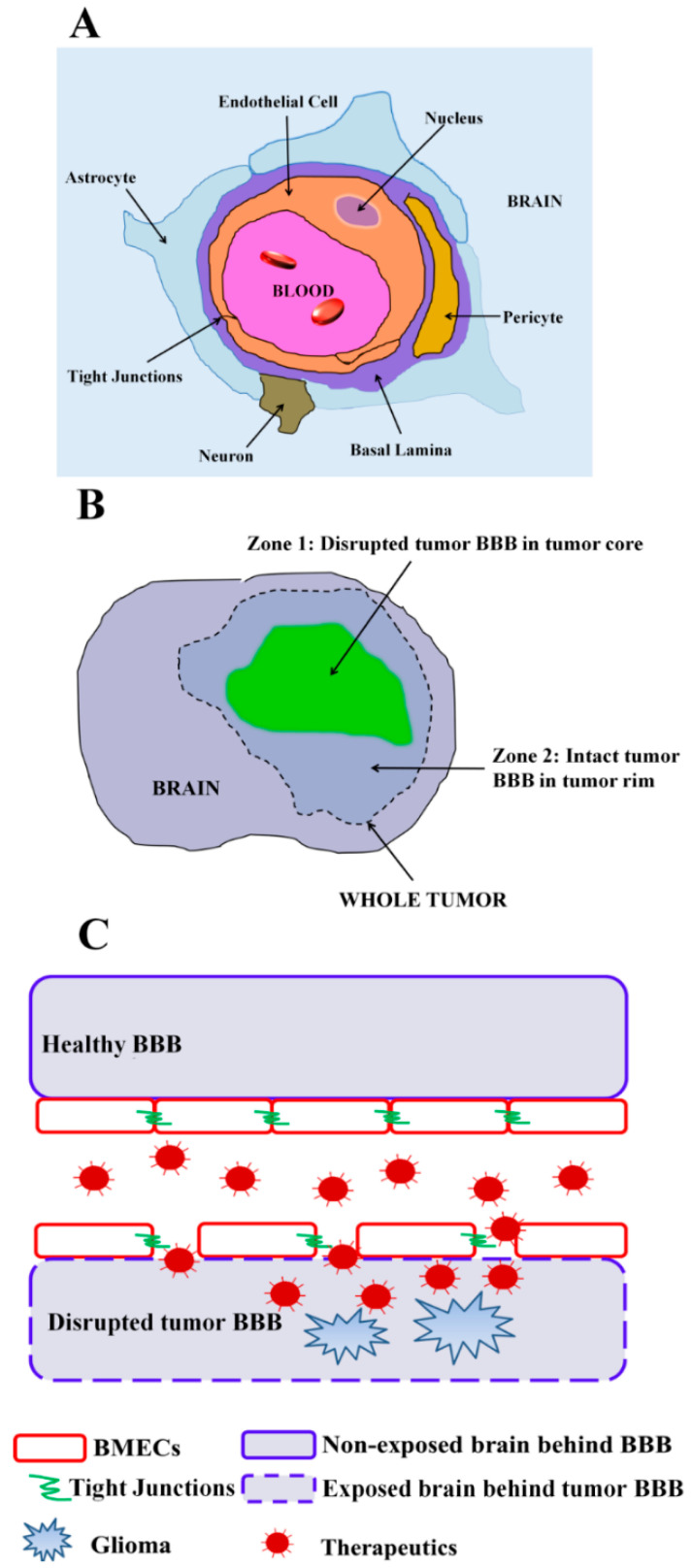
Figure 1.
(A) Cross-sectional view of the neurovascular unit with the brain endothelial cells forming the blood–brain barrier (BMECs). Brain endothelial cells are connected by adherens and tight junctions, share a basement membrane with pericytes, make contacts with astrocyte endfeet and respond to neuronal cues. (B) Cartoon representation of the heterogeneity of tumor BBB permeability in glioma. Two zones can often be observed within the tumor volume—zone 1: disrupted tumor BBB in the tumor core imaged via MRI contrast leakage; zone 2: intact tumor BBB in the tumor rim area. (C) Cartoon depiction of drug delivery through normal and pathologically disrupted tumor BBB. Under normal conditions, the healthy and intact BBB separates the CNS from blood components, thereby preventing therapeutics from accessing the CNS. Under conditions in which glioma induces pathologic tumor BBB disruption, therapeutics can access the CNS via passive penetration or actively targeting the exposed components behind the disrupted tumor BBB.