Abstract
Ruptures of the patellar tendon are rare but potentially devastating injuries reported to occur most commonly in active males in their third and fourth decades of life. Repair failure rates have been reported to range between 2% and 50% based on surgical technique used. There are several inherent challenges associated with revision patellar tendon repair, including quadriceps atrophy, contracture, tissue loss, excessive scarring, and improper patella height. There remains no consensus regarding ideal revision patellar tendon repair technique. The purpose of this Technical Note is to describe our preferred method for revision patellar tendon repair using suture anchors and allograft augmentation with adjustable loop suspensory fixation. On the basis of recent studies, we have carefully chosen our fixation and augmentation methods that have shown biomechanical promise, while allowing the surgeon to carefully titrate the patellar tendon length and accommodate for some patellar tendon tissue loss.
Ruptures of the patellar tendon are rare but potentially devastating injuries reported to occur most commonly in active male patients in their third and fourth decades of life.1 Classically, these injuries occur after a forceful contraction of the quadriceps against a flexed knee.2 Good outcomes have been reported following acute repair of patellar tendon injuries, although re-rupture rates ranging from 2% to 50% have been reported, depending on surgical technique used.3
There are several inherent challenges associated with revision patellar tendon repair, including quadriceps atrophy, contracture, tissue loss, excessive scarring, and improper patella height. Given these difficulties, the use of non-biologic (nonabsorbable suture, synthetic tape, or cerclage wire) and biologic (allograft, autograft tendon or dermal allograft) augments have been used.4, 5, 6, 7 However, there is no consensus regarding a preferred technique for revision patellar tendon repair.
The purpose of this Technical Note is to describe our preferred method for revision patellar tendon repair via suture anchors and allograft augmentation with adjustable-loop suspensory fixation.
Surgical Technique (With Video Illustration)
Before the procedure, lateral radiographs are obtained of both the operative and nonoperative knees. The Caton–Deschamps Index and the length of the patellar tendons of both knees are measured. The nonoperative knee Caton–Deschamps Index and patellar tendon length are used as guides to ensure revision repair results in a matched patellar tendon length and patellar height. Video 1 contains a narrated visual description of the technique.
The patient is positioned supine on the operating table with all bony prominences padded. A nonsterile tourniquet is applied and inflated throughout the case. A standard examination under anesthesia is performed. The lower extremity is prepared and draped in the usual sterile fashion. If preoperative examination and imaging indicates that there is intra-articular pathology to be addressed, a knee arthroscopy is performed at this time.
Graft Preparation
An assistant concurrently prepares a tibialis anterior allograft on the back table folded over 2 adjustable loop buttons (Fig 1). Our preferred adjustable loop button is the Stryker ProCinch (Kalamazoo, MI). The prepared graft length should be equal to the contralateral patellar tendon length plus an additional 20- to 25-mm segment for the patella socket and a 25-mm segment for the tibial socket. A surgical marking pen may be used to mark the desired length of the graft to be docked in each socket resulting in a patellar tendon length comparable to the contralateral side.
Fig 1.

The prepared tibialis anterior allograft, folded over 2 adjustable loop buttons. The prepared graft length should be equal to the contralateral patellar tendon length plus an additional 20-25 mm segment for the patella socket and a 25-mm segment for the tibial socket.
Surgical Approach
A 10- to 15-cm longitudinal incision is made over the patella, preferably through the patient’s previous incision. Dissection is carried down through skin and subcutaneous tissues. Care is taken to develop full-thickness medial and lateral subcutaneous flaps to aid in closure. The pre-patellar bursa is often hypertrophic, and debridement improves visualization. The medial and lateral borders of the tendon are defined, and the tendon is freed from the underlying fat pad. Any remnant patellar tendon is freed from the inferior patella. A midline longitudinal split is made in the native patellar tendon for later midline inlay of the prepared allograft (Fig 2). Hardware and suture from the previous repair are then removed. Heterotopic ossification (HO), which is often present in the revision setting, should also be identified and removed. The interface between the native patella and HO often can be palpated, and the HO is removed. Fluoroscopy may be used to confirm that the HO is completely excised. The inferior pole of the patella is then decorticated to create a bleeding bony bed to facilitate tendon to bone healing.
Fig 2.

With the patient supine, the medial and lateral borders of the right knee patellar tendon are defined, and the tendon is freed from the underlying fat pad. Any remnant patellar tendon is freed from the inferior patella. A midline longitudinal split is made in the native patellar tendon for midline inlay of the prepared allograft.
Next, a large medial subcutaneous flap is created for exposure of the medial tibia. The sartorial fascia is then incised longitudinally and the medial head of the gastrocnemius and soleus muscles are bluntly elevated from the posterior tibia. A blunt retractor is placed around the posterior tibia to protect neurovascular structures when drilling.
Tibia and Patella Preparation
A Beath pin is then placed from distal to proximal through the patella. Care is taken to place the pin midway between the anterior cortex and the articular surface to avoid damage to the articular cartilage. Proper location can be confirmed fluoroscopically. A button drill bit is used to drill over the Beath pin bicortically, and a 25-mm depth socket is drilled from distal to proximal based on the diameter of the allograft. A passing suture is placed.
With the posterior tibial retractor in place, a Beath pin is advanced bicortically through the tibia from anterior to posterior, starting at the center of the patellar tendon insertion and aiming slightly medial. A button drill bit is then used to drill over the Beath pin. A socket for the allograft is drilled to a length of approximately 40 mm. Bony debris is irrigated from the socket, and a Hewson suture passer (Smith and Nephew, Watford, United Kingdom) is used to pass a passing suture through the socket from anterior to posterior.
Allograft Augmentation and Patellar Tendon Repair
The previously prepared tibialis anterior graft is docked in the patellar socket to a depth of 20 mm (Fig 3), and the opposite end is docked in the tibia to the predetermined depth to provide the appropriate length of the patellar tendon. Both buttons are flipped and the knee is cycled in flexion and extension to remove graft creep. Final tensioning with the adjustable loops is performed in full extension on both the patellar and tibial sides (Fig 4). Fluoroscopic images are obtained (Fig 5) and compared with the preoperative contralateral knee images to ensure comparable patellar height.
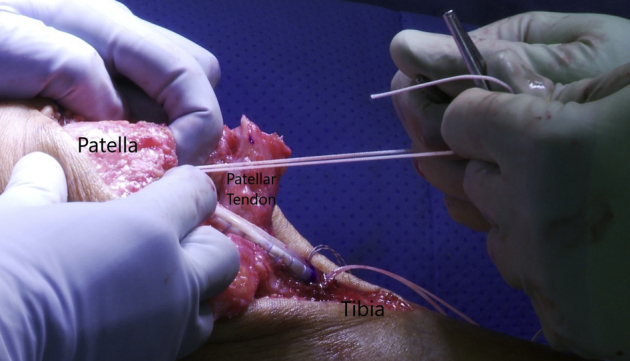
Fig 3.

With the patient supine, the previously prepared tibialis anterior graft is docked in the right knee patellar socket to a depth of 20 mm. A circumferential mark may be placed 20 mm from the graft tip to guide the surgeon in docking the appropriate graft length.
Fig 4.
With the patient supine, final tensioning of the allograft is performed with the adjustable loops while the right knee is in full extension. Tensioning is performed on both the patellar and tibial sides, to advance the graft in each socket. The adjustable loops may be wrapped around 2 Kochers to assist in tensioning.
Fig 5.

Lateral fluoroscopic image of the right knee is performed to confirm both buttons (proximal patellar button and posterior tibial button) are engaged at the cortex and the repair results in appropriate patellar height and patellar tendon length.
Two additional anchors loaded with nonabsorbable suture are placed into the inferior pole of the patella; one medial and one lateral to the socket containing the allograft. Our preferred anchors are the Stryker 2.3-mm Iconix anchor (Kalamazoo, MI). The nonabsorbable suture is used to repair any remaining native proximal tendon back to the patella. The wound is then copiously irrigated, and the retinaculum on the medial and lateral borders of the tendon is repaired with figure of 8 interrupted #1 VICRYL suture. The final repair construct is presented in Figure 6.
Fig 6.
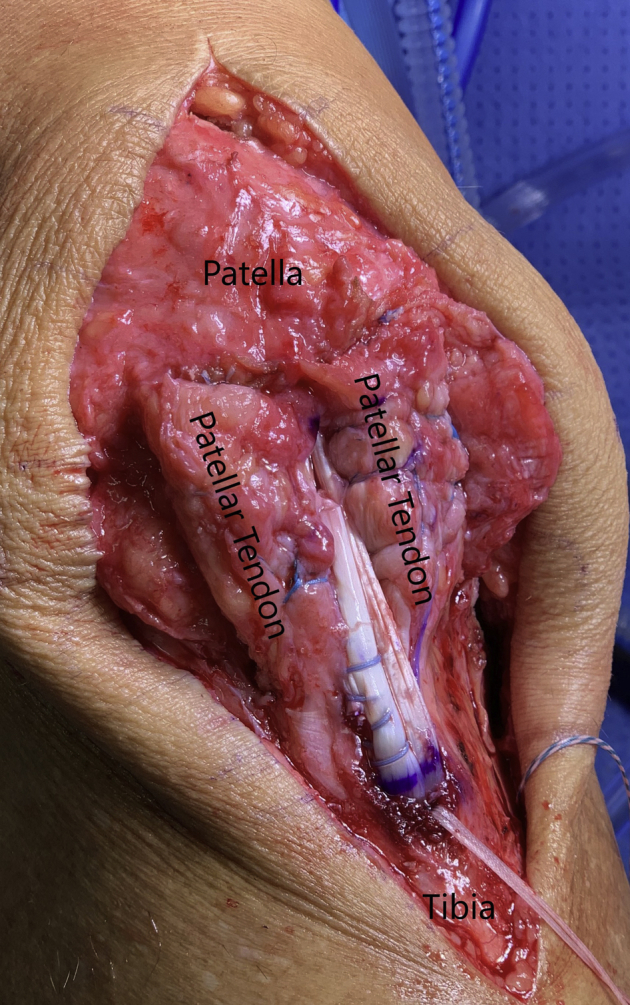
The final right knee patellar tendon repair construct with the allograft inlay positioned centrally within the longitudinal native patellar tendon split. Both ends of the allograft are docked; one in the patella, the other in the tibia. The native patellar tendon is repaired back to the distal pole of the patella with suture anchors. The patient is supine with the knee extended.
The tourniquet is deflated and hemostasis is obtained. The wound is closed in layers, and a sterile dressing with a well-padded cylinder cast is applied with the knee in full extension. Procedural pearls and pitfalls are presented in Table 1. Advantages and disadvantages of this surgical technique are presented in Table 2.8,9
Table 1.
Procedural Pearls and Pitfalls
Pearls
|
Pitfalls
|
Table 2.
Technique Advantages and Disadvantages
Advantages
|
Disadvantages
|
Rehabilitation
The patient is allowed to weight bear as tolerated with the operative knee immobilized in full extension with a cylinder cast for 2 weeks. The cast is removed at 2 weeks, and the patient is transitioned into a hinged knee brace locked in full extension. A continuous passive motion device is used starting at week 5 with range of motion (ROM) 0 to 30°, and increasing flexion by 4 to 6° daily until week 6. At week 6, formal physical therapy is initiated, focusing on gait training and knee flexion to a goal of 90°. At week 8, the patient is weaned from the brace and ROM is increased to 0 to 120°. At week 10, the patient may progress to ROM as tolerated. Blood flow restriction may be used for quadriceps recruitment. Gentle strengthening begins at week 12. Running may begin at 6 months, with gradual return to full activity at seven months.
Discussion
The incidence of patellar tendon rupture is rare, and it is reported to be the third most common injury to the extensor mechanism of the knee after patella fracture and quadriceps tendon rupture.2,10 Rupture most commonly occurs at the inferior pole of the patella where a higher tensional load is applied; mid-substance failure and failure at the tibial tuberosity are less common.11,12 Several risk factors for patellar tendon rupture have been reported, including the use of patellar tendon corticosteroid injections,13 repetitive microtrauma (jumper’s knee),14,15 previous patellar tendon autograft harvest,16,17 and comorbidities such as rheumatoid arthritis,18 diabetes, and renal disease.19,20
Failed acute patellar tendon repairs have been reported to occur in 2% to 50% of patients, depending on surgical technique used.3 Gilmore et al.3 reported an average failure rate of 8% among all techniques. Failure may be, in part, due to the poor blood supply to this tissue and high mechanical loads placed upon the patellar tendon; however, technique also plays a significant role.3,21 Primary repair with transosseous sutures remains common, although this technique has been reported to result in increased gap formation at the repair site due to repetitive loading or a single loading event.22 In biomechanical testing, patellar tendon repair with suture anchors yielded significantly less gap formation during cyclic loading and resisted significantly higher ultimate failure loads compared with transosseous sutures.8 Several authors also have proposed repair augmentation with allograft, autograft, or synthetics in an effort to decrease strain across the repair site, allow early knee motion, and reduce the risk of re-rupture.23, 24, 25, 26, 27, 28 On the basis of the aforementioned studies, we have carefully chosen our fixation and augmentation methods that have shown biomechanical promise.9
This technique is not without limitations. Further study is needed comparing the proposed revision technique to others to fully assess its clinical efficacy. Furthermore, there is potential for neurovascular injury when drilling through the tibia from anterior to posterior for placement of the cortical button. However, the described technique has been carefully detailed in this Technical Note to assist surgeons in avoiding this risk through meticulous dissection and placement of posterior retractors. We hypothesize that this technique allows for substantial improvement in strength of the revision repair construct and allows for precise titration of patellar tendon length while accommodating for some patellar tendon tissue loss.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.F.V. reports personal fees from Arthrex, Smith & Nephew, and Stryker, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
A right knee revision patellar tendon repair is performed using suture anchors, allograft augmentation, and adjustable loop suspensory fixation. The patient is positioned supine and a diagnostic right knee arthroscopy is performed, and any intra-articular pathology is addressed. Through a midline longitudinal incision at the knee, the allograft tendon is positioned in a midline split through the native patellar tendon and secured in bone sockets in the patella and tibia with adjustable loop buttons. Remnant patellar tendon is repaired to the inferior pole of the patella with suture anchors.
References
- 1.Khurana A., Samseier L.E., Heinzelmann M. Quadriceps and patellar tendon rupture [Injury 2006;37:516-19] Injury. 2007;38:1327–1328. doi: 10.1016/j.injury.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 2.Siwek C.W., Rao J.P. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am. 1981;63:932–937. [PubMed] [Google Scholar]
- 3.Gilmore J.H., Clayton-Smith Z.J., Aguilar M., Pneumaticos S.G., Giannoudis P.V. Reconstruction techniques and clinical results of patellar tendon ruptures: Evidence today. Knee. 2015;22:148–155. doi: 10.1016/j.knee.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Meyer Z., Ricci W.M. Knee extensor mechanism repairs: Standard suture repair and novel augmentation technique. J Orthop Trauma. 2016;30(suppl 2):S30–S31. doi: 10.1097/BOT.0000000000000604. [DOI] [PubMed] [Google Scholar]
- 5.Larson R.V., Simonian P.T. Semitendinosus augmentation of acute patellar tendon repair with immediate mobilization. Am J Sports Med. 1995;23:82–86. doi: 10.1177/036354659502300114. [DOI] [PubMed] [Google Scholar]
- 6.Shelbourne K.D., Darmelio M.P., Klootwyk T.E. Patellar tendon rupture repair using Dall-Miles cable. Am J Knee Surg. 2001;14:17–20. [PubMed] [Google Scholar]
- 7.Lindy P.B., Boynton M.D., Fadale P.D. Repair of patellar tendon disruptions without hardware. J Orthop Trauma. 1995;9:238–243. doi: 10.1097/00005131-199506000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Ettinger M., Dratzidis A., Hurschler C. Biomechanical properties of suture anchor repair compared with transosseous sutures in patellar tendon ruptures: A cadaveric study. Am J Sports Med. 2013;41:2540–2544. doi: 10.1177/0363546513500633. [DOI] [PubMed] [Google Scholar]
- 9.Ode G.E., Piasecki D.P., Habet N.A., Peindl R.D. Cortical button fixation: A better patellar tendon repair? Am J Sports Med. 2016;44:2622–2628. doi: 10.1177/0363546516651614. [DOI] [PubMed] [Google Scholar]
- 10.McGrory J.E. Disruption of the extensor mechanism of the knee. J Emerg Med. 2003;24:163–168. doi: 10.1016/s0736-4679(02)00719-9. [DOI] [PubMed] [Google Scholar]
- 11.Rudig L., Ahlers J., Lengsfeld M., Behandlung M.R. Ergebnisse nach Rupturen des Ligamentum patellae. Unfallchirurgie. 1993;19:214–220. doi: 10.1007/BF02588057. [DOI] [PubMed] [Google Scholar]
- 12.Kelly D.W., Carter V.S., Jobe F.W., Kerlan R.K. Patellar and quadriceps tendon ruptures—jumper’s knee. Am J Sports Med. 1984;12:375–380. doi: 10.1177/036354658401200508. [DOI] [PubMed] [Google Scholar]
- 13.Unverferth L.J., Olix M.L. The effect of local steroid injections on tendon. Am J Sports Med. 1973;1:31–37. doi: 10.1177/036354657300100404. [DOI] [PubMed] [Google Scholar]
- 14.Karlsson J., Lundin O., Lossing I.W., Peterson L. Partial rupture of the patellar ligament. Results after operative treatment. Am J Sports Med. 1991;19:403–408. doi: 10.1177/036354659101900415. [DOI] [PubMed] [Google Scholar]
- 15.Rosenberg J.M., Whitaker J.H. Bilateral infrapatellar tendon rupture in a patient with jumper’s knee. Am J Sports Med. 1991;19:94–95. doi: 10.1177/036354659101900117. [DOI] [PubMed] [Google Scholar]
- 16.Benner R.W., Shelbourne K.D., Urch S.E., Lazarus D. Tear patterns, surgical repair, and clinical outcomes of patellar tendon ruptures after anterior cruciate ligament reconstruction with a bone-patellar tendon-bone autograft. Am J Sports Med. 2012;40:1834–1841. doi: 10.1177/0363546512449815. [DOI] [PubMed] [Google Scholar]
- 17.Bonamo J.J., Krinick R.M., Sporn A.A. Rupture of the Patellar ligament after use of its central third for anterior cruciate reconstruction. A report of two cases. J Bone Joint Surg Am. 1984;66:1294–1297. [PubMed] [Google Scholar]
- 18.Peiro A., Ferrandis R., Garcia L., Alcazar E. Simultaneous and spontaneous bilateral rupture of the patellar tendon in rheumatoid arthritis. A case report. Acta Orthop Scand. 1975;46:700–703. doi: 10.3109/17453677508989253. [DOI] [PubMed] [Google Scholar]
- 19.Muratli H.H., Celebi L., Hapa O., Bicimoglu A. Simultaneous rupture of the quadriceps tendon and contralateral patellar tendon in a patient with chronic renal failure. J Orthop Sci. 2005;10:227–232. doi: 10.1007/s00776-004-0868-2. [DOI] [PubMed] [Google Scholar]
- 20.Ramirez-Castillo H.D., Carbajal-Contreras R., Gonzalez-Morales D.D. Acute bilateral lesion of the patellar tendon associated to diabetes mellitus. Case report. Acta Ortoped Mex. 2010;24:23–27. [PubMed] [Google Scholar]
- 21.Bibbo C., Milia M.J., Gehrmann R.M., Patel D.V., Anderson R.B. Strength and knot security of braided polyester and caprolactone/glycolide suture. Foot Ankle Int. 2004;25:712–715. doi: 10.1177/107110070402501004. [DOI] [PubMed] [Google Scholar]
- 22.Ravalin R.V., Mazzocca A.D., Grady-Benson J.C., Nissen C.W., Adams D.J. Biomechanical comparison of patellar tendon repairs in a cadaver model: An evaluation of gap formation at the repair site with cyclic loading. Am J Sports Med. 2002;30:469–473. doi: 10.1177/03635465020300040301. [DOI] [PubMed] [Google Scholar]
- 23.Black J.C., Ricci W.M., Gardner M.J. Novel augmentation technique for patellar tendon repair improves strength and decreases gap formation: A cadaveric study. Clin Orthop Relat Res. 2016;474:2611–2618. doi: 10.1007/s11999-016-5009-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fukuta S., Kuge A., Nakamura M. Use of the Leeds-Keio prosthetic ligament for repair of Patellar tendon rupture after total knee arthroplasty. Knee. 2003;10:127–130. doi: 10.1016/s0968-0160(02)00127-8. [DOI] [PubMed] [Google Scholar]
- 25.Crossett L.S., Sinha R.K., Sechriest V.F., Rubash H.E. Reconstruction of a ruptured Patellar tendon with Achilles tendon allograft following total knee arthroplasty. J Bone Joint Surg Am. 2002;84A:1354–1361. doi: 10.2106/00004623-200208000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Chen B., Li R., Zhang S. Reconstruction and restoration of neglected ruptured patellar tendon using semitendinosus and gracilis tendons with preserved distal insertions: Two case reports. Knee. 2012;19:508–512. doi: 10.1016/j.knee.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 27.Moretti L., Vicenti G., Abate A., Pesce V., Moretti B. Patellar tendon rerupture in a footballer: Our personal surgical technique and review of the literature. Knee. 2014;45:452–456. doi: 10.1016/j.injury.2013.10.043. [DOI] [PubMed] [Google Scholar]
- 28.Sanchez G., Ferrari M.B., Sanchez A. Proximal patellar tendon repair: internal brace technique with unicortical buttons and suture tape. Arthrosc Tech. 2017;6:e491–e497. doi: 10.1016/j.eats.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A right knee revision patellar tendon repair is performed using suture anchors, allograft augmentation, and adjustable loop suspensory fixation. The patient is positioned supine and a diagnostic right knee arthroscopy is performed, and any intra-articular pathology is addressed. Through a midline longitudinal incision at the knee, the allograft tendon is positioned in a midline split through the native patellar tendon and secured in bone sockets in the patella and tibia with adjustable loop buttons. Remnant patellar tendon is repaired to the inferior pole of the patella with suture anchors.


