Abstract
The stigmatization of HIV infection impedes every step along the HIV continuum of care, particularly care engagement and retention. The differential effects of various sources of stigma on retention in HIV care have been the subject of limited research. We examined the accumulation of HIV stigma experiences over 1 year in relationship to treatment retention among 251 men and women marginally engaged in HIV care in the southeastern United States. Results showed that cumulative stigma experiences predicted poorer retention in care, with greater stigma experiences related to less consistency in attending scheduled medical appointments. HIV stigma originating from family members and acts of overt discrimination were the most frequently experienced sources of stigma and were most closely associated with disengagement from HIV care. In addition, analyses by gender indicated that retention in care for men was impacted by stigma to a greater extent than among women. These findings reaffirm the importance of HIV stigma as a barrier to HIV care and provide new directions for interventions to mitigate the negative effects of stigma on patients who are not fully engaged in HIV care. Clinical trials registration NCT104180280.
Keywords: HIV treatment, retention in care, HIV stigma, health disparities
Introduction
The success of combination antiretroviral therapies (ART) hinges on persistent engagement in HIV care.1,2 The CDC estimates that 26% of people diagnosed with HIV in the United States are not fully engaged in care, with as many as 51% of those who were once engaged in care becoming disengaged.3 Snapshots of care engagement and retention, that is whether patients are engaged in care at a given point in time, do not capture the dynamic processes of care engagement, retention, disengagement, and reengagement.4 As few as half of patients who initiate reengagement in care succeed; and patients who are already HIV viral suppressed are more likely to remain in care.5
Long-term retention in care is essential to achieving HIV treatment and prevention goals.6 Although efforts to improve retention in care are cost-effective and deemed a public health priority,7 there are a myriad of challenges that impede engagement and retention in HIV care across cultures,4 with evidence from multiple countries finding that HIV stigma impedes engagement and retention in care.8,9
Stigma is a robust barrier to remaining in HIV care. Typically considered a complex phenomenon, stigma socially devalues and discredits individual characteristics, attributes, and behaviors.10 Since the beginning of the HIV pandemic, stigma has undermined every step along the HIV continuum of care.11–15 In South Africa, the internalization of HIV stigma is related to avoidant coping and delayed initiation of ART.16 Experiencing HIV stigma is also associated with uncontrolled HIV (e.g., detectable viral load), missed clinic visits, poor clinic visit constancy, and disengagement from care.17
Enacted HIV stigma, defined as acts of overt and subtle discrimination experienced by people living with HIV, can be salient and have lasting adverse effects.18 HIV stigma originating from families and its consequential undermining of family support have emerged as a particularly potent predictor of poor engagement in HIV care.19 There is also evidence that patients’ experiences with enacted stigma interact with their connection to care providers, such that people who experience more HIV stigma are less connected to their providers and consequently have poorer retention in care.20 Few studies, however, have examined stigma experiences in relationship to care retention among patients who may be at risk for disengagement from care, specifically patients who are newly engaged, reengaged, or at risk for treatment failure.
This study examined enacted stigma experiences stemming from multiple sources over the course of 1 year in relationship to their cumulative effects on retention in HIV care. We focused on people at high risk for treatment disengagement, specifically newly diagnosed patients, patients who had previously disengaged and were returning to care, and patients identified by providers as marginally engaged in care and at risk for treatment failure.
Further, given that stigma occurs to a greater degree in rural areas relative to urban centers,21,22 we conducted our study at a public clinic serving a rural area in the southeastern United States. We hypothesized that the accumulation of enacted stigma experiences over 1 year would be associated with disengagement from HIV care and that the strongest predictor of disengagement from HIV care would be family-related enacted stigma experiences.
Methods
Participants and procedures
Participants were 175 men and 76 women recruited between September 2015 and December 2017 from a publicly funded HIV clinic in central Georgia, serving a small city and surrounding rural areas. Data from these participants with some overlapping measures have been reported in previous research.23 A total of 375 patients were referred and contacted to explain the study and 251 agreed, yielding a 67% acceptance rate.
Following informed consent, participants completed a computerized interview and provided permission for the researchers to retrieve their HIV viral loads and their medical appointment records from electronic clinic charts. All individuals received behavioral health counseling as part of their participation. Participants were called monthly for health monitoring interviews and were compensated for their time to complete measures over the course of the year with up to $580 cash dispensed through ATM card. The University of Connecticut and Mercer University Institutional Review Boards approved all procedures. These data are from a trial registered at clinicaltrials.gov NCT104180280.
Measures
We utilized data collected within a 12-month period to examine the associations between cumulative enacted stigma experiences and retention in care. Cumulative HIV-related enacted stigma was aggregated from stigma events collected monthly for 1 year. Our approach was to monitor stigma monthly to capture repeated events because stigma is highly impactful and experienced sporadically.24,25
Audio computer-administered self-interviews
We collected participant demographic characteristics (i.e., gender, sexual orientation, race, age, and years of education), and the year and place they tested HIV positive. Participants also completed the full 20-item CESD (Centers for Epidemiological Studies Depression) scale to assess symptoms of depression.26 Items focused on how often participants had specific depression-related thoughts, feelings, and behaviors in the last 7 days. Responses were 0 = 0 days, 1 = 1–2 days, 2 = 3–4 days, and 3 = 5–7 days. Scores range from 0 to 60 and scores greater than 16 indicate possible depression, alpha = 0.90. Alcohol use at baseline was assessed with the Alcohol Use Disorders Identification Test (AUDIT), a 10-item scale designed to measure alcohol consumption and identify risks for alcohol abuse and dependence.27 AUDIT scores between 1 and 7 represent moderate drinking and scores 8 and greater indicate possible hazardous alcohol use.28 We also calculated the distance in miles that participants resided from the clinic using ArcGIS software.
Medical records chart abstraction
HIV viral load
Laboratory reports of blood plasma HIV viral load most proximal and within 3 months of the baseline assessment were abstracted from electronic medical records. In accordance with HIV treatment guidelines,29 we used the clinically recorded value with a threshold of <20 copies/mL to define suppressed (undetectable) viral load.
Retention in care
Retrospective chart reviews at the end of the study were performed to determine whether patients were retained in care. Electronic medical records were examined over the 12 months during which assessments were collected with an additional 6 months of post-assessment period, a total of 18 months to assess care retention. Coding retention in care for an additional 6 months past the final follow-up assessment encompasses the time period during which stigma may have influenced this outcome.
Records were coded for number of clinical/medical appointments scheduled, attended, and not attended. Participants with records marked as “discontinued care” were defined by the clinic as disengaged from care. Typically at the clinic, patients who had not been seen for clinical services with missed appointments over 6 months are defined as disengaged from care. Patients transferred to other providers and patients who died are treated distinctly in the medical records and were not coded as disengaged from care.
Monthly phone assessments: enacted stigma
At each monthly phone interview, we assessed enacted stigma using an adaptation of the HIV Stigma Mechanisms Scale.18,30 We used seven items to assess experiences of enacted stigma each month. We purposefully selected a broad array of stigma experiences to reflect family relationships, experiences of discrimination, and denial of services, including health care (see Results section for exact wording of the seven items). We administered the enacted stigma items at each of the 12-monthly telephone assessments.
Stigma experiences were asked each month referring to the preceding 30 days with responses indicating yes the experience occurred, or no the experience did not occur in the previous month. We summed the stigma experiences for all available assessments to create a cumulative composite representing the frequency of the seven stigma experiences occurring during the course of the 12 months. Cumulative stigma experiences were examined within each of the seven different stigma experiences, scores having a potential range from 0 to 12, as well as for the enacted stigma experiences across 12 months, with scores ranging from 0 to 84.
Data analyses
We conducted descriptive analyses of demographic and health characteristics for individuals identified in their medical records as retained (N = 193) and disengaged (N = 58) from care. Statistical significance between groups was analyzed using contingency table χ2 tests for categorical variables and independent t-tests for continuous variables. Cumulative enacted stigma experiences over the 12-month observation period were examined for the proportion of participants who experienced at least one stigma event, the mean number of stigma events among those who experienced each source of stigma, and the mean number of enacted stigma events for the entire sample.
We tested the main study hypothesis that cumulative enacted stigma experiences would be associated with disengagement from HIV care using Poisson regression for the association between the cumulative number of stigma events and disengagement from care. We subsequently tested models for each of the seven different enacted stigma experiences. All models were tested with robust estimators, included gender as a factor, and controlled for participant age, the distance participants lived from the clinic, depression scores, and alcohol use. All statistical tests defined significance as p < 0.05.
Results
The sample included 131 (52%) patients who had fallen out of HIV care and were returning to care, 47 (19%) patients who were newly diagnosed with HIV and were therefore new to HIV care, and 73 (29%) patients referred by their physician or nurse due to HIV viral load rebound or nonadherence to ART. The sample was predominantly male (70%) and African American (83%). Among men, 96 (55%) identified as gay or bisexual. Nearly half (46%) of participants had no source of employment and 71% had annual incomes under $10,000. On average, participants had been living with an HIV diagnosis for more than 10 years, with 44% demonstrating HIV viral suppression from medical chart data. Two out of three participants reported active use of alcohol at baseline and the sample median CESD score was over the cutoff of 16 for considering probable depression.
Results showed that 58 (23%) participants disengaged from care over the course of the 18 months of medical record chart abstraction. Table 1 shows the demographic and health characteristics of participants who were retained and those who were disengaged from care. The only two distinguishing characteristics between patients retained and those who disengaged from care were age and the distance participants lived from the clinic; patients who disengaged from care were significantly younger and lived significantly farther from the clinic than those who were retained. As would be expected, participants who disengaged from care had fewer clinic appointments and a higher rate of not showing for appointments.
Table 1.
Characteristics of Participants Who Were Retained in Care and Those Who Disengaged from Care
| Characteristic | Retained in care, N = 193 |
Disengaged from care, N = 58 |
χ2 | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Gender | |||||
| Gay/bisexual identified men | 71 | 37 | 25 | 43 | 0.7 |
| Heterosexual identified men | 61 | 32 | 17 | 29 | |
| Women | 60 | 31 | 16 | 28 | |
| Transgender | 7 | 4 | 3 | 5 | 0.2 |
| Race | |||||
| White | 20 | 10 | 12 | 21 | 4.7 |
| African American | 165 | 86 | 43 | 74 | |
| Other | 7 | 4 | 3 | 5 | |
| Unemployed | 154 | 80 | 46 | 79 | 0.4 |
| Income less than $10,000 | 139 | 71 | 41 | 71 | 3.3 |
| Income between $10,000 and 20,000 | 38 | 20 | 8 | 14 | |
| Income greater than $20,000 | 16 | 9 | 9 | 15 | |
| Viral load undetectablea | 75 | 43 | 24 | 46 | 0.2 |
| Viral load detectable | 101 | 57 | 28 | 54 | |
| Care status reengaging in care | 101 | 52 | 20 | 52 | 0.8 |
| Newly diagnosed | 34 | 18 | 13 | 22 | |
| Provider identified at risk | 58 | 30 | 15 | 26 | |
| M | SD | M | SD | t | |
| Age | 43.4 | 12.3 | 37.9 | 11.6 | 2.9** |
| Years since HIV diagnosis | 12.1 | 8.9 | 10.4 | 7.7 | 1.2 |
| Distance in miles residing from clinic | 1.2 | 11.7 | 16.4 | 20.5 | 2.3* |
| AUDIT Alcohol score | 4.0 | 5.4 | 4.2 | 6.8 | 0.2 |
| CES-depression score | 21.1 | 10.3 | 21.7 | 9.9 | 0.4 |
| Clinic appointments attended | 4.6 | 1.9 | 3.1 | 1.5 | 4.9** |
| Clinic appointments no-showed | 3.0 | 1.9 | 2.9 | 1.8 | 0.5 |
| % Clinic appointments attended | 66.1 | 22.3 | 55.5 | 19.4 | 3.1** |
Viral load was unavailable for 23 participants.
p < 0.05, **p < 0.01.
AUDIT, Alcohol Use Disorders Identification Test; CES, Centers for Epidemiological Studies; SD, standard deviation.
Enacted stigma experiences
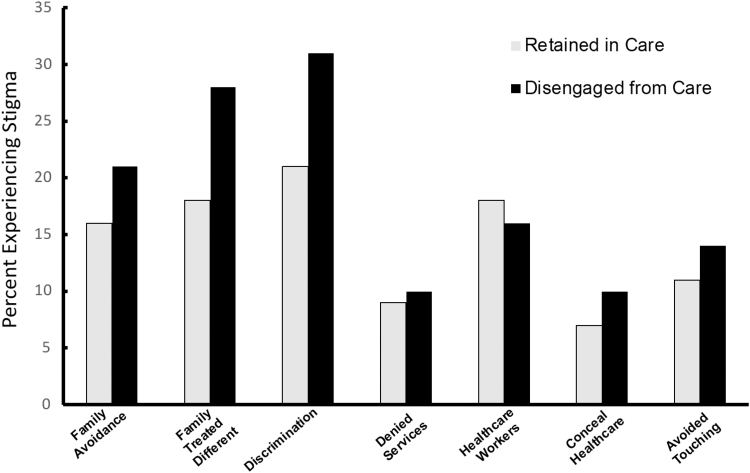
A total of 109 (47%) participants reported experiencing at least one enacted stigma event over the 12-month observation period. For the entire sample, including those who did not report any stigma experiences over the year, the mean number of stigma experiences was 2.6 (SD = 5.8) (Table 2). Among participants who experienced at least one enacted stigma event, the average number of stigma experiences over the year was 5.7 (SD = 7.5). One in five participants reported at least one occurrence of their family treating them differently because they have HIV and one in four participants reported experiencing at least one act of discrimination. As shown in Fig. 1, the most commonly experienced stigma events originated from family and acts of discrimination, with more than one in four participants reporting at least one such experience over the year. Less common were stigma experiences in health care, denial of services, concealing one's health care, and people avoiding touching participants.
Table 2.
Enacted Stigma Experiences Over the 12-Month Study Among Participants Who Were Retained in Care and Those Who Disengaged from Care
| Enacted stigma experience items | Retained in care, N = 193 |
Disengaged from care, N = 58 |
Wald χ2 | ||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Because of your HIV status, did family members avoid you? | 0.4 | 1.1 | 0.8 | 2.1 | 14.2** |
| Among those experiencing this stigma | 2.1 | 1.8 | 3.3 | 3.4 | |
| Because of your HIV status, did family members treat you differently? | 0.4 | 1.3 | 0.9 | 2.1 | 12.4** |
| Among those experiencing this stigma | 2.3 | 2.1 | 2.9 | 3.1 | |
| Did people discriminate against you because of your HIV status? | 0.5 | 1.3 | 1.0 | 1.9 | 4.6* |
| Among those experiencing this stigma | 2.3 | 2.1 | 2.8 | 2.3 | |
| Were you denied services because of your HIV status? | 0.2 | 0.6 | 0.2 | 0.6 | 2.9 |
| Among those experiencing this stigma | 1.8 | 1.1 | 1.5 | 1.2 | |
| Because of your HIV status, did health care workers not listen to your concerns? | 0.3 | 0.8 | 0.2 | 0.6 | 0.4 |
| Among those experiencing this stigma | 1.7 | 1.1 | 1.4 | 1.0 | |
| Did you avoid going to a clinic or health care provider because you did not want others to know your HIV status? | 0.2 | 1.0 | 0.1 | 0.4 | 3.5 |
| Among those experiencing this stigma | 3.1 | 2.3 | 1.2 | 0.4 | |
| Did people avoid touching you because of your HIV status? | 0.2 | 0.6 | 0.2 | 0.9 | 0.6 |
| Among those experiencing this stigma | 1.7 | 1.0 | 1.6 | 1.7 | |
| Any enacted HIV stigma experience | 2.3 | 5.4 | 3.5 | 6.9 | 13.7** |
| Among those experiencing this stigma | 5.2 | 7.2 | 6.2 | 8.3 | |
Items shown as presented to participants; responses were Yes, did occur, and No did not occur. Enacted stigma experiences were asked each month and could be reported more than once during the 12-monthly assessments; Poisson regression models adjusted for gender, age, depression, and alcohol use.
p < 0.05, **p < 0.01.
SD, standard deviation.
FIG. 1.
Percentages of participants experiencing HIV-related stigma events for those retained in care and disengaged from care.
Enacted stigma experiences and retention in care
Poisson regression models for retention in care and gender, controlling for participant age, distance participants lived from the clinic, depression scores, and alcohol use showed a significant association between retention in care and number of stigma experiences over the year, Wald's χ2 = 11.8, p < 001. As shown in Table 2, participants who disengaged from care experienced a greater number of stigma events over the year. In addition, women (mean = 2.9, SD = 7.4) reported a greater number of stigma experiences than men (mean = 2.4, SD = 5.1), Wald's χ2 = 6.8, p < 0.01. The interaction between retention in care and participant gender was also significant, Wald's χ2 = 10.4, p < 0.01; women who disengaged from care experienced only slightly more stigma events (mean = 3.20, SD = 9.71) than women retained in care (mean = 2.82, SD = 6.45), whereas men who disengaged from care (mean = 3.66, SD = 5.58) experienced 43% more stigma events as men who were retained in care (mean = 2.07, SD = 4.93).
Examining each of the seven sources of enacted stigma experiences, controlling for all covariates, patients who disengaged from care experienced more family avoidance and family members treating them differently because of their HIV status, and more acts of discrimination (Table 2).
Discussion
This study found high rates of treatment discontinuation among patients who were deemed to be at risk for disengagement from care. We found that over an 18-month period, more than one in five (23%) participants was disengaged from HIV care. Younger participants residing farther from the clinic were more likely to disengage from care. Participants who ultimately disengaged from care had only attended 55% of their scheduled clinic appointments, significantly fewer than those retained in care. It should be noted, however, that only 66% of clinic appointments were kept by participants who were retained in care.
Confirming our main study hypothesis and consistent with past research,20,31–33 we found that the cumulative effect of enacted stigma experiences over 1 year was associated with disengagement from HIV care. However, we also found a significant interaction between care disengagement and gender for the number of enacted stigma experiences. Comparisons of women retained in care and those disengaged from care indicated that there was no significant difference in stigma experiences. In contrast, men who disengaged from care experienced far more stigma than men who were retained. This interaction occurred in the absence of gender differences in care engagement and suggests that stigma may be a relatively more potent impediment to care retention for men compared to women living with HIV in this setting. One potential explanation for this finding is the intersection of HIV stigma with other stigmatized social identities, such as sexual orientation. For example, men who have sex with men may experience the unique intersection of HIV and homophobia that may compound their experience of stigma.34,35
Although we did not observe an association between having had male sex partners and retention in care, we also did not measure intersectional stigmatized identities per se.34 Previous research has shown that the intersection of race and gender in the experience of subtle forms of discrimination, for example, poses unique barriers to HIV care for women.36 An alternative explanation for the observed interaction of retention in care and gender is a potential resilience among women in terms of managing stigma. Thus, the lack of evidence for a detrimental effect of cumulative stigma on retention in care for women may reflect variables not measured in our study, such as anticipated stigma,37 neighborhood characteristics and community support,38 and relationships with health care providers.5,31 Research is needed to further examine the basis for the observed gender differences and the impact of HIV stigma on men and women with respect to retention in care.
We also confirmed our hypothesis that family-related stigma experiences would be robust predictors of disengagement from care. Participants who disengaged from care reported significantly more experiences where family members avoided them and treated them differently because of their HIV status. Disengagement from care was also associated with an array of discrimination experiences, although at smaller magnitudes than seen for familial stigma. Our findings are therefore consistent with research focused on women living with HIV, demonstrating the importance of family support in facilitating retention in HIV care.19 Stigma experiences originating from family may be particularly detrimental because family may otherwise serve as a supportive buffer against stigma stemming from other sources.
Results of this study should be interpreted in light of its methodological limitations. Although we sampled a clinic serving a broad geographical area within a state with high HIV prevalence, the sample was one of convenience and cannot be considered representative of people living with HIV in this region. In addition, the study was conducted in just one state in the southeastern United States, and is therefore geographically constrained. Although more than 65% of people living with HIV in rural areas of the United States reside in southern states and more than half of people living with HIV in Georgia reside outside of major metropolitan areas,39 our sample cannot be assumed presentative of people living with HIV in southern rural states. Our medical records of viral load data also did not allow us to examine this important health marker in relationship to retention in care because viral loads were missing for those with missed appointments and disengagement from care. Our study also relied on self-reported measures of stigma, which themselves may be prone to underreporting. We also studied only a limited number of stigma events. Although we selected salient experiences, the impact of other sources of stigma as well as less salient microaggressions should be included in future studies.40 It also should be noted that our relatively small sample size precluded examining potential multiple moderators of associations, such as mental health and substance use. Finally, although our study design was prospective in that we examined the cumulative effects of enacted stigma experiences collected over the course of 1 year and retention in care for 18 months, these findings should not be considered causal or directional, given that we did not model temporal associations among variables. With these limitations in mind, we believe that these study findings have implications for designing interventions aimed to address HIV-related stigma, to improve retention in HIV care.
Ameliorating the adverse effects of HIV stigma is a priority in efforts to achieve universal HIV diagnosis, treatment, and prevention goals.8,41 Among people receiving HIV care in the rural southeastern United States, our findings suggest that HIV stigma experiences may have a cumulative effect on retention in care, especially among men, and that stigma from family and acts of discrimination may be of particular importance to address for improving retention in care.
We are not aware of any intervention that has been effective in addressing HIV stigma to improve retention in HIV care. However, interventions have focused on addressing barriers to HIV disclosure in managing stigma more generally, with some approaches demonstrating positive results on health outcomes, including reducing sexual HIV transmission risks, more effective coping, and improvement in mental health.42,43 Interventions have focused on building supportive networks among men at risk for as well as living with HIV to improve engagement in prevention and care services.44 Social media and other electronic communication platforms have also opened avenues for building social support to foster engagement in health care.45 These models may offer a path toward improving HIV care retention for people living in stigmatized environments.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
The study was approved by the University of Connecticut Institutional Review Board Protocol H14-184GDPH and all participants gave written informed consent. This project was supported by National Institute of Alcohol Abuse and Alcoholism Grant R01-AA023727.
References
- 1. Martin M, Del Cacho E, Codina C, et al. . Relationship between adherence level, type of the antiretroviral regimen, and plasma HIV type 1 RNA viral load: A prospective cohort study. AIDS Res Hum Retroviruses 2008;24:1263–1268 [DOI] [PubMed] [Google Scholar]
- 2. Byrd KK, Hou JG, Hazen R, et al. . Antiretroviral adherence level necessary for HIV viral suppression using real-world data. J Acquir Immune Defic Syndr 2019;82:245–251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. CDC. Understanding the HIV Care Continuum. 2020. Available at: https://www.cdc.gov/hiv/pdf/library/factsheets/cdc-hiv-care-continuum.pdf (Last accessed May7, 2020).
- 4. Lee H, Wu XK, Genberg BL, et al. . Beyond binary retention in HIV care: Predictors of the dynamic processes of patient engagement, disengagement, and re-entry into care in a US clinical cohort. AIDS 2018;32:2217–2225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chang EJ, Fleming M, Nunez A, Dombrowski JC. Predictors of successful HIV care re-engagement among persons poorly engaged in HIV care. AIDS Behav 2019;23:2490–2497 [DOI] [PubMed] [Google Scholar]
- 6. Nichols BE, Kissler SM. Ending the HIV epidemic in the USA. Lancet HIV 2020;7:e454–e455 [DOI] [PubMed] [Google Scholar]
- 7. Maulsby C, Jain KM, Weir BW, et al. . Cost-utility of access to care, a national HIV linkage, re-engagement and retention in care program. AIDS Behav 2018;22:3734–3741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sullivan MC, Rosen AO, Allen A, et al. . Falling short of the first 90: HIV stigma and HIV testing research in the 90-90-90 era. AIDS Behav 2020;24:357–362 [DOI] [PubMed] [Google Scholar]
- 9. Treves-Kagan S, Steward WT, Ntswane L, et al. . Why increasing availability of ART is not enough: A rapid, community-based study on how HIV-related stigma impacts engagement to care in rural South Africa. BMC Public Health 2016;16:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Goffman E. Stigma: Notes on the Management of Spoiled Identity, 1st Touchstone ed. New York: Simon & Schuster, 1963. [Google Scholar]
- 11. Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: A systematic review. AIDS Behav 2011;15:1075–1087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: How far have we come? J Int AIDS Soc 2013;16(Suppl 2):18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. van der Straten A, Vernon KA, Knight KR, Gomez CA, Padian NS. Managing HIV among serodiscordant heterosexual couples: Serostatus, stigma and sex. AIDS Care 1998;10:533–548 [DOI] [PubMed] [Google Scholar]
- 14. Fife BL, Wright ER. The dimensionality of stigma: A comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav 2000;41:50–67 [PubMed] [Google Scholar]
- 15. Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Res Nurs Health 2001;24:518–529 [DOI] [PubMed] [Google Scholar]
- 16. Earnshaw VA, Bogart LM, Laurenceau JP, et al. . Internalized HIV stigma, ART initiation and HIV-1 RNA suppression in South Africa: Exploring avoidant coping as a longitudinal mediator. J Int AIDS Soc 2018;21:e25198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Christopoulos KA, Neilands TB, Hartogensis W, et al. . Internalized HIV stigma is associated with concurrent viremia and poor retention in a cohort of US patients in HIV care. J Acquir Immune Defic Syndr 2019;82:116–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS Behav 2009;13:1160–1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Geter A, Sutton MY, Hubbard McCree D. Social and structural determinants of HIV treatment and care among black women living with HIV infection: A systematic review: 2005–2016. AIDS Care 2018;30:409–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Valverde E, Rodriguez A, White B, Guo Y, Waldrop-Valverde D. Understanding the association of internalized HIV stigma with retention in HIV care. J HIV AIDS 2018;4 DOI: 10.16966/2380-5536.159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gonzalez A, Miller CT, Solomon SE, Bunn JY, Cassidy DG. Size matters: Community size, HIV stigma, & gender differences. AIDS Behav 2009;13:1205–1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kalichman S, Katner H, Banas E, Kalichman M. Population density and AIDS-related stigma in large-urban, small-urban, and rural communities of the southeastern USA. Prev Sci 2017;18:517–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kalichman SC, Katner H, Banas E, Hill M, Kalichman MO. HIV-related stigma and non-adherence to antiretroviral medications among people living with HIV in a rural setting. Soc Sci Med 2020;258:113092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Earnshaw V, Kalichman SC. Stigma experienced by people living with HIV/AIDS. In: Liamputtong P, ed. Stigma, Discrimination and Living with HIV/AIDS: A Cross-Cultural Perspective. New York: Springer Science; 2013 [Google Scholar]
- 25. Logie CH, Wang Y, Lacombe-Duncan A, et al. . HIV-related stigma, racial discrimination, and gender discrimination: Pathways to physical and mental health-related quality of life among a national cohort of women living with HIV. Prev Med 2018;107:36–44 [DOI] [PubMed] [Google Scholar]
- 26. Van Dam NT, Earleywine M. Validation of the Center for Epidemiologic Studies Depression Scale—Revised (CESD-R): Pragmatic depression assessment in the general population. Psychiatry Res 2011;186:128–132 [DOI] [PubMed] [Google Scholar]
- 27. Allen JP, Litten RZ, Fertig JB, Babor T. A review of the research on the Alcohol Use Disorders Identification Test (AUDIT). Alcohol Clin Exp Res 1997;21:613–619 [PubMed] [Google Scholar]
- 28. Conigrave KM, Hall WD, Saunders JB. The AUDIT questionnaire: Choosing a cut-off score. Addictions 1995;90:1349–1356 [DOI] [PubMed] [Google Scholar]
- 29. International Advisory Panel on HIVCCO. IAPAC Guidelines for Optimizing the HIV Care Continuum for Adults and Adolescents. J Int Assoc Provid AIDS Care 2015;14(Suppl 1):S3–S34 [DOI] [PubMed] [Google Scholar]
- 30. Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: A test of the HIV stigma framework. AIDS Behav 2013;17:1785–1795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sangaramoorthy T, Jamison AM, Dyer TV. HIV stigma, retention in care, and adherence among older black women living with HIV. J Assoc Nurses AIDS Care 2017;28:518–531 [DOI] [PubMed] [Google Scholar]
- 32. Valenzuela C, Ugarte-Gil C, Paz J, et al. . HIV stigma as a barrier to retention in HIV care at a general hospital in Lima, Peru: A case-control study. AIDS Behav 2015;19:235–245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wohl AR, Galvan FH, Myers HF, et al. . Do social support, stress, disclosure and stigma influence retention in HIV care for Latino and African American men who have sex with men and women? AIDS Behav 2011;15:1098–1110 [DOI] [PubMed] [Google Scholar]
- 34. Earnshaw VA, Reed NM, Watson RJ, Maksut JL, Allen AM, Eaton LA. Intersectional internalized stigma among Black gay and bisexual men: A longitudinal analysis spanning HIV/sexually transmitted infection diagnosis. J Health Psychol 2019. [Epub ahead of print]; DOI: 10.1177/1359105318820101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pachankis JE, Hatzenbuehler ML, Berg RC, et al. . Anti-LGBT and anti-immigrant structural stigma: An intersectional analysis of sexual minority men's HIV risk when migrating to or within Europe. J Acquir Immune Defic Syndr 2017;76:356–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dale SK, Dean T, Sharma R, Reid R, Saunders S, Safren SA. Microaggressions and discrimination relate to barriers to care among black women living with HIV. AIDS Patient Care STDS 2019;33:175–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rice WS, Turan B, Fletcher FE, et al. . A mixed methods study of anticipated and experienced stigma in health care settings among women living with HIV in the United States. AIDS Patient Care STDS 2019;33:184–195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Crockett KB, Edmonds A, Johnson MO, et al. . Neighborhood racial diversity, socioeconomic status, and perceptions of HIV-related discrimination and internalized HIV stigma among women living with HIV in the United States. AIDS Patient Care STDS 2019;33:270–281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Centers for Disease Control and Prevention. HIV/AIDS statistics and surveillance. 2007. Available at: www.cdc.gov/hiv/topics/surveillance/basic.htm#hivaidsexposure (Last accessed July10, 2020).
- 40. Eaton LA, Allen A, Maksut JL, Earnshaw V, Watson RJ, Kalichman SC. HIV microaggressions: A novel measure of stigma-related experiences among people living with HIV. J Behav Med 2020;43:34–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ekstrand ML, Bharat S, Srinivasan K. HIV stigma is a barrier to achieving 90-90-90 in India. Lancet HIV 2018;5:e543–e545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kalichman SC, Rompa D, Cage M, et al. . Effectiveness of an intervention to reduce HIV transmission risks in HIV-positive people. Am J Prev Med 2001;21:84–92 [DOI] [PubMed] [Google Scholar]
- 43. Kalichman SC. The other side of the healthy relationships intervention: Mental health outcomes and correlates of sexual risk behavior change. AIDS Educ Prev 2005;17(Suppl A):66–75 [DOI] [PubMed] [Google Scholar]
- 44. Kegeles S, Hays R, Coates T. The Mpowerment project: A community-level HIV prevention intervention for young gay men. Am J Public Health 1996;86:1129–1136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hightow-Weidman LB, Muessig KE, Pike EC, et al. . HealthMpowerment.org: Building community through a mobile-optimized, online health promotion intervention. Health Educ Behav 2015;42:493–499 [DOI] [PMC free article] [PubMed] [Google Scholar]