Abstract
An anatomic and tension-free repair is the goal of arthroscopic rotator cuff repair. However, this purpose is not always achievable in large and massive tears, and sometimes, even when intraoperative results seem acceptable, clinical and radiologic outcomes can be disappointing shortly afterward. Superior capsule reconstruction has been claimed as a valid and viable joint-preserving option for treating irreparable rotator cuff tears. However, the role of the superior capsule in repairable cuff tears has also been questioned. The aim of this article is to present the so-called arthroscopic cuff-plus technique. This technique consists of superior capsule reconstruction using the proximal part of the long head of the biceps tendon associated with a tension-free repair of the rotator cuff tendons in large to massive delaminated tears.
The ideal goal of arthroscopic rotator cuff repair is to achieve an anatomic, tension-free reattachment of the rotator cuff tendons to the native footprint to obtain a physiological bone-tendon junction. However, the failure rate, especially in large to massive tears, is very high. Excessive tension on the repair, poor tissue quality, and a possible mismatch in the tension of the articular and bursal layers of the cuff in large delaminated tears are surely possible mechanisms of failure.1
In the past decade, a deeper insight into the anatomy of the rotator cuff tendons has clearly elicited the role of the superior capsule. Clinical and biomechanical studies have shown that superior capsule reconstruction (SCR) with autologous fascia lata graft is a viable joint-preserving option in treating irreparable cuff tears.2 Several variations of the original technique for SCR have been further proposed, particularly the use of acellular dermal matrix allograft, albeit the rationale remained unchanged and preliminary good clinical outcomes have been reported.3,4 Some authors have also suggested the use of the autologous long head of the biceps tendon (LHBT) as the graft for SCR, suggesting advantages such as low cost, graft availability, limited donor-site morbidity, ease of use, and reliability.5,6 A recent biomechanical study supported the hypothesis that anatomic reconstruction of the superior capsule and rotator cuff improves biomechanical properties in repairing delaminated rotator cuff tears, opening our minds to the idea that SCR could be a valid option also in treating repairable cuff tears.7
The following Technical Note aims to present the so-called arthroscopic cuff-plus technique. This technique consists of SCR using the proximal part of the LHBT associated with a tension-free repair of the bursal layer of the rotator cuff tendons in large to massive delaminated tears of the posterosuperior cuff that are still repairable. The rationale of the technique is that the LHBT graft should act to reinforce and protect the rotator cuff repair, thus reducing the risk of retear.
Surgical Technique
Indications
The diagnosis of a rotator cuff tear is always made through patient history, physical examination, and imaging. Standard imaging assessment consists of the following:
-
•
Radiographic evaluation (true anteroposterior and axillary views) to assess arthritic changes, as well as to rule out calcific tendinitis
-
•
Magnetic resonance imaging to assess tear characteristics, fatty infiltration, and muscle atrophy
The indications for the arthroscopic cuff-plus technique are always confirmed intraoperatively and are mainly focused on large to massive repairable posterosuperior cuff tears that show delamination with severe retraction and poor mobility of the articular layer. The contraindications are the same as those of a standard arthroscopic rotator cuff repair, such as an irreparable tear, involvement of the teres minor, cuff tear arthropathy, and shoulder stiffness.
Patient Positioning
The procedure can be performed with the patient under general anesthesia or an interscalene block (or a combination thereof). The beach-chair position is our preferred position for cuff repair, but the procedure can alternatively be performed in the lateral decubitus position according to the surgeon’s preference.
Portal Placement
After preparation of the surgical fields, the following bony landmarks are identified with a marking pen: spine of the scapula, acromion, clavicle, and coracoid process. The following standard portals are used:
-
•
Posterior portal, used as a viewing portal or as a working portal for suture management when the scope is in the lateral portal
-
•
Anterosuperior portal, used for suture management
-
•
Lateral portal, used as a viewing portal or as a working portal for suture management when the scope is in the posterior portal
-
•
One or two superolateral portals, used for anchor placement
Two plastic cannulas with different calibers are always used: an 8.0-mm operative cannula and a 5.5-mm outflow cannula.
Step-by-Step Procedure
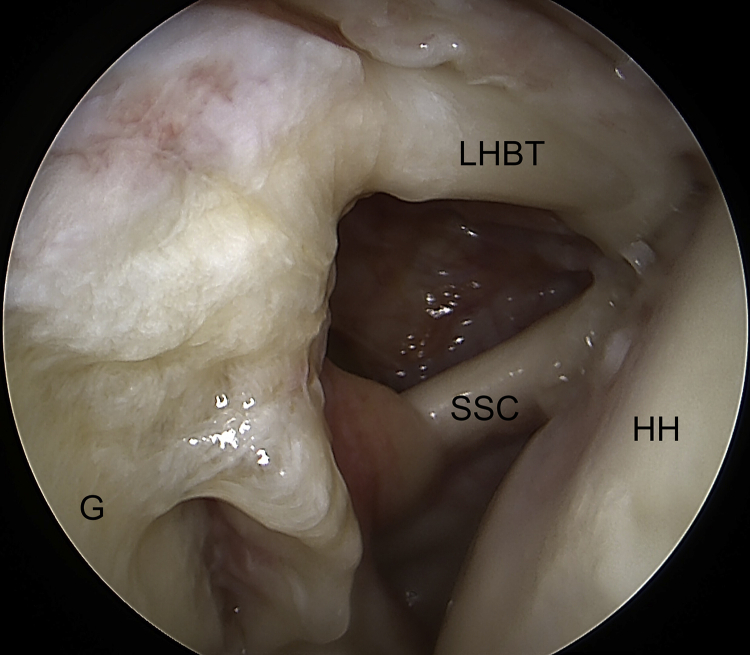
The arthroscopic procedure always starts with an intra-articular diagnostic evaluation on air through the posterior portal to confirm the rotator cuff tear and assess the status of the LHBT, as well as rule out advanced articular degenerative changes and eventual subscapularis tendon tears (Fig 1). If a subscapularis tendon tear is present, it is fixed at this time. A 30° scope is used even in the case of a subscapularis tendon repair.
Fig 1.
Arthroscopic view (joint space) through posterior portal of right shoulder with patient in beach-chair position. Intra-articular diagnostic evaluation is performed to confirm the rotator cuff tear and to assess the long head of the biceps tendon (LHBT). (G, glenoid; HH, humeral head; SSC, subscapularis tendon.)
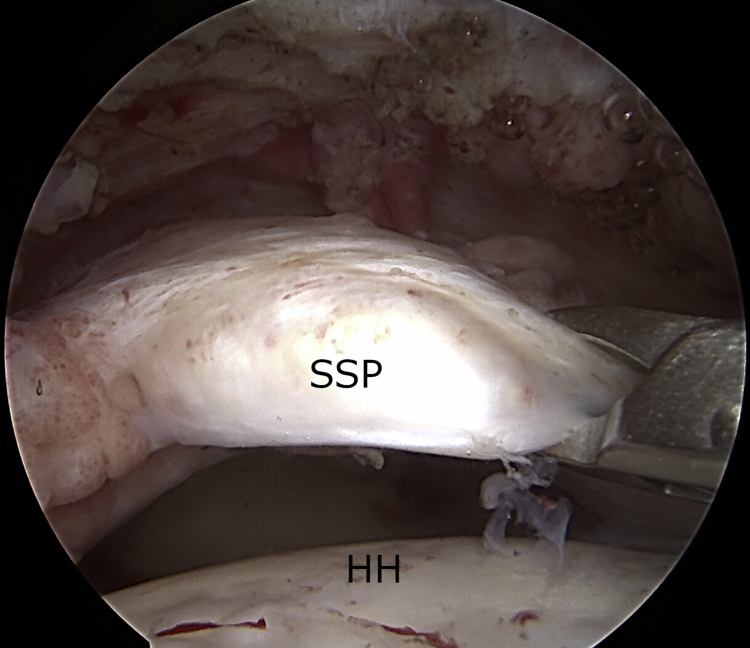
Once the intra-articular phase is completed, the scope is passed into the subacromial space through the posterior portal and the lateral portal is now created. By use of an electrocautery device and a shaver, bursectomy is performed. The scope is then switched to the lateral portal so that the bursectomy can be completed through the posterior or anterosuperior portal. The tear characteristics can then be clearly assessed: Size, shape, delamination, and tear retraction are evaluated, thus confirming the indication for a cuff-plus repair (Fig 2). The mobility and integrity of the LHBT are checked with a tendon grasper through the anterosuperior portal. The scope is now switched again into the posterior portal.
Fig 2.
Arthroscopic view (subacromial space) through lateral portal of right shoulder with patient in beach-chair position. The tear characteristics can be clearly assessed, such as size, shape, delamination, and retraction. (HH, humeral head; SSP, supraspinatus.)
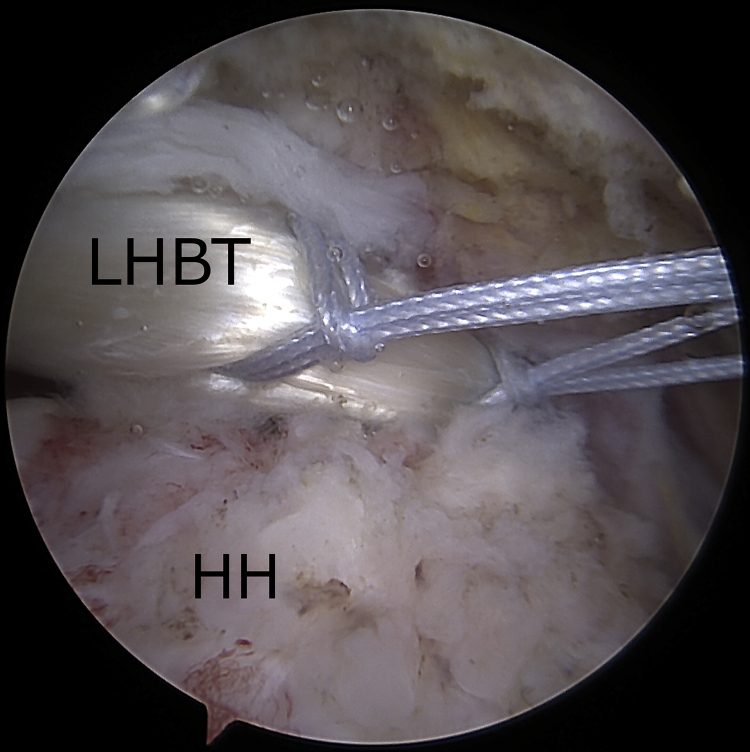
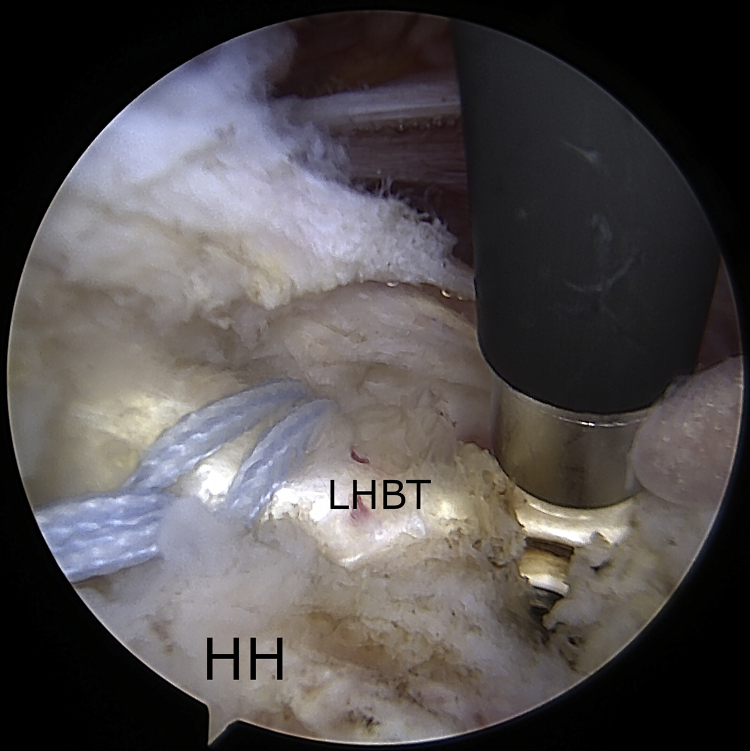
Whenever possible, footprint preservation is attempted and microfractures of the greater tuberosity are always preferred to cortical abrasion.8 By using a direct suture passer (FastPass Scorpion; Arthrex, Naples, FL), 2 high-strength permanent braided sutures (No. 2 FiberWire; Arthrex) are passed through the LHBT with a “lasso-loop” configuration (Fig 3). Sutures are placed at the intra-articular exit of the tendon on top of the intertubercular groove without taking down the transverse ligament. The LHBT is then tenotomized distally to the sutures (Fig 4) so that the proximal stump of the tendon can be rerouted posteriorly and transferred onto the supraspinatus tendon footprint with the aid of a tissue grasper. A knotless PEEK (polyether ether ketone) anchor (4.75-mm SwiveLock; Arthrex), positioned through the superolateral portal, is used to fix the LHBT into the supraspinatus footprint (Fig 5). Care is taken to position the arm in 30° of forward elevation during tendon fixation. In this way, the LHBT, which is natively attached to the glenoid, acts as the autograft for SCR.
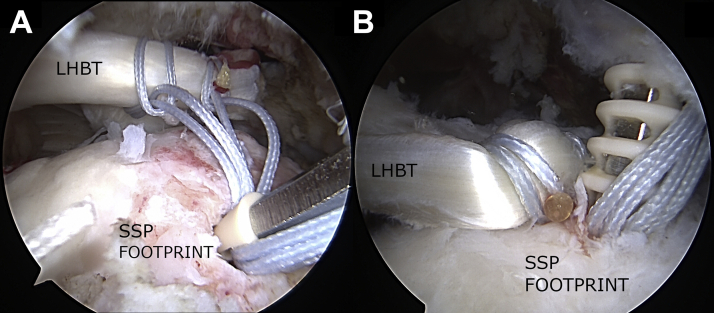
Fig 3.
Arthroscopic view (subacromial space) through posterior portal of right shoulder with patient in beach-chair position. By use of a direct suture passer, 2 high-strength permanent braided sutures (No. 2 FiberWire) are passed into the long head of the biceps tendon (LHBT) with a lasso-loop configuration. (HH, humeral head.)
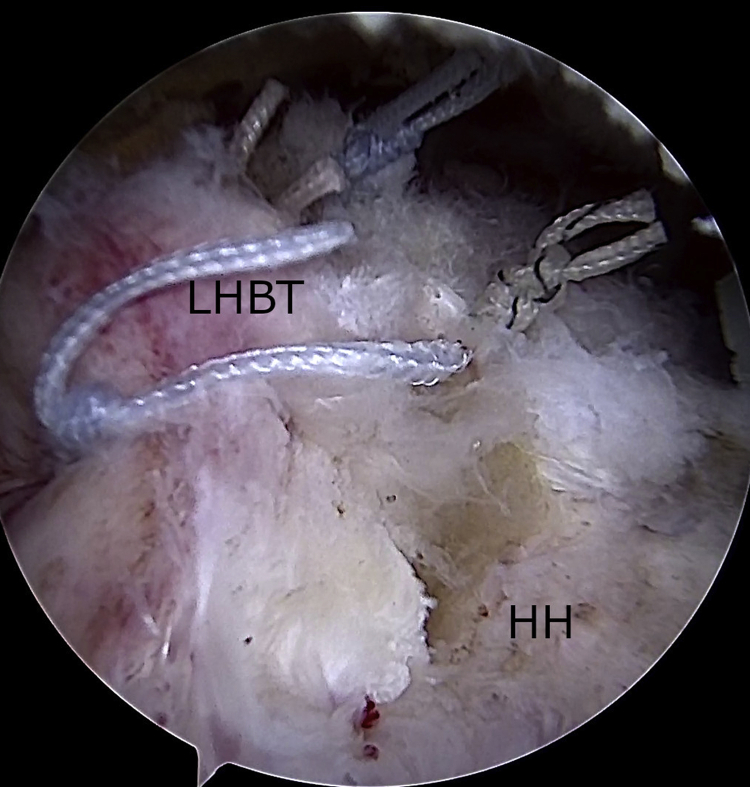
Fig 4.
Arthroscopic view (subacromial space) through posterior portal of right shoulder with patient in beach-chair position. The long head of the biceps tendon (LHBT) is tenotomized distally to the lasso-loop sutures. (HH, humeral head.)
Fig 5.
Arthroscopic view (subacromial space) through posterior portal of right shoulder with patient in beach-chair position. (A) The proximal stump of the long head of the biceps tendon (LHBT) is rerouted posteriorly and transferred onto the supraspinatus (SSP) tendon footprint. (B) A knotless PEEK anchor (4.75-mm SwiveLock), positioned through the superolateral portal, is used to fix the LHBT into the SSP footprint.
A standard cuff repair, based on tear shape, is now performed: Crescent-shaped tears can be repaired directly to the bone using suture anchors, whereas U-shaped, L-shaped, or reverse L–shaped tears require appropriate tear mobilization and side-to-side repair according to the margin convergence technique to restore a crescent shape of the tear and to allow a tension-free anchor repair. If needed, side-to-side repairs are performed with No. 2 FiberWire sutures by also including the biceps tendon (Fig 6). A single-row technique is then performed using double- or triple-loaded metal anchors (Corkscrew FTII; Arthrex) (Fig 7).
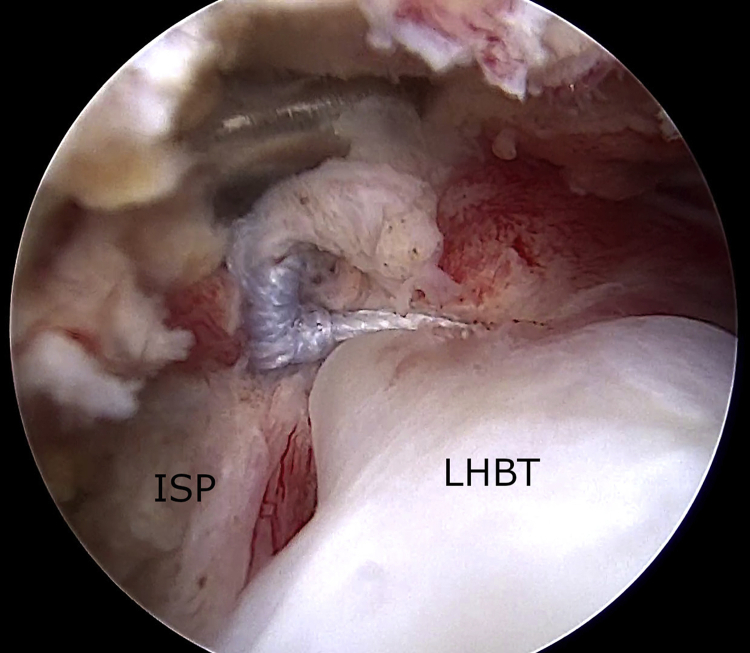
Fig 6.
Arthroscopic view (subacromial space) through lateral portal of right shoulder with patient in beach-chair position. A side-to-side rotator cuff repair is performed with No. 2 FiberWire suture. The sutures can also include the biceps tendon. (ISP, supraspinatus; LHBT, long head of biceps tendon.)
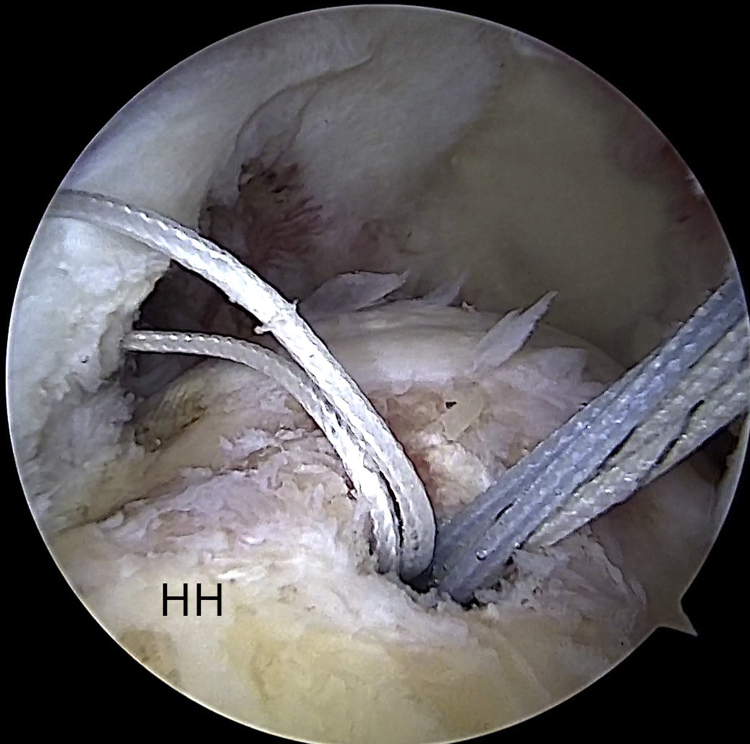
Fig 7.
Arthroscopic view (subacromial space) through posterior portal of right shoulder with patient in beach-chair position. A single-row rotator cuff repair is performed with double-loaded suture anchors (Corkscrew FTII) placed anteriorly and posteriorly to the long head of the biceps tendon. (HH, humeral head.)
Anchors are placed along the articular margin of the humeral head, anterior and/or posterior to the LHBT, depending on tear configuration. Sutures are passed through the bursal layer of the rotator cuff and through the most lateral part of the biceps stump to obtain a robust and solid construct.
If possible, the most posterior suture should include both the articular and bursal layers of the posterior cuff to avoid further delamination and/or tear extension, as well as re-establish a transverse force couple balance. After all the sutures have been passed, microfractures are performed on the greater tuberosity before knot tying (Fig 8). The sutures are finally knotted from posterior to anterior according to the direction of the force vectors (Fig 9). The surgical technique is shown in Video 1.
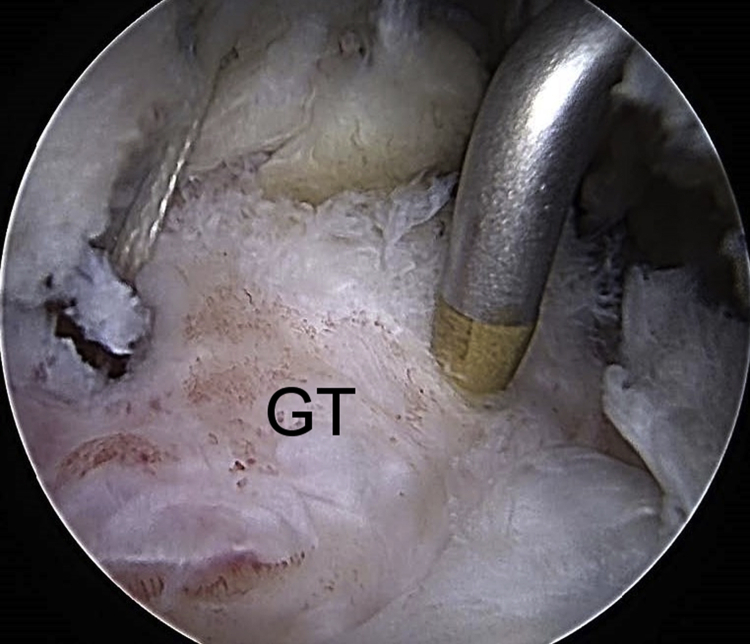
Fig 8.
Arthroscopic view (subacromial space) through posterior portal of right shoulder with patient in beach-chair position. Microfractures are performed on the greater tuberosity (GT) with an arthroscopic awl to enhance tendon-to-bone healing.
Fig 9.
Arthroscopic view (subacromial space) through posterior portal of right shoulder with patient in beach-chair position. The sutures are knotted from posterior to anterior according to the direction of the force vectors. The bursal and articular layers of the torn delaminated rotator cuff and long head of the biceps tendon (LHBT) are included in the repair. (HH, humeral head.)
Postoperative Protocol
The arm is immobilized in an abduction sling in neutral rotation for 4 weeks. The rehabilitation protocol starts 4 weeks after surgery according to the following phases:
-
•
Phase 1 (4-8 weeks after surgery): massotherapy and physical modalities for the management of pain, inflammation, and muscle contractures and passive range-of-motion (ROM) exercises
-
•
Phase 2 (9-12 weeks after surgery): active-assisted ROM exercises and closed–kinetic chain exercises to strengthen the residual rotator cuff, subscapularis, biceps, deltoid, pectoralis major, and scapular stabilizers
-
•
Phase 3 (13-16 weeks after surgery): active ROM exercises and open–kinetic chain exercises, proprioceptive and plyometric exercises, and postural rehabilitation of the kinetic chain (lumbo-pelvic, thoracolumbar, and scapulothoracic muscles)
Return to heavy manual work or sports activities is allowed 6 months after surgery. Magnetic resonance imaging is routinely performed at 12 months’ follow-up. Pearls and pitfalls of the described technique are presented in Table 1, and advantages and disadvantages are listed in Table 2.
Table 1.
Pearls and Pitfalls of Cuff-Plus Technique
| Pearls |
| Using a direct suture passer simplifies the execution of the lasso-loop suture through the LHBT. |
| Sutures should be passed into the LHBT and a pilot hole should be drilled for the anchor before LHBT tenotomy is performed. |
| Tenotomy should be performed >1 cm distal to the sutures. |
| Pitfalls |
| Hypertrophy of the LHBT may compromise the arthroscopic view: Prepare the RC for repair (bursectomy, tendon release) before biceps tenotomy and fixation. |
| Suture placement can affect the tension on the proximal stump of the LHBT (with sutures too proximal yielding high tension and sutures too distal yielding low tension). |
| The arm position can affect the tension on the LHBT during fixation (the arm should be maintained in 30° of forward elevation). |
LHBT, long head of biceps tendon; RC, rotator cuff.
Table 2.
Advantages and Disadvantages of Cuff-Plus Technique
| Advantages |
| Low cost |
| Short operative time |
| Reduced donor-site morbidity compared with other autografts (i.e., fascia lata) |
| Preservation of native glenoid insertion of LHBT (vascular supply) |
| Disadvantages |
| Need for alternative surgical techniques if LHBT is not available (poor tissue quality or previous rupture, tenotomy, and/or tenodesis) |
| Reduced surface coverage of humeral head compared with other grafts |
| Potential pain source (tension on proximal stump of LHBT) |
LHBT, long head of biceps tendon.
Discussion
Arthroscopic SCR has gained great popularity in recent years, setting itself up as one of the best available options for treating irreparable tears before consistent articular degenerative changes occur. This assumption has been progressively confirmed by biomechanical and clinical studies.9,10 Moreover, a recent clinical study showed that SCR, if used as a reinforcement for repairable cuff tears, improves structural integrity at 1 year postoperatively; the authors included medium as well as large tears and used SCR with fascia lata.11
In our opinion, at least 3 major downsides could be claimed regarding the standard SCR technique. First, although fascinating, the technique requires a long learning curve even for expert and skilled shoulder surgeons. Second, SCR surely requires a longer intraoperative time than a standard or functional cuff repair, making the procedure even more difficult owing to soft-tissue imbibition. Finally, the costs are remarkable: 4 to 7 anchors as well as additional sutures and tapes, based on the technique, could be necessary; furthermore, the cost of the graft must be added if an allograft is used.
Alternative graft sources have been proposed recently, such as LHBT autograft.5,6 Arthroscopic SCR using the proximal portion of the LHBT combines several advantages. First, the biomechanical rationale of SCR remains unchanged. Recent biomechanical studies have shown that SCR with LHBT restores shoulder stability in irreparable rotator cuff tears by re-centering the humeral head on the glenoid and that it is biomechanically equivalent to—and potentially even stronger than—fascia lata autograft in the prevention of superior humeral migration.12 Second, intraoperative times and costs are surely reduced because neither additional graft nor anchors for medial fixation are required and the technique does not require a long learning curve. Third, donor-site morbidity and the additional time required for graft harvesting, in the case of fascia lata use, are completely avoided. Finally, this pediculated graft might provide additional blood supply to the repaired rotator cuff tendons.
This article shows that the LHBT represents a viable option even for repairable cuff tears. We have presented an easy technique to perform a solid and robust cuff repair in the setting of large to massive delaminated cuff tears.
On the basis of recent studies in the literature, the incidence of delamination ranges between 37% and 92%.1 Although the role of delamination is still under debate, large to massive tears are surely more likely to retear, and delamination is a common finding in patients with partially healed defects.13,14 Therefore, it is our opinion that the arthroscopic cuff-plus technique can lower the cuff retear rate, especially in the case of large to massive tears when the residual cuff looks insufficient or too thin and reduction of the articular layer is not possible or, even worse, it requires extensive mobilization, which basically will make the repaired tissue even weaker. Moreover, the arthroscopic cuff-plus technique improves the chances of cuff healing by combining the advantages of a tension-free repair and biological augmentation obtained through the vitality of the proximal part of the LHBT.
Indeed, the technique presents some potential disadvantages that should be considered. First, the procedure cannot be accomplished in the case of a previous spontaneous tendon rupture or revision surgical procedure, in which the biceps underwent previous tenotomy or tenodesis. Moreover, degenerative changes of the LHBT cannot be completely ruled out before surgery; therefore, the surgeon has to take into consideration alternative surgical options if the LHBT is unsuitable. Second, the surface coverage of the humeral head is rather small in comparison with that obtained with standard SCR, which could determine possible lower control of superior escape of the humeral head. Finally, the fixed proximal stump of the LHBT might represent a potential source of postoperative pain.
Clinical evidence about the efficacy of the cuff-plus technique is surely needed. Nonetheless, the anatomic and biomechanical features in support of this technique represent a solid foundation for further studies.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: G. Milano receives personal fees from Arthrex and Smith & Nephew and nonfinancial support from Arthrex, Wright, and FGP, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic repair of large to massive delaminated rotator cuff tear in right shoulder with autologous long head of biceps tendon graft using arthroscopic cuff-plus technique.
References
- 1.Kim Y.K., Jung K.H., Park C.K., Yun S.B. Morphologic factors related to repair outcomes for delaminated rotator cuff tears: A minimum 2-year retrospective comparison study. Arthroscopy. 2019;35:332–340. doi: 10.1016/j.arthro.2018.08.040. [DOI] [PubMed] [Google Scholar]
- 2.Mihata T., McGarry M.H., Kahn T., Goldberg I., Neo M., Lee T.Q. Biomechanical role of capsular continuity in superior capsule reconstruction for irreparable tears of the supraspinatus tendon. Am J Sports Med. 2016;44:1423–1430. doi: 10.1177/0363546516631751. [DOI] [PubMed] [Google Scholar]
- 3.Tokish J.M., Beicker C. Superior capsule reconstruction technique using an acellular dermal allograft. Arthrosc Tech. 2015;4:e833–e839. doi: 10.1016/j.eats.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sochacki K.R., McCulloch P.C., Lintner D.M., Harris J.D. Superior capsular reconstruction for massive rotator cuff tear leads to significant improvement in range of motion and clinical outcomes: A systematic review. Arthroscopy. 2019;35:1269–1277. doi: 10.1016/j.arthro.2018.10.129. [DOI] [PubMed] [Google Scholar]
- 5.Chillemi C., Mantovani M., Gigante A. Superior capsular reconstruction of the shoulder: The ABC (arthroscopic biceps Chillemi) technique. Eur J Orthop Surg Traumatol. 2018;28:1215–1223. doi: 10.1007/s00590-018-2183-1. [DOI] [PubMed] [Google Scholar]
- 6.Kim Y.-S., Lee H.-J., Park I., Sung G.Y., Kim D.-J., Kim J.-H. Arthroscopic in situ superior capsular reconstruction using the long head of the biceps tendon. Arthrosc Tech. 2018;7:e97–e103. doi: 10.1016/j.eats.2017.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pauzenberger L., Heuberer P.R., Dyrna F. Double-layer rotator cuff repair: Anatomic reconstruction of the superior capsule and rotator cuff improves biomechanical properties in repairs of delaminated rotator cuff tears. Am J Sports Med. 2018;46:3165–3173. doi: 10.1177/0363546518796818. [DOI] [PubMed] [Google Scholar]
- 8.Li Z., Zhang Y. Efficacy of bone marrow stimulation in arthroscopic repair of full thickness rotator cuff tears: A meta-analysis. J Orthop Surg Res. 2019;14:36. doi: 10.1186/s13018-019-1072-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mihata T., Lee T.Q., Fukunishi K. Return to sports and physical work after arthroscopic superior capsule reconstruction among patients with irreparable rotator cuff tears. Am J Sports Med. 2018;46:1077–1083. doi: 10.1177/0363546517753387. [DOI] [PubMed] [Google Scholar]
- 10.Catapano M., de Sa D., Ekhtiari S., Lin A., Bedi A., Lesniak B.P. Arthroscopic superior capsular reconstruction for massive, irreparable rotator cuff tears: A systematic review of modern literature. Arthroscopy. 2019;35:1243–1253. doi: 10.1016/j.arthro.2018.09.033. [DOI] [PubMed] [Google Scholar]
- 11.Mihata T., Lee T.Q., Hasegawa A. Superior capsule reconstruction for reinforcement of arthroscopic rotator cuff repair improves cuff integrity. Am J Sports Med. 2018;47:379–388. doi: 10.1177/0363546518816689. [DOI] [PubMed] [Google Scholar]
- 12.Han F., Kong C.H., Hasan M.Y., Ramruttun A.K., Kumar V.P. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: A biomechanical study on cadavers. Orthop Traumatol Surg Res. 2019;105:257–263. doi: 10.1016/j.otsr.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 13.Kwon J., Lee Y.H., Kim S.H., Ko J.H., Park B.K., Oh J.H. Delamination does not affect outcomes after arthroscopic rotator cuff repair as compared with nondelaminated rotator cuff tears: A study of 1043 consecutive cases. Am J Sports Med. 2019;47:674–681. doi: 10.1177/0363546518817764. [DOI] [PubMed] [Google Scholar]
- 14.Gwak H.-C., Kim C.-W., Kim J.-H., Choo H.-J., Sagong S.-Y., Shin J. Delaminated rotator cuff tear: Extension of delamination and cuff integrity after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2015;24:719–726. doi: 10.1016/j.jse.2014.09.027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic repair of large to massive delaminated rotator cuff tear in right shoulder with autologous long head of biceps tendon graft using arthroscopic cuff-plus technique.