Abstract
Silver nanoparticles (AgNPs) represent one of the most explored categories of nanomaterials for new and improved biomaterials and biotechnologies, with impressive use in the pharmaceutical and cosmetic industry, anti-infective therapy and wound care, food and the textile industry. Their extensive and versatile applicability relies on the genuine and easy-tunable properties of nanosilver, including remarkable physicochemical behavior, exceptional antimicrobial efficiency, anti-inflammatory action and antitumor activity. Besides commercially available and clinically safe AgNPs-based products, a substantial number of recent studies assessed the applicability of nanosilver as therapeutic agents in augmented and alternative strategies for cancer therapy, sensing and diagnosis platforms, restorative and regenerative biomaterials. Given the beneficial interactions of AgNPs with living structures and their nontoxic effects on healthy human cells, they represent an accurate candidate for various biomedical products. In the present review, the most important and recent applications of AgNPs in biomedical products and biomedicine are considered.
Keywords: antimicrobial therapy, cancer therapy, tissue engineering, wound care
1. Introduction
Nanotechnology and nanoscience represent important fields for the progress of modern society, especially given the incessant efforts and impressive achievements in alternative nano-based therapies [1,2]. A particular interest was oriented towards the revaluation and biofunctional assessment of metallic nanoparticles for biotechnology and biomedicine, especially thanks to their unique physical, chemical and biological features [3,4,5]. Specifically, biocompatible nanoparticles with superior physicochemical properties, suitable biomechanical behavior and tunable therapeutic efficiency can be successfully obtained [6,7]. Thanks to their genuine size-related characteristics, nanoparticles are distinguished as the most versatile candidates for biotechnological and biomedical applications, being considered the star technology of the 21st century [8,9].
Among zero-dimensional nanomaterials, silver nanoparticles (AgNPs) represent one of the most explored and promising candidates for unconventional and performant applications in the contemporary world, with formidable results being reported in pharmaceutical sciences [10,11,12], cosmetic products [13,14], anti-infective coatings [15,16] and wound dressings [17,18], antimicrobial textiles [19,20,21] and food packages [22,23,24]. The particular interest of AgNPs in biomedical applications mainly relies on their excellent and extensive antimicrobial properties, limited anti-pathogenic resistance and impressive efficiency against multidrug-resistant microorganisms [25,26,27].
AgNPs with tunable physicochemical characteristics and versatile functionality can be obtained by various top-down (mainly, evaporation-condensation processes of bulk silver) [28,29] and bottom-up (mainly, electrochemical processes of metallic salts) processing methods [30,31]. Special attention was oriented on the inexpensive and environmentally-friendly synthesis of AgNPs, which either considers the revaluation of plant-derived reducing and antioxidant phytochemicals [32,33] or the microorganism-mediated bioreduction mechanisms [34,35].
Given their intrinsic antimicrobial efficiency, silver-based compounds and materials were used for many centuries in day-to-day applications [36,37,38]. Their versatility and excellent biofunctionality enabled the development and clinical implementation of several human-safe commercial products, as summarized in Table 1.
Table 1.
Commercial products containing ionic (Ag+) or metallic silver (Ag0/AgNPs).
| Product Type | Product Trademark | Company | Note |
|---|---|---|---|
| Wound dressing | Acticoat™ | Smith & Nephew, Inc. (London, UK) | Flexible and nonadherent nanocrystalline silver dressing Provides sustained broad-spectrum bactericidal activity against over 150 strains |
| Allevyn™ Ag | Absorbent and flexible silicone foam dressing impregnated with SSD Provides sustained long-term bactericidal effects |
||
| Actisorb™ Silver | 3M+KCI (MN, USA) | Activated charcoal layer impregnated with silver Provides anti-bacterial barrier action and bactericidal activity |
|
| Silvercel™ | Nonwoven pad of natural polysaccharides blend and nylon fibers impregnated with ionic silver Provides sustained long-term bactericidal and anti-biofilm effects |
||
| Tegaderm™ Alginate Ag | Absorbent soft-gelling alginate dressing impregnated with silver Provides sustained long-term broad-spectrum bactericidal effects |
||
| Maxorb® Extra Ag+ | Medline Industries, Inc. (IL, USA) | Blend fibers of natural polysaccharides impregnated with ionic silver Provides a sustained and long-term barrier against bacteria absorbed in wound exudates |
|
| Opticell® Ag+ | Absorbent and flexible gelling fiber format impregnated with ionic silver Provides sustained long-term bactericidal activity |
||
| SilvaSorb™ Sheet | Super-absorbent hydrogel sheet impregnated with ionic silver Provides sustained long-term bactericidal activity |
||
| SilvaSorb™ Gel | Hydrogel ointment impregnated with ionic silver Provides sustained broad-spectrum antimicrobial action |
||
| Aquacell® Ag | ConvaTec Group (Deeside, UK) | Nonwoven inner pad impregnated with ionic silver Provides long-term broad-spectrum bactericidal and bacteriostatic effects |
|
| PolyMem Silver™ | Ferris Mfg. Corp. (TX, USA) | Foam dressing impregnated with nanocrystalline silver Provides fungicidal and broad-spectrum bactericidal effects |
|
| SilvrSTAT® | ABL Medical (UT, USA) | Hydrogel dressing ointment impregnated with metallic silver Provides antimicrobial action in first- and second-degree burns |
|
| Catheter coating | Silverline® Drainage Catheters | Spiegelberg GmbH & Co. (Hamburg, Germany) | Radiopaque polyurethane or silicone catheters modified with silver Provides antimicrobial and anti-biofilm effects in the case of drainage in central nervous system structures |
| Covidien® Foley Catheter | Medtronic (London, UK) | Outer and inner silicone catheter and balloon coated with ionic silver hydrogel coating Provides substantial antimicrobial activity by consistent release of ionic silver |
|
| SilverSoaker™ Catheter | Halyard Health, Inc., (GA, USA) | Outer and inner catheter coated with metallic silver (SilvaGard™) Provides antimicrobial and anti-biofilm effects |
|
| Bardex® Catheter | C.R. Bard Inc., (NJ, USA) | Latex Foley catheter modified with Bard® hydrogel and Bactiguard® silver coating Provides antibacterial and anti-biofilm effects |
|
| Endotracheal tube | Agento® Silver-coated Endotracheal Tube | C.R. Bard Inc., (NJ, USA) | Endotracheal tube modified with a hydrophilic polymer coating containing silver particles Provides microbiological efficiency against ventilator-associated pneumonia |
Abbreviation: SSD—silver sulfadiazine.
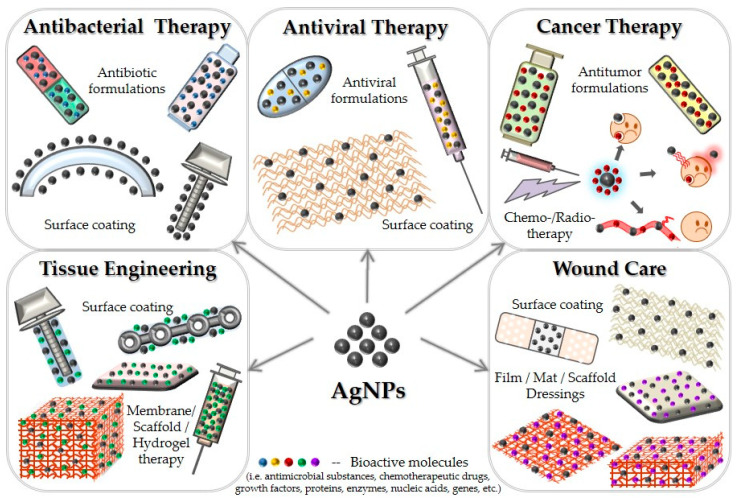
Besides commercial products, an impressive number of preclinical studies reported the successful implications of AgNPs in the development of effective and performance-enhanced unconventional therapeutic strategies. A schematic representation of the most explored therapeutic applications of AgNPs in modern healthcare practice is included in Figure 1. The present paper aimsto survey the most recent biomedical applications of nanosilver-based formulations.
Figure 1.
Applications of silver nanoparticles (AgNPs) in biomedicine.
2. Toxicity of Silver Nanoparticles
Nanosilver is of great interest for modern and personalized biomedical uses, especially since their interactions with living structures may lead to biochemical modifications in cytoskeleton organization and molecule adhesion [39,40], as well as in cell proliferation [41,42]. In a similar way to their intrinsic anti-pathogenic effects, the AgNPs-mediated toxicity in mammalian cells may be induced by a different mechanism, such as: (i) disruption in energy-dependent cellular events and impairment in DNA replication, caused by the uptake of free silver ions; (ii) formation of reactive oxygen species and free radicals; and (iii) local damage of cellular membrane due to direct interactions with AgNPs [43,44].
Biosynthesized nanosilver coated with cetyltrimethylammonium bromide (CTAB) surfactant and polyethylene glycol (PEG) polymer showed time- and dose-dependent effects on erythrocytes with increasing the concentration of coating agent, but exhibited nonhemolytic activity at CTAB and PEG concentrations below 100 µg/mL, being thus considered blood compatible [45]. Highly stable and conductive nanosilver stabilized with a polymer coating of polyvinyl alcohol (PVA)—PEG and poly(3-aminophenyl boronic acid) also proved compatible for human red blood cells. The nanocomposite exhibited nontoxic effects on normal human cell line at bactericidal concentrations [46].
Biosynthesized AgNPs coated with chitosan (CS) exhibited enhanced anticoagulant activity in an animal model, as evidenced by the dose-dependent variation of blood parameters. Also, the treatment with nanoparticles determined increased antiplatelet and thrombolytic effects, as well as low cytotoxicity in different study models [47].
The size-dependent phagocytic internalization of AgNPs proved responsible for cytotoxic effects on macrophages. Significantly increased levels of reactive oxygen species (ROS) and interleukin were reported when treating the cells with 4 nm sized nanosilver, whereas the 20 and 70 nm nanoparticles led to more reduced or even insignificant cytotoxicity [48]. As evidenced by complex structural and functional tests and proteomic assays, macrophages treated with silver nanoparticles stabilized with polyvinylpyrrolidone (PVP) exhibited cellular homeostasis recovery within three days after acute exposure [49]. Moreover, highly antibacterial and anti-biofilm AgNPs coated with bacteria-isolated protein showed no toxic effects against primary macrophage cultures and different vital organs [50].
A complex study proved that AgNPs stabilized with PVP have dose-dependent toxic effects on murine dendritic cells, but the effects were significantly increased against cancerous cells [51]. Particles of 10 nm exhibited toxicity on neural stem cells, regardless the type and charge of a surface coating. Oxidative events, as well as ROS-mediated inflammatory response and DNA damage, caused either apoptotic or necrotic cell death [52]. The size-dependent neurotoxicity of PVP-coated nanosilver was reported by Zhang et al., as 20 nm particles induced increased intracellular silver accumulation and caused significant cytoskeleton modifications and dopamine efflux alterations, in comparison with 70 nm particles [53].
Negatively charged AgNPs biosynthesized with sorrel flower extract determined dose-dependent toxicity in human endothelial cells, causing ROS-mediated apoptosis, as well as cellular morphological and functional impairment. The as-obtained particles induced cell malformations, death and senescence in a zebrafish model due to severe oxidative stress [54]. Also, Jalilian and coworkers reported the dosage-dependent cytotoxicity of nanosilver on normal fibroblasts. The same nanoparticle concentrations induced higher cytotoxic effects against malignant cells [55].
No toxic or genotoxic effects were identified in fibroblast cultures treated with nanoparticles coated with silica (SiO2) [56]. In a comparative study, Verkhovskii et al. reported that highly stable AgNPs coated with PVA and sodium carboxymethyl cellulose (CMC) are safe for dermal fibroblasts, while nanoparticles coated with sodium dodecyl sulfate and sodium oleate proved cytotoxic [57]. The viability of human lung fibroblasts was minimally reduced when treated with AgNPs in concentrations up to 100 µg/mL or 2.5 mg/mL, obtained with Ayurvedic medicinal herb extract [58] or oxidized amylose/curcumin complex [59], respectively. The biosynthesized nanoparticles also exhibited dose-dependent antioxidant activity while showing enhanced antibacterial effects. As well, bactericidal concentrations of lecithin-modified montmorillonite (MMT) embedded with nanosilver showed no toxic effects on normal fibroblasts [60]. Antibacterial composites of high-density polyethylene and AgNPs-decorated MMT exhibited superior cytocompatibility with human erythrocytes and dermal fibroblasts and caused no morphological alterations in the skin tissue of rats after 21 days of exposure [61].
Concentrations lower than 10 µM of highly stable PEG-coated nanosilver proved safe for human keratinocytes, while the higher concentration of 50 µM was associated with intense cell mortality [62]. Graf and coworkers reported no preferential shape-related cellular internalization of AgNPs by keratinocytes, while mesenchymal stem cells exhibited preferential uptake of PVP-stabilized silver nanoprisms, in comparison with silver nanospheres [63]. Reduced levels of cytotoxicity and genotoxicity on human keratinocytes were also reported in the case of nanoparticles biosynthesized by Trichoderma harzianum cultivated with or without pathogenic fungal enzymes [64]. Fungi-mediated bioreduced AgNPs exhibited high antimicrobial efficiency, but showed nontoxic effects against normal human melanocytes for concentrations up to 6 µg/mL [65].
Huy and coworkers reported that silver nanoparticles synthesized by the electrochemical method were nontoxic on striated muscle cell cultures for concentrations up to 100 ppm but displayed strong biocidal effects against enveloped viruses [66]. Mild lung inflammatory infiltrate was observed after the pulmonary exposure of albino mice to AgNPs coated with PVP or citrate. Consequently, dose-dependent effects were evidenced at the cardiovascular level, such as the increase of proinflammatory cytokines and antioxidants, cardiac oxidative stress, DNA damage and apoptosis of cardiac cells, prothrombotic events, and coagulation alterations [67].
Different studies from recent years investigated the toxicity of nanosilver with respect to human tissues and demonstrated their applicability as safe therapeutic agents for pharmaceutical products [68,69]. An important fact is that the toxic effects exhibited by AgNPs are strongly influenced by their morphology and dimension. For example, cytoplasm and cellular organelles are more prone to be affected by smaller particles than bigger particles [70,71].
The main mechanism responsible for AgNPs-related cytotoxicity is the oxidative stress induced by the excessive production of ROS, which can cause structural and functional impairments in proteins, lipids and DNA, resulting in cellular alteration and even cell death [72,73]. More than that, due to their nanodimension and reactive surface chemistry, AgNPs are captured and internalized by the cells [74]. Their intracellular agglomeration can severely damage cellular constituents (cell wall, cytoplasm), as well as vital organelles (mitochondria) and essential macromolecules (proteins, enzymes, DNA) [75,76]. Also, another possible mechanism for nanosilver toxicity is cellular apoptosis [77,78].
Hu and coworkers reported that silver nanoparticles affect the global differentiation of human embryonic stem cells. In particular, dose-dependent effects were evidenced during the differentiation and function of hepatocytes and cardiomyocytes [79]. Using albino mice, Jarrar et al. proved that hepatoprotective agents or coatings are mandatory for the safe administration and suitable drug metabolism of AgNPs-based systems, as citrate-coated nanosilver (20 ± 5 nm size) induced significant downregulation in the gene expression of hepatic drug-metabolizing enzymes, causing important hepatic inflammation [80].
Green synthesized AgNPs altered the levels of glucose and hepatic enzymes in an animal model, but did not induce morphological modifications. The beneficial conjunction between metallic nanoparticles and common dogwood extract resulted in diminished oxidative stress and enhanced antioxidant and anti-inflammatory effects [81]. The functional alteration of liver and kidney was also reported after the inoculation of CS-coated bioreduced nanosilver in rats. Moreover, the proposed AgNPs proved able to cross the placenta and induced minimal toxicity in fetuses. Contrariwise, time-dependent severe fetal hepatotoxicity was evidenced in the case of uncoated nanoparticles inoculation [82].
Other studies reported the importance of surface coating on the bioavailability and toxicity of nanosilver. AgNPs modified with silicate and PVP neutral coatings induced less inflammatory effects and genotoxicity than negatively charged citrate and positively charged branched polyethylenimine (PEI) coatings [83]. In addition, Zucker and coworkers showed that 80 nm AgNPs coated with branched PEI were internalized and accumulated at a greater rate by epithelial cells, in comparison with nanoparticles coated with citrate, PEG, or PVP, causing significant mitochondria damage [84].
Following the subacute exposure of rats to AgNPs, Docea and coworkers evidenced significant antioxidant effects in the case of particles coated with ethylene glycol (EG). For the same doses, PVP-EG-coated AgNPs resulted in important pro-oxidant effects, as indicated by the induction of protein oxidation and decrease of glutathione levels [85]. After subcutaneous implantation in rats, colloidal nanosilver determined important subacute inflammatory response of connective tissue but demonstrated long-term biocompatibility, as evidenced after 60 days of exposure [86].
3. Silver Nanoparticles for Antibacterial Applications
An alarming phenomenon of current healthcare practice is the occurrence of many drug-resistant microorganisms, which leads to ineffective conventional monotherapy. Bacterial infections and their related complications represent a major and frequent cause of death [87,88]. With the aim to overcome the limitations that occurred due to drug-resistant pathogens, worldwide researches focused on the investigation of antibacterial resistance mechanisms, as well as on the development and optimization of unconventional and effective antibacterial strategies.
A concerning number of bacterial strains developed or enlarged their resistance to conventional antibiotherapy, especially due to their versatile mechanisms to adapt to the action of drugs and to the excessive usage of antibiotics [89,90,91]. The clinical implications related to infections caused by drug-resistant bacteria and the particular complications related to biofilm-embedded pathogens led to the necessity to develop new and effective bactericidal products [92,93,94]. In particular, nanomaterial-based formulations represent a feasible choice for modern and therapeutic-enhanced antibacterial agents.
Silver-based compounds have been used as antimicrobial agents for thousands of years, proving the ability to go through biological membranes and to exhibit local or systemic effects, thus being used for different treatments, including dental and digestive pathologies, wounds and burns healing [36,95]. Despite their remarkable therapeutic properties, the weakness of such compounds is related to their toxicity on human cells, which occur at higher concentrations. In addition, if prolonged treatment with silver-based compounds is applied, their accumulation in the organism may lead to vital organs’ impairment and skin discoloration (argyria) [96,97]. Therefore, in order to overcome cytotoxicity, products containing silver compounds and nanoparticles require very low metallic concentrations and suitable delivery systems.
The effects of biocompatible systems based on nanosilver for novel antimicrobial agents were assessed against various planktonic and sessile strains relevant to current clinical practice. In particular, a plethora of research studies investigated the effects of nanosilver-based biomaterials against Escherichia coli (E. coli) and Staphylococcus aureus (S. aureus), as representative (respectively) Gram-negative and Gram-positive pathogens responsible for community-transmitted and hospital-acquired infectious diseases.
In comparison with S. aureus, the increased sensitivity of E. coli to AgNPs bactericidal activity was related to the much thinner peptidoglycan layer and the outer liposaccharide portion within the cell wall, which can modulate bacterial membrane destabilization, cell penetration and leakage of intracellular organelles and macromolecules [98,99]. Due to high surface reactivity, strong interactions formed between nanosilver and bacterial membranes containing phosphorous and sulfur determined significant growth inhibition of both strains [100,101]. The antibacterial effects of AgNPs were also related to cellular stress induced by the alteration of energy-dependent processes mediated by adenosine triphosphate (ATP) [102,103].
Moreover, it was demonstrated that the toxic effects exhibited by AgNPs against E. coli and S. aureus can be mediated by the release of metallic ions (Ag+). The cellular exposure to silver ions was associated with increased levels of highly reactive species, such as singlet oxygen, hydroxyl, superoxide, hydroperoxyl, hydrogen peroxide and nitric oxide. It was reported that the generated ROS were responsible for cellular oxidative stress, induced by lipid peroxidation, impairment of protein and enzyme metabolism, degradation of nucleic acids [104,105].
The electrostatic affinity of Ag+ ions for phosphate- and thiol-containing macromolecules was associated with the inactivation or denaturation of vital macromolecules (proteins, enzymes, nucleic acids), which eventually resulted in bacterial cell death [106,107].
Size-dependent antibacterial effects of AgNPs were evidenced. Due to a larger specific surface area and intense surface reactivity, smaller nanoparticles generate better contacts with cellular structures and subcellular components and are able to induce stronger Ag+-mediated cellular oxidative stress [108,109]. Thermo-sensitive polymer nanoparticles embedded with AgNPs exhibited size-dependent antibacterial activity against both E. coli and S. aureus strains, the effects being more pronounced in the case of the smallest particles [110]. In a similar way, ultrasmall AgNPs (1.59 nm) stabilized with thermo-sensitive copolymer showed enhanced bactericidal effects against E. coli and S. aureus than bigger nanoparticles (2.29 and 3.91 nm sizes). An enhanced cytotoxic effect was observed against the Gram-negative pathogen, as evidenced by nanosilver-mediated damage of bacterial membrane, cellular uptake and ROS generation [111]. Smaller nanoparticles (below 20 nm) were generally reported as more cytotoxic for both Gram-positive and Gram-negative bacteria [112,113].
The antibacterial efficiency of nanosilver also proved to be shape-dependent. Spherical biosynthesized nanosilver (40 nm) showed stronger bactericidal effects against E. coli and S. aureus strains in comparison with NPs with irregular shapes [114]. Due to higher specific surface area and increased ability to release metallic ions, spherical AgNPs exhibited superior antibacterial effects compared with disk and triangular plate morphologies [115]. Excellent inhibitory effects were reported for ultrasmall spherical AgNPs (2–5 nm) bioreduced with fungal extract, in comparison with particles with pentagonal or hexagonal (50–100 nm) and rectangular (40–65) shape [116]. Chemically synthesized spherical AgNPs showed more effective killing bacteria ability than rod-shaped counterparts when used against both Gram-negative and Gram-positive pathogens. It was evidenced that the antibacterial activity of nanosilver is strongly related to their microstructure, namely the presence of (1 1 1) crystallographic plane [117].
Strong bactericidal or bacteriostatic effects against E. coli were also reported for AgNPs biosynthesized with gum kondagogu (4.5 ± 3.1 nm) [118], Arisaema flavum extract (5–8 nm) [119] and Polygonatum graminifolium extract (3–15 nm) [120], but also for nanoparticles capped with PVP (16 ± 2 nm) [121], pectin (8–13 nm) [122] and chitosan (>20 nm) [123]. AgNPs biosynthesized with corn silk extract (10–30 nm) [124], belladonna tincture (15–20 nm) [125], thyme extract (75 nm) [126] and nanosilver bioreduced by Bacillus subtilis (3–20 nm) [127] and Lactobacillus brevis (45 nm) [128] showed pronounced antibacterial effects against S. aureus.
Besides E. coli and S. aureus bacterial strains, nanosilver biomaterials proved efficient against various clinically-relevant pathogens, as summarized in Table 2. A wide variety of studies reported that, following their interaction with AgNPs, microbial cells death occurs due to (i) attachment to the cell surface, followed by modification of membrane permeability, cell wall piercing, intracellular infiltration and cytoplasm leakage [129,130]; (ii) generation of highly reactive species and free radicals, followed by denaturation of microbial proteins and enzymes, alteration in DNA replications [131,132]; (iii) alteration of cellular respiratory chain or / and signal-transduction pathways [133,134].
Table 2.
Effects of AgNPs against various bacterial pathogens.
| Bacterial Strain | Proposed Systems | Effects | Refs. |
|---|---|---|---|
| Bacillus subtilis (B. subtilis) | AgNPs biosynthesized with petai (Parkia speciosa), fig tree (Ficus hispida), pomegranate (Punica granatum), Sida cordifolia and Platycodon grandiflorum extracts | Antibacterial effect due to size-related cytotoxicity and phytochemicals | [135,136,137,138,139] |
| AgNPs biosynthesized with coriander (Coriandrum sativum) leaf extract and AgNPs bioreduced by Actinomycetes strain | Bacterial death due to cellular uptake and Ag+-mediated DNA damage | [140,141] | |
|
Enterococcus faecalis (E. faecalis) |
AgNPs biosynthesized with night-blooming jasmine (Cestrum nocturnum) extract | Bacteriostatic and bactericidal effects exhibited for lower and higher AgNPs concentrations, respectively | [142] |
| AgNPs bioreduced by Fusarium semitectum strain | Strong antibacterial and anti-biofilm activity | [143,144] | |
|
Klebsiella pneumoniae (K. pneumoniae) |
AgNPs biosynthesized with butterfly pea (Clitoria ternatea) and mango (Mangifera indica) flower extracts and wild ginger (Alpinia nigra) fruit extract | Antibacterial effect due to size-related cytotoxicity and phytochemicals | [145,146,147] |
| AgNPs bioreduced by Nostoc Bahar M. cyanobacteria | Strong bactericidal effect due to imbalance in bacterial antioxidants and enzymes, fragmentation and degradation of bacterial proteins | [148] | |
| AgNPs bioreduced by Bifidobacterium bifidum strain | Antibacterial activity due to inhibitory effects on efflux pump genes | [149] | |
| PVP-capped AgNPs | Antibacterial effects due to membrane disruption and cytoplasmic protein leakage, anti-biofilm effects due to inhibitory activity on extracellular protein substances | [150] | |
|
Pseudomonas aeruginosa (P. aeruginosa) |
AgNPs biosynthesized with sesame (Sesamum indicum) oil, horse chestnut (Aesculus hippocastanum) and stonebreaker (Phyllanthus niruri) extracts | Bacterial death due to cellular uptake and size-related intracellular toxicity | [151,152,153] |
| AgNPs dendronized with cationic carbosilane dendrons and modified with PEG | Destabilization of outer membrane, degradation of peptidoglycan layer (in conjunction with endolysin) | [154] | |
| AgNPs biosynthesized with eyebright (Euphrasia officinalis) leaf extract | Strong antibacterial and anti-biofilm activity | [155] | |
| AgNPs biosynthesized with Lysiloma acapulcensis extract | Antibacterial effect due to size-related cytotoxicity and phytochemicals | [156] | |
|
Salmonella enterica (S. enterica) |
AgNPs biosynthesized with green tea (Camellia sinensis) and jackfruit (Artocarpus heterophyllus) extracts | Synergistic inhibitory and bactericidal effects due to size-related toxicity and phytochemicals | [157,158] |
| AgNPs capped with afzelin and quercitrin extracted from Crotolaria tetragona | Bacteriostatic and bactericidal effects, anti-biofilm activity due to alteration of membrane potential and efflux pumps and modification of bacterial surface hydrophobicity | [159] | |
| AgNPs bioreduced by Penicillium polonicum strain | Strong bactericidal activity due to membrane disruption and cytoplasmic protein leakage | [160] | |
|
Staphylococcus epidermidis (S. epidermidis) |
AgNPs biosynthesized with river bushwillow (Combretum erythrophyllum) leaf extract, grape (Vitis vinifera) fruit extract and Elytraria acaulis leaf extract | Bacterial death due to cellular uptake and size-related intracellular toxicity | [161,162,163] |
| AgNPs biosynthesized with tea tree (Melaleuca alternifolia) essential oil | Inhibitory and bactericidal effects due to membrane disruption and bacterial internalization, synergistic toxicity related to AgNPs size and tea tree essential oil | [164] | |
|
Streptococcus mutans (S. mutans) |
AgNPs biosynthesized with citrus (Citrus limetta) peel extract | Antibacterial effect due to size-related membrane permeability alteration and anti-biofilm activity | [165] |
| SiO2-coated AgNPs biosynthesized with green tea (Camellia sinensis) extract | Strong antibacterial and anti-biofilm activity | [166] | |
|
Streptococcus pyogenes (S. pyogenes) |
AgNPs biosynthesized with Dodonaea viscosa extract and AgNPs bioreduced by Saccharopolyspora hirsute strain | Antibacterial effect due to size-related cytotoxicity and phytochemicals | [167,168] |
In addition to their intrinsic antibacterial activity, AgNPs proved impressive synergistic effects in the case of combined treatment with different natural or synthetic compounds. The treatment with PVA-capped nanosilver and hydrogen peroxide determined rapid and synergistic bactericidal effects against both Gram-negative and Gram-positive strains [169]. Biasi-Garbin and coworkers reported that bioreduced AgNPs combined with eugenol had enhanced inhibitory activity against planktonic and biofilm-embedded drug-susceptible and drug-resistant Streptococcus agalactiae isolates [170]. In comparison with conventional PVP-capped AgNPs, curcumin-capped nanosilver showed enhanced bacterial inhibitory and killing activity. The presence of curcumin determined superior interactions with bacterial cells and higher release of silver ions, resulting in ROS-mediated cytotoxicity [171].
Enhanced inhibitory effects on E. coli were reported when using the treatment with AgNPs, Centaurea damascena essential oil and Gentamicin or Amoxicillin. In the case of S. aureus, the most prominent synergistic effect was reported when combining nanoparticles and essential oil with Imipenem [172]. Pronounced antibacterial effects on both strains were also reported when treated with Vancomycin-loaded AgNPs [173].
Similar synergistic effects were reported on S. aureus and P. aeruginosa when treated with triangular-shaped nanosilver and Ampicillin or Gentamicin [174], but also when treated with Metronidazole-capped spherical AgNPs [175]. Streptomycin-resistant B. subtilis exhibited important susceptibility on the antibiotic-conjugated AgNPs treatment [176], while Ciprofloxacin-conjugated nanoparticles caused significant bactericidal effects against S. epidermidis [177]. Biosynthesized nanosilver conjugated with Ampicillin or Vancomycin [178] and Tetracycline [179] determined improved antibacterial effects against K. pneumoniae, whereas 10 nm sized bioreduced AgNPs proved potentiated antibacterial effects on S. mutans treated with Gentamycin and Vancomycin [180].
The exposure of E. coli and S. aureus to the combined treatment with AgNPs and visible light irradiation resulted in enhanced synergistic antibacterial effects against both strains. However, the ROS-mediated cytotoxicity was more evident in the case of Gram-negative bacterium [181]. Light-irradiated enhanced bactericidal effects were also reported for P. aeruginosa treated with citrate-coated nanoparticles [182].
4. Silver Nanoparticles for Antiviral Applications
Given the complexity of pathophysiological interactions established between healthy cells and viruses, the development of specific and effective antiviral agents requires thorough and unceasing efforts [183,184]. The presence of living cells is mandatory for the replication of viruses, which invade and impair or even destroy host cells. Acute and chronic conditions occurred after viral contamination generally cause systemic infections and severe related complications. Few antivirals (generally, inhibitory protein-specific or enzyme-specific drugs and nucleoside or nucleotide analogs that interfere with viral replication cycle) [185] and vaccines (biological formulations containing viral vectors—attenuated or inactivated organisms, toxins or proteins, nucleic acids or genes that activate the innate immune system of the host) [186,187] are currently available to treat viral infections. As a result of nanosize-guided structural and molecular complex studies, nanosilver-based biomaterials proved impressive tools for the development of specific, selective and efficient antiviral therapies.
The intrinsic antiviral mechanism of silver nanoparticles is not completely known and understood, the studies requiring more complex structural, molecular and immunological research than in the case of antibacterial properties. In a similar way with their antibacterial activity, the antiviral effects induced by AgNPs rely on the specific affinity for essential biomolecules (viral proteins and glycoproteins, enzymes, lipids, nucleic acids) and Ag+-mediated biostatic events, such as obstruction of cellular attachment and invasion, the arrest of intracellular viral replication or propagation, hinder of extracellular virions production [188,189,190].
Ultrasound-assisted biosynthesized AgNPs (5–15 nm) exhibited virucide activity against influenza A virus (IAV) at noncytotoxic concentrations [191]. Previous data demonstrated the size-related antiviral action of nanosilver against IAV [192]. Significant antiviral effects were reported for nanoparticles functionalized with IAV inhibitory peptide ligand due to the potentiating effect of released silver ions on the peptide [193]. AgNPs decorated with Oseltamivir and Zanamivir (inhibitors of surface-expressed neuraminidase enzyme) showed synergistic antiviral effects against IAV, by preventing attachment to host cells and hindering viral activity by downregulation in ROS generation [194,195]. Moreover, nanosilver proved to represent a suitable adjuvant for the virus-inactivated vaccine, resulting in reduced lung inflammation and induced mucosal immunity [196].
It was also reported that AgNPs interfere with the host cell attachment of respiratory syncytial virus (RSV). Curcumin-modified nanoparticles (11.95 ± 0.23 nm) significantly inhibited the infectivity of RSV, by interacting with envelope glycoproteins and thus blocking virus internalization by human epithelial cells [197]. Recently, Morris et al. demonstrated that 10 nm PVP-coated nanosilver reduced RSV replication and proinflammatory cytokines production, both in epithelial cell lines and infected mouse lung tissue [198].
Fungal bioreduced AgNPs proved to inhibit cellular attachment and intracellular replication of type 1 herpes simplex virus (HSV-1), in a manner dependent on the particle size [199]. Noncovalent interactions between HSV-1 thymidine kinase ligands and nanoparticles biosynthesized with plant extracts were considered responsible for the antiviral activity of nanosilver [200]. AgNPs modified with tannic acid (33 nm) showed the ability to reduce the cellular infectivity with type 2 HSV (HSV-2), by directly blocking viral glycoproteins and interacting with viral DNA. The treatment with these nanoparticles also reduced local inflammation and potentiated virus-specific immune response in both primary and recurrent HSV-2 infection of mice [201,202]. Noncytotoxic concentrations of nanosilver produced by marine alga effectively reduced the cytopathic effect (an indication of host cell death after virus-related lysis or reproductive inability) in cells infected with HSV-1 and HSV-2 [203].
PVP-coated AgNPs (25 nm) with antitumor activity exhibited high cytotoxicity on cells infected with oncogenic γ-herpesviruses, such as Kaposi’s sarcoma-associated herpesvirus and Epstein–Barr virus. The nanoparticles interfered with viral replication (by inducing ROS generation and activating autophagy) and impaired associated virions [204]. El-Mohamady and coworkers reported that cytocompatible concentrations of spherical AgNPs (<30 nm) induced inhibitory effects on the replication of bovine herpesvirus-1 [205].
It was previously reported that AgNPs show antiviral action against cells infected with type 1 human immunodeficiency virus (HIV-1) [206], but are also able to prevent cell infection [207]. Low concentrations of silver nanorods conjugated with sodium 2-mercaptoethane sulfonate significantly interfered with HIV-1 replication [208]. AgNPs (10–28 nm) biosynthesized with Rhizophora lamarckii extract inhibited the activity of HIV-1 reverse transcriptase, an essential viral replication enzyme [209]. It was determined that positively charged nanosilver can form complexes with either HIV-1 protease (able to split viral polyproteins into mature and infectious particles) or specific peptides (macromolecules similar to HIV-1′s polyproteins). Due to competitive interactions, the early presence of AgNPs resulted in the most important decrease in viral replication [210].
Nanosilver-based formulations proved efficient therapeutic effects against several pathologies caused by clinically-relevant viruses, such as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [211,212], human papilloma virus (HPV) [213], rotavirus [214,215] and other enteric viruses [216,217,218]. It is worth mentioning that new and effective platforms containing AgNPs were evaluated for their biocidal activity against viral vectors, generally mosquito-borne pathogens including Zika virus [219,220], Dengue virus [221,222], West Nile virus [223,224] and Chikungunya virus [225,226].
5. Silver Nanoparticles for Cancer Therapy
Cancer represents a major concern in public health, being a group of aggressive and treatment-deficitary diseases that are incriminated in an alarming number of deaths at a global level [227,228]. In general, the conventional treatment of cancers consists of strategies with reduced selectivity and specificity, such as surgery, radiation therapy and chemotherapy, which lead to inefficient anticancer therapy [229]. With the aim to enhance the patients’ response to the considered anticancer treatment and to improve their general healthcare status, new nano-related strategies were proposed and assessed for cancer therapy [230,231].
Silver nanoparticles have a special role in modern anticancer therapy, being explored for detection and diagnosis of malignant tumors [232,233], controlled and externally triggered drug delivery systems [234,235]. In a similar way with the antimicrobial activity of AgNPs, their efficiency against cancer cells require the cellular uptake of nanosilver, which can be acquired by diffusion, phagocytosis, pinocytosis and receptor-mediated endocytosis [236,237]. The size, morphology and surface properties of AgNPs are favorable for internalization by cancer cells, which results in local release of silver ions and oxidative stress [238,239]. Such events further cause the death of cancer cells, either by (i) apoptosis, which occurs due to alteration of mitochondria and generation of imbalance between antiapoptotic proteins and proapoptotic kinases, and (ii) structural and functional impairment of cellular substructures, which occurs due to specific interactions with silver nanoparticles and ions [240,241].
Mitochondrial-dependent apoptosis of lung adenocarcinoma cells treated with nanosilver biosynthesized in the presence of cotton leaf extract was reported in a study performed by Kanipandian and coworkers. They also evidenced that negatively charged spherical nanoparticles, with 13–40 nm physical size, induced cell cycle arrest [242]. Besides oxidative stress, the treatment of lung cancer cells with AgNPs synthesized with Anemarrhena asphodeloides medicinal plant extract also resulted in decreased cellular migration [243]. The latest nanoparticles also proved anticancer efficiency against human colon and breast cancer cell lines. In addition, pulmonary cancer cells treated with biosynthesized AgNPs overexpressed the pro-apoptotic caspase-3 gene [244,245].
Under biological media, AgNPs may undergo specific processes that may influence their cytotoxicity, such as surface oxidation, biomolecule conjugation or attachment, the release of surface metallic ions [246,247]. In a complex comparative study performed by Ahn and coworkers, nanosilver obtained with thirty medicinal plant extracts exhibited substantial cytotoxicity against lung cancer cells, the results being remarkable in comparison with sole extracts. The authors also reported increased toxic effects in the case of cells cultured in media containing fetal bovine serum, as a consequence of protein corona modulated interactions [248]. Majeed et al., also reported that nanosilver resulting from bacteria-mediated biosynthesis and capped with bovine serum albumin showed important toxicity against breast cancer, colon carcinoma and osteosarcoma cells. In comparison with the initial nanosilver, protein-capped AgNPs (11.26–23.85 nm dimensional range) exhibited increased toxicity at reduced concentrations [249].
Well-dispersed AgNPs (20–30 nm size), obtained with tamarind fruit shell extract, induced apoptotic death in human breast cancer cells. A dose-dependent anticancer effect was reported, as the local increase of ROS led to mitochondrial impairment and DNA damage [250]. The same cytotoxic effects were evidenced after cellular treatment with AgNPs biosynthesized with extract from Ochradenus arabicus medicinal shrub [251] and marine bacilli [252]. Synergistic toxicity against breast cancer cells were reported by using Capecitabine-loaded citrate-capped AgNPs [253] and Gemcitabine-loaded PVP-stabilized nanosilver [235].
Concentration-dependent cytotoxicity of AgNPs (33 nm average size) biosynthesized with extract of Nepeta deflersiana medicinal plant against human cervical cancer cells was reported. In a similar way to previous studies, the AgNPs-mediated oxidative stress was responsible for mitochondrial damage and cell cycle impairment, which further caused the apoptotic and necrotic death of malignant cells [254]. Electrolytically deposited AgNPs capped with black tea extract also proved anticancer efficiency [213]. Sinigrin-mediated synthesized AgNPs, with 20 nm average size, induced dose-dependent toxicity on cervical cancer cells, as well as synergistic apoptotic processes in the case of combined treatment with Camptothecin [255].
Medicinal plant extracts contain substantial amounts of secondary metabolites with important effects against tumor cells. Highly stable spherical AgNPs obtained using neem leaf and shrub root extracts showed toxicity against breast, colon and hepatic cancer cells. Still, the most reliable results were obtained when using ethanolic extracts (instead of aqueous) on the colon adenocarcinoma cell line [256]. Complementary results on the anticancer efficiency were reported for nanosilver obtained with bulletwood fruits extract [257]. AgNPs biosynthesized by freshwater cyanobacterium potentiated the antibacterial effects of commercial antibiotics in the case of combined administration. In addition, they showed dose-dependent cytotoxic effects against human breast and colon cancer cells, apoptotic events being evidenced [258].
In another study, biogenic AgNPs prepared by using honey from distinctive floral sources manifested antiproliferative activity against liver tumor cells [259]. Quasispherical silver nanoparticles biosynthesized with lotus extract showed significant cytotoxic effects against human prostate, liver and gastric cancer cells [260]. Gastric adenocarcinoma cells were also impaired after treatment with AgNPs biosynthesized with medicinal extracts from leaves of felty germander [261] and from fruits of Crataegus microphylla shrub [262]. Other recent data on the toxic effects of silver nanoparticles against cancer cells are included in Table 3.
Table 3.
Cytotoxicity of AgNPs against various cancers.
| Malignant Cells | Proposed Systems | Effects | Refs. |
|---|---|---|---|
| Bladder carcinoma | AgNPs bioreduced by Fusarium oxysporum strain | Apoptosis induced by DNA damage, reduced cellular migration and proliferation, tumor regression | [263] |
| Breast adenocarcinoma | AgNPs bioreduced by Penicillium citrinum strain | Apoptosis induced by DNA damage | [264,265] |
| AgNPs biosynthesized with fineleaf fumitory (Fumaria parviflora), rhododendron (Rhododendron ponticum), rhubarb (Rheum ribes) and cumin (Cuminum cyminum) extracts | Cell death evidenced on distinctive tumor cell lines | [266,267,268,269] | |
| Colorectal cancer | AgNPs biosynthesized with creeping woodsorrel (Oxalis corniculata) leaf extract | Cell death induced by apoptotic and necrotic mechanisms | [270] |
| AgNPs biosynthesized with peacock (Caesalpinia pulcherrima) flower extract | Cell death induced by apoptosis and membrane damage | [271] | |
| Hepatocellular carcinoma | AgNPs bioreduced by Bacillus safensis strain | Cell death induced by apoptotic and necrotic mechanisms | [272] |
| PVP-stabilized AgNPs | Cell death induced by damage of cellular organelles (especially mitochondria) and oxidative stress, upregulation of mitochondrial proapoptotic proteins | [273] | |
| Laryngeal carcinoma | AgNPs bioreduced by Penicillium italicum strain | Cell death induced by ROS-mediated membrane damage and essential enzymes impairment | [274] |
| Lung adenocarcinoma | AgNPs bioreduced by Bacillus amyloliquefaciens strain | Cell death induced by ROS generation and damage of cellular organelles | [275] |
| AgNPs biosynthesized with soursop (Annona muricate) and mangrove (Avicennia marina) leaf extracts | Apoptosis induced by ROS generation, downregulation of antiapoptotic genes and upregulation of proapoptotic genes | [276,277] | |
| Osteosarcoma | AgNPs biosynthesized with cempedak (Artocarpus integer) and mangrove (Rhizophora apiculata) leaf extracts and noni (Morinda citrifolia) bark extract | Cell death evidenced on distinctive tumor cell lines, cell death induced by membrane damage and oxidative stress | [278,279,280] |
| Rhabdomyosarcoma | AgNPs bioreduced by Bacillus sp. strain | Cell death induced by ROS generation | [281] |
Besides their effects on cellular and subcellular structures, AgNPs significantly affect tumor angiogenesis, being responsible for alterations in growth factors’ expression and subsequent restricted proliferation and migration of endothelial cells [282,283]. Yang and coworkers reported that ~10 nm AgNPs induced dose-dependent apoptosis in breast cancer cells but also inhibited the transcription of hypoxia-inducible factor-1 (HIF-1) and the induction of vascular endothelial growth factor-A (VEGF). Together with the inhibition of tube formation in healthy endothelial cells, the authors proved the antiangiogenic effects of nanosilver [284]. Another study evidenced that the inoculation of AgNPs within the chorioallantoic membrane caused an important increase in the expression of caspase-3 and caspase-8 genes, which are responsible for cell apoptosis. The 15 nm particles obtained with red amaranth extract induced an important decrease in the length and number of new blood vessels and showed cytotoxic effects against breast malignant cells [285]. Also, antiangiogenic effects were reported for chicken chorioallantoic membrane treated with AgNPs biosynthesized with madder extract [286].
Except for their intrinsic anticancer effects, particular attention was oriented to the development and assessment of new silver-based nanosystems for boosted chemotherapy and radiotherapy. For example, branched gold-silver nanoparticles coated with dopamine and subjected to near-infrared irradiation determined photothermal-mediated cytotoxicity against colon cancer cell lines. By complex in vitro and in vivo studies, the authors evidenced that NP-mediated photothermal therapy (PTT) occurred by various apoptotic and necrotic mechanisms [287]. Multifunctional core-shell nanosystems based on AgNP core and aggregation-induced emission molecule were recently proposed by He and coworkers. The complex platforms were excellent enhancers for radiotherapy and modulators for PTT and photoacoustic effect but also exhibited excellent potential as contrast agents for fluorescence and computed tomography imaging [288].
Systems based on silver/magnetite nanoparticles coated with PEG, modified with folic acid and loaded with Doxorubicin drug showed great potential for the PTT of cervical cancer. Besides dual chemotherapeutic/photothermal effects, the hierarchical platforms exhibited targeted specificity for cancer cells and imaging potential by fluorescence and magnetic resonance [289]. Due to synergistic chemotherapeutic and photothermal effects that occurred after laser irradiation, enhanced cytotoxicity against malignant cells was reported for nanosystems based on Methotrexate-conjugated nanoparticles based on graphene oxide (GO) and AgNPs [290] and 5-Fluorouracil-loaded mesoporous SiO2-coated silver/gold nanoshells [291].
AgNPs capped with PEG and labeled with I-131 radionuclide showed increased targeting ability for malignant tissues in an animal model, with maximum solid tumor uptake of 35.43 ± 1.12% ID/g (reached at 60 min. after intravenous inoculation) and 63.8 ± 1.3% ID/g (reached at 15 min. after intratumor injection) [292]. Biosynthesized AgNPs with intrinsic cytotoxicity against hepatic malignant cells, proved a potentiating effect on the gamma radiation treatment [293]. Also, the treatment with cold atmospheric plasma-activated PVA-stabilized nanosilver resulted in additive cytotoxic effects against human glioblastoma multiforme cells [294].
AgNPs obtained in the presence of globe artichoke (Cynara scolymus) leaf extract by microwave irradiation showed the photosensitizing ability for the photodynamic therapy (PDT) of human breast adenocarcinoma cells. Synergistic effects were reported following the combined treatment, such as severe mitochondrial damage and ROS generation [295]. Enhanced cytotoxic effects were also reported in the case of melanoma cells, where AgNPs functionalized with porphyrin acted as mediators for enhanced PDT [296].
6. Silver Nanoparticles for Tissue Engineering
At the microstructural level, human tissues consist of highly organized cells with specific functions and their corresponding extracellular matrix (ECM, protein-based environment containing glycosaminoglycans, which in turn provides three-dimensional support for cellular adhesion and proliferation, regulates intercellular communication and tunes cell physiology). Generally, the structural and functional impairment of human tissue may occur due to acute or chronic injuries, severe inflammatory conditions, genetic disorders, degenerative conditions and tumors. With the aim to overcome the limitations of organ transplantation (including reduced bioavailability in the case of autografts and isografts, immunogenicity and graft rejection in the case of allografts and xenografts), healthcare professionals and scientists turned their attention towards the impressive potential of tissue engineering.
As a part of regenerative medicine, the desideratum of tissue engineering (TE) is represented by the fabrication of nonviable complex biocompatible systems that are able to revive the structural integrity and functionality of damaged tissues by restoring, replacing or regenerate them [297]. Nanostructured biomaterials represent a suitable choice for TE applications, not only because they properly interact with living systems and possess specific and selective therapeutic purpose, but also because they possess versatile and tunable characteristics which enable the achievement of particular requirements, such as (i) biocompatibility (a complex feature that relies on the bidirectional interactions between nanomaterials and host cells or tissues); (ii) physicochemical properties (microstructure, phase transitions, porosity, wettability, morphology, topography, composition, stability, reactivity); and (iii) circumstantial bioactivity [298,299].
Given their reduced toxic effects in healthy cells, facile surface functionalization and excellent antimicrobial activity, the impact of nanosilver-based biomaterials for TE was thoroughly evaluated.
To begin with, AgNPs-embedded coatings were reported to boost the biological performances of bioinert materials used in orthopedics and orthodontics. The simple modification of titanium implants’ surface with nanosilver resulted in significant antibacterial effects against strains responsible for implant-associated infections while maintaining excellent biocompatibility [300,301,302]. Nanotubular titanium oxide surface coated with silver nanowires showed prolonged inhibitory action against S. aureus and E. coli, with more prominent effects against the Gram-positive strain. At the same time, the nanostructured surface exhibited protein adsorption capacity and proved an excellent substrate for the adhesion and proliferation of osteoblast-like cells [303]. Similar bactericidal performances were also evidenced for a mixed titanium/niobium oxide nanotube array coated with AgNPs-decorated GO sheets. In comparison with bare titanium-based alloy, the as-modified substrates showed improved cytocompatibility and differentiation of pre-osteoblastic cells, alongside superior corrosion resistance and apatite formation ability [304].
Polymer coatings embedded with AgNPs are unharmful materials for normal cells and only act as protective carriers or enhancers for local anti-infective effects, thus inducing or potentiating the antibacterial activity of metallic biomaterials [305,306]. Titanium implants modified with nanosilver-embedded poly(lactic-co-glycolic) acid (PLGA) coatings showed strong bactericidal activity against opportunistic pathogens, together with important osteoinductive potential [307]. Nanocomposite coatings of chitosan–tragacanth gum embedded with nanoparticles of silica and biosynthesized silver (SiO2@Ag) demonstrated enhanced apatite-forming ability, as well as good antibacterial effects under both acidic and aqueous media [308]. Electrospun composites based on polylactic acid (PLA), GO and AgNPs increased the mechanical properties and anticorrosive behavior of magnesium alloy and encouraged the formation of a stable apatite layer. Such composite coatings reduced the degradation rate of magnesium alloy and proved beneficial for the adhesion, proliferation and normal development of osteoblast-like cells while significantly inhibited bacterial growth [309].
A more attractive and successful strategy to enhance the performance of metallic implants consists of modifying their surfaces with biomimicking coatings containing nanosilver, which simultaneously determine superior osseointegration and anti-infective efficiency [310,311]. Estrada-Cabrera and coworkers reported the potential use of composite coatings based on bioactive glass, CS and AgNPs for surface modification of anodized titanium implants [312]. Nanostructured material composed of hydroxyapatite (HAp), CS, AgNPs and lysozyme proved cytocompatible substrates for osteoblasts. Titanium substrates modified with such hybrid coatings exhibited strong bactericidal effects due to the synergistic activity of the latter two components [313]. Even if nanostructured coatings of HAp, zirconium oxide and nanosilver proved to decrease the corrosion resistance of zirconium/titanium alloy, they showed superior osteoconductive ability and enhanced the in vivo osseointegration of as-modified implants [314,315].
Significant inhibitory activity against planktonic and sessile bacteria was reported in the case of AgNPs-incorporated silk fibroin (SF) films. Low concentrations of nanosilver determined favorable cytocompatibility on fibroblasts and osteoblasts, as well as nondetrimental effects on the osteogenic differentiation ability of human mesenchymal stem cells [316]. The bone-forming potential of SF coatings embedded with AgNPs and Gentamycin was evidenced in an animal model. The highly hydrophilic and protein adsorptive surfaces showed a pH-dependent release of metallic silver, which determined enhanced biocompatibility, mineralization and osteoinductive potential, but also long-term antibacterial efficiency [317]. The potential use of hydrogels of SF and CMC loaded with low concentrations of nanosilver for TE applications was also reported. The highly absorbent composites showed strong antibacterial and mild antifungal efficiency and displayed cytocompatibility with respect to bone marrow stem cells [318].
A recently developed endodontic sealer based on methacrylate derivative embedded with nanoparticles of amorphous calcium phosphate and silver determined remineralization and strengthening effects on dentin, but also strong bactericidal activity against pathogens associated with dentin infections [319]. AgNPs-loaded natural rubber latex showed low toxicity and tissue reaction similar to commercial products, being proposed as an antibacterial occlusive membrane for guided bone regeneration in orthodontics [320]. High bactericidal efficiency and cytocompatibility were also reported by embedding rigid poly(methyl methacrylate) (PMMA) nanoparticles decorated with CS-stabilized AgNPs within soft films of natural rubber [321].
Biodegradable electrospun membranes of poly(caprolactone) (PCL) or polylactide/cellulose acetate (PLA/CA) embedded with nano-HAp and AgNPs promoted the formation of bone-like apatite. The nanofibrous composites exhibited prolonged bactericidal effects, being proposed as suitable materials for orthodontic applications [322]. Liu et al., reported the successful fabrication of nanofibrous materials based on PLA/HAp nanowires modified with polydopamine membrane and coated with polypyrrole-stabilized AgNPs. The obtained hybrid biomaterials possessed good stability under physiological conditions, enhanced mineralization ability, excellent cytocompatibility and long-term antibacterial efficiency, being promising candidates for bone-related regenerative and anti-infective applications [323].
The sustained release of Ag+ from PLA scaffolds modified with nanosilver-loaded halloysite nanotubes determined prolonged antibacterial activity. The as-modified scaffolds showed increased mechanical properties, degradability and mineralization, which positively contributed to supporting cellular proliferation and osteogenic differentiation [324]. Hasan and coworkers reported that CS/CMC scaffolds modified with AgNPs-decorated cellulose nanowhiskers possess suitable porosity and compressive behavior for bone TE applications, in conjunction with intrinsic antibacterial efficiency. The controlled degradability of hybrid scaffolds was adjusted for angiogenesis and vascularization processes and proved beneficial for in vitro mineralization, while the protein adsorption ability determined superior adhesion and proliferation of osteoblasts [325]. Silver nanorods incorporated within highly porous wollastonite scaffolds determined strong bactericidal effects while providing the favorable apatite-forming ability and good cytocompatibility with respect to osteoblast-like cells [326]. Composite freeze-thawed gelatin/alginate/PVA and electrospun PCL scaffolds embedded with a bactericidal concentration of silver-HAp nanoparticles showed suitable porosity and prolonged release metallic ions, with simultaneous favorable adhesion, proliferation and osteogenic potential on mammalian cells [327,328].
Substrate roughness and wettability possess a very important role in protein absorption and cellular attachment, therefore significantly contributing to the biological performance of implanted devices. The addition of AgNPs within electrospun scaffolds of CMC/PVA and PCL loaded with rambutan polyphenolic extract determined higher cellular proliferation rates due to surface modification [329,330]. Titanium oxide nanotube array coated with AgNPs-embedded polydopamine layer was assessed as a feasible option for arthroplasty [331]. CS-SF/PET (polyethylene terephthalate) scaffolds modified with nanosilver/HAp by plasma splashing procedure promoted cellular proliferation and osteogenic differentiation of mesenchymal stem cells. The composite scaffolds restricted the resorption of bone passage and enhanced the biomechanical response of bone–joint interface, being potential candidates for the replacement of anterior cruciate ligament [332]. In addition, AgNPs-decorated nanofibrous membranes of PET, with good cytocompatibility and inhibitory effects against planktonic and sessile bacteria, induced weak inflammation and reduced foreign body response in an animal model [333]. Poly(acrylonitrile-butadiene-styrene) copolymers modified with AgNPs were proposed as suitable candidates for the fabrication of middle ear implants. The composites exhibited pronounced hydrophilicity and long-term mechanical stability while determined no cytotoxic effects and promoted cellular proliferation in both osteoblast and fibroblast cultures [334,335].
Thanks to their excellent mechanical strength, gradual degradation and biological activity, agarose scaffolds impregnated with CS-coated nanosilver were proposed for soft TE applications. In addition to their intrinsic bactericidal efficiency, the biopolymer-based scaffolds showed good hemocompatibility and enhanced cytocompatibility with different epithelial cell lines [336]. The incorporation of AgNPs within composite aerogels of bacterial cellulose (BC) and polyaniline (PANI) determined increased viscoelastic behavior, which is an important factor for the repair and regeneration of soft tissue [337,338]. With the aim to obtain low-cost antibacterial scaffolds for TE applications, the decellularized fish swim bladder matrix was modified with colloidal AgNPs. The resulted collagen-enriched scaffold showed broad-spectrum bactericidal efficiency (due to the gradual release of nanosilver) and biocompatibility, as well as good flexibility and biodegradability [339]. The ultrastructure of decellularized esophageal scaffolds (more regular and enhanced binding of collagen fibers, reduced alteration of pore areas) was improved by modification with 5 µg/mL of citrate-stabilized AgNPs (100 nm), due to their ability to non-covalently interact with the collagenous material. The as-modified scaffolds presented superior water uptake ability, substantial resistance to enzymatic degradation and thermal stability, together with excellent anti calcification effect. Moreover, the nanosilver-modified matrices exhibited highly compatible behavior with respect to stem and endothelial cells, while the intrinsic anti-inflammatory activity of AgNPs led to a reduced immune response of tissue after in vivo implantation [340].
The interconnected porosity of CS scaffolds incorporated with AgNPs-embedded CS microspheres proved beneficial for the adhesion, proliferation and migration of fibroblasts. Given the sustained release of metallic silver and the prolonged antibacterial effects of such nanostructured scaffolds, they were evaluated as suitable candidates for skin TE by Niu and coworkers [341]. Macroporous CS sponge embedded with polysaccharide biosynthesized nanosilver were proposed for the regeneration of skin defects due to excellent water retention property, mechanical behavior and biological performances [342]. SF nanofibrous mats modified with biosynthesized AgNPs were also proposed for skin TE. In comparison with several commercial products, the highly biocompatible constructs showed superior extensibility and flexibility, as well as increased water uptake, which are essential aspects for tissue repair [343].
Thanks to their impressive compositional versatility and high intrinsic hydrophilicity, swelling capacity and tunable degradability, adequate elasticity and flexibility and stimuli-responsive ability, hydrogels attracted particular attention in regenerative medicine. AgNPs-embedded biocompatible platforms with promising potential for TE applications include guar gum hydrogel [344], gelatin/PEG/dopamine hydrogel [345] and carboxymethyl starch/PVA/citric acid hydrogel [346].
7. Silver Nanoparticles for Wound Care
Wounds are defined as damage in the natural structure of the skin and adjacent tissues, which may appear through several traumas, including physical or mechanical injury, chemical or thermal damage and biological impairment. The natural healing process starts right after the occurrence of a wound, by impressive local recruitment of immune, cellular and vascular components that synergistically act for the proper restoration of structural and physiological functions [347,348]. This process relies on the accurate sequence of the following essential stages: hemostasis, inflammation, cellular proliferation, re-epithelialization and tissue remodeling [349,350]. When the affected tissue is not able to heal properly, the wound healing process is inadequate and may further lead to various complications and even life-threatening conditions.
Currently, few strategies are available for the clinical management of wounds. For instance, in terms of compatibility and enhanced healing process, skin autografts and xenografts represent a desirable therapeutic choice for severe wounds. Except for being expensive approaches, these strategies have specific limitations, such as restricted bioavailability, respectively immunogenicity and increased possibility for disease transmission [351,352]. In addition, oxygen-enriched therapy is beneficial for accelerated wound healing, as oxygen is essential for the stimulation of collagen synthesis and subsequent re-epithelialization, as well as for the induction of angiogenesis [353,354]. Besides being a costly and uncomfortable procedure, it was also reported that hyperbaric oxygen therapy has limited efficiency since negative pressure therapy is generally suitable for small wounds and may induce several physical effects that can hamper the healing process [355,356]. Another therapeutic strategy for wound healing consists in using wound dressings, which support the structural and functional restoration of the injured tissue and may additionally provide protection against external pathogens. Several key aspects must be considered for an effective wound dressing, such as biocompatibility, fluid (super)absorption, water and oxygen partial permeability, nonimmunogenicity, facile and nontraumatic removal [357,358]. Even if a wide variety of dressings is commercially available, the current tendency in wound care management is to develop specific and performance-enhanced dressings, which provide suitable compositional, structural and biofunctional features for proper wound healing process [134,359].
The opportunistic microbial contamination and colonization of wounds generally lead to the delayed and circumstantial improper healing process, but it may also lead to severe infections and critical healthcare complications [360,361]. Therefore, impressive attention was oriented on the development of anti-infective wound dressings, which can be produced by embedding dressing materials with different antimicrobial agents, such as synthetic antibiotics [362,363], essential oils [364,365] and antibacterial nanoparticles [366,367,368].
Silver derivatives were used for wound care since ancient times, as even Hippocrates described their efficiency in wound healing [369]. Also, silver-based compounds were used to reduce the intraoperative risk of wound infection from the late XIX century [370] and remained the preferred agent for partial burns treatment since mid of XX century (as they can absorb fluids better and reduce infective processes) [371,372]. However, the decrease observed in the use of SSD-based products (occurred due to different side effects, like eschar formation and tissue irritation) led to the development of unconventional silver-based therapeutic formulations [373,374]. Among noble metals, silver, in the form of nanoparticles and nanosystems, represents the most explored representative for the successful development of innovative and effective wound dressings, thanks to their impressive biocide and biostatic effects, anti-inflammatory activity and reduced or absent toxicity for human tissues [37,375]. Given the above-mentioned aspects, together with tunable surface chemistry, drug delivery ability and low production costs [376,377], different products containing silver nanoparticles and ions are commercially available (as previously summarized in Table 1). Other silver-based nanostructured candidates with promising preclinical performances in wound care management are included in Table 4.
Table 4.
Nanosilver-embedded formulations for wound healing.
| Proposed Systems | In Vitro Effects | In Vivo Effects | Refs. |
|---|---|---|---|
| CS films embedded with CS-stabilized AgNPs | Antibacterial effects against E. coli | Better and faster wound healing rate, reduced local inflammation and enhanced angiogenesis | [413] |
| CS/sericin films conjugated with AgNPs and loaded with Moxifloxacin | Antibacterial effects against E. coli, P. aeruginosa, S. epidermidis, drug-sensitive and drug-resistant S. aureus | Rapid and enhanced repair of infected burn wounds accelerated wound healing, reduced local inflammation, improved collagen deposition and angiogenesis | [414] |
| CS/PEO nanofibrous membranes incorporated with AgNPs | Antibacterial effects against S. aureus | Bactericidal effects in infected wounds, faster wound healing rate, improved regeneration of epidermis and neovascularization | [415] |
| CS/KGM hydrogel embedded with AgNPs | Antibacterial effects against E. coli and S. aureus Good biocompatibility on fibroblasts |
Enhanced repair of infected wounds, reduced inflammation by regulating local levels of proinflammatory and anti-inflammatory interleukins | [416] |
| Collagen/CS dressing loaded with AgNPs | Antibacterial effects against E. coli, P. aeruginosa and S. aureus | Faster wound healing rate, enhanced re-epithelialization, reduced local inflammation, downregulation of inflammatory cytokine and upregulation of growth factors | [417] |
| Galactoxyloglucan hydrogel scaffolds decorated with AgNPs | Antimicrobial effects against E. coli, S. aureus and C. albicans Enhanced cellular adhesion and proliferation of fibroblasts |
Bactericidal effects in infected wounds, better and faster wound healing rate, improved collagen deposition and angiogenesis | [418] |
| PVA/β-cyclodextrin nanofibrous scaffolds loaded with AgNPs and riboflavin | Antibacterial effects against E. coli and S. aureusEnhanced cellular proliferation of epithelial cells | Enhanced wound contraction and re-epithelialization | [419] |
| PVA/PVP/pectin/MF nanofibers embedded with AgNPs | Antibacterial effects against E. coli, P. aeruginosa and S. aureus Enhanced cellular proliferation of fibroblasts |
Faster healing rate and tissue regeneration | [420] |
| PCL/PVA nanofibrous scaffolds loaded with AgNPs | Antibacterial effects against S. aureus Good biocompatibility on fibroblasts |
Improved wound closure, faster healing rate, reduced inflammation, promoted angiogenesis | [421] |
| PU/CA nanofibrous scaffolds incorporated with AgNPs-decorated GO and curcumin | Antibacterial effects against P. aeruginosa and S. aureus Enhanced cellular proliferation of fibroblasts |
Improved neovascularization and collagen deposition, faster adnexal healing response, accelerated wound healing and advanced epidermis regeneration | [422] |
| PU foam dressings incorporated with AgNPs and asiaticoside | Antibacterial effects against B. subtilis, E. coli, P. aeruginosa and S. aureus Enhanced cellular proliferation of fibroblasts |
Safe skin application, improved and accelerated wound healing | [423] |
Abbreviations: PEO—polyethylene oxide; KGM—konjac glucomannan; MF—mafenide acetate.
Depending on the type and localization of tissue injury, cotton dressings, silk sutures and synthetic polymeric mats represent the preferred choice for open wounds. Still, these formulations are effective only for promoting or accelerating the healing process, without preventing or eliminating opportunistic microbial contamination. The facile modification of cotton [378,379] and silk [380,381] materials with nanosilver resulted in promising local antibacterial effects without affecting the intrinsic long-term stability and wound healing ability of initial substrates. Cotton fabrics coated with AgNPs stabilized with CS derivatives exhibited strong and long-lasting bactericidal efficiency [382,383]. Substantial antimicrobial activity was also reported in the case of nanosilver-decorated polypropylene [384,385] and nylon [386,387] fibers and fibrous mats.
As a consequence of synergistic anti-infective efficiency, strong antimicrobial and anti-biofilm effects were reported for textile wound dressings modified with alginate embedded with AgNPs conjugated with essential oils of mandarin, clove and niaouli [388]. Wound dressings coated with biosynthesized AgNPs determined intense collagen deposition and faster re-epithelialization in the case of burn wounds (17 days, in comparison with 25 days for uncoated dressings). The as-modified materials exhibited improved tensile strength and accelerated healing potential, being thus proposed for the management of pediatric wounds [389].
The mechanical properties and antibacterial activity of CS films were experimentally improved by incorporating them with biosynthesized nanosilver [390,391]. CS films embedded with AgNPs were proposed as temporary wound dressings. The bacteriostatic and bactericidal composites showed a water vapor transmission rate comparable with commercial dressings, as well as reduced degradability and prolonged cytocompatibility on human fibroblasts [392]. Moreover, CS derivative films incorporated with AgNPs in 0.125% inorganic/organic ratio showed suitable hemolytic and hemostatic effects for wound healing applications [393].
The capacity of composite films of sodium alginate containing SiO2-coated AgNPs was investigated for wound dressing use. The obtained films showed slow release of silver ions, increased hydration properties and prolonged bactericidal and anti-biofilm activity. Even if comparable antibacterial effects were reported in the case of films incorporating acetate-stabilized nanoparticles, only the presence of silica layer determined excellent compatibility with respect to fibroblasts and keratinocytes [394]. The ability to promote wound healing and exert efficient antibacterial effects against planktonic and biofilm-embedded bacteria were also reported for alginate/HA membranes embedded with Chitlac-stabilized AgNPs [395].
Nanofibrous electrospun mats of hyaluronic acid (HA) and polygalacturonic acid (PGA) embedded with nanosilver showed promising results for wound healing. Increased mechanical behavior and hydrophilicity, but also enhanced antibacterial activity was reported for the composites obtained by electrospinning. Moreover, faster healing and wound epithelialization were evidenced, as well as reduced tissue inflammation. Such behavior was assigned to the presence of AgNPs, which intrinsic anti-inflammatory activity contributed to accelerated wound healing [396].
The hydrophilic nature of hydrogels is closely related to their impressive ability to absorb wound exudates and to maintain adequate wound bed moisture [397,398]. By also considering their intrinsic flexibility and swelling, similar hydration with skin tissue and circumstantial stimuli-responsive ability, (hydro)gel dressings help to substantially reduce pain scores, accelerate wound healing and prevent bacterial contamination by the facile incorporation of antimicrobial agents [358,399].
In order to extend the use of CS hydrogels for wound dressing applications, Wang and coworkers modified them with AgNPs. They demonstrated that the addition of nanoparticles within biopolymeric hydrogel resulted in ultrahigh mechanical properties of the composite hydrogel without affecting its structural integrity. Faster and improved wound healing were evidenced in the case of nanosilver-embedded hydrogel [400]. Also, biocompatible PVA/CS hydrogels loaded with electrochemically synthesized nanosilver showed improved swelling ability, as well as the slower and prolonged release of metallic ions, which are desirable aspects for wound healing applications [401]. Together with favorable mechanical strength and self-healing ability, the excellent biocompatibility and enhanced healing effects evidenced on infected wounds recommend AgNPs-loaded chitosan/carboxymethyl chitosan hydrogel for wound management [402].
Composite hydrogels of alginate/gelatin loaded with AgNPs determined the improved formation and maturation of granular tissue and promoted the earlier formation of primary collagen scars [403]. Effective antibacterial activity accelerated healing process and enhanced re-epithelialization were reported in the case of PVA hydrogel patches loaded with biosynthesized AgNPs [404]. Thanks to their enhanced water vapor transport and increased moisture retention, highly antibacterial starch/PVA hydrogel membranes loaded with biosynthesized AgNPs exhibited impressive potential for wound dressing use [405]. Jaiswal and coworkers demonstrated the promising use of carrageenan hydrogel films embedded with lignin-stabilized nanoparticles for the treatment of full-thickness wounds [406]. The efficiency of Pluronic F-127 gels loaded with nanosilver against planktonic and sessile bacteria was also reported. The proposed formulations showed great cytocompatibility on human cells and excellent thermoreversibility, which determined the facile application of gel dressing [407].
In a complex study, Erring et al. investigated the healing ability of AgNPs gel and nanosilver foam dressings in patients with burn wounds. In comparison with nanostructured gel and collagen dressings, the nanostructured foam exhibited the best results: faster-wound healing rate, a higher number of patients with improved re-epithelialization (55% vs. 20% and 30%, respectively), increased ease of application (95% vs. 78% and 80%, respectively), improved level of tolerance and significantly reduced pain scores. All taken together, nanosilver foam dressings proved a more efficient strategy for the management of partial-thickness burns [18].
Besides their complex cellular compatibility (which enables adhesion, proliferation and circumstantial differentiation) and porous architecture (which is beneficial for cellular migration and angiogenesis), 3D scaffolds designed for wound healing applications possess proper mechanical features, suitable flexibility, swelling ability and tunable biodegradability [134,408].
Highly organized collagen scaffolds stabilized with juglone-functionalized AgNPs were evaluated as beneficial substrates for cellular adhesion and intercellular connection. The as-obtained nanostructured scaffolds exhibited significant antiproteolytic and proangiogenic ability and determined faster and enhanced wound healing [409]. Bergonzi et al. recently proposed 3D-printed scaffolds of alginate and nanocrystalline cellulose incorporated with nanosilver as highly absorbable and elastic macroporous scaffolds with considerable antibacterial effects for wound care applications [410]. AgNPs-impregnated BC/polydopamine scaffolds were proposed for the management of burn wounds, with complete healing being evidenced after 25 days. The nanocomposites facilitated necrotic tissue clearance, promoted collagen deposition and epidermis neoformation. The scaffolds also determined increased/decreased levels of anti-inflammatory/pro-inflammatory interleukins, respectively, and upregulation of growth factor genes involved in wound healing [411]. Highly antimicrobial electrospun PLA scaffolds modified with nanosilver and cellulose nanofibrils promoted the proliferation and normal growth of ocular epithelial cells, with no proinflammatory reaction. The hydrophilic scaffolds were recently proposed as effective ocular bandages [11]. AgNPs and lavender oil-induced synergistic antibacterial effects when incorporated within polyurethane (PU) nanofibrous scaffolds. The resulted hydrophilic nanocomposites encouraged improved proliferation and normal development of fibroblasts [412].
Diabetic wounds are moderate to severe chronic wounds which natural healing is generally disturbed by several disease-associated factors, such as glycemic levels and local hypoxia, peripheral vascular disease and neuropathy, compromised immunodeficiency and opportunistic infections [424]. The successful use of silver-based nanomaterials in wound therapy relies on their ability to be specifically modified and easily incorporated within dressing materials (which facilitates transportation, protection and control of therapeutic agents), respectively, on the improvement of skin remodeling through antioxidant, anti-inflammatory and proliferative properties [425,426]. Nanosilver has the advantage of better chemical stability and catalytic activity, thus being used as an intrinsic therapeutic agent. The limitation of using AgNPs in wound healing consists of their toxicity rate, but this aspect can be tuned by raising the surface-to-volume ratio and by different protective coatings [427]. Taking all into consideration, particular attention was straightened to the use of AgNPs in the management of diabetic wounds.
The mid-term use (three days) of AgNPs-incorporated chitin nanofiber sheet after wound bed cleansing with weakly acidic hypochlorous acid (pH 6.5) determined enhanced disinfection and significant healing efficiency in mice diabetic wounds infected with P. aeruginosa [428]. Hybrid hydrogels of thiolated CS and dextran grafted with maleic acid embedded with AgNPs were proposed as effective dressings for diabetic ulcers. The proposed antifouling hydrogel showed macroporous architecture and excellent water absorption ability while promoted and accelerated the healing process and modulated the host immune response by the local recruitment and activation of immune cells [429]. The slow and sustained release of metallic particles from CS/PEG hydrogels loaded with AgNPs proved beneficial implications on the prolonged antibacterial efficiency and accelerated healing of wounds in diabetic rabbits. The highly porous nature and increased swelling ability of composite hydrogel contributed to faster complete re-epithelialization (12.3 ± 0.8 days) and collagen deposition processes (34.4 ± 2.0 on day 12), while resulted in moderate granulation tissue and reduced inflammation. After 14 days of experimental treatment, blood vessels and nuclei formation were also noticed, an indication the angiogenic potential of nanosilver-embedded CS/PEG hydrogels [430].
8. Concluding Remarks
The genuine size-related physicochemical features, mechanical and optical properties and peculiar biological behavior (including nontoxicity, antimicrobial efficiency and biofunctional ability) represent fundamental characteristics that recommend silver nanoparticles (AgNPs) for the development of unconventional and effective biomedical applications. For such particular use, a real challenge for researchers is to properly tune the biocompatibility/antimicrobial activity balance as to maximize the desired therapeutic effects. Thanks to their impressive versatility, nanosilver-based biomaterials and biosystems are promising candidates for unconventional anti-infective therapy, specific and selective platforms for detection and diagnosis, targeted and controlled drug delivery and gene therapy, soft and tissue engineering and regenerative medicine.
Author Contributions
O.G., R.A.P., A.C.B., A.-C.B. and A.M.G. designed and wrote the paper. All authors have read and agreed to the published version of the manuscript.
Funding
R.A.P. acknowledges the financial support from Operational Programme Human Capital of the Ministry of European Funds through the Financial Agreement 51668/09.07.2019, SMIS code 124705.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Feldman D. Polymer nanocomposites for tissue engineering, antimicrobials and drug delivery. Biointerface Res. Appl. Chem. 2018;8:3153–3160. [Google Scholar]
- 2.Patra J.K., Das G., Fraceto L.F., Campos E.V.R., Rodriguez-Torres M.D.P., Acosta-Torres L.S., Diaz-Torres L.A., Grillo R., Swamy M.K., Sharma S., et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018;16:71. doi: 10.1186/s12951-018-0392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kang T., Kim Y.G., Kim D., Hyeon T. Inorganic nanoparticles with enzyme-mimetic activities for biomedical applications. Coord. Chem. Rev. 2020;403:213092. doi: 10.1016/j.ccr.2019.213092. [DOI] [Google Scholar]
- 4.Sanchez-Lopez E., Gomes D., Esteruelas G., Bonilla L., Lopez-Machado A.L., Galindo R., Cano A., Espina M., Ettcheto M., Camins A., et al. Metal-Based Nanoparticles as Antimicrobial Agents: An Overview. Nanomaterials. 2020;10:292. doi: 10.3390/nano10020292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keshvadi M., Karimi F., Valizadeh S., Valizadeh A. Comparative study of antibacterial inhibitory effect of silver nanoparticles and garlic oil nanoemulsion with their combination. Biointerface Res. Appl. Chem. 2019:9. doi: 10.33263/BRIAC96.560566. [DOI] [Google Scholar]
- 6.Gaafar M., El-Zawawy L., El-Temsahy M., Shalaby T.I., Hassan A. Silver nanoparticles as a therapeutic agent in experimental cyclosporiasis. Exp. Parasitol. 2019;207:107772. doi: 10.1016/j.exppara.2019.107772. [DOI] [PubMed] [Google Scholar]
- 7.Iqbal S., Fakhar-e-Alam M., Akbar F., Shafiq M., Atif M., Amin N., Ismail M., Hanif A., Farooq W.A. Application of silver oxide nanoparticles for the treatment of cancer. J. Mol. Struct. 2019;1189:203–209. [Google Scholar]
- 8.Akter M., Sikder M.T., Rahman M.M., Ullah A.A., Hossain K.F.B., Banik S., Hosokawa T., Saito T., Kurasaki M. A systematic review on silver nanoparticles-induced cytotoxicity: Physicochemical properties and perspectives. J. Adv. Res. 2018;9:1–16. doi: 10.1016/j.jare.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bayda S., Adeel M., Tuccinardi T., Cordani M., Rizzolio F. The History of Nanoscience and Nanotechnology: From Chemical-Physical Applications to Nanomedicine. Molecules. 2019;25:112. doi: 10.3390/molecules25010112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amarnath Praphakar R., Jeyaraj M., Ahmed M., Suresh Kumar S., Rajan M. Silver nanoparticle functionalized CS-g-(CA-MA-PZA) carrier for sustainable anti-tuberculosis drug delivery. Int. J. Biol. Macromol. 2018;118:1627–1638. doi: 10.1016/j.ijbiomac.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Yan D., Yao Q., Yu F., Chen L., Zhang S., Sun H., Lin J., Fu Y. Surface modified electrospun poly(lactic acid) fibrous scaffold with cellulose nanofibrils and Ag nanoparticles for ocular cell proliferation and antimicrobial application. Mater. Sci. Eng. C Mater. Biol. Appl. 2020;111:110767. doi: 10.1016/j.msec.2020.110767. [DOI] [PubMed] [Google Scholar]
- 12.Ma Y., Shi L., Liu F., Zhang Y., Pang Y., Shen X. Self-assembled thixotropic silver cluster hydrogel for anticancer drug release. Chem. Eng. J. 2019;362:650–657. doi: 10.1016/j.cej.2019.01.096. [DOI] [Google Scholar]
- 13.Kraeling M.E.K., Topping V.D., Keltner Z.M., Belgrave K.R., Bailey K.D., Gao X., Yourick J.J. In vitro percutaneous penetration of silver nanoparticles in pig and human skin. Regul. Toxicol. Pharmacol. 2018;95:314–322. doi: 10.1016/j.yrtph.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Odeniyi M.A., Okumah V.C., Adebayo-Tayo B.C., Odeniyi O.A. Green synthesis and cream formulations of silver nanoparticles of Nauclea latifolia (African peach) fruit extracts and evaluation of antimicrobial and antioxidant activities. Sustain. Chem. Pharm. 2020;15:100197. doi: 10.1016/j.scp.2019.100197. [DOI] [Google Scholar]
- 15.Mandakhalikar K.D., Wang R., Rahmat J.N., Chiong E., Neoh K.G., Tambyah P.A. Restriction of in vivo infection by antifouling coating on urinary catheter with controllable and sustained silver release: A proof of concept study. BMC Infect. Dis. 2018;18:370. doi: 10.1186/s12879-018-3296-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gherasim O., Grumezescu A.M., Grumezescu V., Iordache F., Vasile B.S., Holban A.M. Bioactive Surfaces of Polylactide and Silver Nanoparticles for the Prevention of Microbial Contamination. Materials. 2020;13:768. doi: 10.3390/ma13030768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fadlilah D.R., Endarko E., Ratnasari A., Hozairi H., Yusop Z., Syafiuddin A. Enhancement of antibacterial properties of various polymers functionalized with silver nanoparticles. Biointerface Res. Appl. Chem. 2019;10:5592–5598. doi: 10.33263/briac0103.592598. [DOI] [Google Scholar]
- 18.Erring M., Gaba S., Mohsina S., Tripathy S., Sharma R.K. Comparison of efficacy of silver-nanoparticle gel, nano-silver-foam and collagen dressings in treatment of partial thickness burn wounds. Burns. 2019;45:1888–1894. doi: 10.1016/j.burns.2019.07.019. [DOI] [PubMed] [Google Scholar]
- 19.Zhou Y., Tang R.C. Facile and eco-friendly fabrication of AgNPs coated silk for antibacterial and antioxidant textiles using honeysuckle extract. J. Photochem. Photobiol. B Biol. 2018;178:463–471. doi: 10.1016/j.jphotobiol.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 20.Fajar M.N., Endarko E., Rubiyanto A., Malek N.A.N.N., Hadibarata T., Syafiuddin A. A green deposition method of silver nanoparticles on textiles and their antifungal activity. Biointerface Res. Appl. Chem. 2019;10:4902–4907. doi: 10.33263/briac101.902907. [DOI] [Google Scholar]
- 21.Narasaiah B.P., Mandal B.K., Chakravarthula S.N. Mitigation of textile industries generated pollution by agro-waste cotton peels mediated synthesized silver nanoparticles. Biointerface Res. Appl. Chem. 2018;8:3602–3610. [Google Scholar]
- 22.Amini E., Azadfallah M. In situ synthesis of silver nanoparticles on fiber matrix for preparing antibacterial paper. Biointerface Res. Appl. Chem. 2018;8:3449–3456. [Google Scholar]
- 23.Kumar S., Shukla A., Baul P.P., Mitra A., Halder D. Biodegradable hybrid nanocomposites of chitosan/gelatin and silver nanoparticles for active food packaging applications. Food Packag. Shelf Life. 2018;16:178–184. doi: 10.1016/j.fpsl.2018.03.008. [DOI] [Google Scholar]
- 24.Lazić V., Vivod V., Peršin Z., Stoiljković M., Ratnayake I.S., Ahrenkiel P.S., Nedeljković J.M., Kokol V. Dextran-coated silver nanoparticles for improved barrier and controlled antimicrobial properties of nanocellulose films used in food packaging. Food Packag. Shelf Life. 2020;26:100575. doi: 10.1016/j.fpsl.2020.100575. [DOI] [Google Scholar]
- 25.Mishra M.P., Padhy R.N. Antibacterial activity of green silver nanoparticles synthesized from Anogeissus acuminata against multidrug resistant urinary tract infecting bacteria in vitro and host-toxicity testing. J. Appl. Biomed. 2018;16:120–125. doi: 10.1016/j.jab.2017.11.003. [DOI] [Google Scholar]
- 26.Liao S., Zhang Y., Pan X., Zhu F., Jiang C., Liu Q., Cheng Z., Dai G., Wu G., Wang L., et al. Antibacterial activity and mechanism of silver nanoparticles against multidrug-resistant Pseudomonas aeruginosa. Int. J. Nanomed. 2019;14:1469–1487. doi: 10.2147/IJN.S191340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Samoilova N.A., Krayukhina M.A., Popov D.A., Anuchina N.M., Piskarev V.E. 3′-sialyllactose-decorated silver nanoparticles: Lectin binding and bactericidal properties. Biointerface Res. Appl. Chem. 2018;8:3095–3099. [Google Scholar]
- 28.Lampe I., Beke D., Biri S., Csarnovics I., Csik A., Dombradi Z., Hajdu P., Hegedus V., Racz R., Varga I., et al. Investigation of silver nanoparticles on titanium surface created by ion implantation technology. Int. J. Nanomed. 2019;14:4709–4721. doi: 10.2147/IJN.S197782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rafique M., Rafique M.S., Kalsoom U., Afzal A., Butt S.H., Usman A. Laser ablation synthesis of silver nanoparticles in water and dependence on laser nature. Opt. Quantum Electron. 2019:51. doi: 10.1007/s11082-019-1902-0. [DOI] [Google Scholar]
- 30.Han H.J., Yu T., Kim W.S., Im S.H. Highly reproducible polyol synthesis for silver nanocubes. J. Cryst. Growth. 2017;469:48–53. doi: 10.1016/j.jcrysgro.2016.09.038. [DOI] [Google Scholar]
- 31.Kuntyi О.І., Kytsya А.R., Mertsalo I.P., Mazur А.S., Zozula G.І., Bazylyak L.I., Тopchak R.V. Electrochemical synthesis of silver nanoparticles by reversible current in solutions of sodium polyacrylate. Colloid Polym. Sci. 2019;297:689–695. doi: 10.1007/s00396-019-04488-4. [DOI] [Google Scholar]
- 32.Ali G.W., Abd El-Moez S.H., Abdel-Fattah W.A. Synthesis and characterization of nontoxic silver nano-particles with preferential bactericidal activity. Biointerface Res. Appl. Chem. 2019;9:4617–4623. doi: 10.33263/briac96.617623. [DOI] [Google Scholar]
- 33.Ahmad M.A., Salmiati S., Marpongahtun M., Salim M.R., Lolo J.A., Syafiuddin A. Green Synthesis of Silver Nanoparticles Using Muntingia calabura Leaf Extract and Evaluation of Antibacterial Activities. Biointerface Res. Appl. Chem. 2020;10:6253–6261. doi: 10.33263/briac105.62536261. [DOI] [Google Scholar]
- 34.Gupta R.K., Kumar V., Gundampati R.K., Malviya M., Hasan S.H., Jagannadham M.V. Biosynthesis of silver nanoparticles from the novel strain of Streptomyces Sp. BHUMBU-80 with highly efficient electroanalytical detection of hydrogen peroxide and antibacterial activity. J. Environ. Chem. Eng. 2017;5:5624–5635. doi: 10.1016/j.jece.2017.09.029. [DOI] [Google Scholar]
- 35.Shahzad A., Saeed H., Iqtedar M., Hussain S.Z., Kaleem A., Abdullah R., Sharif S., Naz S., Saleem F., Aihetasham A., et al. Size-Controlled Production of Silver Nanoparticles by Aspergillus fumigatus BTCB10: Likely Antibacterial and Cytotoxic Effects. J. Nanomater. 2019;2019:5168698. doi: 10.1155/2019/5168698. [DOI] [Google Scholar]
- 36.Mohler J.S., Sim W., Blaskovich M.A.T., Cooper M.A., Ziora Z.M. Silver bullets: A new lustre on an old antimicrobial agent. Biotechnol. Adv. 2018;36:1391–1411. doi: 10.1016/j.biotechadv.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 37.Deshmukh S., Patil S., Mullani S., Delekar S. Silver nanoparticles as an effective disinfectant: A review. Mater. Sci. Eng. C. 2019;97:954–965. doi: 10.1016/j.msec.2018.12.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sharma N., Phutela K., Goel A., Soni S., Batra N. Exploring the bacterial based silver nanoparticle for their possible application as disinfectants. Biointerface Res. Appl. Chem. 2018;8:3100–3104. [Google Scholar]
- 39.Montano E., Vivo M., Guarino A.M., di Martino O., Di Luccia B., Calabro V., Caserta S., Pollice A. Colloidal Silver Induces Cytoskeleton Reorganization and E-Cadherin Recruitment at Cell-Cell Contacts in HaCaT Cells. Pharmaceuticals. 2019;12:72. doi: 10.3390/ph12020072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cooper R.J., Menking-Colby M.N., Humphrey K.A., Victory J.H., Kipps D.W., Spitzer N. Involvement of β-catenin in cytoskeleton disruption following adult neural stem cell exposure to low-level silver nanoparticles. Neurotoxicology. 2019;71:102–112. doi: 10.1016/j.neuro.2018.12.010. [DOI] [PubMed] [Google Scholar]
- 41.Gurunathan S., Qasim M., Park C., Yoo H., Kim J.H., Hong K. Cytotoxic Potential and Molecular Pathway Analysis of Silver Nanoparticles in Human Colon Cancer Cells HCT116. Int. J. Mol. Sci. 2018;19:2269. doi: 10.3390/ijms19082269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yadav A., Mendhulkar V.D. Antiproliferative activity of Camellia sinensis mediated silver nanoparticles on three different human cancer cell lines. J. Cancer Res. Ther. 2018;14:1316. doi: 10.4103/jcrt.JCRT_575_16. [DOI] [PubMed] [Google Scholar]
- 43.Mei L., Xu Z., Shi Y., Lin C., Jiao S., Zhang L., Li P. Multivalent and synergistic chitosan oligosaccharide-Ag nanocomposites for therapy of bacterial infection. Sci. Rep. 2020;10:10011. doi: 10.1038/s41598-020-67139-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tortella G.R., Rubilar O., Duran N., Diez M.C., Martinez M., Parada J., Seabra A.B. Silver nanoparticles: Toxicity in model organisms as an overview of its hazard for human health and the environment. J. Hazard. Mater. 2020;390:121974. doi: 10.1016/j.jhazmat.2019.121974. [DOI] [PubMed] [Google Scholar]
- 45.Selvakumar P., Sithara R., Viveka K., Sivashanmugam P. Green synthesis of silver nanoparticles using leaf extract of Acalypha hispida and its application in blood compatibility. J. Photochem. Photobiol. B Biol. 2018;182:52–61. doi: 10.1016/j.jphotobiol.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 46.Jayeoye T.J., Nwabor O.F., Rujiralai T. Synthesis of highly stable and dispersed silver nanoparticles/poly(vinyl alcohol-co-ethylene glycol)/poly(3-aminophenyl boronic acid) nanocomposite: Characterization and antibacterial, hemolytic and cytotoxicity studies. J. Ind. Eng. Chem. 2020;89:288–300. doi: 10.1016/j.jiec.2020.05.025. [DOI] [Google Scholar]
- 47.Asghar M.A., Yousuf R.I., Shoaib M.H., Asghar M.A. Antibacterial, anticoagulant and cytotoxic evaluation of biocompatible nanocomposite of chitosan loaded green synthesized bioinspired silver nanoparticles. Int. J. Biol. Macromol. 2020;160:934–943. doi: 10.1016/j.ijbiomac.2020.05.197. [DOI] [PubMed] [Google Scholar]
- 48.Park J., Lim D.H., Lim H.J., Kwon T., Choi J.S., Jeong S., Choi I.H., Cheon J. Size dependent macrophage responses and toxicological effects of Ag nanoparticles. Chem. Commun. 2011;47:4382–4384. doi: 10.1039/c1cc10357a. [DOI] [PubMed] [Google Scholar]
- 49.Dalzon B., Torres A., Diemer H., Ravanel S., Collin-Faure V., Pernet-Gallay K., Jouneau P.H., Bourguignon J., Cianférani S., Carrière M., et al. How reversible are the effects of silver nanoparticles on macrophages? A proteomic-instructed view. Environ. Sci. Nano. 2019;6:3133–3157. doi: 10.1039/c9en00408d. [DOI] [Google Scholar]
- 50.Gupta K., Chhibber S. Biofunctionalization of Silver Nanoparticles With Lactonase Leads to Altered Antimicrobial and Cytotoxic Properties. Front. Mol. Biosci. 2019;6:63. doi: 10.3389/fmolb.2019.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vazquez-Muñoz R., Borrego B., Juárez-Moreno K., García-García M., Morales J.D.M., Bogdanchikova N., Huerta-Saquero A. Toxicity of silver nanoparticles in biological systems: Does the complexity of biological systems matter? Toxicol. Lett. 2017;276:11–20. doi: 10.1016/j.toxlet.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 52.Pavicic I., Milic M., Pongrac I.M., Brkic Ahmed L., Matijevic Glavan T., Ilic K., Zapletal E., Curlin M., Mitrecic D., Vinkovic Vrcek I. Neurotoxicity of silver nanoparticles stabilized with different coating agents: In vitro response of neuronal precursor cells. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2020;136:110935. doi: 10.1016/j.fct.2019.110935. [DOI] [PubMed] [Google Scholar]
- 53.Zhang B., Liu N., Liu Q.S., Zhang J., Zhou Q., Jiang G. Silver nanoparticles induce size-dependent and particle-specific neurotoxicity to primary cultures of rat cerebral cortical neurons. Ecotoxicol. Environ. Saf. 2020;198:110674. doi: 10.1016/j.ecoenv.2020.110674. [DOI] [PubMed] [Google Scholar]
- 54.Khan I., Bahuguna A., Krishnan M., Shukla S., Lee H., Min S.H., Choi D.K., Cho Y., Bajpai V.K., Huh Y.S., et al. The effect of biogenic manufactured silver nanoparticles on human endothelial cells and zebrafish model. Sci. Total Environ. 2019;679:365–377. doi: 10.1016/j.scitotenv.2019.05.045. [DOI] [PubMed] [Google Scholar]
- 55.Jalilian F., Chahardoli A., Sadrjavadi K., Fattahi A., Shokoohinia Y. Green synthesized silver nanoparticle from Allium ampeloprasum aqueous extract: Characterization, antioxidant activities, antibacterial and cytotoxicity effects. Adv. Powder Technol. 2020;31:1323–1332. [Google Scholar]
- 56.Pittol M., Tomacheski D., Simões D.N., Ribeiro V.F., Santana R.M.C. Evaluation of the Toxicity of Silver/Silica and Titanium Dioxide Particles in Mammalian Cells. Braz. Arch. Biol. Technol. 2018;61 doi: 10.1590/1678-4324-2018160667. [DOI] [Google Scholar]
- 57.Verkhovskii R., Kozlova A., Atkin V., Kamyshinsky R., Shulgina T., Nechaeva O. Physical properties and cytotoxicity of silver nanoparticles under different polymeric stabilizers. Heliyon. 2019;5:e01305. doi: 10.1016/j.heliyon.2019.e01305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Subramanian P., Ravichandran A., Manoharan V., Muthukaruppan R., Somasundaram S., Pandi B., Krishnan A., Marimuthu P.N., Somasundaram S.S.N., You S. Synthesis of Oldenlandia umbellata stabilized silver nanoparticles and their antioxidant effect, antibacterial activity, and bio-compatibility using human lung fibroblast cell line WI-38. Process Biochem. 2019;86:196–204. doi: 10.1016/j.procbio.2019.08.002. [DOI] [Google Scholar]
- 59.Lyu Y., Yu M., Liu Q., Zhang Q., Liu Z., Tian Y., Li D., Changdao M. Synthesis of silver nanoparticles using oxidized amylose and combination with curcumin for enhanced antibacterial activity. Carbohydr. Polym. 2020;230:115573. doi: 10.1016/j.carbpol.2019.115573. [DOI] [PubMed] [Google Scholar]
- 60.Ge M., Li J., Song S., Meng N., Zhou N. Development and antibacterial performance of silver nanoparticles-lecithin modified montmorillonite nanoparticle hybrid. Appl. Clay Sci. 2019;183:105334. doi: 10.1016/j.clay.2019.105334. [DOI] [Google Scholar]
- 61.Roy A., Joshi M., Butola B.S., Ghosh S. Evaluation of biological and cytocompatible properties in nano silver-clay based polyethylene nanocomposites. J. Hazard. Mater. 2020;384:121309. doi: 10.1016/j.jhazmat.2019.121309. [DOI] [PubMed] [Google Scholar]
- 62.Pinzaru I., Coricovac D., Dehelean C., Moacă E.A., Mioc M., Baderca F., Sizemore I., Brittle S., Marti D., Calina C.D., et al. Stable PEG-coated silver nanoparticles—A comprehensive toxicological profile. Food Chem. Toxicol. 2018;111:546–556. doi: 10.1016/j.fct.2017.11.051. [DOI] [PubMed] [Google Scholar]
- 63.Graf C., Nordmeyer D., Sengstock C., Ahlberg S., Diendorf J., Raabe J., Epple M., Köller M., Lademann J., Vogt A., et al. Shape-Dependent Dissolution and Cellular Uptake of Silver Nanoparticles. Langmuir. 2018;34:1506–1519. doi: 10.1021/acs.langmuir.7b03126. [DOI] [PubMed] [Google Scholar]
- 64.Guilger-Casagrande M., Germano-Costa T., Pasquoto-Stigliani T., Fraceto L.F., Lima R.d. Biosynthesis of silver nanoparticles employing Trichoderma harzianum with enzymatic stimulation for the control of Sclerotinia sclerotiorum. Sci. Rep. 2019:9. doi: 10.1038/s41598-019-50871-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Khalil N.M., Abd El-Ghany M.N., Rodríguez-Couto S. Antifungal and anti-mycotoxin efficacy of biogenic silver nanoparticles produced by Fusarium chlamydosporum and Penicillium chrysogenum at non-cytotoxic doses. Chemosphere. 2019;218:477–486. doi: 10.1016/j.chemosphere.2018.11.129. [DOI] [PubMed] [Google Scholar]
- 66.Huy T.Q., Thanh N.T.H., Thuy N.T., Van Chung P., Hung P.N., Le A.T., Hanh N.T.H. Cytotoxicity and antiviral activity of electrochemical–synthesized silver nanoparticles against poliovirus. J. Virol. Methods. 2017;241:52–57. doi: 10.1016/j.jviromet.2016.12.015. [DOI] [PubMed] [Google Scholar]
- 67.Ferdous Z., Al-Salam S., Greish Y.E., Ali B.H., Nemmar A. Pulmonary exposure to silver nanoparticles impairs cardiovascular homeostasis: Effects of coating, dose and time. Toxicol. Appl. Pharmacol. 2019;367:36–50. doi: 10.1016/j.taap.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 68.Ontong J.C., Paosen S., Shankar S., Voravuthikunchai S.P. Eco-friendly synthesis of silver nanoparticles using Senna alata bark extract and its antimicrobial mechanism through enhancement of bacterial membrane degradation. J. Microbiol. Methods. 2019;165:105692. doi: 10.1016/j.mimet.2019.105692. [DOI] [PubMed] [Google Scholar]
- 69.Hussein J., El-Naggar M.E., Fouda M.M.G., Morsy O.M., Ajarem J.S., Almalki A.M., Allam A.A., Mekawi E.M. The efficiency of blackberry loaded AgNPs, AuNPs and Ag@AuNPs mediated pectin in the treatment of cisplatin-induced cardiotoxicity in experimental rats. Int. J. Biol. Macromol. 2020;159:1084–1093. doi: 10.1016/j.ijbiomac.2020.05.115. [DOI] [PubMed] [Google Scholar]
- 70.Fahimirad S., Ajalloueian F., Ghorbanpour M. Synthesis and therapeutic potential of silver nanomaterials derived from plant extracts. Ecotoxicol. Environ. Saf. 2019;168:260–278. doi: 10.1016/j.ecoenv.2018.10.017. [DOI] [PubMed] [Google Scholar]
- 71.Perde-Schrepler M., Florea A., Brie I., Virag P., Fischer-Fodor E., Vâlcan A., Gurzău E., Lisencu C., Maniu A. Size-Dependent Cytotoxicity and Genotoxicity of Silver Nanoparticles in Cochlear Cells In Vitro. J. Nanomater. 2019;2019:6090259. doi: 10.1155/2019/6090259. [DOI] [Google Scholar]
- 72.Kumar V., Sharma N., Maitra S.S. In vitro and in vivo toxicity assessment of nanoparticles. Int. Nano Lett. 2017;7:243–256. doi: 10.1007/s40089-017-0221-3. [DOI] [Google Scholar]
- 73.Flores-López L.Z., Espinoza-Gómez H., Somanathan R. Silver nanoparticles: Electron transfer, reactive oxygen species, oxidative stress, beneficial and toxicological effects. Mini review. J. Appl. Toxicol. 2019;39:16–26. doi: 10.1002/jat.3654. [DOI] [PubMed] [Google Scholar]
- 74.Wu F., Harper B.J., Harper S.L. Differential dissolution and toxicity of surface functionalized silver nanoparticles in small-scale microcosms: Impacts of community complexity. Environ. Sci. Nano. 2017;4:359–372. [Google Scholar]
- 75.Heshmati M., Arbabi Bidgoli S., Khoei S., Mahmoudzadeh A., Sorkhabadi S.M.R. Cytotoxicity and genotoxicity of silver nanoparticles in Chinese Hamster ovary cell line (CHO-K1) cells. Nucleus. 2019;62:221–225. doi: 10.1007/s13237-019-00295-y. [DOI] [Google Scholar]
- 76.Tang J., Chen B., Cai E., Liu W., Jiang J., Chen F., Shan X., Zhang H. Mechanisms of silver nanoparticles-induced cytotoxicity and apoptosis in rat tracheal epithelial cells. J. Toxicol. Sci. 2019;44:155–165. doi: 10.2131/jts.44.155. [DOI] [PubMed] [Google Scholar]
- 77.Xue Y., Wang J., Huang Y., Gao X., Kong L., Zhang T., Tang M. Comparative cytotoxicity and apoptotic pathways induced by nanosilver in human liver HepG2 and L02 cells. Hum. Exp. Toxicol. 2018;37:1293–1309. doi: 10.1177/0960327118769718. [DOI] [PubMed] [Google Scholar]
- 78.Plackal Adimuriyil George B., Kumar N., Abrahamse H., Ray S.S. Apoptotic efficacy of multifaceted biosynthesized silver nanoparticles on human adenocarcinoma cells. Sci. Rep. 2018:8. doi: 10.1038/s41598-018-32480-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hu B., Yin N., Yang R., Liang S., Liang S., Faiola F. Silver nanoparticles (AgNPs) and AgNO3 perturb the specification of human hepatocyte-like cells and cardiomyocytes. Sci. Total Environ. 2020;725:138433. doi: 10.1016/j.scitotenv.2020.138433. [DOI] [PubMed] [Google Scholar]
- 80.Jarrar Y., Al-Doaiss A., Alfaifi M., Shati A., Al-Kahtani M., Jarrar B. The influence of five metallic nanoparticles on the expression of major drug-metabolizing enzyme genes with correlation of inflammation in mouse livers. Environ. Toxicol. Pharmacol. 2020;80:103449. doi: 10.1016/j.etap.2020.103449. [DOI] [PubMed] [Google Scholar]
- 81.David L., Moldovan B., Baldea I., Olteanu D., Bolfa P., Clichici S., Filip G.A. Modulatory effects of Cornus sanguinea L. mediated green synthesized silver nanoparticles on oxidative stress, COX-2/NOS2 and NFkB/pNFkB expressions in experimental inflammation in Wistar rats. Mater. Sci. Eng. C. 2020;110:110709. doi: 10.1016/j.msec.2020.110709. [DOI] [PubMed] [Google Scholar]
- 82.Elsharawy K., Abou-Dobara M., El-Gammal H., Hyder A. Chitosan coating does not prevent the effect of the transfer of green silver nanoparticles biosynthesized by Streptomyces malachitus into fetuses via the placenta. Reprod. Biol. 2020;20:97–105. doi: 10.1016/j.repbio.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 83.Auclair J., Turcotte P., Gagnon C., Peyrot C., Wilkinson K.J., Gagné F. The influence of surface coatings on the toxicity of silver nanoparticle in rainbow trout. Comp. Biochem. Physiol. Part C Toxicol. Pharmacol. 2019;226:108623. doi: 10.1016/j.cbpc.2019.108623. [DOI] [PubMed] [Google Scholar]
- 84.Zelikin A.N., Zucker R.M., Ortenzio J., Degn L.L., Lerner J.M., Boyes W.K. Biophysical comparison of four silver nanoparticles coatings using microscopy, hyperspectral imaging and flow cytometry. PLoS ONE. 2019;14:e0219078. doi: 10.1371/journal.pone.0219078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Docea A.O., Calina D., Buga A.M., Zlatian O., Paoliello M.M.B., Mogosanu G.D., Streba C.T., Popescu E.L., Stoica A.E., Bîrcă A.C., et al. The Effect of Silver Nanoparticles on Antioxidant/Pro-Oxidant Balance in a Murine Model. Int. J. Mol. Sci. 2020;21:1233. doi: 10.3390/ijms21041233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Takamiya A.S., Monteiro D.R., Gorup L.F., Silva E.A., de Camargo E.R., Gomes-Filho J.E., de Oliveira S.H.P., Barbosa D.B. Biocompatible silver nanoparticles incorporated in acrylic resin for dental application inhibit Candida albicans biofilm. Mater. Sci. Eng. C. 2021;118:111341. doi: 10.1016/j.msec.2020.111341. [DOI] [PubMed] [Google Scholar]
- 87.Kern W.V., Rieg S. Burden of bacterial bloodstream infection—A brief update on epidemiology and significance of multidrug-resistant pathogens. Clin. Microbiol. Infect. 2020;26:151–157. doi: 10.1016/j.cmi.2019.10.031. [DOI] [PubMed] [Google Scholar]
- 88.Saldana C.S., Vyas D.A., Wurcel A.G. Soft Tissue, Bone, and Joint Infections in People Who Inject Drugs. Infect. Dis. Clin. N. Am. 2020;34:495–509. doi: 10.1016/j.idc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Koulenti D., Song A., Ellingboe A., Abdul-Aziz M.H., Harris P., Gavey E., Lipman J. Infections by multidrug-resistant Gram-negative Bacteria: What’s new in our arsenal and what’s in the pipeline? Int. J. Antimicrob. Agents. 2019;53:211–224. doi: 10.1016/j.ijantimicag.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 90.Escolà-Vergé L., Los-Arcos I., Almirante B. New antibiotics for the treatment of infections by multidrug-resistant microorganisms. Med. Clínica. 2020;154:351–357. doi: 10.1016/j.medcle.2019.11.005. [DOI] [PubMed] [Google Scholar]
- 91.Shahriari S., Monajjemi M., Zare K. Penetrating to cell membrane bacteria by the efficiency of various antibiotics (clindamycin, metronidazole, azithromycin, sulfamethoxazole, baxdela, ticarcillin, and clavulanic acid) using S-NICS theory. Biointerface Res. Appl. Chem. 2018;8:3219–3223. [Google Scholar]
- 92.Pazos-Ortiz E., Roque-Ruiz J.H., Hinojos-Márquez E.A., López-Esparza J., Donohué-Cornejo A., Cuevas-González J.C., Espinosa-Cristóbal L.F., Reyes-López S.Y. Dose-dependent antimicrobial activity of silver nanoparticles on polycaprolactone fibers against gram-positive and gram-negative bacteria. J. Nanomater. 2017;2017:4752314. [Google Scholar]
- 93.Chen K., Wang F., Liu S., Wu X., Xu L., Zhang D. In situ reduction of silver nanoparticles by sodium alginate to obtain silver-loaded composite wound dressing with enhanced mechanical and antimicrobial property. Int. J. Biol. Macromol. 2020;148:501–509. doi: 10.1016/j.ijbiomac.2020.01.156. [DOI] [PubMed] [Google Scholar]
- 94.Shaaban M., Elgaml A., Habib E.E. Biotechnological applications of quorum sensing inhibition as novel therapeutic strategies for multidrug resistant pathogens. Microb. Pathog. 2019;127:138–143. doi: 10.1016/j.micpath.2018.11.043. [DOI] [PubMed] [Google Scholar]
- 95.Sim W., Barnard R.T., Blaskovich M.A.T., Ziora Z.M. Antimicrobial Silver in Medicinal and Consumer Applications: A Patent Review of the Past Decade (2007(-)2017) Antibiotics. 2018;7:93. doi: 10.3390/antibiotics7040093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hadrup N., Sharma A.K., Loeschner K., Jacobsen N.R. Pulmonary toxicity of silver vapours, nanoparticles and fine dusts: A review. Regul. Toxicol. Pharmacol. 2020;115:104690. doi: 10.1016/j.yrtph.2020.104690. [DOI] [PubMed] [Google Scholar]
- 97.Ferdous Z., Nemmar A. Health Impact of Silver Nanoparticles: A Review of the Biodistribution and Toxicity Following Various Routes of Exposure. Int. J. Mol. Sci. 2020;21:2375. doi: 10.3390/ijms21072375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kubo A.L., Capjak I., Vrcek I.V., Bondarenko O.M., Kurvet I., Vija H., Ivask A., Kasemets K., Kahru A. Antimicrobial potency of differently coated 10 and 50 nm silver nanoparticles against clinically relevant bacteria Escherichia coli and Staphylococcus aureus. Colloids Surf. B Biointerfaces. 2018;170:401–410. doi: 10.1016/j.colsurfb.2018.06.027. [DOI] [PubMed] [Google Scholar]
- 99.Huang X., Bao X., Liu Y., Wang Z., Hu Q. Catechol-Functional Chitosan/Silver Nanoparticle Composite as a Highly Effective Antibacterial Agent with Species-Specific Mechanisms. Sci. Rep. 2017;7:1860. doi: 10.1038/s41598-017-02008-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Behravan M., Panahi A.H., Naghizadeh A., Ziaee M., Mahdavi R., Mirzapour A. Facile green synthesis of silver nanoparticles using Berberis vulgaris leaf and root aqueous extract and its antibacterial activity. Int. J. Biol. Macromol. 2019;124:148–154. doi: 10.1016/j.ijbiomac.2018.11.101. [DOI] [PubMed] [Google Scholar]
- 101.Li W.R., Sun T.L., Zhou S.L., Ma Y.K., Shi Q.S., Xie X.B., Huang X.M. A comparative analysis of antibacterial activity, dynamics, and effects of silver ions and silver nanoparticles against four bacterial strains. Int. Biodeterior. Biodegrad. 2017;123:304–310. doi: 10.1016/j.ibiod.2017.07.015. [DOI] [Google Scholar]
- 102.Yuan Y.G., Peng Q.L., Gurunathan S. Effects of Silver Nanoparticles on Multiple Drug-Resistant Strains of Staphylococcus aureus and Pseudomonas aeruginosa from Mastitis-Infected Goats: An Alternative Approach for Antimicrobial Therapy. Int. J. Mol. Sci. 2017;18:569. doi: 10.3390/ijms18030569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chang B.M., Pan L., Lin H.H., Chang H.C. Nanodiamond-supported silver nanoparticles as potent and safe antibacterial agents. Sci. Rep. 2019;9:13164. doi: 10.1038/s41598-019-49675-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Quinteros M.A., Cano Aristizabal V., Dalmasso P.R., Paraje M.G., Paez P.L. Oxidative stress generation of silver nanoparticles in three bacterial genera and its relationship with the antimicrobial activity. Toxicol. Vitr. Int. J. Publ. Assoc. Bibra. 2016;36:216–223. doi: 10.1016/j.tiv.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 105.Quinteros M.A., Viviana C.A., Onnainty R., Mary V.S., Theumer M.G., Granero G.E., Paraje M.G., Paez P.L. Biosynthesized silver nanoparticles: Decoding their mechanism of action in Staphylococcus aureus and Escherichia coli. Int. J. Biochem. Cell Biol. 2018;104:87–93. doi: 10.1016/j.biocel.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 106.Rudakiya D.M., Pawar K. Bactericidal potential of silver nanoparticles synthesized using cell-free extract of Comamonas acidovorans: In vitro and in silico approaches. 3 Biotech. 2017;7:92. doi: 10.1007/s13205-017-0728-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tamiyakul H., Roytrakul S., Jaresitthikunchai J., Phaonakrop N., Tanasupawat S., Warisnoicharoen W. Changes in protein patterns of Staphylococcus aureus and Escherichia coli by silver nanoparticles capped with poly (4-styrenesulfonic acid-co-maleic acid) polymer. Asian Biomed. 2019;13:39–47. doi: 10.1515/abm-2019-0039. [DOI] [Google Scholar]
- 108.Roseli Salomoni P.L. The Battle Against Microbial Pathogens: Basic Science, Technological Advances and Educational Programs. 1st ed. Formatex Research Center; Badajos, Spain: 2015. Maria Filomena de Andrade Rodrigues. Antibacterial Activity of Silver Nanoparticles (AgNPs) in Staphylococcus aureus and Cytotoxicity in Mammalian Cells. [Google Scholar]
- 109.Kim D.H., Park J.C., Jeon G.E., Kim C.S., Seo J.H. Effect of the size and shape of silver nanoparticles on bacterial growth and metabolism by monitoring optical density and fluorescence intensity. Biotechnol. Bioprocess. Eng. 2017;22:210–217. doi: 10.1007/s12257-016-0641-3. [DOI] [Google Scholar]
- 110.Qasim M., Udomluck N., Chang J., Park H., Kim K. Antimicrobial activity of silver nanoparticles encapsulated in poly-N-isopropylacrylamide-based polymeric nanoparticles. Int. J. Nanomed. 2018;13:235–249. doi: 10.2147/IJN.S153485. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 111.Ji H., Zhou S., Fu Y., Wang Y., Mi J., Lu T., Wang X., Lu C. Size-controllable preparation and antibacterial mechanism of thermo-responsive copolymer-stabilized silver nanoparticles with high antimicrobial activity. Mater. Sci. Eng. C Mater. Biol. Appl. 2020;110:110735. doi: 10.1016/j.msec.2020.110735. [DOI] [PubMed] [Google Scholar]
- 112.Wu Y., Yang Y., Zhang Z., Wang Z., Zhao Y., Sun L. A facile method to prepare size-tunable silver nanoparticles and its antibacterial mechanism. Adv. Powder Technol. 2018;29:407–415. doi: 10.1016/j.apt.2017.11.028. [DOI] [Google Scholar]
- 113.Korshed P., Li L., Liu Z., Mironov A., Wang T. Size-dependent antibacterial activity for laser-generated silver nanoparticles. J. Interdiscip. Nanomed. 2019;4:24–33. doi: 10.1002/jin2.54. [DOI] [Google Scholar]
- 114.Ali S., Perveen S., Ali M., Jiao T., Sharma A.S., Hassan H., Devaraj S., Li H., Chen Q. Bioinspired morphology-controlled silver nanoparticles for antimicrobial application. Mater. Sci. Eng. C Mater. Biol. Appl. 2020;108:110421. doi: 10.1016/j.msec.2019.110421. [DOI] [PubMed] [Google Scholar]
- 115.Cheon J.Y., Kim S.J., Rhee Y.H., Kwon O.H., Park W.H. Shape-dependent antimicrobial activities of silver nanoparticles. Int. J. Nanomed. 2019;14:2773–2780. doi: 10.2147/IJN.S196472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kumari M., Pandey S., Giri V.P., Bhattacharya A., Shukla R., Mishra A., Nautiyal C.S. Tailoring shape and size of biogenic silver nanoparticles to enhance antimicrobial efficacy against MDR bacteria. Microb. Pathog. 2017;105:346–355. doi: 10.1016/j.micpath.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 117.Acharya D., Singha K.M., Pandey P., Mohanta B., Rajkumari J., Singha L.P. Shape dependent physical mutilation and lethal effects of silver nanoparticles on bacteria. Sci. Rep. 2018;8:201. doi: 10.1038/s41598-017-18590-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kora A.J., Sashidhar R. Biogenic silver nanoparticles synthesized with rhamnogalacturonan gum: Antibacterial activity, cytotoxicity and its mode of action. Arab. J. Chem. 2018;11:313–323. [Google Scholar]
- 119.Rahman A.U., Khan A.U., Yuan Q., Wei Y., Ahmad A., Ullah S., Khan Z.U.H., Shams S., Tariq M., Ahmad W. Tuber extract of Arisaema flavum eco-benignly and effectively synthesize silver nanoparticles: Photocatalytic and antibacterial response against multidrug resistant engineered E. coli QH4. J. Photochem. Photobiol. B Biol. 2019;193:31–38. doi: 10.1016/j.jphotobiol.2019.01.018. [DOI] [PubMed] [Google Scholar]
- 120.Rawat V., Sharma A., Bhatt V.P., Pratap Singh R., Maurya I.K. Sunlight mediated green synthesis of silver nanoparticles using Polygonatum graminifolium leaf extract and their antibacterial activity. Mater. Today Proc. 2020;29:911–916. doi: 10.1016/j.matpr.2020.05.274. [DOI] [Google Scholar]
- 121.Van Viet P., Sang T.T., Bich N.H.N., Thi C.M. An improved green synthesis method and Escherichia coli antibacterial activity of silver nanoparticles. J. Photochem. Photobiol. B Biol. 2018;182:108–114. doi: 10.1016/j.jphotobiol.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 122.Hileuskaya K., Ladutska A., Kulikouskaya V., Kraskouski A., Novik G., Kozerozhets I., Kozlovskiy A., Agabekov V. ‘Green’ approach for obtaining stable pectin-capped silver nanoparticles: Physico-chemical characterization and antibacterial activity. Colloids Surf. A Physicochem. Eng. Asp. 2020;585:124141. doi: 10.1016/j.colsurfa.2019.124141. [DOI] [Google Scholar]
- 123.Wongpreecha J., Polpanich D., Suteewong T., Kaewsaneha C., Tangboriboonrat P. One-pot, large-scale green synthesis of silver nanoparticles-chitosan with enhanced antibacterial activity and low cytotoxicity. Carbohydr. Polym. 2018;199:641–648. doi: 10.1016/j.carbpol.2018.07.039. [DOI] [PubMed] [Google Scholar]
- 124.Li R., Pan Y., Li N., Wang Q., Chen Y., Phisalaphong M., Chen H. Antibacterial and cytotoxic activities of a green synthesized silver nanoparticles using corn silk aqueous extract. Colloids Surf. A Physicochem. Eng. Asp. 2020;598:124827. doi: 10.1016/j.colsurfa.2020.124827. [DOI] [Google Scholar]
- 125.Das P., Ghosal K., Jana N.K., Mukherjee A., Basak P. Green synthesis and characterization of silver nanoparticles using belladonna mother tincture and its efficacy as a potential antibacterial and anti-inflammatory agent. Mater. Chem. Phys. 2019;228:310–317. doi: 10.1016/j.matchemphys.2019.02.064. [DOI] [Google Scholar]
- 126.Manukumar H.M., Yashwanth B., Umesha S., Venkateswara Rao J. Biocidal mechanism of green synthesized thyme loaded silver nanoparticles (GTAgNPs) against immune evading tricky methicillin-resistant Staphylococcus aureus 090 (MRSA090) at a homeostatic environment. Arab. J. Chem. 2020;13:1179–1197. doi: 10.1016/j.arabjc.2017.09.017. [DOI] [Google Scholar]
- 127.Alsamhary K.I. Eco-friendly synthesis of silver nanoparticles by Bacillus subtilis and their antibacterial activity. Saudi J. Biol. Sci. 2020;27:2185–2191. doi: 10.1016/j.sjbs.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Riaz Rajoka M.S., Mehwish H.M., Zhang H., Ashraf M., Fang H., Zeng X., Wu Y., Khurshid M., Zhao L., He Z. Antibacterial and antioxidant activity of exopolysaccharide mediated silver nanoparticle synthesized by Lactobacillus brevis isolated from Chinese koumiss. Colloids Surf. B Biointerfaces. 2020;186:110734. doi: 10.1016/j.colsurfb.2019.110734. [DOI] [PubMed] [Google Scholar]
- 129.Sabry N.M., Abdel-Gawad F.K., Bassem S.M., Nassar H.F., El-Taweel G.E., Okasha A., Ibrahim M. Interaction between nano silver and bacteria: Modeling approach. Biointerface Res. Appl. Chem. 2018;8:3570–3574. [Google Scholar]
- 130.Zheng K., Setyawati M.I., Leong D.T., Xie J. Antimicrobial silver nanomaterials. Coord. Chem. Rev. 2018;357:1–17. doi: 10.1016/j.ccr.2017.11.019. [DOI] [Google Scholar]
- 131.Chen J., Wang F., Liu Q., Du J. Antibacterial polymeric nanostructures for biomedical applications. Chem. Commun. 2014;50:14482–14493. doi: 10.1039/c4cc03001j. [DOI] [PubMed] [Google Scholar]
- 132.Mahjouri S., Movafeghi A., Divband B., Kosari-Nasab M., Kazemi E.M. Assessing the toxicity of silver nanoparticles in cell suspension culture of nicotiana tabacum. Biointerface Res. Appl. Chem. 2018;8:3252–3258. [Google Scholar]
- 133.Qing Y., Cheng L., Li R., Liu G., Zhang Y., Tang X., Wang J., Liu H., Qin Y. Potential antibacterial mechanism of silver nanoparticles and the optimization of orthopedic implants by advanced modification technologies. Int. J. Nanomed. 2018;13:3311–3327. doi: 10.2147/IJN.S165125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mihai M.M., Dima M.B., Dima B., Holban A.M. Nanomaterials for Wound Healing and Infection Control. Materials. 2019;12:2176. doi: 10.3390/ma12132176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ravichandran V., Vasanthi S., Shalini S., Shah S.A.A., Tripathy M., Paliwal N. Green synthesis, characterization, antibacterial, antioxidant and photocatalytic activity of Parkia speciosa leaves extract mediated silver nanoparticles. Results Phys. 2019;15:102565. doi: 10.1016/j.rinp.2019.102565. [DOI] [Google Scholar]
- 136.Ramesh A.V., Devi D.R., Battu G., Basavaiah K. A Facile plant mediated synthesis of silver nanoparticles using an aqueous leaf extract of Ficus hispida Linn. f. for catalytic, antioxidant and antibacterial applications. S. Afr. J. Chem. Eng. 2018;26:25–34. doi: 10.1016/j.sajce.2018.07.001. [DOI] [Google Scholar]
- 137.Swilam N., Nematallah K.A. Polyphenols profile of pomegranate leaves and their role in green synthesis of silver nanoparticles. Sci. Rep. 2020;10:14851. doi: 10.1038/s41598-020-71847-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Pallela P., Ummey S., Ruddaraju L.K., Pammi S.V.N., Yoon S.G. Ultra Small, mono dispersed green synthesized silver nanoparticles using aqueous extract of Sida cordifolia plant and investigation of antibacterial activity. Microb. Pathog. 2018;124:63–69. doi: 10.1016/j.micpath.2018.08.026. [DOI] [PubMed] [Google Scholar]
- 139.Anbu P., Gopinath S.C.B., Yun H.S., Lee C.G. Temperature-dependent green biosynthesis and characterization of silver nanoparticles using balloon flower plants and their antibacterial potential. J. Mol. Struct. 2019;1177:302–309. doi: 10.1016/j.molstruc.2018.09.075. [DOI] [Google Scholar]
- 140.Rafinska K., Pomastowski P., Buszewski B. Study of Bacillus subtilis response to different forms of silver. Sci. Total Environ. 2019;661:120–129. doi: 10.1016/j.scitotenv.2018.12.139. [DOI] [PubMed] [Google Scholar]
- 141.Ashraf A., Zafar S., Zahid K., Salahuddin Shah M., Al-Ghanim K.A., Al-Misned F., Mahboob S. Synthesis, characterization, and antibacterial potential of silver nanoparticles synthesized from Coriandrum sativum L. J. Infect. Public Health. 2019;12:275–281. doi: 10.1016/j.jiph.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 142.Keshari A.K., Srivastava R., Singh P., Yadav V.B., Nath G. Antioxidant and antibacterial activity of silver nanoparticles synthesized by Cestrum nocturnum. J. Ayurveda Integr. Med. 2020;11:37–44. doi: 10.1016/j.jaim.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Halkai K.R., Mudda J.A., Shivanna V., Rathod V., Halkai R. Evaluation of Antibacterial Efficacy of Fungal-Derived Silver Nanoparticles against Enterococcus faecalis. Contemp. Clin. Dent. 2018;9:45–48. doi: 10.4103/ccd.ccd_703_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Halkai K.R., Mudda J.A., Shivanna V., Rathod V., Halkai R. Antibacterial Efficacy of Biosynthesized Silver Nanoparticles against Enterococcus faecalis Biofilm: An in vitro Study. Contemp. Clin. Dent. 2018;9:237–241. doi: 10.4103/ccd.ccd_828_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Fatimah I., Hidayat H., Nugroho B.H., Husein S. Ultrasound-assisted biosynthesis of silver and gold nanoparticles using Clitoria ternatea flower. S. Afr. J. Chem. Eng. 2020;34:97–106. doi: 10.1016/j.sajce.2020.06.007. [DOI] [Google Scholar]
- 146.Ameen F., Srinivasan P., Selvankumar T., Kamala-Kannan S., Al Nadhari S., Almansob A., Dawoud T., Govarthanan M. Phytosynthesis of silver nanoparticles using Mangifera indica flower extract as bioreductant and their broad-spectrum antibacterial activity. Bioorg. Chem. 2019;88:102970. doi: 10.1016/j.bioorg.2019.102970. [DOI] [PubMed] [Google Scholar]
- 147.Baruah D., Yadav R.N.S., Yadav A., Das A.M. Alpinia nigra fruits mediated synthesis of silver nanoparticles and their antimicrobial and photocatalytic activities. J. Photochem. Photobiol. B Biol. 2019;201:111649. doi: 10.1016/j.jphotobiol.2019.111649. [DOI] [PubMed] [Google Scholar]
- 148.Hamida R.S., Ali M.A., Goda D.A., Khalil M.I., Redhwan A. Cytotoxic effect of green silver nanoparticles against ampicillin-resistant Klebsiella pneumoniae. RSC Adv. 2020;10:21136–21146. doi: 10.1039/d0ra03580g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Dolatabadi A., Noorbazargan H., Khayam N., Moulavi P., Zamani N., Asghari Lalami Z., Ashrafi F. Ecofriendly Biomolecule-Capped Bifidobacterium bifidum-Manufactured Silver Nanoparticles and Efflux Pump Genes Expression Alteration in Klebsiella pneumoniae. Microb. Drug Resist. 2020 doi: 10.1089/mdr.2019.0366. [DOI] [PubMed] [Google Scholar]
- 150.Siddique M.H., Aslam B., Imran M., Ashraf A., Nadeem H., Hayat S., Khurshid M., Afzal M., Malik I.R., Shahzad M., et al. Effect of Silver Nanoparticles on Biofilm Formation and EPS Production of Multidrug-Resistant Klebsiella pneumoniae. BioMed Res. Int. 2020;2020:6398165. doi: 10.1155/2020/6398165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Alfuraydi A.A., Devanesan S., Al-Ansari M., AlSalhi M.S., Ranjitsingh A.J. Eco-friendly green synthesis of silver nanoparticles from the sesame oil cake and its potential anticancer and antimicrobial activities. J. Photochem. Photobiol. B Biol. 2019;192:83–89. doi: 10.1016/j.jphotobiol.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 152.Küp F.Ö., Çoşkunçay S., Duman F. Biosynthesis of silver nanoparticles using leaf extract of Aesculus hippocastanum (horse chestnut): Evaluation of their antibacterial, antioxidant and drug release system activities. Mater. Sci. Eng. C. 2020;107:110207. doi: 10.1016/j.msec.2019.110207. [DOI] [PubMed] [Google Scholar]
- 153.Kumar S., Shahid M., Khan M.A., Kumar N., Khan H.M. Biosynthesis of silver nanoparticles from Phyllanthus niruri leaf extracts and its antibacterial activity against antibiotics-resistant clinical isolates. Pathology. 2020;52:S127. doi: 10.1016/j.pathol.2020.01.432. [DOI] [Google Scholar]
- 154.Ciepluch K., Skrzyniarz K., Barrios-Gumiel A., Quintana S., Sánchez-Nieves J., de la Mata F.J., Maciejewska B., Drulis-Kawa Z., Arabski M. Dendronized Silver Nanoparticles as Bacterial Membrane Permeabilizers and Their Interactions With P. aeruginosa Lipopolysaccharides, Lysozymes, and Phage-Derived Endolysins. Front. Microbiol. 2019;10:2771. doi: 10.3389/fmicb.2019.02771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Singh H., Du J., Singh P., Yi T.H. Ecofriendly synthesis of silver and gold nanoparticles by Euphrasia officinalis leaf extract and its biomedical applications. Artif. Cells Nanomed. Biotechnol. 2017;46:1163–1170. doi: 10.1080/21691401.2017.1362417. [DOI] [PubMed] [Google Scholar]
- 156.Garibo D., Borbón-Nuñez H.A., de León J.N.D., García Mendoza E., Estrada I., Toledano-Magaña Y., Tiznado H., Ovalle-Marroquin M., Soto-Ramos A.G., Blanco A., et al. Green synthesis of silver nanoparticles using Lysiloma acapulcensis exhibit high-antimicrobial activity. Sci. Rep. 2020:10. doi: 10.1038/s41598-020-69606-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Rolim W.R., Pelegrino M.T., de Araújo Lima B., Ferraz L.S., Costa F.N., Bernardes J.S., Rodigues T., Brocchi M., Seabra A.B. Green tea extract mediated biogenic synthesis of silver nanoparticles: Characterization, cytotoxicity evaluation and antibacterial activity. Appl. Surf. Sci. 2019;463:66–74. doi: 10.1016/j.apsusc.2018.08.203. [DOI] [Google Scholar]
- 158.Chandhru M., Logesh R., Rani S.K., Ahmed N., Vasimalai N. One-pot green route synthesis of silver nanoparticles from jack fruit seeds and their antibacterial activities with escherichia coli and salmonella bacteria. Biocatal. Agric. Biotechnol. 2019;20:101241. doi: 10.1016/j.bcab.2019.101241. [DOI] [Google Scholar]
- 159.Lotha R., Sundaramoorthy N.S., Shamprasad B.R., Nagarajan S., Sivasubramanian A. Plant nutraceuticals (Quercetrin and Afzelin) capped silver nanoparticles exert potent antibiofilm effect against food borne pathogen Salmonella enterica serovar Typhi and curtail planktonic growth in zebrafish infection model. Microb. Pathog. 2018;120:109–118. doi: 10.1016/j.micpath.2018.04.044. [DOI] [PubMed] [Google Scholar]
- 160.Neethu S., Midhun S.J., Sunil M.A., Soumya S., Radhakrishnan E.K., Jyothis M. Efficient visible light induced synthesis of silver nanoparticles by Penicillium polonicum ARA 10 isolated from Chetomorpha antennina and its antibacterial efficacy against Salmonella enterica serovar Typhimurium. J. Photochem. Photobiol. B Biol. 2018;180:175–185. doi: 10.1016/j.jphotobiol.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 161.Jemilugba O.T., Sakho E.H.M., Parani S., Mavumengwana V., Oluwafemi O.S. Green synthesis of silver nanoparticles using Combretum erythrophyllum leaves and its antibacterial activities. Colloid Interface Sci. Commun. 2019;31:100191. doi: 10.1016/j.colcom.2019.100191. [DOI] [Google Scholar]
- 162.Hashim N., Paramasivam M., Tan J.S., Kernain D., Hussin M.H., Brosse N., Gambier F., Raja P.B. Green mode synthesis of silver nanoparticles using Vitis vinifera’s tannin and screening its antimicrobial activity/apoptotic potential versus cancer cells. Mater. Today Commun. 2020;25:101511. doi: 10.1016/j.mtcomm.2020.101511. [DOI] [Google Scholar]
- 163.Rangayasami A., Kannan K., Joshi S., Subban M. Bioengineered silver nanoparticles using Elytraria acaulis (L.f.) Lindau leaf extract and its biological applications. Biocatal. Agric. Biotechnol. 2020;27:101690. doi: 10.1016/j.bcab.2020.101690. [DOI] [Google Scholar]
- 164.Ramadan M.A., Shawkey A.E., Rabeh M.A., Abdellatif A.O. Promising antimicrobial activities of oil and silver nanoparticles obtained from Melaleuca alternifolia leaves against selected skin-infecting pathogens. J. Herb. Med. 2020;20:100289. doi: 10.1016/j.hermed.2019.100289. [DOI] [Google Scholar]
- 165.Dutta T., Ghosh N.N., Das M., Adhikary R., Mandal V., Chattopadhyay A.P. Green synthesis of antibacterial and antifungal silver nanoparticles using Citrus limetta peel extract: Experimental and theoretical studies. J. Environ. Chem. Eng. 2020;8:104019. doi: 10.1016/j.jece.2020.104019. [DOI] [Google Scholar]
- 166.Rodrigues M.C., Rolim W.R., Viana M.M., Souza T.R., Gonçalves F., Tanaka C.J., Bueno-Silva B., Seabra A.B. Biogenic synthesis and antimicrobial activity of silica-coated silver nanoparticles for esthetic dental applications. J. Dent. 2020;96:103327. doi: 10.1016/j.jdent.2020.103327. [DOI] [PubMed] [Google Scholar]
- 167.Anandan M., Poorani G., Boomi P., Varunkumar K., Anand K., Chuturgoon A.A., Saravanan M., Gurumallesh Prabu H. Green synthesis of anisotropic silver nanoparticles from the aqueous leaf extract of Dodonaea viscosa with their antibacterial and anticancer activities. Process Biochem. 2019;80:80–88. doi: 10.1016/j.procbio.2019.02.014. [DOI] [Google Scholar]
- 168.Sholkamy E.N., Ahamd M.S., Yasser M.M., Eslam N. Anti-microbiological activities of bio-synthesized silver Nano-stars by Saccharopolyspora hirsuta. Saudi J. Biol. Sci. 2019;26:195–200. doi: 10.1016/j.sjbs.2018.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Alkawareek M.Y., Abulateefeh S.R., Alkilany A.M. Synergistic antibacterial activity of silver nanoparticles and hydrogen peroxide. PLoS ONE. 2019 doi: 10.1371/journal.pone.0220575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Perugini Biasi-Garbin R., Saori Otaguiri E., Morey A.T., Fernandes da Silva M., Belotto Morguette A.E., Armando Contreras Lancheros C., Kian D., Perugini M.R.E., Nakazato G., Durán N. Effect of eugenol against Streptococcus agalactiae and synergistic interaction with biologically produced silver nanoparticles. Evid. Based Complement. Altern. Med. 2015;2015:861497. doi: 10.1155/2015/861497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Song Z., Wu Y., Wang H., Han H. Synergistic antibacterial effects of curcumin modified silver nanoparticles through ROS-mediated pathways. Mater. Sci. Eng. C. 2019;99:255–263. doi: 10.1016/j.msec.2018.12.053. [DOI] [PubMed] [Google Scholar]
- 172.Qaralleh H., Khleifat K.M., Al-Limoun M.O., Alzedaneen F.Y., Al-Tawarah N. Antibacterial and synergistic effect of biosynthesized silver nanoparticles using the fungi Tritirachium oryzae W5H with essential oil of Centaurea damascena to enhance conventional antibiotics activity. Adv. Nat. Sci. Nanosci. Nanotechnol. 2019;10:025016. doi: 10.1088/2043-6254/ab2867. [DOI] [Google Scholar]
- 173.Kaur A., Preet S., Kumar V., Kumar R., Kumar R. Synergetic effect of vancomycin loaded silver nanoparticles for enhanced antibacterial activity. Colloids Surf. B Biointerfaces. 2019;176:62–69. doi: 10.1016/j.colsurfb.2018.12.043. [DOI] [PubMed] [Google Scholar]
- 174.Saha S., Malik M.M., Qureshi M.S. Study of Synergistic Effects of Antibiotics And Triangular Shaped Silver Nanoparticles, Synthesized Using UV-Light Irradiation, on S. Aureus and P. Aeruginosa. Mater. Today Proc. 2019;18:920–927. doi: 10.1016/j.matpr.2019.06.525. [DOI] [Google Scholar]
- 175.Farjadian F., Akbarizadeh A.R., Tayebi L. Synthesis of novel reducing agent for formation of metronidazole-capped silver nanoparticle and evaluating antibacterial efficiency in gram-positive and gram-negative bacteria. Heliyon. 2020;6:e04747. doi: 10.1016/j.heliyon.2020.e04747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Nishanthi R., Malathi S., John Paul S., Palani P. Green synthesis and characterization of bioinspired silver, gold and platinum nanoparticles and evaluation of their synergistic antibacterial activity after combining with different classes of antibiotics. Mater. Sci. Eng. C Mater. Biol. Appl. 2019;96:693–707. doi: 10.1016/j.msec.2018.11.050. [DOI] [PubMed] [Google Scholar]
- 177.Thomas R., Jishma P., Snigdha S., Soumya K.R., Mathew J., Radhakrishnan E.K. Enhanced antimicrobial efficacy of biosynthesized silver nanoparticle based antibiotic conjugates. Inorg. Chem. Commun. 2020;117:107978. doi: 10.1016/j.inoche.2020.107978. [DOI] [Google Scholar]
- 178.Murei A., Ayinde W.B., Gitari M.W., Samie A. Functionalization and antimicrobial evaluation of ampicillin, penicillin and vancomycin with Pyrenacantha grandiflora Baill and silver nanoparticles. Sci. Rep. 2020;10:11596. doi: 10.1038/s41598-020-68290-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Hussein E.A.M., Mohammad A.A.-H., Harraz F.A., Ahsan M.F. Biologically Synthesized Silver Nanoparticles for Enhancing Tetracycline Activity Against Staphylococcus aureus and Klebsiella pneumoniae. Braz. Arch. Biol. Technol. 2019:62. doi: 10.1590/1678-4324-2019180266. [DOI] [Google Scholar]
- 180.Gurunathan S. Rapid biological synthesis of silver nanoparticles and their enhanced antibacterial effects against Escherichia fergusonii and Streptococcus mutans. Arab. J. Chem. 2019;12:168–180. doi: 10.1016/j.arabjc.2014.11.014. [DOI] [Google Scholar]
- 181.Al-Sharqi A., Apun K., Vincent M., Kanakaraju D., Bilung L.M. Enhancement of the Antibacterial Efficiency of Silver Nanoparticles against Gram-Positive and Gram-Negative Bacteria Using Blue Laser Light. Int. J. Photoenergy. 2019;2019:2528490. doi: 10.1155/2019/2528490. [DOI] [Google Scholar]
- 182.da Silva R.T.P., Petri M.V., Valencia E.Y., Camargo P.H.C., de Torresi S.I.C., Spira B. Visible light plasmon excitation of silver nanoparticles against antibiotic-resistant Pseudomonas aeruginosa. Photodiagn. Photodyn. Ther. 2020;31:101908. doi: 10.1016/j.pdpdt.2020.101908. [DOI] [PubMed] [Google Scholar]
- 183.Szymanski C.M., Schnaar R.L., Aebi M. Essentials of Glycobiology [Internet] 3rd ed. Cold Spring Harbor Laboratory Press; New York, NY, USA: 2017. Bacterial and viral infections. [Google Scholar]
- 184.Pezhouh M.K., Yang G.Y. Viral infections of the gastrointestinal tract. Diagn. Histopathol. 2018;24:487–492. doi: 10.1016/j.mpdhp.2018.09.003. [DOI] [Google Scholar]
- 185.Baz M., Boivin G. Antiviral Agents in Development for Zika Virus Infections. Pharmaceuticals. 2019;12:101. doi: 10.3390/ph12030101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Rauch S., Jasny E., Schmidt K.E., Petsch B. New Vaccine Technologies to Combat Outbreak Situations. Front. Immunol. 2018;9:1963. doi: 10.3389/fimmu.2018.01963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Zhang C., Maruggi G., Shan H., Li J. Advances in mRNA Vaccines for Infectious Diseases. Front. Immunol. 2019;10:594. doi: 10.3389/fimmu.2019.00594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Koduru J.R., Kailasa S.K., Bhamore J.R., Kim K.H., Dutta T., Vellingiri K. Phytochemical-assisted synthetic approaches for silver nanoparticles antimicrobial applications: A review. Adv. Colloid Interface Sci. 2018;256:326–339. doi: 10.1016/j.cis.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 189.Nakamura S., Sato M., Sato Y., Ando N., Takayama T., Fujita M., Ishihara M. Synthesis and application of silver nanoparticles (Ag NPs) for the prevention of infection in healthcare workers. Int. J. Mol. Sci. 2019;20:3620. doi: 10.3390/ijms20153620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Salleh A., Naomi R., Utami N.D., Mohammad A.W., Mahmoudi E., Mustafa N., Fauzi M.B. The Potential of Silver Nanoparticles for Antiviral and Antibacterial Applications: A Mechanism of Action. Nanomaterials. 2020;10:1566. doi: 10.3390/nano10081566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Sreekanth T., Nagajyothi P., Muthuraman P., Enkhtaivan G., Vattikuti S., Tettey C., Kim D.H., Shim J., Yoo K. Ultra-sonication-assisted silver nanoparticles using Panax ginseng root extract and their anti-cancer and antiviral activities. J. Photochem. Photobiol. B Biol. 2018;188:6–11. doi: 10.1016/j.jphotobiol.2018.08.013. [DOI] [PubMed] [Google Scholar]
- 192.Mori Y., Miyahira Y., Nguyen V.Q., Matsui T., Ishihara M. Antiviral activity of silver nanoparticle/chitosan composites against H1N1 influenza A virus. Nanoscale Res. Lett. 2013;8:93. doi: 10.1186/1556-276X-8-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Alghrair Z.K., Fernig D.G., Ebrahimi B. Enhanced inhibition of influenza virus infection by peptide-noble-metal nanoparticle conjugates. Beilstein J. Nanotechnol. 2019;10:1038–1047. doi: 10.3762/bjnano.10.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Li Y., Lin Z., Zhao M., Xu T., Wang C., Hua L., Wang H., Xia H., Zhu B. Silver Nanoparticle Based Codelivery of Oseltamivir to Inhibit the Activity of the H1N1 Influenza Virus through ROS-Mediated Signaling Pathways. ACS Appl. Mater. Interfaces. 2016;8:24385–24393. doi: 10.1021/acsami.6b06613. [DOI] [PubMed] [Google Scholar]
- 195.Lin Z., Li Y., Guo M., Xu T., Wang C., Zhao M., Wang H., Chen T., Zhu B. The inhibition of H1N1 influenza virus-induced apoptosis by silver nanoparticles functionalized with zanamivir. RSC Adv. 2017;7:742–750. doi: 10.1039/c6ra25010f. [DOI] [Google Scholar]
- 196.Sanchez-Guzman D., Le Guen P., Villeret B., Sola N., Le Borgne R., Guyard A., Kemmel A., Crestani B., Sallenave J.M., Garcia-Verdugo I. Silver nanoparticle-adjuvanted vaccine protects against lethal influenza infection through inducing BALT and IgA-mediated mucosal immunity. Biomaterials. 2019;217:119308. doi: 10.1016/j.biomaterials.2019.119308. [DOI] [PubMed] [Google Scholar]
- 197.Yang X.X., Huang C.Z. Curcumin Modified Silver Nanoparticles for Highly Efficient Inhibition of Respiratory Syncytial Virus Infection. Nanoscale. 2016;8:3040–3048. doi: 10.1039/C5NR07918G. [DOI] [PubMed] [Google Scholar]
- 198.Morris D., Ansar M., Speshock J., Ivanciuc T., Qu Y., Casola A., Garofalo R. Antiviral and Immunomodulatory Activity of Silver Nanoparticles in Experimental RSV Infection. Viruses. 2019;11:732. doi: 10.3390/v11080732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Gaikwad S., Ingle A., Gade A., Rai M., Falanga A., Incoronato N., Russo L., Galdiero S., Galdiero M. Antiviral activity of mycosynthesized silver nanoparticles against herpes simplex virus and human parainfluenza virus type 3. Int. J. Nanomed. 2013;8:4303–4314. doi: 10.2147/IJN.S50070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Haggag E.G., Elshamy A.M., Rabeh M.A., Gabr N.M., Salem M., Youssif K.A., Samir A., Bin Muhsinah A., Alsayari A., Abdelmohsen U.R. Antiviral potential of green synthesized silver nanoparticles of Lampranthus coccineus and Malephora lutea. Int. J. Nanomed. 2019;14:6217–6229. doi: 10.2147/IJN.S214171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Orlowski P., Tomaszewska E., Gniadek M., Baska P., Nowakowska J., Sokolowska J., Nowak Z., Donten M., Celichowski G., Grobelny J., et al. Tannic acid modified silver nanoparticles show antiviral activity in herpes simplex virus type 2 infection. PLoS ONE. 2014;9:e104113. doi: 10.1371/journal.pone.0104113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Orlowski P., Kowalczyk A., Tomaszewska E., Ranoszek-Soliwoda K., Wegrzyn A., Grzesiak J., Celichowski G., Grobelny J., Eriksson K., Krzyzowska M. Antiviral Activity of Tannic Acid Modified Silver Nanoparticles: Potential to Activate Immune Response in Herpes Genitalis. Viruses. 2018;10:524. doi: 10.3390/v10100524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Dhanasezhian A., Srivani S., Govindaraju K., Parija P., Sasikala S., Kumar M.R.R. Anti-Herpes Simplex Virus (HSV-1 and HSV-2) activity of biogenic gold and silver nanoparticles using seaweed Sargassum wightii. Indian J. Geo Mar. Sci. 2019;48:1252–1257. [Google Scholar]
- 204.Wan C., Tai J., Zhang J., Guo Y., Zhu Q., Ling D., Gu F., Gan J., Zhu C., Wang Y., et al. Silver nanoparticles selectively induce human oncogenic gamma-herpesvirus-related cancer cell death through reactivating viral lytic replication. Cell Death Dis. 2019;10:392. doi: 10.1038/s41419-019-1624-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.El-Mohamady R.S., Ghattas T.A., Zawrah M.F., Abd El-Hafeiz Y.G.M. Inhibitory effect of silver nanoparticles on bovine herpesvirus-1. Int. J. Vet. Sci. Med. 2018;6:296–300. doi: 10.1016/j.ijvsm.2018.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Lara H.H., Ayala-Nuñez N.V., Ixtepan-Turrent L., Rodriguez-Padilla C. Mode of antiviral action of silver nanoparticles against HIV-1. J. Nanobiotechnol. 2020 doi: 10.1186/1477-3155-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Elechiguerra J.L., Burt J.L., Morones J.R., Camacho-Bragado A., Gao X., Lara H.H., Yacaman M.J. Interaction of silver nanoparticles with HIV-1. J. Nanobiotechnology. 2005;3:6. doi: 10.1186/1477-3155-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Etemadzade M., Ghamarypour A., Zabihollahi R., Shabbak G., Shirazi M., Sahebjamee H., Vaziri A.Z., Assadi A., Ardestani M.S., Shandiz S.A.S., et al. Synthesis and evaluation of antiviral activities of novel sonochemical silver nanorods against HIV and HSV viruses. Asian Pac. J. Trop. Dis. 2016;6:854–858. doi: 10.1016/s2222-1808(16)61145-3. [DOI] [Google Scholar]
- 209.Kumar S.D., Singaravelu G., Ajithkumar S., Murugan K., Nicoletti M., Benelli G. Mangrove-Mediated Green Synthesis of Silver Nanoparticles with High HIV-1 Reverse Transcriptase Inhibitory Potential. J. Clust. Sci. 2016;28:359–367. doi: 10.1007/s10876-016-1100-1. [DOI] [Google Scholar]
- 210.Tsai C.H., Whiteley C.G., Lee D.J. Interactions between HIV-1 protease, silver nanoparticles, and specific peptides. J. Taiwan Inst. Chem. Eng. 2019;103:20–32. doi: 10.1016/j.jtice.2019.07.019. [DOI] [Google Scholar]
- 211.Balagna C., Perero S., Percivalle E., Nepita E.V., Ferraris M. Virucidal effect against coronavirus SARS-CoV-2 of a silver nanocluster/silica composite sputtered coating. Open Ceram. 2020;1:100006. doi: 10.1016/j.oceram.2020.100006. [DOI] [Google Scholar]
- 212.Tremiliosi G.C., Simoes L.G.P., Minozzi D.T., Santos R.I., Vilela D.C.B., Durigon E.L., Machado R.R.G., Medina D.S., Ribeiro L.K., Rosa I.L.V., et al. Ag nanoparticles-based antimicrobial polycotton fabrics to prevent the transmission and spread of SARS-CoV-2. bioRxiv. 2020 doi: 10.1101/2020.06.26.152520. [DOI] [Google Scholar]
- 213.Rajawat S., Malik M.M. Anticancer Activity of Green Silver Nanoparticles against He-La Cervical Cancer Cell Lines. Mater. Today Proc. 2019;18:841–847. doi: 10.1016/j.matpr.2019.06.510. [DOI] [Google Scholar]
- 214.Zhang R., Lin Z., Lui V.C.H., Wong K.K.Y., Tam P.K.H., Lee P., Lok C.N., Lamb J.R., Chen Y., Xia H. Silver nanoparticle treatment ameliorates biliary atresia syndrome in rhesus rotavirus inoculated mice. Nanomed. Nanotechnol. Biol. Med. 2017;13:1041–1050. doi: 10.1016/j.nano.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 215.Adebayo-Tayo B.C., Ogunleye G.E., Ogbole O. Biomedical application of greenly synthesized silver nanoparticles using the filtrate of Trichoderma viride: Anticancer and immunomodulatory potentials. Polim. Med. 2019;49:57–62. doi: 10.17219/pim/116086. [DOI] [PubMed] [Google Scholar]
- 216.Lv X., Wang P., Bai R., Cong Y., Suo S., Ren X., Chen C. Inhibitory effect of silver nanomaterials on transmissible virus-induced host cell infections. Biomaterials. 2014;35:4195–4203. doi: 10.1016/j.biomaterials.2014.01.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Castro-Mayorga J.L., Randazzo W., Fabra M.J., Lagaron J.M., Aznar R., Sánchez G. Antiviral properties of silver nanoparticles against norovirus surrogates and their efficacy in coated polyhydroxyalkanoates systems. LWT Food Sci. Technol. 2017;79:503–510. doi: 10.1016/j.lwt.2017.01.065. [DOI] [Google Scholar]
- 218.Sofy A.R., Hmed A.A., Abd El Haliem N.F., Zein M.A., Elshaarawy R.F.M. Polyphosphonium-oligochitosans decorated with nanosilver as new prospective inhibitors for common human enteric viruses. Carbohydr. Polym. 2019;226:115261. doi: 10.1016/j.carbpol.2019.115261. [DOI] [PubMed] [Google Scholar]
- 219.Mane P.C., Chaudhari R.D., Shinde M.D., Kadam D.D., Song C.K., Amalnerkar D.P., Lee H. Designing Ecofriendly Bionanocomposite Assembly with Improved Antimicrobial and Potent on-site Zika Virus Vector Larvicidal Activities with its Mode of Action. Sci. Rep. 2017;7:15531. doi: 10.1038/s41598-017-15537-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Sharma A., Kumar S., Tripathi P. A facile and rapid method for green synthesis of Achyranthes aspera stem extract-mediated silver nano-composites with cidal potential against Aedes aegypti L. Saudi J. Biol. Sci. 2019;26:698–708. doi: 10.1016/j.sjbs.2017.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Amarasinghe L.D., Wickramarachchi P., Aberathna A., Sithara W.S., De Silva C.R. Comparative study on larvicidal activity of green synthesized silver nanoparticles and Annona glabra (Annonaceae) aqueous extract to control Aedes aegypti and Aedes albopictus (Diptera: Culicidae) Heliyon. 2020;6:e04322. doi: 10.1016/j.heliyon.2020.e04322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Aziz A.T., Alshehri M.A., Alanazi N.A., Panneerselvam C., Trivedi S., Maggi F., Sut S., Dall’Acqua S. Phytochemical analysis of Rhazya stricta extract and its use in fabrication of silver nanoparticles effective against mosquito vectors and microbial pathogens. Sci. Total Environ. 2020;700:134443. doi: 10.1016/j.scitotenv.2019.134443. [DOI] [PubMed] [Google Scholar]
- 223.Elumalai D., Hemavathi M., Deepaa C.V., Kaleena P.K. Evaluation of phytosynthesised silver nanoparticles from leaf extracts of Leucas aspera and Hyptis suaveolens and their larvicidal activity against malaria, dengue and filariasis vectors. Parasite Epidemiol. Control. 2017;2:15–26. doi: 10.1016/j.parepi.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Sutthanont N., Attrapadung S., Nuchprayoon S. Larvicidal Activity of Synthesized Silver Nanoparticles from Curcuma zedoaria Essential Oil against Culex quinquefasciatus. Insects. 2019;10:27. doi: 10.3390/insects10010027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Azarudeen R.M.S.T., Govindarajan M., Amsath A., Muthukumaran U., Benelli G. Single-Step Biofabrication of Silver Nanocrystals Using Naregamia alata: A Cost Effective and Eco-Friendly Control Tool in the Fight Against Malaria, Zika Virus and St. Louis Encephalitis Mosquito Vectors. J. Clust. Sci. 2016;28:179–203. doi: 10.1007/s10876-016-1067-y. [DOI] [Google Scholar]
- 226.Jinu U., Rajakumaran S., Senthil-Nathan S., Geetha N., Venkatachalam P. Potential larvicidal activity of silver nanohybrids synthesized using leaf extracts of Cleistanthus collinus (Roxb.) Benth. ex Hook.f. and Strychnos nux-vomica L. nux-vomica against dengue, Chikungunya and Zika vectors. Physiol. Mol. Plant Pathol. 2018;101:163–171. doi: 10.1016/j.pmpp.2017.05.003. [DOI] [Google Scholar]
- 227.Zottel A., Videtič Paska A., Jovčevska I. Nanotechnology meets oncology: Nanomaterials in brain cancer research, diagnosis and therapy. Materials. 2019;12:1588. doi: 10.3390/ma12101588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Hulvat M.C. Cancer Incidence and Trends. Surg. Clin. N. Am. 2020;100:469–481. doi: 10.1016/j.suc.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 229.Liu J., Chen Q., Feng L., Liu Z. Nanomedicine for tumor microenvironment modulation and cancer treatment enhancement. Nano Today. 2018;21:55–73. doi: 10.1016/j.nantod.2018.06.008. [DOI] [Google Scholar]
- 230.Chugh H., Sood D., Chandra I., Tomar V., Dhawan G., Chandra R. Role of gold and silver nanoparticles in cancer nano-medicine. Artif. Cells Nanomed. Biotechnol. 2018;46:1210–1220. doi: 10.1080/21691401.2018.1449118. [DOI] [PubMed] [Google Scholar]
- 231.Gorbet M.J., Ranjan A. Cancer immunotherapy with immunoadjuvants, nanoparticles, and checkpoint inhibitors: Recent progress and challenges in treatment and tracking response to immunotherapy. Pharmacol. Ther. 2020;207:107456. doi: 10.1016/j.pharmthera.2019.107456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Pothipor C., Wiriyakun N., Putnin T., Ngamaroonchote A., Jakmunee J., Ounnunkad K., Laocharoensuk R., Aroonyadet N. Highly sensitive biosensor based on graphene–poly (3-aminobenzoic acid) modified electrodes and porous-hollowed-silver-gold nanoparticle labelling for prostate cancer detection. Sens. Actuators B Chem. 2019;296:126657. doi: 10.1016/j.snb.2019.126657. [DOI] [Google Scholar]
- 233.Hasanzadeh M., Feyziazar M., Solhi E., Mokhtarzadeh A., Soleymani J., Shadjou N., Jouyban A., Mahboob S. Ultrasensitive immunoassay of breast cancer type 1 susceptibility protein (BRCA1) using poly (dopamine-beta cyclodextrine-Cetyl trimethylammonium bromide) doped with silver nanoparticles: A new platform in early stage diagnosis of breast cancer and efficient management. Microchem. J. 2019;145:778–783. doi: 10.1016/j.microc.2018.11.029. [DOI] [Google Scholar]
- 234.Nigam Joshi P., Agawane S., Athalye M.C., Jadhav V., Sarkar D., Prakash R. Multifunctional inulin tethered silver-graphene quantum dots nanotheranostic module for pancreatic cancer therapy. Mater. Sci. Eng. C Mater. Biol. Appl. 2017;78:1203–1211. doi: 10.1016/j.msec.2017.03.176. [DOI] [PubMed] [Google Scholar]
- 235.Karuppaiah A., Siram K., Selvaraj D., Ramasamy M., Babu D., Sankar V. Synergistic and enhanced anticancer effect of a facile surface modified non-cytotoxic silver nanoparticle conjugated with gemcitabine in metastatic breast cancer cells. Mater. Today Commun. 2020;23:100884. doi: 10.1016/j.mtcomm.2019.100884. [DOI] [Google Scholar]
- 236.Brkic Ahmed L., Milic M., Pongrac I.M., Marjanovic A.M., Mlinaric H., Pavicic I., Gajovic S., Vinkovic Vrcek I. Impact of surface functionalization on the uptake mechanism and toxicity effects of silver nanoparticles in HepG2 cells. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2017;107:349–361. doi: 10.1016/j.fct.2017.07.016. [DOI] [PubMed] [Google Scholar]
- 237.Azhar N.A., Ghozali S.Z., Abu Bakar S.A., Lim V., Ahmad N.H. Suppressing growth, migration, and invasion of human hepatocellular carcinoma HepG2 cells by Catharanthus roseussilver nanoparticles. Toxicol. Vitr. Int. J. Publ. Assoc. BIBRA. 2020;67:104910. doi: 10.1016/j.tiv.2020.104910. [DOI] [PubMed] [Google Scholar]
- 238.Zhu B., Li Y., Lin Z., Zhao M., Xu T., Wang C., Deng N. Silver Nanoparticles Induce HePG-2 Cells Apoptosis Through ROS-Mediated Signaling Pathways. Nanoscale Res. Lett. 2016;11:198. doi: 10.1186/s11671-016-1419-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Bin-Jumah M., Al-Abdan M., Albasher G., Alarifi S. Effects of Green Silver Nanoparticles on Apoptosis and Oxidative Stress in Normal and Cancerous Human Hepatic Cells in vitro. Int. J. Nanomed. 2020;15:1537–1548. doi: 10.2147/IJN.S239861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Azizi M., Ghourchian H., Yazdian F., Bagherifam S., Bekhradnia S., Nystrom B. Anti-cancerous effect of albumin coated silver nanoparticles on MDA-MB 231 human breast cancer cell line. Sci. Rep. 2017;7:5178. doi: 10.1038/s41598-017-05461-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Ishida T. Anticancer activities of silver ions in cancer and tumor cells and DNA damages by Ag—DNA base-pairs reactions. MOJ Tumor Res. 2017 doi: 10.15406/mojtr.2017.01.00003. [DOI] [Google Scholar]
- 242.Kanipandian N., Li D., Kannan S. Induction of intrinsic apoptotic signaling pathway in A549 lung cancer cells using Silver nanoparticles from Gossypium hirsutum and evaluation of in vivo toxicity. Biotechnol. Rep. 2019;23:e00339. doi: 10.1016/j.btre.2019.e00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Lee H.A., Castro-Aceituno V., Abbai R., Moon S.S., Kim Y.J., Simu S.Y., Yang D.C. Rhizome of Anemarrhena asphodeloides as mediators of the eco-friendly synthesis of silver and gold spherical, face-centred cubic nanocrystals and its anti-migratory and cytotoxic potential in normal and cancer cell lines. Artif. CellsNanomed. Biotechnol. 2018;46:285–294. doi: 10.1080/21691401.2018.1457038. [DOI] [PubMed] [Google Scholar]
- 244.Castro-Aceituno V., Abbai R., Moon S.S., Ahn S., Mathiyalagan R., Kim Y.J., Kim Y.J., Yang D.C. Pleuropterus multiflorus (Hasuo) mediated straightforward eco-friendly synthesis of silver, gold nanoparticles and evaluation of their anti-cancer activity on A549 lung cancer cell line. Biomed. Pharmacother. Biomed. Pharmacother. 2017;93:995–1003. doi: 10.1016/j.biopha.2017.07.040. [DOI] [PubMed] [Google Scholar]
- 245.Kim C.G., Castro-Aceituno V., Abbai R., Lee H.A., Simu S.Y., Han Y., Hurh J., Kim Y.J., Yang D.C. Caspase-3/MAPK pathways as main regulators of the apoptotic effect of the phyto-mediated synthesized silver nanoparticle from dried stem of Eleutherococcus senticosus in human cancer cells. Biomed. Pharmacother. Biomed. Pharmacother. 2018;99:128–133. doi: 10.1016/j.biopha.2018.01.050. [DOI] [PubMed] [Google Scholar]
- 246.Pareek V., Gupta R., Panwar J. Do physico-chemical properties of silver nanoparticles decide their interaction with biological media and bactericidal action? A review. Mater. Sci. Eng. C Mater. Biol. Appl. 2018;90:739–749. doi: 10.1016/j.msec.2018.04.093. [DOI] [PubMed] [Google Scholar]
- 247.De Matteis V., Cascione M., Toma C.C., Leporatti S. Silver nanoparticles: Synthetic routes, in vitro toxicity and theranostic applications for cancer disease. Nanomaterials. 2018;8:319. doi: 10.3390/nano8050319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Ahn E.Y., Jin H., Park Y. Assessing the antioxidant, cytotoxic, apoptotic and wound healing properties of silver nanoparticles green-synthesized by plant extracts. Mater. Sci. Eng. C Mater. Biol. Appl. 2019;101:204–216. doi: 10.1016/j.msec.2019.03.095. [DOI] [PubMed] [Google Scholar]
- 249.Majeed S., Aripin F.H.B., Shoeb N.S.B., Danish M., Ibrahim M.N.M., Hashim R. Bioengineered silver nanoparticles capped with bovine serum albumin and its anticancer and apoptotic activity against breast, bone and intestinal colon cancer cell lines. Mater. Sci. Eng. C Mater. Biol. Appl. 2019;102:254–263. doi: 10.1016/j.msec.2019.04.041. [DOI] [PubMed] [Google Scholar]
- 250.Gomathi A.C., Xavier Rajarathinam S.R., Mohammed Sadiq A., Rajeshkumar S. Anticancer activity of silver nanoparticles synthesized using aqueous fruit shell extract of Tamarindus indica on MCF-7 human breast cancer cell line. J. Drug Deliv. Sci. Technol. 2020;55:101376. doi: 10.1016/j.jddst.2019.101376. [DOI] [Google Scholar]
- 251.Al-kawmani A.A., Alanazi K.M., Farah M.A., Ali M.A., Hailan W.A.Q., Al-Hemaid F.M.A. Apoptosis-inducing potential of biosynthesized silver nanoparticles in breast cancer cells. J. King Saud Univ. Sci. 2020;32:2480–2488. doi: 10.1016/j.jksus.2020.04.002. [DOI] [Google Scholar]
- 252.Almalki M.A., Khalifa A.Y.Z. Silver nanoparticles synthesis from Bacillus sp KFU36 and its anticancer effect in breast cancer MCF-7 cells via induction of apoptotic mechanism. J. Photochem. Photobiol. B Biol. 2020;204:111786. doi: 10.1016/j.jphotobiol.2020.111786. [DOI] [PubMed] [Google Scholar]
- 253.Hepokur C., Kariper I.A., Misir S., Ay E., Tunoglu S., Ersez M.S., Zeybek U., Kuruca S.E., Yaylim I. Silver nanoparticle/capecitabine for breast cancer cell treatment. Toxicol. Vitr. Int. J. Publ. Assoc. BIBRA. 2019;61:104600. doi: 10.1016/j.tiv.2019.104600. [DOI] [PubMed] [Google Scholar]
- 254.Al-Sheddi E.S., Farshori N.N., Al-Oqail M.M., Al-Massarani S.M., Saquib Q., Wahab R., Musarrat J., Al-Khedhairy A.A., Siddiqui M.A. Anticancer potential of green synthesized silver nanoparticles using extract of Nepeta deflersiana against human cervical cancer cells (HeLA) Bioinorg. Chem. Appl. 2018;2018:9390784. doi: 10.1155/2018/9390784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Yuan Y.G., Zhang S., Hwang J.Y., Kong I.K. Silver Nanoparticles Potentiates Cytotoxicity and Apoptotic Potential of Camptothecin in Human Cervical Cancer Cells. Oxidative Med. Cell. Longev. 2018;2018:6121328. doi: 10.1155/2018/6121328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Algebaly A.S., Mohammed A.E., Abutaha N., Elobeid M.M. Biogenic Synthesis of Silver Nanoparticles: Antibacterial and Cytotoxic Potential. Saudi J. Biol. Sci. 2019;27:1340–1351. doi: 10.1016/j.sjbs.2019.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Korkmaz N., Ceylan Y., Hamid A., Karadağ A., Bülbül A.S., Aftab M.N., Çevik Ö., Şen F. Biogenic silver nanoparticles synthesized via Mimusops elengi fruit extract, a study on antibiofilm, antibacterial, and anticancer activities. J. Drug Deliv. Sci. Technol. 2020;59:101864. doi: 10.1016/j.jddst.2020.101864. [DOI] [Google Scholar]
- 258.Hamouda R.A., Hussein M.H., Abo-Elmagd R.A., Bawazir S.S. Synthesis and biological characterization of silver nanoparticles derived from the cyanobacterium Oscillatoria limnetica. Sci. Rep. 2019;9:13071. doi: 10.1038/s41598-019-49444-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Al-Brahim J.S., Mohammed A.E. Antioxidant, cytotoxic and antibacterial potential of biosynthesized nanoparticles using bee honey from two different floral sources in Saudi Arabia. Saudi J. Biol. Sci. 2020;27:363–373. doi: 10.1016/j.sjbs.2019.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.He Y., Li X., Zheng Y., Wang Z., Ma Z., Yang Q., Yao B., Zhao Y., Zhang H. A green approach of synthesizing of silver nanoparticles and their antibacterial and cytotoxicity activities. New J. Chem. 2018 doi: 10.1039/C7NJ04224H. [DOI] [Google Scholar]
- 261.Hashemi S.F., Tasharrofi N., Saber M.M. Green synthesis of silver nanoparticles using Teucrium polium leaf extract and assessment of their antitumor effects against MNK45 human gastric cancer cell line. J. Mol. Struct. 2020;1208:127889. doi: 10.1016/j.molstruc.2020.127889. [DOI] [Google Scholar]
- 262.Mortazavi-Derazkola S., Ebrahimzadeh M.A., Amiri O., Goli H.R., Rafiei A., Kardan M., Salavati-Niasari M. Facile green synthesis and characterization of Crataegus microphylla extract-capped silver nanoparticles (CME@Ag-NPs) and its potential antibacterial and anticancer activities against AGS and MCF-7 human cancer cells. J. Alloys Compd. 2020;820:153186. doi: 10.1016/j.jallcom.2019.153186. [DOI] [Google Scholar]
- 263.Ferreira L.A.B., Garcia-Fossa F., Radaic A., Duran N., Favaro W.J., de Jesus M.B. Biogenic silver nanoparticles: In vitro and in vivo antitumor activity in bladder cancer. Eur. J. Pharm. Biopharm. 2020;151:162–170. doi: 10.1016/j.ejpb.2020.04.012. [DOI] [PubMed] [Google Scholar]
- 264.Danagoudar A., Pratap G.K., Shantaram M., Ghosh K., Kanade S.R., Joshi C.G. Characterization, cytotoxic and antioxidant potential of silver nanoparticles biosynthesised using endophytic fungus (Penicillium citrinum CGJ-C1) Mater. Today Commun. 2020;25:101385. doi: 10.1016/j.mtcomm.2020.101385. [DOI] [Google Scholar]
- 265.Danagoudar A., Pratap G.K., Shantaram M., Chatterjee B., Ghosh K., Kanade S.R., Joshi C.G. Cancer cell specific cytotoxic potential of the silver nanoparticles synthesized using the endophytic fungus, Penicillium citrinum CGJ-C2. Mater. Today Commun. 2020;25:101442. doi: 10.1016/j.mtcomm.2020.101442. [DOI] [Google Scholar]
- 266.Sattari R., Khayati G.R., Hoshyar R. Biosynthesis and characterization of silver nanoparticles capped by biomolecules by fumaria parviflora extract as green approach and evaluation of their cytotoxicity against human breast cancer MDA-MB-468 cell lines. Mater. Chem. Phys. 2020;241:122438. doi: 10.1016/j.matchemphys.2019.122438. [DOI] [Google Scholar]
- 267.Aygun A., Gulbagca F., Nas M.S., Alma M.H., Calimli M.H., Ustaoglu B., Altunoglu Y.C., Baloglu M.C., Cellat K., Sen F. Biological synthesis of silver nanoparticles using Rheum ribes and evaluation of their anticarcinogenic and antimicrobial potential: A novel approach in phytonanotechnology. J. Pharm. Biomed. Anal. 2020;179:113012. doi: 10.1016/j.jpba.2019.113012. [DOI] [PubMed] [Google Scholar]
- 268.Nesrin K., Yusuf C., Ahmet K., Ali S.B., Muhammad N.A., Suna S., Fatih S. Biogenic silver nanoparticles synthesized from Rhododendron ponticum and their antibacterial, antibiofilm and cytotoxic activities. J. Pharm. Biomed. Anal. 2020;179:112993. doi: 10.1016/j.jpba.2019.112993. [DOI] [PubMed] [Google Scholar]
- 269.Dinparvar S., Bagirova M., Allahverdiyev A.M., Abamor E.S., Safarov T., Aydogdu M., Aktas D. A nanotechnology-based new approach in the treatment of breast cancer: Biosynthesized silver nanoparticles using Cuminum cyminum L. seed extract. J. Photochem. Photobiol. B Biol. 2020;208:111902. doi: 10.1016/j.jphotobiol.2020.111902. [DOI] [PubMed] [Google Scholar]
- 270.Karimzadeh K., Elham S., Bakhshi N., Ramzanpoor M. Biogenic silver nanoparticles using Oxalis corniculata characterization and their clinical implications. J. Drug Deliv. Sci. Technol. 2019;54:101263. doi: 10.1016/j.jddst.2019.101263. [DOI] [Google Scholar]
- 271.Deepika S., Selvaraj C.I., Roopan S.M. Screening bioactivities of Caesalpinia pulcherrima L. swartz and cytotoxicity of extract synthesized silver nanoparticles on HCT116cell line. Mater. Sci. Eng. C Mater. Biol. Appl. 2020;106:110279. doi: 10.1016/j.msec.2019.110279. [DOI] [PubMed] [Google Scholar]
- 272.Ahmed T., Shahid M., Noman M., Bilal Khan Niazi M., Zubair M., Almatroudi A., Khurshid M., Tariq F., Mumtaz R., Li B. Bioprospecting a native silver-resistant Bacillus safensis strain for green synthesis and subsequent antibacterial and anticancer activities of silver nanoparticles. J. Adv. Res. 2020;24:475–483. doi: 10.1016/j.jare.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Li J., Zhang B., Chang X., Gan J., Li W., Niu S., Kong L., Wu T., Zhang T., Tang M., et al. Silver nanoparticles modulate mitochondrial dynamics and biogenesis in HepG2 cells. Environ. Pollut. 2020;256:113430. doi: 10.1016/j.envpol.2019.113430. [DOI] [PubMed] [Google Scholar]
- 274.Majeed S., Danish M., Zahrudin A.H.B., Dash G.K. Biosynthesis and characterization of silver nanoparticles from fungal species and its antibacterial and anticancer effect. Karbala Int. J. Mod. Sci. 2018;4:86–92. [Google Scholar]
- 275.Samuel M.S., Jose S., Selvarajan E., Mathimani T., Pugazhendhi A. Biosynthesized silver nanoparticles using Bacillus amyloliquefaciens; Application for cytotoxicity effect on A549 cell line and photocatalytic degradation of p-nitrophenol. J. Photochem. Photobiol. B Biol. 2020;202:111642. doi: 10.1016/j.jphotobiol.2019.111642. [DOI] [PubMed] [Google Scholar]
- 276.Meenakshisundaram S., Krishnamoorthy V., Jagadeesan Y., Vilwanathan R., Balaiah A. Annona muricata assisted biogenic synthesis of silver nanoparticles regulates cell cycle arrest in NSCLC cell lines. Bioorg. Chem. 2020;95:103451. doi: 10.1016/j.bioorg.2019.103451. [DOI] [PubMed] [Google Scholar]
- 277.Varunkumar K., Anusha C., Saranya T., Ramalingam V., Raja S., Ravikumar V. Avicennia marina engineered nanoparticles induce apoptosis in adenocarcinoma lung cancer cell line through p53 mediated signaling pathways. Process Biochem. 2020;94:349–358. doi: 10.1016/j.procbio.2020.04.034. [DOI] [Google Scholar]
- 278.Majeed S., Bakhtiar N.F.B., Danish M., Mohamad Ibrahim M.N., Hashim R. Green approach for the biosynthesis of silver nanoparticles and its antibacterial and antitumor effect against osteoblast MG-63 and breast MCF-7 cancer cell lines. Sustain. Chem. Pharm. 2019;12:100138. doi: 10.1016/j.scp.2019.100138. [DOI] [Google Scholar]
- 279.Wen X., Wang Q., Dai T., Shao J., Wu X., Jiang Z., Jacob J.A., Jiang C. Identification of possible reductants in the aqueous leaf extract of mangrove plant Rhizophora apiculata for the fabrication and cytotoxicity of silver nanoparticles against human osteosarcoma MG-63 cells. Mater. Sci. Eng. C Mater. Biol. Appl. 2020;116:111252. doi: 10.1016/j.msec.2020.111252. [DOI] [PubMed] [Google Scholar]
- 280.Francis S., Nair K.M., Paul N., Koshy E.P., Mathew B. Green synthesized metal nanoparticles as a selective inhibitor of human osteosarcoma and pathogenic microorganisms. Mater. Today Chem. 2019;13:128–138. doi: 10.1016/j.mtchem.2019.04.013. [DOI] [Google Scholar]
- 281.Khan T., Yasmin A., Townley H.E. An evaluation of the activity of biologically synthesized silver nanoparticles against bacteria, fungi and mammalian cell lines. Colloids Surf. B Biointerfaces. 2020;194:111156. doi: 10.1016/j.colsurfb.2020.111156. [DOI] [PubMed] [Google Scholar]
- 282.Cameron S.J., Hosseinian F., Willmore W.G. A Current Overview of the Biological and Cellular Effects of Nanosilver. Int. J. Mol. Sci. 2018;19:2030. doi: 10.3390/ijms19072030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Yesilot S., Aydin C. Silver nanoparticles; a new hope in cancer therapy? East. J. Med. 2019;24:111–116. [Google Scholar]
- 284.Yang T., Yao Q., Cao F., Liu Q., Liu B., Wang X.H. Silver nanoparticles inhibit the function of hypoxia-inducible factor-1 and target genes: Insight into the cytotoxicity and antiangiogenesis. Int. J. Nanomed. 2016;11:6679–6692. doi: 10.2147/IJN.S109695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Baghani M., Es-haghi A. Characterization of silver nanoparticles biosynthesized using Amaranthus cruentus. Bioinspir. Biomim. Nanobiomater. 2020;9:129–136. doi: 10.1680/jbibn.18.00051. [DOI] [Google Scholar]
- 286.Ghandehari S., Tabrizi M., Ardalan P. Evaluation of Anti-angiogenic Activity of Silver Nanoparticle Synthesis by Rubina tinctorum L (Ru-AgNPs) Using Chicken Chorioallantoic Membrane (CAM) Assay. J. Arak Univ. Med. Sci. 2018;21:82–90. [Google Scholar]
- 287.Hao M., Kong C., Jiang C., Hou R., Zhao X., Li J., Wang Y., Gao Y., Zhang H., Yang B., et al. Polydopamine-coated Au-Ag nanoparticle-guided photothermal colorectal cancer therapy through multiple cell death pathways. Acta Biomater. 2019;83:414–424. doi: 10.1016/j.actbio.2018.10.032. [DOI] [PubMed] [Google Scholar]
- 288.He X., Peng C., Qiang S., Xiong L.H., Zhao Z., Wang Z., Kwok R.T.K., Lam J.W.Y., Ma N., Tang B.Z. Less is more: Silver-AIE core@shell nanoparticles for multimodality cancer imaging and synergistic therapy. Biomaterials. 2020;238:119834. doi: 10.1016/j.biomaterials.2020.119834. [DOI] [PubMed] [Google Scholar]
- 289.Wang M., Liang Y., Zhang Z., Ren G., Liu Y., Wu S., Shen J. AgFe3O4C nanoparticles for multi-modal imaging-guided chemo-photothermal synergistic targeting for cancer therapy. Anal. Chim. Acta. 2019;1086:122–132. doi: 10.1016/j.aca.2019.08.035. [DOI] [PubMed] [Google Scholar]
- 290.Thapa R.K., Kim J.H., Jeong J.H., Shin B.S., Choi H.G., Yong C.S., Kim J.O. Silver nanoparticle-embedded graphene oxide-methotrexate for targeted cancer treatment. Colloids Surf. B Biointerfaces. 2017;153:95–103. doi: 10.1016/j.colsurfb.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 291.Poudel B.K., Soe Z.C., Ruttala H.B., Gupta B., Ramasamy T., Thapa R.K., Gautam M., Ou W., Nguyen H.T., Jeong J.H., et al. In situ fabrication of mesoporous silica-coated silver-gold hollow nanoshell for remotely controllable chemo-photothermal therapy via phase-change molecule as gatekeepers. Int. J. Pharm. 2018;548:92–103. doi: 10.1016/j.ijpharm.2018.06.056. [DOI] [PubMed] [Google Scholar]
- 292.Sakr T.M., Khowessah O.M., Motaleb M.A., Abd El-Bary A., El-Kolaly M.T., Swidan M.M. I-131 doping of silver nanoparticles platform for tumor theranosis guided drug delivery. Eur. J. Pharm. Sci. Off. J. Eur. Fed. Pharm. Sci. 2018;122:239–245. doi: 10.1016/j.ejps.2018.06.029. [DOI] [PubMed] [Google Scholar]
- 293.Jyoti K., Singh A., Fekete G., Singh T. Cytotoxic and radiosensitizing potential of silver nanoparticles against HepG-2 cells prepared by biosynthetic route using Picrasma quassioides leaf extract. J. Drug Deliv. Sci. Technol. 2020;55:101479. doi: 10.1016/j.jddst.2019.101479. [DOI] [Google Scholar]
- 294.Manaloto E., Gowen A.A., Lesniak A., He Z., Casey A., Cullen P.J., Curtin J.F. Cold atmospheric plasma induces silver nanoparticle uptake, oxidative dissolution and enhanced cytotoxicity in glioblastoma multiforme cells. Arch. Biochem. Biophys. 2020;689:108462. doi: 10.1016/j.abb.2020.108462. [DOI] [PubMed] [Google Scholar]
- 295.Erdogan O., Abbak M., Demirbolat G.M., Birtekocak F., Aksel M., Pasa S., Cevik O. Green synthesis of silver nanoparticles via Cynara scolymus leaf extracts: The characterization, anticancer potential with photodynamic therapy in MCF7 cells. PLoS ONE. 2019;14:e0216496. doi: 10.1371/journal.pone.0216496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Mahajan P.G., Dige N.C., Vanjare B.D., Eo S.H., Seo S.Y., Kim S.J., Hong S.K., Choi C.S., Lee K.H. A potential mediator for photodynamic therapy based on silver nanoparticles functionalized with porphyrin. J. Photochem. Photobiol. A Chem. 2019;377:26–35. doi: 10.1016/j.jphotochem.2019.03.034. [DOI] [Google Scholar]
- 297.Zurina I.M., Presniakova V.S., Butnaru D.V., Svistunov A.A., Timashev P.S., Rochev Y.A. Tissue engineering using a combined cell sheet technology and scaffolding approach. Acta Biomater. 2020 doi: 10.1016/j.actbio.2020.06.016. [DOI] [PubMed] [Google Scholar]
- 298.Nguyen M.A., Camci-Unal G. Unconventional Tissue Engineering Materials in Disguise. Trends Biotechnol. 2020;38:178–190. doi: 10.1016/j.tibtech.2019.07.014. [DOI] [PubMed] [Google Scholar]
- 299.Abbasian M., Massoumi B., Mohammad-Rezaei R., Samadian H., Jaymand M. Scaffolding polymeric biomaterials: Are naturally occurring biological macromolecules more appropriate for tissue engineering? Int. J. Biol. Macromol. 2019;134:673–694. doi: 10.1016/j.ijbiomac.2019.04.197. [DOI] [PubMed] [Google Scholar]
- 300.Kirmanidou Y., Sidira M., Bakopoulou A., Tsouknidas A., Prymak O., Papi R., Choli-Papadopoulou T., Epple M., Michailidis N., Koidis P., et al. Assessment of cytotoxicity and antibacterial effects of silver nanoparticle-doped titanium alloy surfaces. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2019;35:e220–e233. doi: 10.1016/j.dental.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 301.van Hengel I.A.J., Putra N.E., Tierolf M., Minneboo M., Fluit A.C., Fratila-Apachitei L.E., Apachitei I., Zadpoor A.A. Biofunctionalization of selective laser melted porous titanium using silver and zinc nanoparticles to prevent infections by antibiotic-resistant bacteria. Acta Biomater. 2020;107:325–337. doi: 10.1016/j.actbio.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 302.Odatsu T., Kuroshima S., Sato M., Takase K., Valanezhad A., Naito M., Sawase T. Antibacterial Properties of Nano-Ag Coating on Healing Abutment: An In Vitro and Clinical Study. Antibiotics. 2020;9:347. doi: 10.3390/antibiotics9060347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Zhang C., Lan J., Wang S., Han S., Yang H., Niu Q., Wang J., Wang Q., Xiang Y., Wu Y., et al. Silver nanowires on acid-alkali-treated titanium surface: Bacterial attachment and osteogenic activity. Ceram. Int. 2019;45:24528–24537. doi: 10.1016/j.ceramint.2019.08.180. [DOI] [Google Scholar]
- 304.Rafieerad A.R., Bushroa A.R., Nasiri-Tabrizi B., Baradaran S., Amiri A., Saber-Samandari S., Khanahmadi S., Zeimaran E., Basirun W.J., Kalaiselvam K., et al. Simultaneous enhanced antibacterial and osteoblast cytocompatibility performance of Ti6Al7Nb implant by nano-silver/graphene oxide decorated mixed oxide nanotube composite. Surf. Coat. Technol. 2019;360:181–195. doi: 10.1016/j.surfcoat.2018.12.119. [DOI] [Google Scholar]
- 305.Cheng Y.F., Zhang J.Y., Wang Y.B., Li C.M., Lu Z.S., Hu X.F., Xu L.Q. Deposition of catechol-functionalized chitosan and silver nanoparticles on biomedical titanium surfaces for antibacterial application. Mater. Sci. Eng. C Mater. Biol. Appl. 2019;98:649–656. doi: 10.1016/j.msec.2019.01.019. [DOI] [PubMed] [Google Scholar]
- 306.Lee J.Y., Aguilar L.E., Park C.H., Kim C.S. UV Light Assisted Coating Method of Polyphenol Caffeic Acid and Mediated Immobilization of Metallic Silver Particles for Antibacterial Implant Surface Modification. Polymers. 2019;11:1200. doi: 10.3390/polym11071200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Zeng X., Xiong S., Zhuo S., Liu C., Miao J., Liu D., Wang H., Zhang Y., Wang C., Liu Y. Nanosilver/poly (dl-lactic-co-glycolic acid) on titanium implant surfaces for the enhancement of antibacterial properties and osteoinductivity. Int. J. Nanomed. 2019;14:1849–1863. doi: 10.2147/IJN.S190954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Mallakpour S., Abbasi M. Hydroxyapatite mineralization on chitosan-tragacanth gum/silica@silver nanocomposites and their antibacterial activity evaluation. Int J. Biol. Macromol. 2020;151:909–923. doi: 10.1016/j.ijbiomac.2020.02.167. [DOI] [PubMed] [Google Scholar]
- 309.Bakhsheshi-Rad H.R., Ismail A.F., Aziz M., Akbari M., Hadisi Z., Khoshnava S.M., Pagan E., Chen X. Co-incorporation of graphene oxide/silver nanoparticle into poly-L-lactic acid fibrous: A route toward the development of cytocompatible and antibacterial coating layer on magnesium implants. Mater. Sci. Eng. C Mater. Biol. Appl. 2020;111:110812. doi: 10.1016/j.msec.2020.110812. [DOI] [PubMed] [Google Scholar]
- 310.Gouveia Z., Perinpanayagam H., Zhu J. Development of Robust Chitosan–Silica Class II Hybrid Coatings with Antimicrobial Properties for Titanium Implants. Coatings. 2020;10:534. doi: 10.3390/coatings10060534. [DOI] [Google Scholar]
- 311.Salaie R.N., Besinis A., Le H., Tredwin C., Handy R.D. The biocompatibility of silver and nanohydroxyapatite coatings on titanium dental implants with human primary osteoblast cells. Mater. Sci. Eng. C Mater. Biol. Appl. 2020;107:110210. doi: 10.1016/j.msec.2019.110210. [DOI] [PubMed] [Google Scholar]
- 312.Estrada-Cabrera E., Torres-Ferrer L.R., Aztatzi-Aguilar O.G., De Vizcaya-Ruiz A., Meraz-Rios M.A., Zarate-Triviño D.G., Arizmendi-Morquecho A., de Luna Bugallo A., Prokhorov E., Luna-Barcenas G. Chitosan-bioglass coatings on partially nanostructured anodized Ti-6Al-4V alloy for biomedical applications. Surf. Coat. Technol. 2019;375:468–476. doi: 10.1016/j.surfcoat.2019.07.002. [DOI] [Google Scholar]
- 313.Yu W.Z., Zhang Y., Liu X., Xiang Y., Li Z., Wu S. Synergistic antibacterial activity of multi components in lysozyme/chitosan/silver/hydroxyapatite hybrid coating. Mater. Des. 2018;139:351–362. doi: 10.1016/j.matdes.2017.11.018. [DOI] [Google Scholar]
- 314.Mareci D., Trincă L.C., Căilean D., Souto R.M. Corrosion resistance of ZrTi alloys with hydroxyapatite-zirconia-silver layer in simulated physiological solution containing proteins for biomaterial applications. Appl. Surf. Sci. 2016;389:1069–1075. doi: 10.1016/j.apsusc.2016.08.046. [DOI] [Google Scholar]
- 315.Trincă L.C., Mareci D., Souto R.M., Lozano-Gorrín A.D., Izquierdo J., Burtan L., Motrescu I., Vulpe V., Pavel G., Strungaru S., et al. Osseointegration evaluation of ZrTi alloys with hydroxyapatite-zirconia-silver layer in pig’s tibiae. Appl. Surf. Sci. 2019;487:127–137. doi: 10.1016/j.apsusc.2019.05.003. [DOI] [Google Scholar]
- 316.Patil S., Singh N. Antibacterial silk fibroin scaffolds with green synthesized silver nanoparticles for osteoblast proliferation and human mesenchymal stem cell differentiation. Colloids Surf. B Biointerfaces. 2019;176:150–155. doi: 10.1016/j.colsurfb.2018.12.067. [DOI] [PubMed] [Google Scholar]
- 317.Wenhao Z., Zhang T., Yan J., Li Q., Xiong P., Li Y., Cheng Y., Zheng Y. In vitro and in vivo evaluation of structurally-controlled silk fibroin coatings for orthopedic infection and in-situ osteogenesis. Acta Biomater. 2020 doi: 10.1016/j.actbio.2020.08.040. [DOI] [PubMed] [Google Scholar]
- 318.Raho R., Nguyen N.Y., Zhang N., Jiang W., Sannino A., Liu H., Pollini M., Paladini F. Photo-assisted green synthesis of silver doped silk fibroin/carboxymethyl cellulose nanocomposite hydrogels for biomedical applications. Mater. Sci. Eng. C Mater. Biol. Appl. 2020;107:110219. doi: 10.1016/j.msec.2019.110219. [DOI] [PubMed] [Google Scholar]
- 319.Baras B.H., Sun J., Melo M.A.S., Tay F.R., Oates T.W., Zhang K., Weir M.D., Xu H.H.K. Novel root canal sealer with dimethylaminohexadecyl methacrylate, nano-silver and nano-calcium phosphate to kill bacteria inside root dentin and increase dentin hardness. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2019;35:1479–1489. doi: 10.1016/j.dental.2019.07.014. [DOI] [PubMed] [Google Scholar]
- 320.Marques L., Martinez G., Guidelli É., Tamashiro J., Segato R., Payão S.L.M., Baffa O., Kinoshita A. Performance on Bone Regeneration of a Silver Nanoparticle Delivery System Based on Natural Rubber Membrane NRL-AgNP. Coatings. 2020;10:323. doi: 10.3390/coatings10040323. [DOI] [Google Scholar]
- 321.Suteewong T., Wongpreecha J., Polpanich D., Jangpatarapongsa K., Kaewsaneha C., Tangboriboonrat P. PMMA particles coated with chitosan-silver nanoparticles as a dual antibacterial modifier for natural rubber latex films. Colloids Surf. B Biointerfaces. 2019;174:544–552. doi: 10.1016/j.colsurfb.2018.11.037. [DOI] [PubMed] [Google Scholar]
- 322.Abdelaziz D., Hefnawy A., Al-Wakeel E., El-Fallal A., El-Sherbiny I.M. New biodegradable nanoparticles-in-nanofibers based membranes for guided periodontal tissue and bone regeneration with enhanced antibacterial activity. J. Adv. Res. 2020 doi: 10.1016/j.jare.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Liu F., Wang X., Chen T., Zhang N., Wei Q., Tian J., Wang Y., Ma C., Lu Y. Hydroxyapatite/silver electrospun fibers for anti-infection and osteoinduction. J. Adv. Res. 2020;21:91–102. doi: 10.1016/j.jare.2019.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Guo W., Liu W., Xu L., Feng P., Zhang Y., Yang W., Shuai C. Halloysite nanotubes loaded with nano silver for the sustained-release of antibacterial polymer nanocomposite scaffolds. J. Mater. Sci. Technol. 2020;46:237–247. doi: 10.1016/j.jmst.2019.11.019. [DOI] [Google Scholar]
- 325.Hasan A., Waibhaw G., Saxena V., Pandey L.M. Nano-biocomposite scaffolds of chitosan, carboxymethyl cellulose and silver nanoparticle modified cellulose nanowhiskers for bone tissue engineering applications. Int J. Biol. Macromol. 2018;111:923–934. doi: 10.1016/j.ijbiomac.2018.01.089. [DOI] [PubMed] [Google Scholar]
- 326.Kumar P., Dehiya B.S., Sindhu A., Kumar R., Pruncu C.I., Yadav A. Fabrication and characterization of silver nanorods incorporated calcium silicate scaffold using polymeric sponge replica technique. Mater. Des. 2020;195:109026. doi: 10.1016/j.matdes.2020.109026. [DOI] [Google Scholar]
- 327.Kumar Saini R., Prasad Bagri L., Bajpai A.K. Nano-silver hydroxyapatite based antibacterial 3D scaffolds of gelatin/alginate/poly (vinyl alcohol) for bone tissue engineering applications. Colloids Surf. B Biointerfaces. 2019;177:211–218. doi: 10.1016/j.colsurfb.2019.01.064. [DOI] [PubMed] [Google Scholar]
- 328.Paterson T.E., Shi R., Tian J., Harrison C.J., De Sousa Mendes M., Hatton P.V., Li Z., Ortega I. Electrospun Scaffolds Containing Silver-Doped Hydroxyapatite with Antimicrobial Properties for Applications in Orthopedic and Dental Bone Surgery. J. Funct. Biomater. 2020;11:58. doi: 10.3390/jfb11030058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Zulkifli F.H., Rani N.A.M., Shahitha F. Carboxymethyl cellulose nanofibres impregnated with silver nanoparticles for tissue engineering applications. Mater. Today Proc. 2019;16:1715–1721. doi: 10.1016/j.matpr.2019.06.041. [DOI] [Google Scholar]
- 330.Urena-Saborio H., Rodríguez G., Madrigal-Carballo S., Gunasekaran S. Characterization and applications of silver nanoparticles-decorated electrospun nanofibers loaded with polyphenolic extract from rambutan (Nepelium lappaceum) Materialia. 2020;11:100687. doi: 10.1016/j.mtla.2020.100687. [DOI] [Google Scholar]
- 331.Xu J., Xu N., Zhou T., Xiao X., Gao B., Fu J., Zhang T. Polydopamine coatings embedded with silver nanoparticles on nanostructured titania for long-lasting antibacterial effect. Surf. Coat. Technol. 2017;320:608–613. doi: 10.1016/j.surfcoat.2016.10.065. [DOI] [Google Scholar]
- 332.Jiang S., Liu X., Liu Y., Liu J., He W., Dong Y. Synthesis of silver @hydroxyapatite nanoparticles based biocomposite and their assessment for viability of Osseointegration for rabbit knee joint anterior cruciate ligament rehabilitation. J. Photochem. Photobiol. B Biol. 2020;202:111677. doi: 10.1016/j.jphotobiol.2019.111677. [DOI] [PubMed] [Google Scholar]
- 333.Grumezescu A.M., Stoica A.E., Dima-Balcescu M.S., Chircov C., Gharbia S., Balta C., Rosu M., Herman H., Holban A.M., Ficai A., et al. Electrospun Polyethylene Terephthalate Nanofibers Loaded with Silver Nanoparticles: Novel Approach in Anti-Infective Therapy. J. Clin. Med. 2019;8:1039. doi: 10.3390/jcm8071039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Ziabka M., Dziadek M., Menaszek E. Biocompatibility of Poly(acrylonitrile-butadiene-styrene) Nanocomposites Modified with Silver Nanoparticles. Polymers. 2018;10:1257. doi: 10.3390/polym10111257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Ziabka M., Dziadek M. Long-Term Stability of Two Thermoplastic Polymers Modified with Silver Nanoparticles. Nanomaterials. 2019;9:61. doi: 10.3390/nano9010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Kumar N., Desagani D., Chandran G., Ghosh N.N., Karthikeyan G., Waigaonkar S., Ganguly A. Biocompatible agarose-chitosan coated silver nanoparticle composite for soft tissue engineering applications. Artif. Cells Nanomed. Biotechnol. 2018;46:637–649. doi: 10.1080/21691401.2017.1337021. [DOI] [PubMed] [Google Scholar]
- 337.Hosseini H., Zirakjou A., Goodarzi V., Mousavi S.M., Khonakdar H.A., Zamanlui S. Lightweight aerogels based on bacterial cellulose/silver nanoparticles/polyaniline with tuning morphology of polyaniline and application in soft tissue engineering. Int. J. Biol. Macromol. 2020;152:57–67. doi: 10.1016/j.ijbiomac.2020.02.095. [DOI] [PubMed] [Google Scholar]
- 338.Farrage N.M., Oraby A.H., Abdelrazek E.M.M., Atta D. Synthesis, characterization of Ag@PANI core-shell nanostructures using solid state polymerization method. Biointerface Res. Appl. Chem. 2019;9:3934–3941. doi: 10.33263/BRIAC93.934941. [DOI] [Google Scholar]
- 339.Howaili F., Mashreghi M., Shahri N.M., Kompany A., Jalal R. Development and evaluation of a novel beneficent antimicrobial bioscaffold based on animal waste-fish swim bladder (FSB) doped with silver nanoparticles. Environ. Res. 2020;188:109823. doi: 10.1016/j.envres.2020.109823. [DOI] [PubMed] [Google Scholar]
- 340.Saleh T., Ahmed E., Yu L., Kwak H.H., Kang B.J., Park K.M., Choi K.Y., Kim B.M., Kang K.S., Woo H.M. Characterization of silver nanoparticle-modified decellularized rat esophagus for esophageal tissue engineering: Structural properties and biocompatibility. J. Biosci. Bioeng. 2019;128:613–621. doi: 10.1016/j.jbiosc.2019.04.017. [DOI] [PubMed] [Google Scholar]
- 341.Niu X., Wei Y., Liu Q., Yang B., Ma N., Li Z., Zhao L., Chen W., Huang D. Silver-loaded microspheres reinforced chitosan scaffolds for skin tissue engineering. Eur. Polym. J. 2020;134:109861. doi: 10.1016/j.eurpolymj.2020.109861. [DOI] [Google Scholar]
- 342.Ran L., Zou Y., Cheng J., Lu F. Silver nanoparticles in situ synthesized by polysaccharides from Sanghuangporus sanghuang and composites with chitosan to prepare scaffolds for the regeneration of infected full-thickness skin defects. Int. J. Biol. Macromol. 2019;125:392–403. doi: 10.1016/j.ijbiomac.2018.12.052. [DOI] [PubMed] [Google Scholar]
- 343.Srivastava C.M., Purwar R., Gupta A.P. Enhanced potential of biomimetic, silver nanoparticles functionalized Antheraea mylitta (tasar) silk fibroin nanofibrous mats for skin tissue engineering. Int. J. Biol. Macromol. 2019;130:437–453. doi: 10.1016/j.ijbiomac.2018.12.255. [DOI] [PubMed] [Google Scholar]
- 344.Talodthaisong C., Boonta W., Thammawithan S., Patramanon R., Kamonsutthipaijit N., Hutchison J.A., Kulchat S. Composite guar gum-silver nanoparticle hydrogels as self-healing, injectable, and antibacterial biomaterials. Mater. Today Commun. 2020;24:100992. doi: 10.1016/j.mtcomm.2020.100992. [DOI] [Google Scholar]
- 345.Pham T.N., Jiang Y.S., Su C.F., Jan J.S. In situ formation of silver nanoparticles-contained gelatin-PEG-dopamine hydrogels via enzymatic cross-linking reaction for improved antibacterial activities. Int. J. Biol. Macromol. 2020;146:1050–1059. doi: 10.1016/j.ijbiomac.2019.09.230. [DOI] [PubMed] [Google Scholar]
- 346.Ounkaew A., Kasemsiri P., Jetsrisuparb K., Uyama H., Hsu Y.I., Boonmars T., Artchayasawat A., Knijnenburg J.T.N., Chindaprasirt P. Synthesis of nanocomposite hydrogel based carboxymethyl starch/polyvinyl alcohol/nanosilver for biomedical materials. Carbohydr. Polym. 2020;248:116767. doi: 10.1016/j.carbpol.2020.116767. [DOI] [PubMed] [Google Scholar]
- 347.Velnar T., Gradisnik L. Tissue Augmentation in Wound Healing: The Role of Endothelial and Epithelial Cells. Med. Arch. 2018;72:444–448. doi: 10.5455/medarh.2018.72.444-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Negut I., Grumezescu V., Grumezescu A.M. Treatment Strategies for Infected Wounds. Molecules. 2018;23:2392. doi: 10.3390/molecules23092392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Velnar T., Bailey T., Smrkolj V. The Wound Healing Process: An Overview of the Cellular and Molecular Mechanisms. J. Int. Med. Res. 2009;37:1528–1542. doi: 10.1177/147323000903700531. [DOI] [PubMed] [Google Scholar]
- 350.Rodrigues M., Kosaric N., Bonham C.A., Gurtner G.C. Wound Healing: A cellular perspective. Physiol. Rev. 2018;99:665–706. doi: 10.1152/physrev.00067.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Atiyeh B.S., Costagliola M. Cultured epithelial autograft (CEA) in burn treatment: Three decades later. Burns. 2007;33:405–413. doi: 10.1016/j.burns.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 352.Diegidio P., Hermiz S.J., Ortiz-Pujols S., Jones S.W., van Duin D., Weber D.J., Cairns B.A., Hultman C.S. Even Better Than the Real Thing? Xenografting in Pediatric Patients with Scald Injury. Clin. Plast. Surg. 2017;44:651–656. doi: 10.1016/j.cps.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 353.Eggleton P., Bishop A., Smerdon G. Safety and efficacy of hyperbaric oxygen therapy in chronic wound management: Current evidence. Chronic Wound Care Manag. Res. 2015;2:81–93. doi: 10.2147/cwcmr.s60319. [DOI] [Google Scholar]
- 354.Kaufman H., Gurevich M., Tamir E., Keren E., Alexander L., Hayes P. Topical oxygen therapy stimulates healing in difficult, chronic wounds: A tertiary centre experience. J. Wound Care. 2018;27:426–433. doi: 10.12968/jowc.2018.27.7.426. [DOI] [PubMed] [Google Scholar]
- 355.Lima R.V.K.S., Coltro P.S., Farina JÚNior J.A. Negative pressure therapy for the treatment of complex wounds. Rev. Colégio Bras. Cir. 2017;44:81–93. doi: 10.1590/0100-69912017001001. [DOI] [PubMed] [Google Scholar]
- 356.Sexton F., Healy D., Keelan S., Alazzawi M., Naughton P. A systematic review and meta-analysis comparing the effectiveness of negative-pressure wound therapy to standard therapy in the prevention of complications after vascular surgery. Int. J. Surg. 2020;76:94–100. doi: 10.1016/j.ijsu.2020.02.037. [DOI] [PubMed] [Google Scholar]
- 357.Ousey K., Cutting K.F., Rogers A.A., Rippon M.G. The importance of hydration in wound healing: Reinvigorating the clinical perspective. J. Wound Care. 2016;25:124–130. doi: 10.12968/jowc.2016.25.3.122. [DOI] [PubMed] [Google Scholar]
- 358.Han G., Ceilley R. Chronic Wound Healing: A Review of Current Management and Treatments. Adv. Ther. 2017;34:599–610. doi: 10.1007/s12325-017-0478-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Stoica A.E., Chircov C., Grumezescu A.M. Nanomaterials for Wound Dressings: An Up-to-Date Overview. Molecules. 2020;25:2699. doi: 10.3390/molecules25112699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Wu Y.K., Cheng N.C., Cheng C.M. Biofilms in Chronic Wounds: Pathogenesis and Diagnosis. Trends Biotechnol. 2019;37:505–517. doi: 10.1016/j.tibtech.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 361.Milne K.E., Penn-Barwell J.G. Classification and management of acute wounds and open fractures. Surgery. 2020;38:143–149. doi: 10.1016/j.mpsur.2020.01.010. [DOI] [Google Scholar]
- 362.Liu X., Nielsen L.H., Klodzinska S.N., Nielsen H.M., Qu H., Christensen L.P., Rantanen J., Yang M. Ciprofloxacin-loaded sodium alginate/poly (lactic-co-glycolic acid) electrospun fibrous mats for wound healing. Eur. J. Pharm. Biopharm. 2018;123:42–49. doi: 10.1016/j.ejpb.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 363.Michalska-Sionkowska M., Kaczmarek B., Walczak M., Sionkowska A. Antimicrobial activity of new materials based on the blends of collagen/chitosan/hyaluronic acid with gentamicin sulfate addition. Mater. Sci. Eng. C Mater. Biol. Appl. 2018;86:103–108. doi: 10.1016/j.msec.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 364.Gunes S., Tihminlioglu F. Hypericum perforatum incorporated chitosan films as potential bioactive wound dressing material. Int. J. Biol. Macromol. 2017;102:933–943. doi: 10.1016/j.ijbiomac.2017.04.080. [DOI] [PubMed] [Google Scholar]
- 365.Altaf F., Niazi M.B.K., Jahan Z., Ahmad T., Akram M.A., Safdar A., Butt M.S., Noor T., Sher F. Synthesis and Characterization of PVA/Starch Hydrogel Membranes Incorporating Essential Oils Aimed to be Used in Wound Dressing Applications. J. Polym. Environ. 2020 doi: 10.1007/s10924-020-01866-w. [DOI] [Google Scholar]
- 366.Radulescu M., Andronescu E., Dolete G., Popescu R.C., Fufa O., Chifiriuc M.C., Mogoanta L., Balseanu T.A., Mogosanu G.D., Grumezescu A.M., et al. Silver Nanocoatings for Reducing the Exogenous Microbial Colonization of Wound Dressings. Materials. 2016;9:345. doi: 10.3390/ma9050345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Balaure P.C., Holban A.M., Grumezescu A.M., Mogosanu G.D., Balseanu T.A., Stan M.S., Dinischiotu A., Volceanov A., Mogoanta L. In vitro and in vivo studies of novel fabricated bioactive dressings based on collagen and zinc oxide 3D scaffolds. Int. J. Pharm. 2019;557:199–207. doi: 10.1016/j.ijpharm.2018.12.063. [DOI] [PubMed] [Google Scholar]
- 368.Wang K., Qi Z., Pan S., Zheng S., Wang H., Chang Y., Li H., Xue P., Yang X., Fu C. Preparation, characterization and evaluation of a new film based on chitosan, arginine and gold nanoparticle derivatives for wound-healing efficacy. RSC Adv. 2020;10:20886–20899. doi: 10.1039/d0ra03704d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Yapijakis C. Hippocrates of Kos, the father of clinical medicine, and Asclepiades of Bithynia, the father of molecular medicine. Review. In Vivo. 2009;23:507–514. [PubMed] [Google Scholar]
- 370.Alexander J.W. History of the Medical use of Silver. Surg. Infect. 2009;10:289–292. doi: 10.1089/sur.2008.9941. [DOI] [PubMed] [Google Scholar]
- 371.Nam G., Purushothaman B., Rangasamy S., Song J.M. Investigating the versatility of multifunctional silver nanoparticles: Preparation and inspection of their potential as wound treatment agents. Int. Nano Lett. 2015;6:51–63. doi: 10.1007/s40089-015-0168-1. [DOI] [Google Scholar]
- 372.Nherera L., Trueman P., Roberts C., Berg L. Cost-effectiveness Analysis of Silver Delivery Approaches in the Management of Partial-thickness Burns. Wounds Compend. Clin. Res. Pract. 2018;30:160–167. [PubMed] [Google Scholar]
- 373.Chae J.K., Kim J.H., Kim E.J., Park K. Values of a patient and observer scar assessment scale to evaluate the facial skin graft scar. Ann. Dermatol. 2016;28:615–623. doi: 10.5021/ad.2016.28.5.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Khansa I., Schoenbrunner A.R., Kraft C.T., Janis J.E. Silver in Wound Care-Friend or Foe: A Comprehensive Review. Plast. Reconstr. Surg. Glob. Open. 2019;7:e2390. doi: 10.1097/GOX.0000000000002390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Rahimi M., Noruzi E.B., Sheykhsaran E., Ebadi B., Kariminezhad Z., Molaparast M., Mehrabani M.G., Mehramouz B., Yousefi M., Ahmadi R., et al. Carbohydrate polymer-based silver nanocomposites: Recent progress in the antimicrobial wound dressings. Carbohydr. Polym. 2020;231:115696. doi: 10.1016/j.carbpol.2019.115696. [DOI] [PubMed] [Google Scholar]
- 376.Tian X., Jiang X., Welch C., Croley T.R., Wong T.Y., Chen C., Fan S., Chong Y., Li R., Ge C. Bactericidal effects of silver nanoparticles on lactobacilli and the underlying mechanism. ACS Appl. Mater. Interfaces. 2018;10:8443–8450. doi: 10.1021/acsami.7b17274. [DOI] [PubMed] [Google Scholar]
- 377.Paladini F., Pollini M. Antimicrobial Silver Nanoparticles for Wound Healing Application: Progress and Future Trends. Materials. 2019;12:2540. doi: 10.3390/ma12162540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Hassabo A.G., El-Naggar M.E., Mohamed A.L., Hebeish A.A. Development of multifunctional modified cotton fabric with tri-component nanoparticles of silver, copper and zinc oxide. Carbohydr. Polym. 2019;210:144–156. doi: 10.1016/j.carbpol.2019.01.066. [DOI] [PubMed] [Google Scholar]
- 379.Montagut A.M., Granados A., Ballesteros A., Pleixats R., Llagostera M., Cortés P., Sebastián R.M., Vallribera A. Antibiotic protected silver nanoparticles for microbicidal cotton. Tetrahedron. 2019;75:102–108. doi: 10.1016/j.tet.2018.11.035. [DOI] [Google Scholar]
- 380.Baygar T., Sarac N., Ugur A., Karaca I.R. Antimicrobial characteristics and biocompatibility of the surgical sutures coated with biosynthesized silver nanoparticles. Bioorg. Chem. 2019;86:254–258. doi: 10.1016/j.bioorg.2018.12.034. [DOI] [PubMed] [Google Scholar]
- 381.Syukri D.M., Nwabor O.F., Singh S., Ontong J.C., Wunnoo S., Paosen S., Munah S., Voravuthikunchai S.P. Antibacterial-coated silk surgical sutures by ex situ deposition of silver nanoparticles synthesized with Eucalyptus camaldulensis eradicates infections. J. Microbiol. Methods. 2020;174:105955. doi: 10.1016/j.mimet.2020.105955. [DOI] [PubMed] [Google Scholar]
- 382.Xu Q., Zheng W., Duan P., Chen J., Zhang Y., Fu F., Diao H., Liu X. One-pot fabrication of durable antibacterial cotton fabric coated with silver nanoparticles via carboxymethyl chitosan as a binder and stabilizer. Carbohydr. Polym. 2019;204:42–49. doi: 10.1016/j.carbpol.2018.09.089. [DOI] [PubMed] [Google Scholar]
- 383.Gadkari R.R., Ali S.W., Joshi M., Rajendran S., Das A., Alagirusamy R. Leveraging antibacterial efficacy of silver loaded chitosan nanoparticles on layer-by-layer self-assembled coated cotton fabric. Int. J. Biol. Macromol. 2020;162:548–560. doi: 10.1016/j.ijbiomac.2020.06.137. [DOI] [PubMed] [Google Scholar]
- 384.López-Saucedo F., Flores-Rojas G.G., López-Saucedo J., Magariños B., Alvarez-Lorenzo C., Concheiro A., Bucio E. Antimicrobial silver-loaded polypropylene sutures modified by radiation-grafting. Eur. Polym. J. 2018;100:290–297. doi: 10.1016/j.eurpolymj.2018.02.005. [DOI] [Google Scholar]
- 385.Chen J., Fan L., Yang C., Wang S., Zhang M., Xu J., Luo S. Facile synthesis of Ag nanoparticles-loaded chitosan antibacterial nanocomposite and its application in polypropylene. Int. J. Biol. Macromol. 2020;161:1286–1295. doi: 10.1016/j.ijbiomac.2020.07.151. [DOI] [PubMed] [Google Scholar]
- 386.Pagnotta G., Graziani G., Baldini N., Maso A., Focarete M.L., Berni M., Biscarini F., Bianchi M., Gualandi C. Nanodecoration of electrospun polymeric fibers with nanostructured silver coatings by ionized jet deposition for antibacterial tissues. Mater. Sci. Eng. C Mater. Biol. Appl. 2020;113:110998. doi: 10.1016/j.msec.2020.110998. [DOI] [PubMed] [Google Scholar]
- 387.Ross J.A., Allan N., Olson M., Schatz C., Nation P.N., Gawaziuk J.P., Sethi J., Liu S., Logsetty S. Comparison of the efficacy of silver-based antimicrobial burn dressings in a porcine model of burn wounds. Burns. 2020 doi: 10.1016/j.burns.2020.04.004. [DOI] [PubMed] [Google Scholar]
- 388.Vasile B.S., Birca A.C., Musat M.C., Holban A.M. Wound Dressings Coated with Silver Nanoparticles and Essential Oils for The Management of Wound Infections. Materials. 2020;13:1682. doi: 10.3390/ma13071682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Ying W., Tan J., Chen C., Sun T., Wang S., Zhang M. Biofabrication of silver nanoparticles and its application for development of wound dressing system in nursing care for burn injuries in children. J. Drug Deliv. Sci. Technol. 2019;54:101236. doi: 10.1016/j.jddst.2019.101236. [DOI] [Google Scholar]
- 390.Mohamed N., Madian N.G. Evaluation of the mechanical, physical and antimicrobial properties of chitosan thin films doped with greenly synthesized silver nanoparticles. Mater. Today Commun. 2020;25:101372. doi: 10.1016/j.mtcomm.2020.101372. [DOI] [Google Scholar]
- 391.Mohamed N., Madian N.G. Enhancement of the dynamic mechanical properties of chitosan thin films by crosslinking with greenly synthesized silver nanoparticles. J. Mater. Res. Technol. 2020;9:12970–12975. doi: 10.1016/j.jmrt.2020.09.028. [DOI] [Google Scholar]
- 392.Hernandez-Rangel A., Silva-Bermudez P., Espana-Sanchez B.L., Luna-Hernandez E., Almaguer-Flores A., Ibarra C., Garcia-Perez V.I., Velasquillo C., Luna-Barcenas G. Fabrication and in vitro behavior of dual-function chitosan/silver nanocomposites for potential wound dressing applications. Mater. Sci. Eng. C Mater. Biol. Appl. 2019;94:750–765. doi: 10.1016/j.msec.2018.10.012. [DOI] [PubMed] [Google Scholar]
- 393.Rahimi M., Ahmadi R., Kafil H.S., Shafiei-Irannejad V. A novel bioactive quaternized chitosan and its silver-containing nanocomposites as a potent antimicrobial wound dressing: Structural and biological properties. Mater. Sci. Eng. C. 2019;101:360–369. doi: 10.1016/j.msec.2019.03.092. [DOI] [PubMed] [Google Scholar]
- 394.Ambrogi V., Pietrella D., Donnadio A., Latterini L., Di Michele A., Luffarelli I., Ricci M. Biocompatible alginate silica supported silver nanoparticles composite films for wound dressing with antibiofilm activity. Mater. Sci. Eng. C. 2020;112:110863. doi: 10.1016/j.msec.2020.110863. [DOI] [PubMed] [Google Scholar]
- 395.Tarusha L., Paoletti S., Travan A., Marsich E. Alginate membranes loaded with hyaluronic acid and silver nanoparticles to foster tissue healing and to control bacterial contamination of non-healing wounds. J. Mater. Sci. Mater. Med. 2018;29:22. doi: 10.1007/s10856-018-6027-7. [DOI] [PubMed] [Google Scholar]
- 396.El-Aassar M.R., Ibrahim O.M., Fouda M.M.G., El-Beheri N.G., Agwa M.M. Wound healing of nanofiber comprising Polygalacturonic/Hyaluronic acid embedded silver nanoparticles: In-vitro and in-vivo studies. Carbohydr. Polym. 2020;238:116175. doi: 10.1016/j.carbpol.2020.116175. [DOI] [PubMed] [Google Scholar]
- 397.Shah S.A., Sohail M., Khan S., Minhas M.U., de Matas M., Sikstone V., Hussain Z., Abbasi M., Kousar M. Biopolymer-based biomaterials for accelerated diabetic wound healing: A critical review. Int. J. Biol. Macromol. 2019;139:975–993. doi: 10.1016/j.ijbiomac.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 398.Stoica A.E., Chircov C., Grumezescu A.M. Hydrogel Dressings for the Treatment of Burn Wounds: An Up-To-Date Overview. Materials. 2020;13:2853. doi: 10.3390/ma13122853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Zhang A., Liu Y., Qin D., Sun M., Wang T., Chen X. Research status of self-healing hydrogel for wound management: A review. Int. J. Biol. Macromol. 2020 doi: 10.1016/j.ijbiomac.2020.08.109. [DOI] [PubMed] [Google Scholar]
- 400.Xie Y., Liao X., Zhang J., Yang F., Fan Z. Novel chitosan hydrogels reinforced by silver nanoparticles with ultrahigh mechanical and high antibacterial properties for accelerating wound healing. Int. J. Biol. Macromol. 2018;119:402–412. doi: 10.1016/j.ijbiomac.2018.07.060. [DOI] [PubMed] [Google Scholar]
- 401.Nešović K., Janković A., Radetić T., Vukašinović-Sekulić M., Kojić V., Živković L., Perić-Grujić A., Rhee K.Y., Mišković-Stanković V. Chitosan-based hydrogel wound dressings with electrochemically incorporated silver nanoparticles—In vitro study. Eur. Polym. J. 2019;121:109257. doi: 10.1016/j.eurpolymj.2019.109257. [DOI] [Google Scholar]
- 402.Yang J., Chen Y., Zhao L., Feng Z., Peng K., Wei A., Wang Y., Tong Z., Cheng B. Preparation of a chitosan/carboxymethyl chitosan/AgNPs polyelectrolyte composite physical hydrogel with self-healing ability, antibacterial properties, and good biosafety simultaneously, and its application as a wound dressing. Compos. Part B Eng. 2020;197:108139. doi: 10.1016/j.compositesb.2020.108139. [DOI] [Google Scholar]
- 403.Diniz F.R., Maia R., Rannier L., Andrade L.N., Chaud M.V., da Silva C.F., Correa C.B., de Albuquerque Junior R.L.C., de Costa L.P., Shin S.R., et al. Silver Nanoparticles-Composing Alginate/Gelatine Hydrogel Improves Wound Healing In Vivo. Nanomaterials. 2020;10:390. doi: 10.3390/nano10020390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Ahsan A., Farooq M.A. Therapeutic potential of green synthesized silver nanoparticles loaded PVA hydrogel patches for wound healing. J. Drug Deliv. Sci. Technol. 2019;54:101308. doi: 10.1016/j.jddst.2019.101308. [DOI] [Google Scholar]
- 405.Batool S., Hussain Z., Niazi M.B.K., Liaqat U., Afzal M. Biogenic synthesis of silver nanoparticles and evaluation of physical and antimicrobial properties of Ag/PVA/starch nanocomposites hydrogel membranes for wound dressing application. J. Drug Deliv. Sci. Technol. 2019;52:403–414. doi: 10.1016/j.jddst.2019.05.016. [DOI] [Google Scholar]
- 406.Jaiswal L., Shankar S., Rhim J.W., Hahm D.H. Lignin-mediated green synthesis of AgNPs in carrageenan matrix for wound dressing applications. Int. J. Biol. Macromol. 2020;159:859–869. doi: 10.1016/j.ijbiomac.2020.05.145. [DOI] [PubMed] [Google Scholar]
- 407.Alvarado-Gomez E., Martínez-Castañon G., Sanchez-Sanchez R., Ganem-Rondero A., Yacaman M.J., Martinez-Gutierrez F. Evaluation of anti-biofilm and cytotoxic effect of a gel formulation with Pluronic F-127 and silver nanoparticles as a potential treatment for skin wounds. Mater. Sci. Eng. C. 2018;92:621–630. doi: 10.1016/j.msec.2018.07.023. [DOI] [PubMed] [Google Scholar]
- 408.Negut I., Dorcioman G., Grumezescu V. Scaffolds for Wound Healing Applications. Polymers. 2020;12:2010. doi: 10.3390/polym12092010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Natarajan D., Kiran M.S. Fabrication of juglone functionalized silver nanoparticle stabilized collagen scaffolds for pro-wound healing activities. Int. J. Biol. Macromol. 2019;124:1002–1015. doi: 10.1016/j.ijbiomac.2018.11.221. [DOI] [PubMed] [Google Scholar]
- 410.Bergonzi C., Remaggi G., Graiff C., Bergamonti L., Potenza M., Ossiprandi M.C., Zanotti I., Bernini F., Bettini R., Elviri L. Three-Dimensional (3D) Printed Silver Nanoparticles/Alginate/Nanocrystalline Cellulose Hydrogels: Study of the Antimicrobial and Cytotoxicity Efficacy. Nanomaterials. 2020;10:844. doi: 10.3390/nano10050844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.Jiji S., Udhayakumar S., Maharajan K., Rose C., Muralidharan C., Kadirvelu K. Bacterial cellulose matrix with in situ impregnation of silver nanoparticles via catecholic redox chemistry for third degree burn wound healing. Carbohydr. Polym. 2020;245:116573. doi: 10.1016/j.carbpol.2020.116573. [DOI] [PubMed] [Google Scholar]
- 412.Sofi H.S., Akram T., Tamboli A.H., Majeed A., Shabir N., Sheikh F.A. Novel lavender oil and silver nanoparticles simultaneously loaded onto polyurethane nanofibers for wound-healing applications. Int. J. Pharm. 2019;569:118590. doi: 10.1016/j.ijpharm.2019.118590. [DOI] [PubMed] [Google Scholar]
- 413.Pansara C., Mishra R., Mehta T., Parikh A., Garg S. Formulation of Chitosan Stabilized Silver Nanoparticle-Containing Wound Healing Film: In Vitro and In Vivo Characterization. J. Pharm. Sci. 2020;109:2196–2205. doi: 10.1016/j.xphs.2020.03.028. [DOI] [PubMed] [Google Scholar]
- 414.Shah A., Ali Buabeid M., Arafa E.A., Hussain I., Li L., Murtaza G. The wound healing and antibacterial potential of triple-component nanocomposite (chitosan-silver-sericin) films loaded with moxifloxacin. Int. J. Pharm. 2019;564:22–38. doi: 10.1016/j.ijpharm.2019.04.046. [DOI] [PubMed] [Google Scholar]
- 415.Shao J., Wang B., Li J., Jansen J.A., Walboomers X.F., Yang F. Antibacterial effect and wound healing ability of silver nanoparticles incorporation into chitosan-based nanofibrous membranes. Mater. Sci. Eng. C Mater. Biol. Appl. 2019;98:1053–1063. doi: 10.1016/j.msec.2019.01.073. [DOI] [PubMed] [Google Scholar]
- 416.Jiang Y., Huang J., Wu X., Ren Y., Li Z., Ren J. Controlled release of silver ions from AgNPs using a hydrogel based on konjac glucomannan and chitosan for infected wounds. Int. J. Biol. Macromol. 2020;149:148–157. doi: 10.1016/j.ijbiomac.2020.01.221. [DOI] [PubMed] [Google Scholar]
- 417.Li R., Xu Z., Jiang Q., Zheng Y., Chen Z., Chen X. Characterization and biological evaluation of a novel silver nanoparticle-loaded collagen-chitosan dressing. Regen. Biomater. 2020;7:371–380. doi: 10.1093/rb/rbaa008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Preethi G.U., Unnikrishnan B.S., Sreekutty J., Archana M.G., Anupama M.S., Shiji R., Raveendran Pillai K., Joseph M.M., Syama H.P., Sreelekha T.T. Semi-interpenetrating nanosilver doped polysaccharide hydrogel scaffolds for cutaneous wound healing. Int. J. Biol. Macromol. 2020;142:712–723. doi: 10.1016/j.ijbiomac.2019.10.012. [DOI] [PubMed] [Google Scholar]
- 419.Balakrishnan S.B., Thambusamy S. Preparation of silver nanoparticles and riboflavin embedded electrospun polymer nanofibrous scaffolds for in vivo wound dressing application. Process Biochem. 2020;88:148–158. doi: 10.1016/j.procbio.2019.09.033. [DOI] [Google Scholar]
- 420.Alipour R., Khorshidi A., Shojaei A.F., Mashayekhi F., Moghaddam M.J.M. Skin wound healing acceleration by Ag nanoparticles embedded in PVA/PVP/Pectin/Mafenide acetate composite nanofibers. Polym. Test. 2019;79:106022. doi: 10.1016/j.polymertesting.2019.106022. [DOI] [Google Scholar]
- 421.Mohseni M., Shamloo A., Aghababaie Z., Afjoul H., Abdi S., Moravvej H., Vossoughi M. A comparative study of wound dressings loaded with silver sulfadiazine and silver nanoparticles: In vitro and in vivo evaluation. Int. J. Pharm. 2019;564:350–358. doi: 10.1016/j.ijpharm.2019.04.068. [DOI] [PubMed] [Google Scholar]
- 422.Esmaeili E., Eslami-Arshaghi T., Hosseinzadeh S., Elahirad E., Jamalpoor Z., Hatamie S., Soleimani M. The biomedical potential of cellulose acetate/polyurethane nanofibrous mats containing reduced graphene oxide/silver nanocomposites and curcumin: Antimicrobial performance and cutaneous wound healing. Int. J. Biol. Macromol. 2020;152:418–427. doi: 10.1016/j.ijbiomac.2020.02.295. [DOI] [PubMed] [Google Scholar]
- 423.Namviriyachote N., Lipipun V., Akkhawattanangkul Y., Charoonrut P., Ritthidej G.C. Development of polyurethane foam dressing containing silver and asiaticoside for healing of dermal wound. Asian J. Pharm. Sci. 2019;14:63–77. doi: 10.1016/j.ajps.2018.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.Dewi F., Hinchliffe R.J. Foot complications in patients with diabetes. Surgery. 2020;38:108–113. doi: 10.1016/j.mpsur.2019.12.002. [DOI] [Google Scholar]
- 425.Hajji S., Khedir S.B., Hamza-Mnif I., Hamdi M., Jedidi I., Kallel R., Boufi S., Nasri M. Biomedical potential of chitosan-silver nanoparticles with special reference to antioxidant, antibacterial, hemolytic and in vivo cutaneous wound healing effects. Biochim. Biophys. Acta Gen. Subj. 2019;1863:241–254. doi: 10.1016/j.bbagen.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 426.Parthasarathy A., Vijayakumar S., Malaikozhundan B., Thangaraj M.P., Ekambaram P., Murugan T., Velusamy P., Anbu P., Vaseeharan B. Chitosan-coated silver nanoparticles promoted antibacterial, antibiofilm, wound-healing of murine macrophages and antiproliferation of human breast cancer MCF 7 cells. Polym. Test. 2020;90:106675. doi: 10.1016/j.polymertesting.2020.106675. [DOI] [Google Scholar]
- 427.Choudhury H., Pandey M., Lim Y.Q., Low C.Y., Lee C.T., Marilyn T.C.L., Loh H.S., Lim Y.P., Lee C.F., Bhattamishra S.K., et al. Silver nanoparticles: Advanced and promising technology in diabetic wound therapy. Mater. Sci. Eng. C Mater. Biol. Appl. 2020;112:110925. doi: 10.1016/j.msec.2020.110925. [DOI] [PubMed] [Google Scholar]
- 428.Kuwabara M., Sato Y., Ishihara M., Takayama T., Nakamura S., Fukuda K., Murakami K., Yokoe H., Kiyosawa T. Healing of Pseudomonas aeruginosa-infected wounds in diabetic db/db mice by weakly acidic hypochlorous acid cleansing and silver nanoparticle/chitin-nanofiber sheet covering. Wound Med. 2020;28:100183. doi: 10.1016/j.wndm.2020.100183. [DOI] [Google Scholar]
- 429.Shi G., Chen W., Zhang Y., Dai X., Zhang X., Wu Z. An Antifouling Hydrogel Containing Silver Nanoparticles for Modulating the Therapeutic Immune Response in Chronic Wound Healing. Langmuir. 2019;35:1837–1845. doi: 10.1021/acs.langmuir.8b01834. [DOI] [PubMed] [Google Scholar]
- 430.Masood N., Ahmed R., Tariq M., Ahmed Z., Masoud M.S., Ali I., Asghar R., Andleeb A., Hasan A. Silver nanoparticle impregnated chitosan-PEG hydrogel enhances wound healing in diabetes induced rabbits. Int. J. Pharm. 2019;559:23–36. doi: 10.1016/j.ijpharm.2019.01.019. [DOI] [PubMed] [Google Scholar]