Abstract
Introduction
Up to one-third of women of reproductive age experience heavy menstrual bleeding (HMB). HMB can give rise to iron deficiency (ID) and, in severe cases, iron-deficiency anemia (IDA).
Aim
To review current guidelines for the management of HMB, with regards to screening for anemia, measuring iron levels, and treating ID/IDA with iron replacement therapy and non-iron-based treatments.
Methods
The literature was searched for English-language guidelines relating to HMB published between 2010 and 2020, using the PubMed database, web searching, and retrieval of clinical guidelines from professional societies.
Results
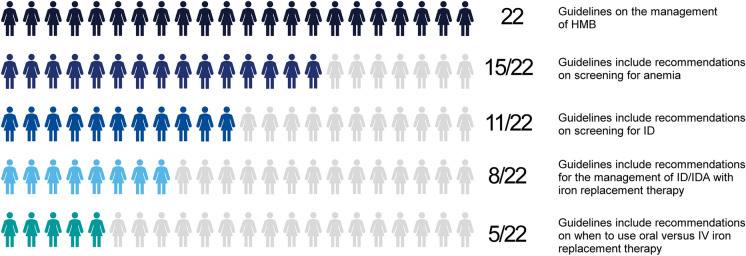
Overall, 55 guidelines mostly originating from North America and Europe were identified and screened. Twenty-two were included in this review, with the majority (16/22) focusing on guidance to screen women with HMB for anemia. The guidance varied with respect to identifying symptoms, the criteria for testing, and diagnostic hemoglobin levels for ID/IDA. There was inconsistency concerning screening for ID, with 11/22 guidelines providing no recommendations for measurement of iron levels and four contrasting guidelines explicitly advising against initial assessment of iron levels. In terms of treatment, 8/22 guidelines provided guidance on iron therapy, with oral iron administration generally recommended as first-line treatment for ID and/or IDA. Four guidelines recommended intravenous iron administration for severe anemia, in non-responders, or before surgery. Three guidelines provided hemoglobin thresholds for choosing between oral or intravenous iron treatment. Four guidelines discussed the use of transfusion for severe IDA.
Conclusion
Many of the guidelines for managing HMB recognize the importance of treating anemia, but there is a lack of consensus in relation to screening for ID and use of iron therapy. Consequently, ID/IDA associated with HMB is likely to be underdiagnosed and undertreated. A consensus guidance, covering all aspects of screening and management of ID/IDA in women with HMB, is needed to optimize health outcomes in these patients.
Keywords: Anemia, Clinical guidelines, Gynecology, Heavy menstrual bleeding, Iron deficiency, Iron-deficiency anemia, Iron treatment, Patient blood management, Women’s health
Plain Language Summary
Women who bleed heavily during menstruation are at risk of iron deficiency and anemia. This can have a negative effect on the well-being of women and can cause serious complications after surgery. Iron is an important part of the hemoglobin in red blood cells that carries oxygen around the body. Bleeding causes iron to be lost from the body. If there is heavy blood loss, iron stores in the body can become low, leading to iron deficiency. If the iron deficiency is severe enough to impair red blood cell production, iron-deficiency anemia can develop. We reviewed the current guidelines for the care of women with heavy menstrual bleeding, focusing on the detection and treatment of iron deficiency and anemia. Most guidelines include routine testing for anemia. Fewer guidelines consider measuring iron levels. Not all the guidelines include advice on the best way to treat iron deficiency and anemia. For those that do, the recommendations vary and sometimes offer conflicting advice. There is little agreement on when to give iron therapy, and whether this should be given by mouth or by infusion. A lack of clear guidance on detecting and treating iron deficiency and anemia caused by heavy menstrual bleeding puts women at risk of being undiagnosed and untreated. To address these concerns, the authors recommend the development of consensus guidelines. These should contain comprehensive recommendations on all aspects of the diagnosis and management of iron deficiency and anemia in women with heavy menstrual bleeding.
Key Summary Points
| Iron deficiency (ID) and iron-deficiency anemia (IDA) can affect the health and quality of life of women with heavy menstrual bleeding (HMB). |
| While anemia is frequently found in this patient group, this review of international guidelines for the management of HMB highlights inconsistencies in the diagnosis and management of IDA, and few guidelines adequately address the need to assess and treat ID. |
| It is proposed that the principles of patient blood management (PBM) in surgical settings could be applied to optimize the care of women with HMB. Recommendations to correct ID/IDA and treat the underlying cause of the excessive bleeding in patients with HMB reflect the PBM principles to treat anemia before surgery and minimize blood loss during surgery. |
| More harmonized, “global” consensus guidelines covering all aspects of managing ID and IDA in women with HMB should be developed as an example of good practice for the management of this condition. |
Digital Features
This article is published with digital features, including a summary slide and plain language summary, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13193969.
Introduction
Heavy menstrual bleeding (HMB) can be defined objectively as a total blood loss per menstrual cycle that regularly exceeds 80 mL [1]. However, a definition requiring quantification of blood loss is only useful for research studies and accurate assessment of menstrual blood flow is difficult. Validated pictorial blood loss assessment charts have been developed, but these are recommended for use in research studies only and have limited value in clinical care [2, 3]. The UK-based National Institute for Health and Care Excellence (NICE) has therefore suggested that HMB should also be diagnosed when there is regularly excessive menstrual blood loss that “affects the physical, social, emotional or material quality of life of the patient” [4, 5]. HMB is estimated to affect approximately 18–38% of women of reproductive age and may increase in prevalence for women approaching menopause [6–12]. However, there is considerable variability in the reporting of HMB, and the condition is likely to be underdiagnosed [6, 13].
Heavy blood loss from menstruation can lead to depletion of iron stores, resulting in iron deficiency (ID) [14]. Prolonged blood loss, such as a menses duration of more than 7 days, or moderate blood loss in combination with an iron-deficient diet, such as often occurs in adolescents and vegans, can also contribute to the risk of depleted iron stores in women [15–17]. Women with HMB lose on average five to six times more iron per menstrual cycle than women with a normal blood loss, resulting in totally depleted iron stores [12]. Iron plays a key role in many physiological processes, including energy production, respiration, DNA synthesis and repair, myocyte function, and cell division [18]. More than two-thirds of the body’s iron is bound as hemoglobin (Hb) within erythroid precursors and mature red blood cells (RBCs) [19]. Severe ID can therefore lead to a fall in Hb levels, impairing RBC production, which in turn gives rise to normocytic or microcytic hypochromic anemia [20]. The World Health Organization (WHO) defines anemia in non-pregnant women (age ≥ 15 years) as a Hb concentration below 12.0 g/dL [21]. ID is the most common cause of anemia and accounts for more than 60% of anemia cases worldwide, with preschool children and girls and women of reproductive age particularly affected [22, 23]. Some 30% of adolescents and women with HMB have been found to have ID (serum ferritin ≤ 15 ng/mL) and 60% iron-deficiency anemia (IDA) [6, 24].
Mild-to-moderate IDA can be asymptomatic. When symptoms are present, they commonly include fatigue, weakness, and shortness of breath [18]. Other symptoms may include headache, pica, hair loss, brittle nails, cold insensitivity, and restless leg syndrome [5, 25]. ID can lead to similar symptoms, and treatment of ID with iron therapy has been shown to improve physical activity and quality of life in patients predisposed to ID due to underlying chronic conditions, such as those with heart failure and inflammatory disease [26–28].
IDA can significantly impair quality of life for women [29], and can lead to reduced cognitive ability and reduced productivity at work [30, 31], as well as increased utilization of healthcare resources [32]. Notably, isolated ID has also been shown to impair cognitive and physical performance in women, and exacerbate fatigue, with the impairments reversed by iron therapy [33–35].
IDA prior to surgery is a risk factor for postsurgical morbidity and mortality, including increased risk of infections, major bleeding, average hospital length of stay, and perioperative blood transfusion in patients of all ages and geographic regions [36–42]. Although less commonly investigated, preoperative ID irrespective of the presence of anemia has been shown to increase the incidence of postoperative mortality, serious adverse events, major cardiac and cerebrovascular events, and use of allogeneic blood transfusions; it also prolongs the length of hospital stay in patients undergoing cardiac surgery [40]. Studies have shown that treatment of ID/IDA prior to surgery can reduce the required number of post-treatment blood transfusions while simultaneously improving hematological parameters [43, 44]. Anemia poses particular challenges when women undergo surgery, particularly for the treatment of their HMB: around 23% of women scheduled for an elective hysterectomy or myomectomy have anemia [39]. Data from an analysis of more than 12,000 women undergoing gynecological surgery in the USA showed that operative morbidity and mortality were increased in those with anemia [36]. Notably, the risks associated with preoperative anemia were not eliminated by perioperative transfusions [36].
Evidence suggests that the diagnosis and effective treatment of ID/IDA in patients with HMB improves health outcomes and quality of life. Iron therapy in menstruating women with ID has been shown to reduce fatigue levels [45, 46], while in patients with ID or IDA, intravenous (IV) iron treatment prior to hysterectomy reduced the prevalence of postoperative anemia and utilization of postoperative blood transfusion compared with no iron treatment [47].
There are a number of national and international guidelines providing recommendations for the management of HMB. In this review, we describe the current recommendations for managing ID and IDA in patients with HMB and identify any gaps where clinical guidance is lacking, or further consensus is required.
Literature Search Methodology
We conducted a literature review to identify guidelines for the management of HMB and evaluated them with regards to screening for anemia and iron status, and managing ID and IDA with iron replacement therapy and non-iron-based treatments.
The literature was searched for all English-language guidelines relating to HMB that were published between 2010 and 2020, using the PubMed database and supplemented with web searching and retrieval of clinical guidelines from professional societies. The PubMed search strategy combined free text and Medical Subject Headings (MeSH) terms related to HMB with search terms to select for guideline articles. The specific terms used were “heavy menstrual bleeding,” “abnormal uterine bleeding,” “menorrhagia,” (“menstrua*” AND (“bleed*” OR “blood loss” OR “Hemorrhag*” OR “Haemorrhag*”)) combined with “guidelines as topic”[MeSH term] OR “guideline”[MeSH term] OR “guidance” OR “guideline*” OR “consensus” OR “statement” OR “recommendation*” OR “delphi” OR “panel” OR “policy” OR “committee”.
Guidelines were excluded if they did not relate to HMB or provided no guidance on the diagnosis and management of HMB. Articles were also excluded if they had been superseded by more up-to-date guidelines.
Using tables, we collated information from the included guidelines on the following prespecified topics of interest: screening for anemia, diagnosis and management of ID/IDA, iron supplementation, non-iron-based strategies to manage ID/IDA, and pharmacological therapies to prevent blood loss from HMB. Areas where consensus was lacking and existing gaps in the guidance were identified and summarized.
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Search Results
In total, 55 potentially relevant guidelines were identified and screened, of which 22 were included in the review.
Characteristics of Included Guidelines
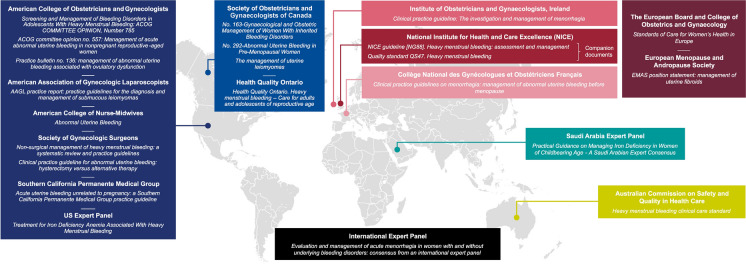
Characteristics of the 22 included guidelines on the management of HMB are summarized in Table 1. Most of the guidelines originated from North America and Europe, with further guidelines from Saudi Arabia, Australia, and an international expert panel (Fig. 1). The guidelines were aimed at a variety of healthcare professionals, including family doctors, gynecologists, nurses, midwives, surgeons, and anesthetists, reflecting the range of settings in which medical professionals encounter women with HMB.
Table 1.
Guidelines included in the review
| Citation | Society | Geographic region | Country | Patient subgroup |
|---|---|---|---|---|
| ACOG Opinion #785 [51] | American College of Obstetricians and Gynecologists | North America | USA | Adolescents with HMB |
| ACOG Opinion #557 [52] | American College of Obstetricians and Gynecologists | North America | USA | AUB |
|
ACOG Practice Bulletin #136 [63] |
American College of Obstetricians and Gynecologists | North America | USA | AUB associated with ovulatory dysfunction |
| AAGL practice report [65] | American Association of Gynecologic Laparoscopists | North America | USA | Uterine fibroids |
| [53] | American College of Nurse-Midwives | North America | USA | AUB |
|
Matteson KA et al. [48] |
Systematic Review Group of the Society of Gynecologic Surgeons | North America/literature review | USA/global | Non-surgical intervention for AUB |
|
Wheeler TL et al. [49] |
Systematic Review Group of the Society of Gynecologic Surgeons | North America/literature review | USA/global | AUB treated with hysterectomy vs. other treatments |
|
Munro MG et al. [54] |
Southern California Permanente Medical Group | North America | USA | AUB |
| Munro MG et al. [5] | US Expert Panel | North America/literature review | USA/global | IDA in women with HMB |
|
Demers C et al. [55] |
Society of Obstetricians and Gynaecologists of Canada | North America | Canada | Gynecological and obstetric management of inherited bleeding disorders |
|
Singh S et al. [56] |
Society of Obstetricians and Gynaecologists of Canada | North America | Canada | AUB |
|
Vilos GA et al. [64] |
Society of Obstetricians and Gynaecologists of Canada | North America | Canada | Uterine fibroids |
| [57] | Health Quality Ontario | North America | Canada | Women and adolescents with HMB |
| Institute of Obstetricians and Gynaecologists [50] | Royal College of Physicians of Ireland | Europe | Ireland | HMB |
| NICE guideline [NG88] [4] | National Institute for Health and Care Excellence | Europe | UK | HMB |
| NICE guideline [QS47] [58] | National Institute for Health and Care Excellence | Europe | UK | HMB |
|
Marret H et al. [61] |
Collège National des Gynécologues et Obstétriciens Français | Europe | France | AUB |
| [88] | The European Board and College of Obstetrics and Gynaecology | Europe | Europe-wide | Menstrual bleeding disorders |
|
Perez-Lopez FR et al. [66] |
European Menopause and Andropause Society | Europe | Europe-wide | Uterine fibroids |
| [59] | Australian Commission on Safety and Quality in Health Care | Australasia | Australia | HMB |
|
James AH et al. [60] |
International Expert Panel | Literature review | Global | HMB with and without underlying bleeding disorders |
|
Arab HA et al. [62] |
Saudi Arabia Expert Panel | Middle East | Saudi Arabia | Iron deficiency |
All guidelines relate to non-pregnant women of reproductive age, unless other specified
AAGL American Association of Gynecologic Laparascopists, ACOG American College of Obstetricians and Gynecologists, AUB abnormal uterine bleeding, HMB heavy menstrual bleeding, IDA iron-deficiency anemia, NICE National Institute for Health and Care Excellence
Fig. 1.
Geographic distribution of guidelines. Most of the guidelines on the management of iron deficiency and iron-deficiency anemia in women with heavy menstrual bleeding originate from Europe and North America
Guideline Recommendations for Diagnosis and Management of ID/IDA
Most of the included guidelines (20/22) provided recommendations on the diagnosis and management of ID and/or IDA. Only two of the included guidelines provided no guidance in relation to ID and IDA; both focused solely on the choice of treatment modality to correct abnormal uterine bleeding, and did not cover the full care continuum [48, 49].
Screening for Anemia
Most guidelines (15/22) included guidance on screening women with HMB for anemia (Table 2) [4, 5, 50–62]. However, the guidance varied with respect to the universal use of screening versus criteria-led testing, identifying relevant symptoms, and diagnostic Hb level. Thirteen guidelines recommended routine initial assessment of Hb levels or a full blood count for all women presenting with HMB [4, 5, 50–60]. Two further guidelines recommended routine assessment of Hb or a full blood count for women with HMB who also met specific criteria—namely an appropriate medical history and/or bleeding score [61], or the presence of physical or psychological symptoms indicative of ID/IDA [62].
Table 2.
Guideline recommendations on screening for anemia in women with HMB
| Citation | Recommends routine screening for anemia (Hb/FBC)? | Recommends screening for anemia (Hb/FBC) in specific groups? | Hb threshold | Recommends routine assessment for symptoms of anemia/ID/IDA? | Recommended symptoms to evaluate |
|---|---|---|---|---|---|
| NICE guideline [NG88] [4] | Y | N/S | N/S | N/S | N/S |
| NICE guideline [QS47] [58] | Y | N/S | N/S | N/S | N/S |
| Munro MG et al. [5] | Y | N/S | < 12 g/dL | N/S | N/S |
| Institute of Obstetricians and Gynaecologists, Ireland [50] | Y | N/S | < 10 g/dL | Y | Breathlessness and postural dizziness, facial, conjunctival, and nail-bed pallor |
|
ACOG Opinion #785 [51] |
Y | N/S | < 12 g/dL | Y | Dermatological signs of anemia and bleeding disorders, including pallor and presence of bruises and petechiae |
|
ACOG Opinion #557 [52] |
Y | N/S | N/S | Y | N/S |
|
American College of Nurse-Midwives [53] |
Y | N/S | N/S | N/S | N/S |
|
Munro MG et al. [54] |
Y | N/S | N/S | N/S | N/S |
|
Demers C et al. [55] |
Y | N/S | N/S | N/S | N/S |
|
Singh S et al. [56] |
Y | N/S | N/S | Y | Shortness of breath with activity, light-headedness |
| Health Quality Ontario [57] | Y | N/S | < 12 g/dL | N/S | N/S |
| Australian Commission on Safety and Quality in Health Care [59] | Y | N/S | N/S | N/S | N/S |
|
James AH et al. [60] |
Y | N/S | N/S | N/S | N/S |
|
Marret H et al. [61] |
N/S | Women with an appropriate medical history and/or bleeding score | N/S | Y | N/S |
|
Arab HA et al. [62] |
N/S | Women with physical or psychological symptoms indicative of ID/IDA | N/S | Y | Fatigue, dizziness, palpitations, hair fall, poor concentration, psychological distress (depression, nightmares, restless leg syndrome), pica |
Fifteen out of 22 guidelines provided recommendations on testing for anemia in women presenting with HMB. Of these, 13 recommend routine assessment for anemia—by means of a FBC/Hb quantification—in all women presenting with heavy menstrual bleeding. A further two guidelines recommend a FBC/Hb quantification in women who fulfill additional criteria
ACOG American College of Obstetricians and Gynecologists, FBC full blood count, Hb hemoglobin, HMB heavy menstrual bleeding, ID iron deficiency, IDA iron-deficiency anemia, N/S not stated, NICE National Institute for Health and Care Excellence
We identified several notable gaps in the guidance around screening for anemia. Of the 15 guidelines that recommended quantification of Hb or a full blood count, only four specified a threshold Hb level indicative of anemia (< 12 g/dL [5, 51, 57] and < 10 g/dL [50], respectively). Although six of the guidelines recommended evaluating symptoms of ID/IDA/anemia during the initial assessment [50–52, 56, 61, 62], only four of these described the specific signs and symptoms of anemia or ID/IDA to check for in the patient [50, 51, 56, 62]. In these four guidelines, pallor [50, 51], shortness of breath with or without activity [50, 56], and light-headedness/dizziness [50, 56, 62] were the most commonly stated signs and symptoms.
Screening for ID
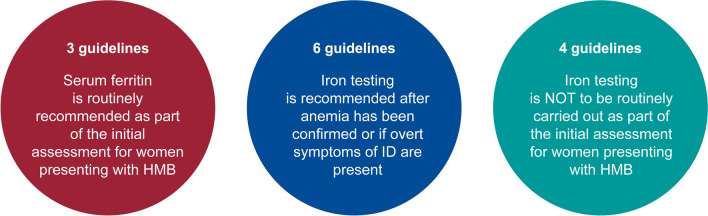
Half of the included guidelines (11/22) provided recommendations around measurement of iron levels in women with HMB (Table 3; Fig. 2) [4, 5, 50–52, 55–57, 59, 60, 62], and only three of these recommended routine assessment of iron levels in individuals presenting with HMB [51, 55, 59]. All three guidelines advised the use of serum ferritin as an indicator of iron status [51, 55, 59].
Table 3.
Guideline recommendations on screening for iron deficiency in women with HMB
| Citation | Recommends first line?a | Advises AGAINST first line?b | Recommends second line?c | Recommends specific ferritin level threshold | Comments |
|---|---|---|---|---|---|
|
ACOG Opinion #785 [51] |
Y (SF) | N | N/S | < 15 μg/L consistent with ID | Relates to management of bleeding disorders in adolescents with HMB |
|
Demers C et al. [55] |
Y (SF) | N | N/S | N/S | Relates to women with inherited bleeding disorders |
| Australian Commission on Safety and Quality in Health Care [59] | Y (SF) | N | N/S | N/S | |
|
Arab HA et al. [62] |
N | N | If ID/IDA suspected | < 30 μg/L for confirmed ID | Recommends assessment of TIBC, hypochromic blood film, and serum sTfR if ferritin is normal, or TSAT if ferritin is increased ID and IDA confirmed if TIBC < 240 μg/dL, hypochromic blood film, and serum sTfR < 2 mg/L, or if TSAT < 20% |
| Institute of Obstetricians and Gynaecologists, Ireland [50] | N | Y | N/S | N/S | |
| NICE guideline [NG88] [4] | N | Y | N/S | N/S | |
|
Singh S et al. [56] |
N | Y | If anemia confirmed | N/S | |
| Health Quality Ontario [57] | N | Y | If patients with anemia do not respond to oral iron therapy/in non-anemic patients with symptoms of ID | < 15 μg/L diagnostic for ID; ≤ 50 μg/L suggestive of ID | Iron therapy can be initiated on the basis of Hb levels from FBC without ferritin testing |
| Munro MG et al. [5] | N/S | N/S | Y |
< 30 μg/L consistent with ID < 10 μg/L consistent with IDA |
Recommends assessment of TSAT if Hb levels are < 12 g/dL, or of erythrocyte morphology (with microcytic hypochromic indicating IDA). ID/IDA confirmed if TSAT < 20% |
|
ACOG Opinion #557 [52] |
N/S | N/S | Y | N/S | |
|
James AH et al. [60] |
N/S | N/S | Y | N/S |
Eleven out of 22 guidelines provided recommendations on the measurement of iron levels in women presenting with HMB, but there were disparities between guidelines in terms of whether this assessment should be first or second line
ACOG American College of Obstetricians and Gynecologists, FBC full blood count, Hb hemoglobin, HMB heavy menstrual bleeding, ID iron deficiency, IDA iron-deficiency anemia, N/S not specified, NICE National Institute for Health and Care Excellence, SF serum ferritin, sTfR soluble transferrin receptor, TIBC total iron-binding capacity, TSAT transferrin saturation
aRecommends routine initial (first-line) assessment of iron levels in women presenting with HMB
bExplicitly advises against routine initial (first-line) assessment of iron levels in women presenting with HMB
cRecommends second-line assessment of iron levels in cases where anemia has been confirmed, or if there are symptoms of overt iron deficiency
Fig. 2.
Guideline recommendations for iron screening. There is high heterogeneity among the guidelines with recommendations for screening iron levels in women with HMB, varying from those that recommend it routinely, those that specifically advise against this practice, and those that recommend iron testing as a second-line investigation. HMB heavy menstrual bleeding, ID iron deficiency. Guidelines referred to: red circle [51, 55, 59], blue circle [5, 52, 56, 57, 60, 62], turquoise circle [4, 50, 56, 57]
In contrast, four guidelines explicitly advised against routine initial assessment of iron levels, citing the limitations of serum ferritin testing [4, 50, 56, 57]. One of these guidelines noted that iron therapy for IDA can be initiated on the basis of Hb levels from a full blood count, without the need for ferritin measurement [57].
Six guidelines, including two that explicitly advised against routine assessment of iron levels, recommended assessment of iron levels as part of second-line or supplementary investigations in cases where anemia had been confirmed or in non-anemic patients with overt symptoms of ID [5, 52, 56, 57, 60, 62]. Three guidelines recommended testing all patients with confirmed anemia for the presence of ID [5, 56, 62], while another recommended testing for ID when anemia did not respond to oral iron therapy [57]. Two guidelines mention tests for serum iron in an additional battery of tests to be considered, but did not specify criteria for conducting them [52, 60].
Finally, four guidelines recommended specific serum ferritin thresholds for diagnosis of ID/IDA, with both < 15 μg/L and < 30 μg/L given as levels consistent with ID [5, 51, 57, 62].
Ferritin is an intracellular glycoprotein that binds iron, and low serum ferritin levels indicate diminished iron stores and thus ID. Serum ferritin tests are easily available, inexpensive to conduct, and an accurate measure of iron levels in women of reproductive age with no concomitant disease. However, as noted in one of the guidelines [51], while low ferritin always indicates low iron stores, serum ferritin may be normal in patients with inflammatory disorders; thus a normal serum ferritin result does not fully rule out ID. While multiple guidelines referred to this limitation of serum ferritin measurement, there was no consensus on which parameters other than serum ferritin to use instead. Suggestions included total iron-binding capacity (TIBC), hypochromic blood film, and serum soluble transferrin receptor (sTfR) if ferritin levels are normal [62], or transferrin saturation (TSAT) if ferritin levels are elevated [62]. Other recommendations included the use of TSAT if Hb levels are < 12 g/dL [5], or to assess erythrocyte morphology and consider a microcytic hypochromic phenotype to be indicative of IDA [5]. The guidelines from Saudi Arabia also recognize that RBCs with a low mean corpuscular volume (microcytosis) or mean corpuscular Hb concentration (hypochromic) may be indicative of ID, and these guidelines recommend testing serum ferritin levels in women suspected of having ID [62].
Management of Iron Deficiency
Only six of the 22 included guidelines recommended treating patients with ID irrespective of the presence or absence of anemia [5, 51, 55, 57, 62, 63], with two also recommending prophylactic oral iron therapy for patients who are asymptomatic but at high risk of developing ID or IDA [62]. Two of the guidelines specifically recommended continuing iron treatment until iron stores are replete [5, 51].
Management of Anemia/IDA: Iron Therapy
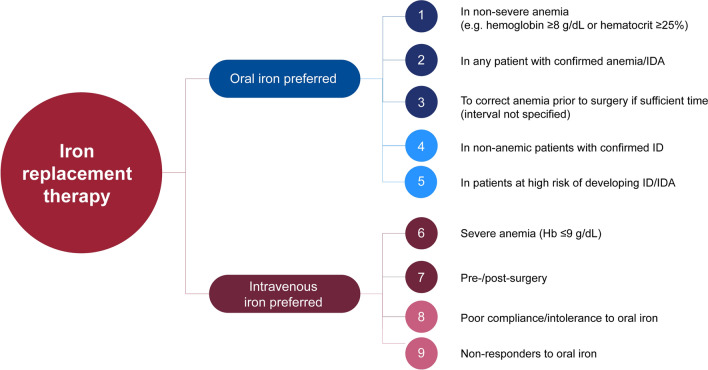
Ten guidelines included recommendations for managing anemia/IDA, all stating that women with IDA should receive iron therapy [5, 51, 53, 55, 57, 58, 61–64]. Strikingly, one of these guidelines provided no guidance on screening for anemia/IDA [63]. Eight of these guidelines gave guidance on providing iron therapy (Table 4; Fig. 3) [5, 51, 53, 55, 57, 62–64]. Five guidelines recommended oral iron administration as the preferred route of treatment if permitted by the patient’s health and circumstances, not only for patients with confirmed ID/IDA but also for those at high risk of developing ID/IDA [5, 51, 57, 62, 63]. If there is sufficient time prior to surgery, oral iron administration can be used to normalize a patient’s Hb [5, 57]. However, both the American College of Obstetricians and Gynecologists and Health Quality Ontario specified that oral iron therapy is only appropriate in cases of non-severe anemia [51, 57].
Table 4.
Guideline recommendations on the use of iron therapy
| Citation | First-line oral iron therapy? | Patient group/circumstance | IV iron therapy? | Patient group/circumstance/first or second line | Threshold Hb level for IV iron therapy |
|---|---|---|---|---|---|
| Munro MG et al. [5] | Y |
In confirmed IDA (Hb < 12 g/dL and MCV low or normal < 100) Prior to surgery if time interval allows |
Y |
First line: if there is a relatively short interval to surgery and SF < 30 ng/mL and/or TSAT < 20% Second line: if Hb does not increase > 1 g/dL with oral iron therapy, and SF < 30 ng/mL and/or TSAT is < 20% |
N/S |
|
ACOG Opinion #785 [51] |
Y | If Hb ≥ 8 g/dL or hematocrit ≥ 25% | Y | Second line: in patients with poor compliance to oral iron therapy | N/S |
| Health Quality Ontario [57] | Y | In ID or any confirmed anemia (with Hb > 9 g/dL), including prior to surgery | Y |
First line: to correct severe anemia, including before and after surgery First line: prior to surgery, particularly if in need of rapid correction, to increase Hb > 12 g/dL Second line: if unresponsive or intolerant to oral iron therapy |
Hb ≤ 9 g/dL |
|
Arab HA et al. [62] |
Y |
In confirmed ID or IDA In women who are asymptomatic but at high risk of ID or IDA |
Y |
First line: prior to surgery/after GI or bariatric surgery First line: in those who express a preference for IV iron therapy, at the treating physician’s discretion Second line: in poor/non-respondersa or those intolerant to oral iron therapy Second line: if Hb does not increase by 2 g/dL and/or SF remains < 30 ng/mL after 3 months of oral iron therapy |
Hb < 8 g/dL |
|
ACOG Opinion #136 [63] |
Y | In confirmed ID or IDA | Y | Second line: in non-responders to oral iron therapy | N/S |
|
American College of Nurse-Midwives [53] |
N/Sb | In anemia | |||
|
Demers C et al. [55] |
N/Sb | In confirmed ID or anemia | |||
|
Vilos GA et al. [64] |
N/Sb | Preoperatively in patients with anemia undergoing surgery for uterine fibroids | |||
Eight out of 22 guidelines provided recommendations on the use of iron therapy in women presenting with HMB. Oral iron therapy is recommended as first-line treatment if patient health and circumstances permit. Intravenous iron therapy is recommended in preference to, or subsequent to, oral iron therapy depending on circumstances
ACOG American College of Obstetricians and Gynecologists, GI gastrointestinal, Hb hemoglobin, HMB heavy menstrual bleeding, ID iron deficiency, IDA iron-deficiency anemia, IV intravenous, MCV mean corpuscular volume, N/S not stated, SF serum ferritin, TSAT transferrin saturation
aWomen with a 1% increase in reticulocyte count and an improvement in Hb by 0.5 g/dL after 30 days are considered responders and should continue on oral iron therapy for 2 further months
bGuidelines do not specify whether iron therapy should be oral or intravenous
Fig. 3.
Patient populations in which iron replacement therapy is recommended by guidelines. Oral iron administration is the preferred route of treatment if permitted by the patient’s health and circumstances, both for patients with confirmed ID/IDA and patients classified at risk of developing ID/IDA. IV iron therapy is most commonly recommended in patients who do not respond, cannot tolerate, or do not comply with oral iron administration, before and after surgery and in patients with severe anemia. ID iron deficiency, IDA iron-deficiency anemia. Guidelines referred to: (1) [51, 57], (2) [5, 62, 63], (3) [5, 57], (4) [57, 62, 63], (5) [62], (6) [57], (7) [5, 57, 62], (8) [51, 57, 62], (9) [5, 57, 62, 63]
Similarly, only five guidelines provide recommendations on the use of IV iron therapy in preference to oral iron therapy, and this was advised as a first-line strategy under certain circumstances—including clinical scenarios warranting immediate correction of anemia, such as imminent surgery [5, 57, 62], or following gastrointestinal or bariatric surgery [62]. IV iron treatment was also recommended for patients with severe anemia and a Hb level ≤ 9 g/dL [57]. Guidelines also recommended IV iron therapy as a second-line treatment in patients with poor compliance and/or intolerance to oral iron therapy [51, 57, 62], as well as in those who did not respond to oral iron therapy [5, 57, 62, 63].
There was a notable lack of guidance around how to select patients for oral versus IV iron therapies, with only Health Quality Ontario recommending a specific threshold of 9 g/dL for use of IV iron administration [57]. In several instances, guidelines did not specify whether iron should be given orally or IV in women diagnosed with ID/IDA [53, 55, 64].
Non-Iron-Based Correction of ID/IDA
Four guidelines recommended blood transfusion for severe anemia, and all recommended basing the treatment decision on the severity of anemia and/or patient symptoms (Table 5) [5, 51, 57, 62]. Specifically, one guideline stated that transfusion should only be used in cases of acute hemorrhage or hemodynamic instability [5]; one recommended basing the decision to transfuse on the severity of symptoms (with transfusion recommended in patients with hypotension, chest pain, syncope or tachycardia [57]), and two recommended that Hb levels should be examined in addition to symptoms [51, 62]. The recommended Hb threshold varied, with one guideline advising consideration of transfusion as a first approach to treatment if Hb levels are < 6 g/dL in symptomatic patients or < 5 g/dL in those who are asymptomatic [62], while a second guideline noted that otherwise healthy adolescents may tolerate Hb levels < 7 g/dL, and stated that the decision to transfuse should not be based solely on Hb levels but should also consider hemodynamic status [51].
Table 5.
Guideline recommendations regarding non-iron-based management of HMB
| Citation | Transfusion | Dietary interventions |
|---|---|---|
|
ACOG Opinion #785 [51] |
If Hb < 7 g/dL In hemodynamically unstable patients/presence of active bleeding |
First-line therapy and long-term management: oral iron administration plus dietary optimization |
|
Arab HA et al [62] |
In asymptomatic patients if Hb < 5 g/dL In symptomatic patients if Hb < 6 g/dL |
Increasing consumption of foods rich in heme iron |
| Health Quality Ontario [57] | With severe symptoms of anemia | N/S |
| Munro MG et al. [5] | In acute hemorrhage/hemodynamic instability | N/S |
|
American College of Nurse-Midwives [53] |
N/S | Nutrition counseling and iron replacement |
Five out of 22 guidelines provided recommendations on the use of non-iron-based management of ID/IDA in women presenting with HMB. Transfusion is sometimes recommended in cases of severe anemia, especially in the event of hemodynamic instability [5, 51, 57, 62]. Dietary interventions may be considered alongside other approaches [51, 53, 62]
ACOG American College of Obstetricians and Gynecologists, Hb hemoglobin, HMB heavy menstrual bleeding, ID iron deficiency, IDA iron-deficiency anemia, N/S not stated
Iron intake may also be boosted through dietary interventions such as increasing consumption of foods rich in heme iron (clams, oysters, shrimp, sardines, liver, red meat), and reducing consumption of foodstuffs that can block iron absorption, including tea and coffee [62]. However, dietary intervention was only recommended in conjunction with iron therapy [51, 53, 62].
Treatments to Reduce Blood Loss from HMB
Several guidelines included recommendations for medical treatments to reduce blood loss from HMB by addressing the underlying cause (Table 6) [4, 5, 51, 54, 56, 57, 63–66]. Hormonal treatments were commonly recommended [4, 5, 51, 54, 56, 57, 63–66]. The 52 mg levonorgestrel-releasing intrauterine system (LNG-IUS) was the most consistently recommended hormonal treatment approach [4, 5, 51, 56, 57, 63, 64, 66], with the UK-based NICE recommending to consider an LNG-IUS as first-line treatment for women with HMB but no identified pathology, uterine fibroids < 3 cm in diameter, or suspected or diagnosed adenomyosis [4]. Other progestogen-only methods, such as depot medroxyprogesterone acetate, and combined oral contraceptive pills (estrogens plus progestogen), can also markedly reduce HMB [4, 5, 51, 56, 57, 63, 64], including in adolescents [51]. Gonadotropin-releasing hormone (GnRH) analogues may be used as a short-term solution to boost iron stores in women due to undergo surgery [54, 56, 64–66] or in those who are experiencing HMB as a result of uterine fibroids [64, 66]. One set of guidelines also recommended considering the use of GnRH analogues to reduce HMB in women in whom other medical or surgical treatment options had failed or were contraindicated [56]. Selective progesterone receptor modulators (SPRM) may also be used in the short term to correct anemia in patients with fibroids [64, 66]. However, ulipristal, the only licensed SPRM in the USA and the European Union, had its European license withdrawn in March 2020 because of safety issues [66, 67].
Table 6.
Guideline recommendations regarding pharmacological treatment of HMB
| Citation | Medications | ||||
|---|---|---|---|---|---|
| LNG-IUS | GnRH | SPRM | Combined oral contraceptives/progestogensa | Non-hormonalb | |
|
ACOG Opinion #785 [51] |
Y | N/S | N/S | Y | N/S |
| Health Quality Ontario [57] | Y | N/S | N/S | Y | Y |
| Munro MG et al. [5] | Y | Pre-surgery | N/S | Y | Y |
|
Munro MG et al. [54] |
N/S | Pre-surgery | N/S | Y | In cyclical HMB |
|
Singh S et al. [56] |
Y | Pre-surgery | N/S | Y | In cyclical HMB |
|
Vilos GA et al. [64] |
Y | Pre-surgery | Short-term use | Y | N/S |
| AAGL practice report [65] | N/S | Pre-surgery | N/S | N/S | N/S |
| NICE guideline [NG88] [4] | Y | N/S | N/S | Y | If women are unsuitable for LNG-IUS |
|
Perez-Lopez FR et al. [66] |
Y | Pre-surgery | Short-term use | Y | Y |
|
ACOG Practice Bulletin #136 [63] |
Y | N/S | N/S | Y | N/S |
Ten out of 22 guidelines provided recommendations on the use of medications (hormonal and/or non-hormonal) to minimize or reduce the bleeding in women presenting with HMB
AAGL American Association of Gynecologic Laparascopists, ACOG American College of Obstetricians and Gynecologists, GnRH gonadotropin-releasing hormone agonist, HMB heavy menstrual bleeding, LNG-IUS levonorgestrel-releasing intrauterine system, N/S not stated, NICE National Institute for Health and Care Excellence, SPRM selective progesterone receptor modulator
aProgestogens include medroxyprogesterone acetate
bNon-hormonal treatments include non-steroidal anti-inflammatory drugs (NSAIDs) or anti-fibrinolytic agents
Non-hormonal treatments are recommended for reducing blood loss from HMB in patients in whom hormonal treatment is not appropriate or desirable [4], as a second-line option after hormonal treatment [4], or as first-line treatment in patients with abnormal uterine function or fibroids [66]. The most frequently recommended options were non-steroidal anti-inflammatory drugs (NSAIDs) and antifibrinolytic agents such as tranexamic acid [4, 5, 54, 56, 57, 66]. Non-hormonal treatments were considered particularly effective in controlling HMB for women with more predictable periods and in those who are planning a pregnancy [54, 56].
Discussion
This is the first review to summarize guideline recommendations for the diagnosis and management of ID, IDA, and anemia in women with HMB. We have identified several gaps in these guidelines and areas where consensus is needed (Fig. 4).
Fig. 4.
Summary of guideline coverage for the diagnosis and management of ID/IDA in women with HMB. There are many gaps in the current guidelines regarding the diagnosis and management of ID and IDA in patients with HMB. HMB heavy menstrual bleeding, ID iron deficiency, IDA iron-deficiency anemia, IV intravenous
Over half (15/22) of the current guidelines recommend routine screening for anemia in women with HMB, recognizing this as a common consequence of heavy and/or prolonged menstrual bleeding. However, discrepancies were noted in the recommended diagnostic Hb thresholds and ID/IDA symptoms. In particular, there was a notable gap around Hb thresholds, with only two guidelines stating Hb cutoffs indicative of anemia (< 10 g/dL and < 12 g/dL, respectively) [50, 57].
Half of the guidelines (11/22) provided guidance on testing iron levels in women with HMB. Only a small number of guidelines currently recommend routine measurement of iron levels in patients with HMB and a similar number recommend against this practice, indicating a lack of consensus on this topic. Routine full blood counts are more widely recommended than iron tests, with iron tests most often featuring as second-line investigations if anemia is detected. Equally, not all guidelines recommend follow-up of anemia cases to determine causative ID. As an example, one set of guidelines recommends initiating iron therapy for IDA based on a full blood count, without the need for ferritin measurement, and recommends testing for ID only when anemia does not respond to oral iron therapy [57]. Consequently, most guidelines recommending only full blood counts will miss diagnosis of ID.
While the limitations of measuring serum ferritin as a proxy for iron levels were cited in several guidelines, there was no consensus on an optimal alternative (potential candidates include TIBC, serum sTfR, and TSAT). In the recently released WHO guidelines, ferritin concentration is strongly recommended as a good marker to diagnose iron deficiency in otherwise healthy individuals [68]. The WHO also specifies a cutoff threshold of < 15 μg/L, which is cited by the American College of Obstetricians and Gynecologists guidelines on HMB management and concurs with the recommendations by Health Quality Ontario. Conversely, this is lower than the < 30 μg/L threshold given by the Saudi Arabian and US expert panel guidelines [5, 62]. This higher threshold is supported by the evidence that ferritin < 30 μg/L has a 98% sensitivity and 92% specificity for detecting ID in patients with anemia [69]. As well as the uncertainty surrounding the most accurate parameter to measure, the paucity of recommendations to test for iron levels in women with HMB may reflect a lack of understanding regarding the benefits of treating ID in the absence of anemia.
We also identified a lack of guidance for the use of iron therapy, with only 8/22 guidelines providing some recommendations on this topic. This is somewhat surprising, given that iron therapy has been shown in multiple settings to be effective in women with HMB [70–75]. This may be because the guidelines are often targeted at specialists treating HMB, covering the diagnosis of ID/IDA as part of the HMB workup on the assumption that patients will then be referred to the family practitioner for treatment of any diagnosed ID/IDA. For this reason, there are often separate guidelines available on the management of ID/IDA that are not targeted to a specialty or patient group. Among the eight guidelines providing some recommendation, further guidance is required on when IV iron therapy is appropriate and what Hb thresholds should be used to choose between the use of oral and IV iron therapies. Generally, when ID or IDA is confirmed, oral iron administration is recommended in HMB guidelines as first-line treatment, with IV iron administration advised in patients who cannot tolerate or do not respond to oral iron therapy. However, it is common for oral iron therapy to be poorly tolerated because of gastrointestinal side effects, which often results in poor adherence [76]. It is also notable that oral iron therapy has a limited capacity to restore iron levels when there is moderate to severe anemia, in which case IV iron therapy is required to achieve rapid and complete restoration of Hb levels [77]. Several guidelines recommend the preferred use of IV iron therapy when patients require rapid elevation of Hb levels, but this is restricted to particular criteria, such as prior to imminent surgery [5, 57, 62]. Notably, dietary intervention was recommended by three guidelines and only in conjunction with iron therapy.
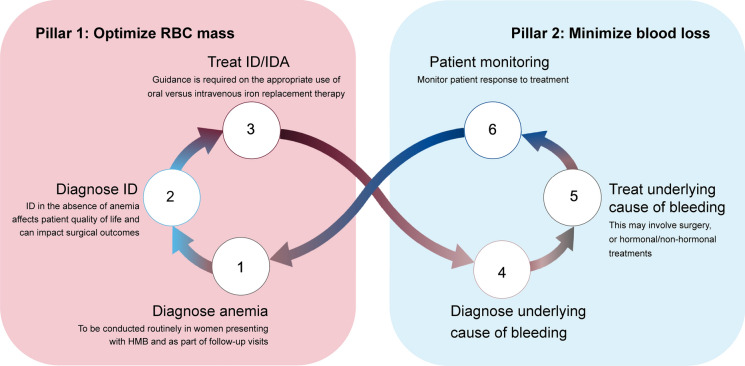
Given the growing awareness that ID as well as anemia can negatively impact surgical outcomes [36–42], and the current recommendations to screen for and treat anemia and ID in patients undergoing gynecological surgery [78], only four guidelines discuss the treatment of ID/IDA prior to surgery [5, 51, 57, 62]. Importantly, in recommending correction of ID/IDA prior to surgery, these guidelines align with the first pillar of patient blood management (PBM) recommended in the wider surgical setting, which advocates treatment of preoperative anemia and optimization of RBC mass prior to surgery (Fig. 5) [79]. When combined with pillars 2 and 3 to minimize blood loss and improve postoperative tolerance of mild or moderate anemia, restrictive transfusion protocols can have similar or better clinical outcomes than liberal use of transfusion [80]. PBM is increasingly being adopted as a way to improve patient outcomes and reduce transfusion requirements and costs [81, 82]. The use of PBM to reduce the global usage of blood transfusions becomes increasingly important when global blood supplies are restricted—for example during pandemics such as the recent COVID-19 pandemic, which halted blood collections and reduced the eligible donor population [83]. PBM has demonstrated success as a strategy to reduce transfusions in anemic women undergoing gynecological surgery [84]. In a study of eight women with HMB undergoing gynecological surgery who refused blood transfusions, severe anemia (Hb < 5 g/dL) either pre- or postoperatively could be effectively managed with IV iron therapy and erythropoiesis-stimulating agents [85] alone. As part of pillar 1 of PBM, it is recommended to screen for anemia once patients are scheduled for surgery, inform patients about the risks of preoperative anemia and benefits of treatment, and treat ID/IDA and replenish iron stores before surgery [79].
Fig. 5.
How treatment of ID/IDA in women with HMB could fit within the “3 pillars” principles of patient blood management. Recommendations to correct ID/IDA in patients with HMB align with pillar 1 of PBM recommendations in surgical settings, which advocates treatment of preoperative anemia and optimization of red blood cell mass prior to surgery. The care of women with HMB could also incorporate pillar 2 of PBM, which aims to minimize blood loss. In HMB, this would involve treatment of the underlying cause of the excessive bleeding. HMB heavy menstrual bleeding, ID iron deficiency, IDA iron-deficiency anemia, IV intravenous, PBM patient blood management, RBC red blood cell
About half of the included guidelines provided advice on pharmacological therapies to minimize or reduce blood loss from HMB. The 52 mg LNG-IUS was the most frequently recommended medical intervention; otherwise, there was generally a lack of consensus across guidelines with regard to recommendations for pharmacological interventions. Where pharmacological intervention is recommended to reduce blood loss, guidance on iron supplementation to restore iron levels is often missing. For example, it can take over a year for serum ferritin levels to normalize in patients with HMB treated with an LNG-IUS, yet quality of life could be improved more quickly with immediate iron supplementation [86, 87].
Limitations of the review include that, despite searching for relevant guidelines from across the world, only those published in the English language and easily accessible through societal websites or web searching were included. This may have excluded guidance documents available locally and not necessarily publicly available. The retrieved guidelines mostly originated from high- or upper-middle-income countries in North America and Europe, and our findings are applicable only to the countries/regions covered by these guidelines. The guidelines examined were often targeting a specialist audience, focusing on an area of expertise rather than the holistic care of patients with HMB (e.g., gynecologists who would be most concerned with preventing bleeding rather than treating ID/IDA). Strengths of our approach include the comprehensive evaluation of relevant guidelines based on prespecified criteria.
Conclusions
Given the gaps and inconsistencies identified in the current guidelines, ID and IDA are likely to be underdiagnosed and undertreated in patients with HMB. One of the challenges to managing women with HMB is the involvement of multiple healthcare practitioners without clear guidance for those ultimately responsible for identifying and treating the resultant ID/IDA. There needs to be a consensus HMB guidance to cover all aspects of care, to improve health outcomes in these patients.
Acknowledgements
Funding
Funding for this review and the Rapid Service and Open Access Fees were provided by Vifor Pharma Group (Glattbrugg, Switzerland).
Medical Writing and Editorial Assistance
Medical writing support (including performing the literature search, development of a draft outline and subsequent drafts in consultation with the authors, collating author comments, copyediting, fact checking and referencing) was provided by Julianna Solomons at Aspire Scientific (Bollington, UK). This assistance was funded by Vifor Pharma Group (Glattbrugg, Switzerland).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
All authors made substantial contributions to the conception and design of the review and the analysis, or interpretation of data for the review; drafted the review or revised it critically for important intellectual content; provided final approval of the version to be published; and agree to be accountable for all aspects of the review in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosures
Diana Mansour has received financial support to attend pharmaceutical advisory board meetings, undertake research studies, to speak at educational meetings/webinars/conferences along with travel grants from Bayer, MSD, Mithra, Mylan, Pfizer, and Vifor Pharma in the last 5 years.
Axel Hofmann has not received any financial support in connection with this work. He has received fees and honoraria for consulting as well as financial support to attend pharmaceutical advisory board meetings, speak at educational meetings/webinars/conferences along with travel grants outside this work from Instrumentation Laboratories/Werfen, Celgene, G1 Therapeutics, Takeda and Vifor Pharma.
Kristina Gemzell-Danielsson reports support to attend pharmaceutical advisory boards, to give lectures or for her hospital to conduct clinical trials from MSD/Merck, Bayer AG, Gedeon Richter, Exeltis, Myovant, Azanta, RemovAid, Actavis, HRA-Pharma, Campus Pharma, Exelgyn, Mithra, and Ferring.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
References
- 1.Sriprasert I, Pakrashi T, Kimble T, Archer DF. Heavy menstrual bleeding diagnosis and medical management. Contracept Reprod Med. 2017;2:20. doi: 10.1186/s40834-017-0047-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Magnay JL, O'Brien S, Gerlinger C, Seitz C. A systematic review of methods to measure menstrual blood loss. BMC Womens Health. 2018;18:142. doi: 10.1186/s12905-018-0627-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Magnay JL, O'Brien S, Gerlinger C, Seitz C. Pictorial methods to assess heavy menstrual bleeding in research and clinical practice: a systematic literature review. BMC Womens Health. 2020;20:24. doi: 10.1186/s12905-020-0887-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Institute for Health and Care Excellence (NICE). NICE guideline [NG88]. Heavy menstrual bleeding: assessment and management. 2020. https://www.nice.org.uk/guidance/ng88. Accessed June 23 2020. [PubMed]
- 5.Munro MG, Boccia R, Friedman AJ, et al. Treatment for iron deficiency anemia associated with heavy menstrual bleeding. 2019. https://www.mdedge.com/obgyn/article/208888/gynecology/treatment-iron-deficiency-anemia-associated-heavy-menstrual-bleeding. Accessed October 31 2019.
- 6.Fraser IS, Mansour D, Breymann C, Hoffman C, Mezzacasa A, Petraglia F. Prevalence of heavy menstrual bleeding and experiences of affected women in a European patient survey. Int J Gynaecol Obstet. 2015;128:196–200. doi: 10.1016/j.ijgo.2014.09.027. [DOI] [PubMed] [Google Scholar]
- 7.Karlsson TS, Marions LB, Edlund MG. Heavy menstrual bleeding significantly affects quality of life. Acta Obstet Gynecol Scand. 2014;93:52–57. doi: 10.1111/aogs.12292. [DOI] [PubMed] [Google Scholar]
- 8.Santos IS, Minten GC, Valle NC, et al. Menstrual bleeding patterns: a community-based cross-sectional study among women aged 18–45 years in Southern Brazil. BMC Womens Health. 2011;11:26. doi: 10.1186/1472-6874-11-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Omani Samani R, Almasi Hashiani A, Razavi M, et al. The prevalence of menstrual disorders in Iran: a systematic review and meta-analysis. Int J Reprod Biomed (Yazd) 2018;16:665–678. [PMC free article] [PubMed] [Google Scholar]
- 10.Ding C, Wang J, Cao Y, et al. Heavy menstrual bleeding among women aged 18–50 years living in Beijing, China: prevalence, risk factors, and impact on daily life. BMC Womens Health. 2019;19:27. doi: 10.1186/s12905-019-0726-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kocaoz S, Cirpan R, Degirmencioglu AZ. The prevalence and impacts heavy menstrual bleeding on anemia, fatigue and quality of life in women of reproductive age. Pak J Med Sci. 2019;35:365–370. doi: 10.12669/pjms.35.2.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Napolitano M, Dolce A, Celenza G, et al. Iron-dependent erythropoiesis in women with excessive menstrual blood losses and women with normal menses. Ann Hematol. 2014;93:557–563. doi: 10.1007/s00277-013-1901-3. [DOI] [PubMed] [Google Scholar]
- 13.Nelson AL, Ritchie JJ. Severe anemia from heavy menstrual bleeding requires heightened attention. Am J Obstet Gynecol. 2015;213(97):e1–e6. doi: 10.1016/j.ajog.2015.04.023. [DOI] [PubMed] [Google Scholar]
- 14.Breymann C, Auerbach M. Iron deficiency in gynecology and obstetrics: clinical implications and management. Hematology Am Soc Hematol Educ Program. 2017;2017:152–159. doi: 10.1182/asheducation-2017.1.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Milman N, Rosdahl N, Lyhne N, Jorgensen T, Graudal N. Iron status in Danish women aged 35–65 years. Relation to menstruation and method of contraception. Acta Obstet Gynecol Scand. 1993;72:601–605. doi: 10.3109/00016349309021150. [DOI] [PubMed] [Google Scholar]
- 16.UK National Health Service. Heavy periods - overview. 2020. https://www.nhs.uk/conditions/heavy-periods/#overview. Accessed May 1 2020
- 17.Hercberg S, Preziosi P, Galan P. Iron deficiency in Europe. Public Health Nutr. 2001;4:537–545. doi: 10.1079/phn2001139. [DOI] [PubMed] [Google Scholar]
- 18.Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372:1832–1843. doi: 10.1056/NEJMra1401038. [DOI] [PubMed] [Google Scholar]
- 19.Andrews NC. Disorders of iron metabolism. N Engl J Med. 1999;341:1986–1995. doi: 10.1056/NEJM199912233412607. [DOI] [PubMed] [Google Scholar]
- 20.National Institute for Health and Care Excellence (NICE). Clinical knowledge summary. Anaemia - iron deficiency. 2018. https://cks.nice.org.uk/anaemia-iron-deficiency#!topicSummary. Accessed June 23 2020.
- 21.World Health Organization et al. Worldwide prevalence of anaemia 1993–2005. In: de Benoist B, et al., editors. WHO global database on anaemia. Geneva: World Health Organization; 2008. [Google Scholar]
- 22.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kassebaum NJ, GBD 2013 Anemia Collaborators The global burden of anemia. Hematol Oncol Clin North Am. 2016;30:247–308. doi: 10.1016/j.hoc.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 24.Wang W, Bourgeois T, Klima J, Berlan ED, Fischer AN, O'Brien SH. Iron deficiency and fatigue in adolescent females with heavy menstrual bleeding. Haemophilia. 2013;19:225–230. doi: 10.1111/hae.12046. [DOI] [PubMed] [Google Scholar]
- 25.Percy L, Mansour D, Fraser I. Iron deficiency and iron deficiency anaemia in women. Best Pract Res Clin Obstet Gynaecol. 2017;40:55–67. doi: 10.1016/j.bpobgyn.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 26.Anker SD, Comin Colet J, Filippatos G, et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med. 2009;361:2436–2448. doi: 10.1056/NEJMoa0908355. [DOI] [PubMed] [Google Scholar]
- 27.van Veldhuisen DJ, Ponikowski P, van der Meer P, et al. Effect of ferric carboxymaltose on exercise capacity in patients with chronic heart failure and iron deficiency. Circulation. 2017;136:1374–1383. doi: 10.1161/CIRCULATIONAHA.117.027497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cappellini MD, Comin-Colet J, de Francisco A, et al. Iron deficiency across chronic inflammatory conditions: international expert opinion on definition, diagnosis, and management. Am J Hematol. 2017;92:1068–1078. doi: 10.1002/ajh.24820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ando K, Morita S, Higashi T, et al. Health-related quality of life among Japanese women with iron-deficiency anemia. Qual Life Res. 2006;15:1559–1563. doi: 10.1007/s11136-006-0030-z. [DOI] [PubMed] [Google Scholar]
- 30.Schoep ME, Adang EMM, Maas JWM, De Bie B, Aarts JWM, Nieboer TE. Productivity loss due to menstruation-related symptoms: a nationwide cross-sectional survey among 32 748 women. BMJ Open. 2019;9:e026186. doi: 10.1136/bmjopen-2018-026186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cote I, Jacobs P, Cumming D. Work loss associated with increased menstrual loss in the United States. Obstet Gynecol. 2002;100:683–687. doi: 10.1016/s0029-7844(02)02094-x. [DOI] [PubMed] [Google Scholar]
- 32.Cote I, Jacobs P, Cumming DC. Use of health services associated with increased menstrual loss in the United States. Am J Obstet Gynecol. 2003;188:343–348. doi: 10.1067/mob.2003.92. [DOI] [PubMed] [Google Scholar]
- 33.Bruner AB, Joffe A, Duggan AK, Casella JF, Brandt J. Randomised study of cognitive effects of iron supplementation in non-anaemic iron-deficient adolescent girls. Lancet. 1996;348:992–996. doi: 10.1016/S0140-6736(96)02341-0. [DOI] [PubMed] [Google Scholar]
- 34.Brownlie T 4th, Utermohlen V, Hinton PS, Haas JD. Tissue iron deficiency without anemia impairs adaptation in endurance capacity after aerobic training in previously untrained women. Am J Clin Nutr. 2004;79:437–443. doi: 10.1093/ajcn/79.3.437. [DOI] [PubMed] [Google Scholar]
- 35.Yokoi K, Konomi A. Iron deficiency without anaemia is a potential cause of fatigue: meta-analyses of randomised controlled trials and cross-sectional studies. Br J Nutr. 2017;117:1422–1431. doi: 10.1017/S0007114517001349. [DOI] [PubMed] [Google Scholar]
- 36.Richards T, Musallam KM, Nassif J, et al. Impact of preoperative anaemia and blood transfusion on postoperative outcomes in gynaecological surgery. PLoS One. 2015;10:e0130861. doi: 10.1371/journal.pone.0130861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Browning RM, Trentino K, Nathan EA, Hashemi N. Western Australian patient blood management program. Preoperative anaemia is common in patients undergoing major gynaecological surgery and is associated with a fivefold increased risk of transfusion. Aust NZ J Obstet Gynaecol. 2012;52:455–459. doi: 10.1111/j.1479-828X.2012.01478.x. [DOI] [PubMed] [Google Scholar]
- 38.Goksever Celik H, Celik E, Turan G, Seckin KD, Gedikbasi A. Risk factors for surgical site infection after hysterectomy. J Infect Dev Ctries. 2017;11:355–360. doi: 10.3855/jidc.9053. [DOI] [PubMed] [Google Scholar]
- 39.Murji A, Lam M, Allen B, et al. Risks of preoperative anemia in women undergoing elective hysterectomy and myomectomy. Am J Obstet Gynecol. 2019;221(629):e1–e18. doi: 10.1016/j.ajog.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 40.Rossler J, Schoenrath F, Seifert B, et al. Iron deficiency is associated with higher mortality in patients undergoing cardiac surgery: a prospective study. Br J Anaesth. 2020;124:25–34. doi: 10.1016/j.bja.2019.09.016. [DOI] [PubMed] [Google Scholar]
- 41.Fowler AJ, Ahmad T, Phull MK, Allard S, Gillies MA, Pearse RM. Meta-analysis of the association between preoperative anaemia and mortality after surgery. Br J Surg. 2015;102:1314–1324. doi: 10.1002/bjs.9861. [DOI] [PubMed] [Google Scholar]
- 42.Fowler AJ, Ahmad T, Abbott TEF, et al. Association of preoperative anaemia with postoperative morbidity and mortality: an observational cohort study in low-, middle-, and high-income countries. Br J Anaesth. 2018;121:1227–1235. doi: 10.1016/j.bja.2018.08.026. [DOI] [PubMed] [Google Scholar]
- 43.Spahn DR, Schoenrath F, Spahn GH, et al. Effect of ultra-short-term treatment of patients with iron deficiency or anaemia undergoing cardiac surgery: a prospective randomised trial. Lancet. 2019;393:2201–2212. doi: 10.1016/S0140-6736(18)32555-8. [DOI] [PubMed] [Google Scholar]
- 44.Triphaus C, Judd L, Glaser P, et al. Effectiveness of preoperative iron supplementation in major surgical patients with iron deficiency: a prospective observational study. Ann Surg. 2019 doi: 10.1097/SLA.0000000000003643. [DOI] [PubMed] [Google Scholar]
- 45.de Souza SS, Camargos AF, Ferreira MC, et al. Hemoglobin levels predict quality of life in women with heavy menstrual bleeding. Arch Gynecol Obstet. 2010;281:895–900. doi: 10.1007/s00404-009-1207-9. [DOI] [PubMed] [Google Scholar]
- 46.Vaucher P, Druais PL, Waldvogel S, Favrat B. Effect of iron supplementation on fatigue in nonanemic menstruating women with low ferritin: a randomized controlled trial. CMAJ. 2012;184:1247–1254. doi: 10.1503/cmaj.110950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Diez-Lobo AI, Fisac-MartÍn MP, Bermejo-Aycar I, MuÑOz M. Preoperative intravenous iron administration corrects anemia and reduces transfusion requirement in women undergoing abdominal hysterectomy. Transfus Altern Transfus Med. 2007;9:114–119. [Google Scholar]
- 48.Matteson KA, Rahn DD, Wheeler TL, 2nd, et al. Nonsurgical management of heavy menstrual bleeding: a systematic review. Obstet Gynecol. 2013;121:632–643. doi: 10.1097/AOG.0b013e3182839e0e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wheeler TL, 2nd, Murphy M, Rogers RG, et al. Clinical practice guideline for abnormal uterine bleeding: hysterectomy versus alternative therapy. J Minim Invasive Gynecol. 2012;19:81–88. doi: 10.1016/j.jmig.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 50.Institute of Obstetricians and Gynaecologists, Royal College of Physicians of Ireland, Clinical Strategy and Programmes Division Health Service Executive. Clinical practice guideline: The investigation and management of menorrhagia. 2018. https://rcpi-live-cdn.s3.amazonaws.com/wp-content/uploads/2016/05/34.-Investigation-and-Management-of-Menorrhagia.pdf. Accessed June 23 2020.
- 51.American College of Obstetricians and Gynecologists (ACOG) ACOG committee opinion no. 785: screening and management of bleeding disorders in adolescents with heavy menstrual bleeding. Obstet Gynecol. 2019;134:e71–e83. doi: 10.1097/AOG.0000000000003411. [DOI] [PubMed] [Google Scholar]
- 52.American College of Obstetricians and Gynecologists (ACOG) ACOG committee opinion no. 557: management of acute abnormal uterine bleeding in nonpregnant reproductive-aged women. Obstet Gynecol. 2013;121:891–896. doi: 10.1097/01.AOG.0000428646.67925.9a. [DOI] [PubMed] [Google Scholar]
- 53.American College of Nurse-Midwives Abnormal uterine bleeding. J Midwifery Womens Health. 2016;61:522–527. doi: 10.1111/jmwh.12514. [DOI] [PubMed] [Google Scholar]
- 54.Munro MG, Southern California Permanente Medical Group's Abnormal Uterine Bleeding Working Group Acute uterine bleeding unrelated to pregnancy: a Southern California Permanente Medical Group practice guideline. Perm J. 2013;17:43–56. doi: 10.7812/TPP/13-018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Demers C, Derzko C, David M, Douglas J. No. 163-Gynaecological and obstetric management of women with inherited bleeding disorders. J Obstet Gynaecol Can. 2018;40:e91–e103. doi: 10.1016/j.jogc.2017.11.036. [DOI] [PubMed] [Google Scholar]
- 56.Singh S, Best C, Dunn S, Leyland N, Wolfman WL. No. 292-Abnormal uterine bleeding in pre-menopausal women. J Obstet Gynaecol Can. 2018;40:e391–e415. doi: 10.1016/j.jogc.2018.03.007. [DOI] [PubMed] [Google Scholar]
- 57.Health Quality Ontario. Heavy menstrual bleeding – Care for adults and adolescents of reproductive age. 2017. https://www.hqontario.ca/portals/0/documents/evidence/quality-standards/qs-heavy-menstrual-bleeding-clinical-guide-en.pdf. Accessed June 23 2020.
- 58.National Institute for Health and Care Excellence (NICE). Quality standard QS47. Heavy menstrual bleeding. 2018. https://www.nice.org.uk/guidance/qs47. Accessed June 23 2020.
- 59.Australian Commission on Safety and Quality in Health Care. Heavy menstrual bleeding clinical care standard. 2017. https://www.safetyandquality.gov.au/sites/default/files/migrated/Heavy-Menstrual-Bleeding-Clinical-Care-Standard.pdf. Accessed June 23 2020.
- 60.James AH, Kouides PA, Abdul-Kadir R, et al. Evaluation and management of acute menorrhagia in women with and without underlying bleeding disorders: consensus from an international expert panel. Eur J Obstet Gynecol Reprod Biol. 2011;158:124–134. doi: 10.1016/j.ejogrb.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 61.Marret H, Fauconnier A, Chabbert-Buffet N, et al. Clinical practice guidelines on menorrhagia: management of abnormal uterine bleeding before menopause. Eur J Obstet Gynecol Reprod Biol. 2010;152:133–137. doi: 10.1016/j.ejogrb.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 62.Arab HA, Gari A, Almomen A, et al. Practical guidance on managing iron deficiency in women of childbearing age—a Saudi Arabian expert consensus. EC Gynaecology. 2019;8:554–574. [Google Scholar]
- 63.American College of Obstetricians and Gynecologists (ACOG) Practice bulletin no. 136: management of abnormal uterine bleeding associated with ovulatory dysfunction. Obstet Gynecol. 2013;122:176–185. doi: 10.1097/01.AOG.0000431815.52679.bb. [DOI] [PubMed] [Google Scholar]
- 64.Vilos GA, Allaire C, Laberge PY, Leyland N, Special C. The management of uterine leiomyomas. J Obstet Gynaecol Can. 2015;37:157–178. doi: 10.1016/S1701-2163(15)30338-8. [DOI] [PubMed] [Google Scholar]
- 65.American Association of Gynecologic Laparoscopists (AAGL) AAGL practice report: practice guidelines for the diagnosis and management of submucous leiomyomas. J Minim Invasive Gynecol. 2012;19:152–171. doi: 10.1016/j.jmig.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 66.Perez-Lopez FR, Ornat L, Ceausu I, et al. EMAS position statement: management of uterine fibroids. Maturitas. 2014;79:106–116. doi: 10.1016/j.maturitas.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 67.European Medicines Agency Pharmacovigilance Risk Assessment Committee (PRAC). Assessment report on temporary measures. 2020. https://www.ema.europa.eu/en/documents/referral/ulipristal-acetate-5mg-medicinal-products-article-31-referral-assessment-report-temporary-measures_en.pdf. Accessed June 12 2020.
- 68.World Health Organization. WHO guidelines on use of ferritin concentrations to assess iron status in individuals and populations. 2020. https://www.who.int/publications-detail/9789240000124. Accessed May 1 2020. [PubMed]
- 69.Mast AE, Blinder MA, Gronowski AM, Chumley C, Scott MG. Clinical utility of the soluble transferrin receptor and comparison with serum ferritin in several populations. Clin Chem. 1998;44:45–51. [PubMed] [Google Scholar]
- 70.Derman R, Roman E, Smith-Nguyen GN, Achebe MM, Thomsen LL, Auerbach M. Iron isomaltoside is superior to iron sucrose in increasing hemoglobin in gynecological patients with iron deficiency anemia. Am J Hematol. 2018;93:E148–E150. doi: 10.1002/ajh.25094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ikuta K, Hanashi H, Hirai K, et al. Comparison of efficacy and safety between intravenous ferric carboxymaltose and saccharated ferric oxide in Japanese patients with iron-deficiency anemia due to hypermenorrhea: a multi-center, randomized, open-label noninferiority study. Int J Hematol. 2019;109:41–49. doi: 10.1007/s12185-018-2501-8. [DOI] [PubMed] [Google Scholar]
- 72.Kim YH, Chung HH, Kang SB, Kim SC, Kim YT. Safety and usefulness of intravenous iron sucrose in the management of preoperative anemia in patients with menorrhagia: a phase IV, open-label, prospective, randomized study. Acta Haematol. 2009;121:37–41. doi: 10.1159/000210062. [DOI] [PubMed] [Google Scholar]
- 73.Lee S, Ryu KJ, Lee ES, Lee KH, Lee JJ, Kim T. Comparative efficacy and safety of intravenous ferric carboxymaltose and iron sucrose for the treatment of preoperative anemia in patients with menorrhagia: an open-label, multicenter, randomized study. J Obstet Gynaecol Res. 2019;45:858–864. doi: 10.1111/jog.13893. [DOI] [PubMed] [Google Scholar]
- 74.Mahey R, Kriplani A, Mogili KD, Bhatla N, Kachhawa G, Saxena R. Randomized controlled trial comparing ferric carboxymaltose and iron sucrose for treatment of iron deficiency anemia due to abnormal uterine bleeding. Int J Gynaecol Obstet. 2016;133:43–48. doi: 10.1016/j.ijgo.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 75.Sharma R, Stanek JR, Koch TL, Grooms L, O'Brien SH. Intravenous iron therapy in non-anemic iron-deficient menstruating adolescent females with fatigue. Am J Hematol. 2016;91:973–977. doi: 10.1002/ajh.24461. [DOI] [PubMed] [Google Scholar]
- 76.Tolkien Z, Stecher L, Mander AP, Pereira DI, Powell JJ. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS One. 2015;10:e0117383. doi: 10.1371/journal.pone.0117383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Elstrott B, Khan L, Olson S, Raghunathan V, DeLoughery T, Shatzel JJ. The role of iron repletion in adult iron deficiency anemia and other diseases. Eur J Haematol. 2020;104:153–161. doi: 10.1111/ejh.13345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Munoz M, Acheson AG, Auerbach M, et al. International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia. 2017;72:233–247. doi: 10.1111/anae.13773. [DOI] [PubMed] [Google Scholar]
- 79.Abdullah HR, Ang AL, Froessler B, et al. Getting patient blood management Pillar 1 right in the Asia-Pacific: a call for action. Singapore Med J. 2020;61:287–96. doi: 10.11622/smedj.2019037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Isbister JP. The three-pillar matrix of patient blood management–an overview. Best Pract Res Clin Anaesthesiol. 2013;27:69–84. doi: 10.1016/j.bpa.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 81.Hofmann A, Farmer S, Shander A. Five drivers shifting the paradigm from product-focused transfusion practice to patient blood management. Oncologist. 2011;16(Suppl 3):3–11. doi: 10.1634/theoncologist.2011-S3-3. [DOI] [PubMed] [Google Scholar]
- 82.Leahy MF, Hofmann A, Towler S, et al. Improved outcomes and reduced costs associated with a health-system-wide patient blood management program: a retrospective observational study in four major adult tertiary-care hospitals. Transfusion. 2017;57:1347–1358. doi: 10.1111/trf.14006. [DOI] [PubMed] [Google Scholar]
- 83.Shander A, Goobie SM, Warner MA, et al. The essential role of patient blood management in a pandemic: a call for action. Anesth Analg. 2020;131:74–85. doi: 10.1213/ANE.0000000000004844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Warner MA, Shore-Lesserson L, Shander A, Patel SY, Perelman SI, Guinn NR. Perioperative anemia: prevention, diagnosis, and management throughout the spectrum of perioperative care. Anesth Analg. 2020;130:1364–1380. doi: 10.1213/ANE.0000000000004727. [DOI] [PubMed] [Google Scholar]
- 85.Lee ES, Kim MJ, Park BR, et al. Avoiding unnecessary blood transfusions in women with profound anaemia. Aust N Z J Obstet Gynaecol. 2015;55:262–267. doi: 10.1111/ajo.12329. [DOI] [PubMed] [Google Scholar]
- 86.Tam WH, Yuen PM, Shan Ng DP, Leung PL, Lok IH, Rogers MS. Health status function after treatment with thermal balloon endometrial ablation and levonorgestrel intrauterine system for idiopathic menorrhagia: a randomized study. Gynecol Obstet Invest. 2006;62:84–88. doi: 10.1159/000092660. [DOI] [PubMed] [Google Scholar]
- 87.Andrade A, Wildemeersch D. Menstrual blood loss in women using the frameless FibroPlant LNG-IUS. Contraception. 2009;79:134–138. doi: 10.1016/j.contraception.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 88.The European Board and College of Obstetrics and Gynaecology. Standards of care for women’s health in Europe. 2014. https://www.uems.eu/__data/assets/pdf_file/0020/8750/Item-5.3.8-EBCOG-Standards-of-Care-for-Gynaecology-PDF-FEB-11-2014-FINAL-DRAFT.pdf. Accessed June 23 2020.