Abstract
There is limited research on the effects of stigma on health outcomes among new-to-HIV care individuals. We examined the effect of changes in internalized stigma over time on health behaviors and outcomes such as viral suppression, antiretroviral therapy (ART) adherence, and visit adherence among new-to-HIV care individuals. We also analyzed the mediating effects of adherence self-efficacy and depressive symptoms in these associations. Participants were 186 persons living with HIV who initiated care at four HIV clinical sites in the United States and had diverse geographical and ethnic backgrounds. Baseline and 48-week follow-up assessments included measures of internalized stigma, ART adherence, depressive symptoms, and adherence self-efficacy. HIV visit adherence and viral load data were extracted from clinic records. Age, race, gender, insurance status, and site were controlled in all analyses. Logistic regression analyses were used to examine predictors of adherence and viral suppression. Change (decrease) in internalized stigma was calculated by subtracting follow-up internalized stigma scores from baseline scores and served as the main predictor. Mediation analyses included calculation of 95% confidence intervals for the indirect effects using bootstrapping. Decreases in internalized stigma over time were positively associated with viral suppression, ART adherence, and visit adherence. Adherence self-efficacy significantly mediated these effects of decrease in internalized stigma on all outcomes. Depressive symptoms only mediated the association between decrease in internalized stigma and ART adherence. Interventions that address internalized stigma and depressive symptoms, as well as adherence self-efficacy, may significantly improve adherence and viral suppression outcomes for individuals new to HIV care.
Keywords: internalized stigma, new-to-care, ART adherence, viral suppression, visit adherence
Introduction
Understanding underlying mechanisms of treatment nonadherence and viremia among people living with HIV (PLWH) is important for developing effective interventions. More importantly, for those who are newly initiating HIV medical care, addressing these mechanisms is necessary for achieving viral suppression early,1,2 a crucial requirement for promoting health and longevity for PLWH and for preventing new HIV infections in the population. HIV-related stigma is a major barrier to retention in HIV care, adherence to HIV care visits, and adherence to antiretroviral therapy (ART) among PLWH.3 HIV-related stigma is a social process that involves prejudice, devaluation, discrimination, and other negative attitudes toward PLWH.4,5 Several dimensions of HIV-related stigma have been defined: anticipated, experienced, perceived community, and internalized stigma.6,7 Internalized stigma refers to accepting and endorsing negative attitudes about having HIV and applying those attitudes to oneself.4,7–9 There is a growing body of empirical and theoretical literature suggesting that internalized stigma is a particularly important stigma dimension that negatively affects retention in HIV care, ART adherence, and visit adherence, as well as quality of life and mental health among PLWH.10–14 However, much of extant research on the association between internalized stigma and HIV treatment behaviors and outcomes has been conducted with PLWH who have been in HIV care for many years and focused on ART adherence as the outcome. This study aims to contribute to this growing field of HIV stigma research by elucidating the extent to which changes in internalized HIV stigma over time are related to clinical health outcomes such as viral suppression in addition to ART adherence and visit adherence among individuals new to HIV care.
Effects of stigma may differ depending not only on levels, but also on how stigma changes over time. In addition to between-person differences in levels of stigma at a given point in time, within-person changes in stigma over time may also predict health outcomes among PLWH. Limited research on within-person changes in HIV-related stigma suggests that on average, stigma decreases over time. For instance, research suggests that HIV-related internalized stigma decreases during the first year after HIV diagnosis or over the first 2 years of ART.15,16 Another study also reported that the rate of stigma events experienced by PLWH declined over a period of 12 months.17 A recent study in South Africa reported that internalized stigma decreased over a period of 6 months among both ART initiators and noninitiators, suggesting that internalized stigma may naturally decline slightly over time as a result of processing and adjusting to the HIV diagnosis and gaining social support.18 However, there is limited evidence indicating that changes in stigma over time are associated with health outcomes for PLWH. For example, one study in African countries found that people with decreasing stigma over a period of 1 year reported fewer medication worries.19 For individuals new to HIV care, there is a need for systematic understanding of how changes in internalized stigma over time contribute to viral suppression, ART adherence, and visit adherence.
Additionally, it is important to elucidate specific mediating mechanisms in the association between change in internalized stigma over time and HIV treatment adherence and clinical health outcomes—such as viral suppression—for PLWH new to care. This insight would have implications for future intervention development for this population. Empirical and conceptual work (largely among individuals who have been in treatment for many years) suggests that low self-efficacy and depression are among the most important intrapersonal mechanisms contributing to nonadherence to HIV treatment and care.6,20–27 Thus, the present study aimed to explore the mediating roles of these mechanisms in the effect of internalized HIV-related stigma in a sample of PLWH new to care. Self-efficacy, referred to as one's confidence to behave in a certain way and perform a task28 is one of the major intrapersonal mechanisms in HIV treatment adherence.20,21 The first year for PLWH new to care may be a critical and vulnerable time, as it involves adjusting to a life-changing diagnosis, initiating HIV treatment and care, including regular HIV clinic visits and life-long ART,1,29 which is likely to decrease a person's ability and motivation to consistently engage in HIV care.
Theoretically, internalized stigma may cause PLWH to perceive themselves as inferior, less capable, and less confident in their capacity to adhere to a treatment plan (i.e., low treatment adherence self-efficacy), which in turn may be expected to result in poor adherence to HIV treatment and care.30 Supporting this hypothesis, a study found that treatment self-efficacy mediates the relationship between internalized HIV-related stigma and adherence.11 Again, the first year following entry into HIV care is more likely to bring about adverse psychological health outcomes due to adjusting to living with HIV and the continuum of HIV medical care, potentially posing challenges to treatment adherence and desired clinical outcomes (e.g., viral suppression). Specifically, depression has received increasing attention as an important mediating mechanism in the association between internalized stigma and HIV treatment adherence for PLWH who have been in care for some time.13,31 Thus, there is considerable (although mostly cross-sectional) evidence that internalized stigma can negatively affect HIV treatment adherence through various potential mechanisms among those who have been living with HIV for many years. However, for those newly initiating HIV care, there remains a paucity of evidence on how changes in internalized stigma affects early retention in care, ART adherence, and—most importantly—viral suppression, and on the roles of potential mediating mechanisms in these associations.
To address these gaps in the stigma literature for PLWH new to care, the current study aims to (1) investigate the effects of changes in internalized HIV stigma over time (the difference between baseline and follow-up scores of internalized stigma) on viral suppression, ART adherence, and HIV visit adherence as clinical outcomes and (2) elucidate potential mediating effects of treatment adherence self-efficacy and depressive symptoms in the association between changes in internalized stigma over time and these clinical outcomes. Given that engagement in HIV care and adherence to medications are especially vital among new-to-care HIV patients,32 enhanced knowledge of how internalized stigma and other mediating mechanisms affect early retention in care, ART adherence, and viral suppression can provide important implications for developing and strengthening interventions at this vulnerable time for PLWH.
Methods
Participants and procedures
Participants were 186 PLWH initiating care at four HIV clinical sites in the United States, including Johns Hopkins University, University of Alabama at Birmingham, The University of North Carolina at Chapel Hill, and University of Washington, who participated in a larger study called “integrating ENGagement and Adherence Goals upon Entry (iENGAGE).” The details of this iENGAGE study can be found elsewhere.29,33 Those who previously received outpatient HIV care were excluded from the study. Of the participants, 148 (79.6%) identified as male, 36 (19.4%) as female, and 2 (1.1%) as transgender; 112 (60.2%) were black or African American, 60 (32.3%) white, 14 (7.5%) other race/ethnicity, with a mean age of 36.33 (SD = 12.78). Participants completed baseline and 48-week follow-up measures using a computer-administered self-interview. Data on viral load and visit adherence were obtained from clinical records. The study was approved by the Institutional Review Board at each site.
Measures
Internalized HIV-related stigma
To assess internalized HIV-related stigma, we used the 7-item Negative Self-Image subscale of the HIV Stigma Scale.34 The items (e.g., “I feel guilty because I have HIV/AIDS”) are rated on a Likert-type scale ranging from 1 (strongly disagree) to 4 (strongly agree). Previous evidence demonstrated that this subscale has high internal consistency and test/retest reliability.35 Higher scores indicate higher levels of internalized stigma. In the current study, Cronbach's alpha reliability coefficient was 0.77 for the baseline scores and 0.82 for the follow-up scores.
HIV clinical outcomes
ART adherence
ART adherence was assessed with the single question,36 “Thinking about the past 4 weeks, on average how would you rate your ability to take all of your HIV antiretroviral medications as your doctor prescribed” with response options ranging from very poor to excellent. Previous research suggests that this item is a valid measure of adherence.37 Similar to previous studies using this measure, we employed a cutoff as less than perfect adherence versus perfect adherence—aligned with the robust negative predictive value of any degree of self-reported nonadherence.11
HIV visit adherence
We obtained data on adherence to HIV primary care visits from clinic records and used it as a dichotomized variable, with 1 = adherence to all scheduled visits (optimal adherence), versus 0 = missed at least one visit (suboptimal adherence) in the 48-week study period. Rescheduled visits were not considered as missed visit. This measure has been used successfully in previous research and associated with clinical outcomes and mortality.10
Viral load
Data on viral load were extracted from each participant's last clinic visit. We used it as a dichotomized variable as not suppressed (≥200 c/mL) versus suppressed (<200 c/mL), in accordance with treatment guidelines.
Depressive symptoms
The Patient Health Questionnaire (PHQ-8)38 was used to measure depressive symptoms over the past 2 weeks. The PHQ-8 includes eight items rated on a 4-point Likert-type scale ranging from 0 (not at all) to 3 (nearly every day). Higher scores indicate higher depressive symptomatology. In the current study, Cronbach's alpha was 0.91.
Treatment adherence self-efficacy
To assess self-efficacy in relation to treatment adherence, we used the HIV Treatment Self-Efficacy Scale.20 The scale has 12 items (e.g., “Integrate your treatment into your daily routine?”) rated on a 10-point rating scale ranging from 1 (cannot do it all) to 10 (certain can do it). In the current study, this measure showed high internal consistency (Cronbach's α = 0.95).
Statistical analyses
First, a series of binary logistic regression analyses were performed to determine predictors of viral suppression, ART adherence, and visit adherence. A score for “decrease in internalized stigma” was calculated for each participant by subtracting follow-up internalized stigma from baseline internalized stigma. Decrease in internalized HIV stigma was the primary independent variable and covariates included age, race, gender, insurance status, and site. Second, mediation models were used to test whether the significant associations between decrease in internalized HIV stigma and outcome variables (viral suppression, ART adherence, visit adherence) were mediated by treatment adherence self-efficacy and depressive symptoms. Follow-up scores at 48 weeks were used for both mediator and outcome variables. The average length of time between the data collection at the 48-week assessment and the final viral load was 21 days. We calculated 95% confidence intervals (CIs) with 2000 bootstrap samples for indirect effects using PROCESS procedure. In this procedure, if the CI does not include the value zero, the indirect effect is significant, suggesting mediation.39 The covariates of age, race, gender, insurance status, and site were also controlled in all of the mediation analyses. The data were analyzed using the Statistical Package for the Social Sciences (version 22; SPSS, Inc., Chicago, IL).
Results
Descriptive statistics of the sample are presented in Table 1. Decrease in internalized HIV stigma was a significant predictor of viral suppression [adjusted odds ratio (AOR) = 8.48, p = 0.006, 95% CI (1.83–39.28)]. Similarly, decrease in internalized HIV stigma was a significant predictor of ART adherence [AOR = 2.05, p = 0.033, 95% CI (1.06–3.98)] as well as of visit adherence [AOR = 2.17, p = 0.028, 95% CI (1.09–4.35)]. Of the covariates, only age was significantly associated with viral suppression (B = 0.09, SE = 0.04) and with visit adherence (B = 0.04, SE = 0.02), but not with ART adherence (B = 0.02, SE = 0.02).
Table 1.
Descriptive Statistics
| N | % | |
|---|---|---|
| Race | ||
| Black or African American | 112 | 60.2 |
| White | 60 | 32.3 |
| Other | 14 | 7.5 |
| Gender | ||
| Male | 148 | 79.6 |
| Female | 36 | 19.4 |
| Transgender | 2 | 1.1 |
| Ethnicity | ||
| Hispanic | 12 | 6.5 |
| Non-Hispanic | 174 | 93.5 |
| Insurance | ||
| Public | 92 | 49.5 |
| Private | 53 | 28.5 |
| None | 41 | 22 |
| Site | ||
| JHU | 39 | 21 |
| UAB | 77 | 41.4 |
| UNC | 38 | 20.4 |
| UW | 32 | 17.2 |
| Mean | SD | |
| Age | 36.22 | 12.78 |
| Internalized stigma | 2.31 (2.23) | 0.74 (0.77) |
| Depressive symptoms | 5.77 | 5.79 |
| Treatment adherence self-efficacy | 9.05 | 1.50 |
The values in parentheses are for internalized stigma at follow-up.
JHU, Johns Hopkins University; UAB, University of Alabama at Birmingham; UNC, The University of North Carolina at Chapel Hill; UW, University of Washington.
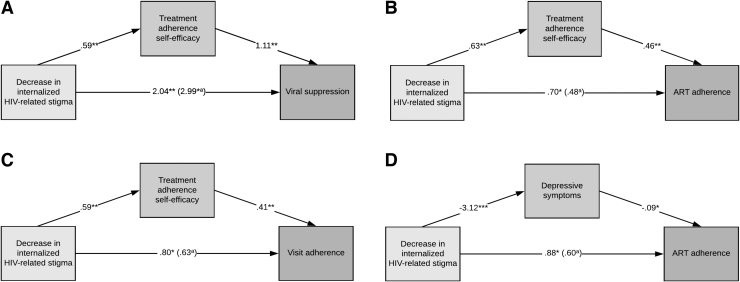
Next, we tested the mediating effect of treatment adherence self-efficacy in the association between decrease in internalized HIV stigma and our outcomes (viral suppression, ART adherence, and visit adherence). The indirect effect of decrease in internalized HIV stigma on all three outcomes through increases in treatment adherence self-efficacy was significant, suggesting mediation [B = 0.65, SE = 0.53, 95% CI (0.12–2.23); B = 0.29, SE = 0.18, 95% CI (0.05–0.76); B = 0.24, SE = 0.15, 95% CI (0.05–0.62), respectively for viral suppression, ART adherence, and visit adherence; Fig. 1A–C]. We also tested the mediating effect of depressive symptoms in the association between decrease in internalized HIV stigma and viral suppression, ART adherence, and visit adherence as outcome variables. These analyses yielded nonsignificant indirect effects on viral suppression [B = 0.26, SE = 0.43, 95% CI (−0.54 to 1.19)] and visit adherence [B = 0.12, SE = 0.16, 95% CI (−0.21 to 0.47)], but a significant indirect effect on ART adherence [B = 0.28, SE = 0.18, 95% CI (0.03–0.76); Fig. 1D].
FIG. 1.
(A–D) Treatment adherence self-efficacy and depressive symptoms mediate the effect of decrease in internalized HIV-related stigma on viral suppression, ART adherence, and visit adherence. aWhen treatment adherence self-efficacy or depressive symptoms are in the model. *p < 0.05, **p < 0.01 (N = 137, 126, 146, and 119 for A–D, respectively). ART, antiretroviral therapy.
Discussion
Previous studies suggest that internalized HIV-related stigma is associated with poorer medication adherence, missed clinic visits, and lower utilization of HIV care, which largely leads to undesired clinical outcomes, including detectable viral load among PLWH.10,13,40 However, most research examining these associations is based on either qualitative or cross-sectional data obtained from individuals who have been living with HIV for many years. Results from our current analyses suggest that a decrease in internalized HIV-related stigma over the first year in medical care is a significant predictor of viral suppression, ART adherence, and visit adherence. Thus, during the first year following entry into HIV care, when PLWH adjust to living with HIV and engage in HIV care, it seems essential that internalized HIV-related stigma be addressed to improve health outcomes for PLWH.
We also found that decrease in internalized HIV-related stigma over time contributes to increased levels of treatment adherence self-efficacy, which in turn results in positive impacts on viral suppression, ART adherence, and visit adherence. This finding is consistent with earlier findings that low adherence self-efficacy mediates the association between internalized stigma and poorer ART adherence for individuals who have been living with HIV for many years.11,31 Initiating HIV treatment and care can be an overwhelming process, which includes adjustment to living with HIV (a lifetime commitment), decisions about disclosure of HIV status to others, initiation of ART, taking HIV medications daily and regularly, and attending regular HIV clinic visits.1,41,42 Results suggest that PLWH who internalize HIV-related stigma have lower confidence in their ability to adhere to treatment regimen, leading to lower medication adherence, missed clinic visits, and eventually viremia.
Another important finding of this study was that depressive symptoms mediate the association between decrease in internalized HIV stigma and ART adherence, suggesting that decreases in internalized HIV-related stigma may lead to lower levels of depressive symptoms, which in turn can positively affect adherence to ART. This finding is also in agreement with previous studies, which have suggested that the associations between internalized stigma and HIV-related health outcomes may work through the pathway of depression.31,43
An understanding of these associations and mechanisms has the potential to inform interventions to maximize their impacts on retention in care, ART adherence, and viral suppression, and also help mitigate the psychological and physical sequelae of internalized HIV-related stigma for PLWH. The results of the present study suggest that in addition to addressing internalized HIV-related stigma, interventions can also target treatment adherence self-efficacy and depressive symptoms to enhance adherence to care and viral suppression. Blocking the path from internalized stigma to depressive symptoms or adherence self-efficacy, or blocking the path from low self-efficacy or depressive symptoms to HIV-related health behaviors and outcomes may also be useful intervention strategies. For instance, at the individual level, cognitive-behavioral therapy (CBT) can be particularly effective in decreasing internalized stigma and depressive symptoms, as well as building skills for HIV treatment adherence, and promoting medication adherence among PLWH.44–46 Moreover, targeted interventions with strategies to help with safe HIV disclosure and building social support, which are important to the development of self-efficacy,28,47 may be effective in developing adaptive health behaviors and outcomes, such as improved medication adherence and viral suppression.
Even though individual counseling or therapies such as CBT are likely to be useful, they place the burden of ending HIV stigma on the individual and do not address social and structural drivers of stigma.48,49 Thus, community- or structural-level approaches, including national communication campaigns,50 mass media programs,51,52 support groups,53,54 personal contact with PLWH programs,53,55 faith- or church-based interventions,56,57 public health programs,58 and stigma-reduction interventions in health care settings,59,60 can be effective in reducing HIV-related stigma.53,61 Lastly, even though internalized stigma tends to decrease over time,15,16,18 the first year of HIV care is of crucial importance in engaging in HIV care and developing adherence skills.29,33 As such, targeting HIV-related stigma immediately after initial entry into HIV care among PLWH using appropriate approaches may contribute to facilitating treatment adherence and retention in care, and thereby to achieving desired clinical outcomes (e.g., viral suppression).
It is important to note that the association between internalized HIV-related stigma and depression may be bidirectional.13 There may be other potential mechanisms (e.g., other dimensions or sources of stigma) that could explain the association between internalized stigma and viral suppression and visit adherence. Research focusing on mediating mechanisms of different types and dimensions of stigma would significantly contribute to our understanding of what psychosocial components should be included in interventions to reduce internalized stigma and associated negative effects on health outcomes.
The current study has several limitations. First, we used a self-report measure for ART adherence, which may be subject to reporting and social desirability biases. Furthermore, in mediation analyses, it is likely that there are unobserved potential confounders and mediator variables associated with both observed mediators and outcome variables. Thus, future studies would add to our understanding of other mechanisms which mediate the effects of internalized stigma on health outcomes. Finally, the participants of the study were recruited from four sites affiliated with major academic health centers, which are not representative of all PLWH in the United States. Therefore, our results only may be generalized to PLWH in similar clinical settings. On the other hand, it is a strength that participants in our sample had diverse geographical and ethnic backgrounds.
Overall, the present study suggests that during the first year following initial entry into HIV care, decrease in internalized HIV-related stigma contributes to HIV treatment adherence and viral suppression, mediated through increased treatment adherence self-efficacy and depressive symptoms. This information can be used for future intervention development and medical and supportive service provision, particularly within a period when PLWH are initiating HIV treatment process.
Author Contributions
All authors contributed to the study conception and design. Data analyses were performed by (B.T.) and (I.Y.). The first draft of the article was written by (I.Y. and B.T.) and all authors contributed to the article. All authors read and approved the final article.
Author Disclosure Statement
M.J.M. has received grant support (to the University of Alabama at Birmingham) from Merck Foundation and consulting fees from Gilead Sciences. The remaining authors declare no conflict of interest.
Funding Information
This work was supported by the National Institutes of Allergy and Infectious Diseases (NIAID) [Grant Nos. R01AI103661 and 3R01AI103661-03S1]. This research was also supported by the University of Alabama at Birmingham (UAB) Center for AIDS Research CFAR, and a National Institutes of Health funded program [P30 AI027767] that was made possible by the following institutes: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIDDK, NIGMS, and OAR.
References
- 1. Mugavero MJ, Amico KR, Westfall AO, et al. Early retention in HIV care and viral load suppression: Implications for a test and treat approach to HIV prevention. J Acquir Immune Defic Syndr 2012;59:86–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gardner EM, McLees MP, Steiner JF, et al. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis 2011;52:793–800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Katz IT, Ryu AE, Onuegbu AG, et al. Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. J Int AIDS Soc 2013;16:18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS Behav 2009;13:1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Herek GM, Capitanio JP. AIDS stigma and contact with persons with AIDS: Effects of direct and vicarious contact. J Appl Soc Psychol 1997;27:1–36 [Google Scholar]
- 6. Turan B, Hatcher AM, Weiser SD, et al. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. Am J Public Health 2017;107:863–869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Earnshaw VA, Smith LR, Chaudoir SR, et al. HIV stigma mechanisms and well-being among PLWH: A test of the HIV stigma framework. AIDS Behav 2013;17:1785–1795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Res Nurs Health 2001;24:518–529 [DOI] [PubMed] [Google Scholar]
- 9. Crockett KB, Edmonds A, Johnson MO, et al. Neighborhood racial diversity, socioeconomic status, and perceptions of HIV-related discrimination and internalized HIV stigma among women living with HIV in the United States. AIDS Patient Care STDS 2019;33:270–281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rice WS, Crockett KB, Mugavero MJ, et al. Association between internalized HIV-related stigma and HIV care visit adherence. J Acquir Immune Defic Syndr 2017;76:482–487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Seghatol-Eslami VC, Dark H, Raper JL, et al. Interpersonal and intrapersonal factors as parallel independent mediators in the association between internalized HIV stigma and ART adherence. J Acquir Immune Defic Syndr 2017;74:e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sweeney SM, Vanable PA. The association of HIV-related stigma to HIV medication adherence: A systematic review and synthesis of the literature. AIDS Behav 2016;20:29–50 [DOI] [PubMed] [Google Scholar]
- 13. Turan B, Smith W, Cohen MH, et al. Mechanisms for the negative effects of internalized HIV-related stigma on antiretroviral therapy adherence in women: The mediating roles of social isolation and depression. J Acquir Immune Defic Syndr 2016;72:198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Christopoulos KA, Neilands TB, Hartogensis W, et al. Internalized HIV stigma is associated with concurrent viremia and poor retention in a cohort of US patients in HIV care. J Acquir Immune Defic Syndr 2019;82:116–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Earnshaw VA, Reed NM, Watson RJ, et al. Intersectional internalized stigma among Black gay and bisexual men: A longitudinal analysis spanning HIV/sexually transmitted infection diagnosis. J Health Psychol 2019. DOI: 10.1177/1359105318820101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tsai AC, Bangsberg DR, Bwana M, et al. How does antiretroviral treatment attenuate the stigma of HIV? Evidence from a cohort study in rural Uganda. AIDS Behav 2013;17:2725–2731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Holzemer WL, Makoae LN, Greeff M, et al. Measuring HIV stigma for PLHAs and nurses over time in five African countries. SAHARA J 2009;6:76–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chan BT, Maughan-Brown BG, Bogart LM, et al. Trajectories of HIV-related internalized stigma and disclosure concerns among art initiators and noninitiators in South Africa. Stigma Health 2019;4:433–441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dlamini PS, Wantland D, Makoae LN, et al. HIV stigma and missed medications in HIV-positive people in five African countries. AIDS Patient Care STDS 2009;23:377–387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Johnson MO, Neilands TB, Dilworth SE, et al. The role of self-efficacy in HIV treatment adherence: Validation of the HIV Treatment Adherence Self-Efficacy Scale (HIV-ASES). J Behav Med 2007;30:359–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Turan B, Fazeli PL, Raper JL, et al. Social support and moment-to-moment changes in treatment self-efficacy in men living with HIV: Psychosocial moderators and clinical outcomes. Health Psychol 2016;35:1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Catz SL, Kelly JA, Bogart LM, et al. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychol 2000;19:124. [PubMed] [Google Scholar]
- 23. Gonzalez JS, Batchelder AW, Psaros C, et al. Depression and HIV/AIDS treatment nonadherence: A review and meta-analysis. J Acquir Immune Defic Syndr 2011;58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Holzemer WL, Corless IB, Nokes KM, et al. Predictors of self-reported adherence in persons living with HIV disease. AIDS Patient Care STDS 1999;13:185–197 [DOI] [PubMed] [Google Scholar]
- 25. Wagner GJ, Goggin K, Remien RH, et al. A closer look at depression and its relationship to HIV antiretroviral adherence. Ann Behav Med 2011;42:352–360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Malta M, Magnanini MM, Strathdee SA, et al. Adherence to antiretroviral therapy among HIV-infected drug users: A meta-analysis. AIDS Behav 2010;14:731–747 [DOI] [PubMed] [Google Scholar]
- 27. Rice WS, Turan B, Fletcher FE, et al. A mixed methods study of anticipated and experienced stigma in health care settings among women living with HIV in the United States. AIDS Patient Care STDS 2019;33:184–195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bandura A. Human agency in social cognitive theory. Am Psychol 1989;44:1175–1184 [DOI] [PubMed] [Google Scholar]
- 29. Modi R, Amico K, Knudson A, et al. Assessing effects of behavioral intervention on treatment outcomes among patients initiating HIV care: Rationale and design of iENGAGE intervention trial. Contemp Clin Trials 2018;69:48–54 [DOI] [PubMed] [Google Scholar]
- 30. Johnson MO, Chesney MA, Goldstein RB, et al. Positive provider interactions, adherence self-efficacy, and adherence to antiretroviral medications among HIV-infected adults: A mediation model. AIDS Patient Care STDS 2006;20:258–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. DiIorio C, McCarty F, DePadilla L, et al. Adherence to antiretroviral medication regimens: A test of a psychosocial model. AIDS Behav 2009;13:10–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ulett KB, Willig JH, Lin H-Y, et al. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS 2009;23:41–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yigit I, Modi RA, Weiser SD, et al. Effects of an intervention on internalized HIV-related stigma for individuals newly entering HIV care. AIDS 2020;34:S73–S82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bunn JY, Solomon SE, Miller C, et al. Measurement of stigma in people with HIV: A reexamination of the HIV Stigma Scale. AIDS Educ Prev 2007;19:198–208 [DOI] [PubMed] [Google Scholar]
- 35. Varni SE, Miller CT, Solomon SE. Sexual behavior as a function of stigma and coping with stigma among people with HIV/AIDS in rural New England. AIDS Behav 2012;16:2330–2339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lu M, Safren SA, Skolnik PR, et al. Optimal recall period and response task for self-reported HIV medication adherence. AIDS Behav 2008;12:86–94 [DOI] [PubMed] [Google Scholar]
- 37. Feldman B, Fredericksen R, Crane P, et al. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS Behav 2013;17:307–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kroenke K, Strine TW, Spitzer RL, et al. The PHQ-8 as a measure of current depression in the general population. J Affect Disord 2009;114:163–173 [DOI] [PubMed] [Google Scholar]
- 39. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Publications, 2017 [Google Scholar]
- 40. Sayles JN, Wong MD, Kinsler JJ, et al. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med 2009;24:1101–1108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kay ES, Batey DS, Mugavero MJ. The HIV treatment cascade and care continuum: Updates, goals, and recommendations for the future. AIDS Res Ther 2016;13:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lambert CC, Tarver WL, Musoke PL, et al. Complexities of HIV disclosure in patients newly entering HIV care: A qualitative analysis. J Assoc Nurses AIDS Care 2020;31:208–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Turan B, Rice WS, Crockett KB, et al. Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: The mediating role of depression. AIDS 2019;33:571–576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Safren SA, O'Cleirigh C, Tan JY, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychol 2009;28:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wagner GJ, Kanouse DE, Golinelli D, et al. Cognitive-behavioral intervention to enhance adherence to antiretroviral therapy: A randomized controlled trial (CCTG 578). AIDS 2006;20:1295–1302 [DOI] [PubMed] [Google Scholar]
- 46. Tshabalala J, Visser M. Developing a cognitive behavioural therapy model to assist women to deal with HIV and stigma. South Afr J Psychol 2011;41:17–28 [Google Scholar]
- 47. Godin G, Cote J, Naccache H, et al. Prediction of adherence to antiretroviral therapy: A one-year longitudinal study. AIDS Care 2005;17:493–504 [DOI] [PubMed] [Google Scholar]
- 48. Pantelic M, Sprague L, Stangl AL. It's not “all in your head”: Critical knowledge gaps on internalized HIV stigma and a call for integrating social and structural conceptualizations. BMC Infect Dis 2019;19:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Heijnders M, Van Der Meij S. The fight against stigma: An overview of stigma-reduction strategies and interventions. Psychol Health Med 2006;11:353–363 [DOI] [PubMed] [Google Scholar]
- 50. Boulay M, Tweedie I, Fiagbey E. The effectiveness of a national communication campaign using religious leaders to reduce HIV-related stigma in Ghana. Afr J AIDS Res 2008;7:133–141 [DOI] [PubMed] [Google Scholar]
- 51. Creel A, Rimal R, Mkandawire G, et al. Effects of a mass media intervention on HIV-related stigma: ‘Radio Diaries’ program in Malawi. Health Educ Res 2011;26:456–465 [DOI] [PubMed] [Google Scholar]
- 52. Kerr JC, Valois RF, DiClemente RJ, et al. The effects of a mass media HIV-risk reduction strategy on HIV-related stigma and knowledge among African American adolescents. AIDS Patient Care STDS 2015;29:150–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: What have we learned? AIDS Educ Prev 2003;15:49–69 [DOI] [PubMed] [Google Scholar]
- 54. Mburu G, Ram M, Skovdal M, et al. Resisting and challenging stigma in Uganda: The role of support groups of people living with HIV. J Int AIDS Soc 2013;16:18636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Chan BT, Tsai AC. Personal contact with HIV-positive persons is associated with reduced HIV-related stigma: Cross-sectional analysis of general population surveys from 26 countries in sub-Saharan Africa. J Int AIDS Soc 2017;20:21395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Berkley-Patton JY, Moore E, Berman M, et al. Assessment of HIV-related stigma in a US faith-based HIV education and testing intervention. J Int AIDS Soc 2013;16:18644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Derose KP, Griffin BA, Kanouse DE, et al. Effects of a pilot church-based intervention to reduce HIV stigma and promote HIV testing among African Americans and Latinos. AIDS Behav 2016;20:1692–1705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Klein SJ, Karchner WD, O'Connell DA. Interventions to prevent HIV-related stigma and discrimination: Findings and recommendations for public health practice. J Public Health Manag Pract 2002;8:44–53 [DOI] [PubMed] [Google Scholar]
- 59. Li L, Lin C, Guan J, Wu Z. Implementing a stigma reduction intervention in healthcare settings. J Int AIDS Soc 2013;16:18710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wu S, Li L, Wu Z, et al. A brief HIV stigma reduction intervention for service providers in China. AIDS Patient Care STDS 2008;22:513–520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Stangl AL, Grossman CI. Global action to reduce HIV stigma and discrimination. J Int AIDS Soc 2013;16(Suppl 2):18881. [DOI] [PMC free article] [PubMed] [Google Scholar]