Dear Editor,
We read with great interest the manuscript entitled “Hyaluronidase: An overview of its properties, applications, and side effects” [1]. We would like to express our respect for the author for this well-organized review article. However, there are a few points that we would like to discuss.
In the section “Action of hyaluronidase,” the author stated that “Hyaluronidase is an endoglycosidase that breaks down hyaluronic acid into monosaccharides” [1]. As described in the article, hyaluronidase breaks β-1,4 glycosidic bonds or β-1,3 glycosidic bonds in a hyaluronic acid chain. However, a hyaluronic acid chain is composed of multiple disaccharide chains and, when hyaluronidase cleaves the β-1,4 or β-1,3 glycosidic bonds of hyaluronic acid, the chain breaks down to form disaccharides, not monosaccharides.
The author stated that “microbial hyaluronidase obtained from Streptococcus agalactiae bacteria was also used to reduce side effects” [1]. As far as we know, many hyaluronidase products are still made from animal testicular preparations. For example, Vitrase (ISTA Pharmaceuticals, Inc., Irvine, CA, USA) is formulated as a solution containing ovine hyaluronidase, Hylenex (Halozyme Therapeutics, Inc., San Diego, CA, USA) is human recombinant hyaluronidase formed by genetically engineered Chinese hamster ovary cells containing a DNA plasmid encoding the enzyme, Liporase (Daehan New Pharm Co., Seoul, Korea) is made from a bovine testicular preparation, and Hirax (BMI Korea, Uiwamg, Korea) is also made from a bovine testicular preparation.
The author stated that “The reasons for the short half-life of hyaluronidase in human plasma are the presence of numerous hyaluronidase inhibitors in the plasma” [1]. However, this has not been proven by any scientific study. A previous study observed that hyaluronidase was deactivated immediately when injected intravenously and it was hypothesized that the process is antibody-mediated; however, the true mechanism of deactivation is unknown [2]. Another article used the term “anti-HYAL enzyme,” but the existence of such an enzyme has also not been scientifically proven [3]. Further evaluation is needed on the mechanism of hyaluronidase inactivation after intravenous injection.
The author stated that “Monophasic fillers are less soluble in hyaluronidase because they are less exposed to hyaluronidase than polyphasic fillers” [1], quoting a previous article [4]. However, in the original article, the researchers wrote that “It is hypothesized that this observation is because of the fact that enzymatic degradation is likely to be orders of magnitude faster in polyphasic compounds because the exposed surface area of cross-linked HA is orders of magnitude greater in polyphasic compounds” [4]. As stated in the original article, this is just a hypothesis, and we believe that the solubility difference between monophasic and polyphasic fillers is because of their cross-linking—a so-called “modification of degree.”
We thank the author for citing our previous article, which dealt with various interventions using perivascular hyaluronidase [5]. However, an important aspect is missing in this article [1]: the different types of hyaluronidase products. As shown in Fig. 1, Vitrase is made of 200 USP, Hylenex 150 USP, and Liporase 1,500 IU. Thus, the products use different units and have different potencies. Additionally, there are thousands of filler products with different hyaluronic acid concentrations, particle sizes, and cross-linking ratios and there are different guidelines for the amount of hyaluronidase to be used. In our previous paper, we recommended the injection of at least 100 IU of hyaluronidase at each site [5]. However, our injection guideline was based on the use of 1,500 IU hyaluronidase. For doctors practicing in Western countries, this dose might be too high, as they usually use 150 or 200 USP formulations.
Fig. 1.
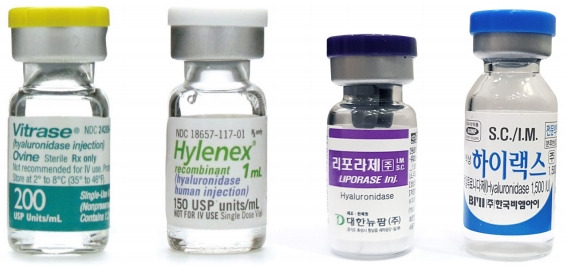
Various types of hyaluronidase.
Once more, we thank the author for the considerable effort invested into this review of the uses of hyaluronidase [1]. More studies are needed to support the use of hyaluronidase.
Footnotes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Jung H. Hyaluronidase: an overview of its properties, applications, and side effects. Arch Plast Surg. 2020;47:297–300. doi: 10.5999/aps.2020.00752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bailey SH, Fagien S, Rohrich RJ. Changing role of hyaluronidase in plastic surgery. Plast Reconstr Surg. 2014;133:127e–132e. doi: 10.1097/PRS.0b013e3182a4c282. [DOI] [PubMed] [Google Scholar]
- 3.DeLorenzi C. New high dose pulsed hyaluronidase protocol for hyaluronic acid filler vascular adverse events. Aesthet Surg J. 2017;37:814–25. doi: 10.1093/asj/sjw251. [DOI] [PubMed] [Google Scholar]
- 4.DeLorenzi C. Transarterial degradation of hyaluronic acid filler by hyaluronidase. Dermatol Surg. 2014;40:832–41. doi: 10.1097/DSS.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 5.Lee W, Oh W, Oh SM, et al. Comparative effectiveness of different interventions of perivascular hyaluronidase. Plast Reconstr Surg. 2020;145:957–64. doi: 10.1097/PRS.0000000000006639. [DOI] [PubMed] [Google Scholar]


