Abstract
Lysophosphatidic acid receptor 1 (LPA1) contributes to brain injury following transient focal cerebral ischemia. However, the mechanism remains unclear. Here, we investigated whether nucleotide-binding oligomerization domain-like receptor family pyrin domain containing 3 (NLRP3) inflammasome activation might be an underlying mechanism involved in the pathogenesis of brain injury associated with LPA1 following ischemic challenge with transient middle cerebral artery occlusion (tMCAO). Suppressing LPA1 activity by its antagonist attenuated NLRP3 upregulation in the penumbra and ischemic core regions, particularly in ionized calcium-binding adapter molecule 1 (Iba1)-expressing cells like macrophages of mouse after tMCAO challenge. It also suppressed NLRP3 inflammasome activation, such as caspase-1 activation, interleukin 1β (IL-1β) maturation, and apoptosis-associated speck-like protein containing a caspase recruitment domain (ASC) speck formation, in a post-ischemic brain. The role of LPA1 in NLRP3 inflammasome activation was confirmed in vitro using lipopolysaccharide-primed bone marrow-derived macrophages, followed by LPA exposure. Suppressing LPA1 activity by either pharmacological antagonism or genetic knockdown attenuated NLRP3 upregulation, caspase-1 activation, IL-1β maturation, and IL-1β secretion in these cells. Furthermore, nuclear factor-κB (NF-κB), extracellular signal-regulated kinase 1/2 (ERK1/2), and p38 were found to be LPA1-dependent effector pathways in these cells. Collectively, results of the current study first demonstrate that LPA1 could contribute to ischemic brain injury by activating NLRP3 inflammasome with underlying effector mechanisms.
Keywords: LPA1, transient middle cerebral artery occlusion, NLRP3 inflammasome, bone marrow-derived macrophage, LPA, lipopolysaccharide
1. Introduction
Lysophosphatidic acid (LPA) is a bioactive lysophospholipid that possesses diverse physiological and pathological functions throughout the body by activating its specific six G protein-coupled receptors (LPA1–6) [1,2]. LPA receptors have been of considerable therapeutic interest for drug development to treat many diseases [2,3]. In particular, targeting LPA1 has become a promising strategy for drug development due to clinical trials for pulmonary fibrosis (ClinicalTrials.gov ID: NCT01766817) and psoriasis (ClinicalTrials.gov ID: NCT02763969). In case of cerebral ischemia that occurs by a sudden blockade of blood supply in the brain and causes severe brain damage, LPA1 has been identified as a pathogenic factor for brain injury after ischemic challenge. Suppressing LPA1 activity by either pharmacological antagonism or genetic deletion can reduce brain damage, such as brain infarction, functional neurological deficits, and pain [4,5,6]. In particular, administration of an LPA1 antagonist (AM095) immediately after reperfusion significantly reduced brain infarction and neurological deficit score in mice at 1 day and 3 days after transient middle cerebral artery occlusion (tMCAO) challenge [4], supporting that LPA1 could contribute to brain injuries after ischemic challenge. As an underlying pathogenesis, LPA1 can regulate immune responses in post-ischemic brain by upregulating proinflammatory cytokines and increasing numbers of cells expressing ionized calcium-binding adapter molecule 1 (Iba1), a marker for activated microglia or infiltrated macrophages [4]. However, how LPA1 can contribute to brain injuries following ischemic challenge remains unclear.
Nucleotide-binding oligomerization domain-like receptor family pyrin domain containing 3 (NLRP3) is a sensor for various pathogen- and host-derived factors [7]. Upon activation, it forms a complex called NLRP3 inflammasome, leading to the production of proinflammatory cytokines, interleukin 1β (IL-1β) and IL-18 [8,9]. NLRP3 inflammasome activation contributes to tissue injuries in various diseases throughout the body [10,11,12,13,14]. In cerebral ischemia, the importance of NLRP3 inflammasome activation as a pathogenic mediator has been suggested [15]. NLRP3 is upregulated and NLRP3 inflammasome is activated in post-ischemic brain [15]. A genetic deletion of NLRP3 can decrease brain damage in mice after ischemic challenge [15]. Its pharmacological suppression can ameliorate ischemic injury and neurovascular complications in cellular and animal models of cerebral ischemia [16,17]. Recently, it was suggested that LPA can regulate NLRP3 inflammasome activation in lipopolysaccharide (LPS)-primed bone marrow-derived macrophages (BMDMs) [18]. Considering increased amounts of LPA in human ischemic patients [19] and animal models of cerebral ischemia [5,20], LPA signaling may regulate NLRP3 inflammasome activation in injured brain following ischemic challenge. Moreover, LPA1 may be responsible for NLRP3 inflammasome activation.
To test such possible role of LPA1, the current study determined whether suppressing LPA1 activity by its specific antagonist could ameliorate NLRP3 upregulation in an injured brain of mouse with tMCAO challenge through biochemical and immunohistochemical analyses. We also determined whether it could suppress NLRP3 inflammasome activation by measuring caspase-1 activation and IL-1β maturation in a post-ischemic brain. Through the previously reported in vitro system using LPS-primed BMDMs, followed by an exposure to LPA [18], we confirmed the role of LPA1 in NLRP3 inflammasome activation. Furthermore, we determined which LPA1-dependent pathways were involved in NLRP3 inflammasome activation.
2. Results
2.1. Suppressing LPA1 Activity Attenuates NLRP3 Inflammasome Activation in an Injured Brain after tMCAO Challenge
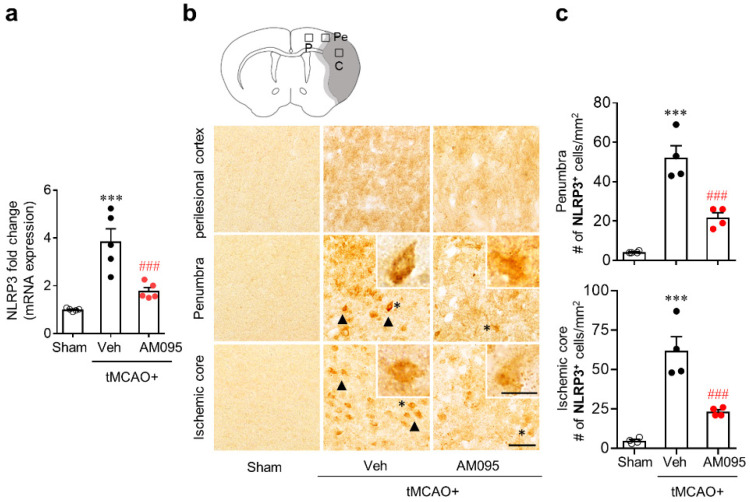
To address whether LPA1 could regulate NLRP3 expression in an injured brain after tMCAO challenge, we first determined mRNA expression levels of NLRP3 by qPCR analysis. Results showed that mRNA expression levels of NLRP3 were significantly increased in the brain at one day after tMCAO challenge compared to those in the sham group (Figure 1a). This upregulation of NLRP3 mRNA in the injured brain was markedly attenuated by AM095 administration immediately after tMCAO challenge (Figure 1a). We further determined whether LPA1 could influence protein expression levels of NLRP3 in an injured brain after tMCAO challenge by immunohistochemical analysis. The number of NLRP3-immunopositive cells was significantly increased after tMCAO challenge (Figure 1b,c). This increase was observed mainly in the penumbra and ischemic core regions, but not in perilesional cortex (Figure 1b,c). AM095 administration significantly reduced the number of NLRP3-immunopositive cells in both the penumbra and ischemic core regions (Figure 1b,c).
Figure 1.
Lysophosphatidic acid receptor 1 (LPA1) antagonist attenuates nucleotide-binding oligomerization domain-like receptor family pyrin domain containing 3 (NLRP3) upregulation in injured brains after transient middle cerebral artery occlusion (tMCAO) challenge. Mice were induced with tMCAO. AM095 (30 mg/kg, p.o.) was administered immediately after reperfusion. (a) mRNA expression levels of NLRP3 at one day after ischemic challenge by qPCR analysis. (b,c) NLRP3 expression determined by immunohistochemistry at one day after tMCAO challenge. (b) Representative images of NLRP3-immunopositive cells in perilesional cortex (P), penumbra (Pe), and ischemic core (C) regions. A graphical abstract image at the top shows cerebral areas where images in top, middle, and bottom planes are taken. Arrows indicate NLRP3-immunopostive cells. Cells in the insets are indicated as asterisks (*). (c) Quantification of NLRP3-immunopositive cells in penumbra and ischemic core regions. Scale bar, 50 µm (inset, 10 µm). n = 4 mice per group. *** p < 0.001 versus sham. ### p < 0.001 versus vehicle-administered tMCAO group. Neurological deficit scores of mice used for qPCR analysis and immunohistochemistry are presented as a supplementary figure (Figure S1a,b).
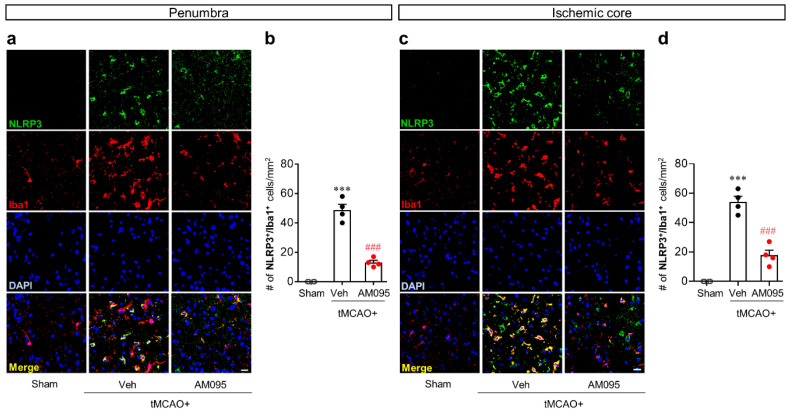
In a post-ischemic brain, NLRP3 upregulation can occur in Iba1-immunopositive cells [15]. Its attenuation by AM095 administration was clearly observed in the penumbra and ischemic core regions (Figure 1b,c). Therefore, we further determined whether the observed attenuation could occur in Iba1-expressing cells of the penumbra and ischemic core regions by NLRP3/Iba1 double immunofluorescence. The number of NLRP3/Iba1-double immunopositive cells was significantly increased in both the penumbra (Figure 2a,b) and ischemic core regions (Figure 2c,d) after tMCAO challenge. AM095 administration significantly reduced the number of NLRP3/Iba1-double immunopositive cells in both regions (Figure 2).
Figure 2.
LPA1 antagonist attenuates NLRP3 upregulation in ionized calcium-binding adapter molecule 1 (Iba1)-immunopostive cells of injured brains after tMCAO challenge. Mice were induced with tMCAO. AM095 (30 mg/kg) was administered immediately after reperfusion. NLRP3 expression in Iba1-immunopositive cells was determined in the penumbra and ischemic core regions at one day after tMCAO challenge by NLRP3/Iba1 double immunofluorescence. Representative image of NLRP3/Iba1-double immunopositive cells in the penumbra (a) and ischemic core regions (c) and quantification of their numbers (b,d) are shown. Scale bars, 20 µm. n = 4 mice per group. *** p < 0.001 versus sham. ### p < 0.001 versus vehicle-administered tMCAO group.
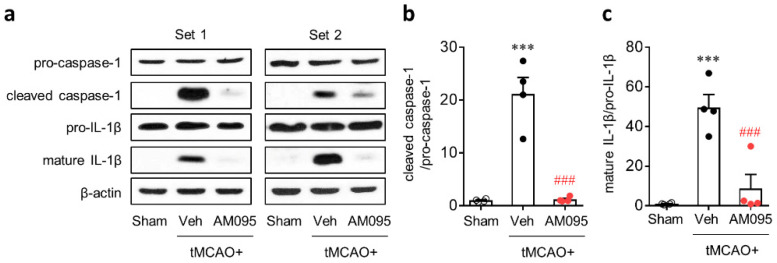
To address whether LPA1 could regulate NLRP3 inflammasome activation in an injured brain after tMCAO challenge, caspase-1 activation and IL-1β maturation were determined by Western blot analysis. Caspase-1 activation and IL-1β maturation were known to be important events for the activation of NLRP3 inflammasome [21,22,23]. Expression levels of cleaved caspase-1 and mature IL-1β were significantly increased in the injured brain at one day after tMCAO challenge compared to those in the sham group (Figure 3). AM095 administration immediately after reperfusion markedly attenuated caspase-1 activation and IL-1β maturation (Figure 3).
Figure 3.
LPA1 antagonist attenuates NLRP3 inflammasome activation in injured brains after tMCAO challenge. Mice were induced with tMCAO. AM095 (30 mg/kg) was administered immediately after reperfusion. Caspase-1 activation and interleukin 1β (IL-1β) maturation were determined by Western blot analysis at 1 day after tMCAO challenge. Representative Western blots of pro-caspase-1, cleaved caspase-1, pro-IL-1β, and mature IL-1β (a) and quantification of caspase-1 activation (b) and IL-1β maturation (c) are shown. n = 4 mice per group. *** p < 0.001 versus sham. ###, p < 0.001 versus vehicle-administered tMCAO group. Neurological deficit scores of mice used for Western blot analysis are presented as a supplementary figure (Figure S1c).
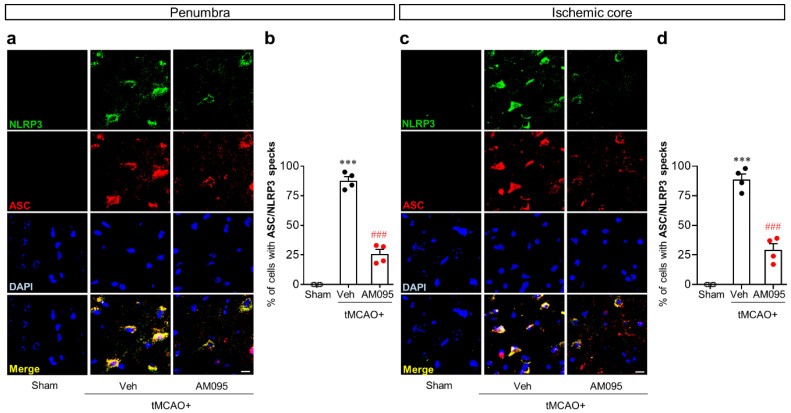
To further address the role of LPA1 in NLRP3 inflammasome activation in an injured brain after tMCAO challenge, the adaptor molecule apoptosis-associated speck-like protein containing a caspase recruitment domain (ASC) speck formation was determined by ASC/NLRP3 double immunofluorescence. The number of cells with ASC/NLRP3 specks was significantly increased in both the penumbra (Figure 4a,b) and ischemic core regions (Figure 4c,d) after tMCAO challenge. AM095 administration significantly reduced the number of cells with ASC/NLRP3 specks in both regions (Figure 4).
Figure 4.
LPA1 antagonist attenuates apoptosis-associated speck-like protein containing a caspase recruitment domain (ASC) speck formation in injured brains after tMCAO challenge. Mice were induced with tMCAO. AM095 (30 mg/kg) was administered immediately after reperfusion. ASC speck formation in NLRP3-immunopositive cells was determined in the penumbra and ischemic core regions at one day after tMCAO challenge by ASC/NLRP3 double immunofluorescence. Representative images of ASC/NLRP3 speck formation in the penumbra (a) and ischemic core regions (c) and quantification of their numbers in percentage (b,d) are shown. Scale bars, 10 µm. n = 4 mice per group. *** p < 0.001 versus sham. ###, p < 0.001 versus vehicle-administered tMCAO group.
2.2. LPA1 Contributes to NLRP3 Upregulation and NLRP3 Inflammasome Activation in LPS-Primed Macrophages Followed by LPA Exposure
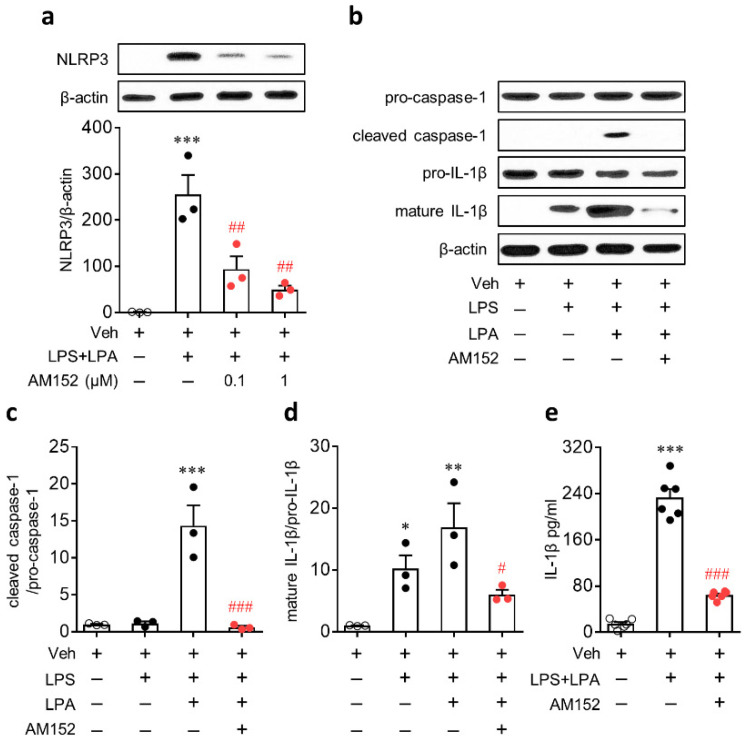
A previous study [15] and the current study (Figure 2) showed that NLRP3 was upregulated in cells expressing Iba1, a marker of infiltrated macrophages or activated microglia in post-ischemic brains [24,25]. These independent studies suggest that NLRP3 upregulation after ischemic challenge can occur in macrophages. Therefore, we studied the role of LPA1 in NLRP3 inflammasome activation in vitro using cultured BMDMs. To induce NLRP3 inflammasome activation, cells were primed with LPS and then exposed to LPA as previously reported [18] because ischemic challenge can increase amounts of LPA [5,20]. However, LPA itself cannot induce NLRP3 upregulation in BMDMs [18]. Instead, LPA was proven to enhance NLRP3 upregulation in LPS-primed BMDMs in a dose-dependent manner [18]. Therefore, we employed the same in vitro system of our previous study [18] to address the role of LPA1 in NLRP3 upregulation and NLRP3 inflammasome activation in macrophages. We first determined whether LPA1 could be involved in NLRP3 upregulation in macrophages. BMDMs were primed with LPS (500 ng/mL) for 4 h, followed by LPA exposure (1 µM) for 1 h. To determine the role of LPA1, cells were pretreated with AM152 (1 µM) for 30 min prior to LPS stimulation. As previously reported [18], NLRP3 was markedly upregulated in LPS-primed BMDMs, followed by LPA exposure (Figure 5a). However, AM152 significantly reduced expression levels of NLRP3 in LPS-primed BMDMs, followed by LPA exposure (Figure 5a).
Figure 5.
LPA1 antagonist attenuates LPA-induced NLRP3 inflammasome activation in lipopolysaccharide (LPS)-primed bone marrow-derived macrophages (BMDMs). Cells were primed with LPS (500 ng/mL) for 4 h, followed by an exposure to LPA (1 μM) for 1 h. (a–d) Protein expression levels of NLRP3, pro-caspase-1, cleaved caspase-1, pro-IL-1β, and mature IL-1β determined by Western blot analysis. (a) NLRP3 expression determined by Western blot analysis. AM152 was treated at different concentration (0; 0.1 and 1 μM). n = 3 per group. *** p < 0.001 versus control BMDMs (Veh). ##, p < 0.01 versus stimulated BMDMs (LPS-primed BMDMs, followed by an exposure to LPA; LPS+LPA). (b–d) Caspase-1 activation and IL-1β maturation determined by Western blot analysis. AM152 was treated at 1 μM. Representative Western blots of pro-caspase-1, cleaved caspase-1, pro-IL-1β, and mature IL-1β (b) and quantification of caspase-1 activation (c) and IL-1β maturation (d) are shown. n = 3 per group. * p < 0.05, ** p < 0.01, and *** p < 0.001 versus control BMDMs (Veh). # p < 0.05 and ### p < 0.001 versus stimulated BMDMs (LPS-primed BMDMs, followed by an exposure to LPA; LPS+LPA). (e) Amounts of secreted IL-1β into the culture medium were measured by enzyme-linked immunosorbent assay (ELISA) analysis. n = 6 per group. *** p < 0.001 versus control BMDMs (Veh). ### p < 0.001 versus stimulated BMDMs (LPS + LPA).
Next, we determined whether LPA1 could regulate LPA-mediated NLRP3 inflammasome activation in LPS-primed BMDMs by analyzing caspase-1 activation and IL-1β production. LPA induced the caspase-1 activation and IL-1β maturation in LPS-primed BMDMs (Figure 5b–d). LPS alone did not induce caspase-1 activation in BMDMs (Figure 5b,c). However, LPS alone induced IL-1β maturation in BMDMs, but to a lesser extent than that in LPS-primed BMDMs, followed by LPA exposure (Figure 5b,c). IL-1β secretion into the culture medium was also elevated in LPS-primed BMDMs, followed by LPA exposure (Figure 5e). AM152 treatment significantly attenuated caspase-1 activation, IL-1β maturation, and IL-1β secretion (Figure 5b–e).
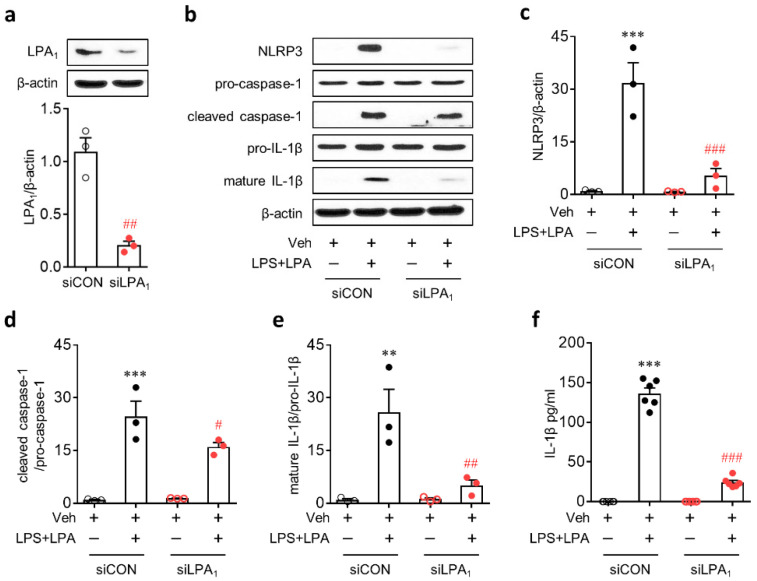
We confirmed the role of LPA1 in NLRP3 inflammasome activation by a genetic knockdown using a specific small interfering RNA (siRNA) for LPA1. LPA1 knockdown (Figure 6a) significantly attenuated NLRP3 upregulation in LPS-primed BMDMs, followed by LPA exposure (Figure 6b,c). It also significantly attenuated NLRP3 inflammasome activation in these cells as evidenced by attenuated caspase-1 activation (Figure 6b,d), IL-1β maturation (Figure 6b,e), and IL-1β secretion (Figure 6f).
Figure 6.
LPA1 knockdown attenuates LPA-induced NLRP3 inflammasome activation in LPS-primed BMDMs. Transfected BMDMs with non-target control small interfering RNA (siRNA) (siCON) or LPA1-specific siRNA (siLPA1) were primed with LPS (500 ng/mL) for 4 h, followed by an exposure to LPA (1 µM) for 1 h. (a) Knockdown efficiency of LPA1 siRNA determined by Western blot analysis. Representative Western blots of LPA1 and quantification. n = 3 per group. ##, p < 0.01 versus control siRNA (siCON)-transfected BMDMs. (b–e) Protein expression levels of NLRP3, pro-caspase-1, cleaved caspase-1, pro-IL-1β, and mature IL-1β determined by Western blot analysis. (b) Representative Western blots of NLRP3, pro-caspase-1, cleaved caspase-1, pro-IL-1β, and mature IL-1β. Quantification of NLRP3 upregulation (c), caspase-1 activation (d), and IL-1β maturation (e). n = 3 per group. ** p < 0.01 and *** p < 0.001 versus control BMDMs transfected with control siRNA (siCON + Veh). # p < 0.05, ## p < 0.01, and ### p < 0.001 versus stimulated BMDMs transfected with control siRNA (siCON + LPS + LPA). (f) Amounts of IL-1β secreted into the culture medium were measured by ELISA analysis. n = 6 per group. *** p < 0.001 versus control BMDMs transfected with control siRNA (siCON + Veh). ### p < 0.001 versus stimulated BMDMs transfected with control siRNA (siCON + LPS + LPA).
2.3. LPA1 Regulates NLRP3 Upregulation in LPS-Primed Macrophages Followed by LPA Exposure by Enhancing Nuclear Factor-κB (NF-κB) Translocation and Activating Extracellular Signal-Regulated Kinase 1/2 (ERK1/2) and p38 Mitogen-Activated Protein Kinase (MAPK)
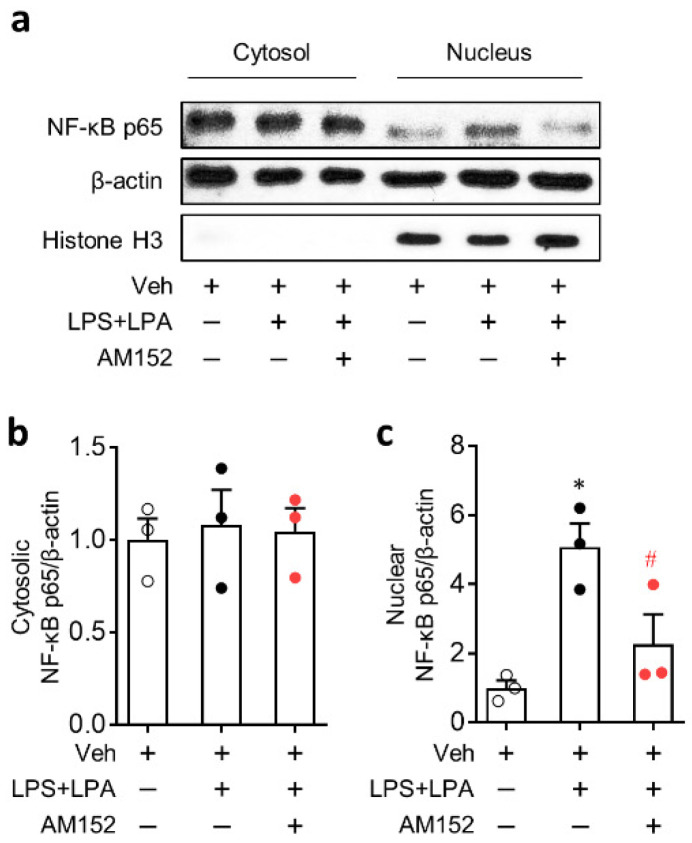
NF-κB pathway is known to play an important role in NLRP3 inflammasome as a priming signal to induce NLRP3 upregulation [26,27,28]. Therefore, the role of LPA1 in NF-κB activation was determined by analyzing NF-κB translocation from the cytosol into the nucleus. LPA caused a marked translocation of NF-κB into the nucleus in LPS-primed BMDMs without affecting expression levels of NF-κB in the cytosol (Figure 7). When LPA1 activity was suppressed by AM152, such marked translocation was significantly weakened (Figure 7). We further determined that LPA1 could regulate NF-κB phosphorylation in BMDMs by Western blot analysis. NF-κB was markedly phosphorylated in LPS-primed BMDMs, followed by LPA exposure (Figure S2). This phosphorylation seemed to be induced solely by LPS priming because LPS itself also induced NF-κB phosphorylation to the similar extent (Figure S2). AM152 did not attenuate NF-κB phosphorylation in both LPS-treated BMDMs and LPS-primed BMDMs, followed by LPA exposure (Figure S2). These data indicate that LPA1 may activate NF-κB pathway by enhancing NF-κB translocation rather than its phosphorylation in LPS-primed BMDMs, followed by LPA exposure.
Figure 7.
LPA1 antagonist inhibits LPA-induced nuclear factor-κB (NF-κB) activation in LPS-primed BMDMs. Cells were primed with LPS (500 ng/mL) for 4 h, followed by an exposure to LPA (1 μM) for 1 h. NF-κB activation was determined by comparing expression levels of cytosolic and nuclear NF-κB p65 based on Western blot analysis. Representative Western blots of cytosolic and nuclear NF-κB p65 (a) and quantification of NF-κB p65 translocation into the nucleus (b,c) are shown. n = 3 per group. * p < 0.05 versus control BMDMs (Veh). # p < 0.05 versus stimulated BMDMs (LPS + LPA).
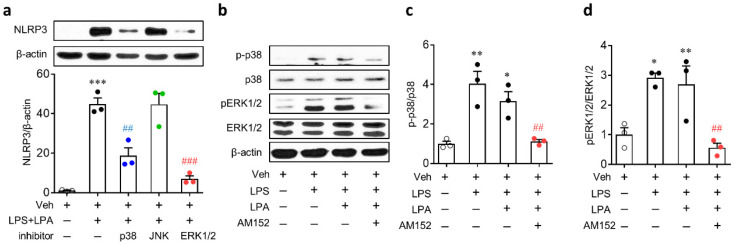
MAPK pathways, such as ERK1/2, p38, and c-Jun N-terminal kinase (JNK), are known to participate in NLRP3 inflammasome by upregulating NLRP3 [29,30,31]. These pathways are effector ones of LPA1 [32]. Therefore, the LPA/LPA1 signaling axis might regulate NLRP3 upregulation by activating MAPKs. To determine which MAPKs might be involved in NLRP3 upregulation in LPS-primed BMDMs, followed by LPA exposure, cells were treated with inhibitors of MAPKs, respectively, for 30 min prior to LPS priming. The upregulation of NLRP3 was significantly attenuated after inhibition of p38 and ERK1/2 but not after inhibition of JNK (Figure 8a). Whether ERK1/2 and p38 pathways could be regulated by LPA1 in LPS-primed BMDMs, followed by LPA exposure, was then determined. Both ERK1/2 and p38 were activated in LPS-primed BMDMs, followed by LPA exposure (Figure 8b–d). Similarly, they were also activated in cells treated with LPS alone (Figure 8b–d). However, AM152 significantly suppressed the activation of ERK1/2 and p38 in LPS-primed BMDMs, followed by LPA exposure (Figure 8b–d).
Figure 8.
Activation of extracellular signal-regulated kinase 1/2 (ERK1/2) and p38 mitogen-activated protein kinase (MAPK) is involved in LPA1-mediated NLRP3 upregulation in LPS-primed BMDMs, followed by LPA exposure. Cells were primed with LPS (500 ng/mL) for 4 h, followed by an exposure to LPA (1 µM) for 1 h. Protein expression levels of NLRP3 and phosphorylation of p38 and ERK1/2 were determined by Western blots. (a) Effects of MAPK inhibitors on NLRP3 upregulation in LPS-primed BMDMs based on Western blot analysis. Representative blots and quantification data are shown. Cells were treated with each inhibitor for 30 min prior to LPS priming. n = 3 per group. *** p < 0.001 versus control BMDMs (Veh). ## p < 0.01 and ### p < 0.001 versus stimulated BMDMs (LPS + LPA). (b-d) Effects of LPA1 antagonist on activation of p38 or ERK1/2 in LPS-primed BMDMs determined by Western blot analysis. Representative Western blots of phosphorylated p38 (p-p38), total p38 (p38), phosphorylated ERK1/2 (pERK1/2), total ERK1/2 (ERK1/2), and β-actin (b) and quantification of activation of p38 (c) and ERK1/2 (d) are shown. n = 3 per group. * p < 0.05 and ** p < 0.01 versus control BMDMs (Veh). ## p < 0.01 versus stimulated BMDMs (LPS + LPA).
3. Discussion
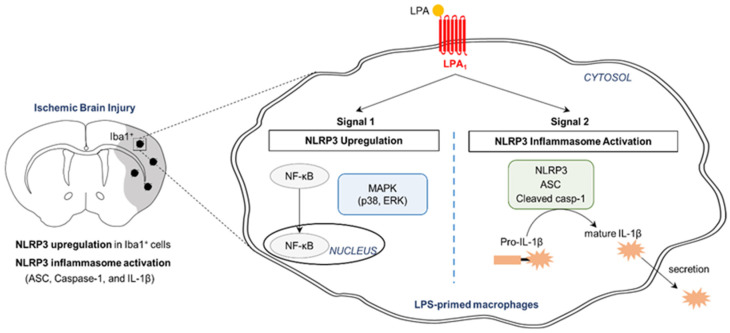
LPA1 is of great interest because it is being therapeutically pursued through ongoing clinical trials (Clinicaltrials.gov ID: NCT01766817; Clinicaltrials.gov ID: NCT02763969) for drug development to treat pulmonary fibrosis and psoriasis [33,34,35]. Other than these diseases, targeting LPA1 has been indicated to be beneficial for various diseases, including neuropathic pain and cerebral ischemia [4,6,36]. In particular, LPA1 antagonism can result in neuroprotection against an acute brain injury following transient ischemic challenge by modulating immune responses in the injured brain [4]. The current study addressed how LPA1 could contribute to an acute brain injury following ischemic challenge along with underlying molecular mechanisms (Figure 9). The pathogenic role of LPA1 in cerebral ischemia was associated with NLRP3 inflammasome activation, including NLRP3 upregulation, ASC speck formation, caspase-1 activation, and IL-1β maturation in a post-ischemic brain. This contribution of NLRP3 inflammasome activation to LPA1-dependent ischemic injury could be supported by the pathogenic role of NLRP3 inflammasome activation in a post-ischemic brain [37,38]. Either a genetic deficiency [37] or a pharmacological inhibition [38] might attenuate brain damages after ischemic challenge. As underlying molecular mechanisms, LPA1 signaling was found to be able to regulate NLRP3 inflammasome activation by activating NF-κB, ERK1/2, and p38 based on in vitro studies using cultured macrophages.
Figure 9.
Schematic diagram showing the mechanism of NLRP3 inflammasome activation by LPA1. In injured brains after tMCAO challenge, NLRP3 is upregulated in the penumbra and ischemic core regions, particularly in cells expressing Iba1 (a marker of macrophages). NLRP3 inflammasome activation including ASC speck formation, caspase-1 activation, and IL-1β maturation occurs in injured brains. LPA1 contributes to NLRP3 upregulation (Signal 1) and NLRP3 inflammasome activation (Signal 2) in injured brains. In cultured macrophages, LPA1 also regulates NLRP3 upregulation and NLRP3 inflammasome activation (caspase-1 activation, IL-1β maturation, and IL-1β secretion) in LPS-primed macrophages, followed by LPA exposure. As underlying mechanisms, LPA1 regulates translocation of NF-κB into the nucleus and activation of p38 and ERK1/2 in these stimulated macrophages. It has been reported that LPA1 can regulate such underlying mechanisms in injured brains after ischemic challenge [4].
NLRP3 inflammasome activation can be regulated by priming signal (signal 1) and activation signal (signal 2) in macrophages [39]. Signal 1 is responsible for the upregulation of NLRP3 and IL-1β via NF-κB activation. Signal 2 is responsible for an assembly of NLRP3 inflammasome complex and caspase-1-dependent IL-1β maturation. A variety of endogenous/exogenous molecules can regulate NLRP3 inflammasome activation [40,41]. Recently, it was demonstrated that LPA signaling can regulate NLRP3 inflammasome activation in primed macrophages [18]. LPA can induce both NLRP3 upregulation and NLRP3 inflammasome activation in LPS-primed BMDMs, but not in unprimed BMDMs [18]. Moreover, LPA5, one of LPA receptors, can regulate both NLRP3 upregulation and NLRP3 inflammasome activation in LPS-primed cells, followed by LPA exposure [18]. The current in vitro study provided evidence that LPA1 could also regulate these events in LPS-primed macrophages, followed by LPA exposure. Importantly, the pathogenic role of LPA1 signaling in cerebral ischemia [4] could be closely associated with NLRP3 inflammasome activation (the current study). LPA amounts are increased in plasma samples of ischemic stroke patients [19] and injured brains of animal models following ischemic challenge [20], indicating that LPA may contribute to ischemic brain injury. Indeed, exogenous LPA can increase cortical infarction in rats after tMCAO challenge [42]. Suppressing LPA production with an autotaxin inhibitor can reduce brain infarction and neural cell apoptosis in rats with the same challenge [20]. It is of note that LPA can induce NLRP3 inflammasome activation as shown in our previous study [18] and the current study. It is also of note that both LPA1 [5,6] and NLRP3 inflammasome activation [16,17,37,38] can contribute to an ischemic brain injury. More importantly, the current in vivo study demonstrated that suppressing LPA1 activity with its specific antagonist attenuated NLRP3 upregulation and NLRP3 inflammasome activation in an injured brain following tMCAO challenge. Therefore, NLRP3 inflammasome activation could be an underlying mechanism of LPA1-mediated brain damage following ischemic challenge. The current study also indicated that LPA1 could be a novel regulator of NLRP3 inflammasome activation.
NF-κB, ERK1/2, and p38 MAPK seemed to be involved in the LPA/LPA1 signaling axis-dependent activation of macrophage NLRP3 inflammasome activation. All these signaling pathways can influence NLRP3 inflammasome activation as players for the priming signal to induce NLRP3 upregulation [26,27,29,30,31]. They are also well-known as effector pathways after LPA1 activation [32]. Indeed, the current in vitro study clearly showed that suppressing LPA1 activity by AM152 treatment attenuated the activation of NF-κB, ERK1/2, and p38 in LPS-primed BMDMs following LPA exposure. Interestingly, LPA1 can regulate the activation of all these signaling molecules in a post-ischemic brain [4]. Suppressing LPA1 activity with AM095 administration can attenuate NF-κB activation in the ischemic core region following tMCAO-challenge [4]. It can also attenuate the activation of ERK1/2 and p38 in an injured brain after tMCAO challenge [4]. Considering the influence of LPA1 signaling on these three effectors in BMDMs in vitro (the current study) and in post-ischemic brains in vivo [4], the role of LPA1 in NLRP3 inflammasome activation in post-ischemic brain observed in the current study might also be regulated by NF-κB, ERK1/2, and p38 signaling pathways.
In the current study, we revealed that LPA1 could regulate neuroinflammatory responses in post-ischemic brains through upregulating NLRP3 expression and promoting NLRP3 inflammasome activation. Such roles of LPA1 were reaffirmed in LPS-primed macrophages, followed by LPA exposure. In fact, neuroinflammation is a key pathogenic event in post-ischemic brains [43,44], and targeting neuroinflammation could be an appealing strategy for developing therapeutics to treat cerebral ischemia [45,46]. In this view, targeting NLRP3 inflammasome activation with LPA1 antagonists could be of interest. However, the multiphasic roles of inflammatory cells, such as neuroprotective and neuroharmful roles, should be considered because the wrong treatment at the wrong time could lead to detrimental effects [47,48]. During the acute phase, inflammatory cells, such as brain resident microglia and infiltrated macrophages, are mainly involved in neuronal damage by accelerating inflammatory cascades through the profound release of proinflammatory cytokines (i.e., tumor necrosis factor-α (TNF-α), IL-1β, and interleukin 6 (IL-6)) [47]. In contrast, at the later stage, these cells are also responsible for ischemic recovery [47]. Therefore, anti-inflammatory treatments might be mostly effective during the acute phase of ischemic challenge. Our recent study revealed that suppressing LPA1 activity could efficiently attenuate inflammatory responses in post-ischemic brains [4]. AM095, an LPA1 antagonist, attenuated activation of microglia and astrocytes, their proliferation, microglial NF-κB activation, and production of proinflammatory cytokines, such as TNF-α, IL-6, and IL-1β, in injured brains during the acute phase after tMCAO challenge (at 1 or 3 days after the challenge) [4]. These findings suggest that targeting LPA1 can lead to significant anti-inflammatory responses during the acute phase after ischemic challenge possibly through suppressing glial activation. However, whether LPA1 can be involved in the ischemic recovery during the later phase after ischemic challenge remains unclear.
In conclusion, the current study demonstrates NLRP3 inflammasome activation is an underlying mechanism for LPA1-mediated brain injury following ischemic challenge with experimental evidence for possible signaling pathways in this event. Other than cerebral ischemia, both NLRP3 inflammation and LPA1 signaling have been independently suggested as promising targets to develop therapeutics in various diseases, including tissue fibrosis and psoriasis. In this context, findings of the current study might be applied to understand how LPA1 can contribute to tissue injuries in these diseases.
4. Materials and Methods
4.1. Animals
Male ICR mice (six weeks old) were purchased from Orient Bio (Seongnam-Si, Gyeonggi-do, Korea). All animal experiments were approved by Lee Gil Ya Cancer and Diabetes Institute (LCDI) at Gachon University (animal protocol approval No.: LCDI-2019-0027, 1 March 2019) and performed in accordance with the Institutional Animal Care and Use guidelines. Mice were housed under controlled conditions: 12 h/12 h light/dark cycle, temperature of 22 ± 2 °C, and humidity of 60 ± 10%. They had free access to food and water through the experiment.
4.2. Transient Focal Cerebral Ischemia Challenge and AM095 Administration
Transient focal cerebral ischemia in mice was induced by MCAO for 90 min and reperfusion (‘tMCAO’) as described previously [49]. Briefly, mice were anesthetized with isoflurane (3% for induction and 1.5% for maintenance) with an air mixture of oxygen:nitrous oxide at ratio of 30:70%. Vertical neck incision was made and the right common carotid artery (CCA) was carefully separated from the vagus nerve. The external carotid artery and internal carotid artery were then carefully separated and MCAO was induced by inserting a silicon coated 5-0 monofilament (9-mm-long) toward the MCA through the internal carotid artery from CCA bifurcation. Mice were allowed to recover and subjected to an examination of intra-ischemic scores [50,51] to confirm successful MCAO at 1 h after occlusion. Monofilament was withdrawn at 90 min after occlusion to restore the blood flow under an anesthetic condition. Body temperature was controlled at 37 °C during surgery. To mitigate the post-operative pain, 2% lidocaine cream was applied to the surgical sites. To replenish a fluid loss during the surgery, physiological saline (10 mL/kg, i.p.) was administered after the surgery. For the sham-operated group, animals underwent the same anesthetic and surgical procedures without MCAO.
AM095 was used as an LPA1 antagonist for in vivo experiments. After MCAO surgery, mice were randomly divided into a vehicle (1% dimethyl sulfoxide in 10% Tween-80)-administered group and an AM095-administered group. Vehicle or AM095 (30 mg/kg) was administered into mice by oral gavage using a stomach tube immediately after reperfusion. The dosage of AM095 was set based on previously reported in vivo studies, including ours [4,52,53,54]. The administration was done by an investigator blinded to treatment groups. In the current study, one mouse from a vehicle-administered group died before an experimental endpoint and this dead mouse was excluded from the study.
4.3. Determination of Functional Neurological Deficit Score
Functional neurological deficit score was analyzed at one day after tMCAO challenge in a ’blinded fashion using a modified neurological severity score (mNSS) grade to assess deficits of motor, sensory, reflex, and balance functions in mice as previously described [55]. The mNSS grade ranged from zero point for normal to 18 points for the maximal deficit. The determined neurological deficit score data for all mice that were used for qPCR analysis, histological assessment, and Western blot analysis are shown in Figure S1.
4.4. Quantitative Real-Time PCR (qPCR) Analysis
Total RNAs were isolated from ipsilateral brains at one day after ischemic challenge using RNAiso plus (Takara, Kusatsu, Japan). Total RNAs (1 µg) were used to synthesize cDNAs by reverse transcription using an All-in-One First-Strand cDNA Synthesis SuperMix (TransGen Biotech, Haidian, China). qPCR analysis was done using a StepOnePlusTM qPCR system (Applied Biosystems, Foster City, CA, USA) with Power SYBR Green PCR master mix (Life Technologies, Carlsbad, CA, USA). Expression levels of NLRP3 mRNA were calculated using the 2−ΔΔCT method. Mouse β-actin housekeeping gene was used as a reference. The following primers were used: β-actin forward, 5′-AGCCTTCCTTCTTGGGTATG-3′; β-actin reverse, 5′-CTTCTGCATCCTGTCAGCAA-3′; NLRP3 forward, 5′-TCG CCC AAG GAG GAA GAA GAA-3′; NLRP3 reverse, 5′-TGA GAA GAG ACC ACG GCA GAA-3′.
4.5. Immunohistochemistry for NLRP3 and Double Immunofluorescence for NLRP3/Iba1 or ASC/NLRP3
Brain samples for histological assessment were collected at one day after ischemic challenge. Mice were anesthetized with a mixture of Zoletil 50® (10 mg/kg, i.m., Virbac Laboratories, Carros, France) and Rompun® (3 mg/kg, i.m., Bayer HealthCare LLC, Shawnee Mission, KS, USA), perfused transcardially with ice-cold phosphate-buffered saline, and fixed with paraformaldehyde (PFA). Brains were removed, post-fixed with 4% PFA overnight, immersed in 30% sucrose solution, embedded in Tissue-Tek Optimal Cutting Temperature compound, and frozen on dry ice. These frozen brain samples were cut into 20-µm coronal sections using a cryostat (RD-2230, Roundfin, Liaoning, China).
For NLRP3 immunohistochemistry, brain sections were post-fixed in PFA, exposed to 0.01M sodium citrate at 90–100 °C and 1% H2O2, blocked with 1% fetal bovine serum (FBS), and incubated with a mouse anti-NLRP3 primary antibody (1:200, AdipoGen Life Sciences, San Diego, CA, USA) overnight at 4 °C, followed by labeling with a biotinylated secondary antibody (1:200, Santa Cruz Biotechnology, Dallas, TX, USA), for 2 h at room temperature (RT). These sections were further incubated with ABC reagent (1:100, Vector Laboratories, Burlingame, CA, USA). Signals were developed with a DAB kit (Dako, Santa Clara, CA, USA), rinsed with water, dehydrated with alcohol and xylene, and mounted with an Entellan media (Merck, Darmstadt, Germany).
For NLRP3/Iba1 double immunofluorescence, brain sections after blocking with 1% FBS were incubated with mouse anti-NLRP3 (1:100) and rabbit anti-Iba1 (1:500, Wako Pure Chemicals, Osaka, Japan) primary antibodies overnight at 4 °C. In case of ASC/NLRP3 double immunofluorescence, rabbit anti-ASC (1:200, AdipoGen Life Sciences) and mouse anti-NLRP3 (1:100) primary antibodies were used. Sections were then labeled with AF488- and Cy3-conjugated secondary antibodies (1:1000, Jackson ImmunoResearch West Grove, PA, USA) for 2 h at RT, followed by counterstaining with 4’,6-diamidino-2-phenylindole (DAPI) (Carl Roth, Karlsruhe, Germany). Labeled sections were mounted with VECTASHIELD® (Vector Laboratories).
Bright-field or fluorescence images were photographed with a microscope equipped with a DP72 camera (BX53T, Olympus, Tokyo, Japan) or with a confocal microscope (Eclipse A1 Plus, Nikon, Tokyo, Japan). All representative images were prepared using Adobe Photoshop Elements 8. For quantification, three different photos (600 µm × 600 µm) of each brain region were taken in a blind fashion. The number of immunopositive cells in each photo was manually counted and then converted to the number of immunopositive cells per unit area (mm2). The mean was used for the number of immunopositive cells for the region of a single mouse. In case of ASC/NLRP3 double immunofluorescence, the number of ASC/NLRP3-double immunopositive cells of each photo (200 µm × 200 µm) was manually counted and then used for calculating % of cells with ASC/NLRP3 specks versus total cells (DAPI-positive cells).
4.6. BMDMs Primary Culture, Treatment, and LPA1 Knockdown
Bone marrow cells isolated from leg bones of ICR mice (male, 8 weeks old, Orient Co. Ltd.) were differentiated into BMDMs for three days by incubation with minimum essential medium alpha (α-MEM) containing recombinant mouse macrophage colony stimulating factor (30 ng/mL, R&D systems, Minneapolis, MN, USA) as described previously [56]. For experiments, BMDMs (5 × 106 cells/well in a 6-well plate) were serum starved overnight by incubation with serum-free α-MEM. Cells were then primed with LPS (500 ng/mL, Sigma-Aldrich, St. Louis, MO, USA) for 4 h, followed by an exposure to LPA (1 µM, Avanti Polar Lipids, Birmingham, AL, USA) for 1 h. Fatty acid-free bovine serum albumin (0.1%, Sigma-Aldrich) was used as a vehicle.
To suppress LPA1 activity in vitro, BMDMs were serum starved overnight and treated with AM152 (another specific antagonist for LPA1) for 30 min. Cells were then primed with LPS and exposed to LPA. Alternatively, BMDMs were subjected to a transient transfection with LPA1 siRNA (Dharmacon, Lafayette, CO, USA) or control siRNA (Dharmacon) with Lipofectamine® RNAiMAX (Life Technologies) under a serum-free and antibiotics-free condition, as previously described [18]. For experiments, transfected cells were serum starved, primed with LPS, and exposed to LPA.
4.7. Western Blot Analysis
Proteins were extracted from either the ipsilateral brain hemisphere at one day after ischemic challenge or cultured BMDMs using a neuronal protein extraction reagent (Thermo Fisher Scientific, Waltham, MA, USA). Protein samples were separated by SDS-PAGE and transferred to polyvinylidene difluoride (PVDF) membranes (Merck Millipore, Burlington, MA, USA). These membranes were blocked with 5% skim milk, incubated overnight with primary antibodies against NLRP3 (1:1000), pro-caspase 1 (1:1000, Abcam, Cambridge, UK), cleaved caspase-1 (1:1000, AdipoGen Life Sciences), pro-IL-1β (1:1000, Cell Signaling Technology, Danvers, MA, USA), mature IL-1β (1:1000, Abcam), phospho-NF-κB p65 (1:1000, Cell Signaling Technology), and β-actin (1:10000, Bethyl Laboratories, Montgomery, TX, USA). They were then incubated with horseradish peroxidase (HRP)-conjugated secondary antibodies (1:10000, Santa Cruz Biotechnology). Protein bands were detected using an enhanced chemiluminescence detection kit (Donginbiotech Co., Seoul, South Korea). Expression levels of target protein bands were quantified using ImageJ software (National Institute of Mental Health, Bethesda, MD, USA).
4.8. Measurement of IL-1β in Conditioned Medium
Cell-free supernatants were collected from treated cells by centrifugation at 1500 rpm for 5 min. They were then concentrated using a VIVASPIN 500 (Sartorius, Goettingen, Germany). Protein levels of secreted IL-1β into the culture medium were determined using IL-1β enzyme-linked immunosorbent assay kits (R&D systems, Minneapolis, MN, USA), according to the manufacturer’s instructions.
4.9. Determination of NF-κB Translocation
Cytosolic and nuclear proteins were extracted from BMDMs using ProteoExtract® Subcellular Proteome Extraction Kit (Merck) according to the manufacturer’s instructions. Briefly, cells on a culture dish (60 mm2) were washed with Wash Buffer three times and incubated with ice-cold Extraction Buffer I containing protease inhibitor cocktail for 10 min at 4 °C under gentle agitation. Supernatant (fraction 1: cytosolic protein) was carefully removed and used for Western blot analysis. Extraction Buffer II containing protease inhibitor cocktail was added to the dish that was further incubated for 30 min at 4 °C under gentle agitation. Supernatant (fraction 2) that contain membrane/organelle protein was carefully removed. Finally, Extraction Buffer III containing protease inhibitor cocktail and Benzonase®Nuclease was added to the dish that was further incubated for 10 min at 4 °C under gentle agitation. Supernatant (fraction 3: nuclear protein) was carefully removed and used for Western blot analysis. Cytosolic and nuclear proteins were subjected to SDS-PAGE gel electrophoresis, transferred into PVDF membranes, and blocked. These membranes were incubated with primary antibodies against NF-κB p65 (1:1000, Cell Signaling Technology), β-actin (1:10000), and histone H3 (1:1000, Abcam) and incubated with HRP-conjugated secondary antibodies (1:10000).
4.10. Statistical Analysis
All data analyses were performed using GraphPad Prism 7 (GraphPad Software Inc., La Jolla, CA, USA). Date are presented as mean ± S.E.M. Statistical significance was analyzed by either Student′s t-test between two groups or one-way ANOVA, followed by a Newman–Keuls post hoc test, for comparisons among groups. Statistical significance was considered when p-value was less than 0.05.
Acknowledgments
We thank YJ Bae for providing assistance for qPCR analysis and BMDM culture.
Abbreviations
| ASC | Apoptosis-associated speck-like protein containing a caspase recruitment domain |
| BMDMs | Bone marrow-derived macrophages |
| CCA | Common carotid artery |
| DAPI | 4′,6-Diamidino-2-phenylindole |
| ELISA | Enzyme-linked immunosorbent assay |
| ERK1/2 | Extracellular signal-regulated kinase 1/2 |
| HRP | Horseradish peroxidase |
| Iba1 | Ionized calcium-binding adapter molecule 1 |
| IL-1β | Interleukin 1β |
| IL-6 | Interleukin 6 |
| JNK | c-Jun N-terminal kinase |
| LPA1 | Lysophosphatidic acid receptor 1 |
| LPS | Lipopolysaccharide |
| MAPK | Mitogen-activated protein kinase |
| α-MEM | Minimum Essential Medium alpha |
| mNSS | Modified neurological severity score |
| NF-κB | Nuclear factor-κB |
| NLRP3 | Nucleotide-binding oligomerization domain-like receptor family pyrin domain containing 3 |
| PFA | Paraformaldehyde |
| PVDF | Polyvinylidene difluoride |
| siRNA | Small interfering RNA |
| tMCAO | Transient middle cerebral artery occlusion |
| TNF-α | Tumor necrosis factor-α |
Supplementary Materials
The following are available online at https://www.mdpi.com/1422-0067/21/22/8595/s1, Figure S1: Administration of a lysophosphatidic acid receptor 1 (LPA1) antagonist, AM095, reduced neurological deficit score in mice after transient middle cerebral artery occlusion (tMCAO) challenge. Figure S2: AM152, an LPA1 antagonist, does not inhibit NF-κB phosphorylation in lipopolysaccharide (LPS)-primed BMDMs, followed by lysophosphatidic acid (LPA) exposure.
Author Contributions
Conceptualization, J.W.C.; Methodology, C.-H.L., A.S., B.P.G., and J.W.C.; Software, C.-H.L. and A.S.; Validation, C.-H.L., A.S., and B.P.G.; Formal analysis, C.-H.L., A.S., B.P.G., and J.W.C.; Investigation, C.-H.L., A.S., and B.P.G.; Resources, J.W.C.; Data curation, C.-H.L., A.S., B.P.G., and J.W.C.; Writing—original draft preparation, C.-H.L., A.S., and J.W.C.; Writing—Review & Editing: J.W.C.; Visualization, C.-H.L., A.S., and B.P.G.; Supervision, J.W.C.; Project administration, J.W.C.; Funding acquisition, J.W.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by grants (NRF-2020R1F1A1067154 and NRF-2020R1A6A1A03043708 to J.W.C.) of the National Research Foundation (NRF) of Korea.
Conflicts of Interest
The authors have no conflict of interest to disclose.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Choi J.W., Chun J. Lysophospholipids and their receptors in the central nervous system. Biochim. et Biophys. Acta. 2013;1831:20–32. doi: 10.1016/j.bbalip.2012.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yung Y.C., Stoddard N.C., Chun J. LPA receptor signaling: Pharmacology, physiology, and pathophysiology. J. Lipid Res. 2014;55:1192–1214. doi: 10.1194/jlr.R046458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stoddard N.C., Chun J. Promising Pharmacological Directions in the World of Lysophosphatidic Acid Signaling. Biomol. Ther. 2015;23:1–11. doi: 10.4062/biomolther.2014.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaire B.P., Sapkota A., Song M.-R., Choi J.W. Lysophosphatidic acid receptor 1 (LPA1) plays critical roles in microglial activation and brain damage after transient focal cerebral ischemia. J. Neuroinflammation. 2019;16:1–16. doi: 10.1186/s12974-019-1555-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ueda H., Neyama H., Sasaki K., Miyama C., Iwamoto R. Lysophosphatidic acid LPA1 and LPA3 receptors play roles in the maintenance of late tissue plasminogen activator-induced central poststroke pain in mice. Neurobiol. Pain. 2019;5:100020. doi: 10.1016/j.ynpai.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halder S., Yano R., Chun J., Ueda H. Involvement of LPA1 receptor signaling in cerebral ischemia-induced neuropathic pain. Neuroscience. 2013;235:10–15. doi: 10.1016/j.neuroscience.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Wen H., Miao E.A., Ting J.P.-Y. Mechanisms of NOD-like Receptor-Associated Inflammasome Activation. Immunity. 2013;39:432–441. doi: 10.1016/j.immuni.2013.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martinon F., Mayor A., Tschopp J. The Inflammasomes: Guardians of the Body. Annu. Rev. Immunol. 2009;27:229–265. doi: 10.1146/annurev.immunol.021908.132715. [DOI] [PubMed] [Google Scholar]
- 9.Yang Y., Wang H., Kouadir M., Song H., Shi F. Recent advances in the mechanisms of NLRP3 inflammasome activation and its inhibitors. Cell Death Dis. 2019;10:1–11. doi: 10.1038/s41419-019-1413-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wen H., Ting J.P.-Y., O’Neill L.A. A role for the NLRP3 inflammasome in metabolic diseases—did Warburg miss inflammation? Nat. Immunol. 2012;13:352–357. doi: 10.1038/ni.2228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Nardo D., De Nardo C.M., Latz E. New Insights into Mechanisms Controlling the NLRP3 Inflammasome and Its Role in Lung Disease. Am. J. Pathol. 2014;184:42–54. doi: 10.1016/j.ajpath.2013.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Szabo G., Csak T. Inflammasomes in liver diseases. J. Hepatol. 2012;57:642–654. doi: 10.1016/j.jhep.2012.03.035. [DOI] [PubMed] [Google Scholar]
- 13.Anders H.-J., Muruve D.A. The Inflammasomes in Kidney Disease. J. Am. Soc. Nephrol. 2011;22:1007–1018. doi: 10.1681/ASN.2010080798. [DOI] [PubMed] [Google Scholar]
- 14.Youm Y.-H., Grant R.W., McCabe L.R., Albarado D.C., Nguyen K.Y., Ravussin A., Pistell P., Newman S., Carter R., Laque A., et al. Canonical Nlrp3 Inflammasome Links Systemic Low-Grade Inflammation to Functional Decline in Aging. Cell Metab. 2013;18:519–532. doi: 10.1016/j.cmet.2013.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abulafia D.P., Vaccari J.P.D.R., Lozano J.D., Lotocki G., Keane R.W., Dietrich W.D. Inhibition of the Inflammasome Complex Reduces the Inflammatory Response after Thromboembolic Stroke in Mice. Br. J. Pharmacol. 2009;29:534–544. doi: 10.1038/jcbfm.2008.143. [DOI] [PubMed] [Google Scholar]
- 16.Ji J., Xiang P., Li T., Lan L., Xu X., Lu G., Ji H., Zhang Y., Li Y. NOSH-NBP, a Novel Nitric Oxide and Hydrogen Sulfide- Releasing Hybrid, Attenuates Ischemic Stroke-Induced Neuroinflammatory Injury by Modulating Microglia Polarization. Front. Cell. Neurosci. 2017;11:154. doi: 10.3389/fncel.2017.00154. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 17.Ye X., Shen T., Hu J., Zhang L., Zhang Y., Bao L., Cui C., Jin G., Zan K., Zhang Z., et al. Purinergic 2X7 receptor/NLRP3 pathway triggers neuronal apoptosis after ischemic stroke in the mouse. Exp. Neurol. 2017;292:46–55. doi: 10.1016/j.expneurol.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Gaire B.P., Lee C.-H., Kim W., Sapkota A., Lee D.Y., Choi J.W. Lysophosphatidic Acid Receptor 5 Contributes to Imiquimod-Induced Psoriasis-Like Lesions through NLRP3 Inflammasome Activation in Macrophages. Cells. 2020;9:1753. doi: 10.3390/cells9081753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Z.-G., Yu Z.-C., Wang D.-Z., Ju W.-P., Zhan X., Wu Q.-Z., Wu X.-J., Cong H.-M., Man H.-H. Influence of acetylsalicylate on plasma lysophosphatidic acid level in patients with ischemic cerebral vascular diseases. Neurol. Res. 2008;30:366–369. doi: 10.1179/174313208X300369. [DOI] [PubMed] [Google Scholar]
- 20.Wang C., Zhang J., Tang J., Li Y.-Y., Gu Y., Yu Y., Xiong J., Zhao X., Zhang Z., Li T.-T., et al. Lysophosphatidic acid induces neuronal cell death via activation of asparagine endopeptidase in cerebral ischemia-reperfusion injury. Exp. Neurol. 2018;306:1–9. doi: 10.1016/j.expneurol.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 21.He Y., Hara H., Núñez G. Mechanism and Regulation of NLRP3 Inflammasome Activation. Trends Biochem. Sci. 2016;41:1012–1021. doi: 10.1016/j.tibs.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schroder K., Sagulenko V., Zamoshnikova A., Richards A.A., Cridland J.A., Irvine K.M., Stacey K.J., Sweet M.J. Acute lipopolysaccharide priming boosts inflammasome activation independently of inflammasome sensor induction. Immunobiololgy. 2012;217:1325–1329. doi: 10.1016/j.imbio.2012.07.020. [DOI] [PubMed] [Google Scholar]
- 23.Juliana C., Fernandes-Alnemri T., Kang S., Farias A., Qin F., Alnemri E.S. Non-transcriptional Priming and Deubiquitination Regulate NLRP3 Inflammasome Activation. J. Biol. Chem. 2012;287:36617–36622. doi: 10.1074/jbc.M112.407130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ito D., Tanaka K., Suzuki S., Dembo T., Fukuuchi Y. Enhanced Expression of Iba1, Ionized Calcium-Binding Adapter Molecule 1, After Transient Focal Cerebral Ischemia in Rat Brain. Stroke. 2001;32:1208–1215. doi: 10.1161/01.STR.32.5.1208. [DOI] [PubMed] [Google Scholar]
- 25.Ahmed Z., Shaw G., Sharma V.P., Yang C., McGowan E., Dickson D.W. Actin-binding Proteins Coronin-1a and IBA-1 are Effective Microglial Markers for Immunohistochemistry. J. Histochem. Cytochem. 2007;55:687–700. doi: 10.1369/jhc.6A7156.2007. [DOI] [PubMed] [Google Scholar]
- 26.Duong B.H., Onizawa M., Oses-Prieto J.A., Advincula R., Burlingame A., Malynn B.A., Ma A. A20 restricts ubiquitination of pro-interleukin-1beta protein complexes and suppresses NLRP3 inflammasome activity. Immunity. 2015;42:55–67. doi: 10.1016/j.immuni.2014.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jiang L., Fei D., Gong R., Yang W., Yu W., Pan S., Zhao M. CORM-2 inhibits TXNIP/NLRP3 inflammasome pathway in LPS-induced acute lung injury. Inflamm. Res. 2016;65:905–915. doi: 10.1007/s00011-016-0973-7. [DOI] [PubMed] [Google Scholar]
- 28.Liu Z., Wang X., Wang Y., Zhao M. NLRP3 inflammasome activation regulated by NF-κB and DAPK contributed to paraquat-induced acute kidney injury. Immunol. Res. 2017;65:687–698. doi: 10.1007/s12026-017-8901-7. [DOI] [PubMed] [Google Scholar]
- 29.Campillo-Gimenez L., Renaudin F., Jalabert M., Gras P., Gosset M., Rey C., Sarda S., Collet C., Cohen-Solal M., Combes C., et al. Inflammatory Potential of Four Different Phases of Calcium Pyrophosphate Relies on NF-kappaB Activation and MAPK Pathways. Front. Immunol. 2018;9:2248. doi: 10.3389/fimmu.2018.02248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li D., Ren W., Jiang Z., Zhu L. Regulation of the NLRP3 inflammasome and macrophage pyroptosis by the p38 MAPK signaling pathway in a mouse model of acute lung injury. Mol. Med. Rep. 2018;18:4399–4409. doi: 10.3892/mmr.2018.9427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.An Y., Zhang H., Wang C., Jiao F., Xu H., Wang X., Luan W., Ma F., Ni L., Tang X., et al. Activation of ROS/MAPKs/NF-kappaB/NLRP3 and inhibition of efferocytosis in osteoclast-mediated diabetic osteoporosis. FASEB J. 2019;33:12515–12527. doi: 10.1096/fj.201802805RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang J., Li Y., Wang C., Wang Y., Zhang Y., Huang L., Zhang Z. Lysophosphatidic Acid Induces Apoptosis of PC12 Cells Through LPA1 Receptor/LPA2 Receptor/MAPK Signaling Pathway. Front. Mol. Neurosci. 2020;13:16. doi: 10.3389/fnmol.2020.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tager A.M., LaCamera P., Shea B.S., Campanella G.S., Selman M., Zhao Z., Polosukhin V., Wain J., Karimi-Shah B.A., Kim N.D., et al. The lysophosphatidic acid receptor LPA1 links pulmonary fibrosis to lung injury by mediating fibroblast recruitment and vascular leak. Nat. Med. 2008;14:45–54. doi: 10.1038/nm1685. [DOI] [PubMed] [Google Scholar]
- 34.Palmer S.M., Snyder L., Todd J.L., Soule B., Christian R., Anstrom K., Luo Y., Gagnon R., Rosen G. Randomized, Double-Blind, Placebo-Controlled, Phase 2 Trial of BMS-986020, a Lysophosphatidic Acid Receptor Antagonist for the Treatment of Idiopathic Pulmonary Fibrosis. Chest. 2018;154:1061–1069. doi: 10.1016/j.chest.2018.08.1058. [DOI] [PubMed] [Google Scholar]
- 35.Lei L., Su J., Chen J., Chen W., Chen X., Peng C. The role of lysophosphatidic acid in the physiology and pathology of the skin. Life Sci. 2019;220:194–200. doi: 10.1016/j.lfs.2018.12.040. [DOI] [PubMed] [Google Scholar]
- 36.Kihara Y., Mizuno H., Chun J. Lysophospholipid receptors in drug discovery. Exp. Cell Res. 2015;333:171–177. doi: 10.1016/j.yexcr.2014.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang F., Wang Z., Wei X., Han H., Meng X., Zhang Y., Shi W., Li F., Xin T., Pang Q., et al. NLRP3 Deficiency Ameliorates Neurovascular Damage in Experimental Ischemic Stroke. Br. J. Pharmacol. 2014;34:660–667. doi: 10.1038/jcbfm.2013.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ismael S., Zhao L., Nasoohi S., Ishrat T. Inhibition of the NLRP3-inflammasome as a potential approach for neuroprotection after stroke. Sci. Rep. 2018;8:1–9. doi: 10.1038/s41598-018-24350-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Benhadou F., Mintoff D., Del Marmol V. Psoriasis: Keratinocytes or Immune Cells—Which Is the Trigger? Dermatology. 2018;235:91–100. doi: 10.1159/000495291. [DOI] [PubMed] [Google Scholar]
- 40.Piazza G.A., Ritter J.L., Baracka C.A. Lysophosphatidic Acid Induction of Transforming Growth Factors α and β: Modulation of Proliferation and Differentiation in Cultured Human Keratinocytes and Mouse Skin. Exp. Cell Res. 1995;216:51–64. doi: 10.1006/excr.1995.1007. [DOI] [PubMed] [Google Scholar]
- 41.Casciano F., Pigatto P.D., Secchiero P., Gambari R., Reali E. T Cell Hierarchy in the Pathogenesis of Psoriasis and Associated Cardiovascular Comorbidities. Front. Immunol. 2018;9:1390. doi: 10.3389/fimmu.2018.01390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chi O.Z., Mellender S.J., Kiss G.K., Chiricolo A., Liu X., Patel N., Jacinto E., Weiss H.R. Lysophosphatidic acid increased infarct size in the early stage of cerebral ischemia-reperfusion with increased BBB permeability. J. Stroke Cerebrovasc. Dis. 2020;29 doi: 10.1016/j.jstrokecerebrovasdis.2020.105029. [DOI] [PubMed] [Google Scholar]
- 43.Jin R., Yang G., Li G. Inflammatory mechanisms in ischemic stroke: Role of inflammatory cells. J. Leukoc. Biol. 2010;87:779–789. doi: 10.1189/jlb.1109766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Levard D., Buendia I., Lanquetin A., Glavan M., Vivien D., Rubio M. Filling the gaps on stroke research: Focus on inflammation and immunity. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barone F., A Parsons A. Therapeutic potential of anti-inflammatory drugs in focal stroke. Expert Opin. Investig. Drugs. 2000;9:2281–2306. doi: 10.1517/13543784.9.10.2281. [DOI] [PubMed] [Google Scholar]
- 46.Tuttolomondo A., Di Sciacca R., Di Raimondo D., Renda C., Pinto A., Licata G. Inflammation as a Therapeutic Target in Acute Ischemic Stroke Treatment. Curr. Top. Med. Chem. 2009;9:1240–1260. doi: 10.2174/156802609789869619. [DOI] [PubMed] [Google Scholar]
- 47.Jayaraj R.L., Azimullah S., Beiram R., Jalal F.Y., Rosenberg G.A. Neuroinflammation: Friend and foe for ischemic stroke. J. Neuroinflammation. 2019;16:1–24. doi: 10.1186/s12974-019-1516-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sochocka M., Diniz B.S., Leszek J. Inflammatory Response in the CNS: Friend or Foe? Mol. Neurobiol. 2017;54:8071–8089. doi: 10.1007/s12035-016-0297-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sapkota A., Lee C.-H., Park S.J., Choi J.W. Lysophosphatidic Acid Receptor 5 Plays a Pathogenic Role in Brain Damage after Focal Cerebral Ischemia by Modulating Neuroinflammatory Responses. Cells. 2020;9:1446. doi: 10.3390/cells9061446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hunter A., Hatcher J., Virley D., Nelson P., Irving E., Hadingham S.J., A Parsons A. Functional assessments in mice and rats after focal stroke. Neuropharmacology. 2000;39:806–816. doi: 10.1016/S0028-3908(99)00262-2. [DOI] [PubMed] [Google Scholar]
- 51.Melani A., Pantoni L., Bordoni F., Gianfriddo M., Bianchi L., Vannucchi M.G., Bertorelli R., Monopoli A., Pedata F. The selective A2A receptor antagonist SCH 58261 reduces striatal transmitter outflow, turning behavior and ischemic brain damage induced by permanent focal ischemia in the rat. Brain Res. 2003;959:243–250. doi: 10.1016/S0006-8993(02)03753-8. [DOI] [PubMed] [Google Scholar]
- 52.Santos-Nogueira E., Francos-Quijorna I., Hernández J., Lago N., Astudillo A.M., Balsinde J., Estivill-Torrús G., De Fonseca F.R., Chun J., López-Vales R. Activation of Lysophosphatidic Acid Receptor Type 1 Contributes to Pathophysiology of Spinal Cord Injury. J. Neurosci. 2015;35:10224–10235. doi: 10.1523/JNEUROSCI.4703-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sakai N., Chun J., Duffield J.S., Wada T., Luster A.D., Tager A.M. LPA 1 -induced cytoskeleton reorganization drives fibrosis through CTGF-dependent fibroblast proliferation. FASEB J. 2013;27:1830–1846. doi: 10.1096/fj.12-219378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Castelino F.V., Seiders J., Bain G., Brooks S.F., King C.D., Swaney J.S., Lorrain D.S., Chun J., Luster A.D., Tager A.M. Amelioration of dermal fibrosis by genetic deletion or pharmacologic antagonism of lysophosphatidic acid receptor 1 in a mouse model of scleroderma. Arthritis Rheum. 2011;63:1405–1415. doi: 10.1002/art.30262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen J., Sanberg P.R., Li Y., Wang L., Lu M., Willing A.E., Sanchez-Ramos J., Chopp M. Intravenous Administration of Human Umbilical Cord Blood Reduces Behavioral Deficits After Stroke in Rats. Stroke. 2001;32:2682–2688. doi: 10.1161/hs1101.098367. [DOI] [PubMed] [Google Scholar]
- 56.Francke A., Herold J., Weinert S., Strasser R.H., Braun-Dullaeus R.C. Generation of Mature Murine Monocytes from Heterogeneous Bone Marrow and Description of Their Properties. J. Histochem. Cytochem. 2011;59:813–825. doi: 10.1369/0022155411416007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.