Abstract
Purpose
We aimed to investigate the effect of a basal opioid infusion in fentanyl-based intravenous patient-controlled analgesia (IV-PCA) on postoperative opioid consumption, pain intensity, and occurrence of opioid-related side effects.
Patients and Methods
We retrospectively reviewed 2097 consecutive patients who received IV-PCA after elective general, thoracic, urologic, and plastic surgery under general anesthesia between June 2019 and October 2019. The patients were divided into two groups: IV-PCA with basal infusion (basal group) and IV-PCA without basal infusion (no basal group). We performed a propensity score matching (PSM) analysis to adjust for baseline differences between both groups. We compared the fentanyl PCA consumption (mcg), pain intensity, rescue analgesic administration, and occurrence of opioid-related side effects (nausea, vomiting, somnolence or dizziness, and overall side effects) during the first 48 hours postoperatively between the two groups before and after PSM.
Results
We analyzed 1317 eligible patients. Of these, 757 (57.5%) patients received IV-PCA without basal infusion. The PSM of the total cohort yielded 539 pairs of cases. After PSM, the fentanyl PCA consumption was significantly lower in the no basal group at 48 hours postoperatively as compared to the basal group (at 24 hours, the median difference: −80 mcg, P<0.001, 95% CI=−112 – −45 mcg; at 48 hours, the median difference: −286 mcg, P<0.001, 95% CI=−380 – −190 mcg), without significantly increasing pain intensity and administration of rescue analgesia. The occurrence of overall opioid-related side effects was also significantly lower in the no basal group (at 24 hours: 31.0% vs 23.0%, OR=0.67, P=0.003, 95% CI=0.51 – 0.87; at 48 hours: 18.9% vs 11.0%, OR=0.48, P<0.001, 95% CI=0.31 – 0.75).
Conclusion
Basal infusion of fentanyl-based IV-PCA was significantly associated with an increase in fentanyl consumption and the occurrence of opioid-related side effects in postsurgical patients.
Keywords: acute pain, analgesia, patient-controlled, opioids, pain, postoperative, perioperative medicine
Introduction
Opioid analgesia using intravenous patient-controlled analgesia (IV-PCA) is widely used for managing postoperative pain.1 Reportedly, it reduces postoperative pain intensity and increases patient satisfaction as compared to pain management without PCA.2 However, it also induces opioid-related side effects, such as postoperative nausea and vomiting (PONV), dizziness, sedation, urinary retention, and respiratory depression.3 These side effects can delay postoperative recovery, increase the length of hospital stay, and increase medical costs.4–6 Therefore, anesthesiologists should try to reduce perioperative opioids and manage postoperative pain effectively.
Basal opioid infusion via an IV-PCA device had been used to improve postoperative pain management.7 However, it does not improve postoperative pain or sleep disturbance and simultaneously increases the incidence of opioid-related side effects.8–10 A previous meta-analysis of 796 postsurgical patients reported that a basal opioid infusion of IV-PCA was significantly associated with a higher incidence of respiratory depression.11 Therefore, routine use of basal opioid infusion in IV-PCA is no longer recommended in practice.1
Nonetheless, IV-PCA with basal fentanyl infusion is still used.12–15 Most of the evidence regarding this issue has been deduced from morphine-based IV-PCA in studies that included a relatively small number of patients.8–10 Due to the different pharmacokinetic properties of fentanyl, evidence of the risks and benefits of basal infusion in fentanyl-based IV-PCA is required. We hypothesized that fentanyl-based IV-PCA without basal infusion could reduce not only opioid-related side effects, but also opioid consumption, without increasing the postoperative pain intensity.
Therefore, we aimed to compare the effect of fentanyl-based IV-PCA with and without basal infusion on the patients’ postoperative opioid consumption via IV-PCA, their pain intensity, and the occurrence of opioid-related side effects during the first 48 hours postoperatively. This study could provide meaningful information on the effective and safe use of fentanyl-based IV-PCA in postsurgical patients.
Patients and Methods
This retrospective observational study was approved by the Institutional Review Board of Seoul National University Hospital, Seoul, Korea (approval no. H-2009-029-1155). Informed consent was waived due to the de-identification and anonymization of the patient records before analysis. All methods were carried out per the STROBE guideline,16 in accordance with the Declaration of Helsinki.
We retrospectively reviewed the acute pain service (APS) database of 2097 consecutive adult patients who received IV-PCA after undergoing elective general, thoracic, urologic, and plastic surgery under general anesthesia. The patients were monitored by the APS team between June 2019 and October 2019. We excluded patients who were admitted to the intensive care unit after surgery, used IV-PCA containing analgesics other than fentanyl, and were absent or discharged when the APS team visited. We did not perform a prior or post hoc power calculation because of our study’s retrospective design and enrolled all patients who met the inclusion criteria.
At our institution, the APS team consists of one anesthesiologist (H-J Lee) and one internist and began the data collection in March 2019. The APS team performed the ward round-up till postoperative day (POD) 2, taking into account the patient’s surgery end time. The APS team investigated the age, sex, type of surgery, pain intensity at rest, and maximal pain intensity during the last 24 hours using an 11-point numeric rating scale (NRS). They also checked the fentanyl consumption (mcg) via IV-PCA and the presence of opioid-related side effects, such as PONV, somnolence, or dizziness, and cessation of IV-PCA and the cause for its cessation. If IV-PCA was temporarily discontinued due to opioid-related side effects and resumed, it was not treated as cessation.
The cohort was divided into two groups: patients who received IV-PCA with basal fentanyl infusion (basal group) and those who received IV-PCA without basal infusion (no basal group). Before the introduction of the IV-PCA without basal infusion, IV-PCA consisted of fentanyl (10–25 μg/mL) at a basal infusion rate of 1 mL/hour (fentanyl 10–25 μg/hour) and a bolus of 1 mL (fentanyl 10–25 μg) with a lockout interval of 10–15 minutes. The dosage of fentanyl was determined according to our previous protocol considering the type of surgery and the patient’s age (Supplemental Table S1). In addition, the attending anesthesiologist decided on the final IV-PCA regimen considering the patient’s weight and underlying disease. During the study period, the APS team changed the IV-PCA regimen. The APS team removed the continuous fentanyl infusion and used only two regimens with different demand doses according to the patient’s age (≤ 80 years: fentanyl of 20 mcg, > 80 years old: fentanyl of 10 mcg), with a lockout interval of 10 minutes. For this evaluation, the surgery type and patient weight were disregarded. The IV-PCA device used during the study period was a semi-electronic disposable pump (AutoMed® 3200, Ace Medical Co., Ltd., Seoul, South Korea). The APS team did not adjust the infusion rate, bolus dose, and lockout time according to the severity of pain during the ward round.
During the study period, there was no change in the anesthetic or perioperative management protocols at our hospital. Anesthesia was induced and maintained with inhalational agents or propofol. Remifentanil was continuously infused during the surgery and titrated to maintain blood pressure within 20% of the baseline ward pressure. Rocuronium was used to maintain neuromuscular blockade. Palonosetron 0.075 mg or ramosetron 0.3 mg was used to prevent PONV.
The patients’ demographic, American Society of Anesthesiologists (ASA) physical status, use of preoperative opioids and antipsychotics, duration of surgery (minutes), and use of continuous wound-infiltration analgesia data were extracted from electronic medical records (EMRs). The extent of the surgery was classified according to the Surgical Outcome Risk Tool (SORT) classification.17 The number of administrations of intravenous rescue analgesics (morphine, fentanyl, tramadol, ketorolac, acetaminophen, pethidine, and nefopam) during the first 24 and 24–48 hours postoperatively was also investigated. The administration of these analgesics was determined by the attending clinicians. We also investigated oxygen administration via the nasal cannula and hypoxemia (defined as an SpO2 of < 90% during the first 48 hours postoperatively), which we retrospectively extracted from the EMRs.
The primary outcome variable was IV fentanyl PCA consumption (mcg) during the first 24 and 24–48 hours postoperatively. We did not calculate the total opioid consumption by converting rescue analgesics to morphine equivalent doses because the rescue analgesics used varied according to the physician and were not administered as per a specific protocol. The secondary outcome variables included pain intensity, rescue analgesic administration, number of rescue analgesics administered, the occurrence of opioid-related side effects (nausea, vomiting, and somnolence or dizziness), cessation of IV-PCA, and the cause of its cessation. The overall opioid-related side effect was defined as the presence of at least one of the following three opioid-related side effects: nausea, vomiting, and somnolence or dizziness.
Statistical Analysis
A propensity score matching (PSM) analysis was conducted to reduce the influence of confounding variables. It was particularly important to minimize the influence of the type of surgery because of the variation in the postoperative pain management protocols depending on the hospital department. Preemptive intercostal nerve blockade was performed by thoracic surgeons in patients who underwent thoracic surgery. IV nonsteroidal anti-inflammatory drugs were routinely administered for multimodal analgesia after plastic surgery. The following variables were used as contributors to the propensity score: age, height, weight, body mass index, preoperative analgesic use, preoperative opioid and antipsychotic use, department of surgery, SORT classification, duration of surgery (minutes), and use of continuous wound-infiltration analgesia. We used a ratio of 1:1 to match patients and employed the neighbor method with a caliper width of 0.1 mm from the pooled standard deviation of the propensity score logit. The balance of the matched patients was evaluated with the standardized mean difference for each contributor. Before and after PSM, we compared the primary and secondary outcomes.
The normality of continuous data was statistically determined by examining the quantile-quantile plot and conducting the Shapiro–Wilk test. Continuous variables were presented as the mean and standard deviation or median and interquartile range. They were compared between the two groups using the independent t-test or Mann–Whitney U-test according to their normality. Categorical variables were presented as frequency or percentage values and were compared between two groups using the χ2 or Fisher’s exact test where appropriate. The median differences and 95% confidence intervals (CIs) between the two groups were estimated using the Hodges-Lehmann method. A two-sided P-value of < 0.05 was considered statistically significant for the primary outcome. R version.3.6.1 software (R Foundation for Statistical Computing, Vienna, Austria) was used to analyze the data.
Results
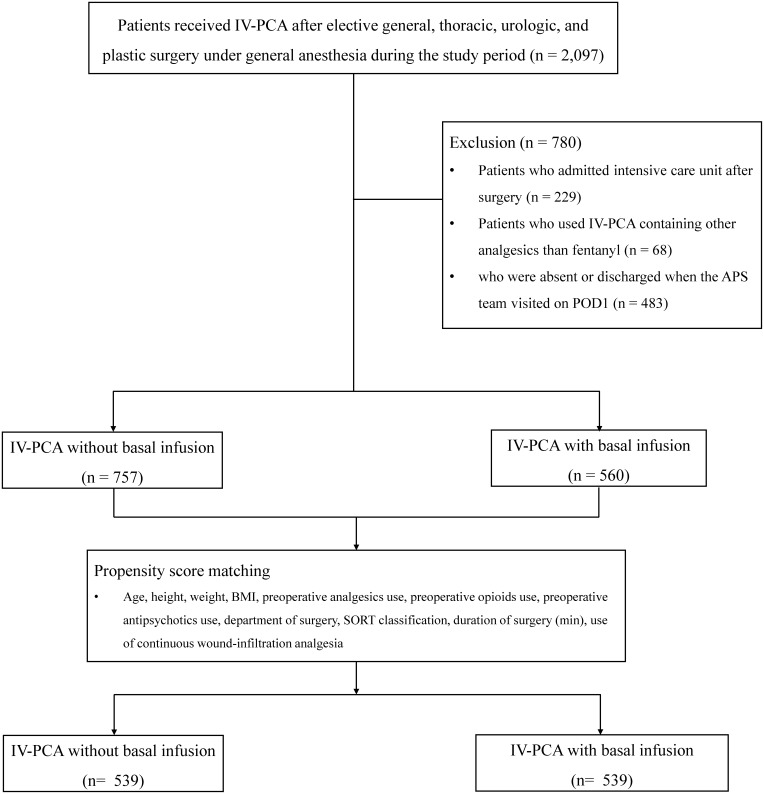
A total of 2097 patients received IV-PCA after elective general, thoracic, urologic, and plastic surgery under general anesthesia during the study period. Finally, data from 1317 eligible patients were analyzed after excluding those who were admitted to the intensive care unit after surgery (n = 229), used IV-PCA containing analgesics other than fentanyl (n = 68), and were absent or discharged when the APS team visited on POD1 (n = 483). Among the included patients, 757 (57.5%) received fentanyl IV-PCA without basal infusion and 560 (42.5%) received fentanyl IV-PCA with basal infusion. After the PSM, 539 patients remained in each group (Figure 1). There were no unbalanced confounders with a standardized difference of > 0.1.
Figure 1.
Flow diagram of the study.
Abbreviations: APS, acute pain service team; BMI, body mass index; IV-PCA, intravenous patient-controlled analgesia; POD, postoperative day; SORT, Surgical Outcome Risk Tool.
Demographic and clinical characteristics are presented in Table 1. Before matching, there were significant differences in the patients’ age and type of surgery between the two groups in the entire cohort. However, there was no significant difference in baseline characteristics between the matched cohorts.
Table 1.
Clinical Comparison Between Patients with and without Basal Infusion of Intravenous Patient-Controlled Analgesia Before and After Propensity Score Matching
| Before Matching | After Matching | |||||||
|---|---|---|---|---|---|---|---|---|
| Basal Group (n=560) | No Basal Group (n=757) | P-value | Standardized Difference | Basal Group (n=539) | No Basal Group (n=539) | P-value | Standardized Difference | |
| Female | 243 (43.4) | 316 (41.7) | 0.588 | 0.033 | 233 (43.2) | 231 (42.9) | 0.951 | 0.007 |
| Age, year | 60 (51–67) | 63 (53–72) | < 0.001 | −0.255 | 60 (51–67) | 61 (51–70) | 0.283 | −0.048 |
| Height, cm | 163.8 (157.2–169.6) | 163.3 (157.2–168.9) | 0.310 | 0.051 | 163.8 (157.2–169.4) | 163.5 (157.1–169.0) | 0.535 | 0.035 |
| Weight, kg | 63.4 (56.2–71.2) | 63.2 (55.8–70.9) | 0.459 | 0.070 | 63.1 (56.0–70.8) | 64.0 (55.8–71.3) | 0.831 | 0.021 |
| BMI, kg/m2 | 23.8 (21.5–26.0) | 23.9 (21.8–25.9) | 0.971 | 0.046 | 23.7 (21.5–25.9) | 24.1 (21.7–26.1) | 0.483 | −0.002 |
| ASA physical status, I/II/III/IV | 115 (20.5)/364 (65.0)/81 (14.5)/0 | 128 (16.9)/532 (70.3)/96 (12.7)/1 (0.1) | 0.129 | 0.037 | 108 (20.0)/352 (65.3)/79 (14.7)/0 | 100 (18.6)/374 (69.4)/64 (11.9)/1 (0.2) | 0.277 | 0.016 |
| Current smoker | 85 (15.2) | 106 (14.0) | 0.549 | 0.033 | 77 (14.3) | 80 (14.8) | 0.796 | 0.016 |
| Preoperative analgesic use | 25 (4.5) | 48 (6.3) | 0.177 | 0.091 | 25 (4.6) | 25 (4.6) | > 0.999 | < 0.001 |
| Preoperative strong opioid use | 4 (0.7) | 8 (1.1) | 0.724 | 0.037 | 4 (0.7) | 4 (0.7) | > 0.999 | 0 |
| Preoperative antipsychotics use | 12 (2.1) | 21 (2.8) | 0.585 | 0.041 | 12 (2.2) | 12 (2.2) | > 0.999 | 0 |
| Type of surgery | 0.007 | −0.191 | 0.484 | 0.006 | ||||
| General surgery | 366 (65.4) | 446 (58.9) | 347 (64.4) | 358 (66.4) | ||||
| Thoracic surgery | 61 (10.9) | 72 (9.5) | 60 (11.1) | 46 (8.5) | ||||
| Urologic surgery | 105 (18.8) | 171 (22.6) | 104 (19.3) | 102 (18.9) | ||||
| Plastic surgery | 28 (5.0) | 68 (9.0) | 28 (5.2) | 33 (6.1) | ||||
| SORT classification, II/III/IV | 31(5.5)/140 (25.0)/389 (69.5) | 51 (6.7)/179 (23.6)/527 (69.6) | 0.609 | 0.018 | 31 (5.8)/134 (24.9)/374 (69.4) | 36 (6.7)/119 (22.1)/384 (71.2) | 0.498 | −0.016 |
| Type of anesthesia | 0.337 | 0.053 | 0.682 | 0.025 | ||||
| Inhalation agent | 404 (72.1) | 564 (74.5) | 388 (72.0) | 394 (73.1) | ||||
| TIVA | 156 (27.9) | 193 (25.5) | 151 (28.0) | 145 (26.9) | ||||
| Surgical time, min | 135 (91–199) | 125 (85–191) | 0.105 | 0.063 | 135.0 (91.0–198.0) | 130.0 (83.0–199.0) | 0.525 | 0.022 |
| Continuous wound-infiltration analgesia use | 12 (2.1) | 28 (3.7) | 0.143 | −0.107 | 11 (2.0) | 14 (2.6) | 0.686 | −0.038 |
Note: The values are presented as the median (interquartile range) or number (%).
Abbreviations: ASA, American society of anesthesiologists; SORT, Surgical Outcome Risk Tool; TIVA, total intravenous anesthesia.
Table 2 shows the comparison between postoperative pain intensity, fentanyl consumption via IV-PCA, and administration of rescue analgesics in both groups. In the entire cohort before matching, fentanyl consumption via IV-PCA during the first 24 hours and 48 hours postoperatively was significantly lower in the no basal group than in the basal group, with median differences of −126 mcg (P<0.001, 95% CI=−180 – −90 mcg) and −378 mcg (P<0.001, 95% CI=−464 − −288 mcg), respectively. Significant differences in fentanyl consumption remained between the matched groups (during the first 24 hours: median difference = −80 mcg, P<0.001, 95% CI=−112 − −45 mcg; during the first 48 hours: median difference = −286 mcg, P<0.001, 95% CI=−380 – −190 mcg).
Table 2.
Comparison Between Postoperative Pain Intensity, Fentanyl Consumption Using Intravenous Patient-Controlled Analgesia (IV-PCA), and Rescue Analgesic Use in Patients with and without Basal Infusion of Fentanyl in IV-PCA Before and After Propensity Score Matching
| Before Matching | After Matching | |||||||
|---|---|---|---|---|---|---|---|---|
| Basal Group | No Basal Group | P-value | Median Difference (95% CI) | Basal Group | No Basal Group | P-value | Median Difference (95% CI) | |
| At 24h postoperatively | ||||||||
| Total numbers | 560 | 757 | 539 | 539 | ||||
| NRS at resting, 0–10 | 4 (2–6) | 4 (2–6) | 0.044 | 0 (0–1) | 4 (2–6) | 4 (2–6) | 0.032 | 0 (0–1) |
| Maximal NRS, 0–10 | 7 (5–8) | 7 (5–8) | 0.910 | 0 (0–0) | 7 (5–8) | 7 (5–8) | 0.620 | 0 (0–0) |
| IV fentanyl PCA use, mcg | 604 (480–742) | 460 (120–740) | < 0.001 | −126 (−180 – −90) | 600 (480–743) | 520 (160–760) | < 0.001 | −80 (−112 – −45) |
| Rescue analgesics use during first 24 h postoperatively | 333 (59.5) | 456 (60.2) | 0.821 | 319 (59.2) | 316 (58.6) | 0.901 | ||
| Number of rescue analgesics during first 24 h postoperatively | 1 (0–2) | 1 (0–2) | 0.456 | 0 (0–0) | 1 (0–2) | 1 (0–1) | 0.971 | 0 (0–0) |
| At 48h postoperatively | ||||||||
| Total numbers | 352 | 419 | 338 | 300 | ||||
| NRS at resting, 0–10 | 3 (1–4) | 3 (1–4) | 0.152 | 0 (0–1) | 3 (1–4) | 3 (1–4) | 0.146 | 0 (0–1) |
| Maximal NRS, 0–10 | 5 (4–7) | 5 (3–7) | 0.143 | 0 (−1 – 0) | 5 (4–7) | 5 (3–7) | 0.347 | 0 (−1 – 0) |
| IV fentanyl PCA use, mcga | 1080 (768–1340) | 600 (230–1140) | < 0.001 | −378 (−464 – −288) | 1074 (757–1299) | 720 (300–1200) | < 0.001 | −286 (−380 – −190) |
| Rescue analgesics use during 24–48h postoperatively | 57 (16.2) | 92 (22.0) | 0.054 | 87 (25.8) | 86 (28.7) | 0.420 | ||
| Number of rescue analgesics during 24–48h postoperatively | 0 (0–0) | 0 (0–0) | 0.043 | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0.068 | 0 (0–0) |
Notes: The values are presented as the median (interquartile range). aThis included 367 patients without basal infusion and 314 patients with basal infusion before matching. This included 266 patients without basal infusion and 303 patients with basal infusion after matching.
Abbreviations: NRS, numeric rating scale; PCA, patient-controlled analgesia.
Table 3 shows the comparison of opioid-related side effects between the two groups. In the entire cohort before matching, the occurrence of overall opioid-related side effects during the first 24 hours and at 24–48 hours postoperatively was significantly lower in the no basal group (during the first 24 hours: odds ratio [OR]=0.75, P=0.019, 95% CI=0.58–0.95; at 24–48 hours: OR=0.57, P=0.005, 95% CI=0.38–0.84). In the matched cohort, after matching the overall opioid-related side effects during the first 24 hours and at 24–48 hours postoperatively remained significantly lower in the basal group (during the first 24 hours: OR=0.67, P=0.003, 95% CI=0.51–0.87; at 24–48 hours: OR=0.48, P<0.001, 95% CI=0.31–0.75). Oxygen administration via the nasal cannula and occurrence of hypoxemia during the first 48 hours postoperatively did not show significant differences between the two groups before and after PSM.
Table 3.
Comparison Between the Opioid-Related Side Effects Between Patients with and without a Basal Infusion of Intravenous Patient-Controlled Analgesia Before and After Propensity Score Matching
| Before Matching | After Matching | |||||||
|---|---|---|---|---|---|---|---|---|
| Basal Group | No Basal Group | P-value | Odds Ratio (95% CI) | Basal Group | No Basal Group | P-value | Odds Ratio (95% CI) | |
| During the first 24h postoperatively | ||||||||
| Total numbers | 560 | 757 | 539 | 539 | ||||
| Overall opioid-related side effects | 171 (30.5) | 187 (24.7) | 0.019 | 0.75 (0.58–0.95) | 167 (31.0) | 124 (23.0) | 0.003 | 0.67 (0.51–0.87) |
| Nausea | 121 (21.6) | 135 (17.8) | 0.088 | 0.79 (0.60–1.04) | 119 (22.1) | 85 (15.8) | 0.008 | 0.66 (0.49–0.90) |
| Vomiting | 15 (2.7) | 11 (1.5) | 0.120 | 0.54 (0.24–1.18) | 15 (2.8) | 7 (1.3) | 0.092 | 0.46 (0.19–1.14) |
| Somnolence or dizziness | 72 (12.9) | 78 (10.3) | 0.150 | 0.78 (0.55–1.09) | 70 (13.0) | 54 (10.0) | 0.128 | 0.75 (0.51–1.09) |
| During the 24–48h postoperatively | ||||||||
| Total numbers | 353 | 419 | 300 | 338 | ||||
| Overall opioid-related side effects | 67 (19.0) | 49 (11.7) | 0.005 | 0.57 (0.38–0.84) | 64 (18.9) | 33 (11.0) | < 0.001 | 0.48 (0.31–0.75) |
| Nausea | 48 (13.6) | 38 (9.1) | 0.046 | 0.63 (0.40–1.00) | 45 (13.3) | 24 (8.0) | 0.002 | 0.43 (0.26–0.73) |
| Vomiting | 6 (1.7) | 2 (0.5) | 0.118 | 0.28 (0.06–1.38) | 6 (1.8) | 1 (0.3) | 0.075 | 0.15 (0.02–1.21) |
| Somnolence or dizziness | 21 (6.0) | 15 (3.6) | 0.124 | 0.59 (0.30–1.16) | 21 (6.2) | 13 (4.3) | 0.081 | 0.53 (0.26–1.08) |
| O2 administration via nasal cannula in the ward during the first 48h postoperatively | 26 (4.6) | 32 (4.2) | 0.890 | 1.04 (0.61–1.78) | 26 (4.8) | 22 (4.1) | 0.304 | 0.73 (0.41–1.32) |
| Hypoxemia during the first 48h postoperatively | 3 (0.5) | 3 (0.4) | - | 3 (0.6) | 3 (0.6) | - | ||
Note: The values are presented as the number (%) or the odds ratio (95% confidence interval [CI]).
Table 4 shows the comparison between the cessation of IV-PCA during the first 48 hours postoperatively and its cause in both groups. In the entire cohort before PSM, the cessation of IV-PCA during the first 24 hours and at 24–48h hours postoperatively were significantly higher in the basal group than in the no basal group (during the first 24 hours: OR=0.45, P<0.001, 95% CI=0.30–0.67; 24–48h: OR 0.63, P=0.015, 95% CI=0.43–0.91). The proportion of cessations of IV-PCA due to opioid-related side effects were also significantly higher in the basal group than in the no basal group (during the first 24 hours: OR=0.35, P<0.001, 95% CI=0.22–0.55; at 24–48 hours: OR=0.37, P=0.002, 95% CI=0.20–0.70). All these significant differences remained after PSM.
Table 4.
Comparison Between the Cessation of Intravenous Patient-Controlled Analgesia (IV-PCA) and Its Cause Between Patients with and without Basal Infusion of Fentanyl Before and After Propensity Score Matching
| Before Matching | After Matching | |||||||
|---|---|---|---|---|---|---|---|---|
| Basal Group | No Basal Group | P-value | Odds Ratio (95% CI) | Basal Group | No Basal Group | P-value | Odds Ratio (95% CI) | |
| During the first 24h postoperatively | ||||||||
| Total numbers, n | 560 | 757 | 539 | 539 | ||||
| IV-PCA cessation | 66 (11.8) | 43 (5.7) | < 0.001 | 0.45 (0.30–0.67) | 65 (12.1) | 31 (5.8) | < 0.001 | 0.45 (0.29–0.69) |
| Cause of IV-PCA cessation | ||||||||
| Opioids related side effects | 56 (10.0) | 28 (3.7) | < 0.001 | 0.35 (0.22–0.55) | 55 (10.2) | 19 (3.5) | < 0.001 | 0.32 (0.19–0.55) |
| Other than side effects | 10 (1.8) | 15 (2.0) | 10 (1.9) | 12 (2.2) | ||||
| Tolerable pain | 4 (0.7) | 10 (1.3) | 4 (0.7) | 8 (1.5) | ||||
| Conversion to oral analgesics | 5 (0.9) | 4 (0.5) | 5 (0.9) | 3 (0.6) | ||||
| Patient refusal | 1 (0.2) | 1 (0.1) | 1 (0.3) | 1 (0.3) | ||||
| During the 24–48h postoperatively | ||||||||
| Total numbers, n | 352 | 419 | 338 | 300 | ||||
| IV-PCA cessation | 74 (21.0) | 60 (14.3) | 0.015 | 0.63 (0.43–0.91) | 70 (20.7) | 42 (14.0) | 0.027 | 0.62 (0.41–0.95) |
| Cause of IV-PCA cessation | ||||||||
| Opioids related side effects | 32 (9.1) | 15 (3.6) | 0.002 | 0.37 (0.20–0.70) | 29 (8.6) | 8 (2.7) | 0.003 | 0.29 (0.13–0.65) |
| Other than side effects | 42 (11.9) | 45 (10.7) | 51 (15.1) | 34 (11.3) | ||||
| Tolerable pain | 19 (5.4) | 15 (3.6) | 18 (5.3) | 10 (3.3) | ||||
| Conversion to oral analgesics | 22 (6.3) | 32 (7.6) | 32 (9.5) | 24 (8.0) | ||||
| Patient refusal | 1 (0.3) | 0 | 1 (0.3) | 0 | ||||
Note: The values are presented as the number (%) or the odds ratio (95% confidence interval [CI]).
Discussion
In this study, we investigated the effect of basal opioid infusion in fentanyl-based IV-PCA on postoperative opioid consumption and opioid-related side effects in postsurgical patients. Our major finding was that not administering a basal infusion in fentanyl-based IV-PCA significantly reduced the patients’ postoperative fentanyl consumption via IV-PCA and the occurrence of opioid-related side effects. Further, it did not increase the pain intensity or lead to the requirement of a rescue analgesic during the first 48 hours postoperatively. Our results could provide useful information to physicians, allowing them to eliminate the use of basal infusion in fentanyl-based IV-PCA.
Fentanyl is likely more suitable for IV-PCA than morphine due to its rapid onset and short duration of action.18 Fentanyl reportedly causes less respiratory depression than morphine.19 Further, in a previous study, the occurrence of opioid-related side effects and the median pain score were lower in postsurgical patients using a fentanyl-based IV-PCA as compared to those using morphine-based IV-PCA.20 Another study that compared continuous IV infusions of fentanyl and morphine found that as compared to morphine, fentanyl resulted in a decreased need for rescue analgesics, rapid bowel recovery, and shorter hospital stay in patients who underwent open gynecological surgery.21
However, to the best of our knowledge, there is little evidence regarding the effect of basal infusion in fentanyl-based IV-PCA.22,23 One retrospective study suggested that a basal infusion rate of 0.12–0.67 mcg/kg/hour of fentanyl could be used safely in IV-PCA without any serious side effects.22 However, the study investigated only the postoperative rescue analgesic and antiemetic requirements as binary outcomes without providing any information regarding the pain intensity and occurrence of opioid-related side effects.22 Although the authors described that the rescue drugs were administered according to hospital protocol, this might not have been properly controlled considering the retrospective study design.22 They also did not explain the inclusion of IV-PCA patients with a basal infusion rate of 2 mL/hour, while excluding patients with a basal infusion rate of 1 mL/hour.22 Another retrospective study conducted on patients undergoing gynecological laparoscopic surgery reported that basal infusion of fentanyl was significantly associated with delayed ambulation and orthostatic intolerance on POD1.23 However, the infusion device was only used for continuous infusion and not for PCA, and the number of patients with delayed ambulation was too small (5/195) to support their conclusion.23 Therefore, the rationale for the use of basal infusion in the fentanyl-based IV-PCA is not sufficient in the literature.
Our results are largely consistent with those of previous studies that investigated the analgesic effect of basal infusion in morphine-based IV-PCA. Prior studies reported that a basal infusion in the morphine-based IV-PCA did not improve postoperative pain control, but increased the postoperative opioid consumption.9,10,24,25 Basal infusion administered only at nighttime also failed to improve postoperative pain and sleep patterns.8 One randomized controlled study on patients who underwent coronary artery bypass grafting surgery reported that the addition of a basal infusion of morphine improved postoperative analgesia; however, it increased postoperative morphine consumption.26 In our study, the fentanyl-based IV-PCA without basal infusion significantly decreased the postoperative opioid consumption and did not lead to an increase in postoperative pain intensity or the rescue analgesic requirement.
Reducing perioperative opioid use is an important task in perioperative medicine.27 Although opioids are still widely used in postoperative pain management, they can induce tolerance and hyperalgesia, which can make postoperative pain control difficult.28 Additionally, perioperative opioids can also induce opioid-related side effects (such as PONV), decrease gastrointestinal motility, and delay postoperative recovery.29,30 Therefore, opioid-sparing by not administering basal infusion in fentanyl-based IV-PCA is expected to improve postoperative recovery.
One of the advantages of not using basal infusion was highlighted in our study, i.e., not administering basal infusion was significantly associated with a decrease in the occurrence of opioid-related side effects, especially postoperative nausea. Unlike our study, previous studies on morphine-based IV-PCA did not report a significant association between not using basal infusion and a reduction in opioid-related side effects.9,10,24 However, these studies may have failed to produce significant results due to relatively small sample sizes. On the other hand, although our study is limited due to its retrospective design, we were able to identify a significant association between basal infusion and the occurrence of opioid-related side effects in a sufficient number of patients even after PSM.
Unlike a previous meta-analysis in morphine-based IV-PCA,11 our results failed to show a significant association between not using basal infusion and the occurrence of respiratory depression. This might be due to the limitation of power because postoperative respiratory depression rarely occurred in our subjects. The relatively low incidence rate of respiratory depression after the use of fentanyl as compared to morphine also may have contributed to this insignificant result.
Our study should be interpreted cautiously in light of its limitations. First, this study is inherently limited in its retrospective design. Although we performed PSM analysis to reduce the bias, unknown or unmeasured covariates could have affected our results. Second, because our results were obtained from a single tertiary university hospital, it is difficult to generalize the findings. Third, although we investigated the pain intensity and rescue analgesic requirement, these parameters may not be enough to assess the quality of postoperative pain management. Fourth, we used only two IV-PCA regimens with different bolus doses depending on the patient’s age. However, the outcome could vary depending on the bolus dose and lockout time of IV-PCA. Further studies regarding the optimal bolus dose and lockout time of fentanyl-based IV-PCA are required to determine its optimal use. Finally, a substantial number of patients were excluded because they were lost to follow-up. Especially, since the APS team worked only during the week, patients who underwent surgery on Friday or the day before a holiday were excluded. Despite these limitations, to the best of our knowledge, this is the first study to evaluate the effect of not administering basal infusion in fentanyl-based IV-PCA for postsurgical patients.
Conclusion
In conclusion, not administering a basal infusion in fentanyl-based IV-PCA was significantly associated with a reduction in postoperative fentanyl consumption and the occurrence of opioid-related side effects. Our study supports the justification for not using basal infusions in fentanyl-based IV-PCA for postsurgical patients. Our findings will be useful for physicians and recovery nurses and enable them to ultimately eliminate basal infusions in their patients.
Acknowledgments
We would like to thank Editage (www.editage.co.kr) for English language editing. These two authors equally contributed to this work as co-first authors: Haesun Jung and Kook Hyun Lee.
Funding Statement
This work was supported by a grant from the Seoul National University Hospital (0620062449).
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Chou R, Gordon DB, de Leon-casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regio;nal Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131–157. doi: 10.1016/j.jpain.2015.12.008 [DOI] [PubMed] [Google Scholar]
- 2.McNicol ED, Ferguson MC, Hudcova J. Patient controlled opioid analgesia versus non-patient controlled opioid analgesia for postoperative pain. Cochrane Database Syst Rev. 2015;6:Cd003348. doi: 10.1002/14651858.CD003348.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Momeni M, Crucitti M, De Kock M. Patient-controlled analgesia in the management of postoperative pain. Drugs. 2006;66(18):2321–2337. doi: 10.2165/00003495-200666180-00005 [DOI] [PubMed] [Google Scholar]
- 4.Park KO, Lee YY. Orthostatic intolerance ambulation in patients using patient controlled analgesia. Korean J Pain. 2013;26(3):277–285. doi: 10.3344/kjp.2013.26.3.277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oderda GM, Evans RS, Lloyd J, et al. Cost of opioid-related adverse drug events in surgical patients. J Pain Symptom Manage. 2003;25(3):276–283. doi: 10.1016/s0885-3924(02)00691-7 [DOI] [PubMed] [Google Scholar]
- 6.Eberhart LH, Morin AM, Wulf H, Geldner G. Patient preferences for immediate postoperative recovery. Br J Anaesth. 2002;89(5):760–761. doi: 10.1093/bja/89.5.760 [DOI] [PubMed] [Google Scholar]
- 7.Sinatra R, Chung KS, Silverman DG, et al. An evaluation of morphine and oxymorphone administered via patient-controlled analgesia (PCA) or PCA plus basal infusion in postcesarean-delivery patients. Anesthesiology. 1989;71(4):502–507. doi: 10.1097/00000542-198910000-00005 [DOI] [PubMed] [Google Scholar]
- 8.Parker RK, Holtmann B, White PF. Effects of a nighttime opioid infusion with PCA therapy on patient comfort and analgesic requirements after abdominal hysterectomy. Anesthesiology. 1992;76(3):362–367. doi: 10.1097/00000542-199203000-00007 [DOI] [PubMed] [Google Scholar]
- 9.Parker RK, Holtmann B, White PF. Patient-controlled analgesia. Does a concurrent opioid infusion improve pain management after surgery? JAMA. 1991;266:1947–1952. doi: 10.1001/jama.1991.03470140059024 [DOI] [PubMed] [Google Scholar]
- 10.Russell AW, Owen H, Ilsley AH, Kluger MT, Plummer JL. Background infusion with patient-controlled analgesia: effect on postoperative oxyhaemoglobin saturation and pain control. Anaesth Intensive Care. 1993;21(2):174–179. doi: 10.1177/0310057X9302100207 [DOI] [PubMed] [Google Scholar]
- 11.George JA, Lin EE, Hanna MN, et al. The effect of intravenous opioid patient-controlled analgesia with and without background infusion on respiratory depression: a meta-analysis. J Opioid Manag. 2010;6(1):47–54. doi: 10.5055/jom.2010.0004 [DOI] [PubMed] [Google Scholar]
- 12.Hwang J, Min SK, Chae YJ, Lim GM, Joe HB. Continuous fentanyl background infusion regimen optimised by patient-controlled analgesia for acute postoperative pain management: a randomised controlled trial. J Clin Med. 2020;9(1):211. doi: 10.3390/jcm9010211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chae D, Kim SY, Song Y, et al. Dynamic predictive model for postoperative nausea and vomiting for intravenous fentanyl patient-controlled analgesia. Anaesthesia. 2020;75(2):218–226. doi: 10.1111/anae.14849 [DOI] [PubMed] [Google Scholar]
- 14.Lee CY, Narm KS, Lee JG, et al. A prospective randomized trial of continuous paravertebral infusion versus intravenous patient-controlled analgesia after thoracoscopic lobectomy for lung cancer. J Thorac Dis. 2018;10(6):3814–3823. doi: 10.21037/jtd.2018.05.161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim K-M. Analysis of the current state of postoperative patient-controlled analgesia in Korea. Anesth Pain Med. 2016;11(1):28–35. doi: 10.17085/apm.2016.11.1.28 [DOI] [Google Scholar]
- 16.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. doi: 10.1016/j.ijsu.2014.07.013 [DOI] [PubMed] [Google Scholar]
- 17.Protopapa KL, Simpson JC, Smith NC, Moonesinghe SR. Development and validation of the Surgical Outcome Risk Tool (SORT). Br J Surg. 2014;101(13):1774–1783. doi: 10.1002/bjs.9638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grass JA. Patient-controlled analgesia. Anesth Analg. 2005;101(Supplement):S44–S61. doi: 10.1213/01.ane.0000177102.11682.20 [DOI] [PubMed] [Google Scholar]
- 19.Cepeda MS, Farrar JT, Baumgarten M, Boston R, Carr DB, Strom BL. Side effects of opioids during short-term administration: effect of age, gender, and race. Clin Pharmacol Ther. 2003;74(2):102–112. doi: 10.1016/S0009-9236(03)00152-8 [DOI] [PubMed] [Google Scholar]
- 20.Hutchison RW, Chon EH, Tucker WF, Gilder R, Moss J, Daniel P. A comparison of a fentanyl, morphine, and hydromorphone patient-controlled intravenous delivery for acute postoperative analgesia: a multicenter study of opioid-induced adverse reactions. Hosp Pharm. 2006;41(7):659–663. doi: 10.1310/hpj4107-659 [DOI] [Google Scholar]
- 21.Russo A, Grieco DL, Bevilacqua F, et al. Continuous intravenous analgesia with fentanyl or morphine after gynecological surgery: a cohort study. J Anesth. 2017;31(1):51–57. doi: 10.1007/s00540-016-2268-0 [DOI] [PubMed] [Google Scholar]
- 22.Shin S, Min KT, Shin YS, Joo HM, Yoo YC. Finding the ‘ideal’ regimen for fentanyl-based intravenous patient-controlled analgesia: how to give and what to mix? Yonsei Med J. 2014;55(3):800–806. doi: 10.3349/ymj.2014.55.3.800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iwata Y, Mizota Y, Mizota T, Koyama T, Shichino T. Postoperative continuous intravenous infusion of fentanyl is associated with the development of orthostatic intolerance and delayed ambulation in patients after gynecologic laparoscopic surgery. J Anesth. 2012;26(4):503–508. doi: 10.1007/s00540-012-1391-9 [DOI] [PubMed] [Google Scholar]
- 24.Mota FA, Marcolan JF, Pereira MH, Milanez AM, Dallan LA, Diccini S. Comparison study of two different patient-controlled anesthesia regiments after cardiac surgery. Rev Bras Cir Cardiovasc. 2010;25(1):38–44. doi: 10.1590/S0102-76382010000100011 [DOI] [PubMed] [Google Scholar]
- 25.Hansen LA, Noyes MA, Lehman ME. Evaluation of patient-controlled analgesia (PCA) versus PCA plus continuous infusion in postoperative cancer patients. J Pain Symptom Manage. 1991;6(1):4–14. doi: 10.1016/0885-3924(91)90066-D [DOI] [PubMed] [Google Scholar]
- 26.Guler T, Unlugenc H, Gundogan Z, Ozalevli M, Balcioglu O, Topcuoglu MS. A background infusion of morphine enhances patient-controlled analgesia after cardiac surgery. Can J Anaesth. 2004;51(7):718–722. doi: 10.1007/BF03018432 [DOI] [PubMed] [Google Scholar]
- 27.Alexander JC, Patel B, Joshi GP. Perioperative use of opioids: current controversies and concerns. Best Pract Res Clin Anaesthesiol. 2019;33(3):341–351. doi: 10.1016/j.bpa.2019.07.009 [DOI] [PubMed] [Google Scholar]
- 28.Colvin LA, Bull F, Hales TG. Perioperative opioid analgesia-when is enough too much? A review of opioid-induced tolerance and hyperalgesia. Lancet. 2019;393(10180):1558–1568. doi: 10.1016/S0140-6736(19)30430-1 [DOI] [PubMed] [Google Scholar]
- 29.Tripathy S, Rath S, Agrawal S, et al. Opioid-free anesthesia for breast cancer surgery: an observational study. J Anaesthesiol Clin Pharmacol. 2018;34(1):35–40. doi: 10.4103/joacp.JOACP_143_1729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keller DS, Zhang J, Chand M. Opioid-free colorectal surgery: a method to improve patient & financial outcomes in surgery. Surg Endosc. 2019;33(6):1959–1966. doi: 10.1007/s00464-018-6477-5 [DOI] [PubMed] [Google Scholar]