Abstract
Background
Uncorrected refractive errors can be corrected by spectacles which improve visual functioning, academic performance and quality of life. However, spectacle wear can be low due to teasing/bullying, parental disapproval and no perceived benefit.
Hypothesis: higher proportion of children with uncorrected refractive errors in the schools allocated to the intervention will wear their spectacles 3–4 months after they are dispensed.
Methods
A superiority, cluster-randomised controlled trial was undertaken in 50 government schools in Hyderabad, India using a superiority margin of 20%. Schools were the unit of randomization. Schools were randomized to intervention or a standard school programme. The same clinical procedures were followed in both arms and free spectacles were delivered to schools. Children 11–15 years with a presenting Snellen visual acuity of <6/9.5 in one or both eyes whose binocular acuity improved by ≥2 lines were recruited.
In the intervention arm, classroom health education was delivered before vision screening using printed images which mimic the visual blur of uncorrected refractive error (PeekSim). Children requiring spectacles selected one image to give their parents who were also sent automated voice messages in the local language through Peek. The primary outcome was spectacle wear at 3–4 months, assessed by masked field workers at unannounced school visits. www.controlled-trials.com ISRCTN78134921 Registered on 29 June 2016
Findings
701 children were prescribed spectacles (intervention arm: 376, control arm: 325). 535/701 (80%) were assessed at 3–4 months: intervention arm: 291/352 (82.7%); standard arm: 244/314 (77.7%). Spectacle wear was 156/291 (53.6%) in the intervention arm and 129/244 (52.9%) in the standard arm, a difference of 0.7% (95% confidence interval (CI), -0.08, 0.09). amongst the 291 (78%) parents contacted, only 13.9% had received the child delivered PeekSim image, 70.3% received the voice messages and 97.2% understood them.
Interpretation
Spectacle wear was similar in both arms of the trial, one explanation being that health education for parents was not fully received. Health education messages to create behaviour change need to be targeted at the recipient and influencers in an appropriate, acceptable and accessible medium.
Funding
USAID (Childhood Blindness Programme), Seeing is Believing Innovation Fund and the Vision Impact Institute.
Research in context.
Evidence before this study
In this study we built upon previous research implemented in Kenya and Botswana using Peek as an mHealth intervention. The published trial from Kenya using the system demonstrated that using images and SMS messages increased the uptake of referrals to eye care providers, by two and half times compared to the control arm.
Added value of this study
This study shows that non-compliance to spectacles in children requires complex and context specific interventions for children who require spectacles, their classmates who do not, as well as teachers, parents, other family members and the community. Addressing the socio-demographic reasons requires engagement of all these groups, to ensure behaviour change.
Implications of all the available evidence
There is evidence that visual impairment in children has adverse effects on a child's academic performance, visual functioning, behavioural development and quality of life.
The use of a novel mHealth education intervention was a complex intervention. Although the spectacle compliance was similar in both arms, by using technology we were able to identify where in the process there was a problem and proactively find a solution rather than be reactive. Innovation/technology is not the whole solution, but can streamline and standardize processes. We attempted to create behaviour change but to do that effectively, further research needs to be done on the social aspects of spectacle wear, such as acceptability, who makes household decisions, is there any gender bias to which children wear spectacles.
Alt-text: Unlabelled box
1. Introduction
Uncorrected refractive errors (uREs) are the commonest cause of visual loss in children. Myopia (short-sightedness), the commonest form, usually starts around the age of eight years, progressing in severity throughout adolescence [1,2]. Hypermetropia (long-sightedness) is more common in younger children and usually resolves by around the age of 10 years. Astigmatism (distorted vision) affects all age groups and does not change over time. Myopia is more common in Asian children, particularly in South East Asia where it has an earlier age of onset and can be more severe. Approximately 12.8 million children worldwide are visually impaired from uREs [3], which is increasing, largely due to the increasing incidence of myopia in children in what is described as an ‘epidemic’ in East Asia, Europe and United States [4,5]. In Singapore, China, Taiwan, Hong Kong, Japan and Korea, 80–90% of children completing high school are now myopic [4,6]. All types of RE are less common in African children [7].
The increase in myopia is attributed to environmental factors associated with urbanisation, particularly prolonged near work and lack of time spent outdoors [6,8]. Urban children are at greater risk of myopia and there is increasing evidence that time spent outdoors is protective, although the biological mechanisms are not clear [9], [10], [11], [12], [13]. Correcting RE in children can lead to improvement in visual functioning [14] academic performance [15], social development [16,17] and quality of life [18].
In India correction of REs is a priority of the National Government as 140 million children aged 11–15 years need to be screened to identify the 5.6 million children who need spectacles [19]. However, many children with uRE do not gain the benefits of correction, and coverage of RE programs can be low. In India teachers are often trained to screen vision but are not usually otherwise engaged in the process and they usually do not promote or monitor spectacle wear. It is not standard practice in India to send explanatory pamphlets to parents of children requiring spectacles, and parents are not typically made aware of the benefits of spectacle wear. In all settings a relatively high proportion of children do not wear their spectacles [20,21], which was recently reported to be 70% in a study undertaken in a rural area of India [22]. There are many reasons why children do not wear spectacles such as being teased or bullied, they perceive no benefit, and concerns by parents that spectacles will weaken their child's eyes or are stigmatizing [23,[24], [25], [26], [27]]. Some of these reasons are amenable to health education. Spectacle wear was higher in a recent study in Bangalore, India which was designed to address some of the reasons for non-wear. Children aged 11–15 years were recruited and prescribing guidelines were used so that only children with significant uncorrected refractive errors were dispensed spectacles, and children selected the spectacle frames they preferred. In this study almost 75% of children were wearing their spectacles at unannounced visits 3–4 months later [28].
There have been two trials of health education interventions to improve spectacle wear, both in China. In one trial health education was delivered to students, and had negative results, suggesting that educating children alone is not effective [29]. The other trial had a factorial design with six subgroups. Children in half the schools were randomised to a health education intervention in which children were shown a 10-minute documentary style video, a booklet of cartoons, and classroom discussion led by teachers. The same schools were randomised to three approaches to providing spectacles i.e. free spectacles, a voucher, or children were given a prescription for spectacles. Spectacle wear was assessed by observation and self-report. Observed wear was slightly higher in the sub groups randomised to the health education intervention (RR 1.14 (1.03 to 1.26) but there was no difference in observed wear (RR 1.11 (0.94 to 1.30) [15].
Mobile phone technology is a rapidly expanding area in health care, including eye care and school eye health programmes [30]. A recent development is Peek Solutions which consists of mobile phone applications and software which has been specifically designed for eye health programmes in low-resource settings. Peek Solutions includes smartphone-based applications for vision screening (Peek Acuity) [31], and a vision simulator application which mimics the visual blur of uRE (PeekSim). PeekSim images can be printed. Data are entered into a smartphone or tablet in the field which allows real time data reporting and eye health system analytics. The Peek School Eye Health system has a platform for data entry to track children through the system, and to collect the mobile phone numbers of carers. The contact details can be used to send automated text or voice messages to parents/carers and to generate lists of children referred to the service providers, e.g. optometrists or hospital. Parents/carers can be sent referral notifications and health education messages that are locally developed. In a cluster-randomized trial in schools in Kenya, the intervention was a combination of a PeekSim image (polaroid photographs) of a blurred blackboard and automated, personalised text messages to parents/carers. At eight weeks, the uptake of referrals to the eye care providers was two and a half times higher in the Peek intervention arm than in the control arm [32]. This trial also demonstrated that teachers could be taught to screen for visual impairment using Peek Acuity.
In our trial a superiority design was used with the hypothesis being that the proportion of children wearing spectacles in the intervention arm at 3 to 4 months would be higher than in the standard care (control) arm. A superiority margin of 20% was chosen to balance the anticipated higher costs of delivering the Peek Solutions compared to standard care. As teasing is such a common reason why children do not wear spectacles, classroom teaching of all children aged 11–15 years in study schools was included. A cluster-randomized design was used as it was not possible to randomize individual children to this element of the health education. The trial protocol was published in March 2017 [33].
2. Methods
This study was undertaken in government and public-funded schools in and around Hyderabad, India. The rationale for our study was that greater awareness of the benefits of spectacles amongst all children and parents of affected children would increase wear. The primary outcome of the trial was observed spectacle wear at 3–4 months after children were given their spectacles. Reporting follows the CONSORT 2010 checklist for randomized controlled trials [34].
Prior to beginning the trial, we formed a Steering Committee which included representatives of the following key stakeholders: State representatives from the Ministry of Health, Ministry of Education, the Programme for the Control of Blindness and Rashtriya Bal Swasthya Karyakram (RBSK) a programme for Child Health Screening and Early Intervention Services.
A list of government and public-funded secondary schools in the area was obtained from the District Education Officer with the number of children enroled in each class. Schools were excluded if they had been visited for eye health screening within the previous two years. Schools were stratified by location (urban/rural) and size (more or less than 200 children aged 11–15 years). Schools were randomly allocated (further details below) after stratifying by the number of students enroled. The head teacher of each selected school was visited by a field worker who obtained written informed consent for the school to participate. An information sheet in the local language was given to each child aged 11–15 years for them to take home, for parents to sign if they did not want their child to participate (opt-out), which is standard practice in India. All children eligible to be recruited to the trial provided assent.
2.1. Participants
Recruitment took place between 5 January 2017 and 14 February 2017. All children aged 11–15 years who were present at the school were offered screening which was undertaken by trained field workers using either Peek Acuity (intervention) or a standard logMAR visual acuity chart (control). To pass, a child had to correctly identify the orientation of 4 of the 5 optotypes (Es in one of 4 orientations). Children who failed screening i.e. presenting visual acuity of less than Snellen 6/9.5 (logMAR 0.2) in one or both eyes, were referred for triage to the next room. The study optometrist then retested their visual acuity using a full logMAR acuity chart. If a child could see 6/9.5 in both eyes on repeat testing no further action was taken. Children confirmed with a visual acuity of less than 6/9.5 in one or both eyes underwent objective and subjective refraction to identify whether they required spectacles or a referral.
2.2. Interventions
The intervention was a complex intervention delivered using Peek Solutions. In this trial, PeekSim images deemed relevant to Indian children aged 11–15 years were used. Images were selected after formative research which entailed focus group discussions (FGD) with head teachers, parents, and boys and girls aged 11–15 years in different age groups. The FDGs explored participants views of spectacle wear by children and to seek their opinions on the PeekSim images to use in the trial. Parents and teachers gave input to the content of the voice messages, when they should be sent and how often. Teachers recommended that the classroom health education sessions using PeekSim images be delivered by members of the study team, as they were the “experts”. The teachers sat in the classroom when education was delivered. Based on the findings the following images were selected: a classroom with a blackboard, a famous South Indian movie celebrity, children playing the local game ‘khokho’, (Fig. 2) the Indian national cricket team, a market stall selling flowers, a clean village setting, and finally P.V. Sindhu (the first female Indian badminton player to win a silver Olympic medal). These images were printed A3 size for classroom teaching by members of the study team for all children in the classroom prior to screening.
Fig. 2.
Example of a PeekSim image – children playing ‘kho-kho’.
Children who required spectacles were given an A6 image of their choice to take home to show their parents, to demonstrate how much clearer their child's world would be if they wore their spectacles. Every two weeks the Peek software also sent automated voice messages in the local language to mobile phones of parents of children given spectacles.
In the control arm, the 6/9.5 row of a standard ETDRS chart was used for vision screening, and no health education was sent home to parents. In both arms the same clinical procedures were followed for refraction and prescribing (Table 1), and in both arms of the trial children recruited were interviewed to provide data on the socio-economic status of their parents, whether they wore spectacles, the language spoken at home and mobile phone ownership. Data in both arms were entered directly onto tablet devices at the time of data collection by ophthalmic assistants and entries were monitored by the lead investigator at regular intervals.
Table 1.
An overview of the two arms of the trial.
| Intervention arm | Comparator arm | |
|---|---|---|
| Age group | 11–15 years | 11–15 years |
| Screening method | Peek Acuity | Standard ETDRS chart |
| Screening VA level | <6/9.5 in one or both eyes | <6/9.5 in one or both eyes |
| Health education | • PeekSim images for classroom teaching by field workers, after sensitization and orientation i.e. for all children | None |
| • Eligible children selected a PeekSim image of their choice from a range of pre-tested images to take home to show their parents, with wording in the relevant local language | ||
| • Personalized voice messages for parents in the relevant local language | ||
| Data collection | Entered directly into Peek Solutions software using tablets | |
| Refraction | Trained optometrist | |
| Prescribing criteria | VA improves by 2 or more lines tested binocularly | |
| Frame types | A range of different coloured plastic frames | |
| Selection of frames | Children selected their preferred frame | |
| Delivery of spectacles | Delivery of free spectacles to schools within 2 weeks by trained field workers, and VA re-tested with correction | |
| Assessment of primary outcome | Observation during unannounced visits 3–4 months after spectacles were delivered | |
2.3. Sample size calculation
The sample size was calculated with a superiority margin of 20%, using the sampsi command in Stata Statistical Software version 14 (StataCorp, College Station, TX, USA). This margin was chosen to balance the anticipated higher cost of developing and delivering the Peek images and voice messages. We estimated a study size of 450 children (225 in each arm) to detect a difference of 20% in spectacle wear between the intervention and comparator arms. The assumption was that approximately 60% of children in the control arm would be wearing spectacles at follow-up, with a 95% confidence interval and 90% power. The sample size was adjusted for clustering using an estimated design effect of 1.5 from our previous study. We increased the sample size by 20% to allow for loss to follow-up. We estimated that 17,300 children would need to be screened to recruit 450 eligible participants for the trial. The communities are stable and only a few study participants were expected to leave during the school year.
2.4. Eligibility criteria
Eligibility criteria for the trial were a) children aged 11–15 years b) parents do not refuse participation, and c) presenting visual acuity (i.e. with spectacles if usually worn) of less than 6/9.5 in one or both eyes. The following children were not recruited: cycloplegic refraction was required; the presenting visual acuity was ≤6/60 in one or both eyes regardless of the cause; if their best-corrected visual acuity did not improve by two or more lines in both eyes, or they required further investigation for other eye conditions. These children were dispensed spectacles or referred, as required.
Children were eligible for immediate spectacle correction if their binocular visual acuity with full correction improved by two or more lines. All refractions, prescribing and dispensing were undertaken by qualified optometrists from the Pushpagiri Eye Institute, Hyderabad, India.
2.5. Randomisation and masking
Head teachers were visited and those giving permission were allocated a unique school ID. All the schools were randomised at once, so allocation concealment was not an issue. Randomization was done using a web-based randomisation service Sealed Envelope Ltd. 2016 simple randomisation service [Online]). Available from: https://www.sealedenvelope.com/simple-randomiser/v1/ [Accessed 3 Jan 2017]). Schools were randomised to intervention or comparator arm stratified by size, i.e. the number of children enroled at the school aged between 11 and 15 years. Schools were allocated to the intervention or control arm and not individual children to avoid contamination.
Recruitment bias was not likely as all children who failed screening had similar procedures thereafter which took place after recruitment. Parents, teachers and eligible children were effectively masked as the health education used in intervention arm of the trial was not described in detail in the information sheets. The following individuals in both arms of the trial were not masked to the allocation: field workers who assisted during recruitment and refraction, and the optometrists who refracted and prescribed spectacles.
2.6. Dispensing and delivery of spectacles
Children were allowed to select the frames they preferred from a range of different coloured plastic frames. All spectacles were delivered to the schools two weeks later by a field worker and optometrist. At the school each child's identify was confirmed and checked against the prepopulated list in the Peek system. Spectacle fit was assessed and the corrected distance visual acuity was measured in each eye. Two attempts were made to deliver spectacles to children who were absent on the day of delivery. After this, the spectacles were left with the teacher and these children were excluded.
2.7. Ascertainment of the primary outcome
New field workers were trained to assess the primary outcome at unannounced visits 3–4 months after spectacles were delivered. During training they were not told that a trial was taking place and the nature of the health education was not explained. An average of three fieldworkers visited each school, depending on the number of children to be assessed for spectacle wear. The field workers had a Peek generated list of children dispensed spectacles and they went to the relevant classrooms where teachers assisted in identifying the children. Whether each child was wearing their spectacles or not was noted. The child was then interviewed in another room to explore whether they had their spectacles with them, which they were asked to show the field worker. Spectacle wear was categorised as follows: children were a) wearing their spectacles at the time of the unannounced visit; b) not wearing their spectacles but had them at school (observed); c) were not wearing their spectacles but said they were at home; and d) children said they no longer had the spectacles as they were broken or lost [23]. Categories a) and b) were defined as wearing and categories c) and d) as non-wearing [23,28]. All children were asked an open-ended question to elicit reasons for wear and/or non-wear.
2.8. Statistical analysis
After data cleaning and range and consistency checks, the primary analysis was undertaken. Analyses were pre-specified, and were undertaken using STATA 14.1 (StataCorp, Texas, USA). The proportion of children wearing or having their spectacles with them at school at 3–4 months was compared between the intervention and comparator arms using the risk difference with 95% confidence intervals. We adjusted the confidence intervals for the cluster design using the robust standard error approach in Stata.
All analyses were undertaken according to the group to which the child had been allocated. No interim or subgroup analyses were planned or performed. However, we undertook a post hoc analysis of spectacle wear in children whose parents received the images. We observed that the two trial arms were not balanced for VA at baseline. From previous research we know that poorer presenting VA is a predictor of spectacle wear [35] and we undertook post hoc analysis that stratified the risk difference of spectacle wear by baseline VA.
2.9. Ethics
The trial was approved by the Interventions and Research Ethics Committee, London School of Hygiene & Tropical Medicine and the Institutional Review Board of Public Health Foundation India, Hyderabad. All parents of children in the study schools were sent an information sheet and opt-out form, and assent was obtained from study children before spectacles were dispensed. Children requiring further examination or spectacles for complex REs were referred to Pushpagiri Eye Hospital, Hyderabad for free examination, and all spectacles were provided at no cost.
2.10. Role of the funding source
The study was designed by the principal investigator (PM) and CG in collaboration with the other authors. The funders had no role in the design, data analysis, data interpretation, or writing the report. The corresponding author had full access to the data and had final responsibility for the decision to submit for publication.
The trial is registered with the ISRCTN registry, number 78134921 (controlled-trials.com).
3. Results
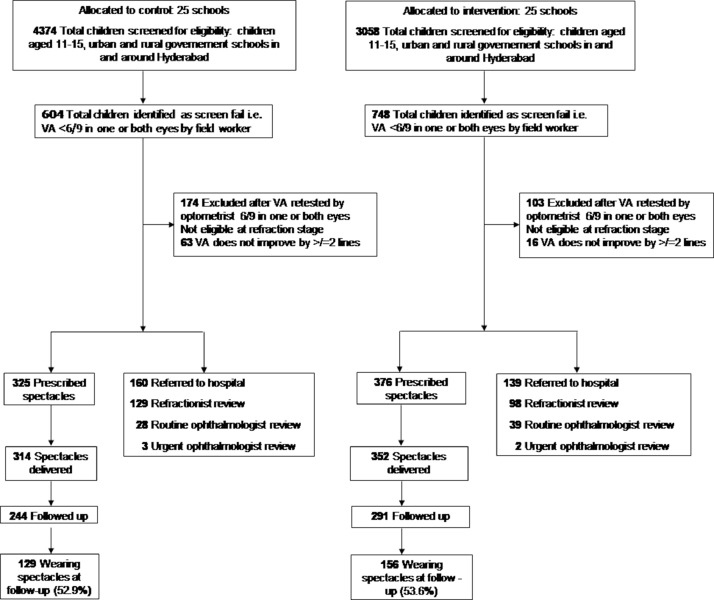
All school head teachers approached agreed that their school take part in the trial and no parent or child refused consent. 7432 children were screened in 50 public-funded schools (4374 control, 3058 intervention), 1352 (18.2%) of whom failed the screening test i.e. they had presenting visual acuity <6/9.5 in one or both eyes. 277 (20%) children were excluded as their visual acuity was 6/9.5 in both eyes on retesting (174/604 (29%) control, 103/748 (14%) intervention). A further 79 were excluded after refraction and basic eye examination and were referred (63 control, 16 intervention). 299 children required specialist refraction or examination and were referred (Fig. 1). amongst the 1352 children who screened positive, 701 (51.8%) were recruited and prescribed spectacles: 325 control, 376 intervention. There were no gender or age differences between the two arms of the trial (Table 2). Parents in the intervention arm were less well educated and only 2.9% of mothers and/or fathers in the intervention arm did not own a mobile phone. A higher proportion of children in the control arm had a binocular presenting visual acuity of <6/18 than in the intervention arm (52.0% and 40.7%, respectively).
Fig. 1.
Participant flow chart.
Table 2.
Baseline characteristics of study children, by trial arm.
| Control arm |
Intervention arm |
||||
|---|---|---|---|---|---|
| Socio-demographic variables | Spectacles prescribed (n = 325) | Spectacles prescribed(n = 376) | |||
| Mean (SD) | Range | Mean (SD) | Range | ||
| Age | 13.5 (1.30) | 11 to 15 | 13.4 (1.30) | 11 to 15 | |
| Gender | Female | 180 | 56.0 | 191 | 50.8 |
| N | % | N | % | ||
| Parental literacy* | Father only | 43 | 14.1 | 70 | 21.3 |
| Mother only | 25 | 8.2 | 35 | 10.7 | |
| Both parents | 201 | 66.1 | 135 | 41.2 | |
| Neither parent | 35 | 11.5 | 88 | 26.8 | |
| Parental spectacle wear | Father only | 42 | 12.9 | 35 | 9.3 |
| Mother only | 38 | 11.7 | 55 | 14.6 | |
| Both parents | 38 | 11.7 | 33 | 8.8 | |
| Neither parent | 207 | 63.7 | 253 | 67.3 | |
| Mobile phone ownership | Father only | 54 | 16.6 | 88 | 23.4 |
| Mother only | 27 | 8.3 | 44 | 11.7 | |
| Both parents | 238 | 73.2 | 233 | 62.0 | |
| Neither parent | 6 | 1.8 | 11 | 2.9 | |
| Presenting binocular vision | <6/9.5 - 6/12 | 133 | 40.9 | 172 | 45.7 |
| <6/12 - 6/18 | 23 | 7.1 | 51 | 13.6 | |
| <6/18 - 6/60 | 167 | 51.4 | 150 | 39.9 | |
| <6/60 | 2 | 0.6 | 3 | 0.8 | |
deceased parents are not included.
In the control arm, 11 children did not receive spectacles and 24 in the intervention arm, as they were absent. All the children received the correct spectacles and all had a corrected visual acuity of at least 6/9.5 in each eye with their new spectacles at the time of delivery.
At follow up, 76% (535/701) children were present: 244/314 (77.7%) in the control arm and 291/352 (82.7%) in the intervention arm. All 166 children (23.7%) not present had changed schools or moved to a different area and could not be traced. None of the children could transfer to a school in the other arm as no recruitment could take place after commencement of the trial. When we compared the characteristics of children that were absent at follow-up to those that were present, they were similar proportions of gender: absent male 44.3% and present male 47.9%. There were also more older children who were absent (14–15 years) compared to those in the younger age group 11–13 years). Overall 53.3% (285/535) of children were wearing their spectacles or had them at school; 52.9% (129/244) in the control arm and 53.6% (156/291) in the intervention arm, a difference of 0.7% (95% CI, −7.7 to 9.2). Adjusting for baseline characteristics in table 1 resulted in an adjusted risk difference of 3.7% (−5.6% to 12.6%).
Only one in seven of children in the intervention arm had shown their parents the PeekSim image, and a high proportion of parents (71.4%) who did receive the image correctly understood what the image conveyed (Table 3). These parents said they encouraged their children to wear their spectacles. The voice message reached a far higher proportion of parents (70.3%) and the vast majority understood the message.
Table 3.
Phone calls to parents whose children were given a PeekSim image to take home.
| Intervention arm (n = 376) |
Control arm (n = 325) |
|||
|---|---|---|---|---|
| N | % | N | % | |
| Parents called* | 292 | 77.7% | 244 | 75.1% |
| Calls answered | 202 | 69.2% | 151 | 61.9% |
| Aware their child had undergone an eye test and were given spectacles at school | 195 | 96.5% | 141 | 93.4% |
| Parents received image | 28 | 13.9% | NA | NA |
| Parents understood image | 20 | 71.4% | NA | NA |
| Parents received the voice message | 145 | 71.8% | NA | NA |
| Parents understood the voice message | 141 | 97.2% | NA | NA |
some mobile phone numbers were incorrect or unreachable
Spectacle wear amongst children whose parents received and understood the image was 45% (9/20), 56% (79/141) for those receiving and understanding the voice message, and (22/81) (27.2%) for those receiving and understanding both.
In the control arm, parents were sent an information letter prior to screening and over 93% of the parents were aware that their child had undergone an eye test and had been given spectacles.
4. Discussion
At the 3–4-month follow-up, spectacle wear was almost identical in both arms of the trial, suggesting that the health education intervention (simulated images for classroom education and parents; voice messages for parents) had not brought about behaviour change. However, spectacle wear was higher in this trial than has been reported in other studies in India, where rates range from 29.4% [36] to 58.0% [37], but lower than in our earlier trial of ready-made vs custom-made spectacles (overall 75%) [28]. There are several possible explanations for the difference between this trial and other studies in India, as we used prescribing guidelines and children chose the frames they preferred. Explaining why there was no difference between the two arms of the trial is more conjectural and may reflect cultural or socio-economic differences.
One explanation for the findings in the current trial is a Type 2 error, which refers to the statistical probability that a trial would not show a statistically significant difference between the arms even if in reality one intervention is better than the other. Having said this, it is important to explore why trials might have negative findings [38]. Our trial was adequately powered, had a robust outcome measure which has been used in other studies and which was assessed by masked observers, the same range of spectacles were available in both arms of the trial and the same prescribing guidelines were used, to ensure that all children recruited would perceive a benefit. Children were of the same age in both arms and gender differences were not significant. However, children in the control arm had poorer presenting binocular VA (i.e., <6/18: 52.0% in the control arm; 40.7% in the intervention arm), which may have led to greater spectacle wear in the control arm on account of greater improvement in vision (Appendix 1).
Table A1.
Proportion wearing and not-wearing spectacles by allocation group and presenting vision.
| Presenting binocular vision | Control (n = 244) |
Peek (n = 291) |
Risk difference | CI | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Wearing spectacles (n) | Not wearing spectacles (n) | Total | % wearing spectacles | Wearing spectacles (n) | Not wearing spectacles (n) | Total | % wearing spectacles | |||
| <6/9.5 - 6/12 | 11 | 18 | 29 | 38% | 17 | 18 | 35 | 49% | 10.6% | −13% to 35% |
| <6/12 - 6/18 | 38 | 48 | 86 | 44% | 67 | 68 | 135 | 50% | 6.2% | −80% to 19% |
| <6/18 - 6/60 | 80 | 49 | 129 | 62% | 72 | 49 | 121 | 60% | −2.5% | −15% to 10% |
| <6/60 | 129 | 115 | 244 | 53% | 156 | 135 | 291 | 54% | 0.7% | −7% to 9% |
A likely explanation for the lack of difference relates to the fidelity of the health education package (simulated images and voice messages generated through Peek). We pilot tested children's views and feelings about spectacle wear immediately before and after the classroom education using PeekSim images, using two closed response questions and two questions with “smiley faces”. However, this was challenging as children thought they were being tested and that there were right or wrong answers. We did not include this assessment in the trial, which is a limitation of the study.
Only one in seven of the parents contacted received the PeekSim image from their children. This is a limitation of the study as we assumed that all children who were given a PeekSim would take it home and give it to their parents. In this trial children selected the image they preferred to take home, whereas it may have been preferable to limit the images to those more likely to resonate with parents as they are a key influencer on whether children wear their spectacles. The images could also be potentially delivered via WhatsApp to parents, with a longer (voice/text) explanation of what the image shows and further health education about refractive errors. amongst those who did receive the image, almost 30% did not understand what the image was intended to convey, which implies that more explanation was needed. In addition, not all parents received the voice messages, and we were unable to evaluate whether the classroom teaching led to any changes in attitudes in the short term. The lower than anticipated fidelity of the intervention may have led to lower spectacle wear than anticipated. These two factors in combination (i.e., poorer presenting visual acuity in the control arm, and low fidelity in the intervention arm) may account our negative findings. However, a similar intervention in Kenyan schools where parents were sent an image of blackboard that mimicked visual blur, in which the primary outcome was adherence to hospital referral, gave positive results [32]. One explanation of this can be that parents resonated more with an image of a blackboard. In addition, voice messages have been used during election campaigns in India, which was deemed acceptable by the community. Our findings align with a recent Cochrane review on vision screening found that health education initiatives (as currently formulated and tested) had little impact on spectacle wear [39].
The intervention used in this trial was based on some of the elements of the Social Ecological framework [40], which describes the multifaceted and interactive effects of personal and environmental factors that determine behaviours. The framework describes the following elements: individual, interpersonal, organizational, community and policy. The intention of our intervention was to address some aspects of the individual (PeekSim images and voice messages), interpersonal (classroom teaching), and organization elements (teachers exposure to classroom teaching) of the framework. Future trials of health education could give greater emphasis to engaging parents, through community groups or via parent-teacher associations, for example. Addressing the broader community component i.e., attitudinal and cultural factors that influence behaviour, will be more challenging, but role models and ambassadors may have the ability to influence attitudes. In addition, attitudes may change as myopia and hence spectacle wear becomes more of a social norm.
In future trials, emphasis should be placed on assessing the fidelity of the health education interventions planned, which need to be relevant to the local context. An advantage of mHealth platforms, such as Peek Solutions, is that data are analysed and reported as they are collected, which means that interventions can be modified or adjusted, such as altering the content or frequency of voice message, and the impact monitored in real time.
Author contributions
The study was designed by the principal investigator Priya Morjaria and Clare Gilbert in collaboration with the other authors.
Data collection: Mekala Jayanthi Sagar, Pallepogula Dinesh Raj
Analysis and interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Priya Morjaria, Jennifer Evans, Clare Gilbert, Andrew Bastawrous
Administrative, technical, or material support: Priya Morjaria.
Declaration of Competing Interest
All authors except Dr Morjaria and Dr Bastawrous declare no conflicts of interest.
Dr. Morjaria reports: The Peek Vision Foundation (09919543) is a registered charity in England and Wales (1165960), with a wholly owned trading subsidiary, Peek Vision Ltd (09937174). Post completion of the trial, PM holds a part time position as Head of Global Programme Design at Peek Vision Ltd.
Dr. Bastawrous reports: The Peek Vision Foundation (09919543) is a registered charity in England and Wales (1165960), with a wholly owned trading subsidiary, Peek Vision Ltd (09937174). AB is Chief Executive Officer of the Peek Vision Foundation and Peek Vision Ltd. All other authors have nothing to disclose
Acknowledgments
Acknowledgements
The authors thank all the children and their families for participating in the study. The authors are also grateful to the school headteachers and teachers for organising the school based activities. Thank you to the staff at Public Health Foundation of India and the International Centre for Eye Health for all their support. Finally, a thank you the team from Pushpagiri Vitreo Retina Institute.
Funding
The study was funded by USAID – Child Blindness Program, Standard Chartered – Seeing is Believing Innovation Fund and the Vision Impact Institute. The funders had no role in the design, data analysis, data interpretation, or writing the report.
Data sharing
The datasets used and/or analysed during this study can be obtained from the corresponding author upon appropriate request. Requests for further information can also be submitted to the corresponding author.
References
- 1.Morgan I., Rose K. How genetic is school myopia? Prog Retin Eye Res. 2005 Jan;24(1):1–38. doi: 10.1016/j.preteyeres.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 2.Cumberland P.M., Peckham C.S., Rahi J.S. Inferring myopia over the lifecourse from uncorrected distance visual acuity in childhood. Br J Ophthalmol. 2007 Feb;91(2):151–153. doi: 10.1136/bjo.2006.102277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Resnikoff S., Pascolini D., Mariotti S.P., Pokharel G.P. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008 Jan;86(1):63–70. doi: 10.2471/BLT.07.041210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morgan I.G., Ohno-Matsui K., Saw S.M. Myopia. Lancet. 2012 May 5;379(9827):1739–1748. doi: 10.1016/S0140-6736(12)60272-4. [DOI] [PubMed] [Google Scholar]
- 5.Holden B.A., Fricke T.R., Wilson D.A. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016 May;123(5):1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 6.Pan C.W., Ramamurthy D., Saw S.M. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2012 Jan;32(1):3–16. doi: 10.1111/j.1475-1313.2011.00884.x. [DOI] [PubMed] [Google Scholar]
- 7.Rudnicka A.R., Kapetanakis V.V., Wathern A.K. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016 Jul;100(7):882–890. doi: 10.1136/bjophthalmol-2015-307724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rose K.A., French A.N., Morgan I.G. Environmental factors and myopia: paradoxes and prospects for prevention. Asia Pac J Ophthalmol (Phila) 2016 Nov/Dec;5(6):403–410. doi: 10.1097/APO.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 9.French A.N., Morgan I.G., Mitchell P., Rose K.A. Risk factors for incident myopia in Australian schoolchildren: the Sydney adolescent vascular and eye study. Ophthalmology. 2013 Oct;120(10):2100–2108. doi: 10.1016/j.ophtha.2013.02.035. [DOI] [PubMed] [Google Scholar]
- 10.He M., Xiang F., Zeng Y. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical Trial. JAMA. 2015 Sep 15;314(11):1142–1148. doi: 10.1001/jama.2015.10803. [DOI] [PubMed] [Google Scholar]
- 11.Sherwin J.C., Reacher M.H., Keogh R.H. The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis. Ophthalmology. 2012 Oct;119(10):2141–2151. doi: 10.1016/j.ophtha.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 12.Wu P.C., Tsai C.L., Wu H.L., Yang Y.H., Kuo H.K. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology. 2013 May;120(5):1080–1085. doi: 10.1016/j.ophtha.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Xiong S., Sankaridurg P., Naduvilath T. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017 Sep;95(6):551–566. doi: 10.1111/aos.13403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dirani M., Zhang X., Goh L.K. The role of vision in academic school performance. Ophthalmic Epidemiol. 2010 Jan-Feb;17(1):18–24. doi: 10.3109/09286580903450320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ma X., Zhou Z., Yi H. Effect of providing free glasses on children's educational outcomes in China: cluster randomized controlled trial. BMJ. 2014 Sep 23;349:g5740. doi: 10.1136/bmj.g5740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ibironke J.O., Friedman D.S., Repka M.X. Child development and refractive errors in preschool children. Optom Vis Sci. 2011 Feb;88(2):181–187. doi: 10.1097/OPX.0b013e318204509b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kilic-Toprak E., Toprak I. Future problems of uncorrected refractive errors in children. Procedia - Social and Behavioral Sciences. 2014;159:534–536. 2014/12/23/ [Google Scholar]
- 18.Pizzarello L., Tilp M., Tiezzi L., Vaughn R., McCarthy J. A new school-based program to provide eyeglasses: childsight. J AAPOS. 1998 Dec;2(6):372–374. doi: 10.1016/s1091-8531(98)90038-6. [DOI] [PubMed] [Google Scholar]
- 19.Jose R., Sachdeva S. School eye screening and the national program for control of blindness. Indian Pediatr. 2009 Mar;46(3):205–208. [PubMed] [Google Scholar]
- 20.Sharma A., Congdon N., Patel M., Gilbert C. School-based approaches to the correction of refractive error in children. Surv Ophthalmol. 2012 May-Jun;57(3):272–283. doi: 10.1016/j.survophthal.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Morjaria P., McMormick I., Gilbert C. Compliance and predictors of spectacle wear in schoolchildren and reasons for non-wear: a review of the literature. [Review]. In press 2018. [DOI] [PubMed]
- 22.Gogate P., Mukhopadhyaya D., Mahadik A. Spectacle compliance amongst rural secondary school children in Pune district, India. Indian J Ophthalmol. 2013 Jan-Feb;61(1):8–12. doi: 10.4103/0301-4738.99996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wedner S., Masanja H., Bowman R. Two strategies for correcting refractive errors in school students in Tanzania: randomised comparison, with implications for screening programmes. Br J Ophthalmol. 2008 Jan;92(1):19–24. doi: 10.1136/bjo.2007.119198. [DOI] [PubMed] [Google Scholar]
- 24.Rustagi N., Uppal Y., Taneja D.K. Screening for visual impairment: outcome among schoolchildren in a rural area of Delhi. Indian J Ophthalmol. 2012 May-Jun;60(3):203–206. doi: 10.4103/0301-4738.95872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Castanon Holguin A.M., Congdon N., Patel N. Factors associated with spectacle-wear compliance in school-aged Mexican children. Invest Ophthalmol Vis Sci. 2006 Mar;47(3):925–928. doi: 10.1167/iovs.05-0895. [DOI] [PubMed] [Google Scholar]
- 26.Zeng Y., Keay L., He M. A randomized, clinical trial evaluating ready-made and custom spectacles delivered via a school-based screening program in China. Ophthalmology. 2009 Oct;116(10):1839–1845. doi: 10.1016/j.ophtha.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ethan D., Basch C.E. Promoting healthy vision in students: progress and challenges in policy, programs, and research. J Sch Health. 2008 Aug;78(8):411–416. doi: 10.1111/j.1746-1561.2008.00323.x. [DOI] [PubMed] [Google Scholar]
- 28.Morjaria P., Evans J., Murali K., Gilbert C. Spectacle wear among children in a school-based program for ready-made vs custom-made spectacles in India: a randomized clinical trial. JAMA Ophthalmol. 2017 Jun 1;135(6):527–533. doi: 10.1001/jamaophthalmol.2017.0641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Congdon N., Li L., Zhang M. Randomized, controlled trial of an educational intervention to promote spectacle use in rural China: the see well to learn well study. Ophthalmology. 2011 Dec;118(12):2343–2350. doi: 10.1016/j.ophtha.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 30.Morjaria P., Bastawrous A. Helpful developments and technologies for school eye health programmes. Community Eye health. 2017;30(98):34–36. [PMC free article] [PubMed] [Google Scholar]
- 31.Bastawrous A., Rono H.K., Livingstone I.A. Development and validation of a smartphone-based visual acuity test (peek acuity) for clinical practice and community-based fieldwork. JAMA Ophthalmol. 2015 Aug;133(8):930–937. doi: 10.1001/jamaophthalmol.2015.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rono H.K., Bastawrous A., Macleod D. Smartphone-based screening for visual impairment in Kenyan school children: a cluster randomised controlled trial. Lancet Glob Health. 2018 Aug;6(8):e924–ee32. doi: 10.1016/S2214-109X(18)30244-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morjaria P., Bastawrous A., Murthy G.V.S., Evans J., Gilbert C. Effectiveness of a novel mobile health education intervention (Peek) on spectacle wear among children in India: study protocol for a randomized controlled trial. Trials. 2017 Apr 8;18(1):168. doi: 10.1186/s13063-017-1888-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moher D., Hopewell S., Schulz K.F. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int J Surg. 2012;10(1):28–55. doi: 10.1016/j.ijsu.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 35.Morjaria P., Evans J., Gilbert C. Predictors of spectacle wear and reasons for nonwear in students randomized to ready-made or custom-made spectacles: results of secondary objectives from a randomized noninferiority trial. JAMA Ophthalmol. 2019 Apr 1;137(4):408–414. doi: 10.1001/jamaophthalmol.2018.6906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rustagi N., Uppal Y., Taneja D.K. Screening for visual impairment: outcome among schoolchildren in a rural area of Delhi. Indian J Ophthalmol. 2012 May-Jun;60(3):203–206. doi: 10.4103/0301-4738.95872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pavithra M.B., Hamsa L., Suwarna M. Factors associated with spectacle-wear compliance among school children of 7-15 years in South India. Int J Med Public Health. 2014;4(2):146–150. [Google Scholar]
- 38.Pocock S.J., Stone G.W. The primary outcome fails - what next? N Engl J Med. 2016 Sep 1;375(9):861–870. doi: 10.1056/NEJMra1510064. [DOI] [PubMed] [Google Scholar]
- 39.Evans J.R., Morjaria P., Powell C. Vision screening for correctable visual acuity deficits in school-age children and adolescents. Cochrane Datab Syst Rev. 2018 Feb 15;2 doi: 10.1002/14651858.CD005023.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gregson J., Foerster S.B., Orr R. System, environmental, and policy changes: using the social-ecological model as a framework for evaluating nutrition education and social marketing programs with low-income audiences. J Nutr Educ. 2001;33(Suppl 1):S4–15. doi: 10.1016/s1499-4046(06)60065-1. [DOI] [PubMed] [Google Scholar]