Abstract
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is an infectious disease with multiple severe symptoms, such as fever over 37.5°C, cough, dyspnea, and pneumonia. In our research, microRNAs (miRNAs) binding to the genome sequences of severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory-related coronavirus (MERS-CoV), and SARS-CoV-2 were identified by bioinformatic tools. Five miRNAs (hsa-miR-15a-5p, hsa-miR-15b-5p, hsa-miR-195-5p, hsa-miR-16-5p, and hsa-miR-196a-1-3p) were found to commonly bind to SARS-CoV, MERS-CoV, and SARS-CoV-2. We also identified miRNAs that bind to receptor proteins, such as ACE2, ADAM17, and TMPRSS2, which are important for understanding the infection mechanism of SARS-CoV-2. The expression patterns of those miRNAs were examined in hamster lung samples infected by SARS-CoV-2. Five miRNAs (hsa-miR-15b-5p, hsa-miR-195-5p, hsa-miR-221-3p, hsa-miR-140-3p, and hsa-miR-422a) showed differential expression patterns in lung tissues before and after infection. Especially, hsa-miR-15b-5p and hsa-miR-195-5p showed a large difference in expression, indicating that they may potentially be diagnostic biomarkers for SARS-CoV-2 infection.
Keywords: hamster lung, hsa-miR-15b-5p, hsa-miR-195-5p, microRNA, severe acute respiratory syndrome coronavirus 2
INTRODUCTION
In December 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), called coronavirus disease 2019 (COVID-19), believed to have originated in Wuhan, China, emerged and spread rapidly across more than 30 countries worldwide, resulting in a pandemic (World Health Organization, 2020b). COVID-19 presents with several severe symptoms, such as fever over 37.5°C, dry cough, severe dyspnea, and pneumonia (Anderson and Reiter, 2020; Wang et al., 2020). In addition, some patients have severe cardiovascular and permanent lung damage. COVID-19 is transmitted when droplets from an infected person penetrate the respiratory tract or mucous membrane of the eyes, nose, or mouth of another person. The World Health Organization (WHO) declared the COVID-19 outbreak as a Public Health Emergency of International Concern (PHEIC) on 30th January 2020, and, then, on 11th March 2020 COVID-19 was declared a “pandemic” (World Health Organization, 2020a). COVID-19 has been widely transmitted in the community compared to severe acute respiratory syndrome (SARS), which emerged in 2003, and Middle East respiratory syndrome (MERS), which emerged in 2012 (Zheng et al., 2020). Genome sequence analysis demonstrated that SARS-CoV, MERS-CoV, and SARS-CoV-2 belong to the beta-coronavirus genus (Chen et al., 2020c; Munster et al., 2020). There are only 380 amino acid substitutions that distinguish SARS-CoV-2 from SARS-like coronaviruses. Twenty-seven of these substitution mutations have been observed in genes encoding viral spike protein (S), although most differences were found in non-structural protein-coding genes. The viral spike protein is essential for cell receptor binding, cell entry, and viral infection. Studies suggest that the lower pathogenicity of SARS-CoV-2 compared to that of SARS-CoV is correlated to differences their genomic sequences (Benvenuto et al., 2020; Wu et al., 2020a). The pathogenesis and structure of SARS-CoV-2 were also analyzed in several previous studies (Gao et al., 2020; Mousavizadeh and Ghasemi, 2020; ul Qamar et al., 2020). However, research regarding molecular mechanisms and therapeutics is still required.
MicroRNAs (miRNAs) are a class of small non-coding RNA, 20-22 nucleotides in length. The seed region in miRNAs, approximately six nucleotides long, recognizes and binds to the complementary binding site of the target mRNA 3’untranslated region (3’UTR) to regulate its expression. Numerous studies suggest that miRNAs play an important role in diverse biological processes, such as cell differentiation, proliferation, apoptosis, oncogenesis, viral replication, and pathogenesis (Bartel, 2004; Cheng et al., 2005; Trobaugh and Klimstra, 2017; Zhang et al., 2007). miRNAs regulate several diseases, such as cancers, diabetes, and cardiovascular disease, by regulating the expression of target genes (Barwari et al., 2016; Cao et al., 2020; Chakraborty et al., 2014; Chen et al., 2020d; Liang and Li, 2020; Reddy, 2015). Moreover, recent studies have identified the association of miRNAs with antiviral effects by targeting both the 3’UTR and coding region of the viral genome (Gambardella et al., 2020; Guterres et al., 2020; Ivashchenko et al., 2020; Song et al., 2010; Wang et al., 2012). One study identified several miRNAs that interact with SARS-CoV, MERS-CoV, and SARS-CoV-2 viral genomes (Ivashchenko et al., 2020). Another study suggested that the virulence of COVID-19 in elderly patients is correlated with the types and abundances of host cellular miRNAs (Fulzele et al., 2020). Based on these previous studies (Hooykaas et al., 2016; Jopling et al., 2005; Trobaugh and Klimstra, 2017), we analyzed miRNAs binding to the sequences of SARS-CoV, MERS-CoV, and SARS-CoV-2. Additionally, we investigated miRNAs binding to receptor proteins, including ACE2 (angiotensin-converting enzyme 2), ADAM17 (ADAM metallopeptidase domain 17), and TMPRSS2 (type II transmembrane serine proteases), that are important for the entry of the SARS-CoV-2 into host cells. In this study, bioinformatic and evolutionary analyses of SARS-CoV-2 were performed, and the expression of miRNAs was also confirmed. Our findings suggest that specific miRNAs may potentially be diagnostic biomarkers for COVID-19 and present new therapeutic insights regarding COVID-19.
MATERIALS AND METHODS
Ethical statement
Experiments with the Male golden Syrian hamsters were carried out in accordance with the guidelines and regulations approved by the Institutional Animal Care and Use Committee of Jeonbuk National University (No. CBNU 2020-56).
Cell culture and virus
African green monkey kidney clone E6 (Vero-E6) cells were grown in Dulbecco’s modified Eagle’s medium containing 10% fetal bovine serum, MEM non-essential amino acids, 2 mM L-Glutamine, 100 Units/ml penicillin, and 0.1 mg/ml streptomycin (Hyclone, USA). Cells were cultured at 37°C in a 5% CO2 incubator. SARS-CoV-2 (NCCP43326) was obtained from the Korean Centers for Disease Control and Prevention (Korea). Virus stocks were prepared and concentrated by ultracentrifugation with 30% sucrose at 23,000 rpm for 5 h, using an Optima XPN-100 ultracentrifuge (Beckman Coulter, USA). The collected pellets were dissolved in phosphate buffered saline (PBS) pH 7.4. The final viral titer was determined using the plaque assay. All experimental procedures were performed in the Biosafety Level 3 (BSL-3) facility of the Korea Zoonosis Research Institute at Jeonbuk National University.
Hamster infection and lung RNA preparation
Male golden Syrian hamsters were acclimatized at the BSL-3 facility and maintained according to protocols approved by the Institutional Animal Care and Use Committee of Jeonbuk National University (No. CBNU 2020-56). Five golden Syrian hamsters were lightly anesthetized with isoflurane and intra-nasally inoculated with 1 × 106 PFU SARS-CoV-2 in a 100 μl volume. As an uninfected control, five hamsters were intra-nasally inoculated with 100 μl of PBS. All hamsters were euthanized 4 days post-infection, and lungs were collected for RNA extraction. Lung tissues were homogenized in RNAiso plus (Takara, Japan), and total RNA was prepared according to the manufacturer’s protocol.
Viral genome sequences acquirement and bioinformatic analysis of miRNAs
Complete viral genome sequences of SARS-CoV-2 isolated from nine countries were obtained using the National Center for Biotechnology Information (NCBI) database (http://www.ncbi.nlm.nih.gov/); the accession numbers are as follows: MT077125, MT188339, MT292573, MT320891, MT192759, MT327745, MT007544, MT281577, and MT304476. SARS-CoV (AY394850.2) and MERS-CoV (KT326819.1) sequences were also obtained from the NCBI database. Prediction of human miRNAs that bind to each viral genome was conducted using the miRDB software (http://www.mirdb.org/), and only those miRNAs with target scores over 95 were selected (Fulzele et al., 2020). Moreover, miRNAs that bind to three important genes (ACE2, TMPRSS2, and ADAM17) relating to the internalization of SARS-CoV-2 were detected using TargetScan 7.2 (http://www.targetscan.org/vert_72/). Five common miRNAs (hsa-miR-15a-5p, hsa-miR-15b-5p, hsa-miR-195-5p, hsa-miR-16-5p, and hsa-miR-196a-1-3p) that bind to all three viral genomes were analyzed using the Cytoscape software (v3.7.2). The mature sequences of five miRNAs were identified using miRBase v22.1 (http://www.mirbase.org), and four miRNAs were identified as belonging to the miR-15 family. The weblogo 3 database (http://weblogo.threeplusone.com/) was used to visualize the sequence conservation of the four miRNAs.
Phylogenetic analysis
Five common mature miRNAs sequences were aligned using the program, Bioedit (v7.0.5). The phylogenetic tree was constructed through the Neighbor joining method using the MEGA7 software (http://www.megasoftware.net/mega.php). For the phylogenetic tree, the Maximum Composite Likelihood method was used, and bootstrap evaluation of the branching patterns was estimated with 500 replicates.
Quantitative real-time polymerase chain reaction (qRT-PCR) amplification of miRNAs
Five hundred nanograms of total RNA samples from infected hamster lung tissues and the control tissues were used for the synthesis of complementary DNA (cDNA), required for the analysis of miRNAs. The HB miR Multi Assay Kit™ System I (HeimBiotek, Korea) was used to investigate miRNA expression in a 2-step process. In the initial step—cDNA synthesis—the HB_I Reverse Transcription (RT) Reaction Kit was used in accordance with the manufacturer's instructions, with a thermal cycler (Eppendorf, Germany), with cycling conditions of at 37°C for 60 min, followed by incubation at 95°C for 5 min, and then holding at 4°C. The final cDNA product, 20 μl per sample, was then used for step two of the HB miR Multi Assay Kit™ System I (HeimBiotek)—qRT-PCR. This step was performed using HB_I Real-time PCR Master mix kit according to manufacturer’s protocol in a Rotor-Gene Q system (Qiagen, Germany); amplification conditions were as follows: initial denaturation for 15 min at 95°C; 45 thermal cycles of 95°C for 10 s and 60°C for 40 s; standard melting conditions of ramp ranging from 55°C to 99°C, rising by 1°C at each step. The small nuclear RNA (snRNA), U6 was used as the reference gene for miRNA expression analysis. All samples were amplified in triplicate, and the relative expression data were analyzed in accordance with the 2-ΔCt method. The mean ± SD of triplicate data were plotted on bar graphs.
RESULTS
Bioinformatic analysis of miRNA binding sites in the SARS-CoV, MERS-CoV, and SARS-CoV-2 genomes
Sequences of SARS-CoV, MERS-CoV, and SARS-CoV-2 complete viral genomes were obtained using the NCBI database, and prediction of miRNAs that bind to each viral genome was conducted using the miRDB software (Fulzele et al., 2020). The number of miRNAs with target scores over 95 for SARS-CoV-2, MERS-CoV, and SARS-CoV were 49, 19, and 16, respectively; the highest number of such miRNAs was for SARS-CoV-2 (Table 1). There were two miRNAs, hsa-miR-15a-5p and hsa-miR-15b-5p, that bound to SARS-CoV with a target score of 100, but none that bound to MERS-CoV and SARS-CoV-2 with such a target score. Six miRNAs with a target score of 99 for binding to SARS-CoV-2 and SARS-CoV each were as follows: hsa-miR-4288, hsa-miR-195-5p, hsa-miR-16-5p, hsa-miR-15b-5p, hsa-miR-15a-5p, and hsa-miR-6838-5p for SARS-CoV-2 and hsa-miR-195-5p, hsa-miR-16-5p, hsa-miR-497-5p, hsa-miR-424-5p, hsa-miR-6838-5p, and hsa-miR-4291 for SARS-CoV. The miRNAs binding to each viral genome according and their target scores are listed in Table 1.
Table 1.
The list of predicted miRNAs that bind to viral genome
| Target score | SARS-CoV-2 | MERS-CoV | SARS-CoV |
|---|---|---|---|
| 100 | 0 | 0 | hsa-miR-15b-5p, hsa-miR-15a-5p |
| 99 | has-miR-4288, has-miR-195-5p has-miR-16-5p, has-miR-15b-5p has-miR-15a-5p, has-miR-6838-5p |
0 | hsa-miR-195-5p, hsa-miR-16-5p hsa-miR-497-5p, hsa-miR-424-5p hsa-miR-6838-5p, hsa-miR-4291 |
| 98 | has-miR-497-5p, hsa-miR-424-5p hsa-miR-3133, hsa-miR-21-3p |
hsa-miR-633 | hsa-miR-196a-1-3p |
| 97 | hsa-miR-122b-3p, hsa-miR-559 hsa-miR-196a-1-3p, hsa-miR-548y hsa-miR-548w, hsa-miR-548o-5p hsa-miR-548h-5p, hsa-miR-548d-5p hsa-miR-548c-5p, hsa-miR-548bb-5p hsa-miR-548b-5p, hsa-miR-548ay-5p hsa-miR-548au-5p, hsa-miR-548ar-5p hsa-miR-548am-5p, hsa-miR-548ak hsa-miR-548ae-5p, hsa-miR-548ad-5p hsa-miR-548aq-5p, hsa-miR-302c-5p |
hsa-miR-4477a hsa-miR-381-3p hsa-miR-300 hsa-miR-551b-5p |
hsa-miR-451b hsa-miR-505-3p |
| 96 | hsa-miR-548a-5p, hsa-miR-548as-5p hsa-miR-548ab, hsa-miR-4684-3p hsa-miR-409-3p, hsa-miR-548j-5p hsa-miR-548i, hsa-miR-548ap-5p |
hsa-miR-302c-5p, hsa-miR-29c-3p hsa-miR-29b-3p, hsa-miR-29a-3p hsa-miR-196a-1-3p, hsa-miR-15b-5p hsa-miR-195-5p, hsa-miR-16-5p hsa-miR-15a-5p, hsa-miR-5688 |
hsa-miR-597-5p hsa-miR-4524b-5p hsa-miR-4524a-5p hsa-miR-585-5p |
| 95 | hsa-miR-186-5p, hsa-miR-545-3p hsa-miR-6835-3p, hsa-miR-30c-5p hsa-miR-30b-5p, hsa-miR-6830-3p hsa-miR-30e-5p, hsa-miR-30d-5p hsa-miR-30a-5p, hsa-miR-3686 hsa-miR-505-3p |
hsa-miR-548e-5p hsa-miR-7-1-3p hsa-miR-495-3p hsa-miR-7159-5p |
hsa-miR-4672 |
| Total | 49 | 19 | 16 |
Predicted miRNAs that bind to each viral genome of SARS-CoV-2, MERS-CoV, and SARS-CoV were listed. Prediction of the miRNAs were conducted by using miRDB database and only those target scores over 95 have selected. Each row showed miRNAs that correspond to indicated target score. The number of the total miRNAs were counted bottom of the table.
Bioinformatic and evolutionary analyses of five miRNAs binding to all three viral genomes assessed
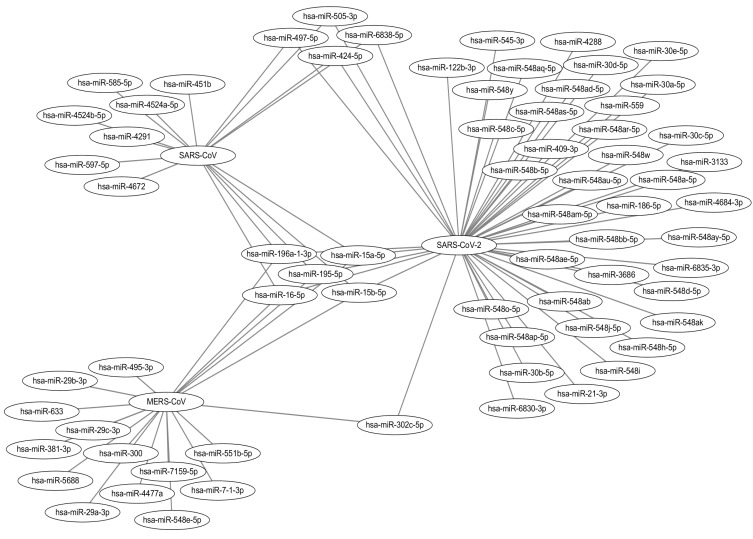
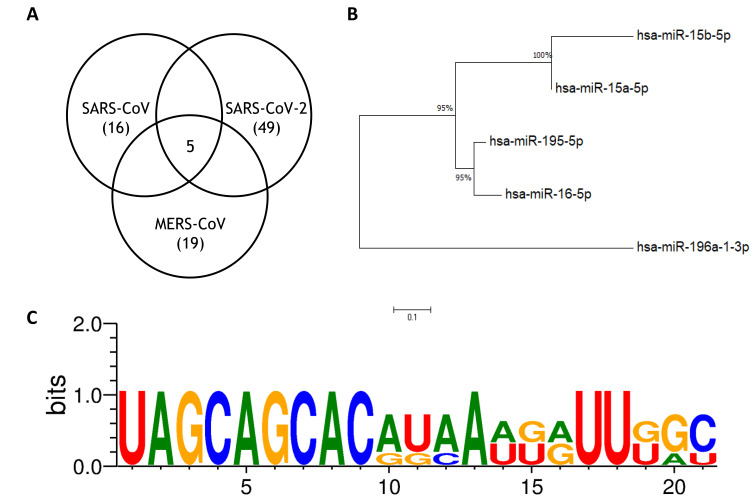
To find miRNAs that bind to all three viral genomes assessed, a Cytoscape program was used, with a list of miRNAs bound to each virus (Fig. 1). This result was also indicated as vann-diagrams (Fig. 2A). Five miRNAs, hsa-miR-15a-5p, hsa-miR-15b-5p, hsa-miR-16-5p, hsa-miR-195-5p, and hsa-miR-196a-1-3p, were found to bind to all their viral genomes. Phylogenetic analysis was conducted to identify the relationship between these miRNAs (Fig. 2B). hsa-miR-15b-5p and hsa-miR-15a-5p were combined into a sister group. hsa-miR-195-5p and hsa-miR-16-5p were combined into another sister group. hsa-miR-196a-1-3p was placed in an outgroup. The mature miRNA seed sequences obtained from the miRBase database were the same for all the above-mentioned miRNAs, except hsa-miR-196a-1-3p. The four miRNAs included in the two sister groups were revealed to be part of the miR-15 family in a previous study (Finnerty et al., 2010). Sequence conservation was visually determined using the weblogo 3 database (Fig. 2C).
Fig. 1. Common miRNAs that bind to all three viral genomes.
Common miRNAs that bind to all three viral genomes (SARS-CoV-2, MERS-CoV, and SARS-CoV). Five miRNAs named hsa-miR-15a-5p, hsa-miR-15b-5p, hsa-miR-16-5p, hsa-miR-195-5p, and hsa-miR-196a-1-3p are represented as common miRNAs by Cytoscape.
Fig. 2. Phylogenetic tree and the conservation of the five common miRNAs.
(A) The number of the total miRNAs that bind to each viral genome and the common miRNAs are represented by Venn diagram. (B) Phylogenetic tree of the five common miRNAs mature sequences obtained from miRbase database. The tree was constructed by Neighbor joining method implemented in the MEGA7 program. (C) Evolutionary conserved miRNA seed sequences of two sister group was shown using weblogo3 database.
Locations of the miRNA seed binding sites and the lengths of the target sites on the SARS-CoV-2 viral genome
Isolates from nine countries were selected to identify the number of binding regions and locations of the target sites for the five common miRNAs in the SARS-CoV-2 viral genome. Since the four miRNAs in the miR-15 family have the same seed region, their results are presented together in Table 2. For these four miRNAs, a total of 14 binding sites were detected in all nine countries; however, the binding locations were different in some countries. The binding sites in the USA and Spain isolates were the same; those in the Australia, China, and South Korea isolates were the same; and those in the isolates from the other four countries were different. The seed types corresponding to the binding locations are shown on the right side of the table and indicate the types of pairing between the viral genome and the seed sequences of the miRNAs. The seed types for all 14 binding sites were the same in the nine countries, despite the sequences of isolates from the nine countries being different. In Table 3, the binding sites and seed types of hsa-miR-196a-1-3p for the SARS-CoV-2 genome isolated from nine countries were indicated. The binding locations and the corresponding seed types were different from those indicated in Table 2 because of the sequence difference between the miRNAs, but the same countries were grouped for hsa-miR-196a-1-3p binding locations as in the abovementioned results.
Table 2.
Locations of miR-15 family seed binding sites and target site length on SARS-CoV-2 viral genome
| Italy (MT077125) |
USA (MT188339) |
Spain (MT292573) |
Iran (MT320891) |
Taiwan (MT192759) |
Turkey (MT327745) |
Australia (MT007544) |
China (MT281577) |
South Korea (MT304476) |
|
|---|---|---|---|---|---|---|---|---|---|
| 3107 | 3109 | 3109 | 3119 | 3136 | 3159 | 3163 | 3163 | 3163 | 7mer-m8 |
| 8401 | 8403 | 8403 | 8413 | 8430 | 8453 | 8457 | 8457 | 8457 | 9mer |
| 8558 | 8560 | 8560 | 8570 | 8587 | 8610 | 8614 | 8614 | 8614 | 8mer |
| 13034 | 13036 | 13036 | 13046 | 13063 | 13086 | 13090 | 13090 | 13090 | 8mer |
| 14506 | 14508 | 14508 | 14518 | 14535 | 14558 | 14562 | 14562 | 14562 | 7mer-m8 |
| 14725 | 14727 | 14727 | 14743 | 14754 | 14777 | 14781 | 14781 | 14781 | 8mer |
| 19801 | 19803 | 19803 | 19819 | 19830 | 19853 | 19857 | 19857 | 19857 | 8mer |
| 24038 | 24040 | 24040 | 24056 | 24067 | 24090 | 24094 | 24094 | 24094 | 8mer |
| 24578 | 24580 | 24580 | 24596 | 24607 | 24630 | 24634 | 24634 | 24634 | 8mer |
| 25627 | 25629 | 25629 | 25645 | 25656 | 25679 | 25683 | 25683 | 25683 | 7mer-m8 |
| 26667 | 26669 | 26669 | 26685 | 26696 | 26719 | 26723 | 26723 | 26723 | 7mer-m8 |
| 28865 | 28867 | 28867 | 28883 | 28894 | 28917 | 28921 | 28921 | 28921 | 7mer-m8 |
| 28879 | 28881 | 28881 | 28897 | 28908 | 28931 | 28935 | 28935 | 28935 | 7mer-m8 |
| 28967 | 28969 | 28969 | 28985 | 28996 | 29019 | 29023 | 29023 | 29023 | 7mer-m8 |
Four miRNAs, hsa-miR-15a-5p, hsa-miR-15b-5p, hsa-miR-16-5p and hsa-miR-195-5p, which belongs to the miR-15 family, have the same seed region and target sites. SARS-CoV-2 sequences isolated from nine countries were obtained from NCBI database to identify the miRNAs binding. Among them, the sequences that isolated from USA and Spain showed the same binding locations, and Australia, China, and South Korea were the same.
Table 3.
Locations of hsa-miR-196a-1-3p seed binding sites and target site length on SARS-CoV-2 viral genome
| Italy(MT077125) | USA(MT188339) | Spain(MT292573) | Iran(MT320891) | Taiwan(MT192759) | Turkey(MT327745) | Australia(MT007544) | China(MT281577) | South Korea(MT304476) | |
|---|---|---|---|---|---|---|---|---|---|
| 1301 | 1303 | 1303 | 1313 | 1330 | 1353 | 1357 | 1357 | 1357 | 8mer |
| 1520 | 1522 | 1522 | 1532 | 1549 | 1572 | 1576 | 1576 | 1576 | 8merα |
| 2021 | 2023 | 2023 | 2033 | 2050 | 2073 | 2077 | 2077 | 2077 | 7mer-m8 |
| 4075 | 4077 | 4077 | 4087 | 4104 | 4127 | 4131 | 4131 | 4131 | 8merβ |
| 5867 | 5869 | 5869 | 5879 | 5896 | 5919 | 5923 | 5923 | 5923 | 7mer-m8 |
| 8158 | 8160 | 8160 | 8170 | 8187 | 8210 | 8214 | 8214 | 8214 | 9merα |
| 10882 | 10884 | 10884 | 10894 | 10911 | 10934 | 10938 | 10938 | 10938 | 8merβ |
| 16804 | 16806 | 16806 | 16822 | 16833 | 16856 | 16860 | 16860 | 16860 | 7mer-m8 |
| 21878 | 21880 | 21880 | 21896 | 21907 | 21930 | 21934 | 21934 | 21934 | 10merβ |
| 25245 | 25247 | 25247 | 25263 | 25274 | 25297 | 25301 | 25301 | 25301 | 7mer-m8 |
| 25587 | 25589 | 25589 | 25605 | 25616 | 25639 | 25643 | 25643 | 25643 | 8merα |
| 28182 | 28184 | 28184 | 28200 | 28211 | 28234 | 28238 | 28238 | 28238 | 7mer-m8 |
In case of hsa-miR-196a-1-3p, which is out group of the five miRNAs, showed same aspect with the four miRNAs; hsa-miR-15a-5p, hsa-miR-15b-5p, hsa-miR-16-5p, and hsa-miR-195-5p.
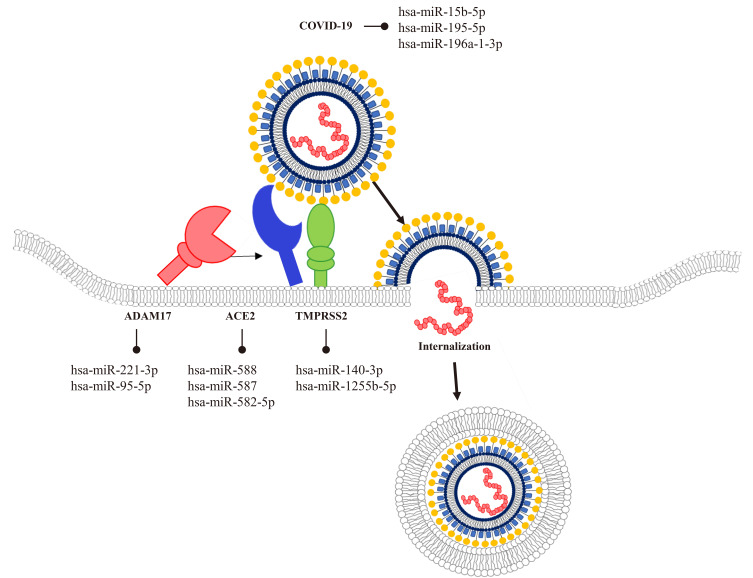
Basic understanding of the ACE2-dependent SARS-CoV-2 infection
ACE2, TMPRSS2, and ADAM17 are important proteins involved in SARS-CoV-2 infection. ACE2 binds to the S protein processed by TMPRSS2, and ADAM17 is involved in ACE2- dependent shedding, which is associated with lung pathogenesis (Heurich et al., 2014; Wang et al., 2008). In our study, miRNAs targeting three proteins (ACE2, TMPRSS2, and ADAM17) associated with SARS-CoV-2 were identified using the TargetScan and miRDB databases (Fig. 3). Among the predicted miRNAs, seven candidates were selected; hsa-miR-221-3p and hsa-miR-95-5p targeting ADAM17; hsa-miR-588, hsa-miR-587, and hsa-miR-582-5p targeting ACE2; and hsa-miR-140-3p and hsa-miR-1255b targeting TMPRSS2.
Fig. 3. Schematic illustration of ACE2-dependent SARS-CoV-2 infection.
ACE2 is the key entry receptor for internalization of SARS-CoV-2 that interacts with the viral spike (S) protein. As one of the structural proteins of the virus, S protein is processed by TMPRSS2 and then binds to the ACE2. When the protein binds to the extracellular domain of the receptor, endocytosis is mediated and then endosome is acidified. Acidification of the endosome results in fusion of the viral and cellular membrane, and then the single stranded RNA enters to the cytosol of the host cell.
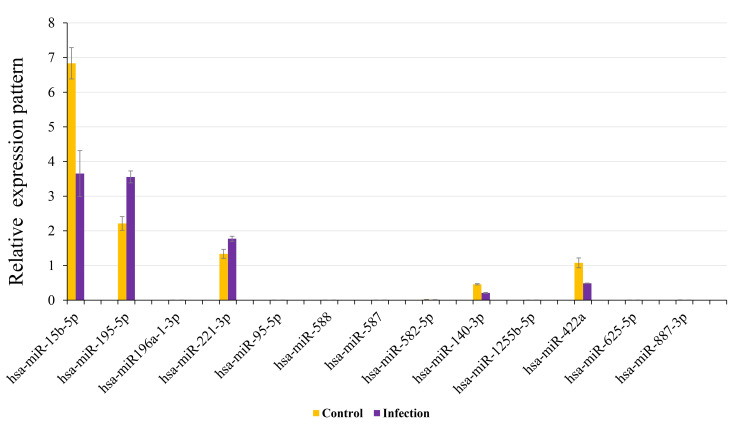
Relative expression analyses of miRNAs in hamster lung tissue infected with SARS-CoV-2
The relative expression levels of miRNAs binding to the SARS-CoV, MERS-CoV, and SARS-CoV-2 genomes were examined in hamster lung samples before and after infection (Fig. 4). Among the five miRNAs which bind to all three viral genomes, the expression levels of hsa-miR-15b-5p, hsa-miR-195-5p, and hsa-miR-196a-1-3p were identified by qRT-PCR. hsa-miR-15b-5p was downregulated and hsa-miR-195-5p was upregulated in infected samples compared to the control. No significant difference in hsa-miR-196a-1-3p expression was revealed. With regards to miRNAs targeting the above-mentioned proteins, hsa-miR-221-3p and hsa-miR-140-3p, targeting ADAM17 and TMPRSS2, respectively, showed opposite expression patterns in the infected samples; hsa-miR-221-3p was upregulated and hsa-miR-140-3p was downregulated. Other miRNAs showed no significant expression differences. Moreover, the expression patterns of miRNAs derived from transposable elements (hsa-miR-422a, hsa-miR-625-5p, hsa-miR-887-3p) were also analyzed. Among these miRNAs, only hsa-miR-422a displayed a significant difference in expression before and after infection. Taken together, these findings indicate that hsa-miR-15b-5p, hsa-miR-140-3p, and hsa-miR-422a were downregulated, and hsa-miR-195-5p and hsa-miR-221-3p were upregulated in infected samples. hsa-miR-15b-5p and hsa-miR-195-5p showed the most significant differences in expression before and after infection.
Fig. 4. Expression Analysis of miRNAs in hamster lung tissue.
Comparative expression patterns of total thirteen miRNAs are analyzed using infected hamster lung tissue and its control by qPCR. Expression data were normalized to U6 in miRNAs. The miRNAs are classified into 5 groups; targeting SARS-CoV-2, AMAM17, ACE2, TMPRSS2 and the miRNAs derived from transposable elements.
DISCUSSION
The present study suggests that specific miRNAs will show distinct relative expression to against SARS-CoV-2 infection and could have an important role while the viral infection. For evolutionary and bioinformatic analyses, we selected candidates of specific miRNAs which target all three viral genome, SARS-CoV, MERS-CoV, and SARS-CoV-2. In addition, miRNAs that target core receptor proteins, ACE2, TMPRSS2, and ADAM17 were also identified. The relative expression analyses in hamster lung tissues for the viral infection were performed by qRT-PCR. These analyses could provide further understanding on correlation between relative miRNA expressions and virus infection.
SARS-CoV-2 has a typical genomic structure, similar to those of other beta coronaviruses. Its genome contains 14 open reading frames (ORFs), encoding 27 proteins. ORF1 and ORF2 in the 50-terminal region of the SARS-CoV-2 genome encode 15 non-structural proteins crucial for virus replication (Malik et al., 2020; Wu et al., 2020a). SARS-CoV-2 consists of three structural proteins encoded by the 30-terminal region of the genome, the spike (S), envelope (E), and membrane (M) proteins, which form the viral envelope, and the nucleocapsid proteins, which includes the single-stranded RNA virus genome. Through genomic analysis, SARS-CoV-2 was found to have the same human membrane receptor as SARS-CoV, ACE2 (Wan et al., 2020). The viral spike protein mediates the entry of SARS-CoV-2 by binding to ACE2 (Das et al., 2020). ACE2, an ectoenzyme, is anchored to the plasma membrane of cells in the lower respiratory tract, heart, kidney, and gastrointestinal tract (Imai et al., 2010). Host cell-receptor binding is facilitated via the viral spike protein, processed by the type II transmembrane serine protease, TMPRSS2. The processed spike protein interacts with the extracellular domain of ACE2, forming a complex that is subsequently internalized with the help of clathrin (Chen et al., 2020b; Groß et al., 2020; Hoffmann et al., 2020). ADAM17, a transmembrane proteinase, cleaves the extracellular juxta-membrane region of ACE2. The ectodomain is catalytically activated and then released into the extracellular milieu through a process referred to as “shedding” (Wang et al., 2008). Some studies suggested that ACE2 shedding might be related to SARS-CoV entry into cells and replication (Haga et al., 2008; Liu et al., 2020). One study suggested that ADAM17-dependent ACE2 shedding promotes lung pathogenesis by reducing the expression level of the ACE2, which is known to prevent lung injury associated with SARS-CoV infection (Heurich et al., 2014). Our research found that the number of miRNAs that bind to SARS-CoV, MERS-CoV and SARS-CoV-2 were different. The number of miRNA binding to SARS-CoV-2 genome was much more than to the other two viruses (Table 1). The difference of the binding number between the three viral genomes may suggest the possibility of the SARS-CoV-2 evolution, gaining its own specific traits over time. Infection of the SARS-CoV and MERS-CoV is transmitted through unciliated bronchial epithelial cells and type II pneumocytes, and then cause several symptoms such as fever, dry cough, respiratory failure, and severe complications including pneumonia and kidney failure (Ashour et al., 2020; Drosten et al., 2003; Li et al., 2003; Zaki et al., 2012). In case of the SARS-CoV-2, it causes similar symptoms with the two viruses, but induces even severe cardiovascular damage and permanent lung damage (Anderson and Reiter, 2020; Chen et al., 2020a; Pedersen and Ho, 2020; Wang et al., 2020; Xu et al., 2020; Yang et al., 2020).
In accordance with the analysis of receptor affinity, SARS-CoV-2 has higher binding affinity to ACE2 than the 2003 strain of SARS-CoV (Wan et al., 2020). Compared to SARS-CoV and MERS-CoV, SARS-CoV-2 has a higher infectiousness and a lower mortality rate, resulting in a rapid transmission rate. Genetic analyses using the genomes of SARS-CoV-2 obtained from infected patients demonstrated that SARS-CoV-2 has 88% sequence similarity to bat SARSr-CoV, 79% similarity to SARS-CoV, and only 50% to MERS-CoV (Lu et al., 2020). According to the WHO report, the reproductive number (R0) of SARS-CoV-2 is 2 to 2.5, higher than those of SARS-CoV (1.7-1.9) and MERS-CoV (< 1) (Chen, 2020; Wu et al., 2020b). R0 indicates the average number of people who would catch the disease from one infected person in a population without previous disease records and represents the potential of disease spread (Delamater et al., 2019). Consistent with a recent, large descriptive study, the mortality rate of COVID-19 (2.3%) is lower than that of SARS (9.5%) and MERS (34.4%) (Chen, 2020; Munster et al., 2020; Epidemiology Working Group for NCIP Epidemic Response and Chinese Center for Disease Control and Prevention, 2020). These studies indicate that SARS-CoV-2 has more evolutionary suitable traits to infection compared to SARS-CoV and MERS-CoV. Our bioinformatic study identified there were much more miRNA binding sites in SARS-CoV-2 genome than other two viruses. We assumed that increasing of binding sites in viral genome could contribute to enhanced evolutionary traits through more sophisticated epigenetic controls.
Many studies have shown that miRNAs have a strong relationship with the pathogens (Abdel-Mohsen et al., 2014; Aqeilan et al., 2010; Pineau et al., 2010; Small et al., 2010; Zhu et al., 2018). In case of the viral infection, miRNAs could response in two conflicting ways; As an assistant of the virus to avoid host immune responses or as a protector of the host to fight against the virus. These regulations were may accomplished by directly bind to the viral genome or because of the gene regulation targeted by miRNAs (Ho et al., 2016; Piedade and Azevedo-Pereira, 2016; Scheel et al., 2016; Trobaugh and Klimstra, 2017). From the bioinformatic analysis in our study, 13 miRNAs were chosen as candidate key regulators of SARS-CoV-2 infection. As a result, five miRNAs, hsa-miR-15b-5p, hsa-miR-195-5p, hsa-miR-221-3p, hsa-miR-140-3p, and hsa-miR-422a, showed significant differences in expression against to SARS-CoV-2 infection. hsa-miR-15b-5p and hsa-miR-195-5p are members of the miR-15 family, which have the similar binding regions for target sites. The miR-15 family is known to regulate cell proliferation by targeting cell cycle proteins, such as cyclin D3 (CCND3), cyclin E1 (CCNE1), and CDK6 (Linsley et al., 2007; Liu et al., 2008). Furthermore, miR-15 family regulates apoptosis by targeting antiapoptotic gene Bcl-2 (Aqeilan et al., 2010; Bandi et al., 2009). One study demonstrated that the regulation of cell proliferation and apoptosis is controlled by hsa-miR-15b-5p which targets extracellular signal-regulated kinase 1 (ERK1) in rat PC12 cells. ERK1 is an essential component of the MAP kinase signaling pathway and regulates various cellular processes. Down-regulated ERK1 suppresses cell proliferation and promotes apoptosis (Luo et al., 2017; Wortzel and Seger, 2011; Zeng et al., 2005). hsa-miR-195-5p is well studied in cardiovascular diseases. In accordance with research regarding hsa-miR-195-5p expression during cardiac hypertrophy, hsa-miR-195-5p is up-regulated, potentially leading to fatal dilated cardiomyopathy because of the down regulation of the antiapoptotic factor, Bcl-2 (Small et al., 2010). In our study, the expression of hsa-miR-15b-5p was down-regulated and that of hsa-miR-195-5p was the up-regulated after SARS-CoV-2 infection. According to the above-mentioned studies, down regulation of hsa-miR-15b-5p may enable SARS-CoV-2 to escape the host immune defense by inhibiting apoptosis and promote the proliferation of infected cells. On the contrary, up-regulated hsa-miR-195-5p promotes apoptosis by inducing cell cycle arrest and prevents excessive proliferation of the infected cells as the host immune response.
The expression of hsa-miR-221-3p and hsa-miR-140-3p was also confirmed in both normal and infected samples, as miRNAs that bind to ADAM17 and TMPRSS2, respectively, which are important to SARS-CoV-2 infection. In one study, the expression of the hsa-miR-221-3p during the Hepatitis B virus (HBV) infection was analyzed. TANK Binding Kinase 1 (TBK1), the target gene of the hsa-miR-221-3p, encodes an important protein involved in interferon production and virus clearance (Pineau et al., 2010; Zhao, 2013). At the initial stage of the HBV infection, known as the immune-tolerant phase, hsa-miR-221-3p is highly expressed. Thereafter, down regulation of TBK1 suppresses the innate immune response and promotes viral persistence by permitting HBV replication (Singh et al., 2018). Based on this previous research, elevated hsa-miR-221-3p could be said to suppress the innate immune system and facilitate virus replication in the SARS-CoV-2 infected sample via similar molecular mechanisms as in HBV infection. Moreover, hsa-miR-140-3p is related to the regulation of cell proliferation and apoptosis by targeting the Bcl-2 gene, similarly to other members of the miR-15 family. A previous study revealed that decreased expression of hsa-miR140-3p and increased cell proliferation were observed in artery smooth muscle cells isolated from peripheral artery disease arteries (Zhu et al., 2018). In our study, the down regulation of hsa-miR-140-3p may have supported virus infection by inhibiting apoptosis and promoting cell proliferation.
We also conducted expression analysis of the miRNAs derived from transposable elements (TE), which have the ability to move around the host genome and are involved in many biological processes (Casacuberta and González, 2013; McCue et al., 2012; Slotkin and Martienssen, 2007). Moreover, TEs could generate new factors, and one of these factors is non-coding RNAs, including miRNAs (Piriyapongsa et al., 2007; Roberts et al., 2013; Smalheiser and Torvik, 2005). Research regarding hsa-miR-307, derived from the long terminal repeat element of an endogenous retrovirus in olive flounder, provided insight about the enhancer activity of the miRNA (Lee et al., 2019). miRNAs derived from TEs also have a strong relationship with human diseases (Jin and Lee, 2016; Lee et al., 2020; Murakami et al., 2006; Pinto et al., 2018); for instance, hsa-miR-422a is significantly down-regulated after IFN-α/ribavirin treatment in patients infected with HIV-1 (Abdel-Mohsen et al., 2014). The study suggested that hsa-miR-422a targets genes associated with p53-dependent apoptosis, such as MLH1 and TP53 (Abdel-Mohsen et al., 2014; Yanamadala and Ljungman, 2003; Zhang et al., 1999). We observed that hsa-miR-422a was down-regulated in the SARS-CoV-2-infected sample; thus, it could be assumed that hsa-miR-422a promotes the apoptosis of infected cells by inducing the host immune response. In conclusion, we suggest that multiple miRNAs are involved in the regulation of the human immune response to SARS-CoV-2 infection. Above all, hsa-miR-15b-5p and hsa-miR-195-5p showed the most distinctive expression patterns compared to other miRNAs. This study suggests that specific miRNAs which directly bind to the SARS-CoV-2 genome, including hsa-miR-15b-5p and hsa-miR-195-5p could have important function in SARS-CoV-2 infection.
Footnotes
AUTHOR CONTRIBUTIONS
W.R.K. and E.G.P. designed and performed all the experiments and wrote the manuscript, K.W.K., S.M.L., and B.K. provided the hamster samples, and H.S.K. commented on and revised the manuscript. All authors have read and agree to the final version of the manuscript.
CONFLICT OF INTEREST
The authors have no potential conflicts of interest to disclose.
REFERENCES
- Abdel-Mohsen M., Deng X., Danesh A., Liegler T., Jacobs E.S., Rauch A., Ledergerber B., Norris P.J., Günthard H.F., Wong J.K., et al. Role of microRNA modulation in the interferon-α/ribavirin suppression of HIV-1 in vivo. PLoS One. 2014;9:e109220. doi: 10.1371/journal.pone.0109220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson G., Reiter R.J. Melatonin: roles in influenza, Covid‐19, and other viral infections. Rev. Med. Virol. 2020;30:e2109. doi: 10.1002/rmv.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aqeilan R., Calin G.A., Croce C.M. miR-15a and miR-16-1 in cancer: discovery, function and future perspectives. Cell Death Differ. 2010;17:215–220. doi: 10.1038/cdd.2009.69. [DOI] [PubMed] [Google Scholar]
- Ashour H.M., Elkhatib W.F., Rahman M., Elshabrawy H.A. Insights into the recent 2019 novel coronavirus (SARS-CoV-2) in light of past human coronavirus outbreaks. Pathogens. 2020;9:186. doi: 10.3390/pathogens9030186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandi N., Zbinden S., Gugger M., Arnold M., Kocher V., Hasan L., Kappeler A., Brunner T., Vassella E. miR-15a and miR-16 are implicated in cell cycle regulation in a Rb-dependent manner and are frequently deleted or down-regulated in non-small cell lung cancer. Cancer Res. 2009;69:5553–5559. doi: 10.1158/0008-5472.CAN-08-4277. [DOI] [PubMed] [Google Scholar]
- Bartel D.P. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116:281–297. doi: 10.1016/S0092-8674(04)00045-5. [DOI] [PubMed] [Google Scholar]
- Barwari T., Joshi A., Mayr M. MicroRNAs in cardiovascular disease. J. Am. Coll. Cardiol. 2016;68:2577–2584. doi: 10.1016/j.jacc.2016.09.945. [DOI] [PubMed] [Google Scholar]
- Benvenuto D., Giovanetti M., Ciccozzi A., Spoto S., Angeletti S., Ciccozzi M. The 2019‐new coronavirus epidemic: evidence for virus evolution. J. Med. Virol. 2020;92:455–459. doi: 10.1002/jmv.25688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao X., Zhang G., Li T., Zhou C., Bai L., Zhao J., Tursun T. LINC00657 knockdown suppresses hepatocellular carcinoma progression by sponging miR-424 to regulate PD-L1 expression. Genes Genomics. 2020;42:1361–1368. doi: 10.1007/s13258-020-01001-y. [DOI] [PubMed] [Google Scholar]
- Casacuberta E., González J. The impact of transposable elements in environmental adaptation. Mol. Ecol. 2013;22:1503–1517. doi: 10.1111/mec.12170. [DOI] [PubMed] [Google Scholar]
- Chakraborty C., Doss C.G.P., Bandyopadhyay S., Agoramoorthy G. Influence of miRNA in insulin signaling pathway and insulin resistance: micro‐molecules with a major role in type‐2 diabetes. Wiley Interdiscip. Rev. RNA. 2014;5:697–712. doi: 10.1002/wrna.1240. [DOI] [PubMed] [Google Scholar]
- Chen J. Pathogenicity and transmissibility of 2019-nCoV-a quick overview and comparison with other emerging viruses. Microbes Infect. 2020;22:69–71. doi: 10.1016/j.micinf.2020.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Li X., Chen M., Feng Y., Xiong C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc. Res. 2020a;116:1097–1100. doi: 10.1093/cvr/cvaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Chang G., Chen X., Li Y., Li H., Cheng D., Tang Y., Sang H. IL-6-miR-210 suppresses regulatory T cell function and promotes atrial fibrosis by targeting Foxp3. Mol. Cells. 2020b;43:438–447. doi: 10.14348/molcells.2019.2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Guo Y., Pan Y., Zhao Z.J. Structure analysis of the receptor binding of 2019-nCoV. Biochem. Biophys. Res. Commun. 2020c;525:135–140. doi: 10.1016/j.bbrc.2020.02.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Liu Q., Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J. Med. Virol. 2020d;92:418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng A.M., Byrom M.W., Shelton J., Ford L.P. Antisense inhibition of human miRNAs and indications for an involvement of miRNA in cell growth and apoptosis. Nucleic Acids Res. 2005;33:1290–1297. doi: 10.1093/nar/gki200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das G., Mukherjee N., Ghosh S. Neurological insights of COVID-19 pandemic. ACS Chem. Neurosci. 2020;11:1206–1209. doi: 10.1021/acschemneuro.0c00201. [DOI] [PubMed] [Google Scholar]
- Delamater P.L., Street E.J., Leslie T.F., Yang Y.T., Jacobsen K.H. Complexity of the basic reproduction number (R0) Emerg. Infect. Dis. 2019;25:1–4. doi: 10.3201/eid2501.171901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drosten C., Günther S., Preiser W., Van Der Werf S., Brodt H.R., Becker S., Rabenau H., Panning M., Kolesnikova L., Fouchier R.A. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N. Engl. J. Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- Epidemiology Working Group for NCIP Epidemic Response and Chinese Center for Disease Control and Prevention. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. Chinese. [DOI] [PubMed] [Google Scholar]
- Finnerty J.R., Wang W.X., Hébert S.S., Wilfred B.R., Mao G., Nelson P.T. The miR-15/107 group of microRNA genes: evolutionary biology, cellular functions, and roles in human diseases. J. Mol. Biol. 2010;402:491–509. doi: 10.1016/j.jmb.2010.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulzele S., Sahay B., Yusufu I., Lee T.J., Sharma A., Kolhe R., Isales C.M. COVID-19 virulence in aged patients might be impacted by the host cellular MicroRNAs abundance/profile. Aging Dis. 2020;11:509. doi: 10.14336/AD.2020.0428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambardella J., Sardu C., Morelli M.B., Messina V., Castellanos V., Marfella R., Maggi P., Paolisso G., Wang X., Santulli G. Exosomal microRNAs drive thrombosis in COVID-19. medRxiv. 2020 doi: 10.1101/2020.06.16.20133256. [DOI] [Google Scholar]
- Gao Y., Yan L., Huang Y., Liu F., Zhao Y., Cao L., Wang T., Sun Q., Ming Z., Zhang L. Structure of the RNA-dependent RNA polymerase from COVID-19 virus. Science. 2020;368:779–782. doi: 10.1126/science.abb7498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groß S., Jahn C., Cushman S., Bär C., Thum T. SARS-CoV-2 receptor ACE2-dependent implications on the cardiovascular system: from basic science to clinical implications. J. Mol. Cell. Cardiol. 2020;144:47–53. doi: 10.1016/j.yjmcc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guterres A., de Azeredo Lima C.H., Miranda R.L., Gadelha M.R. What is the potential function of microRNAs as biomarkers and therapeutic targets in COVID-19? Infect. Genet. Evol. 2020;85:104417. doi: 10.1016/j.meegid.2020.104417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haga S., Yamamoto N., Nakai-Murakami C., Osawa Y., Tokunaga K., Sata T., Yamamoto N., Sasazuki T., Ishizaka Y. Modulation of TNF-α-converting enzyme by the spike protein of SARS-CoV and ACE2 induces TNF-α production and facilitates viral entry. Proc. Natl. Acad. Sci. U. S. A. 2008;105:7809–7814. doi: 10.1073/pnas.0711241105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heurich A., Hofmann-Winkler H., Gierer S., Liepold T., Jahn O., Pöhlmann S. TMPRSS2 and ADAM17 cleave ACE2 differentially and only proteolysis by TMPRSS2 augments entry driven by the severe acute respiratory syndrome coronavirus spike protein. J. Virol. 2014;88:1293–1307. doi: 10.1128/JVI.02202-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho B.C., Yang P.C., Yu S.L. MicroRNA and pathogenesis of enterovirus infection. Viruses. 2016;8:11. doi: 10.3390/v8010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.H., Nitsche A., et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.:e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooykaas M.J., Kruse E., Wiertz E.J., Lebbink R.J. Comprehensive profiling of functional Epstein-Barr virus miRNA expression in human cell lines. BMC Genom. 2016;17:1–13. doi: 10.1186/s12864-016-2978-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai Y., Kuba K., Ohto-Nakanishi T., Penninger J.M. Angiotensin-converting enzyme 2 (ACE2) in disease pathogenesis. Circ. J. 2010;74:405–410. doi: 10.1253/circj.CJ-10-0045. [DOI] [PubMed] [Google Scholar]
- Ivashchenko A., Rakhmetullina A., Aisina D. How miRNAs can protect humans from coronaviruses COVID-19, SARS-CoV, and MERS-CoV. Research Square. 2020 doi: 10.21203/rs.3.rs-16264/v1. https://doi.org/10.21203/rs.3.rs-16264/v1. [DOI] [Google Scholar]
- Jin D., Lee H. Prioritizing cancer-related microRNAs by integrating microRNA and mRNA datasets. Sci. Rep. 2016;6:35350. doi: 10.1038/srep35350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jopling C.L., Yi M., Lancaster A.M., Lemon S.M., Sarnow P. Modulation of hepatitis C virus RNA abundance by a liver-specific MicroRNA. Science. 2005;309:1577–1581. doi: 10.1126/science.1113329. [DOI] [PubMed] [Google Scholar]
- Lee H.E., Huh J.W., Kim H.S. Bioinformatics analysis of evolution and human disease related transposable element-derived microRNAs. Life. 2020;10:95. doi: 10.3390/life10060095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H.E., Jo A., Im J., Cha H.J., Kim W.J., Kim H.H., Kim D.S., Kim W., Yang T.J., Kim H.S. Characterization of the long terminal repeat of the endogenous retrovirus-derived microRNAs in the olive flounder. Sci. Rep. 2019;9:1–10. doi: 10.1038/s41598-019-50492-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Moore M.J., Vasilieva N., Sui J., Wong S.K., Berne M.A., Somasundaran M., Sullivan J.L., Luzuriaga K., Greenough T.C. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang H.X., Li Y.H. MiR-873, as a suppressor in cervical cancer, inhibits cells proliferation, invasion and migration via negatively regulating ULBP2. Genes Genomics. 2020;42:371–382. doi: 10.1007/s13258-019-00905-8. [DOI] [PubMed] [Google Scholar]
- Linsley P.S., Schelter J., Burchard J., Kibukawa M., Martin M.M., Bartz S.R., Johnson J.M., Cummins J.M., Raymond C.K., Dai H. Transcripts targeted by the microRNA-16 family cooperatively regulate cell cycle progression. Mol. Cell. Biol. 2007;27:2240–2252. doi: 10.1128/MCB.02005-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu M., Wang T., Zhou Y., Zhao Y., Zhang Y., Li J. Potential role of ACE2 in coronavirus disease 2019 (COVID-19) prevention and management. J. Transl. Int. Med. 2020;8:9–19. doi: 10.2478/jtim-2020-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q., Fu H., Sun F., Zhang H., Tie Y., Zhu J., Xing R., Sun Z., Zheng X. miR-16 family induces cell cycle arrest by regulating multiple cell cycle genes. Nucleic Acids Res. 2008;36:5391–5404. doi: 10.1093/nar/gkn522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu R., Zhao X., Li J., Niu P., Yang B., Wu H., Wang W., Song H., Huang B., Zhu N., et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo H., Li Y., Liu B., Yang Y., Xu Z.Q.D. MicroRNA-15b-5p targets ERK1 to regulate proliferation and apoptosis in rat PC12 cells. Biomed. Pharmacother. 2017;92:1023–1029. doi: 10.1016/j.biopha.2017.05.140. [DOI] [PubMed] [Google Scholar]
- Malik Y.S., Sircar S., Bhat S., Sharun K., Dhama K., Dadar M., Tiwari R., Chaicumpa W. Emerging novel coronavirus (2019-nCoV)-current scenario, evolutionary perspective based on genome analysis and recent developments. Vet. Q. 2020;40:68–76. doi: 10.1080/01652176.2020.1727993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCue A.D., Nuthikattu S., Reeder S.H., Slotkin R.K. Gene expression and stress response mediated by the epigenetic regulation of a transposable element small RNA. PLoS Genet. 2012;8:e1002474. doi: 10.1371/journal.pgen.1002474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mousavizadeh L., Ghasemi S. Genotype and phenotype of COVID-19: their roles in pathogenesis. J. Microbiol. Immunol. Infect. 2020 doi: 10.1016/j.jmii.2020.03.022. https://doi.org/10.1016/j.jmii.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munster V.J., Koopmans M., van Doremalen N., van Riel D., de Wit E. A novel coronavirus emerging in China-key questions for impact assessment. N. Engl. J. Med. 2020;382:692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- Murakami Y., Yasuda T., Saigo K., Urashima T., Toyoda H., Okanoue T., Shimotohno K. Comprehensive analysis of microRNA expression patterns in hepatocellular carcinoma and non-tumorous tissues. Oncogene. 2006;25:2537–2545. doi: 10.1038/sj.onc.1209283. [DOI] [PubMed] [Google Scholar]
- Pedersen S.F., Ho Y.C. SARS-CoV-2: a storm is raging. J. Clin. Invest. 2020;130:2202–2205. doi: 10.1172/JCI137647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piedade D., Azevedo-Pereira J.M. The role of microRNAs in the pathogenesis of herpesvirus infection. Viruses. 2016;8:156. doi: 10.3390/v8060156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pineau P., Volinia S., McJunkin K., Marchio A., Battiston C., Terris B., Mazzaferro V., Lowe S.W., Croce C.M., Dejean A. miR-221 overexpression contributes to liver tumorigenesis. Proc. Natl. Acad. Sci. U. S. A. 2010;107:264–269. doi: 10.1073/pnas.0907904107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto Y., Buchumenski I., Levanon E.Y., Eisenberg E. Human cancer tissues exhibit reduced A-to-I editing of miRNAs coupled with elevated editing of their targets. Nucleic Acids Res. 2018;46:71–82. doi: 10.1093/nar/gkx1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piriyapongsa J., Mariño-Ramírez L., Jordan I.K. Origin and evolution of human microRNAs from transposable elements. Genetics. 2007;176:1323–1337. doi: 10.1534/genetics.107.072553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy K.B. MicroRNA (miRNA) in cancer. Cancer Cell Int. 2015;15:1–6. doi: 10.1186/s12935-015-0185-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts J.T., Cooper E.A., Favreau C.J., Howell J.S., Lane L.G., Mills J.E., Newman D.C., Perry T.J., Russell M.E., Wallace B.M., et al. Continuing analysis of microRNA origins: formation from transposable element insertions and noncoding RNA mutations. Mob. Genet. Elements. 2013;3:e27755. doi: 10.4161/mge.27755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheel T.K., Luna J.M., Liniger M., Nishiuchi E., Rozen-Gagnon K., Shlomai A., Auray G., Gerber M., Fak J., Keller I., et al. A broad RNA virus survey reveals both miRNA dependence and functional sequestration. Cell Host Microbe. 2016;19:409–423. doi: 10.1016/j.chom.2016.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A.K., Rooge S.B., Varshney A., Vasudevan M., Bhardwaj A., Venugopal S.K., Trehanpati N., Kumar M., Geffers R., Kumar V., et al. Global microRNA expression profiling in the liver biopsies of hepatitis B virus-infected patients suggests specific microRNA signatures for viral persistence and hepatocellular injury. Hepatology. 2018;67:1695–1709. doi: 10.1002/hep.29690. [DOI] [PubMed] [Google Scholar]
- Slotkin R.K., Martienssen R. Transposable elements and the epigenetic regulation of the genome. Nat. Rev. Genet. 2007;8:272–285. doi: 10.1038/nrg2072. [DOI] [PubMed] [Google Scholar]
- Smalheiser N.R., Torvik V.I. Mammalian microRNAs derived from genomic repeats. Trends Genet. 2005;21:322–326. doi: 10.1016/j.tig.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Small E.M., Frost R.J., Olson E.N. MicroRNAs add a new dimension to cardiovascular disease. Circulation. 2010;121:1022–1032. doi: 10.1161/CIRCULATIONAHA.109.889048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song L., Liu H., Gao S., Jiang W., Huang W. Cellular microRNAs inhibit replication of the H1N1 influenza A virus in infected cells. J. Virol. 2010;84:8849–8860. doi: 10.1128/JVI.00456-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trobaugh D.W., Klimstra W.B. MicroRNA regulation of RNA virus replication and pathogenesis. Trends Mol. Med. 2017;23:80–93. doi: 10.1016/j.molmed.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ul Qamar M.T., Alqahtani S.M., Alamri M.A., Chen L.L. Structural basis of SARS-CoV-2 3CLpro and anti-COVID-19 drug discovery from medicinal plants. J. Pharm. Anal. 2020;10:313–319. doi: 10.1016/j.jpha.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan Y., Shang J., Graham R., Baric R.S., Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J. Virol. 2020;94:e00127–20. doi: 10.1128/JVI.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Yang P., Liu K., Guo F., Zhang Y., Zhang G., Jiang C. SARS coronavirus entry into host cells through a novel clathrin-and caveolae-independent endocytic pathway. Cell Res. 2008;18:290–301. doi: 10.1038/cr.2008.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Qin Y., Tong L., Wu S., Wang Q., Jiao Q., Guo Z., Lin L., Wang R., Zhao W., et al. MiR-342-5p suppresses coxsackievirus B3 biosynthesis by targeting the 2C-coding region. Antiviral Res. 2012;93:270–279. doi: 10.1016/j.antiviral.2011.12.004. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Coronavirus disease (COVID-19) Situation Report - 80. 2020a. [accessed April 9, 2020]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200409-sitrep-80-covid-19.pdf?sfvrsn=1b685d64_6 .
- World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) 2020b. [accessed March 9, 2020]. Available from: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
- Wortzel I., Seger R. The ERK cascade: distinct functions within various subcellular organelles. Genes Cancer. 2011;2:195–209. doi: 10.1177/1947601911407328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu A., Peng Y., Huang B., Ding X., Wang X., Niu P., Meng J., Zhu Z., Zhang Z., Wang J., et al. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe. 2020a;27:325–328. doi: 10.1016/j.chom.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020b;395:689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X., Yu C., Qu J., Zhang L., Jiang S., Huang D., Chen B., Zhang Z., Guan W., Ling Z.J., et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur. J. Nucl. Med. Mol. Imaging. 2020;47:1275–1280. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanamadala S., Ljungman M. Potential role of MLH1 in the induction of p53 and apoptosis by blocking transcription on damaged DNA templates1 1 NIH grant CA82376, a grant from the Gastrointestinal Oncology Program Fund of the University of Michigan Comprehensive Cancer Center, and a grant from the Biomedical Research Council at the University of Michigan Medical School. Mol. Cancer Res. 2003;1:747–754. [PubMed] [Google Scholar]
- Yang X., Yu Y., Xu J., Shu H., Liu H., Wu Y., Zhang L., Yu Z., Fang M., Yu T., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki A.M., Van Boheemen S., Bestebroer T.M., Osterhaus A.D., Fouchier R.A. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N. Engl. J. Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- Zeng P., Wagoner H.A., Pescovitz O.H., Steinmetz R. RNA interference (RNAi) for extracellular signal-regulated kinase 1 (ERK1) alone is sufficient to suppress cell viability in ovarian cancer cells. Cancer Biol. Ther. 2005;4:961–967. doi: 10.4161/cbt.4.9.1912. [DOI] [PubMed] [Google Scholar]
- Zhang B., Pan X., Cobb G.P., Anderson T.A. microRNAs as oncogenes and tumor suppressors. Dev. Biol. 2007;302:1–12. doi: 10.1016/j.ydbio.2006.08.028. [DOI] [PubMed] [Google Scholar]
- Zhang H., Richards B., Wilson T., Lloyd M., Cranston A., Thorburn A., Fishel R., Meuth M. Apoptosis induced by overexpression of hMSH2 or hMLH1. Cancer Res. 1999;59:3021–3027. [PubMed] [Google Scholar]
- Zhao W. Negative regulation of TBK1-mediated antiviral immunity. FEBS Lett. 2013;587:542–548. doi: 10.1016/j.febslet.2013.01.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y.Y., Ma Y.T., Zhang J.Y., Xie X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020;17:259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Z.R., He Q., Wu W.B., Chang G.Q., Yao C., Zhao Y., Wang M., Wang S.M. MiR-140-3p is involved in in-stent restenosis by targeting C-Myb and BCL-2 in peripheral artery disease. J. Atheroscler. Thromb. 2018;25:1168–1181. doi: 10.5551/jat.44024. [DOI] [PMC free article] [PubMed] [Google Scholar]