Abstract
Introduction
Every year, >5 million people worldwide die from trauma. In Kigali, Rwanda, 50% of prehospital care provided by SAMU, the public prehospital system, is for trauma. Our collaboration developed and implemented a context-specific, prehospital Emergency Trauma Care Course (ETCC) and train-the-trainers program for SAMU, based on established international best practices.
Methods
A context-appropriate two-day ETCC was developed using established best practices consisting of traditional 30-minute lectures followed by 20-minute practical scenario-based team-driven simulation sessions. Also, hands-on skill sessions covered intravenous access, needle thoracostomy and endotracheal intubation among others. Two cohorts participated — SAMU staff who would form an instructor core and emergency staff from ten district, provincial and referral hospitals who are likely to respond to local emergencies in the community. The instructor core completed ETCC 1 and a one-day educator course and then taught the second cohort (ETCC2). Pre and post course assessments were conducted and analyzed using Student's t-test and matched paired t-tests.
Results
ETCC 1 had 17 SAMU staff and ETCC 2 had 19 hospital staff. ETCC 1 mean scores increased from 40% to 63% and ETCC 2 increased from 41% to 78% after the course (p < 0.001 using matched pair analysis). A one-way ANOVA mean square analysis showed that regardless of the baseline level of training for each participant, all trainees reached similar post-course assessment scores, F (1) = 15.18, p = 0.0004.
Discussion
This study demonstrates effective implementation of a context-appropriate prehospital trauma training program for prehospital staff in Kigali, Rwanda. The course resulted in improved knowledge for an instructor core and for staff from district and provincial hospitals confirming the effectiveness of a train-the-trainers model. This program may be effective to support capacity development for prehospital trauma care in the country using a qualified local source of instructors.
Keywords: Trauma, Prehospital, Education, Africa, Rwanda
African relevance
-
•
Fifty percent of prehospital care provided in Rwanda is for trauma
-
•
In Rwanda injury counts for 14% of all reported deaths
-
•
A prehospital emergency trauma care course was effective in training prehospital providers, physicians and nurses in Rwanda
-
•
An instructor core has been created in Rwanda that can effectively teach prehospital trauma care in East Africa
Introduction
Trauma represents a significant burden of disease throughout the world. Every year, >5 million people die from trauma which is 1.7 times more than the number who die from HIV/AIDS, malaria and tuberculosis combined. Additionally, 20–50 million people experience significant disability secondary to trauma yearly [1]. The greatest burden of trauma-related death and disability falls on low and middle-income countries (LMIC) [1]. In addition to the public health implications of this unequal burden, trauma-related death and disability often carry with it a significant economic impact. Expenses associated with road traffic incidents alone were estimated to cost low-income countries US$65 billion as of 2006 and largely involve economically productive young adults, thus contributing to catastrophic expenditure [2]. Road traffic crashes are on track to become the 7th leading cause of death in the world by 2030 [1].
The World Bank estimates that nearly 45% of all deaths in low-income countries are potentially addressable through effective emergency medical services (EMS). Prehospital care provided by an EMS system is critical for optimal outcomes [3., [4], [5]]. In high-income countries with EMS systems, there has been a steady decline in trauma mortality [2]. For a variety of reasons, LMICs have been slow to establish EMS systems to address the burden of trauma even though they could have a significant impact on reducing one of the leading causes of morbidity and mortality.
In Rwanda, injury accounts for 14% of all reported deaths (2016) [6]. In Kigali, the capital of Rwanda, trauma accounted for 22% of deaths between 2012 and 2014 [7]. A quarter of all deaths (trauma included), occurred in the prehospital setting and 49% of trauma-related deaths occurred within 24 h of arriving at the hospital [4,8]. The mortality rate of injured patients transported to the country's main teaching hospital, CHUK was 5.5% overall [9]. Fifty percent of the cases in Kigali that are managed by Service d'Aide Medicale Urgente (SAMU), Rwanda's national EMS system, are due to physical trauma [10]. However, the SAMU staff have not had any standardized prehospital trauma training. While a simple trauma quality improvement program led to substantial improvement in prehospital care delivery, this did not address the need for prehospital trauma training [8].
Short trauma training sessions have been effective to increase knowledge and improve patient outcomes in the hospital setting. A three-day trauma education course for surgeons and trauma nurses in Rwanda led to improvements in mortality for injured patients [11]. The College of Surgeons of South East Central and Southern Africa use of primary trauma management courses to doctors, nurses and medical students led to an improvement in knowledge and clinical confidence in the majority of its participants [12]. Though limited to in-hospital settings, these studies enforce the likelihood of success of our model in the prehospital setting.
This project aimed to develop and implement a context-specific, prehospital trauma training course and train-the-trainers program for SAMU based on established international best practices and build a local Instructor core which can serve as a resource of prehospital trauma education for the country and the region.
Methods
Study context and setting
Rwanda is one of the only countries in Sub-Saharan Africa to have a publicly run, national ambulance service, which was established in 2007, SAMU previously described [8]. SAMU manages a fleet of 16 ambulances in Kigali and treats roughly 4500 patients annually at the centralized call center in Kigali. Ambulances are staffed by nurses and anesthetists. However there has been no established systematic training in prehospital care [13]. Anesthetists earn a bachelor's degree in anesthesia focusing on training in the operating room, while nurses receive a bachelor's degree in nursing similar to a registered nursing program in the United States. Both are trained for in-hospital care and receive no prehospital specific training. At SAMU, anesthetists perform traditional ALS skills such as endotracheal intubation and medication administration, while nurses perform BLS skills such as bandaging and splinting. Through a memorandum of understanding with the Rwandan Ministry of Health (MOH), SAMU and Virginia Commonwealth University (VCU), we developed and implemented a prehospital trauma training course and train-the-trainers program for SAMU that included a two-day trauma course followed by a one-day educator course and a second two day trauma course using the train-the-trainer model.
Study design
A baseline pre-assessment of SAMU staff was conducted in November 2017 to determine knowledge across basic anatomy and physiology, medicine, obstetrics, pediatrics, trauma and scene safety. The pre-assessment was administered as a written, 100-question multiple choice, English-language exam and was based on standardized evaluations of prehospital staff in the United States. The questions were customized to the context with the help of SAMU leadership, which includes nurses and anesthetists with equivalent experts from VCU, as necessary. This was essential, as medications and materials for intervention in the United States are not all available in Rwanda. Deficiencies were identified and used to enhance a context-specific curriculum. The curriculum of the two-day Emergency Trauma Care Course (ETCC) consisted of traditional 30 minute lectures on a topic (e.g. pathophysiology of airway and breathing) followed by 20 min a practical scenario-based team-driven simulation sessions designed to test application of knowledge and skills (e.g., Crowd control, scene safety, etc.) and 10 min of debriefing, as well as hands-on individual skill stations on endotracheal intubation, needle thoracostomy, nasopharyngeal airway insertion, infant bag valve mask, intravenous access, etc. (Table 1). The curriculum was developed by the VCU Center for Trauma and Critical Care Education collaboratively with SAMU based on best practices outlined by the WHO, the Virginia Department of Health Mass Casualty Management, the American College of Surgeons Prehospital Trauma Life Support as well as texts on emergency response and emergency nursing [[13], 14., [15], [16]]. In addition, a one-day educator course was developed and implemented for the instructor core group to cover educational theory [17], learning styles, and effective teaching and feedback delivery strategies. The ETCC train-the-trainers program was conducted in January 2018.
Table 1.
Topics and hands on sessions covered during ETCC1/2.
| Course section | Topics |
|---|---|
| Lecture |
|
| Simulation sessions |
|
| Hands on sessions |
|
Participants
SAMU leadership selected a cohort of SAMU staff to participate in the first course and form an instructor core. A second cohort of ambulance and emergency staff from ten referral, provincial and district hospitals was chosen by the MOH to participate in the second trauma course taught by the initial instructor Core.
Measurement of proficiency and data analysis
A 50-question multiple-choice timed written assessment was administered in English before and after each two-day ETCC program. All assessments were captured confidentially, and each participant was assigned a unique ID for de-identified analysis. Passing score was set at 80%. Instructors had to pass ETCC 1, complete the educator course and conduct a pre-specified section of ETCC 2 under direct observation of VCU instructor staff, including a trauma nurse, emergency medicine physician, trauma surgeon and a paramedic educator, to be certified as ETCC instructors. Certificates were given to attendees for the trainee course (ETCC1 and ETCC 2) based on assessment scores, for completing the educator course and for meeting the requirements for course instructor which included observation and critical feedback of teaching didactic, skills and simulation-based content in ETCC 2. Trainees who failed to meet the passing score on their post-course assessment were remediated by taking the same exam in English at a later date with one on one supervision by the SAMU leadership.
Matched paired t-tests were used to evaluate assessment scores of each course, and an unmatched t-test was used for comparison of both courses with p < 0.05 considered statistically significant. Questions were grouped into easy, knowledge based, intermediate, application based and difficult, problem solving questions. Pre and post test differences were calculated to determine whether participants had a statistically significant difference in scores for the easy, intermediate and difficult level questions. A chi-square test of equal proportions was used to determine the difference in knowledge, application and problem-solving scores with an alpha value of 0.05 considered significant.
This study was conducted as part of an ongoing IRB approved project at VCU and the Rwanda MOH.
Results
The baseline assessment involved 25 SAMU staff. The mean score was 49.7 ± SD 14.
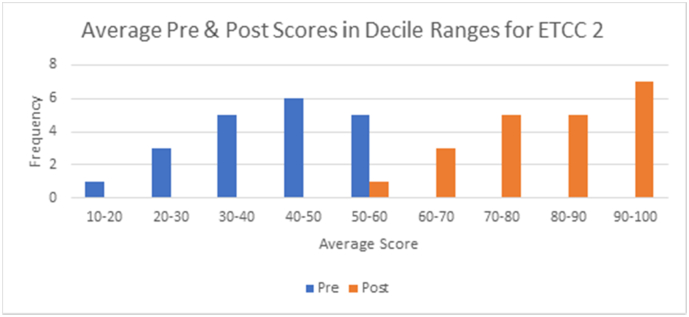
ETCC1 was attended by 17 SAMU staff. Mean scores on the pre-assessment were 40% and increased to 63% on post-assessment. Fig. 1 shows the frequency distribution of pre and post test scores in decile ranges for ETCC 1. Two students out of 17 in the initial cohort did not meet the minimum passing requirements in the post test with scores of 61% and 71% respectively. These trainees were remediated at the end of the course, retook the exam and passed. ETCC2 was attended by 19 hospital staff. Mean scores on the pre-assessment were 41% and increased to 78% on post-assessment. Fig. 2 shows the frequency distribution of pre and post test scores in decile ranges for ETCC 2. Of this cohort of 19 trainees, 6 did not meet the minimum passing requirements of 80% on the post-assessment. One reason for them not passing could have been due to language barriers since this cohort was less comfortable in English and yet the assessment was given in English. These trainees were also remediated by the SAMU leadership at the end of the course.
Fig. 1.
Frequency of scores from pre and post assessment for ETCC 1 Trainees.
Fig. 2.
Frequency of scores from pre and post assessment for ETCC 2 Trainees.
A one way ANOVA mean square analysis was used to compare the mean scores across all trainees before and after ETCC. Analysis of all pre- assessment scores demonstrated a significant difference between the two groups: F(1) = 16.31, p = 0.0003. However, the difference in means of post-assessment scores was not significantly different, F(1) = 3.44, p = 0.07. Thus, regardless of the baseline level of training for each participant, all trainees reached similar post- assessment scores. The change was significantly different: F(1) = 15.18, p = 0.0004.
A paired t-test comparing pre to post assessment means demonstrated an increase by 0.24 ± 0.11 (SD) for ETCC 1 (p < 0.001) and 0.37 ± 0.09 (SD) for ETCC 2 (p < 0.001) with a 95% confidence (Table 2). When comparing unequal variances across the two groups with a two-tailed paired t-test, ETCC 1 had a statistically significant mean change in pre to assessment test scores of 24% compared to 37% for ETCC 2, p < 0.001, with a 95% confidence.
Table 2.
Comparison of assessment scores by cohort.
| Cohort | Pre-assessment mean & SD | Post-assessment mean & SD | Difference in mean from pre to post assessment | p-Value (using matched pair t–test) |
|---|---|---|---|---|
| ETCC 1 | 0.39 ± 0.29 | 0.63 ± 0.4 | 0.24 ± 0.11 | <0.0001 |
| ETCC 2 | 0.41 ± 0.13 | 0.78 ± 0.22 | 0.37 ± 0.09 | <0.0001 |
A chi-square test was used to compare the ETCC1 and ETCC2 differences in knowledge, application and problem-solving questions. There was a statistically significant difference in ETCC1 and ETCC2 for knowledge (p < 0.0001), application (p < 0.0001) and problem solving (p = 0.0008) with an alpha value of 0.05 (Table 3). Similarly, a chi-square test was used to compare knowledge, application and problem-solving questions within each cohort. Not only did groups improve on the easier knowledge-based questions but also on the more difficult problem-solving questions with a statistically significant difference in ETCC2 of p = 0.0118 (Table 4).
Table 3.
Comparison of assessment scores based on difficulty of question by cohort.
| ETCC1 pre | ETCC2 post | ETCC1 diff | ETCC2 pre | ETCC2 post | ETCC2 diff | p-Value | |
|---|---|---|---|---|---|---|---|
| Knowledge | 0.3397 | 0.5032 | 0.1635 | 0.3815 | 0.7220 | 0.3405 | <0.0001 |
| Application | 0.2978 | 0.5069 | 0.2091 | 0.3818 | 0.7273 | 0.3455 | <0.0001 |
| Problem solving | 0.2947 | 0.4909 | 0.1962 | 0.4000 | 0.6826 | 0.2826 | 0.0008 |
Table 4.
Chi square test comparing difficulty of question within groups.
| ETCC1 pre | ETCC1 post | ETCC1 diff | ETCC2 pre | ETCC2 post | ETCC2 diff | |
|---|---|---|---|---|---|---|
| Knowledge | 0.3397 | 0.5032 | 0.1635 | 0.3815 | 0.7220 | 0.3405 |
| Application | 0.2978 | 0.5069 | 0.2091 | 0.3818 | 0.7273 | 0.3455 |
| Problem solving | 0.2947 | 0.4909 | 0.1962 | 0.4000 | 0.6826 | 0.2826 |
| p-Value | 0.3429 | 0.0118 |
Discussion
There is a wide awareness of the need for robust prehospital systems around the world. According to the Disease Control Priorities in Developing Countries, there is little data on how to accomplish this with meaningful efficacy [18]. This is one of the first studies in the literature to describe the implementation of a prehospital trauma training within an existing publicly supported EMS system in an LMIC setting. Rwanda is an unusual example across LMICs of a well-organized health system that had invested heavily in emergency medical services. This care is provided by SAMU's nurses and anesthetists. Our collaboration has written about the provision of prehospital care by SAMU and implementation of a continuous quality improvement program for trauma had immediate and substantial improvement in five critical pre-hospital trauma care metrics [8,10].
However, there is little written on tools to accurately assess clinical staff for their ability to provide prehospital care. In the US, prehospital or EMS staff have defined scope of practice outside of facility-based clinicians. In fact, the existence of nurse to paramedic programs in the US and EMS subspecialty fellowships for emergency physicians demonstrate the need for specific training in prehospital care to be able to effectively provide it. In this study, we first evaluated the current knowledge base of the SAMU staff using a baseline assessment across all EMS topics which was developed from standardized questions and were written by one of the authors (BA) who is experienced at writing questions for national nursing and EMS exams in the US. These questions were fine-tuned for language and context by our collaboration prior to implementation to ensure accuracy. The results of this assessment demonstrated that the SAMU team clearly needed training across all EMS topics. While SAMU is fortunate to have trained clinical staff, clearly nurses and nurse anesthesia programs train staff do not cover the content and skills for prehospital management of a diverse set of patients in Rwanda, much as they do not in the US. This and the 50% incidence of trauma in this setting made trauma training for SAMU an especially important focus for our collaboration. Trauma team training has previously been proven to reduce mortality and improve hospital-based outcomes [19]. This encouraged us to teach the prehospital staff to improve the outcomes of their patients.
Many studies have focused on improving access to emergency services in LMIC settings. These have largely focused on educating lay first responders to provide basic trauma care in an emergency since many settings have not meaningfully invested in creating a formal EMS system [4,20]. Others have examined the role of lay-person disaster response training [[21], [22], [23], [24]]. Similar to our study, in Botswana, a two-day prehospital course taught by US practitioners on a variety of prehospital care topics and not limited to trauma led to improvements in post test scores [25]. This study, though limited to trauma, demonstrates the development and implementation of formal prehospital trauma care training within an established EMS program which is unusual in the LMIC setting. The course content was developed based on extensive regional and national level experience in designing and teaching prehospital and emergency courses by some of the authors (BA, SJ, SL) at the VCU Center for Trauma and Critical Care Education. The content was designed based on international literature and developed collaboratively to ensure rigor and context appropriateness.
Furthermore, based on the immense evidence that problem-based and experiential learning is vastly more effective than traditional didactic teaching, the curriculum of the course was developed to largely emphasize scenario-based learning and skills practice with short didactic sections [26]. Such interactive educational methods are increasingly being implemented in trauma training [4]. Our results showed 50% increases in assessment scores across both cohorts (p < 0.001 in a matched pair analysis) and therefore demonstrates the effectiveness of this pre-hospital trauma education program. ETCC2 improved more than ETCC1 which validated the effectiveness of the newly trained SAMU ETCC instructors using this “train the trainers” model. In addition to increasing the mean assessment scores, both cohorts increased their scores in the more difficult questions as well as the easier knowledge-based questions (p < 0.0001 vs p = 0.0008).
Our program also had a special emphasis on adult education which has not yet been reported by others conducting train-the-trainers type education programs in trauma. An unusual feature of this program was the inclusion of an educator course that reviewed Bloom's taxonomy of adult learning, effective techniques in adult learning and teaching, approaches to giving effective feedback to trainees in order to ensure that the SAMU instructors had robust training in effective education methods [27]. There is no comparative literature in LMIC settings on training instructors to teach trauma courses effectively although instructor courses do exist for courses such as ATLS™ in the United States. The results of ETCC 2 especially highlight the effectiveness of the newly trained instructors which in part may have been due to this specialized educator training.
While this study has demonstrated the improvement in knowledge base of the prehospital staff, we did not seek data on change in clinical outcomes as that was beyond the scope of our project at this time. Evaluation of hospital-based outcomes is another avenue of quality improvement research in Kigali in the future. Lastly, language challenges may have affected results. Since the national language of Rwanda is English, the program was conducted largely in English with SAMU staff translating verbal content into French or Kinyarwanda as needed. This translation was performed by SAMU staff who were assisting with the course, it was very limited. However, trainees may have underperformed on both pre and post assessments since both were given in English. On discussing the results of trainees who did not pass ETCC 1 and had to remediate, language was immediately apparent as the main issue, especially since each assessment had a time limit of 1 h. Those who were not comfortable in English needed more time for translation, as SAMU staff was available for translation questions during the exam and could not get through all of the questions in the allotted time. It may be more effective to have local health care providers lead educational sessions compared to foreigners to avoid these issues. The pre and post assessments for ETCC 2 were conducted with more translation support. However, this may still have not been adequate and may have added to bias.
Conclusion
Prehospital care and the development of adequate EMS systems have resulted in substantial reduction in trauma-related deaths in high-income countries. Based on the trauma burden in Rwanda, education and training in prehospital trauma care has the potential to reduce trauma-related morbidity and mortality immensely along with associated potential for minimizing the economic impact of trauma. This study addresses the need for effective prehospital trauma training in Kigali where almost half of all trauma-related deaths occur in the prehospital setting and many more occur within the first 24 h of the hospital stay. This program, developed based on best practices to address the specific trauma training needs in Kigali, created a core of instructors in prehospital trauma care who can sustainably enhance the growth and expansion of prehospital trauma care in the country.
Funding
This project was funded through the Rotary Foundation Global Grant #GG1749568 and supported by the Ministry of Health of Rwanda through a Memorandum of Understanding with Virginia Commonwealth University. Neither influenced the conduct of this project to cause any meaningful bias in the results. SJ has had support from these sources during the course of this project: NIH R21: 1R21TW010439-01A1 (PI); Rotary Foundation Global Grant #GG1749568 (PI); NIH P20: 1P20CA210284-01A1 (PI); VCU Quest for Innovation Commercialization Grant (PI); and DOD grant W81XWH-16-2-0040 (PI).
Dissemination of results
Results from this course were shared with prehospital staff members from SAMU, the Ministry of Health of Rwanda, and at the American College of Surgeons Annual Meeting both through informal and formal presentations.
Authors' contribution
Authors contributed as follow to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: AR contributed 40%; CV 13%; SJ 10%; LW 7%; and IK, BA, JU, MN, GM, SL, TD contributed 5% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgements
We thank all SAMU and hospital staff who participated in the ETCC program and Dr Patrick Ndimubanzi, Minister of State at the Ministry of Health of Rwanda, for his support of the partnership with VCU and Rotary Foundation.
Contributor Information
Ashley Rosenberg, Email: Ashley.Rosenberg@vcuhealth.org.
Sudha Jayaraman, Email: sudhapjay@gmail.com.
References
- 1.Injury and violence: the facts 2014. 2014. http://apps.who.int/iris/bitstream/10665/149798/1/9789241508018_eng.pdf
- 2.Chen Simiao, Kuhn Michael, Prettner Klaus, Bloom David E. The global macroeconomic burden of road injuries: estimates and projections for 166 countries. Lancet Planet Health. 2019;3(9):e390–e398. doi: 10.1016/S2542-5196(19)30170-6. [DOI] [PubMed] [Google Scholar]
- 3.Organization, W. H . World Health Organization; Geneva: 2005. Prehospital trauma care systems. [Google Scholar]
- 4.Aekka A. Prehospital trauma care education for first responders in India. J Surg Res. 2015;197:331–338. doi: 10.1016/j.jss.2015.03.047. [DOI] [PubMed] [Google Scholar]
- 5.Oliver G.J., Walter D.P., Redmond A.D. Are prehospital deaths from trauma and accidental injury preventable? A direct historical comparison to assess what has changed in two decades. Injury. 2017;48:978–984. doi: 10.1016/j.injury.2017.01.039. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization Noncommunicable diseases (NCD) country profiles-Rwanda. 2018. https://www.who.int/nmh/countries/rwa_en.pdf
- 7.Kim W.C. Vital statistics: estimating injury mortality in Kigali, Rwanda. World J Surg. 2016;40:6–13. doi: 10.1007/s00268-015-3258-3. [DOI] [PubMed] [Google Scholar]
- 8.Scott J.W. Improving prehospital trauma care in Rwanda through continuous quality improvement: an interrupted time series analysis. Injury. 2017;48:1376–1381. doi: 10.1016/j.injury.2017.03.050. [DOI] [PubMed] [Google Scholar]
- 9.Mbanjumucyo G. Epidemiology of injuries and outcomes among trauma patients receiving prehospital care at a tertiary teaching hospital in Kigali, Rwanda. Afr J Emerg Med. 2016;6:191–197. doi: 10.1016/j.afjem.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Enumah S. Rwanda’s model prehospital emergency care service: a two-year review of patient demographics and injury patterns in Kigali. Prehosp Disaster Med. 2016;31:614–620. doi: 10.1017/S1049023X16000807. [DOI] [PubMed] [Google Scholar]
- 11.Petroze R.T. Can focused trauma education initiatives reduce mortality or improve resource utilization in a low-resource setting? World J Surg. 2015;39:926–933. doi: 10.1007/s00268-014-2899-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peter N.A. Delivering a sustainable trauma management training programme tailored for low-resource settings in East, Central and Southern African countries using a cascading course model. Injury. 2016;47:1128–1134. doi: 10.1016/j.injury.2015.11.042. [DOI] [PubMed] [Google Scholar]
- 13.Mock C., Lormand J.D., Goosen J. 2004. Guidelines for essential trauma care. [Google Scholar]
- 14.Mass casualty incident management – emergency medical services. http://www.vdh.virginia.gov/emergency-medical-services/emergency-operations-2/mass-casualty-incident-management/
- 15.American Academy of Orthopaedic Surgeons, Schottke D. Jones & Bartlett Learning; 2016. Emergency medical responder: your first response in emergency care. [Google Scholar]
- 16.Holbery N., Newcombe P. Wiley-Blackwell; 2016. Emergency nursing at a glance (at a glance (nursing and healthcare)) [Google Scholar]
- 17.National Association of EMS Educators . Cengage Learning; 2012. Foundations of education: an EMS approach. [Google Scholar]
- 18.Kobusingye Olive C., Hyder Adnan A., Bishai David. Emergency medical services. In: Jamison Dean T., Breman Joel G., Measham Anthony R., Alleyne George, Claeson Mariam, Evans David B., editors. Disease control priorities in developing countries. 2nd ed. Oxford University Press; 2006. pp. 1261–1279. [Google Scholar]
- 19.Georgiou A., Lockey D.J. The performance and assessment of hospital trauma teams. Scand J Trauma Resusc Emerg Med. 2010;18:66. doi: 10.1186/1757-7241-18-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vyas D. Prehospital care training in a rapidly developing economy: a multi-institutional study. J Surg Res. 2016;203:22–27. doi: 10.1016/j.jss.2016.03.026. [DOI] [PubMed] [Google Scholar]
- 21.Walker R.J., Campbell J.A., Egede L.E. Effective strategies for global health research, training and clinical care: a narrative review. Glob J Health Sci. 2014;7:119–139. doi: 10.5539/gjhs.v7n2p119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jayaraman S. Current patterns of prehospital trauma care in Kampala, Uganda and the feasibility of a lay-first-responder training program. World J Surg. 2009;33:2512–2521. doi: 10.1007/s00268-009-0180-6. [DOI] [PubMed] [Google Scholar]
- 23.Delaney P.G., Bamuleke R., Lee Y.J. Lay first responder training in eastern Uganda: leveraging transportation infrastructure to build an effective prehospital emergency care training program. World J Surg. 2018;42:2293–2302. doi: 10.1007/s00268-018-4467-3. [DOI] [PubMed] [Google Scholar]
- 24.Chokotho L. First responders and prehospital care for road traffic injuries in Malawi. Prehosp Disaster Med. 2017;32:14–19. doi: 10.1017/S1049023X16001175. [DOI] [PubMed] [Google Scholar]
- 25.Kosoko A.A. Evaluating a novel simulation course for prehospital provider resuscitation training in Botswana. West J Emerg Med. 2019;20:731–739. doi: 10.5811/westjem.2019.6.41639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shreeve M.W. Beyond the didactic classroom: educational models to encourage active student involvement in learning. J Chiropr Educ. 2008;22:23–28. doi: 10.7899/1042-5055-22.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor D.C.M., Hamdy H. Adult learning theories: implications for learning and teaching in medical education: AMEE Guide No. 83. Med Teach. 2013;35:e1561–e1572. doi: 10.3109/0142159X.2013.828153. [DOI] [PubMed] [Google Scholar]