Abstract
The role of telehealth in orthopedic surgery is rapidly expanding, a movement largely brought about by the coronavirus disease 2019 (COVID-19) pandemic. Virtual clinic encounters using a video chat platform or a simple telephone call offer the patient and surgeon numerous advantages that are now better appreciated by the orthopedic community at large. However, barriers to effective patient evaluation exist, and a successful patient assessment is highly dependent on technique. In particular, performing a shoulder physical examination during a virtual encounter poses many obstacles. We present a technique to complete a patient-led, comprehensive shoulder physical examination using an easy-to-understand pictorial guide called the Shoulder Telehealth Assessment Tool (STAT). A STAT form is provided to the patient and designed to be completed at home without the real-time instruction of a provider, before the virtual encounter. Parameters include assessments of all planes of shoulder range of motion, visual analog scale (VAS) and Single Assessment Numeric Evaluation (SANE) scores, and the components necessary to allow for conversion to an abbreviated Constant shoulder score if the provider so desires.
Telehealth is a relatively new entity in orthopedics. By the definition of the Centers for Medicare and Medicare Services, a telehealth visit uses any telecommunication system between a provider and a patient, including telephone encounters.1, 2, 3, 4 Telemedicine is a form of telehealth that uses, at minimum, video and audio equipment.3,4 Telehealth services afford patients and providers certain advantages over in-person clinical visits. These services have been shown to increase access to health care in rural populations.5,6 The use of telemedicine technology has been shown to be cost effective, and patients were equally satisfied with telemedicine and in-person follow-up appointments.6, 7, 8, 9, 10 A major limitation to the widespread use of telehealth services has been its slow acceptance by Medicare.11
The coronavirus disease 2019 (COVID-19) pandemic has had far-reaching effects on the American medical infrastructure nationwide, allowing for an unprecedented peek at what possibilities lie ahead in the field of telehealth. The Centers for Disease Control and Prevention (CDC) promoted the increased use of telehealth services to facilitate patient encounters while maintaining proper social distancing precautions.1,2 Subsequently, Medicare temporarily expanded reimbursements to include encounters using video or phone conferencing under the Coronavirus Preparedness and Response Supplemental Appropriations Act and Section 1135 waiver.3 Through somewhat of a trial by error, telehealth and orthopedics have been merged, with 73% of orthopedic departments implementing telehealth services, in 1 study.12 In the process, barriers to effective patient evaluation using phone or video conference were identified. As telehealth in orthopedics is likely here to stay, technological innovation and practical adaptations are of value now, and for the future.
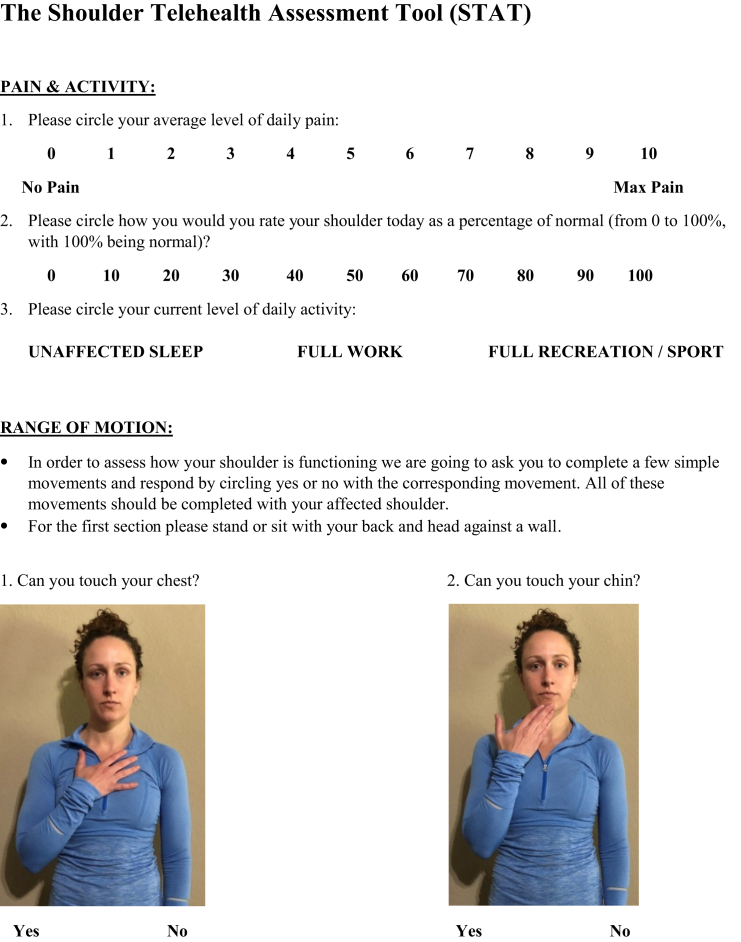
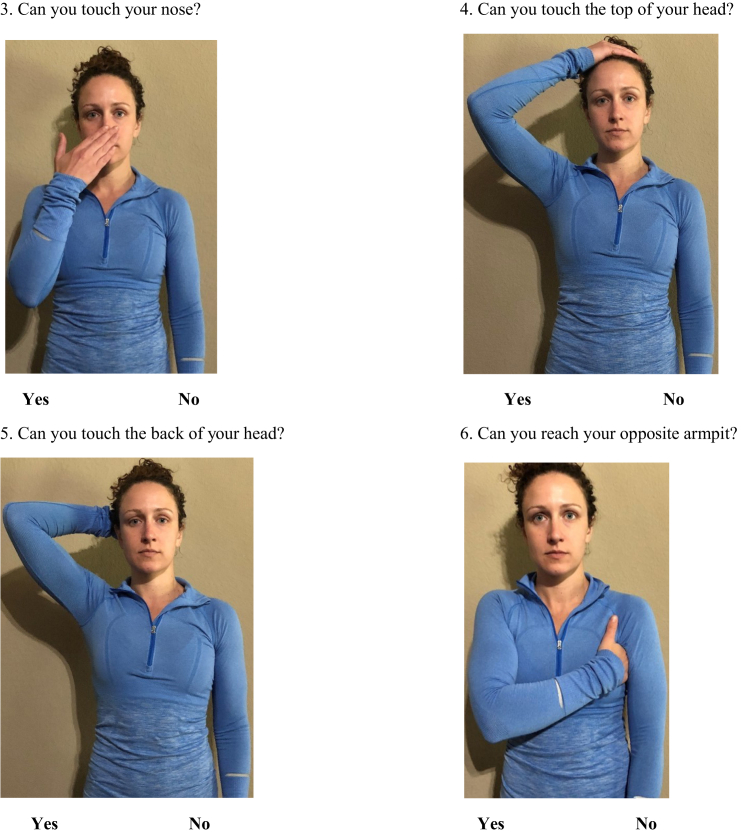
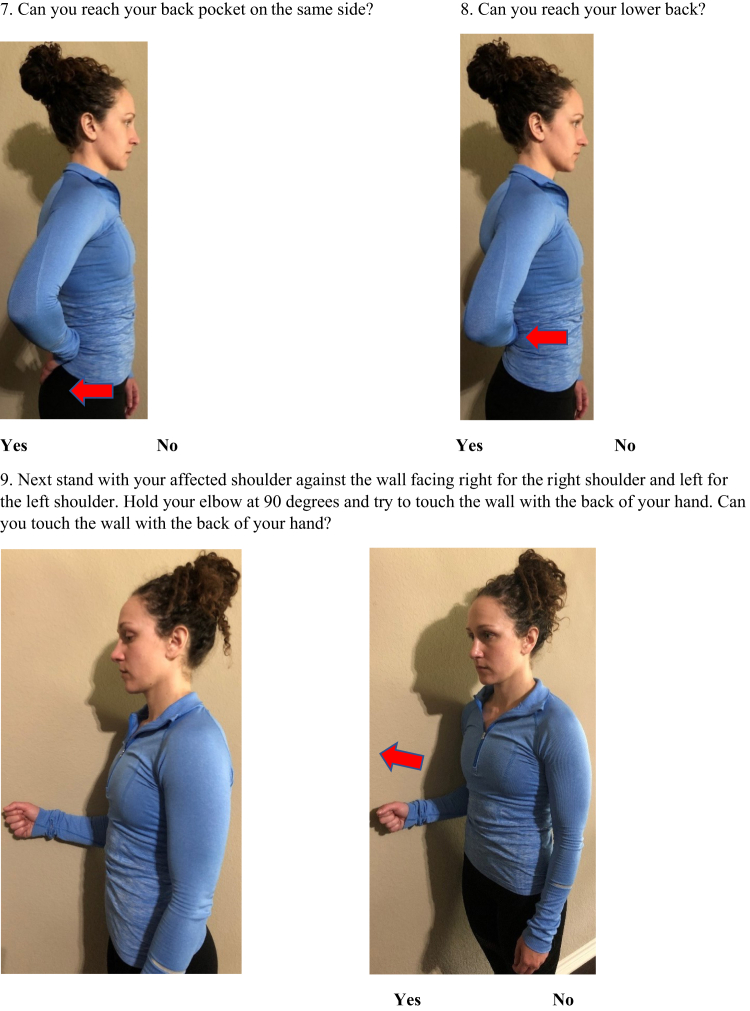
With the Shoulder Telehealth Assessment Tool (STAT), the authors sought to develop a shoulder physical examination routine that could be easily completed by the patient at home before the electronic visit, without the real-time instruction of a provider. The form includes visual analog scale (VAS) and Single Assessment Numeric Evaluation (SANE) scores and was designed using previous literature that correlates simple movements to degrees of motion.9,13, 14, 15, 16, 17, 18 The comprehensive examination was designed to provide accurate data regarding shoulder range of motion and identify shoulder pathology in the preoperative or postoperative patient, even if the visit is limited to a simple phone call. An abbreviated Constant score can then be calculated from the collected data.13 Secondarily, this technique could serve as an example for further research in the development of reliable telehealth physical examination tools for other joints.
Technique
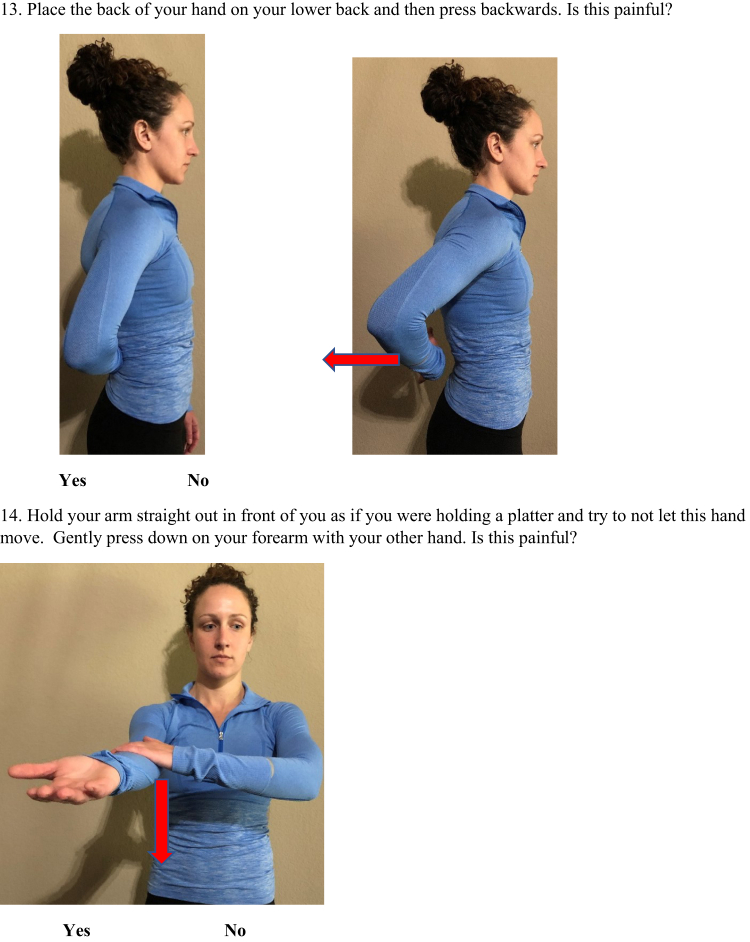
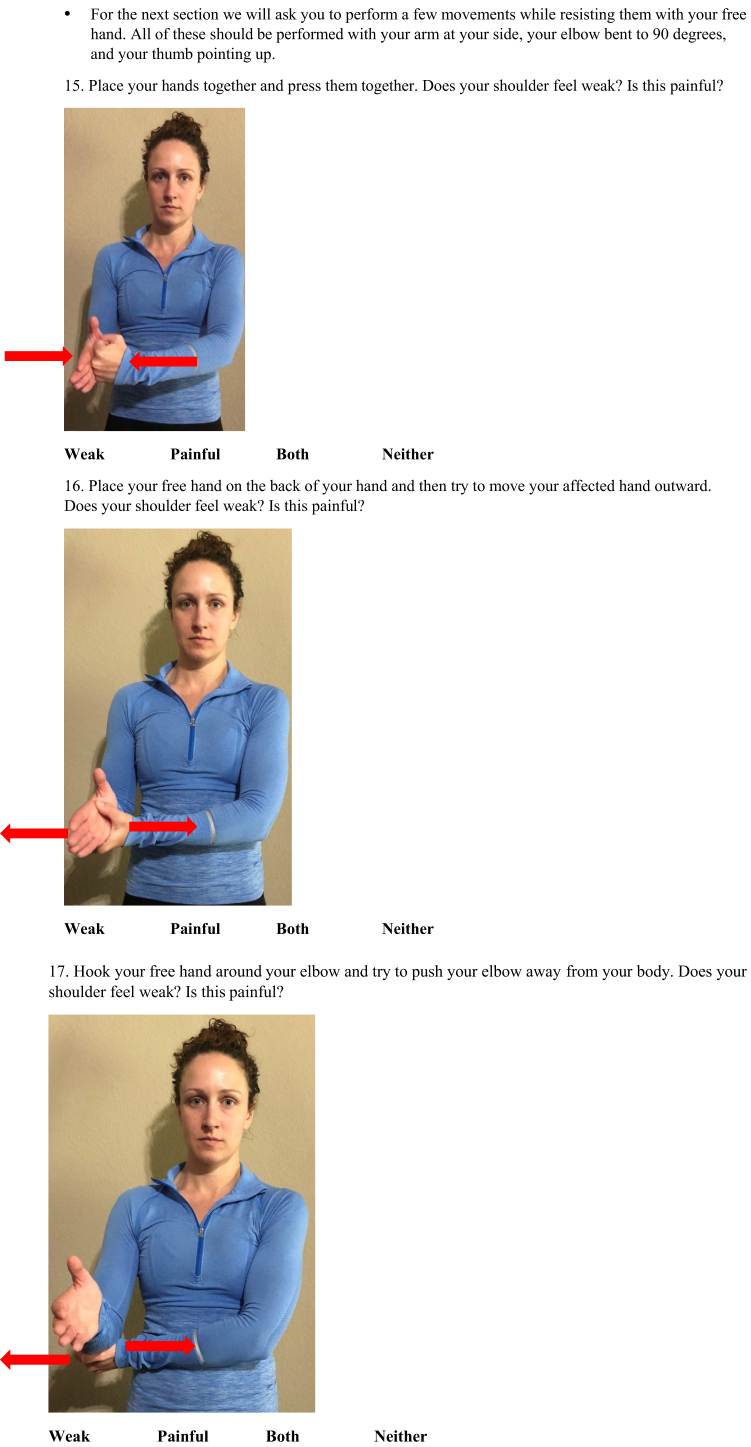
The patient is instructed through simple movements compiled in an easy-to-understand, pictorial guide (Fig 1) that is distributed electronically or through regular mail before the scheduled e-visit (Video 1). The patient is instructed to complete this form before the e-visit. The form can be reviewed with either a clinic staff member or the surgeon directly during the encounter. Any questions the patient has regarding the prescribed maneuvers can be addressed during the encounter. If the encounter is performed using video chat, the patient and provider have the added advantage of visually communicating about the movements to aid in patient understanding. However, the physical examination form design is intended to limit the amount of required communication about maneuver technique between patient and surgeon during the encounter. We aimed to eliminate the need for video chat altogether, to avoid increased equipment requirements for the patient, obviate the need to instruct patients during the encounter, and remove the hassle with adjusting the video angle to capture the maneuvers.
Fig 1.
The Shoulder Telehealth Assessment Tool (STAT) includes visual analog scale (VAS) and Single Assessment Numeric Evaluation (SANE) scores and was designed using previous literature that correlates simple movements to degrees of motion. An abbreviated Constant score can be calculated from the collected data, if the provider so desires.
We use a standard set of tasks to assess multiple planes of shoulder range of motion and special tests of the shoulder to simulate a standard in-person physical examination performed by an orthopedic surgeon (Fig 1). These movements have been previously studied in the physical therapy literature to correspond to minimum shoulder ranges of motion.14, 15, 16,19 This form is complete with ≥1 illustration per movement and “yes or no” options listed to allow the patient to accurately track responses. The tasks are numbered for review during the encounter. With the data collected from the form, an abbreviated Constant shoulder score can be calculated, if the provider so desires.13
First, VAS score, SANE score, and activity level assessment provide patient feedback and aid in conversion to the Constant shoulder score.13,17,18 To assess forward flexion, the patient is asked, “While standing or sitting upright with your head and back against a wall, with your affected shoulder, can you touch your chest, chin, nose, top of your head, and back of your head?” These movements correspond to a minimum of 30°, 35°, 60°, 105°, and 110°, respectively, of forward flexion as well as 0°, 30°, 55°, 110°, and 125° of shoulder abduction.14 Each of these movements should be completed with the back and head against the wall to control for scapular and thoracic motion. To assess adduction, the patient is asked, “While standing or sitting upright, can you touch your opposite armpit with your palm?” This corresponds not only to 115° of adduction, but also ∼55° of forward flexion.14 For internal rotation, the patient is asked, “Can you reach your back pocket on the same side, and can you touch your lower back?” These movements correspond to a minimum of 50° of internal rotation and 50° of shoulder extension.14, 15, 16,19 The “hand-behind-the-back” maneuver is an accepted method to quantify shoulder internal rotation.20 However, determining the exact level would be difficult without an in-person examination. For external rotation, the patient is instructed to stand with the affected shoulder against the wall and elbow flexed to 90° and asked, “Can you place the back of your hand against the wall?” This corresponds to approximately neutral external rotation.19
Special tests are more complicated, but several can be performed without an examiner or assistant present, with discernable results. For example, drop arm, cross body, belly press, lift off, and Speed's tests can elicit pain at the shoulder and signal a positive test to the patient that can be recorded. Isometric strength testing of internal and external rotation and abduction can provide the clinician with additional valuable information if the patient notes feelings of subjective weakness, pain, both, or neither with these maneuvers.
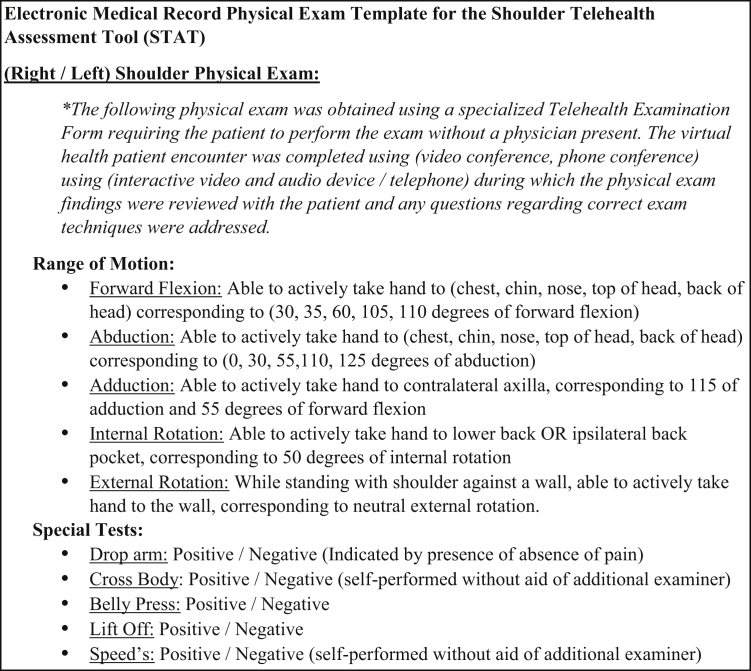
Finally, we provide an example documentation template that can be used alongside the examination form when documenting the patient encounter in an electronic medical record system (Fig 2).
Fig 2.
The text in this figure can be copied as a saved template into the individual provider's electronic medical record program and used during or after each telehealth visit to enhance documentation efficiency.
Discussion
The abrupt turn to telehealth during the coronavirus pandemic will likely result in a large amount of data and anecdotal provider testimonials regarding its usefulness. Separate from the influence of the pandemic crisis, in 2020, legislation passed to increase telehealth services covered under the Medicare Advantage plan.11 The role of telehealth in orthopedics can only be expected to expand.
Previous studies have described successful telehealth physical examination using live video feed to observe patient movements.21, 22, 23 However, this requires the patient and provider to carefully coordinate a routine while also capturing the necessary angles to record the examination, often requiring another person to assist with filming.21,23 The provider must instruct the patient in these movements, ensure that the recording is adequate, and observe to assess range of motion. In a recent study, 70.8% of orthopedic telemedicine encounters were performed by the surgeon without clinic staff or advanced practice provider assistance.24 The time constraints of a telemedicine visit might preclude the surgeon from performing a thorough and effective video-based physical examination with each patient.
Although good results were found in a study of video chat postoperative visits after arthroscopic rotator cuff surgery, there were limitations to the study design.22 Patients were excluded if they were unwilling or unable to use the video platform becuase of lack of skill, equipment, or high-speed internet.22 The results demonstrate that motivated, capable patients can have successful follow-up using telemedicine. The utility of these services for patients who are resistant to the idea of telemedicine or lack the resources necessary to partake in videoconferencing is less clear. Cellular devices with functioning cameras are nearly ubiquitous across our society,25 but the added patient requirements to possess a functioning videoconferencing device (smartphone, tablet, or computer), the correct teleconferencing application to connect with the physician, and the skills necessary to effectively film physical examination maneuvers may actually present additional obstacles to health care accessibility.
If implemented effectively, telehealth services have the potential to increase health care availability to elderly patients, nursing home residents, or patients in rural settings or socioeconomically disadvantaged situations. It is our hope that patient-led, picture-driven physical examination forms might help simplify the process of obtaining physical examination data in the most limited social situations. Although videoconferencing certainly aids in telehealth patient evaluations, the physical examination form presented in this study can be effective even if the telehealth encounter is limited to a simple telephone call.
A limitation of this technique is the lack of validation data to correlate it with a standard, in-person physical examination completed by an orthopedic surgeon. Patient safety must be assessed using this form in place of regular clinic follow-up. We sought to incorporate previously validated and published pain scores and movements in the design of the form. Future validation of this physical examination form is planned. The authors believe that the physical examination form could be of great use during the transition to telehealth and thus felt it prudent to disseminate this material in a timely manner. In addition, we hope that this physical examination form will serve as a template for additional physical examination aids, applicable to other orthopedic subspecialties and other components of a comprehensive orthopedic physical examination.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Using the Shoulder Telehealth Assessment Tool (STAT), a comprehensive shoulder physical examination can be completed by the patient at home before the electronic visit, without the real-time instruction of a provider. The form includes visual analog scale (VAS) and Single Assessment Numeric Evaluation (SANE) scores and was designed using previous literature that correlates simple movements to degrees of motion. An Apple Mac Book Pro, Apple iPhone, Apple air pods, and Dell desktop computer were used for the telehealth encounter filmed in the video.
References
- 1.Centers for Disease Control and Prevention Interim guidance for Healthcare Facilities: Preparing for community Transmission of COVID-19 in the US. Feb. 29, 2020. www.cdc.gov/coronavirus/2019-ncov/healthcare-facilities/guidance-hcf.html
- 2.American College of Surgeons COVID-19 Guidelines for triage of orthopaedic patients. March 24, 2020. www.facs.org/covid-19/clinical-guidance/elective-case/orthopaedics
- 3.Centers for Medicare & Medicaid Services Medicare telemedicine health care provider provider Fact Sheet. March 17, 2020, CMS. www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- 4.Centers for Medicare & Medicaid Services Telemedicine. www.medicaid.gov/medicaid/benefits/telemedicine/index.html
- 5.Prada C., Izquierdo N., Traipe R., Figueroa C. Results of a new telemedicine strategy in traumatology and orthopedics. Telemed J E Health. 2020;26:665–670. doi: 10.1089/tmj.2019.0090. [DOI] [PubMed] [Google Scholar]
- 6.Buvik A., Bergmo T.S., Bugge E., Smaabrekke A., Wilsgaard T., Olsen J.A. Cost-effectiveness of telemedicine in remote orthopedic consultations: Randomized controlled trial. J Med Internet Res. 2019;21:e11330. doi: 10.2196/11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sathiyakumar V., Apfeld J.C., Obremskey W.T., Thakore R.V., Sethi M.K. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: A pilot study. J Orthop Trauma. 2015;29:e139–e145. doi: 10.1097/BOT.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 8.Buvik A., Bugge E., Knutsen G., Småbrekke A., Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: A randomised controlled trial. J Telemed Telecare. 2019;25:451–459. doi: 10.1177/1357633X18783921. [DOI] [PubMed] [Google Scholar]
- 9.Buvik A., Bugge E., Knutsen G., Småbrekke A., Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: A randomised controlled trial. BMC Health Serv Res. 2016;16:483. doi: 10.1186/s12913-016-1717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wongworawat M.D., Capistrant G., Stephenson J.M. The opportunity awaits to lead orthopaedic telehealth innovation: AOA critical issues. J Bone Joint Surg Am. 2017;99:e93. doi: 10.2106/JBJS.16.01095. [DOI] [PubMed] [Google Scholar]
- 11.Rubin R. Medicare advantage expands telehealth services. JAMA. 2019;321:1964. doi: 10.1001/jama.2019.6674. [DOI] [PubMed] [Google Scholar]
- 12.Lezak B.A., Cole P.A., Jr., Schroder L.K., Cole P.A. Global experience of orthopaedic trauma surgeons facing COVID-19: A survey highlighting the global orthopaedic response. Int Orthop. 2020;44:1519–1529. doi: 10.1007/s00264-020-04644-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Constant C.R., Murley A.H. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 14.Oosterwijk A.M., Nieuwenhuis M.K., van der Schans C.P., Mouton L.J. Shoulder and elbow range of motion for the performance of activities of daily living: A systematic review. Physiother Theory Pract. 2018;34:505–528. doi: 10.1080/09593985.2017.1422206. [DOI] [PubMed] [Google Scholar]
- 15.Gates D.H., Walters L.S., Cowley J., Wilken J.M., Resnik L. Range of motion requirements for upper-limb activities of daily living. Am J Occup Ther. 2016;70 doi: 10.5014/ajot.2016.015487. 7001350010p1-700135001010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sraj S.A. Internal rotation behind-the-back angle: A reliable angular measurement for shoulder internal rotation behind the back. Sports Health. 2015;7:299–302. doi: 10.1177/1941738113502159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reed M.D., Van Nostran W. Assessing pain intensity with the visual analog scale: A plea for uniformity. J Clin Pharmacol. 2014;54:241–244. doi: 10.1002/jcph.250. [DOI] [PubMed] [Google Scholar]
- 18.Retzky J.S., Baker M., Hannan C.V., Srikumaran U. Single assessment numeric evaluation scores correlate positively with American Shoulder and Elbow Surgeons scores postoperatively in patients undergoing rotator cuff repair. J Shoulder Elbow Surg. 2020;29:146–149. doi: 10.1016/j.jse.2019.05.039. [DOI] [PubMed] [Google Scholar]
- 19.Khadilkar L., MacDermid J.C., Sinden K.E., Jenkyn T.R., Birmingham T.B., Athwal G.S. An analysis of functional shoulder movements during task performance using Dartfish movement analysis software. Int J Shoulder Surg. 2014;8:1–9. doi: 10.4103/0973-6042.131847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richards R.R., An K.N., LU Bigliani. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 21.Good D.W., Lui D.F., Leonard M., Morris S., McElwain J.P. Skype: A tool for functional assessment in orthopaedic research. J Telemed Telecare. 2012;18:94–98. doi: 10.1258/jtt.2011.110814. [DOI] [PubMed] [Google Scholar]
- 22.Kane L.T., Thakar O., Jamgochian G. The role of telehealth as a platform for postoperative visits following rotator cuff repair: A prospective, randomized controlled trial. J Shoulder Elbow Surg. 2020;29:775–783. doi: 10.1016/j.jse.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Cabana F., Boissy P., Tousignant M., Moffet H., Corriveau H., Dumais R. Interrater agreement between telerehabilitation and face-to-face clinical outcome measurements for total knee arthroplasty. Telemed J E Health. 2010;16:293–298. doi: 10.1089/tmj.2009.0106. [DOI] [PubMed] [Google Scholar]
- 24.Parisien R.L., Shin M., Constant M. Telehealth utilization in response to the novel coronavirus (COVID-19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg. 2020;28:e487–e492. doi: 10.5435/JAAOS-D-20-00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Langford A.T., Solid C.A., Scott E. Mobile phone ownership, health apps, and tablet use in US adults with a self-reported history of hypertension: Cross-sectional study. JMIR Mhealth Uhealth. 2019;7:e12228. doi: 10.2196/12228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Using the Shoulder Telehealth Assessment Tool (STAT), a comprehensive shoulder physical examination can be completed by the patient at home before the electronic visit, without the real-time instruction of a provider. The form includes visual analog scale (VAS) and Single Assessment Numeric Evaluation (SANE) scores and was designed using previous literature that correlates simple movements to degrees of motion. An Apple Mac Book Pro, Apple iPhone, Apple air pods, and Dell desktop computer were used for the telehealth encounter filmed in the video.