Abstract
Protein phosphorylation is a post-translational modification essential for the control of the activity of most enzymes in the cell. This protein modification results from a fine-tuned balance between kinases and phosphatases. PP2A is one of the major serine/threonine phosphatases that is involved in the control of a myriad of different signaling cascades. This enzyme, often misregulated in cancer, is considered a tumor suppressor. In this review, we will focus on PP2A-B55, a particular holoenzyme of the family of the PP2A phosphatases whose specific role in cancer development and progression has only recently been highlighted. The discovery of the Greatwall (Gwl)/Arpp19-ENSA cascade, a new pathway specifically controlling PP2A-B55 activity, has been shown to be frequently altered in cancer. Herein, we will review the current knowledge about the mechanisms controlling the formation and the regulation of the activity of this phosphatase and its misregulation in cancer.
Keywords: PP2A-B55, cancer, Greatwall, Arpp19, ENSA
1. Introduction
Most cellular processes are regulated by protein phosphorylation. This post-translational modification allows cells to react rapidly to the external environment by controlling the activity, localization, and substrate specificity of enzymes involved in most cell signaling pathways. Protein phosphorylation results from a fine-tuned balance between kinases and phosphatases, the disruption of which can lead to altered cellular behavior and many diseases including cancer. Despite their abundance, owing to conserved structural features, kinases have been the target of the cancer research field for decades. Deregulation of kinase activity has emerged as a major mechanism by which cancer cells evade normal physiological constraints on growth and survival. A considerable number of chemical inhibitors targeting these enzymes have been developed and have proven to be very successful in cancer therapy [1]. Nonetheless, these treatments have been limited by the development of drug resistance and/or loss of specificity [2].
Since they antagonize kinases, phosphatases are equally important for normal and tumoral cell proliferation. However, the role of these enzymes has been underestimated in the past, and phosphatases have been considered as housekeeping enzymes due to an erroneous preconceived hypothesis regarding their lack of specificity and regulation. Nevertheless, research over the last few years highlighted an essential role of phosphatase regulation in the control of cell proliferation and cancer development. These enzymes have now been identified as tumor suppressors involved in a large range of cancers [3] and have been considered as attractive targets for the development of new cancer therapies [4].
Phosphatases are classified into two different types, Protein Tyrosine Phosphatases (PTP) and serine/threonine phosphatases. The latter include three families: Phosphoprotein phosphatases (PPPs), metal-dependent protein phosphatases (PP2C), and Aspartate Based phosphatases (FCP1, SCP1) [5,6]. PPP represents the most abundant family of phosphatases in the cell and includes the members PP1, PP2A, PP2B, PP4, PP5, PP6, and PP7.
This review will focus on PP2A and more specifically PP2A-B55. This holoenzyme, tightly controlled by the cell, has an essential function in cell division and cell growth. Although it has been involved in the control of a high number of physiological cascades, its specific role in cancer development and progression has only recently been highlighted thanks to the recent identification of the Greatwall (Gwl)/Arpp19-ENSA cascade, a new pathway specifically controlling PP2A-B55 activity. Increasing data identifies Gwl, Arpp19, and ENSA as proteins commonly misregulated in a high number of cancers displaying prognostic and therapeutic value. However, although their specific role in the control of the cell cycle has been well documented [7,8,9,10,11,12,13,14,15,16], very few reviews appeared in the literature on its involvement in cancer development and progression. This review will cover the different contributions that have recently appeared on the role of Gwl, Arpp19, ENSA, and PP2A-B55 in tumoral cascades and their misregulation in cancer.
2. PP2A Structure
PP2A is a family of holoenzymes formed of three different subunits: A catalytic subunit or C subunit, a scaffold subunit or A subunit, and a regulatory subunit or B subunit, and each of them comprises several isoforms. The combination of all these subunits results in the formation of more than 90 holoenzymes. This diversity creates specificity and confers to the phosphatase the capacity to distinctively recognize and dephosphorylate a high number of proteins. Additionally, the different isoforms display a particular tissue expression and a precise subcellular localization, conferring to every single phosphatase holoenzyme a unique pattern of activity for each specific substrate.
The catalytic subunit is a globular protein ubiquitously expressed in almost all tissues that exists in two isoforms α and β. These two isoforms are encoded by two different genes (PPP2CA and PPP2CB) and display 97% of sequence similarity. However, despite this high similarity, these two isoforms appear to play a non-redundant role [17,18]. The C subunit can bind to the A subunit by its N-terminus to form a dimer, or to both the A and B subunits to form the active heterodimer enzyme.
The scaffold A subunit is composed of 15 tandem Huntington-Elongation-A subunit-TOR (HEAT) repeats forming a horseshoe-like structure that binds to the different B subunits via its C-terminus, and to the catalytic C subunits by its N-terminus [19,20]. As for the C subunit, the scaffold A subunit displays isoforms α and β, sharing 86% of sequence similarity and encoded by PPP2R1A and PPP2R1B genes, respectively.
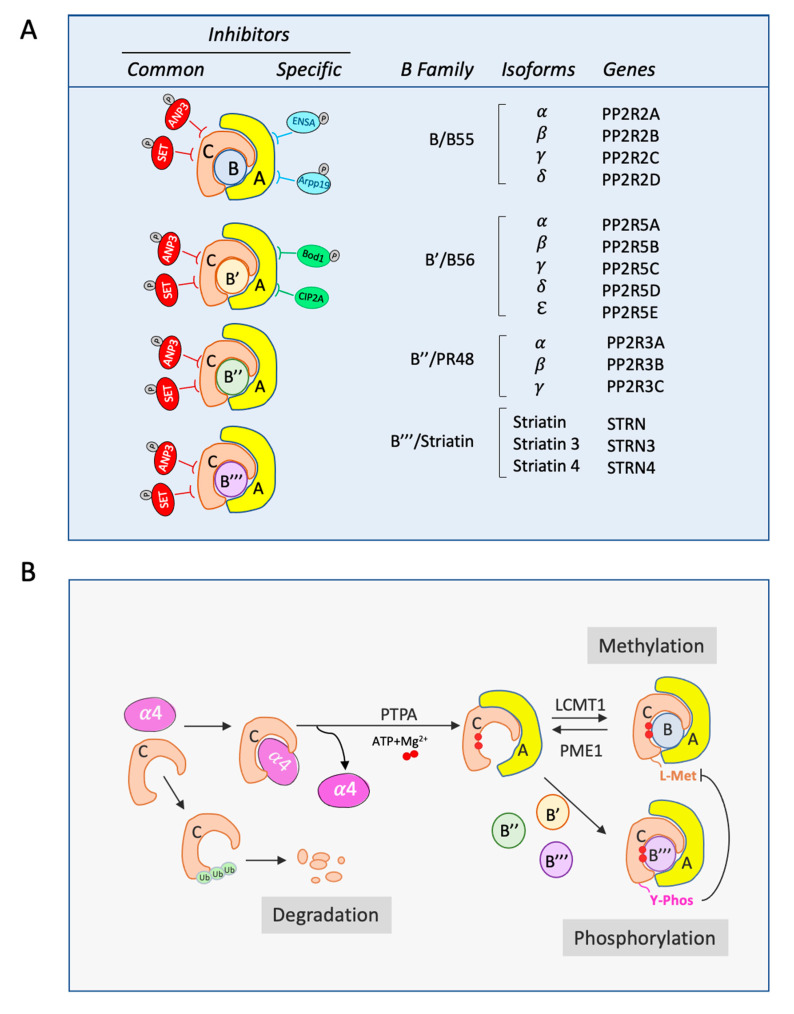
The regulatory subunit or B subunit includes four different families: B (B55/PR55), B’ (B56/PR61), B’’ (PR48/PR72/PR130), and B’’’ (PR93/PR110/Striatins). There is a low sequence similarity between the four families, and each of them can display several isoforms (Figure 1A).
Figure 1.
Composition and biogenesis of the PP2A holoenzymes. (A) Genes coding for the different isoforms of PP2A B subunits. Represented are also common and specific inhibitors of the PP2A holoenzymes. (B) Biogenesis of the PP2A complex. Monomeric C subunits binds α4 protein or is directly ubiquitinated and degraded. C/α4 complex formation mediates A/C association that will be subsequently activated by PTPA by the introduction of Mg2+ ions (red circles). This activation will permit the methylation or phosphorylation of the C subunit and the formation of PP2A-B55 or of the other holoenzymes respectively.
The B/B55 family includes isoforms α, β, γ, and δ, encoded by the genes PPP2R2A, PPP2R2B, PPP2R2C, and PPP2R2D. These isoforms are differently distributed, with α and δ widely present in most tissues, whereas β and γ are mostly enriched in the brain. Expression is specific and developmentally regulated, with B55γ increasing and B55β decreasing after birth [21]. This family of proteins are structurally composed of seven-bladed β-propellers formed of WD40 repeats. B/B55 proteins make several contacts with the HEAT domains of the A subunit (repeats 1–7), but very few contacts with the catalytic subunit [22]. The association of C/A with B/B55 to form an active holoenzyme depends on the methylation of the catalytic subunit in L309 and is inhibited by the phosphorylation of this subunit on Thr304 and Y308 [23].
The B’/B56 family is formed by α, β, γ, δ, and ε isoforms (genes PPP2R5A, PPP2R5B, PPP2R5C, PPP2R5D, and PPP2R5E). They are structurally composed of eight HEAT-like repeats similar to the A scaffold subunits. Unlike the B subunits, the B’ regulatory subunits display quite a high number of contacts not only with the A subunit but also with the C subunit.
The B’/B56 proteins can be directly modified by phosphorylation and nitrosilation, two post-translational modifications that severely impact the activity of the PP2A holoenzyme. Kinases such as MAPK or ERK can phosphorylate B56 and positively [24] or negatively [25,26] modulate PP2A-B56 activity. Conversely, the nitrosilation of these subunits induces the inhibition of the phosphatase [27].
The B’’/PR48 family contains isoforms α, β, and γ (genes PPP2R3A, PPP2R3B, and PPP2R3C). All the members of this family are composed of Ca2+-binding EF motifs, and they require the presence of calcium to bind to A/C subunits [28]. They establish several contacts with the N-terminal Heat domains of the A subunit (1–7), and their C-terminus mediates the interaction with the C subunit and acts as a substrate binding site [29].
Finally, the B’’’/Striatin family includes the proteins Striatin, Striatin 3 (or SG2NA), and Striatin 4 (or Zinedin) (genes STRN, STRN3, and STRN4) [30]. These members cannot only bind to A/C subunits of PP2A, but can also interact with other proteins, including some kinases, to form the complexes named STRIPAKs [31]. These complexes participate to the modulation of several cell signaling cascades controlling cellular events such as clathrin-dependent endocytosis, cell junction stability, golgi assembly, polarity and migration, and Ca2+ signaling [32]. The association of the different components of these STRIPAK complexes are mediated by three different domains, a caveolin/Ca2+-CaM binding domain and a coiled-coil domain present at the N-terminus, and a WD-repeat domain at the C-terminus. It is proposed that these complexes could modulate the dephosphorylation of some of their components by the PP2A-associated phosphatase.
3. PP2A Activation
During PP2A active complex formation, the C subunit is submitted to different post-translational modifications and associations to ensure the correct and selective formation of the different PP2A holoenzymes. From its synthesis, the catalytic subunit is partly bound to α4 protein (Figure 1B). This binding keeps the C subunit inactive while facilitating its assembly with A and B subunits to form the trimeric complex. Moreover, it maintains C subunit levels by preventing its ubiquitination and degradation by the proteasome [33]. The assembly of the PP2A trimeric complex continues via the loading of Mg2+ metal ions into the catalytic site. This loading, which is crucial for acquisition of the Ser/Thr-specific phosphatase activity, requires ATP hydrolysis and is mediated by the phosphotyrosil phosphatase activator (PTPA) [34]. Once the Mg2+ ions are introduced to the catalytic site, the C subunit can bind to the A scaffolding subunit. However, the former can still be submitted to different posttranslational modifications such as phosphorylation on Y307 or carboxymethylation on L309. Reversible carboxymethylation is controlled by a balance between leucine carboximethyltransferase (LCMT-1) and the reverse enzyme PP2A-specific methylesterase 1 (PME-1). As described above, this post-translation modification of the catalytic subunit positively impacts the binding of B/B55 subunits while it does not affect the association of the rest of B subunits. Accordingly, deletion of the LCMT-1 gene on S Cerevisiae results in the inhibition of Cdc55 binding to yeast PP2A-C without affecting Tpd3p (A yeast subunit) or Rts1p (B56 yeast subunit) interaction [35,36,37,38]. In the same line, in mammalian cells, decreased methylation of PP2A C subunit resulting from LCMT-1 knockdown, prevents recruitment of B55 to PP2A C but not of B56 or PR48 [39,40,41]. Finally, when immunoprecipitated, methylated C subunit is exclusively present in endogenous PP2A-B55 holoenzyme [23]. L309 carboxymethylation is counterbalanced by the phosphorylation of C subunit on Y307. As such, phosphomimetic mutants of this residue cannot be methylated and fail to bind B55.
4. PP2A Endogenous Inhibitors Regulating C Subunit and PP2A-B56
PP2A activity is modulated by several endogenous inhibitors. Although discovered almost twenty years ago [42], the mechanism of action and the specific PP2A holoenzymes targeted by these proteins have been only recently discovered. PP2A C and PP2A-B56 inhibitors include: ANP32a (or Inhibitor 1 of PP2A), SET (or Inhibitor 2 of PP2A), CIP2A, and Bod1 (Figure 1A).
ANP32a and SET were both isolated from bovine kidneys as two potent heat stable PP2A inhibitors [42]. Both proteins directly bind and inhibit the C subunit of PP2A independently of A and B subunits [43,44], and can be localized both in the nucleus and the cytoplasm. Their localization, as well as their binding to PP2A and their inhibitory activity, are modulated by phosphorylation [45,46,47]. SET stability is also controlled by its association to the SET binding protein 1 (SETBP1) [48]. ANP32a has been shown to modulate the PP2A-dependent dephosphorylation of the Tau [44] protein, whereas SET controls the dephosphorylation by this phosphatase of several substrates including Rec8 [49], ERK, AKT, c-Myc, Rb [50], PTEN [51], Mcl1 [52], and c-Jun [53]. SET can act as an oncogene, and its overexpression has been frequently detected and associated with poor prognostics in a series of cancers such as breast cancer, non-small cell lung cancer, or colorectal cancer [48,54,55]. Finally, increased mRNA levels of SET have also been associated with a poor prognosis in chronic lymphocytic leukemia [56].
CIP2A (Cancerous Inhibitor of PP2A), firstly identified as a co-precipitation partner of PP2A [57], is an inhibitor that specifically binds and inhibits the PP2A-B56 holoenzyme [58]. This inhibitor of PP2A-B56 has been shown to directly associate with and stabilize c-Myc by preventing its PP2A-B56-dependent dephosphorylation on S62 [57]. Similarly, CIP2A stabilizes E2F by preventing S364 PP2A-B56-dependent dephosphorylation and induces hyperactivation of Akt by inhibiting the dephosphorylation of S473 by this phosphatase [59,60]. CIP2A is widely overexpressed in human cancers including gastric, bladder, ovarian, tongue, hepatocellular, colon, non-small cell lung carcinoma, and chronic myelogenous leukemia, and is correlated with tumor grade [61].
As for CIP2A, Bod1 has been identified as a specific inhibitor of PP2A-B56 holoenzyme whose depletion results in changes in the phosphorylation balance at the kinetochores during mitosis, although the exact signaling pathway mediating this phenotype is unknown [62].
5. PP2A Endogenous Inhibitors Regulating PP2A-B55
Arpp19 and ENSA are the unique specific inhibitors of PP2A-B55 known so far [63,64]. Although PP2A-B55 is involved in the control of a high number of signaling cascades in the cell, due to their recent identification, little is known about the physiologic implication of these two inhibitors. Arpp19 and ENSA were first identified as two substrates of Gwl, a mitotic kinase whose activity is essential for mitotic entry and progression [65,66]. The phosphorylation of Arpp19 and ENSA by Gwl transforms these two proteins into potent inhibitors of PP2A-B55, the phosphatase identified as responsible for counterbalancing the pivotal mitotic kinase cyclin B/Cdk1 [63,64]. Gwl-mediated phosphorylation of Arpp19 and ENSA is performed at the FDSGDY sequence, a motif that is conserved in these two proteins from yeast to plants [67,68]. Data first demonstrated that this phosphorylation is essential and sufficient to promote Arpp19/ENSA-dependent PP2A-B55 inhibition and mitotic entry in interphase Xenopus egg extracts [63,64]. In the same line, the depletion of Arpp19 from mitotic Xenopus egg extracts results in mitotic exit by the re-activation of PP2A-B55 and cyclin B/Cdk1 substrate dephosphorylation [63]. A key role of these two proteins in conferring the correct temporal pattern of mitotic substrate dephosphorylation by PP2A-B55 has been reported in human and mouse cells. Accordingly, the knockdown/knockout of ENSA and Arpp19 results in dramatic mitotic defects including premature DNA decondensation and reformation of the nuclear envelope, as well as perturbed cytokinesis furrow formation [69,70,71].
Besides mitosis, Arpp19 and ENSA also control meiotic division. In this line, Arpp19 phosphorylation by PKA has been shown to be essential for prophase I arrest in Xenopus oocytes [72], whereas ENSA is required for prophase I exit in mouse oocytes [73].
Although both Arpp19 and ENSA regulate protein phosphorylation during mitosis and meiosis, they appear to perform differential roles in the control of the cell cycle of human and mouse somatic cells. This hypothesis is supported by previous results demonstrating that, whereas Arpp19 is essential for mice embryonic development by controlling mitotic division, ENSA is dispensable for mitosis and is mostly involved in normal DNA replication [70]. Accordingly, the knockdown of ENSA in human cells results in an extension of the timing of S phase consequent to the decline of the number of activated replication origins. This phenotype results from the dephosphorylation and subsequent ubiquitination and degradation of Treslin, a replication factor whose loading is essential for replication origin firing [74].
Interestingly, a new role of Gwl/Arpp19-ENSA/PP2A-B55 has also been suggested in platelet aggregation. In this model, the phosphorylation of ENSA and Arpp19 at the conserved FDSGDY motif has been demonstrated [75]. Moreover, a substitution of aspartic for glutamic acid at position 167 of the Gwl kinase was present in all the members of a thrombocytopenic family [76]. This mutation was associated with aberrant activation and survival of platelets, a phenotype that was accompanied by abnormal protein phosphorylation in these thrombocytes [77]. Further studies are required to establish the biological significance of the Gwl/Arpp19-ENSA/PP2A-B55 pathway in platelets and its impact on thrombocytopenia.
6. Signaling Cascades Regulated by PP2A-B55
PP2A-B55 regulates the activity of key proteins controlling cell growth and survival. These proteins include Akt, Ras/Mapk, Src, mTOR, and Wnt/βCatenin.
The Akt pathway is activated in response to stimuli such as insulin, growth factors, or cytokines. This activation results in the phosphorylation of two different residues of Akt, Thr308 and S473, and potentiates the pro-proliferative and pro-survival properties of this kinase [78]. PP2A-B55 holoenzyme directly dephosphorylates Thr308 and inactivates Akt, resulting in the inhibition of cell growth and survival [79].
PP2A-B55 additionally participates in both the negative and the positive modulation of the Ras/Mapk pathway by dephosphorylating three key constituents of this cascade: The Kinase Suppressor of Ras 1 scaffold protein (KSR1), Raf1, and Mekk3. In response to growth factors, PP2A-B55 binds KSR1-Raf1 complex and dephosphorylates critical 14.3.3 binding sites on these proteins. Dephosphorylation of the KSR1-Raf complex promotes its dissociation from 14.3.3 and its recruitment to the plasma membrane resulting in Mapk activation [80]. Furthermore, PP2A-B55 holoenzyme can directly dephosphorylate an activatory site of Mekk3, causing its inhibition and thus participating in the negative regulation of this cascade [81]. A negative regulation of Mapk upstream of Raf1 has also been described for PP2A-B55 by directly dephosphorylating and inactivating Src [82].
PP2A-B55 has also been shown to positively modulate the Wnt/βCatenin pathway by directly dephosphorylating and preventing the ubiquitination and degradation of βCatenin [83]. This cascade plays an essential role in embryogenesis, however its misregulation in somatic cells results in tumorigenesis [84]. By maintaining βCatenin levels in somatic cells, PP2A-B55 can participate in the tumoral activity of this pathway.
Finally, PP2A-B55 additionally participates to the control of autophagy. Autophagy is an essential property used by cancer cells to survive under high energy consumption. This property is negatively regulated by the mTOR kinase that, by phosphorylating Ulk1, prevents its subsequent activatory phosphorylation by AMPK and the autophagic response. PP2A-B55 plays a prominent role in the control of autophagy via Ulk1 dephosphorylation by indirectly modulating mTOR activity and by directly dephosphorylating mTOR-dependent phospho-residues of this protein [85].
Besides Ulk1 phosphorylation, the autophagic response is regulated by the levels of the hypoxia-inducible factors (HIFs) as well. Under hypoxic conditions, these transcription factors promote the expression of Redd1 and the Redd1-dependent dissociation of TSC1/TSC2 from 14.3.3, permitting the binding of these inhibitors to mTOR and the negative modulation of this kinase. HIF stability is controlled by the hypoxia-inducible factor prolyl hydroxylase 1/2 (PHD1/2) [86]. These enzymes hydroxylate HIFs and target them for ubiquitination and degradation. PP2A-B55, by dephosphorylating and inactivating PHD1/2, stabilizes HIFs and triggers TSC1/TSC2-dependent mTOR inhibition, potentiating autophagy-mediated cell survival [87].
7. PP2A-B55 Misregulation in Cancer
PP2A was first suggested to act as a tumor suppressor based on the studies showing that okadaic acid, a chemical inhibitor of PP2A, caused tumors in mice [88]. This hypothesis was further supported by the fact that viral particles including the polyoma small and middle T antigens, the simian virus SV40 small T antigen, and the E4orf4 antigen promote cell transformation by inducing B55 subunit dissociation from PP2A [89,90]. Genetic and epigenetic alterations linked to B55 downregulation also support the role of PP2A-B55 as a tumor suppressor. Deletions and mutations on the B55 genes PPP2R2 have been found in breast, prostate, primary plasma leukemia, acute myeloid leukemia (AML), and ovarian cell carcinoma. A study of 995 primary breast tumors identified heterozygous and homozygous deletions of the PPP2R2A gene associated with loss of B55α transcript in Estrogen Receptor (ER)-positive luminal B breast cancer [91] (Table 1). Somatic deletions were also observed in 67% prostate tumor samples [92] and deletions encompassing B55α and B55β genes PPP2R2A and PPP2R2B were found in primary plasma cell leukemia [93] and in multiple myeloma patients [94], respectively. Loss of function mutations on the PPP2R2A gene were additionally observed in acute leukemia blasts and were associated with the disappearance of B55α expression [95]. Interestingly, these cells were more sensitive to treatment with the Akt inhibitor, but less responsive to the PP2A activator FTY720, supporting the role of PP2A-B55α holoenzyme in the regulation of Akt phosphorylation in AML.
Table 1.
Alterations reported for the distinct B55 isoforms in different types of cancers.
| PP2A-B55: Tumour Suppressor Activity | ||||
| Subunit | Gene | Alteration | Disease | Ref. |
| B55𝛼 | PPP2R2A | Deletions | Luminal B breast cancer | [91] |
| B55𝛼 | PPP2R2A | Deletions | Prostate cancer | [92] |
| B55𝛼 | PPP2R2A | Deletions | Primary plasma cell leukaemia | [93] |
| B55𝛽 | PPP2R2B | Deletions | Myeloma | [94] |
| B55𝛼 | PPP2R2A | Loss of function mutation | AML | [95] |
| B55𝛼 | PPP2R2A | B55 downregulation | AML | [96] |
| B55𝛼 | PPP2R2A | Decreased mRNA | Lung & thyroid carcinoma | [97] |
| B55𝛽 | PPP2R2B | Epigenetic silencing | Colorectal cancer | [98] |
| B55𝛽 | PPP2R2B | Epigenetic silencing | Ductal breast carcinoma | [99] |
| B55𝛾 | PPP2R2C | B55 downregulation | Prostate cancer | [100] |
| B55𝛿 | PPP2R2D | Up miRNA/down mRNA | Hepatocellular carcinoma | [101] |
| PP2A-B55: Oncogenic Activity | ||||
| Subunit | Gene | Alteration | Disease | Ref. |
| B55𝛼 | PPP2R2A | B55 overexpression | Pancreatic cancer | [103] |
Besides deletions and mutations, diminished protein expression of the B55 isoforms was found to be associated with different tumors. Accordingly, in a study of 511 AML patients, the expression of B55α was found decreased in AML cells compared to normal cells. This expression negatively correlated with Thr308 phosphorylation of Akt, supporting again the role of PP2A-B55α holoenzyme in Akt hyperphosphorylation in AML [96]. In the same line, decreased PPP2R2A mRNA has been found in lung and thyroid carcinomas [97] and downregulation of PPP2R2B by epigenetic silencing has been observed in colorectal cancer [98] and in ductal breast carcinoma [99]. The cellular levels of B55γ were analyzed by immunohistochemistry as well and found to be lost in prostate cancer, a fact that correlated with metastasis and mortality [100]. Finally, the expression of B55δ in hepatocellular carcinomas decreases inversely to the level of the 133b miRNA, a microRNA known to target B55δ mRNA. This suggests that 133b miRNA could act as an oncogene by reducing B55δ levels and PP2A-B55δ activity [101].
Although PP2A has been assumed to play a major role as a tumor suppressor, several studies indicate that this phosphatase can also activate several oncogenic cascades and positively participate in the oncogenic process [80,102]. Consistently, a significant enhancement in the levels of the B55α subunit has been described in pancreatic ductal adenocarcinoma. In these cancer cells, the increase of B55α levels correlate with poor survival of pancreatic cancer patients. Moreover, the depletion of this protein by siRNA in pancreatic cancer cell lines resulted in a drop of the phosphorylation of Akt and Erk1/2 and in a decrease of the levels of βCatenin. This phenotype was associated with a reduction of the oncogenic properties including attenuated cell growth, clonogenicity, mobility and anchorage-independent growth, supporting an effect of PP2A-B55α as an oncogene in pancreatic cancer [103].
8. Arpp19 and ENSA Misregulation in Cancer
Arpp19 overexpression associated with a gain of tumorigenic properties has been reported in a high number of cancers, indicating that, as expected by its PP2A-B55 inhibitory activity, it acts as an oncogene. Interestingly, Arpp19 upregulation in most cases results from the decreased levels of different microRNAs targeting this gene.
In cervical cancer, the overexpression of the long noncoding RNA DLX6-AS1 results in the drop of the microRNA miR-16-5p and the upregulation of its downstream target Arpp19. DLX6-AS1 silencing attenuates oncogenic properties in cervical cancer cells, whereas its overexpression results in the opposite phenotype [104] (Table 2).
Table 2.
Mechanisms triggering Arpp19 overexpression in the indicated types of cancers.
| Arpp19 Overexpression | |||
|---|---|---|---|
| Alteration | miRNA | Disease | Ref. |
| Long Noncoding RNA DLX6-AS1 overexpression | Drop miR-16-5p | Cervical cancer | [104] |
| Long Noncoding RNA IGFL2-AS1 overexpression | Drop miR-802 | Gastric cancer | [105] |
| _ | Drop miR-802 | Laryngeal cancer | [106] |
| _ | Drop miR-26A | Papillary thyroid Cancer | [107] |
| _ | Drop miR-320 | Breast cancer | [108] |
| Increased mRNA levels | _ | Hepatocellular carcinoma | [109] |
| Increased mRNA levels | _ | AML | [110] |
In gastric cancer, other long coding RNA, IGFL2-AS1, is overexpressed. IGFL2-AS1 sponges miR-802, which in turn targets Arpp19 [105]. This alteration is associated with Arpp19 overexpression and increased oncogenic properties. miR-802 level attenuation has also been found in laryngeal cancer [106]. In these cancer cells, colony formation and cell proliferation, migration, and invasion are attenuated upon miR-802 ectopic expression and this attenuation is reversed by the overexpression of Arpp19.
Two additional microRNAs, miR-26A and miR-320, have been shown to be involved in Arpp19 overexpression and cancer treatment resistance. miR-26A down-regulation in Papillary Thyroid Carcinoma is associated with increased cell proliferation and treatment resistance, and the knockdown of Arpp19 sensitizes these cancer cells to tamoxifen [107]. Similarly, downregulation of miR-320 in estrogen receptor positive breast cancer cells results in Arpp19 overexpression and in the loss of tamoxifen sensitivity, a phenotype that is reversed by miR-320 restoration [108].
Finally, increased Arpp19 mRNA expression has been reported in hepatocellular carcinoma [109] and AML [110] tissue samples, and high levels of this protein have been identified as an independent predictor of relapse in AML patients.
Unlike Arpp19, ENSA expression appears to be less involved in cancer development and progression. Surprisingly, although ENSA amplification and upregulation is observed in tumoral samples (cBioportal database), it has not been strongly linked with cancer patient outcomes, with only one study reporting the hypomethylation of the ENSA gene promoter and the overexpression of this protein in liver cancer cell lines and patient samples. Contrary to Arpp19, this overexpression was linked with tumor suppression [111].
Unfortunately, despite compelling data identifying Arpp19 as a potent oncogene, nothing is known about the underlying molecular mechanisms involved in oncogenesis and tumoral progression upon Arpp19 overexpression. No data exists about the putative involvement of Arpp19-dependent inhibition of PP2A-B55. Moreover, the direct targets of Arpp19 in the oncogenic process are completely unknown. Finally, nothing is known about the mechanisms by which ENSA, the other inhibitor of PP2A-B55, participates in the oncogenic processes. Further studies are required to uncover the exact role of these two proteins in cancer development and progression, the participation of PP2A-B55 in this phenotype, and to unravel whether they could represent interesting targets for cancer therapy.
9. Gwl/Mastl Misregulation in Cancer
As for Arpp19, Gwl (Mastl in humans) acts as an oncogene. The overexpression of Gwl has been reported in a high number of cancer types including hepatocarcinoma [112], neuroblastoma [113], head and neck squamous cell carcinoma [114], and breast [115,116,117,118], gastric [119], and colorectal [120,121] cancers. In all these cancers, the upregulation of Gwl correlates with increased risk of relapse and poor prognosis, specifically in head and neck carcinoma [114], neuroblastoma [113] and in breast [115,116,117], gastric [119], and colorectal [120] cancers. In these cases, the levels of this kinase could be used as a valuable indicator of metastatic relapse and death.
The upregulation of Gwl is also associated with an increase of the oncogenic capacities such as cell proliferation, migration, and invasion [114,116,120,121], and its silencing is linked with a drop of these properties as well as with a drop of xenograft tumor growth “in vivo” [115,116,120,121,122]. Decreased cell proliferation under these conditions is mostly induced by mitotic catastrophe and apoptosis [115,116,122].
Interestingly, all tumoral cells are not impacted at the same level by Gwl knockdown. Notably, whereas some breast cancer cell lines such as MDA-MB-231 or BT-549 are highly sensitive to Gwl knockdown, others such as EVSA-T or T47D are largely insensitive [115]. For some cancer cells, including AML cells [123] and thyroid cancer cells [124], Gwl depletion was specifically affecting tumoral but not normal cells, pointing to Gwl as a novel therapeutic target. In the same line, the downregulation of this kinase has been shown to sensitize tumoral cell response to anticancer treatments such as radiation in breast [122] and non-small cell lung cancer cells [125], cisplatin in thyroid cancer cells [126], and 5 fluorouracil in colorectal cancer cells [120].
The oncogenic activity of Gwl has been attributed to the modulation of different underlying signaling cascades. First, analysis in breast and colorectal cancer cell lines pointed to a role of Gwl overexpression in the hyperphosphorylation and hyperactivation of the oncogenic kinase Akt. The reported data demonstrated that increased Gwl levels correlates with dephosphorylation and activation of the GSK3 kinase as well as with the phosphorylation and subsequent SCF-dependent ubiquitination and degradation of PHLPP, the phosphatase targeting Akt. A model was proposed in which Gwl, via GSK3 activation, promotes PHLPP degradation and as a consequence, Akt hyperphosphorylation and hyperactivation, thus potentiating its oncogenic activities [121].
In a second study, a role of Gwl in the upregulation of the Wnt/βCatenin pathway and of the anti-apoptotic proteins Survivin and Bcl-xL has also been suggested. Notably, the levels of these antiapoptotic proteins correlates with Gwl levels in HCT116 and SW620 colorectal cancer cells. Gwl overexpression was associated with an increase of the amount of βCatenin and of its target c-Myc that was attributed to the phosphorylation and inactivation of GSK3 [120]. From this data, authors proposed that Gwl silencing could positively modulate GSK3 dephosphorylation and activation, and destabilization of βCatenin. Low βCatenin levels would result in decreased expression of cMyc and of its targets Survivin and Bcl-xL, and would promote colorectal cancer cell sensitization to 5-fluorouracil treatment.
Finally, Gwl overexpression has been proposed to play a pleiotropic role via the drop of PP2A-B55-dependent dephosphorylation of multiple components of the different signaling pathways. These pathways regulate actin dynamics, cell-cell junctions, MAPK signaling, and DNA damage [116]. A SILAC-phosphoproteomic analysis in MCF10 breast cancer cells overexpressing the Gwl kinase revealed an enrichment of up or down phosphorylated proteins upon Gwl overexpression. The up-regulated phosphopeptide group upon Gwl overexpression displays an enrichment of proteins involved in desmosomes, actin dynamics, MAPK signaling, and DNA damage. Conversely, down-phosphorylated proteins were clustered around protein kinase D1, vimentin, and Akt downstream targets. According to a role of Gwl in the control of cell-cell junctions, the overexpression of this kinase in MCF10A cells resulted in the disorganization of actin cytoskeleton and the reduced expression and mislocalization of E-cadherin and βCatenin. As a consequence, Gwl overexpression disrupted collective cell migration [116]. Interestingly, a recent report identified Gwl as an activator of cell contractility via the positive modulation of MRTF-A/SRF (myocardin-related transcription factor A/serum response factor) signaling [127]. By directly binding to MRTF-A, the Gwl kinase promotes the nuclear retention of this transcription factor and mediates the transcription of genes related to actin dynamics, cell adhesion, and actomyosin contraction via its association to SRF. Altogether, these data suggest a pleiotropic role of Gwl on the control of different signaling pathways involved, not only in cell cycle control, but also in cell proliferation, cell survival, and cell-cell contact regulation. Unfortunately, although the causes of the oncogenic Gwl activity are beginning to be understood, nothing is known about the underlying mechanisms promoting Gwl overexpression and tumor formation.
10. Summary
Phosphatases have been identified as tumor suppressors very commonly misregulated during cancer and consequently have become suitable candidates for anticancer therapies. From all these phosphatases, PP2A-B55 is emerging as a key holoenzyme often misregulated in a high number of cancer types. Although the constituents and the protein structure of this complex have been largely investigated, the molecular mechanisms regulating its activity were unknown, notably, no specific inhibitors of this holoenzyme were identified. The discovery of the Gwl/Arpp19-ENSA pathway, together with the finding of an increasing number of PP2A-B55 substrates and the advances on the molecular mechanisms conferring substrate specificity, bring to the forefront the study of this holoenzyme, both under physiological and pathological conditions. In this review, our objective was to summarize the main data recently provided in the bibliography about PP2A-B55 and to highlight the prominent impact of its misregulation in the oncogenic process.
Funding
This work was supported by the Agence National de la Recherche (KiPARPP, ANR-18-CE13-0013 and REPLIGREAT, ANR-18-CE13-0018-01), La Ligue Nationale Contre le Cancer (Equipe Labellisée), the Fondation ARC (PJA 20181207931) and the LABEX EpiGenMed (ANR-10-LABEX-12-01). S.A. is a Labex EpiGenMed “Investissement d’avenir” program fellowship (ANR-10-LABX-12-01).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhang J., Yang P.L., Gray N.S. Targeting cancer with small molecule kinase inhibitors. Nat. Rev. Cancer. 2009;9:28–39. doi: 10.1038/nrc2559. [DOI] [PubMed] [Google Scholar]
- 2.Knight Z.A., Lin H., Shokat K.M. Targeting the cancer kinome through polypharmacology. Nat. Rev. Cancer. 2010;10:130–137. doi: 10.1038/nrc2787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stebbing J., Lit L.C., Zhang H., Darrington R.S., Melaiu O., Rudraraju B., Giamas G. The regulatory roles of phosphatases in cancer. Oncogene. 2014;33:939–953. doi: 10.1038/onc.2013.80. [DOI] [PubMed] [Google Scholar]
- 4.Chen W., Wang Z., Jiang C., Ding Y. PP2A-Mediated Anticancer Therapy. Gastroenterol. Res. Pract. 2013;2013:1–10. doi: 10.1155/2013/675429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shi Y. Serine/Threonine Phosphatases: Mechanism through Structure. Cell. 2009;139:468–484. doi: 10.1016/j.cell.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 6.Brautigan D.L., Shenolikar S. Protein Serine/Threonine Phosphatases: Keys to Unlocking Regulators and Substrates. Annu. Rev. Biochem. 2018;87:921–964. doi: 10.1146/annurev-biochem-062917-012332. [DOI] [PubMed] [Google Scholar]
- 7.Pérez-Hidalgo L., Moreno S. Coupling TOR to the Cell Cycle by the Greatwall-Endosulfine-PP2A-B55 Pathway. Biomolecules. 2017;7:59. doi: 10.3390/biom7030059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crncec A., Hochegger H. Triggering mitosis. FEBS Lett. 2019;593:2868–2888. doi: 10.1002/1873-3468.13635. [DOI] [PubMed] [Google Scholar]
- 9.Glover D.M. The overlooked greatwall: A new perspective on mitotic control. Open Biol. 2012;2:120023. doi: 10.1098/rsob.120023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castro A., Lorca T. Greatwall kinase at a glance. J. Cell Sci. 2018;131:jcs222364. doi: 10.1242/jcs.222364. [DOI] [PubMed] [Google Scholar]
- 11.Lorca T., Castro A. The Greatwall kinase: A new pathway in the control of the cell cycle. Oncogene. 2013;32:537–543. doi: 10.1038/onc.2012.79. [DOI] [PubMed] [Google Scholar]
- 12.Lorca T., Castro A. Deciphering the New Role of the Greatwall/PP2A Pathway in Cell Cycle Control. Genes Cancer. 2012;3:712–720. doi: 10.1177/1947601912473478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vigneron S., Robert P., Hached K., Sundermann L., Charrasse S., Labbe J.C., Castro A., Lorca T. The master Greatwall kinase, a critical regulator of mitosis and meiosis. Int. J. Dev. Biol. 2016;60:245–254. doi: 10.1387/ijdb.160155tl. [DOI] [PubMed] [Google Scholar]
- 14.Dupré A., Jessus C. ARPP19 Phosphorylations by PKA and Greatwall: The Yin and the Yang of the Cell Decision to Divide. Protein Phosphorylation. 2017 doi: 10.5772/intechopen.71332. [DOI] [Google Scholar]
- 15.Hunt T. On the regulation of protein phosphatase 2A and its role in controlling entry into and exit from mitosis. Adv. Biol. Regul. 2013;53:173–178. doi: 10.1016/j.jbior.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 16.Mochida S., Hunt T. Protein phosphatases and their regulation in the control of mitosis. EMBO Rep. 2012;13:197–203. doi: 10.1038/embor.2011.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gu P., Qi X., Zhou Y., Wang Y., Gao X. Generation of Ppp2Ca and Ppp2Cb conditional null alleles in mouse. Genesis. 2012;50:429–436. doi: 10.1002/dvg.20815. [DOI] [PubMed] [Google Scholar]
- 18.Gotz J., Probst A., Ehler E., Hemmings B., Kues W. Delayed embryonic lethality in mice lacking protein phosphatase 2A catalytic subunit C. Proc. Natl. Acad. Sci. 1998;95:12370–12375. doi: 10.1073/pnas.95.21.12370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu Y., Chen Y., Zhang P., Jeffrey P.D., Shi Y. Structure of a Protein Phosphatase 2A Holoenzyme: Insights into B55-Mediated Tau Dephosphorylation. Mol. Cell. 2008;31:873–885. doi: 10.1016/j.molcel.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wlodarchak N., Guo F., Satyshur K.A., Jiang L., Jeffrey P.D., Sun T., Stanevich V., Mumby M.C., Xing Y. Structure of the Ca2+-dependent PP2A heterotrimer and insights into Cdc6 dephosphorylation. Cell Res. 2013;23:931–946. doi: 10.1038/cr.2013.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strack S., Chang D., Zaucha J.A., Colbran R.J., Wadzinski B.E. Cloning and characterization of Bδ, a novel regulatory subunit of protein phosphatase 2A. FEBS Lett. 1999;460:462–466. doi: 10.1016/S0014-5793(99)01377-0. [DOI] [PubMed] [Google Scholar]
- 22.Xing Y., Li Z., Chen Y., Stock J.B., Jeffrey P.D., Shi Y. Structural Mechanism of Demethylation and Inactivation of Protein Phosphatase 2A. Cell. 2008;133:154–163. doi: 10.1016/j.cell.2008.02.041. [DOI] [PubMed] [Google Scholar]
- 23.Longin S., Zwaenepoel K., Louis J.V., Dilworth S., Goris J., Janssens V. Selection of Protein Phosphatase 2A Regulatory Subunits Is Mediated by the C Terminus of the Catalytic Subunit. J. Biol. Chem. 2007;282:26971–26980. doi: 10.1074/jbc.M704059200. [DOI] [PubMed] [Google Scholar]
- 24.Margolis S.S., Perry J.A., Forester C.M., Nutt L.K., Guo Y., Jardim M.J., Thomenius M.J., Freel C.D., Darbandi R., Ahn J.-H., et al. Role for the PP2A/B56δ Phosphatase in Regulating 14-3-3 Release from Cdc25 to Control Mitosis. Cell. 2006;127:759–773. doi: 10.1016/j.cell.2006.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Letourneux C., Rocher G., Porteu F. B56-containing PP2A dephosphorylate ERK and their activity is controlled by the early gene IEX-1 and ERK. EMBO J. 2006;25:727–738. doi: 10.1038/sj.emboj.7600980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cho U.S., Xu W. Crystal structure of a protein phosphatase 2A heterotrimeric holoenzyme. Nature. 2007;445:53–57. doi: 10.1038/nature05351. [DOI] [PubMed] [Google Scholar]
- 27.Low I.C.C., Loh T., Huang Y., Virshup D.M., Pervaiz S. Ser70 phosphorylation of Bcl-2 by selective tyrosine nitration of PP2A-B56δ stabilizes its antiapoptotic activity. Blood. 2014;124:2223–2234. doi: 10.1182/blood-2014-03-563296. [DOI] [PubMed] [Google Scholar]
- 28.Janssens V., Jordens J., Stevens I., Van Hoof C., Martens E., De Smedt H., Engelborghs Y., Waelkens E., Goris J. Identification and Functional Analysis of Two Ca 2+ -binding EF-hand Motifs in the B"/PR72 Subunit of Protein Phosphatase 2A. J. Biol. Chem. 2003;278:10697–10706. doi: 10.1074/jbc.M211717200. [DOI] [PubMed] [Google Scholar]
- 29.Yan Z., Fedorov S.A., Mumby M.C., Williams R.S. PR48, a Novel Regulatory Subunit of Protein Phosphatase 2A, Interacts with Cdc6 and Modulates DNA Replication in Human Cells. Mol. Cell. Biol. 2000;20:1021–1029. doi: 10.1128/MCB.20.3.1021-1029.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haesen D., Sents W., Lemaire K., Hoorne Y., Janssens V. The Basic Biology of PP2A in Hematologic Cells and Malignancies. Front. Oncol. 2014;4 doi: 10.3389/fonc.2014.00347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goudreault M., D’Ambrosio L.M., Kean M.J., Mullin M.J., Larsen B.G., Sanchez A., Chaudhry S., Chen G.I., Sicheri F., Nesvizhskii A.I., et al. A PP2A Phosphatase High Density Interaction Network Identifies a Novel Striatin-interacting Phosphatase and Kinase Complex Linked to the Cerebral Cavernous Malformation 3 (CCM3) Protein. Mol. Cell. Proteom. 2009;8:157–171. doi: 10.1074/mcp.M800266-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hwang J., Pallas D.C. STRIPAK complexes: Structure, biological function, and involvement in human diseases. Int. J. Biochem. Cell Biol. 2014;47:118–148. doi: 10.1016/j.biocel.2013.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kong M., Ditsworth D., Lindsten T., Thompson C.B. α4 is an essential regulator of PP2A phosphatase activity. Mol. Cell. 2009;36:51–60. doi: 10.1016/j.molcel.2009.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guo F. Structural basis of PP2A activation by PTPA, an ATP-dependent activation chaperone. Cell Res. 2014;24:190–203. doi: 10.1038/cr.2013.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Evans D.R.H., Hemmings B.A. Mutation of the C-terminal leucine residue of PP2Ac inhibits PR55/B subunit binding and confers supersensitivity to microtubule destabilization in Saccharomyces cerevisiae. Mol. Gen. Genet. 2000;264:425–432. doi: 10.1007/s004380000302. [DOI] [PubMed] [Google Scholar]
- 36.Wei H., Ashby D.G., Moreno C.S., Ogris E., Yeong F.M., Corbett A.H., Pallas D.C. Carboxymethylation of the PP2A Catalytic Subunit inSaccharomyces cerevisiae Is Required for Efficient Interaction with the B-type Subunits Cdc55p and Rts1p. J. Biol. Chem. 2001;276:1570–1577. doi: 10.1074/jbc.M008694200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gentry M.S., Li Y., Wei H., Syed F.F., Patel S.H., Hallberg R.L., Pallas D.C. A Novel Assay for Protein Phosphatase 2A (PP2A) Complexes In Vivo Reveals Differential Effects of Covalent Modifications on Different Saccharomyces cerevisiae PP2A Heterotrimers. Eukaryot. Cell. 2005;4:1029–1040. doi: 10.1128/EC.4.6.1029-1040.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Koren R., Rainis L., Kleinberger T. The Scaffolding A/Tpd3 Subunit and High Phosphatase Activity Are Dispensable for Cdc55 Function in the Saccharomyces cerevisiae Spindle Checkpoint and in Cytokinesis. J. Biol. Chem. 2004;279:48598–48606. doi: 10.1074/jbc.M409359200. [DOI] [PubMed] [Google Scholar]
- 39.Ogris E., Gibson D.M., Pallas D.C. Protein phosphatase 2A subunit assembly: The catalytic subunit carboxy terminus is important for binding cellular B subunit but not polyomavirus middle tumor antigen. Oncogene. 1997;15:911–917. doi: 10.1038/sj.onc.1201259. [DOI] [PubMed] [Google Scholar]
- 40.Tolstykh T., Lee J., Vafai S., Stock J.B. Carboxyl methylation regulates phosphoprotein phosphatase 2A by controlling the association of regulatory B subunits. EMBO J. 2000;19:5682–5691. doi: 10.1093/emboj/19.21.5682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nunbhakdi-Craig V., Schuechner S., Sontag J.-M., Montgomery L., Pallas D.C., Juno C., Mudrak I., Ogris E., Sontag E. Expression of protein phosphatase 2A mutants and silencing of the regulatory Bα subunit induce a selective loss of acetylated and detyrosinated microtubules. J. Neurochem. 2007;101:959–971. doi: 10.1111/j.1471-4159.2007.04503.x. [DOI] [PubMed] [Google Scholar]
- 42.Li M., Guo H., Damuni Z. Purification and Characterization of Two Potent Heat-Stable Protein Inhibitors of Protein Phosphatase 2A from Bovine Kidney. Biochemistry. 1995;34:1988–1996. doi: 10.1021/bi00006a020. [DOI] [PubMed] [Google Scholar]
- 43.Reilly P.T., Yu Y., Hamiche A., Wang L. Cracking the ANP32 whips: Important functions, unequal requirement, and hints at disease implications. Bioessays. 2014;36:1062–1071. doi: 10.1002/bies.201400058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen S., Li B., Grundke-Iqbal I., Iqbal K. I PP2A 1 Affects Tau Phosphorylation via Association with the Catalytic Subunit of Protein Phosphatase 2A. J. Biol. Chem. 2008;283:10513–10521. doi: 10.1074/jbc.M709852200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Adachr Y., Pavlakis G.N., Copeland T.D. Identification of in vivo phosphorylation sites of SET, a nuclear phosphoprotein encoded by the translocation breakpoint in acute undifferentiated leukemia. FEBS Lett. 1994;340:231–235. doi: 10.1016/0014-5793(94)80144-4. [DOI] [PubMed] [Google Scholar]
- 46.Irie A., Harada K., Araki N., Nishimura Y. Phosphorylation of SET Protein at Ser171 by Protein Kinase D2 Diminishes Its Inhibitory Effect on Protein Phosphatase 2A. PLoS ONE. 2012;7:e51242. doi: 10.1371/journal.pone.0051242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vasudevan N.T., Mohan M.L., Gupta M.K., Hussain A.K., Prasad S.V.N. Inhibition of Protein Phosphatase 2A Activity by PI3Kγ Regulates β-Adrenergic Receptor Function. Mol. Cell. 2011;41:636–648. doi: 10.1016/j.molcel.2011.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cristóbal I., Blanco F.J., Garcia-Orti L., Marcotegui N., Vicente C., Rifon J., Novo F.J., Bandres E., Calasanz M.J., Bernabeu C., et al. SETBP1 overexpression is a novel leukemogenic mechanism that predicts adverse outcome in elderly patients with acute myeloid leukemia. Blood. 2010;115:615–625. doi: 10.1182/blood-2009-06-227363. [DOI] [PubMed] [Google Scholar]
- 49.Chambon J.-P., Touati S.A., Berneau S., Cladière D., Hebras C., Groeme R., McDougall A., Wassmann K. The PP2A Inhibitor I2PP2A Is Essential for Sister Chromatid Segregation in Oocyte Meiosis II. Curr. Biol. 2013;23:485–490. doi: 10.1016/j.cub.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 50.Neviani P., Santhanam R., Trotta R., Notari M., Blaser B.W., Liu S., Mao H., Chang J.S., Galietta A., Uttam A., et al. The tumor suppressor PP2A is functionally inactivated in blast crisis CML through the inhibitory activity of the BCR/ABL-regulated SET protein. Cancer Cell. 2005;8:355–368. doi: 10.1016/j.ccr.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 51.Leopoldino A.M., Squarize C.H., Garcia C.B., Almeida L.O., Pestana C.R., Polizello A.C.M., Uyemura S.A., Tajara E.H., Gutkind J.S., Curti C. Accumulation of the SET protein in HEK293T cells and mild oxidative stress: Cell survival or death signaling. Mol. Cell Biochem. 2012;363:65–74. doi: 10.1007/s11010-011-1158-x. [DOI] [PubMed] [Google Scholar]
- 52.Christensen D.J., Chen Y., Oddo J., Matta K.M., Neil J., Davis E.D., Volkheimer A.D., Lanasa M.C., Friedman D.R., Goodman B.K., et al. SET oncoprotein overexpression in B-cell chronic lymphocytic leukemia and non-Hodgkin lymphoma: A predictor of aggressive disease and a new treatment target. Blood. 2011;118:4150–4158. doi: 10.1182/blood-2011-04-351072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Al-Murrani S.W.K., Woodgett J.R., Damuni Z. Expression of I2PP2A, an inhibitor of protein phosphatase 2A, induces c-Jun and AP-1 activity. Biochem. J. 1999;341:293–298. doi: 10.1042/bj3410293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huang Y.-H., Chu P.-Y., Chen J.-L., Huang C.-T., Lee C.-H., Lau K.-Y., Wang W.-L., Wang Y.-L., Lien P.-J., Tseng L.-M., et al. SET Overexpression is Associated with Worse Recurrence-Free Survival in Patients with Primary Breast Cancer Receiving Adjuvant Tamoxifen Treatment. J. Clin. Med. 2018;7:245. doi: 10.3390/jcm7090245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu H., Gu Y., Wang H., Yin J., Zheng G., Zhang Z., Lu M., Wang C., He Z. Overexpression of PP2A inhibitor SET oncoprotein is associated with tumor progression and poor prognosis in human non-small cell lung cancer. Oncotarget. 2015;6:14913–14925. doi: 10.18632/oncotarget.3818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brander D.M., Friedman D.R., Volkheimer A.D., Christensen D.J., Rassenti L.Z., Kipps T.J., Guadalupe E., Chen Y., Zhang D., Wang X., et al. SET alpha and SET beta mRNA isoforms in chronic lymphocytic leukaemia. Br. J. Haematol. 2019;184:605–615. doi: 10.1111/bjh.15677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Junttila M.R., Puustinen P., Niemelä M., Ahola R., Arnold H., Böttzauw T., Ala-aho R., Nielsen C., Ivaska J., Taya Y., et al. CIP2A Inhibits PP2A in Human Malignancies. Cell. 2007;130:51–62. doi: 10.1016/j.cell.2007.04.044. [DOI] [PubMed] [Google Scholar]
- 58.Wang J., Okkeri J., Pavic K., Wang Z., Kauko O., Halonen T., Sarek G., Ojala P.M., Rao Z., Xu W., et al. Oncoprotein CIP2A is stabilized via interaction with tumor suppressor PP2A/B56. EMBO Rep. 2017;18:437–450. doi: 10.15252/embr.201642788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Laine A., Sihto H., Come C., Rosenfeldt M.T., Zwolinska A., Niemelä M., Khanna A., Chan E.K., Kähäri V.-M., Kellokumpu-Lehtinen P.-L., et al. Senescence Sensitivity of Breast Cancer Cells Is Defined by Positive Feedback Loop between CIP2A and E2F1. Cancer Discov. 2013;3:182–197. doi: 10.1158/2159-8290.CD-12-0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen K.-F., Liu C.-Y., Lin Y.-C., Yu H.-C., Liu T.-H., Hou D.-R., Chen P.-J., Cheng A.-L. CIP2A mediates effects of bortezomib on phospho-Akt and apoptosis in hepatocellular carcinoma cells. Oncogene. 2010;29:6257–6266. doi: 10.1038/onc.2010.357. [DOI] [PubMed] [Google Scholar]
- 61.Khanna A., Pimanda J.E., Westermarck J. Cancerous Inhibitor of Protein Phosphatase 2A, an Emerging Human Oncoprotein and a Potential Cancer Therapy Target. Cancer Res. 2013;73:6548–6553. doi: 10.1158/0008-5472.CAN-13-1994. [DOI] [PubMed] [Google Scholar]
- 62.Porter I.M., Schleicher K., Porter M., Swedlow J.R. Bod1 regulates protein phosphatase 2A at mitotic kinetochores. Nat. Commun. 2013;4:2677. doi: 10.1038/ncomms3677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gharbi-Ayachi A., Labbe J.C., Burgess A., Vigneron S., Strub J.M., Brioudes E., Van-Dorsselaer A., Castro A., Lorca T. The substrate of Greatwall kinase, Arpp19, controls mitosis by inhibiting protein phosphatase 2A. Science. 2010;330:1673–1677. doi: 10.1126/science.1197048. [DOI] [PubMed] [Google Scholar]
- 64.Mochida S., Maslen S.L., Skehel M., Hunt T. Greatwall phosphorylates an inhibitor of protein phosphatase 2A that is essential for mitosis. Science. 2010;330:1670–1673. doi: 10.1126/science.1195689. [DOI] [PubMed] [Google Scholar]
- 65.Mochida S., Ikeo S., Gannon J., Hunt T. Regulated activity of PP2A-B55 delta is crucial for controlling entry into and exit from mitosis in Xenopus egg extracts. EMBO J. 2009;28:2777–2785. doi: 10.1038/emboj.2009.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vigneron S., Brioudes E., Burgess A., Labbe J.C., Lorca T., Castro A. Greatwall maintains mitosis through regulation of PP2A. EMBO J. 2009;28:2786–2793. doi: 10.1038/emboj.2009.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Juanes M.A., Khoueiry R., Kupka T., Castro A., Mudrak I., Ogris E., Lorca T., Piatti S. Budding yeast greatwall and endosulfines control activity and spatial regulation of PP2A(Cdc55) for timely mitotic progression. PLoS Genet. 2013;9:e1003575. doi: 10.1371/journal.pgen.1003575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Labandera A.-M., Vahab A.R., Chaudhuri S., Kerk D., Moorhead G.B.G. The mitotic PP2A regulator ENSA/ARPP-19 is remarkably conserved across plants and most eukaryotes. Biochem. Biophys. Res. Commun. 2015;458:739–744. doi: 10.1016/j.bbrc.2015.01.123. [DOI] [PubMed] [Google Scholar]
- 69.Cundell M.J., Bastos R.N., Zhang T., Holder J., Gruneberg U., Novak B., Barr F.A. The BEG (PP2A-B55/ENSA/Greatwall) pathway ensures cytokinesis follows chromosome separation. Mol. Cell. 2013;52:393–405. doi: 10.1016/j.molcel.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hached K., Goguet P., Charrasse S., Vigneron S., Sacristan M.P., Lorca T., Castro A. ENSA and ARPP19 differentially control cell cycle progression and development. J. Cell Biol. 2019;218:541–558. doi: 10.1083/jcb.201708105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hegarat N., Vesely C., Vinod P.K., Ocasio C., Peter N., Gannon J., Oliver A.W., Novak B., Hochegger H. PP2A/B55 and Fcp1 regulate Greatwall and Ensa dephosphorylation during mitotic exit. PLoS Genet. 2014;10:e1004004. doi: 10.1371/journal.pgen.1004004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dupré A., Daldello E.M., Nairn A.C., Jessus C., Haccard O. Phosphorylation of ARPP19 by protein kinase A prevents meiosis resumption in Xenopus oocytes. Nat. Commun. 2014;5 doi: 10.1038/ncomms4318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Matthews L.M., Evans J.P. alpha-endosulfine (ENSA) regulates exit from prophase I arrest in mouse oocytes. Cell Cycle. 2014;13:1639–1649. doi: 10.4161/cc.28606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Charrasse S., Gharbi-Ayachi A., Burgess A., Vera J., Hached K., Raynaud P., Schwob E., Lorca T., Castro A. Ensa controls S-phase length by modulating Treslin levels. Nat. Commun. 2017;8:206. doi: 10.1038/s41467-017-00339-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kumm E.J., Pagel O., Gambaryan S., Walter U., Zahedi R.P., Smolenski A., Jurk K. The Cell Cycle Checkpoint System MAST(L)-ENSA/ARPP19-PP2A is Targeted by cAMP/PKA and cGMP/PKG in Anucleate Human Platelets. Cells. 2020;9:472. doi: 10.3390/cells9020472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gandhi M.J., Cummings C.L., Drachman J.G. FLJ14813 Missense Mutation: A Candidate for Autosomal Dominant Thrombocytopenia on Human Chromosome 10. Hum. Hered. 2003;55:66–70. doi: 10.1159/000071812. [DOI] [PubMed] [Google Scholar]
- 77.Hurtado B., Trakala M., Ximénez-Embún P., El Bakkali A., Partida D., Sanz-Castillo B., Álvarez-Fernández M., Maroto M., Sánchez-Martínez R., Martínez L., et al. Thrombocytopenia-associated mutations in Ser/Thr kinase MASTL deregulate actin cytoskeletal dynamics in platelets. J. Clin. Investig. 2018;128:5351–5367. doi: 10.1172/JCI121876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Manning B.D., Cantley L.C. AKT/PKB Signaling: Navigating Downstream. Cell. 2007;129:1261–1274. doi: 10.1016/j.cell.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kuo Y.C., Huang K.Y., Yang C.H., Yang Y.S., Lee W.Y., Chiang C.W. Regulation of phosphorylation of Thr-308 of Akt, cell proliferation, and survival by the B55alpha regulatory subunit targeting of the protein phosphatase 2A holoenzyme to Akt. J. Biol. Chem. 2008;283:1882–1892. doi: 10.1074/jbc.M709585200. [DOI] [PubMed] [Google Scholar]
- 80.Ory S., Zhou M., Conrads T.P., Veenstra T.D., Morrison D.K. Protein Phosphatase 2A Positively Regulates Ras Signaling by Dephosphorylating KSR1 and Raf-1 on Critical 14-3-3 Binding Sites. Curr. Biol. 2003;13:1356–1364. doi: 10.1016/S0960-9822(03)00535-9. [DOI] [PubMed] [Google Scholar]
- 81.Fritz A., Brayer K.J., McCormick N., Adams D.G., Wadzinski B.E., Vaillancourt R.R. Phosphorylation of Serine 526 Is Required for MEKK3 Activity, and Association with 14-3-3 Blocks Dephosphorylation. J. Biol. Chem. 2006;281:6236–6245. doi: 10.1074/jbc.M509249200. [DOI] [PubMed] [Google Scholar]
- 82.Eichhorn P.J.A., Creyghton M.P., Wilhelmsen K., van Dam H., Bernards R. A RNA Interference Screen Identifies the Protein Phosphatase 2A Subunit PR55c as a Stress-Sensitive Inhibitor of c-SRC. PLoS Genet. 2007;3:14. doi: 10.1371/journal.pgen.0030218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhang W., Yang J., Liu Y., Chen X., Yu T., Jia J., Liu C. PR55α, a Regulatory Subunit of PP2A, Specifically Regulates PP2A-mediated β-Catenin Dephosphorylation. J. Biol. Chem. 2009;284:22649–22656. doi: 10.1074/jbc.M109.013698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Clevers H. Wnt/β-Catenin Signaling in Development and Disease. Cell. 2006;127:469–480. doi: 10.1016/j.cell.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 85.Wong P.-M., Feng Y., Wang J., Shi R., Jiang X. Regulation of autophagy by coordinated action of mTORC1 and protein phosphatase 2A. Nat. Commun. 2015;6:8048. doi: 10.1038/ncomms9048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Brugarolas J., Lei K., Hurley R.L., Manning B.D., Reiling J.H., Hafen E., Witters L.A., Ellisen L.W., Kaelin W.G. Regulation of mTOR function in response to hypoxia by REDD1 and the TSC1/TSC2 tumor suppressor complex. Genes Dev. 2004;18:2893–2904. doi: 10.1101/gad.1256804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Di Conza G., Cafarello S.T., Loroch S., Mennerich D., Deschoemaeker S., Di Matteo M., Ehling M., Gevaert K., Prenen H., Zahedi R.P., et al. The mTOR and PP2A Pathways Regulate PHD2 Phosphorylation to Fine-Tune HIF1α Levels and Colorectal Cancer Cell Survival under Hypoxia. Cell Rep. 2017;18:1699–1712. doi: 10.1016/j.celrep.2017.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fujiki H., Suganuma M. Tumor Promotion by Inhibitors of ProteinZ Phosphatases 1 and 2A: The Okadaic Acid Class of Compounds. In: Woude G.F.V., Klein G., editors. Advances in Cancer Research. Volume 61. Academic Press; Cambridge, MA, USA: 1993. pp. 143–194. [DOI] [PubMed] [Google Scholar]
- 89.Dilworth S.M. Polyoma virus middle T antigen and its role in identifying cancer-related molecules. Nat. Rev. Cancer. 2002;2:951–956. doi: 10.1038/nrc946. [DOI] [PubMed] [Google Scholar]
- 90.Skoczylas C., Fahrbach K.M., Rundell K. Cellular targets of the SV40 small-t antigen in human cell transformation. Cell Cycle. 2004;3:606–610. doi: 10.4161/cc.3.5.836. [DOI] [PubMed] [Google Scholar]
- 91.Curtis C., Shah S.P., Chin S.F., Turashvili G., Rueda O.M., Dunning M.J., Speed D., Lynch A.G., Samarajiwa S., Yuan Y., et al. The genomic and transcriptomic architecture of 2000 breast tumours reveals novel subgroups. Nature. 2012;486:346–352. doi: 10.1038/nature10983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cheng Y., Liu W., Kim S.T., Sun J., Lu L., Sun J., Zheng S.L., Isaacs W.B., Xu J. Evaluation of PPP2R2A as a prostate cancer susceptibility gene: A comprehensive germline and somatic study. Cancer Genet. 2011;204:375–381. doi: 10.1016/j.cancergen.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mosca L., Musto P., Todoerti K., Barbieri M., Agnelli L., Fabris S., Tuana G., Lionetti M., Bonaparte E., Sirchia S.M., et al. Genome-wide analysis of primary plasma cell leukemia identifies recurrent imbalances associated with changes in transcriptional profiles. Am. J. Hematol. 2013;88:16–23. doi: 10.1002/ajh.23339. [DOI] [PubMed] [Google Scholar]
- 94.Kamada Y., Sakata-Yanagimoto M., Sanada M., Sato-Otsubo A., Enami T., Suzukawa K., Kurita N., Nishikii H., Yokoyama Y., Okoshi Y., et al. Identification of unbalanced genome copy number abnormalities in patients with multiple myeloma by single-nucleotide polymorphism genotyping microarray analysis. Int. J. Hematol. 2012;96:492–500. doi: 10.1007/s12185-012-1171-1. [DOI] [PubMed] [Google Scholar]
- 95.Shouse G., de Necochea-Campion R., Mirshahidi S., Liu X., Chen C.-S. Novel B55α-PP2A mutations in AML promote AKT T308 phosphorylation and sensitivity to AKT inhibitor-induced growth arrest. Oncotarget. 2016;7:61081–61092. doi: 10.18632/oncotarget.11209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ruvolo P.P., Qui Y.H., Coombes K.R., Zhang N., Ruvolo V.R., Borthakur G., Konopleva M., Andreeff M., Kornblau S.M. Low expression of PP2A regulatory subunit B55α is associated with T308 phosphorylation of AKT and shorter complete remission duration in acute myeloid leukemia patients. Leukemia. 2011;25:1711–1717. doi: 10.1038/leu.2011.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kalev P., Simicek M., Vazquez I., Munck S., Chen L., Soin T., Danda N., Chen W., Sablina A. Loss of PPP2R2A Inhibits Homologous Recombination DNA Repair and Predicts Tumor Sensitivity to PARP Inhibition. Cancer Res. 2012;72:6414–6424. doi: 10.1158/0008-5472.CAN-12-1667. [DOI] [PubMed] [Google Scholar]
- 98.Tan J., Lee P.L., Li Z., Jiang X., Lim Y.C., Hooi S.C., Yu Q. B55β-Associated PP2A Complex Controls PDK1-Directed Myc Signaling and Modulates Rapamycin Sensitivity in Colorectal Cancer. Cancer Cell. 2010;18:459–471. doi: 10.1016/j.ccr.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 99.Muggerud A.A., Rønneberg J.A., Wärnberg F., Botling J., Busato F., Jovanovic J., Solvang H., Bukholm I., Børresen-Dale A.-L., Kristensen V.N., et al. Frequent aberrant DNA methylation of ABCB1, FOXC1, PPP2R2B and PTEN in ductal carcinoma in situ and early invasive breast cancer. Breast Cancer Res. 2010;12:1–10. doi: 10.1186/bcr2466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bluemn E.G., Spencer E.S., Mecham B., Gordon R.R., Coleman I., Lewinshtein D., Mostaghel E., Zhang X., Annis J., Grandori C., et al. PPP2R2C Loss Promotes Castration-Resistance and Is Associated with Increased Prostate Cancer-Specific Mortality. Mol. Cancer Res. 2013;11:568–578. doi: 10.1158/1541-7786.MCR-12-0710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zhuang Q., Zhou T., He C., Zhang S., Qiu Y., Luo B., Zhao R., Liu H., Lin Y., Lin Z. Protein phosphatase 2A-B55δ enhances chemotherapy sensitivity of human hepatocellular carcinoma under the regulation of microRNA-133b. J. Exp. Clin. Cancer Res. 2016;35:1–15. doi: 10.1186/s13046-016-0341-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bajpai R., Makhijani K., Rao P.R., Shashidhara L.S. Drosophila Twins regulates Armadillo levels in response to Wg/Wnt signal. Development. 2004;131:1007–1016. doi: 10.1242/dev.00980. [DOI] [PubMed] [Google Scholar]
- 103.Hein A.L., Seshacharyulu P., Rachagani S., Sheinin Y.M., Ouellette M.M., Ponnusamy M.P., Mumby M.C., Batra S.K., Yan Y. PR55α Subunit of Protein Phosphatase 2A Supports the Tumorigenic and Metastatic Potential of Pancreatic Cancer Cells by Sustaining Hyperactive Oncogenic Signaling. Cancer Res. 2016;76:2243–2253. doi: 10.1158/0008-5472.CAN-15-2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Xie F., Xie G., Sun Q. Long Noncoding RNA DLX6-AS1 Promotes the Progression in Cervical Cancer by Targeting miR-16-5p/ARPP19 Axis. Cancer Biother. Radiopharm. 2020;35:129–136. doi: 10.1089/cbr.2019.2960. [DOI] [PubMed] [Google Scholar]
- 105.Ma Y., Liu Y., Pu Y.-S., Cui M.-L., Mao Z.-J., Li Z.-Z., He L., Wu M., Wang J.-H. LncRNA IGFL2-AS1 functions as a ceRNA in regulating ARPP19 through competitive binding to miR-802 in gastric cancer. Mol. Carcinog. 2020;59:311–322. doi: 10.1002/mc.23155. [DOI] [PubMed] [Google Scholar]
- 106.Ye H., Jin Q., Wang X., Li Y. MicroRNA-802 Inhibits Cell Proliferation and Induces Apoptosis in Human Laryngeal Cancer by Targeting cAMP-Regulated Phosphoprotein 19. [(accessed on 28 May 2020)]; doi: 10.2147/CMAR.S228429. Available online: https://www.dovepress.com/microrna-802-inhibits-cell-proliferation-and-induces-apoptosis-in-huma-peer-reviewed-article-CMAR. [DOI] [PMC free article] [PubMed] [Retracted]
- 107.Gong Y., Wu W., Zou X., Liu F., Wei T., Zhu J. MiR-26a inhibits thyroid cancer cell proliferation by targeting ARPP19. Am. J. Cancer Res. 2018;8:1030–1039. [PMC free article] [PubMed] [Google Scholar]
- 108.Lü M., Ding K., Zhang G., Yin M., Yao G., Tian H., Lian J., Liu L., Liang M., Zhu T., et al. MicroRNA-320a sensitizes tamoxifen-resistant breast cancer cells to tamoxifen by targeting ARPP-19 and ERRγ*. Sci. Rep. 2015;5 doi: 10.1038/srep08735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Song H., Pan J., Liu Y., Wen H., Wang L., Cui J., Liu Y., Hu B., Yao Z., Ji G. Increased ARPP-19 Expression Is Associated with Hepatocellular Carcinoma. Int. J. Mol. Sci. 2014;16:178–192. doi: 10.3390/ijms16010178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mäkelä E., Löyttyniemi E., Salmenniemi U., Kauko O., Varila T., Kairisto V., Itälä-Remes M., Westermarck J. Arpp19 Promotes Myc and Cip2a Expression and Associates with Patient Relapse in Acute Myeloid Leukemia. Cancers. 2019;11:1774. doi: 10.3390/cancers11111774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chen Y.-L., Kuo M.-H., Lin P.-Y., Chuang W.-L., Hsu C.-C., Chu P.-Y., Lee C.-H., Huang T.H.-M., Leu Y.-W., Hsiao S.-H. ENSA expression correlates with attenuated tumor propagation in liver cancer. Biochem. Biophys. Res. Commun. 2013;442:56–61. doi: 10.1016/j.bbrc.2013.10.165. [DOI] [PubMed] [Google Scholar]
- 112.Cao L., Li W.-J., Yang J.-H., Wang Y., Hua Z.-J., Liu D., Chen Y.-Q., Zhang H.-M., Zhang R., Zhao J.-S., et al. Inflammatory cytokine-induced expression of MASTL is involved in hepatocarcinogenesis by regulating cell cycle progression. Oncol. Lett. 2019;17:3163–3172. doi: 10.3892/ol.2019.9983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Dahlhaus M., Burkovski A., Hertwig F., Mussel C., Volland R., Fischer M., Debatin K.M., Kestler H.A., Beltinger C. Boolean modeling identifies Greatwall/MASTL as an important regulator in the AURKA network of neuroblastoma. Cancer Lett. 2016;371:79–89. doi: 10.1016/j.canlet.2015.11.025. [DOI] [PubMed] [Google Scholar]
- 114.Wang L., Luong V., Giannini P., Peng A. Mastl kinase, a promising therapeutic target, promotes cancer recurrence. Oncotarget. 2014;5:11479–11489. doi: 10.18632/oncotarget.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Álvarez-Fernández M., Sanz-Flores M., Sanz-Castillo B., Salazar-Roa M., Partida D., Zapatero-Solana E., Ali H.R., Manchado E., Lowe S., VanArsdale T., et al. Therapeutic relevance of the PP2A-B55 inhibitory kinase MASTL/Greatwall in breast cancer. Cell Death Differ. 2018;25:828–840. doi: 10.1038/s41418-017-0024-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rogers S., McCloy R.A., Parker B.L., Gallego-Ortega D., Law A.M.K., Chin V.T., Conway J.R.W., Fey D., Millar E.K.A., O’Toole S., et al. MASTL overexpression promotes chromosome instability and metastasis in breast cancer. Oncogene. 2018;37:4518–4533. doi: 10.1038/s41388-018-0295-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zhuge B.Z., Du B.R., Meng X.L., Zhang Y.Q. MASTL is a potential poor prognostic indicator in ER+ breast cancer. Eur. Rev. Med. Pharmacol. Sci. 2017;21:2413–2420. [PubMed] [Google Scholar]
- 118.Tian J., Lin Y., Yu J. E2F8 confers cisplatin resistance to ER+ breast cancer cells via transcriptionally activating MASTL. Biomed. Pharmacother. 2017;92:919–926. doi: 10.1016/j.biopha.2017.05.118. [DOI] [PubMed] [Google Scholar]
- 119.Sun X.-J., Li Y.-L., Wang L.-G., Liu L.-Q., Ma H., Hou W.-H., Yu J.-M. Mastl overexpression is associated with epithelial to mesenchymal transition and predicts a poor clinical outcome in gastric cancer. Oncol. Lett. 2017;14:7283–7287. doi: 10.3892/ol.2017.7155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Uppada S.B., Gowrikumar S., Ahmad R., Kumar B., Szeglin B., Chen X., Smith J.J., Batra S.K., Singh A.B., Dhawan P. MASTL induces Colon Cancer progression and Chemoresistance by promoting Wnt/β-catenin signaling. Mol. Cancer. 2018;17 doi: 10.1186/s12943-018-0848-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Vera J., Lartigue L., Vigneron S., Gadea G., Gire V., Del Rio M., Soubeyran I., Chibon F., Lorca T., Castro A. Greatwall promotes cell transformation by hyperactivating AKT in human malignancies. eLife. 2015;4 doi: 10.7554/eLife.10115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Yoon Y.N., Choe M.H., Jung K.-Y., Hwang S.-G., Oh J.S., Kim J.-S. MASTL inhibition promotes mitotic catastrophe through PP2A activation to inhibit cancer growth and radioresistance in breast cancer cells. BMC Cancer. 2018;18:1–13. doi: 10.1186/s12885-018-4600-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Tzelepis K., Koike-Yusa H., De Braekeleer E., Li Y., Metzakopian E., Dovey O.M., Mupo A., Grinkevich V., Li M., Mazan M., et al. A CRISPR Dropout Screen Identifies Genetic Vulnerabilities and Therapeutic Targets in Acute Myeloid Leukemia. Cell Rep. 2016;17:1193–1205. doi: 10.1016/j.celrep.2016.09.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Anania M., Gasparri F., Cetti E., Fraietta I., Todoerti K., Miranda C., Mazzoni M., Re C., Colombo R., Ukmar G., et al. Identification of thyroid tumor cell vulnerabilities through a siRNA-based functional screening. Oncotarget. 2015;6:34629–34648. doi: 10.18632/oncotarget.5282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Nagel R., Stigter-van Walsum M., Buijze M., van den Berg J., van der Meulen I.H., Hodzic J., Piersma S.R., Pham T.V., Jiménez C.R., van Beusechem V.W., et al. Genome-wide siRNA Screen Identifies the Radiosensitizing Effect of Downregulation of MASTL and FOXM1 in NSCLC. Mol. Cancer. 2015;14:1434–1444. doi: 10.1158/1535-7163.MCT-14-0846. [DOI] [PubMed] [Google Scholar]
- 126.Cetti E., Di Marco T., Mauro G., Mazzoni M., Lecis D., Minna E., Gioiosa L., Brich S., Pagliardini S., Borrello M.G., et al. Mitosis perturbation by MASTL depletion impairs the viability of thyroid tumor cells. Cancer Lett. 2019;442:362–372. doi: 10.1016/j.canlet.2018.11.010. [DOI] [PubMed] [Google Scholar]
- 127.Taskinen M.E., Närvä E., Conway J.R.W., Hinojosa L.S., Lilla S., Mai A., De Franceschi N., Elo L.L., Grosse R., Zanivan S., et al. MASTL promotes cell contractility and motility through kinase-independent signaling. J. Cell Biol. 2020;219:e201906204. doi: 10.1083/jcb.201906204. [DOI] [PMC free article] [PubMed] [Google Scholar]