] [Google Scholar]
- 26.Meersseman W., Lagrou K., Spriet I., Maertens J., Verbeken E., Peetermans W.E., Van Wijngaerden E. Significance of the isolation of Candida species from airway samples in critically ill patients: A prospective, autopsy study. Intensiv. Care Med. 2009;35:1526–1531. doi: 10.1007/s00134-009-1482-8. [DOI] [PubMed] [Google Scholar]
- 27.Drell T., Lillsaar T., Tummeleht L., Simm J., Aaspõllu A., Väin E., Saarma I., Salumets A., Donders G.G.G., Metsis M. Characterization of the Vaginal Micro- and Mycobiome in Asymptomatic Reproductive-Age Estonian Women. PLoS ONE. 2013;8:e54379. doi: 10.1371/journal.pone.0054379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garnacho-Montero J., Olaechea P., Alvarez-Lerma F., Alvarez-Rocha L., Blanquer J., Galván B., Rodriguez A., Zaragoza R., Aguado J.-M., Mensa J., et al. Epidemiology, diagnosis and treatment of fungal respiratory infections in the critically ill patient. Rev. Esp. Quimioter. 2013;26:173–188. [PubMed] [Google Scholar]
- 29.Neville B.A., D’Enfert C., Bougnoux M.-E. Candida albicanscommensalism in the gastrointestinal tract. FEMS Yeast Res. 2015;15:15. doi: 10.1093/femsyr/fov081. [DOI] [PubMed] [Google Scholar]
- 30.Bertolini M., Dongari-Bagtzoglou A. The Relationship of Candida albicans with the Oral Bacterial Microbiome in Health and Disease. Adv. Exp. Med. Biol. 2019:69–78. doi: 10.1007/978-3-030-28524-1_6. [DOI] [PubMed] [Google Scholar]
- 31.Gow N.A.R., Hube B. Importance of the Candida albicans cell wall during commensalism and infection. Curr. Opin. Microbiol. 2012;15:406–412. doi: 10.1016/j.mib.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 32.Griffiths E.C., Pedersen A.B., Fenton A., Petchey O.L. The nature and consequences of coinfection in humans. J. Infect. 2011;63:200–206. doi: 10.1016/j.jinf.2011.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gorsich E., Etienne R.S., Medlock J., Beechler B.R., Spaan J.M., Spaan R.S., Ezenwa V.O., Jolles A.E. Opposite outcomes of coinfection at individual and population scales. Proc. Natl. Acad. Sci. USA. 2018;115:7545–7550. doi: 10.1073/pnas.1801095115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Petney T.N., Andrews R.H. Multiparasite communities in animals and humans: Frequency, structure and pathogenic significance. Int. J. Parasitol. 1998;28:377–393. doi: 10.1016/S0020-7519(97)00189-6. [DOI] [PubMed] [Google Scholar]
- 35.Canetti D., Riccardi N., Martini M., Villa S., Di Biagio A., Codecasa L., Castagna A., Barberis I., Gazzaniga V., Besozzi G. HIV and Tuberculosis: The Paradox of Dual Illnesses and the Challenges of Their Fighting in the History. Volume 122. Churchill Livingstone; London, UK: 2020. [DOI] [PubMed] [Google Scholar]
- 36.Sharan R., Bucşan A.N., Ganatra S., Paiardini M., Mohan M., Mehra S., Khader S.A., Kaushal D. Chronic Immune Activation in TB/HIV Co-Infection. Elsevier Ltd.; Amsterdam, The Netherlands: 2020. [Google Scholar]
- 37.Birger R., Kouyos R.D., Cohen T., Griffiths E.C., Huijben S., Mina M.J., Volkova V., Grenfell B., Metcalf C.J.E. The potential impact of coinfection on antimicrobial chemotherapy and drug resistance. Trends Microbiol. 2015;23:537–544. doi: 10.1016/j.tim.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McArdle A.J., Turkova A., Cunnington A.J. When do co-infections matter? Curr. Opin. Infect. Dis. 2018;31:209–215. doi: 10.1097/QCO.0000000000000447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang X.-S., Cao K.-F. The Impact of Coinfections and Their Simultaneous Transmission on Antigenic Diversity and Epidemic Cycling of Infectious Diseases. BioMed Res. Int. 2014;2014:1–23. doi: 10.1155/2014/375862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dietrich A., Hermans C., Heppt M.V., Ruzicka T., Schauber J., Reinholz M. Human papillomavirus status, anal cytology and histopathological outcome in HIV-positive patients. J. Eur. Acad. Dermatol. Venereol. 2015;29:2011–2018. doi: 10.1111/jdv.13205. [DOI] [PubMed] [Google Scholar]
- 41.Henn G.A.D.L., Júnior A.N.R., Colares J.K.B., Mendes L.P., Silveira J.G.C., Lima A.A.F., Aires B.P., Facanha M.C. Is Visceral Leishmaniasis the same in HIV-coinfected adults? Braz. J. Infect. Dis. 2018;22:92–98. doi: 10.1016/j.bjid.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nunes J.D.O., Bizerra P.L., Paniago A.M.M., Mendes R.P., Chang M.R., Pillon K.R.A.P. The Simultaneous Occurrence of Histoplasmosis and Cryptococcal Fungemia: A Case Report and Review of the Literature. Mycopathologia. 2016;181:891–897. doi: 10.1007/s11046-016-0036-1. [DOI] [PubMed] [Google Scholar]
- 43.Ioannou P., Papakitsou I., Kofteridis D.P. Fungal endocarditis in transplant recipients: A systematic review. Mycoses. 2020;63:952–963. doi: 10.1111/myc.13132. [DOI] [PubMed] [Google Scholar]
- 44.Shah M.M., Hsiao E.I., Kirsch C.M., Gohil A., Narasimhan S., Stevens D.A. Invasive pulmonary aspergillosis and influenza co-infection in immunocompetent hosts: Case reports and review of the literature. Diagn. Microbiol. Infect. Dis. 2018;91:147–152. doi: 10.1016/j.diagmicrobio.2018.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reece E., Segurado R., Jackson A., McClean S., Renwick J., Greally P. Co-colonisation with Aspergillus fumigatus and Pseudomonas aeruginosa is associated with poorer health in cystic fibrosis patients: An Irish registry analysis. BMC Pulm. Med. 2017;17:70. doi: 10.1186/s12890-017-0416-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chermetz M., Gobbo M., Rupel K., Ottaviani G., Tirelli G., Bussani R., Luzzati R., Di Lenarda R., Biasotto M. Combined Orofacial Aspergillosis and Mucormycosis: Fatal Complication of a Recurrent Paediatric Glioma—Case Report and Review of Literature. Mycopathologia. 2016;181:723–733. doi: 10.1007/s11046-016-0021-8. [DOI] [PubMed] [Google Scholar]
- 47.Maalouly C., Devresse A., Martin A., Rodriguez-Villalobos H., Kanaan N., Belkhir L. Coinfection of Mycobacterium malmoense and Mycobacterium chimaera in a kidney transplant recipient: A case report and review of the literature. Transpl. Infect. Dis. 2020:e13241. doi: 10.1111/tid.13241. [DOI] [PubMed] [Google Scholar]
- 48.Hirabayashi R., Nakagawa A., Takegawa H., Tomii K. A case of pleural effusion caused by Mycobacterium fortuitum and Mycobacterium mageritense coinfection. BMC Infect. Dis. 2019;19:1–3. doi: 10.1186/s12879-019-4366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shin S.H., Jhun B.W., Kim S.-Y., Choe J., Jeon K., Huh H.J., Ki C.-S., Lee N.Y., Shin S.J., Daley C.L., et al. Nontuberculous Mycobacterial Lung Diseases Caused by Mixed Infection with Mycobacterium avium Complex and Mycobacterium abscessus Complex. Antimicrob. Agents Chemother. 2018;62 doi: 10.1128/AAC.01105-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Furuta K., Ito A., Ishida T., Ito Y., Sone N., Takaiwa T., Yokoyama T., Tachibana H., Arita M., Hashimoto T. 18 Cases of pulmonary Mycobacterium abscessus: Clinical difference depending on the presence or absence of Mycobacterium avium complex. J. Infect. Chemother. 2016;22:622–628. doi: 10.1016/j.jiac.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 51.Naito K., Noguchi S., Yatera K., Kawanami T., Yamasaki K., Fukuda K., Ikegami H., Akata K., Kido T., Sakamoto N., et al. Coinfection With Multiple Nontuberculous Mycobacteria as a Possible Exacerbating Factor in Pulmonary Nontuberculous Mycobacteriosis. Chest. 2020 doi: 10.1016/j.chest.2020.06.027. [DOI] [PubMed] [Google Scholar]
- 52.Lai C.-C., Wang C.-Y., Hsueh P.-R. Co-infections among patients with COVID-19: The need for combination therapy with non-anti-SARS-CoV-2 agents? J. Microbiol. Immunol. Infect. 2020;53:505–512. doi: 10.1016/j.jmii.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Genus: Mycobacterium. [(accessed on 26 September 2020)]; Available online: https://www.bacterio.net/genus/mycobacterium.
- 54.Swift S., Cohen H. Granulomas of the Skin Due toMycobacterium balneiafter Abrasions from a Fish Tank. N. Engl. J. Med. 1962;267:1244–1246. doi: 10.1056/NEJM196212132672408. [DOI] [PubMed] [Google Scholar]
- 55.Walsh U.S., Meyers W.M., Abalos R.M., Portaels F., Cruz E.C.D., Walsh G.P., Tan E.V. CLINICAL AND HISTOLOGIC FEATURES OF SKIN LESIONS IN A CYNOMOLGUS MONKEY EXPERIMENTALLY INFECTED WITH MYCOBACTERIUM ULCERANS (BURULI ULCER) BY INTRADERMAL INOCULATION. Am. J. Trop. Med. Hyg. 2007;76:132–134. doi: 10.4269/ajtmh.2007.76.132. [DOI] [PubMed] [Google Scholar]
- 56.Walsh D.S., Portaels F., Meyers W.M. Buruli ulcer (Mycobacterium ulcerans infection) Trans. R. Soc. Trop. Med. Hyg. 2008;102:969–978. doi: 10.1016/j.trstmh.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 57.Swenson C., Zerbe C.S., Fennelly K. Host Variability in NTM Disease: Implications for Research Needs. Front. Microbiol. 2018;9:2901. doi: 10.3389/fmicb.2018.02901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Falkinham J.O. Environmental Sources of Nontuberculous Mycobacteria. Clin. Chest Med. 2015;36:35–41. doi: 10.1016/j.ccm.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 59.Edwards A.J., Chen C., Kemski M.M., Hu J., Mitchell T., Rappleye C.A. Histoplasma yeast and mycelial transcriptomes reveal pathogenic-phase and lineage-specific gene expression profiles. BMC Genom. 2013;14:695. doi: 10.1186/1471-2164-14-695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cauchie M., Desmet S., Lagrou K. Candida and its dual lifestyle as a commensal and a pathogen. Res. Microbiol. 2017;168:802–810. doi: 10.1016/j.resmic.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 61.Kullberg B.J., Arendrup M.C. Invasive Candidiasis. N. Engl. J. Med. 2015;373:1445–1456. doi: 10.1056/NEJMra1315399. [DOI] [PubMed] [Google Scholar]
- 62.De Medeiros M.A.P., De Melo A.P.V., Bento A.D.O., De Souza L.B.F.C., Neto F.D.A.B., Garcia J.B.-L., Zuza-Alves D.L., Francisco E.C., Melo A.S.D.A., Chaves G.M. Epidemiology and prognostic factors of nosocomial candidemia in Northeast Brazil: A six-year retrospective study. PLoS ONE. 2019;14:e0221033. doi: 10.1371/journal.pone.0221033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Koehler P., Stecher M., Cornely O., Vehreschild M., Bohlius J., Wisplinghoff H., Vehreschild J. Morbidity and mortality of candidaemia in Europe: An epidemiologic meta-analysis. Clin. Microbiol. Infect. 2019;25:1200–1212. doi: 10.1016/j.cmi.2019.04.024. [DOI] [PubMed] [Google Scholar]
- 64.Zhang J., Zhang D., Xue X., Yang L., Chen L., Pan L. Clinical analysis of 16 cases of pulmonary cryptococcosis in patients with normal immune function. Ann. Palliat. Med. 2020;9:1117–1124. doi: 10.21037/apm-20-897. [DOI] [PubMed] [Google Scholar]
- 65.Moretti M.L., Busso-Lopes A.F., Tararam C.A., Moraes R., Muraosa Y., Mikami Y., Gonoi T., Taguchi H., Lyra L., Reichert-Lima F., et al. Airborne transmission of invasive fusariosis in patients with hematologic malignancies. PLoS ONE. 2018;13:e0196426. doi: 10.1371/journal.pone.0196426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Prigitano A., Cavanna C., Passera M., Gelmi M., Sala E., Ossi C., Grancini A., Calabrò M., Bramati S., Tejada M., et al. Evolution of fungemia in an Italian region. J. Mycol. Médicale. 2020;30:100906. doi: 10.1016/j.mycmed.2019.100906. [DOI] [PubMed] [Google Scholar]
- 67.Faria S., Joao I., Jordao L. General Overview on Nontuberculous Mycobacteria, Biofilms, and Human Infection. J. Pathog. 2015;2015:1–10. doi: 10.1155/2015/809014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ratnatunga C.N., Lutzky V.P., Kupz A., Doolan D.L., Reid D.W., Field M., Bell S.C., Thomson R.M., Miles J.J. The Rise of Non-Tuberculosis Mycobacterial Lung Disease. Front. Immunol. 2020;11:303. doi: 10.3389/fimmu.2020.00303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bryant J.M., Grogono D.M., Greaves D., Foweraker J., Roddick I., Inns T., Reacher M., Haworth C.S., Curran M.D., Harris S.R., et al. Whole-genome sequencing to identify transmission of Mycobacterium abscessus between patients with cystic fibrosis: A retrospective cohort study. Lancet. 2013;381:1551–1560. doi: 10.1016/S0140-6736(13)60632-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lutzky V.P., Ratnatunga C.N., Smith D.J., Kupz A., Rn D.M.D., Reid D.W., Thomson R.M., Bell S.C., Miles J.J. Anomalies in T Cell Function Are Associated With Individuals at Risk of Mycobacterium abscessus Complex Infection. Front. Immunol. 2018;9:9. doi: 10.3389/fimmu.2018.01319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dellière S., Angebault C., Fihman V., Foulet F., Lepeule R., Maitre B., Schlemmer F., Botterel F. Concomitant Presence of Aspergillus Species and Mycobacterium Species in the Respiratory Tract of Patients: Underestimated Co-occurrence? Front. Microbiol. 2020;10:2980. doi: 10.3389/fmicb.2019.02980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Totaro M., Costa A.L., Casini B., Profeti S., Gallo A., Frendo L., Porretta A., Valentini P., Privitera G.P., Baggiani A. Microbiological Air Quality in Heating, Ventilation and Air Conditioning Systems of Surgical and Intensive Care Areas: The Application of a Disinfection Procedure for Dehumidification Devices. Pathogens. 2019;8:8. doi: 10.3390/pathogens8010008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Romo J.A., Kumamoto C.A. On Commensalism of Candida. J. Fungi. 2020;6:16. doi: 10.3390/jof6010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hoefsloot W., Van Ingen J., Andrejak C., Ängeby K., Bauriaud R., Bemer P., Beylis N., Boeree M.J., Cacho J., Chihota V., et al. The geographic diversity of nontuberculous mycobacteria isolated from pulmonary samples: An NTM-NET collaborative study. Eur. Respir. J. 2013;42:1604–1613. doi: 10.1183/09031936.00149212. [DOI] [PubMed] [Google Scholar]
- 75.Wagner D., Lipman M., Cooray S., Ringshausen F.C., Morimoto K., Koh W.-J., Thomson R.M. Global Epidemiology of NTM Disease (Except Northern America) Ultrasound Intensive Care Unit. 2018:163–260. doi: 10.1007/978-3-319-93473-0_8. [DOI] [Google Scholar]
- 76.Varghese B., Memish Z., Abuljadayel N., Al-Hakeem R., Alrabiah F., Al-Hajoj S. Emergence of Clinically Relevant Non-Tuberculous Mycobacterial Infections in Saudi Arabia. PLoS Negl. Trop. Dis. 2013;7:e2234. doi: 10.1371/journal.pntd.0002234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Simons S.O., Van Ingen J., Hsueh P.-R., Van Hung N., Dekhuijzen P.R., Boeree M.J., Van Soolingen D. Nontuberculous Mycobacteria in Respiratory Tract Infections, Eastern Asia. Emerg. Infect. Dis. 2011;17:343–349. doi: 10.3201/eid170310060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mortazavi Z., Bahrmand A., Sakhaee F., Doust R.H., Vaziri F., Siadat S.D., Fateh A. Evaluating the clinical significance of nontuberculous mycobacteria isolated from respiratory samples in Iran: An often overlooked disease. Infect. Drug Resist. 2019;12:1917–1927. doi: 10.2147/IDR.S214181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tortoli E. Clinical manifestations of nontuberculous mycobacteria infections. Clin. Microbiol. Infect. 2009;15:906–910. doi: 10.1111/j.1469-0691.2009.03014.x. [DOI] [PubMed] [Google Scholar]
- 80.Bahr N.C., Antinori S., Wheat L.J., Sarosi G.A. Histoplasmosis Infections Worldwide: Thinking Outside of the Ohio River Valley. Curr. Trop. Med. Rep. 2015;2:70–80. doi: 10.1007/s40475-015-0044-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Baker J., Setianingrum F., Wahyuningsih R., Denning D.W. Mapping histoplasmosis in South East Asia—Implications for diagnosis in AIDS. Emerg. Microbes Infect. 2019;8:1139–1145. doi: 10.1080/22221751.2019.1644539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brescini L., Mazzanti S., Orsetti E., Morroni G., Masucci A., Pocognoli A., Barchiesi F. Species distribution and antifungal susceptibilities of bloodstream Candida isolates: A nine-years single center survey. J. Chemother. 2020;32:244–250. doi: 10.1080/1120009X.2020.1783154. [DOI] [PubMed] [Google Scholar]
- 83.Muderris T., Kaya S., Ormen B., Gokmen A.A., Akpinar C.V., Gul S.Y. Mortality and risk factor analysis for Candida blood stream infection: A three-year retrospective study. J. Mycol. Médicale. 2020;30:101008. doi: 10.1016/j.mycmed.2020.101008. [DOI] [PubMed] [Google Scholar]
- 84.Ricotta E.E., Lai Y.L., Babiker A., Strich J.R., Kadri S.S., Lionakis M.S., Prevots D.R., Adjemian J. Invasive candidiasis species distribution and trends, United States, 2009–2017. J. Infect. Dis. 2020 doi: 10.1093/infdis/jiaa502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pinto-Magalhães S., Martins A., Lacerda S., Filipe R., Prista-Leão B., Pinheiro D., Silva-Pinto A., Santos L. Candidemia in a Portuguese tertiary care hospital: Analysis of a 2-year period. J. Mycol. Médicale. 2019;29:320–324. doi: 10.1016/j.mycmed.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 86.Warris A., Pana Z.-D., Oletto A., Lundin R., Castagnola E., Lehrnbecher T., Groll A.H., Roilides E., Andersen C.T., Arendrup M.C., et al. Etiology and Outcome of Candidemia in Neonates and Children in Europe. Pediatr. Infect. Dis. J. 2020;39:114–120. doi: 10.1097/INF.0000000000002530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Adenis A.A., Valdes A., Cropet C., McCotter O.Z., Derado G., Couppié P., Chiller T., Nacher M. Burden of HIV-associated histoplasmosis compared with tuberculosis in Latin America: A modelling study. Lancet Infect. Dis. 2018;18:1150–1159. doi: 10.1016/S1473-3099(18)30354-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lahiri S., Manjunath N., Bhat M., Hagen F., Bahubali V.H., Palaniappan M., Maji S., Chandrashekar N. Clinical insights and epidemiology of central nervous system infection due to Cryptococcus neoformans/gattii species complexes: A prospective study from South India. Med. Mycol. 2019;58:600–608. doi: 10.1093/mmy/myz097. [DOI] [PubMed] [Google Scholar]
- 89.Zhou J., Tan J., Gong Y., Li N., Luo G. Candidemia in major burn patients and its possible risk factors: A 6-year period retrospective study at a burn ICU. Burns. 2019;45:1164–1171. doi: 10.1016/j.burns.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 90.Martini C., Torelli R., De Groot T., De Carolis E., Morandotti G.A., De Angelis G., Posteraro B., Meis J.F., Sanguinetti M. Prevalence and Clonal Distribution of Azole-Resistant Candida parapsilosis Isolates Causing Bloodstream Infections in a Large Italian Hospital. Front. Cell. Infect. Microbiol. 2020;10:232. doi: 10.3389/fcimb.2020.00232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Prevots D.R., Marras T.K. Epidemiology of human pulmonary infection with nontuberculous mycobacteria a review. Clin. Chest Med. 2015;36:13–34. doi: 10.1016/j.ccm.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Iseman M.D., Chan E.D. Underlying Host Risk Factors for Nontuberculous Mycobacterial Lung Disease. Semin. Respir. Crit. Care Med. 2013;34:110–123. doi: 10.1055/s-0033-1333573. [DOI] [PubMed] [Google Scholar]
- 93.Kousha M., Tadi R., Soubani O.A. Pulmonary aspergillosis: A clinical review. Eur. Respir. Rev. 2011;20:156–174. doi: 10.1183/09059180.00001011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Honda J.R., Alper S., Bai X., Chan E.D. Acquired and genetic host susceptibility factors and microbial pathogenic factors that predispose to nontuberculous mycobacterial infections. Curr. Opin. Immunol. 2018;54:66–73. doi: 10.1016/j.coi.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 95.Marochi-Telles J.P., Muniz R., Jr., Sztajnbok J., Oliveira A.C.-D. Disseminated Mycobacterium avium on HIV/AIDS: Historical and Current Literature Review. Aids Rev. 2020;22:9–15. doi: 10.24875/AIDSRev.20000104. [DOI] [PubMed] [Google Scholar]
- 96.Siberry G.K., Abzug M.J., Nachman S., Brady M.T., Dominguez K.L., Handelsman E., Mofenson L.M., Nesheim S., Children P.O.O.I.I.H.-E.A.H.-I. Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Exposed and HIV-Infected Children. Pediatr. Infect. Dis. J. 2013;32 doi: 10.1097/01.inf.0000437856.09540.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kaplan J.E., Benson C., Holmes K.K., Brooks J.T., Pau A., Masur H., Centers for Disease Control and Prevention (CDC) National Institutes of Health. HIV Medicine Association of the Infectious Diseases Society of America Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: Recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm. Rep. Morb. Mortal. Wkly. Rep. Recomm. Rep. 2009;58:1–207. [PubMed] [Google Scholar]
- 98.Browne S.K., Burbelo P.D., Chetchotisakd P., Suputtamongkol Y., Kiertiburanakul S., Shaw P.A., Kirk J.L., Jutivorakool K., Zaman R., Ding L., et al. Adult-Onset Immunodeficiency in Thailand and Taiwan. N. Engl. J. Med. 2012;367:725–734. doi: 10.1056/NEJMoa1111160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sampaio E.P., Hsu A.P., Pechacek J., Bax H.I., Dias D.L., Paulson M.L., Chandrasekaran P., Rosen L.B., Carvalho D.S., Ding L., et al. Signal transducer and activator of transcription 1 (STAT1) gain-of-function mutations and disseminated coccidioidomycosis and histoplasmosis. J. Allergy Clin. Immunol. 2013;131:1624–1634. doi: 10.1016/j.jaci.2013.01.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nielsen J., Kofod-Olsen E., Spaun E., Larsen C.S., Christiansen M., Mogensen T.H. A STAT1-gain-of-function mutation causing Th17 deficiency with chronic mucocutaneous candidiasis, psoriasiform hyperkeratosis and dermatophytosis. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-211372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Odio C.D., Milligan K.L., E McGowan K., Spergel A.K.R., Bishop R.J., Boris L., Urban A., Welch P., Heller T., Kleiner E.D., et al. Endemic mycoses in patients with STAT3-mutated hyper-IgE (Job) syndrome. J. Allergy Clin. Immunol. 2015;136:1411–1413. doi: 10.1016/j.jaci.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhang Q., Boisson B., Béziat V., Puel A., Casanova J.-L. Human hyper-IgE syndrome: Singular or plural? Mamm. Genome. 2018;29:603–617. doi: 10.1007/s00335-018-9767-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Merkhofer R.M., Klein B.S. Advances in Understanding Human Genetic Variations That Influence Innate Immunity to Fungi. Front. Cell. Infect. Microbiol. 2020;10:69. doi: 10.3389/fcimb.2020.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Vaezi A., Fakhim H., Abtahian Z., Khodavaisy S., Geramishoar M., Alizadeh A., Meis J.F., Badali H. Frequency and Geographic Distribution of CARD9 Mutations in Patients With Severe Fungal Infections. Front. Microbiol. 2018;9:2434. doi: 10.3389/fmicb.2018.02434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lionakis M.S., Levitz S.M. Host Control of Fungal Infections: Lessons from Basic Studies and Human Cohorts. Annu. Rev. Immunol. 2018;36:157–191. doi: 10.1146/annurev-immunol-042617-053318. [DOI] [PubMed] [Google Scholar]
- 106.Smith N.L.D., Hankinson J., Simpson A., Denning D.W., Bowyer P. Reduced expression of TLR3, TLR10 and TREM1 by human macrophages in Chronic cavitary pulmonary aspergillosis, and novel associations of VEGFA, DENND1B and PLAT. Clin. Microbiol. Infect. 2014;20:O960–O968. doi: 10.1111/1469-0691.12643. [DOI] [PubMed] [Google Scholar]
- 107.Smith N., Hankinson J., Simpson A., Bowyer P., Denning D.W. A prominent role for the IL1 pathway and IL15 in susceptibility to chronic cavitary pulmonary aspergillosis. Clin. Microbiol. Infect. 2014;20:O480–O488. doi: 10.1111/1469-0691.12473. [DOI] [PubMed] [Google Scholar]
- 108.Henkle E., Winthrop K.L. Nontuberculous mycobacteria infections in immunosuppressed hosts. Clin. Chest Med. 2015;36:91–99. doi: 10.1016/j.ccm.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Tufariello J.M., Chan J., Flynn J.L. Latent tuberculosis: Mechanisms of host and bacillus that contribute to persistent infection. Lancet Infect. Dis. 2003;3:578–590. doi: 10.1016/s1473-3099(03)00741-2. [DOI] [PubMed] [Google Scholar]
- 110.Abe Y., Fukushima K., Hosono Y., Matsumoto Y., Motooka D., Ose N., Nakamura S., Kitada S., Kida H., Kumanogoh A. Host Immune Response and Novel Diagnostic Approach to NTM Infections. Int. J. Mol. Sci. 2020;21 doi: 10.3390/ijms21124351. 4351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Luckett K., Dummer J.S., Miller G., Hester S., Thomas L.D. Histoplasmosis in Patients With Cell-Mediated Immunodeficiency: Human Immunodeficiency Virus Infection, Organ Transplantation, and Tumor Necrosis Factor-α Inhibition. Open Forum Infect. Dis. 2015;2 doi: 10.1093/ofid/ofu116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Herring A.C., Lee J., McDonald R.A., Toews G.B., Huffnagle G.B. Induction of Interleukin-12 and Gamma Interferon Requires Tumor Necrosis Factor Alpha for Protective T1-Cell-Mediated Immunity to Pulmonary Cryptococcus neoformans Infection. Infect. Immun. 2002;70:2959–2964. doi: 10.1128/iai.70.6.2959-2964.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chandra J., McCormick T.S., Imamura Y., Mukherjee P.K., Ghannoum M.A. Interaction of Candida albicans with Adherent Human Peripheral Blood Mononuclear Cells Increases C. albicans Biofilm Formation and Results in Differential Expression of Pro- and Anti-Inflammatory Cytokines. Infect. Immun. 2007;75:2612–2620. doi: 10.1128/iai.01841-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Rosati D., Bruno M., Jaeger M., Kullberg B.-J., Van De Veerdonk F., Netea M.G., Oever J.T. An Exaggerated Monocyte-Derived Cytokine Response to Candida Hyphae in Patients With Recurrent Vulvovaginal Candidiasis. J. Infect. Dis. 2020 doi: 10.1093/infdis/jiaa444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Carrion S.D.J., Leal S.M., Ghannoum M.A., Aimanianda V., Latgé J.-P., Pearlman E. The RodA Hydrophobin on Aspergillus fumigatus Spores Masks Dectin-1– and Dectin-2–Dependent Responses and Enhances Fungal Survival In Vivo. J. Immunol. 2013;191:2581–2588. doi: 10.4049/jimmunol.1300748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Murayama T., Amitani R., Tsuyuguchi K., Watanabe I., Kimoto T., Suzuki K., Tanaka E., Kamei K., Nishimura K. Polypoid bronchial lesions due to Scedosporium apiospermum in a patient with Mycobacterium avium complex pulmonary disease. Eur. Respir. J. 1998;12:745–747. doi: 10.1183/09031936.98.12030745. [DOI] [PubMed] [Google Scholar]
- 117.Gifford A.H., Lahey T., Von Reyn C.F. Fatal hemoptysis from invasiveAspergillus nigerin a patient with cavitary lung disease andMycobacterium avium complexinfection. Med. Mycol. 2006;44:557–560. doi: 10.1080/13693780600575635. [DOI] [PubMed] [Google Scholar]
- 118.Joury A., AlShehri M., Alhasan M. Concurrent Persistent Cryptococcosis and Mycobacterium avium Complex Infections in a Patient With Human Immunodeficiency Virus. Ochsner J. 2019;19:169–173. doi: 10.31486/toj.17.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kaneko T., Jr D.A.M., Marty F.M., Colson Y. Triple opportunistic pulmonary cavitary disease after cord blood transplantation. Transpl. Infect. Dis. 2014;16:818–821. doi: 10.1111/tid.12279. [DOI] [PubMed] [Google Scholar]
- 120.Kobashi Y., Yoshida K., Miyashita N., Niki Y., Matsushima T. Chronic Necrotizing Pulmonary Aspergillosis Complicated by a Cavitary Lesion Caused by Pulmonary Mycobacterium-avium Complex Disease. Intern. Med. 2005;44:246–250. doi: 10.2169/internalmedicine.44.246. [DOI] [PubMed] [Google Scholar]
- 121.Zhang J., Huang X., Zhang X., Zhu Y., Liao K., Ma J., Wang G., Guo Y., Xie C. Coinfection of disseminated Talaromyces marneffei and Mycobacteria kansasii in a patient with papillary thyroid cancer. Medicine. 2017;96:e9072. doi: 10.1097/MD.0000000000009072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Rujirachun P., Sangwongwanich J., Chayakulkeeree M. Triple infection with Cryptococcus, varicella-zoster virus, and Mycobacterium abscessus in a patient with anti-interferon-gamma autoantibodies: A case report. BMC Infect. Dis. 2020;20:1–7. doi: 10.1186/s12879-020-4949-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Pietras T.A., Baum C.L., Swick B.L. Coexistent Kaposi sarcoma, cryptococcosis, and Mycobacterium avium intracellulare in a solitary cutaneous nodule in a patient with AIDS: Report of a case and literature review. J. Am. Acad. Dermatol. 2010;62:676–680. doi: 10.1016/j.jaad.2008.12.052. [DOI] [PubMed] [Google Scholar]
- 124.Seok H., Ko J.-H., Shin I., Eun Y.H., Lee S.-E., Lee Y.-B., Peck K.R. Disseminated Talaromyces marneffei and Mycobacterium intracellulare coinfection in an HIV-infected patient. Int. J. Infect. Dis. 2015;38:86–88. doi: 10.1016/j.ijid.2015.07.020. [DOI] [PubMed] [Google Scholar]
- 125.Yuan C., Lu H., Yang C., Gao W., Wang H., Wu G. Case report: Mycobacterium monacense isolated from the blood culture of a patient with pulmonary infection. BMC Infect. Dis. 2020;20:1–5. doi: 10.1186/s12879-020-4936-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kim J.S., Choi M., Nam C.H., Kim J.Y., Hong S.P., Kim M.H., Park B.C. Co-infection of Scedosporium apiospermum and Mycobacterium chelonae in an immunocompetent host. J. Dermatol. 2014;41:922–925. doi: 10.1111/1346-8138.12601. [DOI] [PubMed] [Google Scholar]
- 127.Furuuchi K., Ito A., Hashimoto T., Kumagai S., Ishida T. Clinical significance of Aspergillus species isolated from respiratory specimens in patients with Mycobacterium avium complex lung disease. Eur. J. Clin. Microbiol. Infect. Dis. 2017;37:91–98. doi: 10.1007/s10096-017-3105-6. [DOI] [PubMed] [Google Scholar]
- 128.Zoumot Z., Boutou A.K., Gill S.S., Van Zeller M., Hansell D.M., Wells A.U., Wilson R., Loebinger M.R. Mycobacterium aviumcomplex infection in non-cystic fibrosis bronchiectasis. Respirology. 2014;19:714–722. doi: 10.1111/resp.12287. [DOI] [PubMed] [Google Scholar]
- 129.Bansod S., Rai M. Emerging of Mycotic Infection in Patients Infected with Mycobacterium tuberculosis. World J. Med. Sci. 2008;7:74–80. [Google Scholar]
- 130.Kosmidis C., Muldoon E.G. Challenges in the management of chronic pulmonary aspergillosis. Med. Mycol. 2016;55:63–68. doi: 10.1093/mmy/myw119. [DOI] [PubMed] [Google Scholar]
- 131.Samayoa B., Aguirre L., Bonilla O., Medina N., Lau-Bonilla D., Mercado D., Moller A., Perez J.C., Alastruey-Izquierdo A., Arathoon E., et al. The Diagnostic Laboratory Hub: A New Health Care System Reveals the Incidence and Mortality of Tuberculosis, Histoplasmosis, and Cryptococcosis of PWH in Guatemala. Open Forum Infect. Dis. 2020;7:ofz534. doi: 10.1093/ofid/ofz534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Jhun B.W., Jung W.J., Hwang N.Y., Park H.Y., Jeon K., Kang E.-S., Koh W.-J. Risk factors for the development of chronic pulmonary aspergillosis in patients with nontuberculous mycobacterial lung disease. PLoS ONE. 2017;12:e0188716. doi: 10.1371/journal.pone.0188716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Amiri M.R.J., Siami R., Khaledi A. Tuberculosis Status and Coinfection of Pulmonary Fungal Infections in Patients Referred to Reference Laboratory of Health Centers Ghaemshahr City during 2007–2017. Ethiop. J. Health Sci. 2018;28:683–690. doi: 10.4314/ejhs.v28i6.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Johnston I. Mycobacterium xenopi infection and aspergilloma. Tubercle. 1988;69:139–143. doi: 10.1016/0041-3879(88)90077-3. [DOI] [PubMed] [Google Scholar]
- 135.Kobashi Y., Fukuda M., Yoshida K., Miyashita N., Niki Y., Oka M. Chronic necrotizing pulmonary aspergillosis as a complication of pulmonary Mycobacterium avium complex disease. Respirology. 2006;11:809–813. doi: 10.1111/j.1440-1843.2006.00952.x. [DOI] [PubMed] [Google Scholar]
- 136.Torres-González P., Niembro-Ortega M.D., Martínez-Gamboa A., Ahumada-Topete V.H., Andrade-Villanueva J.F., Araujo-Meléndez J., Chaparro-Sánchez A., Crabtree-Ramírez B., Cruz-Martínez S., Gamboa-Domínguez A., et al. Diagnostic accuracy cohort study and clinical value of the Histoplasma urine antigen (ALPHA Histoplasma EIA) for disseminated histoplasmosis among HIV infected patients: A multicenter study. PLoS Negl. Trop. Dis. 2018;12:e0006872. doi: 10.1371/journal.pntd.0006872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wickremasinghe M., Ozerovitch L.J., Davies G., Wodehouse T., Chadwick M.V., Abdallah S., Shah P., Wilson R. Non-tuberculous mycobacteria in patients with bronchiectasis. Thorax. 2005;60:1045–1051. doi: 10.1136/thx.2005.046631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Fujita K., Ito Y., Hirai T., Kubo T., Togashi K., Ichiyama S., Mishima M. Prevalence and risk factors for chronic co-infection in pulmonaryMycobacterium aviumcomplex disease. BMJ Open Respir. Res. 2014;1:e000050. doi: 10.1136/bmjresp-2014-000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Takeda K., Imamura Y., Takazono T., Yoshida M., Ide S., Hirano K., Tashiro M., Saijo T., Kosai K., Morinaga Y., et al. The risk factors for developing of chronic pulmonary aspergillosis in nontuberculous mycobacteria patients and clinical characteristics and outcomes in chronic pulmonary aspergillosis patients coinfected with nontuberculous mycobacteria. Med. Mycol. 2015;54:120–127. doi: 10.1093/mmy/myv093. [DOI] [PubMed] [Google Scholar]
- 140.Choudat D., Horreard P., Pretet S., Grosset J., Toty L. Superinfection by Aspergillus fumigatus of a pulmonary lesion caused by Mycobacterium xenopi. Tubercle. 1986;67:71–74. doi: 10.1016/0041-3879(86)90035-8. [DOI] [PubMed] [Google Scholar]
- 141.Kimmerling E.A., Fedrick J.A., Tenholder M.F. Invasive Aspergillus niger with Fatal Pulmonary Oxalosis in Chronic Obstructive Pulmonary Disease. Chest. 1992;101:870–872. doi: 10.1378/chest.101.3.870. [DOI] [PubMed] [Google Scholar]
- 142.Montaigne E., Petit F.-X., Gourdier A.-L., Urban T., Gagnadoux F. Aspergillose pulmonaire compliquant une infection à mycobactérie atypique chez deux patients atteints de bronchopneumopathie chronique obstructive. Rev. des Mal. Respir. 2012;29:79–83. doi: 10.1016/j.rmr.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 143.Kampitak T., Suwanpimolkul G., Browne S., Suankratay C. Anti-interferon-γ autoantibody and opportunistic infections: Case series and review of the literature. Infection. 2011;39:65–71. doi: 10.1007/s15010-010-0067-3. [DOI] [PubMed] [Google Scholar]
- 144.Kampmann B., Hemingway C., Stephens A., Davidson R., Goodsall A., Anderson S., Nicol M., Schölvinck E., Relman D., Waddell S., et al. Acquired predisposition to mycobacterial disease due to autoantibodies to IFN-γ. J. Clin. Investig. 2005;115:2480–2488. doi: 10.1172/JCI19316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Reischl U., Melzl H., Kroppenstedt R.M., Miethke T., Naumann L., Mariottini A., Mazzarelli G., Tortoli E. Mycobacterium monacense sp. nov. Int. J. Syst. Evol. Microbiol. 2006;56:2575–2578. doi: 10.1099/ijs.0.64527-0. [DOI] [PubMed] [Google Scholar]
- 146.Chmiel J.F., Aksamit T.R., Chotirmall S.H., Dasenbrook E.C., Elborn J.S., Lipuma J.J., Ranganathan S.C., Waters V.J., Ratjen F.A. Antibiotic Management of Lung Infections in Cystic Fibrosis. II. Nontuberculous Mycobacteria, Anaerobic Bacteria, and Fungi. Ann. Am. Thorac. Soc. 2014;11:1298–1306. doi: 10.1513/AnnalsATS.201405-203AS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Jones P.G., Cohen R.L., Batts D.H., Jr J.S. Disseminated Histoplasmosis, Invasive Pulmonary Aspergillosis, and Other Opportunistic Infections in a Homosexual Patient with Acquired Immune Deficiency Syndrome. Sex. Transm. Dis. 1983;10:202–204. doi: 10.1097/00007435-198311000-00010. [DOI] [PubMed] [Google Scholar]
- 148.Wheat L., Slama T.G., Zeckel M.L. Histoplasmosis in the acquired immune deficiency syndrome. Am. J. Med. 1985;78:203–210. doi: 10.1016/0002-9343(85)90427-9. [DOI] [PubMed] [Google Scholar]
- 149.Maliwan N., Zvetina J.R. Pulmonary Mycetoma Following Mycobacterium kansasii Infection. Arch. Intern. Med. 1985;145:2180–2183. doi: 10.1001/archinte.1985.00360120048007. [DOI] [PubMed] [Google Scholar]
- 150.Johnson P.C., Khardor N., Najjar A.F., Butt F., Mansell P.W., Sarosi G.A. Progressive disseminated histoplasmosis in patients with acquired immunodeficiency syndrome. Am. J. Med. 1988;85:152–158. doi: 10.1016/S0002-9343(88)80334-6. [DOI] [PubMed] [Google Scholar]
- 151.Crothers K., Huang L. Recurrence of Pneumocystis carinii pneumonia in an HIV-infected patient: Apparent selective immune reconstitution after initiation of antiretroviral therapy. HIV Med. 2003;4:346–349. doi: 10.1046/j.1468-1293.2003.00170.x. [DOI] [PubMed] [Google Scholar]
- 152.Castelli A.A., Rosenthal D.G., Ignacio R.B., Chu H.Y. Hemophagocytic Lymphohistiocytosis Secondary to Human Immunodeficiency Virus-Associated Histoplasmosis. Open Forum Infect. Dis. 2015;2:ofv140. doi: 10.1093/ofid/ofv140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Pinheiro M.V.C., Ho Y.-L., Nicodemo A.C., Duarte-Neto A. The diagnosis of multiple opportunistic infections in advanced stage AIDS: When Ockham’s Razor doesn’t cut it. Autops. Case Rep. 2018;8:8. doi: 10.4322/acr.2018.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Basso R.P., Poester V.R., Silveira J.M., Vieira R.S., Da Mota L.D., Klafke G.B., Müller J.N., Penna C.P., Vianna J.S., Busatto C., et al. Histoplasma capsulatum and Mycobacterium avium co-infection in an immunocompromised patient: Case report and literature review. Med. Mycol. Case Rep. 2020;28:29–32. doi: 10.1016/j.mmcr.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Choi J., Nikoomanesh K., Uppal J., Wang S. Progressive disseminated histoplasmosis with concomitant disseminated nontuberculous mycobacterial infection in a patient with AIDS from a nonendemic region (California) BMC Pulm. Med. 2019;19:46. doi: 10.1186/s12890-019-0808-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Tajan J., Espasa M., Sala M., Navarro M., Font B., González-Martín J., Segura F. Disseminated Infection by Mycobacterium sherrisii and Histoplasma capsulatum in an African HIV-Infected Patient. Am. J. Trop. Med. Hyg. 2013;88:914–917. doi: 10.4269/ajtmh.12-0572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Souilamas R., Danel C., Chauffour X., Riquet M. Lung cancer occurring with Mycobacterium xenopi and Aspergillus. Eur. J. Cardio Thoracic Surg. 2001;20:211–213. doi: 10.1016/S1010-7940(01)00720-5. [DOI] [PubMed] [Google Scholar]
- 158.Wu M.-L., Aziz D.B., Dartois V., Dick T. NTM drug discovery: Status, gaps and the way forward. Drug Discov. Today. 2018;23:1502–1519. doi: 10.1016/j.drudis.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Daley C.L., Iaccarino J.M., Lange C., Cambau E., Wallace R.J., Jr., Andrejak C., Böttger E.C., Brozek J., Griffith E.D.E., Guglielmetti L., et al. Treatment of Nontuberculous Mycobacterial Pulmonary Disease: An Official ATS/ERS/ESCMID/IDSA Clinical Practice Guideline. Clin. Infect. Dis. 2020;71:905–913. doi: 10.1093/cid/ciaa1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Haworth C.S., Banks J., Capstick T., Fisher A.J., Gorsuch T., Laurenson I.F., Leitch A., Loebinger M.R., Milburn H.J., Nightingale M., et al. British Thoracic Society guidelines for the management of non-tuberculous mycobacterial pulmonary disease (NTM-PD) Thorax. 2017;72:ii1–ii64. doi: 10.1136/thoraxjnl-2017-210927. [DOI] [PubMed] [Google Scholar]
- 161.Gopalaswamy R., Shanmugam S., Mondal R., Subbian S. Of tuberculosis and non-tuberculous mycobacterial infections—A comparative analysis of epidemiology, diagnosis and treatment. J. Biomed. Sci. 2020;27:1–17. doi: 10.1186/s12929-020-00667-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Lu M., Fitzgerald D., Karpelowsky J., Selvadurai H., Pandit C., Robinson P., Marais B.J. Surgery in nontuberculous mycobacteria pulmonary disease. Breathe. 2018;14:288–301. doi: 10.1183/20734735.027218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.A Brown-Elliott B., Mann L.B., Hail D., Whitney C., Wallace R.J. Antimicrobial Susceptibility of Nontuberculous Mycobacteria From Eye Infections. Cornea. 2012;31:900–906. doi: 10.1097/ICO.0b013e31823f8bb9. [DOI] [PubMed] [Google Scholar]
- 164.Ganapathy U.S., Dartois V., Dick T. Repositioning rifamycins for Mycobacterium abscessus lung disease. Expert Opin. Drug Discov. 2019;14:867–878. doi: 10.1080/17460441.2019.1629414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Griffith D.E. Treatment of Mycobacterium avium Complex (MAC) Semin. Respir. Crit. Care Med. 2018;39:351–361. doi: 10.1055/s-0038-1660472. [DOI] [PubMed] [Google Scholar]
- 166.Koh W.-J., Jeon K., Lee N.Y., Kim B.-J., Kook Y.-H., Lee S., Jo E.-K., Kim C.K., Shin S.J., Huitt G.A., et al. Clinical Significance of Differentiation ofMycobacterium massiliensefromMycobacterium abscessus. Am. J. Respir. Crit. Care Med. 2011;183:405–410. doi: 10.1164/rccm.201003-0395OC. [DOI] [PubMed] [Google Scholar]
- 167.Kim H.-Y., Kim B.J., Kook Y., Yun Y.-J., Shin J.H., Kim B.-J., Kook Y.-H. Mycobacterium massiliense is differentiated from Mycobacterium abscessus and Mycobacterium bolletii by erythromycin ribosome methyltransferase gene (erm) and clarithromycin susceptibility patterns. Microbiol. Immunol. 2010;54:347–353. doi: 10.1111/j.1348-0421.2010.00221.x. [DOI] [PubMed] [Google Scholar]
- 168.Philley J.V., Griffith D.E. Medical Management of Pulmonary Nontuberculous Mycobacterial Disease. Thorac. Surg. Clin. 2019;29:65–76. doi: 10.1016/j.thorsurg.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 169.Martiniano S.L., Wagner B.D., Levin A., Nick J.A., Sagel S.D., Daley C.L. Safety and Effectiveness of Clofazimine for Primary and Refractory Nontuberculous Mycobacterial Infection. Chest. 2017;152:800–809. doi: 10.1016/j.chest.2017.04.175. [DOI] [PubMed] [Google Scholar]
- 170.Ellis D. Amphotericin B: Spectrum and resistance. J. Antimicrob. Chemother. 2002;49:7–10. doi: 10.1093/jac/49.suppl_1.7. [DOI] [PubMed] [Google Scholar]
- 171.Sangalli-Leite F., Scorzoni L., Mesa-Arango A.C., Casas C., Herrero E., Gianinni M.J.S.M., Rodriguez-Tudela J., Cuenca-Estrella M., Zaragoza O. Amphotericin B mediates killing in Cryptococcus neoformans through the induction of a strong oxidative burst. Microbes Infect. 2011;13:457–467. doi: 10.1016/j.micinf.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 172.Sanglard D. Resistance of human fungal pathogens to antifungal drugs. Curr. Opin. Microbiol. 2002;5:379–385. doi: 10.1016/S1369-5274(02)00344-2. [DOI] [PubMed] [Google Scholar]
- 173.Hamill R.J. Amphotericin B Formulations: A Comparative Review of Efficacy and Toxicity. Drugs. 2013;73:919–934. doi: 10.1007/s40265-013-0069-4. [DOI] [PubMed] [Google Scholar]
- 174.Kathiravan M.K., Salake A.B., Chothe A.S., Dudhe P.B., Watode R.P., Mukta M.S., Gadhwe S. The biology and chemistry of antifungal agents: A review. Bioorganic Med. Chem. 2012;20:5678–5698. doi: 10.1016/j.bmc.2012.04.045. [DOI] [PubMed] [Google Scholar]
- 175.Polak A., Scholer H. Mode of Action of 5-Fluorocytosine and Mechanisms of Resistance. Chemother. 1975;21:113–130. doi: 10.1159/000221854. [DOI] [PubMed] [Google Scholar]
- 176.Perfect J.R., Dismukes W.E., Dromer F., Goldman D.L., Graybill J.R., Hamill R.J., Harrison T.S., Larsen R.A., Lortholary O., Nguyen M., et al. Clinical Practice Guidelines for the Management of Cryptococcal Disease: 2010 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2010;50:291–322. doi: 10.1086/649858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Chastain D.B., Henao-Martínez A.F., Franco-Paredes C. Opportunistic Invasive Mycoses in AIDS: Cryptococcosis, Histoplasmosis, Coccidiodomycosis, and Talaromycosis. Curr. Infect. Dis. Rep. 2017;19:36. doi: 10.1007/s11908-017-0592-7. [DOI] [PubMed] [Google Scholar]
- 178.Johansen H.K., Gøtzsche P.C. Amphotericin B versus fluconazole for controlling fungal infections in neutropenic cancer patients. Cochrane Database Syst. Rev. 2014;2014:CD000239. doi: 10.1002/14651858.CD000239.pub2. [DOI] [PubMed] [Google Scholar]
- 179.Wheat L.J., Freifeld A.G., Kleiman M.B., Baddley J.W., McKinsey D.S., Loyd J.E., Kauffman C.A. Clinical Practice Guidelines for the Management of Patients with Histoplasmosis: 2007 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2007;45:807–825. doi: 10.1086/521259. [DOI] [PubMed] [Google Scholar]
- 180.Denning D.W. Echinocandin antifungal drugs. Lancet. 2003;362:1142–1151. doi: 10.1016/S0140-6736(03)14472-8. [DOI] [PubMed] [Google Scholar]
- 181.Cornely O., Bassetti M., Calandra T., Garbino J., Kullberg B., Lortholary O., Meersseman W., Akova M., Arendrup M., Arikan-Akdagli S., et al. ESCMID* *This guideline was presented in part at ECCMID 2011. European Society for Clinical Microbiology and Infectious Diseases. guideline for the diagnosis and management of Candida diseases 2012: Non-neutropenic adult patients. Clin. Microbiol. Infect. 2012;18:19–37. doi: 10.1111/1469-0691.12039. [DOI] [PubMed] [Google Scholar]
- 182.Vazquez J.A. Anidulafungin: A new echinocandin with a novel profile. Clin. Ther. 2005;27:657–673. doi: 10.1016/j.clinthera.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 183.LeDoux M.-P., Guffroy B., Nivoix Y., Simand C., Herbrecht R. Invasive Pulmonary Aspergillosis. Semin. Respir. Crit. Care Med. 2020;41:80–98. doi: 10.1055/s-0039-3401990. [DOI] [PubMed] [Google Scholar]
- 184.Malki M.A., Pearson E. Drug–drug–gene interactions and adverse drug reactions. Pharm. J. 2019;20:355–366. doi: 10.1038/s41397-019-0122-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Philley J.V., Wallace R.J., Benwill J.L., Taskar V., Brown-Elliott B.A., Thakkar F., Aksamit T.R., Griffith D.E. Preliminary Results of Bedaquiline as Salvage Therapy for Patients With Nontuberculous Mycobacterial Lung Disease. Chest. 2015;148:499–506. doi: 10.1378/chest.14-2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Alexander D.C., Vasireddy R., Vasireddy S., Philley J.V., Brown-Elliott B.A., Perry B.J., Griffith D.E., Benwill J.L., Cameron A.D.S., Wallace R.J. Emergence ofmmpT5Variants during Bedaquiline Treatment of Mycobacterium intracellulare Lung Disease. J. Clin. Microbiol. 2016;55:574–584. doi: 10.1128/JCM.02087-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Pavić K., Perković I., Pospisilova S., Machado M., Fontinha D., Prudêncio M., Jampilek J., Coffey A., Endersen L., Rimac H., et al. Primaquine hybrids as promising antimycobacterial and antimalarial agents. Eur. J. Med. Chem. 2018;143:769–779. doi: 10.1016/j.ejmech.2017.11.083. [DOI] [PubMed] [Google Scholar]
- 188.Boelaert J.R., Appelberg R., Gomes M.S., Blasi E., Mazzolla R., Grosset J., Lounis N., Soteriadou K., Thiakaki M., Taramelli D., et al. Experimental Results on Chloroquine and AIDS-Related Opportunistic Infections. JAIDS J. Acquir. Immune Defic. Syndr. 2001;26:300–301. doi: 10.1097/00126334-200103010-00017. [DOI] [PubMed] [Google Scholar]
- 189.Banaschewski B., Verma D., Pennings L.J., Zimmerman M., Ye Q., Gadawa J., Dartois V., Ordway D., Van Ingen J., Ufer S., et al. Clofazimine inhalation suspension for the aerosol treatment of pulmonary nontuberculous mycobacterial infections. J. Cyst. Fibros. 2019;18:714–720. doi: 10.1016/j.jcf.2019.05.013. [DOI] [PubMed] [Google Scholar]
- 190.Thanukrishnan H., Corcoran T.E., Iasella C.J., Moore C.A., Nero J.A., Morrell M.R., McDyer J.F., Hussain S., Nguyen M.H., Venkataramanan R., et al. Aerosolization of Second-generation Triazoles. Transplantion. 2019;103:2608–2613. doi: 10.1097/TP.0000000000002697. [DOI] [PubMed] [Google Scholar]
- 191.Godet C., Goudet V., Laurent F., Le Moal G., Gounant V., Frat J.-P., Cateau E., Cazenave-Roblot F., Cadranel J. Nebulised liposomal amphotericin B for Aspergillus lung diseases: Case series and literature review. Mycoses. 2015;58:173–180. doi: 10.1111/myc.12294. [DOI] [PubMed] [Google Scholar]
- 192.Portell-Buj E., Vergara A., Alejo I., López-Gavín A., Monté M.R., Nicolás L.S., González-Martín J., Tudó G. In vitro activity of 12 antimicrobial peptides against Mycobacterium tuberculosis and Mycobacterium avium clinical isolates. J. Med. Microbiol. 2019;68:211–215. doi: 10.1099/jmm.0.000912. [DOI] [PubMed] [Google Scholar]
- 193.Azimi T., Mosadegh M., Nasiri M.J., Sabour S., Karimaei S., Nasser A. Phage therapy as a renewed therapeutic approach to mycobacterial infections: A comprehensive review. Infect. Drug Resist. 2019;12:2943–2959. doi: 10.2147/IDR.S218638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Millar B.C., Moore J.E. Antimycobacterial strategies to evade antimicrobial resistance in the nontuberculous mycobacteria. Int. J. Mycobacteriology. 2019;8:7–21. doi: 10.4103/ijmy.ijmy_153_18. [DOI] [PubMed] [Google Scholar]
- 195.Simões M.F., Ottoni C.A., Antunes A. Mycogenic Metal Nanoparticles for the Treatment of Mycobacterioses. Antibiotics. 2020;9:569. doi: 10.3390/antibiotics9090569. [DOI] [PMC free article] [PubMed] [Google Scholar]