Abstract
Aim
In addition to its respiratory impact of SARS-CoV2, skin lesions of probable vascular origin have been described. This study intends to quantify the incidence of acro-ischemic lesions in COVID-19 infected adult subjects in our population, describing clinical patterns and associated findings.
Methods
All adult confirmed cases of COVID-19 infection who presented with acro-ischemic lesions and received care in our institution were prospectively enrolled up to May 15th, 2020. The variables included demographics, comorbidities, analytical parameters, clinical presentations and COVID-19 treatment.
Results
We enrolled 24 patients. The overall rate of acro-ischemic findings in COVID-19 patients was 1.2% [0.6% for outpatients and 2.9% for hospitalized (ICU and non-ICU patients)], but the observed incidence for acro-ischemia in ICU patients was remarkably higher (23.0%, p<0.001). We have described four different clinical patterns of acroischemia: atypical Raynaud´s phenomenon (ARP), (4); pseudo-pernio (PP), (5); severe microcirculatory ischemia with preserved pulse (SMI), (6); and dry gangrene with arteriosclerosis obliterans (AO), (9). Kendall´s τ correlation with lung disease severity was 0.877 (95% CI, 0.756 to 0.968); p<0.01). ARP individuals were predominantly female, while SMI appeared lately in elderly hospitalized subjects with better prognosis. AO occurred in patients with more comorbidity and younger than those with SMI. We observed other associated lesions of suggestive ischemic nature in other organs in all groups (15 patients of total sample). Plasma procalcitonin was significantly higher in patients who developed SMI (median and interquartile range: 9.99 (4.2, 12.3) mg/mL vs 0.26 (0.11, 0.89) mg/mL; p<0.001), and D-dimer level at hospital admission was significantly higher in AO patients (median and interquartile range: 1166 (1050, 2111) mg/L vs 502 (448, 777) mg/L; p<0.001).
Conclusion
The observed risk for acroischemia in COVID-19 is high in ICU patients (23%). We have described four different clinical patterns of acroischemia (ARP, PP, SMI and AO) associated with lung disease severity. Authors have communicated various lesions of suggestive ischemic nature in other organs. Raynaud-like pattern is reported as a ”novelty”.
Keywords: acro-ischemia, COVID-19, Raynaud´s phenomenon, ischemia reperfusion injury, hypercoagulability, thromboinflammation
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Severe acute respiratory distress syndrome-coronavirus 2 (SARS-CoV-2) was initially identified in Wuhan, in December 20191 and later declared by the World Health Organization as a pandemic.2 During the first wave, Spain was the second country in number of infected people, with 247,000 confirmed cases and 28,678 deaths on June 24 2020. Madrid was the most affected community, reaching more than 70,934 cases and 8931 deaths in the same period.3 SARS-CoV-2 infects the endothelial cells using the angiotensin converting enzyme 2 (ACE2) receptor with subsequent severe endothelial injury.4,5 This endothelial disfunction would lead to the loss of these cells fibrinolytic function, predisposing to thrombus formation.6–9 Besides, the activation of the innate and adaptative immune cells and insufficient clearance of chemokines induce progressive thromboinflamatory response and hypercoagulability.10 Clinical symptoms of COVID-19 vary widely. Most of the patients remain asymptomatic or present a mild form with flu-like symptoms. Additional symptoms may include shivering, throat pain, anosmia, headache, joint pain, nausea and diarrhea. In moderate forms, marked inflammation and progressive pneumonia may cause dyspnea, respiratory failure, acute respiratory distress syndrome (ARDS) and multiorgan failure, with death rates ranging from 4.4% to 10%.11,12 The severity of the disease depends on several co-factors (age, sex, etc.) and comorbidities.13–15
Since the pandemic outbreak, new clinical features have been reported, such as neurological, myocardial, ophthalmic or cutaneous events.16 Pseudo-chilblains in pauci-symptomatic children and adults have been widely described as a new late clinical manifestation. However, the true incidence of this type of skin injury remains unknown.17–20 More severe manifestations of thrombotic affectation, such as acro-ischemia and its complications, are also infrequent in adults and still do not have a well-quantified incidence and management pathway. Most of the reports on a high incidence of thrombotic complications are in relation to deep vein thrombosis and pulmonary embolism, while the evidence about arterial thrombosis in patients with COVID-19 is lower and limited to case reports.10,21–25
This study intends to quantify the incidence of acro-ischemic lesions (AIL) in COVID-19-infected adults in our population, describing clinical patterns and associated findings.
Methods
Our tertiary care hospital covers sanitary area of Carabanchel, one of the three most affected districts. All adult cases of COVID-19 infection who presented acro-ischemic lesions and received care in our institution (hospitalised or telematic) were prospectively enrolled in a database up to May 15th, 2020. In accordance with the criteria of the European Society for Vascular Surgery (ESVS) Clinical Practice Guidelines for the Management of Acute Limb Ischemia, patients with ordinary causes of acute ischemia and COVID-19 infection were not included, considering a non-causal relationship. Cases with bilateral ischemic necrosis after vasoactive drug support in Intensive Care Units were also excluded.
Working Definitions
Acro-ischemic lesions (AIL): Extremities vasomotor disorders responsible of distal acute ischemia. This name groups together different patterns.
Atypical Raynaud phenomenon (ARP): asymmetrical episodic reversible discoloration without tissue loss. No association with cold exposure. It appears to be due to a local alteration in thermoregulatory vessels although central nervous system´s influence cannot be ruled out. It shares characteristics of primary and secondary Raynaud´s phenomenon.
Pseudo-pernio (PP): mimics chilblains except for its asymmetrical topography, the absence of pain and cold exposure.
Severe microcirculatory ischemia (livedo, purpura) with preserved pulse (SMI): mimics blue toe syndrome by cholesterol crystal embolism but it is reversible and involves hands and feet, not limiting to fingers and toes. They were usually tender to palpation.
Dry gangrene with arteriosclerosis obliterans (AO): mimics Buerger´s disease. Absence of distal pulses and gangrene establishment. Deficiency in blood perfusion related to occlusion of distal (tibial, cubital, radial) or ultra-distal (below-ankle/wrist) arteries was documented by plain Duplex examination.
COVID-19 infection was confirmed by means of a reverse transcription polymerase chain reaction (RT-PCR) test from nasopharyngeal samples. Since the sensitivity of RT-PCR is in the 50–80% range, negative patients with symptoms consistent with COVID-19 were diagnosed as probable cases. Serological tests were also performed to check the immunological status in relation to the COVID infection.
The gathered variables included demographics, comorbidities, analytical parameters, clinical presentations and COVID-19 treatment. Follow-up included periodical visits both during hospitalization and by remote assistance (including imaging) after discharge. Informed consent was obtained from all included patients. This study was conducted in accordance with the Declaration of Helsinki. Ethics Committee of Drug Research of the Central Defense Hospital provided authorization for this study (Code 25/20. COVID-19 Research Area; date of approval: 07/04/2020).
Statistical analysis was mostly descriptive. Categorical variables were described as frequencies, and quantitative variables using mean and standard deviation. If a distribution non-assumable to a Gaussian normal curve was detected, median and interquartile range were used instead. Frequencies were compared using Pearson’s Chi-square test. Quantitative variables were compared using Mann–Whitney’s U-test. Kendall´s tau and Spearman´s rank correlation coefficients (95% CI) were used to measure association strength of the main ordinal variables of the study. All calculations were performed using IBM SPSS version 25.0 (IBM Corp., Armonk, NY, USA).
Results
A total of 2051 cases of COVID-19 were diagnosed in our institution’s assigned area up to May 15th. Five hundred and fourteen (25,1%) of them needed a hospital admission and 39 (1.9%) were transferred to the intensive care unit. The overall rate of acro-ischemic findings in COVID-19 patients was 1.2% (0,6% for outpatients and 2.9% for hospitalized patients), but the observed incidence for acro-ischemia in ICU patients was remarkably higher (23.0%, p<0.001).
Four different clinical patterns of AIL could be identified (Figure 1): ARP(4), PP(5), SMI(6) and AO(9). All types were a late manifestation of COVID-19 infection and SMI debut was the one to appear the latest. None of the patients had fever documented in the days prior to the appearance of the acro-ischemic event.
Figure 1.
Clinical patterns of acroischemia. Upper: Outpatients (ARP and PP). Lower: Hospitalized patients (SMI and AO).
Tables 1–3 show the demographic and clinical characteristics of the included patients. According to COVID-19 clinical severity, ARP and PP were considered mild manifestations and could be observed only in patients managed without in-hospital admission. ARP individuals were predominantly female (75%). SMI was considered as a moderate affectation and AO as severe; both were observed only in hospitalized patients. ARP episodes were painful with a mean duration of 15 minutes, and occurring mostly in the evenings. All cases referred a very characteristic frequency of appearance: the first episode occurred 10 days after the viral symptoms; the second one, 4–5 days after the first one; and the last one, 9–10 days from the second one, alternating between hands and feet. Headache was the commonest accompanying symptom, while two subjects presented strong low back pain of inflammatory characteristics. No one had a previous history of primary Raynaud´s phenomenon. No new episode occurred during follow-up.
Table 1.
Demographic Characteristics of Patients with COVID-19 Infection and Acro-Ischemia
| Demographic Characteristics | Atypical Raynaud Phenomenon (n=4) | Pseudo-Pernio (n=5) | Severe Microcirculatory Ischemia with Preserved Pulse (n=6) | Dry Gangrene with Arteriosclerosis Obliterans (n=9) |
|---|---|---|---|---|
| Age; yr (mean±standard deviation) | 45±5 | 44±25 | 78±19 | 70±10 |
| Race (caucasian:hispanic) | 4:0 | 5:0 | 5:1 | 9:0 |
| Sex (female:male) | 3:1 | 2:3 | 0:6 | 2:7 |
| Covid-19 environment (%) | ||||
| Health workers | 3/4 | 3/5 | UK | UK |
| Nursing home | – | 1/5 | UK | UK |
| Other | 1/4 | 1/5 | UK | UK |
| Number of tests done:positive results | ||||
| PCR | 4:2 | 5:3 | 6:5 | 9:8 |
| Serological | 2:0 | 1:0 | – | – |
| CV risk factor (%, count) | ||||
| Tobacco use | 0 | 0 | 17 (n=1) | 44 (n=4) |
| HBP | 25 (n=1) | 20 (n=1) | 83 (n=5) | 89 (n=8) |
| Obesity | 0 | 0 | 17 (n=1) | 78 (n=7) |
| Dyslipidemia | 0 | 20 (n=1) | 50 (n=3) | 67 (n=6) |
| Diabetes mellitus | 0 | 0 | 17 (n=1) | 67 (n=6) |
| COPD | 0 | 0 | 33 (n=2) | 11 (n=1) |
| Medical history (%) | 0 | 0 | 17 | 22 |
| Cancer | 0 | 0 | 17 | 22 |
| Venous thromboembolism | 0 | 0 | 33 | 0 |
| Cardiovascular disease | 0 | 0 | 50 | 55 |
| Cerebrovascular disease | 0 | 0 | 0 | 11 |
| Autoimmune disease | 0 | 0 | 0 | 0 |
| Charlson comorbidity index (%) | ||||
| 0–1 | – | – | 67 | 22 |
| ≤ 2 | – | – | 0 | 55 |
| > 3 | – | – | 33 | 22 |
| Previous treatment (%) | ||||
| ACE inhibitor | 25 | 20 | 83 | 89 |
| Statin | 0 | 20 | 50 | 67 |
| Antiplatelet | 0 | 0 | 33 | 55 |
| Anticoagulant | 0 | 0 | 33 | 11 |
Abbreviations: ACE, angiotensin converting enzyme; COPD, chronic obstructive pulmonary disease; CV, cardiovascular; HBP, hypertension; PCR, polymerase chain reaction; UK, unknown.
Table 2.
Clinical Characteristics of Patients with COVID-19 Infection and Acro-Ischemia (I)
| Clinical Characteristics | Atypical Raynaud Phenomenon (n=4) | Pseudo-Pernio (n=5) | Severe Microcirculatory Ischemia with Preserve Pulse (n=6) | Dry Gangrene with Arteriosclerosis Obliterans (n=9) |
|---|---|---|---|---|
| Type of patient | ||||
| Outpatients | 4 | 5 | 0 | 0 |
| Hospital: ward | 0 | 0 | 6 | 1 |
| Hospital: critical care | 0 | 0 | 0 | 8 |
| Covid-19 symptoms (%) | ||||
| Fever | 100 | 100 | 100 | 100 |
| Malaise | 100 | 100 | 100 | 100 |
| Cough | 100 | 100 | 100 | 100 |
| Diarrhea | 75 | 100 | 100 | 100 |
| Headache | 100 | 80 | 100 | 100 |
| Hyposmia | 50 | 0 | 50 | 55 |
| Dysgeusia | 50 | 40 | 50 | 67 |
| Others symptoms (%) | ||||
| Arthralgia | 25 | 40 | 50 | 55 |
| Loin pain | 50 | 0 | 0 | 0 |
| Otalgia | 25 | 0 | 0 | 0 |
| Lymphadenopathy | 25 | 20 | 0 | 0 |
| Genitalia (ulcer) | 25 | 0 | 0 | 0 |
| Viral pneumonia (%) | 0 | 0 | 100 | 100 |
| Disease severity (%) | ||||
| Mild | 100 | 100 | – | – |
| Moderate | – | – | 33 | – |
| Severe | – | – | 67 | 100 |
| CURB-65 score 2 (%) | 67 | 77 | ||
| SaO2/FiO2 | – | – | >140 | <140 |
| Covid-19 treatment (%) | ||||
| Hydroxychloroquine | – | – | 100 | 100 |
| Lopinavir/Ritonavir | – | – | 67 | 77 |
| Interferon | – | – | 50 | 77 |
| Glucocorticoids | – | – | 83 | 55 |
| Tocilizumab | – | – | – | 22 |
| Cyclosporine | – | – | – | 22 |
| Colchicine | – | – | – | 11 |
| LMWH before skin event (%) | ||||
| Prophylactic doses | – | – | 50 | 44 |
| Medium doses | – | – | 16,7 | 22 |
| High doses | – | – | 33 | 33 |
| Skin event treatment (%) | ||||
| Antiplatelet | 25 | 20 | 17 | 22 |
| Anticoagulant | 0 | 0 | 100 | 100 |
| Statin | 0 | 40 | 17 | 22 |
Table 3.
Clinical Characteristics of Patients with COVID-19 Infection and Acro-Ischemia (II)
| Clinical Characteristics | Atypical Raynaud Phenomenon (n=4) | Pseudo-Pernio (n=5) | Severe Microcirculatory Ischemia with Preserve Pulse (n=6) | Dry Gangrene with Arteriosclerosis Obliterans (n=9) |
|---|---|---|---|---|
| Days from disease onset to vascular skin event (mean-range) | 13 (10–14) | 13 (10–14) | 20 (6–24) | 14 (11–18) |
| Skin lesions duration (mean-range) | 15 minutes pulses (7–14) | 10 days (2–14) | 28 days (21–59) | unresolved |
| Other vascular skin lesions (%) | ||||
| Splinter hemorrhage | – | – | 17 | – |
| Livedo racemosa | – | – | – | 33 |
| Ischemic events (%) | ||||
| Cardiac | – | – | 17 | 44 |
| Brain | – | – | 67 | 22 |
| Retina | – | 20 | – | – |
| Spleen | – | – | – | 11 |
| Gut | – | – | – | 22 |
| Nerve | – | – | – | 22 |
| Acute kidney injury (%) | – | – | 0 | 100 |
| Liver failure (%) | – | – | 0 | 33 |
| VTE (%) | – | – | 0 | 22 |
| Atrial fibrillation (%) | – | – | 33 | 22 |
| Syncope (%) | – | – | 50 | 44 |
| Bacterial superinfection (%) | – | – | 0 | 44 |
| SOFA | 0 | 0 | ≤ 2 | >2 |
| Exitus (%) | – | – | 17 | 67 |
| Discharged (%) | – | – | 67 | 11 |
| Readmission (%) | – | – | 0 | 0 |
| Follow-up, days (mean-range) |
38 (21–63) |
19 (11–24) |
44 (15–59) |
54 (2–90) |
PP injuries were more varied. Some lesions were multiple, mainly rounded and a few millimeters in size. While other cases referred a big lesion affecting the entire phalanx, with a clear preference for the metacarpophalangeal level. Initially they had a reddish-purple or bluish color and, afterwards, they became bullous. They mainly affected the toes, but not all of them at the same time. In some cases, even the plantar region and the heel were affected. They usually remained stable during the following days and evolved within 10 days with restitutio ad integrum. SMI lesions took longer to resolve. The 3 AO patients who survived underwent different types of minor amputations (1. Hand amputation, 2. Big toe amputation, 3. Multiple digital amputation of several toes).
The association strength of lung disease severity with the different patterns of acro-ischemia is high: Kendall´s τ =0.877 (95% CI, 0.756 to 0.968) and Spearman´s Rho=0.915 (95% CI, 0.812 to 0.963); p<0.001).
Patients were followed for up to a mean of 38 days for ARP, 19 for PP, 44 for SMI and 54 for AO, as seen in Table 3. Mortality rate was 0% (ARP, PP), 17% for SMI and higher (67%) in AO patients.
Associated Multi-Organic Affectation
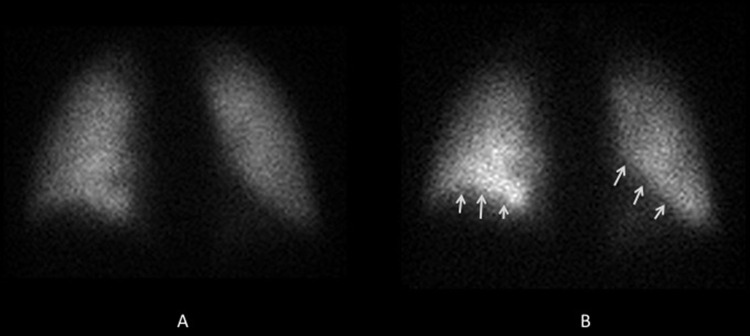
In addition to the cutaneous expressions of acro-ischemic origin already described, we observed other associated lesions of suggestive ischemic nature in other organs (Table 3). One PP individual consulted his family practitioner for perceptual visual disturbances. He also described an intense night otalgia and often headache. Fundus autofluorescence detected abnormalities in branches of central retinal artery as these found in cholesterol emboli (Figure 2). It resolved completely within a week. That scenario mimicked a mild Susac syndrome. Other PP patients consulted for painful limp during follow-up. Magnetic resonance imaging (MRI) was obtained in all cases, finding images interpretable as femoral condyle ischemia (Figure 3). Up to three SMI subjects showed a Sneddon-like syndrome. They presented unusual ischemic stroke with atypical clinical manifestations such as seizures, movement disorders and deficits in concentration, attention and visual perception. One of them presented a splinter hemorrhage as a warning sign of digital ischemia. Both MRI and CT-scan were performed, finding that brain MRI was superior to CT scan in detecting small infarctions. Rare patterns were observed, including occlusion of Percheron artery, deep white matter infarction due to thrombosis of deep perforating artery or ischemic lesions of branches of the middle cerebral artery (Figure 4). One severe SMI case presented a platypnea-orthodeoxia syndrome during pneumonia evolution (Figure 5). An echocardiography ruled out interatrial communication. A 99mTc-macroaggregated albumin pulmonary perfusion scan in the sitting position allowed to confirm the presence of the intrapulmonary shunt.
Figure 2.
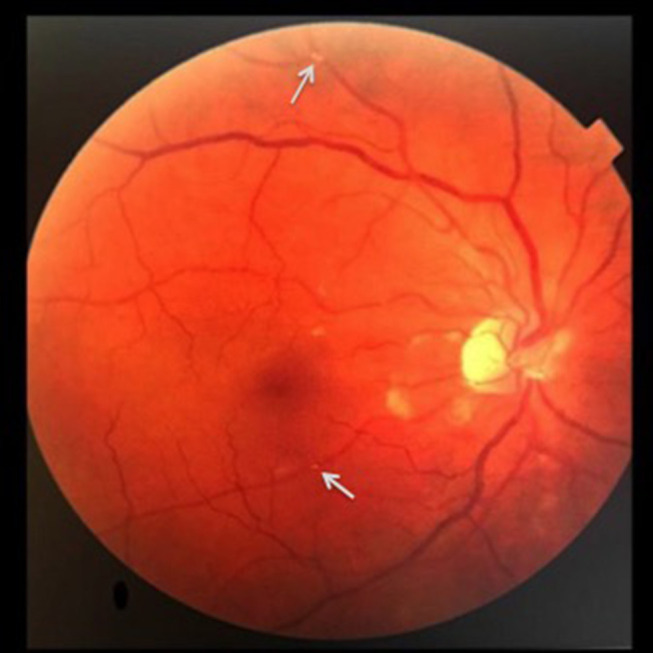
Fundus autofluorescence: abnormalities in branches of central retinal artery.
Figure 3.
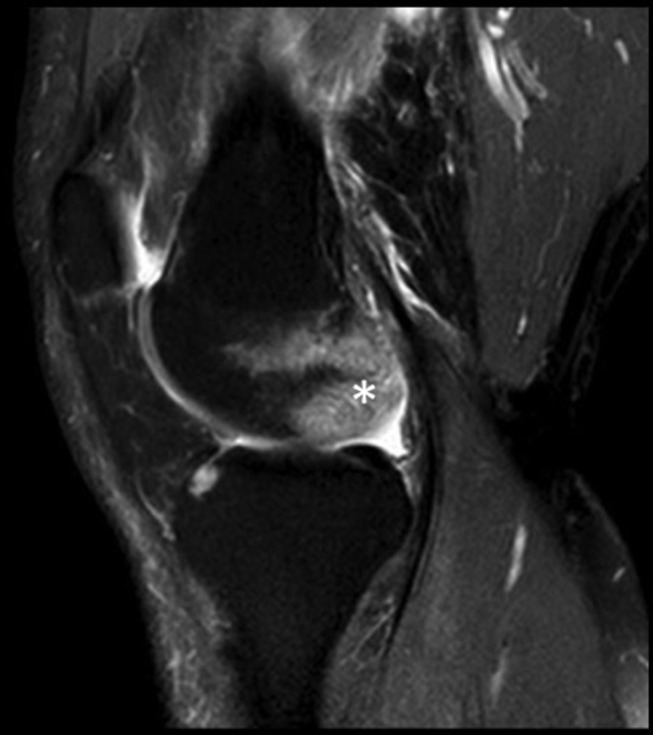
MRI: femoral condyle ischemia.
Figure 4.
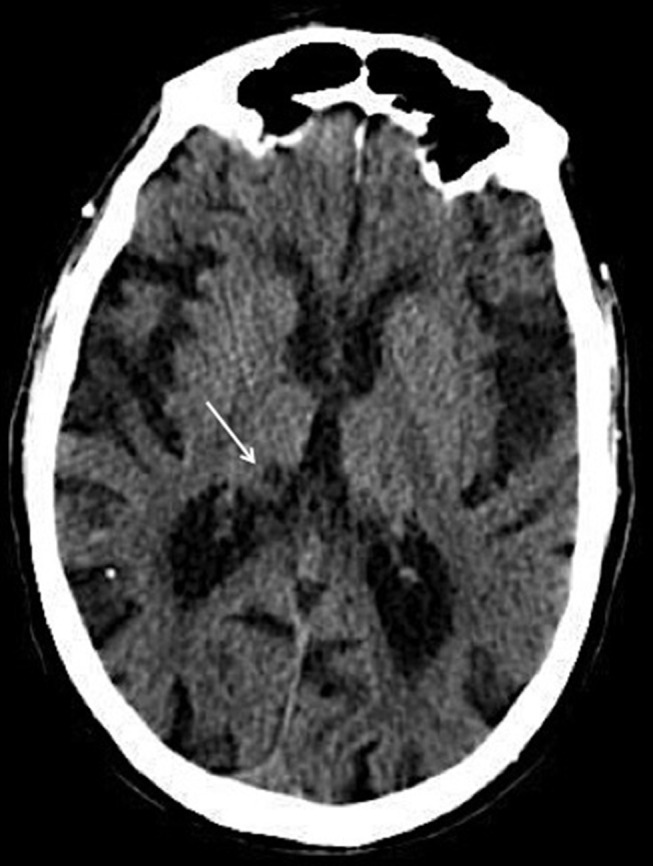
CT-scan: Thalamic infarct.
Figure 5.
99mTc macroaggregated albumin pulmonary perfusion scan: change in regional pulmonary perfusion as a result of posture. Lower lobes are affected by gravity.
A: supine; B: sitting.
One of the AO cases was diagnosed of deep vein thrombosis and peripheral neuropathy on the same leg, the day before appearance of acro-ischemic signs. Angio-CT and echocardiography were performed to rule out an embolic source. All imaging tests were negative. He finally died due to a terminal ileal perforation. Other AO individual died with intermittent intestinal bleeding; both cases were considered as having bowel ischemia. Different cardiac events appeared associated with the AO. Two critical female patients presented non-structural reversible cardiomyopathy such as Tako-Tsubo syndrome, while one critical male subject debuted with syncope and Brugada type 1-like electrocardiographic pattern. One of the female finally died with an acute coronary syndrome. Acute kidney injury was always present in hospitalized patients with AO and 33.3% also presented liver failure. There was no significant improvement in clinical symptoms of patients with AO who were treated with low molecular weight heparin (LMWH).
Laboratory Findings
Plasma procalcitonin was significantly higher in patients who developed SMI (median and interquartile range: 9.99 (4.2, 12.3) mg/mL vs 0.26 (0.11, 0.89) mg/mL; p<0.001) and D-dimer level at hospital admission was significantly higher in AO patients (median and interquartile range: 1166 (1050, 2111) mg/L vs 502 (448, 777) mg/L; p<0.001). No significant differences were observed with regard to inflammatory markers (Lymphocytes, Lactate dehydrogenase, C-reactive protein, Triglycerides, Serum ferritin, Creatin-Kinase), or the reminder coagulation parameters (Fibrinogen, Platelets, Prothrombin time, aPPT) between the two patterns. In both cases, at least 18.5% increase D-Dimer level was observed as predictor of ischemic event.
Discussion
This study describes acro-ischemic lesions associated with COVID-19 infection, with follow-up over time and laboratory associated findings. The degree of severity was strongly related to the overall prognosis of the patient. Remarkably, a Raynaud-like pattern of disease is described and has not been found elsewhere.
In our study, various cases of acro-ischemia were managed with the help of telemedicine. This technique can be used for the delivery of health care services (diagnosis, treatment and prevention of disease), where distance or safety is a critical factor. In the current pandemic, telemedicine has played a key role in the management of such a highly contagious infectious disease.26,27 Besides, health workers represent between 3.8% and 20% of the infected population. In our sample, it reached 25%. They should be considered as an accessible study group in which data collection will be easier than in other population groups.28
The pathophysiology of acro-ischemic injury in COVID-19 patients is probably multi-factorial and difficult to establish at this point. AIL seen in COVID-19 patients show signs that recall Virchow´s triad: altered blood flow, abnormalities in the platelet function and vascular endothelium that would lead to venous and arterial thromboses.8,29 One possible hypothesis is the ischemic lesions mimicking a faster Buerger’s disease, being thereforea vasa-nervorumitis the eventual pathological substrate. In case of Buerger’s disease, Rickettsia spp. has been postulated as causal agent and not tobacco itself.30,31 After pulmonary Raynaud´s phenomenon, proinflammatory biomarkers are increased in distance organs, which could explain all microvascular events of the disease´s inflammatory phases.32,33 The balance between the thrombotic and inflammatory states is only the response of each organism to a multisystemic ischemia-reperfusion syndrome. Davidson has reported that patients with higher morbidity/vascular age would have worse ischemic preconditioning with poor collateral vessels. Hence, reperfusion would generate devastating consequences related to the activation of macrophage response.34 In contrast, older patients and these with less comorbidity would have a lower immunometabolic response, with the acro-ischemia pattern appearing later.35 Therefore, in these cases, the ischemic pattern would be the most significant, as seen in the coagulation abnormalities found. Our outpatient data further suggest that women´s lower sensitivity to swelling may be related to higher ischemic tolerance.36
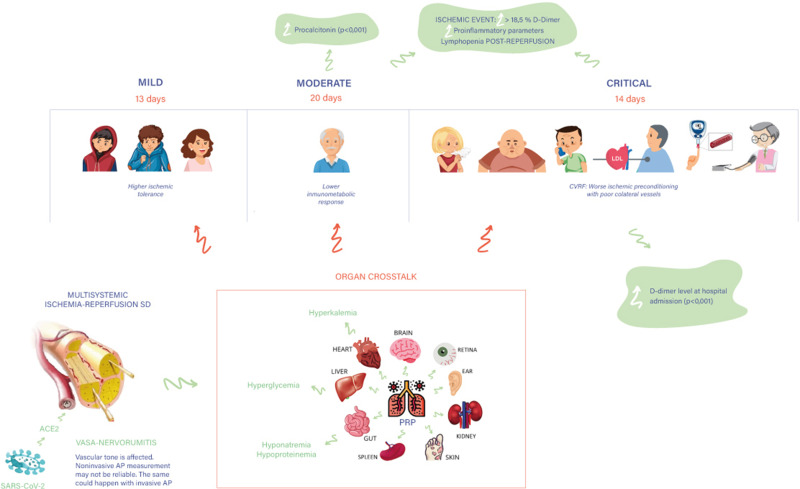
The onset form of atypical Raynaud phenomenon (ARP) episodes (non-sustained and repetitive sub-lethal ischemic stimulation) would promote the release of autocrine bradykinine, which would play a key role as a systemic mediator of cytoprotective ischemic preconditioning.37 Vasa-nervorumitis would explain why these patients show weak peripheral pulses, even in the absence of overt hypotension.38,39 However, in order to corroborate these claims, more exhaustive studies are definitely required. Sustained total hypoperfusion of the small vessels and then multisystemic ischemia-reperfusion syndrome would justify any clinical, analytical or imaging findings found in our sample. Headache and loin pain could be correlated with kidney and cerebral transient ischemia phenomena. Typical analytical findings of hospitalized COVID-19 patients include hyperglycemia, hypoproteinemia, hyperkalemia and hyponatremia, which also are common findings in the ischemia-reperfusion syndrome.40 As said before, this pathophysiological hypothesis needs to see further confirmation, although it offers a reasonable explanation for all the involved clinical and laboratory findings (Figure 6).
Figure 6.
Pathophysiological hypothesis and clinical-demographic phenotypes of COVID-19 infection. CVRF: Cardiovascular Risk Factors.
Abbreviations: AP, arterial pressure; PRP, pulmonary Raynaud´s phenomenon.
Pseudo-pernio (PP) is the skin lesion most frequently found in COVID-19 patients, according to Kluger et al, but the real incidence remains unknown.41 The way these lesions are named can be controversial. We have used a doctor´s consensus to describe four clinical patterns but, unfortunately, there is no common terminology in the literature. Our study agrees with previously published dermatological research in PP being a mild late manifestation of COVID-19 in young patients.17–19 In a Spanish cohort, SMI and AO appeared in elderly patients with a severe clinical grade.17 In the Chinese AIL series, AO appears in patients who need critical care. As we did in our study, they concluded that anticoagulant treatment did not achieve skin restitutio ad integrum.23
There is also a lack of consensus on D-dimer levels’ role among the studies. Zhou describes percentual increments in D-Dimer figures (14–46%) for ischemic events in COVID-19.13 In our case, this increment was as higher than 18.5%. Middeldrop et al propose to use D-dimer and lymphocytes as high-risk markers of thrombotic events.42 As other authors, we saw that after the ischemic event, reperfusion was accompanied by lymphopenia.43 In addition, patients in whom the D-dimer level at hospital admission was significantly elevated presented a worse therapeutic response, since they remained in a thrombo-inflammatory state.10 This finding, together with the significant increase in procalcitonin levels in SMI cases, is concordant with clinical phenotypes of SARS-CoV-2 described by Rello et al.44
As in our case, Violi reported high number of thrombotic complications in COVID-19 patients, even when receiving thrombo-prophylaxis.45 Mild thrombocytopenia has been described in 5 to 20% of infected patients in the context of systemic microvascular thrombosis.46 In our hospitalized subjects, platelet levels remained within the normal range. On the other hand, although Zhang described four cases of intravascular disseminated coagulation (ICD), in our sample we found abnormal coagulation parameters, but no CID.22 Moreover, Magro obtained skin and lung biopsies from five patients with severe infection. They found a catastrophic inflammatory and thrombogenic syndrome with microvascular injury caused by systemic activation of lecithin-based complement pathways. However, the authors could not locate any viral cytopathic changes.9
Suggested Management
Based on our experience, from now on, we suggest to routinely perform non-invasive tests to improve diagnosis, such as capillaroscopy or fundus autofluorescence. We suggest analytic determinations up to three times a week (D-dimer, lymphocytes, procalcitonin, triglycerides, ferritin and C-reactive protein) for patients in whom a worse ischemic preconditioning can be identified. Endothelium stabilizing drugs (ACE inhibitors, statins and antiplatelet drugs) during the viral replication phase with anticytokine may have a role to play. The role of halogenated gases, such as sevoflurane, isoflurane and desflurane, in preventing cell damage at the time of reperfusion is partially elucidated. If we extrapolate the protective action of gases and hypnotic agents (propofol) to peripheral arteries, we could suggest that its administration would reduce the ischemic-reperfusion damage and, thus, diminish the morbimortality of COVID patients.47,48 We could not find any studies of sevoflurane being used in acro-ischemia induced by COVID. The reason may be that Anesthetic Conserving Devices (AnaConDa) are not so commonly found in adults Intensive Care Units (ICU). All our severe COVID patients underwent deep sedation with propofol, but it is really difficult to assess the benefit of its administration. That is because all ICU patients received vasoactive drugs (norepinephrine) related to the hypotension provoked by the systemic inflammatory responses caused by the viral infection, by the decrease in peripheral vascular resistance associated to the hypnotic and, probably, by the vasa-nervorumitis. The administration of vasoactive amines can generate a bias on the vasoconstrictor alteration caused by the virus per se.
In terms of treatment, we believe that the prevention and optimal management of vascular complications with adequate hydration and vasodilators can significantly improve the prognosis in symptomatic patients, reducing multi-organ failure and consequently the mortality rate and sequelae. Restoring blood flow produces a complex cellular and systemic response that depends on the affected tissue, the duration of the ischemia and the ability of the tissues to reperfuse. Thus, some regional blocks can also be performed to prevent vascular spasm and improve distal perfusion.29 This is why more research is needed to determine the vascular bed damage caused by this virus. With our study, we have tried to improve the understanding of how SARS-CoV-2 works at the skin level. However, regulation of skin vascular tone is complex because it involves not only endothelium-derived mediators but also peripheral and central neurogenic mechanisms.39 More studies are needed to assess the possibility that vasa-nervorumitis is the main physiopathological cause of acro-ischemic lesions. The multisystemic ischemia-reperfusion syndrome hypothesis and demographic-clinical phenotypes would benefit the optimization of therapies and improve outcomes (Supplementary material Table S1).
Limitations
The major limitation of this study is the sample size. There are also some parameters that we could not collect due to lack of outpatients´ access to health centers and that could have modified our estimations. As a result, we were also unable to obtain lesion biopsies and proceed with a histological study. Determination of autoimmunity parameters would have also been useful. In addition, it would have been highly desirable to have factor VIII and von Willebrand factor measurements to assess endothelial damage caused by the virus binding to its ACE2 receptor.49
Conclusion
The observed risk for acroischemia in COVID-19 is high in ICU patients (23%). We have described four different clinical patterns of acroischemia (ARP, PP, SMI and AO) associated with lung disease severity. Authors have communicated various lesions of suggestive ischemic nature in other organs. Raynaud-like pattern is reported as a ”novelty”.
Acknowledgments
MEMBERS OF THE ANTI-COVID-19 TEAM FROM HOSPITAL CENTRAL DE LA DEFENSA “GÓMEZ-ULLA”. All of them provided and cared for study patients.
Abbreviations
AIL, acro-ischemic lesions; ARP, atypical Raynaud phenomenon; PP, pseudo-pernio; SMI, severe microcirculatory ischemia; AO, arteriosclerosis obliterans.
Disclosure
The authors report no conflicts of interest for this work.
References
- 1.Zhu N, Zhang D, Wang W, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johns Hopkins: Coronavirus Resource Center. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) [consulted 2020 May 22]. Available from: https://coronavirus.jhu.edu/map.html.
- 3.National Center for Epidemiology. Institute of health Carlos III (ISCIII) [consulted 2020 Jun 24]. Available from: https://cnecovid.isciii.es/covid19.
- 4.Brake S, Barnsley K, Lu W, et al. Smoking upregulates angiotensin-Converting enzyme-2 receptor: a potential adhesion site for novel coronavirus SARS- CoV-2 (Covid-19). JMC. 2020;9:841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferrario C, Jessup J, Chappell M, et al. Effect of Angiotensin-Converting Enzyme Inhibition and Angiotensin II Receptor Blockers on Cardiac Angiotensin-Converting Enzyme 2. Circulation. 2005;111(20):2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461 [DOI] [PubMed] [Google Scholar]
- 6.Mackman N, Antoniak S, Wolberg AS, et al. Coagulation Abnormalities and Thrombosis in Patients Infected With SARS-CoV-2 and Other Pandemic Viruses. Arteriosclerosis Thrombosis Vasc Biol. 2020;40(9):2033–2044. doi: 10.1161/ATVBAHA.120.314514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020;383(2):120–128. doi: 10.1056/NEJMoa2015432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmed S, Zimba O, Gasparyan AY. Thrombosis in Coronavirus disease 2019 (COVID-19) through the prism of Virchow’s triad. Clin Rheumatol. 2020;39(9):2529–2543. doi: 10.1007/s10067-020-05275-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Magro C, Mulvey JJ, Berlin D, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Connors JM, Levy JH. Thromboinflammation and the Hypercoagulability of COVID-19. J Thromb Haemost. 2020;18(7):1559–1561. doi: 10.1111/jth.14849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hu Y, Sun J, Dai Z, et al. Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis. J Clin Virol. 2020;127:104371. doi: 10.1016/j.jcv.2020.104371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Verma V, Vishwakarma RK, Verma A, Nath DC, Khan HTA, Navaneetham K. Time-to-Death Approach in Revealing Chronicity and Severity of COVID-19 Across the World. PLoS One. 2020;15(5):e0233074. doi: 10.1371/journal.pone.0233074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;13:3200994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jain U. Effect of COVID-19 on the Organs. Cureus. 2020;12:e9540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Galván Casas C, Catalá A, Carretero Hernández G, et al. Classification of the cutaneous manifestations of COVID −19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020;183(1):71–77. doi: 10.1111/bjd.19163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bouaziz JD, Duong T, Jachiet M, et al. Vascular skin symptoms in COVID-19: a french observational study. J Eur Acad Dermatol Venereol. 2020;27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fernandez-Nieto D, Jimenez-Cauhe J, Suarez-Valle A, et al. Characterization of acute acral skin lesions in nonhospitalized patients: A case series of 132 patients during the COVID-19 outbreak. J Am Acad Dermatol. 2020;83(1):e61–3. doi: 10.1016/j.jaad.2020.04.093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Piccolo V, Neri I, Filippeschi C, et al. Chilblain-like lesions during COVID-19 epidemic: a preliminary study on 63 patients. J Eur Acad Dermatol Venereol. 2020;34(7). doi: 10.1111/jdv.16526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bikdeli B, Madhavan MV, Jimenez D, et al. COVID-19 and Thrombotic or Thromboembolic Disease: implications for Prevention, Antithrombotic Therapy, and Follow-up. J Am Coll Cardiol. 2020;pii: S0735-1097(20)35008–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Y, Xiao M, Zhang S, et al. Coagulopathy and Antiphospholipid Antibodies in patients with Covid-19. N Engl J Med. 2020;382(17):e38. doi: 10.1056/NEJMc2007575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang Y, Cao W, Xiao M, et al. Clinical and coagulation characteristics of 7 patients with critical COVID-2019 pneumonia and acro-ischemia. Zhinghua Xue Xue Za Zhi. 2020;41:E006. [DOI] [PubMed] [Google Scholar]
- 24.Perini P, Nabulsi B, Massoni CB, et al. Acute limb ischaemia in two young, non-atherosclerotic patients with COVID-19. Lancet. 2020;395(10236):1546. doi: 10.1016/S0140-6736(20)31051-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gomez-Arbelaez D, Ibarra-Sanchez G, Garcia-Gutierrez A, et al. COVID-19-Related Aortic Thrombosis: A Report of Four Cases. Ann Vasc Surg. 2020;67:10–13. doi: 10.1016/j.avsg.2020.05.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chiappelli F, Bakhordarian A, Thames AD, et al. Ebola: translational science considerations. J Transl Med. 2015;13:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khan ID, Khan SA, Asima B, Hussaini SB, Zakiuddin M, Faisal FA. Morbidity and mortality amongst Indian Hajj pilgrims: A 3-year experience of Indian Hajj medical mission in mass-gathering medicine. J Infect Public Health. 2018;11(2):165–170. doi: 10.1016/j.jiph.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lancet T, The Lancet. COVID-19. COVID-19: protecting health-care workers. Lancet. 2020;395(10228):922. doi: 10.1016/S0140-6736(20)30644-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mahli A, Coskun D, Cosarcan K. Peripheral sympathetic block with therapeutic local anesthesia for the management of upper limb digital ischemia. Hippokratia. 2018;22:141–143. [PMC free article] [PubMed] [Google Scholar]
- 30.Fakoor F, Fazeli B. <p>Visceral bed involvement in thromboangiitis obliterans: a systematic review. Vasc Health Risk Manag. 2019;15:317–353. doi: 10.2147/VHRM.S182450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fazeli B, Farzadnia M, Taheri TH. <p>Vaso-nervorumitis: responsible for pain in Buerger’s disease? Int Med Case Rep. 2019;12:119–123. doi: 10.2147/IMCRJ.S197862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Batlle D, Soler MJ, Sparks MA, et al. Acute Kidney Injury in COVID-19: emerging Evidence of a Distinct Pathophysiology. J Am Soc Nephrol. 2020;31(7):1380–1383. doi: 10.1681/ASN.2020040419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.White LE, Hassoun HT. Inflammatory mechanisms of Organ Crosstalk during Ischemic Acute Kidney Injury. Int J Nephrology. 2012;2012:505197. doi: 10.4061/2012/505197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davidson SM, Ferdinandy P, Andreadou I, et al. Multitarget Strategies to Reduce Myocardial Ischemia/Reperfusion Injury: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;73(1):89–99. doi: 10.1016/j.jacc.2018.09.086 [DOI] [PubMed] [Google Scholar]
- 35.Ghimire A, Bisset ES, Howlett SE. Ischemia and reperfusion injury following cardioplegic arrest is attenuated by age and testosterone deficiency in male but not female mice. Biol Sex Differences. 2019;10(1):42. doi: 10.1186/s13293-019-0256-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mester A, Magyar Z, Molnar A, et al. Age- and gender-related hemorheological alterations in intestinal ischemia-reperfusion in the rat. J Surg Res. 2018;225:68–75. doi: 10.1016/j.jss.2017.12.043 [DOI] [PubMed] [Google Scholar]
- 37.Bellis A, Sorriento D, Fiordelisi A, et al. Autocrine Bradykinin Release Promotes Ischemic Preconditioning-Induced Cytoprotection in Bovine Aortic Endothelial Cells. Int J Mol Sci. 2020;21(8):2965. doi: 10.3390/ijms21082965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li H, Liu L, Zhang D, et al. SARS-CoV-2 and viral sepsis: observations and hypotheses. Lancet. 2020;395(10235):1517–1520. doi: 10.1016/S0140-6736(20)30920-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Devgire V, Hughes M. Raynaud’s phenomenon. Br J Hospital Med. 2019;80(11):658–664. doi: 10.12968/hmed.2019.80.11.658 [DOI] [PubMed] [Google Scholar]
- 40.Brencher L, Verhaegh R, Kirsch M. Attenuation of intestinal ischemia-reperfusion-injury by β-alanine: a potentially glycine-receptor mediated effect. J Surg Res. 2017;211:233–241. doi: 10.1016/j.jss.2016.12.023 [DOI] [PubMed] [Google Scholar]
- 41.Kluger N, Scrivener JN. The use of Google trends for acral symptoms during COVID-19 outbreak in France. J Eur Acad Dermatol Venereol. 2020;34(8):e358–60. doi: 10.1111/jdv.16572 [DOI] [PubMed] [Google Scholar]
- 42.Middeldorp S, Coppens M, van Haaps T, et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18(8):1995–2002. doi: 10.1111/jth.14888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boag SE, Andreano E, Spyridopoulos I. Lymphocyte Communication in Myocardial Ischemia/Reperfusion Injury. Antioxid Redox Signal. 2017;26(12):660–675. doi: 10.1089/ars.2016.6940 [DOI] [PubMed] [Google Scholar]
- 44.Rello J, Storti E, Belliato M, Serrano R. Clinical Phenotypes of SARS-CoV-2: implications for Clinicians and Researchers. Eur Resp J. 2020;55(5):2001028. doi: 10.1183/13993003.01028-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Violi F, Pastori D, Cangemi R, Pignatelli P, Loffredo LL. Hypercoagulation and Antithrombotic Treatment in Coronavirus 2019: A New Challenge. Thromb Haemost. 2020;120(06):949–956. doi: 10.1055/s-0040-1710317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18(7):1738–1742. doi: 10.1111/jth.14850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang P, Du Y, Zeng H, Xing H, Tian C, Zou X. Comparison of inflammatory markers between the sevoflurane and isoflurane anesthesia in a rat model of liver ischemia/reperfusion injury. Transplant Proc. 2019;51(6):2071–2075. doi: 10.1016/j.transproceed.2019.04.022 [DOI] [PubMed] [Google Scholar]
- 48.Chen X, Wang Y, Xiao Z-Y, Hou D-N, Li D-B, Zhang X-P. Effect of propofol on myocardial ischemia/reperfusion injury in rats through JAK/STAT signaling pathway. Eur Rev Med Pharmacol Sci. 2019;23:6330–6338. [DOI] [PubMed] [Google Scholar]
- 49.Jacquemin M, NeyrincK A, Hermanns MI, et al. FVIII production by human lung microvascular endothelial cells. Blood. 2006;108(2):515–517. doi: 10.1182/blood-2005-11-4571 [DOI] [PubMed] [Google Scholar]