Primary care and alcohol use
Primary care providers (PCPs) play an essential role in screening for and treating alcohol use disorders (AUDs) and hazardous drinking. According to a recent Lancet tutorial, primary care ‘is not only the entry point for most people’ with AUD but also ‘where secondary prevention and most clinical interventions should take place’ (1). Screening, brief intervention, pharmacotherapy, treating common comorbid mental health conditions, and referral to counselling are all within the purview of primary care practice. Thus, it is important for PCPs to be aware of the changing landscape of AUD and other alcohol-related problems and to be at the forefront in expanding interventions to address problematic alcohol use. In the paragraphs below, we focus on recent epidemiological trend data from the USA. While trends in alcohol use, related morbidity and mortality, and exacerbating risk factors may vary by country, it is essential to keep in mind that alcohol remains a leading contributor to morbidity and mortality internationally, and especially in high- and middle-income countries (2).
Increasing alcohol-related morbidity and mortality
The number of deaths from alcohol-related causes in the USA has more than doubled since 1999. In 2017 alone, more than 72 000 Americans died from alcohol-related causes, comparable to the number of deaths from drug overdoses (3). Similarly, the rate of alcohol-related emergency department (ED) visits increased by 50% between 2006 and 2014 (4). These trends reflect morbidity and mortality associated with chronic illness like liver disease and acute events such as accidents, alcohol poisoning, and adverse alcohol–drug interactions. Paradoxically, trends in alcohol consumption and AUD have been relatively stable. Representative surveys of US household residents suggest that the prevalence of AUD among adults 18 and over actually decreased slightly over the years 2002 through 2014 (9.4% versus 8.4%) (5).
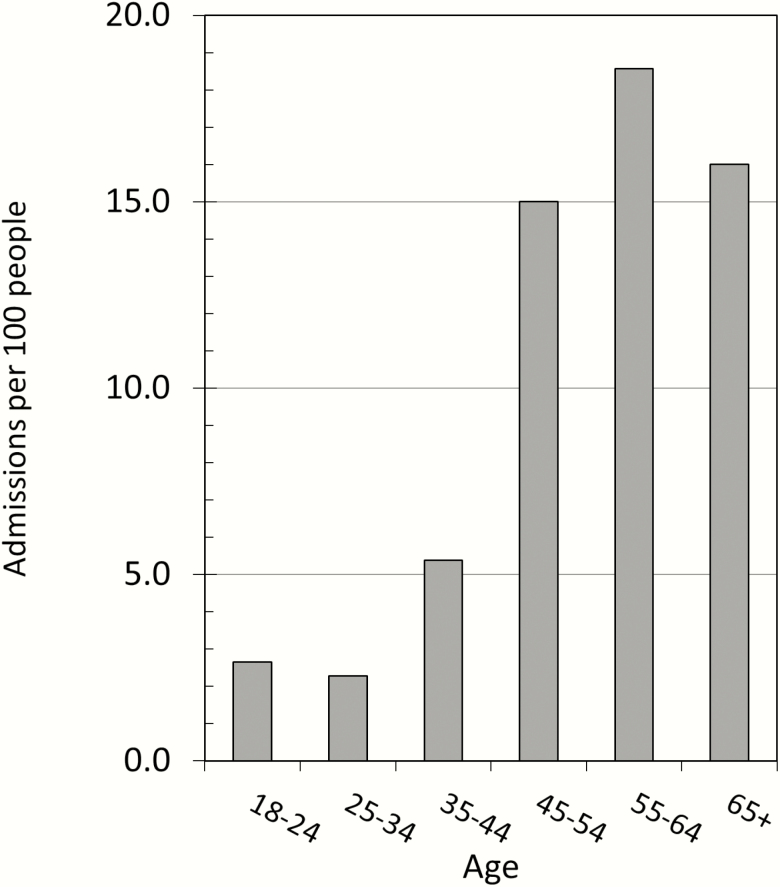
What do these divergent trends tell us about the clinical picture of a high-risk drinker? Perhaps foremost, it is essential to consider that the US population has been ageing (6). Because older people generally drink less than younger adults, the USA might have expected a decrease in per capita consumption in recent years, but instead saw modest increases (7). In fact, rates of ‘binge’ drinking—usually operationalized in US surveys as drinking five or more drinks in 1 day or on one occasion—have risen most rapidly among middle-aged and older adults while remaining relatively stable 18–29-year-olds (8). Excessive drinking is still more common among young adults, but ED visits for alcohol-related accidents and injury are more common in middle-adulthood, i.e. among 35–64 adults. Further, the age-gap in alcohol-related ED admission rates is growing: the largest increases between 2006 and 2014 were among adults ages 45–64. If we consider that alcohol consumption generally decreases with age, but illness and injury related to alcohol consumption increase with age, the stark age-related differences in morbidity risk associated with alcohol consumption become apparent. In Figure 1, we use past-year binge drinking prevalence in each age-group as a rough estimate of the size of the at-risk population to illustrate variation in rates of alcohol-related ED admission by age conditional on high-risk drinking. Dividing the rates of alcohol-related ED admissions by this proportion, results suggest that high-risk drinkers in the 45 and over age categories are 6–7.5 times more likely to be admitted to the ED for alcohol-related injury than those aged 18–34.
Figure 1.
Number of acute alcohol-related ED admissions per 100 people as estimated in ref (2), divided by the estimated proportion of that age-group to report one or more binge drinking episodes over the past 30 days from the 2017 National Health Interview Survey (see ref 8).
Exacerbating risk factors
In terms of morbidity and mortality due to acute events such as falls and other accidents, age-related changes in strength, body composition, and reflexes are likely contributors to increased risk. But increasing age-related risk may also stem from rising rates of utilization of medications that interact with alcohol, especially those with sedating effects (9). Use of these medications increases rapidly with age (10–12). Although rates of opioid prescriptions have begun to stabilize (13), the proportion of the population using other central nervous system depressants such as benzodiazepines, GABA-ergic sleep medications, muscle relaxants, and gabapentanoids has increased markedly since the early 2000s, more than doubling in most cases (11,14,15). While individuals who drink are slightly less likely to use these medications than non-drinkers, the increases among drinkers have paralleled trends among non-drinkers (16). The combination of increased rates of binge drinking and polypharmacy among middle-aged and older adults seems a conspicuously likely contributor to trends in acute alcohol-related morbidity and mortality.
Two other important social trends likely contribute to increasing rates of alcohol-related morbidity and mortality. The first is that rates of heavy drinking and AUD among women have increased over the past several decades, while rates among men changed little (8,17,18). Because women have lower body mass and a higher percentage of body fat on average, intoxication occurs at lower levels of consumption relative to men, leading to increased risk for acute alcohol-related injury, and higher risk for chronic disease over the long-term. Women are also disproportionally likely to use sedative medications (15,19). Second, the four-decade-long increase in obesity rates is a likely contributor to liver-disease trends because excess weight is an independent risk factor for alcoholic-liver disease progression (20). Liver disease is the most common alcohol-related chronic condition, and its prevalence is increasing not only in the population at large but also at shockingly high rates among adults ages 25–34, a demographic for whom such deaths were previously exceedingly rare (3,21).
Because of these other contributing factors, accurately assessing the risk for alcohol-related morbidity involves understanding the characteristics of the patient who drinks as much as examining the amount and frequency of alcohol consumed. Sex, body mass, adiposity, age, and polypharmacy are significant risk factors for illness and injury related to alcohol consumption. With this understanding, drinking associated with a high risk for injury or illness may not always occur in the context of severe AUD. Accordingly, moderation-oriented interventions as opposed to abstinence-based approaches may be appropriate for many high-risk drinkers.
Screening and intervention
Conventional screening based on quantity and frequency of alcohol consumption is an essential part of any general health assessment, but the exacerbating risk factors discussed here are essential to consider as well. Additionally, some patients may be reticent to discuss excessive alcohol use frankly with a physician if they are not ready to change their behaviour. If a clinician suspects a patient who reports moderate drinking may be at risk for alcohol-related injury or illness based on other risk factors, referral to online resources may be a non-intrusive way to encourage the patient to self-assess and to seek appropriate help. The ‘Rethinking Drinking’ website hosted by the National Institute on Alcohol Abuse and Alcoholism provides assessment and motivational tools for both moderation and abstinence as well as treatment resources (22). The Center for Technology and Behavioral Health website provides a list of ‘program reviews’ for free and commercial online and mobile technology interventions for problem alcohol use and other behavioural health problems (23). The list is intended for providers to identify tools that may be appropriate for their patients and clients. Many free or low-cost technologies are available and can provide screening, motivational tools, coaching, and peer support. A more recent, but higher cost, generation of technologies include remote blood-alcohol monitoring and telemedicine (e.g. ref 24). Referral to technology-based sources is not a substitute for in-person clinician-administered intervention (25), but can be an effective complementary approach (26).
Summary and conclusion
Primary care practitioners can be on the frontlines in mitigating upward trends in alcohol-related morbidity and mortality by being attentive to relevant shifts in the demographics of hazardous alcohol use and thinking beyond conventional screening approaches to identify aggravating risk factors in addition to amount and frequency of alcohol consumed. This will likely lead to increased identification of at-risk drinkers who may benefit from both traditional interventions and newer technology-based and moderation-oriented approaches interventions. Further research into characterizing the demographic and clinical characteristics of drinkers at high risk for injury and chronic illness may help tailor existing interventions or develop new approaches appropriate to the needs of these patients.
It has been hypothesized that alcohol-related morbidity and mortality in the USA are part of a broader ‘deaths of despair’ phenomenon that may result from socioeconomic and cultural conditions unique to the USA (27). Nonetheless, many developed nations resemble the USA in terms of increasing obesity rates, ageing populations, and use of psychotropic prescription drugs, and increasing rates of drinking among women (6,18,28,29). Detailed epidemiologic analyses of alcohol-related morbidity and mortality in other countries are warranted and will shed light on whether the clinical and research implications noted here extend across countries.
Declaration
Funding: National Institutes of Health (NIH) R21 AA025689 (RAG).
Ethical approval: no human subjects involved.
Conflict of interest: none.
References
- 1. Carvalho AF, Heilig M, Perez A, Probst C, Rehm J. Alcohol use disorders. Lancet 2019; 394 (10200):781–92. [DOI] [PubMed] [Google Scholar]
- 2. Griswold MG, Fullman N, Hawley C et al. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018; 392 (10152):1015–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. White AM, Castle I-JP, Hingson RW, Powell PA. Using death certificates to explore changes in alcohol-related mortality in the United States, 1999 to 2017. Alcohol Clin Exp Res 2020; 44 (1):178–87. [DOI] [PubMed] [Google Scholar]
- 4. White AM, Slater ME, Ng G, Hingson R, Breslow R. Trends in alcohol-related emergency department visits in the United States: results from the nationwide emergency department sample, 2006 to 2014. Alcohol Clin Exp Res 2018; 42 (2):352–9. [DOI] [PubMed] [Google Scholar]
- 5. Lipari RN, Van Horn SL. Trends in Substance use Disorders Among Adults Aged 18 or Older.Rockville, MD: Substance Abuse and Mental Health Services Administration, 2017. https://www.samhsa.gov/data/sites/default/files/report_2790/ShortReport-2790.html (accessed on 13 May 2020). [Google Scholar]
- 6. Schumpeter. The Silver Tsunami. The Economist. https://www.economist.com/business/2010/02/04/the-silver-tsunami (accessed on 4 February 2010). [Google Scholar]
- 7. Slater ME, Alpert HR. Apparent per Capita Alcohol Consumption: National, State, and Regional Trends, 1977–2017.National Institute on Alcohol Abuse and Alcoholism, 2019. https://pubs.niaaa.nih.gov/publications/surveillance113/CONS17.htm (accessed on 13 May 2020). [Google Scholar]
- 8. Grucza RA, Sher KJ, Kerr WC et al. Trends in adult alcohol use and binge drinking in the early 21st-century United States: a meta-analysis of 6 national survey series. Alcohol Clin Exp Res 2018; 42 (10):1939–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Castle I-JP, Dong C, Haughwout SP, White AM. Emergency department visits for adverse drug reactions involving alcohol: United States, 2005 to 2011. Alcohol Clin Exp Res 2016; 40 (9):1913–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kaufmann CN, Spira AP, Alexander GC, Rutkow L, Mojtabai R. Trends in prescribing of sedative-hypnotic medications in the USA: 1993–2010: sedative-hypnotic prescribing in the USA. Pharmacoepidemiol Drug Saf 2016; 25 (6):637–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Borodovsky JT, Krauss MJ, Chi T, Bierut LJ, Grucza RA. Trends in prescribed central nervous system depressant medications among adults who regularly consume alcohol: United States 1999 to 2014. Alcohol Clin Exp Res 2019; 43 (7):1510–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mojtabai R. National trends in long-term use of prescription opioids. Pharmacoepidemiol Drug Saf 2018; 27 (5):526–34. [DOI] [PubMed] [Google Scholar]
- 13. Pezalla E, Rosen D, Erensen J, Haddox D, Mayne T. Secular trends in opioid prescribing in the USA. J Pain Res 2017; 10: 383–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA 2015; 314 (17):1818–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Olfson M, Wall M, Wang S, Crystal S, Blanco C. Risks of fatal opioid overdose during the first year following nonfatal overdose. Drug Alcohol Depend 2018; 190: 112–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Borodovsky JT, Krueger RF, Agrawal A, Grucza RA. A decline in propensity toward risk behaviors among U.S. adolescents. J Adolesc Health 2019; 65 (6):745–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Grucza RA, Bucholz KK, Rice JP, Bierut LJ. Secular trends in the lifetime prevalence of alcohol dependence in the United States: a re-evaluation. Alcohol Clin Exp Res 2008; 32 (5):763–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Keyes KM, Grant BF, Hasin DS. Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug Alcohol Depend 2008; 93 (1–2):21–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bertisch SM, Herzig SJ, Winkelman JW, Buettner C. National use of prescription medications for insomnia: NHANES 1999–2010. Sleep 2014; 37 (2):343–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chiang DJ, McCullough AJ. The impact of obesity and metabolic syndrome on alcoholic liver disease. Clin Liver Dis 2014; 18 (1):157–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study. BMJ. 2018; 362: k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. National Institute on Alcohol Abuse and Alcoholism. Rethinking Drinking: Alcohol & Your Health.https://www.rethinkingdrinking.niaaa.nih.gov/ (accessed on 3 March 2020).
- 23. Center for Technology and Behavioral Health. Program Reviews.https://www.c4tbh.org/program-reviews/?f=true&category=mix&commercially_available=mix (accessed on 3 March 2020).
- 24. Mitchell MM, Mendelson J, Gryczynski J, Carswell SB, Schwartz RP. A novel telehealth platform for alcohol use disorder treatment: preliminary evidence of reductions in drinking. Am J Drug Alcohol Abuse. 2020; 46 (3): 297–303. [DOI] [PubMed] [Google Scholar]
- 25. Kaner EF, Beyer FR, Muirhead C et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Drugs and Alcohol Group, ed. Cochrane Database Syst Rev. 2018; 2 (2): CD004148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kaner EF, Beyer FR, Garnett C et al. Personalised digital interventions for reducing hazardous and harmful alcohol consumption in community-dwelling populations. Cochrane Drugs and Alcohol Group, ed. Cochrane Database Syst Rev. 2017; 9 (9): CD011479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci USA 2015; 112 (49):15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wastesson JW, Morin L, Tan ECK, Johnell K. An update on the clinical consequences of polypharmacy in older adults: a narrative review. Expert Opin Drug Saf 2018; 17 (12):1185–96. [DOI] [PubMed] [Google Scholar]
- 29. Agha M, Agha R. The rising prevalence of obesity: part A. Int J Surg Oncol 2017; 2 (7):e17. [DOI] [PMC free article] [PubMed] [Google Scholar]