Abstract
Background
Obstructive sleep apnea syndrome (OSAS) is associated with cardiovascular mortality and morbidity. Several studies have reported that it affects the left ventricle; however, large randomized controlled trials are lacking. The current study aimed to summarize the association between OSAS and left ventricular (LV) structure and function.
Methods
Electronic databases (PubMed, Embase, and Cochrane) and references were searched for articles published until March 2018. A systematic review and meta-analysis were performed to assess LV structure and function in OSAS patients based on echocardiography.
Results
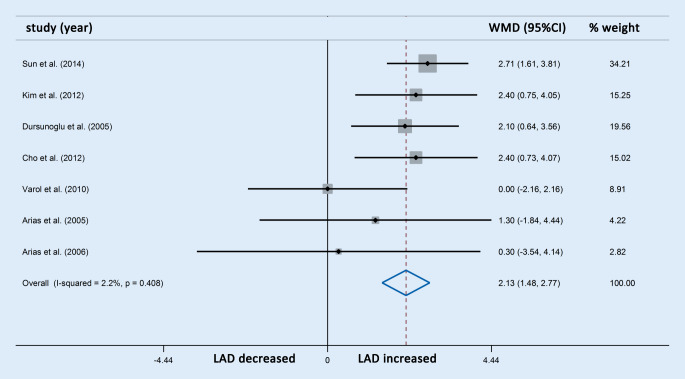
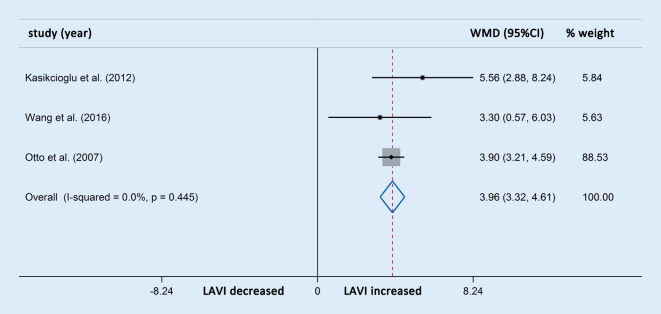
In total, 17 studies with 747 OSAS patients and 426 control participants were included. Patients with OSAS showed an increase in LV diastolic diameter (weighted mean difference [WMD], 95% CI: 1.24 [0.68, 1.80]; p < 0.001), LV systolic diameter (WMD, 95% CI: 1.14 [0.47, 1.81]; p = 0.001), and LV mass (WMD, 95% CI: 35.34 [20.67, 50.00]; p < 0.001). In addition, left ventricular ejection fraction (LVEF) significantly decreased in the OSAS group compared with the controls (WMD, 95% CIs: −1.82 [−2.76, −0.87]; p < 0.001), and the reduction in LVEF was consistent with the severity of OSAS. The OSAS group also showed an increase in left atrial diameter (WMD, 95% CI: 2.13 [1.48, 2.77]; p < 0.001) and left atrial diameter volume index (WMD, 95% CIs: 3.96 [3.32, 4.61]; p < 0.001).
Conclusion
Obstructive sleep apnea syndrome leads to atrial dilatation, left ventricular hypertrophy, enlargement, mass increase and reduction of systolic function. Treatments for OSAS might be beneficial for the preservation of left cardiac structure and function.
Electronic supplementary material
The online version of this article (10.1007/s00059-019-04850-w) contains supplementary material, which is available to authorized users.
Keywords: Left ventricular hypertrophy, Cardiac remodeling, Left ventricular ejection fraction, Hypoxia, Echocardiography
Abstract
Hintergrund
Das obstruktive Schlafapnoesyndrom (OSAS) geht mit kardiovaskulärer Mortalität und Morbidität einher. Im Rahmen verschiedener Studien wurde berichtet, dass es sich auf den linken Ventrikel auswirkt; allerdings fehlen bisher große randomisierte kontrollierte Studien. Die aktuelle Studie zielte darauf ab, eine zusammenfassende Übersicht über den Zusammenhang zwischen OSAS und linksventrikulärer Struktur und Funktion zu geben.
Methoden
Elektronische Datenbanken (PubMed, Embase und Cochrane) sowie Literaturangaben wurden nach Artikeln durchsucht, die bis März 2018 publiziert worden waren. Dann wurden eine systematische Übersicht und eine Metaanalyse erstellt, um die LV-Struktur und Funktion bei Patienten mit OSAS auf der Grundlage der Echokardiographie zu untersuchen.
Ergebnisse
Insgesamt wurden 17 Studien mit 747 OSAS-Patienten und 426 Kontrollen in die Studie einbezogen. Patienten mit OSAS zeigten einen Anstieg des diastolischen Durchmessers des LV (gewichtete mittlere Differenz, WMD: 1,24; 95 %-KI, 95 %-KI: 0,68–1,80; p < 0,001), des systolischen Durchmessers des LV (WMD: 1,14; 95 %-KI: 0,47–1,81; p = 0,001) und der LV-Masse (WMD: 35,34; 95 %-KI: 20,67–50,00; p < 0,001). Außerdem nahm die linksventrikuläre Ejektionsfraktion (LVEF) signifikant in der OSAS-Gruppe im Vergleich zu den Kontrollen ab (WMD: −1,82; 95 %-KI: −2,76 bis −0,87; p < 0,001), und die Abnahme der LVEF stand in Übereinstimmung mit dem Schweregrad des OSAS. In der OSAS-Gruppe zeigte sich auch ein Anstieg des linksatrialen Durchmessers (WMD: 2,13; 95 %-KI: 1,48–2,77; p < 0,001) und des Volumenindex des linksatrialen Durchmessers (WMD: 3,96; 95 %-KI: 3,32–4,61; p < 0,001).
Schlussfolgerung
Ein obstruktives Schlafapnoesyndrom führt zur Vorhofdilatation, linksventrikulären Hypertrophie, Vergrößerung, Massenzunahme und Abnahme der systolischen Funktion. Die Behandlung eines OSAS könnte sich günstig auf den Erhalt der Linksherzstruktur und -funktion auswirken.
Schlüsselwörter: Linksventrikuläre Hypertrophie, Kardiales Remodeling, Linksventrikuläre Ejektionsfraktion, Hypoxie, Echokardiographie
Obstructive sleep apnea syndrome (OSAS) is a common chronic disorder characterized by recurrent episodes of upper respiratory tract obstruction and hypoxia during sleep, leading to the occurrence of loud snoring, breathing interruptions, frequent awakenings or insomnia, morning fatigue, daytime sleepiness, attention deficit, and cognitive dysfunction[18]. The diagnosis and severity of OSAS are usually assessed by the total number of apnea and hypopnea episodes per hour of sleep, namely, the apnea hypopnea index (AHI). This condition is highly prevalent in the general population, affecting 2%–15% of adults [7, 20, 21, 23, 44, 56, 57], particularly those older than 65 years.
Obstructive sleep apnea syndrome is not only associated with a higher risk of occupational accidents but also leads to more cardiovascular diseases such as cardiac remodeling and dysfunction [7, 41]. Echocardiography is a noninvasive, low-cost, time-saving and accurate tool for assessing alterations in cardiac structure and function, and has been widely used in the clinic. To date, there have been some studies exploring the alternations in echocardiographic parameters in OSAS patients. However, large-scale clinical controlled trials on this field are still lacking, and most of the related research had small sample sizes and used inconsistent inclusion and exclusion criteria.
Owing to the overall low awareness of the relationship between OSAS and left ventricular (LV) dysfunction in clinical management, the aim of the current study was to summarize the association between OSAS and LV function and structure, in order to provide guidelines for clinical decision-making.
Methods
Data source, search strategy, and selection criteria
Electronic databases including PubMed, Embase, and the Cochrane Library were searched from database inception to March 2018 using the following terms: “ventricular function, left”; “ventricular dysfunction, left”; “heart failure”; “echocardiography”; “sleep apnea, obstructive”; and “sleep-disordered breathing” (see Supplementary Table S1). In addition, we also checked the reference lists of identified reports for other potentially relevant studies. The literature search and study selection were undertaken by two reviewers independently. Any inconsistencies were settled by another researcher. A systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
The following criteria were used to identify potentially suitable studies: (1) articles were written fully in English; (2) enrolled participants were all adults (older than 18 years); (3) OSAS was diagnosed by polysomnography and assessed with the AHI; (4) the study included a control group; (5) the study reported at least one of the measures of LV function or structure; (6) there was no significant difference in the body mass index (BMI) of the two groups.
The exclusion criteria were: (1) duplicate reports; (2) studies that had not yet terminated; (3) reviews, case reports, or animal experiments; (4) central sleep apnea; (5) OSAS patients with major comorbidities such as structural heart disease, cardiomyopathy, obstructive or restrictive lung disease demonstrated on pulmonary function testing, pulmonary hypertension, etc.; (6) previous or current treatment for OSAS; (7) studies with hypertension in OSAS group or in control group were excluded in order to avoid the definite effect of hypertension or antihypertension drugs on cardiac remodeling (as an exception, one article was included because the blood pressure level and antihypertensive drugs were both matched between the control group and OSAS group).
Data extraction and synthesis
Two independent readers screened and extracted data from eligible articles. The following data were extracted from the relevant studies: first author, year of publication, country, number of participants, mean age, BMI, mean AHI, OSAS diagnostic criteria, and LV morphology and function parameters. The main echocardiographic parameters included early diastolic peak flow velocity (E), late diastolic peak flow velocity (A), deceleration time of E wave (DT), early myocardial Doppler peak velocity (Em), late myocardial Doppler peak velocity (Am), LV diastolic diameter (LVEDD), LV systolic diameter (LVESD), ejection fraction (EF), isovolumetric relaxation time (IVRT), interventricular septum diameter (IWD), posterior wall diameter (PWD), LV mass (LVM), LV mass index (LVMI), left atrial diameter (LAD), left atrial diameter volume index (LAVI).
Statistical analysis
Several studies stratified patients on the basis of OSAS severity (mild, moderate, or severe) and reported the grouped LV function data within each stratum. The two formulae presented here were used to combine subgroups and calculate the overall means and standard deviations. However, in the subgroup analysis, each stratum was considered as a separate substudy.
The equations are listed in Supplementary Table S2.
Cochran’s χ2 test and the I 2 statistic were applied to estimate the percentage of variability across studies due to between-study heterogeneity. Heterogeneity was considered statistically significant at p < 0.10 and I 2 > 50%. The weighted mean difference (WMD) with 95% confidence intervals (CIs) was calculated using a fixed-effects model if I 2 < 50% and using a random-effects model if I 2 > 50%. Fisher’s z test was used to determine the statistical significance of the pooled WMDs. We conducted sensitivity analyses or subgroup analysis if I 2 > 50%. Egger’s test and Begg’s test were used to examine the presence of publication bias. All analyses were performed using the statistical package Stata, version 14.0 (StataCorp., College Station, TX, USA). The quality of the enrolled studies was evaluated by two independent reviewers according to the Newcastle–Ottawa Scale ranging from 0 to 8.
Results
Search results
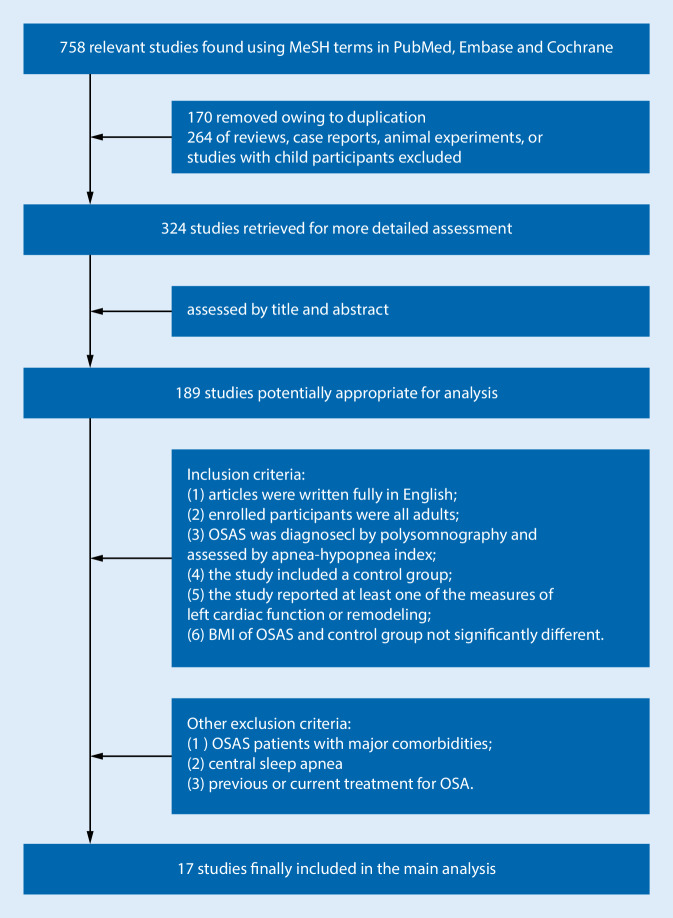
After a strict screening, 739 citations were removed according to the inclusion and exclusion criteria described earlier, and a total of 17 studies with 747 OSAS patients and 426 control participants were included in the final meta-analysis (see Fig. 1).
Fig. 1.
Study selection. BMI body mass index, OSAS obstructive sleep apnea syndrome
Characteristics of studies
The publication years of the eligible studies ranged from 2005 to 2016. The majority of the studies (nine studies, 52.9%) were conducted in Turkey; two studies were conducted in China, two were conducted in Spain, two were conducted in South Korea, one study was conducted in the United States, and one in Italy. In all studies, OSAS was diagnosed and assessed by polysomnography: The control group was defined as having AHI < 5 events/h, while mild, moderate, and severe OSAS were rated as, respectively, 5 ≤ AHI < 15 events/h, 15 ≤ AHI < 30 events/h, and AHI ≥ 30 events/h. For the assessment of left atrial (LA) remodeling, seven studies (41.2%) used LAD and four studies (23.5%) used LAVI. For the assessment of LV remodeling, 13 studies (76.4%) used LVEDD, 11 studies (64.7%) used LVESD, and six studies (35.3%) used LVM. For the assessment of LV function, 15 studies (88.2%) used LVEF. The main characteristics of the studies in this systematic review are listed in Table 1 and the quality of included studies are listed in Supplementary Table S3.
Table 1.
Characteristics of the included studies
| Study | Year of publication | Country | Number of participants | Mean (SD) age (year) | BMI | OSAS diagnostic criteria | Mean (SD) AHI | LA remodeling and dysfunction measures | LV remodeling and dysfunction measures |
|---|---|---|---|---|---|---|---|---|---|
| Kasikcioglu et al. [27] | 2005 | Turkey | Control (14) | 51.8 (12.9) | 27.9 (2.5) | PSG: AHI < 5 events/h | 1.7 (1.1) | N/A | LVM, LVMI, PWD, IVSd, E, A, E/A, DT, DTc, DTm, DTmc, Em, Am, Sm, Em/Am |
| OSAS (14) | 49.7 (11.6) | 28.7 (2.9) | PSG: AHI ≥ 15 events/h | 32.9 (7.1) | |||||
| Ozkececi et al. [37] | 2016 | Turkey | Control (30) | 46.4 (14) | 29.3 (4.8) | PSG: AHI ≤ 5 events/h | 1 (1–4) | N/A | LVEDD, LVESD, Left Tei index, LVEF |
| OSAS (60) | 49.6 (11.7) | 31.6 (5.8) | PSG: AHI ≥ 5 events/h | 24.5 (6–98) | |||||
| Altekin et al. [2] | 2012 | Turkey | Control (21) | 45.38 (4.588) | 26.35 (4.14) | N/A | N/A | N/A | EF, DVI, SVI, IVSD, PWD, LVM, LAVI, E/A, MPI, DT, E/E′ |
| Mild (20) | 46.95 (6.468) | 28.68 (3.44) | 5 ≤ AHI < 15 events/h | 10.73 (2.57) | N/A | ||||
| Moderate (19) | 46.79 (5.029) | 29.05 (2.26) | 15 ≤ AHI < 30 events/h | 20.52 (2.6) | N/A | ||||
| Severe (19) | 46.68 (7.660) | 29.80 (2.38) | AHI ≥ 30 events/h | 58.1 (16.27) | N/A | ||||
| Sun et al. [45] | 2014 | China | Control (50) | 62.2 (10.8) | 29.66 (4.22) | PSG: AHI < 5 events/h | RDI: 26 (19) | LAD | LVEDD, IVSD, LVPW, LVM, LVMI, |
| OSAS (136) | 63.3 (10.6) | 30.94 (4.15) | PSG: AHI ≥ 5 events/h | RDI: 14 (6) | |||||
| Tanriverdi et al. [46] | 2006 | Turkey | Control (24) | 51.9 (5.2) | 29.4 (3.9) | PSG: AHI < 5 events/h | 3 (1.5) | N/A | IVSD, PWD, LVEDD, LVESD, LVMI, LVEF, peakE/A, Em/Am |
| OSAS (40) | 51.3 (9) | 29.8 (5.3) | AHI ≥ 5 events/h | 25.3 (11.4) | N/A | ||||
| Kim et al. [28] | 2012 | South Korea | Control (24) | 48.42 (7.45) | 27.45 (2.41) | PSG: AHI < 5 events/h | 2.94 (1.44) | LAD、LAVI | IVSD, PWTD, LVMI, RWT, LVEDD, LVESD, LVEF, LVFS |
| OSAS (25) | 43.48 (11.32) | 28.1 (3.1) | AHI ≥ 5 events/h | 19.66 (11.64) | |||||
| Dursunoglu et al. [17] | 2005 | Turkey | Control (20) | 43.5 (6) | 29.3 (2.4) | PSG: AHI < 5 events/h | 5.2 (2.8) | LAD | IVSD, PWD, LVEDD, LVESD, E/A, DT, IVRT, LVEF, MPI |
| Mild (11) | 46.0 (5.6) | 30.4 (4.0) | 5 ≤ AHI < 15 events/h | 25.3 (2.6) | |||||
| Moderate to severe (18) | 46.5 (4.9) | 30.6 (4) | AHI ≥ 15 events/h | 50.1 (11.6) | |||||
| Cho et al. [13] | 2012 | South Korea | Control (20) | 47.2 (7.1) | 27.9 (1.7) | PSG: AHI < 5 events/h | 2.93 (1.44) | LAD | LVEDD, LVESD, IVSTD, PWTD, RWT, LVMI |
| OSAS (25) | 43.5 (11.3) | 28.0 (3.4) | AHI ≥ 5 events/h | 19.7 (11.6) | |||||
| Varol et al. [50] | 2010 | Turkey | Control (18) | 44.8 (11.6) | 29.2 (4.8) | PSG: AHI < 5 events/h | 2.1 (1.6) | LAD | IVSD, LVPWD, LVEDD, LVESD, LVM, LVMI, DT, E/A, IVRT, LVEF, MPI |
| Mild to moderate (25) | 51.2 (8.7) | 29.9 (4.3) | 5 ≤ AHI ≤ 30 events/h | 15.8 (7.4) | |||||
| Severe (21) | 48.9 (9.3) | 32.2 (3.6) | AHI > 30 events/h | 60.7 (24.5) | |||||
| Wang et al. [53] | 2016 | China | Control (30) | 45 (6) | 25 (4) | PSG: AHI < 5 events/h | 2.7 (1.2) | LAV、LAEF、LAVI | LVEDD, LVESD, LVEF, RWTD, LVMI, E, A, E/A, E′, E/E′, DT, IVRT, LVRI |
| Mild (26) | 48 (8) | 26 (4) | 5 ≤ AHI < 15 events/h | 10.5 (3.2) | |||||
| Moderate (29) | 45 (8) | 27 (3) | 15 ≤ AHI < 30 events/h | 18.7 (5.6) | |||||
| Severe (23) | 46 (6) | 27 (4) | AHI ≥ 30 events/h | 57.2 (2.6) | |||||
| Vitarelli et al. [51] | 2013 | Italy | Control (35) | 45.1 (12.2) | 26.8 (4.3) | PSG: AHI < 5 events/h | 3.8 (1.1) | N/A | LVEF, LVMI, IVRT, DT, MPI, E/A |
| Mild (19) | 48.3 (8.2) | 27.5 (5.4) | 5 ≤ AHI < 30 events/h | 15.4 (2.2) | N/A | ||||
| Severe (23) | 47.4 (8.1) | 28.3 (6.5) | AHI ≥ 30 events/h | 59.4 (9.3) | N/A | ||||
| Arias et al. [5] | 2005 | Spain | Control (15) | 48 (9) | 28.7 (4.7) | PSG: AHI < 5 events/h | 3.9 (3.3) | LAD | E, A, E/A, DT, IVRT, LVESD, LVEDD, LVEF, IVSD, PWD, LVM, LVMI |
| OSAS (27) | 52 (13) | 30.5 (4.0) | AHI ≥ 10 events/h | 44.0 (27.5) | |||||
| Arias et al. [6] | 2006 | Spain | Control (10) | 50 (10) | 27.7 (3) | PSG: AHI < 5 events/h | 4.2 (3.5) | LAD | E, A, E/A, DT, LAD, LVEDD, LVESD, LVSF, LVEF, IVSD, LVM, LVMI, LVPWD |
| OSAS (23) | 51 (13) | 30.9 (4) | AHI ≥ 10 events/h | 44.1 (29.3) | |||||
| Altiparmak et al. [3] | 2016 | Turkey | Control (35) | 43.0 (6.4) | 26.2 (3.2) | PSG: AHI < 5 events/h | N/A | LAVI | LVEDD, LVESD, DT, E′, E/A, E/E′, LVMI, |
| OSAS (31) | 45.5 (6.6) | 26.7 (2.1) | AHI ≥ 5 events/h | 45.4 (28.1) | |||||
| Balci et al. [8] | 2012 | Turkey | Control (33) | 41.6 (11.6) | 26.3 (1.4) | PSG: AHI < 5 events/h | 3.2 (1.9) | N/A | IVSD, PWD, LVEDD, LVESD, E/A, DT, LVEF, MPI, LVMI, LV MPI |
| Mild to moderate (30) | 42.5 (11.2) | 26.9 (2.4) | 5 ≤ AHI < 30 events/h | 14.2 (14.6) | N/A | ||||
| Severe (31) | 45.7 (10.3) | 27.3 (2.3) | AHI ≥ 30 events/h | 66.3 (39.9) | N/A | ||||
| Tavil et al. [47] | 2007 | Turkey | Control (29) | 49 (11) | 29 (5) | PSG: AHI < 5 events/h | 2.5 (0.8) | N/A | LVEDD, LVEDD, LVESD, IWSD, PWD, LVEF, LVMI, E, A, E/A, IVRT, E′, A′, E′/A′ |
| OSAS (29) | 48 (10) | 29 (6) | AHI ≥ 5 events/h | 25 (16) | N/A | ||||
| Otto et al. [36] | 2007 | USA | Control (18) | 45 (2) | 32.3 (0.9) | PSG: AHI < 5 events/h | 2 (0.4) | LAVI | LVMI, EF, DT, IVRT |
| OSAS (23) | 45 (3) | 33.7 (0.8) | AHI ≥ 15 events/h | 50 (7) |
OSAS obstructive sleep apnea syndrome, AHI apnea–hypopnea index, BMI body mass index, E early diastolic peak flow velocity, A late diastolic peak flow velocity, DT deceleration time of E wave, DTc heart-rate-corrected DT; DT m Em-wave deceleration time, DT mc heart-rate-corrected DTm, E m early myocardial Doppler peak velocity, A m late myocardial Doppler peak velocity, S m peak velocity of myocardial systolic wave, LVEDD left ventricular diastolic diameter, LVESD left ventricular systolic diameter, LVEF LV ejection fraction, IVRT isovolumetric relaxation time, IWDs interventricular septum diameter, PSG polysomnography, PWD posterior wall diameter, LVM left ventricular mass, LVMI left ventricular mass index, N/A not applicable
Meta-analysis
Table 2 summarizes the data for all the parameters of LA structure, LV structure, and LV function determined by the meta-analysis. Heterogeneity was obvious in the assessment of several parameters, which was speculated as a result of the inconsistent degree of severity of OSAS, varied ages of participants, BMI, geographical location, and duration of OSAS.
Table 2.
Results of the meta-analysis comparing OSAS patients and controls
| Echocardiographic parameters | Number of studies | OSAS/control | WMD (95%CI) | p | Study heterogeneity | Egger’s test p | Begg’s test p | ||
|---|---|---|---|---|---|---|---|---|---|
| I 2 (%) | χ2 | p | |||||||
| LVEDD (mm) | 13 | 563/319 | 1.24 (0.68, 1.80) | <0.001 | 0.0 | 9.52 | 0.658 | 0.431 | 0.951 |
| LVESD (mm) | 11 | 396/234 | 1.14 (0.47, 1.81) | 0.001 | 0.0 | 7.31 | 0.696 | 0.722 | 1.00 |
| LVM | 6 | 304/128 | 35.34 (20.67, 50.00) | <0.001 | 79.1 | 66.05 | <0.001 | 0.914 | 0.917 |
| LVEF (%) | 15 | 710/394 | −3.01 (−1.90, −0.79) | 0.001 | 64.7 | 39.72 | <0.001 | 0.048 | 0.038 |
| LAD | 7 | 311/157 | 2.13 (1.48, 2.77) | <0.001 | 2.2 | 6.13 | 0.408 | 0.072 | 0.05 |
| LAVI | 3 | 159/69 | 3.96 (3.32, 4.61) | <0.001 | 0.0 | 1.62 | 0.445 | 0.735 | 1.000 |
OSAS obstructive sleep apnea syndrome, LVEDD left ventricular diastolic diameter, LVESD left ventricular systolic diameter, LVM left ventricular mass, LVMI left ventricular mass index, LVEF LV ejection fraction, E early diastolic peak flow velocity, A late diastolic peak flow velocity, CI confidence interval
Left ventricular structure
The parameters LVEDD, LVESD, and LVM were used to assess LV structure.
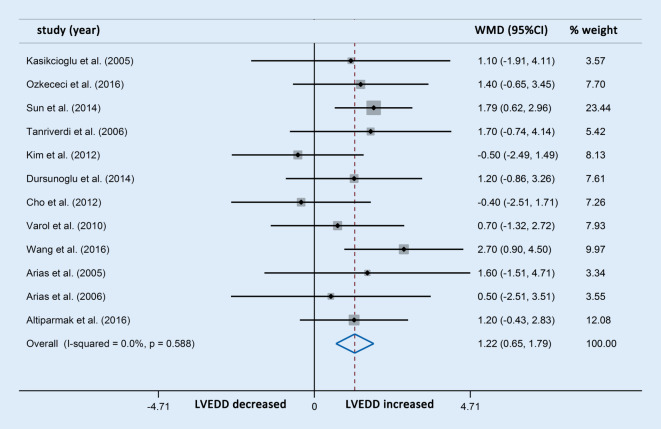
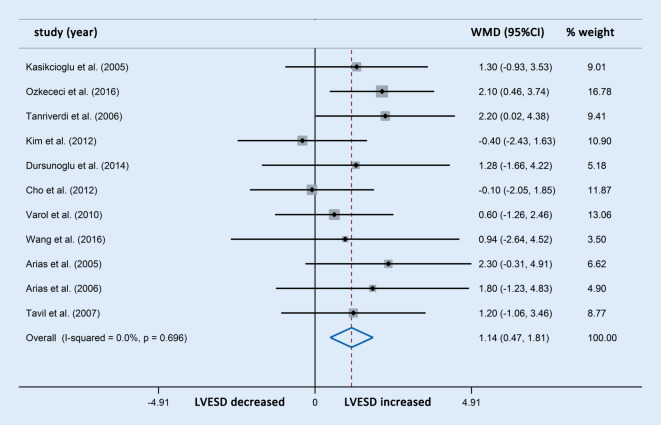
Differences in LVEDD were reported in 13 studies involving 563 OSAS patients and 319 control participants. The meta-analysis showed that the LVEDD in patients with OSAS was significantly higher compared with the controls (WMD [95% CIs]: 1.24 [0.68, 1.80]; p < 0.001; nonsignificant heterogeneity; Fig. 2). In addition, differences in LVESD were reported in 11 studies involving 396 OSAS patients and 243 control participants, which showed that patients with OSAS also had significantly increased LVESD compared with the controls (WMD [95% CIs]: 1.14 [0.47, 1.81]; p = 0.001; nonsignificant heterogeneity; Fig. 3). The subgroup analysis was not performed owing to the limited number of studies with OSAS stratification.
Fig. 2.
Forest plot of the differences in left ventricular end diastolic diameter (LVEDD) between the patients with obstructive sleep apnea syndrome and healthy controls based on echocardiography. WMD weighted mean difference
Fig. 3.
Forest plot of the differences in left ventricular end-systolic diameter (LVESD) between the patients with obstructive sleep apnea syndrome and healthy controls based on echocardiography. WMD weighted mean difference
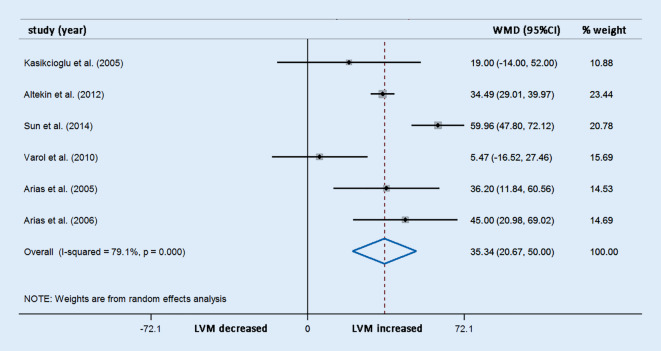
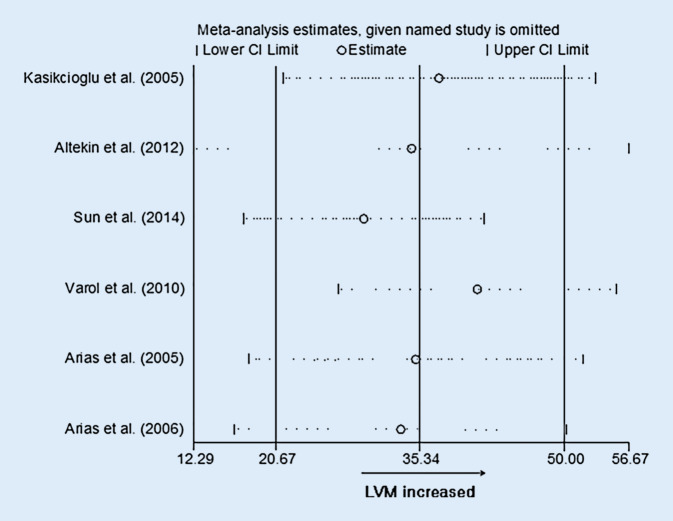
Differences in LVM were reported in six studies involving 304 OSAS patients and 128 control participants. The meta-analysis demonstrated that the LVM (WMD [95% CIs]: 35.34 [20.67, 50.00]; p < 0.001; Fig. 4) was significantly elevated compared with the controls. However, potential evidence of significant heterogeneity was detected, and thus sensitivity analysis was conducted. After exclusion of each study from the pooled analysis, the WMDs were always >0, which confirmed the reliability of these results (Fig. 5).
Fig. 4.
Forest plot of the differences in left ventricular mass (LVM) between patients with obstructive sleep apnea syndrome patients and healthy controls based on echocardiography. WMD weighted mean difference
Fig. 5.
Sensitivity analyses of left ventricular mass (LVM). CI confidence interval
Left ventricular function
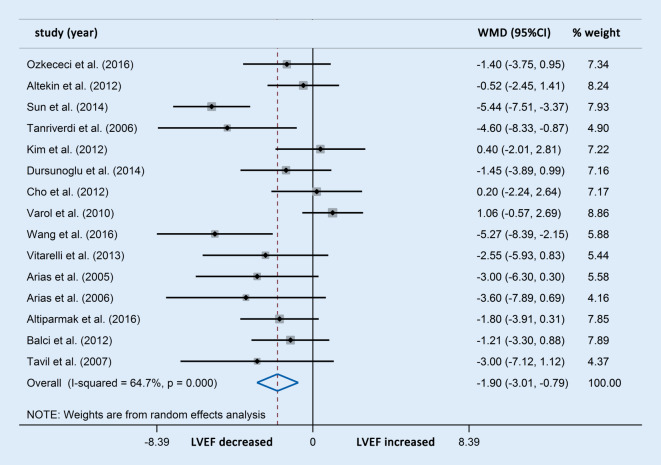
Left ventricular ejection fraction was used to assess LV systolic function and LV diastolic function. Differences in LVEF were reported in 15 studies involving 710 OSAS patients and 394 control participants. The LVEF in patients with OSAS decreased significantly compared with the controls (WMD [95% CIs]: −3.01 [−1.90, −0.79]; p < 0.001; Fig. 6).
Fig. 6.
Forest plot of the differences in left ventricular ejection fraction (LVEF) between patients with obstructive sleep apnea syndrome and healthy controls based on echocardiography. WMD weighted mean difference
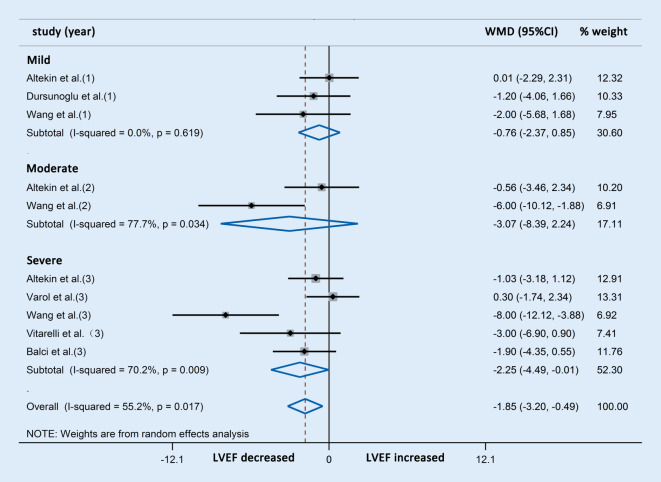
Further subgroup analysis indicated that the reduction in LVEF was consistent with the severity of OSAS (Fig. 7).
Fig. 7.
Forest plot of the differences in left ventricular ejection fraction (LVEF) between patients with obstructive sleep apnea syndrome and healthy controls based on echocardiography (subgroup analysis). WMD weighted mean difference
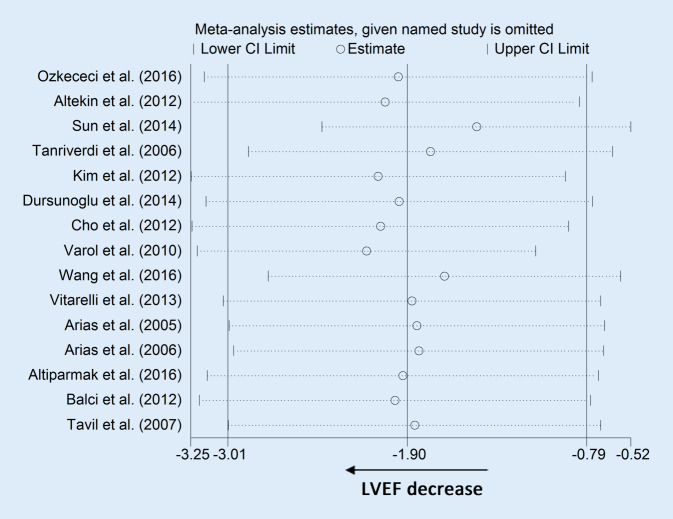
Significant heterogeneity was detected in the analysis of LVEF. However, sensitivity analysis showed that after exclusion of each study from the pooled analysis, the results were reliable (Fig. 8).
Fig. 8.
Sensitivity analyses of left ventricular ejection fraction (LVEF). CI confidence interval
Left atrial structure
The parameters LAD and LAV were used to evaluate LA structure.
Differences in LAD were reported in seven studies involving 311 OSAS patients and 157 control participants. The meta-analysis showed that the LAD in patients with OSAS was significantly higher than in the control group (WMD [95% CIs]: 2.13 [1.48, 2.77]; p < 0.001; nonsignificant heterogeneity; Fig. 9). The LAVI was also compared through an analysis of four studies comprising 184 OSAS patients and 93 control participants. Owing to apparent heterogeneity, sensitivity analysis was conducted and one study was accordingly removed. The three studies finally selected involving 159 OSAS patients and 69 control participants showed that patients with OSAS also had significantly increased LAVI compared with the controls (WMD [95% CIs]: 3.96 [3.32, 4.61]; p < 0.001; nonsignificant heterogeneity; Fig. 10). Neither subgroup analysis of the LAD nor of the LAVI was performed because of the limited number of studies with OSAS stratification.
Fig. 9.
Forest plot of the differences in left atrial diameter (LAD) between patients with obstructive sleep apnea syndrome and healthy controls based on echocardiography. WMD weighted mean difference
Fig. 10.
Forest plot of the differences in left atrial diameter volume index (LAVI) between patients obstructive sleep apnea syndrome and healthy controls based on echocardiography. WMD weighted mean difference
Discussion
Main findings
To our knowledge, this is the first meta-analysis to systematically evaluate changes in left cardiac structure and function in OSAS patients. Particularly, the effect of systemic hypertension was eliminated in the current analysis by excluding those studies with hypertensive patients enrolled, since many ultrasonic parameters may be affected by hypertension. Thus, we demonstrate that OSAS induces cardiac abnormality independent of systemic hypertension. Finally, 17 case–control studies were included in this meta-analysis with a total of 747 patients with OSAS and 426 controls.
We found that alterations in the echocardiographic parameters of LV and LA remodeling, including an increase in LVEDD, LVESD, LVM, LAD, and LAVI, were important features in OSA patients without major comorbidities, which indicated that OSAS resulted in enlargement and hypertrophy of the left ventricle and atrium. Moreover, significant decreases in LVEF were observed in OSAS patients. It should be noted that the alterations in LVEF seemed not to be remarkable enough to induce obvious clinical symptoms of LV dysfunction.
In the analysis of LVEF, we found significant heterogeneity between studies. The heterogeneity is to be expected given the variation in disease severity. However, subgroup analysis still showed significant heterogeneity, which may stem from the variety of studies conducted by different teams at various geographic locations as well as the differences in the patient populations.
LV remodeling and dysfunction in OSAS patients
It has been reported that intermittent hypoxia could induce LV remodeling, which was regarded as the basis of LV dysfunction caused by OSAS [15]. Although the negative effect of intermittent hypoxia on the cardiovascular system has not been completely clarified, multiple putative mechanisms including sympathetic overactivation, oxidative stress, inflammation, metabolic deregulation, and endothelial dysfunction have been suggested to be involved.
Hypoxemia, hypercapnia, and acidosis, induced by chronic intermittent hypoxia in OSAS patients, could activate the sympathetic nervous system. Prior studies showed that patients with metabolic syndrome and comorbid OSAS have a higher sympathetic drive than do patients with metabolic syndrome without OSAS [22, 49]. Furthermore, Scala et al. reported a significant correlation between OSAS and cardiac adrenergic impairment in patients with heart failure [43]. The exposure to intermittent hypoxia and hypercapnia, elicited by OSAS, increases muscle sympathetic nerve activity (MSNA) acutely during sleep [10], and the over-activation of the sympathetic nervous system is persistent even after removal of the hypoxic stimulus [4, 54]. Bradley et al. reported that LV transmural pressure was increased in response to the generation of negative intrathoracic pressure (Pit) and the elevation of systemic blood pressure secondary to hypoxia-induced sympathetic nervous system activation [11]. This results in the reduction of LV preload and increased afterload, which can directly affect LV systolic function [26]. The combination of increased LF afterload and increased heart rate (HR) promotes myocardial oxygen demand, thus brings a higher risk of cardiac ischemia and arrhythmias, and chronically contributes to LV hypertrophy and failure. It is well known that the sympathetic nervous system is the most prominent among neurohormonal mechanisms in HF, which pushes the heart to work at an overloaded level, and confers significant toxicity to the failing heart and increases morbidity and mortality in chronic decompensated HF [32].
In addition, systemic inflammation triggered by OSAS plays an important role in intermittent hypoxia-induced LV remodeling, as was confirmed by elevated plasma levels of tumor necrosis factor-alpha (TNF-α) and interleukin‑6 (IL-6) in patients with OSA [34]. Inflammatory response and free radical generation could cause an imbalance between myocardial oxidation and antioxidant activity, result in myocardial injury, and increase susceptibility to myocardial ischemia [19]. The consequent myocardial ischemia leads to a shortage in ATP production, inorganic phosphate accumulation, and myocardial acidosis, which inhibit excitement–contraction coupling and cause regional ventricular systolic dysfunction [40]. Besides, in the case of OSAS, exposure to intermittent hypoxia elevates blood pressure, and thus may induce functional, mechanical, and structural changes in the aortic wall in response to hemodynamic and biomechanical stress, which has been verified in mice [12]. Hypoxia stimulates the elastic fiber network with disorganization, fragmentation, and estrangement between the endpoints of disrupted fibers, and induces collagen and mucoid interlaminar accumulation in the extracellular matrix as well as LF perivascular fibrosis. These cardiovascular remodeling events induced by hypoxia were normalized after continuous positive airway pressure (CPAP) treatment.
The hemodynamic changes associated with obesity might contribute to the increased LV mass observed in patients with OSA. Of interest, Parisi et al. have pointed out that HF patients with sleep disordered-breathing have higher epicardial adipose tissue (EAT) thickness values than do HF patients without nocturnal apneas [39], which indicates EAT might be a pathophysiological link between OSAS and increased cardiovascular risk [31, 33]. Besides, CPAP therapy reduces EAT and significantly ameliorates cardiometabolic parameters in obese OSAS patients [29]. Moreover, EAT is a source of several adipocytokines and directly affects the myocardium through vasocrine and paracrine mechanisms [24]. Exposure to hypoxia leads to higher production of factor-1a and Fos-like antigen (FOSL) 2, resulting in up-regulation of leptin expression in the EAT, along with increased vascularization, inflammation, and fibrosis [16]. It has been demonstrated that EAT thickness has a high correlation with sympathetic nervous system hyperactivity and it is a local source of catecholamines in HF patients, which suggests sympathetic nervous system hyperactivity is a potential pathophysiological link between sleep apneas and EAT in HF [38].
Overall, increased sympathetic activity, endothelial dysfunction, systemic inflammation, oxidative stress, and metabolic anomalies induced by intermittent hypoxia play major roles in the progression of LV remodeling and dysfunction.
LA remodeling in OSAS patients
Our analysis revealed a significant increase in LA volume in patients with OSAS. Left atrial enlargement was considered to occur owing to elevated LV pressure and diastolic dysfunction. Sympathetic activation, decreased parasympathetic tone, and inflammation associated with intermittent hypoxia might contribute to atrial structural and electrical remodeling.
It should be noted that recent evidence has indicated OSAS patients might be predisposed to the development and recurrence of atrial fibrillation [48]. The forced inspiration-induced acute LA dilation related to diastolic dysfunction may be an important component of the arrhythmogenic substrate for atrial fibrillation during sleep apnea episodes [9, 25]. More explorations of treatment for OSAS, such as CPAP, are expected to alter the anticipated frequency of OSAS-related cardiac arrhythmias.
RV remodeling and dysfunction in OSAS patients
The correlation between OSAS and right ventricular (RV) remodeling and dysfunction has also raised intense interest from researchers, but the conclusions from various have differed. Yang et al. found the inner diameters and the anterior wall thickness of the RV were increased in patients with severe OSAS and deteriorated as the disease course progressed [55]. Vitarelli et al. reported that RV dilatation and dysfunction were significantly associated with AHI and the severity and frequency of apnea episodes [52]. Similarly, several other studies reported that OSAS patients presented with right cardiac dysfunction [1, 30]. By contrast, other studies did not reveal any significant changes in RV morphology and function in OSA patients [14, 17].
Several mechanisms were raised to illustrate the potential relationship between OSAS and RV changes. Prior studies suggested that permanent pulmonary hypertension was an important factor. Repetitive nocturnal arterial oxygen desaturation and hypercapnia lead to pulmonary vascular endothelium remodeling and vasoconstriction, thus increasing pulmonary artery pressure [42], leading to RV overload and inducing the release of inflammatory factors. As a result, the compensatory hypertrophic RV gradually presents with dysfunction. However, recent studies pointed out that RV alternations occurred in early stage of OSAS in the absence of pulmonary hypertension [30, 52], indicating that pulmonary hypertension was not the only cause. Some other studies reported the intrathoracic negative pressure against an occluded airway increased venous return and volume overload, and consequently expanded and remodeled the RV [1]. Another possible mechanism is that intermittent hypoxia and CO2 retention stimulated central and peripheral chemoreceptors and increased sympathetic nerve activity, which induced RV dysfunction. In addition, LV dysfunction induced by OSAS may also lead to RV dysfunction, since there is a close anatomical association between the two ventricles [35].
Since the effects of OSAS on the LV and RV may be different, we should conduct further analyses to uncover the precise correlation and mechanism between OSAS and RV remodeling and dysfunction.
Limitations
The present study was a clinical observational study. The follow-up time was not controlled. In our opinion, the duration of OSAS might be a relevant factor when assessing the effect of OSAS on cardiac structure and function, but it is very difficult to assess the duration of OSAS owing the rate of missed diagnoses in the clinic. Besides, this analysis involved no outcome data such as survival rate and risk of cardiovascular events during follow-up. Further research is needed to clarify the effect of OSAS on the long-term prognosis of patients. Additional analyses may identify the correlation and precise mechanisms between OSAS and RV remodeling.
Conclusion
On the basis of this meta-analysis, we conclude that patients with obstructive sleep apnea syndrome (OSAS) display increased left atrial dilatation and left ventricular (LV) hypertrophy and dilatation, along with impaired LV systolic function. Therefore, more emphasis should be placed on the clinical significance of OSAS in cardiovascular risk. Treatment against OSAS such as continuous positive airway pressure can attenuate sleep apnea and might prevent the decrease in LV ejection fraction in the long term.
Caption Electronic Supplementary Material
Supplementary Table S1. Search Strategy.
Supplementary Table S3. Quality of included studies.
Acknowledgments
Funding
There was no funding source for this study. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author Contribution
Fan Jiaqi and Li Huajun searched the scientific literature. Yu Lei conducted the statistical analyses, participated in data interpretation, drafted the report, and conceived the study. Zhu Qifeng revised the paper.
Compliance with ethical guidelines
Conflict of interest
L. Yu, H. Li, X. Liu, J. Fan, Q. Zhu, J. Li, J. Jiang, and J. Wang declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. The current systematic review and meta-analysis was based on previously published studies with the informed consent of participants prior to inclusion.
References
- 1.Altekin RE, Karakas MS, Yanikoglu A, Ozel D, et al. Determination of right ventricular dysfunction using the speckle tracking echocardiography method in patients with obstructive sleep apnea. Cardiol J. 2012;19:130–139. doi: 10.5603/CJ.2012.0024. [DOI] [PubMed] [Google Scholar]
- 2.Altekin RE, Yanikoglu A, Baktir AO, et al. Assessment of subclinical left ventricular dysfunction in obstructive sleep apnea patients with speckle tracking echocardiography. Int J Cardiovascular Imaging. 2012;28(8):1917–1930. doi: 10.1007/s10554-012-0026-4. [DOI] [PubMed] [Google Scholar]
- 3.Altıparmak IH, et al. Relation of elastic properties of pulmonary artery with left ventricular abnormalities and aortic stiffness in patients with moderate to severe obstructive sleep apnea: A cross-sectional echocardiographic study. Turk Kardiyol Dern Ars. 2016;44(4):289–299. doi: 10.5543/tkda.2015.67862. [DOI] [PubMed] [Google Scholar]
- 4.Arabi Y, Morgan BJ, Goodman B, Puleo DS, et al. Daytime blood pressure elevation after nocturnal hypoxia. J. Appl. Physiol. 1999;87:689–698. doi: 10.1152/jappl.1999.87.2.689. [DOI] [PubMed] [Google Scholar]
- 5.Arias MA, García-Rí F, Alonso-Fernández A, et al. Obstructive Sleep Apnea Syndrome Affects Left Ventricular Diastolic Function. Circulation. 2005;112(3):375–383. doi: 10.1161/CIRCULATIONAHA.104.501841. [DOI] [PubMed] [Google Scholar]
- 6.Arias MA, García-Río F, Alonso-Fernández A, et al. Pulmonary hypertension in obstructive sleep apnoea: effects of continuous positive airway pressure. Eur Heart J. 2006;27(9):1106–1113. doi: 10.1093/eurheartj/ehi807. [DOI] [PubMed] [Google Scholar]
- 7.Arnardottir ES, Bjornsdottir E, Olafsdottir KA, Benediktsdottir B, et al. Obstructive sleep apnoea in the general population: highly prevalent but minimal symptoms. Eur Respir J. 2016;47:194–202. doi: 10.1183/13993003.01148-2015. [DOI] [PubMed] [Google Scholar]
- 8.Balci MM, Arslan U, Firat H, et al. Serum Levels of Adipocyte Fatty Acid–Binding Protein Are Independently Associated With Left Ventricular Mass and Myocardial Performance Index in Obstructive Sleep Apnea Syndrome. J Investig Med. 2015;60(7):1020–1026. doi: 10.2310/JIM.0b013e31826868f2. [DOI] [PubMed] [Google Scholar]
- 9.Baranchuk A, Simpson CS, Redfearn DP, Fitzpatrick M. It’s time to wake up! Sleep apnea and cardiac arrhythmias. Europace. 2008;10:666–667. doi: 10.1093/europace/eun078. [DOI] [PubMed] [Google Scholar]
- 10.Bradley TD, Floras JS. Sleep apnea and heart failure: part I: obstructive sleep apnea. Circulation. 2003;107:1671–1678. doi: 10.1161/01.cir.0000061757.12581.15. [DOI] [PubMed] [Google Scholar]
- 11.Bradley TD, Floras JS. Sleep apnea and heart failure: part II: central sleep apnea. Circulation. 2003;107:1822–1826. doi: 10.1161/01.cir.0000061758.05044.64. [DOI] [PubMed] [Google Scholar]
- 12.Castro-Grattoni AL, Alvarez-Buve R, Torres M, Farre R, et al. Intermittent hypoxia-induced cardiovascular remodeling is reversed by Normoxia in a mouse model of sleep apnea. Chest. 2016;149:1400–1408. doi: 10.1016/j.chest.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 13.Cho KI, Kwon JH, Kim SM, et al. Impact of Obstructive Sleep Apnea on the Global Myocardial Performance Beyond Obesity. Echocardiography. 2012;29(9):1071–1080. doi: 10.1111/j.1540-8175.2012.01762.x. [DOI] [PubMed] [Google Scholar]
- 14.D’andrea A, Martone F, Liccardo B, Mazza M, et al. Acute and chronic effects of Noninvasive ventilation on left and right myocardial function in patients with obstructive sleep apnea syndrome: a speckle tracking Echocardiographic study. Echocardiography. 2016;33:1144–1155. doi: 10.1111/echo.13225. [DOI] [PubMed] [Google Scholar]
- 15.Dematteis M, Julien C, Guillermet C, Sturm N, et al. Intermittent hypoxia induces early functional cardiovascular remodeling in mice. Am J Respir Crit Care Med. 2008;177:227–235. doi: 10.1164/rccm.200702-238OC. [DOI] [PubMed] [Google Scholar]
- 16.Drosos I, Chalikias G, Pavlaki M, Kareli D, et al. Differences between perivascular adipose tissue surrounding the heart and the internal mammary artery: possible role for the leptin-inflammation-fibrosis-hypoxia axis. Clin Res Cardiol. 2016;105:887–900. doi: 10.1007/s00392-016-0996-7. [DOI] [PubMed] [Google Scholar]
- 17.Dursunoglu N, Dursunoglu D, Kilic M. Impact of obstructive sleep apnea on right ventricular global function: sleep apnea and myocardial performance index. Respiration. 2005;72:278–284. doi: 10.1159/000085369. [DOI] [PubMed] [Google Scholar]
- 18.Epstein LJ, Kristo D, Strollo PJ, Jr, Friedman N, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. JCSM. 2009;5:263. doi: 10.5664/jcsm.27497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feng J, Zhang D, Chen B. Endothelial mechanisms of endothelial dysfunction in patients with obstructive sleep apnea. Sleep Breath. 2012;16:283–294. doi: 10.1007/s11325-011-0519-8. [DOI] [PubMed] [Google Scholar]
- 20.Ferini-Strambi L, Fantini ML, Castronovo C. Epidemiology of obstructive sleep apnea syndrome. Minerva Med. 2004;95:187–202. [PubMed] [Google Scholar]
- 21.Franklin KA, Sahlin C, Stenlund H, Lindberg E. Sleep apnoea is a common occurrence in females. Eur Respir J. 2013;41:610–615. doi: 10.1183/09031936.00212711. [DOI] [PubMed] [Google Scholar]
- 22.Grassi G, Seravalle G, Quarti-Trevano F, Mineo C, et al. Reinforcement of the adrenergic overdrive in the metabolic syndrome complicated by obstructive sleep apnea. J Hypertens. 2010;28:1313–1320. doi: 10.1097/HJH.0b013e328337a9. [DOI] [PubMed] [Google Scholar]
- 23.Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3:310–318. doi: 10.1016/s2213-2600(15)00043-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iacobellis G, Corradi D, Sharma AM. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med. 2005;2:536–543. doi: 10.1038/ncpcardio0319. [DOI] [PubMed] [Google Scholar]
- 25.Iwasaki YK, Shi Y, Benito B, Gillis MA, et al. Determinants of atrial fibrillation in an animal model of obesity and acute obstructive sleep apnea. Heart Rhythm. 2012;9:1409–1416.e1401. doi: 10.1016/j.hrthm.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 26.Jean-Louis G, Zizi F, Brown D, Ogedegbe G, et al. Obstructive sleep apnea and cardiovascular disease: evidence and underlying mechanisms. Minerva Pneumol. 2009;48:277–293. [PMC free article] [PubMed] [Google Scholar]
- 27.Kasikcioglu HA, Karasulu L, Durgun E, et al. Aortic elastic properties and left ventricular diastolic dysfunction in patients with obstructive sleep apnea. Heart Vessels. 2005;20(6):239–244. doi: 10.1007/s00380-005-0839-3. [DOI] [PubMed] [Google Scholar]
- 28.Kim SM, Cho KI, Kwon JH, et al. Impact of obstructive sleep apnea on left atrial functional and structural remodeling beyond obesity. J Cardiol. 2012;60(6):475–483. doi: 10.1016/j.jjcc.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 29.Kostopoulos K, Alhanatis E, Pampoukas K, Georgiopoulos G, et al. CPAP therapy induces favorable short-term changes in epicardial fat thickness and vascular and metabolic markers in apparently healthy subjects with obstructive sleep apnea-hypopnea syndrome (OSAHS) Sleep Breath. 2016;20:1–11. doi: 10.1007/s11325-015-1236-5. [DOI] [PubMed] [Google Scholar]
- 30.Li J, Wang Z, Li Y, Meng Y, et al. Assessment of regional right ventricular systolic function in patients with obstructive sleep apnea syndrome using velocity vector imaging. Medicine. 2016;95:e4788–e4788. doi: 10.1097/MD.0000000000004788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lubrano C, Saponara M, Barbaro G, Specchia P, et al. Relationships between body fat distribution, epicardial fat and obstructive sleep apnea in obese patients with and without metabolic syndrome. PLoS ONE. 2012;7:e47059. doi: 10.1371/journal.pone.0047059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lymperopoulos A, Rengo G, Koch WJ. Adrenergic nervous system in heart failure: pathophysiology and therapy. Circ Res. 2013;113:739–753. doi: 10.1161/circresaha.113.300308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mariani S, Fiore D, Barbaro G, Basciani S, et al. Association of epicardial fat thickness with the severity of obstructive sleep apnea in obese patients. International Journal of Cardiology. 2013;167:2244–2249. doi: 10.1016/j.ijcard.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 34.Matsumoto C, Hayashi T, Kitada K, Yamashita C, et al. Chymase plays an important role in left ventricular remodeling induced by intermittent hypoxia in mice. Hypertension. 2009;54:164–171. doi: 10.1161/hypertensionaha.109.131391. [DOI] [PubMed] [Google Scholar]
- 35.Mittal SR, Barar RV, Arora H. Echocardiographic evaluation of left and right ventricular function in mild hypertension. Int J Cardiovasc Imaging. 2001;17:263–270. doi: 10.1023/A:1011660827368. [DOI] [PubMed] [Google Scholar]
- 36.Otto ME, Belohlavek M, Romero-Corral A, et al. Comparison of Cardiac Structural and Functional Changes in Obese Otherwise Healthy Adults With Versus Without Obstructive Sleep Apnea. Am J Cardiol. 2007;99(9):1298–1302. doi: 10.1016/j.amjcard.2006.12.052. [DOI] [PubMed] [Google Scholar]
- 37.Ozkececi G, Ulasli SS, Akci O, et al. Assessment of pulmonary arterial stiffness in obstructive sleep apnea. Int J Cardiovascular Imaging. 2016;32(5):799–805. doi: 10.1007/s10554-016-0841-0. [DOI] [PubMed] [Google Scholar]
- 38.Parisi V, Rengo G, Perrone-Filardi P, Pagano G, et al. Increased Epicardial adipose tissue volume correlates with cardiac sympathetic Denervation in patients with heart failure. Circ Res. 2016 doi: 10.1161/CIRCRESAHA.115.307765. [DOI] [PubMed] [Google Scholar]
- 39.Parisi V, Paolillo S, Rengo G, Formisano R, et al. Sleep-disordered breathing and epicardial adipose tissue in patients with heart failure. Nutr Metab Cardiovasc Dis. 2017 doi: 10.1016/j.numecd.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 40.Perrelli MG, Pagliaro P, Penna C. Ischemia/reperfusion injury and cardioprotective mechanisms: role of mitochondria and reactive oxygen species. World J Cardiol. 2011;3:186–200. doi: 10.4330/wjc.v3.i6.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Phillipson EA. Sleep apnea—a major public health problem. N Engl J Med. 1993;328:1271–1273. doi: 10.1056/nejm199304293281712. [DOI] [PubMed] [Google Scholar]
- 42.Sajkov D, Mcevoy RD. Obstructive sleep apnea and pulmonary hypertension. Prog Cardiovasc Dis. 2009;51:363–370. doi: 10.1016/j.pcad.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 43.Scala O, Paolillo S, Formisano R, Pellegrino T, et al. Sleep-disordered breathing, impaired cardiac adrenergic innervation and prognosis in heart failure. Heart. 2016 doi: 10.1136/heartjnl-2015-309215. [DOI] [PubMed] [Google Scholar]
- 44.Shochat T, Pillar G. Sleep apnoea in the older adult: Pathophysiology, epidemiology, consequences and management. Drugs Aging. 2003;20:551–560. doi: 10.2165/00002512-200320080-00001. [DOI] [PubMed] [Google Scholar]
- 45.Sun Y, Yuan H, Zhao MQ, et al. Cardiac structural and functional changes in old elderly patients with obstructive sleep apnoea–hypopnoea syndrome. J Int Med Res. 2014;42(2):395–404. doi: 10.1177/0300060513502890. [DOI] [PubMed] [Google Scholar]
- 46.Tanriverdi H, Evrengul H, Kaftan A, et al. Effect of Obstructive Sleep Apnea on Aortic Elastic Parameters. Circ J. 2006;70(6):737–743. doi: 10.1253/circj.70.737. [DOI] [PubMed] [Google Scholar]
- 47.Tavil Y, Kanbay A, Sen N, et al. The Relationship Between Aortic Stiffness and Cardiac Function in Patients with Obstructive Sleep Apnea, Independently from Systemic Hypertension. J Am Soc Echocardiogr. 2007;20(4):366–372. doi: 10.1016/j.echo.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 48.Todd K, Mcintyre WF, Baranchuk A. Obstructive sleep apnea and atrial fibrillation. NSS. 2010;2:39–45. doi: 10.2147/NSS.S7625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Trombetta IC, Somers VK, Maki-Nunes C, Drager LF, et al. Consequences of comorbid sleep apnea in the metabolic syndrome—implications for cardiovascular risk. Sleep. 2010;33:1193–1199. doi: 10.1055/s-0030-1254404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Varol E, Akcay S, Ozaydin M, et al. Influence of obstructive sleep apnea on left ventricular mass and global function: sleep apnea and myocardial performance index. Heart Vessels. 2010;25(5):400–404. doi: 10.1007/s00380-009-1225-3. [DOI] [PubMed] [Google Scholar]
- 51.Vitarelli A, D’Orazio S, Caranci F, et al. Left ventricular torsion abnormalities in patients with obstructive sleep apnea syndrome: An early sign of subclinical dysfunction. Int J Cardiol. 2013;165(3):512–518. doi: 10.1016/j.ijcard.2011.09.030. [DOI] [PubMed] [Google Scholar]
- 52.Vitarelli A, Terzano C, Saponara M, Gaudio C, et al. Assessment of right ventricular function in obstructive sleep apnea syndrome and effects of continuous positive airway pressure therapy: a pilot study. Can J Cardiol. 2015;31:823–831. doi: 10.1016/j.cjca.2015.01.029. [DOI] [PubMed] [Google Scholar]
- 53.Wang D, Ma GS, Wang XY, et al. Left ventricular subclinical dysfunction associated with myocardial deformation changes in obstructive sleep apnea patients estimated by real-time 3D speckle-tracking echocardiography. Sleep Breath. 2016;20(1):135–144. doi: 10.1007/s11325-015-1197-8. [DOI] [PubMed] [Google Scholar]
- 54.Xie A, Skatrud JB, Puleo DS, Morgan BJ. Exposure to hypoxia produces long-lasting sympathetic activation in humans. J Appl Physiol. 2001;91:1555–1562. doi: 10.1152/jappl.2001.91.4.1555. [DOI] [PubMed] [Google Scholar]
- 55.Yang SQ, Han LL, Dong XL, Wang CY, et al. Mal-effects of obstructive sleep apnea on the heart. Sleep Breath. 2012;16:717–722. doi: 10.1007/s11325-011-0566-1. [DOI] [PubMed] [Google Scholar]
- 56.Young T, Palta M, Dempsey J, Skatrud J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–1235. doi: 10.1056/nejm199304293281704. [DOI] [PubMed] [Google Scholar]
- 57.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–1239. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1. Search Strategy.
Supplementary Table S3. Quality of included studies.