Abstract.
Hepatitis B virus (HBV) vaccination patterns and the understanding of its risks among healthcare workers (HCWs) is a critical step to decrease transmission. However, the depth of this understanding is understudied. We distributed surveys to HCWs in 12 countries in Africa. Surveys had nine multiple-choice questions that assessed HCWs’ awareness and understanding of HBV. Participants included consultants, medical trainees, nurses, students, laboratory personnel, and other hospital workers. Surveys were completed anonymously. Fisher’s exact test was used for analysis, with a P-value of < 0.05 considered significant; 1,044 surveys were collected from Kenya, Egypt, Sudan, Tanzania, Ethiopia, Uganda, Malawi, Madagascar, Nigeria, Cameroon, Ghana, and Sierra Leone. Hepatitis B virus serostatus awareness, vaccination rate, and vaccination of HCWs’ children were 65%, 61%, and 48%, respectively. Medical trainees had higher serostatus awareness, vaccination rate, and vaccination of their children than HCWs in other occupations (79% versus 62%, P < 0.001; 74% versus 58%, P < 0.001; and 62% versus 45%, P = 0.006, respectively). Cost was cited as the most frequent reason for non-vaccination. West African countries were more aware of their serostatus but less often vaccinated than East African countries (79% versus 59%, P < 0.0001 and 52% versus 60%, P = 0.03, respectively). West African countries cited cost as the reason for non-vaccination more than East African countries (59% versus 40%, P = 0.0003). Our study shows low HBV serostatus awareness and vaccination rate among HCWs in Africa, and reveals gaps in the perception and understanding of HBV prevention that should be addressed to protect HCWs and improve their capacity to control HBV infection.
INTRODUCTION
Infection with hepatitis B virus (HBV) is a leading cause of liver disease worldwide, affecting an estimated 240 million people.1,2 Chronic HBV infection is an important cause of cirrhosis and hepatocellular cancer, leading to significant morbidity and mortality across the globe. Recent data from the Global Burden of Disease Study show that mortality attributable to HBV has risen from 1990 to 2013.3 This is particularly concerning in sub-Saharan Africa where the seroprevalence of HBV is among the highest, with rates of infected individuals greater than 8%.4 Although several countries are beginning to develop protocols to manage the hidden HBV pandemic, overall access to diagnostics and effective treatment remains poor.5,6 Most African countries have implemented early-life vaccination to prevent complications of HBV7,8; however, prevention of infection and vaccination of adults, particularly those at risk, remain inadequate.
Healthcare workers (HCWs) are known to have a higher risk of contracting HBV than the general population because of needle stick injuries and continuous contact with seropositive patients.6 Transmission of HBV via a needle stick injury is thought to be 2% from HBV e antigen negative blood and 19% from e antigen positive blood,9 and this leads to an estimated 66,000 infections among HCWs every year.10 Standard precautions to mitigate this risk are present in many countries. However, full implementation of safe practices is still lacking in low- and middle-income countries, such as those in sub-Saharan Africa,11–15 with estimates showing that about one-third of HCWs are exposed to body fluids every year.16 As such, awareness of this elevated risk of infection and prophylaxis against it are key to minimizing the risk of infection.
Few studies have examined HCWs’ perception of HBV.17–19 This is important as awareness and attitudes of HCWs toward HBV represent a double impact: prevention of HBV infection for HCWs themselves because they are a high-risk population and understanding the overall impact of HBV to properly advise patients in terms of prophylaxis and transmission mitigation. A study from our group in northern Tanzania noted that about 90% of HCWs were not aware of their HBV serostatus and had not been vaccinated for HBV, with these results varying significantly depending on the type of medical occupation.17 A group out of Adama, Ethiopia, obtained survey data from their hospital staff and found that although 75% were aware that working in the hospital would put them at a higher risk of infection, their vaccination rate was only 25%.18 In Yaoundé, Cameroon, 47% of HCWs showed awareness of HBV with significant differences between gender and an overall vaccination rate of 19%.19 All these studies focused on specific populations, and a continent-wide assessment of the understanding of HBV among HCWs in Africa is lacking. Meta-analyses have been carried out on studies performed in individual countries, but differing methodologies and survey questions preclude firm conclusions.20,21 In this study, we aimed to address this gap by performing the first pan-African assessment of HBV awareness among HCWs in the continent.
MATERIALS AND METHODS
Development of a HBV awareness network.
Multiple institutions throughout Africa were approached based on previous publications in the field, identification of interest in the field due to personal conversation or previous email contact, or discussion with trainees in scientific meetings. Individual participants from each institution were contacted via email following identification of interested subjects. Each email was personalized to an individual institution and contained information regarding the purpose of the survey and a specific time line. Following responses to the initial email by interested institutions, further communication was via email or telephone, and surveys were submitted electronically (to be printed) in the preferred language of the participating institution.
Surveys.
We formed a research network aimed at understanding HBV awareness among HCWs and distributed paper surveys across hospitals in 12 countries in Africa as described earlier (Figure 1). All hospitals surveyed are considered teaching institutions with a varying number of clinical residents as well as medical and nursing students. Inclusion to the network was achieved by email invitation to senior employees in hospitals from capital and noncapital cities across the continent. A minimum of 20 surveys and more than two occupations per hospital (physician, nurse, laboratory technician, and so forth) were requested. The survey consisted of nine multiple-choice questions, assessing knowledge of modes of HBV transmission and existing treatment as well as the participants’ awareness of their serostatus and increased risk of disease, vaccination status, reasons for non-vaccination, children’s vaccination status, family members with HBV, occupation, age, and gender (Supplemental Figure 1). To indicate their occupation, participants chose from intern, resident, registrar, consultant, assistant medical officer (AMO), nurse, AMO student, nursing student, laboratory technician, and other occupation not listed. An intern is defined as a person who is in his or her first year of training after finishing medical school. A registrar is defined as someone who has finished intern year and works in a specific specialty but is not a consultant in that specialty. A resident is defined as someone who has finished intern year and is training to be a consultant in a specialty. Henceforth, interns, residents, and registrars are collectively referred to as medical trainees. An AMO is similar to a physician assistant, having completed advanced medical training after working as a clinical officer and then working independently.22 The surveys were written in English, Swahili (regional language of East Africa), and French (one of the official languages of Madagascar). To maximize participation, surveys used simple language and easy-to-follow formatting. They were distributed to medical and nonmedical support staff, with anonymous collection arranged either by drop box or to a staff member collecting surveys.
Figure 1.
Survey distribution by country. Countries included in the study and the number of surveys obtained per country.
Ethical approval.
Participation in the study was voluntary and non-paid. The study was approved by the Ethics Committee of Hennepin Healthcare in Minneapolis, MN, and each center obtained their respective institutional research board approval.
Statistical analysis.
Analyses were performed using Fisher’s exact test, with a P-value of < 0.05 considered significant. For the analysis, Kenya, Sudan, Tanzania, Ethiopia, Uganda, Malawi, and Madagascar were considered part of East Africa, and Nigeria, Cameroon, Ghana, and Sierra Leone were considered part of West Africa. Comparisons were made between the various populations of interest using Statistical Analysis System Enterprise Guide 4.3 (SAS, Cary, NC).
RESULTS
Demographics.
A total of 1,044 surveys were collected from 12 African countries, which included Kenya, Egypt, Sudan, Tanzania, Ethiopia, Uganda, Malawi, Madagascar, Nigeria, Cameroon, Ghana, and Sierra Leone (Table 1). Of all participants, 92% (n = 959) completed the survey in English, 6% (n = 58) in Swahili, and 2% (n = 27) in French. Female participants accounted for 54% (n = 558) of the responders, and the median age of the participants was 30 years (interquartile range [IQR]: 25–37). Twenty-four percent (n = 248) of participants were nurses, 18% (n = 189) medical trainees, 11% (n = 112) laboratory personnel, 16% (n = 162) nursing students and AMO students, 6% (n = 60) consultants, and 4% (n = 38) were AMOs. The remaining 22% (n = 225) were a combination of staff performing different duties in the hospital (janitor, midwife, medical technician, pharmacy technician, and housekeeping). Overall, responses to the survey questions by all participants are presented in Table 2.
Table 1.
Demographics of survey participants
| Survey | 1,044 |
|---|---|
| Completed in English | 959 (92) |
| Completed in Swahili | 58 (6) |
| Completed in French | 27 (2) |
| Female responders | 558 (54) |
| Male responders | 483 (46) |
| Median age (years) (IQR) | 30 (25–37) |
| Nurses | 248 (24) |
| Medical trainees | 189 (18) |
| Laboratory personnel | 112 (11) |
| Nursing students | 82 (8) |
| AMO students | 80 (8) |
| Consultants | 60 (6) |
| AMOs | 38 (4) |
| Other (janitor, midwife, medical technician, pharmacy technician, and housekeeping) | 225 (22) |
AMO = assistant medical officer. Results are expressed as n (%) or median (IQR).
Table 2.
Participant responses regarding HBV
| HBV serostatus aware | 673 (65) |
| Vaccinated against HBV | 627 (61) |
| Cost as a reason for non-vaccination | 167 (46) |
| Lack of awareness as a reason for non-vaccination | 81 (22) |
| Other reasons for non-vaccination | 119 (32) |
| Correct understanding of HBV transmission routes | 881 (84) |
| Family member with HBV | 45 (4) |
| Aware of increased risk of HBV | 988 (95) |
| Children vaccinated | 221 (48) |
| Aware of available treatment for HBV | 689 (66) |
HBV = hepatitis B virus. Results are expressed as n (%).
Hepatitis B virus serostatus awareness.
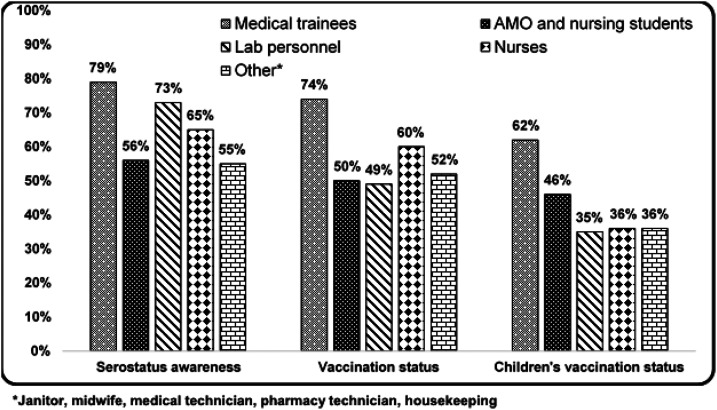
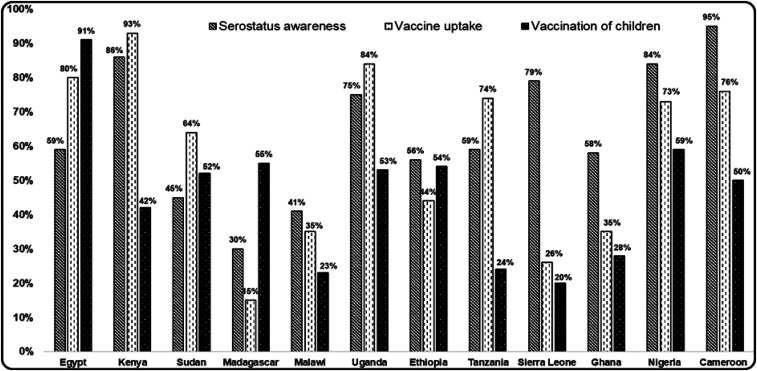
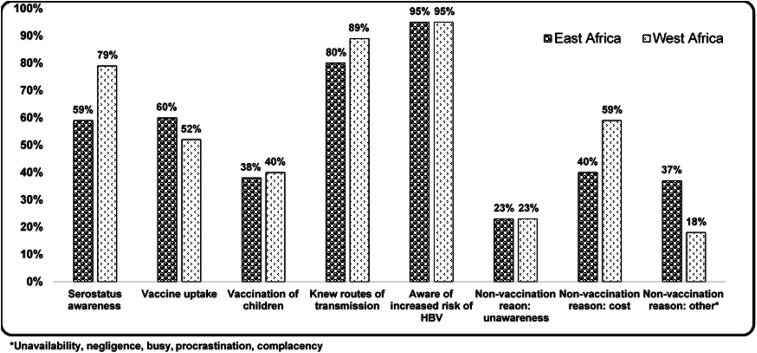
Participant awareness of their HBV serostatus was relatively low at 65% (n = 673) with considerable variability among occupations and geographical location. Medical trainees had the highest awareness and were significantly more aware of their HBV serostatus than those of other occupations combined (79% versus 62%; P < 0.0001, Figure 2). Awareness among students (AMOs and nursing) was significantly lower than that of other occupations combined (56% versus 67%; P = 0.01). Laboratory personnel’s awareness of HBV serostatus was not significantly different from that of other occupations (73% versus 64%; P = 0.06). Serostatus awareness among nurses was not significantly different from that of the rest of the occupations (65% versus 65%; P = 1.0). On performing country-specific analyses, we found a significant variation among countries with regard to HBV serostatus awareness, with the lowest being in Madagascar at 30% and highest in Cameroon at 95% (Figure 3). When this was analyzed geographically, we found that participants in West Africa had a significantly higher serostatus awareness than those from East Africa (79% versus 59%; P < 0.0001, Figure 4).
Figure 2.
Awareness of serostatus, vaccination, and children’s vaccination by occupation. Responses to survey questions of serostatus, vaccination, and children’s vaccination by occupation.
Figure 3.
Participant responses by country. Responses to survey questions on serostatus, vaccine uptake, and vaccination of children by country.
Figure 4.
Comparison of responses between East African (Kenya, Sudan, Tanzania, Ethiopia, Uganda, Malawi, and Madagascar) and West African (Nigeria, Cameroon, Ghana, and Sierra Leone) countries.
Hepatitis B virus vaccination rate.
Vaccination rate among participants averaged 61% (n = 627), with medical trainees having a significantly higher rate of HBV vaccination than people in other occupations (74% versus 58%; P < 0.001, Figure 2). Vaccination rate among students was significantly lower than that among people of other occupations (50% versus 63%; P < 0.01), and laboratory personnel also had a significantly lower rate of vaccination than the rest of the population (49% versus 62%; P = 0.01). Nurses’ vaccination rate was not significantly different from that of people of the rest of the occupations (61% versus 61%; P = 1.0). Country-specific analyses showed that the vaccination rate was lowest in Madagascar at 15% and highest in Kenya at 93% (Figure 3). Interestingly, geographical analysis showed that West African countries had a lower rate of vaccination than East African ones (52% versus 60%; P = 0.03, Figure 4).
Reasons for non-vaccination.
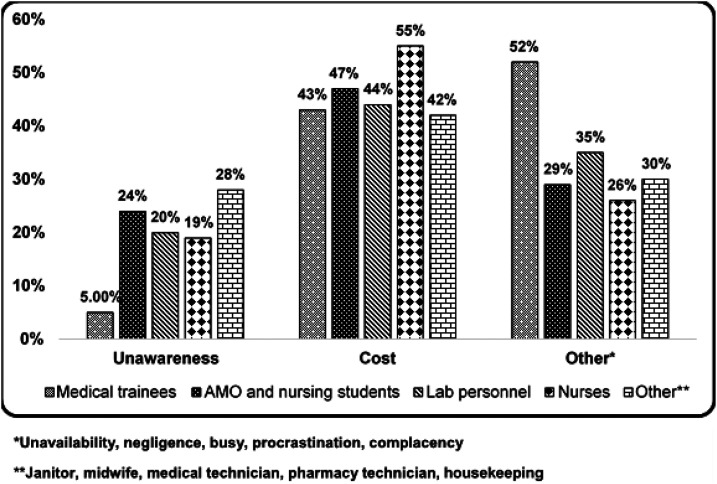
Among the reasons participants provided for non-vaccination, cost was the most frequently cited, at 46% (n = 167), whereas lack of awareness was indicated by 22% (n = 81) of the participants (Table 2). Other reasons such as unavailability, negligence, too busy, procrastination, and complacency accounted for the remaining 32% (n = 119). When analyzed by occupation, medical trainees reported vaccine unawareness significantly less often in comparison to the rest of the occupations combined (5% versus 22%; P = 0.007, Figure 5), but they reported “other reasons” significantly more than the other occupations (52% versus 32%; P = 0.01). None of the occupations reported cost or “other reasons” as a reason for non-vaccination more often than the other occupations combined (Figure 5). When reasons for non-vaccination were compared between West and East Africa, unawareness was not significantly different (22% versus 23%; P = 0.9, Figure 4); however, West Africans cited cost as a reason for non-vaccination more than East Africans (59% versus 40%; P = 0.0003, Figure 5). East Africans were significantly more likely to report “other reasons” for non-vaccination than West Africans (37% versus 18%; P = 0.0002, Figure 4).
Figure 5.
Reasons for not vaccinating based on occupation. Survey participants’ stated reasons for not vaccinating for hepatitis B virus.
Hepatitis B virus vaccination of children.
Among all participants, 50% (n = 516) reported having children, with the vaccination rate among their children being 48% (n = 221) (Table 2). When this was analyzed by occupation, children of medical trainees had a significantly higher rate of vaccination than the rest of the children (62% versus 45%; P = 0.006, Figure 2). The vaccination rate of children of laboratory personnel and nurses was lower than that of children of the other professions, but the difference was not significant (35% versus 50%; P = 0.07 and 41% versus 51%; P = 0.06, respectively). Country-specific analysis showed that children’s vaccination rates varied from a low of 15% in Sierra Leone to a high of 91% in Egypt (Figure 3). Regional analysis showed that the vaccination rate of children of West African HCWs was not significantly different from that of children of East African HCWs (40% versus 38%; P = 0.7, Figure 4).
Understanding of HBV transmission route.
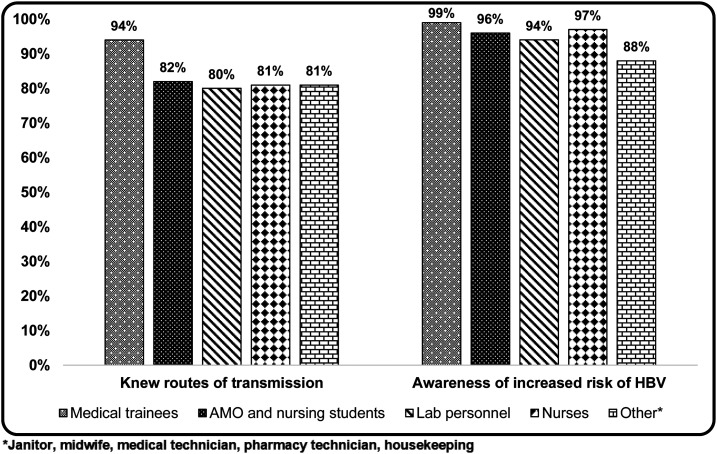
Overall, 84% (n = 881) of the participants correctly identified all routes of transmission (percutaneous, intercourse, and vertical; Table 2). When analyzed by occupation, medical trainees accurately identified all transmission routes significantly more often than people in the rest of the occupations (94% versus 83%; P < 0.0001, Figure 6). Students’ knowledge of transmission routes was not significantly different from that of people in the rest of the occupations (82% versus 85%; P = 0.34), just as there was no significant difference between knowledge of transmission routes for laboratory personnel and nurses (80% versus 85%; P = 0.13 and 81% versus 85%; P = 0.13, respectively). Geographical analysis showed that West African countries properly identified all the routes of transmission significantly more often than East African countries (89% versus 80%; P = 0.0002, Figure 4).
Figure 6.
Awareness of transmission routes and risk of hepatitis B virus (HBV) by occupation. Responses by occupation to survey questions on routes of transmission of HBV and increased risk of HBV.
Awareness of increased risk of HBV due to hospital work.
Of all responders, 95% (n = 988) were aware of their increased risk of contracting HBV due to working in a hospital. Medical trainees and nurses were significantly more aware of that possibility than people in the rest of the occupations (99% versus 95%; P = 0.001 and 98% versus 94%; P = 0.02, respectively, Figure 6). Students’ and laboratory personnel’s awareness rate was not significantly different from that of people in other occupations (96% versus 96%; P = 1.0 and 94% versus 96%; P = 0.32, respectively, Figure 6). There were no significant differences between West African and East African countries related to awareness of increased risk (95% versus 95%, P = 0.9, Figure 4).
DISCUSSION
Chronic hepatitis B infection is a silent disease until it reaches advanced stages (cirrhosis and hepatocellular carcinoma) when therapeutic approaches are limited. This situation is aggravated in many regions of the African continent where resources are limited, HBV rates are high, and access to advanced health care such as liver transplantation is low.23,24 Healthcare workers are at increased risk of contracting HBV and are also in a strategic position to educate patients and raise awareness about the risks of HBV. Because it is a vaccine-preventable disease, understanding the risk factors for HBV and prioritizing vaccination of HCWs in resource-poor areas is critical.
Our study is the first pan-African assessment of HBV awareness among HCWs, and the results are striking. Analyses show that the overall HBV serostatus awareness and vaccination rate among HCWs are low, with significant variability among occupations. Even though more than 95% of participants expressed understanding that working in a hospital increased their risk for HBV infection, there was a surprisingly low degree of HBV serostatus awareness. Our study found that physicians were more likely to be tested and vaccinated for HBV than people in the rest of the occupations (students, nurses, and laboratory personnel). Indeed, physicians were also more likely than people in other occupations to be aware of their increased risk of HBV transmission, to properly know all the routes of transmission, and to be aware of the vaccine, likely explaining their higher serostatus awareness and vaccination rate. These results are consistent with those of a study conducted in Nigeria which found a higher level of knowledge, serostatus awareness, and vaccine uptake among physicians.25 Similar results were obtained at a tertiary care hospital in Dar es Salaam, Tanzania, and in Gondar, Ethiopia, where physicians were more likely to be vaccinated than medical attendants and laboratory personnel.26,27 Taken together, these findings are particularly concerning because outside of surgical specialties, needle stick injuries and contaminated fluid exposure are more likely to occur to nurses and laboratory personnel than to physicians,15,28,29 and thus, those populations are at a higher risk of occupational HBV exposure. Because adults may develop HBV immunity from natural exposure, one reasonable approach could be to withhold HBV vaccination in HCWs until serostatus is determined. However, most hospitals in Africa do not offer HBV screening to HCWs as a standard policy.17 Given this inconsistency and the higher likelihood of needle stick injuries in Africa than elsewhere (due to unsafe needle practices),29 primary prevention alone is not enough. Universal vaccination of HCWs, as the WHO recommends,30 should be thoroughly implemented.
Among reasons participants provided for non-vaccination, cost was cited most often. Likewise, a study from Yaoundé, Cameroon, revealed cost as one of the leading reasons for non-vaccination among HCWs.19 However, this differs from that of a study conducted in Gondar, Ethiopia, where participants stated vaccine unavailability as the major hurdle to vaccination.27 A likely explanation for this trend could be related to geographical variation in HBV vaccine price. As such, it is important to note that our analysis showed that participants from West African countries cited cost as a reason for non-vaccination significantly more than those from East African countries. Thus, higher HBV vaccine prices may have led to the lower rate of vaccination observed in West African participants, despite their higher serostatus awareness and knowledge of routes of transmission. The price of the HBV vaccine, when provided by the Global Alliance for Vaccines and Immunization, has dropped steadily, and in 2010, the cost for one monovalent dose of HBV vaccine was $0.18 U.S. cents.31 However, this is usually the amount paid by health ministries to include the HBV vaccine in childhood immunization programs and not the cost paid by HCWs to obtain the vaccine. In general, vaccine costs vary significantly between countries (and depend on government–pharmaceutical company agreements), and HCWs who are not provided with vaccination by their employer and seek to purchase the vaccine in a private pharmacy face much higher costs.
Our study found a low rate of vaccination among the children of HCWs, with children of physicians again demonstrating a higher rate of vaccination than those in the rest of the occupations. This is concerning because the likelihood of developing chronic HBV is much higher when individuals are exposed at an earlier age,32 and our analysis exposes a generational decrease in HBV vaccination rate from parent to child. Having baseline vaccination rates of children in the countries studied would be useful, but an explanation for the low rate of vaccination in children may be the lack of the birth dose of HBV vaccine. It has been well documented that administration of the first HBV vaccine dose at birth, instead of waiting several weeks after birth (which would increase the number of concurrent injections during future healthcare encounters), decreases parental anxiety and therefore increases the likelihood of completing the HBV vaccine series.33 This policy is lacking in most sub-Saharan countries surveyed, except Nigeria,34 whose vaccination rate was higher than that of the rest of the sub-Saharan countries (59% versus 40%; P = 0.006). However, even in countries where this policy is in place, there are significant barriers to the administration of the birth dose vaccine, such as unavailability of the monovalent HBV vaccine and a high proportion of home births.34 It is possible, however, that a lack of specific understanding of vaccine administration by HCWs could have contributed to a negative answer (i.e., children have been vaccinated but the HCW does not know if it was specifically for HBV because the vaccine was grouped with those against other pathogens during the same visit). Because we did not request vaccination cards for children during the survey, it was not possible to clarify this variable.
Our study has several limitations. Among them is the fact that most of the participating centers are medical institutions in major cities which may skew the data because knowledge and awareness are likely lower in smaller and rural institutions.35 Moreover, we did not keep track of the number of surveys distributed, and there were differences in the number of surveys received from each institution. This prevented us from calculating a response rate, and it could have led to misinterpretation of data from one center that provided a small number of surveys. Also, our study relies on survey data that are self-reported and is thus subject to recall and observational bias by participants. Moreover, the distributed surveys were brief and did not examine in detail the barriers for the lack of awareness or vaccination. We did not perform analysis by age-groups, which could have some utility as well, because it is possible that medical trainees, who are younger, may have a higher likelihood of being vaccinated. Finally, in most of the surveyed countries (apart from Egypt, Uganda, Nigeria, and Tanzania), we received surveys from only one institution. It is unlikely that one institution represents the current situation in the entire country (or city); however, we expect the overall large number of surveys and wide distribution to compensate for this, and provide a comprehensive outlook of the continent.
Our study shows low HBV vaccination rates and serostatus awareness among HCWs across Africa, with geographic variations and differences among occupations. Increasing parity across the continent by raising awareness of HBV and increased utilization of the vaccine among those at risk are vital. However, it is difficult for healthcare providers to educate patients and promote HBV awareness and vaccination if they themselves do not completely understand the risks of HBV and benefits of vaccination. Ample evidence shows that increasing knowledge about the HBV vaccine improves vaccination rates by conveying its efficacy and allaying fears about safety and adverse effects.26,36,37 In fact, participants in our center in Arusha, Tanzania, requested the HBV vaccine from hospital administration after completing the survey and taking part in a HBV awareness seminar. Adding the HBV vaccine to mandatory onboarding requirements when hiring new HCWs would substantially reduce the rate of unvaccinated HCWs. This could be performed within existing hospital infrastructure or by extending the Expanded Program of Immunization, as shown by a study performed in Kenya.38 Last, awareness should be raised to make standard precautions universal to help prevent needle stick injuries and thus transmission of blood-borne diseases such as HBV. In conclusion, our study provides valuable information by revealing gaps in knowledge, awareness, and vaccine availability that should be addressed to improve HCWs ability to prevent HBV infection.
Supplemental tables and figures
Acknowledgment:
We thank André Boonstra (Erasmus MC, Rotterdam, the Netherlands) for critical input of the study and assistance with funding.
Note: Supplemental figure appears at www.ajtmh.org.
REFERENCES
- 1.Tang LSY, Covert E, Wilson E, Kottilil S, 2018. Chronic hepatitis B infection: a review. JAMA 319: 1802–1813. [DOI] [PubMed] [Google Scholar]
- 2.WHO , 2018. Hepatitis B. Geneva, Switzerland: World Health Organization; Available at: https://www.who.int/news-room/fact-sheets/detail/hepatitis-b. Accessed February 12, 2019. [Google Scholar]
- 3.Stanaway JD, et al. 2016. The global burden of viral hepatitis from 1990 to 2013: findings from the Global Burden of Disease Study 2013. Lancet 388: 1081–1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ott JJ, Stevens GA, Groeger J, Wiersma ST, 2012. Global epidemiology of hepatitis B virus infection: new estimates of age-specific HBsAg seroprevalence and endemicity. Vaccine 30: 2212–2219. [DOI] [PubMed] [Google Scholar]
- 5.Cainelli F, 2012. Liver diseases in developing countries. World J Hepatol 4: 66–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spearman CW, et al. Gastroenterology and Hepatology Association of sub-Saharan Africa (GHASSA) , 2017. Hepatitis B in sub-Saharan Africa: strategies to achieve the 2030 elimination targets. Lancet Gastroenterol Hepatol 2: 900–909. [DOI] [PubMed] [Google Scholar]
- 7.Schweitzer A, Akmatov MK, Krause G, 2017. Hepatitis B vaccination timing: results from demographic health surveys in 47 countries. Bull World Health Organ 95: 199–209G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Breakwell L, Tevi-Benissan C, Childs L, Mihigo R, Tohme R, 2017. The status of hepatitis B control in the African region. Pan Afr Med J 27 (Suppl 3): 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewis JD, Enfield KB, Sifri CD, 2015. Hepatitis B in healthcare workers: transmission events and guidance for management. World J Hepatol 7: 488–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prüss-Ustün A, Rapiti E, Hutin Y, 2005. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med 48: 482–490. [DOI] [PubMed] [Google Scholar]
- 11.Stockdale AJ, Geretti AM, 2015. Chronic hepatitis B infection in sub-Saharan Africa: a grave challenge and a great hope. Trans R Soc Trop Med Hyg 109: 421–422. [DOI] [PubMed] [Google Scholar]
- 12.Hutin YJ, Hauri AM, Armstrong GL, 2003. Use of injections in healthcare settings worldwide, 2000: literature review and regional estimates. BMJ 327: 1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO , 2016. WHO Guideline on the Use of Safety-Engineered Syringes for Intramuscular, Intradermal and Subcutaneous Injections in Health Care Settings. Geneva, Switzerland: World Health Organization. [PubMed] [Google Scholar]
- 14.Nsubuga FM, Jaakkola MS, 2005. Needle stick injuries among nurses in sub-Saharan Africa. Trop Med Int Health 10: 773–781. [DOI] [PubMed] [Google Scholar]
- 15.Mashoto KO, Mubyazi GM, Mohamed H, Malebo HM, 2013. Self-reported occupational exposure to HIV and factors influencing its management practice: a study of healthcare workers in Tumbi and Dodoma hospitals, Tanzania. BMC Health Serv Res 13: 276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Auta A, Adewuyi EO, Tor-Anyiin A, Aziz D, Ogbole E, Ogbonna BO, Adeloye D, 2017. Health-care workers’ occupational exposures to body fluids in 21 countries in Africa: systematic review and meta-analysis. Bull World Health Organ 95: 831–841F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Debes JD, Kayandabila J, Pogemiller H, 2016. Knowledge of hepatitis B transmission risks among health workers in Tanzania. Am J Trop Med Hyg 94: 1100–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akibu M, Nurgi S, Tadese M, Tsega WD, 2018. Attitude and vaccination status of healthcare workers against hepatitis B infection in a teaching hospital, Ethiopia. Scientifica (Cairo) 2018: 6705305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tatsilong HO, Noubiap JJ, Nansseu JR, Aminde LN, Bigna JJ, Ndze VN, Moyou RS, 2016. Hepatitis B infection awareness, vaccine perceptions and uptake, and serological profile of a group of health care workers in Yaoundé, Cameroon. BMC Public Health 15: 706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Auta A, Adewuyi EO, Kureh GT, Onoviran N, Adeloye D, 2018. Hepatitis B vaccination coverage among health-care workers in Africa: a systematic review and meta-analysis. Vaccine 36: 4851–4860. [DOI] [PubMed] [Google Scholar]
- 21.Malewezi B, Omer SB, Mwagomba B, Araru T, 2016. Protecting health workers from nosocomial hepatitis B infections: a review of strategies and challenges for implementation of hepatitis B vaccination among health workers in sub-Saharan Africa. J Epidemiol Glob Health 6: 229–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rick TJ, Moshi DD, 2018. The Tanzanian assistant medical officer. JAAPA 31: 43–47. [DOI] [PubMed] [Google Scholar]
- 23.Song E, et al. 2018. Adult liver transplantation in Johannesburg, South Africa (2004–2016): balancing good outcomes, constrained resources and limited donors. S Afr Med J 108: 929–936. [DOI] [PubMed] [Google Scholar]
- 24.Vento S, Dzudzor B, Cainelli F, Tachi K, 2018. Liver cirrhosis in sub-Saharan Africa: neglected, yet important. Lancet Glob Health 6: e1060–e1061. [DOI] [PubMed] [Google Scholar]
- 25.Adekanle O, Ndububa DA, Olowookere SA, Ijarotimi O, Ijadunola KT, 2015. Knowledge of hepatitis B virus infection, immunization with hepatitis B vaccine, risk perception, and challenges to control hepatitis among hospital workers in a Nigerian tertiary hospital. Hepat Res Treat 2015: 439867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aaron D, Nagu TJ, Rwegasha J, Komba E, 2017. Hepatitis B vaccination coverage among healthcare workers at national hospital in Tanzania: how much, who and why? BMC Infect Dis 17: 786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Biset Ayalew M, Adugna Horsa B, 2017. Hepatitis B vaccination status among health care workers in a tertiary hospital in Ethiopia. Hepat Res Treat 2017: 6470658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Adefolalu A, 2014. Needle stick injuries and health workers: a preventable menace. Ann Med Health Sci Res 4 (Suppl 2): S159–S160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sagoe-Moses C, Pearson RD, Perry J, Jagger J, 2001. Risks to health care workers in developing countries. N Engl J Med 345: 538–541. [DOI] [PubMed] [Google Scholar]
- 30.WHO , 2017. Weekly Epidemiological Record. Geneva, Switzerland, World Health Organization. [Google Scholar]
- 31.GAVI.org , 2010. GAVI Impact on Vaccine Market behind Price Drop. Available at: https://www.gavi.org/news/media-room/gavi-impact-vaccine-market-behind-price-drop. [Google Scholar]
- 32.Shimakawa Y, Yan HJ, Tsuchiya N, Bottomley C, Hall AJ, 2013. Association of early age at establishment of chronic hepatitis B infection with persistent viral replication, liver cirrhosis and hepatocellular carcinoma: a systematic review. PLoS One 8: e69430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yusuf HR, Daniels D, Smith P, Coronado V, Rodewald L, 2000. Association between administration of hepatitis B vaccine at birth and completion of the hepatitis B and 4:3:1:3 vaccine series. JAMA 284: 978–983. [DOI] [PubMed] [Google Scholar]
- 34.Lemoine M, Thursz MR, 2017. Battlefield against hepatitis B infection and HCC in Africa. J Hepatol 66: 645–654. [DOI] [PubMed] [Google Scholar]
- 35.Kisangau EN, Awour A, Juma B, Odhiambo D, Muasya T, Kiio SN, Too R, Lowther SA, 2019. Prevalence of hepatitis B virus infection and uptake of hepatitis B vaccine among healthcare workers, Makueni County, Kenya 2017. J Public Health (Oxf) 41: 765–771. [DOI] [PubMed] [Google Scholar]
- 36.Briggs MJ, Thomas J, 1994. Obstacles to hepatitis B vaccine uptake by health care staff. Public Health 108: 137–148. [DOI] [PubMed] [Google Scholar]
- 37.Fatusi AO, Fatusi OA, Esimai AO, Onayade AA, Ojo OS, 2000. Acceptance of hepatitis B vaccine by workers in a Nigerian teaching hospital. East Afr Med J 77: 608–612. [DOI] [PubMed] [Google Scholar]
- 38.Suckling RM, Taegtmeyer M, Nguku PM, Al-Abri SS, Kibaru J, Chakaya JM, Tukei PM, Gilks CF, 2006. Susceptibility of healthcare workers in Kenya to hepatitis B: new strategies for facilitating vaccination uptake. J Hosp Infect 64: 271–277. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.