Abstract
Psoriatic arthritis (PsA) is a chronic immune-mediated disease characterized by psoriatic skin and nail changes, peripheral joint inflammation, enthesitis, dactylitis, and/or axial involvement, either alone or in combination with each other. The presence of axial involvement has been shown to be a marker of PsA severity; however, there is no widely accepted definition of axial involvement in PsA (axPsA) or consensus on how or when to screen and treat patients with suspected axPsA. Chronic back pain is a prominent feature of axPsA and is thought to have a relevant role in early identification of disease. Chronic back pain can be caused by inflammatory back pain (IBP) or mechanical back pain (MBP). However, MBP can complicate recognition of IBP and delay diagnosis of axPsA. While MBP can also be associated with chronic back pain of ≥ 3 months in duration that is typical of IBP, IBP is characterized by inflammation of the sacroiliac joint and lower spine that is differentiated from MBP by key characteristic features, including insidious onset at age < 40 years, improvement with exercise but not with rest, and nighttime pain. This review discusses the differences in identification and management of IBP and MBP in patients with PsA with axPsA. The summary of available evidence highlights the importance of appropriate and timely screening, difficulties and limitations of differential diagnoses and treatment, and unmet needs in axPsA.
Keywords: Diagnosis, Inflammatory back pain, Mechanical back pain, Psoriatic arthritis
Plain Language Summary
Psoriatic arthritis (PsA) is a long-term disease that may lead to psoriatic changes in skin and nails; inflammation of some joints, including finger and toe joints (dactylitis); inflammation of sites where tendons and ligaments connect to bone (enthesitis); and/or problems in the spine (axial involvement). Approximately 25–70% of patients with PsA have axial involvement (axPsA); this number varies because there is no widely accepted definition for axPsA. Chronic (long-lasting) back pain is a major feature of axSpA and can help doctors recognize axPsA early. Chronic back pain can be caused by inflammatory back pain (IBP) or mechanical back pain (MBP). IBP is described by back pain lasting ≥ 3 months, gradual onset at age < 40 years, improvement with exercise, no improvement with rest, pain at night (with improvement upon getting up), and changes in some laboratory test results. On the other hand, MBP is caused by a physical injury to the lower back. Both IBP and MBP can occur in patients with PsA, but they are treated in different ways. Being able to tell the difference between IBP and MBP is important to make sure that patients receive the right treatment. This review looks at the differences between IBP and MBP, screening for IBP, the difficulties and limitations of diagnosing and treating axPsA, and the needs of patients with axPsA for better diagnosis and treatment.
Key Summary Points
| Axial involvement is present in 25–70% of patients with psoriatic arthritis (PsA) and is an accepted marker of PsA disease severity. |
| Improved recognition of axial involvement may help to identify patients who are candidates for more aggressive and appropriate therapy that effectively treats the complete spectrum of PsA, including axial disease in PsA (axPsA). |
| Chronic back pain is also thought to have a relevant role in the early identification of axPsA and is usually accompanied by inflammatory back pain (IBP) symptoms but can be confused with mechanical back pain (MBP). |
| It is important to differentiate between IBP and MBP to ensure that patients with axPsA receive the most appropriate treatment. |
Digital Features
This article is published with digital features to facilitate understanding of the article. To view digital features for this article go to 10.6084/m9.figshare.12906404.
Introduction
Psoriatic arthritis (PsA) is a chronic immune-mediated disease characterized by psoriatic skin and nail changes, peripheral joint inflammation, enthesitis, dactylitis, and/or axial involvement [1–3]. The prevalence of PsA varies globally, ranging from 0.05 to 0.25% in the general population and increasing in those with psoriasis, with rates of approximately 30%, depending on the epidemiological methods used and populations studied [3, 4]. Early identification and appropriate treatment can significantly improve the quality of life of affected patients [5]. However, PsA is a heterogeneous disease and can have a wide range of effects and symptoms, making it difficult to distinguish from other musculoskeletal conditions [2, 6].
PsA involves genetic, environmental, and epigenetic factors, which contribute to disease risk and pathophysiology [1, 7–9]. For example, the major histocompatibility complex I molecules are involved in the development and proliferation of immune responses, including HLA-B27 [10]. HLA-B27 is a genetic marker of disease expression in PsA [9, 11], and its association with spondyloarthritis (SpA) has been recognized since the 1970s and varies across ethnicities and spondyloarthropathies [12]. HLA-B27 is associated with manifestations related to axial inflammation in SpA (axSpA) [13] and is more common in patients with axial involvement (axPsA) than in those without axial involvement [9]. Thus, HLA-B27 has been proposed as a genetic marker of axPsA [9, 14]. B*08:01:01–C*07:01:01 and its component alleles are associated with joint deformities and fusion, asymmetrical sacroiliitis, and dactylitis [15]. HLA-B*08:01:01-C*07:01:01 and HLA-B*37:01:01-C*06:02:01 have also been linked to the highest propensity score for severe PsA [15]. The association of HLA-B27 with axPsA has led to greater awareness of inflammatory back pain (IBP) as a discrete entity in PsA [16]. Although no laboratory tests specifically diagnose axPsA, testing for HLA-B27 may aid in diagnosis. Because the HLA-B27 gene is expressed in ≤ 8% of the general population, HLA-B27 positivity alone or the lack of HLA-B27 positivity should not be regarded as diagnostic for SpA. Random HLA-B27 testing is more likely to yield false-positive results than true-positive results [17–19].
Axial involvement is present in 25–70% of patients with PsA [14, 20], with variability that may reflect different criteria used across studies for defining the axial involvement (e.g., clinical and/or imaging criteria), and is an accepted marker of PsA disease severity [21]. Chronic back pain, a prominent feature of axSpA, is thought to have a relevant role in the early identification of axPsA and is usually accompanied by IBP symptoms [22, 23], suggesting potential inflammation of the sacroiliac joint and lower spine [24–26]. Conversely, mechanical back pain (MBP) is an injury or derangement of an anatomical structure in the lower back [27]. Both IBP and MBP can occur in patients with PsA [21, 28]. It is important to differentiate between IBP and MBP to ensure that patients with axPsA receive the most appropriate treatment. Methods for characterizing IBP in patients with axSpA may not perform well in patients with PsA; therefore, improved recognition of axial involvement may help to identify patients who are candidates for more aggressive and appropriate therapy that effectively treats the complete spectrum of PsA, including axial disease [21].
No widely accepted definition of axPsA exists, and guidelines vary on how and when to screen for back pain in PsA [29–39]. In this narrative review, we discuss the differences associated with identification and management of IBP versus MBP in axPsA, highlighting the importance of appropriate and timely screening, the difficulties and limitations of differential diagnosis, and the unmet needs of axPsA patients with IBP.
Search Strategy
We used the following search strings to identify articles of interest published on PubMed between January 1, 2009, and June 1, 2020: the primary search included (“mechanical” OR “inflammatory”) AND “psoriatic arthritis” AND “back pain”; secondary searches included “psoriatic arthritis” AND “back pain,” “psoriatic arthritis” AND “axial disease,” “back pain” AND (“mechanical” OR “inflammatory”) AND (“psoriatic arthritis” OR “axial spondyloarthritis”), “axial psoriatic arthritis,” and “psoriatic arthritis” AND “unmet need.”
The full text and bibliographies of relevant English-language articles were evaluated for specific data relating to IBP and MBP in patients with PsA, thus focusing on those with axPsA. Only those deemed relevant to the objectives of this study were included. This article is a review of previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Importance of Assessing AXPSA
axPsA is accompanied by significant clinical morbidity; it is associated with a higher likelihood of moderate/severe psoriasis, higher PsA disease activity, and greater impact on quality of life [40]. Because PsA (and axPsA) mostly manifest between the ages of 30–50 years [41, 42], back pain from axPsA, as with back pain in the general population, may have a greater impact on work productivity and social and mental aspects of quality of life, including fatigue, than in patients without axial involvement. Work disability is common in PsA, and many with this disease have health-related limitations, including time away or reduced effectiveness at work [38, 40]. In a Work Limitations Questionnaire of 107 patients with PsA, work productivity decreased by 6.7%, and more than half of those surveyed also reported fatigue [43]. In the Corrona Psoriasis Registry, work productivity and activity were significantly affected by axial involvement; patients with axial involvement reported a significantly higher percentage of work time missed, impairment while working, overall work impairment, and overall activity impairment versus those without axial involvement (P < 0.001) [40].
Therefore, patients with PsA should be assessed for axial involvement as soon as possible to ensure that they receive appropriate disease management and treatment [40] because patients with axial involvement may require more aggressive therapy [21]. However, characterization of axPsA remains poorly understood because limited data are available on this specific patient population [40]. Because few adequate studies have been conducted in patients with axPsA, criteria and outcome measures specifically for axSpA have been widely accepted for axPsA; responses to therapy are presumed to be equivalent for axPsA and ankylosing spondylitis (AS) [44]. In addition, no consensus exists on how and when to screen for axial disease in PsA [45]. Patients with PsA with more severe peripheral disease are reported to have a higher risk of underdiagnosed axPsA [29]. Tools currently available to score axSpA, including the modified Stoke Ankylosing Spondylitis Spinal Score, the Radiographic Ankylosing Spondylitis Spinal Score, the Bath Ankylosing Spondylitis Disease Activity Index, and the Ankylosing Spondylitis Disease Activity Score, but not the Bath Ankylosing Spondylitis Radiology Index-spine, are reportedly reliable for axPsA [30, 32, 34, 37]. Spinal mobility measurements and the Bath Ankylosing Spondylitis Metrology Index score may be valuable in differentiating axPsA from peripheral PsA [38]. Imaging can be useful for differential diagnosis and monitoring for inflammatory and structural changes [33]. Radiographic assessment is considered the gold standard for distinguishing axPsA from axSpA and other degenerative or inflammatory conditions [39]; Feld and colleagues recently reported that patients with AS have a higher grade of sacroiliitis than those with axPsA [46]. Ibrahim and colleagues reported the use of an electronic application that specifically documents axPsA manifestations [36]. In this study, radiographs from patients with axPsA were blindly scored by three rheumatologists using the app and yielded high specificity and moderate sensitivity; these results were independently confirmed by a nonblinded, external expert as true radiographic progression [36]. In addition, the extent of inflammation shown for HLA-B27–related active axPsA on magnetic resonance imaging (MRI) was similar to that associated with axSpA and AS and was superior to that associated with HLA-B27–negative PsA [31].
Appropriate Screening for Back Pain in PSA
Back pain is one of the most common reasons for physician visits globally and the most costly in terms of healthcare provider visits [47], leading to significant direct medical costs and indirect societal costs arising from absenteeism, presenteeism, disability, and workers’ compensation claims [48]. Because back pain has many different causes that can present with similar symptoms, it can be difficult to identify its fundamental pathological features during musculoskeletal evaluation [27, 48]. Back pain is very common in the general population; approximately 80% of people experience it in some form at least once in their lifetimes [25]. Most (97%) chronic back pain episodes are reported to be mechanical in nature. Nonmechanical causes may include those being of rheumatologic, vascular, gastrointestinal, renal, infectious, or oncologic origin [48].
Back pain can impair productivity, which influences long-term profitability [49]. In a 4-year review of presenteeism data among employees of a large US healthcare system, chronic back pain ranked among the highest for minutes of daily productivity loss (16.7) and annual cost per person ($1920) [49]. Low back pain with or without lower extremity pain is one of the most common reasons for physician visits, and treatment costs remain a significant burden on healthcare resources [47]. In a recent US study, the total cost of care over 12 months after diagnosis was $1.8 billion among patients with low back pain with or without lower extremity pain and not undergoing surgery [47].
Therefore, accurate identification of back pain is important in determining the underlying cause and the most appropriate treatment [48]. MBP persisting for > 4 to 6 weeks warrants further investigation for possible nonmechanical causes, such as IBP [48]. It is important that patients with probable axSpA or axPsA, based on the identification criteria for IBP, are referred to a rheumatology specialist [25–27]. This screening approach would ensure the timely identification and management of IBP and result in the best outcome for patients and appropriate utilization of resources [25, 26]. Identification of back pain could be improved by using predictors of axial involvement, including HLA-B27 positivity, nail dystrophy, number of radiographically damaged joints, periostitis, elevated acute phase reactants, and disease duration [9, 16, 50, 51].
Differential Diagnosis of IBP versus MBP
Fibromyalgia, characterized by chronic, widespread pain, reportedly occurs in up to 22% of patients with PsA [52–55]. The presence of comorbid fibromyalgia may mask PsA disease severity, especially when subjective measures and patient-reported outcomes are being considered [56, 57]. Accordingly, distinguishing fibromyalgia from PsA may be addressed using screening instruments such as the Widespread Pain Index and Symptom Severity Score [58, 59].
IBP Versus MBP Key Features
It is important to distinguish between IBP and MBP as early as possible in the disease course because management and treatment of the two types of back pain are very different. IBP is differentiated from MBP by key characteristic features identified by experts from the Assessment of SpondyloArthritis international Society (ASAS) (Table 1) [27, 48, 60], including chronic back pain of ≥ 3 months in duration (which may not always be present in MBP), insidious onset at age < 40 years, improvement with exercise, no improvement with rest, pain at night (with improvement upon getting up), and elevated acute phase reactants (erythrocyte sedimentation rate and/or C-reactive protein [CRP]). IBP is present in axSpA (nonradiographic and radiographic) and the axial form of PsA, and is typically associated with early pain onset localized to the axial spine, sacroiliac joints, and buttocks [24, 26, 27, 29, 61]. MBP is identified by first ruling out red flags and symptoms, including trauma, unexplained weight loss, neurological signs, age > 50 years, fever, intravenous drug use, long-term steroid use, and history of cancer [62]; however, there is no clear evidence about which are clinically relevant [27, 48]. Onset of MBP can occur at any age and can be acute; pain may worsen with movement and improve with rest [27, 48].
Table 1.
Classification criteria of IBP versus MBP from various mechanical and nonmechanical causes
| IBP (according to ASAS experts’ criteria, axSpA) [60] | MBP (injury to or derangement of spine structures or rheumatologic, vascular, gastrointestinal, renal, infectious, or oncologic causes) [27, 48] |
|---|---|
|
ASAS criteria: when patient presents with back pain of ≥ 3 months in duration • Age at onset < 40 years • Insidious onset • Improvement with exercise • No improvement with rest • Pain at night (with improvement upon getting up) Diagnoses are made by combining clinical criteria with radiological findings (MRI, CT, ultrasound) and/or laboratory test results (e.g., testing for HLA-B27) |
Identification of symptoms (no clear evidence about which are clinically relevant) • Onset at any age; may be more common in middle-aged, working individuals • Variable onset; may be acute • Pain may worsen with movement • Pain often improves with rest Physical examination involving patient history, such as an acute injury • This process can involve ruling out IBP along with other causes of back pain (e.g., malignancies, infection) Injury or derangement of an anatomical structure in the lower back • Soft tissue (lumbar sprain or strain) • Muscle/fascia (myofascial pain) • Disks (herniated disk, discogenic pain) • Joints (zygapophysial joint and sacroiliac joint pain) • Bone (vertebral fractures, spondylolisthesis, kyphosis, scoliosis) MBP persisting for > 4 to 6 weeks may warrant further diagnostic testing and imaging |
ASAS Assessment of SpondyloArthritis international Society, axSpA axial spondyloarthritis, CT computed tomography, IBP inflammatory back pain, MBP mechanical back pain, MRI magnetic resonance imaging
Identification of IBP
IBP pathophysiology stems from a systemic response to inflammatory mediators localized to the axial skeletal joints that induces proinflammatory intracellular changes [26]. This chronic inflammation leads to a reactive cycle of unbalanced bone remodeling associated with bone loss and possible bone fusion, which may result in ankylosis of the sacroiliac joints and formation of syndesmophytes in the spine [26, 63]. It has been suggested that mechanical strain on the entheses may drive both processes of inflammation and bone remodeling [64].
Numerous criteria exist to identify probable IBP, including the Calin, Berlin, and ASAS criteria [60, 65, 66]. The ASAS criteria are commonly used when patients present with back pain of ≥ 3 months in duration; the criteria comprise five parameters (Table 2) [60]. If ≥ 4 parameters are present, ASAS criteria have a reported sensitivity and specificity of 77% and 91.7%, respectively, for identifying IBP [60, 67]. Validated classification criteria for IBP in axPsA are not yet available; however, ASAS and the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) are making efforts to develop such criteria [68]. Although age of onset < 40 years is one of the parameters used for identifying probable IBP, it should be noted that axial manifestations develop in patients with PsA at an older age, and that not all patients with radiographic changes may present with symptoms [21, 69–72].
Table 2.
Treatment pathways for managing IBP and MBP in PsA
| IBP (EULAR recommendations) [51] | IBP (GRAPPA, GRADE recommendations for axPsA) [93] | MBP [27, 48] |
|---|---|---|
|
NSAIDs may be used to relieve musculoskeletal signs and symptoms (grade A recommendation) Local injections of glucocorticoids should be considered as adjunctive therapy in PsA; systemic glucocorticoids may be used with caution at the lowest effective dose (grade C recommendation) In patients with predominantly axial disease that is active and has insufficient response to NSAIDs, therapy with a bDMARD should be considered, which according to current practice is a TNFi; when there is relevant skin involvement, IL-17 inhibitor may be preferred (grade B recommendation) In patients who fail to respond adequately to, or are intolerant of a bDMARD, switching to another bDMARD or tsDMARD should be considered, including one switch within a class (grade B recommendation) Optimal management of patients with PsA also requires nonpharmacological strategies, such as patient education and regular physical exercise, and may also require topical medication (overarching principle) |
Biologic naive Strongly recommended: NSAIDs, physiotherapy, simple analgesia, TNFis Conditionally recommended: IL-17 inhibitor, SI joint CS injections, bisphosphonates, IL-12/23 inhibitor Inadequate response to bDMARDs Strongly recommended: physiotherapy, simple analgesia Conditionally recommended: NSAIDs, TNFi, IL-12/23 inhibitor, IL-17 inhibitor |
Current guidance reinforces the primary emphasis of nonpharmacological measures NSAIDs/analgesics; CS can be used when necessary Physiotherapy (activity over bed rest), but rest (if acute) Behavioral approaches (mindfulness) Patient education (self-management recommendations) |
axPsA axial psoriatic arthritis, bDMARD biologic disease-modifying antirheumatic drug, CS corticosteroids, EULAR European League Against Rheumatism, GRADE Grading of Recommendations, Assessment, Development and Evaluation, GRAPPA Group for Research and Assessment of Psoriasis and Psoriatic Arthritis, IBP inflammatory back pain, IL interleukin, MBP mechanical back pain, NSAID nonsteroidal anti-inflammatory drug, PsA psoriatic arthritis, SI sacroiliac, TNFi tumor necrosis factor inhibitor
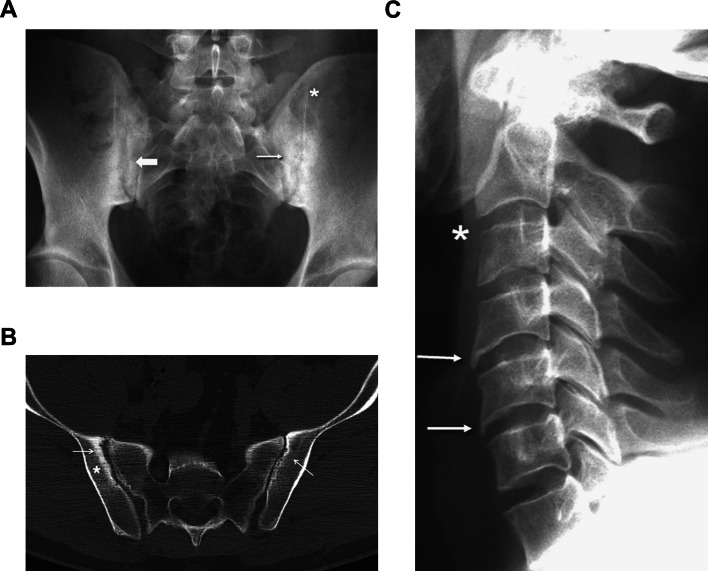
Imaging techniques are also useful in identifying IBP (Fig. 1) [73–75]. MRI can detect the signs of initial inflammatory processes associated with the early stages of axSpA/PsA or structural changes associated with AS/PsA [73]. Ultrasound is being used in PsA to primarily examine peripheral joints and entheses; however, interest in analyzing axPsA and sacroiliitis is increasing [75]. A Bath Ankylosing Spondylitis Disease Activity Index score of ≥ 4, the cutoff for active disease, can also help identify spinal disease [76]. The ASAS MRI working group recently generated a consensus update on standardized definitions for MRI lesions in the sacroiliac joint of patients with SpA [77]. The reliability of definitions was satisfactory for most inflammatory and mechanical lesions, even among some lesions occurring at a frequency of < 10% [77]. Computed tomography (CT) is useful for detecting bone erosions in joints and entheses, and may be easier to interpret than radiographs due to its high resolution [33, 78]; however, CT does not show active inflammation and has limited use in diagnosis or in monitoring progression of disease. The role of CT in clinical practice remains unclear and it is largely limited to research settings [78].
Fig. 1.
a Typical findings of sacroiliac joint involvement in a patient with ankylosing spondylitis (AS), showing extensive sclerosis (thin arrow), pseudodilation (thick arrow), and partial ankylosis (asterisk). b Computed tomography of the sacroiliac joints of a patient with AS. Note the areas with erosions (arrows) and sclerosis (asterisk), which represent characteristic signs of the disease. c Typical osteodestructive changes seen as erosion (asterisk) and osteoproliferative changes seen as syndesmophytes (arrows) in the cervical spine of a patient with AS. Reprinted from Hochberg MC, et al. Rheumatology. 7th ed.
Copyright © 2019 with permission from Elsevier
Identification of MBP
Compared with IBP, MBP more often results from acute injury or derangement of an anatomical structure in the lower back and can occur at any age, though it may be more common in middle-aged, working individuals compared with the younger age of onset of IBP [27, 48]. Because of the complexity of identifying MBP, distinguishing IBP from MBP remains difficult. Table 1 describes the criteria used to classify IBP and MBP resulting from various mechanical and nonmechanical causes. Symptoms of MBP often worsen with movement and exercise and appear to correlate with injury and more acute onset [26]. Typically, its insidious onset occurs at an older age than IBP and can be acute or chronic [27, 79].
MBP is usually identified through a physical examination involving patient history, such as an acute injury. This process can involve ruling out IBP based on the above-mentioned criteria, along with other causes of back pain (e.g., malignancies, infection) [25–27]. Imaging techniques such as X-ray, MRI, and computed tomography can be used if necessary [27, 48].
Limitations of Identification Criteria and Measurement of IBP and MBP
The current standard ASAS criteria used to identify IBP are limited by sensitivity and specificity; the reported sensitivity would result in 23% of IBP cases not being identified in patients with chronic back pain [60]. Identification of IBP by MRI is limited by low specificity [80]. Many patients with non-SpA, including healthy individuals, show evidence of sacroiliitis when the sacroiliac joint is examined for lesions [80]. Limitations of MRI include the subjectivity and variability of the radiologist/rheumatologist examining the scan results for signs indicating inflammation, often in terms of confidence levels rather than a simple yes or no [80]. Signs and symptoms of MBP differ across guidelines, and little consensus or evidence exists about which are clinically relevant [27].
Is There an Inflammatory Component in MBP?
Any inflammation observed in MBP is the result of an initiating event (e.g., injury, wear and tear), which propagates further degeneration [27, 48]. All structures within the spine, including the vertebral bodies, intervertebral discs, zygapophysial joints, sacroiliac joints, spinal ligaments, paraspinal muscles, dura, spinal cord, and nerves are potential pain generators for MBP [48]. For example, intervertebral disc degeneration is a major contributor to MBP and/or lower back pain and can be accompanied by inflammation at the site of the damage/degeneration [81, 82]. It is unclear whether inflammation is the root cause or a consequence of intervertebral disc degeneration [81, 82]. First, an initiating event causes increased production of cytokines and chemokines by nucleus pulposus and annulus fibrosus cells. This is followed by further inflammation, neovascularization, and nerve growth into the structurally deficient discal tissues. Finally, the nerve endings become sensitized and dorsal root ganglion pain channel activity is modulated via inflammatory mediators, which result in pain. Therefore, the inflammatory response to the initiating event perpetuates further degeneration in MBP [81, 82]. In contrast, the inflammatory response of IBP is the cause, with no mechanical initiating event [27, 48].
Is IBP a symptom of different diseases?
Once IBP has been determined, it becomes important to identify the root cause of the condition. IBP is associated strongly with, but not diagnostic of, several inflammatory conditions that may have both axial and peripheral pain features [26]. The classic association of IBP symptoms is with axSpA; however, IBP may also be present in conjunction with other seronegative spondyloarthropathies such as PsA, enteropathic arthropathy, juvenile idiopathic arthritis, and reactive arthritis [26]. The accuracy of IBP in differentiating patients with axPsA from patients with other causes of back pain has not been fully clarified [83]. AxSpA consists of several inflammatory conditions—an umbrella state—of which the radiographic version is AS. These disease states are all characterized clinically by IBP [84]. Considerable overlap exists between the symptoms of these diseases, which can make differential diagnosis difficult [26].
Nonradiographic and radiographic axSpA are often considered two stages of the same disease, because the nonradiographic form can progress to the radiographic form; however, not all nonradiographic cases progress to radiographic disease [85]. The only difference between nonradiographic and radiographic axSpA is radiographic changes in the sacroiliac joints [84]. The decision to initiate biologic treatment in the absence of sacroiliitis is predicted mainly by the presence of active inflammation, as identified by MRI findings or elevated CRP levels—the latter of which may be a correlate of radiographic progression [84, 86–88]. Differential diagnosis between nonradiographic and radiographic axSpA can be performed by investigating structural damage with imaging (usually MRI) [85]. Although it is still debatable whether axPsA is radiographic axSpA with concomitant psoriasis or whether they are distinct conditions that share similar characteristics [39, 89], Feld and colleagues concluded from their study that AS—with or without psoriasis—is different from axPsA [46]. The Psoriatic Arthritis Spondylitis Radiology Index is useful for assessing structural damage in axPsA [30]. Clinicians still struggle to differentiate axPsA from concomitant radiographic axSpA and psoriasis [33, 69, 89, 90]. It may help that spinal involvement in PsA is more frequently unilateral (asymmetric) and is often less severe than radiographic axSpA [69]. Notable differences exist in the morphology of syndesmophytes, the development of which is correlated with elevated CRP levels; those in PsA have a larger volume and appear to progress more randomly along the spine [69, 74, 91]. The finding that inflammation in patients with axPsA responds better to corticosteroids than it does in patients with radiographic axSpA further supports the argument that axPsA and concomitant radiographic axSpA and psoriasis are two distinct diseases [92].
Management of IBP and MBP
Standard management of IBP symptoms includes patient education, the use of nonsteroidal anti-inflammatory drugs (NSAIDs), and structured physiotherapy/exercise programs (Table 2) [25–27]. Patient education is an important aspect of IBP management, allowing patients to make informed shared decisions with their doctors [27]. Conventional synthetic disease-modifying anti-rheumatic drugs (DMARDs) can also be prescribed in addition to biologic DMARDs (bDMARDs) in patients with consistently high disease activity [26, 27].
In 2019, the European League Against Rheumatism (EULAR) published updated guidelines for managing PsA with pharmacological therapies (Table 2) [51]. Phase 1 of treatment consists of NSAIDs with or without local glucocorticoid injections, and phase 2 treatment consists of methotrexate; however, patients with predominantly axial disease directly enter phase 3 of treatment after phase 1 failure, which involves initiation of a bDMARD (usually a tumor necrosis factor inhibitor [TNFi]); interleukin (IL)-17A inhibitors would be preferred over TNFis in the presence of relevant skin involvement [51]. Because of the lack of clear efficacy in axSpA, drugs targeting the IL-12/23 pathway are not indicated for patients with predominantly axial disease [51].
GRAPPA guidelines for PsA call for an individualized approach to therapeutic decisions based on specific disease subtypes, including axial arthritis (Table 2) [93]. Treatment recommendations for axial disease are derived from diagnostic criteria, screening, monitoring, and response to therapy in axSpA. NSAIDs, physiotherapy, and TNFis are recommended, while IL-17 and IL-12/23 inhibitors are conditionally recommended [93]; however, GRAPPA guidelines are now a few years old and do not include more recent evidence of biologics targeting IL-17, IL-12/23, and IL-23 for the treatment of axial disease. Moreover, the IL-23 inhibitor risankizumab failed to demonstrate clinically meaningful improvements in patients with AS vs placebo [94].
Biologic treatments that affect the Th17 axis (e.g., ixekizumab and secukinumab) have shown to be beneficial in patients with PsA and in those with axSpA [95–99]. Thus, based on the similar inflammatory mechanisms of disease, these treatments may prove beneficial in patients with axPsA. However, to date, only secukinumab has been shown to have clinical benefits in patients with axPsA [68]. Although targeting the IL-23 pathway has not been effective in treating patients with AS [100] and is not recommended in more recent treatment guidelines for patients with PsA who have axial involvement [51], post hoc analyses have explored the benefit of ustekinumab in biologic-naive patients with PsA with peripheral arthritis and physician-reported spondylitis [101].
Current guidelines for managing MBP emphasize the use of nonpharmacological measures (Table 2) [27, 48]. However, evidence exists that patients may experience small benefits from anti-inflammatories/painkillers and corticosteroids, rest (if acute), physiotherapy (activity over bed rest), and behavioral approaches [27]. A Cochrane review showed limited, low-quality evidence of reduced pain severity and improved physical function in patients engaging in physical activity and exercise; therefore, patients should be encouraged to remain active if possible [102].
Unmet Needs
Several critical questions still remain, such as how common is IBP as a manifestation of peripheral PsA despite its prominence in axPsA [27], how should axPsA be defined, what role does imaging play in the identification of axPsA among patients with IBP, and how do we evaluate patients with PsA who have inflammation on imaging and yet do not present with inflammatory symptoms or clinical features of IBP or sacroiliitis [21, 51, 103]. A joint effort by ASAS and GRAPPA is underway to better define axial involvement in PsA through a prospective study [103, 104]. It also remains to be seen how data obtained from new therapies will affect refinement of treatment guidelines. The 2019 update to the EULAR recommendations for management of PsA now contains language noting that IL-17 inhibitors may be preferred over TNFis in the presence of relevant skin involvement, and that therapies targeting the IL-12/23 axis are not indicated for patients with axial involvement [51]. GRAPPA bases their recommendations on whether patients are biologic naive (strong recommendations for NSAIDs, physiotherapy, simple analgesia, and TNFis) or have an inadequate response to bDMARDs (strong recommendations for physiotherapy and simple analgesia; conditional recommendations for NSAIDs, TNFis, IL-12/23 inhibitors, and IL-17 inhibitors) [93]. However, phase 3/4 clinical trials for different bDMARDs and targeted synthetic DMARDs are ongoing, including the IL-17A inhibitor secukinumab (NCT02721966 [MAXIMISE]; completed June 2019) and the oral JAK inhibitor tofacitinib (NCT04062695 [PASTOR]; expected to be completed June 2022) [105, 106]. In the phase 3b, double-blind, placebo-controlled, multicenter, 52-week MAXIMISE trial, secukinumab (150 and 300 mg) provided rapid and significant improvement in ASAS20 response through week 12 in patients with axPsA with an inadequate response to NSAIDs [68]. Additionally, at week 52, secukinumab improved clinical and imaging outcomes among patients with axPsA [107]. No interim results have been published for the PASTOR trial [106]. A trial evaluating the impact of secukinumab on bone health and metabolism is ongoing in patients with AS, which may help provide additional information on bone loss and remodeling among all patients with axial involvement [108]. Improved management and treatment adherence may reduce the unmet need and disease burden of PsA, particularly a patient’s mental and physical health, employment, and healthcare utilization [109].
Another unanswered question is whether and to what extent MBP can confound treatment for PsA and what treatment strategies are available for patients with PsA and concurrent MBP. Improved doctor–patient communication is needed to establish realistic goals of care and treatment and to determine whether a patient’s back pain has a mechanical or inflammatory origin. Last, a better understanding of the various mechanisms of pain is required, including central sensitization and osteoarthritis, correlation of physical examination with advanced imaging (e.g., ultrasound, MRI), and standardized characterization and measurement of PsA domains [110]. In chronic painful disorders such as PsA, pain stems not only from inflammation and mechanical soreness but from a myriad of mechanisms, including central sensitization—an amplification of neural signaling that leads to pain hypersensitivity [111]. Similarly, osteoarthritis—once thought to be a disease caused by “wear and tear”—is now recognized as low-grade inflammation [112] and possibly shares characteristic features with PsA [113]. Indeed, the mechanisms underlying chronic pain states, such as axPsA, are thought to differ from those underlying acute pain [114].
Multimorbidity, the coexistence of ≥ 2 conditions in an individual, is common in axSpA and is associated with more severe disease [115]. However, no published studies on the effects of multimorbidity on axPsA outcomes are currently available.
Finally, clearer education of back pain, communication, and screening approaches (including development of cross-specialty clinics and standardized identification protocols) are needed for rheumatologists, dermatologists, and primary care providers caring for patients with PsA [110].
Expert Commentary
Recognizing and diagnosing axial involvement, either within PsA or independent of it, early in its disease course is challenging, and the diagnosis is often made long after symptoms initially begin. Collaboration and communication between clinicians and their patients may lead to timelier diagnosis with early referral and treatment, which is the goal. This topic is of continual interest to our field because of its very debatable, at times conflated, and unfortunately delayed diagnosis. In the primary care setting, there is a large prevalence of back pain that resolves in a short period of time with conservative management. In the rheumatological setting, demands are much more stringent and require a more specific approach.
There are numerous additional variables to be considered when eliciting a history for potential inflammatory back pain. Is there any family or personal history of AS, psoriasis, uveitis, or inflammatory bowel disease? Is there any secondary history of past or present spontaneous pain or tenderness at the insertion sites of the Achilles tendons or plantar fascia at the calcaneus? Is back pain improved significantly with NSAIDs? Is there any history of spontaneous joint effusions? Is there any history of soft tissue differential such as fibromyalgia? Is there any history of hypermobility in younger patients (e.g., differential Ehlers–Danlos)?
Key takeaways to identify or questions to elicit from patients when assessing for IBP, with or without an established diagnosis, include history or present symptoms of spinal pain in back, dorsal, or cervical regions, with at least four of the following: (a) onset before age 40 years; (b) insidious onset; (c) pain relief with exercise or activity, not improved by rest; (d) associated with morning stiffness or alternating buttock pain; (e) duration of at least 3 months; or (f) pain at night with improvement upon awakening. If ≥ 4 of these criteria are fulfilled, and no other diagnosis can be considered in patients displaying PsA symptoms regardless of treatment status, then a referral to a rheumatologist must be made without further delay. In this instance, consider the patient with PsA who develops IBP in later years after he/she has been diagnosed and treated with not entirely comprehensive therapy. For example, a 56-year-old patient with PsA/psoriasis receiving methotrexate, which does not seem to be effective in axPsA [116] and NSAIDs for years whose symptomatology vastly improves after introduction of effective targeted biologic DMARD treatment addressing IBP based on the above criteria.
Conclusions
The presence of axial involvement is a marker of PsA severity. Therefore, recognizing axial involvement may help identify those patients who are candidates for more aggressive and appropriate therapy that effectively treats the complete spectrum of PsA, including axial disease. However, clinicians are still debating the definition of axPsA, how to screen patients, and when to initiate treatment. Few effective first-line treatments specifically for axPsA are available, mainly due to the lack of supporting evidence. EULAR and GRAPPA recommend bDMARDs for active axPsA that insufficiently responds to NSAIDs or TNFis, but most therapies—based on the quality and the range of available data—are only conditionally recommended [51, 93]. Clinical trials studying the efficacy of bDMARDs and targeted synthetic DMARDs for axPsA are ongoing [105, 106], and the results have the potential to change the treatment landscape and influence recommendations for managing axPsA. Chronic IBP is the most prominent feature of axPsA and is thought to play a key role in early identification of disease. It is important to differentiate IBP from MBP based on key characteristic features and to realize that IBP is a key component of other diseases unrelated to PsA.
The summary of available evidence highlights the importance of appropriate and timely screening of IBP, the difficulties and limitations of differential diagnoses and treatment, and unmet needs in axPsA. Additional data regarding the use of therapies targeting the Th17 axis in patients with axPsA, as well as findings from ASAS and GRAPPA on defining classification criteria for axPsA, are eagerly anticipated.
Acknowledgements
Funding
This study and the Rapid Service Fee were funded by Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA.
Medical Writing and Editorial Assistance
The authors thank Kheng Bekdache, PhD, and Eric Deutsch, PhD, CMPP, of Health Interactions, Inc, Hamilton, NJ, USA, for providing medical writing support/editorial support, which was funded by Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA, in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Authorship
All named authors meet the International Committee of Medical Journal Editors criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Linda L. Grinnell-Merrick received speaker and/or consulting fees/honoraria from AbbVie, Amgen (previously Celgene), Novartis, Pfizer, and Regeneron. Eileen J. Lydon received speaker fees/honoraria from AbbVie and Sanofi. Amanda M. Mixon received speaker fees/honoraria from AbbVie, Lilly, and Novartis, and has participated in an advisory board for Novartis. William Saalfeld received speaker and/or honoraria from Amgen (previously Celgene), Novartis, Pfizer, and Regeneron.
Compliance with Ethics Guidelines
This article is a review of previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
Digital Features
To view digital features for this article go to 10.6084/m9.figshare.12906404.
References
- 1.Veale DJ, Fearon U. The pathogenesis of psoriatic arthritis. Lancet. 2018;391:2273–2284. doi: 10.1016/S0140-6736(18)30830-4. [DOI] [PubMed] [Google Scholar]
- 2.Ritchlin CT, Colbert RA, Gladman DD. Psoriatic arthritis. N Engl J Med. 2017;376:957–970. doi: 10.1056/NEJMra1505557. [DOI] [PubMed] [Google Scholar]
- 3.Ogdie A, Weiss P. The epidemiology of psoriatic arthritis. Rheum Dis Clin N Am. 2015;41:545–568. doi: 10.1016/j.rdc.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mease PJ, Gladman DD, Papp KA, Khraishi MM, Thaci D, Behrens F, et al. Prevalence of rheumatologist-diagnosed psoriatic arthritis in patients with psoriasis in European/North American dermatology clinics. J Am Acad Dermatol. 2013;69:729–735. doi: 10.1016/j.jaad.2013.07.023. [DOI] [PubMed] [Google Scholar]
- 5.Koolaee RM, Takeshita J, Ogdie A. Epidemiology and natural history of psoriatic arthritis: an update on what dermatologists need to know. Curr Dermatol Rep. 2013;2:66–76. [Google Scholar]
- 6.Mease PJ, Garg A, Gladman DD, Helliwell PS. Development of simple clinical criteria for the definition of inflammatory arthritis, enthesitis, dactylitis, and spondylitis: a report from the GRAPPA 2012 annual meeting. J Rheumatol. 2013;40:1442–1445. doi: 10.3899/jrheum.130459. [DOI] [PubMed] [Google Scholar]
- 7.Barnas JL, Ritchlin CT. Etiology and pathogenesis of psoriatic arthritis. Rheum Dis Clin N Am. 2015;41:643–663. doi: 10.1016/j.rdc.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 8.Nograles KE, Brasington RD, Bowcock AM. New insights into the pathogenesis and genetics of psoriatic arthritis. Nat Clin Pract Rheumatol. 2009;5:83–91. doi: 10.1038/ncprheum0987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Queiro R, Morante I, Cabezas I, Acasuso B. HLA-B27 and psoriatic disease: a modern view of an old relationship. Rheumatology (Oxford) 2016;55:221–229. doi: 10.1093/rheumatology/kev296. [DOI] [PubMed] [Google Scholar]
- 10.Chen B, Li J, He C, Li D, Tong W, Zou Y, et al. Role of HLA-B27 in the pathogenesis of ankylosing spondylitis (review) Mol Med Rep. 2017;15:1943–1951. doi: 10.3892/mmr.2017.6248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eder L, Chandran V, Pellet F, Shanmugarajah S, Rosen CF, Bull SB, et al. Human leucocyte antigen risk alleles for psoriatic arthritis among patients with psoriasis. Ann Rheum Dis. 2012;71:50–55. doi: 10.1136/ard.2011.155044. [DOI] [PubMed] [Google Scholar]
- 12.Khan MA. Update on spondyloarthropathies. Ann Intern Med. 2002;136:896–907. doi: 10.7326/0003-4819-136-12-200206180-00011. [DOI] [PubMed] [Google Scholar]
- 13.Chung HY, Machado P, van der Heijde D, D'Agostino MA, Dougados M. HLA-B27 positive patients differ from HLA-B27 negative patients in clinical presentation and imaging: results from the DESIR cohort of patients with recent onset axial spondyloarthritis. Ann Rheum Dis. 2011;70:1930–1936. doi: 10.1136/ard.2011.152975. [DOI] [PubMed] [Google Scholar]
- 14.Chandran V, Tolusso DC, Cook RJ, Gladman DD. Risk factors for axial inflammatory arthritis in patients with psoriatic arthritis. J Rheumatol. 2010;37:809–815. doi: 10.3899/jrheum.091059. [DOI] [PubMed] [Google Scholar]
- 15.Haroon M, Winchester R, Giles JT, Heffernan E, FitzGerald O. Certain class I HLA alleles and haplotypes implicated in susceptibility play a role in determining specific features of the psoriatic arthritis phenotype. Ann Rheum Dis. 2016;75:155–162. doi: 10.1136/annrheumdis-2014-205461. [DOI] [PubMed] [Google Scholar]
- 16.Reveille JD, Weisman MH. The epidemiology of back pain, axial spondyloarthritis and HLA-B27 in the United States. Am J Med Sci. 2013;345:431–436. doi: 10.1097/maj.0b013e318294457f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown MA. Human leucocyte antigen-B27 and ankylosing spondylitis. Intern Med J. 2007;37:739–740. doi: 10.1111/j.1445-5994.2007.01491.x. [DOI] [PubMed] [Google Scholar]
- 18.Sheehan NJ. The ramifications of HLA-B27. J R Soc Med. 2004;97:10–14. doi: 10.1258/jrsm.97.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gardner GC, Kadel NJ. Ordering and interpreting rheumatologic laboratory tests. J Am Acad Orthop Surg. 2003;11:60–67. doi: 10.5435/00124635-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Gladman DD. Axial disease in psoriatic arthritis. Curr Rheumatol Rep. 2007;9(6):455–460. doi: 10.1007/s11926-007-0074-2. [DOI] [PubMed] [Google Scholar]
- 21.Yap KS, Ye JY, Li S, Gladman DD, Chandran V. Back pain in psoriatic arthritis: defining prevalence, characteristics and performance of inflammatory back pain criteria in psoriatic arthritis. Ann Rheum Dis. 2018;77:1573–1577. doi: 10.1136/annrheumdis-2018-213334. [DOI] [PubMed] [Google Scholar]
- 22.Caso F, Costa L, Atteno M, Del Puente A, Cantarini L, Lubrano E, et al. Simple clinical indicators for early psoriatic arthritis detection. Springerplus. 2014;3:759. doi: 10.1186/2193-1801-3-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lindstrom U, Bremander A, Haglund E, Bergman S, Petersson IF, Jacobsson LT. Back pain and health status in patients with clinically diagnosed ankylosing spondylitis, psoriatic arthritis and other spondyloarthritis: a cross-sectional population-based study. BMC Musculoskelet Disord. 2016;17:106. doi: 10.1186/s12891-016-0960-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Braun A, Saracbasi E, Grifka J, Schnitker J, Braun J. Identifying patients with axial spondyloarthritis in primary care: how useful are items indicative of inflammatory back pain? Ann Rheum Dis. 2011;70:1782–1787. doi: 10.1136/ard.2011.151167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burgos-Vargas R, Braun J. Inflammatory back pain. Rheum Dis Clin N Am. 2012;38:487–499. doi: 10.1016/j.rdc.2012.08.014. [DOI] [PubMed] [Google Scholar]
- 26.Lassiter W, Allam AE. Inflammatory back pain. Treasure Island: Statpearls Publishing; 2019. [PubMed] [Google Scholar]
- 27.Ledford C. Spine conditions: mechanical and inflammatory low back pain. FP Essent. 2017;461:15–20. [PubMed] [Google Scholar]
- 28.Baraliakos X, Coates LC, Braun J. The involvement of the spine in psoriatic arthritis. Clin Exp Rheumatol. 2015;33(5 Suppl 93):S31–S35. [PubMed] [Google Scholar]
- 29.Aydin SZ, Kilic L, Kucuksahin O, Ureyen SB, Kalyoncu U. Performances of inflammatory back pain criteria in axial psoriatic arthritis. Rheumatology (Oxford) 2017;56:2031–2032. doi: 10.1093/rheumatology/kex307. [DOI] [PubMed] [Google Scholar]
- 30.Biagioni BJ, Gladman DD, Cook RJ, Eder L, Wakhlu A, Shen H, et al. Reliability of radiographic scoring methods in axial psoriatic arthritis. Arthritis Care Res (Hoboken) 2014;66:1417–1422. doi: 10.1002/acr.22308. [DOI] [PubMed] [Google Scholar]
- 31.Castillo-Gallego C, Aydin SZ, Emery P, McGonagle DG, Marzo-Ortega H. Magnetic resonance imaging assessment of axial psoriatic arthritis: extent of disease relates to HLA-B27. Arthritis Rheum. 2013;65:2274–2278. doi: 10.1002/art.38050. [DOI] [PubMed] [Google Scholar]
- 32.Eder L, Chandran V, Shen H, Cook RJ, Gladman DD. Is ASDAS better than BASDAI as a measure of disease activity in axial psoriatic arthritis? Ann Rheum Dis. 2010;69:2160–2164. doi: 10.1136/ard.2010.129726. [DOI] [PubMed] [Google Scholar]
- 33.Felbo SK, Terslev L, Ostergaard M. Imaging in peripheral and axial psoriatic arthritis: contributions to diagnosis, follow-up, prognosis and knowledge of pathogenesis. Clin Exp Rheumatol. 2018;36(Suppl 114):24–34. [PubMed] [Google Scholar]
- 34.Fernandez-Sueiro JL, Willisch A, Pertega-Diaz S, Tasende JA, Fernandez-Lopez JC, Villar NO, et al. Validity of the Bath Ankylosing Spondylitis Disease Activity Index for the evaluation of disease activity in axial psoriatic arthritis. Arthritis Care Res (Hoboken) 2010;62:78–85. doi: 10.1002/acr.20017. [DOI] [PubMed] [Google Scholar]
- 35.Haroon M, Gallagher P, FitzGerald O. Inflammatory back pain criteria perform well in subset of patients with active axial psoriatic arthritis but not among patients with established axial disease. Ann Rheum Dis. 2019;78:1003–1004. doi: 10.1136/annrheumdis-2018-214583. [DOI] [PubMed] [Google Scholar]
- 36.Ibrahim A, Gladman DD, Thavaneswaran A, Eder L, Helliwell P, Cook RJ, et al. Sensitivity and specificity of radiographic scoring instruments for detecting change in axial psoriatic arthritis. Arthritis Care Res (Hoboken) 2017;69:1700–1705. doi: 10.1002/acr.23189. [DOI] [PubMed] [Google Scholar]
- 37.Kilic G, Kilic E, Nas K, Karkucak M, Capkin E, Dagli AZ, et al. Comparison of ASDAS and BASDAI as a measure of disease activity in axial psoriatic arthritis. Clin Rheumatol. 2015;34:515–521. doi: 10.1007/s10067-014-2734-8. [DOI] [PubMed] [Google Scholar]
- 38.Leung YY, Ho KW, Tam LS, Zhu TY, Kwok LW, Li TK, et al. Evaluation of spinal mobility measurements in predicting axial psoriatic arthritis. Clin Rheumatol. 2011;30:1157–1162. doi: 10.1007/s10067-011-1717-2. [DOI] [PubMed] [Google Scholar]
- 39.Lubrano E, Parsons WJ, Marchesoni A, Olivieri I, D'Angelo S, Cauli A, et al. The definition and measurement of axial psoriatic arthritis. J Rheumatol Suppl. 2015;93:40–42. doi: 10.3899/jrheum.150634. [DOI] [PubMed] [Google Scholar]
- 40.Mease PJ, Palmer JB, Liu M, Kavanaugh A, Pandurengan R, Ritchlin CT, et al. Influence of axial involvement on clinical characteristics of psoriatic arthritis: analysis from the Corrona Psoriatic Arthritis/Spondyloarthritis Registry. J Rheumatol. 2018;45:1389–1396. doi: 10.3899/jrheum.171094. [DOI] [PubMed] [Google Scholar]
- 41.Gottlieb A, Korman NJ, Gordon KB, Feldman SR, Lebwohl M, Koo JY, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 2. Psoriatic arthritis: overview and guidelines of care for treatment with an emphasis on the biologics. J Am Acad Dermatol. 2008;58:851–864. doi: 10.1016/j.jaad.2008.02.040. [DOI] [PubMed] [Google Scholar]
- 42.National Psoriasis Foundation. About psoriatic arthritis. 2019. https://www.Psoriasis.Org/about-psoriatic-arthritis. Accessed Aug 2020.
- 43.Walsh JA, McFadden ML, Morgan MD, Sawitzke AD, Duffin KC, Krueger GG, et al. Work productivity loss and fatigue in psoriatic arthritis. J Rheumatol. 2014;41:1670–1674. doi: 10.3899/jrheum.140259. [DOI] [PubMed] [Google Scholar]
- 44.Nash P, Lubrano E, Cauli A, Taylor WJ, Olivieri I, Gladman DD. Updated guidelines for the management of axial disease in psoriatic arthritis. J Rheumatol. 2014;41:2286–2289. doi: 10.3899/jrheum.140877. [DOI] [PubMed] [Google Scholar]
- 45.Aydin SZ, Kucuksahin O, Kilic L, Dogru A, Bayindir O, Ozisler C, et al. Axial psoriatic arthritis: the impact of underdiagnosed disease on outcomes in real life. Clin Rheumatol. 2018;37:3443–3448. doi: 10.1007/s10067-018-4173-4. [DOI] [PubMed] [Google Scholar]
- 46.Feld J, Ye JY, Chandran V, Inman RD, Haroon N, Cook R, et al. Is axial psoriatic arthritis distinct from ankylosing spondylitis with and without concomitant psoriasis? Rheumatology (Oxford) 2020;59:1340–1346. doi: 10.1093/rheumatology/kez457. [DOI] [PubMed] [Google Scholar]
- 47.Kim LH, Vail D, Azad TD, Bentley JP, Zhang Y, Ho AL, et al. Expenditures and health care utilization among adults with newly diagnosed low back and lower extremity pain. JAMA Netw Open. 2019;2:e193676. doi: 10.1001/jamanetworkopen.2019.3676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chien JJ, Bajwa ZH. What is mechanical back pain and how best to treat it? Curr Pain Headache Rep. 2008;12:406–411. doi: 10.1007/s11916-008-0069-3. [DOI] [PubMed] [Google Scholar]
- 49.Allen D, Hines EW, Pazdernik V, Konecny LT, Breitenbach E. Four-year review of presenteeism data among employees of a large United States health care system: a retrospective prevalence study. Hum Resour Health. 2018;16:59. doi: 10.1186/s12960-018-0321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Feld J, Chandran V, Gladman DD. What is axial psoriatic arthritis? J Rheumatol. 2018;45:1611–1613. doi: 10.3899/jrheum.180802. [DOI] [PubMed] [Google Scholar]
- 51.Gossec L, Baraliakos X, Kerschbaumer A, de Wit M, McInnes I, Dougados M, et al. EULAR recommendations for the management of psoriatic arthritis with pharmacological therapies: 2019 update. Ann Rheum Dis. 2020;79:700–712. doi: 10.1136/annrheumdis-2020-217159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Husted JA, Thavaneswaran A, Chandran V, Gladman DD. Incremental effects of comorbidity on quality of life in patients with psoriatic arthritis. J Rheumatol. 2013;40:1349–1356. doi: 10.3899/jrheum.121500. [DOI] [PubMed] [Google Scholar]
- 53.Brikman S, Furer V, Wollman J, Borok S, Matz H, Polachek A, et al. The effect of the presence of fibromyalgia on common clinical disease activity indices in patients with psoriatic arthritis: a cross-sectional study. J Rheumatol. 2016;43:1749–1754. doi: 10.3899/jrheum.151491. [DOI] [PubMed] [Google Scholar]
- 54.Salaffi F, De Angelis R, Carotti M, Gutierrez M, Sarzi-Puttini P, Atzeni F. Fibromyalgia in patients with axial spondyloarthritis: epidemiological profile and effect on measures of disease activity. Rheumatol Int. 2014;34:1103–1110. doi: 10.1007/s00296-014-2955-9. [DOI] [PubMed] [Google Scholar]
- 55.Graceffa D, Maiani E, Sperduti I, Ceralli F, Bonifati C. Clinical remission of psoriatic arthritis in patients receiving continuous biological therapies for 1 year: the experience of an outpatient dermatological clinic for psoriasis. Clin Exp Dermatol. 2015;40:136–141. doi: 10.1111/ced.12504. [DOI] [PubMed] [Google Scholar]
- 56.Marchesoni A, Atzeni F, Spadaro A, Lubrano E, Provenzano G, Cauli A, et al. Identification of the clinical features distinguishing psoriatic arthritis and fibromyalgia. J Rheumatol. 2012;39:849–855. doi: 10.3899/jrheum.110893. [DOI] [PubMed] [Google Scholar]
- 57.Marchesoni A, De Marco G, Merashli M, McKenna F, Tinazzi I, Marzo-Ortega H, et al. The problem in differentiation between psoriatic-related polyenthesitis and fibromyalgia. Rheumatology (Oxford) 2018;57:32–40. doi: 10.1093/rheumatology/kex079. [DOI] [PubMed] [Google Scholar]
- 58.Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RL, et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46:319–329. doi: 10.1016/j.semarthrit.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 59.Wolfe F, Butler SH, Fitzcharles M, Häuser W, Katz RL, Mease PJ, et al. Revised chronic widespread pain criteria: development from and integration with fibromyalgia criteria. Scand J Pain. 2019;20:77–86. doi: 10.1515/sjpain-2019-0054. [DOI] [PubMed] [Google Scholar]
- 60.Sieper J, van der Heijde D, Landewe R, Brandt J, Burgos-Vagas R, Collantes-Estevez E, et al. New criteria for inflammatory back pain in patients with chronic back pain: a real patient exercise by experts from the Assessment of SpondyloArthritis international Society (ASAS) Ann Rheum Dis. 2009;68:784–788. doi: 10.1136/ard.2008.101501. [DOI] [PubMed] [Google Scholar]
- 61.Dubreuil M, Sieper J. Editorial: inflammatory back pain and axial spondyloarthritis: lessons for clinical practice and epidemiologic research. Arthritis Rheumatol. 2018;70:981–983. doi: 10.1002/art.40462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chou R. In the clinic. Low back pain. Ann Intern Med. 2014;160:ITC6–1. doi: 10.7326/0003-4819-160-11-201406030-01006. [DOI] [PubMed] [Google Scholar]
- 63.de Koning A, Schoones JW, van der Heijde D, van Gaalen FA. Pathophysiology of axial spondyloarthritis: consensus and controversies. Eur J Clin Invest. 2018;48:e12913. doi: 10.1111/eci.12913. [DOI] [PubMed] [Google Scholar]
- 64.Jacques P, Lambrecht S, Verheugen E, Pauwels E, Kollias G, Armaka M, et al. Proof of concept: enthesitis and new bone formation in spondyloarthritis are driven by mechanical strain and stromal cells. Ann Rheum Dis. 2014;73:437–445. doi: 10.1136/annrheumdis-2013-203643. [DOI] [PubMed] [Google Scholar]
- 65.Calin A, Porta J, Fries JF, Schurman DJ. Clinical history as a screening test for ankylosing spondylitis. JAMA. 1977;237:2613–2614. [PubMed] [Google Scholar]
- 66.Rudwaleit M, Metter A, Listing J, Sieper J, Braun J. Inflammatory back pain in ankylosing spondylitis: a reassessment of the clinical history for application as classification and diagnostic criteria. Arthritis Rheum. 2006;54:569–578. doi: 10.1002/art.21619. [DOI] [PubMed] [Google Scholar]
- 67.Akgul O, Ozgocmen S. Classification criteria for spondyloarthropathies. World J Orthop. 2011;2(107):15. doi: 10.5312/wjo.v2.i12.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Baraliakos X, Coates LC, Gossec L, Jeka S, Varela AM, Schulz B, et al. OP0235 Secukinumab improves axial manifestations in patients with psoriatic arthritis and inadequate response to NSAIDs: primary analysis of the MAXIMISE trial. Ann Rheum Dis. 2019;78(Suppl 2):195–196. [Google Scholar]
- 69.Feld J, Chandran V, Haroon N, Inman R, Gladman D. Axial disease in psoriatic arthritis and ankylosing spondylitis: a critical comparison. Nat Rev Rheumatol. 2018;14:363–371. doi: 10.1038/s41584-018-0006-8. [DOI] [PubMed] [Google Scholar]
- 70.Chandran V, Barrett J, Schentag CT, Farewell VT, Gladman DD. Axial psoriatic arthritis: update on a long-term prospective study. J Rheumatol. 2009;36:2744–2750. doi: 10.3899/jrheum.090412. [DOI] [PubMed] [Google Scholar]
- 71.Queiro R, Belzunegui J, Gonzalez C, De DJ, Sarasqueta C, Torre JC, et al. Clinically asymptomatic axial disease in psoriatic spondyloarthropathy. A retrospective study. Clin Rheumatol. 2002;21:10–13. doi: 10.1007/s100670200003. [DOI] [PubMed] [Google Scholar]
- 72.Queiro R, Alperi M, Lopez A, Sarasqueta C, Riestra JL, Ballina J. Clinical expression, but not disease outcome, may vary according to age at disease onset in psoriatic spondylitis. Jt Bone Spine. 2008;75:544–547. doi: 10.1016/j.jbspin.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 73.Arnbak B, Jurik AG, Jensen TS, Manniche C. Association between inflammatory back pain characteristics and magnetic resonance imaging findings in the spine and sacroiliac joints. Arthritis Care Res (Hoboken) 2018;70:244–251. doi: 10.1002/acr.23259. [DOI] [PubMed] [Google Scholar]
- 74.Gladman DD. Inflammatory spinal disease in psoriatic arthritis: a report from the GRAPPA 2010 annual meeting. J Rheumatol. 2012;39:418–420. doi: 10.3899/jrheum.111238. [DOI] [PubMed] [Google Scholar]
- 75.Coates LC, Hodgson R, Conaghan PG, Freeston JE. MRI and ultrasonography for diagnosis and monitoring of psoriatic arthritis. Best Pract Res Clin Rheumatol. 2012;26:805–822. doi: 10.1016/j.berh.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 76.Gossec L, Smolen JS, Ramiro S, de Wit M, Cutolo M, Dougados M, et al. European League Against Rheumatism (EULAR) recommendations for the management of psoriatic arthritis with pharmacological therapies: 2015 update. Ann Rheum Dis. 2016;75:499–510. doi: 10.1136/annrheumdis-2015-208337. [DOI] [PubMed] [Google Scholar]
- 77.Maksymowych WP, Lambert RG, Ostergaard M, Pedersen SJ, Machado PM, Weber U, et al. MRI lesions in the sacroiliac joints of patients with spondyloarthritis: an update of definitions and validation by the ASAS MRI working group. Ann Rheum Dis. 2019;78:1550–1558. doi: 10.1136/annrheumdis-2019-215589. [DOI] [PubMed] [Google Scholar]
- 78.Ostergaard M, Lambert RG. Imaging in ankylosing spondylitis. Ther Adv Musculoskelet Dis. 2012;4:301–311. doi: 10.1177/1759720X11436240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ureyen SB, Ivory C, Kalyoncu U, Karsh J, Aydin SZ. What does evidence-based medicine tell us about treatments for different subtypes of psoriatic arthritis? A systematic literature review on randomized controlled trials. Rheumatol Adv Pract. 2018;2:rkx019. doi: 10.1093/rap/rkx019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lukas C, Cyteval C, Dougados M, Weber U. MRI for diagnosis of axial spondyloarthritis: major advance with critical limitations ‘Not everything that glisters is gold (standard)’. RMD Open. 2018;4:e000586. doi: 10.1136/rmdopen-2017-000586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Molinos M, Almeida CR, Caldeira J, Cunha C, Goncalves RM, Barbosa MA. Inflammation in intervertebral disc degeneration and regeneration. J R Soc Interface. 2015;12:20141191. doi: 10.1098/rsif.2015.0429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Risbud MV, Shapiro IM. Role of cytokines in intervertebral disc degeneration: pain and disc content. Nat Rev Rheumatol. 2014;10:44–56. doi: 10.1038/nrrheum.2013.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Arnbak B, Hendricks O, Horslev-Petersen K, Jurik AG, Pedersen SJ, Ostergaard M, et al. The discriminative value of inflammatory back pain in patients with persistent low back pain. Scand J Rheumatol. 2016;45:321–328. doi: 10.3109/03009742.2015.1105289. [DOI] [PubMed] [Google Scholar]
- 84.Ghosh N, Ruderman EM. Nonradiographic axial spondyloarthritis: clinical and therapeutic relevance. Arthritis Res Ther. 2017;19:286. doi: 10.1186/s13075-017-1493-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dubash S, McGonagle D, Marzo-Ortega H. New advances in the understanding and treatment of axial spondyloarthritis: from chance to choice. Ther Adv Chronic Dis. 2018;9:77–87. doi: 10.1177/2040622317743486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Poddubnyy D, Rudwaleit M, Haibel H, Listing J, Marker-Hermann E, Zeidler H, et al. Rates and predictors of radiographic sacroiliitis progression over 2 years in patients with axial spondyloarthritis. Ann Rheum Dis. 2011;70:1369–1374. doi: 10.1136/ard.2010.145995. [DOI] [PubMed] [Google Scholar]
- 87.Haroon N, Inman RD, Learch TJ, Weisman MH, Lee M, Rahbar MH, et al. The impact of tumor necrosis factor α inhibitors on radiographic progression in ankylosing spondylitis. Arthritis Rheum. 2013;65:2645–2654. doi: 10.1002/art.38070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kroon F, Landewé R, Dougados M, van der Heijde D. Continuous NSAID use reverts the effects of inflammation on radiographic progression in patients with ankylosing spondylitis. Ann Rheum Dis. 2012;71:1623–1629. doi: 10.1136/annrheumdis-2012-201370. [DOI] [PubMed] [Google Scholar]
- 89.Lubrano E, Spadaro A. Axial psoriatic arthritis: an intriguing clinical entity or a subset of an intriguing disease? Clin Rheumatol. 2012;31:1027–1032. doi: 10.1007/s10067-012-1990-8. [DOI] [PubMed] [Google Scholar]
- 90.Coates LC, Helliwell PS. Psoriatic arthritis: state of the art review. Clin Med (Lond) 2017;17:65–70. doi: 10.7861/clinmedicine.17-1-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jadon DR, Sengupta R, Nightingale A, Lindsay M, Korendowych E, Robinson G, et al. Axial Disease in Psoriatic Arthritis study: defining the clinical and radiographic phenotype of psoriatic spondyloarthritis. Ann Rheum Dis. 2017;76:701–707. doi: 10.1136/annrheumdis-2016-209853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Haroon M, Ahmad M, Baig MN, Mason O, Rice J, FitzGerald O. Inflammatory back pain in psoriatic arthritis is significantly more responsive to corticosteroids compared to back pain in ankylosing spondylitis: a prospective, open-labelled, controlled pilot study. Arthritis Res Ther. 2018;20:73. doi: 10.1186/s13075-018-1565-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Coates LC, Kavanaugh A, Mease PJ, Soriano ER, Laura Acosta-Felquer M, Armstrong AW, et al. Group for Research and Assessment of Psoriasis and Psoriatic Arthritis 2015 treatment recommendations for psoriatic arthritis. Arthritis Rheumatol. 2016;68:1060–1071. doi: 10.1002/art.39573. [DOI] [PubMed] [Google Scholar]
- 94.Baeten D, Østergaard M, Wei JC, Sieper J, Järvinen P, Tam LS, et al. Risankizumab, an IL-23 inhibitor, for ankylosing spondylitis: results of a randomised, double-blind, placebo-controlled, proof-of-concept, dose-finding phase 2 study. Ann Rheum Dis. 2018;77:1295–1302. doi: 10.1136/annrheumdis-2018-213328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Deodhar A, Poddubnyy D, Pacheco-Tena C, Salvarani C, Lespessailles E, Rahman P, et al. Efficacy and safety of ixekizumab in the treatment of radiographic axial spondyloarthritis: sixteen-week results from a phase III randomized, double-blind, placebo-controlled trial in patients with prior inadequate response to or intolerance of tumor necrosis factor inhibitors. Arthritis Rheumatol. 2019;71:599–611. doi: 10.1002/art.40753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mease P, Roussou E, Burmester GR, Goupille P, Gottlieb A, Moriarty SR, et al. Safety of ixekizumab in patients with psoriatic arthritis: results from a pooled analysis of three clinical trials. Arthritis Care Res (Hoboken) 2019;71:367–378. doi: 10.1002/acr.23738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mease PJ, Smolen JS, Behrens F, Nash P, Liu Leage S, Li L, et al. A head-to-head comparison of the efficacy and safety of ixekizumab and adalimumab in biological-naïve patients with active psoriatic arthritis: 24-week results of a randomised, open-label, blinded-assessor trial. Ann Rheum Dis. 2020;79:123–131. doi: 10.1136/annrheumdis-2019-215386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Deodhar A, Blanco R, Dokoupilova E, Hall S, Kameda H, Kivitz AJ, et al. Secukinumab improves signs and symptoms of non-radiographic axial spondyloarthritis: primary results of a randomized controlled phase III study. Arthritis Rheumatol. 2020 Aug 7. (Epub ahead of print). [DOI] [PMC free article] [PubMed]
- 99.Baeten D, Sieper J, Braun J, Baraliakos X, Dougados M, Emery P, et al. Secukinumab, an interleukin-17A inhibitor, in ankylosing spondylitis. N Engl J Med. 2015;373:2534–2548. doi: 10.1056/NEJMoa1505066. [DOI] [PubMed] [Google Scholar]
- 100.Deodhar A, Gensler LS, Sieper J, Clark M, Calderon C, Wang Y, et al. Three multicenter, randomized, double-blind, placebo-controlled studies evaluating the efficacy and safety of ustekinumab in axial spondyloarthritis. Arthritis Rheum. 2019;71:258–270. doi: 10.1002/art.40728. [DOI] [PubMed] [Google Scholar]
- 101.Helliwell PS, Gladman DD, Chakravarty SD, Kafka S, Karyekar CS, You Y, et al. Effects of ustekinumab on spondylitis-associated endpoints in TNFi-naïve active psoriatic arthritis patients with physician-reported spondylitis: pooled results from two phase 3, randomised, controlled trials. RMD Open. 2020;6:e001149. doi: 10.1136/rmdopen-2019-001149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane reviews. Cochrane Database Syst Rev. 2017;1:CD011279. doi: 10.1002/14651858.CD011279.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Helliwell PS. Axial disease in psoriatic arthritis. Rheumatology (Oxford) 2020;59:1193–1195. doi: 10.1093/rheumatology/kez629. [DOI] [PubMed] [Google Scholar]
- 104.Goel N, Coates LC, De Marco G, Eder L, FitzGerald O, Helliwell PS, et al. GRAPPA 2019 project report. J Rheumatol Suppl. 2020;96:53–57. doi: 10.3899/jrheum.200129. [DOI] [PubMed] [Google Scholar]
- 105.ClinicalTrials.gov. Study of the efficacy and safety of secukinumab in participants with active psoriatic arthritis with axial skeleton involvement (MAXIMISE). https://clinicaltrials.gov/ct2/show/NCT02721966?cond=axial+psoriatic+arthritis&rank=4. Accessed Aug 2020.
- 106.ClinicalTrials.gov. Tofacitinib for reduction of spinal inflammation in patients with psoriatic arthritis presenting with axial involvement (PASTOR). https://clinicaltrials.gov/ct2/show/NCT04062695?cond=axial+psoriatic+arthritis&rank=7. Accessed Aug 2020.
- 107.Baraliakos X, Gossec L, Pournara E, Jeka S, Blanco R, D'Angelo S, et al. Secukinumab improves clinical and imaging outcomes in patients with psoriatic arthritis and axial manifestations with inadequate response to NSAIDs: week 52 results from the MAXIMISE trial [abstract OP0053] Ann Rheum Dis. 2020;79(Suppl 1):35–6. [Google Scholar]
- 108.Hospital for Special Surgery. HSS researchers launch study to measure bone effects of new rheumatologic agent. 2018. https://news.hss.edu/hss-researchers-launch-study-to-measure-bone-effects-of-new-rheumatologic-agent/. Accessed Aug 2020.
- 109.Gottlieb A, Gratacos J, Dikranian A, van Tubergen A, Fallon L, Emir B, et al. Treatment patterns, unmet need, and impact on patient-reported outcomes of psoriatic arthritis in the United States and Europe. Rheumatol Int. 2019;39:121–130. doi: 10.1007/s00296-018-4195-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Winthrop KL, Strand V, van der Heijde DM, Mease PJ, Crow MK, Weinblatt M, et al. The unmet need in rheumatology: reports from the targeted therapies meeting 2016. Clin Exp Rheumatol. 2016;34(4 Suppl 98):69–76. [PubMed] [Google Scholar]
- 111.Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 Suppl):S2–15. doi: 10.1016/j.pain.2010.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Millerand M, Berenbaum F, Jacques C. Danger signals and inflammaging in osteoarthritis. Clin Exp Rheumatol. 2019;37(Suppl 120):48–56. [PubMed] [Google Scholar]
- 113.McGonagle D, Hermann KG, Tan AL. Differentiation between osteoarthritis and psoriatic arthritis: implications for pathogenesis and treatment in the biologic therapy era. Rheumatology (Oxford) 2015;54:29–38. doi: 10.1093/rheumatology/keu328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Clauw DJ, Hassett AL. The role of centralised pain in osteoarthritis. Clin Exp Rheumatol. 2017;35(Suppl 107):79–84. [PubMed] [Google Scholar]
- 115.Fitzgerald G, Gallagher P, O'Shea FD. Multimorbidity in axial spondyloarthropathy and its association with disease outcomes: results from the Ankylosing Spondylitis Registry of Ireland cohort. J Rheumatol. 2020;47:218–226. doi: 10.3899/jrheum.181415. [DOI] [PubMed] [Google Scholar]
- 116.Chen J, Veras MM, Liu C, Lin J. Methotrexate for ankylosing spondylitis. Cochrane Database Syst Rev. 2013;2:CD004524. doi: 10.1002/14651858.CD004524.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]