Abstract
The awareness of anterior cruciate ligament (ACL) injuries and their treatment is increasing among athletes and within the general population, so patients report early to orthopaedic surgeons. Because we encounter a thick ACL stump during arthroscopic ACL reconstruction, an attempt is made to preserve this stump. Remnant preservation—although promising in terms of graft healing because it enhances cell proliferation, revascularization, and regeneration of the proprioceptive organs in the reconstructed ACL—does not come without complications, such as cyclops lesions, impingement, and extension loss. These problems can be detrimental to an athlete's return to his or her preinjury level after ACL reconstruction. Therefore, we describe a technique in which the ACL is reconstructed using hamstring autograft and suture passes are made through the remnant with an antegrade suture-passing device. After anatomic tunnel drilling, the remnant is tensioned, along with the reconstructed ACL, at the femoral end without the use of an extra implant. Femoral-side fixation is achieved with an adjustable-loop button (Procinch; Stryker) and a bio-composite interference screw (Biosure Regenesorb; Smith & Nephew) on the tibial end. As the sutured remnant is tensioned and knots are made over the button, the remnant envelopes the graft in the orientation of the native ACL, which can be helpful for early and better ligamentization of the graft. The potential advantages of this technique are as follows: orientation of the remnant along the collagen of the ACL graft; no loose ACL stump in the notch, thus preventing cyclops lesions; retention of the proprioceptive organs in the ligament; and no extra implant.
Arthroscopic anterior cruciate ligament reconstruction (ACLR) surgery has become an effective and popular treatment for anterior cruciate ligament (ACL)–deficient knees. Moreover, after surgery, 83% of elite athletes can return to their preinjury level.1 Owing to the awareness of ACL injury and its treatment is increasing among athletes and within the general population, patients report to orthopaedic surgeons early after injury. With an early presentation, we encounter a thick ACL stump bridging between the femur and tibia because most of the ruptures are from the proximal third.2 Preservation of the ACL stump during arthroscopic ACLR surgery is being practiced because it enhances cell proliferation, revascularization, and regeneration of the proprioceptive organs in the reconstructed ACL. In addition, it may improve graft healing after ACLR.3 Apart from being technically demanding, the main complications of remnant preservation are cyclops lesions, graft impingement, and extension loss.4, 5, 6 These complications arise from the stump lying loose in the notch, overstuffing of the notch, and faulty tunnel placement. Tensioning of the stump on the femoral side can help prevent these complications.7 So, we describe a technique in which the ACL is reconstructed using hamstring autograft and the sutured remnant is tensioned along with the reconstructed ACL without using an extra implant. Femoral-side fixation is achieved with an adjustable-loop button (Procinch; Stryker) and a bio-composite interference screw (Biosure Regenesorb; Smith & Nephew) on the tibial end (Video 1).
Surgical Technique
General Preparation
The patient is examined under anesthesia (regional or general) and is placed supine; a tourniquet is applied to the proximal thigh. A side support and 2 foot supports are applied to hold the knee in 90° of flexion and full flexion. The operative knee is painted and draped. Standard anteromedial (AM) and anterolateral (AL) portals are created. During diagnostic arthroscopy, the type of ACL tear is determined and decision is made to preserve the ACL stump (Figs 1 and 2). The AL portal is the viewing portal during most of the procedure, and the AM portal is the working portal. The meniscal and articular cartilage is evaluated, and meniscal repair or meniscectomy and cartilage treatment are performed. Ipsilateral hamstring autograft is harvested.
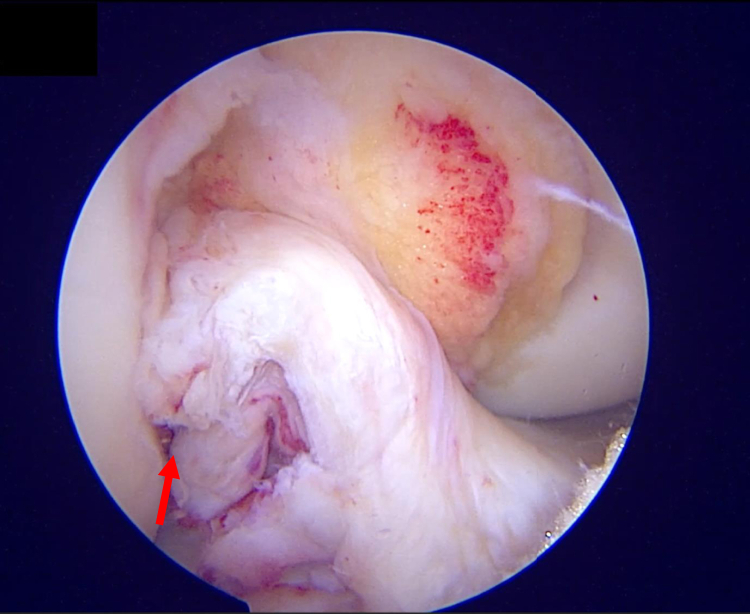
Fig 1.
Viewing from the anterolateral portal, a femoral-side (proximal) tear of the anterior cruciate ligament (red arrow) is shown in a right knee. The anterolateral portal is the viewing portal during most of the steps of the procedure, and the anteromedial portal is the working portal.
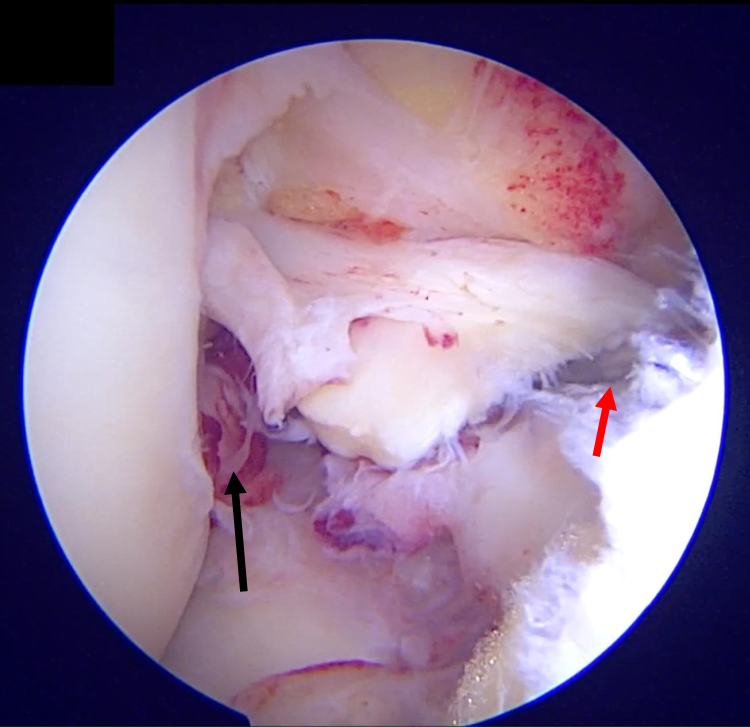
Fig 2.
View from anterolateral portal in a right knee. Assessment of the detached anterior cruciate ligament stump is performed with a probe (red arrow) coming in from the anteromedial portal; the anterior cruciate ligament is found to be completely torn from the femoral attachment (black arrow). This is a very important step because the type of tear is determined and the decision is made to proceed with remnant preservation.
Preparation of Tunnels and Remnant
By viewing from the AL portal, the anatomic femoral starting point of the tunnel is marked with an angled awl; the appropriate size of tunnel is then created (minimum of 8 mm in diameter up to a minimum depth of 20 mm to accommodate the graft) by independent tunnel drilling from the AM portal (Fig 3, Fig 4, Fig 5). During reaming of the femoral tunnel, the knee is held in full flexion. Bony notchplasty particularly of the medial wall of the lateral femoral condyle can be performed if graft impingement is anticipated (Fig 6). The next step involves passing suture into the remnant, which is performed after the passage of a flexible cannula (Passport; Arthrex) with an antegrade self-retrieving suture passer (Firstpass; Smith & Nephew). No. 2 ultrahigh-molecular-weight polyethylene suture material (Clinifibre; Sutures India) is used (Fig 7). An attempt is made to make crisscross suture passes in the ACL stump from distal to proximal. A minimum of 4 or 5 passes into the remnant are attempted (Fig 8). The sutures are then retrieved through the AM portal. With the knee in 90° of flexion and viewing from the AL portal, tibial tunnel drilling is performed with a guide (Acufex tip aimer; Smith & Nephew). The tunnel's exit is parallel to the posterior border of the anterior horn of the lateral meniscus and within the native ACL stump (Fig 9). It is very important to hand ream the inner cortex because it prevents damage to the stump and sutures. It is also better to clear both tunnels of soft-tissue and bone debris because this will aid in graft passage (Fig 10).
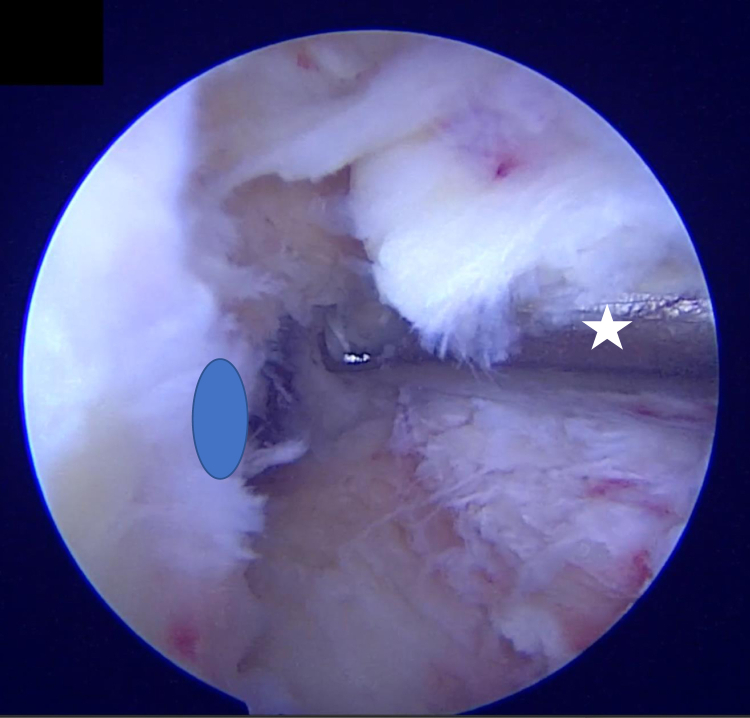
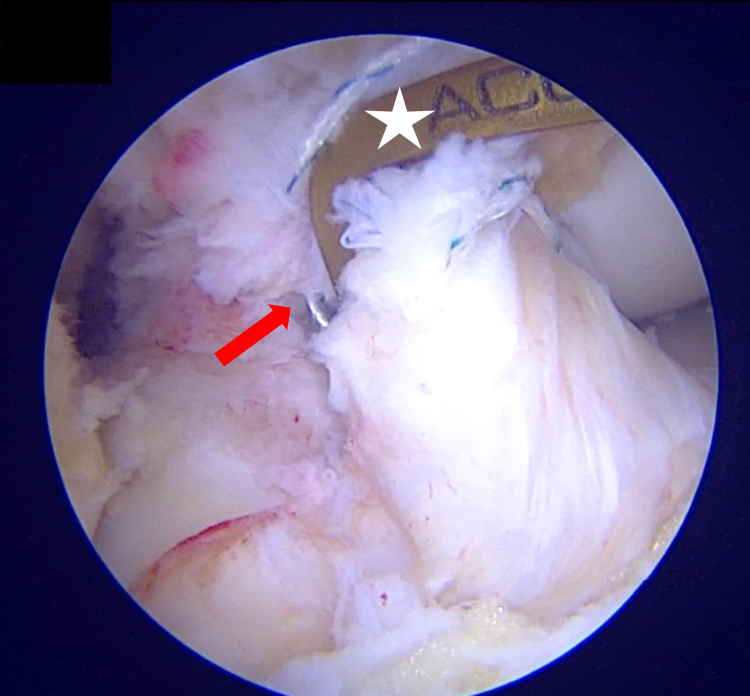
Fig 3.
Determining femoral footprint of anterior cruciate ligament (blue oval) after retraction of remnant fibers of anterior cruciate ligament. This is achieved by viewing from the anterolateral portal. Gentle shaving of the injured tissue can be performed with the hood of the shaver blade protecting the remnant (white star).
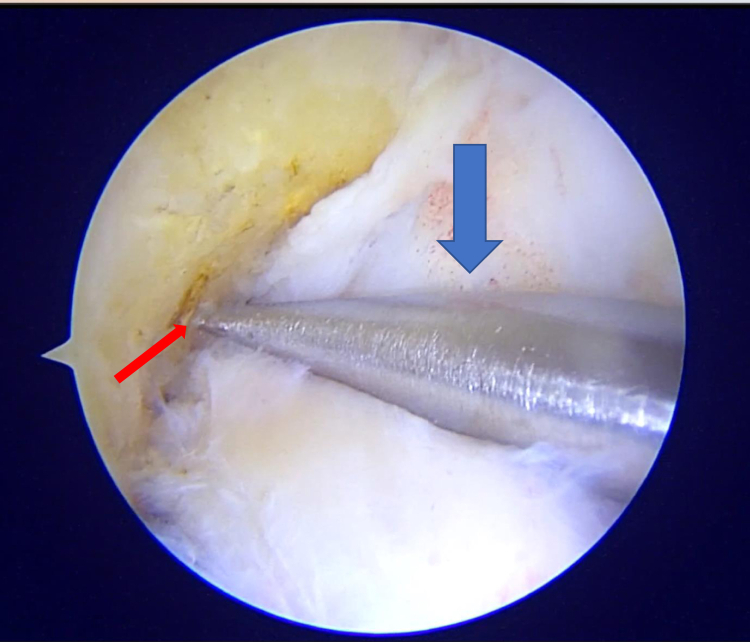
Fig 4.
Viewing from the anterolateral portal, an angled awl (blue arrow) is introduced from the anteromedial portal. The femoral footprint is marked (red arrow) with the awl, and its anatomic location is ascertained.
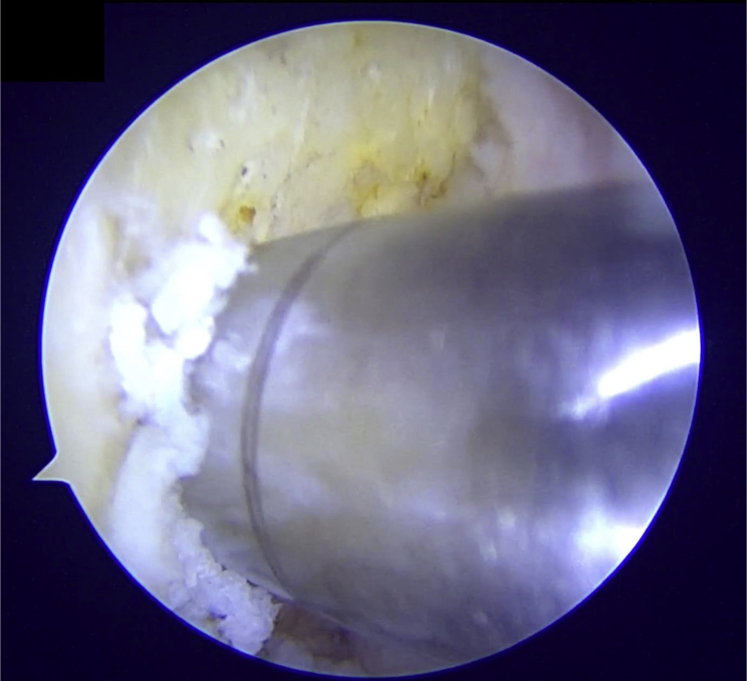
Fig 5.
Reaming of the femoral socket is performed with acorn reamers of appropriate diameter to accommodate the hamstring autograft. The minimum acceptable diameter of the graft is 8 mm. Because the minimum amount of graft required in the socket should be greater than 15 mm, the length of reaming should not be less than 18 to 20 mm.
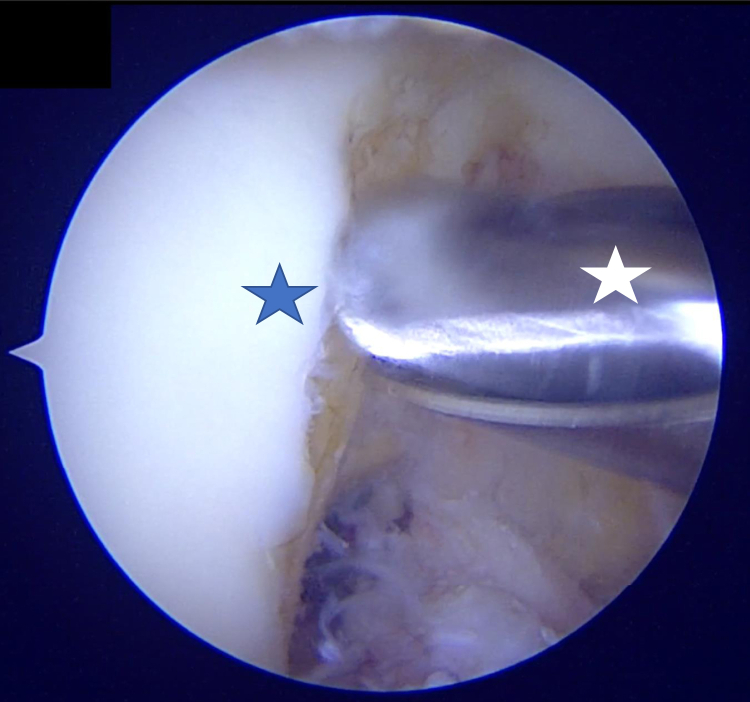
Fig 6.
Bony notchplasty of the medial wall of the lateral femoral condyle (blue star) can be performed to prevent graft impingement and overstuffing of the notch. It is important to protect the remnant with the hood of the burr (white star).
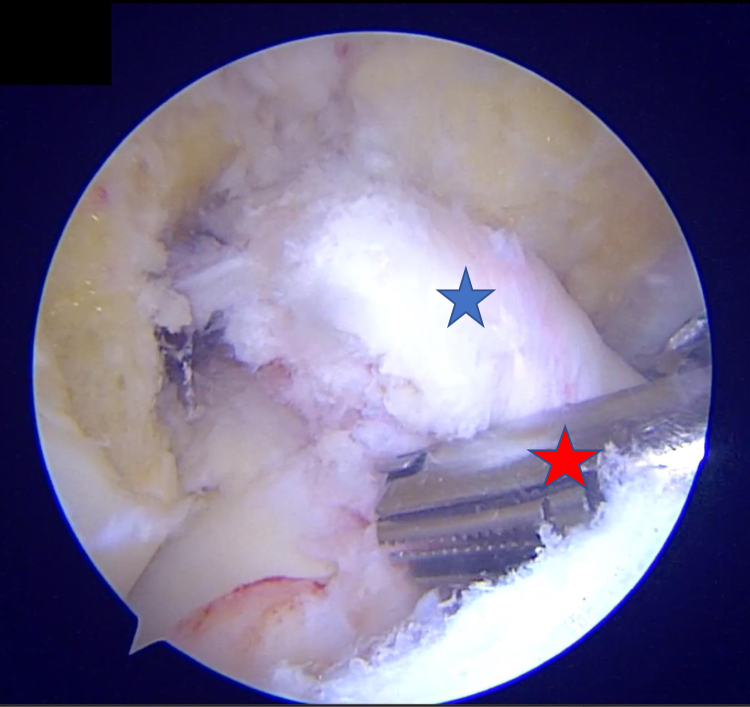
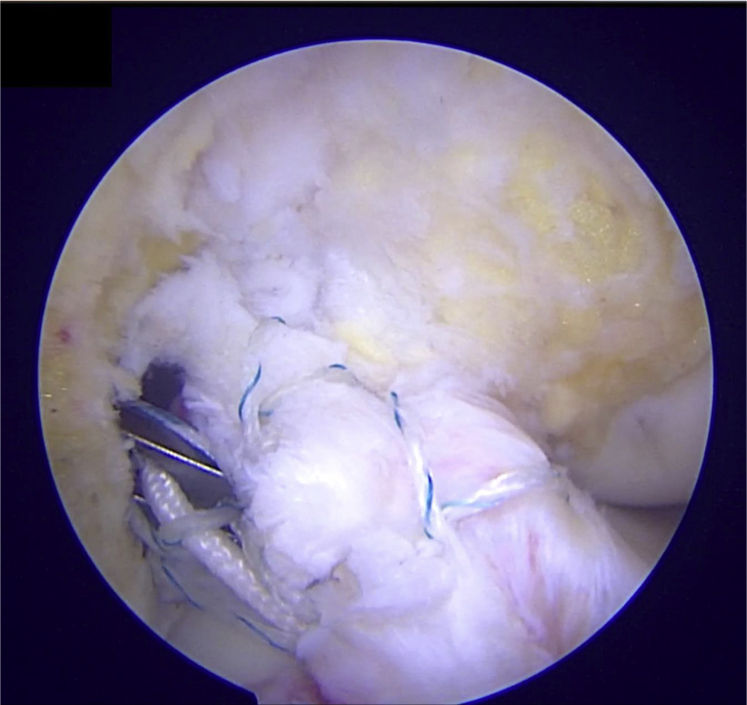
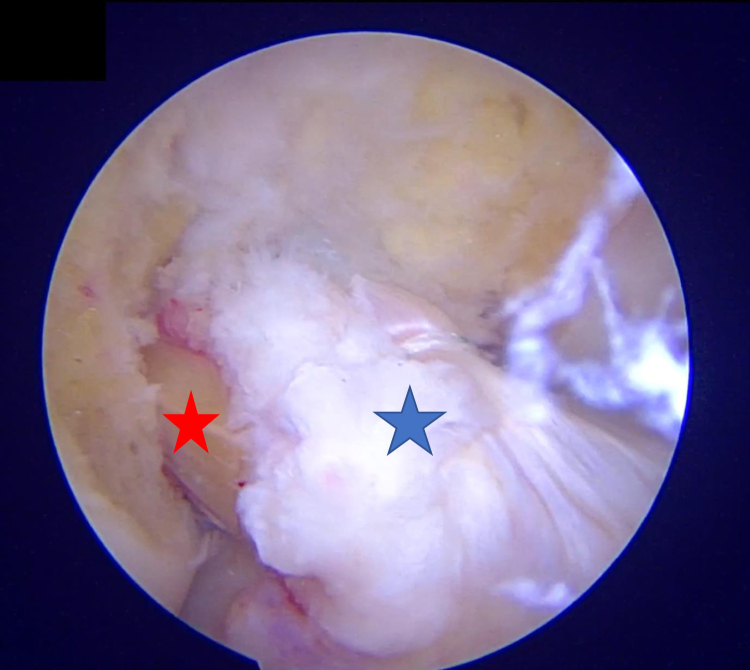
Fig 7.
Suture passage into the anterior cruciate ligament stump (blue star) with an antegrade suture-passing device (Firstpass; red star) is performed from the anteromedial portal with No. 2 ultrahigh-molecular-weight polyethylene suture, with an attempt to crisscross the sutures in the stump from distal to proximal. This is performed through a flexible cannula (Passport) (not shown) to prevent any tissue bridges within each suture pass.
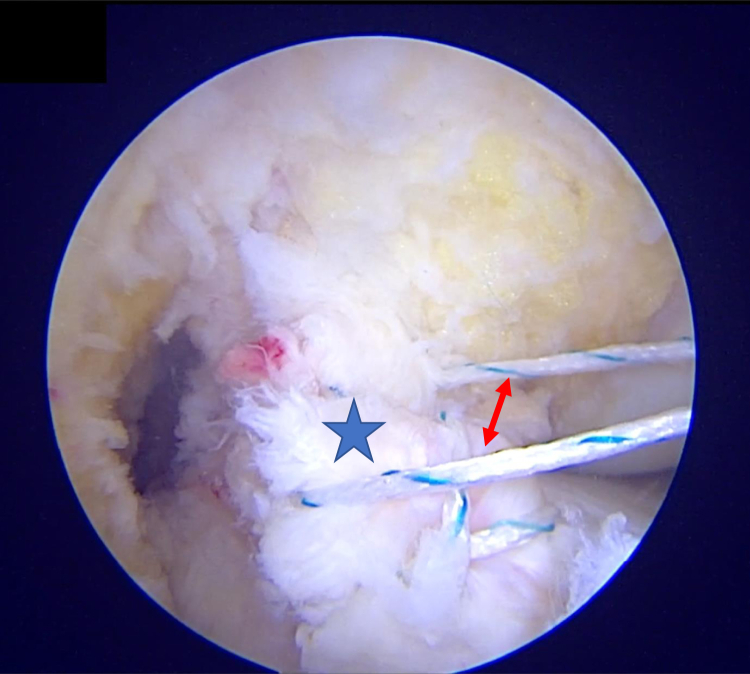
Fig 8.
Suture (red arrow) passed into anterior cruciate ligament stump (blue star) from distal to proximal in crisscross fashion and free ends retrieved through anteromedial portal.
Fig 9.
Tibial tunnel drilling is performed with a tip-aiming device (Acufex, white star), and the wire (red arrow) exit is parallel to the posterior border of the anterior horn of the lateral meniscus and within the native anterior cruciate ligament stump.
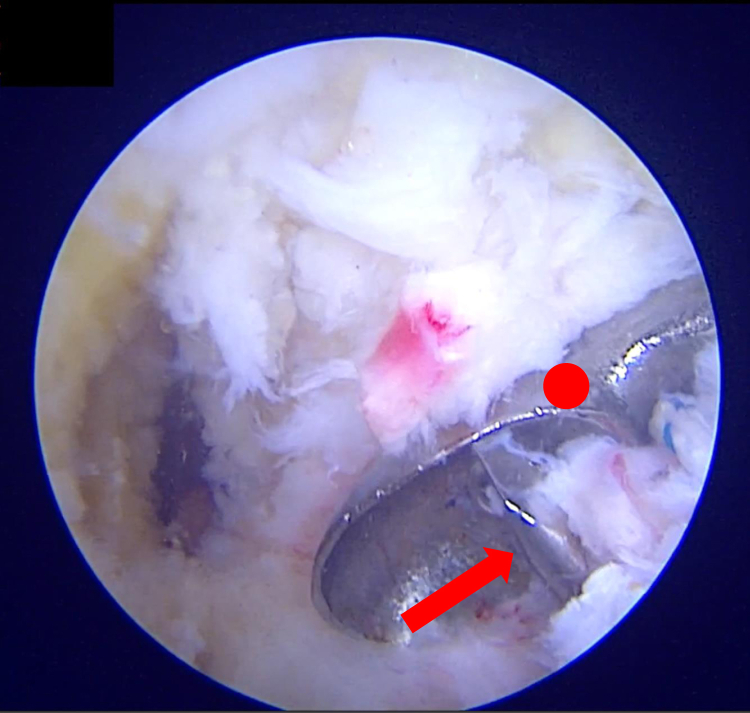
Fig 10.
Reaming of tibial tunnel over guidewire (red arrow). The guidewire, sutures, and anterior cruciate ligament remnant are protected with a curette (red circle) during reaming. Utmost care is taken while reaming and the inner cortex is hand reamed to prevent iatrogenic damage to the stump and sutures.
Graft Passage and Tensioning of Remnant
A Beath pin loaded with shuttle suture is passed into the femoral tunnel through the AM portal; it exits on the lateral side of the thigh. The free ends of shuttle suture are clamped and parked (Fig 11). Now, with the help of a suture grasper, all the sutures are brought out through the tibial tunnel in a single pass because it prevents tissue entanglement (Fig 12). The sutures of the adjustable-loop button (Procinch) are passed into the shuttle suture. No. 2 ultrahigh-molecular-weight polyethylene sutures (sutures from the remnant) are passed into the button from below up and then into the shuttle suture in the same direction as that of the sutures of the button (Fig 13). The adjustable-loop button is passed and flipped. The passage and flipping of the button can be viewed by inserting the scope in the AM portal because it gives an end-on view of the tunnel. Thereafter, the scope is switched back to the AL portal for viewing after flipping of the button is confirmed. The graft is pulled into the joint, and simultaneously, the sutures of the remnant are tensioned (Figs 14 and 15). After the graft is pulled up to the ascertained depth (minimum of 20 mm), the sutures from the remnant are tensioned (Fig 16).
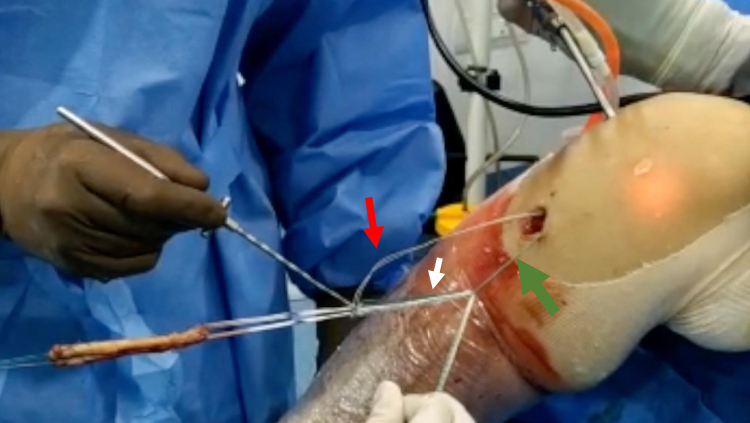
Fig 11.
A shuttle suture (green arrow) loaded into a Beath pin is passed into the femoral tunnel (red arrow) from the anteromedial portal; it exits on the lateral side of the thigh. The free ends of the shuttle suture are clamped and parked.
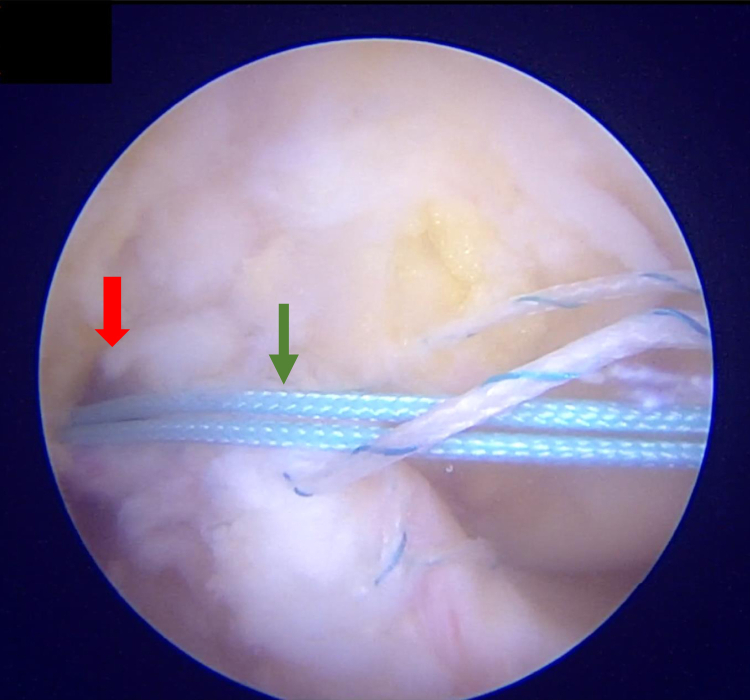
Fig 12.
All the sutures (No. 2 ultrahigh-molecular-weight polyethylene suture [blue arrow] and shuttle suture [green arrow]) are retrieved through the tibial tunnel in a single pass with a suture retriever (red circle); this prevents tissue entanglement.
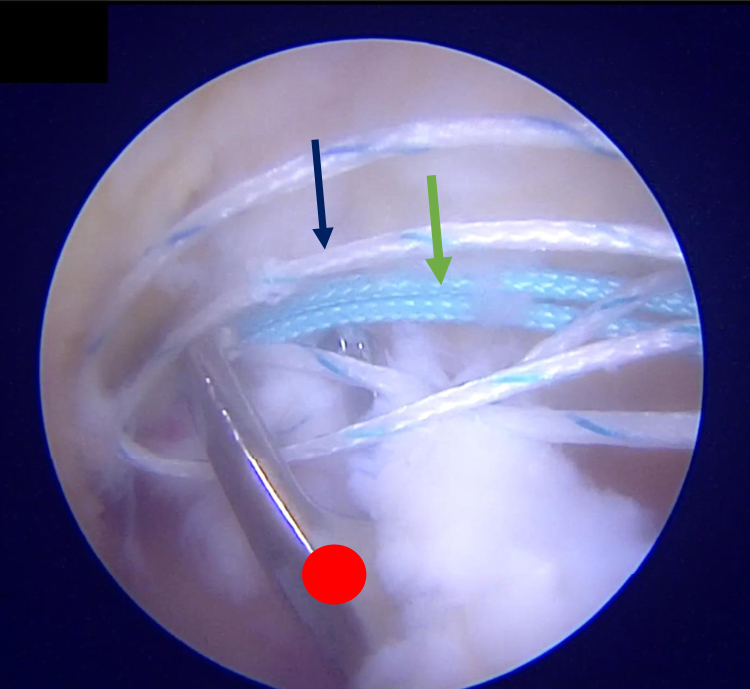
Fig 13.
The sutures of the adjustable loop button (white arrow) are passed into the shuttle suture. The No. 2 ultrahigh-molecular-weight polyethylene sutures (red arrow) are passed into the button from below up and then into the shuttle suture (green arrow) in the same direction as that of the sutures of the button.
Fig 14.
All the sutures are pulled laterally along with the pulling sutures of the button. Slack in the sutures is gradually tightened as the button-graft construct passes into the femoral socket.
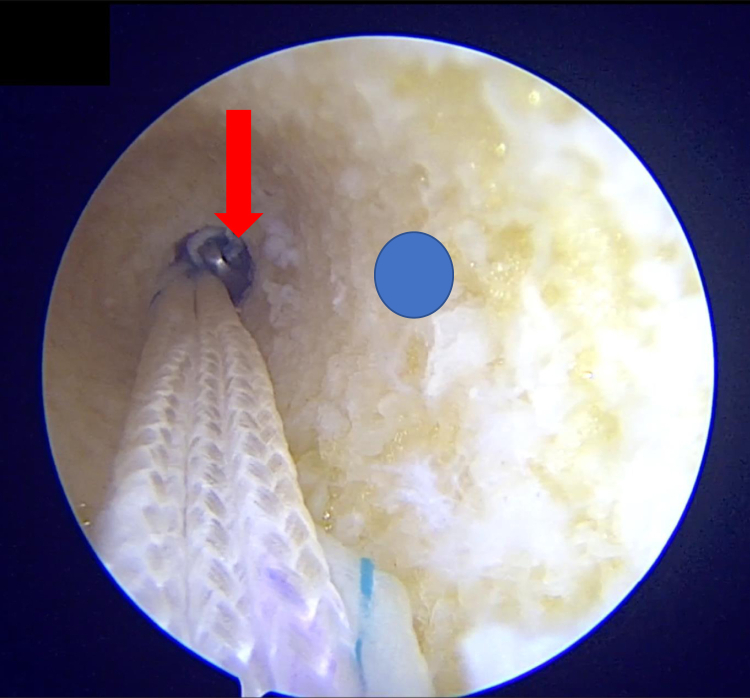
Fig 15.
In this step, the anteromedial portal becomes the viewing portal. This gives an end-on view of the femoral socket (blue circle) and helps in flipping the button (red arrow) on the lateral cortex under vision. The button is pulled to the measured length and flipped on the lateral femoral cortex.
Fig 16.
Viewing from the anterolateral portal, hamstring autograft (red star) is pulled into the tunnel up to the determined length (minimum of 18-20 mm).
Tibial fixation is carried out with a bio-composite interference screw (Biosure Regenesorb) 1 size bigger than the diameter of the tibial tunnel after cycling in 30° of knee flexion (Figs 17 and 18). The sutures from the remnant are tensioned, knotted with 4 or 5 reversing half-hitches over the button with a knot pusher, and cut. It is imperative to push the knot over the button so that it does not become locked over the iliotibial band. At the end of the procedure, it appears as if the remnant envelopes the graft (Fig 19). Additional or loose remnants can be shaved off to prevent roof impingement or cyclops lesion formation. Pearls and pitfalls of the described technique are shown in Table 1, and advantages and disadvantages are listed in Table 2.
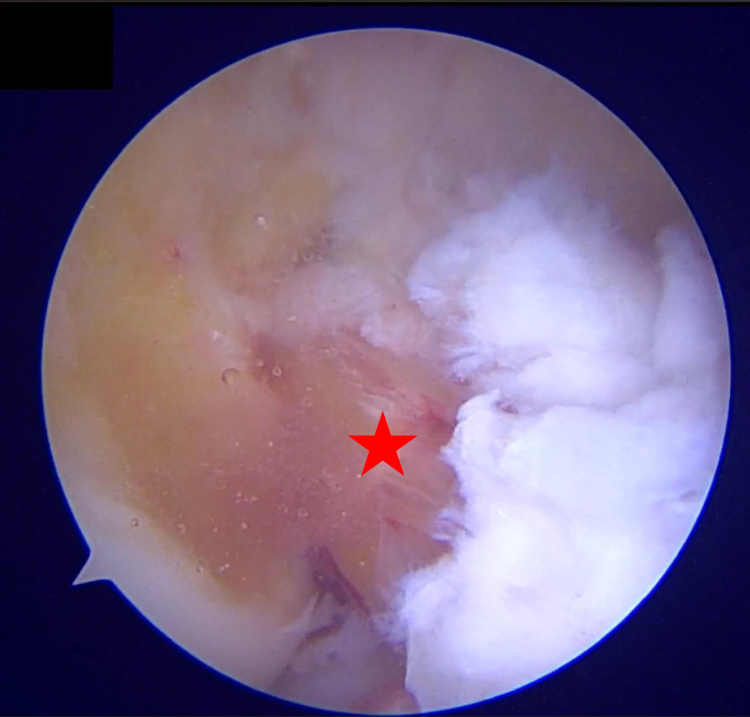
Fig 17.
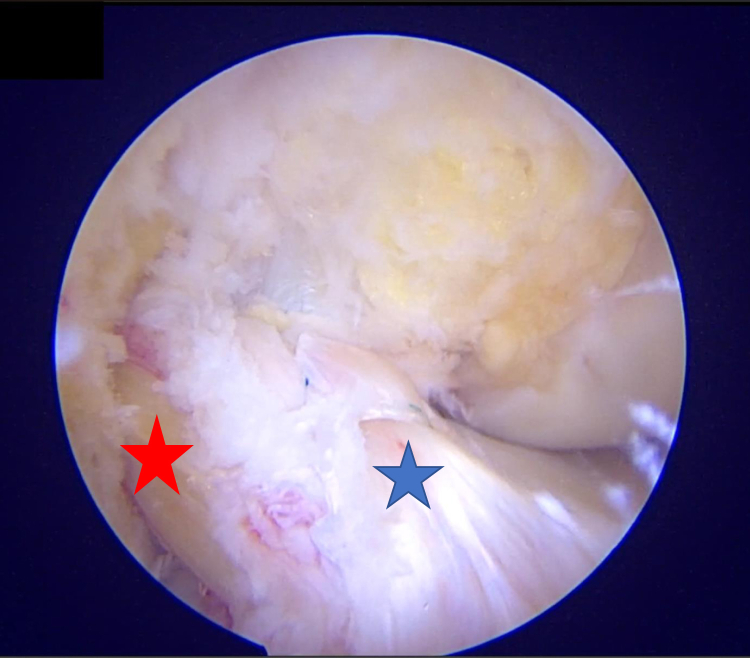
The remnant (blue star) sutures are pulled to the point where there is no slack in the stump and they are closely hugging the autograft (red star).
Fig 18.
The anterior cruciate ligament remnant (blue star) gives the appearance of enveloping the hamstring autograft (red star).
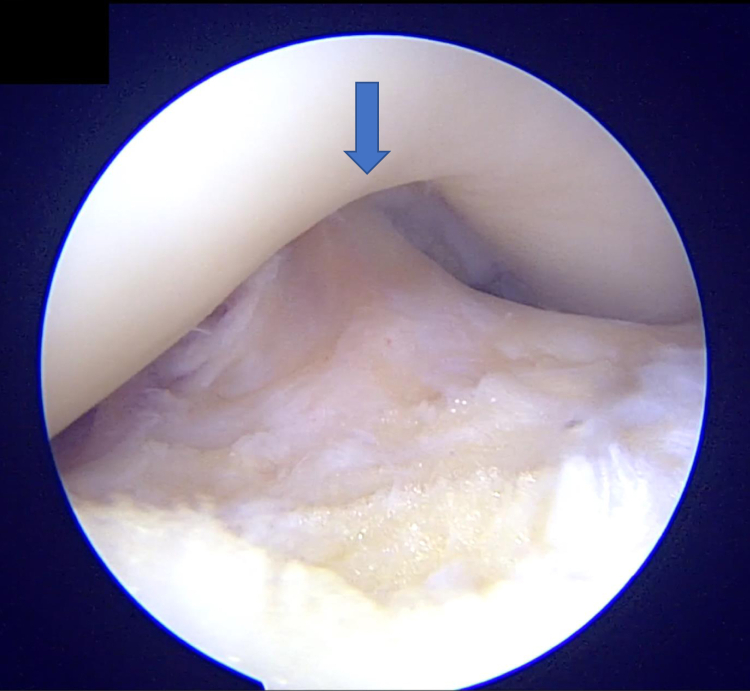
Fig 19.
Final arthroscopic image depicting no roof impingement (blue arrow) of the reconstructed anterior cruciate ligament along with the remnant and full extension of the knee at time zero.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| The anterior fat pad and ligamentum mucosum are cleared to obtain better visibility. | Excessive debridement of the fat pad can cause anterior knee pain and/or crepitus in the postoperative phase because of excessive scarring. |
| Debris near the ACL footprint is cleared. | The ACL remnant can be damaged in the process, thus decreasing the length of remnant. |
| The starting point of the femoral tunnel is marked with an angled awl from the AM portal so that the femoral tunnel will be anatomic. | Visibility is always a challenge; it is important to have proper vision to access the native footprint. |
| Minimal bony notchplasty of the medial wall of the lateral femoral condyle is performed. | Excessive bone takedown can lead to cartilage problems. |
| Suture passage into the ACL remnant is performed over a flexible cannula to prevent tissue bridges. | If a cannula is not used, tissue entanglement can occur. |
| Tibial tunnel drilling must be performed with care; the inner cortex should be hand reamed. | The remnant, as well as the sutures through it, can be damaged. |
| An antegrade self-retrieving suture-passing device is used. | Forcefully pushing the trigger of the device can lead the needle from the device to hit the notch and cause needle breakage in the joint. |
| The sutures from the shuttle suture and remnant should be pulled through the tibial tunnel in a single pass with a suture retriever. | |
| The remnant sutures are loaded into the button from below up and then into the shuttle suture. | Too many sutures can cause confusion intraoperatively. |
| Switching the viewing portal to the AM portal will allow an end-on view of the femoral tunnel during passage and flipping of the adjustable loop button. | |
| During pulling of graft intra-articularly, the sutures from the remnant should be simultaneously tensioned. | Over-tensioning can cause suture to cut through the remnant. |
| With the help of a knot pusher, 4-5 half-hitches are made over the button. | The knot must be tied over the button past the iliotibial band because knots over the iliotibial band can cause lateral-sided thigh pain. |
ACL, anterior cruciate ligament; AM, anteromedial.
Table 2.
Advantages and Disadvantages
| Advantages |
| Orients native collagen in direction of ACL graft |
| Advantages of standard anatomic ACL reconstruction are not forfeited |
| No loose stump in notch |
| Prevents cyclops lesion formation |
| Better healing and ligamentization |
| No extra implant |
| Disadvantages |
| Not possible in chronic injuries when stump has been resorbed |
| Tunnel drilling can be nonanatomic if visibility is not good, thus compromising advantages of standard anatomic ACL reconstruction |
| Need for antegrade suture-passing device and short flexible cannula |
| Care must be practiced while drilling tunnels |
ACL, anterior cruciate ligament.
Rehabilitation
All patients began hamstring isometrics and active range of movement based on associated lesions. In patients with an isolated ACLR, weight bearing as tolerated is started on postoperative day 1. In those with associated meniscal repairs or articular cartilage repairs, weight bearing is delayed for 6 weeks. The target for range of movement is 90° at the end of 3 weeks. At 9 months, patient undergo assessment for return to sport.
Discussion
A process occurs after acute injury to the ACL that leads to its rapid degeneration and resorption. This happens because of its intra-articular location.8,9 The potential role of remnants has been widely studied, and the presence of mechanoreceptors in the stump influences motor function.10 Remnant preservation acts as a biological sleeve; hence, it accelerates revascularization and ligamentization and preserves proprioception.11 Crain et al.12 described variation in the patterns of scarring of the ACL stump. Their patients were divided into 4 groups based on the ACL remnant morphology: (1) ACL remnant scarring to the posterior cruciate ligament (38%), (2) ACL stump scarring to the roof of the notch (8%), (3) ACL remnant scarring to the lateral wall of the notch or the medial aspect of the lateral femoral condyle (12%), and (4) no identifiable ligament tissue remaining (42%). Adachi et al.13 found favorable results on second-look arthroscopy in patients in whom the remnant was preserved and found remodeling of the graft covered with synovium. Moreover, remnant preservation has been reported to have an advantage in reducing the rate of graft rupture after primary ACLR; it also facilitates early functional recovery.14 Noh et al.15 described a technique using remnant preservation and re-tensioning to cover the ACL graft; on second-look arthroscopy 1 year after the procedure, they found that synovium covered 70% or more of the graft. The anterior portion of the graft was entirely covered in their re-tensioning technique.15 Kim et al.16 compared second-look arthroscopic findings and clinical results according to the amount of remnant preserved in ACLR and found a statistically significant difference in hypertrophy and synovialization in the group of patients in whom more than 50% of the remnant was preserved. In addition, a significant difference in pivot-shift test findings was found between the 2 groups in their study. Zhang et al.,17 in a prospective randomized control trial, looked at the effects of remnant preservation on tibial tunnel enlargement in ACLR with hamstring autograft. They found that remnant preservation can resist tibial tunnel enlargement possibly by preventing seepage of synovial fluid between graft and bone. However, the clinical results were the same after both the remnant-preserving and non–remnant-preserving techniques. If tunnel enlargement occurs, however, it can contribute to decision making during revision ACLR.
ACLR with remnant preservation does not come without complications. It leads to cyclops lesions, graft impingement, and extension loss.4, 5, 6 This can be attributed to the remnant lying loose in the notch, overstuffing of the notch, and faulty tunnel position. Re-tensioning of the remnant along with the graft can prevent cyclops lesion formation. A technique described by Ahn et al.7 re-tensions the remnant using cross pins. In our technique, we use an adjustable-loop button and knot down the sutures passed through the remnant over the button laterally because it gives the advantage of orienting the native collagen in the same direction as that of the graft; thus, both tissues work synergistically. Re-tensioning prevents the stump from lying loose in the notch and prevents cyclops lesion formation, along with the added advantages of remnant preservation. A systematic review by Tanabe et al.18 showed that remnant preservation does not increase the rate of cyclops syndrome or lesions. However, re-tensioning of the remnant theoretically decreases the risk of cyclops lesion formation, which may be a cause of symptomatic extension deficit.19 Impingement, which most commonly occurs on the medial surface of the lateral femoral condyle, can be prevented by adding minimal bony notchplasty. There can be overstuffing of the notch because of remnant preservation and the graft. This also is taken care of by notchplasty and anatomic tunnel drilling. Faulty tunnel placement can be a reason for extension loss, but with skill enhancement and careful drilling can protect the remnant as well as prevent this complication. Lu et al.20 performed a clinical study comparing the tunnel placement during ACLR using bony landmarks and the remnant footprint. This study concluded that tunnel placement performed using the remnant footprint yields better functional results and higher subjective outcome scores with better second-look arthroscopy findings and no revision cases.
However, a limitation of our technique is the requirement for a special set of instruments such as an antegrade suture passer and cannula that may not be required during standard ACLR. In addition, because the visibility of the footprint is obscured by the presence of remnant tissue, surgical time may increase and this technique will need high surgical skills to avoid complications.
In conclusion, the described technique can be a good option because it may provide a better scaffold along the direction of the native ACL collagen for early and better ligamentization of the graft. However, during remnant preservation, one should not compromise on tunnel placement, which can be less forgiving than preserving the remnant. Randomized controlled trials with long-term follow-up, along with comparative and radiologic studies, would add to our knowledge of preserving and tensioning the remnant as in this technique.
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Each step of the remnant envelope technique of remnant-preserving arthroscopic anterior cruciate ligament (ACL) reconstruction is shown. The patient is placed supine, and a tourniquet is applied to the proximal thigh of the right leg. A side support and 2 foot supports are applied to hold the knee in 90° of flexion and full flexion. Standard anteromedial (AM) and anterolateral (AL) portals are created. During diagnostic arthroscopy, the type of ACL tear is determined and the decision is made to preserve the ACL stump. The AL portal is the viewing portal during most of the procedure, and the AM portal is the working portal. Ipsilateral hamstring autograft is harvested. Viewing from the AL portal, after clearance of the ACL footprint, the anatomic femoral starting point of the tunnel is marked with an angled awl; the appropriate size of tunnel is then created (minimum of 8 mm in diameter up to a minimum depth of 20 mm to accommodate the graft) by independent tunnel drilling from the AM portal. During reaming of the femoral tunnel, the knee is held in full flexion. Bony notchplasty particularly of the medial wall of the lateral femoral condyle can be performed if graft impingement is anticipated. The next step involves passing suture into the remnant, which is performed after the passage of a flexible cannula (Passport) with an antegrade self-retrieving suture passer (Firstpass). No. 2 ultrahigh-molecular-weight polyethylene suture material (Clinifibre) is used. An attempt is made to make crisscross suture passes in the ACL stump from distal to proximal. A minimum of 4 or 5 passes into the remnant are attempted. The sutures are then retrieved through the AM portal. With the knee in 90° of flexion and viewing from the AL portal, tibial tunnel drilling is performed with a guide (Acufex tip aimer). The tunnel's exit is parallel to the posterior border of the anterior horn of the lateral meniscus and within the native ACL stump. It is very important to hand ream the inner cortex because it prevents damage to the stump and sutures. It is also better to clear both tunnels of soft-tissue and bone debris because this will aid in graft passage. A Beath pin loaded with shuttle suture is passed into the femoral tunnel through the AM portal; it exits on the lateral side of the thigh. The free ends of shuttle suture are clamped and parked. Now, with the help of a suture grasper, all the sutures are brought out through the tibial tunnel in a single pass because it prevents tissue entanglement. The sutures of the adjustable loop button (Procinch) are passed into the shuttle suture. No. 2 ultrahigh-molecular-weight polyethylene sutures (sutures from the remnant) are passed into the button from below up and then into the shuttle suture in the same direction as that of the sutures of the button. The adjustable loop button is passed and flipped. The passage and flipping of the button can be viewed by inserting the scope in the AM portal because it gives an end-on view of the tunnel. Thereafter, the scope is switched back to the AL portal for viewing after flipping of the button is confirmed. The graft is pulled into the joint, and simultaneously, the sutures of the remnant are tensioned. After the graft is pulled up to the ascertained depth (minimum of 20 mm), the sutures from the remnant are tensioned. Tibial fixation is carried out with a bio-composite interference screw (Biosure Regenesorb) 1 size bigger than the diameter of the tibial tunnel after cycling in 30° of knee flexion. The sutures from the remnant are tensioned, knotted with 4 or 5 reversing half-hitches over the button with a knot pusher, and cut. It is imperative to push the knot over the button so that it does not become locked over the iliotibial band. At the end of the procedure, it appears as if the remnant envelopes the graft. Additional or loose remnant can be shaved off to prevent roof impingement or cyclops lesion formation.
References
- 1.Lai C.C.H., Ardern C.L., Feller J.A., Webster K.E. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: A systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018;52:128–138. doi: 10.1136/bjsports-2016-096836. [DOI] [PubMed] [Google Scholar]
- 2.Sherman M.F., Lieber L., Bonamo J.R., Podesta L., Reiter I. The long-term followup of primary anterior cruciate ligament repair: Defining a rationale for augmentation. Am J Sports Med. 1991;19:243–255. doi: 10.1177/036354659101900307. [DOI] [PubMed] [Google Scholar]
- 3.Takahashi T., Kondo E., Yasuda K. Effects of remnant tissue preservation on the tendon graft in anterior cruciate ligament reconstruction: A biomechanical and histological study. Am J Sports Med. 2016;44:1708–1716. doi: 10.1177/0363546516643809. [DOI] [PubMed] [Google Scholar]
- 4.Nakayama H., Kambara S., Iseki T., Kanto R., Kurosaka K., Yoshiya S. Double-bundle anterior cruciate ligament reconstruction with and without remnant preservation—Comparison of early postoperative outcomes and complications. Knee. 2017;24:1039–1046. doi: 10.1016/j.knee.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 5.Wang H., Liu Z., Li Y. Is remnant preservation in anterior cruciate ligament reconstruction superior to the standard technique? A systematic review and meta-analysis. Biomed Res Int. 2019;2019:1652901. doi: 10.1155/2019/1652901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abouheif M.M. Midterm results of remnant preserving ACL reconstruction, using hamstring tendon autograft and a special surgical technique. J Clin Exp Orthop. 2017;3:44. [Google Scholar]
- 7.Ahn J.H., Lee Y.S., Ha H.C. Anterior cruciate ligament reconstruction with preservation of remnant bundle using hamstring autograft: Technical note. Arch Orthop Trauma Surg. 2009;129:1011–1015. doi: 10.1007/s00402-008-0597-7. [DOI] [PubMed] [Google Scholar]
- 8.Murray M.M., Martin S.D., Martin T.L., Spector M. Histological changes in the human anterior cruciate ligament after rupture. J Bone Joint Surg Am. 2000;82:1387–1397. doi: 10.2106/00004623-200010000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Kohn D. Arthroscopy in acute injuries of anterior cruciate-deficient knees: Fresh and old intraarticular lesions. Arthroscopy. 1986;2:98–102. doi: 10.1016/s0749-8063(86)80022-6. [DOI] [PubMed] [Google Scholar]
- 10.Lee B.I., Min K.D., Choi H.S. Immunohistochemical study of mechanoreceptors in the tibial remnant of the ruptured anterior cruciate ligament in human knees. Knee Surg Sports Traumatol Arthrosc. 2009;17:1095–1101. doi: 10.1007/s00167-009-0831-z. [DOI] [PubMed] [Google Scholar]
- 11.Lee B.-I., Kwon S.-W., Kim J.-B., Choi H.-S., Min K.-D. Comparison of clinical results according to amount of preserved remnant in arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft. Arthroscopy. 2008;24:560–568. doi: 10.1016/j.arthro.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 12.Crain E.H., Fithian D.C., Paxton E.W., Luetzow W.F. Variation in anterior cruciate ligament scar pattern: Does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy. 2005;21:19–24. doi: 10.1016/j.arthro.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 13.Adachi N., Ochi M., Uchio Y., Sumen Y. Anterior cruciate ligament augmentation under arthroscopy. Arch Orthop Trauma Surg. 2000;120:128–133. doi: 10.1007/s004020050028. [DOI] [PubMed] [Google Scholar]
- 14.Takazawa Y., Ikeda H., Kawasaki T. ACL reconstruction preserving the ACL remnant achieves good clinical outcomes and can reduce subsequent graft rupture. Orthop J Sports Med. 2013;1 doi: 10.1177/2325967113505076. 2325967113505076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Noh J.H., Kyung H.S., Roh Y.H., Kang T.S. Remnant-preserving and re-tensioning technique to cover the graft in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25:1205–1210. doi: 10.1007/s00167-015-3854-7. [DOI] [PubMed] [Google Scholar]
- 16.Kim M.K., Lee S.R., Ha J.K., Ra H.J., Kim S.B., Kim J.G. Comparison of second-look arthroscopic findings and clinical results according to the amount of preserved remnant in anterior cruciate ligament reconstruction. Knee. 2014;21:774–778. doi: 10.1016/j.knee.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Q., Zhang S., Cao X., Liu L., Liu Y., Li R. The effect of remnant preservation on tibial tunnel enlargement in ACL reconstruction with hamstring autograft: A prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2014;22:166–173. doi: 10.1007/s00167-012-2341-7. [DOI] [PubMed] [Google Scholar]
- 18.Tanabe Y., Yasuda K., Kondo E., Kitamura N. Clinical results of anterior cruciate ligament reconstruction with ligament remnant tissue preservation: A systematic review. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2016;4:1–8. doi: 10.1016/j.asmart.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sonnery-Cottet B., Panisset J.-C., Colombet P. Partial ACL reconstruction with preservation of the posterolateral bundle. Orthop Traumatol Surg Res. 2012;98(suppl):S165–S170. doi: 10.1016/j.otsr.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 20.Lu W., Wang D., Zhu W. Placement of double tunnels in ACL reconstruction using bony landmarks versus existing footprint remnant: A prospective clinical study with 2-year follow-up. Am J Sports Med. 2015;43:1206–1214. doi: 10.1177/0363546515570850. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Each step of the remnant envelope technique of remnant-preserving arthroscopic anterior cruciate ligament (ACL) reconstruction is shown. The patient is placed supine, and a tourniquet is applied to the proximal thigh of the right leg. A side support and 2 foot supports are applied to hold the knee in 90° of flexion and full flexion. Standard anteromedial (AM) and anterolateral (AL) portals are created. During diagnostic arthroscopy, the type of ACL tear is determined and the decision is made to preserve the ACL stump. The AL portal is the viewing portal during most of the procedure, and the AM portal is the working portal. Ipsilateral hamstring autograft is harvested. Viewing from the AL portal, after clearance of the ACL footprint, the anatomic femoral starting point of the tunnel is marked with an angled awl; the appropriate size of tunnel is then created (minimum of 8 mm in diameter up to a minimum depth of 20 mm to accommodate the graft) by independent tunnel drilling from the AM portal. During reaming of the femoral tunnel, the knee is held in full flexion. Bony notchplasty particularly of the medial wall of the lateral femoral condyle can be performed if graft impingement is anticipated. The next step involves passing suture into the remnant, which is performed after the passage of a flexible cannula (Passport) with an antegrade self-retrieving suture passer (Firstpass). No. 2 ultrahigh-molecular-weight polyethylene suture material (Clinifibre) is used. An attempt is made to make crisscross suture passes in the ACL stump from distal to proximal. A minimum of 4 or 5 passes into the remnant are attempted. The sutures are then retrieved through the AM portal. With the knee in 90° of flexion and viewing from the AL portal, tibial tunnel drilling is performed with a guide (Acufex tip aimer). The tunnel's exit is parallel to the posterior border of the anterior horn of the lateral meniscus and within the native ACL stump. It is very important to hand ream the inner cortex because it prevents damage to the stump and sutures. It is also better to clear both tunnels of soft-tissue and bone debris because this will aid in graft passage. A Beath pin loaded with shuttle suture is passed into the femoral tunnel through the AM portal; it exits on the lateral side of the thigh. The free ends of shuttle suture are clamped and parked. Now, with the help of a suture grasper, all the sutures are brought out through the tibial tunnel in a single pass because it prevents tissue entanglement. The sutures of the adjustable loop button (Procinch) are passed into the shuttle suture. No. 2 ultrahigh-molecular-weight polyethylene sutures (sutures from the remnant) are passed into the button from below up and then into the shuttle suture in the same direction as that of the sutures of the button. The adjustable loop button is passed and flipped. The passage and flipping of the button can be viewed by inserting the scope in the AM portal because it gives an end-on view of the tunnel. Thereafter, the scope is switched back to the AL portal for viewing after flipping of the button is confirmed. The graft is pulled into the joint, and simultaneously, the sutures of the remnant are tensioned. After the graft is pulled up to the ascertained depth (minimum of 20 mm), the sutures from the remnant are tensioned. Tibial fixation is carried out with a bio-composite interference screw (Biosure Regenesorb) 1 size bigger than the diameter of the tibial tunnel after cycling in 30° of knee flexion. The sutures from the remnant are tensioned, knotted with 4 or 5 reversing half-hitches over the button with a knot pusher, and cut. It is imperative to push the knot over the button so that it does not become locked over the iliotibial band. At the end of the procedure, it appears as if the remnant envelopes the graft. Additional or loose remnant can be shaved off to prevent roof impingement or cyclops lesion formation.