Abstract
Introduction
Spontaneous perforation of the colon (SPC) is a rare disease characterized by sudden perforation of a clinically healthy colon in the absence of underlying disease or trauma. The aim of reporting this case is to highlight this surgical emergency in terms of clinical presentations, surgical management and outcomes.
Presentation of case
A 68 year-old male with history of diabetes mellitus, hypertension and chronic constipation on daily laxatives presented to the emergency department with a diffuse abdominal pain and distention for 4 days associated with vomiting and absence of defecation where he was prescribed phosphate rectal enemas. Patient was in sepsis with generalized abdominal tenderness and distention. Intraoperative findings of feculent peritonitis with isolated cecal perforation was identified, for which a right hemicolectomy with end ileostomy was performed.
Discussion
The first case was described in a woman presented with spontaneous rectum rupture by Brodie in 1827, with a less than 100 cases being reported in literature. In 1984, spontaneous perforations were classified into either “stercoral” or “idiopathic” perforations. More than 60% of colonic perforations were reported in the sigmoid or at the recto-sigmoid junction, mainly at the anti-mesenteric border, making spontaneous cecal perforation a very uncommon condition. Cecal perforation is associated with high mortality in the range of 30%–72%.
Conclusion
The outcome of SPC depends on multiple factors like onset of perforation, peritoneal contamination, and time of intervention. Regardless the surgical technique, early detection and surgical management are the main strategies associated with improving the outcomes.
Keywords: Spontaneous perforation of the colon, Cecal perforation, Surgery
Highlights
-
•
Spontaneous perforation of the cecum can be classified as sterocral or idiopathic perforations.
-
•
Early recognition of the pathology and prompt intervention is critical for management.
-
•
A high mortality rates associated with cecal perforation might be related to the delay of diagnosis.
-
•
No surgical intervention is reported to be superior in terms of mortality.
1. Introduction
Spontaneous perforation of the colon (SPC) is a rare disease characterized by sudden perforation of a clinically healthy colon in the absence of underlying disease or trauma. Fewer than 100 cases have been reported in the literature to date [1]. It can be classified into either stercoral or idiopathic.
Patient clinical presentation can be variable with majority of cases presented with feature of diffuse peritonitis. Being an infrequent pathology, spontaneous cecal perforation is mostly an intraoperative diagnosis, which is associated with high mortality rates.
The aim of reporting this case is to highlight this surgical emergency in terms of clinical presentations, surgical management and outcomes.
2. Case presentation
A 68 year-old male with history of diabetes mellitus, hypertension and chronic constipation on daily laxatives presented to the ER with a diffuse abdominal pain and distention for 4 days associated with vomiting and absence of defecation where he was prescribed phosphate rectal enemas. Patient was on insulin, antihypertensive medications with no known drug allergies. Patient family history was unremarkable for malignancies. Physically, the patient was conscious, blood pressure 100/60 mmHg, Pulse 110/min, RR 24/min and body temperature 38.4 °C. He presented with abdominal distention and generalized guarding with rebound tenderness and absence of bowel sounds with no surgical scars. On digital rectal exam (DRE), the rectum was collapsed and empty.
His laboratory findings were leukocytosis (18,000/mm3) with neutrophilia, hemoglobin level of 11 g/dl, blood urea nitrogen and creatinine were elevated, electrolyte and coagulation profile were normal. Arterial blood gas analysis showed a non-compensated metabolic acidosis. The diagnosis of acute generalized peritonitis was the primary diagnosis that indicated the need for urgent laparotomy. Patient and his family counseled regarding the general condition, management options and possible outcomes including the high risk of mortality because of delayed presentation and clinical features of sepsis.
Preoperative resuscitation initiated using crystalloids, and an exploratory laparotomy performed. Intraoperative findings showed Large Amount of Feces, food particles all over the abdominal cavity and an anti-mesenteric cecal perforation measuring approximately 1 × 1 cm, there was no evidence of local inflammatory process or obstruction distal to the cecum down to the rectum (Fig. 1).
Fig. 1.
Intraoperative finding of an isolated cecal perforation with feculent material.
Peritoneal cavity irrigation with saline was performed, and the cecal defect was primarily sutured to control the leak of feculent material. Right Hemicolectomy with end ileostomy and transverse colon mucous fistula performed as a definitive surgery, and 2 large abdominal drains placed, the operation performed by consultant surgeon. Postoperatively, prophylaxis for thromboembolism, analgesia, and wide spectrum antibiotics covering and gram-negative and anaerobic bacteria were administered. Patient recovery was uneventful in the first 24 hours and he tolerate the treatment on antibiotics; later on, he started to have a decrease in consciousness level, persistent hyperthermia and tachycardia. Patient's new coagulation profile showed evidence of disseminated intravascular coagulation (DIC), and he developed a septic shock and passed away on the 3rd postoperative day.
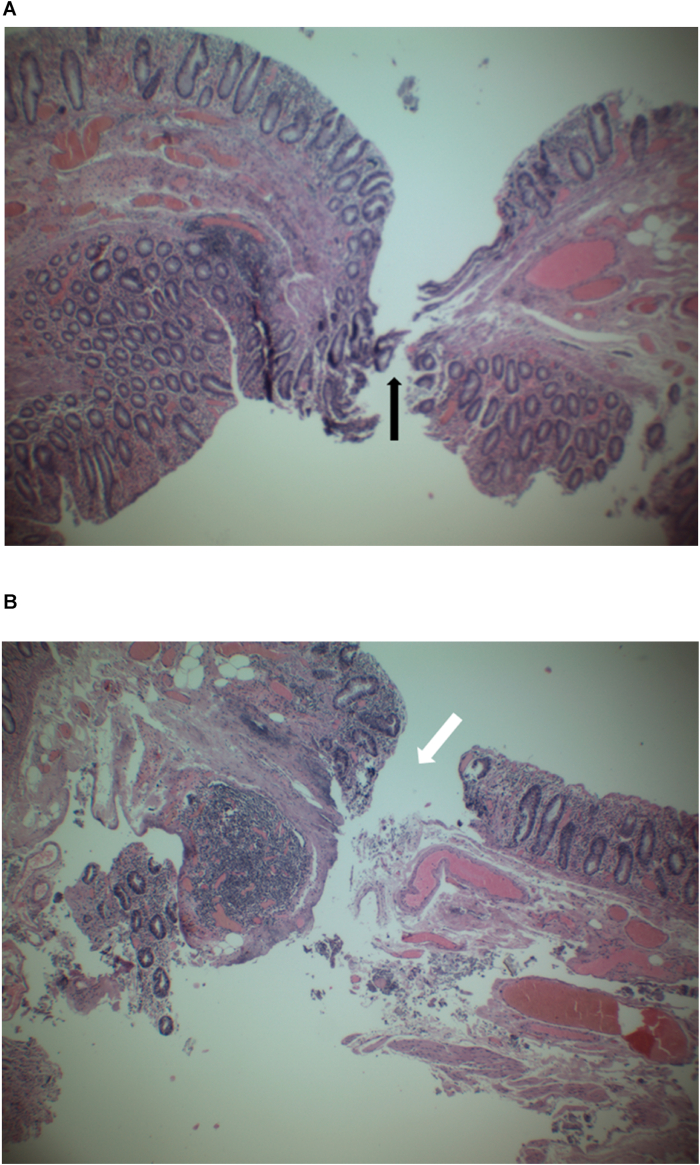
The final histopathology report showed an isolated cecal perforation with congested edges without local inflammatory process or tissue necrosis at ulcer edge (Fig. 2). There was no evidence of malignancy in the resected specimen.
Fig. 2.
A and 2B low power views of sections from the cecal perforation site (arrows) showing submucosal congestion, but otherwise normal colonic mucosa (Both are Hematoxylin and Eosine stained sections X100).
3. Discussion
Spontaneous cecal perforation is a sudden perforation of a previously clinically healthy colon in the absence of underlying disease or injury. Fewer than 100 cases have been reported in the literature to date [1]. Brodie first described spontaneous colonic perforation in 1827, when he described a case of a middle aged woman with spontaneous rectal perforation. In 1984, J.A. Berry classified spontaneous perforations into either stercoral or idiopathic perforations. This classification was based on underlying etiologic and pathologic factors [2]. The Stercoral perforation is characterized by a rounded or ovoid shaped defect with underlying necrotic and inflammatory edges in the absence of significant case like injury, obstruction, tumors and diverticulosis [3].
Maurer adopted criteria for diagnosing stercoral perforation based on shape of the defect, diameter, relation to the mesentery and presence of fecalomas protruding through the defect. Microscopically, there is pressure necrosis or ulcer in presence of chronic inflammatory reaction around the perforation. The presence of any additional pathology leads to exclude it form this category [3].
Two hypotheses proposed to explain underlying cause for idiopathic perforations. The first is vascular theory while the second one is related to constitutional weakness of the bowel wall with increased intraluminal pressure [4]. Both conditions are difficult to distinguish at surgery even they are different macroscopically and microscopically, so pathological examination is essential to reach the diagnosis [5]. Elderly and infants age group represent the majority of cases [6].
Spontaneous viscous perforations are mostly located at the anti-mesenteric border of the sigmoid colon and recto-sigmoid junction (60%), while spontaneous cecal perforations are uncommon [1,7]. Being an infrequent pathology, spontaneous cecal perforation is mostly an intraoperative diagnosis as in our patient. Various techniques have been described in literature for the surgical management of such cases, including primary closure of the defect with protective ileostomy, primary closure with or without omentoplasty and right hemicolectomy. In cases of uncomplicated perforations and in the absence of severe inflammation, primary repair with omental patch can be considered otherwise right hemicolectomy is advised. No one technique has been proved superior in terms of final clinical outcome [[8], [9], [10]].
Mortality rates associated with cecal perforation is high; it ranges from 30% to 72% [11]. The outcome of SPC depends on multiple factors mainly the onset of perforation, degree of peritoneal contamination, and time of intervention [1]. This case is reported in concordance with the SCARE 2018 criteria [12].
4. Conclusion
Idiopathic spontaneous cecal perforation is a very rare disease that is associated with increased rate of morbidity and mortality. Regardless the surgical technique, early detection and surgical management are the main strategies associated with improving the outcomes, this case increase our attention to idiopathic cecal perforation diagnosis and management, the learning point regards our knowledge is to start management as soon as possible regardless the type of surgical technique.
For early diagnosis for such cases, we recommend full blood investigation including complete blood count, kidney function test with blood gases followed immediately with CT scan.
5. Declaration of conflicting interests
The author(s) declared no potential conflicts of interests with respect to research, authorship and/or publication of the article.
Ethics approval
Reporting this case was ethically approved by our institution.
Funding
The author(s) received no financial support for the research, authorship and/or publication of this article.
Author contribution
Study design, writing, and the final approval of the manuscript: Dr Hamzeh Al-Balas.
Study design, Literature review and Data collection: Dr. Mahmoud Al-Balas.
Literature review, patient follow up and manuscript revision: Mohammad Al-Wiswasy.
6. Trial registry number
1. Name of the registry:
2. Unique Identifying number or registration ID:
3. Hyperlink to your specific registration (must be publicly accessible and will be checked):
Non applicable.
Guarantor
Dr. Mahmoud Al-Balas.
Assistant professor of surgery.
Department of general and special surgery.
Faculty of medicine.
Hashemite university.
Zarqa, Jordan.
7. Informed consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
8. Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
No conflict of interest between authors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2020.11.047.
Contributor Information
Hamzeh Al-Balas, Email: hamzeh.albalas@hu.edu.jo, D.hbalas87@gmail.com.
Mahmoud Al-Balas, Email: Mahmoud_albalas@hu.edu.jo.
Mohammad Al-Wiswasy, Email: mkalwiswasy@yahoo.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Makki A.M., Hejazi S., Zaidi N.H., Johari A., Altaf A. Spontaneous perforation of colon: a case report and review of literature. Case Rep. Clin. Med. 2014;3:392–397. [Google Scholar]
- 2.Al Shukry S. Spontaneous perforation of the colon: clinical review of five episodes in four patients. omj. 2009;24:137–141. doi: 10.5001/omj.2009.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maurer C.A., Renzulli P., Mazzucchelli L., Egger B., Seiler C.A., Buchler M.W. Use of accurate diagnostic criteria may increase incidence of stercoral perforation of the colon. Dis. Colon Rectum. 2000;43:991–998. doi: 10.1007/BF02237366. [DOI] [PubMed] [Google Scholar]
- 4.Serpell J.W., Nicholls R.J. Stercoral perforation of the colon. Br. J. Surg. 1990;77:1325–1329. doi: 10.1002/bjs.1800771204. [DOI] [PubMed] [Google Scholar]
- 5.Kasahara Y., Matsumoto H., Umemura H., Shirafa S., Kuyama T. Idiopathic perforation of the sigmoid colon in Japan. World J. Surg. 1981;5:125–130. doi: 10.1007/BF01657857. [DOI] [PubMed] [Google Scholar]
- 6.Kumar A., Griwan M.G., Naresh P. Spontaneous colonic perforation—rare presentation. J. Surg. Acad. 2013;3 [Google Scholar]
- 7.Yang Bo, Ni Huai-Kun. Diagnosis and treatment of spontaneous colonic perforation: analysis of 10 cases. World J. Gastroenterol. 2008;14(28):4569–4572. doi: 10.3748/wjg.14.4569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kouam Cyrille, Passang Ouasso, Guifo Marc-Leroy, Atem Nkolaka. Spontaneous cecal perforation in a 40-yearold pregnant woman treated by primary repair and omental patch: a case report. J. Med. Case Rep. 2017;11:162. doi: 10.1186/s13256-017-1336-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong C.S., Naqvi S.A. Appendicular perforation at the base of the caecum, a rare operative challenge in acute appendicitis, a literature review. World J. Emerg. Surg. 2011;6:36. doi: 10.1186/1749-7922-6-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Butt U.I., Mansoor R., Khan A., Siddique S., Khan H.S., Iftikhar M.A. An unusual cause of right iliac fossa pain: cecal diverticulum perforation. J Coll Physicians Surg Pak. 2015;25(Suppl 2):S115–S116. doi: 10.2015/JCPSP.S411S116. [DOI] [PubMed] [Google Scholar]
- 11.Laskin M.D., Tessler K., Kives S. Cecal perforation due to paralytic ileus following primary caesarean section. J. Obstet. Gynaecol. Can. 2009;31:167–171. doi: 10.1016/s1701-2163(16)34102-0. [DOI] [PubMed] [Google Scholar]
- 12.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the Scare Group The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.