Abstract
Dysfunction of the SWI/SNF complex has been observed in various cancers including urothelial carcinomas. However, the clinical impact of the SWI/SNF complex in squamous-differentiated bladder cancers (sq-BLCA) remains unclear. Therefore, we aimed to analyze potential expression loss and genetic alterations of (putative) key components of the SWI/SNF complex considering the co-occurrence of genetic driver mutations and PD-L1 expression as indicators for therapeutic implications. Assessment of ARID1A, SMARCA2, SMARCA4, SMARCB1/INI1, SMARCC1, SMARCC2 and PBRM1 mutations in a TCGA data set of sq-BLCA (n = 45) revealed that ARID1A was the most frequently altered SWI/SNF gene (15%) while being associated with protein downregulation. Genetic alterations and loss of ARID1A were confirmed by Targeted Next Generation Sequencing (NGS) (3/6) and immunohistochemistry (6/116). Correlation with further mutational data and PD-L1 expression revealed co-occurrence of ARID1A loss and TP53 mutations, while positive correlations with other driver mutations such as PIK3CA were not observed. Finally, a rare number of sq-BLCA samples were characterized by both ARID1A protein loss and strong PD-L1 expression suggesting a putative benefit upon immune checkpoint inhibitor therapy. Hence, for the first time, our data revealed expression loss of SWI/SNF subunits in sq-BLCA, highlighting ARID1A as a putative target of a small subgroup of patients eligible for novel therapeutic strategies.
Keywords: SWI/SNF complex, ARID1A, squamous bladder cancer, immune checkpoint inhibitors
1. Introduction
In 2018, bladder cancer was the 10th most common cancer worldwide, with estimated 549,000 new cases and 200,000 deaths. It is more common in men than in women, with respective incidence and mortality rates of 9.6 and 3.2 per 100,000 men, about four times those of women globally [1]. Furthermore, bladder cancer is the second most common genitourinary malignancy [2]. The most significant risk factor is age and the median age at diagnosis is 70 years [3]. Because of the demographic change, it can be assumed that the number of new cases will increase in the near future. Over 90% of bladder cancers are urothelial carcinomas with distinct molecular characteristics for muscle-invasive bladder cancers (MIBCs) such as TP53 mutations or non-muscle-invasive bladder cancers (NMIBCs) including activating FGFR3 mutations or PIK3CA alterations [3]. Only 5% of all bladder cancers are squamous cell carcinomas (SCCs) [4] characterized by low frequent alterations of ERBB genes but frequent TP53 mutations, while alterations of the FGFR3 gene are rare but associated with worse patients’ outcome [5,6]. SCCs are mostly diagnosed in the seventh decade of life and are commonly associated with poor prognosis. Usually SCC presents at an advanced stage with an average death within 1 to 3 years [7,8]. The leading cause of SCC worldwide is a chronic infection with Schistosoma haematobium. While SCC is the predominant histological type of bladder cancer in countries where schistosomiasis is endemic—such as Egypt, Algeria, Uganda or Zimbabwe—it is rare in western countries. However, due to preventive measures and improved treatment of bilharziosis, the number of SCC in endemic areas also has decreased within the past 20 years [9]. In western countries, chronic infections and irritations appear to be the main cause of non-schistosomiasis-associated SCC. It occurs in patients with chronic inflammatory disorders of the bladder, persistent calculi, chronic cystitis and bladder diverticuli [10].
Switch/sucrose-nonfermenting (SWI/SNF) complexes are members of the chromatin-remodeling family. To date, 29 components have been identified involved in assembling three different SWI/SNF complexes—i.e., the canonical BRG1/BRM-associated factor (cBAF), the polybromo-associated BAF (PBAF) and the recently described non-canonical BAF (ncBAF) complex [11,12]. While distinct subunits are commonly found in all three SWI/SNF protein complexes (referred to as “shared”—e.g., SMARCA4) or at least part of the BAF and/or PBAF complex (e.g., SMARCC2), there are also subcomplex-specific members such as ARID1A (BAF-specific) [11,13]. In general, SWI/SNF complexes play a central role in cellular processes such as transcription, cell cycle control, proliferation, differentiation and repair of DNA lesions [14]. Furthermore, mutations and loss of expression of central SWI/SNF proteins were found in over 20% of different neoplasms, such as oesophageal adenocarcinoma, lung cancer, ovarian clear cell and endometrioid cancers as well as uterine endometrioid carcinomas [14,15,16,17]. Underlying mechanisms are not fully understood; however, several components of the SWI/SNF are thought to function as tumor suppressors [18]. In addition, loss of SWI/SNF subunits, in particular of ARID1A, is of interest with regard to the development of novel therapeutic strategies [19,20,21,22,23,24,25,26,27] mostly based on synthetic lethality—i.e., affecting only those cancer cells that are characterized by functional loss of two genes leading to cell death, whereas individual alterations alone are compatible with viability [28,29].
Among the identified subunits to date, the AT-rich interactive domain-containing protein 1A (ARID1A) is the most frequently mutated SWI/SNF component in urothelial bladder cancer [30]. Loss of ARID1A expression is associated with higher stage and more aggressive variants of urothelial carcinomas. Therefore, low expression of ARID1A appears to be an indicator of poor survival [31]. The role of SWI/SNF in squamous cell carcinomas of the urinary bladder has not yet been investigated. Since standard chemo- or immunotherapy for advanced, metastasized squamous bladder cancer is of limited success, the knowledge of SWI/SNF alteration-mediated therapeutic vulnerabilities might offer a chance to develop more effective therapeutic strategies.
2. Materials and Methods
2.1. Patient Samples and Tissue Microarrays
Squamous differentiated bladder cancers were retrospectively collected from pathology archives of the German Study Group of bladder cancer (n = 68 pure, n = 48 Mixed) over 17 years (1998–2015). For cohort characteristics see Table 1. Tissue microarrays of formalin-fixed paraffin-embedded (FFPE) surgical specimens were used as previously described [32,33,34]. The RWTH University Hospital Aachen local ethics committee approved the retrospective, pseudonymized study of archival tissues (RWTH EK 009/12).
Table 1.
Clinicopathological and demographical characteristics of the study cohort.
| Categorization | ∑ | n SCC | n MIX-SCC | |
|---|---|---|---|---|
| Parameter: | ||||
| Age at diagnosis | median 67.5 years | |||
| (range 33–91 years) | ||||
| ≤67.5 years | 59 | 38 | 21 | |
| >67.5 years | 57 | 30 | 27 | |
| Gender | Female | 59 | 34 | 23 |
| Male | 56 | 33 | 25 | |
| unknown | 1 | 1 | 0 | |
| Histological tumor grade | G1 | 1 | 1 | 0 |
| G2 | 34 | 25 | 9 | |
| G3 | 77 | 40 | 37 | |
| G4 | 2 | 0 | 2 | |
| unknown | 2 | 2 | 0 | |
| Tumor stage | pTx | 5 | 5 | 0 |
| pT1 | 1 | 1 | 0 | |
| pT2 | 16 | 12 | 4 | |
| pT3 | 76 | 37 | 39 | |
| pT4 | 18 | 13 | 5 | |
| Lymph node status | Negative (pN0) | 72 | 41 | 31 |
| Positive (pN1 + pN2) | 22 | 11 | 11 | |
| unknown | 22 | 16 | 6 |
2.2. Immunohistochemistry
Overall, TMAs used in this study comprise two 1.5 mm cores of different tumor areas for each patient tumor sample. For anti-ARID1A stainings, TMA sections were pretreated with DAKO PT-Link heat induced antigen retrieval with high pH (pH9) Target Retrieval Solution (DAKO, Hamburg, Germany), incubated for 60 min at room temperature with anti-ARID1A (1:250, D2A8U, Cell Signaling) as previously specified [30]. An EnVision FLEX/HRP detection system and counterstaining with EnVision FLEX Hematoxylin were applied. For stainings of further components of the SWI/SNF complex, the BenchMark ULTRA system (Ventana Medical Systems Inc, 1910 Innovation Park Drive, Tucson, AZ, USA) and antibodies against the following antigens were used: anti-SMARCB1 (INI1) (ZSI1, 1:50, Zytomed), anti-SMARCA2 (polyclonal antibody, 1:100, Atlas Antibodies AB, Stockholm, Sweden), anti-SMARCA4 (anti-BRG1 antibody, clone EPNCIR111A, 1:100, Abcam; Cambridge, UK), anti-SMARCC1 (HPA026853, 1:50, Atlas Antibodies AB), anti-SMARCC2 (HPA021213, 1:50, Atlas Antibodies AB) and anti-PBRM1 (clone CL0331, dilution 1:50, Atlas Antibodies AB). Immunohistochemical stainings were evaluated by two medical doctors/one senior specialist in uropathology (F.A. and N.T.G.). Staining intensities (0 = no staining, 1 = weak staining, 2 = moderate staining, 3 = strong staining) and percentages of positive stained viable tumor cells according to the system of Remmele and Stegner were reported [35]. Strong nuclear staining of accompanying stromal fibroblasts, inflammatory cells, vascular endothelial cells or normal epithelial cells served as internal positive control. If normal (inflammatory) cells showed only weak expression, immunohistochemical staining was repeated on a second TMA section. Finally, cases with absent or very weak staining in normal lymphocytes after repeated staining were excluded.
2.3. DNA Extraction
DNA extraction of FFPE tissue samples (n = 69 samples) was performed using a QIAamp DNA Mini Kit (Qiagen, Hilden, Germany) as previously described [36]. For Targeted Next Generation Sequencing (NGS) analyses, DNA was isolated from FFPE tissue (n = 6) using the automated Maxwell 16 system and corresponding FFPE Tissue LEV DNA Purification Kit (Promega, Mannheim, Germany) according to the manufacturer’s instructions.
2.4. SNaPshot and Sanger Sequencing
PIK3CA and FGFR3 mutational analyses were performed using the SNaPshot method for the simultaneous detection of hotspot mutations according to Hurst et al. [37] and as described previously [38]. PCR-amplification and Sanger sequencing was performed for TP53 and CDKN2A as specified in 2016 [6]. For details of primer sequences and PCR conditions see Supplementary Table S1.
2.5. Targeted Next Generation Sequencing (NGS) Analysis
Targeted NGS was conducted for n = 6 samples to evaluate the ARID1A, SMARCA4 and SMARCB1 mutation status. Tumor cellularity was >20% for all samples. For library preparation, between 45 and 55 ng DNA were used. However, DNA quality assessment (GeneRead DNA QuantiMIZE Assay Kit, Qiagen, Hilden, Germany) revealed sufficient quality for only five samples. Libraries were generated using the AmpliSeq for Illumina Comprehensive Panel v3 (Illumina, San Diego, USA; reference genome hg19), according to the manufacturer’s instructions. Normalized libraries were sequenced on a NextSeq 500 platform (Illumina, San Diego, CA, USA) using a NextSeq 500/550 Mid Output kit (2 × 150 cycles; Illumina). Bam-file generation was performed with the DNA amplicon module version 1.0.2.1415 (Illumina, San Diego, CA, USA). Single-nucleotide variant analysis was conducted using Sequence Pilot Software version 5.1.0 (SeqNext module; JSI Medical Systems, Ettenheim, Germany). A virtual panel was created to analyze the coding and adjacent intronic regions of ARID1A, SMARCA4 and SMARCB1 (reference sequences: ARID1A: HGNC:11110, RefSeq: NM_006015.6; SMARCA4: HGNC:11100, RefSeq: NM_003072.3; SMARCB1: HGNC:11103, RefSeq: NM_003073.4). Changes with an allele frequency above 10% were taken into account if not already classified as known artifacts for the panel. Further variant filtering was conducted as follows: Missense variants with an allele frequency >2% in the normal population (according to 1000 Genomes (http://www.internationalgenome.org, last accessed 2nd September 2019) or dbSNP v153 (https://www.ncbi.nlm.nih.gov/snp, last accessed 27 September 2019)) and non-splicing–relevant silent, untranslated region (UTR) and intronic variants not affecting the canonical splice-site were considered benign. Additionally, we excluded missense variants classified as benign or likely benign in the ClinVar database (https://www.ncbi.nlm.nih.gov/clinvar, last accessed 27 September 2019). A possible effect of mutations on splicing was determined using Alamut software (Alamut VISUAL v2.14.0, SOPHiA interactive biosoftware, Rouen, France) (included splicing predictions: SpliceSiteFinder-like, MaxEntScan, NNSPLICE 0.9, GeneSplicer; for detailed information see software documentation). For ARID1A, SMARCA4 and SMARCB1 copy number variation (CNV) analysis, an in-house algorithm (validated using three NGS panels; >150 samples) was used. The ACopy tool is based on an exponential growth model for amplification of PCR products [39].
2.6. Analysis of the TCGA Sq-BLCA Data Set
To identify mutations for seven genes of the SWI/SNF-complex of SCC in the TCGA-BLCA cohort [40] we extracted the patient IDs for samples classified as “NOS with squamous differentiation” (n = 42) and “Squamous cell carcinoma” (n = 3) based on the pathologic classification described by Robertson et al. [40]. No further publicly available platforms providing additional squamous bladder cancer data sets exist. Not without reason, in particular pure, non-schistosomiasis-associated SCC is a rare disease in the western world, with very low incidence rates (e.g., 0.6–1.2 per 100,000 person-years) [41]. Assessment of genetic alterations and the mutation spectrum was performed using cBioPortal (https://www.cbioportal.org/, [42,43]) filtering for the extracted patient IDs.
2.7. Statistical Analysis
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) software version 26.0 (SPSS inc., Chicago, IL, USA). p-values < 0.05 were considered significant. Statistical associations between clinico-pathological and molecular factors were determined by Fisher’s exact test. Survival curves for recurrence-free (RFS) and overall survival (OS) were calculated using the Kaplan–Meier method with log-rank statistics. RFS/OS was measured from surgery until relapse/death and was censored for patients alive without evidence of relapse/death at the last follow-up date. Correlation analysis was performed by calculating a Spearman’s rank correlation coefficient. The Expression correlation network was plotted using the R package “Rgraphviz” [44], and significant correlations (Spearman correlation coefficient, p < 0.05) between subunits were plotted as edges.
3. Results
3.1. Analysis of Frequently Altered Subunits of the BAF and PBAF SWI/SNF Complexes in TCGA Sq-BLCA
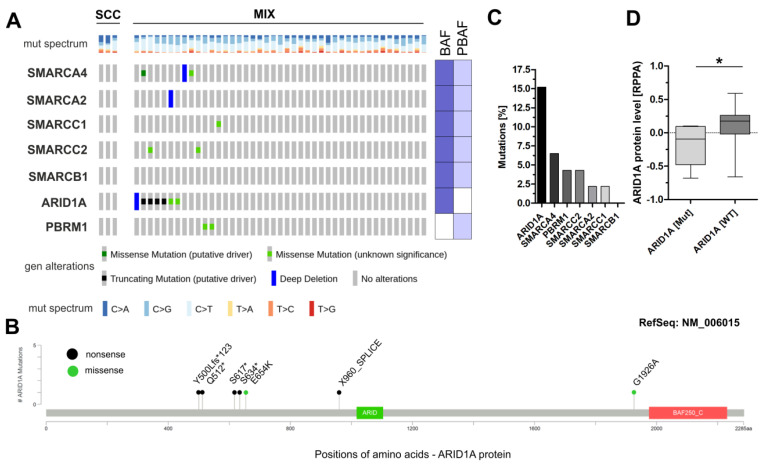
In order to give first insights into the mutational status of (putative) key components of the SWI/SNF complex in squamous bladder cancers (for study design see Supplementary Figure S1), carcinomas with histologically squamous differentiation (n = 3 pure SCC and n = 42 MIX) of The Cancer Genome Atlas (TCGA) were analyzed for genetic alterations of seven frequently affected subunits of the SWI/SNF complexes BAF and PBAF [11,12]. Alterations of the BAF-specific component ARID1A were the most frequent events (15.2%, 7/46), comprising one deep deletion, four truncating mutations and two missense mutations indicating impaired protein function (Figure 1A,B).
Figure 1.
SWI/SNF alterations and ARID1A protein expression in the sq-BLCA cohort of the TCGA network. (A) Genetic alterations of different subunits of the SWI/SNF complex (including missense mutations, truncating mutations, amplifications and deep deletions). (B) Mutation Mapper illustrating positions of identified ARID1A alterations (nonsense and missense) relative to the protein sequence and domains (green and red box). Protein domains are indicated according to PFAM: green box: ARID domain; red box: BAF250_C domain. (C) Mutational frequencies of analyzed subunits of the SWI/SNF complex. (D) Box plots illustrating ARID1A protein expression classified by ARID1A mutations. BAF (dark blue): BRG1/BRM-associated factor; PBAF (light blue): polybromo-associated BAF; MUT: mutated; WT: wildtype. * p < 0.05.
Only low mutation frequencies were observed in sq-BLCA for components potentially involved in assembly of both complexes—i.e., BAF and PBAF: SMARCA4 6.5% (3/46), SMARCC2 4.3% (2/46), SMARCA2 2.2% (1/46), SMARCC1 2.2% (1/46) and SMARCB1 0% (0/46). The gene encoding the PBAF-specific subunit PBRM1 was mutated in 4.3% of samples (2/46) (Figure 1A). Determining the ARID1A protein level in dependency of its mutational status, we confirmed a significantly lower expression in tumors with genetic alterations of the ARID1A gene including missense mutations (Figure 1C)—i.e., frequent ARID1A mutations correlate with loss of ARID1A protein in TCGA Sq-BLCA.
As genetic alterations of SWI/SNF components are known to be associated with patients’ outcome, we correlated SWI/SNF mutations with clinico-pathological parameters and analyzed recurrence-free (RFS) and overall survival (OS) as an indicator of potential prognostic impact. We focused on patients with at least one genetic alteration in one or more of the analyzed components as well as on those harboring ARID1A mutations (missense vs. nonsense). Using a Fisher’s exact test, no associations of SWI/SNF mutations or ARID1A mutations with clinico-pathological characteristics were observed (Supplementary Tables S2–S4). Kaplan–Meier analysis did not show any association of mutated SWI/SNF components and/or ARID1A mutations with RFS and OS (Supplementary Figure S2).
3.2. Immunohistochemical Analysis of Frequently Altered Subunits of the SWI/SNF-Complex in an Independent Squamous Bladder Cancer Cohort
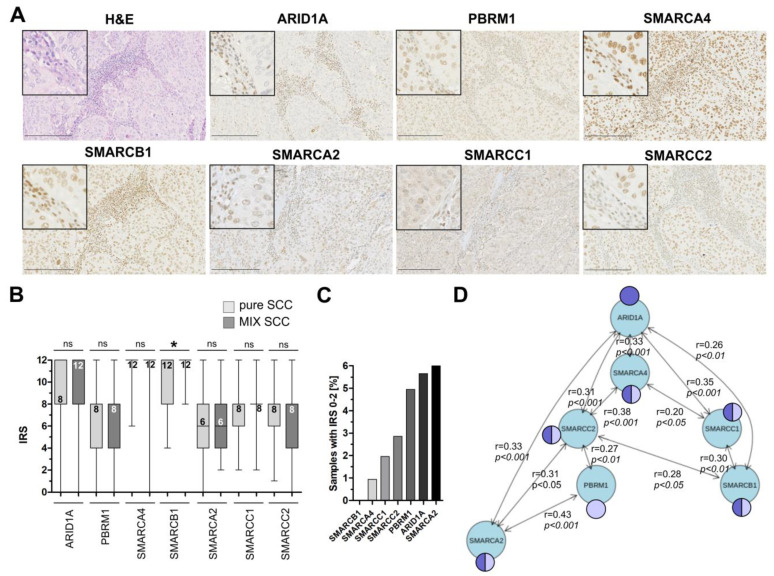
Next, n = 116 samples of patients with pure squamous cell carcinoma (n = 68) and mixed urothelial carcinoma with substantial squamous differentiation (n = 48) were analyzed for seven SWI/SNF complex proteins (ARID1A, SMARCA4, SMARCB1, SMARCC1, SMARCC2, SMARCA2 and PBRM1) by immunohistochemistry (Figure 2A). In total, 68.1% of the carcinomas presented as high-grade cancers, while except for one sample, all bladder tumors showed muscle-invasion (for cohort characteristics see Table 1).
Figure 2.
Protein expression of subunits of the SWI/SNF complexes BAF and PBAF in squamous-differentiated bladder cancers (sq-BLCA). (A) H&E and immunohistochemical staining of seven subunits of the SWI/SNF complex are shown for a representative tissue core with ARID1A mutation (c.4005-2A>G, p.(?)). Black scale bar: 100 µM. For further immunohistochemical ARID1A staining according to the range of Immune Reactive Scores (IRSs) see Supplementary Figure S3. (B) Box plot graphs show overall distribution of IRS staining results of subunits for urothelial cancers with squamous components (MIX SCC) and pure squamous cancers (SCC). The numeric values correspond to the median value. (C) Frequencies of expression loss (IRS ≤ 2) shown for all analyzed subunits. (D) Expression network illustrating the statistical correlation between analyzed subunits of BAF and PBAF. Only significant (p ≤ 0.05) spearman correlations (r-values as indicated) are shown. Dark blue: component of the BAF complex; light blue: component of the PBAF complex; * p < 0.05.
Based on an adapted Immune Reactive Score (IRS) by Remmele and Stegner [35], a semiquantitative score (0–2 = negative; 3–12 = positive) was applied. Considering the different subunits of the SWI/SNF-complex which have been previously shown to be frequently altered in various cancer entities including urothelial carcinomas [13], we found no significant differences between pure and mixed squamous carcinomas regarding the median expression for ARID1A (median IRS SCC: 8 (n = 64); median IRS MIX: 12 (n = 45)), SMARCA4 (median IRS SCC: 12 (n = 62); median IRS MIX: 12 (n = 44)), SMARCC1 (IRS SCC: 8 (n = 61); IRS MIX: 8 (n = 41)), SMARCC2 (IRS SCC: 8 (n = 62); IRS MIX: 8 (n = 43)), SMARCA2 (IRS SCC: 6 (n = 57); IRS MIX: 6 (n = 43)) and PBRM1 (IRS SCC: 8 (n = 56); IRS MIX: 8 (n = 45)) (Figure 2B). Expression of SMARCB1 significantly differs (p < 0.05) between pure SCC and MIX-SCC ranging between IRS 4–12 for SCC (n = 62) and 8–12 for MIX tumors (n = 42). However, the median expression did not differ (IRS SCC: 12; IRS MIX: 12) (Figure 2B). Focusing on those candidates lacking expression (IRS 0–2), 6% of our squamous bladder cancers were identified to show loss of expression of SMARCA2, followed by ARID1A (5.5%), PBRM1 (5.0%), SMARCC2 (2.9%), SMARCC1 (2.0%) and SMARCA4 (0.9%) (Figure 2C). For detailed data of expression loss see Table 2.
Table 2.
Loss of SWI/SNF proteins in squamous bladder cancer.
| SCC | MIX | |||
|---|---|---|---|---|
| neg | pos | neg | pos | |
| ARID1A | 2 | 62 | 4 | 41 |
| PBRM1 | 2 | 54 | 3 | 42 |
| SMARCC1 | 1 | 60 | 1 | 40 |
| SMARCC2 | 2 | 60 | 1 | 42 |
| SMARCA2 | 4 | 53 | 2 | 41 |
| SMARCA4 | 0 | 62 | 1 | 43 |
| SMARCB1 | 0 | 62 | 0 | 42 |
As previous studies revealed involvement of distinct components in assembly of different SWI/SNF complexes [11,12], we further analyzed statistical associations between expression of subunits known to be potentially present in both protein complexes (either BAF and/or PBAF) as well as the BAF- (ARID1A) and PBAF-specific (PBRM1) components using a non-parametric Spearman-rank correlation. A frequent and significant similarity of ARID1A expression with five BAF-associated subunits was observed in our cohort (Figure 2D).
PBRM1 (PBAF-specific complex) correlated with two PBAF-associated subunits. Contrary to that, ARID1A loss correlated with lack of expression of the BAF subunits SMARCA4 (Spearman r: 0.438, p ≤ 0.001), SMARCC1 (Spearman r: 0.492, p ≤ 0.001) and SMARCC2 (Spearman r: 0.296, p ≤ 0.01). No correlation was found between ARID1A and PBRM1, SMARCA2 or SMARCB1.
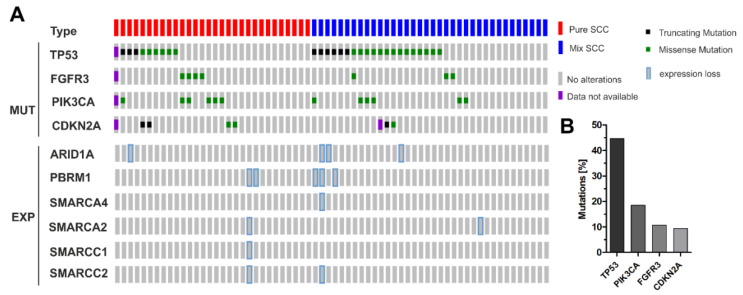
3.3. Correlation of ARID1A Expression Loss with Clinico-Pathological Parameters and Known Genetic Drivers
Next, we tested associations between expression loss of analyzed subunits with both clinico-pathological characteristics and driver mutations as indicators for prognostic risk and therapeutic implication (Figure 3A,B). Novel PIK3CA mutational analyses were performed by SNaPshot according to Hurst et al. [37], while PCR-amplification and Sanger sequencing was performed for CDKN2A as specified in 2016 [6]. All findings were correlated including previously published mutational data for TP53 and FGFR3 [5]. With the exception of ARID1A, neither associations between expression loss and clinico-pathological parameters—such as age at diagnosis, tumor size and histological tumor type - nor driver mutations were found. ARID1A expression did not significantly correlate with clinico-pathological parameters (Table 3). Please note that the sample number showing ARID1A expression loss is limited, which could affect statistical accuracy. However, all six tumors that did not express ARID1A were diagnosed in advanced stages—i.e., n = 5 pT3, n = 1 pT4, n = 2 with positive lymph node status, and n = 4 with high-grade differentiation. ARID1A expression was further significantly associated with TP53 mutations (p < 0.05) (Table 3). Interestingly, ARID1A expression loss was not observed in tumors with genetic alterations of FGFR3 or PIK3CA.
Figure 3.
Expression loss of SWI/SNF subunits in sq-BLCA with known genetic driver mutations. (A) Upper lines: mutational spectrum of genes (TP53, FGFR3, PIK3CA, CDKN2A) potentially involved in bladder cancer development and progression (SCC: n = 30; MIX SCC: n = 36). TP53 was the most frequently mutated gene in pure SCC (9/29) as well as MIX-SCC (20/36), while FGFR3 (SCC: 4/29; MIX: 3/36) and CDKN2A (SCC: 4/29; MIX: 2/35) mutations were less abundant (SCC: 4/29; MIX: 3/36). PIK3CA driver mutations were observed in 6/29 (SCC) and in 6/36 (MIX) tumors. Lower lines: corresponding expression loss of subunits of the SWI/SNF complex. MUT: mutations; EXP: expression. (B) Overall mutational frequencies of analyzed driver genes.
Table 3.
Clinico-pathological parameters and known driver mutations in relation to ARID1A expression loss.
| ARID1A Expression b | |||||
|---|---|---|---|---|---|
| n a | 0–2 | 3–12 | p-Value c | ||
| Parameter: | |||||
| Age at diagnosis | |||||
| median age: 67 years | |||||
| ≤67 years | 56 | 3 | 53 | 0.954 | |
| >67 years | 53 | 3 | 50 | ||
| Gender | |||||
| female | 55 | 3 | 52 | 0.963 | |
| male | 53 | 3 | 50 | ||
| Histological tumor grade d | |||||
| G1-G2 | 30 | 2 | 28 | 0.816 | |
| G3 | 73 | 4 | 69 | ||
| Tumor stage d | |||||
| pT1-pT2 | 13 | 0 | 13 | 0.328 | |
| pT3-pT4 | 86 | 6 | 80 | ||
| Lymph node status | |||||
| neg | 65 | 4 | 61 | 0.600 | |
| neg | 21 | 2 | 19 | ||
| TP53 mut e | |||||
| neg | 30 | 0 | 30 | 0.030 | |
| neg | 27 | 4 | 23 | ||
| FGFR3 mut e | |||||
| neg | 50 | 4 | 46 | 0.442 | |
| neg | 7 | 0 | 7 | ||
| CDKNA2 mut e | |||||
| neg | 51 | 4 | 47 | 0.520 | |
| neg | 5 | 0 | 5 | ||
| PIK3CA mut e | |||||
| neg | 45 | 4 | 41 | 0.288 | |
| pos | 12 | 0 | 12 | ||
a Only patients with primary bladder cancer were included: b IRS according to Remmele [35]; c Fisher’s exact test; d according to WHO 2004 classification; e due to limited availability of material, experimental data, case numbers vary for different methods as indicated. Significant p-values are marked in bold face.
3.4. ARID1A Protein Loss Overlaps with Genetic ARID1A Alterations and PD-L1 Expression in the Independent Squamous Bladder Cancer Cohort
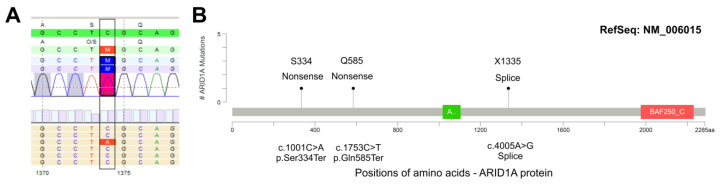
Since ARID1A loss seems to be associated with advanced tumor stages, we focused on this important SWI/SNF component with therapeutic potential to confirm that ARID1A protein loss results from genetic ARID1A gene alterations. Six tumors (n = 4 MIX, n = 2 SCC) with loss of ARID1A expression (Figure 4) were sequenced by NGS. Three out of the six ARID1A-deficient samples showed ARID1A mutations (c.1001C>A, p.(Ser334Ter), allele frequency (AF) 20%; c.1753C>T, p.(Gln585Ter), AF 23%; c.4005-2A>G, p.(?), canonical splice site, AF 27%). No high-level copy number alteration was detected for ARID1A.
Figure 4.
ARID1A mutations in sq-BLCA. (A) Exemplary illustration of a nonsense ARID1A mutation with an allele frequency of 20% (c.1001C>T, p.Ser334Ter, estimated tumor cell content 40%). (B) Summarized ARID1A mutations identified in Sq-BLCA with clear expression loss (IRS < 2). Protein domains are indicated according to PFAM: green box: ARID domain; red box: BAF250_C domain.
To our knowledge, none of the three mutations has been previously described in the literature, but all three mutations are annotated in the COSMIC database v92 (https://cancer.sanger.ac.uk/cosmic; c.1001C>T (p.Ser334Ter/COSM6983737): n = 1, pancreatic carcinoid-endocrine tumor [P-0012246-T01-IM5]; c.1753C>T (p.Gln585Ter/COSM1133047): n = 2, breast carcinoma [H_KU-1186-1186_A2_core], Burkitt lymphoma BL-6; c.4005-2A>G (COSM6925751): n = 1, transitional cell bladder carcinoma [P-0003024-T01-IM3]). Two of the three mutations are also (redundantly) listed in the cBioPortal database v3.4.13 (https://www.cbioportal.org/; c.1001C>T: n = 1, pancreatic neuroendocrine tumor [P-0012246-T01-IM5], classification: likely oncogenic; c.4005-2A>G: n = 1, bladder urothelial carcinoma [P-0003024-T01-IM3], classification: likely oncogenic). The mutation c.4005-2A>G affects the canonical splice site and leads to loss of the acceptor splice site according to distinct prediction tools. All three mutations are, therefore, most likely deleterious and probably lead to a nonsense-mediated decay of the truncated protein and, therefore, to a protein loss.
It is thought that ARID1A-mutated cancers may cooperate with immune checkpoint blockade therapy [19], thus providing novel therapeutic strategies for cancer management. As we recently showed that PD-L1 was frequently expressed in squamous bladder cancer [45], ARID1A alterations were correlated with expression of PD-L1 using the 28-8 antibody clone as an indicator of immune checkpoint inhibitor (ICI) treatment access. According to current European Medicines Agency (EMA)-approved guidelines for first line therapy of bladder cancer with pembrolizumab (CPS ≥ 10) and atezolizumab (IC-score ≥ 2/IC ≥ 5%), a single ARID1A-mutated cancer (1/3) was identified to be potentially eligible for atezolizumab first line therapy (Supplementary Table S5). Considering protein loss of ARID1A, another case was revealed—i.e., overall two SCC/MIX specimens of the urinary bladder were characterized by ARID1A protein loss and strong PD-L1 expression (IC-score ≥ 2/IC ≥ 5%) suggesting a putative synergistic impact and improved ICI therapy success similar to recent studies in urothelial cancers [24].
4. Discussion
To date, dysfunction of the components of the SWI/SNF complex has been shown for various cancer entities [17] including urothelial cancer [13]. TCGA data demonstrate that ARID1A is among the most frequently mutated genes among different types of cancer, such as stomach adenocarcinomas (18–31%) or uterine corpus endometrioid carcinomas (34%) [46]. Most ARID1A mutations are inactivating truncating mutations [46]—e.g., 63% of ARID1A gene alterations in urothelial carcinomas [30] or over 90% of ARID1A mutations in ovarian clear cell carcinoma [47]. ARID1A mutated carcinomas are associated with poor prognosis, and for instance, in breast cancer patients, inactivated ARID1A suggests a tumor suppressive function [48,49].
Recently, we revealed frequent genetic alterations of genes encoding for SWI/SNF subunits including ARID1A with a frequency of 26% in urothelial bladder cancer [30]. Most of these mutations, in particular truncating alterations, are likely associated with a functional loss of proteins. In line with this, we identified ARID1A mutations in 15% of sq-BLCA of the TCGA data set. The pathological/functional significance of identified missense mutations remains elusive; however, by stratifying the mutations we significantly observed reduced ARID1A protein levels for both—i.e., for nonsense mutations as well as for the combined group of nonsense and missense mutations. Further mechanisms potentially involved in gene silencing such as epigenetic silencing or mutations in non-coding regions as well as post-transcriptional or translational modifications [50] might be likely. Wu and colleagues showed, for instance, that heterozygous ARID1A mutations correlated with loss of protein expression—i.e., 73% of tumors with heterozygous ARID1A mutations lacked protein expression [48]—suggesting a second hit on the remaining allele. Considering that, we confirmed missense and nonsense mutations of ARID1A in both pure and mixed SCC samples which were characterized by ARID1A protein loss. Interestingly, we found that protein loss of the BAF-specific subunit ARID1A was closely associated with expression loss of the commonly shared and central subunits SMARCA4 and SMARCC1, as well as with the BAF/PBAF-associated factor SMARCC2. In turn, ARID1A expression correlates with all analyzed components potentially involved in assembly of the BAF complex [11,12] suggesting a predominant role of this canonical SWI/SNF complex in SCC. However, we are aware that a statistical correlation does not provide the exact protein interaction in single cells. In addition, residual subunits could be of importance to compensate missing factors, thus maintaining the SWI/SNF activity as, for instance, already demonstrated for the catalytic subunits SMARCA4 and SMARCA2. Both subunits have been shown to be mutually exclusive subunits in SWI/SNF complexes, and survival of SMARCA2-mutated cells depends on the residual SMARCA4-containing complex activity in specific tumor entities [51]. Thus, future studies addressing the role and function of the different SWI/SNF complexes and their corresponding subunits are required to decipher the mechanisms behind this in sq-BLCA.
Besides involvement of ARID1A in SW/SNF-mediated chromatin remodeling, ARID1A is thought to contribute to DNA damage repair, especially DNA double strand break (DSB) repair [50]. It has been shown that suppression of ARID1A led to a higher cellular sensitivity to cisplatin due to higher rates of DSB, triggered by deficient DNA repair [52]. In endometrial carcinomas, ARID1A mutations are associated with mismatch repair deficiency and normal p53 expression [53]. Bosse and colleagues showed a nearly mutual exclusivity of ARID1A loss and mutant-like TP53 expression, while alterations of the PI3K-AKT pathway were more frequent when ARID1A expression was lost [54]. Coexistence of PIK3CA and ARID1A mutations has been shown before [55], whereas association of both events was not observed in our SCC/MIX samples of the urinary bladder. We are aware of the potential bias due to the low number of PIK3CA mutations; however, none of the tumors lacking ARID1A expression showed evidence for any of the analyzed driver mutations (i.e., PIK3CA and CDKN2A). Thus, a hypothesized causal and functional link between both events (e.g., PIK3CA and ARID1A mutations/expression) seems unlikely in squamous bladder cancer. In turn, ARID1A loss occurred in a TP53-deficient genetic background suggesting a regulation of potentially different biological processes to those described to date [56], but affecting cell cycle control which should be further studied in more detail in the future.
However, accumulating studies propose the involvement of functional ARID1A loss in synthetic lethality, which contributes to the response to various classical [20,21] and novel therapeutic options, including immune checkpoint inhibitors (ICI) [19,22,23]. Goswami and colleagues have recently shown that ARID1A mutation in combination with immune cytokine CXCL13 expression predicts response to immune checkpoint inhibitors in metastasized bladder cancers [24]. As we already provided a rationale for ICI treatment of SCC of the urinary bladder [45], ARID1A protein loss may predict increased efficiency of ICI therapy. However, a correlation between ARID1A mutations and increased PD-L1 expression as previously reported [19] could not be confirmed in sq-BLCA. The co-occurrence was rare, and only a subgroup of patients with ARID1A mutations may benefit from ICI treatment. In addition, Fukumoto and colleagues showed that inhibition of histone deacetylase 6 (HDAC6) contributes to growth suppression of ARID1A-mutated tumors, while synergistic effects were shown in combination with anti-PDL1 therapy [25]. Although the clinical results of HDAC-inhibitors have generally been disappointing in the past [26], current studies indicate a specific targeted benefit applying HDAC-inhibitors in tumors with ARID1A loss [25,27]. Thus, ARID1A might be used as an additional biomarker for clinical response to both HDAC inhibition and anti-PD-L1 therapy, albeit its function as a biomarker has only been described for patients with advanced urothelial carcinoma yet [27]. Further clinical trials may be necessary to prove the possible synergistic effect of both HDAC- and PD-L1-inhibitors on squamous bladder cancer cells with ARID1A mutation.
In conclusion, we provide, for the first time, data describing expression loss of components of the SWI/SNF-complex in sq-BLCA including pure SCC, highlighting ARID1A as an interesting target for a small subgroup of patients which may benefit from novel therapeutics in an ARID1A mutated background.
Acknowledgments
The authors appreciate the excellent technical support of Ursula Schneider.
Supplementary Materials
The following are available online at https://www.mdpi.com/2073-4425/11/11/1368/s1. The datasets supporting the conclusions of this article are included within the article and its additional files: Supplementary Table S1: Primer sequences for Sanger sequencing of FFPE Material. Supplementary Tables S2–S4: Clinico-pathological parameters of the TCGA sq-BLCA data set in relation to SWI/SNF/ARID1A mutations. Supplementary Table S5: Overlap of ARID1A mutations/expression loss with PD-L1 expression. Supplementary Table S6: Abbreviation list. Supplementary Figure S1: Study design of the project. Supplementary Figure S2: Prognostic impact of SWI/SNF and ARID1A mutations on tumor patients’ survival. Supplementary Figure S3: Immunohistochemical staining of ARID1A according to calculated IRS.
Author Contributions
Conceptualization: N.T.G, M.R. and S.G.; Methodology, F.A., V.W., R.M., A.M., N.O.-B. and M.R.; Software, Statistics and Databases, M.R. and L.S.; Resources, A.H., T.H.E. and R.K.; Writing—Original Draft Preparation, F.A.; Review and Editing, M.R., S.G. and N.T.G.; Visualization, F.A., M.R. and N.O.-B.; Supervision, N.T.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2018. CA Cancer J. Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 3.Knowles M.A., Hurst C.D. Molecular biology of bladder cancer: New insights into pathogenesis and clinical diversity. Nat. Rev. Cancer. 2015;15:25–41. doi: 10.1038/nrc3817. [DOI] [PubMed] [Google Scholar]
- 4.Kaufman D.S., Shipley W.U., Feldman A.S. Bladder cancer. Lancet. 2009;374:239–249. doi: 10.1016/S0140-6736(09)60491-8. [DOI] [PubMed] [Google Scholar]
- 5.Rose M., Maurer A., Wirtz J., Bleilevens A., Waldmann T., Wenz M., Eyll M., Geelvink M., Gereitzig M., Rüchel N., et al. EGFR activity addiction facilitates anti-ERBB based combination treatment of squamous bladder cancer. Oncogene. 2020;39:6856–6870. doi: 10.1038/s41388-020-01465-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baldia P.H., Maurer A., Heide T., Rose M., Stoehr R., Hartmann A., Williams S.V., Knowles M.A., Knuechel R., Gaisa N.T. Fibroblast growth factor receptor (FGFR) alterations in squamous differentiated bladder cancer: A putative therapeutic target for a small subgroup. Oncotarget. 2016;7:71429–71439. doi: 10.18632/oncotarget.12198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abol-Enein H., Kava B.R., Carmack A.J. Nonurothelial cancer of the bladder. Urology. 2007;69:93–104. doi: 10.1016/j.urology.2006.08.1107. [DOI] [PubMed] [Google Scholar]
- 8.Gaisa N.T., Braunschweig T., Reimer N., Bornemann J., Eltze E., Siegert S., Toma M., Villa L., Hartmann A., Knuechel R. Different immunohistochemical and ultrastructural phenotypes of squamous differentiation in bladder cancer. Virchows Arch. 2011;458:301–312. doi: 10.1007/s00428-010-1017-2. [DOI] [PubMed] [Google Scholar]
- 9.Martin J.W., Carballido E.M., Ahmed A., Farhan B., Dutta R., Smith C., Youssef R.F. Squamous cell carcinoma of the urinary bladder: Systematic review of clinical characteristics and therapeutic approaches. Arab J. Urol. 2016;14:183–191. doi: 10.1016/j.aju.2016.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen S.M., Shirai T., Steineck G. Epidemiology and etiology of premalignant and malignant urothelial changes. Scand. J. Urol. Nephrol. Suppl. 2000:105–115. doi: 10.1080/00365590050509869. [DOI] [PubMed] [Google Scholar]
- 11.Michel B.C., D’Avino A.R., Cassel S.H., Mashtalir N., McKenzie Z.M., McBride M.J., Valencia A.M., Zhou Q., Bocker M., Soares L.M.M., et al. A non-canonical SWI/SNF complex is a synthetic lethal target in cancers driven by BAF complex perturbation. Nat. Cell Biol. 2018;20:1410–1420. doi: 10.1038/s41556-018-0221-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mashtalir N., D’Avino A.R., Michel B.C., Luo J., Pan J., Otto J.E., Zullow H.J., McKenzie Z.M., Kubiak R.L., St Pierre R., et al. Modular Organization and Assembly of SWI/SNF Family Chromatin Remodeling Complexes. Cell. 2018;175:1272–1288.e1220. doi: 10.1016/j.cell.2018.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agaimy A., Bertz S., Cheng L., Hes O., Junker K., Keck B., Lopez-Beltran A., Stockle M., Wullich B., Hartmann A. Loss of expression of the SWI/SNF complex is a frequent event in undifferentiated/dedifferentiated urothelial carcinoma of the urinary tract. Virchows Arch. 2016;469:321–330. doi: 10.1007/s00428-016-1977-y. [DOI] [PubMed] [Google Scholar]
- 14.Schallenberg S., Bork J., Essakly A., Alakus H., Buettner R., Hillmer A.M., Bruns C., Schroeder W., Zander T., Loeser H., et al. Loss of the SWI/SNF-ATPase subunit members SMARCF1 (ARID1A), SMARCA2 (BRM), SMARCA4 (BRG1) and SMARCB1 (INI1) in oesophageal adenocarcinoma. BMC Cancer. 2020;20:12. doi: 10.1186/s12885-019-6425-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guan B., Wang T.L., Shih Ie M. ARID1A, a factor that promotes formation of SWI/SNF-mediated chromatin remodeling, is a tumor suppressor in gynecologic cancers. Cancer Res. 2011;71:6718–6727. doi: 10.1158/0008-5472.CAN-11-1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodriguez-Nieto S., Cañada A., Pros E., Pinto A.I., Torres-Lanzas J., Lopez-Rios F., Sanchez-Verde L., Pisano D.G., Sanchez-Cespedes M. Massive parallel DNA pyrosequencing analysis of the tumor suppressor BRG1/SMARCA4 in lung primary tumors. Hum. Mutat. 2011;32:E1999–E2017. doi: 10.1002/humu.21415. [DOI] [PubMed] [Google Scholar]
- 17.Kadoch C., Hargreaves D.C., Hodges C., Elias L., Ho L., Ranish J., Crabtree G.R. Proteomic and bioinformatic analysis of mammalian SWI/SNF complexes identifies extensive roles in human malignancy. Nat. Genet. 2013;45:592–601. doi: 10.1038/ng.2628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reisman D., Glaros S., Thompson E.A. The SWI/SNF complex and cancer. Oncogene. 2009;28:1653–1668. doi: 10.1038/onc.2009.4. [DOI] [PubMed] [Google Scholar]
- 19.Shen J., Ju Z., Zhao W., Wang L., Peng Y., Ge Z., Nagel Z.D., Zou J., Wang C., Kapoor P., et al. ARID1A deficiency promotes mutability and potentiates therapeutic antitumor immunity unleashed by immune checkpoint blockade. Nat. Med. 2018;24:556–562. doi: 10.1038/s41591-018-0012-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuroda T., Ogiwara H., Sasaki M., Takahashi K., Yoshida H., Kiyokawa T., Sudo K., Tamura K., Kato T., Okamoto A., et al. Therapeutic preferability of gemcitabine for ARID1A-deficient ovarian clear cell carcinoma. Gynecol. Oncol. 2019;155:489–498. doi: 10.1016/j.ygyno.2019.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Kuroda T., Kohno T. Precision medicine for ovarian clear cell carcinoma based on gene alterations. Int. J. Clin. Oncol. 2020;25:419–424. doi: 10.1007/s10147-020-01622-z. [DOI] [PubMed] [Google Scholar]
- 22.Shen J., Peng Y., Wei L., Zhang W., Yang L., Lan L., Kapoor P., Ju Z., Mo Q., Shih I.M., et al. ARID1A Deficiency Impairs the DNA Damage Checkpoint and Sensitizes Cells to PARP Inhibitors. Cancer Discov. 2015;5:752–767. doi: 10.1158/2159-8290.CD-14-0849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Williamson C.T., Miller R., Pemberton H.N., Jones S.E., Campbell J., Konde A., Badham N., Rafiq R., Brough R., Gulati A., et al. ATR inhibitors as a synthetic lethal therapy for tumours deficient in ARID1A. Nat. Commun. 2016;7:13837. doi: 10.1038/ncomms13837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goswami S., Chen Y., Anandhan S., Szabo P.M., Basu S., Blando J.M., Liu W., Zhang J., Natarajan S.M., Xiong L., et al. mutation plus CXCL13 expression act as combinatorial biomarkers to predict responses to immune checkpoint therapy in mUCC. Sci. Transl. Med. 2020;12 doi: 10.1126/scitranslmed.abc4220. [DOI] [PubMed] [Google Scholar]
- 25.Fukumoto T., Fatkhutdinov N., Zundell J.A., Tcyganov E.N., Nacarelli T., Karakashev S., Wu S., Liu Q., Gabrilovich D.I., Zhang R. HDAC6 Inhibition Synergizes with Anti-PD-L1 Therapy in ARID1A-Inactivated Ovarian Cancer. Cancer Res. 2019;79:5482–5489. doi: 10.1158/0008-5472.CAN-19-1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nervi C., De Marinis E., Codacci-Pisanelli G. Epigenetic treatment of solid tumours: A review of clinical trials. Clin. Epigenetics. 2015;7:127. doi: 10.1186/s13148-015-0157-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gupta S., Albertson D.J., Parnell T.J., Butterfield A., Weston A., Pappas L.M., Dalley B., O’Shea J.M., Lowrance W.T., Cairns B.R., et al. Histone Deacetylase Inhibition Has Targeted Clinical Benefit in. Mol. Cancer Ther. 2019;18:185–195. doi: 10.1158/1535-7163.MCT-17-0957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaelin W.G. The concept of synthetic lethality in the context of anticancer therapy. Nat. Rev. Cancer. 2005;5:689–698. doi: 10.1038/nrc1691. [DOI] [PubMed] [Google Scholar]
- 29.O’Neil N.J., Bailey M.L., Hieter P. Synthetic lethality and cancer. Nat. Rev. Genet. 2017;18:613–623. doi: 10.1038/nrg.2017.47. [DOI] [PubMed] [Google Scholar]
- 30.Garczyk S., Schneider U., Lurje I., Becker K., Vögeli T.A., Gaisa N.T., Knüchel R. ARID1A-deficiency in urothelial bladder cancer: No predictive biomarker for EZH2-inhibitor treatment response? PLoS ONE. 2018;13:e0202965. doi: 10.1371/journal.pone.0202965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li J., Lu S., Lombardo K., Monahan R., Amin A. ARID1A alteration in aggressive urothelial carcinoma and variants of urothelial carcinoma. Hum. Pathol. 2016;55:17–23. doi: 10.1016/j.humpath.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 32.Gaisa N.T., Graham T.A., McDonald S.A., Canadillas-Lopez S., Poulsom R., Heidenreich A., Jakse G., Tadrous P.J., Knuechel R., Wright N.A. The human urothelium consists of multiple clonal units, each maintained by a stem cell. J. Pathol. 2011;225:163–171. doi: 10.1002/path.2945. [DOI] [PubMed] [Google Scholar]
- 33.Fischbach A., Rogler A., Erber R., Stoehr R., Poulsom R., Heidenreich A., Schneevoigt B.S., Hauke S., Hartmann A., Knuechel R., et al. Fibroblast growth factor receptor (FGFR) gene amplifications are rare events in bladder cancer. Histopathology. 2015;66:639–649. doi: 10.1111/his.12473. [DOI] [PubMed] [Google Scholar]
- 34.Molitor M., Junker K., Eltze E., Toma M., Denzinger S., Siegert S., Knuechel R., Gaisa N.T. Comparison of structural genetics of non-schistosoma-associated squamous cell carcinoma of the urinary bladder. Int. J. Clin. Exp. Pathol. 2015;8:8143–8158. [PMC free article] [PubMed] [Google Scholar]
- 35.Remmele W., Stegner H.E. Recommendation for uniform definition of an immunoreactive score (IRS) for immunohistochemical estrogen receptor detection (ER-ICA) in breast cancer tissue. Pathologe. 1987;8:138–140. [PubMed] [Google Scholar]
- 36.Rose M., Gaisa N.T., Antony P., Fiedler D., Heidenreich A., Otto W., Denzinger S., Bertz S., Hartmann A., Karl A., et al. Epigenetic inactivation of ITIH5 promotes bladder cancer progression and predicts early relapse of pT1 high-grade urothelial tumours. Carcinogenesis. 2014;35:727–736. doi: 10.1093/carcin/bgt375. [DOI] [PubMed] [Google Scholar]
- 37.Hurst C.D., Zuiverloon T.C., Hafner C., Zwarthoff E.C., Knowles M.A. A SNaPshot assay for the rapid and simple detection of four common hotspot codon mutations in the PIK3CA gene. BMC Res. Notes. 2009;2:66. doi: 10.1186/1756-0500-2-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Keck B., Stoehr R., Wach S., Rogler A., Hofstaedter F., Lehmann J., Montironi R., Sibonye M., Fritsche H.M., Lopez-Beltran A., et al. The plasmacytoid carcinoma of the bladder--rare variant of aggressive urothelial carcinoma. Int. J. Cancer. 2011;129:346–354. doi: 10.1002/ijc.25700. [DOI] [PubMed] [Google Scholar]
- 39.Guricova K., Maurer A., Gaisa N., Garczyk S., Knüchel-Clarke R., Dahl E., Ortiz B.N. AG12.P.03: Ein Robustes Tool zur Kopienzahlanalyse für Verschiedene Amplikon-Basierte NGS-Panel (ACopy). Abstracts 103. Jahrestagung der Deutschen Gesellschaft für Pathologie, Frankfurt, 13.06.2019–15.06.2019. Pathologe. 2019;40:196. [Google Scholar]
- 40.Robertson A.G., Kim J., Al-Ahmadie H., Bellmunt J., Guo G., Cherniack A.D., Hinoue T., Laird P.W., Hoadley K.A., Akbani R., et al. Comprehensive Molecular Characterization of Muscle-Invasive Bladder Cancer. Cell. 2017;171:540–556. doi: 10.1016/j.cell.2017.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Porter M.P., Voigt L.F., Penson D.F., Weiss N.S. Racial variation in the incidence of squamous cell carcinoma of the bladder in the United States. J. Urol. 2002;168:1960–1963. doi: 10.1016/S0022-5347(05)64272-3. [DOI] [PubMed] [Google Scholar]
- 42.Cerami E., Gao J., Dogrusoz U., Gross B.E., Sumer S.O., Aksoy B.A., Jacobsen A., Byrne C.J., Heuer M.L., Larsson E., et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401–404. doi: 10.1158/2159-8290.CD-12-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gao J., Aksoy B.A., Dogrusoz U., Dresdner G., Gross B., Sumer S.O., Sun Y., Jacobsen A., Sinha R., Larsson E., et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 2013;6:pl1. doi: 10.1126/scisignal.2004088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hansen K.D., Gentry J., Long L., Gentleman R., Falcon S., Hahne F., Sarkar D. Rgraphviz: Provides Plotting Capabilities for R Graph Objects, R Package Version 2.32.0. 2020. [(accessed on 17 October 2020)]. Available online: https://www.bioconductor.org/packages/release/bioc/html/Rgraphviz.html. [DOI] [Google Scholar]
- 45.Morsch R., Rose M., Maurer A., Cassataro M.A., Braunschweig T., Knüchel R., Vögeli T.A., Ecke T., Eckstein M., Weyerer V., et al. Therapeutic implications of PD-L1 expression in bladder cancer with squamous differentiation. BMC Cancer. 2020;20:230. doi: 10.1186/s12885-020-06727-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen J., Herlong F.H., Stroehlein J.R., Mishra L. Mutations of Chromatin Structure Regulating Genes in Human Malignancies. Curr. Protein Pept. Sci. 2016;17:411–437. doi: 10.2174/1389203717666160122120008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wiegand K.C., Shah S.P., Al-Agha O.M., Zhao Y., Tse K., Zeng T., Senz J., McConechy M.K., Anglesio M.S., Kalloger S.E., et al. ARID1A mutations in endometriosis-associated ovarian carcinomas. N. Engl. J. Med. 2010;363:1532–1543. doi: 10.1056/NEJMoa1008433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wu J.N., Roberts C.W. ARID1A mutations in cancer: Another epigenetic tumor suppressor? Cancer Discov. 2013;3:35–43. doi: 10.1158/2159-8290.CD-12-0361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Luchini C., Veronese N., Solmi M., Cho H., Kim J.H., Chou A., Gill A.J., Faraj S.F., Chaux A., Netto G.J., et al. Prognostic role and implications of mutation status of tumor suppressor gene ARID1A in cancer: A systematic review and meta-analysis. Oncotarget. 2015;6:39088–39097. doi: 10.18632/oncotarget.5142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Caumanns J.J., Wisman G.B.A., Berns K., van der Zee A.G.J., De Jong S. ARID1A mutant ovarian clear cell carcinoma: A clear target for synthetic lethal strategies. Biochim. Biophys. Acta Rev. Cancer. 2018;1870:176–184. doi: 10.1016/j.bbcan.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 51.Ehrenhöfer-Wölfer K., Puchner T., Schwarz C., Rippka J., Blaha-Ostermann S., Strobl U., Hörmann A., Bader G., Kornigg S., Zahn S., et al. SMARCA2-deficiency confers sensitivity to targeted inhibition of SMARCA4 in esophageal squamous cell carcinoma cell lines. Sci. Rep. 2019;9:11661. doi: 10.1038/s41598-019-48152-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Watanabe R., Ui A., Kanno S., Ogiwara H., Nagase T., Kohno T., Yasui A. SWI/SNF factors required for cellular resistance to DNA damage include ARID1A and ARID1B and show interdependent protein stability. Cancer Res. 2014;74:2465–2475. doi: 10.1158/0008-5472.CAN-13-3608. [DOI] [PubMed] [Google Scholar]
- 53.Allo G., Bernardini M.Q., Wu R.C., Shih I.M., Kalloger S., Pollett A., Gilks C.B., Clarke B.A. ARID1A loss correlates with mismatch repair deficiency and intact p53 expression in high-grade endometrial carcinomas. Mod. Pathol. 2014;27:255–261. doi: 10.1038/modpathol.2013.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bosse T., ter Haar N.T., Seeber L.M., Diest P.J.V., Hes F.J., Vasen H.F., Nout R.A., Creutzberg C.L., Morreau H., Smit V.T. Loss of ARID1A expression and its relationship with PI3K-Akt pathway alterations, TP53 and microsatellite instability in endometrial cancer. Mod. Pathol. 2013;26:1525–1535. doi: 10.1038/modpathol.2013.96. [DOI] [PubMed] [Google Scholar]
- 55.Chandler R.L., Damrauer J.S., Raab J.R., Schisler J.C., Wilkerson M.D., Didion J.P., Starmer J., Serber D., Yee D., Xiong J., et al. Coexistent ARID1A-PIK3CA mutations promote ovarian clear-cell tumorigenesis through pro-tumorigenic inflammatory cytokine signalling. Nat. Commun. 2015;6:6118. doi: 10.1038/ncomms7118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bitler B.G., Fatkhutdinov N., Zhang R. Potential therapeutic targets in ARID1A-mutated cancers. Expert Opin. Ther. Targets. 2015;19:1419–1422. doi: 10.1517/14728222.2015.1062879. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.