Abstract
The COVID-19 pandemic significantly altered much of US life with shifts to working-from-home and social distancing changing day-to-day behavior. We aimed to determine the self-reported prevalence of meeting US physical activity guidelines, stratified by sitting time during the early lockdown phase of COVID-19 in US adults. We conducted two cross-sectional internet-based studies April 3rd-May 4th, 2020 in convenience samples of US adults. Participants self-reported daily sitting time and weekly moderate-to-vigorous physical activity (MVPA) via questions from the International Physical Activity Questionnaire. A total of 5036 US adults (65.3% women, 30.2% with chronic conditions) provided complete physical activity and sitting time data (80.3% of total). Overall, 42.6% of participants reported sitting for > 8 h/day (95% CI: 41.2%–44.0%) and 72.5% (71.2%–73.7%) reported being either sufficiently (150–300 MVPA minutes) or highly active (>300 min). The greatest proportion of people self-reported being highly active and sitting for > 8 h/day (24.0%; 22.8%-25.2%), followed by being highly active and sitting for 6–8 h/day (20.9%; 19.8%–22.1%). Sitting and activity appeared similar between sexes, while there was evidence of some age differences. For example, more young adults (ages 18–34) appeared to self-report being inactive and more appeared to sit for > 8 h/day compared to older adults. High sitting time was reported by US adults (>40% sitting > 8 h/day) during April 2020. However, high levels of physical activity (>70% meeting guidelines) were also reported. Since physical activity cannot eliminate the negative health effects of sitting, maintaining activity and limiting sitting during periods of large workplace and societal shifts is encouraged.
Keywords: Sedentary behavior, Exercise, Pandemic, Coronavirus, US guidelines
1. Introduction
The novel Coronavirus Disease 2019 (COVID-19) pandemic was first diagnosed in December 2019 in China (Wang et al., 2020) and has since changed the world in ways we have not witnessed in recent times. The efforts to contain this pandemic have brought unprecedented efforts to institute the practice of physical/social distancing in countries all around the world, resulting in shutdowns of day-to-day functioning and changes in interaction and activity patterns (Lewnard and Lo, 2020). These important steps to mitigate the spread of COVID-19 (Lewnard and Lo, 2020, Greenstone and Nigam, 2020), will undoubtedly lead to both short- and long-term mental and physical health consequences (Venkatesh and Edirappuli, 2020, Galea et al., 2020). Multiple studies have explored the National Health and Nutrition Examination Survey (NHANES) data to determine sitting time and physical activity behavior of adults in the United States (US) prior to the pandemic (e.g. in 2015–2016 (Ussery et al., 2018, Yang et al., 2019); however, there is limited data on sedentary time and physical activity levels during the time when most of the US was under a stay-at-home order. Therefore, this short report examines the prevalence of patterns in joint categories of sitting time and physical activity among US adults between April 3rd, 2020 and May 4th, 2020.
2. Methods
Data for this study were obtained from two separate cross-sectional surveys that examined physical activity, sedentary time, and COVID-19 lifestyle changes. Participants in each study were recruited through mass emails, snowball sampling, researcher networks, and posts to social media pages. Interested participants were directed to a link to an anonymous electronic survey to read and consent to enrollment in the study.
The first survey (study 1) was administered by researchers at Iowa State University (approval #: 20–144-00) to 5021 US adults from April 3rd-May 4th, 2020. Inclusion criteria were being ≥ 18 years of age and current US residence. The full survey took 20–30 min to complete and included demographic information and health history (i.e. age, gender, sex, race, education, marital status, occupational status, height, weight, and current chronic health conditions), COVID-19-related restrictions participants were following (i.e., quarantined or self-isolating, under a shelter-in-place or stay-at-home order, and social distancing), COVID-19-related health behaviors and their changes (i.e., smoking and drinking status, average daily time spent sitting, average daily minutes in moderate and vigorous activity (MVPA), and average daily screen-time), and mental health questionnaires. Participants self-reported daily time spent in physical activity and sedentary behavior by answering: “How much time on an average day have you spent [in moderate activity, in vigorous activity, sitting] since making COVID-related behavioral changes?”
The second survey (study 2) was administered by researchers at Clarkson University (approval #20–5.1) and George Mason University (approval #1592393–1) to 1,250 US adults from April 14th-May 4th, 2020. Inclusion criteria were: being ≥ 18 years of age. The full survey took ~18 min to complete and included demographic information (i.e., sex, education, relationship status, occupation status) mood, trait moods, grit, sitting time, moderate physical activity, and vigorous physical activity using the International Physical Activity Questionnaire-Short Form (IPAQ-SF).
The following variables from each survey were harmonized and used in the present analysis: demographic information (including age, sex, employment status, relationship status, living situation, education level, presence of chronic disease), average minutes of sitting, moderate physical activity and vigorous physical activity.
For sitting, individuals were grouped by the following amounts of self-reported sitting time: 0 to < 4 h, 4 to < 6 h, 6–8 h, or > 8 h per day. In accordance with the US Physical Activity Guidelines (US Department of Health and Human Services, 2018), weekly physical activity was categorized as weekly minutes of moderate activity plus twice the number of minutes of vigorous activity. Individuals were then grouped by weekly physical activity level as inactive (0 min), insufficiently active (1–150 min/day), sufficiently active (150–300 min/day), or highly active (>300 min/day).8 Data are presented as percentages with 95% confidence intervals in-text and with sample sizes in tables.
3. Results
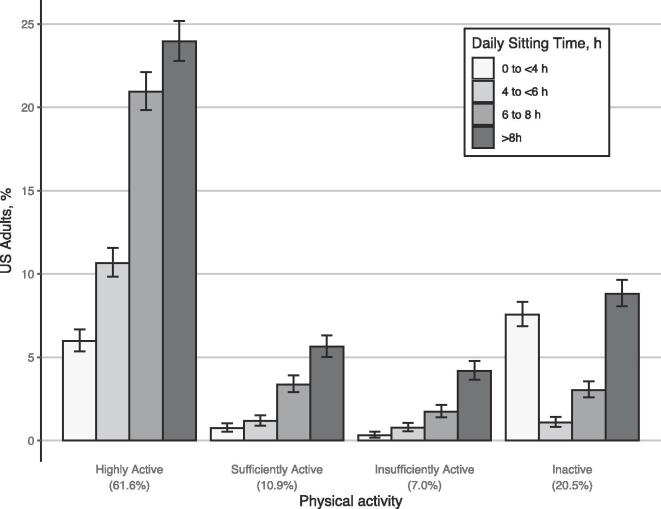
A total of 5036 US Adults with complete data (80.3% of total) provided physical activity and sitting time data across two pooled studies. The sample was predominantly female (65.3%), without chronic conditions (67.3%) married (58.0%) and had a college degree (81.0%; Supplementary Material 1). Overall, 42.6% of the sample reported sitting for >8 h per day (95% CI: 41.2%–44.0%) and 72.5% (95% CI, 71.2%–73.7%) of the sample reported being either sufficiently (150–300 min of MVPA) or highly active (>300 min). From the stratification analyses (Fig. 1), the greatest proportion of people self-reported being highly active and sitting for >8 h per day (24.0%; 22.8%-25.2%), followed by being highly active and sitting for 6 to 8 h per day (20.9%; 19.8%–22.1%). Of the inactive participants (0 min of MVPA; 20.5% of the sample), most self-reported either sitting for 0 to < 4 h per day (7.6%; 6.9%-8.3%) or > 8 h per day (8.8%; 8.1%-9.6%). Sitting and activity patterns appeared similar between the sexes, while there was evidence of some differences across age categories (Table 1). For example, more young adults (18–34) appeared to self-report being inactive and more appeared to sit for > 8 h per day compared to the other age groups.
Fig. 1.
Prevalence of Meeting Physical Activity Guidelines Stratified by Daily Sitting Time among US Adults During Early COVID-19 Lockdowns, April 3rd-May 4th, 2020. Footnotes: Data represent percentage of US adults who reported each joint category of daily sitting time and total daily physical activity. 95% confidence intervals are represented by error bars. Abbreviation: COVID-19 = coronavirus disease 2019.
Table 1.
Joint Distribution of Self-Reported Sitting Time and Physical Activity by Sex and Age During COVID-19.
| Daily Sitting Time,b No. (%) [95% CI] |
||||
|---|---|---|---|---|
| Weekly physical activitya | 0 to < 4 h | 4 to < 6 h | 6 to 8 h | >8h |
| Sex | ||||
| Men (n = 1724) | ||||
| Inactive | 130 (7.5) [6.4–8.9] | 16 (0.9) [0.5–1.5] | 42 (2.4) [1.8–3.3] | 128 (7.4) [6.3–8.8] |
| Insufficiently Active | 6 (0.3) [0.1–0.8] | 8 (0.5) [0.2–1.0] | 29 (1.7) [1.1–2.4] | 70 (4.1) [3.2–5.1] |
| Sufficiently Active | 11 (0.6) [0.3–1.2] | 24 (1.4) [0.9–2.1] | 40 (2.3) [1.7–3.2] | 98 (5.7) [4.7–6.9] |
| Highly Active | 95 (5.5) [4.5–6.7] | 212 (12.3) [10.8–14.0] | 368 (21.3) [19.4–23.4] | 447 (25.9) [23.9–28.1] |
| Women (n = 3286) | ||||
| Inactive | 242 (7.4) [6.5–8.3] | 39 (1.2) [0.9–1.6] | 111 (3.4) [2.8–4.1] | 312 (9.5) [8.5–10.6] |
| Insufficiently Active | 9 (0.3) [0.1–0.5] | 30 (0.9) [0.6–1.3] | 57 (1.7) [1.3–2.3] | 139 (4.2) [3.6–5.0] |
| Sufficiently Active | 27 (0.8) [0.6–1.2] | 35 (1.1) [0.8–1.5] | 129 (3.9) [3.3–4.7] | 185 (5.6) [4.9–6.5] |
| Highly Active | 206 (6.3) [5.5–7.2] | 325 (9.9) [8.9–11.0] | 685 (20.8) [19.5–22.3] | 755 (23.0) [21.6–24.5] |
| Age, y | ||||
| Young, 18–34 (n = 1988) | ||||
| Inactive | 163 (12.1) [10.5–13.9] | 20 (0.7) [0.4–1.3] | 60 (2.8) [2.0–3.8] | 249 (12.4) [10.8–14.3] |
| Insufficiently Active | 6 (0.3) [0.1–0.9] | 21 (0.4) [0.2–1.0] | 36 (1.0) [0.6–1.7] | 89 (3.9) [3.0–5.1] |
| Sufficiently Active | 18 (1.1) [0.7–1.8] | 25 (0.4) [0.2–1.0] | 73 (2.3) [1.6–3.2] | 149 (7.4) [6.2–8.9] |
| Highly Active | 83 (4.2) [3.2–5.4] | 145 (5.0) [4.0–6.3] | 315 (15.2) [13.4–17.2] | 536 (30.8) [28.4–33.3] |
| Middle, 35–64 (n = 1983) | ||||
| Inactive | 134 (7.7) [6.5–9.1] | 24 (0.9) [0.5–1.5] | 66 (2.8) [2.1–3.8] | 157 (7.7) [6.5–9.1] |
| Insufficiently Active | 6 (0.2) [0.0–0.6] | 11 (0.2) [0.0–0.6] | 34 (1.5) [1.0–2.3] | 88 (4.7) [3.8–5.8] |
| Sufficiently Active | 15 (0.5) [0.2–1.0] | 25 (0.9) [0.6–1.6] | 68 (3.4) [2.6–4.3] | 91 (4.9) [3.9–6.0] |
| Highly Active | 142 (6.0) [4.9–7.3] | 221 (10.8) [9.3–12.4] | 431 (22.6) [20.6–24.7] | 470 (25.3) [23.3–27.5] |
| Old, 65+ (n = 1062) | ||||
| Inactive | 82 (8.4) [6.8–10.3] | 11 (0.9) [0.4–1.7] | 27 (2.4) [1.6–3.6] | 38 (2.9) [2.0–4.2] |
| Insufficiently Active | 4 (0.2) [0.0–0.8] | 7 (0.5) [0.2–1.2] | 17 (1.5) [0.9–2.5] | 33 (2.8) [1.9–4.1] |
| Sufficiently Active | 5 (0.7) [0.3–1.5] | 9 (0.8) [0.4–1.6] | 29 (2.7) [1.9–4.0] | 44 (4.1) [3.0–5.6] |
| Highly Active | 76 (7.2) [5.8–9.0] | 170 (16.1) [13.9–18.5] | 309 (29.6) [26.8–32.5] | 201 (19.1) [16.8–21.7] |
Data presented were collected April 3-May 4, 2020 from adult respondents in all 50 US states. Abbreviation: COVID-19 = coronavirus disease 2019.
In study 1, meeting physical activity guidelines was assessed with the following questions: “Think about all the vigorous and moderate activities that you did on average daily… Vigorous physical activities refer to activities that take hard physical effort and make you breathe much harder than normal. Moderate activities refer to activities that take moderate physical effort and make you breathe somewhat harder than normal. How much time on an average day have you spent in moderate activity since making COVID-related behavioral changes? How much time on and average day do you usually spend in vigorous activity before making COVID-related behavioral changes?” In study 2, physical activity minutes were recorded similarly via the IPAQ-SF. Minutes counting toward meeting physical activity guidelines were based upon achieving 150 min/week of moderate-to-vigorous physical activity counting one minute for every moderate minute and two minutes for every minute of vigorous physical activity.
In study 1, sitting time was assessed with the following questions: “The next questions are about the time that you spent sitting on average. Include time at work, at home, while doing course work and during leisure time. This may include time spent sitting at a desk, visiting friends, reading or sitting or lying down to watch television. Since making COVID-related behavioral changes how much time have you spent sitting daily?” In study 2, sitting time was assessed similarly with the single sitting time question from the IPAQ-SF.
4. Discussion
Compared to a previously reported nationally representative sample from the 2015–2016 wave of NHANES (Ussery et al., 2018), many more people in the present sample report sitting more > 8 h per day (42.6% v. 25.7%). However, the current population also reported being more physically active with 61.6% reporting high physical activity compared to 25.2% in the sample in 2015–2016. Interestingly a majority of our physically active participants also reported being sedentary for > 8 h per day. This may be an interesting development during the COVID-19 pandemic as many people were forced to work from home and could have used physical activity as an outlet for socialization or found the lack of their commute may have provided more leisure time. Our younger population reported the most sitting time, however, this group was also the group that mostly dichotomously fell into the inactive or highly active group, while most older adults (79.4% of those 65 + ) reported being at least sufficiently active. These results differ greatly from Ussery et al.’s NHANES report (Ussery et al., 2018) as physical activity levels declined with age in that sample, although they are similar to data collected during COVID-19 in the United Kingdom (Smith et al., 2020). As high sedentary time is associated with higher mortality risk independent of physical activity participation (Ekelund et al., 2016), the present high prevalence of > 8 h/day of sitting time during the response to COVID is troubling. This is concerning as high levels of sedentary time are associated with worse overall health across many metrics (Dunstan et al., 2012) and lifestyle risk factors (such as inactivity) have been found to be associated with an increased risk for hospitalization due to COVID-19 (Hamer et al., 2020). As increased screen time and reduced activity during the pandemic have been associated with worse mental health (Meyer et al., 2020), the high levels of sitting in this dataset are of significant public health concern. The limitations of this study are that: our sample was not a nationally representative sample, was highly educated, and was collected through convenience sampling which introduces selection bias. As NHANES was a nationally-representative sample, contrasts between the present findings and previous NHANES data adds context to the present findings, but differences in the samples limit direct comparison. Additionally, there is inherent bias in self-reported data generally leading to over-reporting of physical activity and under-reporting of sedentary time.
5. Conclusions
Both high sedentary behavior and physical inactivity have deleterious mental and physical health effects (Kodama et al., 2009, Kandola et al., 2019) and US adults reported engaging in high levels of sitting time but also high levels of activity during the initial COVID-19 lockdown phase in April 2020. If major workplace and societal shifts are needed (e.g. during this or future pandemics), evidence-based strategies to limit sitting time, increase physical activity, or both would be potentially beneficial to most US adults, particularly young adults. Practitioners and researchers should support efforts to develop and implement programs, practices and policies that can provide physically distant interventions to help US adults sit less and become more physically active. In particular, strategies that minimize or limit required sitting time may be particularly influential given the present high prevalence of sitting time.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
JM, MH, CM, JL, CB, FS, LS, MT were involved in the conception, design and acquisition of data for study 1, while JL, SC, NC and AB were involved in the conception, design and acquisition of data for study 2. JM and AB pooled the data and ran the analyses for this manuscript. All authors were involved in drafting and revising the work critically for important intellectual content. The contents of this article have not been previously presented elsewhere.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101256.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern [published correction appears in. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewnard J.A., Lo N.C. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect Dis. 2020;20(6):631–633. doi: 10.1016/S1473-3099(20)30190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenstone M, Nigam V. Does social distancing matter? University of Chicago, Becker Friedman Institute for Economics Working Paper. 2020;(2020–26). https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3561244.
- A. Venkatesh S. Edirappuli Social distancing in covid-19: what are the mental health implications? BMJ. 2020;369:m1379. 10.1136/bmj.m1379 Published 2020 Apr 6. [DOI] [PubMed]
- Galea S, Merchant RM, Lurie N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention [published online ahead of print, 2020 Apr 10]. JAMA Intern Med. 2020;10.1001/jamainternmed.2020.1562. doi:10.1001/jamainternmed.2020.1562. [DOI] [PubMed]
- Ussery E.N., Fulton J.E., Galuska D.A., Katzmarzyk P.T., Carlson S.A. Joint prevalence of sitting time and leisure-time physical activity among US adults. JAMA. 2018;320(19):2036–2038. doi: 10.1001/jama.2018.17797. 2015–2016 [published correction appears in JAMA. 2019 Jan 15;321(2):209] [published correction appears in JAMA. 2019 Apr 9;321(14):1412] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L., Cao C., Kantor E.D. Trends in sedentary behavior among the US population, 2001–2016. JAMA. 2019;321(16):1587–1597. doi: 10.1001/jama.2019.3636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services . Second Edition. US Dept of Health and Human Services; Washington, DC: 2018. Physical Activity Guidelines for Americans. [Google Scholar]
- Smith L., Jacob L., Butler L., Schuch F., Barnett Y., Grabovac I. Prevalence and correlates of physical activity in a sample of UK adults observing social distancing during the COVID-19 pandemic. BMJ Open SEM. 2020;6(1) doi: 10.1136/bmjsem-2020-000850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women [published correction appears in Lancet. 2016 Sep 24;388(10051):e6]. Lancet. 2016;388(10051):1302-13doi:10.1016/S0140-6736(16)30370-1. [DOI] [PubMed]
- Dunstan D.W., Howard B., Healy G.N., Owen N. Too much sitting – A health hazard. Diabetes Res. Clin. 2012;97(3):368–376. doi: 10.1016/j.diabres.2012.05.020. [DOI] [PubMed] [Google Scholar]
- Hamer M., Kivimäki M., Gale C.R., Batty G.D. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK. Brain Behav Immun. 2020;1(87):184–187. doi: 10.1016/j.bbi.2020.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer J., McDowell C., Lansing J., Brower C., Smith L., Tully M. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int. J. Environ. Res. Public Health. 2020;17(18):6469. doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodama S., Saito K., Tanaka S., Maki M., Yachi Y., Asumi M. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301(19):2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- Kandola A., Ashdown-Franks G., Stubbs B., Osborn D.P.J., Hayes J.F. The association between cardiorespiratory fitness and the incidence of common mental health disorders: a systematic review and meta-analysis. J. Affect. Disord. 2019;01(257):748–757. doi: 10.1016/j.jad.2019.07.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.