Abstract
Background
Most services for individuals at Clinical High Risk for Psychosis (CHR-P) provide short-term clinical care. This study determines the real-world and long-term clinical outcomes beyond transition to psychosis in a large cohort of CHR-P individuals.
Method
Retrospective RECORD-compliant real-world Electronic Health Records (EHR) cohort study in secondary mental health care (the South London and the Maudsley -SLaM- NHS Foundation Trust). All CHR-P patients accessing the CHR-P service at SLaM in the period 2001–2018 were included. Main outcomes were long-term cumulative risk of first: (i) developing an ICD-10 psychotic disorder (primary outcome), receiving a treatment with (iia) antipsychotic medication, (iib) benzodiazepines, (iic) other psychotropic medications, (iid) psychotherapy, receiving an (iiia) informal or (iiib) compulsory admission into a mental health hospital, and the time to these events; (iiic) number of days spent in hospital and (iv) cumulative risk of death for any reason and age/gender Standardised Mortality Ratio (SMR). Data were extracted from the EHR and analysed with Kaplan Meier failure functions, Cox and zero-inflated negative binomial regressions.
Findings
600 CHR-P patients (80.43% Attenuated Psychotic Symptoms, APS; 18.06%, Brief and Limited Intermittent Psychotic Symptoms, BLIPS, 1.51% Genetic Risk and Deterioration Syndrome) were included (mean age 22.63 years, range 13–36; 55.33% males; 46.44% white, mean duration of untreated attenuated psychotic symptoms 676.32 days, 1105.40 SD). The cumulative risk to first psychosis was 0.365 (95%CI 0.302–0.437) at 11 years; first antipsychotic 0.777 (95%CI 0.702–0.844) at 9 years; first benzodiazepine 0.259 (95%CI 0.183–0.359) at 12 years; first other types of medications 0.630 (95%CI 0.538–0.772) at 9 years; first psychotherapy 0.814 (95%CI 0.764–0.859) at 9 years; first informal admission 0.378 (95%CI 0.249–0.546) at 12 years; first compulsory admission 0.251 (95%CI 0.175–0.352) at 12 years; those admitted spent on average 94.84 (SD=169.94) days in hospital; the cumulative risk of death for any reason was 0.036 (95%CI 0.012–0.103) at 9 years, with an SMR of 3.9 (95%CI 1.20–6.6). Compared to APS, BLIPS had a higher risk of developing psychosis, being admitted compulsorily into hospital, receiving antipsychotics and benzodiazepines and lower probability of receiving psychotherapy. Other prognostic factors of long-term outcomes included age, symptoms severity, duration of untreated attenuated psychotic symptoms, ethnicity and employment status.
Interpretation
Duration of care provided by CHR-P services should be expanded to address long-term real-world outcomes.
Funding
This study was supported by the King's College London Confidence in Concept award from the Medical Research Council (MRC) (MC_PC_16048) to PF-P. GSP is supported by the Alicia Koplowitz Foundation. HB is supported by a National Institute for Health Research Maudsley Biomedical Research Centre studentship.
Keywords: Psychosis, Prevention, Schizophrenia, Clinical high risk, Long-term outcome, Real-world, Electronic health record
Research in context.
Evidence before this study
Preventive interventions implemented in specialised mental health services for young individuals at clinical high risk for psychosis improve outcomes of the most severe psychiatric disorder. To address the real-world long-term outcomes of this population we conducted a systematic Web of Knowledge literature search from inception to 1 January 2020. We only found a few long-term studies limiting their focus on transition to psychosis, transition and clinical/functional remission or symptomatic persistence, neurocognition, employment or brain structure, while other relevant real-world clinical outcomes such as utilisation of mental health resources have not been investigated in the long-term.
Added value of this study
Overall, broader long-term real-world clinical outcomes in this patient population are not fully characterised. In this clinical register-based Electronic Health Record real-world cohort study, 600 individuals accessing the Outreach and Support in South-London specialised service for individuals at clinical high risk for psychosis, showed a substantial long-term risk of developing the disorder, being treated with medications, admitted to mental health hospitals and spending several days in hospitals. Some of them may be at risk of premature death in the long-term.
Implications of all the available evidence
This study demonstrates that the current short-term duration of care offered by specialised mental health services is unlikely to capture most real-world clinical outcomes presented by individuals at clinical high risk of psychosis. The available evidence indicates that specialised services for individuals at clinical high risk for psychosis should extend the duration of the care offered to capture the real-world, long-term outcomes of this vulnerable group. These findings should inform clinical guidelines and health service research in the field of preventive psychiatry.
Alt-text: Unlabelled box
Introduction
Young individuals at Clinical High-Risk for Psychosis (CHR-P) [1,2] accumulate risk factors for the disorder [3], [4], [5], attenuated psychotic symptoms [6] and functional impairments [7], and seek help [8] at specialised CHR-P clinical services [9], [10], [11]. The preventive care (termed primary indicated prevention) implemented in these CHR-P services has the potential to maximise the benefits of early interventions for psychosis [12]. The accomplishments and challenges of the CHR-P paradigm, two decades since being first conceived [13,14], have been recently appraised in this journal [15,16] by the European College of Neuropsychopharmacology Network for the Prevention of Mental Disorders and Mental Health Promotion [17]. The study found that a core limitation of knowledge is that, to date, research has mostly focused on prediction of transition to psychosis in the short term [15]. The broad clinical and long-term fate of CHR-P individuals beyond transition to psychosis is relatively undetermined because tracking these real-world outcomes is logistically challenging. A few studies followed up CHR-P individuals for more than 10 years but limited their focus on transition to psychosis (baseline sample: n = 416 [18]), transition and clinical/functional remission or symptomatic persistence (n = 702 [19], 363 [20], 255 [21], 246 [22]), neurocognition (n = 325 [23], 80 [24]), employment (n = 268 [25]) or brain structure (n = 109 [26]). Other relevant real-world clinical outcomes such as utilisation of mental health resources (formal and informal admission to mental health units, numbers of days spent in hospital, exposure to treatments) have been investigated only in the short term (n = 432 [27]). Because of the limited knowledge of long-term outcomes, preventive interventions have similarly targeted the short-term period [28]. Accordingly, most CHR-P services worldwide limit the duration of care to the short-term (median 2 years [11]) period since the initial presentation. Another limitation of knowledge is that factors predicting long term outcomes are not completely clear. In the short -term, CHR-P subgroups (Attenuated Psychosis Symptoms, APS; Brief and Limited Intermittent Psychotic Symptoms, BLIPS; Genetic Risk and Deterioration syndrome, GRD) have been demonstrated to be associated with differential risk to psychosis [29, 30]. Other short-term prognostic factors include sociodemographic and clinical features that characterise the CHR-P state [3], [4], [5].
This study fills in this gap of knowledge describing as primary aim the long-term and broad real-world clinical outcomes in a large sample of CHR-P individuals. As secondary step we explored potential prognostic factors predicting long term outcomes in this population.
Methods
Design
Clinical real-world, long-term prospective cohort study using Electronic Health Records (EHRs).
Data source
Real-world EHR data on routine mental healthcare [31] from all patients managed by the South London and Maudsley (SLaM) National Health Service Foundation Trust, UK (eMethods 1).
Study population
OASIS [10] is an early detection service which was set up in 2001, and it is one of the oldest CHR-P services in the UK [10]. The level of risk enrichment observed at OASIS (pretest risk [32]: 14.6% at more than 3 years [33]) aligns with that observed in CHR-P services worldwide (meta-analytical pretest risk 15% at more than 3 years [34]), indicating that OASIS population is representative of the general CHR-P samples. OASIS focuses on the identification, prognostic assessment and treatment of help-seeking CHR-P individuals aged 14–35 years, serving the SLaM catchment area. The OASIS team offers focused interventions spanning pharmacological, psychological [35] (i.e. cognitive behavioural therapy, the only recommended first-line preventive treatment for CHR-P individuals [35]) and psychoeducational activities for a period of two years [36]. Clinical follow-up is usually performed as part of the standard care. OASIS is integrated into the Pan-London Network for Psychosis-prevention (PNP) [9].
The study population included a convenience sample of all individuals accessing OASIS in the period January 2001 to June 2018, assessed with the CHR-P instrument and meeting Comprehensive Assessment of At Risk Mental State (CAARMS) [37] criteria: BLIPS, APS, GRD. All OASIS staff undergo extensive psychometric training as part of numerous research studies (EUGEI, PSYSCAN, HARMONY) to ensure high reliability in the designation of at-risk cases.
Study measures
Variables
Baseline descriptive variables included sociodemographic (age, sex, ethnicity, marital status, employment status, accommodation status, SLaM borough) and clinical characteristics (severity of CHR-P symptoms, type of CHR-P subgroup, Duration of Untreated Attenuated Psychotic Symptoms [DUAPS]; Social and Occupational Functioning Assessment Scale [SOFAS] [38]; Health Of the Nation Outcome Scale [HoNOS] [39], for details see eMethods 2).
Follow-up
Follow-up started at the time of acceptance to OASIS and ended when an outcome was recorded, or when the patient dropped out of the EHR (as documented by the last entry on the EHR).
Outcomes
The real-world outcomes of the current study were the long-term cumulative risk of first: (i) developing an ICD-10 psychotic disorder (primary outcome), receiving a treatment with (iia) antipsychotic medication (complemented by type of molecule and chlorpromazine equivalent), (iib) benzodiazepines (complemented by type of molecule), (iic) other psychotropic medications (i.e. excluding antipsychotics and benzodiazepines, type of molecules were described), (iid) psychotherapy (complemented by the number of psychotherapy sessions), receiving an (iiia) informal or (iiib) compulsory admission to a mental health hospital (involving a Mental Health Act [MHA] assessment), and the time to these events. Additional outcomes included (iiic) number of days spent in mental health hospital and (iv) risk of death for any reason, with age/gender Standardised Mortality Ratio (SMR).
Statistical analysis
This clinical register-based cohort study was conducted according to the REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement [40] (see eTable 1). Sociodemographic and clinical characteristics of the sample (including missing data), were described with mean and SD for continuous variables, and absolute and relative frequencies for categorical variables. The cumulative probability of developing a (i) first episode of psychosis (primary outcome), (iia-d) receiving a first treatment or a (iiia-b) first informal or compulsory admission to a mental health hospital and (iv) risk of death were described through Kaplan Meier [41] failure functions (1-survival) [41] and Greenwood 95% CIs [42]. For each outcome, we reported the numbers of those at risk and truncate the failure function when less than 10 patients were still at risk (50 for risk of death). Therefore, the follow-up time reported in the Kaplan Meier failure functions varied across each outcome. Counts and relative frequencies were used to describe the type of molecules; mean and SD and percentiles were used to describe the chlorpromazine equivalents and the number of psychotherapy sessions. Counts were reported to describe the (iiic) number of days spent in hospital. The SMR was defined as the ratio between the number of deaths observed in the OASIS cohort at the end of follow-up and the annualised number of deaths expected in a similar size general population. The expected deaths were estimated using the Office for National Statistics [43] death rates in the OASIS catchment area, stratified for individuals aged 15–34 (the 15–35 stratum was not available) and weighted by OASIS gender. We then conducted two types of sensitivity complete-case analyses (missing variables were not imputed). First, we described the association between CHR-P subgroups (BLIPS, APS, GRD) and the outcomes (i-iv). As an additional exploratory outcome, we analysed the number of psychotherapy sessions. Second, we described the multivariable association between putative prognostic factors (age, CAARMS severity, DUAPS, gender, ethnicity, employment status) selected a priori on the basis of clinical knowledge and outcomes i-iv. For each sensitivity analysis, the association between predictors and the time-dependent outcomes (i, iia-d and iiia-b) was explored using Cox regression models, after checking for proportional hazards assumptions [44]. Since the numbers of days spent in hospitals were characterised by an excess of zero values and overdispersion, they were analysed with zero-inflated negative binomial regression analyses [45]. Because of small counts, sensitivity analyses were not performed for outcome iv. The association with the number of psychotherapy sessions was explored with Poisson regression.
Table 1.
Clinical and sociodemographic characteristics of the CHR-P sample.
| N | Mean | SD | ||
|---|---|---|---|---|
| Age (years) | 598 | 22.63 | 4.94(a) | |
| CAARMS severity(b) | 470 | 34.35 | 15.83 | |
| DUAPS (days) | 522 | 676.32 | 1105.40 | |
| Baseline SOFAS | 527 | 54.09 | 13.02 | |
| HONOS (adjusted total) | 379 | 11.68 | 6.95 | |
| Median | IQR | |||
| N | Count | % | ||
| Type of CHR-P subgroup | 598 | |||
| APS | 481 | 80.43 | ||
| BLIPS | 108 | 18.06 | ||
| GRD | 9 | 1.51 | ||
| Gender | 600 | |||
| Females | 268 | 44.67 | ||
| Males | 332 | 55.33 | ||
| Borough | 567 | |||
| Lambeth | 250 | 44.09 | ||
| Southwark | 178 | 31.39 | ||
| Lewisham | 75 | 13.23 | ||
| Croydon | 56 | 9.88 | ||
| Homeless | 8 | 1.41 | ||
| Ethnicity | 590 | |||
| White | 274 | 46.44 | ||
| Asian | 42 | 7.12 | ||
| Black | 191 | 32.37 | ||
| Other | 83 | 14.07 | ||
| Marital status | 583 | |||
| Married | 24 | 4.12 | ||
| Separated or divorced | 13 | 2.23 | ||
| Single | 464 | 79.59 | ||
| In a relationship | 82 | 14.07 | ||
| Employment status | 589 | |||
| Employed | 151 | 25.64 | ||
| Student | 207 | 35.14 | ||
| Unemployed | 231 | 39.22 | ||
| Accommodation status | 561 | |||
| Living with own family | 278 | 49.55 | ||
| Owner | 7 | 1.25 | ||
| Rental | 146 | 26.02 | ||
| Council flat or hostel | 98 | 17.47 | ||
| Homeless | 17 | 3.03 | ||
| Other | 15 | 2.67 |
range 13–36 (although the OASIS age range is typically 14–35 there are a few exceptions).
sum of CAARMS severity by frequency across each P1-P4 CAARMS domains; CAARMS: Comprehensive Assessment of At Risk Mental State; SOFAS: Social and Occupational Functioning Assessment Scale; DUAPS: Duration of Untreated Attenuated Psychotic Symptoms; HONOS: Health Of the Nation Outcome Scale; APS: Attenuated Psychotic Symptoms; BLIPS: Brief and Limited Intermittent Psychotic Symptoms; GRD: Genetic Risk and Deterioration syndrome.
For all analyses, statistical tests were two-sided and statistical significance was defined as p<0.05. All analyses were conducted in STATA 14 (STATA Corp., TX, USA).
Role of funding
The founders had no influence on the analysis of the data, interpretation of the results and drafting of the current manuscript.
Ethics
Approval for the study was granted by the Oxfordshire Research Ethics Committee C.
Results
Baseline characteristics of the sample
As shown in Table 1, 600 CHR-P individuals (55.33% males) attended the OASIS service from its set up until June 2018 across all SLaM boroughs (mostly Lambeth, [44.09%] and Southwark [31.39%]). At presentation, their mean age was 22.63 years (range 13–36); 79.59% of them were single, 39.22% unemployed and about one-third (35.14%) were students. Half of CHR-P individuals lived with their own family (49.55%); 17.47% lived in supported accommodations (council flats or hostels) and 3.03% were homeless. The proportion of white (46.44%) and non-white (black 32.37%, Asian 7.12%, other 14.07%) ethnicities was similar. The baseline severity of the total CAARMS symptoms was 34.35; baseline functional level was rather low (SOFAS=54.09) and reflected by an average HONOS score of 11.68. The onset of attenuated psychotic symptoms occurred on average about 1.85 years ahead of the CHR-P designation (DUAPS=676.32 days). DUAPS was 202.42 days in the GRD (SD 125.27), 302.03 days in the BLIPS (SD=896.06) and 773.88 days in the APS (SD=1139.69) subgroups. At OASIS, 80.43% CHR-P individuals met APS criteria, followed by a substantial proportion of BLIPS (18.06%), while GRD cases were rarer (1.51%).
Real-world, long-term clinical outcomes in CHR-P patients
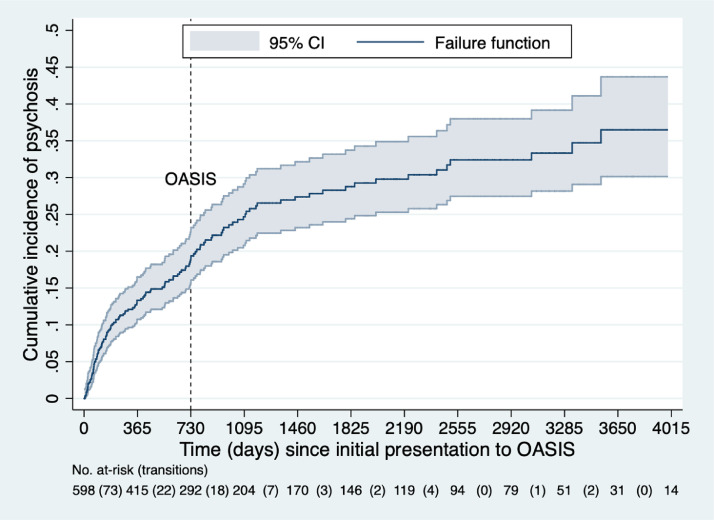
Cumulative risk of developing a first ICD-10 psychotic disorder
The cumulative risk to psychosis was 0.133 (95%CI 0.107–0.165) at 1 year, 0.191 (95%CI 0.158–0.229) at 2 years, 0.247 (95%CI 0.208–0.291) at 3 years, 0.273 (95%CI 0.231–0.321) at 4 years, 0.288 (95%CI 0.244–0.337) at 5 years, 0.298 (95%CI 0.252–0.349) at 6 years,0.324 (95%CI 0.275–0.379) at 7 and 8 years, 0.333 (95%CI 0.282–0.392) at 9 years, 0.365 (95%CI 0.302–0.437) at 10 and 11 years (Fig. 1).
Fig. 1.
Real-world cumulative risk of transition to psychosis in CHR-P individuals in the long-term. The dotted line indicates the median duration of care provided by CHR-P services (such as OASIS) worldwide [11].
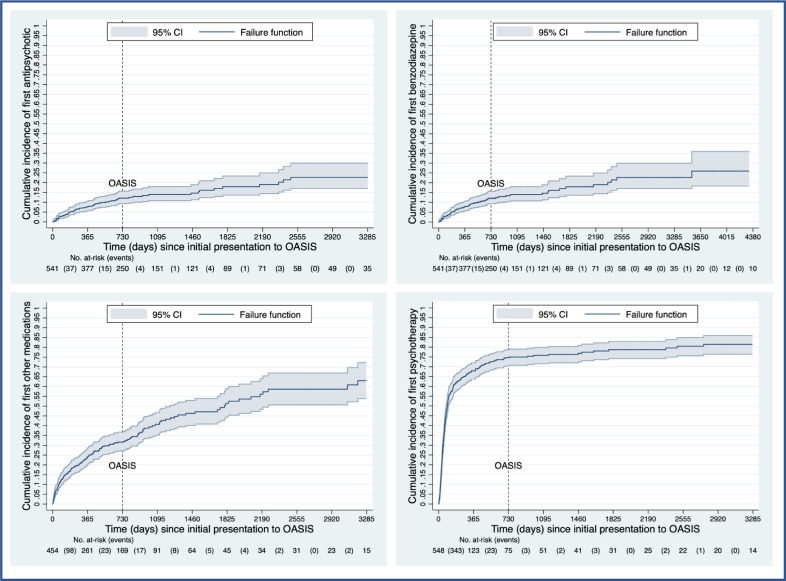
Cumulative probability of receiving a first psychotropic or psychotherapeutic treatment
The cumulative risk to first receiving antipsychotic medication was 0.427 (95%CI 0.378–0.478) at 1 year, 0.530 (95%CI 0.477–0.585) at 2 years, 0.622 (95%CI 0.561–0.683) at 3 years, 0.672 (95%0.607–0.736) at 4 years, 0.729 (95%CI 0.657–0.796) at 5 years, 0.740 (95%CI 0.668–0.808) at 6 years, 0.777 (95%CI 0.702–0.844) at 8 and 9 years (Fig. 2). Most of those treated with antipsychotics received quetiapine (38.25%) followed by olanzapine (18.43%), risperidone (18.89%), aripiprazole (14.75%), amisulpride (3.69%) and promethazine (5.99%) (eTable 2). The mean chlorpromazine equivalent was 156.94 mg (SD 148,92, 25%−75% percentiles 25mg-675 mg).
Fig. 2.
Cumulative long-term risk of receiving the first psychopharmacological treatment with antipsychotics, benzodiazepines or other medications and the first psychotherapeutic treatment in CHR-P individuals. The dotted line indicates the median duration of care provided by CHR-P services (such as OASIS) worldwide [11].
The cumulative risk to first receiving benzodiazepines was 0.077 (95%CI 0.056–0.105) at 1 year, 0.121 (95%CI 0.093–0.156) at 2 years, 0.139 (95%CI 0.108–0.180) at 3 years, 0.147 (95%CI 0.113–0.189) at 4 years, 0.161 (95%CI 0.124–0.209) at 5 years, 0.191 (95%CI 0.114–0.249) at 6 years, 0.227 (95%CI 0.171–0.299) at 7–9 years, 0.259 (95%CI 0.183–0.359) at 10–12 years (Fig. 2). The most frequently prescribed benzodiazepines are reported in eTable 3.
The cumulative risk to first receiving other medications was 0.242 (95%CI 0.203–0.288) at 1 year, 0.316 (95%CI 0.271–0.367) at 2 years, 0.407 (95%CI 0.351–0.467) at 3 years, 0.463 (95%CI 0.401–0.529) at 4 years, 0.514 (95%CI 0.440–0.588) at 5 years, 0.560 (95%CI 0.484–0.640) at 6 years, 0.587 (95%CI 0.506–0.669) at 7 and 8 years, 0.630 (95%CI 0.538–0.772) at 9 years (Fig. 2). The most frequently prescribed other medications are reported in eTable 4.
The cumulative risk of receiving a first psychotherapeutic treatment was of 0.670 (95%CI 0.637–0.720) at 1 year, 0.746 (0.704–0.787) at 2 years, 0.758 (95%CI 0.715–0.793) at 3 years, 0.763 (95%CI 0.719–0.803) at 4 years, 0.787 (95%CI 0.742–0.829) at 5 years, 0.786 (95%CI 0.742–0.829) at 6 years, 0.805 (95%CI 0.756–0.849) at 7 years, 0.814 (95%CI 0.764–0.859) at 8 and 9 years (Fig. 2). On average CHR-P individuals received 10.42 sessions of psychotherapy (SD 11.74); among those who received it, the mean number of sessions was 15.09 (SD 11.39).
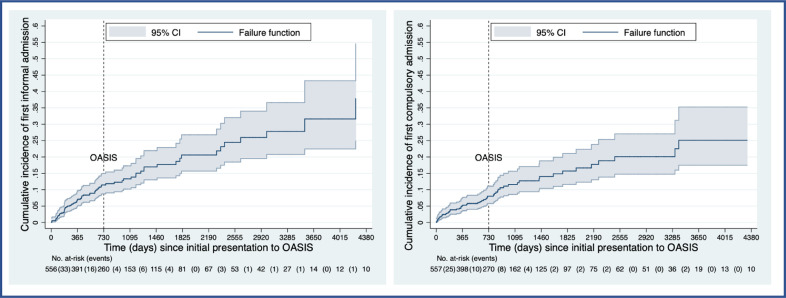
Cumulative probability of being admitted into a mental health hospital and days spent in hospital
The cumulative risk to the first informal admission to a mental health hospital was 0.068 (95%CI 0.049–0.095) at 1 year, 0.115 (95%CI 0.087–0.149) at 2 years, 0.133 (95%CI 0.102–0.173) at 3 years, 0.169 (0.130–0.219) at 4 years, 0.206 (95%CI 0.157–0.268) at 5 and 6 years, 0.245 (95%CI 0.185–0.320) at 7 years, 0.259 (95%CI 0.195–0.340) at 8 years, 0.278 (95%CI 0.208–0.366) at 9 years, 0.316 (95%CI 0.225–0.433) at 10 and 11 years, 0.378 (95%CI 0.249–0.546) at 12 years (Fig. 3).
Fig. 3.
. Cumulative long-term risk of receiving a first informal or compulsory admission to mental health hospitals in CHR-P individuals. The dotted line indicates the median duration of care provided by CHR-P services (such as OASIS) worldwide [11].
The cumulative risk to the first compulsory admission to mental health hospital was 0.050 (95%CI 0.034–0.074) at 1 year, 0.080 (95%CI 0.0578–0.111) at 2 years, 0.116 (95%CI 0.086–0.156) at 3 years, 0.141 (0.104–0.188) at 4 years, 0.157 (95%CI 0.116–0.211) at 5 years, 0.177 (95%CI 0.131–0.238) at 6 years, 0.201 (95%CI 0.148–0.271) at 7–9 years, 0.251 (95%CI 0.175–0.352) at 10–12 years (Fig. 3).
Among CHR-P individuals who were admitted to mental health hospital, the average number of days spent in mental health hospital was 94.84 (SD=169.94).
Cumulative risk of death for any reason
The cumulative risk of death for any reason (n = 8) was 0.004 (95%CI 0.001–0.025) at 3–4 years, 0.009 (95%CI 0.002–0.040) at 5–8 years, 0.036 (95%CI 0.012–0.103) at 9 years: 3 committed suicide, 2 died of other causes, and in 2 cases the cause of death was unknown. The SMR standardised for age/sex was 3.9 (95%CI 1.20–6.60).
Sensitivity analyses
Sensitivity analyses (eTable 5) showed that, compared to APS, BLIPS individuals had a higher risk of developing psychosis, being compulsorily admitted into mental health hospitals, receiving antipsychotics and benzodiazepines treatments, lower likelihood of receiving other medications, a comparable likelihood of receiving psychotherapy but fewer psychotherapy sessions, a comparable likelihood of informal admission and a comparable numbers of days spent in hospital.
Multivariable sensitivity analyses (eTable 6) showed that age, CAARMS severity and black ethnicities were associated with an increased risk of psychosis; age, CAARMS severity and unemployment with an increased risk of antipsychotic treatment; age and DUAPS with an increased and decreased risk of benzodiazepines treatment respectively; female gender female and black ethnicity with an increased and decreased risk of other medications respectively; CAARMS severity, DUAPS with an increased likelihood of receiving psychotherapy; CAARMS severity and DUAPS with an increased risk of informal admission; age, CAARMS severity, male gender, black ethnicities with an increased risk of formal admission; DUAPS and unemployment with a decreased and increased number of days spent in hospital respectively.
Discussion
To our best knowledge, this is the largest cohort study addressing the broadest real-world outcomes for CHR-P individuals beyond psychosis onset in the long-term. In 600 individuals accessing OASIS, there was a substantial long-term risk of developing psychosis, being treated with psychotropic medications, admitted formally or compulsorily into mental health hospitals and spending several days in hospitals. Some CHR-P individuals may be at risk of premature death in the long-term.
This study advances clinical knowledge on several lines. Firstly, it suggests that the real-world risk of psychosis in CHR-P individuals almost double from the short-term (0.191 at 2 years) to the long-term (0.365 at 10–11 years). CHR-P individuals have about a 50-fold increase in the probability of developing a psychotic disorder, compared to the local general population (South London, risk of psychosis: 0.72 at 10 years, estimated as in Fig. 3 in [46]). This finding contradicts the criticisms that the group of CHR-P patients only display a negligible risk of psychosis and that prevention of psychosis in this group should, therefore, be dismissed [47]. This result also suggests that the real-world risk of psychosis in CHR-P individuals may be higher than that observed in research studies or trials, which typically filter their participants through additional entry criteria or sampling biases. This finding is relevant to inform ongoing large-scale international consortia (e.g. PSYSCAN [48, 49], PRONIA [50], NAPLS [51], PNC [52], HARMONY) that are developing and validating risk prediction models in this group. Furthermore, the notion of declining transition risk in CHR-P samples over the most recent years may also represent -at least partially- an artefact of research recruitment [33] and insufficient duration of follow-up.
Secondly, this study demonstrates that CHR-P individuals display several poor mental health outcomes beyond transition to psychosis with about one-third of them (informal admission 0.378 at 12 years; formal admission 0.251 at 12 years) being admitted into mental health hospitals. This is also the first study to indicate that CHR-P individuals have a threefold risk (SMR=3.9) of death compared to age and sex matched individuals living in the local general population (cumulative risk of death for any cause 0.036 at 9 years). The magnitude of the SMR in the CHR-P state is comparable to that observed in young people from the same geographical area for severe mental disorders (4.47, 95%CI 3.49–5.64 [53]) such as established psychosis or affective disorders. Another proxy of poor mental health outcomes is indexed by the high exposure to psychotropic medications that do not typically represent the recommended first-line treatment for this group (antipsychotics: 0.777 at 9 years, benzodiazepines 0.259 at 10–12 years, other medications 0.630 at 9 years), although these findings should be interpreted with caution. For example, the average chlorpromazine equivalent is lower than the minimum effective dose (200mg [54]), and the most frequently used antipsychotic was quetiapine: this suggests that low-dosage antipsychotics may have been used to treat comorbid disorders as opposed to primarily treating emerging psychosis. This is substantiated by the relatively high proportion of those receiving benzodiazepines or antidepressants, which again may reflect the substantial prevalence of comorbid affective disorders in this group [55].
Interpretation of these outcomes in the context of a non-randomised naturalistic study is not straightforward. OASIS fully aligned with the current clinical recommendations, and by the end of their care, most CHR-P individuals (0.746 at 2 years) had been offered the recommended preventive cognitive behavioural therapy. The hypothesis that cognitive behavioural therapy is substantially effective to prevent psychosis conflicts with the substantial transition risk observed in this cohort. Furthermore, the number of sessions provided to individuals accepting cognitive behavioural therapy is close to the recommended standard for efficacy [56]. Alternatively, a possibility may be that cognitive behavioural therapy is only effective to delay the onset of the disorder and that its effect vanishes over the long-term. A further possibility is that the magnitude of the putative preventive effects of cognitive behavioural therapy is too small to be observed across the heterogeneous CHR-P group. The latter hypothesis is supported by recent evidence synthesis studies that indicated no robust evidence to favour cognitive behavioural therapy over other treatments for preventing psychosis in CHR-P individuals [28, [57], [58], [59]].
Thirdly, this study is also the first to stratify broad, long-term outcomes beyond transition to psychosis across CHR-P subgroups. Since in SLaM there is one of the highest rates of psychosis in the world [60] (and therefore a large proportion [18%] of BLIPS [61]), this study was also best placed on demonstrating that BLIPS individuals have a higher risk than APS of developing psychosis, being compulsorily admitted into mental health hospitals, being exposed to non-recommended treatments (antipsychotics and benzodiazepines) and receiving lower intensity of the recommended treatments (i.e. a lower number of psychotherapy sessions). Conversely, they had a lower likelihood of receiving antidepressants or mood stabilizers, presumably in the light of the lower prevalence of affective or personality comorbidities in this subgroup [62]. This implies that preventive treatments should be stratified across APS and BLIPS subgroups [1]. To date, only 3% of BLIPS individuals receive the appropriate “dose” of the recommended preventive treatment (cognitive behavioural therapy) [56], because it primarily targets attenuated psychotic symptoms and not their specific needs.
This study is also the first one to investigate the potential significance of several prognostic factors for long-term outcomes in this population. We found that age, baseline symptoms severity, duration of untreated attenuated psychotic symptoms, ethnicity and employment status are consistently associated with various long-term clinical outcomes in CHR-P individuals. Although subsequent independent studies are needed to replicate these findings, our results could be used to inform the building of new clinical prediction models to forecast various long-term clinical outcomes beyond the onset of psychosis.
The above findings converge towards the most important clinical implication of the current study: the short-term duration of care currently offered by CHR-P services [11] worldwide is unlikely to be sufficient to capture the complex and broad long-term outcomes of this group, and should, therefore, be extended. The likelihood of severe real-world outcomes almost doubles from the short-term to the long-term: psychosis risk from 0.191 at 2 years to 0.365 at 10–11 years; risk of informal hospital admission from 0.115 at 2 years to 0.316 at 10–11 years, risk of compulsory admission from 0.080 at 2 years to 0.251 at 10–12 years. This is paralleled by a similar increase in psychotropic treatments, which is a proxy of long-term mental health problems: risk of a first antipsychotic from 0.530 at 2 years to 0.777 at 8–9 years; risk of a first benzodiazepine from 0.121 at 2 years to 0.259 at 10–12 years, risk to first receiving other medications from 0.316 at 2 years to 0.630 at 9 years. This is further aggravated by the fact that the median duration of follow-up assessment offered to CHR-P individuals after being discharged from CHR-P services is only 12 months [11]. Monitoring for broad clinical outcomes in the long-term is extremely challenging. This study further advances knowledge by demonstrating that a possible way of overcoming these challenges may be to leverage EHRs, which are increasingly adopted across several primary and secondary health care systems. EHR not only represent real-word clinical information but can incorporate automatic detection or prognostic algorithms [63], [64], [65], [66], translating stratified and precision medicine approaches in this field. Overall, these results will inform future studies such as the proposed 26-site ProNET cohort study and global health policies relating to CHR-P service development as well as worldwide clinical guidelines.
The main limitation of this study is that it did not employ structured psychometric interviews to ascertain the onset of outcomes at follow-up including the diagnostic stability of psychotic onset [67]. Therefore, while the current EHR findings have high ecological validity (i.e. they represent real-world clinical practice), they have not been subjected to formal validation with research-based criteria. However, the aim of the present study was to assess real-world clinical outcomes rather than psychometric outcomes in this cohort. The use of structured diagnostic interviews in research settings can itself lead to the selection of white, more highly educated and “squeaky-clean” [68] patient subsamples [69], further exaggerating sampling biases that are already affecting this field [34]. Additionally, some of the current results should be interpreted cautiously because of the limited counts, in particular the SMR. Another limitation is that patients moving outside the SLaM catchment area may have not been followed up.
A final important limitation is that the current study simply described outcomes in the long-term without addressing the effectiveness of CHR-P clinics (or interventions), given the naturalistic design. Testing the effectiveness of CHR-P clinics would require randomised designs, which are ethically and logistically difficult to implement.
In conclusion, this study suggests that duration of care provided by CHR-P services should be expanded to better capture the long-term real-world outcomes displayed by this group.
Declaration of Competing Interest
Dr. Fusar-Poli reports grants and personal fees from Lundbeck, personal fees from Menarini, personal fees from Angelini, outside the submitted work. Dr. Salazar de Pablo reports grants from Fundación Alicia Koplowitz, outside the submitted work. The other authors have nothing to disclose.
Acknowledgments
Author contribution
PFP conceived and led the study. ADM, LS, HB, GSDP, PM gave substantial contributions to the acquisition and interpretation of data. PFP drafted the work and conducted the analyses. PM gave substantial contributions to the interpretation of the results.
ADM, LS, HB, GSDP, PM revised it critically for important intellectual content. All authors approved the final version to be published and agreed to be accountable for all the aspects of the work. PFP had full access to all the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
This study was supported by the King's College London Confidence in Concept award from the Medical Research Council (MRC) (MC_PC_16048) to PF-P. GSP is supported by the Alicia Koplowitz Foundation. HB is supported by a National Institute for Health Research Maudsley Biomedical Research Centre studentship. The founders had no influence on the analysis of the data, interpretation of the results and drafting of the current manuscript.
Data sharing statement
There is no ethical permission for data sharing.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2020.100578.
Appendix. Supplementary materials
References
- 1.Fusar-Poli P. The clinical high-risk state for psychosis (CHR-P), Version II. Schizophr Bull. 2017;43(1):44–47. doi: 10.1093/schbul/sbw158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fusar-Poli P., Cappucciati M., Rutigliano G. At risk or not at risk? A meta-analysis of the prognostic accuracy of psychometric interviews for psychosis prediction. World Psychiatry. 2015;14(3):322–332. doi: 10.1002/wps.20250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Radua J., Ramella-Cravaro V., Ioannidis J.P.A. What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry. 2018;17(1):49–66. doi: 10.1002/wps.20490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oliver D., Reilly T., Baccaredda Boy O. What causes the onset of psychosis in individuals at clinical high risk? A meta-analysis of risk and protective factors. Schizophr Bull. 2020;46(1):110–120. doi: 10.1093/schbul/sbz039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fusar-Poli P., Tantardini M., De Simone S. Deconstructing vulnerability for psychosis: meta-analysis of environmental risk factors for psychosis in subjects at ultra high-risk. Eur Psychiatry. 2017;40:65–75. doi: 10.1016/j.eurpsy.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Fusar-Poli P., Borgwardt S., Bechdolf A. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013;70(1):107–120. doi: 10.1001/jamapsychiatry.2013.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fusar-Poli P., Rocchetti M., Sardella A. Disorder, not just state of risk: meta-analysis of functioning and quality of life in people at high risk of psychosis. Br J Psychiatry. 2015;207(3):198–206. doi: 10.1192/bjp.bp.114.157115. [DOI] [PubMed] [Google Scholar]
- 8.Falkenberg I., Valmaggia L., Byrnes M. Why are help-seeking subjects at ultra-high risk for psychosis help-seeking. Psychiatry Res. 2015;228(3):808–815. doi: 10.1016/j.psychres.2015.05.018. [DOI] [PubMed] [Google Scholar]
- 9.Fusar-Poli P., Estrade A., Spencer T.J. Pan-London network for psychosis-prevention (PNP) Front Psychiatry. 2019;10:707. doi: 10.3389/fpsyt.2019.00707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fusar-Poli P., Byrne M., Badger S., Valmaggia L.R., McGuire P.K. Outreach and support in south London (OASIS), 2001-2011: ten years of early diagnosis and treatment for young individuals at high clinical risk for psychosis. Eur Psychiatry. 2013;28(5):315–326. doi: 10.1016/j.eurpsy.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 11.Kotlicka-Antczak M., Podgorski M., Oliver D., Maric N.P., Valmaggia L., Fusar-Poli P. Worldwide implementation of clinical services for the prevention of psychosis: the IEPA early intervention in mental health survey. Early Interv Psychiatry. 2020 doi: 10.1111/eip.12950. [DOI] [PubMed] [Google Scholar]
- 12.Fusar-Poli P., McGorry P.D., Kane J.M. Improving outcomes of first-episode psychosis: an overview. World Psychiatry. 2017;16(3):251–265. doi: 10.1002/wps.20446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yung A.R., Phillips L.J., McGorry P.D. Prediction of psychosis. A step towards indicated prevention of schizophrenia. Br J Psychiatry Suppl. 1998;172(33):14–20. [PubMed] [Google Scholar]
- 14.Yung A.R., McGorry P.D., McFarlane C.A., Jackson H.J., Patton G.C., Rakkar A. Monitoring and care of young people at incipient risk of psychosis. Schizophr Bull. 1996;22(2):283–303. doi: 10.1093/schbul/22.2.283. [DOI] [PubMed] [Google Scholar]
- 15.Fusar-Poli P., Salazar de Pablo G., Correll C. Prevention of psychosis: advances in detection, prognosis and intervention. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2019.4779. [DOI] [PubMed] [Google Scholar]
- 16.Salazar de Pablo G., Catalan A., Fusar-Poli P. Clinical validity of DSM-5 attenuated psychosis syndrome: advances in diagnosis, prognosis, and treatment. JAMA Psychiatry. 2010;77(3):311–320. doi: 10.1001/jamapsychiatry.2019.3561. [DOI] [PubMed] [Google Scholar]
- 17.Fusar-Poli P., Bauer M., Borgwardt S. European college of neuropsychopharmacology network on the prevention of mental disorders and mental health promotion (ECNP PMD-MHP) Eur Neuropsychopharmacol. 2019 doi: 10.1016/j.euroneuro.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 18.Nelson B., Yuen H.P., Wood S.J. Long-term follow-up of a group at ultra high risk ("prodromal") for psychosis: the PACE 400 study. JAMA Psychiatry. 2013;70(8):793–802. doi: 10.1001/jamapsychiatry.2013.1270. [DOI] [PubMed] [Google Scholar]
- 19.McHugh M.J., McGorry P.D., Yuen H.P. The Ultra-High-Risk for psychosis groups: evidence to maintain the status quo. Schizophr Res. 2018;195:543–548. doi: 10.1016/j.schres.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Yung A.R., Nelson B., McGorry P.D., Wood S.J., Lin A. Persistent negative symptoms in individuals at Ultra High Risk for psychosis. Schizophr Res. 2019;206:355–361. doi: 10.1016/j.schres.2018.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beck K., Studerus E., Andreou C. Clinical and functional ultra-long-term outcome of patients with a clinical high risk (CHR) for psychosis. Eur Psychiatry. 2019;62:30–37. doi: 10.1016/j.eurpsy.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Michel C., Ruhrmann S., Schimmelmann B.G., Klosterkotter J., Schultze-Lutter F. Course of clinical high-risk states for psychosis beyond conversion. Eur Arch Psychiatry Clin Neurosci. 2018;268(1):39–48. doi: 10.1007/s00406-016-0764-8. [DOI] [PubMed] [Google Scholar]
- 23.Lin A., Yung A.R., Nelson B. Neurocognitive predictors of transition to psychosis: medium- to long-term findings from a sample at ultra-high risk for psychosis. Psychol Med. 2013;43(11):2349–2360. doi: 10.1017/S0033291713000123. [DOI] [PubMed] [Google Scholar]
- 24.Allott K., Wood S.J., Yuen H.P. Longitudinal cognitive performance in individuals at ultrahigh risk for psychosis: a 10-year follow-up. Schizophr Bull. 2019;45(5):1101–1111. doi: 10.1093/schbul/sby143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cotter J., Lin A., Drake R.J. Long-term employment among people at ultra-high risk for psychosis. Schizophr Res. 2017;184:26–31. doi: 10.1016/j.schres.2016.11.033. [DOI] [PubMed] [Google Scholar]
- 26.Cropley V.L., Lin A., Nelson B. Baseline grey matter volume of non-transitioned "ultra high risk" for psychosis individuals with and without attenuated psychotic symptoms at long-term follow-up. Schizophr Res. 2016;173(3):152–158. doi: 10.1016/j.schres.2015.05.014. [DOI] [PubMed] [Google Scholar]
- 27.Yoviene Sykes L.A., Ferrara M., Addington J. Predictive validity of conversion from the clinical high risk syndrome to frank psychosis. Schizophr Res. 2019 doi: 10.1016/j.schres.2019.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Davies C., Cipriani A., Ioannidis J.P.A. Lack of evidence to favor specific preventive interventions in psychosis: a network meta-analysis. World Psychiatry. 2018;17(2):196–209. doi: 10.1002/wps.20526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fusar-Poli P., Cappucciati M., Borgwardt S. Heterogeneity of psychosis risk within individuals at clinical high risk a meta-analytical stratification. JAMA Psychiatry. 2016;73(2):113–120. doi: 10.1001/jamapsychiatry.2015.2324. [DOI] [PubMed] [Google Scholar]
- 30.Fusar-Poli P., Cappucciati M., Bonoldi I. Prognosis of brief psychotic episodes: a meta-analysis. JAMA Psychiatry. 2016;73(3):211–220. doi: 10.1001/jamapsychiatry.2015.2313. [DOI] [PubMed] [Google Scholar]
- 31.Perera G., Broadbent M., Callard F. Cohort profile of the South London and Maudsley NHS foundation trust biomedical research centre (SLaM BRC) case register: current status and recent enhancement of an electronic mental health record-derived data resource. BMJ Open. 2016;6(3) doi: 10.1136/bmjopen-2015-008721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fusar-Poli P., Schultze-Lutter F. Predicting the onset of psychosis in patients at clinical high risk: practical guide to probabilistic prognostic reasoning. Evid Based Ment Health. 2016;19(1):10–15. doi: 10.1136/eb-2015-102295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fusar-Poli P., Palombini E., Davies C. Why transition risk to psychosis is not declining at the OASIS ultra high risk service: the hidden role of stable pretest risk enrichment. Schizophr Res. 2017 doi: 10.1016/j.schres.2017.06.015. [DOI] [PubMed] [Google Scholar]
- 34.Fusar-Poli P., Schultze-Lutter F., Cappucciati M. The dark side of the moon: meta-analytical impact of recruitment strategies on risk enrichment in the clinical high risk state for psychosis. Schizophr Bull. 2016;42(3):732–743. doi: 10.1093/schbul/sbv162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.NICE. Psychosis and schizophrenia in adults: prevention and management. Feb 2014, 2014. https://www.nice.org.uk/guidance/cg178/chapter/1-Recommendations#preventing-psychosis-2(accessed April 8th 2016).
- 36.Fusar-Poli P., Frascarelli M., Valmaggia L. Antidepressant, antipsychotic and psychological interventions in subjects at high clinical risk for psychosis: OASIS 6-year naturalistic study. Psychol Med. 2015;45(6):1327–1339. doi: 10.1017/S003329171400244X. [DOI] [PubMed] [Google Scholar]
- 37.Yung A.R., YHP Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Aust N Z J Psychiatry. 2005;39(11–12):964–971. doi: 10.1080/j.1440-1614.2005.01714.x. [DOI] [PubMed] [Google Scholar]
- 38.Association A.P.Diagnostic and statistical manual of mental disorders. Text Revision, Fourth Edition. 2000.
- 39.Orrell M., Yard P., Handysides J., Schapira R. Validity and reliability of the health of the nation outcome scales in psychiatric patients in the community. Br J Psychiatry. 1999;174:409–412. doi: 10.1192/bjp.174.5.409. [DOI] [PubMed] [Google Scholar]
- 40.Benchimol E.I., Smeeth L., Guttmann A. The REporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. 2015;12(10) doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kaplan E., Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457–481. [Google Scholar]
- 42.Greenwood M.The natural duration of cancer. . London: His Majesty's Stationery Office, 1926.
- 43.Office for National Statistics . In: Deaths registered by area of usual residence. Government U., editor. 2019. UK. UKeditor. [Google Scholar]
- 44.Grambsch P., Therneau T. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–526. [Google Scholar]
- 45.Greene W.H.Accounting for excess zeros and sample selection in poisson and negative binomial regression models. NYU Working Paper No EC-94-10, 1994. https://ssrn.com/abstract=1293115 (accessed.
- 46.Fusar-Poli P., Rutigliano G., Stahl D. Deconstructing pretest risk enrichment to optimize prediction of psychosis in individuals at clinical high risk. JAMA Psychiatry. 2016;73(2):1260–1267. doi: 10.1001/jamapsychiatry.2016.2707. [DOI] [PubMed] [Google Scholar]
- 47.van Os J., Guloksuz S. A critique of the "ultra-high risk" and "transition" paradigm. World Psychiatry. 2017;16(2):200–206. doi: 10.1002/wps.20423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.PSYSCAN. Translating neuroimaging findings from research into clinical practice project website.
- 49.Tognin S., van Hell H.H., Merritt K. Towards precision medicine in psychosis: benefits and challenges of multimodal multicenter studies-PSYSCAN: translating neuroimaging findings from research into clinical practice. Schizophr Bull. 2020;46(2):432–441. doi: 10.1093/schbul/sbz067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.PRONIA. Personalised prognostic tools for early psychosis management project website.
- 51.NAPLS. The North American prodrome longitudinal study project website.
- 52.Satterthwaite T.D., Connolly J.J., Ruparel K. The Philadelphia neurodevelopmental cohort: a publicly available resource for the study of normal and abnormal brain development in youth. Neuroimage. 2016;124(Pt B):1115–1119. doi: 10.1016/j.neuroimage.2015.03.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chang C.K., Hayes R.D., Broadbent M. All-cause mortality among people with serious mental illness (SMI), substance use disorders, and depressive disorders in southeast London: a cohort study. BMC Psychiatry. 2010;10:77. doi: 10.1186/1471-244X-10-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Taylor D., Barnes T.R.E., Young A.H. 13th Edition. Wiley-Blackwell; London: 2018. The Maudsley prescribing guidelines in psychiatry. [Google Scholar]
- 55.Fusar-Poli P., Nelson B., Valmaggia L., Yung A.R., McGuire P.K. Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: impact on psychopathology and transition to psychosis. Schizophr Bull. 2014;40(1):120–131. doi: 10.1093/schbul/sbs136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fusar-Poli P., De Micheli A., Chalambrides M., Singh A., Augusto C., McGuire P. Unmet needs for treatment in 102 individuals with brief and limited intermittent psychotic symptoms (BLIPS): implications for current clinical recommendations. Epidemiol Psychiatr Sci. 2019;29:e67. doi: 10.1017/S2045796019000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Davies C., Radua J., Cipriani A. Efficacy and acceptability of interventions for attenuated positive psychotic symptoms in individuals at clinical high risk of psychosis: a network meta-analysis. Front Psychiatry. 2018;9:187. doi: 10.3389/fpsyt.2018.00187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fusar-Poli P., Davies C., Solmi M. Preventive treatments for psychosis: umbrella reivew (just the evidence) Front Psychiatry. 2019;11(10):764. doi: 10.3389/fpsyt.2019.00764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bosnjak Kuharic D., Kekin I., Hew J., Rojnic Kuzman M., Puljak L. Interventions for prodromal stage of psychosis. Cochrane Database Syst Rev. 2019;2019(11) doi: 10.1002/14651858.CD012236.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kirkbride J.B., Errazuriz A., Croudace T.J. Incidence of schizophrenia and other psychoses in England, 1950–2009: a systematic review and meta-analyses. PLoS ONE. 2012;7(3):e31660. doi: 10.1371/journal.pone.0031660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fusar-Poli P., Cappucciati M., Borgwardt S. Heterogeneity of risk for psychosis within subjects at clinical high risk: meta-analytical stratification. JAMA Psychiatry. 2016;73(2):113–120. doi: 10.1001/jamapsychiatry.2015.2324. [DOI] [PubMed] [Google Scholar]
- 62.Fusar-Poli P., Rutigliano G., Stahl D. Long-term validity of the at risk mental state (ARMS) for predicting psychotic and non-psychotic mental disorders. Eur Psychiatry. 2017;42:49–54. doi: 10.1016/j.eurpsy.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 63.Fusar-Poli P., Werbeloff N., Rutigliano G. Transdiagnostic risk calculator for the automatic detection of individuals at risk and the prediction of psychosis: second replication in an independent national health service trust. Schizophr Bull. 2018 doi: 10.1093/schbul/sby070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fusar-Poli P., Rutigliano G., Stahl D. Development and validation of a clinically based risk calculator for the transdiagnostic prediction of psychosis. JAMA Psychiatry. 2017;74(5):493–500. doi: 10.1001/jamapsychiatry.2017.0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fusar-Poli P., Oliver D., Spada G. Real-world implementation of a transdiagnostic risk calculator for the automatic detection of individuals at risk of psychosis in clinical routine: study protocol. Frontiers Psychiatry. 2019;10:109. doi: 10.3389/fpsyt.2019.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Raket L., Jaskolowski J., Kinon B. Dynamic ElecTronic hEalth reCord deTection (DETECT) of individuals at risk of a first-episode of psychosis: case-control development and validation study. Lancet Digital. 2020;2(5):E229–E239. doi: 10.1016/S2589-7500(20)30024-8. [DOI] [PubMed] [Google Scholar]
- 67.Fusar-Poli P., Cappucciati M., Rutigliano G. Diagnostic stability of ICD/DSM first episode psychosis diagnoses: meta-analysis. Schizophr Bull. 2016;42(6):1395–1406. doi: 10.1093/schbul/sbw020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shah J.L., Peters M.I. Early intervention in psychiatry: scotomas, representativeness, and the lens of clinical populations. Soc Psychiatry Psychiatr Epidemiol. 2019 doi: 10.1007/s00127-019-01686-x. [DOI] [PubMed] [Google Scholar]
- 69.Webb J.R., Addington J., Perkins D.O. Specificity of incident diagnostic outcomes in patients at clinical high risk for psychosis. Schizophr Bull. 2015;41(5):1066–1075. doi: 10.1093/schbul/sbv091. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.