Abstract
Simple Summary
Understanding how heart muscle cells function and developing new strategies for repairing the damaged heart are important challenges for tackling heart disease. Human cells from the heart are required in the laboratory for these investigations, but are difficult to obtain in large numbers from patients. As an alternative, stem cells can be used which can be cultured indefinitely in the laboratory and then turned into heart muscle cells. The current methods lead to a mixture of cell types, belonging to the different regions of the heart, creating difficulties when trying to understand the biology of a particular area of the heart, or for future applications when these stem cell-derived cell types are used to repair the heart. Genetic modification of stem cells provides a solution to this problem, as these techniques allow fluorescent markers, so-called reporters, to be inserted into key genes that are active in the different cell types. The different coloured reporters thus allow the identification and purification of specific cell types. In this review, we discuss the various methods that can be used to establish these reporter systems and highlight their applications in different aspects of cardiovascular medicine.
Abstract
Recent advances have made pluripotent stem cell (PSC)-derived cardiomyocytes an attractive option to model both normal and diseased cardiac function at the single-cell level. However, in vitro differentiation yields heterogeneous populations of cardiomyocytes and other cell types, potentially confounding phenotypic analyses. Fluorescent PSC-derived cardiomyocyte reporter systems allow specific cell lineages to be labelled, facilitating cell isolation for downstream applications including drug testing, disease modelling and cardiac regeneration. In this review, the different genetic strategies used to generate such reporter lines are presented with an emphasis on their relative technical advantages and disadvantages. Next, we explore how the fluorescent reporter lines have provided insights into cardiac development and cardiomyocyte physiology. Finally, we discuss how exciting new approaches using PSC-derived cardiomyocyte reporter lines are contributing to progress in cardiac cell therapy with respect to both graft adaptation and clinical safety.
Keywords: fluorescent PSC-CM reporter lines, transgenic methods, CM purification, cardiac development, optical electrophysiology
1. Introduction
Pluripotent stem cells (PSCs), including embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), have revolutionised the study of developmental biology and diseases [1,2,3,4,5]. Although animal models provide valuable in vivo insights into developmental processes, they may not recapitulate human biology fully due to species-specific characteristics [6,7,8,9]. PSCs, on the other hand, are obtainable from humans. Human ESCs (hESCs) are derived from preimplantation human embryos, generally donated as a by-product of fertility treatment, which has raised ethical concerns [10]. Human iPSCs (hiPSCs), however, avoid these issues, as they can be reprogrammed from somatic cells [11]. Potential challenges in the use of iPSCs primarily lie in their preparation. The reprogramming process leaves epigenetic relics, e.g., DNA methylation, which may cause variation in gene expression profiles among different iPSC lines and between iPSC and ESC lines [12]. Compared to ESCs, some iPSC lines exhibit differentiation delay or defects [13], partly due to incomplete reprogramming. The choice of iPSC lines needs to be validated for the desired lineages as there may be biases in differentiation capacity due to the somatic origin from which the lines were reprogrammed [14]. In addition, substantial iPSC passaging increases the risk of genome instability and possibly leads to phenotypic variation in iPSC-derived progenies [15].
Although primary adult cardiomyocytes (CMs) have provided important insights [16,17], their lack of proliferation and short culture life prevents long-term studies. By contrast, PSCs are pluripotent and can self-renew, making them powerful research tools. They can be cultured indefinitely and can be differentiated into various types of cells, including cardiac lineages. In vitro PSC-CM differentiation involves sequential steps, primarily regulated by the WNT signalling pathway [18]. WNT activation induces PSC transition to mesodermal stages and subsequent inhibition of the pathway steers the fate of the cells towards cardiac mesoderm and cardiac progenitor cells (CPCs), giving rise to both CM and non-CM progenies. PSC-CMs may also have a potential therapeutic application in cardiac tissue repair. However, two limitations complicate such applications. Firstly, PSC-CMs display embryonic characteristics, both structurally and functionally, and secondly, the differentiation protocols yield mixed populations of different CM subtypes, including atrial, ventricular and nodal cells, and non-CM cell types.
The ability to label individual cell types non-invasively using a genetically encoded fluorescent reporter offers the prospect of greater insight into cardiac differentiation and the isolation of pure populations of specific cell types. In this review, we will discuss how such fluorescent reporter lines are generated and how reporter cells can be used to study developmental cardiology, CM function and how they have advanced cardiovascular medicine.
2. Establishment of Transgenic Fluorescent Reporter Lines
In order to produce a fluorescent reporter line, a transgenic construct is required comprising a fluorescent protein (FP) inserted downstream of a promoter or gene of interest (GOI). A reporter line can be generated as a transient line, where the transgene remains episomal, or as a stable line, where the transgene becomes integrated into the host genome, either site-specifically or randomly. A summary of the various methods is presented in Table 1.
Table 1.
A summary of different transgenic approaches used to generate fluorescent reporter cell lines.
| Method | Advantage | Disadvantage |
|---|---|---|
| (1) Transient fluorescent reporter lines |
|
|
| (2) Random integration of a fluorescent reporter transgene |
|
|
| (3) Targeted integration of a fluorescent reporter transgene |
|
|
| (3.1) Homologous recombination |
|
|
| (3.2) Advanced genome engineering technologies |
|
|
| (3.2.1) Safe habour site targeting |
|
|
| (3.2.2) Specific locus of interest targeting |
|
|
2.1. Transient Fluorescent Reporter Lines
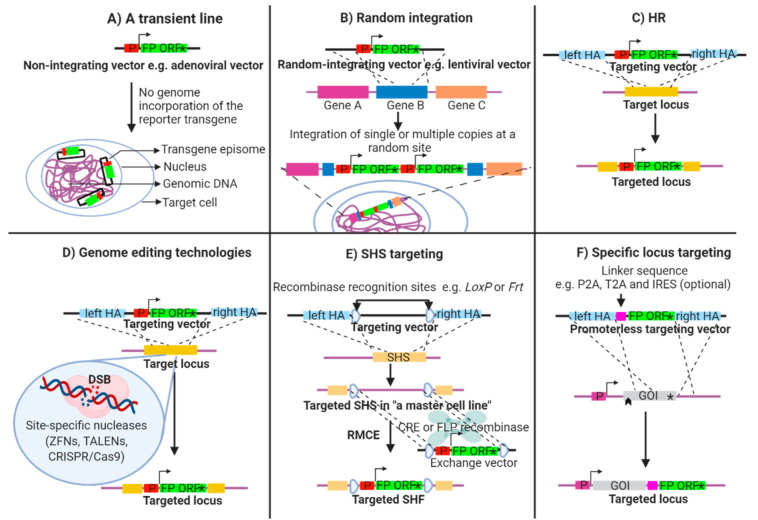
A transient reporter line is produced by introducing the reporter construct as a non-integrating plasmid or vector, e.g., adenovirus [19] into the host cell (Figure 1A). The reporter expression level obtained is dependent upon the copy number, and typically decays as the non-integrated copies are lost, leading to cell-to-cell phenotypic variation. An application in developmental studies is limited since the transfection needs to be performed at a time where the ectopic promoter driving the FP is active. To avoid such difficulties, stable lines generated by the following methods are preferred.
Figure 1.
Schematic illustration of transgenic methods for fluorescent reporter line generation. A simple fluorescent reporter vector consists of an ectopic fluorescent protein (FP) open reading frame (ORF) preceded by a promoter (P) of a gene of interest (GOI) (A,B). (A) A non-integrating vector, e.g., adenoviral vector is used to produce a transient reporter line whereas using (B) a random-integrating vector, e.g., lentiviral vector results in a genomic insertion of either a single copy or a concatemer of the transgene at random loci. (C) Positioning a reporter construct at a specific locus via homologous recombination (HR), flanking genetic arms (HA) homologous to a target site are required. (D) The HR efficiency can be improved by incorporating genome editing technologies, e.g., zinc finger nucleases (ZNFs), transcription activator-like effector nucleases (TALENs) and clustered regularly interspaced palindromic repeat (CRISPR)/CRISPR-associated protein 9 (Cas9), which introduce a double strand break (DSB) at a specific site, stimulating HR. A fluorescent reporter can be integrated into (E) a safe harbor site (SHS) or (F) an endogenous GOI. (E) “A master cell line” can be prepared by specifically introducing a pair of recombinase recognition site, e.g., LoxP and Frt at a SHS. Subsequently, the flanked sequence can be exchanged for a fluorescent reporter construct by transfecting an exchange vector carrying a reporter construct flanked by equivalent recombination recognition sequences together with a corresponding recombinase enzyme, e.g., CRE or FLP, facilitating the production of multiple fluorescent reporter lines from the same master line via a method known as recombinase-mediated cassette exchanged (RMCE). (F) To allow FP expression under an endogenous gene promoter, a promoterless targeting vector is used to target a specific GOI, e.g., at the stop codon. Alternatively, a link sequence, e.g., P2A, T2A and IRES is added between the FP and the target gene ORF to allow bicistronic expression of both the fluorophore and the target protein.
2.2. Random Integration of a Fluorescent Reporter Transgene
This method relies on the reporter construct being cloned, packaged and delivered via a genome-integrating viral system, e.g., a lentiviral vector [19] (Figure 1B) or in the form of linear or circular DNA. In this latter method, a plasmid or bacterial artificial chromosome (BAC) encoding the fluorescent reporter is introduced by chemical transfection or electroporation and the stability of the integration is ensured through antibiotic selection.
This technique is relatively simple but possesses many biological and technical risks attributable to the random insertion into the genome [20]. Firstly, the transgene copy number cannot be controlled and the insertion of multiple copies of the construct has been linked to a loss of transgene expression in hESCs [21]. Secondly, the transgene expression may be influenced by the genomic context [22] and vice versa, leading to clonal variability in the fluorescent signal. Thirdly, transgene silencing upon differentiation may occur if the transgene is marked by epigenetic factors, or if the transgene is under the influence of altered chromosomal architecture [23,24,25]. All these risks lead to a situation where the fluorescent signal may not reliably mirror the GOI’s promoter activity, confusing the downstream analysis.
2.3. Targeted Integration of a Fluorescent Reporter Transgene
In order to avoid the undesirable effects of a random integration, fluorescent reporter constructs can be inserted into specific genomic sites. Homologous recombination (HR) (Figure 1C) [26] is a DNA repair process that utilises homologous DNA as a template to regenerate lost sequence. Transfecting cells with a reporter construct harbouring an FP flanked with upstream and downstream “arms” homologous to the target locus, the sequence in between the homology arms can be exchanged, and thus the FP inserted. The main disadvantage of this method lies in the low targeting efficiency that can make such experiments challenging [27].
2.4. Advanced Genome Engineering Technologies
The development of site-specific endonucleases including zinc finger nucleases (ZFNs), transcription activator-like effector nucleases (TALENs) and clustered regularly interspaced short palindromic repeat (CRISPR)/CRISPR associated protein 9 (Cas9) has transformed our ability to manipulate the genome [28]. These custom-designed genome-engineering nucleases serve as molecular scissors to cleave specific DNA sequences. The introduction of a double strand break (DSB) can stimulate the HR mechanism, thereby increasing its efficiency [29] (Figure 1D).
With respect to site-specific integration of a fluorescent reporter, there are two common strategies. In the first strategy, the reporter construct can be introduced into a so-called safe harbour site (SHS) (Figure 1E), e.g., adeno-associated virus integration site 1 (AAVS1) [30], chemokine receptor 5 or the human homolog of murine Gt(ROSA)26Sor [31]. These genomic sites have been found to be suitable for transgene expression, ensuring the stable expression of the FP in the majority of cell types [32] and the insertion event is not associated with any major deleterious consequences. In this scenario, a reporter construct is flanked with homology arms designed against the SHS sequence. To simplify insertion at these well-used sites, systems have been engineered which enable a catalytic insertion of a transgene with recombinases. Here, recombination sites, such as heterotypic LoxP or Frt sites, are inserted into the SHS, and equivalent sites are incorporated into the reporter construct, enabling the sequences to be efficiently exchanged through the activity of recombinases [33]. This method, known as recombination-mediated cassette exchange (RMCE), demands the production of “a master cell line” into which multiple fluorescent reporter derivatives can be inserted, permitting the production of isogenic lines without the requirement for retargeting by HR [31,34].
A general disadvantage for all exogenous fluorescent reporter constructs is that a minimal promoter region is used. Subsequently, the fluorescence readout may not faithfully recapitulate the biological expression of the GOI. To avoid this issue, endogenous regulatory elements can be exploited for FP expression, allowing a higher fidelity between reporter and actual promoter activity. Using HR, FPs can be inserted downstream (Figure 1F) of an endogenous GOI or directly upstream of the endogenous start codon. This strategy can directly perturb the GOI locus leading to loss-of-function; hence, a careful design is a prerequisite to ascertain whether the normal function of the GOI is to be retained. Bicistronic expression of the FP downstream of the GOI may provide one way of avoiding loss-of-function. In these cases, linker sequences such as porcine teschovirus-1 2A (P2A), Thosea asigna virus 2A (T2A) [35] or internal ribosomal entry sites (IRES) [36] can be included to separate the GOI ORF and FP [35,37].
Each construct design has inherent advantages and disadvantages and the exact approach adopted should be tailored to the study. Random integration may be a sensible approach for studying gene function and pre-screening of biological effects. A master cell line is more suitable for lineage-specific labelling where multiple reporter lines are needed. Lastly, endogenous locus targeting is safer for projects that rely on the sensitivity of the reporter system.
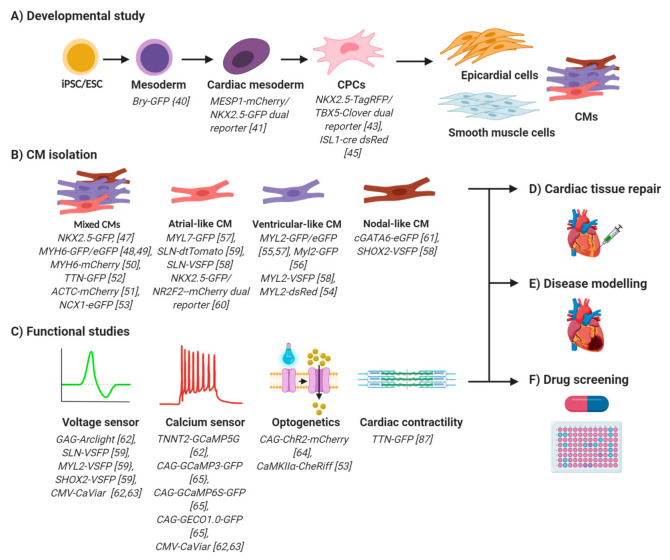
3. PSC-CM Reporter Lines: An Insight into Cardiac Biology
In vitro PSC-CM differentiation involves sequential stages of mesoderm induction, cardiac mesoderm determination, lineage specification and terminal differentiation [18]. WNT/β-catenin signalling plays stage-specific, biphasic roles in CM differentiation [38]. Canonical WNT promotes mesoderm differentiation but inhibits subsequent cardiac mesoderm specification. Despite a greater understanding of developmental pathways, pure CMs are not attainable from in vitro differentiation of PSCs. Fluorescent reporter cell lines, therefore, serve as a powerful tool for deciphering key transition stages essential for cardiogenesis and thus help improve in vitro differentiation protocols. A summary of applications of fluorescent PSC-CM reporter lines, including the steps of in vitro cardiac development, are illustrated in Figure 2 with additional details of published studies presented in Table 2.
Figure 2.
An overview of potential applications for fluorescent PSC-CMs reporter lines. (A) Stage-specific fluorescent reporters provide insights into cardiac development, which help improve PSC-CM differentiation protocols. (B) CM-specific PSC-CM fluorescent reporter lines facilitate FACS-based CM isolation. Purification that is based on a pan-cardiac promoter activity yields mixed types of CMs, each of which can be further selected by using subtype-specific PSC-CM reporter lines. (C) Optical action potential and Ca2+ dynamic measurements can be made using PSC-CMs lines expressing fluorescent voltage (first panel) and fluorescent Ca2+ sensors (second panel). Optogenetic technology aids in spatiotemporal CM activation, which can be used to pace CMs optically for rate-sensitive electrophysiology (third panel). Fluorescent tagging of the sarcomere components such as titin allows a real time observation of CM contractility (fourth panel). Exploiting the advantages of fluorescent PSC-CM reporter lines for cell purification and functional investigation facilitate (D) cardiac tissue repair, (E) disease modelling and (F) high throughput drug screening.
Table 2.
A summary of published fluorescent PSC-CM reporter systems.
| Reporter Construct | Type of Promoter Used | Labelled Cell Population | Utility | Host PSC System | Transgenesis Method | Ref |
|---|---|---|---|---|---|---|
| Bry-GFP | Endogenous Bry | Mesoderm | Tracking mesodermal cell differentiation towards cardiogenic and haematopoietic lineages | mESC | HR by electroporation of the BAC-derived targeting vector into mESCs | [40] |
| MESP1-mCherry/NKX2.5-eGFP | Endogenous MESP1 and NKX2.5 | Cardiac mesoderm (MESP1) and CPCs (NKX2.5) | Tracking of transition of cardiac mesoderm toward CPCs and subsequent CM differentiation | hESC | HR by electroporation of BAC-derived targeting vector into hESCs | [41] |
| NKX2.5-IRES- TagRed/TBX5-IRES-Clover | Endogenous NXK2.5 and TBX5 | CPC subsets | Identification and characterisation of presumptive FHF, SHF, pro-pericardial and pre-endothelial progenitors | hiPSC | CRISPR/Cas9 editing in hiPSC at the NKX2.5 and TBX5 loci using plasmid-based lipofection | [45] |
| ISL1-cre dsRed | Endogenous ISL1 | ISL1+ CPC | Characterisation of ISL1+ CPC derivation | hESC | HR by electroporation of BAC-derived ISL1-cre vector into hESCs followed by transfection of floxed dsRed vector | [44] |
| NKX2.5-GFP | Endogenous NKX2.5 | NKX2.5+ CPC/CMs | Isolation of NKX2.5+ CPC and CMs | hESC | HR by electroporation of BAC-derived targeting vector | [47] |
| MYH6-GFP | Ectopic MYH6 | Beating CMs | Purification of beating CMs and development of PSC-CM differentiation protocol | hESCs and hiPSCs | Lentiviral transduction/ random integration of the transgene into differentiating hPSCs | [48] |
| MYH6-eGFP | Ectopic MYH6 | CM progenitor /beating CMs | Identification of early CM progenitor and purification of CMs | hESC | Lentiviral transduction/random integration of the transgene into hESCs | [49] |
| MYH6-mCherry | Endogenous MYH6 | Beating CMs | Purification of beating CMs for cardiotoxicity evaluation | hESC | CRISPR/Cas9 editing in hiPSC at the MYH6 locus using plasmid-based nucleofection | [50] |
| ACTC-mCherry-WPRE-EF1-neo¥ | Ectopic ACTC | Beating CMs | Purification of CMs | hiPSC | Lentiviral transduction/random integration of the transgene into hiPSCs | [51] |
| TTN-GFP | Endogenous TTN | Beating CMs | Purification of beating CMs and, potentially, study of sarcomere functions | hiPSC | CRISPR/Cas9 editing in hiPSC at the TTN locus | [52] |
| NCX1-eGFP-WPRE | Ectopic NCX1 | Beating CMs | Purification of beating CMs | hiPSC and hESC | Lentiviral transduction/random integration of the transgene into hPSCs | [53] |
| MYL2-dsRed | Ectopic MYL2 | Ventricular-like CMs | Purification of ventricular-like CMs | hESC | Lentiviral transduction/ random integration of the transgene into hESCs | [54] |
| MYL2-eGFP | Ectopic MYL2 | Ventricular-like CMs | Purification of ventricular-like CMs | hESC | Lentriviral transduction/ random integration of the transgene into hESCs | [55] |
| Myl2-eGFP | Ectopic Myl2 promoter + human CMVehc | Ventricular-like CMs | Purification of ventricular-like CMs for cell transplantation study | mES | Random integration of the transgene into mESCs via electroporation delivery | [56] |
| MYL2-GFP φ | Ectopic MYL2 | Ventricular-like CMs | Purification of ventricular-like CMs | hiPSC | Adenoviral transduction of the transgene into hiPSCs | [57] |
| MYL2-VSFP | Ectopic MYL2 promoter-enhancer | Ventricular-like CMs | Purification of ventricular-like CMs and study of optical AP | hiPSC | Lentiviral transduction/random integration of the transgene into hiPSC | [58] |
| MYL7-GFP φ | Ectopic MYL7 | Atrial-like CMs | Identification of atrial-like CMs | hiPSC | Adenoviral transduction/random integration of the transgene into hiPSC | [57] |
| SLN-tdTomato | Endogenous SLN | Atrial-like CMs | Purification of atrial-like CMs | hiPSC | HR by electroporation of recombineered BAC DNA into hiPSCs | [59] |
| SLN-VSFP | Ectopic SLN | Atrial-like CMs | Purification of atrial-like CMs and study of optical AP | hiPSC | Lentiviral transduction/random integration of the transgene into hiPSC | [58] |
| NKX2.5-GFP/NR2F2-mCherry | Endogenous NR2F2 and NKX2.5 | Atrial-like CMs | Identification and purification of atrial-like cells and functional study of NR2F2 | hESC | CRISPR/Cas9 targeting (NR2F2-mCherry) into NKX2.5-GFP hESC reporter line [47] | [60] |
| cGATA6-eGFP | Ectopic cGATA6 promoter-enhancer | Nodal-like cells | Identification and purification of nodal-like cells and development of PSC-derived nodal cell differentiation protocol | hESC | Lentriviral transduction/ random integration of the transgene into differentiated hESC-CMs | [61] |
| SHOX2-VSFP | Ectopic SHOX2 | Nodal-like cells | Purification of nodal-like CMs and study of optical AP | hiPSC | Lentiviral transduction/random integration of the transgene into hiPSC | [58] |
| CAG-Arclight | Synthetic CAG | Ubiquitous | Overexpression of Arclight GEVI for optical AP recording in normal and pathological condition in engineered heart tissue | hiPSC | Lentiviral transduction/random integration of the transgene into healthy individual derived hiPSCs and long QT2 patient-derived hiPSCs | [62] |
| TNNT2-GCaMP5G | Ectopic TNNT2 | Beating CMs | Overexpression of GCAPMP5 GECI for optical CT recording in normal and pathological condition in engineered heart tissue | hiPSC | Lentiviral transduction/random integration of the transgene into healthy individual derived hiPSCs and catecholaminergic polymorphic ventricular tachycardia type 2 patient-derived hiPSCs | [62] |
| CaViar (CMV-Arch(D95N)-linker-GCaMP5G-WPRE) | Ectopic CMV promoter-enhancer | Ubiquitous | Overexpression of Arch(D95N) GEVI and GCaPMP5 GECI for simultaneous recordings of AP and CT | hiPSC | Lentiviral transduction/random integration of the transgene into hiPSC | [62] |
| CaViar (CMV-QuasAr2-linker-GCaMP6f-WPRE) OR CaMKIIa-Cheriff-eGFP | Ectopic CMV promoter-enhancer OR ectopic Ca2+/calmodulin-dependent protein kinase II (CaMKIIa) promoter | Ubiquitous | Overexpression of QuasAr2 GEVI and GCaMP5f GECI for simultaneous optical AP and CT recordings in combination with overexpression of optogenetic Cheriff for synchronising CM contraction | hiPSC | Lentiviral transduction/random integration of the transgene into differentiated hiPSC-CMs | [63] |
| CAG-hChR2-mCherryφ | Synthetic CAG | Ubiquitous | Transient overexpression of the optogenetic ChR2 for frequency-dependent drug screening purpose | hiPSC | Adenoviral transduction of the transgene vector into differentiated hiPSC-CMs | [64] |
| CAG-GCaMP3 OR CAG-GCaMP6s OR GAG-G-GECO1.0 | Synthetic CAG | Ubiquitous | Overexpression of a different GECI version for optimising optical CT imaging in rhesus iPSC-CMs | Rhesus iPSC | CRISPR/Cas9 editing in rhiPSC at the AAVS1 locus via plasmid-based chemical transfection | [65] |
| CMV-tri reporter | Ectopic CMV | Ubiquitous | Overexpression of luciferase (for bioluminescent cell tracking after transplantation), mRFP (purification of transduced cells) and thymidine kinase (following dividing cells and tumouriginicity) | miPSC | Lentiviral transduction/random integration of the transgene into miPSC | [66] |
¥; WPRE, Woodchuck hepatitis virus posttranscriptional regulatory element used for enhancing gene expression; EF1α, eukaryotic translation elongation factor 1 α promoter driving neomycin resistant gene expression (neo). φ; transient lines.
In a developing mammalian embryo, the earliest cardiovascular progenitors are identified in gastrulation, where cells enter epithelial-mesenchymal transition and form mesendoderm. These progenitors express a mesodermal marker T-box transcription factor brachyury (BRY) which has been used to drive a GFP fluorescent reporter. In vitro differentiation of mouse ESCs (mESCs) revealed a multipotency of canonical WNT-activated Bry-GFP+ cells. Under cardiogenesis-promoting conditions, Bry-GFP+ cells with low expression of kinase insert domain receptor (Kdrlow) exhibit cardiogenic potential whilst, Bry-GFP+, Kdrhigh populations possess haematopoietic potential [39,40].
The transition from common mesoderm towards cardiac mesoderm requires canonical WNT inhibition and non-canonical WNT activation. These intermediate cells are marked by an expression of mesoderm posterior basic helix-loop-helix transcription factor 1 (MESP1). Investigations which used a fluorescently-tagged MESP1-mCherry/ NK2 homeobox 5 (NKX2.5)-eGFP dual reporter hESCs [41] demonstrated a transient MESP1-mCherry expression followed by NKX2.5-eGFP expression. Enrichment of WNT5A, receptor tyrosine kinase-like orphan receptor 2 and frizzled class receptor 2 in MESP1-mCherry+ cells suggested roles of non-canonical WNT pathway in cardiac progenitor determination [42].
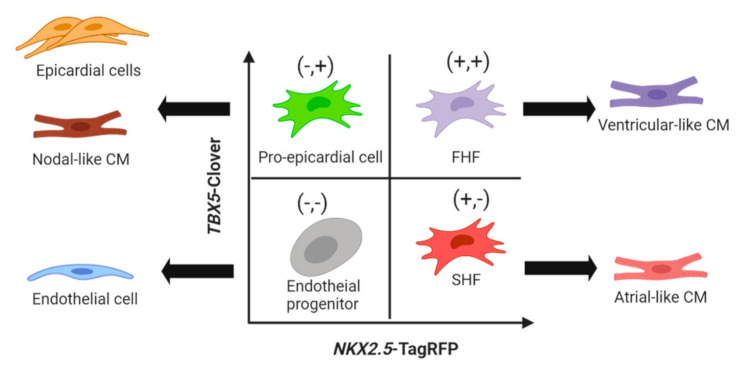
The nascent cardiac progenitors undergo another transitory stage towards more defined cardiac lineages termed the first heart field (FHF), which contributes to the left ventricle and a portion of the atria, and the second heart field (SHF), which gives rise to the right ventricle, atria, outflow tract and inflow tract [43]. In the human heart, insulin gene enhancer protein (ISL1) is a potential SHF marker [44]. A study using an ISL1-cre dsRed reporter hESC line [44] ascertained an ISL1+ multipotent status with differentiation potential for CMs, smooth muscle, endothelial and epicardial lineages. This finding may highlight a common ancestor shared between pro-epicardial progenitor and SHF CPCs since time-course analysis showed that the ISL1 expression preceded the expression of SHF markers T-box transcription factor 1 and NKX2.5. NKX2.5/ISL1 or ISL1/epicardial-specific Wilm’s tumour protein 1 dual reporter systems may be able to elucidate the diversification of ISL1+ progenitor and SHF CPCs further. More recently, CRISPR-Cas9-assisted generation of a NKX2.5-TagRFP/T-box transcription factor 5 (TBX5)-Clover dual reporter hiPSC line [45] has offered a phenotypic strategy to isolate four distinct subsets of cardiac progenitors (CPCs); presumptive FHF (NKX2.5-TagRFP+/TBX5-Clover+); presumptive SHF (the NKX2.5-TagRFP+/TBX5-Clover−); pro-epicardial cells (NKX2.5-TagRFP−/TBX5-Clover+), which diversified into nodal-like CMs and epicardial cells; and endothelial progenitors (NKX2.5-TagRFP−/TBX5-Clover−) (Figure 3).
Figure 3.
The TBX5-Clover/NKX2.5-TagRFP reporter PSC-CM line uncovers four distinct cardiac progenitor subsets [45]. The TBX5-Clover+/NKX2.5-TagRFP+ (+,+) (top right) and TBX5-Clover−/NKX2.5-TagRFP+ (+,−) (bottom right) show phenotypic features of presumptive first heart field and second heart field progenitors which give rise primarily to ventricular-like and atrial-like CMs, respectively. The TBX5-Clover+/NKX2.5-TagRFP− (+/−) population (top left) resembles epicardial precursors which can then differentiate into epicardial cell and nodal CM lineages. The TBX5-Clover−/NKX2.5-TagRFP− (−,−) population (bottom left) represents distinct endothelial lineage progenitors.
Taken together, the stage-specific fluorescent PSC-CM reporter cell lines offer an optical tracking strategy for cell identity and enable in vitro studies of cardiac development. Uniquely, hiPSC-CM reporter cells provide insights into human cardiogenesis without embryo donor requirements and without the concerns over species differences encountered with mouse models. Future multi-coloured reporter lines [46] may enable the discovery of novel cardiac progenitors, and the improvement of CM derivation and differentiation protocols.
4. Fluorescence-Guided PSC-CM Purification
Despite the refinement of in vitro cardiac induction protocols [67], PSC-CM purification is still needed to ensure sufficiently pure populations for downstream applications. Contamination by non-CM cell types, including fibroblasts, endothelial, epicardial and smooth muscle cells [45,68,69], and undifferentiated cells may hamper the detection and analysis of the actual signals from CMs. The heterogeneity of PSC-CM subtypes may also dilute the degree of pharmacological response originated from a certain subtype.
Percoll gradient centrifugation [70] allowed hES-derived CMs enrichment up to 70% from initial beating embryoid bodies, but this technique is labour-intensive and requires high numbers of large beating embryoid bodies. Metabolic selection [71] enables the elimination of non-cardiac cells that rely on the glycolytic pathway, although may be subject to biases which could lead to considerable variability in CM yield due to the metabolic immaturity of PSC-CMs [72]. Relying on the high mitochondrial content in CMs, fluorescent mitochondrial dyes offer a way in which CMs can be transiently labelled and purified by fluorescence-activated cell sorting (FACS) [73]. Nonetheless, the purification outcome will depend on the stage of PSC-CM maturity [74].
Genetically engineered reporter lines provide a robust alternative. Reporter lines carrying an antibiotic-resistant cassette under the control of cardiac-specific gene’s regulatory elements, e.g., α-myosin heavy chain (MYH6) [75,76,77,78,79,80], cardiac troponin (TNNT2) [51], NKX2.5 [68] and Na+/Ca2+ antiporter (NCX1) [53] allow effective PSC-CM purification (up to 99% purity) [75,76]. However, the consequence of antibiotic selection may adversely influence the native physiology of the cells. Prolonged drug application, e.g., puromycin and neomycin in CMs was reported to modulate Ca2+ transient (CT) reduction and action potential (AP) shortening [80,81]. Meanwhile, fluorescent reporter cell lines not only allow PSC-CM purification via FACS, but also enable real-time tracking of the cells during differentiation and maturation. As we explore below, the choice of control elements incorporated in the fluorescent reporter will vary widely depending on the target population to be distinguished.
4.1. Functional CMs
NKX2.5 is an early transcription factor in the FHF and SHF CPCs and plays supportive roles in cardiac contraction [82]. An engineered NKX2.5-GFP reporter hESC line [47] allowed efficient functional CM purification, as confirmed by electrophysiological phenotype. It is should be noted that NKX2.5 expression is also detectable in non-cardiac tissues such as the spleen, stomach and thyroid [83]; hence, exploiting multiple markers in addition to NKX2.5 may be advantageous.
Fluorescent reporter transgenes under the control of a sarcomere gene/promoter offer a more cardiac-specific cell labelling. Isolated fluorescent MYH6-GFP+[48,49] or MYH6-mCherry+ [50] hPSC-CMs expressed pan-cardiac markers while each cell displayed functional phenotypes representing atrial, ventricular or nodal CMs. Importantly, as CMs mature, the cells undergo sarcomere reorganisation, including myosin heavy chain α-to-β isoform switching in human or β-to-α switching in mouse [84,85,86]. Therefore, MYH6 reporter systems are better suited for the isolation of early committed human CMs and vice versa for mouse CMs. The ability of sarcomere-specific reporters to aid in isolation of beating CMs was also recently reported for a number of key genes: α-cardiac actin (ACTC)-mCherry [51], TNNT2-firefly luciferase /puromycin resistance [51] and titin (TTN)-GFP hPSC lines [52]. In addition to the CM purification utility, the fluorescent N-terminal tagging of endogenous titin facilitated observation of the sarcomere dynamics in a cardiomyopathy condition [87].
NCX1 plays essential roles in intracellular Ca2+ flux and excitation-contraction coupling [54]. An NCX1-eGFP hPSC reporter line [53] offered an optical selection method for functional PSC-CMs. Although the fluorescent signals preceded the contractile activity, the sorted NCX1-eGFP+ cells displayed both molecular and functional characteristics of typical hPSC-CMs.
Irrespective of the pan-cardiac promoter used in these reporter systems, FACS purification yielded a mixture of atrial, ventricular and nodal CM subtypes. These reporter lines benefit cardiotoxic screening and developmental studies, but the heterogeneous nature of the cell population complicates chamber-specific drug discovery, disease modelling and therapeutic applications. Each subtype exhibits unique physiological characteristics [88], leading to different drug responses. Similarly, some pathological conditions, e.g., atrial fibrillation, develop within specific heart regions, thus purified CM subtypes serves as a more precise disease model [89]. Furthermore, subtype mismatching or mislocation may exert adverse effects in cardiac cell therapy, such as pro-arrhythmia. Therefore, CM subtype selection is necessary to overcome these limitations.
4.2. Ventricular CM
Myosin light chain 2 (MYL2), is the most attractive ventricular marker with an expression restricted to ventricular compartments throughout mammalian development [85,90]. Success in ventricular-like CMs enrichment by FACS has been reported in several fluorescent MYL2 PSC-CM reporter lines [54,55,56,57,58], each of which was verified by molecular and/or electrophysiological phenotype. It is noteworthy that MYL2 is considered a late cardiac gene, where its expression level increases consistently with the stage of CM maturation, with the upregulation seen being more pronounced than other maturation factors, such as β myosin heavy chain [91]. Therefore, the selection of a suitable time point for sorting MYL2-FP+ cells is important to optimise the yield of ventricular-like cells.
4.3. Atrial CM
The selection of atrial-like cells is more challenging owing to the lack of a reliable genetic marker. Myosin light chain 7 (MYL7) is ubiquitously expressed within the primitive heart tube and only becomes confined to atrial compartments at later developmental stages [92]. Analysis of a transient MYL7-GFP hiPSC-CMs identified co-expression of MYL2 and MYL7 in 96% of the MYL7-GFP+ fraction [57], perhaps underscoring the foetal nature of PSC-CMs. Nevertheless, stable reporter lines, especially those established by gene targeting approaches, may behave differently.
During mammalian heart development, sarcolipin (SLN) expression is confined to atrial lineages [93]. Electrophysiological measurements revealed atrial characteristics of sorted SLN-tdTomato+ hiPSC-CMs [59], highlighting SLN as an alternative atrial marker. Following this report, an SLN-driven voltage-sensitive fluorescent protein (SLN-VSFP) hiPSC reporter line was generated [58], which allowed FACS isolation of atrial-like CMs coupled with the functional study of the sorted cells by optical AP imaging. However, the temporal concern of SLN-based atrial cell purification has been emphasised due to the downregulation of the gene as the cells become more mature [59].
Evidence from a gene knockdown in hiPSC-CMs, supported by human tissue analysis, suggested nuclear receptor NR2F1/2 as being important players in retinoic acid-induced atrialisation [94]. This was exploited with an NKX2.5-GFP/NR2F2-mCherry hESC dual reporter system, enabling two chamber-type CMs to be distinguished [60]. Molecular and electrophysiological analysis of NKX2.5-GFP+/NR2F2-mCherry+ confirmed an atrial phenotype while NKX2.5-GFP+/NR2F2-mCherry- cells showed more ventricular characteristics.
4.4. Nodal CM
PSC-derived nodal-like CM enrichment is demanding due to this subtype being a relatively minor population under WNT-modulated differentiation procedures [95]. Investigations in transgenic mice found chick GATA6 (cGATA6) enhancer activity restricted to the atrioventricular conduction system [96]. An engineered cGATA6-eGFP hESC reporter line [61] enabled FACS enrichment of non-working CMs (95% purity) with expected nodal type APs and expression of nodal-specific hyperpolisation-activated cyclic nucleotide-gated K+ channel 4 (HCN4).
A transgenic short stature homeobox 2 (SHOX2)-VSFP hiPSC line [58] offered an alternative genetic selection of nodal-like cell isolation, as confirmed by high expression of HCN4 and nodal-type AP. SHOX2 promotes the transcription of HCN4 [97], the key channel responsible for the pacemaker-specific funny current. The transient expression of exogenous SHOX2 was sufficient to induce endogenous SHOX2 expression and steered the differentiation of ESCs towards the nodal lineage [98].
In summary, fluorescent PSC-CM reporter systems facilitate optical CM identification and, depending on the cardiac-specific control element used, isolation of sub-populations from the pool of PSC-derived cells. Exploiting pan-cardiac promoters allows purification of mixed atrial, ventricular and nodal CMs while avoiding non-CMs contamination, providing a source for in vitro cardiotoxic screening and developmental studies. Meanwhile, each CM subtype can be optically selected using subtype-specific fluorescent PSC-CMs reporter lines. The development of CM subtype purification techniques holds great promise for CM subtype-selective drug discovery, subtype-specific disease modelling and scalable subtype-specific CM production that future cardiac regeneration therapies may demand.
5. Applications towards Optical Measurements of Cardiac Functions
Electrophysiological measurements are not only a reliable strategy to identify individual CM subtypes, they also allow investigation of either genetically inherited or acquired functional cardiac defects. Patch-clamp electrophysiology is the gold standard AP recording technique [99], but it is labour-intensive and low throughput. Intracellular Ca2+ level coordinates CM excitability and contraction. Membrane depolarisation causes Ca2+ influx through the L-type voltage-gated Ca2+ channel, in addition to NCX1 activity [54], which triggers Ca2+-induced Ca2+ release from the sarcoplasmic reticulum, thereby activating the contraction [100]. Although the use of fluorescent Ca2+ dyes (such as Fura2/4) for CT measurement is common, these chemicals are known to suppress cardiac functions [101] and prevent long-term studies of pharmacological effects [102]. Genetically encoded voltage and Ca2+ reporters are being explored as we outline below.
5.1. Genetically Encoded Fluorescent Voltage-Sensitive and Ca2+ Indicators
The development of genetically encoded fluorescent voltage-sensitive indicators (GEVIs) has opened a new window for electrophysiological studies. Arclight is a synthetic protein containing a voltage-sensing domain from Ciona intestinalis and a super ecliptic pH-sensitive GFP variant (pHluorin A227D) [103,104]. Randomly integrating a CAG-Arclight transgene into hiPSC-CMs enabled the ubiquitous expression of the GEVI driven by a synthetic CAG control element [105]. The fluorescence pattern observed in these cells was comparable to the AP recording using fluorescent Di-8-ANEPPS dye and even recapitulated drug-induced and genetically-caused AP prolongation and arrhythmias (long QT2 syndrome) [62,106]. Furthermore, the Arclight reporter showed improved signal-to-noise ratios and was less affected by photobleaching than conventional dyes. To facilitate simultaneous subtype identification and electrophysiological studies, a GEVI can be directed by a CM subtype-specific promoter. As an alternative, VSFP-based GEVIs [58] rely on Förster resonance energy transfer (FRET) [107] to track oscillations of membrane potential causing conformational changes of two attached tandem FPs, resulting in the dynamic rise and fall of the fluorescent intensity of FRET donor and FRET receptor. The ratiometric readout of VSFPs, compared to the single fluorescent unit used in the Arclight system, provides a more stable AP pattern, unaffected by movement artefacts and photobleaching.
Several versions of genetically encoded fluorescent Ca2+ indicators (GECIs) have been engineered and tested in PSC-CMs [62,63,65,106]. GECIs contains three major components: a Ca2+-modulating protein (CaM), a CaM-interacting peptide, e.g., myosin light chain kinase-derived M13 and a circularly permuted GFP [108]. Following Ca2+-induced Ca2+ release, cytosolic Ca2+ binds to CaM which promotes the formation of Ca2+-CaM-M13, resulting in increased fluorescence [109]. Similar to GEVIs, the key advantage of GECIs over traditional fluorescent Ca2+ dyes is the stable expression of the transgene, facilitating observations of the chronic effects of pharmacological molecules, and non-cytotoxic properties [63]. The fidelity of GECI reporter systems is comparable to fluorescent dyes, with abilities to elucidate drug-induced changes in beat rate and beat interval. Furthermore, such genetic reporters have been used to model inherited arrhythmic disorders such as catecholaminergic polymorphic ventricular tachycardia type 2 [62,106].
5.2. Optogenetics
The field of optogenetics has captured interest in neurophysiology because of the ability to track spatiotemporal activation of neurons [110]. Upon blue light illumination, the Chlamydomonas reinhardtii-derived channelrhodopsin 2 protein (ChR2) mediates inward cation currents [111], resulting in membrane depolarisation. In the PSC-CMs field, optogenetics enables light-triggered synchronisation of beating CM patches and promotes CM maturation [112]. Differentiated PSC-CMs contract spontaneously but largely non-uniformly, potentially resulting in AP and CT variance. Instead of using an invasive electrical impulse, CAG-humanised ChR2 (hChR2)-mCherry reporter hiPSC-CMs could be optically paced at different beat rates [64], offering an in vitro model to study rate-sensitive conditions, e.g., long QT1 [113]. Furthermore, a combination of the optogenetics technology with GECIs and/or GEVIs [63] allows an all-optical detection for high throughput drug screening purposes.
6. Emerging Insights into Cardiac Tissue Repair
The adult human heart has limited regenerative capacity to self-repair [114]. hiPSC-CMs have been proposed as a promising approach for immunocompetent cardiac cell therapy. As a vision for future treatment, somatic cells, e.g., skin fibroblasts or blood cells, could be extracted from a patient and reprogrammed into iPSCs. In vitro cardiac differentiation of these cells would yield an autologous CM source, allowing reintroduction without immune-rejection [115]. Nonetheless, the immature nature of the potential hiPSC-CM graft raises concerns over clinical safety [112,116].
The proliferative capacity of stem cells is desirable for cardiac regeneration to compensate for the massive cell loss seen following transplantation [117]. However, subcutaneous injection of purified mouse iPSCs (miPSCs) ubiquitously expressing a tri-reporter into mice suggested a significant tumourigenic potential by bioluminescent signal, as compared to miPSC-CMs [66]. This indicates that iPSC-derived CPCs may be a safer source of cells for cardiac repair [118]. In support, biopsy analysis of the pre-infarcted mouse heart intramyocardially transplanted with purified Nkx2.5-GFP+ miPSCs confirmed the cardiac differentiation potential of the CPCs without teratoma formation [119]. Future multi-coloured reporter CPC lines will offer a wide variety of transplants customisable to specific impaired region.
Host-graft adaptation is another concern for cardiac cell therapy. Importantly, fluorescent PSC-CM reporters provide not only a tool for tracking the cell fate after transplantation but also provide information about graft–host structural and functional integration. Histological analysis of rat heart pre-intramyocardially injected with MYL2-eGFP+ hPSC-CMs revealed signs of morphological maturation and connexin 43 (CX43) expression at the host–graft interface [55]. Since CX43 is a major ventricular gap junction protein that plays an integral role in the excitation–contraction coupling [120], the presence of the donor CX43 at the donor–recipient cell interface may be indirectly indicative of functional adaptation of the graft.
Notwithstanding, the immaturity of hPSC-CMs still represents a challenge for cardiac cell therapy. New methodologies focused on promoting more adult phenotypes are needed to ensure clinical safety and maximize therapeutic benefit.
7. Maturation Approaches
Several techniques have been developed to improve iPSC-CM maturity including biochemical, physical and environmental stimulation [121]. Modulating pathways promoting CM differentiation improves adult CM phenotypes. For example, insulin-like growth factor/AKT1 supplementation supports the expression of CM markers and enhances intracellular Ca2+ fluxes and β-adrenergic response [122]. Similarly, thyroid hormone increases hiPSC-CM contractile force, Ca2+ cycling and mitochondrial respiratory capacity while promoting sarcomere organisation [123].
Unlike PSC-CMs, primary adult atrial and ventricular CMs do not beat spontaneously, but require an electrical signal from nodal CMs. Mimicking the in vivo situation, extrinsic electrical or optical (for optogenetics) impulses not only help to pace cultured CMs but also exert positive effects on the ultrastructural organisation and functional properties [124,125].
Extracellular matrix stiffness changes dramatically during cardiac development and has an impact on the mechanical force experienced by CMs [126]. 3-dimentional (3D) culture provides closer phenotypes to native CMs than conventional 2-dimentional culture, facilitating in vivo topology that supports cell–cell interactions and exposure to biochemical and physical factors. Advances in the fields of biomaterial [127] and 3D PSC-CM culture present an opportunity to attain more mature PSC-CMs. Engineered heart tissue [128] and cardiac microtissue [129] are generated by casting a cell–hydrogel mixture in moulds tethered to elastic anchors. The mechanical force applied on the anchors (or a passive stretcher for ring-shaped engineered heart tissues [130]) can be varied to simulate physiological/pathophysiological conditions.
Combinations of 3D hiPSC-CMs with biochemical [106] or electrical [131] administrations promote adult phenotypes and enhance electrophysiological properties and contraction [132]. The presence of non-CMs such as fibroblasts [69,133], endothelial [133] and epicardial cells [134] also elicits favourable consequences on PSC-CM differentiation and maturation in 3D format. GECIs [62], GEVIs [62] and optogentics [135] have been applied to 3D hiPSC-CM culture recently, which allow optical measurements of electrophysiology in normal and drug-induced or inherited diseased models. Meanwhile, a fluorescent reporter that is tagged to a maturation marker, e.g., CX43 [85] may be beneficial to follow the maturation of implants. Similarly, the transduction of GECI and GEVI into PSC-CMs would allow in vivo studies for functional adaption/maturation of the graft.
8. Conclusions
The indefinite source of PSC-CMs has the potential to provide scalable CM production for cardiovascular research. However, immature and embryonic-like phenotypes as well as the heterogeneous nature of PCS-CMs present challenges for their use in drug discovery, disease modelling and transplantation. Stage-specific fluorescent PSC-CM lines generated by different transgenic methods have helped researchers monitor cardiac development and improved in vitro differentiation protocols. The discovery of additional CM maturation-promoting pathways will require multi-coloured reporter systems in combination with advances in 3D PSC-CM culture.
CM surface markers are largely unknown and thus FACS-mediated PSC-CMs sorting by fluorescent markers provide a genetic-based solution for specific cell-type isolation. Purified fluorescent PSC-derived CPCs have been successfully differentiated into functional CMs in vivo, devoid of tumorigenic risk, promising clinical safety for cardiac regeneration. Novel fluorescent PSC reporter lines will help identify the various CPCs that give rise to unique cell-type compositions specifically required for treating different pathological conditions. Furthermore, the isolation of subtype-specific PSC-CMs will enable subtype-specific cardiogenic drug discovery and disease modelling. Unlike nodal and ventricular types, the atrial PSC-CM markers are not fully characterised. Further insights from novel fluorescent atrial PSC-CM reporter lines, such as PITX2 and KCNA5, in combination with atrial-promoting differentiation approaches including retinoic acid treatment and CRISPRa/CRISPRi-mediated transcriptional activation/inhibition of atrial-regulating pathways [136,137], could assist the development of atrial cell isolation protocols.
Lastly, optogenetics is an emerging biotechnology that has recently been applied in PSC-CMs for spatiotemporal CM activation and maturation. The combination of optogenetics with fluorescent physiological reporters allows an all-optical measurement of CM function that benefits high throughput drug screening. We look forward to seeing the implementation of combined optogenetics and physiological sensors with minimised optical crosstalk in cell transplantation, which will allow PSC-CM graft performance to be followed in vivo.
Acknowledgments
We thank Lisa Leinhos for fruitful discussions. All figures in this review were created with Biorender.com.
Abbreviations
| 3D | 3-dimentional |
| ACTC | α-cardiac actin |
| AP | action potential |
| BAC | bacterial artificial chromosome |
| BRY | T-box transcription factor brachyury |
| CaM | Ca2+-modulating protein |
| cGATA6 | chick GATA6 |
| ChR2 | channelrhodopsin 2 |
| CMs | cardiomyocytes |
| CPCs | cardiac progenitor cells |
| CRISPR/Cas9 | clustered regularly interspaced short palindromic repeat (CRISPR)/CRISPR associated protein 9 (Cas9) |
| CT | Ca2+ transient |
| CX43 | connexin 43 |
| DSB | double strand break |
| ESCs | embryonic stem cells |
| FACS | fluorescence-activated cell sorting |
| FHF | first heart field |
| FP | fluorescent protein |
| GECIs | genetically encoded Ca2+ indicator |
| GEVIs | genetically encoded voltage-sensitive indicators |
| GOI | gene of interest |
| HCN4 | hyperpolisation-activated cyclic nucleotide gated K+ channel 4 |
| hESC-CMs | human embryonic stem cell-derived cardiomyocytes |
| hESCs | human embryonic stem cells |
| hiPSC-CMs | human induced pluripotent stem cell-derived cardiomyocytes |
| hiPSCs | human induced pluripotent stem cells |
| hPSC-CMs | human pluripotent stem cell-derived cardiomyocytes |
| HR | homologous recombination |
| iPSCs | induced pluripotent stem cells |
| IRES | internal ribosomal entry sites |
| ISL1 | insulin gene enhancer protein |
| Kdr | kinase insert domain receptor |
| mESCs | mouse embryonic stem cells |
| MESP1 | mesoderm posterior basic helix-loop-helix transcription factor 1 |
| miPSC-CMs | mouse induced pluripotent stem cell-derived cardiomyocytes |
| miPSCs | mouse induced pluripotent stem cells |
| MYH6 | α-myosin heavy chain |
| MYL2 | myosin light chain 2 |
| MYL7 | myosin light chain 7 |
| NCX1 | Na+/Ca2+ antiporter |
| NKX2.5 | NK2 homeobox 5 |
| P2A | porcine teschovirus-1 2A |
| PSCs | pluripotent stem cells |
| RMCE | recombination-mediated cassette exchange |
| SHF | second heart field |
| SHOX2 | short stature homeobox 2 |
| SHS | safe harbour site |
| SLN | sarcolipin |
| T2A | Thosea asigna virus 2A |
| TALENs | transcription activator-like effector nucleases |
| TBX5 | T-box transcription factor 5 |
| TNNT | cardiac troponin |
| TTN | titin |
| VSFP | voltage sensitive fluorescent protein |
| ZFNs | zinc finger nucleases |
Author Contributions
Writing–original draft preparation, N.S.; writing–review and editing and supervision, C.R., B.D. and K.G. All authors have read and agreed to the published version of the manuscript.
Funding
The authors acknowledge support by the BHF Centre of Research Excellence Oxford [RE/18/3/34214]. N.S. is funded by the Royal Thai Government Scholarship. Work in K.G.’s lab is funded by the British Heart Foundation (BHF) (FS/12/40/29712), the Wellcome Trust (201543/B/16/Z) and the National Centre for Replacement, Refinement and Reduction of Animals in Research (NC3R, NC/T001747/1). Work in C.R.’s laboratory is funded by the British Heart Foundation (PG/18/68/33883, RG/18/9/33887). B.D. is funded by the Wellcome Trust (203141/Z/16/Z).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Penney J., Ralvenius W.T., Tsai L.H. Modeling Alzheimer’s disease with iPSC-derived brain cells. Mol. Psychiatry. 2020;25:148–167. doi: 10.1038/s41380-019-0468-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corbett J.L., Duncan S.A. iPSC-derived hepatocytes as a platform for disease modeling and drug discovery. Front. Med. 2019;6:265. doi: 10.3389/fmed.2019.00265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prajumwongs P., Weeranantanapan O., Jaroonwitchawan T., Noisa P. Human Embryonic Stem Cells: A Model for the Study of Neural Development and Neurological Diseases. Stem Cells Int. 2016;2016:2958210. doi: 10.1155/2016/2958210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu C., Oikonomopoulos A., Sayed N., Wu J.C. Modeling human diseases with induced pluripotent stem cells: From 2D to 3D and beyond. Development. 2018;145:dev156166. doi: 10.1242/dev.156166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Passier R., Orlova V., Mummery C. Complex tissue and disease modeling using hiPSCs. Cell Stem Cell. 2016;18:309–321. doi: 10.1016/j.stem.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 6.Le Bras A. A resource for selecting animal models of heart disease. Lab Anim. 2019;48:332. doi: 10.1038/s41684-019-0425-4. [DOI] [Google Scholar]
- 7.Camacho P., Fan H., Liu Z., He J.Q. Large Mammalian Animal Models of Heart Disease. J. Cardiovasc. Dev. Dis. 2016;3:30. doi: 10.3390/jcdd3040030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perlman R.L. Mouse models of human diseaseAn evolutionary perspective. Evol. Med. Public Health. 2016;2016:170–176. doi: 10.1093/emph/eow014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barre-Sinoussi F., Montagutelli X. Animal models are essential to biological research: Issues and perspectives. Future Sci. OA. 2015;1 doi: 10.4155/fso.15.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robertson J.A. Human embryonic stem cell research: Ethical and legal issues. Nat. Rev. Genet. 2001;2:74–78. doi: 10.1038/35047594. [DOI] [PubMed] [Google Scholar]
- 11.Takahashi K., Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 12.Ohnuki M., Takahashi K. Present and future challenges of induced pluripotent stem cells. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2015;370:20140367. doi: 10.1098/rstb.2014.0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bilic J., Belmonte J.C.I. Concise review: Induced pluripotent stem cells versus embryonic stem cells: Close enough or yet too far apart? Stem Cells. 2012;30:33–41. doi: 10.1002/stem.700. [DOI] [PubMed] [Google Scholar]
- 14.Bilousova G., Roop D.R. Induced pluripotent stem cells in dermatology: Potentials, advances, and limitations. Cold Spring Harb. Perspect. Med. 2014;4:a015164. doi: 10.1101/cshperspect.a015164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoshihara M., Hayashizaki Y., Murakawa Y. Genomic instability of iPSCs: Challenges towards their clinical applications. Stem Cell Rev. Rep. 2017;13:7–16. doi: 10.1007/s12015-016-9680-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen N., Nguyen W., Nguyenton B., Ratchada P., Page G., Miller P.E., Ghetti A., Abi-Gerges N. Adult Human Primary Cardiomyocyte-Based Model for the Simultaneous Prediction of Drug-Induced Inotropic and Pro-arrhythmia Risk. Front. Physiol. 2017;8:1073. doi: 10.3389/fphys.2017.01073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abi-Gerges N., Indersmitten T., Truong K., Nguyen W., Ratchada P., Nguyen N., Page G., Miller P.E., Ghetti A. Multiparametric Mechanistic Profiling of Inotropic Drugs in Adult Human Primary Cardiomyocytes. Sci. Rep. 2020;10:7692. doi: 10.1038/s41598-020-64657-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang J.Z., Guo H., Wu J.C. Applications of genetically engineered human pluripotent stem cell reporters in cardiac stem cell biology. Curr. Opin. Biotechnol. 2018;52:66–73. doi: 10.1016/j.copbio.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nayerossadat N., Maedeh T., Ali P.A. Viral and nonviral delivery systems for gene delivery. Adv. Biomed. Res. 2012;1:27. doi: 10.4103/2277-9175.98152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Den Hartogh S.C., Passier R.J.S.C. Concise review: Fluorescent reporters in human pluripotent stem cells: Contributions to cardiac differentiation and their applications in cardiac disease and toxicity. Stem Cells. 2016;34:13–26. doi: 10.1002/stem.2196. [DOI] [PubMed] [Google Scholar]
- 21.Smith J.R., Maguire S., Davis L.A., Alexander M., Yang F., Chandran S., Ffrench-Constant C., Pedersen R.A. Robust, persistent transgene expression in human embryonic stem cells is achieved with AAVS1-targeted integration. Stem Cells. 2008;26:496–504. doi: 10.1634/stemcells.2007-0039. [DOI] [PubMed] [Google Scholar]
- 22.Wilson C., Bellen H.J., Gehring W.J. Position effects on eukaryotic gene expression. Annu. Rev. Cell Biol. 1990;6:679–714. doi: 10.1146/annurev.cb.06.110190.003335. [DOI] [PubMed] [Google Scholar]
- 23.Klatt D., Cheng E., Hoffmann D., Santilli G., Thrasher A.J., Brendel C., Schambach A. Differential Transgene Silencing of Myeloid-Specific Promoters in the AAVS1 Safe Harbor Locus of Induced Pluripotent Stem Cell-Derived Myeloid Cells. Hum. Gene Ther. 2020;31:199–210. doi: 10.1089/hum.2019.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Calero-Nieto F.J., Bert A.G., Cockerill P.N. Transcription-dependent silencing of inducible convergent transgenes in transgenic mice. Epigenetics Chromatin. 2010;3:3. doi: 10.1186/1756-8935-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosenqvist N., Jakobsson J., Lundberg C. Inhibition of chromatin condensation prevents transgene silencing in a neural progenitor cell line transplanted to the rat brain. Cell Transpl. 2005;14:129–138. doi: 10.3727/000000005783983188. [DOI] [PubMed] [Google Scholar]
- 26.Sung P., Klein H. Mechanism of homologous recombination: Mediators and helicases take on regulatory functions. Nat. Rev. Mol. Cell Biol. 2006;7:739–750. doi: 10.1038/nrm2008. [DOI] [PubMed] [Google Scholar]
- 27.Leavitt A.D., Hamlett I. Homologous recombination in human embryonic stem cells: A tool for advancing cell therapy and understanding and treating human disease. Clin. Transl. Sci. 2011;4:298–305. doi: 10.1111/j.1752-8062.2011.00281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim H., Kim J.S. A guide to genome engineering with programmable nucleases. Nat. Rev. Genet. 2014;15:321–334. doi: 10.1038/nrg3686. [DOI] [PubMed] [Google Scholar]
- 29.Rouet P., Smih F., Jasin M. Introduction of double-strand breaks into the genome of mouse cells by expression of a rare-cutting endonuclease. Mol. Cell. Biol. 1994;14:8096–8106. doi: 10.1128/MCB.14.12.8096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oceguera-Yanez F., Kim S.-I., Matsumoto T., Tan G.W., Xiang L., Hatani T., Kondo T., Ikeya M., Yoshida Y., Inoue H. Engineering the AAVS1 locus for consistent and scalable transgene expression in human iPSCs and their differentiated derivatives. Methods. 2016;101:43–55. doi: 10.1016/j.ymeth.2015.12.012. [DOI] [PubMed] [Google Scholar]
- 31.Irion S., Luche H., Gadue P., Fehling H.J., Kennedy M., Keller G. Identification and targeting of the ROSA26 locus in human embryonic stem cells. Nat. Biotechnol. 2007;25:1477–1482. doi: 10.1038/nbt1362. [DOI] [PubMed] [Google Scholar]
- 32.Papapetrou E.P., Schambach A.J.M.T. Gene insertion into genomic safe harbors for human gene therapy. Mol. Ther. 2016;24:678–684. doi: 10.1038/mt.2016.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Turan S., Galla M., Ernst E., Qiao J., Voelkel C., Schiedlmeier B., Zehe C., Bode J. Recombinase-mediated cassette exchange (RMCE): Traditional concepts and current challenges. J. Mol. Biol. 2011;407:193–221. doi: 10.1016/j.jmb.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 34.Pei Y., Sierra G., Sivapatham R., Swistowski A., Rao M.S., Zeng X. A platform for rapid generation of single and multiplexed reporters in human iPSC lines. Sci. Rep. 2015;5:9205. doi: 10.1038/srep09205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu Z., Chen O., Wall J.B.J., Zheng M., Zhou Y., Wang L., Vaseghi H.R., Qian L., Liu J. Systematic comparison of 2A peptides for cloning multi-genes in a polycistronic vector. Sci. Rep. 2017;7:2193. doi: 10.1038/s41598-017-02460-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Komar A.A., Hatzoglou M. Cellular IRES-mediated translation: The war of ITAFs in pathophysiological states. Cell Cycle. 2011;10:229–240. doi: 10.4161/cc.10.2.14472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Szymczak A.L., Vignali D.A. Development of 2A peptide-based strategies in the design of multicistronic vectors. Expert Opin. Biol. Ther. 2005;5:627–638. doi: 10.1517/14712598.5.5.627. [DOI] [PubMed] [Google Scholar]
- 38.Naito A.T., Shiojima I., Akazawa H., Hidaka K., Morisaki T., Kikuchi A., Komuro I. Developmental stage-specific biphasic roles of Wnt/beta-catenin signaling in cardiomyogenesis and hematopoiesis. Proc. Natl. Acad. Sci. USA. 2006;103:19812–19817. doi: 10.1073/pnas.0605768103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kouskoff V., Lacaud G., Schwantz S., Fehling H.J., Keller G. Sequential development of hematopoietic and cardiac mesoderm during embryonic stem cell differentiation. Proc. Natl. Acad. Sci. USA. 2005;102:13170–13175. doi: 10.1073/pnas.0501672102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fehling H.J., Lacaud G., Kubo A., Kennedy M., Robertson S., Keller G., Kouskoff V. Tracking mesoderm induction and its specification to the hemangioblast during embryonic stem cell differentiation. Development. 2003;130:4217–4227. doi: 10.1242/dev.00589. [DOI] [PubMed] [Google Scholar]
- 41.Den Hartogh S.C., Schreurs C., Monshouwer-Kloots J.J., Davis R.P., Elliott D.A., Mummery C.L., Passier R. Dual reporter mesp1mcherry/w-nkx2-5egfp/w hescs enable studying early human cardiac differentiation. Stem Cells. 2015;33:56–67. doi: 10.1002/stem.1842. [DOI] [PubMed] [Google Scholar]
- 42.Chiapparo G., Lin X., Lescroart F., Chabab S., Paulissen C., Pitisci L., Bondue A., Blanpain C. Mesp1 controls the speed, polarity, and directionality of cardiovascular progenitor migration. J. Cell Biol. 2016;213:463–477. doi: 10.1083/jcb.201505082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang J.Z., Termglinchan V., Shao N.Y., Itzhaki I., Liu C., Ma N., Tian L., Wang V.Y., Chang A.C.Y., Guo H., et al. A Human iPSC Double-Reporter System Enables Purification of Cardiac Lineage Subpopulations with Distinct Function and Drug Response Profiles. Cell Stem Cell. 2019;24:802–811.e5. doi: 10.1016/j.stem.2019.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Meilhac S.M., Buckingham M.E. The deployment of cell lineages that form the mammalian heart. Nat. Rev. Cardiol. 2018;15:705–724. doi: 10.1038/s41569-018-0086-9. [DOI] [PubMed] [Google Scholar]
- 45.Bu L., Jiang X., Martin-Puig S., Caron L., Zhu S., Shao Y., Roberts D.J., Huang P.L., Domian I.J., Chien K.R. Human ISL1 heart progenitors generate diverse multipotent cardiovascular cell lineages. Nature. 2009;460:113–117. doi: 10.1038/nature08191. [DOI] [PubMed] [Google Scholar]
- 46.El-Nachef D., Shi K., Beussman K.M., Martinez R., Regier M.C., Everett G.W., Murry C.E., Stevens K.R., Young J.E., Sniadecki N.J. A Rainbow Reporter Tracks Single Cells and Reveals Heterogeneous Cellular Dynamics among Pluripotent Stem Cells and Their Differentiated Derivatives. Stem Cell Rep. 2020;15:226–241. doi: 10.1016/j.stemcr.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Elliott D.A., Braam S.R., Koutsis K., Ng E.S., Jenny R., Lagerqvist E.L., Biben C., Hatzistavrou T., Hirst C.E., Yu Q.C., et al. NKX2-5(eGFP/w) hESCs for isolation of human cardiac progenitors and cardiomyocytes. Nat. Methods. 2011;8:1037–1040. doi: 10.1038/nmeth.1740. [DOI] [PubMed] [Google Scholar]
- 48.Moon S.H., Ban K., Kim C., Kim S.S., Byun J., Song M.K., Park I.H., Yu S.P., Yoon Y.S. Development of a novel two-dimensional directed differentiation system for generation of cardiomyocytes from human pluripotent stem cells. Int. J. Cardiol. 2013;168:41–52. doi: 10.1016/j.ijcard.2012.09.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ritner C., Wong S.S., King F.W., Mihardja S.S., Liszewski W., Erle D.J., Lee R.J., Bernstein H.S. An engineered cardiac reporter cell line identifies human embryonic stem cell-derived myocardial precursors. PLoS ONE. 2011;6:e16004. doi: 10.1371/journal.pone.0016004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tsai S.-Y., Ghazizadeh Z., Wang H.-J., Amin S., Ortega F.A., Badieyan Z.S., Hsu Z.-T., Gordillo M., Kumar R., Christini D.J. A human embryonic stem cell reporter line for monitoring chemical-induced cardiotoxicity. Cardiovasc. Res. 2020;116:658–670. doi: 10.1093/cvr/cvz148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Katarzyna F., Natalia R., Agnieszka Z., Agnieszka M., Katarzyna T., Izabela S., Karolina N.-B., Magdalena N., Kolanowski T.J., Wojciech Ł. Tissue-specific promoter-based reporter system for monitoring cell differentiation from iPSCs to cardiomyocytes. Sci. Rep. 2020;10:1895. doi: 10.1038/s41598-020-58050-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sharma A., Toepfer C.N., Schmid M., Garfinkel A.C., Seidman C.E. Differentiation and Contractile Analysis of GFP-Sarcomere Reporter hiPSC-Cardiomyocytes. Curr. Protoc. Hum. Genet. 2018;96:21.12.1–21.12.12. doi: 10.1002/cphg.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ovchinnikov D.A., Hidalgo A., Yang S.-K., Zhang X., Hudson J., Mazzone S.B., Chen C., Cooper-White J.J., Wolvetang E.J. Isolation of contractile cardiomyocytes from human pluripotent stem-cell-derived cardiomyogenic cultures using a human NCX1-EGFP reporter. Stem Cells Dev. 2015;24:11–20. doi: 10.1089/scd.2014.0195. [DOI] [PubMed] [Google Scholar]
- 54.Fu J.-D., Jiang P., Rushing S., Liu J., Chiamvimonvat N., Li R.A. Na+/Ca2+ exchanger is a determinant of excitation–contraction coupling in human embryonic stem cell–derived ventricular cardiomyocytes. Stem Cells Dev. 2010;19:773–782. doi: 10.1089/scd.2009.0184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Huber I., Itzhaki I., Caspi O., Arbel G., Tzukerman M., Gepstein A., Habib M., Yankelson L., Kehat I., Gepstein L. Identification and selection of cardiomyocytes during human embryonic stem cell differentiation. FASEB J. 2007;21:2551–2563. doi: 10.1096/fj.05-5711com. [DOI] [PubMed] [Google Scholar]
- 56.Muller M., Fleischmann B.K., Selbert S., Ji G.J., Endl E., Middeler G., Muller O.J., Schlenke P., Frese S., Wobus A.M., et al. Selection of ventricular-like cardiomyocytes from ES cells in vitro. FASEB J. 2000;14:2540–2548. doi: 10.1096/fj.00-0002com. [DOI] [PubMed] [Google Scholar]
- 57.Bizy A., Guerrero-Serna G., Hu B., Ponce-Balbuena D., Willis B.C., Zarzoso M., Ramirez R.J., Sener M.F., Mundada L.V., Klos M., et al. Myosin light chain 2-based selection of human iPSC-derived early ventricular cardiac myocytes. Stem Cell Res. 2013;11:1335–1347. doi: 10.1016/j.scr.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen Z., Xian W., Bellin M., Dorn T., Tian Q., Goedel A., Dreizehnter L., Schneider C.M., Ward-van Oostwaard D., Ng J.K.M., et al. Subtype-specific promoter-driven action potential imaging for precise disease modelling and drug testing in hiPSC-derived cardiomyocytes. Eur. Heart J. 2016;38:292–301. doi: 10.1093/eurheartj/ehw189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Josowitz R., Lu J., Falce C., D’Souza S.L., Wu M., Cohen N., Dubois N.C., Zhao Y., Sobie E.A., Fishman G.I., et al. Identification and purification of human induced pluripotent stem cell-derived atrial-like cardiomyocytes based on sarcolipin expression. PLoS ONE. 2014;9:e101316. doi: 10.1371/journal.pone.0101316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schwach V., Verkerk A.O., Mol M., Monshouwer-Kloots J.J., Devalla H.D., Orlova V.V., Anastassiadis K., Mummery C.L., Davis R.P., Passier R. A COUP-TFII Human Embryonic Stem Cell Reporter Line to Identify and Select Atrial Cardiomyocytes. Stem Cell Rep. 2017;9:1765–1779. doi: 10.1016/j.stemcr.2017.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhu W.Z., Xie Y., Moyes K.W., Gold J.D., Askari B., Laflamme M.A. Neuregulin/ErbB signaling regulates cardiac subtype specification in differentiating human embryonic stem cells. Circ. Res. 2010;107:776–786. doi: 10.1161/CIRCRESAHA.110.223917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shinnawi R., Huber I., Maizels L., Shaheen N., Gepstein A., Arbel G., Tijsen A.J., Gepstein L. Monitoring Human-Induced Pluripotent Stem Cell-Derived Cardiomyocytes with Genetically Encoded Calcium and Voltage Fluorescent Reporters. Stem Cell Rep. 2015;5:582–596. doi: 10.1016/j.stemcr.2015.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dempsey G.T., Chaudhary K.W., Atwater N., Nguyen C., Brown B.S., McNeish J.D., Cohen A.E., Kralj J.M. Cardiotoxicity screening with simultaneous optogenetic pacing, voltage imaging and calcium imaging. J. Pharmacol. Toxicol. Methods. 2016;81:240–250. doi: 10.1016/j.vascn.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 64.Lapp H., Bruegmann T., Malan D., Friedrichs S., Kilgus C., Heidsieck A., Sasse P. Frequency-dependent drug screening using optogenetic stimulation of human iPSC-derived cardiomyocytes. Sci. Rep. 2017;7:9629. doi: 10.1038/s41598-017-09760-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lin Y., Liu H., Klein M., Ostrominski J., Hong S.G., Yada R.C., Chen G., Navarengom K., Schwartzbeck R., San H., et al. Efficient differentiation of cardiomyocytes and generation of calcium-sensor reporter lines from nonhuman primate iPSCs. Sci. Rep. 2018;8:5907. doi: 10.1038/s41598-018-24074-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Liu Z., Tang Y., Lü S., Zhou J., Du Z., Duan C., Li Z., Wang C. The tumourigenicity of iPS cells and their differentiated derivates. J. Cell Mol. Med. 2013;17:782–791. doi: 10.1111/jcmm.12062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mummery C.L., Zhang J., Ng E.S., Elliott D.A., Elefanty A.G., Kamp T.J. Differentiation of human embryonic stem cells and induced pluripotent stem cells to cardiomyocytes: A methods overview. Circ. Res. 2012;111:344–358. doi: 10.1161/CIRCRESAHA.110.227512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Christoforou N., Liau B., Chakraborty S., Chellapan M., Bursac N., Leong K.W. Induced pluripotent stem cell-derived cardiac progenitors differentiate to cardiomyocytes and form biosynthetic tissues. PLoS ONE. 2013;8:e65963. doi: 10.1371/journal.pone.0065963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhang J., Tao R., Campbell K.F., Carvalho J.L., Ruiz E.C., Kim G.C., Schmuck E.G., Raval A.N., da Rocha A.M., Herron T.J. Functional cardiac fibroblasts derived from human pluripotent stem cells via second heart field progenitors. Nat. Commun. 2019;10:2238. doi: 10.1038/s41467-019-09831-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xu C., Police S., Rao N., Carpenter M.K. Characterization and enrichment of cardiomyocytes derived from human embryonic stem cells. Circ. Res. 2002;91:501–508. doi: 10.1161/01.RES.0000035254.80718.91. [DOI] [PubMed] [Google Scholar]
- 71.Sharma A., Li G., Rajarajan K., Hamaguchi R., Burridge P.W., Wu S.M. Derivation of highly purified cardiomyocytes from human induced pluripotent stem cells using small molecule-modulated differentiation and subsequent glucose starvation. JoVE. 2015:e52628. doi: 10.3791/52628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hu D., Linders A., Yamak A., Correia C., Kijlstra J.D., Garakani A., Xiao L., Milan D.J., van der Meer P., Serra M., et al. Metabolic Maturation of Human Pluripotent Stem Cell-Derived Cardiomyocytes by Inhibition of HIF1alpha and LDHA. Circ. Res. 2018;123:1066–1079. doi: 10.1161/CIRCRESAHA.118.313249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hattori F., Chen H., Yamashita H., Tohyama S., Satoh Y.S., Yuasa S., Li W., Yamakawa H., Tanaka T., Onitsuka T., et al. Nongenetic method for purifying stem cell-derived cardiomyocytes. Nat. Methods. 2010;7:61–66. doi: 10.1038/nmeth.1403. [DOI] [PubMed] [Google Scholar]
- 74.Dai D.F., Danoviz M.E., Wiczer B., Laflamme M.A., Tian R. Mitochondrial Maturation in Human Pluripotent Stem Cell Derived Cardiomyocytes. Stem Cells Int. 2017;2017:5153625. doi: 10.1155/2017/5153625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Klug M.G., Soonpaa M.H., Koh G.Y., Field L.J. Genetically selected cardiomyocytes from differentiating embronic stem cells form stable intracardiac grafts. J. Clin. Investig. 1996;98:216–224. doi: 10.1172/JCI118769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kita-Matsuo H., Barcova M., Prigozhina N., Salomonis N., Wei K., Jacot J.G., Nelson B., Spiering S., Haverslag R., Kim C., et al. Lentiviral vectors and protocols for creation of stable hESC lines for fluorescent tracking and drug resistance selection of cardiomyocytes. PLoS ONE. 2009;4:e5046. doi: 10.1371/journal.pone.0005046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Xu X., Zweigerdt R., Xu X., Zweigerdt R., Soo S., Ngoh Z., Tham S., Wang S., Graichen R., Davidson B. Highly enriched cardiomyocytes from human embryonic stem cells. Cytotherapy. 2008;10:376–389. doi: 10.1080/14653240802105307. [DOI] [PubMed] [Google Scholar]
- 78.Anderson D., Self T., Mellor I.R., Goh G., Hill S.J., Denning C. Transgenic enrichment of cardiomyocytes from human embryonic stem cells. Mol. Ther. 2007;15:2027–2036. doi: 10.1038/sj.mt.6300303. [DOI] [PubMed] [Google Scholar]
- 79.Jung J.J., Husse B., Rimmbach C., Krebs S., Stieber J., Steinhoff G., Dendorfer A., Franz W.-M., David R. Programming and isolation of highly pure physiologically and pharmacologically functional sinus-nodal bodies from pluripotent stem cells. Stem Cell Rep. 2014;2:592–605. doi: 10.1016/j.stemcr.2014.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hannes T., Wolff M., Doss M.X., Pfannkuche K., Haustein M., Müller-Ehmsen J., Sachinidis A., Hescheler J., Khalil M., Halbach M. Electrophysiological characteristics of embryonic stem cell-derived cardiomyocytes are cell line-dependent. Cell. Physiol. Biochem. 2015;35:305–314. doi: 10.1159/000369697. [DOI] [PubMed] [Google Scholar]
- 81.Belus A., White E. Effects of antibiotics on the contractility and Ca2+ transients of rat cardiac myocytes. Eur. J. Pharmacol. 2001;412:121–126. doi: 10.1016/S0014-2999(01)00717-8. [DOI] [PubMed] [Google Scholar]
- 82.Anderson D.J., Kaplan D.I., Bell K.M., Koutsis K., Haynes J.M., Mills R.J., Phelan D.G., Qian E.L., Leitoguinho A.R., Arasaratnam D., et al. NKX2-5 regulates human cardiomyogenesis via a HEY2 dependent transcriptional network. Nat. Commun. 2018;9:1373. doi: 10.1038/s41467-018-03714-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kasahara H., Bartunkova S., Schinke M., Tanaka M., Izumo S. Cardiac and extracardiac expression of Csx/Nkx2.5 homeodomain protein. Circ. Res. 1998;82:936–946. doi: 10.1161/01.RES.82.9.936. [DOI] [PubMed] [Google Scholar]
- 84.LaBarge W., Mattappally S., Kannappan R., Fast V.G., Pretorius D., Berry J.L., Zhang J. Maturation of three-dimensional, hiPSC-derived cardiomyocyte spheroids utilizing cyclic, uniaxial stretch and electrical stimulation. PLoS ONE. 2019;14:e0219442. doi: 10.1371/journal.pone.0219442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Guo Y., Pu W.T. Cardiomyocyte maturation: New phase in development. Circ. Res. 2020;126:1086–1106. doi: 10.1161/CIRCRESAHA.119.315862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cui M., Wang Z., Bassel-Duby R., Olson E.N. Genetic and epigenetic regulation of cardiomyocytes in development, regeneration and disease. Development. 2018;145:dev171983. doi: 10.1242/dev.171983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Toepfer C.N., Garfinkel A.C., Venturini G., Wakimoto H., Repetti G., Alamo L., Sharma A., Agarwal R., Ewoldt J.F., Cloonan P., et al. Myosin Sequestration Regulates Sarcomere Function, Cardiomyocyte Energetics, and Metabolism, Informing the Pathogenesis of Hypertrophic Cardiomyopathy. Circulation. 2020;141:828–842. doi: 10.1161/CIRCULATIONAHA.119.042339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kane C., Terracciano C.M. Concise Review: Criteria for Chamber-Specific Categorization of Human Cardiac Myocytes Derived from Pluripotent Stem Cells. Stem Cells. 2017;35:1881–1897. doi: 10.1002/stem.2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Paik D.T., Chandy M., Wu J.C. Patient and Disease–Specific Induced Pluripotent Stem Cells for Discovery of Personalized Cardiovascular Drugs and Therapeutics. Pharmacol. Rev. 2020;72:320–342. doi: 10.1124/pr.116.013003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sheikh F., Lyon R.C., Chen J. Functions of myosin light chain-2 (MYL2) in cardiac muscle and disease. Gene. 2015;569:14–20. doi: 10.1016/j.gene.2015.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Piccini I., Rao J., Seebohm G., Greber B. Human pluripotent stem cell-derived cardiomyocytes: Genome-wide expression profiling of long-term in vitro maturation in comparison to human heart tissue. Genom. Data. 2015;4:69–72. doi: 10.1016/j.gdata.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Franco D., Lamers W.H., Moorman A.F. Patterns of expression in the developing myocardium: Towards a morphologically integrated transcriptional model. Cardiovasc. Res. 1998;38:25–53. doi: 10.1016/S0008-6363(97)00321-0. [DOI] [PubMed] [Google Scholar]
- 93.Minamisawa S., Wang Y., Chen J., Ishikawa Y., Chien K.R., Matsuoka R. Atrial chamber-specific expression of sarcolipin is regulated during development and hypertrophic remodeling. J. Biol. Chem. 2003;278:9570–9575. doi: 10.1074/jbc.M213132200. [DOI] [PubMed] [Google Scholar]
- 94.Devalla H.D., Schwach V., Ford J.W., Milnes J.T., El-Haou S., Jackson C., Gkatzis K., Elliott D.A., de Sousa Lopes S.M.C., Mummery C.L., et al. Atrial-like cardiomyocytes from human pluripotent stem cells are a robust preclinical model for assessing atrial-selective pharmacology. EMBO Mol. Med. 2015;7:394–410. doi: 10.15252/emmm.201404757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yechikov S., Copaciu R., Gluck J.M., Deng W., Chiamvimonvat N., Chan J.W., Lieu D.K. Same-Single-Cell Analysis of Pacemaker-Specific Markers in Human Induced Pluripotent Stem Cell-Derived Cardiomyocyte Subtypes Classified by Electrophysiology. Stem Cells. 2016;34:2670–2680. doi: 10.1002/stem.2466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Davis D.L., Edwards A.V., Juraszek A.L., Phelps A., Wessels A., Burch J.B. A GATA-6 gene heart-region-specific enhancer provides a novel means to mark and probe a discrete component of the mouse cardiac conduction system. Mech. Dev. 2001;108:105–119. doi: 10.1016/S0925-4773(01)00500-7. [DOI] [PubMed] [Google Scholar]
- 97.Sun C., Yu D., Ye W., Liu C., Gu S., Sinsheimer N.R., Song Z., Li X., Chen C., Song Y. The short stature homeobox 2 (Shox2)-bone morphogenetic protein (BMP) pathway regulates dorsal mesenchymal protrusion development and its temporary function as a pacemaker during cardiogenesis. J. Biol. Chem. 2015;290:2007–2023. doi: 10.1074/jbc.M114.619007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ionta V., Liang W., Kim E.H., Rafie R., Giacomello A., Marbán E., Cho H.C. SHOX2 overexpression favors differentiation of embryonic stem cells into cardiac pacemaker cells, improving biological pacing ability. Stem Cell Rep. 2015;4:129–142. doi: 10.1016/j.stemcr.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Polonchuk L. Toward a new gold standard for early safety: Automated temperature-controlled hERG test on the PatchLiner®. Front. Pharmacol. 2012;3:3. doi: 10.3389/fphar.2012.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Herron T.J., Lee P., Jalife J. Optical imaging of voltage and calcium in cardiac cells & tissues. Circ. Res. 2012;110:609–623. doi: 10.1161/CIRCRESAHA.111.247494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Smith N.A., Kress B.T., Lu Y., Chandler-Militello D., Benraiss A., Nedergaard M. Fluorescent Ca(2+) indicators directly inhibit the Na,K-ATPase and disrupt cellular functions. Sci. Signal. 2018;11:eaal2039. doi: 10.1126/scisignal.aal2039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Grienberger C., Konnerth A. Imaging calcium in neurons. Neuron. 2012;73:862–885. doi: 10.1016/j.neuron.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 103.Sankaranarayanan S., De Angelis D., Rothman J.E., Ryan T.A. The use of pHluorins for optical measurements of presynaptic activity. Biophys. J. 2000;79:2199–2208. doi: 10.1016/S0006-3495(00)76468-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jin L., Han Z., Platisa J., Wooltorton J.R., Cohen L.B., Pieribone V.A. Single action potentials and subthreshold electrical events imaged in neurons with a fluorescent protein voltage probe. Neuron. 2012;75:779–785. doi: 10.1016/j.neuron.2012.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hitoshi N., Ken-ichi Y., Jun-ichi M. Efficient selection for high-expression transfectants with a novel eukaryotic vector. Gene. 1991;108:193–199. doi: 10.1016/0378-1119(91)90434-D. [DOI] [PubMed] [Google Scholar]
- 106.Goldfracht I., Efraim Y., Shinnawi R., Kovalev E., Huber I., Gepstein A., Arbel G., Shaheen N., Tiburcy M., Zimmermann W.H., et al. Engineered heart tissue models from hiPSC-derived cardiomyocytes and cardiac ECM for disease modeling and drug testing applications. Acta Biomater. 2019;92:145–159. doi: 10.1016/j.actbio.2019.05.016. [DOI] [PubMed] [Google Scholar]
- 107.Jares-Erijman E.A., Jovin T.M. FRET imaging. Nat. Biotechnol. 2003;21:1387–1395. doi: 10.1038/nbt896. [DOI] [PubMed] [Google Scholar]
- 108.Akerboom J., Rivera J.D., Guilbe M.M., Malave E.C., Hernandez H.H., Tian L., Hires S.A., Marvin J.S., Looger L.L., Schreiter E.R. Crystal structures of the GCaMP calcium sensor reveal the mechanism of fluorescence signal change and aid rational design. J. Biol. Chem. 2009;284:6455–6464. doi: 10.1074/jbc.M807657200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Nagai T., Sawano A., Park E.S., Miyawaki A. Circularly permuted green fluorescent proteins engineered to sense Ca2+ Proc. Natl. Acad. Sci. USA. 2001;98:3197–3202. doi: 10.1073/pnas.051636098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Deisseroth K. Optogenetics: 10 years of microbial opsins in neuroscience. Nat. Neurosci. 2015;18:1213–1225. doi: 10.1038/nn.4091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Nagel G., Szellas T., Huhn W., Kateriya S., Adeishvili N., Berthold P., Ollig D., Hegemann P., Bamberg E. Channelrhodopsin-2, a directly light-gated cation-selective membrane channel. Proc. Natl. Acad. Sci. USA. 2003;100:13940–13945. doi: 10.1073/pnas.1936192100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ye F., Setozaki S., Kowalski W.J., Dwenger M., Yuan F., Tinney J.P., Nakane T., Masumoto H., Keller B.B. Molecular Mechanism of Congenital Heart Disease and Pulmonary Hypertension. Springer; Singapore: 2020. Progress in the Generation of Multiple Lineage Human-iPSC-Derived 3D-Engineered Cardiac Tissues for Cardiac Repair; pp. 353–361. [Google Scholar]
- 113.Schwartz P.J., Priori S.G., Spazzolini C., Moss A.J., Vincent G.M., Napolitano C., Denjoy I., Guicheney P., Breithardt G., Keating M.T., et al. Genotype-phenotype correlation in the long-QT syndrome: Gene-specific triggers for life-threatening arrhythmias. Circulation. 2001;103:89–95. doi: 10.1161/01.CIR.103.1.89. [DOI] [PubMed] [Google Scholar]
- 114.Buja L.M. Cardiac repair and the putative role of stem cells. J. Mol. Cell. Cardiol. 2019;128:96–104. doi: 10.1016/j.yjmcc.2019.01.022. [DOI] [PubMed] [Google Scholar]
- 115.Tiercy J.-M. How to select the best available related or unrelated donor of hematopoietic stem cells? Haematologica. 2016;101:680–687. doi: 10.3324/haematol.2015.141119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rikhtegar R., Pezeshkian M., Dolati S., Safaie N., Rad A.A., Mahdipour M., Nouri M., Jodati A.R., Yousefi M. Stem cells as therapy for heart disease: iPSCs, ESCs, CSCs, and skeletal myoblasts. Biomed. Pharmacother. 2019;109:304–313. doi: 10.1016/j.biopha.2018.10.065. [DOI] [PubMed] [Google Scholar]
- 117.Mingliang R., Bo Z., Zhengguo W. Stem cells for cardiac repair: Status, mechanisms, and new strategies. Stem Cells Int. 2011;2011:310928. doi: 10.4061/2011/310928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lalit P.A., Hei D.J., Raval A.N., Kamp T.J. Induced pluripotent stem cells for post-myocardial infarction repair: Remarkable opportunities and challenges. Circ. Res. 2014;114:1328–1345. doi: 10.1161/CIRCRESAHA.114.300556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.van Laake L.W., Qian L., Cheng P., Huang Y., Hsiao E.C., Conklin B.R., Srivastava D. Reporter-based isolation of induced pluripotent stem cell- and embryonic stem cell-derived cardiac progenitors reveals limited gene expression variance. Circ. Res. 2010;107:340–347. doi: 10.1161/CIRCRESAHA.109.215434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sottas V., Wahl C.M., Trache M.C., Bartolf-Kopp M., Cambridge S., Hecker M., Ullrich N.D. Improving electrical properties of iPSC-cardiomyocytes by enhancing Cx43 expression. J. Mol. Cell. Cardiol. 2018;120:31–41. doi: 10.1016/j.yjmcc.2018.05.010. [DOI] [PubMed] [Google Scholar]
- 121.Denning C., Borgdorff V., Crutchley J., Firth K.S., George V., Kalra S., Kondrashov A., Hoang M.D., Mosqueira D., Patel A. Cardiomyocytes from human pluripotent stem cells: From laboratory curiosity to industrial biomedical platform. Biochim. Biophys. Acta. 2016;1863:1728–1748. doi: 10.1016/j.bbamcr.2015.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhou H., Dickson M.E., Kim M.S., Bassel-Duby R., Olson E.N. Akt1/protein kinase B enhances transcriptional reprogramming of fibroblasts to functional cardiomyocytes. Proc. Natl. Acad. Sci. USA. 2015;112:11864–11869. doi: 10.1073/pnas.1516237112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yang X., Rodriguez M., Pabon L., Fischer K.A., Reinecke H., Regnier M., Sniadecki N.J., Ruohola-Baker H., Murry C.E. Tri-iodo-l-thyronine promotes the maturation of human cardiomyocytes-derived from induced pluripotent stem cells. J. Mol. Cell. Cardiol. 2014;72:296–304. doi: 10.1016/j.yjmcc.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Radisic M., Park H., Shing H., Consi T., Schoen F.J., Langer R., Freed L.E., Vunjak-Novakovic G. Functional assembly of engineered myocardium by electrical stimulation of cardiac myocytes cultured on scaffolds. Proc. Natl. Acad. Sci. USA. 2004;101:18129–18134. doi: 10.1073/pnas.0407817101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Dwenger M., Kowalski W.J., Ye F., Yuan F., Tinney J.P., Setozaki S., Nakane T., Masumoto H., Campbell P., Guido W. Chronic optical pacing conditioning of h-iPSC engineered cardiac tissues. J. Tissue Eng. 2019;10:2041731419841748. doi: 10.1177/2041731419841748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Yang X., Pabon L., Murry C.E. Engineering adolescence: Maturation of human pluripotent stem cell–derived cardiomyocytes. Circ. Res. 2014;114:511–523. doi: 10.1161/CIRCRESAHA.114.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Huyer L.D., Montgomery M., Zhao Y., Xiao Y., Conant G., Korolj A., Radisic M. Biomaterial based cardiac tissue engineering and its applications. Biomed. Mater. 2015;10:034004. doi: 10.1088/1748-6041/10/3/034004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mannhardt I., Breckwoldt K., Letuffe-Brenière D., Schaaf S., Schulz H., Neuber C., Benzin A., Werner T., Eder A., Schulze T. Human engineered heart tissue: Analysis of contractile force. Stem Cell Rep. 2016;7:29–42. doi: 10.1016/j.stemcr.2016.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Giacomelli E., Bellin M., Sala L., Van Meer B.J., Tertoolen L.G., Orlova V.V., Mummery C.L. Three-dimensional cardiac microtissues composed of cardiomyocytes and endothelial cells co-differentiated from human pluripotent stem cells. Development. 2017;144:1008–1017. doi: 10.1242/dev.143438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Goldfracht I., Protze S., Shiti A., Setter N., Gruber A., Shaheen N., Nartiss Y., Keller G., Gepstein L. Generating ring-shaped engineered heart tissues from ventricular and atrial human pluripotent stem cell-derived cardiomyocytes. Nat. Commun. 2020;11:75. doi: 10.1038/s41467-019-13868-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Nunes S.S., Miklas J.W., Liu J., Aschar-Sobbi R., Xiao Y., Zhang B., Jiang J., Massé S., Gagliardi M., Hsieh A. Biowire: A platform for maturation of human pluripotent stem cell–derived cardiomyocytes. Nat. Methods. 2013;10:781–787. doi: 10.1038/nmeth.2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Huang C.Y., Maia-Joca R.P.M., Ong C.S., Wilson I., DiSilvestre D., Tomaselli G.F., Reich D.H. Enhancement of human iPSC-derived cardiomyocyte maturation by chemical conditioning in a 3D environment. J. Mol. Cell. Cardiol. 2020;138:1–11. doi: 10.1016/j.yjmcc.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 133.Giacomelli E., Meraviglia V., Campostrini G., Cochrane A., Cao X., van Helden R.W., Garcia A.K., Mircea M., Kostidis S., Davis R.P. Human-iPSC-Derived Cardiac Stromal Cells Enhance Maturation in 3D Cardiac Microtissues and Reveal Non-cardiomyocyte Contributions to Heart Disease. Cell Stem Cell. 2020;26:862–879.e11. doi: 10.1016/j.stem.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bargehr J., Ong L.P., Colzani M., Davaapil H., Hofsteen P., Bhandari S., Gambardella L., Le Novère N., Iyer D., Sampaziotis F. Epicardial cells derived from human embryonic stem cells augment cardiomyocyte-driven heart regeneration. Nat. Biotechnol. 2019;37:895–906. doi: 10.1038/s41587-019-0197-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Lemme M., Braren I., Prondzynski M., Aksehirlioglu B., Ulmer B.M., Schulze M.L., Ismaili D., Meyer C., Hansen A., Christ T. Chronic intermittent tachypacing by an optogenetic approach induces arrhythmia vulnerability in human engineered heart tissue. Cardiovasc. Res. 2020;116:1487–1499. doi: 10.1093/cvr/cvz245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hazelbaker D.Z., Beccard A., Mazzucato P., Angelini G., Messana A., Lam D., Eggan K., Barrett L.E. A multiplexed gRNA piggyBac transposon system facilitates efficient induction of CRISPRi and CRISPRa in human pluripotent stem cells. Sci. Rep. 2020;10:635. doi: 10.1038/s41598-020-57500-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Truong V.A., Hsu M.N., Kieu Nguyen N.T., Lin M.W., Shen C.C., Lin C.Y., Hu Y.C. CRISPRai for simultaneous gene activation and inhibition to promote stem cell chondrogenesis and calvarial bone regeneration. Nucleic Acids Res. 2019;47:e74. doi: 10.1093/nar/gkz267. [DOI] [PMC free article] [PubMed] [Google Scholar]