Abstract
The superior capsular reconstruction (SCR) is an arthroscopic surgical technique recently introduced as an effective solution to restore the defect of superior articular capsule in massive rotator cuff tears that cannot be repaired anatomically. The SCR retains static stability and inhibits the proximal humeral migration, thereby optimizing the force couples about the shoulder. In this surgical technique paper, we present our technique of SCR using a double bundle construct of long head of biceps tendon, called the “box” technique. It is always combined with partial rotator cuff repair.
Massive irreparable rotator cuff (RC) tears (RCT) in a young and active population have been a challenging clinical problem to treat. The defect of the superior capsule in these cases results in increased glenohumeral translation, particularly in the superior direction.1 The biomechanical consequences are the loss of superior stabilization, the humeral head malposition, and the dysfunctional muscular fulcrum, which contribute to the clinical manifestations of pain and ineffective muscle action. Superior capsular reconstruction (SCR) with fascia lata autograft could reverse proximal humeral migration, thereby optimizing the force couples about the shoulder.2, 3, 4 Recently, several new graft sources and techniques for SCR have emerged.5, 6, 7, 8, 9
In young or active patients with massive RCT without glenohumeral arthritis, joint preservation is the preferable treatment principle.10 If complete anatomical repair is not possible, partial repair combined with SCR leads to improved functional outcome and active range of motion for active elevation and external rotation.11, 12, 13
The long head of biceps tendon (LHBT) has recently gained attention as an alternative autograft source to fascia lata autografts or dermal allografts because it is available locally and, as such, is free of costs and potentially time-saving, theoretically less technically demanding, and also minimizes donor site morbidity.14, 15, 16, 17, 18 We use this graft source for SCR for our patients with massive irreparable RCT without glenohumeral arthritis in combination with partial RC repair. The need for a more effective coverage of the humeral head to have the most effective restoration of biomechanics made us to develop a technique that uses 2 bundles of LHBT instead of 1 and therefore more sites of fixation; the “box” technique and the rationale are described in this study.
Surgical Technique
Patient Evaluation and Indications
After physical examination and imaging evaluation with radiographs and magnetic resonance imaging, patients with the findings listed in Table 1 are the best candidates for this technique.
Table 1.
Indications and Contraindications of the Box Technique Using a Double-Bundle LHBT Autograft for SCR
| Indications | Contraindications |
|---|---|
| Intact subscapularis tendon or tear without anterosuperior escape (Lafosse types I-IV19) | Glenohumeral joint osteoarthritis Cuff tear arthropathy Hamada ≥3 |
| Symptomatic massive (diameter >5 cm20 or involvement of 2 or more tendons21) superior or posterosuperior rotator cuff tear (supraspinatus and/or infraspinatus) | Intra-articular tear of LHBT >30% of its substance SLAP III or greater22 Already torn proximal LHBT |
If this RC tear is irreparable∗
|
Anterosuperior escape Lafosse type V subscapularis tendon tear19 (MRI tendon retraction, fatty infiltration) Arthroscopic confirmation (not amenable to repair) |
| LHBT intra-articular part with fraying or tear no more than 30%, SLAP no worse than type II22 | Deltoid muscle atrophy or axillary nerve injury |
| Intact teres minor No or minimal (stage 1) fatty infiltration of teres minor |
Active elevation at scapular plane <45° (after lidocaine injection if pain exists), with normal passive ROM |
LHBT, long head biceps tendon; MRI, magnetic resonance imaging; RC, rotator cuff; SCR, superior capsular reconstruction; SLAP, superior labrum tear from anterior to posterior.
Irreparable means inability to anatomically restore the RC tear. Therefore, “partial repaired RC tears” belong within this definition of “irreparable tears” because partial repair is not an anatomical repair of the tear.
Glenohumeral Arthroscopy
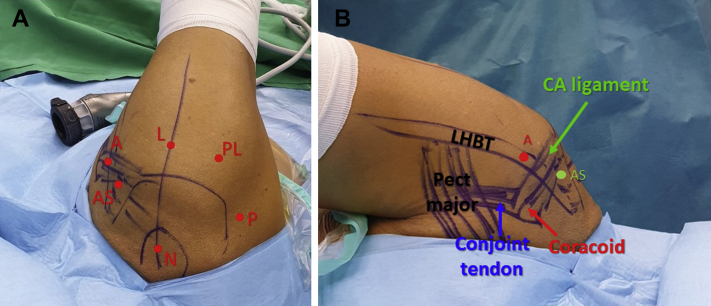
The patient is placed in the lateral decubitus position with 3 to 4 kg traction in 30° abduction at scapular plane (Fig 1). We first perform glenohumeral arthroscopy via the standard posterior portal with a 30° scope. Any subscapularis tendon tear is repaired with anchors-sutures through the anterosuperior portal.
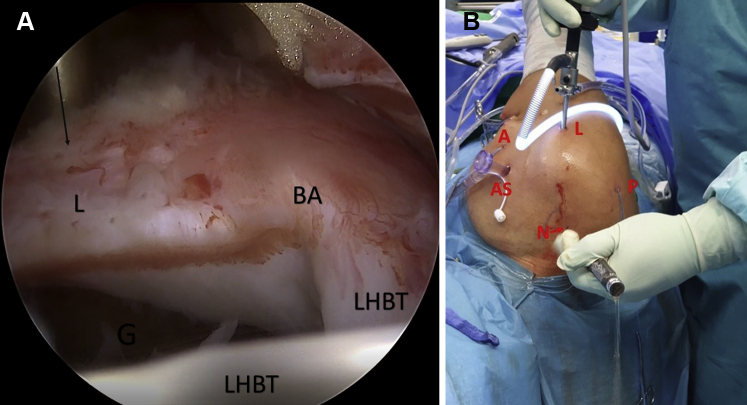
Fig 1.
Positioning and portals, (A) outside superior and (B) anterior view. The patient is placed in the lateral decubitus position with 3 to 4 kg traction in 30° abduction at the scapular plane. The standard glenohumeral portals that are used are the posterior portal, created 2 cm inferiorly and 1 to 2 cm medially to the posterior acromial corner and the anterosuperior portal (using a spinal needle outside-inside technique) created just medially to the anterolateral corner of the acromion, through the rotator interval, just distally to the intraarticular part of the long head biceps tendon (LHBT). Also, standard subacromial portals are used: anterior portal (using a spinal needle outside-inside technique), at the level of bicipital groove directed perpendicularly to the LHBT; lateral portal, located 2 to 3 cm distal to the lateral edge of the acromion passing through the deltoid muscle. Accessory portals that are usually required are the Neviaser portal (created in the superior soft spot surrounded by the clavicle anteriorly, the medial acromion, and the spine of the scapula posteriorly. The skin incision is located 1 cm medial to the medial border of the acromion) and the posterolateral portal (from a skin incision located 2 cm below the lateral edge of the acromion, slightly anteriorly to the prolongation of the posterior edge of the acromion into the subacromial bursa).
LHBT Evaluation
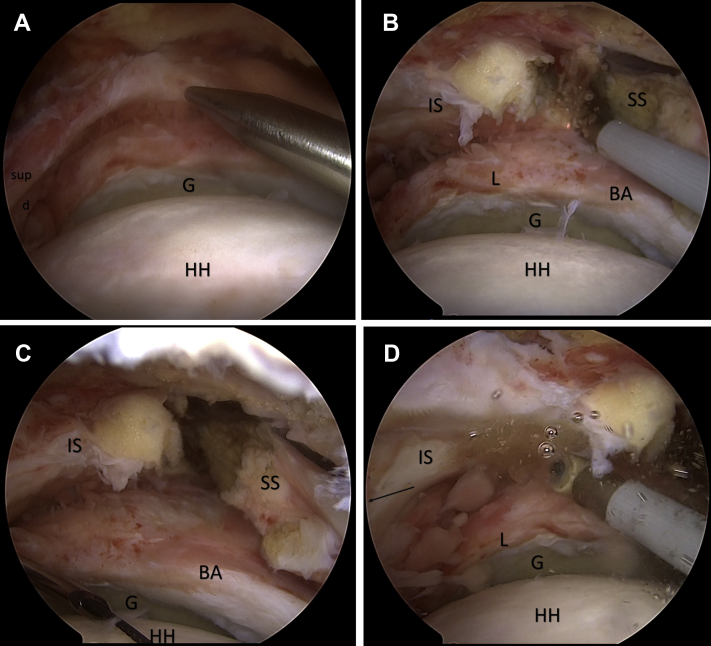
The intraarticular part of the LHBT is evaluated and the stability of the biceps anchor insertion is tested using a probe to exclude a SLAP lesion worse than type II (Snyder classification22) or an intraarticular tear >30% (Table 1; Fig 2; Video 1). In cases of SLAP II, we always consider repair with suture anchor.
Fig 2.
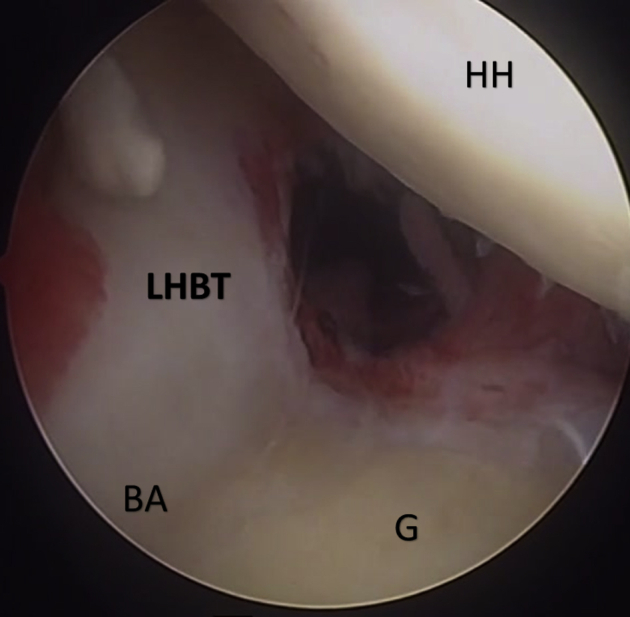
Arthroscopic view from the posterior portal of the right shoulder with patient in lateral decubitus position. Inspection of the glenohumeral joint and the LHBT. The intraarticular part of the LHBT is evaluated and the stability of the biceps anchor insertion is tested. The ideal cases for the superior capsular reconstruction with the double-bundle LHBT are complete posterosuperior rotator cuff tears with suitable LHBT quality: intra-articular LHBT tear <30% and no worse than type II SLAP lesion. In cases of SLAP II, we always consider repair with suture anchor. (BA, biceps anchor; G, glenoid surface; HH, humeral head; LHBT, long head of the biceps tendon).
Subacromial Arthroscopy, Recognition, and Preparation of RCT
We scope the subacromial space through the posterior portal. We create the lateral portal and we debride the subacromial space, the subdeltoid bursa, and the bursa over the torn rotator cuff to recognize the pattern and size of the tear. We use the anterior and anterosuperior portals to approach the anterior part of subacromial space. With the scope in the lateral portal, we perform in all cases anterior slide release, articular and bursal side release of the rotator cuff to mobilize it, evaluate its excursion, and have an estimation for the tension on the site of the repair (Video 1; Fig 3).
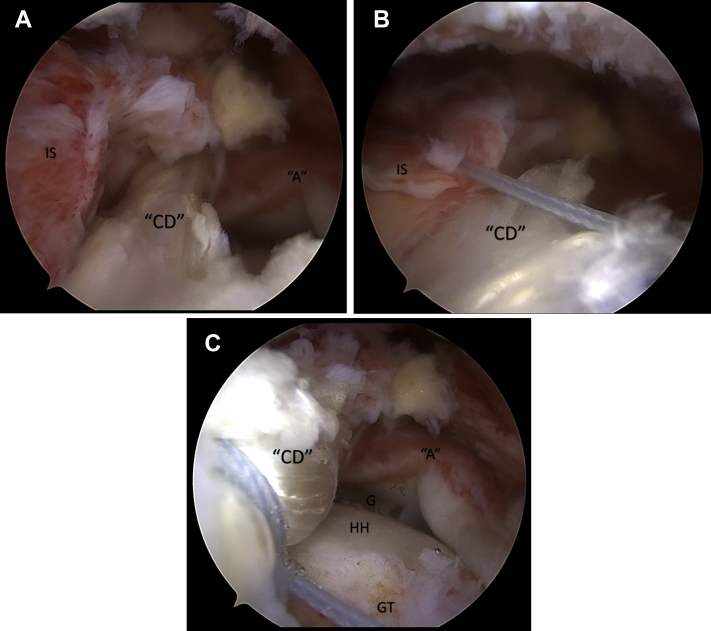
Fig 3.
Subacromial view from lateral arthroscopic portal (right shoulder, with patient in lateral decubitus position). (A) Massive posterosuperior rotator cuff tear retracted at glenoid level with tendon delamination. (B, C) We perform in all cases anterior slide release. In cases of massive retracted rotator cuff tears, the supraspinatus is often immobile and no excursion is obtained even after slide and articular side release. In these cases, a modified anterior release of the anterior supraspinatus that is too far retracted and immobile may be performed. The slide is performed more posteriorly than originally described,23 approximately at the level of the biceps anchor and over it proceeding from laterally to medially, 1 to 2 cm medially from the superior glenoid rim. The purpose is to release and mobilize the posterior leaf that consists of the infraspinatus and part of posterior supraspinatus. Anteriorly to our slide, the anterior part of supraspinatus is useless as no mobility and excursion are obtained in such massive retracted chronic tears. (D) Articular and bursal side release of the rotator cuff is always performed to mobilize the cuff tendons, evaluate the excursion, and have an estimation for the tension on the site of the repair. The infraspinatus is pulled in the direction indicated (black arrow) with use of a pulling suture, in order to facilitate the articular side release. (d, deep layer of infraspinatus; G, glenoid; HH, humeral head; IS, infraspinatus and posterior portion of supraspinatus; SS, anterior portion of supraspinatus; sup, superior layer of infraspinatus).
Preparation of Greater Tuberosity and Release of LHBT in the Bicipital Groove
For our double bundle SCR procedure, the LHBT autograft is fixed in 2 sites at superior glenoid (1 of these, the anterior one, is the native LHBT anchor) and in 2 or 3 sites at the greater tuberosity (GT) (usually 1), thus creating a box configuration (for descriptive purposes, we name the 4 corners of the box as ABCD, each corner representing a fixation point, where A stands for the native biceps anchor and moves in a clockwise manner; Fig 4). First, we debride the soft tissue from GT to prepare and refresh the bone bed for the biceps graft SCR and the part of the infraspinatus that we aim to repair. In cases of osteophytes or hard bone, we use with caution the burr to avoid any anchors subsidence. We also debride any soft tissue around the LHBT and any remaining tissue from the biceps pulley, which is sometimes already torn. Attention is needed to avoid damaging the LHBT with the electrocautery device or the shaver (Fig 5, Video 1).
Fig 4.
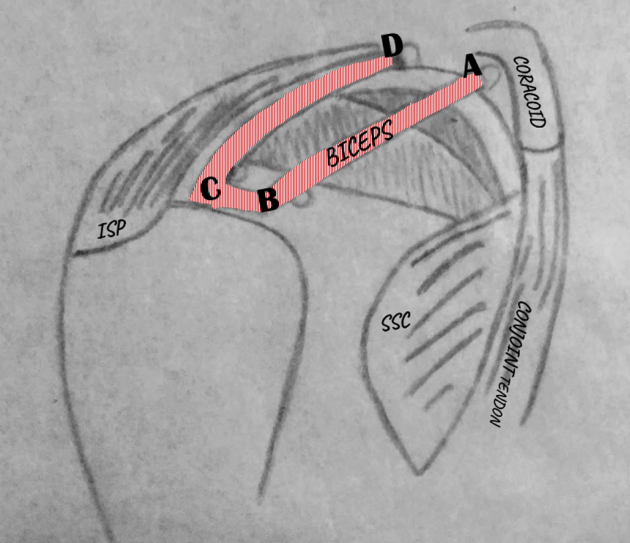
For the double-bundle superior capsular reconstruction (SCR) procedure, the long head biceps tendon (LHBT) autograft is fixed in 2 sites at superior glenoid (A and D) and 2 sites at the greater tuberosity (B and C), thus creating a box configuration shown in this schematic draw. For a universal description and better communication when we describe these points of fixation, the final construct is described as “ABCD,” each letter representing each of the 4 corners of the box construct. The letter A represents the native attachment of LHBT at anterior glenoid (or the glenoid fixation in case of SLAP II), and the nomenclature ABCD proceeds in a clockwise manner, so that B stands for the anterior fixation point at greater tuberosity, C represents the posterior fixation point at greater tuberosity, and D the posterior fixation point at glenoid. The sequence of fixation according to our technique is DBC in case of intact LHBT anchor, or ADBC in cases of SLAP II that the native point A should be repaired with a knotless anchor. (ISP, infraspinatus tendon; SSC, subscapularis tendon).
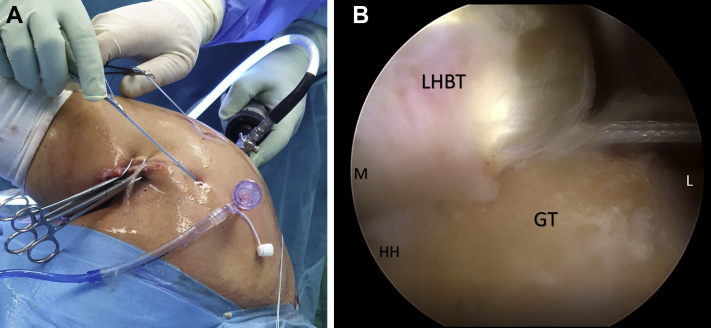
Fig 5.
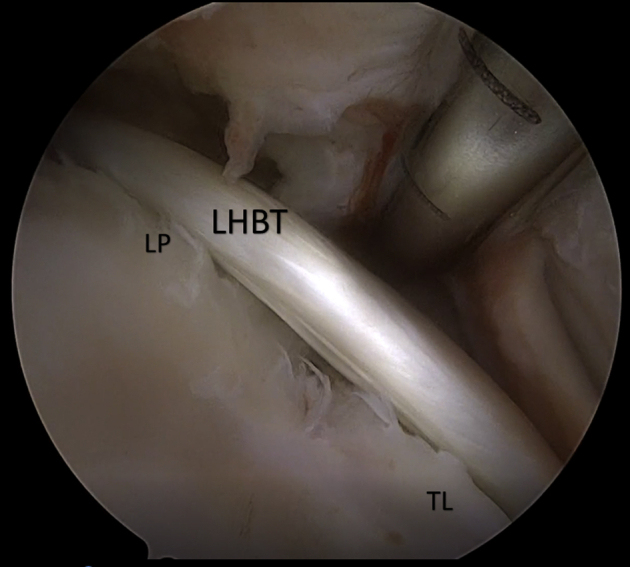
While viewing from the lateral portal (right shoulder, lateral decubitus position), we work through the anterior portal to debride any soft tissue around the long head biceps tendon (LHBT) in the bicipital groove and any remaining tissue from the biceps pulley, which is usually already torn. Through this anterior portal, we debride the bicipital groove tissue as distally as possible and remove the transverse ligament. The mobility and integrity of this distal part of the LHBT can be tested. (LP, remnants of lateral pulley; TL, remnants of the transverse ligament).
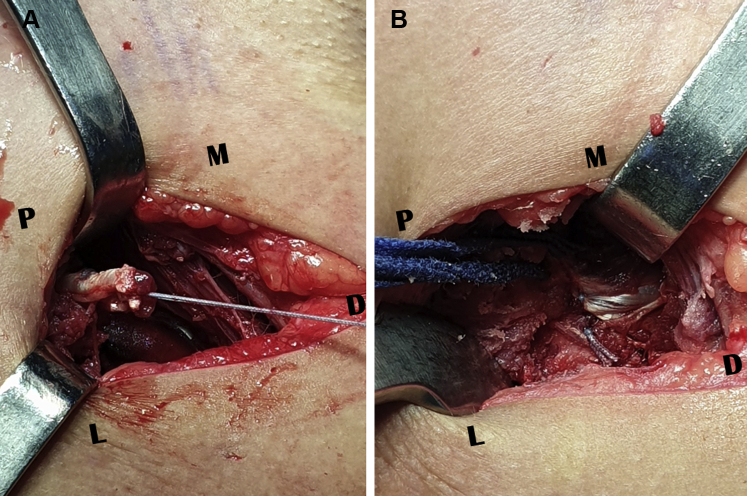
Graft Harvesting and Subpectoral Tenodesis
For graft harvesting and subpectoral tenodesis the patient is tilted 10° to the surgeon's side to facilitate the access to the anterior humerus. Subpectoral approach is performed through an incision 3 to 4 cm at the level of the inferior border of pectoralis major tendon at its insertion. The LHBT is recognized underneath the tendon and is tenotomized approximately 1 cm above the musculotendinous junction. The proximal part is secured using simple running ultrabraided suture and forms the distal portion of the LHBT graft that will be used for SCR, whereas its origin has been left intact. The musculotendinous part of the LHBT is fixed to the bone with suture-anchor or a tension slide technique with a button (Fig 6). A blunt open or semiopen stripper, from the anterior cruciate ligament instrumentation, can be used to release with gentle maneuvers any adhesions of the LHBT to the bicipital groove to the entrance to the joint. Cannulas are optionally inserted subacromially in the anterosuperior and lateral portals. We may create an additional posterolateral portal as viewing portal, and we insert an additional cannula in the standard posterior portal (Fig 1A). We advance the sutures of the LHBT with a grasper from the subpectoral incision to the joint and we retrieve the sutures and the LHBT from the anterosuperior portal (Video 1).
Fig 6.
(A) View through subpectoral approach. The long head biceps tendon (LHBT) has been tenotomized approximately 1 cm above the musculotendinous junction. The proximal part is secured with running suturing using FiberLoop suture (Arthrex). This part forms the distal portion of the LHBT graft that will be used for superior capsular reconstruction, whereas its origin has been left intact. (B) The musculotendinous part of the LHBT is fixed to the bone with a button using again FiberLoop running suture (biceps button 12 × 3 mm, Arthrex).
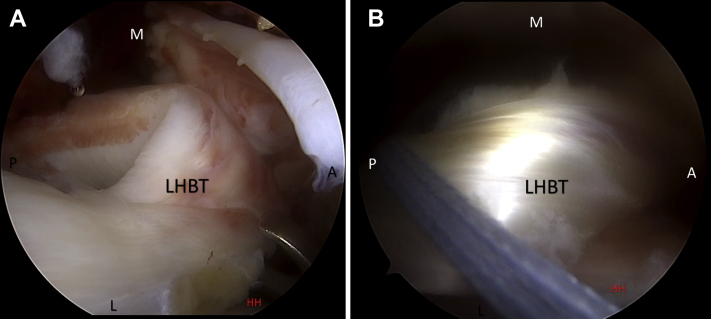
Glenoid Preparation and Graft Fixation (at Glenoid Side)
With the scope to the lateral portal, we prepare the superior glenoid rim by debriding part of the superior labrum and soft tissue 1 to 3 mm medial to labrum with the electrocautery and the shaver at the point that the anchor will be inserted, usually at the 10 to 11 o'clock positions (point D). We retrieve the LHBT sutures to the posterior portal. We pass a free suture through the anterosuperior portal around the LHBT to keep the tension and facilitate the glenoid fixation (Fig 7). The optimal direction for the hole preparation and anchor placement can be found via the standard posterior portal, a posterolateral or the Neviaser portal (Fig 8). The hole for the anchor is created 2 to 3 mm medial to the superior glenoid rim in 30° to 45° angulation to the glenoid surface. We retrieve the LHBT sutures to the appropriate portal, load the sutures of the LHBT to a knotless push-in anchor (PushLock, BioComposite, 2.9 mm × 12.5 mm; Arthrex), and we insert the anchor. This is point D of the box configuration.
Fig 7.
(A) View from the lateral portal of the right shoulder with patient in lateral decubitus position. The long head biceps tendon (LHBT) graft has been brought intraarticularly. The suture retriever through the anterosuperior portal may facilitate the handling of the LHBT. The LHBT sutures of the distal end of the graft have been retrieved to the posterior portal to further facilitate its handling. (B) We pass a free suture through the anterosuperior portal around the LHBT and then retrieve it through the anterior portal as shown in the figure. This suture helps to keep the tension and the shape of the LHBT graft and facilitate its manipulation and handling during glenoid fixation. (A, anteriorly; HH, humeral head; L, laterally; M, medially; P, posteriorly).
Fig 8.
(A) After the preparation for the exact point of fixation to the glenoid, we try to find the proper direction (black arrow) to prepare the hole for the anchor through the Neviaser portal. The point that the anchor will be inserted is around 10.30 o'clock position and is the point D of the box configuration ABCD construct (view from the lateral portal, right shoulder, with patient in lateral decubitus position). (B) Outside view. The scope is in the lateral portal (L) and the long head biceps tendon (LHBT) sutures have been retrieved to the posterior portal (P). A cannula has been placed at the anterosuperior portal (AS). The free suture around the LHBT (was entered through anterosuperior portal) has been retrieved to the anterior portal (A). Preparation of the best direction for the point D (glenoid fixation) is performed through the Neviaser portal (N).
Graft Fixation at Greater Tuberosity
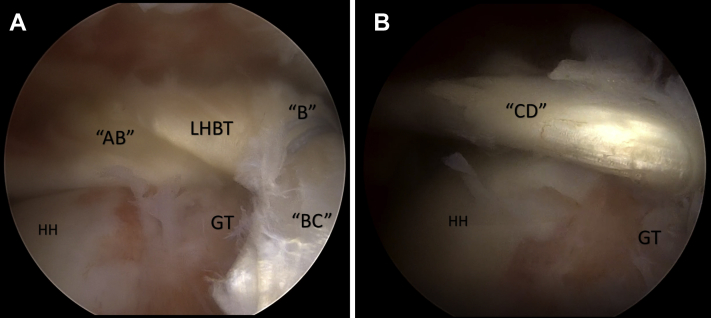
Then we move the scope to the standard posterior portal. We load a second free suture as a loop to the free central looped part of LHBT from the lateral portal to manipulate the looped graft and check the 2 points of fixation to the GT (points B and C) (Fig 9). The points of fixation at the GT will be placed laterally to the articular cartilage margin in an anteroposterior configuration between each other (B anteriorly, C posteriorly) (Fig 9). The exact points of fixation mediolaterally may change a few mm in each case and are determined by (1) the best tension of the graft, (2) the length of the graft available, and (3) the native capsule insertion. Based on previous anatomical study regarding the attachments of the native superior capsule, the maximum mediolateral distance from the cartilage margin that the fixation points should be placed at GT are approximately 9 mm for the posterior point C and 5 mm for the anterior point B.24 Our aim is to tense the biceps and fix it at the GT with 2 knotless anchors (with the arm in 30° abduction) creating the final box configuration with no laxity or any mobile part of the tendon on the bone to have the maximum contact between tendon and bone (represented by the “BC” part of the graft).
Fig 9.
(A) Anterior outside view of right shoulder with patient in lateral decubitus position. The scope is at the posterior portal. A cannula has been inserted in the anterosuperior portal. Two free pulling sutures have been loaded as loops to the free central looped part of the LHBT graft from the anterior and lateral portal to manipulate the looped graft and check the 2 points of fixation to the greater tuberosity (points B and C, respectively). (B) Arthroscopic view with scope in posterior portal showing the 1 of the 2 lateral pulling sutures (the posterior one) that has been loaded as a loop around the LHBT graft to adjust the tension of point (C) (GT, greater tuberosity; HH, humeral head; L, laterally; LHBT, long head of the biceps tendon graft; M, medially.)
First, we fix the biceps with a knotless anchor (BioComposite SwiveLock, 4.75 mm × 19.1 mm; Arthrex) on the anterior part of the GT (point B) giving tension of the biceps between its native origin (point A) and the fixation point B. At the same time, we keep tension of the posterolateral corner of the construct (the later point C) with the free suture that has been passed as a loop around the LHBT graft to estimate the best tension and best position for both points B and C (Fig 10, Video 1).
Fig 10.
(A) Arthroscopic view with scope in posterior portal (right shoulder, lateral decubitus position). The long head biceps tendon (LHBT) graft has been fixed with a knotless anchor (BioComposite SwiveLock, 4.75 mm × 19.1 mm; Arthrex) on the anterior part of the greater tuberosity (point B) giving tension of the biceps between its native origin and the fixation point B (part AB). At the same time, we keep tension of the posterolateral corner of the construct (the later point C) with the free suture that has been passed as a loop around the LHBT graft to estimate the best tension and best fixation position. (B) After the fixation of the graft at point B (anterior point of fixation at the greater tuberosity), we proceed in the same way to the fixation more posteriorly on the greater tuberosity at point (C) In this arthroscopic view from the posterior portal (right shoulder, lateral decubitus position), we show the part CD of the graft, which is tensioned by use of a free looped suture to find the appropriate point of fixation that lies laterally to the cartilage-greater tuberosity margin. (GT, greater tuberosity; HH, humeral head.).
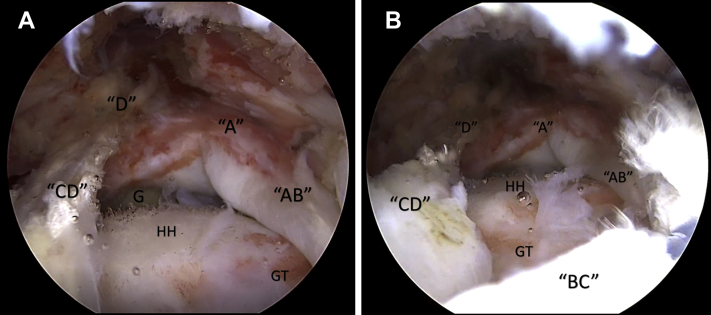
After placement of the point B, we proceed in the same way to the fixation more posteriorly on the GT at point C. This time, the free looped suture is used to give tension between the anterior and posterior points at GT (B and C) if needed and may show if a third anchor is needed to have a well-tensioned but not too lateralized graft (Figs 10 and 11; Video 1).
Fig 11.
(A) Arthroscopic view from the lateral portal of the right shoulder with patient in lateral decubitus position showing the final box configuration. The 2 bundles of the superior capsular reconstruction (SCR) construct (AB and CD) connecting the superior glenoid (G) and the greater tuberosity (GT) were tight in examination with the probe and resisted superior migration of humeral head (HH) (Video 1). A, long head of the biceps tendon (LHBT) anchor; D, posterior point of fixation at glenoid. (B) Same view. The part BC represents the broad attachment of native superior capsule on the GT in anteroposterior dimension and provides a site for healing between the LHBT graft and the GT that may further enhance the resistance of the double bundle construct against superior HH migration. For this reason, we always refresh the bone bed of superior GT (with shaver or burr) to promote healing of LHBT graft on it.
Partial Rotator Cuff Repair
With the scope on the lateral portal (or posterolateral), we estimate the position of fixation of the infraspinatus depending on its excursion, mobility, and tension. In case of a delamination, we fix the deep layer in a separate way if it is reparable. We fix the superficial layer with a second anchor free of tension on the GT. If the infraspinatus needs medialization (close to the articular cartilage margin) to have a less tensioned repair; this is not a contraindication for us. Finally, we suture the anterior part of the infraspinatus with the posterior bundle of the LHBT construct (DC) to reinforce our construction (Fig 12, Video 1).
Fig 12.
(A-C) Once the infraspinatus tendon has been repaired, we suture the anterior part of the infraspinatus with the posterior bundle (DC) of the long head biceps tendon (LHBT) box construct to reinforce our construction (view from the lateral portal of the right shoulder with patient in lateral decubitus position). The posterior bundle (DC) of the LHBT is narrower than the anterior bundle (AB) (because distally, the LHBT has smaller diameter than proximally). For this reason, we avoid piercing the part DC and we prefer passing around it when we suture the infraspinatus with the posterior bundle (DC) of the LHBT graft. (A, LHBT anchor; CD, the posterior bundle of superior capsular reconstruction box construct; G, glenoid surface; GT, greater tuberosity; HH, humeral head; IS, infraspinatus tendon.).
We do not perform acromioplasty, but in cases of extreme spur, we excise it and perform the Mumford procedure in cases of symptomatic acromioclavicular joint arthrosis.
The same postoperative rehabilitation protocol as for our large and massive rotator cuff repairs is performed. Immobilization in a 10° abduction pillow with almost neutral rotation for 5 weeks is followed by another 7 weeks of passive and gradually assisted activated exercises. At 3 months postoperatively, active, overhead forward elevation is allowed and at 4 months strengthening of the rotator cuff is initiated.
Discussion
Recent literature, biomechanical research, and clinical evidence on massive and irreparable RCT have clearly shown the vital function and role of the superior capsule on glenohumeral biomechanics.1, 2, 3, 4,24, 25, 26, 27 We present the surgical technique for SCR using the double-bundle LHBT autograft in a box configuration that is a modification and evolution of a V-shaped technique proposed in a previous biomechanical study.18 The best candidate for this procedure is a patient with massive RCT, which results in pain, dysfunction, and limited active range of motion, intact or reparable subscapularis, no glenohumeral arthritis, rotator cuff arthropathy up to stage Hamada 2, intact LHBT anchor (i.e. no complex SLAP lesions), and intact intraarticular LHBT or fraying that does not exceed 30% of its substance (Table 1). The SCR is worthwhile, especially in cases where a partial repair is feasible, and this is the reason that we always aim to combine the SCR with partial RC repair.
Regarding its humeral insertion, the superior capsule of the glenohumeral joint attaches at 30% to 61% of the GT.24 In the mediolateral dimension, it attaches laterally to the articular cartilage margin and the width of attachment varies ranging from 4 to 5 mm at the anterior parts of supraspinatus and infraspinatus, whereas it is thickest at the posterior part of infraspinatus that is approximately 9 mm.24 These data show that the attachment of superior capsule at the GT has a broader and thicker footprint than previously considered at the humeral side.24 The broad insertion on GT (regarding its mediolateral dimension or width) was imitated in our technique with the thick tendon-bone interface between our LHBT graft and GT (width of part BC). Also, the large anteroposterior insertion of the native superior capsule that extends through the anteroposterior dimension of the greater tuberosity24 is better reproduced in our technique (length of BC part). This feature of the native superior capsule cannot be imitated by the previously described single bundle or V-shaped LHBT techniques.14, 15, 16, 17, 18 The fixation of the SCR graft at the humeral side was in 30° abduction which is the optimal position for graft fixation and tension.4,17
The use of LHBT autograft seems the ideal solution among available graft sources for SCR.9 The eliminated cost compared with dermal or fascia lata allografts, the lack of donor side morbidity compared with fascial lata autograft and the shorter operation time compared with the techniques that require preparation of the dermal allograft or graft harvest from lower limb are important factors that should be considered. The subpectoral tenodesis that we perform allows us to avoid complications of tenotomy such as deformity from retraction (Popeye sign), pain during resisted flexion or supination, as well as loss of supination strength. The subpectoral tenodesis provides a mean tendon length 98.5 mm (range, 80-126 mm) that is sufficient for our double bundle technique.28 Regarding the fixation of LHBT on glenoid side we rely on previous biomechanical data for double anchorage.18 The optimal point for the second more posterior anchor at humeral side and any interplay between humeral points of fixation with different positioning of the posterior anchor at glenoid side (a wider box configuration with glenoid insertion at 9-10 o'clock positions or a narrower box configuration at 10-11 o'clock positions) remain to be determined in relevant biomechanical study. Another advantage of using the LHBT autograft is its diameter that ranges from 5.1 to 6.6 throughout its course.28 This diameter resembles the ideal graft thickness of 6 to 8 mm for SCR but does not exceed too much the native capsule thickness that ranges from 1.3 to 4.5 mm.4,11 Also, this diameter of the graft allows over-the-SCR coverage with RC according to surgeon's preference in cases that the RC can be sufficiently repaired. Last, this diameter is achieved without the need to fold the graft several times to obtain this optimal thickness as in the case of a fascia lata autograft, where this folding creates “dead” space and possible sites for articular fluid entrapment with the potential of infection. Another advantage over other autograft or allograft sources is the preservation of the vascularity of the LHBT graft while keeping its origin at superior labrum. This allows for undisrupted vascularization of the graft that may allow for optimum graft incorporation and healing on the bony surface. Comparison of our double-bundle technique to previously reported single-bundle SCR techniques with LHBT is outlined in Table 2.
Table 2.
Advantages and Disadvantages of SCR Using LHBT Autograft: A Comparison Between Single- and Double-Bundle Techniques
| Single-Bundle LHBT |
Double-Bundle LHBT |
||
|---|---|---|---|
| Advantages | Disadvantages | Advantages | Disadvantages |
| Simple technique | Relatively simple technique Simple for arthroscopists who already perform SCR with other grafts |
||
| Partial superior capsule reconstruction Small coverage of the GT One point of fixation at glenoid and one at GT One bundle of LHBT tissue to resist superior humeral migration |
Subtotal superior capsule reconstruction Greater coverage of the GT; imitates better the broad superior capsule attachment in AP dimension (part BC); offers increased healing surface between the LHBT graft and GT Two points of fixation at glenoid, two or three points at the GT Two bundles of LHBT tissue (AB and CD) to resist superior humeral migration |
||
| Usually the anterior part of infraspinatus cannot be sutured to the single bundle of LHBT | The posterior bundle of the LHBT (CD) may be sutured with the anterior part of infraspinatus to create a more solid construct | ||
| No additional approach for graft harvesting | Subpectoral approach: Already well-known approach Small incision No cosmesis problem |
Additional subpectoral approach (open) | |
| Cost effective | More anchors or buttons or interference screw | ||
| No longer rehabilitation than other techniques | |||
AB, the anterior bundle of the “box” construct extending from the native LHBT anchor (point A) to the anterior point of fixation at GT (point B); BC, extends between the anterior and posterior point of fixation at GT (points B and C respectively) and represents the broad attachment of native superior capsule on the GT in anteroposterior dimension; CD, the posterior bundle of the double bundle box construct extending from the posterior point of fixation at GT (point C) to the posterior point of fixation to the glenoid (point D); GT, greater tuberosity; LHBT, long head biceps tendon; SCR, superior capsular reconstruction.
Regarding possible risks of the procedure, superficial and deep wound infection, hematomas, peripheral nerve injuries, humeral shaft fractures, biceps rupture, and failure of the tenodesis are possible related to subpectoral tenodesis. It should be warranted to stay laterally to LHBT to avoid neurovascular structures medially and drill vertically to the humeral shaft to avoid fractures. Regarding the glenoid fixation of the LHBT graft, the surgeon should use the Neviaser portal and aim to find the appropriate orientation to avoid fracture of the glenoid rim. Finally, another risk of the procedure is possible pullout of the anchor from soft osteoporotic bone at greater tuberosity. Skepticism regarding the use of LHBT autograft for SCR has been related to the use of a potentially diseased or inflamed tissue and to the preservation of neural elements at the origin that may be a source of continuous postoperative pain.29 However, degenerative and inflammatory changes of LHBT on histologic examination are not the same throughout the course of the tendon.30 The sites with the most intense histologic findings are the origin of the LHBT at the glenoid labrum and the part near its distal exit from the bicipital groove, whereas such degenerative changes were rarely seen in the other parts of the tendon including the intraarticular part.30,31 These degenerative and inflammatory changes have been related to mechanical stress, which derives from the eccentric contraction of the biceps tendon for the origin and from the narrow distal bicipital groove for the most distal part.30 Both of these disadvantageous mechanical conditions are eliminated after biceps subpectoral tenodesis because the eccentric biceps contraction and the narrow distal bicipital groove are no longer mechanical reasons predisposing to further degenerative and inflammatory reaction to the proximal part of the LHBT that is used for the SCR in our technique. Furthermore, a recent study showed that the regenerative potential of biceps tendon is preserved even for the inflamed tendon, which may be valuable for the incorporation and healing at tendon–bone interface at both glenoid and humeral sites.32
In summary, our technique for the SCR with the double-bundle long head of biceps tendon is described. LHBT has advantages of an autograft with the preservation of its origin and the box technique may imitate the superior capsule more anatomically than the single-bundle techniques. This technique is always combined with partial repair of posterosuperior rotator cuff rupture in patients with massive tears and no or minimal arthrosis. Finally, biomechanical studies will better clarify the exact position of the fixation points of the LHBT (BCD points) and clinical studies are necessary to analyze the benefits and possible pitfalls of our technique.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
We present our novel arthroscopic assisted technique of superior capsular reconstruction with double bundle long head of the biceps autograft on a “box” configuration. Our patient suffers of a massive posterosuperior cuff tear of the right shoulder. By glenohumeral arthroscopy, we inspect the integrity and the degeneration of the long head of biceps (LHB). We continue with the subacromial arthroscopy. We debride the subdeltoid and subacromial bursa with the scope on lateral portal and working on the standard posterior and anterosuperior portal. We evaluate the mobility of the cuff pulling its posterior and anterior part. We look for delamination of the posterior cuff. We always perform in similar tears release of the interval, release of the intraarticular part of the cuff and bursal adhesions in order to free the posterior cuff. We reevaluate the tear and the point that we can fix the cuff on the greater tuberosity with no tension and feasibility of repairing both layers of the posterior cuff. We debride the soft tissue around the biceps toward the direction of the bicipital groove. Traction suture may be used on the infraspinatus to assist the further release. We try to have a free with no tension posterior cuff. With the scope in lateral portal, we create the anterior portal at the level of the bicipital groove. We debride cautiously the LHB until the transverse ligament to free the biceps, especially from the posterior soft tissues. With the open subpectoral approach, we free and suture the distal end of the tendinous part of LHB and we fix the musculotendinous part of LHB with a button technique. With the scope on lateral portal, we retrieve the tendon on the subacromial space from the posterior portal and we assist pushing the tendon with a grasper from the open subpectoral approach towards the anterior subacromial space. With the scope on lateral portal we pass a strong ultra-braided suture around the LHB via the anterior portal. This suture helps to control the tension of LHB. One suture now is on its free edge at the posterior portal and 1 suture is on the anterior portal. We prepare the superior glenoid surface 2 mm medial to the labrum. We use a needle to find the best direction to the glenoid surface through the Neviaser portal. We prepare the hole through the guide, we retrieve the sutures of the free tendon to Neviaser portal, and we load the knotless anchor. This is the D point of fixation at the glenoid. We move the scope to standard posterior portal and through the lateral portal we prepare the greater tuberosity with the burr, freshing the bone with no aggressive debridement. We load a second traction suture around the LHB from the lateral portal. We pull the 2 free sutures around the LHB to control the tension. We check with the needle the direction of the fixation point at the greater tuberosity anteriorly. We retrieve the anterior free suture around the LHB, we prepare the hole, and insert the knotless anchor. This is the first fixation of the LHB at the greater tuberosity and we name it point B. In a similar way, we check the direction of the second anchor at the posterior part of greater tuberosity. We load the second free suture and we insert the knotless anchor. This is the second fixation point at the greater tuberosity, the point C. We check the stability of the whole construction. We check also the stability of the construction with the scope in the lateral portal and the probe through the anterior or anterosuperior portal. With the scope in the lateral portal, we retrieve the traction suture of infraspinatus and we fix it with a double-loaded metallic anchor with no tension. We may suture the anterior part of the infraspinatus with the posterior bundle of LHB to reinforce the whole construction. It is better to go around the LHB to avoid any damage on the biceps tendon. With the scope on the lateral portal, this is the final view of our patient with massive cuff tear that we performed partial repair of infraspinatus combined with the double bundle of LHB as the superior capsule.
References
- 1.Ishihara Y., Mihata T., Tamboli M. Role of the superior shoulder capsule in passive stability of the glenohumeral joint. J Shoulder Elbow Surg. 2014;23:642–648. doi: 10.1016/j.jse.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 2.Mihata T., McGarry M.H., Pirolo J.M., Kinoshita M., Lee T.Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med. 2012;40:2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 3.de Campos Azevedo C.I., Andrade R., Leiria Pires Gago Ângelo A.C., Espregueira-Mendes J., Ferreira N., Sevivas N. Fascia lata autograft versus human dermal allograft in arthroscopic superior capsular reconstruction for irreparable rotator cuff tears: A systematic review of clinical outcomes. Arthroscopy. 2020;36:579–591.e2. doi: 10.1016/j.arthro.2019.08.033. [DOI] [PubMed] [Google Scholar]
- 4.Mihata T., McGarry M.H., Kahn T., Goldberg I., Neo M., Lee T.Q. Biomechanical effect of thickness and tension of fascia lata graft on glenohumeral stability for superior capsule reconstruction in irreparable supraspinatus tears. Arthroscopy. 2016;32:418–426. doi: 10.1016/j.arthro.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 5.Makki D., Tang Q.O., Sandher D., Morgan B.W., Ravenscroft M. Arthroscopic superior capsular reconstruction of the shoulder using dermal allograft. Orthopedics. 2020;5:1–6. doi: 10.3928/01477447-20200428-05. [DOI] [PubMed] [Google Scholar]
- 6.Lubowitz J.H., Brand J.C., Rossi M.J. Shoulder superior capsular reconstruction using acellular human dermal allograft. Arthroscopy. 2019;35:2769–2770. doi: 10.1016/j.arthro.2019.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Mease S.J., Moontasri N.J., Kurowicki J., Long C.L., Simone E.S., Scillia A.J. Superior capsular reconstruction with Achilles tendon allograft. Arthrosc Tech. 2020;9:e527–e533. doi: 10.1016/j.eats.2019.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim J.W., Nam D.J. Arthroscopic superior capsular reconstruction by the mini-open modified keyhole technique using an Achilles tendon-bone allograft. Arthrosc Tech. 2020;9:e275–e281. doi: 10.1016/j.eats.2019.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kocaoglu B., Firatli G., Ulku T.K. Partial rotator cuff repair with superior capsular reconstruction using the biceps tendon is as effective as superior capsular reconstruction using a tensor fasciae latae autograft in the treatment of irreparable massive rotator cuff tears. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120922526. 2325967120922526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Denard P.J., Lädermann A., Jiwani A.Z., Burkhart S.S. Functional outcome after arthroscopic repair of massive rotator cuff tears in individuals with pseudoparalysis. Arthroscopy. 2012;28:1214–1219. doi: 10.1016/j.arthro.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 11.Burkhart S.S., Hartzler R.U. Superior capsular reconstruction reverses profound pseudoparalysis in patients with irreparable rotator cuff tears and minimal or no glenohumeral arthritis. Arthroscopy. 2019;35:22–28. doi: 10.1016/j.arthro.2018.07.023. [DOI] [PubMed] [Google Scholar]
- 12.Mihata T., Lee T.Q., Hasegawa A. Arthroscopic superior capsule reconstruction can eliminate pseudoparalysis in patients with irreparable rotator cuff tears. Am J Sports Med. 2018;46:2707–2716. doi: 10.1177/0363546518786489. [DOI] [PubMed] [Google Scholar]
- 13.Burkhart S.S., Pranckun J.J., Hartzler R.U. Superior capsular reconstruction for the operatively irreparable rotator cuff tear: Clinical outcomes are maintained 2 years after surgery. Arthroscopy. 2020;36:373–380. doi: 10.1016/j.arthro.2019.08.035. [DOI] [PubMed] [Google Scholar]
- 14.Kim Y.S., Lee H.J., Park I., Sung G.Y., Kim D.J., Kim J.H. Arthroscopic in situ superior capsular reconstruction using the long head of the biceps tendon. Arthrosc Tech. 2018;7:e97–e103. doi: 10.1016/j.eats.2017.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barth J., Olmos M.I., Swan J., Barthelemy R., Delsol P., Boutsiadis A. Superior capsular reconstruction with the long head of the biceps autograft prevents infraspinatus retear in massive posterosuperior retracted rotator cuff tears. Am J Sports Med. 2020;48:1430–1438. doi: 10.1177/0363546520912220. [DOI] [PubMed] [Google Scholar]
- 16.Adrian S.C., Field L.D. Biceps transposition for biological superior capsular reconstruction. Arthrosc Tech. 2020;9:e841–e846. doi: 10.1016/j.eats.2020.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Han F., Kong C.H., Hasan M.Y., Ramruttun A.K., Kumar V.P. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: A biomechanical study on cadavers. Orthop Traumatol Surg Res. 2019;105:257–263. doi: 10.1016/j.otsr.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 18.El-Shaar R., Soin S., Nicandri G., Maloney M., Voloshin I. Superior capsular reconstruction with a long head of the biceps tendon autograft: A cadaveric study. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118785365. 2325967118785365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lafosse L., LanzU, Saintmard B., Campens C. Arthroscopic repair of subscapularis tear: Surgical technique and results. Orthop Traumatol Surg Res. 2010;96:S99–S108. doi: 10.1016/j.otsr.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Cofield R.H. Subscapular muscle transposition for repair of chronic rotator cuff tears. Surg Gynecol Obstet. 1982;154:667–672. [PubMed] [Google Scholar]
- 21.Gerber C., Fuchs B., Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Snyder S.J., Karzel R.P., Del Pizzo W., Ferkel R.D., Friedman M.J. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274–279. doi: 10.1016/0749-8063(90)90056-j. [DOI] [PubMed] [Google Scholar]
- 23.Lo I.K.Y., Burkhart S.S. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: Technique and preliminary results. Arthroscopy. 2004;20:22–33. doi: 10.1016/j.arthro.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 24.Nimura A., Kato A., Yamaguchi K. The superior capsule of the shoulder joint complements the insertion of the rotator cuff. J Shoulder Elbow Surg. 2012;21:867–872. doi: 10.1016/j.jse.2011.04.034. [DOI] [PubMed] [Google Scholar]
- 25.Adams C.R., DeMartino A.M., Rego G., Denard P.J., Burkhart S.S. The rotator cuff and the superior capsule: Why we need both. Arthroscopy. 2016;32:2628–2637. doi: 10.1016/j.arthro.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 26.Makovicka J.L., Chung A.S., Patel K.A., Deckey D.G., Hassebrock J.D., Tokish J.M. Superior capsule reconstruction for irreparable rotator cuff tears: A systematic review of biomechanical and clinical outcomes by graft type. J Shoulder Elbow Surg. 2020;29:392–401. doi: 10.1016/j.jse.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 27.Sochacki K.R., McCulloch P.C., Lintner D.M., Harris J.D. Superior capsular reconstruction for massive rotator cuff tear leads to significant improvement in range of motion and clinical outcomes: A systematic review. Arthroscopy. 2019;35:1269–1277. doi: 10.1016/j.arthro.2018.10.129. [DOI] [PubMed] [Google Scholar]
- 28.Denard P.J., Dai X., Hanypsiak B.T., Burkhart S.S. Anatomy of the biceps tendon: Implications for restoring physiological length-tension relation during biceps tenodesis with interference screw fixation. Arthroscopy. 2012;28:1352–1358. doi: 10.1016/j.arthro.2012.04.143. [DOI] [PubMed] [Google Scholar]
- 29.Pauzenberger L., Hurley E.T. Editorial commentary: Finally, something positive about the long head of the biceps tendon?! Soulder superior capsular reconstruction. Arthroscopy. 2018;34:2601–2603. doi: 10.1016/j.arthro.2018.06.039. [DOI] [PubMed] [Google Scholar]
- 30.Refior H.J., Sowa D. Long tendon of the biceps brachii: Sites of predilection for degenerative lesions. J Shoulder Elbow Surg. 1995;4:436–440. doi: 10.1016/s1058-2746(05)80035-7. [DOI] [PubMed] [Google Scholar]
- 31.Murthi A.M., Vosburgh C.L., Neviaser T.J. The incidence of pathologic changes of the long head of the biceps tendon. J Shoulder Elbow Surg. 2000;9:382–385. doi: 10.1067/mse.2000.108386. [DOI] [PubMed] [Google Scholar]
- 32.Schmalzl J., Plumhoff P., Gilbert F. Tendon-derived stem cells from the long head of the biceps tendon: Inflammation does not affect the regenerative potential. Bone Joint Res. 2019;8:414–424. doi: 10.1302/2046-3758.89.BJR-2018-0214.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
We present our novel arthroscopic assisted technique of superior capsular reconstruction with double bundle long head of the biceps autograft on a “box” configuration. Our patient suffers of a massive posterosuperior cuff tear of the right shoulder. By glenohumeral arthroscopy, we inspect the integrity and the degeneration of the long head of biceps (LHB). We continue with the subacromial arthroscopy. We debride the subdeltoid and subacromial bursa with the scope on lateral portal and working on the standard posterior and anterosuperior portal. We evaluate the mobility of the cuff pulling its posterior and anterior part. We look for delamination of the posterior cuff. We always perform in similar tears release of the interval, release of the intraarticular part of the cuff and bursal adhesions in order to free the posterior cuff. We reevaluate the tear and the point that we can fix the cuff on the greater tuberosity with no tension and feasibility of repairing both layers of the posterior cuff. We debride the soft tissue around the biceps toward the direction of the bicipital groove. Traction suture may be used on the infraspinatus to assist the further release. We try to have a free with no tension posterior cuff. With the scope in lateral portal, we create the anterior portal at the level of the bicipital groove. We debride cautiously the LHB until the transverse ligament to free the biceps, especially from the posterior soft tissues. With the open subpectoral approach, we free and suture the distal end of the tendinous part of LHB and we fix the musculotendinous part of LHB with a button technique. With the scope on lateral portal, we retrieve the tendon on the subacromial space from the posterior portal and we assist pushing the tendon with a grasper from the open subpectoral approach towards the anterior subacromial space. With the scope on lateral portal we pass a strong ultra-braided suture around the LHB via the anterior portal. This suture helps to control the tension of LHB. One suture now is on its free edge at the posterior portal and 1 suture is on the anterior portal. We prepare the superior glenoid surface 2 mm medial to the labrum. We use a needle to find the best direction to the glenoid surface through the Neviaser portal. We prepare the hole through the guide, we retrieve the sutures of the free tendon to Neviaser portal, and we load the knotless anchor. This is the D point of fixation at the glenoid. We move the scope to standard posterior portal and through the lateral portal we prepare the greater tuberosity with the burr, freshing the bone with no aggressive debridement. We load a second traction suture around the LHB from the lateral portal. We pull the 2 free sutures around the LHB to control the tension. We check with the needle the direction of the fixation point at the greater tuberosity anteriorly. We retrieve the anterior free suture around the LHB, we prepare the hole, and insert the knotless anchor. This is the first fixation of the LHB at the greater tuberosity and we name it point B. In a similar way, we check the direction of the second anchor at the posterior part of greater tuberosity. We load the second free suture and we insert the knotless anchor. This is the second fixation point at the greater tuberosity, the point C. We check the stability of the whole construction. We check also the stability of the construction with the scope in the lateral portal and the probe through the anterior or anterosuperior portal. With the scope in the lateral portal, we retrieve the traction suture of infraspinatus and we fix it with a double-loaded metallic anchor with no tension. We may suture the anterior part of the infraspinatus with the posterior bundle of LHB to reinforce the whole construction. It is better to go around the LHB to avoid any damage on the biceps tendon. With the scope on the lateral portal, this is the final view of our patient with massive cuff tear that we performed partial repair of infraspinatus combined with the double bundle of LHB as the superior capsule.