Abstract
This evidence-based consensus aims to establish the role of point-of-care lung ultrasound in the management of pneumonia and bronchiolitis in paediatric patients. A panel of thirteen experts form five Polish tertiary pediatric centres was involved in the development of this document. The literature search was done in PubMed database. Statements were established based on a review of full-text articles published in English up to December 2019. The development of this consensus was conducted according to the GRADE (Grading of Recommendations, Assessment, Development and Evaluations)—adopted and Delphi method. Initially, 22 proposed statements were debated over 3 rounds of on-line discussion and anonymous voting sessions. A total of 17 statements were agreed upon, including four statements referring to general issues, nine referring to pneumonia and four to bronchiolitis. For five statements experts did not achieve an agreement. The evidence supporting each statement was evaluated to assess the strength of each statement. Overall, eight statements were rated strong, five statements moderate, and four statements weak. For each statement, experts provided their comments based on the literature review and their own experience. This consensus is the first to establish the role of lung ultrasound in the diagnosis and management of pneumonia and bronchiolitis in children as an evidence-based method of imaging.
Keywords: paediatric pneumonia, bronchiolitis, point-of-care ultrasound, LUS
1. Introduction
Although the diagnosis of respiratory tract infections, including pneumonia and bronchiolitis, is based on clinical data, in some cases, performance of imaging modalities is necessary [1]. Chest X-ray (CXR) is the most commonly performed test. However, it has significant limitations such as patient exposure to ionising radiation, relatively low sensitivity in detecting pulmonary inflammatory lesions, low negative predictive value (NPV), and interpretation discrepancies among specialists [2]. In comparison, the diagnostic performance of chest computed tomography (chest CT) is much better, but as it exposes patients to a high radiation dose, the benefit–risk balance does not allow for its routine use in children [3]. The radiation exposure of CT could be avoided using MRI. Modern technology has enabled high-quality three-dimensional lung imaging with this tool, which proved especially promising for the detection of complicated pneumonia. However, it is still too expensive, and like CT may demand sedation or anesthesia in young, uncooperative children, demands long training and thus is not widely available even in tertiary centers [4].
Lung ultrasound (LUS) is an alternative tool unburdened with the above-mentioned limitations. Numerous advantages of LUS include continuous bedside availability, short performing time, no radiation risk, smaller dependence on a patient’s movements (including crying), relatively low costs, and an encouraging learning curve [5]. It can also be repeated multiple times if needed, and therefore can be used for treatment monitoring [6].
In emergency medicine, sonographers are equipped with standardised LUS protocols enabling rapid patient assessment [7,8]. For adult patients, both Polish recommendations on LUS application in internal medicine [9,10], and international evidence-based recommendations on the point of care lung ultrasound are followed. Few recommendations regarding the use of LUS in neonatal and paediatric diseases are outlined in the latter [11]. Nevertheless, the role of LUS in a paediatric population is not firmly established yet.
The purpose of this consensus is to define the position of point-of-care LUS in the management of pneumonia and bronchiolitis in children.
2. Materials and Methods
2.1. Expert Panel Selection
An expert panel of specialists from five different Polish tertiary paediatric centres was selected. Experts (paediatricians, peadiatric pulmonologists and radiologists) who had published articles regarding LUS in the past 10 years and/or have at least 4 years of experience in performing LUS, with at least 300 examinations per year, were chosen.
2.2. Literature Search
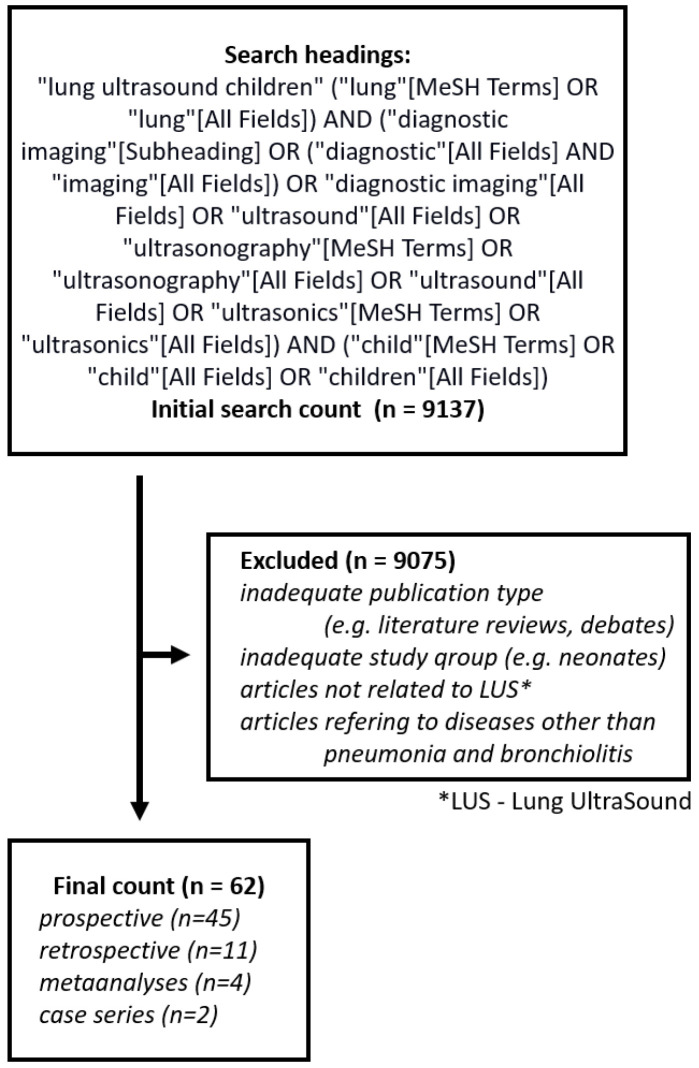
The literature search was conducted in PubMed database and included articles published prior to January 2020. The search included headings: “lung ultrasound children”. The literature search and review process is presented in Figure 1. The database containing all the publications was created using the free on-line program Zotero available at www.zotero.org. The articles limited to perinatal, neonatal, and adult patients were excluded except for articles which included both children and young adults (up to 21 years of age). For further evaluation, only English language full-text original papers were chosen including meta-analyses, case series, but not case reports. Since there is a very limited number of publications focusing on the use of LUS in children with pneumothorax, foreign body aspiration, cystic fibrosis, atelectasis, chest tumours, congenital abnormalities of the respiratory tract and undergoing cardiac surgery, the expert panel has decided to narrow the scope of the analysis to pneumonia and bronchiolitis.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram.
2.3. Statement Development
Experts submitted proposals for possible statements while paying special attention to the following: examination technique, diagnostic criteria for pneumonia and bronchiolitis, the role of LUS in the management of these diseases, comparison of LUS to other imaging methods, and finally, the role of LUS in the follow-up of the patients. Each statement was independently assessed in terms of the degree of agreement/disagreement between experts.
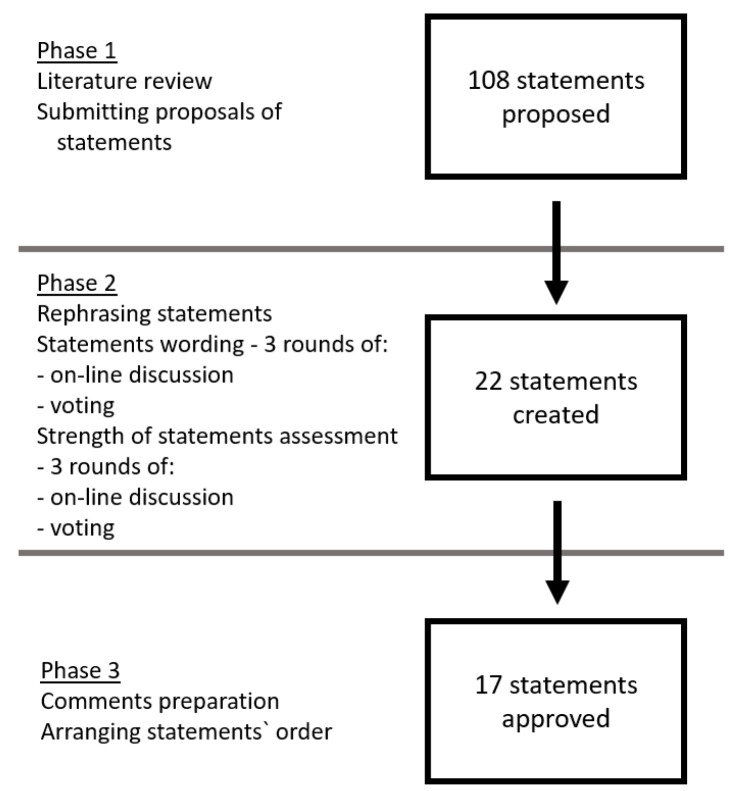
In compliance with Delphi method, the experts shared their opinions about the statements in 3 on-line discussion rounds, each round being followed by anonymous voting [12]. If a statement received ≥80% positive votes or >50% negative votes, the statement was approved and incorporated in the consensus. If the voting result was still indeterminate after third Delphi round, the statement was rejected (Table 1). The process of statements development and strength assessment is presented in Figure 2.
Table 1.
Degree of experts’ agreement, Delphi method.
| Experts’ Opinion | % Positive Votes |
|---|---|
| Agreed for—1 | ≥80% |
| Agreed against—2 | ≤50% |
| Indeterminate—rejected | 51–79% |
Figure 2.
The process of statements’ development and strength assessment.
2.4. Strength of Statements
The assessment of statements’ strength was based on the quality of evidence and parameters including sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood ratios, following GRADE-adopted methodology [13]. Quality of evidence was assessed following the Tool for Quality Assessment of Diagnostic Accuracy Studies, which included such variables as publication type, study group size and homogeneity, inclusion and exclusion criteria, a diagnostic method used as a reference and criteria for establishing the final diagnosis [14]. Similarly to statement development, the strength of evidence for each formulated statement was rated as either high (A), moderate (B), low or very low (C) (Table 2 and Table 3). The strength assessment group consisted of eight experts.
Table 2.
GRADE-adopted classification.
| Level of Evidence | Criteria for Quality of Evidence |
|---|---|
| A (high) |
Data come from many meta-analyses, and/or it is unlikely that further research will change the credibility of effectiveness or accuracy of the method. |
| B (moderate) |
Data come from individual large non-randomized trials (meta-analysis, prospective cohort study), and/or further testing may have a significant impact on the credibility of effectiveness or accuracy of the method. |
| C (low or very low) |
Agreed expert opinion and/or data from small studies, retrospective studies, registers, case series, or case reports, and/or it is very likely that further testing will have an important impact on the credibility of effectiveness or accuracy of the method. Very low in case any estimation of the effects or accuracy of the method is very uncertain. |
Table 3.
Strength of statements.
| Expert’s Opinion | Level of Evidence | Strength of Statement | Strength of Statement—Practical Implications |
|---|---|---|---|
| 1 | A | A1 | Strong statement; the given statement should be widely followed, as long as there are no major obstacles. |
| 1 | B | B1 | Strong statement, but with less degree of certainty; probably right in most individual cases. |
| 1 | C | C1 | The average (moderate) strength of statement; the statement may change after obtaining more reliable data; probably right. |
| 2 | A | A2 | The average (moderate) strength of statement; the decision on its adoption is a matter of choice and may depend on local and individual conditions; intervention does not have to be used. |
| 2 | B | B2 | Weak statement; alternative conduct can be just as good or better. |
| 2 | C | C2 | Weak statement; alternative conduct is probably equally acceptable. |
2.5. Comments
For each statement, the authors provided comments based not only on the literature review, but also on their own experience. Experts paid special attention to addressing practical issues regarding LUS performance. Basic definitions of LUS findings are presented in Table 4 [15].
Table 4.
Basic definitions of lung ultrasound (LUS) findings.
| LUS Finding | Definition |
|---|---|
| A-lines (A-line artefacts) |
Repetition of the pleural line at a standardized distance equal to the skin–pleural line distance. |
| B-lines (B-line artefacts) |
Comet-tail artefacts that arise from the pleural line and move simultaneously with the breathing cycle. The other optional 4 criteria are: screen-long, well-defined, erasing A-lines, and hyperechoic. |
| Consolidation | Hypoechoic, subpleural tissue-like area, caused by fluid displacing alveolar air. In case of a large consolidation, the appearance is characteristically liver-like. Usually, a consolidation has blurred margins and the following associated features:
|
| I-lines, Z-lines (I- and Z-line artefacts) |
Short vertical hyperechoic artefacts arising from the pleural line, not reaching the distal edge of the screen. |
| Interstitial syndrome | ≥3 B-lines visible in the longitudinal plane between two ribs. |
2.6. Statements
Experts’ shared opinion preceding statements: Interpretation of LUS should be performed within a clinical context [16,17,18,19,20,21,22,23,24,25,26,27,28].
3. General Statements
-
1.
A linear transducer is the most commonly used transducer for LUS examination of a suspected lower respiratory tract infection (LRTI) in children (A1) [29,30,31,32,33,34].
Comments:- a.
-
b.The appropriate transducer must balance acquiring the best possible image quality with the maintenance of adequate ultrasound wave penetration. The examining conditions may be affected by:
- Lesion size—in case of abnormalities involving a large area of the lung parenchyma (e.g., large consolidations) or massive pleural effusion, transducers with a wide field of view;
- Deeper penetration may prove necessary [33].
-
c.Differentiation between B-lines and other vertical artefacts (I- and Z-lines) may require the use of a convex or microconvex transducer.
-
2.
The entire available lung surface should be examined in children with suspected LRTI (A1) [31,35,42,43,44,45,46,47].
Comments:-
a.The recommended examination technique includes the assessment of the entire available lung surface, i.e., anterior, lateral and posterior surface of both lungs [6,16,19,23,25,28,34,42,43,44,45,48,49,50,51,52,53,54,55]. The examined area may be limited to anterior and lateral surfaces in the case of patients who are:
- Hospitalised in the intensive care unit due to the risk posed by changing their position;
- In life-threatening conditions, examined following quick-assessment protocols, such as EFAST, BLUE, PEA, RADIUS.
Should examining the entire available lung surface prove impossible (due to patients’ anxiety), such information must be included in the examination result.- b.
- c.
- d.
-
a.
-
3.
Diagnostic value of LUS in children with suspected LRTI to a limited extent depends on the sonographer’s experience (B1) [16,27,28,47,56,57].
Comments:- Sonographers, who are novices in diagnosing CAP, can acquire high concordance with experienced sonographers relatively quickly [56].
-
4.
LUS has high diagnostic value in assessing the presence of fluid in pleural cavities (A1) [16,18,24,26,32,35,36,38,40,44,48,60,63,64].
Comments:- In case of small-volume fluid detection with LUS, it is crucial to evaluate the fluid’s clinical significance.
- LUS enables visualization of small-volume pleural fluid directly adjacent to the area of consolidation.
- To standardise the model result of LUS in case of pleural effusion, we suggest including the following information: the patient’s position during the examination, the precise location (including the maximal height of the fluid, its maximal depth with determining the intercostal space and body line) as well as the characteristics of the fluid.
3.1. Pneumonia
-
5.
LUS is useful for diagnosing CAP in children (A1) [6,16,19,20,22,24,25,26,27,29,30,33,35,36,37,38,39,40,41,43,44,45,48,49,51,55,57,58,60,65,66,67,68].
-
6.
LUS has at least equal diagnostic value to CXR in detecting CAP in children (A1) [6,16,19,26,30,35,37,39,41,44,45,48,51,55,58,60].
Comments:- Some patients will benefit from having both CXR and LUS performed, as these two imaging methods should be regarded as complementary [40].
-
7.
Normal LUS results in children with suspected LRTI significantly reduce the probability of diagnosing CAP (A1) [16,24,25,26,33,41,49,51,55,60,67].
Comments:- Despite high sensitivity of LUS in diagnosing pneumonia, some lesions remain undetectable (false-negative result) if the lesion:
-
8.
Consolidation is the most commonly reported LUS finding in children with pneumonia (A1) [6,20,22,24,26,29,30,32,33,35,37,39,41,42,46,51,58,60,67,69].
Comments:- Should a consolidation be detected, it is crucial to measure it in at least two, optimally three, dimensions [67].
-
9.
LUS is more sensitive in detecting consolidations than CXR (A1) [16,28,33,39,44,48,49,51,58].
-
10.
Assessment of the vascular pattern of the consolidation may improve the diagnostic value of LUS in children with suspected LRTI (C1) [31,36,38].
Comments:- An abnormal vascular pattern may be indicative of other aetiology of the lesions (tuberucolous, fungal or non-infectious).
- Vascular pattern assessment may be hindered in cases of examining an anxious child, small consolidations or lesions located in the pericardiac area (due to cardiac pulse).
-
11.
LUS does not determine the aetiology of CAP in children (C1) [27,42].
Comments:- Like other imaging techniques, LUS cannot indicate the aetiologic factor. However, regarding pathophysiology and the whole clinical picture, LUS findings can be suggestive of certain groups of pathogens. Features suggestive of viral or atypical aetiology include bilateral consolidations, which are usually smaller compared to the ones observed in bacterial pneumonia, as well as more frequent presence of B-lines forming interstitial syndromes [16,27,58].
-
12.
LUS is useful in monitoring the course of pneumonia in children (B1) [6,37,38,42,51,67,70].
Comments:- In patients with pneumonia, LUS monitoring enables early detection of complications [38].
- It is worth performing an additional control LUS examination 1-2 months after the treatment has been completed. The knowledge of residual findings can facilitate correct interpretation of LUS, should the patient be suspected of a next episode of LRTI [21].
-
13.
LUS is useful in diagnosing complications of pneumonia in children (B1) [31,36,40,46,57].
Comments:- LUS accuracy of lung abscess detection depends mainly on localisation of the lesion.
- LUS seems to be useful in diagnosing pneumothorax in children, though it does not allow air volume assessment, and it cannot aid in the choice of the treatment method.
3.2. Bronchiolitis
Bronchiolitis is per se a clinical diagnosis and therefore there is no need for routine imaging evaluation [72,73]. However, in some patients, who are at risk of requiring intensive therapy, in whom complications or other diagnosis is being considered, imaging modalities may prove helpful. The statements below relate to the latter situation.
-
14.
LUS is useful in bronchiolitis diagnosis (B1) [23,52,53,54,63,64].
-
15.
LUS has a diagnostic value equal or greater than CXR in bronchiolitis diagnosis (C1) [23,63,64].
Comments:- We suggest LUS as the first-choice method in patients with bronchiolitis who require diagnostic imaging.
As LUS is a relatively new method and has certain limitations (as described above), in case of equivocal results, it may be reasonable to perform both—LUS and CXR. LUS is not only safer (no radiation risk), but also allows assessment of the severity of bronchiolitis, as mentioned below (statement 16, comments a, b and c).
-
16.
LUS is useful in assessing the severity of bronchiolitis (B1) [23,34,52,53,54,64].
Comments: -
17.
LUS is useful in monitoring patients with bronchiolitis (C1) [54,64].
The statements, grouped by their strength, are presented in Table 5.
Table 5.
The statements grouped by their strength.
| Strength of Statement * | Statement | |
|---|---|---|
| A1 | 1. | A linear transducer is the most commonly used transducer for LUS examination of a suspected lower respiratory tract infection (LRTI) in children. |
| 2. | The entire available lung surface should be examined in children with suspected LRTI. | |
| 4. | LUS has high diagnostic value in assessing the presence of fluid in pleural cavities. | |
| 5. | LUS is useful for diagnosing community-acquired pneumonia (CAP) in children. | |
| 6. | LUS has at least equal diagnostic value to chest X-ray (CXR) in detecting CAP in children. | |
| 7. | Normal LUS results in children with suspected LRTI significantly reduce the probability of diagnosing CAP. | |
| 8. | Consolidation is the most commonly reported LUS finding in children with pneumonia. | |
| 9. | LUS is more sensitive in detecting consolidations than CXR. | |
| B1 | 3. | Diagnostic value of LUS in children with suspected LRTI to a limited extent depends on the sonographer’s experience. |
| 12. | LUS is useful in monitoring the course of pneumonia in children. | |
| 13. | LUS is useful in diagnosing complications of pneumonia in children. | |
| 14. | LUS is useful in bronchiolitis diagnosis. | |
| 16. | LUS is useful in assessing the severity of bronchiolitis. | |
| C1 | 10. | Assessment of the vascular pattern of the consolidation may improve the diagnostic value of LUS in children with suspected LRTI. |
| 11. | LUS does not determine the aetiology of CAP in children. | |
| 15. | LUS has a diagnostic value equal or greater than CXR in bronchiolitis diagnosis. | |
| 17. | LUS is useful in monitoring patients with bronchiolitis. | |
* No statements were ranked A2, B2 or C2.
4. Discussion and Conclusions
To the best of the authors’ knowledge, this is the first evidence-based document substantiating the role of LUS in the management of pneumonia and bronchiolitis in children. Volpicelli et al. published international recommendations, which included only three statements concerning the paediatric population [11]. Our consensus complies with two of the statements entirely: 1. “LUS is a clinically useful tool in children with suspected pneumonia” and 2. “LUS has at least the same diagnostic value as chest X-ray in diagnosing” this disease entity. In this document, we did not address the third statement: “The ultrasound signs of lung and pleural diseases described in adults are also found in paediatric patients” as we did not analyse data from adults. Volpicelli also states that “if pneumonia is suspected, positive LUS excludes the need to perform CXR”, which supports our suggestion to treat LUS as the first-choice method in paediatric patients suspected of CAP who require diagnostic imaging (statement 6, comment c).
There are some limitations to our consensus. Firstly, the literature search was performed in only one database and included only articles published in English. Secondly, even though the literature search was wide, there were few documents concerning LUS in children. Moreover, due to constrained data regarding the use of LUS in many respiratory tract diseases in children, the spectrum of this consensus had to be limited to pneumonia and bronchiolitis. Finally, although all the statements are firmly based on evidence research, the comments are based both on the literature review and the authors’ personal experiences. Despite all the above-mentioned limitations, this consensus establishes the role of LUS in the management of pneumonia and bronchiolitis in children. It gathers the opinions of experts in different fields of respiratory tract diseases ranging from radiologists, paediatricians, to paediatric pulmonologists. Moreover, it addresses many practical issues regarding the performance technique and the result preparation process of LUS and, therefore, may provide guidance for sonographers of different levels of experience. Finally, this document also addresses all the physicians who do not perform LUS themselves but utilize the results obtained by LUS. In this case, it offers guidance on when to order LUS, its capabilities and limitations, and how to interpret the results of this relatively new imaging tool. Given the possibility of acquiring clinically significant information with the use of LUS, the authors expect that in the next few years this modality will be included in the new guidelines and recommendations for the diagnosis and management of respiratory tract infections in children.
The consensus will be updated every three years as new relevant reports in the literature will emerge.
Articles included in the literature review, but not cited before: [75,76].
Acknowledgments
The authors would like to thank Marianne Suwalski (Lawson Health Research Institute, University of Western Ontario) for proofreading this document.
Author Contributions
Conceptualization: N.B., A.P., J.W., B.L., A.K.P., J.J., W.K. Investigation: A.P., J.J., J.W., A.K.P., B.L., M.K., P.K., J.S., M.W., K.K.S., N.B., Z.D., W.K. Supervision: N.B., W.K. Writing—original draft: A.K.P., J.J., A.P., J.W. Writing—review and editing: A.K.P., J.J., N.B.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Harris M., Clark J., Coote N., Fletcher P., Harnden A., McKean M., Thomson A., British Thoracic Society Standards of Care Committee British Thoracic Society guidelines for the management of community acquired pneumonia in children: update 2011. Thorax. 2011;66(Suppl 2):ii1–23. doi: 10.1136/thoraxjnl-2011-200598. [DOI] [PubMed] [Google Scholar]
- 2.Williams G.J., Macaskill P., Kerr M., Fitzgerald D.A., Isaacs D., Codarini M., McCaskill M., Prelog K., Craig J.C. Variability and accuracy in interpretation of consolidation on chest radiography for diagnosing pneumonia in children under 5 years of age. Pediatr. Pulmonol. 2013;48:1195–1200. doi: 10.1002/ppul.22806. [DOI] [PubMed] [Google Scholar]
- 3.Brenner D.J., Hall E.J. Computed tomography—An increasing source of radiation exposure. N. Engl. J. Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 4.Zar H.J., Andronikou S., Nicol M.P. Advances in the diagnosis of pneumonia in children. BMJ. 2017;358:j2739. doi: 10.1136/bmj.j2739. [DOI] [PubMed] [Google Scholar]
- 5.Stadler J.A.M., Andronikou S., Zar H.J. Lung ultrasound for the diagnosis of community-acquired pneumonia in children. Pediatr. Radiol. 2017;47:1412–1419. doi: 10.1007/s00247-017-3910-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caiulo V.A., Gargani L., Caiulo S., Fisicaro A., Moramarco F., Latini G., Picano E., Mele G. Lung ultrasound characteristics of community-acquired pneumonia in hospitalized children. Pediatr. Pulmonol. 2013;48:280–287. doi: 10.1002/ppul.22585. [DOI] [PubMed] [Google Scholar]
- 7.Lichtenstein D.A., Mezière G.A. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: The BLUE protocol. Chest. 2008;134:117–125. doi: 10.1378/chest.07-2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kirkpatrick A.W., Sirois M., Laupland K.B., Liu D., Rowan K., Ball C.G., Hameed S.M., Brown R., Simons R., Dulchavsky S.A., et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: The Extended Focused Assessment with Sonography for Trauma (EFAST) J. Trauma. 2004;57:288–295. doi: 10.1097/01.TA.0000133565.88871.E4. [DOI] [PubMed] [Google Scholar]
- 9.Buda N., Kosiak W., Radzikowska E., Olszewski R., Jassem E., Grabczak E.M., Pomiecko A., Piotrkowski J., Piskunowicz M., Soltysiak M., et al. Polish recommendations for lung ultrasound in internal medicine (POLLUS-IM) J. Ultrason. 2018;18:198–206. doi: 10.15557/JoU.2018.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buda N., Kosiak W., Wełnicki M., Skoczylas A., Olszewski R., Piotrkowski J., Skoczyński S., Radzikowska E., Jassem E., Grabczak E.M., et al. Recommendations for Lung Ultrasound in Internal Medicine. Diagnostics. 2020;10:597. doi: 10.3390/diagnostics10080597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Volpicelli G., Elbarbary M., Blaivas M., Lichtenstein D.A., Mathis G., Kirkpatrick A.W., Melniker L., Gargani L., Noble V.E., Via G., et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38:577–591. doi: 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 12.Boulkedid R., Abdoul H., Loustau M., Sibony O., Alberti C. Using and reporting the Delphi method for selecting healthcare quality indicators: A systematic review. PLoS ONE. 2011;6:e20476. doi: 10.1371/journal.pone.0020476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guyatt G.H., Oxman A.D., Schünemann H.J., Tugwell P., Knottnerus A. GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. J. Clin. Epidemiol. 2011;64:380–382. doi: 10.1016/j.jclinepi.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 14.Willis B.H., Quigley M. Uptake of newer methodological developments and the deployment of meta-analysis in diagnostic test research: A systematic review. BMC Med. Res. Methodol. 2011;11:27. doi: 10.1186/1471-2288-11-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lichtenstein D. Novel approaches to ultrasonography of the lung and pleural space: Where are we now? Breathe (Sheff) 2017;13:100–111. doi: 10.1183/20734735.004717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shah V.P., Tunik M.G., Tsung J.W. Prospective evaluation of point-of-care ultrasonography for the diagnosis of pneumonia in children and young adults. JAMA Pediatr. 2013;167:119–125. doi: 10.1001/2013.jamapediatrics.107. [DOI] [PubMed] [Google Scholar]
- 17.Tripathi S., Ganatra H., Martinez E., Mannaa M., Peters J. Accuracy and reliability of bedside thoracic ultrasound in detecting pulmonary pathology in a heterogeneous pediatric intensive care unit population. J. Clin. Ultrasound. 2019;47:63–70. doi: 10.1002/jcu.22657. [DOI] [PubMed] [Google Scholar]
- 18.de Souza T.H., Nadal J.A.H., Peixoto A.O., Pereira R.M., Giatti M.P., Soub A.C.S., Brandão M.B. Lung ultrasound in children with pneumonia: interoperator agreement on specific thoracic regions. Eur. J. Pediatr. 2019;178:1369–1377. doi: 10.1007/s00431-019-03428-2. [DOI] [PubMed] [Google Scholar]
- 19.Yilmaz H.L., Özkaya A.K., Sarı Gökay S., Tolu Kendir Ö., Şenol H. Point-of-care lung ultrasound in children with community acquired pneumonia. Am. J. Emerg. Med. 2017;35:964–969. doi: 10.1016/j.ajem.2017.01.065. [DOI] [PubMed] [Google Scholar]
- 20.Özkaya A.K., Başkan Vuralkan F., Ardıç Ş. Point-of-care lung ultrasound in children with non-cardiac respiratory distress or tachypnea. Am. J. Emerg. Med. 2019;37:2102–2106. doi: 10.1016/j.ajem.2019.05.063. [DOI] [PubMed] [Google Scholar]
- 21.Wojsyk-Banaszak I., Krenke K., Jończyk-Potoczna K., Ksepko K., Wielebska A., Mikoś M., Bręborowicz A. Long-term sequelae after lung abscess in children—Two tertiary centers’ experience. J. Infect. Chemother. 2018;24:376–382. doi: 10.1016/j.jiac.2017.12.020. [DOI] [PubMed] [Google Scholar]
- 22.Ellington L.E., Gilman R.H., Chavez M.A., Pervaiz F., Marin-Concha J., Compen-Chang P., Riedel S., Rodriguez S.J., Gaydos C., Hardick J., et al. Lung ultrasound as a diagnostic tool for radiographically-confirmed pneumonia in low resource settings. Respir. Med. 2017;128:57–64. doi: 10.1016/j.rmed.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Özkaya A.K., Yilmaz H.L., Kendir Ö., Gökay S.S., Eyüboğlu İ. Lung Ultrasound Findings and Bronchiolitis Ultrasound Score for Predicting Hospital Admission in Children With Acute Bronchiolitis. Pediatr. Emerg. Care. 2020;36:e135–e142. doi: 10.1097/PEC.0000000000001705. [DOI] [PubMed] [Google Scholar]
- 24.Man S.C., Fufezan O., Sas V., Schnell C. Performance of lung ultrasonography for the diagnosis of communityacquired pneumonia in hospitalized children. Med. Ultrason. 2017;19:276–281. doi: 10.11152/mu-1027. [DOI] [PubMed] [Google Scholar]
- 25.Lissaman C., Kanjanauptom P., Ong C., Tessaro M., Long E., O’Brien A. Prospective observational study of point-of-care ultrasound for diagnosing pneumonia. Arch. Dis. Child. 2019;104:12–18. doi: 10.1136/archdischild-2017-314496. [DOI] [PubMed] [Google Scholar]
- 26.Reali F., Sferrazza Papa G.F., Carlucci P., Fracasso P., Di Marco F., Mandelli M., Soldi S., Riva E., Centanni S. Can lung ultrasound replace chest radiography for the diagnosis of pneumonia in hospitalized children? Respiration. 2014;88:112–115. doi: 10.1159/000362692. [DOI] [PubMed] [Google Scholar]
- 27.Tsung J.W., Kessler D.O., Shah V.P. Prospective application of clinician-performed lung ultrasonography during the 2009 H1N1 influenza A pandemic: Distinguishing viral from bacterial pneumonia. Crit. Ultrasound. J. 2012;4:16. doi: 10.1186/2036-7902-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Biagi C., Pierantoni L., Baldazzi M., Greco L., Dormi A., Dondi A., Faldella G., Lanari M. Lung ultrasound for the diagnosis of pneumonia in children with acute bronchiolitis. BMC Pulm. Med. 2018;18:191. doi: 10.1186/s12890-018-0750-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pereda M.A., Chavez M.A., Hooper-Miele C.C., Gilman R.H., Steinhoff M.C., Ellington L.E., Gross M., Price C., Tielsch J.M., Checkley W. Lung ultrasound for the diagnosis of pneumonia in children: A meta-analysis. Pediatrics. 2015;135:714–722. doi: 10.1542/peds.2014-2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Balk D.S., Lee C., Schafer J., Welwarth J., Hardin J., Novack V., Yarza S., Hoffmann B. Lung ultrasound compared to chest X-ray for diagnosis of pediatric pneumonia: A meta-analysis. Pediatr. Pulmonol. 2018;53:1130–1139. doi: 10.1002/ppul.24020. [DOI] [PubMed] [Google Scholar]
- 31.Lai S.H., Wong K.S., Liao S.L. Value of Lung Ultrasonography in the Diagnosis and Outcome Prediction of Pediatric Community-Acquired Pneumonia with Necrotizing Change. PLoS ONE. 2015;10:e0130082. doi: 10.1371/journal.pone.0130082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guerra M., Crichiutti G., Pecile P., Romanello C., Busolini E., Valent F., Rosolen A. Ultrasound detection of pneumonia in febrile children with respiratory distress: A prospective study. Eur J. Pediatr. 2016;175:163–170. doi: 10.1007/s00431-015-2611-8. [DOI] [PubMed] [Google Scholar]
- 33.Claes A.S., Clapuyt P., Menten R., Michoux N., Dumitriu D. Performance of chest ultrasound in pediatric pneumonia. Eur. J. Radiol. 2017;88:82–87. doi: 10.1016/j.ejrad.2016.12.032. [DOI] [PubMed] [Google Scholar]
- 34.Varshney T., Mok E., Shapiro A.J., Li P., Dubrovsky A.S. Point-of-care lung ultrasound in young children with respiratory tract infections and wheeze. Emerg. Med. J. 2016;33:603–610. doi: 10.1136/emermed-2015-205302. [DOI] [PubMed] [Google Scholar]
- 35.Iuri D., De Candia A., Bazzocchi M. Evaluation of the lung in children with suspected pneumonia: Usefulness of ultrasonography. Radiol. Med. 2009;114:321–330. doi: 10.1007/s11547-008-0336-8. [DOI] [PubMed] [Google Scholar]
- 36.Kurian J., Levin T.L., Han B.K., Taragin B.H., Weinstein S. Comparison of ultrasound and CT in the evaluation of pneumonia complicated by parapneumonic effusion in children. Am. J. Roentgenol. 2009;193:1648–1654. doi: 10.2214/AJR.09.2791. [DOI] [PubMed] [Google Scholar]
- 37.Ho M.C., Ker C.R., Hsu J.H., Wu J.R., Dai Z.K., Chen I.C. Usefulness of lung ultrasound in the diagnosis of community-acquired pneumonia in children. Pediatr. Neonatol. 2015;56:40–45. doi: 10.1016/j.pedneo.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 38.Ianniello S., Piccolo C.L., Buquicchio G.L., Trinci M., Miele V. First-line diagnosis of paediatric pneumonia in emergency: Lung ultrasound (LUS) in addition to chest-X-ray (CXR) and its role in follow-up. Br. J. Radiol. 2016;89:20150998. doi: 10.1259/bjr.20150998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang L., Song W., Wang Y., Han J., Lv K. Lung ultrasonography versus chest radiography for the diagnosis of pediatric community acquired pneumonia in emergency department: A meta-analysis. J. Thorac. Dis. 2019;11:5107–5114. doi: 10.21037/jtd.2019.11.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hajalioghli P., Nemati M., Dinparast Saleh L., Fouladi D.F. Can Chest Computed Tomography Be Replaced by Lung Ultrasonography With or Without Plain Chest Radiography in Pediatric Pneumonia? J. Thorac. Imaging. 2016;31:247–252. doi: 10.1097/RTI.0000000000000209. [DOI] [PubMed] [Google Scholar]
- 41.Boursiani C., Tsolia M., Koumanidou C., Malagari A., Vakaki M., Karapostolakis G., Mazioti A., Alexopoulou E. Lung Ultrasound as First-Line Examination for the Diagnosis of Community-Acquired Pneumonia in Children. Pediatr. Emerg. Care. 2017;33:62–66. doi: 10.1097/PEC.0000000000000969. [DOI] [PubMed] [Google Scholar]
- 42.Berce V., Tomazin M., Gorenjak M., Berce T., Lovrenčič B. The Usefulness of Lung Ultrasound for the Aetiological Diagnosis of Community-Acquired Pneumonia in Children. Sci. Rep. 2019;9:17957. doi: 10.1038/s41598-019-54499-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Milliner B.H.A., Tsung J.W. Lung Consolidation Locations for Optimal Lung Ultrasound Scanning in Diagnosing Pediatric Pneumonia. J. Ultrasound Med. 2017;36:2325–2328. doi: 10.1002/jum.14272. [DOI] [PubMed] [Google Scholar]
- 44.Iorio G., Capasso M., Prisco S., De Luca G., Mancusi C., Laganà B., Piscopo M.A., Comune V. Lung Ultrasound Findings Undetectable by Chest Radiography in Children with Community-Acquired Pneumonia. Ultrasound. Med. Biol. 2018;44:1687–1693. doi: 10.1016/j.ultrasmedbio.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 45.Copetti R., Cattarossi L. Ultrasound diagnosis of pneumonia in children. Radiol. Med. 2008;113:190–198. doi: 10.1007/s11547-008-0247-8. [DOI] [PubMed] [Google Scholar]
- 46.Lovrenski J., Petrović S., Balj-Barbir S., Jokić R., Vilotijević-Dautović G. Stethoscope vs. ultrasound probe—Which is more reliable in children with suspected pneumonia? Acta Med. Acad. 2016;45:39–50. doi: 10.5644/ama2006-124.155. [DOI] [PubMed] [Google Scholar]
- 47.Heuvelings C.C., Belard S., Andronikou S., Jamieson-Luff N., Grobusch M.P., Zar H.J. Chest ultrasound findings in children with suspected pulmonary tuberculosis. Pediatr. Pulmonol. 2019;54:463–470. doi: 10.1002/ppul.24230. [DOI] [PubMed] [Google Scholar]
- 48.Esposito S., Papa S.S., Borzani I., Pinzani R., Giannitto C., Consonni D., Principi N. Performance of lung ultrasonography in children with community-acquired pneumonia. Ital. J. Pediatr. 2014;40:37. doi: 10.1186/1824-7288-40-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Samson F., Gorostiza I., González A., Landa M., Ruiz L., Grau M. Prospective evaluation of clinical lung ultrasonography in the diagnosis of community-acquired pneumonia in a pediatric emergency department. Eur J. Emerg. Med. 2018;25:65–70. doi: 10.1097/MEJ.0000000000000418. [DOI] [PubMed] [Google Scholar]
- 50.Zhan C., Grundtvig N., Klug B.H. Performance of Bedside Lung Ultrasound by a Pediatric Resident: A Useful Diagnostic Tool in Children With Suspected Pneumonia. Pediatr. Emerg. Care. 2018;34:618–622. doi: 10.1097/PEC.0000000000000888. [DOI] [PubMed] [Google Scholar]
- 51.Omran A., Eesai S., Ibrahim M., El-Sharkawy S. Lung ultrasound in diagnosis and follow up of community acquired pneumonia in infants younger than 1-year old. Clin. Respir. J. 2018;12:2204–2211. doi: 10.1111/crj.12790. [DOI] [PubMed] [Google Scholar]
- 52.Supino M.C., Buonsenso D., Scateni S., Scialanga B., Mesturino M.A., Bock C., Chiaretti A., Giglioni E., Reale A., Musolino A.M. Point-of-care lung ultrasound in infants with bronchiolitis in the pediatric emergency department: A prospective study. Eur. J. Pediatr. 2019;178:623–632. doi: 10.1007/s00431-019-03335-6. [DOI] [PubMed] [Google Scholar]
- 53.Bueno-Campaña M., Sainz T., Alba M., Del Rosal T., Mendez-Echevarría A., Echevarria R., Tagarro A., Ruperez-Lucas M., Herrreros M.L., Latorre L., et al. Lung ultrasound for prediction of respiratory support in infants with acute bronchiolitis: A cohort study. Pediatr. Pulmonol. 2019;54:873–880. doi: 10.1002/ppul.24287. [DOI] [PubMed] [Google Scholar]
- 54.Basile V., Di Mauro A., Scalini E., Comes P., Lofù I., Mostert M., Tafuri S., Manzionna M.M. Lung ultrasound: A useful tool in diagnosis and management of bronchiolitis. BMC Pediatr. 2015;15:63. doi: 10.1186/s12887-015-0380-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Iorio G., Capasso M., De Luca G., Prisco S., Mancusi C., Laganà B., Comune V. Lung ultrasound in the diagnosis of pneumonia in children: Proposal for a new diagnostic algorithm. PeerJ. 2015;3:e1374. doi: 10.7717/peerj.1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pervaiz F., Hossen S., Chavez M.A., Miele C.H., Moulton L.H., McCollum E.D., Roy A.D., Chowdhury N.H., Ahmed S., Begum N., et al. Training and standardization of general practitioners in the use of lung ultrasound for the diagnosis of pediatric pneumonia. Pediatr. Pulmonol. 2019;54:1753–1759. doi: 10.1002/ppul.24477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Musolino A.M., Tomà P., Supino M.C., Scialanga B., Mesturino A., Scateni S., Battaglia M., Pirozzi N., Bock C., Buonsenso D. Lung ultrasound features of children with complicated and noncomplicated community acquired pneumonia: A prospective study. Pediatr. Pulmonol. 2019;54:1479–1486. doi: 10.1002/ppul.24426. [DOI] [PubMed] [Google Scholar]
- 58.Jones B.P., Tay E.T., Elikashvili I., Sanders J.E., Paul A.Z., Nelson B.P., Spina L.A., Tsung J.W. Feasibility and Safety of Substituting Lung Ultrasonography for Chest Radiography When Diagnosing Pneumonia in Children: A Randomized Controlled Trial. Chest. 2016;150:131–138. doi: 10.1016/j.chest.2016.02.643. [DOI] [PubMed] [Google Scholar]
- 59.Chavez M.A., Naithani N., Gilman R.H., Tielsch J.M., Khatry S., Ellington L.E., Miranda J.J., Gurung G., Rodriguez S., Checkley W. Agreement Between the World Health Organization Algorithm and Lung Consolidation Identified Using Point-of-Care Ultrasound for the Diagnosis of Childhood Pneumonia by General Practitioners. Lung. 2015;193:531–538. doi: 10.1007/s00408-015-9730-x. [DOI] [PubMed] [Google Scholar]
- 60.Yadav K.K., Awasthi S., Parihar A. Lung Ultrasound is Comparable with Chest Roentgenogram for Diagnosis of Community-Acquired Pneumonia in Hospitalised Children. Indian J. Pediatr. 2017;84:499–504. doi: 10.1007/s12098-017-2333-1. [DOI] [PubMed] [Google Scholar]
- 61.Nadimpalli A., Tsung J.W., Sanchez R., Shah S., Zelikova E., Umphrey L., Hurtado N., Gonzalez A., Teicher C. Feasibility of Training Clinical Officers in Point-of-Care Ultrasound for Pediatric Respiratory Diseases in Aweil, South Sudan. Am. J. Trop. Med. Hyg. 2019;101:689–695. doi: 10.4269/ajtmh.18-0745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gravel C.A., Monuteaux M.C., Levy J.A., Miller A.F., Vieira R.L., Bachur R.G. Interrater reliability of pediatric point-of-care lung ultrasound findings. Am. J. Emerg. Med. 2020;38:1–6. doi: 10.1016/j.ajem.2019.01.047. [DOI] [PubMed] [Google Scholar]
- 63.Jaszczołt S., Polewczyk T., Dołęga-Kozierowska M., Woźniak M., Doniec Z. Comparison of lung ultrasound and chest X-ray findings in children with bronchiolitis. J. Ultrason. 2018;18:193–197. doi: 10.15557/JoU.2018.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Caiulo V.A., Gargani L., Caiulo S., Fisicaro A., Moramarco F., Latini G., Picano E. Lung ultrasound in bronchiolitis: Comparison with chest X-ray. Eur. J. Pediatr. 2011;170:1427–1433. doi: 10.1007/s00431-011-1461-2. [DOI] [PubMed] [Google Scholar]
- 65.Ambroggio L., Sucharew H., Rattan M.S., O’Hara S.M., Babcock D.S., Clohessy C., Steinhoff M.C., Macaluso M., Shah S.S., Coley B.D. Lung Ultrasonography: A Viable Alternative to Chest Radiography in Children with Suspected Pneumonia? J. Pediatr. 2016;176:93–98.e97. doi: 10.1016/j.jpeds.2016.05.033. [DOI] [PubMed] [Google Scholar]
- 66.Harel-Sterling M., Diallo M., Santhirakumaran S., Maxim T., Tessaro M. Emergency Department Resource Use in Pediatric Pneumonia: Point-of-Care Lung Ultrasonography versus Chest Radiography. J. Ultrasound Med. 2019;38:407–414. doi: 10.1002/jum.14703. [DOI] [PubMed] [Google Scholar]
- 67.Urbankowska E., Krenke K., Drobczyński Ł., Korczyński P., Urbankowski T., Krawiec M., Kraj G., Brzewski M., Kulus M. Lung ultrasound in the diagnosis and monitoring of community acquired pneumonia in children. Respir. Med. 2015;109:1207–1212. doi: 10.1016/j.rmed.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 68.Lenahan J.L., Volpicelli G., Lamorte A., Jehan F., Bassat Q., Ginsburg A.S. Multicentre pilot study evaluation of lung ultrasound for the management of paediatric pneumonia in low-resource settings: A study protocol. BMJ Open Respir. Res. 2018;5:e000340. doi: 10.1136/bmjresp-2018-000340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Orso D., Ban A., Guglielmo N. Lung ultrasound in diagnosing pneumonia in childhood: A systematic review and meta-analysis. J. Ultrasound. 2018;21:183–195. doi: 10.1007/s40477-018-0306-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Buonsenso D., Musolino A.M., Gatto A., Lazzareschi I., Curatola A., Valentini P. Lung ultrasound in infants with bronchiolitis. BMC Pulm. Med. 2019;19:159. doi: 10.1186/s12890-019-0925-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Buonsenso D., Brancato F., Valentini P., Curatola A., Supino M., Musolino A.M. The Use of Lung Ultrasound to Monitor the Antibiotic Response of Community-Acquired Pneumonia in Children: A Preliminary Hypothesis. J. Ultrasound Med. 2020;39:817–826. doi: 10.1002/jum.15147. [DOI] [PubMed] [Google Scholar]
- 72.Ricci V., Delgado Nunes V., Murphy M.S., Cunningham S., The Guideline Development Group and Technical Team Bronchiolitis in children: Summary of NICE guidance. BMJ. 2015;350:h2305. doi: 10.1136/bmj.h2305. [DOI] [PubMed] [Google Scholar]
- 73.Silver A.H., Nazif J.M. Bronchiolitis. Pediatr. Rev. 2019;40:568–576. doi: 10.1542/pir.2018-0260. [DOI] [PubMed] [Google Scholar]
- 74.Cohen J.S., Hughes N., Tat S., Chamberlain J.M., Teach S.J., Boniface K. The Utility of Bedside Lung Ultrasound Findings in Bronchiolitis. Pediatr. Emerg. Care. 2017;33:97–100. doi: 10.1097/PEC.0000000000000820. [DOI] [PubMed] [Google Scholar]
- 75.Correa M., Zimic M., Barrientos F., Barrientos R., Román-Gonzalez A., Pajuelo M.J., Anticona C., Mayta H., Alva A., Solis-Vasquez L., et al. Automatic classification of pediatric pneumonia based on lung ultrasound pattern recognition. PLoS ONE. 2018;13:e0206410. doi: 10.1371/journal.pone.0206410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cisneros-Velarde P., Correa M., Mayta H., Anticona C., Pajuelo M., Oberhelman R., Checkley W., Gilman R.H., Figueroa D., Zimic M., et al. Automatic pneumonia detection based on ultrasound video analysis. Conf Proc. IEEE Eng. Med. Biol Soc. 2016;2016:4117–4120. doi: 10.1109/EMBC.2016.7591632. [DOI] [PubMed] [Google Scholar]