To the Editor: The COVID-19 pandemic has had a devastating impact on humans, society, and the global economy. Returning to pre-pandemic activity hinges on the development of robust immunization against SARS-CoV-2. Successful immunization through vaccination or post-exposure to SARS-CoV-2 largely depends on the adaptive immune response. In clinical trials of COVID-19 vaccines, detection of SARS-CoV-2 specific IgG antibodies is an accepted endpoint for establishing immune response. Unfortunately, several studies have reported rapid decline in IgG titters following both SARS-CoV-2 infection or vaccination [1]. Our recent work has explored the influence of the androgen receptor (AR) on COVID-19 disease severity [2]. We have elucidated that androgen sensitive phenotypes, e.g., androgenetic alopecia (AGA), are associated with increased disease severity [3]. Here we propose that the dependence of SARS-CoV-2 on the AR may extend to the immune response and might be an important consideration for vaccine development.
T-cell mediated immunity is dependent on B-cell or dendritic cell presenting antigen fragments. B-cells and dendritic cells effectiveness are suppressed by androgens. In mice, the AR modulates B-cell homeostasis and the loss of AR results in increased B-cells in blood and marrow [4]. Hepworth et al. [5] experimented with bone marrow-derived dendritic cells (BMDC) exposed to dihydrotestosterone (DHT). BMDC cells exposed to DHT during antigen uptake exhibited reduced T-cells stimulation capacity compared to BMDC cells not exposed to DHT.
More generally, androgens and the androgen receptor are associated with suppressed immune function. In men, high testosterone levels have been associated with reduced trivalent inactivated seasonal influenza vaccine antibody response [6]. Similarly, in Paracoccidioidomycosis infection androgens drive immunosuppression and Th2 response while estrogens drive a Th1 response [7]. Additionally, Tessnow et al. [8] reported that genetic variations in the AR CAG repeat length was associated with varied levels IgG autoantibodies. In particular, longer AR CAG repeat length was associated with a predominately IgG autoimmunity in men. Finally, Deng et al. [9] demonstrated that AR expression is inversely correlated with IgG levels in prostate cancer cells.
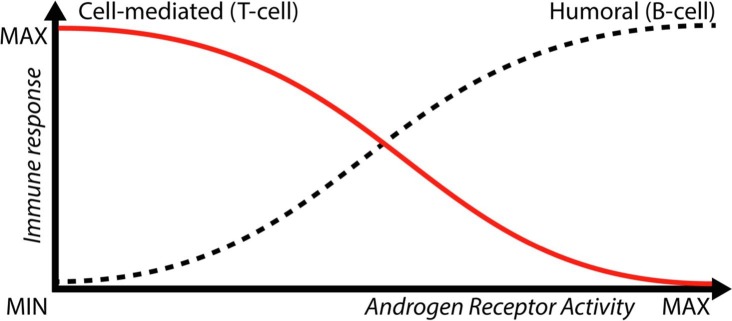
Taken together, these data suggest that anti-androgen therapy when combined with a vaccine for COVID-19 may improve specific T-cell mediated immune response, Fig. 1 . To test this hypothesis, it would be informative to study IgG levels as well as SARS-CoV-2 T-cell response (with assays such as T-cell receptor dependent activation induced markers) in COVID-19 patients with AGA. Moreover, sub-analysis of immune response in vaccinated or recovered COVID-19 patients taking 5-alpha-reductase inhibitors (dutasteride, finasteride) or androgen deprivation therapy should be conducted. If the theory demonstrates that androgens or the androgen receptor play a role in modulating the SARS-CoV-2 adaptive immune response, it would be an important design consideration for COVID-19 vaccine trails. Further, COVID-19 vaccination of AGA patients may require the addition of an anti-androgen therapy as a means to boost the cellular immune response. At minimum, the evidence warrants further studies to elucidate the role (if any) of androgens and the androgen receptor in modulating SARS-CoV-2 adaptive immunity.
Fig. 1.
Theoretical Androgen Receptor modulation of humoral and cell-mediated immune response. Dihydrotestosterone (DHT) increases androgen expression and may cause a decrease in the protective immune response for SARS-CoV-2.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Ibarrondo F.J., Fulcher J.A., Goodman-Meza D. Rapid decay of anti–SARS-CoV-2 antibodies in persons with mild covid-19. N Engl J Med. 2020;383(11):1085–1087. doi: 10.1056/NEJMc2025179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goren A, McCoy J, Wambier CG, et al. What does androgenetic alopecia have to do with COVID-19? An insight into a potential new therapy. Dermatol Ther 2020:e13365. doi:10.1111/dth.13365. [DOI] [PMC free article] [PubMed]
- 3.Wambier C.G., Vaño-Galván S., McCoy J. Androgenetic alopecia present in the majority of hospitalized COVID-19 patients – the “Gabrin sign”. J Am Acad Dermatol. 2020 doi: 10.1016/j.jaad.2020.05.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Altuwaijri S., Chuang K.-H., Lai K.-P. Susceptibility to autoimmunity and B cell resistance to apoptosis in mice lacking androgen receptor in B cells. Mol Endocrinol. 2009;23(4):444–453. doi: 10.1210/me.2008-0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hepworth M.R., Hardman M.J., Grencis R.K. The role of sex hormones in the development of Th2 immunity in a gender-biased model of Trichuris muris infection. Eur J Immunol. 2010;40(2):406–416. doi: 10.1002/eji.200939589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Furman D., Hejblum B.P., Simon N. Systems analysis of sex differences reveals an immunosuppressive role for testosterone in the response to influenza vaccination. Proc Natl Acad Sci USA. 2014;111(2):869–874. doi: 10.1073/pnas.1321060111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shankar J., Restrepo A., Clemons K.V., Stevens D.A. Hormones and the resistance of women to paracoccidioidomycosis. Clin Microbiol Rev. 2011;24(2):296–313. doi: 10.1128/CMR.00062-10. PMID: 21482727; PMCID: PMC3122492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tessnow A.H., Olsen N.J., Kovacs W.J. Expression of humoral autoimmunity is related to androgen receptor CAG repeat length in men with systemic lupus erythematosus. J Clin Immunol. 2011;31(4):567–573. doi: 10.1007/s10875-011-9519-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deng Y.-L., Guo K., Zeng Y.-K., Wu K.-H., Tang C., Zheng S.-B. Effect of androgen receptor on IgG expression, proliferation and migration of prostate cancer cells in vitro. Nan Fang Yi Ke Da Xue Xue Bao. 2017;37(3):388–392. doi: 10.3969/j.issn.1673-4254.2017.03.19. http://www.ncbi.nlm.nih.gov/pubmed/28377358. [DOI] [PMC free article] [PubMed] [Google Scholar]