Abstract
Ochrobactrum species are non-enteric, Gram-negative organisms that are closely related to the genus Brucella. Since the designation of the genus in 1988, several distinct species have now been characterised and implicated as opportunistic pathogens in multiple outbreaks. Here, we examine the genus, its members, diagnostic tools used for identification, data from recent Ochrobactrum whole genome sequencing and the pathogenicity associated with reported Ochrobactrum infections. This review identified 128 instances of Ochrobactrum spp. infections that have been discussed in the literature. These findings indicate that infection review programs should consider investigation of possible Ochrobactrum spp. outbreaks if these bacteria are clinically isolated in more than one patient and that Ochrobactrum spp. are more important pathogens than previously thought.
Keywords: Ochrobactrum, nosocomial infection, environmental bacteria
1. Introduction
Gram-negative, non-fermenting bacteria are an emergent worry in medical situations and are becoming a growing cause of severe infections. Pathogens of this type are opportunistic and include many different bacterial species, such as Ralstonia spp., Pseudomonas aeruginosa, Sphingomonas paucimobilis and Brevundimonas spp. [1,2,3,4,5]. Gram-negative, non-fermenting bacteria can infect both patients undergoing treatments and individuals outside of a clinical setting with various underlying conditions or diseases. Another type of these bacteria are the members of the α-proteobacterial genus Ochrobactrum [6].
Ochrobactrum spp. are found in a wide variety of environments including water, aircraft water, soil, plants and animals [6,7,8,9,10,11,12]. Several Ochrobactrum spp. have been investigated for their potential to degrade xenobiotic pollutants and for heavy metal detoxification under a variety of environmental conditions [13,14,15,16]. Ochrobactrum spp. are very closely related to brucellae, and even though they are considered to be of low virulence, they have increasingly been found to cause infections (some serious including endocarditis and septicaemia) in immunocompetent hosts [17,18].
Investigation of the scientific/medical literature presented a wide variety of infections resultant from Ochrobactrum spp. and these were resistant to wide variety of antibiotics. Our data point to the genus being a more common pathogen than previously supposed, with many of the infections/conditions caused by Ochrobactrum spp. being aggressive and debilitating. The overall aim of this work is to present a summary of the types of Ochrobactrum spp. infections, any underlying disorders/illnesses in patients that accompany these infections and the potential treatments that can be used in the management of infections to support medical specialists.
2. Genus Ochrobactrum
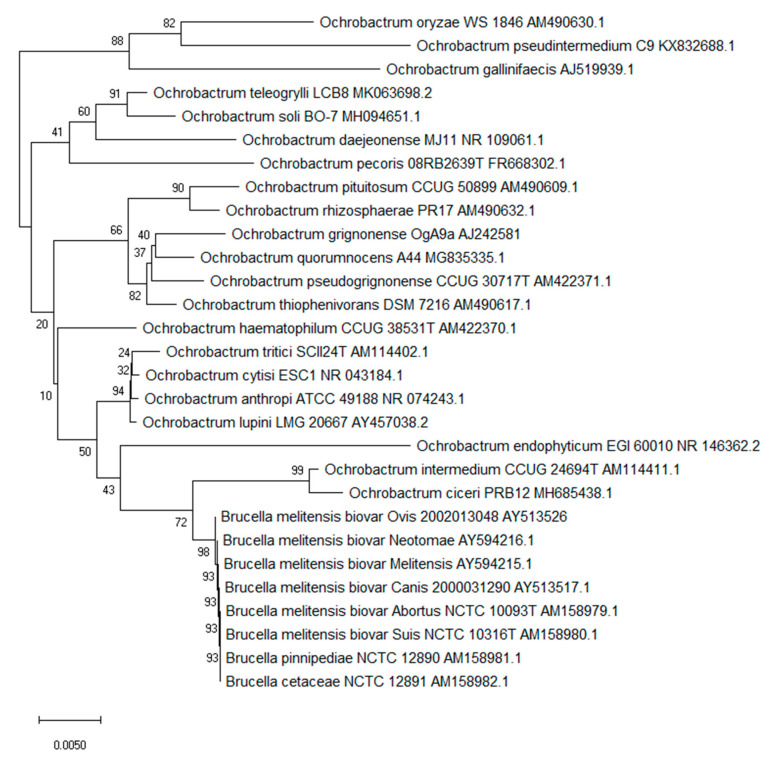
The genus Ochrobactrum emerged from what was previously categorised as the CDC group VD1-2. The type species Ochrobactrum anthropi had previous been called Achromobacter VD based on the Special Bacteriology Section of the US Center for Disease Control [19]. Initial results indicate members of the group grew on MacConkey agar producing catalase, oxidase and urease; strains could be Gram-negative to variable [20]. However, the taxonomic position of Achromobacter became complicated and the name Achromobacter and related CDC group VD were no longer accepted by Bergeys Manual [19] leading to a new classification and the emergence of the genus Ochrobactrum [21]. Ochrobactrum spp. are phylogenetically related to members of the alpha-2 subdivision of Proteobacteria. They are catalogued on the Brucella rRNA branch of rRNA superfamily IV. Thus, from the previous CDC group Vd, a novel genus and a new species, Ochrobactrum anthropi, was proposed [21,22]. The type strain was Gram-negative, aerobic, rod shaped, non-pigmented and motile. It produced acid from a selection of carbohydrates and reduced both nitrate and nitrite and possessed a GC ratio between 56 to 59% [21]. Almost all 56 strains categorised as CDC GroupVD that were used to support the new genus Ochrobactrum came from various human clinical specimens. Since the initial description of O. anthropi, several other species have since been described (Table 1 and Figure 1). Certain Ochrobactrum spp. can be opportunistic pathogens especially in a hospital environment with the majority of reported cases due to hospital-acquired infections in patients with indwelling and invasive medical devices, including central venous catheters and drainage tubes [23]. In addition, the organism shows widespread resistance to penicillins and other antibiotics that cause clinical management issues with immunocompromised hosts [24,25]. The phylogenetic relationship between all described Ochrobactrum spp. can be seen in Figure 1.
Table 1.
List of current accepted Ochrobactrum species.
| Species | Isolation | Genome Sequences | Reference |
|---|---|---|---|
| Ochrobactrum anthropi | Clinical isolate | Strain: OAB; Size: 4.9 Mbp; Ref Genome: GCA_000742955.1 (41 genomes) | [22] |
| Ochrobactrum ciceri | Nodules of Cicer | No Genome | [26] |
| Ochrobactrum cytisi | Cystisus nodules | Strain: IPA7.2; Size: 5.96 Mpb; Ref Genome: GCA_001876955.1 (1 genome) | [27] |
| Ochrobactrum daejeonense | Sludge | Strain: JCM 16234; Size: 4.8 Mbp, Ref Genome: GCA_012103095.1 (1 genome) | [28] |
| Ochrobactrum endophyticum | Roots of Glycyrrhiza | No Genome | [29] |
| Ochrobactrum gallinifaecis | Chicken faeces | Strain: ISO196; Ref Genome: GCF_006476605.1; Size: 3.74 Mbp (1 genome) | [11] |
| Ochrobactrum grignonense | Wheat Roots | Strain: OgA9a; Size: 4.84 Mbp; Ref Genome: NZ_NNRL00000000.1 (1 genome) | [9] |
| Ochrobactrum haematophilum | Clinical Isolate | Strain: LISuc1; Size: 4.91 Mbp; Ref Genome: GCA_003550135.1 (3 genomes) | [30] |
| Ochrobactrum intermedium | Human blood | Strain: NCTC12171; Size: 4.73 Mbp; Ref Genome: GCA_900454225.1 (18 genomes) | [22] |
| Ochrobactrum lupini | Lupinus albus rhizosphere | Strain: LUP21; Size: 5.5 Mbp; Ref Genome: GCA_002252535.1 (2 genomes) | [31,32] * |
| Ochrobactrum oryzae | Rice rhizosphere | Strain: OA447; Size: 4.47 Mbp; Ref Genome: NZ_PTRC00000000.1 (1 genome) | [33] |
| Ochrobactrum pecoris | Farm Animals | Strain: 08RB2639; Size: 5.06 Mbp; Ref Genome: GCA_006376675.1 (1 genome) | [34] |
| Ochrobactrum pituitosum | Industrial Environment | Strain: AA2 Size: 5.47 Mbp; Ref Genome: GCA_002025625.1 (4 genomes) | [35] |
| Ochrobactrum pseudintermedium | Clinical isolate | Strain: CCUG34735; Size: 4.39 Mbp; Ref Genome: GCA_008932435.1 (1 genome) | [36] |
| Ochrobactrum pseudogrignonense | Clinical isolate | Strain: K8; Size: 4.99 Mbp; Ref Genome: GCA_001652485.1 (6 genomes) | [30] |
| Ochrobactrum quorumnocens | Potato rhizosphere | Strain: A44; Size: 5.5 Mbp; Ref Genome: GCA_002278035.1 (2 genomes) | [37] |
| Ochrobactrum rhizosphaerae | Potato rhizosphere | Strain: PR17; Size: 4.9 Mbp; Ref Genome: GCF_002252475.1 (2 genomes) | [38] |
| Ochrobactrum soli | Cattle farm soil | Strain: BO-7; Size: 45 Mbp; Ref Genome: GCA_003664555.1 (3 genomes) | [39] |
| Ochrobactrum thiophenivorans | Industrial Environment | Strain: DSM 7216; Size: 4.4 Mbp; Ref Genome: GCA_002252445.1 (2 genomes) | [38] |
| Ochrobactrum teleogrylli | insect Teleogryllus occipitalis | No Genome | [40] |
| Ochrobactrum tritici | wheat rhizosphere root soil | Strain: DSM 13340; Size: 5.5 Mbp; Ref Genome: GCA_012395245.1 (6 genomes) | [9] |
Figure 1.
Phylogenetic structure of the genus Ochrobactrum along with the genus Brucella. The tree based on partial 16S rRNA gene sequences obtained using neighbour joining with Maximum Composite Likelihood method (MEGA package). GenBank accession numbers are given with the species name. Numbers at nodes are bootstrap values based on 1000 resamplings. Bar, 0.0050 substitutions per site [41,42].
3. Identification of Ochrobactrum spp.
Ochrobactrum species are Gram-negative and composed of short rods that are straight or slightly curved with one end flame shaped. They are generally motile and do not produce haemolysis on blood agar [43].
3.1. Biochemical Identification
Biochemical identification can be carried out using biochemical-testing kits such as the API 20NE or Vitek-2 (BioMèrieux, Las Balmas, France). When biochemical testing is carried out, it is normal to test isolates against Brucella agglutinating sera to prevent misdiagnosis with Brucella its close neighbour [44]. It has been shown that commercial kits are generally unsuitable for identification or differentiation amongst Ochrobactrum [45]. Analysis of 103 clinically relevant Ochrobactrum strains indicated that biochemical reaction profiles of the API and BD Phoenix™ 100 systems for identifying Ochrobactrum isolates can only be used at the genus level [46]. Care is required when identifying Ochrobactrum in clinical situations as misidentification has occurred with Brucella melitensis [47].
For identification of Ochrobactrum spp., it was proposed that the isolation of non-fastidious, non-fermenting, oxidase-positive, Gram-negative rods that are resistant to Beta-lactams (except imipenem) indicates the isolate is from the genus Ochrobactrum [43]. The API 20NE will confirm the identification to genus level for the majority of strains (Table 2). In addition, it has been proposed that urease activity, the mucoidy of the colonies and growth at 45 °C on tryptic soy agar coupled to susceptibility to colistin, tobramycin and netilmicin should be used as differentiating characteristics in the determination of O. anthropi and O. intermedium to the species level [43].
Table 2.
Phenotypic characteristics observed for Ochrobactrum strains based on reactivity within the API 20E Biolog GN and API 20NE systems [9,43,51].
| Using the API 20E, API 20NE, Biolog GN 1 | Reaction |
|---|---|
| Indole | −ve |
| Catalase | +ve |
| Cytochrome oxidase | +ve |
| H2S | - |
| Acetoin | −ve |
| Citrate utilisation | −ve |
| Carbohydrate fermentation | −ve |
| Adipate assimilation | −ve |
| Detection Arginine dihydrolase | −ve |
| Detection Lysine decarbooxylase | −ve |
| Detection Ornithine decarboxylase | −ve |
| Detection Beta galactosidase | −ve |
| Detection Gelatinase | −ve |
| Urease O. anthropi | +ve |
| O. intermedium | variable |
| O. grignonens | −ve |
| O. tritici | −ve |
| O. gallinifaecis | −ve |
| Assimilation glucose, arabinose, mannose, N-acetylglucosamine, maltose and malate | +ve |
In many clinical situations, the Microscan Walkaway system is used for primary identification and any unusual non-fermentative bacteria are analysed via biochemical analysis methods such as the RapID NF Plus system. This strategy has been shown to generally perform very well [48]. There have been cases of misdiagnosis of Ochrobactrum anthropi (subsequently confirmed by VITEK) as Shewanella putrefaciens [48]. Of course, the opposite has also been reported where a Brucella suis bacteraemia was mistakenly identified as Ochrobactrum anthropi by the VITEK 2 system [49,50]. These studies underscore the difficulty encountered in identifying unusual Gram-negative, non-fermentative bacteria such as Ochrobactrum.
3.2. Fatty Acid Analysis
Use of fatty acid analysis as a differentiation marker using the Sherlock System and comparison with the Sherlock database provided the identification result for O. anthropi with an ID score of 0.556, indicating its poor utility for differentiation at the species level [45].
3.3. Molecular Identification
Molecular tools have long been applied to the typing of Ochrobactrum species. Early studies utilised pulsed-field gel electrophoresis and rep-PCR for the epidemiological analysis [52] followed by AFLP (Amplified Restriction Fragment Length Polymorphism) to confirm the relatedness of O. anthropi and O. intermedium with its Brucella relatives [53] using a limited number of isolates. The molecular diversity of a larger number of Ochrobactrum strains were investigated by comparing environmental isolates from soil and the rhizoplane and comparing these to a number of clinical isolates [12]. Rep-PCR using a combination of BOX and REP primers were used to profile the isolates. The isolates used in this study clustered according to their species designation [12] indicating that rep-PCR profiling offered a good tool for species delineation.
However, the differentiation of species is somewhat difficult because of their phenotypic similarity and indeed confusion amongst 16s rDNA sequences [45]. Errors still occur such as in the case of bacteraemia where the causative agent was recognised as Ralstonia paucula by the Microscan Walkaway system but later following DNA sequencing was identified as O. anthropi [54].
16s rDNA sequence similarity between O. anthropi and O. intermedium ranged from 97.9% to 98.7% depending on the strains compared [43] suggesting a higher genetic deviation in O. intermedium than is found in O. anthropi. The genetic structure of a collection of 65 isolates (37 clinical, 11 environmental and 17 from culture collections) illustrative of the known natural distribution of O. intermedium was analysed by MLSA (Multi-Locus Sequence Analysis) [53].
A recA-PCR RFLP (Restriction Fragment Length Polymorphism) assay was also developed to study interspecies variability within Ochrobactrum using recA sequences from known isolates including 38 O. anthropi strains and type strains of O. intermedium, O. tritici and O. lupini and comparing these with closely related Brucella strains [54]. It was concluded that recA-sequence analysis provided a reliable molecular subtyping tool for Ochrobactrum at both the inter- and intraspecies level. Subsequently, a sensitive recA gene-based multi-primer single-target PCR assay has been created to differentiate O. anthropi, O. intermedium and Brucella that had been reported to cause diagnostic difficulty (Table 3) [55,56,57]. Teyssier et al. used 35 clinical isolates and the type strains of all known Ochrobactrum species (all confirmed as Ochrobactrum species by 16s rDNA sequencing) to examine comparative identification techniques ranging from commercial kits to biochemical and ribotyping [43].
Table 3.
Molecular methods applied to identify Ochrobactrum spp. [57].
| Method | Target | Sequence | Amplicon (bp) | Species |
|---|---|---|---|---|
| PCR | recA | Anth-f GCAAGCTGGGTGTCGATCTGG Anth- r TTCTCGACGACACCGGCCTTTA |
544 | Ochrobactrum anthropi |
| PCR | recA | Inter-f CGGCGTTGGTGGCTTGCCTAA Inter-r GGAACGAGAGATAGACGCGGTA |
402 | Ochrobactrum intermedium |
3.4. MALDI-TOF MS
MALDI-TOF MS (Matrix-Assisted Laser Desorption/Ionisation–Time-of-Flight) was initially used to identify Ochrobactrum intermedium from a range of difficult to identify strains as an alternative to Vitek, API or 16s rDNA sequencing in a large validation screen with some 204 genera showing discordant results from different identification methods [58]. The method has since found utility for evaluation within the Ochrobactrum genus. The utility of automated rep-PCR (DiversiLabTM system, BioMèrieux, Las Balmas, France) and MALDI-TOF MS analysis was compared for typing of 23 O. anthropi clinical isolates (bacteraemias) [44]. MALDI-TOF MS evaluation clustered the 23 strains of O. anthropi into a single group containing four distinct subgroups at close distance, indicating a high similarity between the isolates but also its accuracy in identification [44]. The technique of MALDI-TOF MS is gaining widespread usage in clinical situations and is increasingly utilised for Ochrobactrum identification in the clinic [59].
4. Ochrobactrum spp. Virulence
Ochrobactrum spp. are considered to be of low virulence. A study carried out by Yagel et al. into the virulome of Ochrobactrum spp. looked at the genomes of 130 isolates [60]. These isolates were taken from clinical, environmental, animal and plant settings. The study identified a limited number of virulence factors in the majority of these isolates. They found lipid A biosynthesis genes in all genomes analysed. They also found other virulence-associated genes in the majority of isolates such as genes associated with fatty acid biosynthesis (fabZ), carbohydrate metabolism (pgm and cgs), cell wall biosynthesis (wbpL) and biofilm formation (ricA, 95%). Genes for other more widespread Gram-negative virulence-associated proteins were not found in these genomes [60].
5. Ochrobactrum spp. Outbreaks
5.1. Outbreak Identification
All obtainable publications (journal articles, case reports and conference proceedings) discussing Ochrobactrum spp. infections were recovered using the PubMed, Web of Knowledge and Google Scholar search databases from 1980 to April 2020. The terms “CDC group VD1-2”, “Ochrobactrum”, “Ochrobactrum spp.”, “Ochrobactrum anthropi” and “Ochrobactrum intermedium” as well as all species names listed in Table 1 were searched. Any publications that discussed infection were set aside. These papers/abstracts were then read and the required information extracted from them. This information included year, geographic location, patient information (age, sex and any underlying medical conditions), antimicrobial testing, treatment and patient outcomes where available. The references cited from these publications were also checked for any publications/reports that may not have been found during the database searches.
5.2. Outbreak Analysis
The results of the investigations of the literature can be seen in Table 4 and Table 5. The tables summarise year, geographic location, patient information (age, sex and any underlying medical conditions), antimicrobial testing, treatment and patient outcome. One hundred seventeen separate instances of Ochrobactrum anthropi infection (277 individual cases) were identified along with a further eleven instances (twelve cases) of Ochrobactrum intermedium, Ochrobactrum oryzae, Ochrobactrum pseudogrignonense, Ochrobactrum pseudintermedium and Ochrobactrum tritici infection. The major breakdown of O. anthropi related conditions were as follows: forty-six instances of bacteraemia (42%) from which three were described as “bloodstream infections” that were usually associated with catheters, fourteen instances of septicaemia/sepsis/septic shock (12%) and two further instances of biliary sepsis (2%), nine instances of endophthalmitis, eight instances of peritonitis, four instances of pneumonia (8%) and two instances each endocarditis (2%). Other infections included two cases of keratitis (2%), four of various types of abscess (neck, pelvic, pancreatic and retropharyngeal) (3%) and one instance each of “hand infection” and brain empyema (1%). There have also been multiple reported instances of Ochrobactrum spp. infection that have caused two or more conditions. These include bacteraemia and necrotising fasciitis, bacteraemia and pneumonia, septicaemia and peritonitis and two instances of septic shock and endocarditits. Ten cases of death associated to Ochrobactrum spp. infection (all O. anthropi) have also been reported in the literature, four with sepsis/septicaemia (one with endocarditis), two with peritonitis and one each with a bloodstream infection, pyrogenic infection, endocarditis and infection of transjugular intrahepatic portosystemic shunt.
Table 4.
Incidences of Ochrobactrum anthropi infection from 1980 to 2020. Main characteristics of the case reports.
| Author (Ref) | Year | Sex/Age | Country | Co-Morbidity | Type of Infection | Susceptible to * | Resistance to * | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Appelbaum and Campbell [62] | 1980 | M/75 years old | USA | COPD, MI, CVA | Pancreatic abscess | Gentamicin, TMP-SMZ | Amikacin, Chloramphenicol, Tetracycline, Tobramycin | Gentamicin | Died of respiratory failure |
| Kish [63] | 1984 | F/21 years old | USA | Astrocytoma | Bacteraemia (catheter related) | Amikacin, Gentamicin Imipenem, Moxalactam, Gentamicin, Tetracycline, TMP-SMZ | Chloramphenicol, Netilmicin, Rifampin, Tobramycin | TMP-SMZ, Gentamicin | Complete Recovery |
| Barson et al. [20] | 1987 | M/14 years old | USA | Puncture wound of the foot | Osteochondritis | Amikacin, Gentamicin Imipenem, Moxalactam, Gentamicin, Rifampin Tetracycline, TMP-SMZ | Chloramphenicol, Netilmicin, Tobramycin | TMP-SMZ, Gentamicin | Complete Recovery |
| Van Horn [64] | 1989 | F/23 years old | USA | Hodgkin’s disease, had undergone bone marrow transplantation | Bacteraemia (catheter related), Urinary Tract Infection | Amikacin, Norfloxacin, Tetracycline, TMP-SMZ | Ampicillin, Aztreonam, Carbenicillin, Cefoperazone, Cefoxitin, Ceftazidime, Cephalothin, Chloramphenicol, Gentamicin, Mezlocillin, Piperacillin, Ticarcillin, Tobramycin | Norfloxacin (400 mg orally twice a day), TMP-SMZ (320/1600 mg orally every 6 h), Amikacin (500 mg intravenously every 12 h) | Complete Recovery |
| Cieslak et al. [65] | 1992 | F/3 years old | USA | Retinoblastoma | Bacteraemia (catheter related) | Amikacin, Ciprofloxacin, Gentamicin, Imipenem, Polymyxin E, TMP-SMZ, | Ampicillin, Aztreonam, Cefoxitin, Ceftazidime, Ceftriaxone, Cephalothin, Mezlocillin, Rifampin, Tetracycline, Tobramycin | Vancomycin and Ceftazidime Followed by Amikacin and TMP-SMZ, | Complete Recovery |
| Gransden et al. [66] | 1992 | Multiple (7 cases) | UK | Multiple | Sepsis (catheter related) | Amikacin, Ciprofloxacin, Gentamicin, Imipenem, TMP-SMZ, Tobramycin | Amoxicillin, Amoxicillin–clavulanate, Azlocillin, Aztreonam Cefuroxime, Cefotaxime, Cefoxitin, Ceftazidime, Ticarcillin Trimethoprim | Ciprofloxacin, Gentamicin, Imipenem | 5 complete Recovery, 2 deaths unrelated to infection |
| Brivet et al. [67] | 1993 | F/74 years old | France | Alcoholism | Necrotising fasciitis, bacteraemia and multiorgan failure, | Amikacin, Ceftazidime, Cefotaxime, Ciprofloxacin, Imipenem, Pefloxacin, Ciprofloxacin, TMP-SMZ | Amoxicillin, Amoxicillin–clavulanic acid, Carbenicillin, Cephalothin, Colimycin, Piperacillin | Amoxicillin–clavulanic acid and amikacin. Followed by Imipenem | Complete Recovery |
| Kern et al. [68] | 1993 | Multiple (4 Cases—F 2–77 years old) | USA | Leukaemia | Bacteraemia (catheter related) | Imipenem | Ampicillin Amoxicillin–Clavulanic acid, Chloramphenicol Mezlocillin, Piperacillin | Amikacin, Ceftazidime–Netilmicin, Piperacillin–Netilmicin Catheter removal in one case | Complete Recovery |
| Klein & Eppes 1993 [69] | 1993 | F/7 years old | USA | Leukaemia | Bacteraemia (catheter related) | Amikacin, Ceftriaxone, Ciprofloxacin, Gentamicin, Imipenem, TMP-SMZ, Tobramycin | Ampicillin, Aztreonam, Ceftazidime, Cephalothin, Mezlocillin, | Gentamicin, Imipenem Catheter Removal | Complete Recovery |
| Alnor et al. 1994 [70] | 1994 | Multiple (3 Cases) | Denmark | Crohn’s disease, Gastric ulcer | Septicaemia Peritonitis (catheter related) | Ciprofloxacin, Gentamicin, Imipenem, Tetracycline | Ampicillin, Aztreonam, Cefuroxime, Cefotaxime, Ceftazidime, Ceftiaxione, Erythromycin, Nitrofurantoin, Piperacillin, Rifampin, TMP-SMZ | N/A | Complete Recovery |
| Ezzedine et al. [71] | 1994 | Multiple (5 Cases) | Organ transplant patients | Bacteraemia in rabbit anti-thymocyte globulin (RATG) infusion vials | Amikacin, Imipenem, Ofloxacin | Ampicillin, Amoxicillin–Clavulanic, Aztreonam Cefazolin, Temocillin, | N/A | Complete Recovery | |
| Haditsch et al. [72] | 1994 | F/14 years old | Austria | Leukaemia | Bacteraemia | Amikacin, Polymyxin B, Imipenem, Norfloxacin, Tetracycline | Ampicillin, Amoxicillin–Clavulanic acid, Cefazolin, Cefoxitin, Ceftriaxone, Ceftazidime, Gentamicin, Piperacillin Tobramycin, TMP-SMZ | N/A | Complete Recovery |
| Braun et al. [73] | 1996 | M/66 years old | Germany | Cataract surgery | Endophthalmitis after cataract surgery | Amikacin, Ciprofloxacin, Imipenem, Tetracycline | Cephalosporins, Penicillins, Tobramycin, TMP-SMZ | Ciprofloxacin (400 mg two times daily) | Complete Recovery |
| Chang et al. [74] | 1996 | Multiple (3 Cases) | USA | Neurosurgery Patients | Meningitis | Ciprofloxacin, Gentamicin, Imipenem–cilastatin, Tetracycline | N/A | Imipenem–Cilastatin, Gentamicin (Six weeks) | Complete Recovery |
| Cieslak et al. [75] | 1996 | F/61 years old | USA | Hypertension, hypothyroidism, Renal insufficiency, chronic congestive heart failure | Pyogenic Infection | N/A | N/A | Gentamicin, Ceftazidime, Gentamicin, Vancomycin After failure TMP-SMZ | Died |
| Cieslak et al. [75] | 1996 | M/66 years old | USA | Small cell carcinoma | Pyogenic Infection | N/A | N/A | Aztreonam, Ceftazidime, Vancomycin After failure TMP-SMZ | Complete Recovery |
| Cieslak et al. [75] | 1996 | M/29 years old | USA | None | Pyogenic Infection | N/A | N/A | Cephradine | Complete Recovery |
| Ramos et al. [76] | 1996 | F/26 years old | Spain | Cancer | Bacteraemia (catheter related) | Ciprofloxacin, Gentamicin, Imipenem, TMP-SMZ | Ampicillin, Ceazolin, Cefotaxime, Ceftazidime | Ciprofloxacin (oral for 10 days) | Complete Recovery |
| Ramos et al. [76] | 1996 | F/62 years old | Spain | Cancer | Bacteraemia (catheter related) | Ciprofloxacin, Gentamicin, Imipenem, TMP-SMZ | Ampicillin, Ceazolin, Cefotaxime, Ceftazidime | Gentamicin and Catheter removal | Complete Recovery |
| Berman et al. [77] | 1997 | F/74 years old | USA | Pneumonia | Endophthalmitis with indwelling catheters for venous access | N/A | N/A | Ciprofloxacin (Oral 500 mg twice daily for 2 weeks) | Complete Recovery |
| Christenson et al. [78] | 1997 | Multiple (3 Cases) | USA | Various | Meningitis (pericardial allograft tissue) | Ciprofloxacin, Gentamicin, Imipenem, Tetracycline | Amikacin, Ampicillin, Cefotaxime. Ceftazidime, Cefuroxime. Cephalothin. Chloramphenicol, Piperacillin, Rifampin, Ticarcillin, Ticarcillin–Clavulanic acid, TMP-SMZ | Removal of tissue allograft implants | Complete Recovery |
| Earhart et al. [79] | 1997 | F/40 years old | USA | Rheumatic heart disease | Infection of retained pacemaker leads | Ciprofloxacin, Gentamicin Imipenem, TMP-SMZ | N/A | Ciprofloxacin, Rifampin Vancomycin, TMP-SMZ for 6 weeks Followed by Ciprofloxacin TMP-SMZ for 4 1/2 months | Complete Recovery |
| Gill et al. [80] | 1997 | M/45 years old | USA | Coronary artery disease | Intravenous line infection | N/A | N/A | None Administered | Complete Recovery |
| Torres et al. 1998 [81] | 1998 | N/A | Spain | AIDS | Bacteraemia | N/A | N/A | N/A | N/A |
| Yu et al. [82] | 1998 | Multiple (15 Cases) 10 Cases CA | China | Various | Bacteraemia (3 catheter related) | Amikacin, Ceftriaxone, Cefoperazone, Gentamicin, Imipenem | Ampicillin, Aztreonam, Amoxicillin–Clavulanic acid, Ceftazidime, Cephalothin, Cefonicid, Piperacillin, | Aminoglycoside | Complete Recovery |
| Jelveh & Cunha 1999 [6] | 1999 | M/33 month old CA | USA | Osteomyelitis | Bacteraemia | Gentamicin Levofloxacin, TMP-SMZ | N/A | N/A | Complete Recovery |
| Hay & Lo 1999 [83] | 1999 | F/Neonate HA |
UK | Neonate | Meningitis | Amikacin, Ciprofloxacin, Gentamicin, Meropenem, Tobramycin, TMP-SMZ | Ampicillin, Amoxicillin–clavulanic acid, Aztreonam, Cefotaxime. Ceftazidime, Cefuroxime, Piperacillin–Tazobactam | Gentamicin | Complete Recovery |
| Inoue et al. 1999 [84] | 1999 | M/64 years old | Japan | None | Endophthalmitis | Amikacin, Cefmetazole, Cefbuperazone, Gentamicin, Imipenem, Levofloxacin, Minocycline, Tobramycin | Ampicillin, Piperacillin, Cefazolin, Cefotiam, Ceftazidime Flomoxef | Imipenem (Intravenously), Ciprofloxacin, Minocycline | Complete Recovery |
| Manfredi et al. 1999 [85] | 1999 | M/41 years old | Italy | HIV | Septicaemia | Amikacin, Carbapenems, Ciprofloxacin, Gentamicin, Ticarcilllin–Clavulanate TMP-SMZ | Aztreonam, Ceftazidime, Tobramycin | Meropenem (3 g/day) | Complete Recovery |
| Manfredi et al. [85] | 1999 | M/35 years old | Italy | HIV | Septicaemia | Amikacin, Carbapenems, Ceftazidime, Ciprofloxacin, Gentamicin, TMP-SMZ | Aztreonam, Ticarcilllin–Clavulanate, Tobramycin | Amikacin (500 mg/day), Ceftazidime (3 g/day) | Complete Recovery |
| Mastroianni et al. [86] | 1999 | M/47 years old | Italy | None | Bacteraemia | Amikacin, Amoxicillin Carbenicillin, Chloramphenicol, Ciprofloxacin, Gentamicin, TMP-SMZ, Tobramycin | Cephalosporins, Imipenem, Tetracycline | Ciprofloxacin (14-day course, intravenous, 400 mg/day) | Complete Recovery |
| Saavedra et al. [87] | 1999 | M/4 years old | Spain | Neuroblastoma | Bacteraemia (catheter related) | N/A | Amikacin, TMP-SMZ | Imipenem (14 days) | Complete Recovery |
| Stiakaki et al. [88] | 1999 | Multiple (9 Cases—All children) | Greece | Cancer | Bacteraemia (7 catheter related) | Amikacin, Ciprofloxacin Imipenem, TMP-SMZ | β-lactam antibiotics | Imipenem, Ciprofloxacin or catheter removal (2 cases) | Complete Recovery |
| Chertow 2000 [89] | 2000 | F/74 years old | USA | Renal Failure | Bacteraemia (catheter related-Haemodialysis) | Aminoglycosides Imipenem, Quinolones | Penicillins, Cephalosporins, TMP-SMZ | Ciprofloxacin (500 mg daily) and Tobramycin (40 mg intravenously) | Complete Recovery |
| Deliere et al. [90] | 2000 | Multiple (2 Cases) HA |
France | Leukaemia | Sepsis (catheter related) | Ciprofloxacin, Colistin Imipenem, Rifampicin | Beta-lactams, Chloramphenicol, Fosfomycin | Imipenem (and catheter removal in one patient | Complete Recovery |
| Esteban et al. [91] | 2000 | F/79 years old | Spain | Diabetic nephropathy | Peritonitis in CAPD patient | Amikacin, Ciprofloxacin Gentamicin, Imipenem, Meropenem, TMP-SMZ | Ampicillin, Amoxicillin–Clavulanate, Cefazolin, Cefuroxime, Ceftriaxone, Ceftazidime, Cefepime, Piperacillin–Tazobactam, Ticarcillin | Ofloxacin (200 mg/day for 14 days) | Died (Unrelated to infection) |
| Mahmood et al. [92] | 2000 | F/39 years old | Pakistan | Asthmatic and non-insulin dependent diabetic | Infective Endocarditis and Septic Embolization | Ciprofloxacin, Gentamicin, Imipenem, Meropenem, Ofloxacin, TMP-SMZ | Ampicillin, Cefotaxime Piperacillin–Tazobactam, | Gentamicin (1 mg/kg 8-hourly) | Complete Recovery |
| Peltroche-Llacsahuanga et al. [93] | 2000 | F/39 years old | Germany | End-stage renal disease | Peritonitis in CAPD patient | Amikacin, Ciprofloxacin, Colistin Gentamicin, Imipenem, Meropenem, TMP-SMZ, Tobramycin | Ampicillin, Cefotiam, Cefotaxime, Ceftazidime, Cefepime, Mezlocillin, Piperacillin, Piperacillin–Tazobactam, Vancomycin | Imipenem (200 mg/1500 mL bag; four bags/day) and Ceftazidime (250 mg/1500 mL bag; four bags/day) | Complete Recovery |
| Shelly and Mortensen [94] | 2000 | M/2.5 years old | USA | None | Infection | Ampicillin, Gentamicin | Cefuroxime, Ceftriaxone, TMP-SMZ | Cefazolin Followed by Ampicillin–Subactam | Complete Recovery |
| El-Zimaity et al. [95] | 2001 | N/A | UK | None | Pseudo-bacteraemia | N/A | N/A | N/A | N/A |
| Greven et al. [96] | 2001 | N/A | USA | N/A | Chronic postoperative endophthalmitis | N/A | N/A | N/A | N/A |
| Daxboeck et al. [97] | 2002 | Multiple (2 Cases) | Austria | Chronic renal failure resulting from diabetic nephropathy | Bacteraemia (haemodialysis patients) | Amikacin, Ciprofloxacin Doxycycline, Gentamicin, Imipenem | β-lactam antibiotics, TMP-SMZ | Gentamicin | One patient recovered, one died due to MI |
| Galanakis et al. [98] | 2002 | Multiple (11 Cases—All less than 7 years old) | Greece | None | Bacteraemia | Amikacin, Ciprofloxacin Gentamicin, Imipenem, Nalidixic acid, Ofloxacin, Perfloxacin, Netilmicin, Norofloxacin Streptomycin, TMP-SMZ, Tobramycin | Ampicillin, Amoxicillin, Amoxicillin–Clavulanic acid, Aztreonam, Cefalothin, Cefepime, Cefotaxime, Cefuroxime, Piperacillin, Piperacillin–Tazobactam, Ticarcillin, Ticarcillin–Clavulanate | TMP-SMZ (oral delivery in one patient) | Complete Recovery |
| Stiakaki et al. [99] | 2002 | Multiple (11 Cases) | Greece | Various Cancers | Bacteraemia (catheter related) | Aminoglycosides, Colistin, Imipenem, Quinolones, TMP-SMZ | Ampicillin, Amoxicillin, Amoxicillin–Clavulanate, Aztreonam, Cefalothin, Cefepime, Cefotaxime Cefuroxime, Ticarcillin, Ticarcillin–Clavulanate, Piperacillin, Piperacillin–Tazobactam, Ticarcillin, Ticarcillin–Clavulanate | Various different treatments in all 11 cases | N/A |
| Wheen et al. 2002 [100] | 2002 | F/62 years old | New Zealand | None | Osteomyelitis (vertebral) | Aminoglycosides, Amoxicillin, Cephalosporins, Fluoroquinolones, TMP-SMZ | N/A | Ceftriaxone (Intravenously for 6 weeks) followed by Ciprofloxacin (orally for 6 weeks) | Complete Recovery |
| Gascón et al. [101] | 2003 | M/3 years old CA | Spain | None | Bacteraemia | Aminoglycosides, Ciprofloxacin, Imipenem, TMP-SMZ | Aztreonam, Ceftazidime Cefsulodin, Phosphomycin, Piperacillin–Tazobactam, Ticarcillin–Clavulanic acid | Gentamicin TMP-SMZ | Complete Recovery |
| Hill [102] | 2003 | N/A | UK | N/A | Pseudo-bacteraemia | N/A | N/A | N/A | N/A |
| Kettaneh et al. [17] | 2003 | F/30 years old | France | None | Septic Shock | Amikacin, Gentamicin, Imipenem, Netilmicin, Pefloxacin, Tobramycin, TMP-SMZ | N/A | Gentamicin infusion (infusion of 240 mg once), Ofloxacin (200 mg infusion twice a day for 11 days) | Complete Recovery |
| Oliver [48] | 2003 | 30 years old | USA | N/A | Infection | N/A | N/A | N/A | N/A |
| Romero Gomez et al. [103] | 2004 | F/65 years old | Spain | Hypertension and rheumatic heart disease | Prosthetic mitral valve endocarditis | Aminoglycosides, Meropenem, Quinolones | β-lactams, TMP-SMZ | Meropenem (Intravenously 1 g every 6 h) and Gentamicin. | Complete Recovery |
| Oliver et al. [104] | 2005 | M/30 years old | USA | None | Bacteraemia (gunshot wound) | Amikacin, Ciprofloxacin Gentamicin, Imipenem, TMP-SMZ, Tobramycin | Aztreonam, Cefepime, Cefotaxime, Ceftazidime, Ceftiaxione, Piperacillin, Piperacillin–Tazobactam | Cefepime (2 g IV BID for 3 days) Ciprofloxacin (400 mg IV BID for 8 days) Imipenem (1 g IV for 7 days) | Complete Recovery |
| Cho et al. [105] | 2006 | F/69 years old | Korea | Hypertension | Bacteraemia (associated with medicinal plants) | Colistin, Imipenem, Meropenem, Tetracycline | Amikacin, Aztreonam, Cefepime, Ceftazidime, Cefpirome, Ciprofloxacin, Gentamicin, Isepamcin, Netilmicin, Pefloxacin, Piperacillin, Piperacillin–Tazobactam, Ticarcillin, Ticarcillin–Clavulanate, TMP-SMZ, Tobramycin | Imipenem | Complete Recovery |
| Ozdemir et al. [18] | 2006 | F/42 years old CA | Turkey | None | Endocarditis and septic shock | Amikacin, Ciprofloxacin Gentamicin, Imipenem, TMP-SMZ | β-lactams (Excluding Carbapenases) Erythromycin, Chloramphenicol | Meropenem (500 mg Twice daily) Vancomycin (500 mg Twice daily) | Died |
| Vaidya et al. [106] | 2006 | M/49 years old | USA | None | Pelvic Abscess | Gentamicin, Imipenem, Levofloxacin, TMP-SMZ | Cefepime, Tobramycin | Levofloxacin Metronidazole | Complete Recovery |
| Aly et al. [107] | 2007 | F/2 years old | Long-chain 3-hydroxyacyl-coenzyme A dehydrogenase deficiency | Bacteraemia | Ciprofloxacin, Levofloxacin, Piperacillin–Tazobactam TMP-SMZ | Amikacin, Cefotaxime, Ceftazidime, Ceftriaxone, Cefepime, Gentamicin, Imipenem Piperacillin, Tetracycline, Ticarcillin–Clavulanate, Tobramycin | Cefotaxime | Complete Recovery | |
| Labarca et al. [108] | 2007 | Multiple (8 Cases) | Chile | N/A | Pseudo-bacteraemia | N/A | N/A | N/A | N/A |
| Lee et al. [109] | 2007 | M/80 years old | Korea | intrahepatic duct carcinoma | Bacteraemia | N/A | N/A | N/A | Complete Recovery |
| Song et al. [110] | 2007 | Multiple (9 Cases) | Korea | N/A | Chronic pseudophakic endophthalmitis | Ciprofloxacin, Imipenem, Ofloxacin, TMP-SMZ, | Ampicillin, Amoxicillin, Ceftazidime, Gentamicin Piperacillin, Ticarcillin, Tobramycin | N/A | Complete Recovery |
| Yu et al. [111] | 2007 | M/62 years old CA | Korea | Liver cirrhosis | Peritonitis | Amikacin, Ciprofloxacin Gentamicin, Imipenem, Levofloxacin, Meropenem, TMP-SMZ, Tobramycin | β-lactams | Imipenem (250 mg every 6 h) | Died |
| Arora et al. [112] | 2008 | M/64 years old | India | Hypertension, Diabetes, Coronary artery disease | Septicaemia (intra-aortic balloon pump (IABP) insertion) | Ciprofloxacin, Cefoperazone–Sulbactam, Imipenem, Tobramycin | Amikacin, Aztreonam, Cefotaxime, Cefoperazone, Gentamicin, Piperacillin, Ticarcillin | Ciprofloxacin (100 mL intravenous, twice a day), Cefazolin (1 g IV thrice a day), meropenem (1 g IV tds) metronidazole (100 mL IV tds) | Died |
| Battaglia et al. [113] | 2008 | M/17 years old | USA | None | Septic arthritis | N/A | N/A | Ciprofloxacin (oral 500 mg twice daily for 4 week), TMP-SMZ (Oral 160 mg/800 mg twice daily for 2 weeks) | Complete Recovery |
| Javaid et al. [114] | 2008 | M/84 years old | UK | Acute renal failure | Bacteraemia (catheter related) | Ciprofloxacin, Meropenem | Ceftazidime, Gentamicin, Ticarcillin–Clavulanate | Ciprofloxacin (250 mg orally twice a day for 2 weeks), After failure Catheter removal Meropenem (250 mg/day) | Complete Recovery |
| Menuet et al. [115] | 2008 | F/17 years old | France | Cystic Fibrosis. Diabetes | Pneumonia | Amikacin, Ciprofloxacin, Gentamicin, Imipenem, Isepamicin, Rifampicin, TMP-SMZ, Tobramycin | Amoxicillin, Amoxicillin–Clavulanate, Ceftazidime, Ceftriaxone, Colistin, Ticarcillin, Ticarcillin–Clavulanate, Piperacillin–Tazobactam | Imipenem (4 g/day) Tobramycin (2 g/day) | Complete Recovery |
| Chiang et al. [116] | 2009 | M/75 years old | Taiwan | MI | Endophthalmitis (Cataract surgery) | N/A | N/A | Ciprofloxacin | Complete Recovery |
| Duran et al. [117] | 2009 | M/Neonate | Turkey | Neonate (meconium peritonitis) | Bacteraemia (catheter related) | Ciprofloxacin, Gentamicin, Imipenem | Amikacin, Ampicillin–Sulbactam, Aztreonam, Cefepime, Ceftriaxone, TMP-SMZ Tobramycin | Ciprofloxacin Gentamicin | Died (Unrelated to Ochrobactrum infection) |
| Kim et al. [118] | 2009 | F/46 years old | Korea | Ovarian cancer | Bacteraemia (catheter related) | Amikacin, Colistin, Ciprofloxacin, Gentamicin, Netilmicin, Pefloxacin, TMP-SMZ, Tobramycin | Aztreonam, Ceftazidime, Cefpirome, Cefepime Meropenem, Piperacillin, Piperacillin–Tazobactam, Ticarcillin Ticarcillin–Clavulanate | Ciprofloxacin, Imipenem for 3 weeks | Complete Recovery |
| Ospina et al. [119] | 2009 | F/49 years old | Colombia | Alcoholism | Bacteraemia | Carbapenem | Ampicillin–Sulbactam | Meropenem | Complete Recovery |
| Rihova et al. [120] | 2009 | M/51 years old | Belgium | Chronic kidney disease | Peritonitis (CAPD patient) | N/A | N/A | Amikacin Meropenem | Complete Recovery |
| Soloaga et al. [25] | 2009 | M/69 years old | Argentina | Type 2 diabetes | Bacteraemia (catheter related) | Ciprofloxacin, Imipenem, Meropenem, TMP-SMZ | Amikacin, Ceftazidime, Cefepime, Gentamicin, Piperacillin–Tazobactam | Ciprofloxacin (200 mg/12 h) Meropenem (500 mg/24 h post dialysis) | Complete Recovery |
| Adeyemi et al. [121] | 2010 | N/A | Nigeria | HIV | Bloodstream infections | Amikacin, Ampicillin, Cefuroxime, Chloramphenicol, Gentamicin, Ofloxacin, TMP-SMZ | Ceftazidime, Cefotaxime, Nalidixic acid | N/A | N/A |
| Quintela et al. [122] | 2010 | F/50 years old | Spain | Terminal chronic renal failure | Peritonitis (peritoneal dialysis) | N/A | N/A | PD catheter removal | Complete Recovery |
| Saveli et al. [123] | 2010 | M/53 years old | USA | Gout, Alcoholism | Septic arthritis | N/A | N/A | TMP-SMZ (800 mg/160 mg 2 tablets every 12 h) | Complete Recovery |
| Sepe et al. [124] | 2010 | M/71 years old | Italy | Type 2 diabetes | Peritonitis (automated peritoneal dialysis) | N/A | N/A | Cefotaxime (1 g), Gentamicin (80 mg intraperitoneal) | Complete Recovery |
| Starr [125] | 2010 | N/A | USA | N/A | N/A | N/A | N/A | N/A | N/A |
| Wi & Peck [126] | 2010 | Multiple (12 Cases) | Korea | Cancer (11 cases) and Liver Cirrhosis (1 case) | Biliary sepsis (8 Cases), peritonitis (1 case), catheter-related infection (3 cases) | Amikacin, Ciprofloxacin, Gentamicin, Imipenem, Meropenem, TMP-SMZ | Aztreonam, Ceftazidime, Ceftriaxone, Cefotaxime, Piperacillin–Tazobactam, | Various | Complete Recovery (11 cases) Died (1 case) |
| Woo Nho et al. [127] | 2010 | M/66 years old | Korea | Diabetes mellitus | Peritonitis (peritoneal dialysis) | Amikacin, Ciprofloxacin, Colistin, Gentamicin, Minocycline, TMP-SMZ, Tobramycin | Aztreonam, Meropenem, All β-lactams | Amikacin, Ciprofloxacin, Meropenem catheter removal | Complete Recovery |
| Yagüe-Muñoz et al. [128] | 2010 | M/8 years old CA | Spain | Cystic fibrosis | Bacteraemia | Amikacin, Ciprofloxacin, Colistin, Gentamicin, Imipenem, Levofloxacin, Meropenem Netilmicin, TMP-SMZ Tobramycin | Ampicillin–Sulbactam, Aztreonam, Ceftazidime, Piperacillin, Piperacillin–Tazobactam, Ticarcillin | Tobramycin | Complete Recovery |
| Obando et al. [129] | 2011 | F/19 years old | Chile | Hypothyroidism, end-stage chronic renal failure | Bacteraemia (catheter related) | Amikacin, Gentamicin, Imipenem Levofloxacin, Meropenem | Ampicillin–Sulbactam, Aztreonam Ceftazidime, Cefepime, | Levofloxacin and Catheter removal | Complete Recovery |
| Shivaprakasha et al. [130] | 2011 | M/75 years old | India | Aortic valve replacement | Endocarditis (prosthetic aortic valve endocarditis) | Amikacin, Ciprofloxacin, Doripenem Gentamicin, Imipenem, Meropenem Netilmicin, TMP-SMZ | N/A | Ceftriaxone (1 g intravenous twice daily), Amikacin (1 g intravenous once daily) Followed by Meropenem (500 mg 8 hourly) | Died |
| Chan & Holland [131] | 2012 | F/21 years old | USA | Asthma, hypertension, gastric reflux | Endophthalmitis (Boston type 1 keratoprosthesis implantation) | N/A | N/A | Levofloxacin | Complete Recovery |
| Shrishrimal [132] | 2012 | M/78 years old | USA | Diabetes mellitus type 2, peripheral vascular disease | Bloodstream infection (Haemodialysis associated) | Aminoglycosides, Ciprofloxacin | Aztreonam Ceftazidime, Cefepime, Piperacillin–Tazobactam, | Gentamicin, Ciprofloxacin | Complete Recovery |
| Alparslan et al. [133] | 2013 | M/12 years old | Turkey | End stage renal disease | Peritonitis (peritoneal dialysis infection) | N/A | N/A | Meropenem (initially 500 mg/L and then 200 mg/L), TMP-SMZ (TMP 320 mg/L-STX 1600 mg/L) PD catheter Removal | Complete Recovery |
| Chiu & Wang [134] | 2013 | M/34 years old | Singapore | None | Septic arthritis | Gentamicin, Meropenem, TMP-SMZ | Ceftazidime | TMP-SMZ (Oral) | Complete Recovery |
| Hagiya et al. [51] | 2013 | M/85 years old | Japan | Hepatocellular carcinoma, Liver cirrhosis | Bacteraemia | Amikacin, Colistin, Imipenem, Meropenem, Minocycline | Piperacillin, Piperacillin–Tazobactam, Aztreonam, Ceftazidime, Cefepime, Ciprofloxacin Levofloxacin, Gentamicin, TMP-SMZ | Cefcapene pivoxil (Oral) | Complete Recovery |
| Kumar et al. [135] | 2013 | M/45 days old | India | Neonate (congenital abnormalities) | Septicaemia and pneumonia | Ciprofloxacin, Gentamicin, Imipenem, Meropenem, Piperacillin–Tazobactam | Amikacin, Aztreonam | Meropenem | Complete Recovery |
| Mattos et al. [136] | 2013 | Multiple (12 Cases) | Brazil | Various | Endophthalmitis (Tubing following cataract surgery) | N/A | N/A | N/A | Complete Recovery |
| Mudshingkar et al. [137] | 2013 | M/Neonate | India | Neonate | Septicaemia | Amikacin, Imipenem, Meropenem | Ceftazidime, Cefepime, Gentamicin | Cefotaxime Gentamicin | Died |
| Mudshingkar et al. [137] | 2013 | M/Neonate | India | Neonate | Septicaemia | Amikacin, Imipenem, Meropenem | Ceftazidime, Cefepime, Gentamicin | Meropenem | Complete Recovery |
| Naik et al. [138] | 2013 | M/45 years old | USA | Hypotensive and Hypoxic | Pneumonia | Ciprofloxacin, Gentamicin Meropenem, Tobramycin | Ampicillin, Ampicillin–Sulbactam, Aztreonam, Cefazolin Cefepime, Cefotaxime, Ceftazidime, Piperacillin–Tazobactam, TMP-SMZ | Ciprofloxacin | Complete Recovery |
| Siti Rohani et al. [139] | 2013 | M/60 years old | Malaysia | Ischaemic heart disease, diabetes mellitus type 2, hypertension and end stage renal failur | Bacteraemia (catheter related) | Amikacin, Cefepime, Ciprofloxacin, Gentamicin Imipenem, Meropenem, TMP-SMZ | Ceftazidime, Piperacillin–Tazobactam Polymyxin-B | Imipenem 500 mg with Cilastatin (Intravenous 500 mg 12-hourly for 2 weeks) Catheters removal | Complete Recovery |
| Al-Naami et al. [140] | 2014 | M/15 years old | Australia | None | Retropharyngeal abscess | Amikacin, Cefepime, Ciprofloxacin, Gentamicin, Imipenem | N/A | N/A | Complete Recovery |
| Hernández-Torres et al. [141] | 2014 | M/73 years old | Spain | COPD, Hypertension, ischemic heart disease and chronic renal failure | Pneumonia | Ciprofloxacin, Doxicycline, Meropenem, Levofloxacin, TMP-SMZ, Tobramycin, Toimipenem | Amikacin, Aztreonam, Cephalosporins Piperacillin–Tazobactam | Levofloxacin (Oral) | Complete Recovery |
| Hernández-Torres et al. [141] | 2014 | M/38 years old | Spain | None | Bacteraemia (catheter related) | N/A | Amikacin, Aztreonam, Ciprofloxacin, Ceftazidime, Cefepime, Doxycycline Imipenem, Levofloxacin, Meropenem, Piperacillin–Tazobactam, TMP-SMZ, Tobramycin | Meropenem Teicoplanin | Complete Recovery |
| Hernández-Torres et al. [141] | 2014 | F/49 years old | Spain | Diabetes mellitus type 2 Adenocarcinoma | Biliary sepsis | Ciprofloxacin, Gentamicin, Imipenem, Levofloxacin, Meropenem | Amikacin, Cephalosporins, Piperacillin–Tazobactam, TMP-SMZ, Tobramycin | Piperacillin–Tazobactam Followed by Levofloxacin | Complete Recovery |
| Hernández-Torres et al. [141] | 2014 | M/61 years old | Spain | Liver cirrhosis | Transjugular intrahepatic portosystemic shunt device infection | Amikacin, Cefepime, Ciprofloxacin, Colistin, Gentamicin, Imipenem, Levofloxacin, Meropenem, Minocycline, Tigecycline, TMP-SMZ, Tobramycin | Ampicillin–Sulbactam, Aztreonam, Ceftazidime, Piperacillin, Piperacillin–Tazobactam | Meropenem | Died |
| Hernández-Torres et al. [141] | 2014 | F/56 years old | Spain | Acute myeloblastic leukaemia | Catheter-related infection | Ciprofloxacin, Imipenem, Levofloxacin, Meropenem, TMP-SMZ | Aminoglycosides, Aztreonam, Cephalosporins, Piperacillin–Tazobactam | Meropenem | Complete Recovery |
| Hernández-Torres et al. [141] | 2014 | 5 Months old | Spain | None | Pseudo-bacteraemia | Amikacin, Carbapenems, Colistin, Doxycycline, TMP-SMZ | Aztreonam, Cephalosporins, Piperacillin–Tazobactam, Tobramycin | N/A | N/A |
| Khan et al. [142] | 2014 | F.53 years old | India | Chronic kidney disease, diabetes mellitus | Sepsis (catheter related) | Imipenem, TMP-SMZ | Aminoglycosides, β-lactams, Colistin, Quinolones | N/A | Died |
| Menezes et al. [143] | 2014 | F/Neonate | Brazil | Neonate with Cystic Fibrosis | Bacteraemia (catheter related) | Amikacin, Meropenem, TMP-SMZ | Ceftazidime | Amikacin and meropenem | Complete Recovery |
| Mrozek et al. [144] | 2014 | M/28 years old | France | Brain Trauma | Brain empyema | Carbapenems, Ciprofloxacin, Levofloxacin | Cefotaxime, Ceftazidime, Ticarcillin, Ticarcillin–Clavulanic acid, Piperacillin, Piperacillin–Tazobactam, Tobramycin, TMP-SMZ | Ciprofloxacin, Meropenem (IV for 6 weeks) | Complete Recovery |
| Quirino et al. [44] | 2014 | Multiple (19 Cases) | Italy | N/A | Bacteraemia | Amikacin, Ciprofloxacin, Gentamicin, Imipenem, Levofloxacin, TMP-SMZ | Ampicillin, Ampicillin–Sulbactam, Cefazolin, Cefepime, Cefoxitine, Ceftazidime, Ceftriaxone, Nitrofurantoin, Piperacillin–Tazobactam | N/A | N/A |
| Qasimyar et al. [145] | 2014 | M/Neonate | USA | Neonate | Sepsis (catheter related) | Amikacin, Levofloxacin, Meropenem | Β-lactams | Amikacin Meropenem (IV) | Complete Recovery |
| Wu et al. [146] | 2014 | M/35 years old | China | None | Neck abscess | Amikacin, Ciprofloxacin, Chloromycetin, Gentamicin, Meropenem, Imipenem, Levofloxacin Sulfamethoxazole, Tetracycline | Ampicillin, Ampicillin–Sulbactam, Amoxicillin–clavulanic acid, Aztreonam, Ceftazidime, Cefotaxime, Piperacillin Piperacillin–Tazobactam, | Levofloxacin | Complete Recovery |
| Cenkçi et al. [147] | 2015 | F/13 months old | Turkey | None | Bacteraemia, pneumonia | Cefepime, Gentamicin, Imipenem, Meropenem, Piperacillin–Tazobactam, TMP-SMZ | Cefotaxime, Ceftazidime, Ceftriaxone | Ceftriaxone | Complete Recovery |
| Hindilerden et al. [148] | 2015 | N/A | N/A | N/A | Bacteraemia | N/A | N/A | N/A | N/A |
| Patra et al. [149] | 2015 | M/54 years old | India | Guillain Barre Syndrome | Septicaemia | Amikacin, Ciprofloxacin, Gentamicin, Imipenem, Meropenem, Ofloxacin, TMP-SMZ, Piperacillin–Tazobactam | Ampicillin Aztreonam Ceftazidime, Ceftriaxone, Cefotaxime, Chloramphenicol, Piperacillin | Amikacin (15 mg/kg/day intravenous) Piperacillin–Tazobactam (3.375 g intravenous every 8 h) | Complete Recovery |
| Ashraf [150] | 2016 | F/58 years old | USA | Atrial fibrillation, End- stage renal disease with a failed kidney transplant, Coronary artery disease, | Septic shock, Infective endocarditis | N/A | N/A | Piperacillin–Tazobactum, vancomycin Followed by Meropenam | Complete Recovery |
| Haviari et al. [151] | 2016 | Multiple (3 Cases) | France | None | Bacteraemia (1 case)Urinary Tract Infection (2 cases) | Aminoglycosides, Carbapenems, Ciprofloxacin, Rifampin, Tigecycline, TMP-SMZ | Amoxicillin, Aztreonam, Cefalotine, Cefoxitine, Cefotaxime, Ceftazidime, Cefepime, Fosfomycin, Piperacillin, Ticarcillin | Ceftriaxone (1 g/day intravenously for 2/3 days) Ofloxacin (200 mg 2×/day orally for 10/21 days) | Complete Recovery |
| Jimenez and Antony, 2016 [152] | 2016 | M/40 years old | USA | Osteomyelitis and liver cirrhosis | Sepsis | Amikacin, Levofloxacin | Ampicillin–Sulbactam, Aztreonam, Cefepeme, Cefotaxime, Ceftazidime, Ceftriaxone | Levofloxacin | Complete Recovery |
| Kanjee et al. 2016 [153] | 2016 | F/60 years old | USA | None | Endophthalmitis | N/A | N/A | Moxifloxacin | Complete Recovery |
| Venkateswaran et al. [154] | 2016 | F/57 years old | USA | Herpetic keratitis and persistent central neurotrophic ulcer | Corneal ulcer keratitis (ocular detachment) | N/A | N/A | Tobramycin | Eye evisceration |
| Gigi et al. [155] | 2017 | M/18 years old | Israel | None | Osteomyelitis in the (Foot puncture) | N/A | N/A | Ciprofloxacin (Oral 750 mg 2/day) Clindamycin | Complete Recovery |
| Khasawneh & Yusef [156] | 2017 | F/Neonate | Jordan | Neonate | Sepsis (catheter related) | Amikacin, Imipenem, Meropenem, Piperacillin–Tazobactam | Ceftazidime, Cefipime, Gentamicin | Imipenem (25 mg/kg twice daily) Amikacin (15 mg/kg) | Complete Recovery |
| Rastogi & Mathur [23] | 2017 | M/58 years old | India | Severe head injury | Septicaemia with meningitis (catheter related) | Amikacin, Cefepime–Tazobactam, Colistin, Tigecycline TMP-SMZ | Ceftazidime, Cefepime, Cefoperazone–Sulbactam, Chloramphenicol, Ciprofloxacin, Imipenem, Meropenem Piperacillin–Tazobactam, | Cefepime–Tazobactam (1.12 gm) Amikacin (400 mg) (injection every 12 h) | Complete Recovery |
| Torres Aguilera et al. [157] | 2017 | F/88 years old | Spain | Diabetic and hypertensive, with significant vascular disease | Bacteraemia (catheter related) | N/A | N/A | Ciprofloxacin Catheter removal | Complete Recovery |
| Torres Aguilera et al. [157] | 2017 | M/84 years old HA |
Spain | Diabetic nephropathy | Bacteraemia (catheter related) | N/A | N/A | Initial treatment Ciprofloxacin Followed by Meropenem and TMP-SMZ Catheter removal | Complete Recovery |
| Cipolla et al. [158] | 2018 | Multiple (20 Cases) | Argentina | N/A | Bacteraemia | N/A | N/A | N/A | N/A |
| Hafeez et al. [159] | 2018 | M/64 years old | USA | Alcohol abuse, Hypertension | Pneumonia | N/A | N/A | Ciprofloxacin followed by Meropenem | Complete Recovery |
| Montaña et al. [61] | 2018 | Multiple (6 Cases) | Argentina | N/A | Pseudo-bacteraemia | N/A | Meropenem | N/A | N/A |
| Zhu et al. [160] | 2018 | Multiple (11 Cases) HA +CA | China | Various | Bloodstream infection (catheter related) | Ciprofloxacin, Levofloxacin, Imipenem, TMP-SMZ | Ampicillin, Cefoperazone–Sulbactam, Ceftazidime, Cefuroxime, Cefazolin, Piperacillin | Various | Complete Recovery (10 Cases) Died (1 case) |
| Caroleo et al. [161] | 2019 | Multiple (4 Cases) HA |
Italy | Cancer | Catheter-related bloodstream infections | N/A | N/A | N/A | N/A |
| Grabowska-Markowska et al. [162] | 2019 | M/13 years old | Poland | Neurodegenerative disorder | Bacteraemia | Imipenem, Meropenem | Ceftazidime, Piperacillin–Tazobactam | None | Complete Recovery |
| Kang et al. [163] | 2019 | F/53 years old | Korea | None | Keratitis | Ciprofloxacin, Gentamicin | Amoxicillin, Ampicillin, Benzylpenicillin, Cefepime, Ceftazidime, Ceftriaxone, Imipenem, Piperacillin | Gentamicin | Complete Recovery |
| Roussotte et al. [164] | 2019 | F/53 years old HA |
France | Facial oedema | Catheter-related infection associated with superior vena cava | Amikacin, Ciprofloxacin, Ertapenem Gentamicin Imipenem, Meropenem, Moxifloxacin, TMP-SMZ, Tobramycin | Ampicillin, Amoxicillin, Amoxicillin–Clavulanate, Aztreonam, Cefepime, Cefoxitine, Cefotaxime, Ceftazidime, Fosfomycin, Nalidixic acid, Piperacillin, Piperacillin–Tazobactam Ticarcillin–Clavulanate | Imipenem–Cilastine, Ciprofloxacin Catheter removal | Complete Recovery |
| Arimuthu and Seong Lim [165] | 2020 | M/24 years old HA |
Malaysia | Dengue viral fever | Bacteraemia (catheter related) | Ciprofloxacin, Gentamicin, Imipenem Meropenem, Tigecycline | Ceftazidime, Cefepime, Piperacillin–Tazobactam, Polymyxin B, TMP-SMZ | Meropenem (2 g thrice a day) After failure Catheter removal Ciprofloxacin (Intravenously 400 mg thrice a day) | Complete Recovery |
| Arimuthu and Seong Lim [165] | 2020 | M/64 years old HA |
Malaysia | Diabetes, end stage renal disease, Hypertension, Ischemic dilated cardiomyopathy | Bacteraemia (catheter related) | Ciprofloxacin, TMP-SMZ | N/A | Ciprofloxacin | Complete Recovery |
| Bratschi et al. [166] | 2020 | M/70 years old CA |
Switzerland | None | Hand infection | N/A | N/A | Surgical debridement Amoxicillin–clavulanic acid (empirically) Cefepime (2 g 3 times/day intravenously for 15 days) Co-trimoxazole (960 mg 3 times/day orally for 2 weeks) |
Complete Recovery |
| Ko et al. [167] | 2016–2020 | Multiple (5 cases) | Korea | Various (Pneumonia, Hypertension, Diabetes mellitus | Various | Ciprofloxacin, Levofloxacin, TMP-SMZ | Aztreonam, Cefepime, Cefotaxime; Ceftazidime, Piperacillin, Piperacillin–Tazobactam Ticacillin–Clavulanic acid |
Complete Recovery in 3 patients Death in 2 patients |
M, Male; F, Female; N/A, Not Available; CA, Community Acquired; HA, Hospital Acquired; TMP-SMZ, Trimethoprim–sulfamethoxazole. * Antibiotic susceptibility testing was carried out using a variety of methods including disk diffusion testing, agar and broth dilution testing and E-testing methods.
Table 5.
Incidences of Ochrobactrum spp. (excluding Ochrobactrum anthropi) infection from 1998–2020. Main characteristics of the case reports.
| Author (Ref) Bacteria |
Year | Sex/Age | Country | Co-Morbidity | Type of Infection | Susceptible to * | Resistance to * | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Möller et al. [8] Ochrobactrum intermedium |
1999 | F/45 years old | The Netherlands | Liver transplant patient | Bacteraemia | Ciprofloxacin, Imipenem, TMP-SMZ | Amoxicillin, Cefuroxime, Cefotaxime, Ceftazidime, Colistin, Piperacillin, Polymyxin B, Tobramycin | Imipenem Tobramycin | Complete Recovery |
| Apisarnthanarak et al. [171] Ochrobactrum intermedium |
2005 | M/74 years old | Thailand | Bladder cancer | Bacteraemia | Aminoglycosides, Carbapenems, Fluoroquinolones, TMP-SMZ | N/A | Ciprofloxacin Imipenem | Complete Recovery |
| Vaidya et al. [106] Ochrobactrum intermedium |
2006 | M/49 years old | USA | None | Pelvic abscess | Gentamicin, Imipenem, Levofloxacin, TMP-SMZ | Cefepime, Tobramycin | Levofloxacin, Metronidazole | Complete Recovery |
| Teyssier et al. [36] Ochrobactrum pseudintermedium |
2007 | Multiple (2 cases) | France | N/A | ICU patient | Ciprofloxacin, Gentamicin, Nalidixic acid, Ofloxacin, Pefloxacin, Rifampicin | Fosfomycin | N/A | N/A |
| Dharne et al. [172] Ochrobactrum intermedium |
2008 | M/ | India | N/A | Stomach isolate from non-ulcer dyspeptic patient | N/A | N/A | N/A | N/A |
| Jacobs et al. [173] Ochrobactrum intermedium |
2013 | M/34 years old | USA | None | Endophthalmitis (metallic intraocular foreign body contamination) | Ciprofloxacin, Levofloxacin, TMP-SMZ | Amikacin, Ampicillin, Ampicillin–Sulbactam, Ceftazidime, Ceftriaxone, Gentamicin, Piperacillin–Tazobactam, Tobramycin | Moxifloxacin | Complete Recovery |
| Hirai et al. 2016 [59] Ochrobactrum intermedium |
2016 | M/86 years old | Japan | N/A | Pneumonia (catheter related) | Amikacin, Ciprofloxacin, Imipenem, Levofloxacin, Meropenem, Minocycline | Aztreonam, Ceftazidime | Ampicillin–Sulbactam followed by Meropenem (2 g/day) | Complete Recovery |
| Borges et al. [174] Ochrobactrum oryzae | 2016 | M/86 years old | Brazil | Hypertension, type II diabetes mellitus, dyslipideamia, end stage renal disease | Bloodstream infection | Amikacin, Ciprofloxacin, Imipenem, Meropenem, | Polymyxin B | Imipenem | Complete Recovery |
| Hong et al. [175] Ochrobactrum tritici |
2016 | M/70 years old | Korea | Cholangiocellular carcinoma | Bacteraemia, Cholecystitis | N/A | Ceftriaxone, Cefepime, Ticarcillin | Cefoperazone–Sulbactam (2000 mg every 12 h), Metronidazole (500 mg every 8 h) | Complete Recovery |
| Bharucha et al. [176] Ochrobactrum intermedium |
2019 | M/23 years old | UK | Undergoing haemodialysis | Endocarditis (catheter related) | Ertapenem, Meropenem, Tigecycline | Ciprofloxacin, Colistin, Fosfomycin | Meropenem (1 g iv twice daily), Minocycline (100 mg iv twice daily) | Complete Recovery |
| Cho et al. [177] Ochrobactrum pseudogrignonense |
2020 | M/44 years old | Korea | Hypertension, diabetes mellitus, dilated cardiomyopathy | Bacteraemia | Amikacin, Ampicillin–Sulbactam, Ceftazidime, Cefepime, Cefotaxime, Ciprofloxacin, Colistin, Gentamicin, Imipenem, Meropenem, Minocycline, TMP-SMZ | Aztreonam, Piperacillin, Piperacillin–Tazobactam | Vancomycin and Piperacillin–Tazobactam Followed by Meropenem | Complete Recovery |
M, Male; F, Female; N/A, Not Available; CA, Community Acquired; HA, Hospital Acquired; TMP-SMZ, Trimethoprim–sulfamethoxazole. * Antibiotic susceptibility testing was carried out using a variety of methods including disk diffusion testing, agar and broth dilution testing and E-testing methods.
6. Factors Linked with Ochrobactrum spp. Infection
6.1. Underlying Conditions/Illness
The bulk of Ochrobactrum related infections (Table 4 and Table 5) had an associated underlying disorder or disease that increased patient susceptibility to infection. Multiple patients, who were afflicted with a variety of different cancers or those with kidney failure (caused by diabetes mellitus), contracted Ochrobactrum-related bacteraemia/septicaemia due to a catheter/undergoing dialysis. These demonstrate how Ochrobactrum acts as an opportunistic pathogen in immunocompromised individuals. Infections were both hospital and community acquired. This is of interest as opportunistic pathogens such as Ochrobactrum spp. are mostly contracted in clinical environments. It was also interesting that a high level of instances of infection, 23 separate instances, occurred where patients had no underlying health conditions.
6.2. Pseudo-Outbreaks
To date, six pseudo-outbreaks have been described with Ochrobactrum spp. (Table 4 and Table 5). These may be challenging as they may lead to unessential/unneeded treatments such as needless courses of antibiotics or patient interventions (e.g., the removal of indwelling devices including various catheter types) and can waste both time and resources in both the clinical laboratory and treatment ward settings. Pseudo-outbreaks have many possible causes including contaminated water or materials used in the clinical testing laboratory or contaminated medical solutions such as saline. Montaña et al. described how O. anthropi was the reason for a pseudo-outbreak in a general treatment ward in an Argentinean hospital due to contaminated collection tubes [61]. No symptoms connected with bacterial infection were observed in any patients, even though O. anthropi was identified in microbiological testing. The recovered bacteria were carbapenem-resistant.
7. Treatment of Ochrobactrum spp. Infections
Treatment of Ochrobactrum spp. infections is often problematic, due to their resistance to different families of antibiotics such as β-lactams (penicillins, cephlasporins and emerging cases of carbapenem resistance). The antibiotic susceptibility profiles of some 103 typed strains of Ochrobactrum were analysed using the E-test™ for 19 clinically relevant antimicrobials [46]. In general, strains were highly resistant to β-lactam antibiotics, susceptible to ciprofloxacin, and 97.1% of the strains tested were susceptible to trimethoprim/sulfamethoxazole. This suggests that ciprofloxacin and/or trimethoprim/sulfamethoxazole in combination may be useful for empirical treatment of Ochrobactrum infections [46]. In the majority of outbreaks described in Table 4, aminoglycoside, fluoroquinolone, carbapenem or trimethoprim/sulfamethoxazole antibiotics were used in patient treatment. In the majority of cases, these treatments were successful in curing infections. However, as can be seen in Table 4, resistance was observed in various different outbreaks to all these antibiotics. An example of this is reported in a case of O. anthropi bacteraemia in a patient in Japan in 2013 where susceptibility testing showed the organism to be resistant to aztreonam, ceftazidime, cefepime, ciprofloxacin, gentamicin, levofloxacin, piperacillin, piperacillin–tazobactam and trimethoprim–sulfamethoxazole [51]. There have been no controlled trials of antibiotic therapies for Ochrobactrum spp. infections in humans therefore treatment should be based upon the results of in vitro susceptibility testing on the isolated clinical strains. Resistance to β-lactam antibiotics (cephalosporins, cephamycins and β-lactamase inhibitors) is due to a chromosomal gene (blaoch) that is similar to the Ambler class C β-lactamase gene. This gene encodes an AmpC-like enzyme that is called OCH [168]. In addition, a plasmid-borne blaoxa-181 gene has been found in some Ochrobactrum intermedium strains giving resistance to carbapenems [169]. Three Ochrobactrum spp. strains isolated from birds in Pakistan harboured aminoglycoside (aadB, aadA2, aac6-Ib and strA, strB) β-lactam (blaoch2 and carb2), tetracycline (tetG), chloramphenicol (floR), sulphonamide (sulI) and trimethoprim (dfrA10) resistance genes [170].
8. Conclusions
Ochrobactrum spp. are not presently thought of as major pathogens. Nevertheless, as a result of our literature search, it can be seen that there have been 128 separate outbreaks of Ochrobactrum spp. infections reported. Thus, the consideration that they may be innocuous should in our opinion be reconsidered based on these findings. Although the genus is considered of low virulence and of lower risk compared to other non-fermenting Gram-negative bacteria such as Pseudomonas aeruginosa, we feel it must not be ignored as a potential cause of infections (nosocomial or otherwise) and should be included in routine screening programs in hospitals.
Author Contributions
Conceptualisation, M.P.R.; methodology, M.P.R. and J.T.P.; formal analysis, M.P.R. and J.T.P.; investigation, M.P.R. and J.T.P.; data curation, M.P.R. and J.T.P.; writing—original draft preparation, M.P.R. and J.T.P.; writing—review and editing, M.P.R. and J.T.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ryan M.P., Adley C.C. Ralstonia spp.: Emerging global opportunistic pathogens. Eur. J. Clin. Microbiol. Infect. Dis. 2014;33:291–304. doi: 10.1007/s10096-013-1975-9. [DOI] [PubMed] [Google Scholar]
- 2.Ryan M.P., Pembroke J.T., Adley C.C. Ralstonia pickettii: A persistent Gram-negative nosocomial infectious organism. J. Hosp. Infect. 2006;62:278–284. doi: 10.1016/j.jhin.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Ryan M.P., Adley C.C. Sphingomonas paucimobilis: A persistent Gram-negative nosocomial infectious organism. J. Hosp. Infect. 2010;75:153–157. doi: 10.1016/j.jhin.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 4.Coughlan A., Ryan M.P., Cummins N.M., Towler M.R. The response of Pseudomonas aeruginosa biofilm to the presence of a glass polyalkenoate cement formulated from a silver containing glass. J. Mater. Sci. 2011;46:285–287. doi: 10.1007/s10853-010-4945-y. [DOI] [Google Scholar]
- 5.Ryan M.P., Pembroke J.T. Brevundimonas spp.: Emerging global opportunistic pathogens. Virulence. 2018;9:480–493. doi: 10.1080/21505594.2017.1419116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jelveh N., Cunha B.A. Ochrobactrum anthropi bacteremia. Hear. Lung J. Acute Crit. Care. 1999;28:145–146. doi: 10.1053/hl.1999.v28.a94602. [DOI] [PubMed] [Google Scholar]
- 7.Handschuh H., Ryan M.P., O’Dwyer J., Adley C.C. Assessment of the bacterial diversity of aircraft water: Identification of the frequent fliers. PLoS ONE. 2017;12:e0170567. doi: 10.1371/journal.pone.0170567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Möller L.V.M., Arends J.P., Harmsen H.J.M., Talens A., Terpstra P., Slooff M.J.H. Ochrobactrum intermedium infection after liver transplantation. J. Clin. Microbiol. 1999;37:241–244. doi: 10.1128/JCM.37.1.241-244.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lebuhn M., Achouak W., Schloter M., Berge O., Meier H., Barakat M., Hartmann A., Heulin T. Taxonomic characterization of Ochrobactrum sp. isolates from soil samples and wheat roots, and description of Ochrobactrum tritici sp. nov. and Ochrobactrum grignonense sp. nov. Int. J. Syst. Evol. Microbiol. 2000;50:2207–2223. doi: 10.1099/00207713-50-6-2207. [DOI] [PubMed] [Google Scholar]
- 10.Goris J., Boon N., Lebbe L., Verstraete W., De Vos P. Diversity of activated sludge bacteria receiving the 3-chloroaniline-degradative plasmid pC1gfp. FEMS Microbiol. Ecol. 2003;46:221–230. doi: 10.1016/S0168-6496(03)00231-9. [DOI] [PubMed] [Google Scholar]
- 11.Kämpfer P., Buczolits S., Albrecht A., Busse H.J., Stackebrandt E. Towards a standardized format for the description of a novel species (of an established genus): Ochrobactrum gallinifaecis sp. nov. Int. J. Syst. Evol. Microbiol. 2003;53:893–896. doi: 10.1099/ijs.0.02710-0. [DOI] [PubMed] [Google Scholar]
- 12.Bathe S., Achouak W., Hartmann A., Heulin T., Schloter M., Lebuhn M. Genetic and phenotypic microdiversity of Ochrobactrum spp. FEMS Microbiol. Ecol. 2006;56:272–280. doi: 10.1111/j.1574-6941.2005.00029.x. [DOI] [PubMed] [Google Scholar]
- 13.El-Sayed W.S., Ibrahim M.K., Abu-Shady M., El-Beih F., Ohmura N., Saiki H., Ando A. Isolation and Identification of a Novel Strain of the Genus Ochrobactrum with Phenol-Degrading Activity. J. Biosci. Bioeng. 2003;96:310–312. doi: 10.1016/S1389-1723(03)80200-1. [DOI] [PubMed] [Google Scholar]
- 14.Sultan S., Hasnain S. Reduction of toxic hexavalent chromium by Ochrobactrum intermedium strain SDCr-5 stimulated by heavy metals. Bioresour. Technol. 2007;98:340–344. doi: 10.1016/j.biortech.2005.12.025. [DOI] [PubMed] [Google Scholar]
- 15.Wu Y., He T., Zhong M., Zhang Y., Li E., Huang T., Hu Z. Isolation of marine benzo[a]pyrene-degrading Ochrobactrum sp. BAP5 and proteins characterization. J. Environ. Sci. 2009;21:1446–1451. doi: 10.1016/S1001-0742(08)62438-9. [DOI] [PubMed] [Google Scholar]
- 16.Zhang X.H., Zhang G.S., Zhang Z.H., Xu J.H., Li S.P. Isolation and characterization of a dichlorvos-degrading strain DDV-1 of Ochrobactrum sp. Pedosphere. 2006;16:64–71. doi: 10.1016/S1002-0160(06)60027-1. [DOI] [Google Scholar]
- 17.Kettaneh A., Weill F.X., Poilane I., Fain O., Thomas M., Herrmann J.L., Hocqueloux L. Septic shock caused by Ochrobactrum anthropi in an otherwise healthy host. J. Clin. Microbiol. 2003;41:1339–1341. doi: 10.1128/JCM.41.3.1339-1341.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ozdemir D., Soypacaci Z., Sahin I., Bicik Z., Sencan I. Ochrobactrum anthropi endocarditis and septic shock in a patient with no prosthetic valve or rheumatic heart disease: Case report and review of the literature. Jpn. J. Infect. Dis. 2006;59:264–265. [PubMed] [Google Scholar]
- 19.Chester B., Cooper L.H. Achromobacter species (CDC group Vd): Morphological and biochemical characterization. J. Clin. Microbiol. 1979;9:425–436. doi: 10.1128/jcm.9.3.425-436.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barson W.J., Cromer B.A., Marcon M.J. Puncture wound osteochondritis of the foot caused by CDC group Vd. J. Clin. Microbiol. 1987;25:2014–2016. doi: 10.1128/JCM.25.10.2014-2016.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holmes B., Popoff M., Kiredjian M., Kersters K. Ochrobactrum anthropi gen. nov., sp. nov. from human clinical specimens and previously known as group Vd. Int. J. Syst. Bacteriol. 1988;38:406–416. doi: 10.1099/00207713-38-4-406. [DOI] [Google Scholar]
- 22.Velasco J., Romero C., López-Goñi I., Leiva J., Dĩaz R., Moriyón I. Evaluation of the relatedness of Brucella spp. and Ochrobactrum anthropi and description of Ochrobactrum intermedium sp. nov., a new species with a closer relationship to Brucella spp. Int. J. Syst. Bacteriol. 1998;48:759–768. doi: 10.1099/00207713-48-3-759. [DOI] [PubMed] [Google Scholar]
- 23.Rastogi N., Mathur P. Ochrobactrum anthropi: An emerging pathogen causing meningitis with sepsis in a neurotrauma patient. J. Infect. Dev. Ctries. 2017;11:733–735. doi: 10.3855/jidc.9146. [DOI] [PubMed] [Google Scholar]
- 24.Nadjar D., Labia R., Cerceau C., Bizet C., Philippon A., Arlet G. Molecular characterization of chromosomal class C β-lactamase and its regulatory gene in Ochrobactrum anthropi. Antimicrob. Agents Chemother. 2001;45:2324–2330. doi: 10.1128/AAC.45.8.2324-2330.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Soloaga R., Carrion N., Pidone J., Guelfand L., Margari A., Altieri R. Bacteremia relacionada a cateter por Ochrobactrum anthropi. Medicina. 2009;69:655–657. [PubMed] [Google Scholar]
- 26.Imran A., Hafeez F.Y., Frühling A., Schumann P., Malik K.A., Stackebrandt E. Ochrobactrum ciceri sp. nov., isolated from nodules of Cicer arietinum. Int. J. Syst. Evol. Microbiol. 2010;60:1548–1553. doi: 10.1099/ijs.0.013987-0. [DOI] [PubMed] [Google Scholar]
- 27.Zurdo-Piñeiro J.L., Rivas R., Trujillo M.E., Vizcaíno N., Carrasco J.A., Chamber M., Palomares A., Mateos P.F., Martínez-Molina E., Velázquez E. Ochrobactrum cytisi sp. nov., isolated from nodules of Cytisus scoparius in Spain. Int. J. Syst. Evol. Microbiol. 2007;57:784–788. doi: 10.1099/ijs.0.64613-0. [DOI] [PubMed] [Google Scholar]
- 28.Woo S.G., Ten L.N., Park J., Lee M. Ochrobactrum daejeonense sp. nov., a nitrate-reducing bacterium isolated from sludge of a leachate treatment plant. Int. J. Syst. Evol. Microbiol. 2011;61:690–696. doi: 10.1099/ijs.0.025510-0. [DOI] [PubMed] [Google Scholar]
- 29.Li L., Li Y.Q., Jiang Z., Gao R., Nimaichand S., Duan Y.Q., Egamberdieva D., Chen W., Li W.J. Ochrobactrum endophyticum sp. nov., isolated from roots of Glycyrrhiza uralensis. Arch. Microbiol. 2016;198:171–179. doi: 10.1007/s00203-015-1170-8. [DOI] [PubMed] [Google Scholar]
- 30.Kämpfer P., Scholz H.C., Huber B., Falsen E., Busse H.J. Ochobactrum haematophilum sp. nov. and Ochrobactrum pseudogrignonense sp. nov., isolated from human clinical specimens. Int. J. Syst. Evol. Microbiol. 2007;57:2513–2518. doi: 10.1099/ijs.0.65066-0. [DOI] [PubMed] [Google Scholar]
- 31.Trujillo M.E., Willems A., Abril A., Planchuelo A.M., Rivas R., Ludeña D., Mateos P.F., Martínez-Molina E., Velázquez E. Nodulation of Lupinus albus by Strains of Ochrobactrum lupini sp. nov. Appl. Environ. Microbiol. 2005;71:1318–1327. doi: 10.1128/AEM.71.3.1318-1327.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Volpiano C.G., Sant’anna F.H., Ambrosini A., Lisboa B.B., Vargas L.K., Passaglia L.M.P. Reclassification of Ochrobactrum lupini as a later heterotypic synonym of Ochrobactrum anthropi based on whole-genome sequence analysis. Int. J. Syst. Evol. Microbiol. 2019;69:2312–2314. doi: 10.1099/ijsem.0.003465. [DOI] [PubMed] [Google Scholar]
- 33.Tripathi A.K., Verma S.C., Chowdhury S.P., Lebuhn M., Gattinger A., Schloter M. Ochrobactrum oryzae sp. nov., an endophytic bacterial species isolated from deep-water rice in India. Int. J. Syst. Evol. Microbiol. 2006;56:1677–1680. doi: 10.1099/ijs.0.63934-0. [DOI] [PubMed] [Google Scholar]
- 34.Kämpfer P., Huber B., Busse H.J., Scholz H.C., Tomaso H., Hotzel H., Melzer F. Ochrobactrum pecoris sp. nov., isolated from farm animals. Int. J. Syst. Evol. Microbiol. 2011;61:2278–2283. doi: 10.1099/ijs.0.027631-0. [DOI] [PubMed] [Google Scholar]
- 35.Huber B., Scholz H.C., Kämpfer P., Falsen E., Langer S., Busse H.J. Ochrobactrum pituitosum sp. nov., isolated from an industrial environment. Int. J. Syst. Evol. Microbiol. 2010;60:321–326. doi: 10.1099/ijs.0.011668-0. [DOI] [PubMed] [Google Scholar]
- 36.Teyssier C., Marchandin H., Jean-Pierre H., Masnou A., Dusart G., Jumas-Bilak E. Ochrobactrum pseudintermedium sp. nov., a novel member of the family Brucellaceae, isolated from human clinical samples. Int. J. Syst. Evol. Microbiol. 2007;57:1007–1013. doi: 10.1099/ijs.0.64416-0. [DOI] [PubMed] [Google Scholar]
- 37.Krzyżanowska D.M., Maciąg T., Ossowicki A., Rajewska M., Kaczyński Z., Czerwicka M., Rąbalski Ł., Czaplewska P., Jafra S. Ochrobactrum quorumnocens sp. Nov., a quorum quenching bacterium from the potato rhizosphere, and comparative genome analysis with related type strains. PLoS ONE. 2019;14:e0210874. doi: 10.1371/journal.pone.0210874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kämpfer P., Sessitsch A., Schloter M., Huber B., Busse H.J., Scholz H.C. Ochrobactrum rhizosphaerae sp. nov. and Ochrobactrum thiophenivorans sp. nov., isolated from the environment. Int. J. Syst. Evol. Microbiol. 2008;58:1426–1431. doi: 10.1099/ijs.0.65407-0. [DOI] [PubMed] [Google Scholar]
- 39.Choi G.M., Kim K.M., Yun C.S., Lee S.Y., Kim S.Y., Wee J.H., Im W.T. Ochrobactrum soli sp. nov., Isolated from a Korean cattle farm. Curr. Microbiol. 2020;77:1104–1110. doi: 10.1007/s00284-020-01882-y. [DOI] [PubMed] [Google Scholar]
- 40.Hu M., Li X., Li Z., Liu B., Yang Z., Tian Y. Ochrobactrum teleogrylli sp. nov., a pesticide-degrading bacterium isolated from the insect Teleogryllus occipitalis living in deserted cropland. Int. J. Syst. Evol. Microbiol. 2020;70:2217–2225. doi: 10.1099/ijsem.0.003964. [DOI] [PubMed] [Google Scholar]
- 41.Kumar S., Stecher G., Li M., Knyaz C., Tamura K. MEGA X: Molecular Evolutionary Genetics Analysis across computing platforms. Mol. Biol. Evol. 2018;35:1547–1549. doi: 10.1093/molbev/msy096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ryan M.P., Adley C.C., Pembroke J.T. The use of MEGA as an educational tool for examining the phylogeny of antibiotic resistance genes. In: Méndez-Vilas A., editor. Microbial Pathogens and Strategies for Combating Them: Science, Technology and Education. Volume 4. Formatex; Badajoz, Spain: 2013. pp. 736–743. [Google Scholar]
- 43.Teyssier C., Marchandin H., Jean-Pierre H., Diego I., Darbas H., Jeannot J.L., Gouby A., Jumas-Bilak E. Molecular and phenotypic features for identification of the opportunistic pathogens Ochrobactrum spp. J. Med. Microbiol. 2005;54:945–953. doi: 10.1099/jmm.0.46116-0. [DOI] [PubMed] [Google Scholar]
- 44.Quirino A., Pulcrano G., Rametti L., Puccio R., Marascio N., Catania M.R., Matera G., Liberto M.C., Focà A. Typing of Ochrobactrum anthropi clinical isolates using automated repetitive extragenic palindromic-polymerase chain reaction DNA fingerprinting and matrix-assisted laser desorption/ionization-time-of-flight mass spectrometry. BMC Microbiol. 2014;14:74. doi: 10.1186/1471-2180-14-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kämpfer P., Citron D.M., Goldstein E.J.C., Scholz H.C. Difficulty in the identification and differentiation of clinically relevant Ochrobactrum species. J. Med. Microbiol. 2007;56:1571–1573. doi: 10.1099/jmm.0.47350-0. [DOI] [PubMed] [Google Scholar]
- 46.Thoma B., Straube E., Scholz H.C., Al Dahouk S., Zöller L., Pfeffer M., Neubauer H., Tomaso H. Identification and antimicrobial susceptibilities of Ochrobactrum spp. Int. J. Med. Microbiol. 2009;299:209–220. doi: 10.1016/j.ijmm.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 47.Elsaghir A.A.F., James E.A. Misidentification of Brucella melitensis as Ochrobactrum anthropi by API 20NE. J. Med. Microbiol. 2003;52:441–442. doi: 10.1099/jmm.0.05153-0. [DOI] [PubMed] [Google Scholar]
- 48.Oliver J.W. Ochrobactrum anthropi misidentified as Shewanella putrefaciens. J. Clin. Microbiol. 2003;41:4486. doi: 10.1128/JCM.41.9.4486.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Trêpa J., Mendes P., Gonçalves R., Chaves C., Brás A.M., Mesa A., Ramos I., Sá R., da Cunha J.G.S. Brucella vertebral osteomyelitis misidentified as an Ochrobactrum anthropi infection. IDCases. 2018;11:74–76. doi: 10.1016/j.idcr.2018.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vila A., Pagella H., Bello G.V., Vicente A. Brucella suis bacteremia misidentified as Ochrobactrum anthropi by the VITEK 2 system. J. Infect. Dev. Ctries. 2016;10:432–436. doi: 10.3855/jidc.7532. [DOI] [PubMed] [Google Scholar]
- 51.Hagiya H., Ohnishi K., Maki M., Watanabe N., Murasec T. Clinical Characteristics of Ochrobactrum anthropi Bacteremia. J. Clin. Microbiol. 2013;51:1330–1333. doi: 10.1128/JCM.03238-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Van Dijck P., Delmée M., Ezzedine H., Deplano A., Struelens M.J. Evaluation of pulsed-field gel electrophoresis and rep-PCR for the epidemiological analysis of Ochrobactrum anthropi strains. Eur. J. Clin. Microbiol. Infect. Dis. 1995;14:1099–1102. doi: 10.1007/BF01590948. [DOI] [PubMed] [Google Scholar]
- 53.Leal-Klevezas D.S., Martínez-De-La-Vega O., Ramírez-Barba E.J., Osterman B., Martínez-Soriano J.P., Simpson J. Genotyping of Ochrobactrum spp. by AFLP analysis. J. Bacteriol. 2005;187:2537–2539. doi: 10.1128/JB.187.7.2537-2539.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Aujoulat F., Romano-Bertrand S., Masnou A., Marchandin H., Jumas-Bilak E. Niches, population structure and genome reduction in Ochrobactrum intermedium: Clues to technology-driven emergence of pathogens. PLoS ONE. 2014;9:e83376. doi: 10.1371/journal.pone.0083376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Scholz H.C., Tomaso H., Dahouk S.A., Witte A., Schloter M., Kämpfer P., Falsen E., Neubauer H. Genotyping of Ochrobactrum anthropi by recA-based comparative sequence, PCR-RFLP, and 16S rRNA gene analysis. FEMS Microbiol. Lett. 2006;257:7–16. doi: 10.1111/j.1574-6968.2006.00153.x. [DOI] [PubMed] [Google Scholar]
- 56.Scholz H.C., Al Dahouk S., Tomaso H., Neubauer H., Witte A., Schloter M., Kämpfer P., Falsen E., Pfeffer M., Engel M. Genetic diversity and phylogenetic relationships of bacteria belonging to the Ochrobactrum-Brucella group by recA and 16S rRNA gene-based comparative sequence analysis. Syst. Appl. Microbiol. 2008;31:1–16. doi: 10.1016/j.syapm.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 57.Scholz H.C., Pfeffer M., Witte A., Neubauer H., Dahouk S.A., Wernery U., Tomaso H. Specific detection and differentiation of Ochrobactrum anthropi, Ochrobactrum intermedium and Brucella spp. by a multi-primer PCR that targets the recA gene. J. Med. Microbiol. 2008;57:64–71. doi: 10.1099/jmm.0.47507-0. [DOI] [PubMed] [Google Scholar]
- 58.Bizzini A., Jaton K., Romo D., Bille J., Prod’hom G., Greub G. Matrix-assisted laser desorption ionization—Time of flight mass spectrometry as an alternative to 16S rRNA gene sequencing for identification of difficult-to-identify bacterial strains. J. Clin. Microbiol. 2011;49:693–696. doi: 10.1128/JCM.01463-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hirai J., Yamagishi Y., Sakanashi D., Koizumi Y., Suematsu H., Mikamo H. A case of bacteremia caused by Ochrobacterium intermedium. Kansenshogaku Zasshi. 2016;90:129–133. doi: 10.11150/kansenshogakuzasshi.90.129. [DOI] [PubMed] [Google Scholar]
- 60.Yagel Y., Sestito S., Motro Y., Shnaiderman-Torban A., Khalfin B., Sagi O., Navon-Venezia S., Steinman A., Moran-Gilad J. Genomic characterization of antimicrobial resistance, virulence, and phylogeny of the genus Ochrobactrum. Antibiotics. 2020;9:177. doi: 10.3390/antibiotics9040177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Montaña S., Fernandez J.S., Barenboim M., Hernandez M., Kayriyama C., Carulla M., Iriarte A., Ramirez M.S., Almuzara M. Whole-genome analysis and description of an outbreak due to carbapenem-resistant Ochrobactrum anthropi causing pseudo-bacteraemias. New Microbes New Infect. 2018;26:100–106. doi: 10.1016/j.nmni.2018.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Appelbaum P.C., Campbell D.B. Pancreatic abscess associated with Achromobacter group Vd biovar 1. J. Clin. Microbiol. 1980;12:282–283. doi: 10.1128/JCM.12.2.282-283.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kish M.A., Buggy B.P., Forbes B.A. Bacteremia caused by Achromobacter species in an immunocompromised host. J. Clin. Microbiol. 1984;19:947–948. doi: 10.1128/JCM.19.6.947-948.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Van Horn K.G., Gedris C.A., Ahmed T., Wormser G.P. Bacteremia and urinary tract infection associated with CDC group Vd biovar 2. J. Clin. Microbiol. 1989;27:201–202. doi: 10.1128/JCM.27.1.201-202.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cieslak T.J., Robb M.L., Drabick C.J., Fischer G.W. Catheter-associated sepsis caused by Ochrobactrum anthropi: Report of a case and review of related non-fermentative bacteria. Clin. Infect. Dis. 1992;14:902–907. doi: 10.1093/clinids/14.4.902. [DOI] [PubMed] [Google Scholar]
- 66.Gransden W.R., Eykyn S.J. Seven cases of bacteremia due to Ochrobactrum anthropi. Clin. Infect. Dis. 1992;15:1068–1069. doi: 10.1093/clind/15.6.1068. [DOI] [PubMed] [Google Scholar]
- 67.Brivet F., Guibert M., Kiredjian M., Dormont J. Necrotizing Fasciitis, bacteremia, and multiorgan failure caused by Ochrobactrum anthropi. Clin. Infect. Dis. 1993;17:516–517. doi: 10.1093/clinids/17.3.516. [DOI] [PubMed] [Google Scholar]
- 68.Kern W.V., Oethinger M., Marre R., Kaufhold A., Rozdzinski E. Ochrobactrum anthropi bacteremia: Report of four cases and short review. Infection. 1993;21:306–310. doi: 10.1007/BF01712451. [DOI] [PubMed] [Google Scholar]
- 69.Klein J.D., Eppes S.C. Ochrobactrum anthropi bacteremia in a child. Del. Med. J. 1993;65:493–495. [PubMed] [Google Scholar]
- 70.Alnor D., Frimodt-Møller N., Espersen F., Frederiksen W. Infections with the unusual human pathogens agrobacterium species and Ochrobactrum anthropi. Clin. Infect. Dis. 1994;18:914–920. doi: 10.1093/clinids/18.6.914. [DOI] [PubMed] [Google Scholar]
- 71.Ezzedine H., Mourad M., Van Ossel C., Logghe C., Squifflet J.P., Renault F., Wauters G., Gigi J., Wilmotte L., Haxhe J.J. An outbreak of Ochrobactrum anthropi bacteraemia in five organ transplant patients. J. Hosp. Infect. 1994;27:35–42. doi: 10.1016/0195-6701(94)90066-3. [DOI] [PubMed] [Google Scholar]
- 72.Haditsch M., Binder L., Tschurtschenthaler G., Watschinger R., Zauner G., Mittermayer H. Bacteremia caused by Ochrobactrum anthropi in an immunocompromised child. Infection. 1994;22:291–292. doi: 10.1007/BF01739922. [DOI] [PubMed] [Google Scholar]
- 73.Braun M., Jonas J.B., Schonherr U., Naumann G.O.H. Ochrobactrum anthropi endophthalmitis after uncomplicated cataract surgery. Am. J. Ophthalmol. 1996;122:272–273. doi: 10.1016/S0002-9394(14)72025-2. [DOI] [PubMed] [Google Scholar]
- 74.Chang H.J., Christenson J.C., Pavia A.T., Bobrin B.D., Bland A.L., Carson L.A., Arduino M.J., Verma P., Aguero S.M., Carroll K., et al. Ochrobactrum anthropi meningitis in pediatric pericardial allograft transplant recipients. J. Infect. Dis. 1996;173:656–660. doi: 10.1093/infdis/173.3.656. [DOI] [PubMed] [Google Scholar]
- 75.Cieslak T.J., Drabick C.J., Robb M.L. Pyogenic infections due to Ochrobactrum anthropi. Clin. Infect. Dis. 1996;22:845–847. doi: 10.1093/clinids/22.5.845. [DOI] [PubMed] [Google Scholar]
- 76.Ramos J.M., Román A., Fernández-Roblas R., Cabello A., Soriano F. Infection caused by Ochrobactrum anthropi. Clin. Microbiol. Infect. 1996;1:214–216. doi: 10.1111/j.1469-0691.1996.tb00561.x. [DOI] [PubMed] [Google Scholar]
- 77.Berman A.J., Del Priore L.V., Fischer C.K. Endogenous Ochrobactrum anthropi endophthalmitis. Am. J. Ophthalmol. 1997;123:560–562. doi: 10.1016/S0002-9394(14)70190-4. [DOI] [PubMed] [Google Scholar]
- 78.Christenson J.C., Pavia A.T., Seskin K., Brockmeyer D., Korgenski E.K., Jenkins E., Pierce J., Daly J.A. Meningitis due to Ochrobactrum anthropi: An emerging nosocomial pathogen. Pediatr. Neurosurg. 1997;27:218–221. doi: 10.1159/000121256. [DOI] [PubMed] [Google Scholar]
- 79.Earhart K.C., Boyce K., Bone W.D., Wallace M.R. Ochrobactrum anthropi infection of retained pacemaker leads. Clin. Infect. Dis. 1997;24:281–282. doi: 10.1093/clinids/24.2.281. [DOI] [PubMed] [Google Scholar]
- 80.Gill M.V., Ly H., Mueenuddin M., Schoch P.E., Cunha B.A. Intravenous line infection due to Ochrobactrum anthropi (CDC group Vd) in a normal host. Hear. Lung J. Acute Crit. Care. 1997;26:335–336. doi: 10.1016/S0147-9563(97)90092-3. [DOI] [PubMed] [Google Scholar]
- 81.Torres L., Arazo P., Seoane A., Marco M.L. Bacteriemia por Ochrobactrum anthropi en un paciente con sida Ochrobactrum anthropi bacteremia in a patient with AIDS. Med. Clin. 1998;111:318. [PubMed] [Google Scholar]
- 82.Yu W.L., Lin C.W., Wang D.Y. Clinical and microbiologic characteristics of Ochrobactrum anthropi bacteremia. J. Formos. Med. Assoc. 1998;97:106–112. [PubMed] [Google Scholar]
- 83.Hay A.J., Lo T.Y. Ochrobactrum anthropi meningitis in a pre-term neonate. J. Infect. 1999;38:134–135. doi: 10.1016/S0163-4453(99)90088-9. [DOI] [PubMed] [Google Scholar]
- 84.Inoue K., Numaga J., Nagata Y., Sakurai M., Aso N., Fujino Y. Ochrobactrum anthropi endophthalmitis after vitreous surgery. Br. J. Ophthalmol. 1999;83:501b. doi: 10.1136/bjo.83.4.501b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Manfredi R., Nanetti A., Ferri M., Chiodo F. Nosocomial sepsis due to Ochrobactrum anthropi in HIV positive patients: Two case reports. Infez. Med. 1999;7:119–124. [PubMed] [Google Scholar]
- 86.Mastroianni A., Cancellieri C., Montini G. Ochrobactrum anthropi bacteremia: Case report and review of the literature. Clin. Microbiol. Infect. 1999;5:570–573. doi: 10.1111/j.1469-0691.1999.tb00437.x. [DOI] [PubMed] [Google Scholar]
- 87.Saavedra J., Garrido C., Folgueira D., Torres M.J., Ramos J.T. Ochrobactrum anthropi bacteremia associated with a catheter in an immunocompromised child and review of the pediatric literature. Pediatr. Infect. Dis. J. 1999;18:658–660. doi: 10.1097/00006454-199907000-00023. [DOI] [PubMed] [Google Scholar]
- 88.Stiakaki E., Bolonaki I., Maraki S., Samonis G., Kambourakis A., Tselentis I., Kalmanti M. Ochrobactrum anthropi bacterenha in children with central venous catheters. J. Pediatr. Hematol. Oncol. 1999;21:338. doi: 10.1097/00043426-199907000-00135. [DOI] [Google Scholar]
- 89.Blecker Shelly D., Mortensen J.E. A pediatric case report and review of infections caused by Ochrobactrum anthropi. Clin. Microbiol. Newsl. 2000;22:45–47. doi: 10.1016/S0196-4399(00)88662-6. [DOI] [Google Scholar]
- 90.Chertow G.M. Ochrobactrum anthropi bacteremia in a patient on hemodialysis. Am. J. Kidney Dis. 2000;35:e30-1. doi: 10.1016/S0272-6386(00)70069-2. [DOI] [PubMed] [Google Scholar]
- 91.Delière E., Vu-Thien H., Lévy V., Barquins S., Schlegel L., Bouvet A. Epidemiological investigation of Ochrobactrum anthropi strains isolated from a haematology unit. J. Hosp. Infect. 2000;44:173–178. doi: 10.1053/jhin.1999.0690. [DOI] [PubMed] [Google Scholar]
- 92.Esteban J., Ortiz A., Rollan E., Reyero-Lopez A., Soriano E. Peritonitis due to Ochrobactrum anthropi in a patient undergoing continuous ambulatory peritoneal dialysis. J. Infect. 2000;40:205–206. doi: 10.1016/S0163-4453(00)80023-7. [DOI] [PubMed] [Google Scholar]
- 93.Peltroche-Llacsahuanga H., Brandenburg V., Riehl J., Haase G. Ochrobactrum anthropi peritonitis in a CAPD patient. J. Infect. 2000;40:299–301. doi: 10.1053/jinf.2000.0648. [DOI] [PubMed] [Google Scholar]
- 94.Saeed Mahmood M., Sarwari A.R., Khan M.A., Sophie Z., Khan E., Sami S. Infective endocarditis and septic embolization with Ochrobactrum anthropi: Case report and review of literature. J. Infect. 2000;40:287–290. doi: 10.1053/jinf.2000.0644. [DOI] [PubMed] [Google Scholar]
- 95.El-Zimaity D., Harrison G.A.J., Keen A.P., Price S., Evans S.E., Lewis A.M., Thomas I., Bevan V., Djemal K. Ochrobactrum anthropi pseudobacteraemia. J. Infect. 2001;43:217–218. doi: 10.1053/jinf.2001.0896. [DOI] [PubMed] [Google Scholar]
- 96.Greven C.M., Nelson K.C. Chronic postoperative endophthalmitis secondary to Ochrobactrum anthropi. Retina. 2001;21:279–280. doi: 10.1097/00006982-200106000-00021. [DOI] [PubMed] [Google Scholar]
- 97.Daxboeck F., Zitta S., Assadian O., Krause R., Wenisch C., Kovarik J. Ochrobactrum anthropi bloodstream infection complicating hemodialysis. Am. J. Kidney Dis. 2002;40:e17.1–e17.4. doi: 10.1053/ajkd.2002.35759. [DOI] [PubMed] [Google Scholar]
- 98.Galanakis E., Bitsori M., Samonis G., Christidou A., Georgiladakis A., Sbyrakis S., Tselentis Y. Ochrobactrum anthropi bacteraemia in immunocompetent in children. Scand. J. Infect. Dis. 2002;34:800–803. doi: 10.1080/0036554021000026935. [DOI] [PubMed] [Google Scholar]
- 99.Stiakaki E., Galanakis E., Samonis G., Christidou A., Maraka S., Tselentis Y., Kalmanti M. Ochrobactrum anthropi bacteremia in pediatric oncology patients. Pediatr. Infect. Dis. J. 2002;21:72–74. doi: 10.1097/00006454-200201000-00018. [DOI] [PubMed] [Google Scholar]
- 100.Wheen L., Taylor S., Godfrey K. Vertebral osteomylitis due to Ochrobactrum anthropi. Intern. Med. J. 2002;32:426–428. doi: 10.1046/j.1445-5994.2002.00248.x. [DOI] [PubMed] [Google Scholar]
- 101.Gascón F., Zafra M., Castaño M., Valle M., Sánchez I. Neumonía extrahospitalaria con bacteriemia por Ochrobactrum anthropi en un niño inmunocompetente. Rev. Diagn. Biol. 2002;51:69–70. [Google Scholar]
- 102.Hill S. Ochrobactrum anthropi bacteraemia. Scand. J. Infect. Dis. 2003;35:913. doi: 10.1080/00365540310016574. [DOI] [PubMed] [Google Scholar]
- 103.Romero Gómez M.P., Peinado Esteban A.M., Sobrino Daza J.A., Sáez Nieto J.A., Alvarez D., Peña García P. Prosthetic mitral valve endocarditis due to Ochrobactrum anthropi: Case report. J. Clin. Microbiol. 2004;42:3371–3373. doi: 10.1128/JCM.42.7.3371-3373.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Oliver J.W., Stapenhorst D., Warraich I., Griswold J.A. Ochroboctrum anthropi and Delftia acidovorans to bacteremia in a patient with a gunshot wound. Infect. Dis. Clin. Pract. 2005;13:78–81. [Google Scholar]
- 105.Cho S.-S., Cheun J.-W., Jeun C.-B., Park S.-M., Sook-Jin Jang D.-S.M., Park Y.-J. A case of Ochrobactrum anthropi infection after using medicinal plants. Korean J. Clin. Lab. Sci. 2006;38:22–25. [Google Scholar]
- 106.Vaidya S.A., Citron D.M., Fine M.B., Murakami G., Goldstein E.J.C. Pelvic abscess due to Ochrobactrum anthropi in an immunocompetent host: Case report and review of the literature. J. Clin. Microbiol. 2006;44:1184–1186. doi: 10.1128/JCM.44.3.1184-1186.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Aly N.Y.A., Salmeen H.N., Joshi R.M. Ochrobactrum anthropi bacteremia in a child with inborn error of mitochondrial fatty acid oxidation. Med. Princ. Pract. 2007;16:463–465. doi: 10.1159/000107753. [DOI] [PubMed] [Google Scholar]
- 108.Labarca J.A., Garcia P., Balcells M.E., de la Cerda G., Salinas A.M., Román J.C., Guzmán A.M., Pérez C.M. Pseudo-outbreak of Ochrobactrum anthropi bacteremia related to cross-contamination from erythrocyte sedimentation tubes. Infect. Control Hosp. Epidemiol. 2007;28:763–765. doi: 10.1086/517979. [DOI] [PubMed] [Google Scholar]
- 109.Lee S.S., Yoo K.S., Cho J.H., Kim H.S., Kim T.S., Ha C.O., Kim J.S., Kang H.J. A case of Ochrobactrum anthropi bacteremia. Korean J. Nosocom. Infect. Control. 2007;12:65–68. [Google Scholar]
- 110.Song S., Ahn J.K., Lee G.H., Park Y.G. An epidemic of chronic pseudophakic endophthalmitis due to Ochrobactrum anthropi: Clinical findings and managements of nine consecutive cases. Ocul. Immunol. Inflamm. 2007;15:429–434. doi: 10.1080/09273940701798546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yu M.W., Sohn K.M., Rhee J.Y., Won S.O., Kyong R.P., Nam Y.L., Song J.H. Spontaneous bacterial peritonitis due to Ochrobactrum anthropi: A case report. J. Korean Med. Sci. 2007;22:377–379. doi: 10.3346/jkms.2007.22.2.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Arora U., Kaur S., Devi P. Ochrobactrum anthropi septicaemia. Indian J. Med. Microbiol. 2008;26:81–83. doi: 10.4103/0255-0857.38868. [DOI] [PubMed] [Google Scholar]
- 113.Battaglia T.C. Ochrobactrum anthropi septic arthritis of the acromioclavicular joint in an immunocompetent 17 year old. Orthopedics. 2008;31:1–3. doi: 10.3928/01477447-20080601-02. [DOI] [PubMed] [Google Scholar]
- 114.Javaid M.M., Rumjon A., Cubbon M. Ochrobactrum anthropi bacteremia in a non-diabetic, immunocompetent hemodialysis patient. Dial. Transplant. 2008;37:452–453. doi: 10.1002/dat.20277. [DOI] [Google Scholar]
- 115.Menuet M., Bittar F., Stremler N., Dubus J.C., Sarles J., Raoult D., Rolain J.M. First isolation of two colistin-resistant emerging pathogens, Brevundimonas diminuta and Ochrobactrum anthropi, in a woman with cystic fibrosis: A case report. J. Med. Case Rep. 2008;2:373. doi: 10.1186/1752-1947-2-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chiang C.C., Tsai Y.Y., Lin J.M., Chen W.L. Chronic endophthalmitis after cataract surgery secondary to Ochrobactrum anthropi. Eye. 2009;23:1237–1238. doi: 10.1038/eye.2008.137. [DOI] [PubMed] [Google Scholar]
- 117.Duran R., Vatansever Ü., Acunaş B., Başaran Ü.N. Ochrobactrum anthropi bacteremia in a preterm infant with meconium peritonitis. Int. J. Infect. Dis. 2009;13:e61–e63. doi: 10.1016/j.ijid.2008.06.027. [DOI] [PubMed] [Google Scholar]
- 118.Kim G., Jin S., Yoo J., Kim C., Choi J., Kim J., Song Y. A Case of Meropenem-Resistant Ochrobactrum anthropi Bacteremia. Infect. Chemother. 2009;41:62–64. doi: 10.3947/ic.2009.41.1.62. [DOI] [Google Scholar]
- 119.Ospina S., Muñoz S.A., Zapata J. Bacteriemia por Ochrobactrum anthropi en paciente con obstrucción de la vía biliar. Infectio. 2009;13:293–295. doi: 10.1016/S0123-9392(09)70160-2. [DOI] [Google Scholar]
- 120.Rihova Z., Mascart G., Dratwa M. Ochrobactrum anthropi peritonitis in an Immunocompetent CAPD Patient. Perit. Dial. Int. 2009;29:675–676. doi: 10.1177/089686080902900616. [DOI] [PubMed] [Google Scholar]
- 121.Adeyemi A.I., Sulaiman A.A., Solomon B.B., Chinedu O.A., Victor I.A. Bacterial bloodstream infections in HIV-infected adults attending a lagos teaching hospital. J. Health Popul. Nutr. 2010;28:318–326. doi: 10.3329/jhpn.v28i4.6037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Quintela Obregón E., Palomar Fontanet R., Salas C., Rodrigo Calabia E., Arias Rodríguez M. Ochrobactrum anthropi y peritonitis polimicrobiana en diálisis peritoneal: Un predictor de resistencia. Nefrologia. 2010;30:591–592. doi: 10.3265/Nefrologia.pre2010.Jun.10376. [DOI] [PubMed] [Google Scholar]
- 123.Saveli C.C., Levi M., Koeppe J. Ochrobactrum anthropi septic arthritis: Case report and implications in orthopedic infections. Infect. Dis. Rep. 2010;2:5–6. doi: 10.4081/idr.2010.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Sepe V., Esposito P., Sacco L., Ceci A., Magrassi A., Negri M.T., Libetta C., Canton A.D. Peritonitis in type 2 diabetes mellitus due to Ochrobactrum anthropi complicating automated peritoneal dialysis. Acta Diabetol. 2010;47:341–344. doi: 10.1007/s00592-010-0204-6. [DOI] [PubMed] [Google Scholar]
- 125.Starr N. Pseudo-outbreak of Ochrobactrum anthropi in post-operative tissue: Cultures. Am. J. Infect. Control. 2010;38:e139–e140. [Google Scholar]
- 126.Wi Y.M., Peck K.R. Biliary sepsis caused by Ochrobactrum anthropi. Jpn. J. Infect. Dis. 2010;63:444–446. [PubMed] [Google Scholar]
- 127.Woo Nho K., Chae J.D., Sung S.-A.S. Case report: A case of continuous ambulatory peritoneal dialysis related peritonitis caused by Ochrobactrum anthropi. Kidney Res. Clin. Pract. 2010;29:839–841. [Google Scholar]
- 128.Yagüe-Muñoz A., Gregori-Roig P., Valls-López S., Pantoja-Martínez J. Bacteriemia por Ochrobactrum anthropi en un niño con fibrosis quística. Enferm. Infecc. Microbiol. Clin. 2010;28:137–138. doi: 10.1016/j.eimc.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 129.Nicolás Obando M., Marta Badilla S. Bacteriemia por Ochrobactrum anthropi en paciente en hemodiálisis por catéter tunelizado permanente. Caso clínico. Rev. Med. Chil. 2011;139:1344–1346. doi: 10.4067/S0034-98872011001000015. [DOI] [PubMed] [Google Scholar]
- 130.Shivaprakasha S., Rajdev S., Singh H., Velivala S. Prosthetic aortic valve endocarditis due to Ochrobactrum anthropi. Indian J. Med. Sci. 2011;65:69–72. doi: 10.4103/0019-5359.103968. [DOI] [PubMed] [Google Scholar]
- 131.Chan C.C., Holland E.J. Infectious endophthalmitis after boston type 1 keratoprosthesis implantation. Cornea. 2012;31:346–349. doi: 10.1097/ICO.0b013e31821eea2f. [DOI] [PubMed] [Google Scholar]
- 132.Shrishrimal K. Recurrent Ochrobactrum anthropi and Shewanella putrefaciens bloodstream infection complicating hemodialysis. Hemodial. Int. 2012;16:113–115. doi: 10.1111/j.1542-4758.2011.00586.x. [DOI] [PubMed] [Google Scholar]
- 133.Alparslan C., Yavascan O., Kose E., Sanlioglu P., Aksu N. An opportunistic pathogen in a peritoneal dialysis patient: Ochrobactrum anthropi. Indian J. Pediatr. 2013;80:72–74. doi: 10.1007/s12098-012-0800-2. [DOI] [PubMed] [Google Scholar]
- 134.Chiu L.Q., Wang W. A case of unusual Gram-negative bacilli septic arthritis in an immunocompetent patient. Singap. Med. J. 2013;54:e164–e168. doi: 10.11622/smedj.2013162. [DOI] [PubMed] [Google Scholar]
- 135.Kumar S., Kapoor S., Chadha S., Saigal S.R. Ochrobactrum anthropi septicemia and pneumonia in a preterm, small for gestational age infant with multiple congenital anomalies. Indian J. Pathol. Microbiol. 2013;56:317–318. doi: 10.4103/0377-4929.120411. [DOI] [PubMed] [Google Scholar]
- 136.Mattos F.B., Saraiva F.P., Angotti-Neto H., Passos A.F. Outbreak of Ochrobactrum anthropi endophthalmitis following cataract surgery. J. Hosp. Infect. 2013;83:337–340. doi: 10.1016/j.jhin.2012.11.027. [DOI] [PubMed] [Google Scholar]
- 137.Mudshingkar S., Choure A., Palewar M., Dohe V., Kagal A. Ochrobactrum anthropi: An unusual pathogen: Are we missing them? Indian J. Med. Microbiol. 2013;31:306–308. doi: 10.4103/0255-0857.115664. [DOI] [PubMed] [Google Scholar]
- 138.Naik C., Kulkarni H., Darabi A., Bhanot N. Ochrobactrum anthropi: A rare cause of pneumonia. J. Infect. Chemother. 2013;19:162–165. doi: 10.1007/s10156-012-0436-1. [DOI] [PubMed] [Google Scholar]
- 139.Siti Rohani A.H., Tzar M.N. Ochrobactrum anthropi catheter-related bloodstream infection: The first case report in Malaysia. Med. J. Malays. 2013;68:267–268. [PubMed] [Google Scholar]
- 140.Al-naami A.Q., Ali Khan L., Ali Athlawy Y., Sun Z. Ochrobactrum anthropi induced retropharyngeal abscess with mediastinal extension complicating airway obstruction: A case report. J. Med. Radiat. Sci. 2014;61:126–129. doi: 10.1002/jmrs.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hernández-Torres A., Ruiz Gomez J., García-Vázquez E., Gómez-Gómez J. Ochrobactrum anthropi bacteraemia: Report of six cases and review of the literature. Intern. Med. Open Access. 2014;4:134. [Google Scholar]
- 142.Khan I.D., Mukherjee T., Gupta S., Haleem S., Sahni A.K., Banerjee S., Konar J. Ochrobactrum anthropi sepsis in intensive tertiary care. J. Basic Clin. Med. 2014;3:18–20. [Google Scholar]
- 143.Menezes F.G., Abreu M.G.B., Kawagoe J.Y., Warth A.N., Deutsch A.D., Dornaus M.F.P.S., Martino M.D.V., Correa L. Ochrobactrum anthropi bacteremia in a preterm infant with cystic fibrosis. Braz. J. Microbiol. 2014;45:559–561. doi: 10.1590/S1517-83822014005000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Mrozek S., Dupuy M., Hoarau L., Lourtet J., Martin-Blondel G., Geeraerts T. Brain empyema due to Ochrobactrum anthropi. Med. Mal. Infect. 2014;44:128–129. doi: 10.1016/j.medmal.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 145.Qasimyar H., Hoffman M.A., Simonsen K.A. Late-onset Ochrobactrum anthropi sepsis in a preterm neonate with congenital urinary tract abnormalities. J. Perinatol. 2014;34:489–491. doi: 10.1038/jp.2014.31. [DOI] [PubMed] [Google Scholar]
- 146.Wu X., Zhu W., Fu Z.Y., Ai Q., Yang L.X. A case report of a neck abscess caused by Ochrobactrum anthropi in a previously healthy person. Rev. Med. Microbiol. 2014;25:77–79. doi: 10.1097/MRM.0000000000000007. [DOI] [Google Scholar]
- 147.Cenkçi K., Kamit Can F., Can E., Yılmaz Hancı S., Anıl A.B., Anıl M. Ochrobactrum anthropi bacteremia and pneumonia in a previously healthy child. Turkish J. Pediatr. Emerg. Intensive Care Med. 2015;2:137–140. doi: 10.5505/cayb.2015.24633. [DOI] [Google Scholar]
- 148.Hindilerden F., Ozcelik T., Koculu S., Goksoy H.S., Guvenc S., Diz Kucukkaya R. Ochrobactrum anthropi bacteraemia after allogeneic stem cell transplantation: Report of a newly emerging pathogen. Bone Marrow Transplant. 2015;50:S554–S632. [Google Scholar]
- 149.Patra N., Raju R., Prakash M.R., Mustare V.K. Septicaemia due to Ochrobactrum anthropi in a patient with Guillain Barre Syndrome. JMS J. Med. Soc. 2015;29:182–184. [Google Scholar]
- 150.Ashraf F. A case of Ochrobactrum anthropi-induced septic shock and infective endocarditis. Rhode Isl. Med. J. 2016;99:27–28. [PubMed] [Google Scholar]
- 151.Haviari S., Cassier P., Dananché C., Hulin M., Dauwalder O., Rouvière O., Bertrand X., Perraud M., Bénet T., Vanhems P. Outbreak of Achromobacter xylosoxidans and Ochrobactrum anthropi infections after prostate biopsies, France, 2014. Emerg. Infect. Dis. 2016;22:1412–1419. doi: 10.3201/eid2208.151423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Jimenez G., Antony S. Ochrobactrum anthropi—An unusual cause of line related sepsis. Current knowledge of the epidemiology and clinical features of this pathogen. Br. J. Med. Med. Res. 2016;18:1–7. doi: 10.9734/BJMMR/2016/29365. [DOI] [Google Scholar]
- 153.Kanjee R., Koreishi A.F., Tanna A.P., Goldstein D.A. Chronic postoperative endophthalmitis after cataract surgery secondary to vancomycin-resistant Ochrobactrum anthropi: Case report and literature review. J. Ophthalmic Inflamm. Infect. 2016;6:1–5. doi: 10.1186/s12348-016-0094-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Venkateswaran N., Wozniak R.A.F., Hindman H.B. Ochrobactrum anthropi keratitis with Focal Descemet’s Membrane Detachment and Intracorneal Hypopyon. Case Rep. Ophthalmol. Med. 2016;2016:1–4. doi: 10.1155/2016/4502105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Gigi R., Flusser G., Kadar A., Salai M., Elias S. Ochrobactrum anthropi-caused osteomyelitis in the foot mimicking a bone tumor: Case report and review of the literature. J. Foot Ankle Surg. 2017;56:851–853. doi: 10.1053/j.jfas.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 156.Khasawneh W., Yusef D. Ochrobactrum anthropi fulminant early-onset neonatal sepsis, A case report and review of literature. Pediatr. Infect. Dis. J. 2017;36:1167–1168. doi: 10.1097/INF.0000000000001660. [DOI] [PubMed] [Google Scholar]
- 157.Torres Aguilera E., Verde Moreno E., Muñoz P., Valerio M., Luño J. Nuevo microorganismo en la bacteriemia asociada a catéter? Nefrologia. 2017;37:98–100. doi: 10.1016/j.nefro.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 158.Cipolla L., Gañete M., Serra D., Sampere C., Santillan P., Dinerstein E., Sztokhamer D., Perez M., Prieto M., Togneri A. Identification and molecular epidemiology of a nosocomial outbreak of Ochrobactrum anthropi bacteriemia. First report in Argentina. Int. J. Infect. Dis. 2018;73:298. doi: 10.1016/j.ijid.2018.04.4094. [DOI] [Google Scholar]
- 159.Hafeez Z., Ohar J., Ahmad M.I., Zeeshan A., Sunkara P.R., Marupudi S., Usman S., Malik A. Ochrobactrum anthropi pneumonia: A rare cause of acute respiratory distress syndrome (ARDS) Am. J. Respir. Crit. Care Med. 2018;197:A5332. [Google Scholar]
- 160.Zhu M., Zhao X., Zhu Q., Zhang Z., Dai Y., Chen L., Liang Z. Clinical characteristics of patients with Ochrobactrum anthropi bloodstream infection in a Chinese tertiary-care hospital: A 7-year study. J. Infect. Public Health. 2018;11:873–877. doi: 10.1016/j.jiph.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 161.Caroleo B., Malandrino P., Liberto A., Condorelli D., Patanè F., Maiese A., Casella F., Geraci D., Ricci P., Di Mizio G. Catheter-related Bloodstream Infections: A root cause analysis in a series of simultaneous Ochrobactrum anthropi infections. Curr. Pharm. Biotechnol. 2019;20:609–614. doi: 10.2174/1389201020666190405182025. [DOI] [PubMed] [Google Scholar]
- 162.Grabowska-Markowska J., Pawłowska I., Ziółkowski G., Wójkowska-Mach J. Bacteraemia caused by Ochrobactrum anthropi—Unusual behavior. Wiad. Lek. 2019;72:489–492. doi: 10.36740/WLek201903131. [DOI] [PubMed] [Google Scholar]
- 163.Kang J.Y., Song J.H., Nam K.Y., Lee S.U., Lee S.J. Polymicrobial keratitis of Pseudomonas aeruginosa, Acinetobacter baumannii, and Ochrobactrum anthropi. J. Korean Ophthalmol. Soc. 2019;60:474–479. doi: 10.3341/jkos.2019.60.5.474. [DOI] [Google Scholar]
- 164.Roussotte M., Gerfaud-Valentin M., Perpoint T., Dauwalder O., Sève P. Ochrobactrum anthropi catheter-related infection associated with superior vena cava syndrome. Med. Mal. Infect. 2019;49:551–553. doi: 10.1016/j.medmal.2019.04.393. [DOI] [PubMed] [Google Scholar]
- 165.Arimuthu D.A., Seong Lim C.T. Ochrobactrum anthropi bacteremia with variable clinical course: Report of two cases. Malays. J. Med. Health Sci. 2020;16:339–341. [Google Scholar]
- 166.Bratschi C., Ly T., Weber A., Meuli-Simmen C., Conen A., Mauler F. Ochrobactrum anthropi Infection of the Hand. J. Hand Surg. Glob. Online. 2020 doi: 10.1016/j.jhsg.2020.08.006. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Ko H.M., Jo J.N., Baek H.G. Effective Identification of Ochrobactrum anthropi Isolated from Clinical Specimens. Korean J. Clin. Lab. Sci. 2020;52:221–228. doi: 10.15324/kjcls.2020.52.3.221. [DOI] [Google Scholar]
- 168.Higgins C.S. Characterization, cloning and sequence analysis of the inducible Ochrobactrum anthropi AmpC beta-lactamase. J. Antimicrob. Chemother. 2001;47:745–754. doi: 10.1093/jac/47.6.745. [DOI] [PubMed] [Google Scholar]
- 169.Shanthini T., Manohar P., Samna S., Srividya R., Bozdogan B., Rameshpathy M., Ramesh N. Emergence of plasmid-borne blaoxa-181 gene in Ochrobactrum intermedium: First report from India. Access Microbiol. 2019;1:e000024. doi: 10.1099/acmi.0.000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Sharma P., Killmaster L.F., Volkening J.D., Cardenas-Garcia S., Wajid A., Rehmani S.F., Basharat A., Miller P.J., Afonso C.L. Draft genome sequences of three Ochrobactrum spp. isolated from different avian hosts in Pakistan. Genome Announc. 2018;6:e00269-18. doi: 10.1128/genomeA.00269-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Apisarnthanarak A., Kiratisin P., Mundy L.M. Evaluation of Ochrobactrum intermedium bacteremia in a patient with bladder cancer. Diagn. Microbiol. Infect. Dis. 2005;53:153–155. doi: 10.1016/j.diagmicrobio.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 172.Dharne M.S., Misra S.P., Misra V., Dwivedi M., Patole M.S., Shouche Y.S. Isolation of urease-positive Ochrobactrum intermedium in the stomach of a non-ulcer dyspeptic patient from north India. J. Microbiol. Immunol. Infect. 2008;41:183–186. [PubMed] [Google Scholar]
- 173.Jacobs D.J., Grube T.J., Flynn H.W., Greven C.M., Pathengay A., Miller D., Sanke R.F., Thorman J. Intravitreal moxifloxacin in the management of Ochrobactrum intermedium endophthalmitis due to metallic intraocular foreign body. Clin. Ophthalmol. 2013;7:1727–1730. doi: 10.2147/OPTH.S44212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Borges L.S.B., Monteiro J., Miglioli L., Inoue F., Coelho F., Barbosa V., Cortez D., Vasconcelos E., Souza E., Abboud C. Identification of Ochrobactrum oryzae in Bloodstream Primary Infection in a Dialysis Patient: Can it be an Emerging Pathogen? J. Microbiol. Infect. Dis. 2016;6:128–131. doi: 10.5799/jmid.vi.328984. [DOI] [Google Scholar]
- 175.Hong D.J., Kim K.H., Kim J.O., Hong J.S., Jeong S.H., Lee K. First case report of human infection with Ochrobactrum tritici causing bacteremia and cholecystitis. Ann. Lab. Med. 2016;36:278–280. doi: 10.3343/alm.2016.36.3.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Bharucha T., Sharma D., Sharma H., Kandil H., Collier S. Ochrobactrum intermedium: An emerging opportunistic pathogen—Case of recurrent bacteraemia associated with infective endocarditis in a haemodialysis patient. New Microbes New Infect. 2017;15:14–15. doi: 10.1016/j.nmni.2016.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Cho H.W., Byun J.H., Kim D., Lee H., Yong D., Lee K.W. The first case of Ochrobactrum pseudogrignonense bacteremia in Korea. Ann. Lab. Med. 2020;40:331–333. doi: 10.3343/alm.2020.40.4.331. [DOI] [PMC free article] [PubMed] [Google Scholar]